Abstract
Simple Summary
Oesophagogastric cancer is the fifth most common cancer worldwide, with poor survival outcomes. Emerging data suggest that bacteria specific to cancer may play a role in earlier disease detection and treatment strategies. This study aimed to evaluate all microbiome studies identifying bacteria enriched in oesophagogastric cancer and appraisal of the methods. Eighty-nine studies demonstrated an enrichment of five bacteria in gastric cancer (Lactobacillus, Streptococcus, Prevotella, Fusobacterium, Veillonella) and three bacteria in oesophageal squamous cell carcinoma (Streptococcus, Prevotella, Fusobacterium). No differences were observed in oesophageal adenocarcinoma. Functional analysis supports the role of immune cells, localised inflammation and cancer-specific pathways in cancer progression. There is evidence that batch effects and contamination in sample analysis are poorly reported. The STORMS checklist provides a framework for high-quality microbiome studies. Whole-genome sequencing is recommended to provide key metabolic and functional pathway analysis of potentially important bacteria influencing cancer progression.
Abstract
Objective. Oesophagogastric cancer is the fifth most common cancer worldwide, with poor survival outcomes. The role of bacteria in the pathogenesis of oesophagogastric cancer remains poorly understood. Design. A systematic search identified studies assessing the oesophagogastric cancer microbiome. The primary outcome was to identify bacterial enrichment specific to oesophagogastric cancer. Secondary outcomes included appraisal of the methodology, diagnostic performance of cancer bacteria and the relationship between oral and tissue microbiome. Results. A total of 9295 articles were identified, and 87 studies were selected for analysis. Five genera were enriched in gastric cancer: Lactobacillus, Streptococcus, Prevotella, Fusobacterium and Veillonella. No clear trends were observed in oesophageal adenocarcinoma. Streptococcus, Prevotella and Fusobacterium were abundant in oesophageal squamous cell carcinoma. Functional analysis supports the role of immune cells, localised inflammation and cancer-specific pathways mediating carcinogenesis. STORMS reporting assessment identified experimental deficiencies, considering batch effects and sources of contamination prevalent in low-biomass samples. Conclusions. Functional analysis of cancer pathways can infer tumorigenesis within the cancer–microbe–immune axis. There is evidence that study design, experimental protocols and analytical techniques could be improved to achieve more accurate and representative results. Whole-genome sequencing is recommended to identify key metabolic and functional capabilities of candidate bacteria biomarkers.
Keywords: oesophageal cancer, gastric cancer, adenocarcinoma, squamous cell carcinoma, microbiome, diagnosis, metagenomics, biomarkers
1. Introduction
Worldwide, oesophagogastric cancer is the fifth most common cancer, with over 1.5 million new cases and over 1.3 million associated deaths annually [1]. Prognosis remains poor despite advances in oncological and surgical treatment, which is primarily due to delayed diagnosis. Recent interest in the role of the tumour-associated microbiome in oesophagogastric cancer pathogenesis may offer an opportunity for new advancements in diagnostics, therapeutics and prognostication.
Previous studies have identified characteristic bacterial phenotypes related to intestinal cancers, including oesophageal, gastric and colorectal cancer [2,3]. Concurrent studies also found that the oral microbiome of gastric, colorectal, pancreatic and lung cancer patients was unique, offering a potentially non-invasive diagnostic window into the digestive tract [2,3,4,5]. In recent years, the emerging link between the gut microbiome and immunotherapy has provided a platform for potential treatment prediction. A less diverse gut microbiome following anti-PD-L1 immunotherapy plus chemotherapy in oesophageal squamous cell carcinomas may predict treatment responders [6]. Similarly, the gut microbiome has been shown to influence the therapeutic effect of anti-PD-L1 immunotherapy in colorectal cancer by modulating tumour-specific T-cells, and it plays a critical role in facilitating immunotherapy treatment in hepatocellular carcinoma, lung cancer and renal cell carcinoma [7,8,9,10]. In addition, microbial variance in pre-operative saliva samples predicted anastomotic leak and pneumonia following oesophagectomy [11,12].
Despite this interest, the microbiome of the upper gastrointestinal tract remains poorly understood compared to that of the colon and rectum [13,14]. This may be due in part to the presumed paucity of bacteria within the oesophagus and stomach and uncertainty as to their clinical significance. A notable exception is Helicobacter pylori and its established role in the pathogenesis of gastritis and gastric cancer [15]. Advances in sequencing techniques have led to a better understanding of microbial communities within the intestinal tract. Several disease processes within the gut have been shown to be associated with reduced microbial diversity and a change in bacterial composition [16,17,18]. It remains unclear whether this change is the cause or effect of a disease process.
2. Methods
2.1. Search Strategy
A systematic search was performed using the MEDLINE (OvidSP), EMBASE (OvidSP) and Cochrane databases to identify potentially relevant articles published between 1966 to 11 August 2022. A search strategy was formed with keywords and MeSH headings relating to “oesophageal cancer”, “gastric cancer” and “microbiome” used in combination with the Boolean operators AND and OR. Other databases, including the World Health Organisation International Clinical Trials Registry, ClinicalTrials.gov, ISRCTN Register and PROSPERO, were reviewed to identify ongoing studies.
2.2. Eligibility Assessment and Data Extraction
Studies that reported any aspect of the microbiome in patients with oesophagogastric cancer were selected from the electronic search results. Specific inclusion criteria were studies reporting named bacteria identified in patients with oesophageal and gastric cancer (any histological type) and compared to an appropriate control group of healthy subjects or patients with benign conditions of the upper gastrointestinal tract. All bio-sample types and methods for bacterial identification were included. Review articles, case reports, editorials, opinions, conference abstracts and articles not written in the English language were excluded. Two independent reviewers (BV, MT) screened all titles and abstracts to identify relevant articles for full-text review. A third reviewer (PRB) resolved any disagreements in article selection. Reference lists of all selected articles were also searched to identify additional relevant articles.
Data extraction from full-text review included: study design, cohort demographics, specimen type, microbiome assessment method, diversity characteristics (including α- and β diversity metrics) and bacteria identified at all taxonomic levels with p-values < 0.05.
2.3. Definitions of Groups
Subjects were classified into three groups: (i) patients with histologically proven oesophageal and gastric cancer; (ii) benign disease of the upper gastrointestinal tract, including superficial gastritis, atrophic gastritis; and (iii) healthy controls with no known pathology of the upper gastrointestinal tract. Premalignant conditions such as Barrett’s oesophagus, gastric intestinal metaplasia or any form of dysplasia were not included in the analysis.
2.4. Outcomes
The primary outcome was to identify bacterial enrichment specific to oesophagogastric cancer in comparison to a relevant control group. All bacteria identified were recorded, focusing on those reported in five or more studies. Other microorganisms such as fungi, viruses and protozoa were not recorded. Secondary outcomes included: investigating the relationship between the oral and cancer tissue microbiome; assessing the diagnostic performance of the cancer-associated microbiome; describing the microbial diversity and methodology appraisal.
2.5. Quality Assessment
The Newcastle-Ottawa Scale was used to assess the quality and risk of bias for case-control and cohort studies. Two independent researchers (MT, BV) graded the studies across three domains: selection of the study groups (adequacy of case definition, representativeness of the cases, selection of controls, definition of controls), comparability of the groups (based on design and accountability of confounding factors) and outcome of the studies (exposure, assessment methods, follow-up).
Studies were also evaluated using the Strengthening The Organisation and Reporting of Microbiome Studies (STORMS) checklist, recently developed for reporting on the quality of human microbiome studies [19]. It comprises a comprehensive structured 17-item checklist intended to standardise reporting of important quality and methodology parameters.
3. Results
3.1. Study Selection
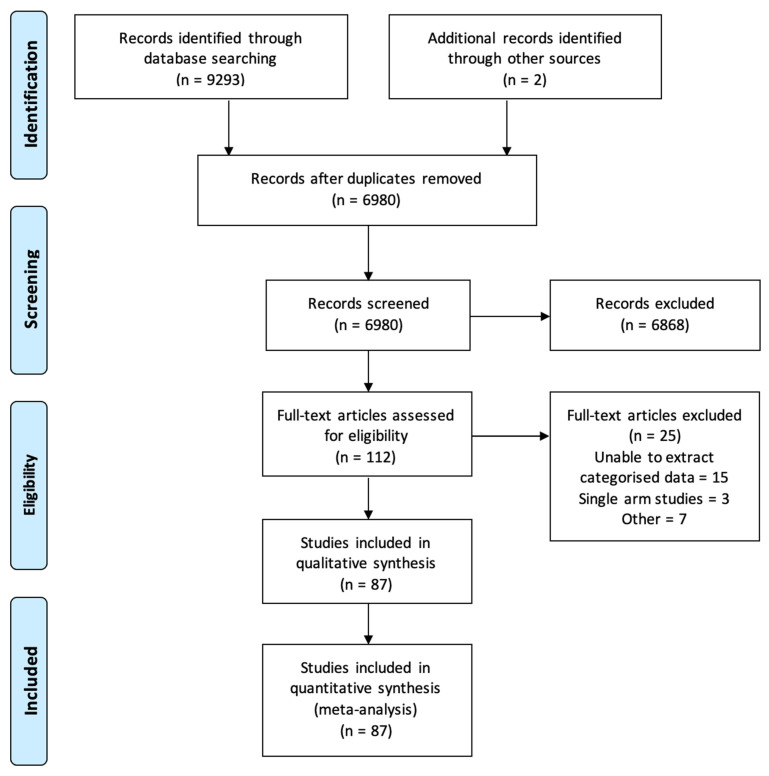
A total of 9295 articles were identified from the online literature search. A total of 112 studies were selected for full-text review, of which 25 were excluded, as they were either a single-arm study (without control group), or they did not report relevant information (e.g., named bacteria). Final analysis included 87 studies: 56 studies assessing gastric adenocarcinoma [3,16,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48] and 42 studies assessing oesophageal carcinoma (adenocarcinoma and/or squamous cell carcinoma) [12,35,38,49,50,51,52,53,54,55,56,57,58,59,60,61,62] (Figure 1). Two studies reported data from both oesophageal and gastric cancers [35,38].
Figure 1.
Flow chart demonstrating article selection.
3.2. Gastric Adenocarcinoma
Study characteristics: Fifty-six studies included analysis of 4545 patients with either: gastric adenocarcinoma (n = 4346); benign disease (n = 1364); or a healthy upper gastrointestinal tract (n = 2394) (Table 1; detailed study characteristics are provided in Table S1). The majority of studies were conducted in Asian populations (n = 46, 82%). Four studies were performed retrospectively from registered databases [22,63,64,65]. The majority of studies were prospective case-control studies, where the control group comprised either unrelated healthy (non-cancer) patients or healthy tissues samples (adjacent to the tumour) acquired from cancer patients.
Table 1.
Study characteristics of articles reporting on the microbiome of gastric adenocarcinoma compared to a non-cancer group.
| Author | Year | Country | Specimen Type | Microbiome Assessment Method |
NAT | PPI | Abx | Ref. |
|---|---|---|---|---|---|---|---|---|
| Sjostedt | 1985 | Sweden | Saliva, OG fluid | Culture | - | No | No | [20] |
| Dicksved | 2009 | Sweden | Tissue | T-RFLP | - | - | No | [21] |
| Seo | 2014 | Korea | Tissue | RNA seq database | - | - | - | [22] |
| Aviles-Jimenez | 2014 | Mexico City | Tissue | 16S, microarray hybridization | - | No | No | [23] |
| Eun | 2014 | Korea | Tissue | 16S V5, pyroseq | - | No | No | [24] |
| Hu | 2015 | China | Tongue coating | 16S V2-4, Illumina seq | No | - | No | [25] |
| Wang | 2016 | China | Tissue | 16S V1-3, pyrosequencing | - | No | No | [26] |
| Yu | 2017 | China/Mexico | Tissue | 16S V3-4, MiSeq | No | - | - | [27] |
| Li | 2017 | Hong Kong | Tissue | 16S V3-4, Solexa Illumina seq | - | No | No | [28] |
| Castano-Rodriguez | 2017 | Malaysia | Tissue | 16S, MiSeq | No | No | No | [29] |
| Ferreira | 2018 | Portugal | Tissue | 16S V5-6, NGS | - | No | No | [30] |
| Sun | 2018 | China | Saliva, SP | 16S, MiSeq | - | - | No | [3] |
| Hu | 2018 | China | Gastric fluid | Shotgun, HiSeq | No | No | No | [31] |
| Wu | 2018 | China | Tongue coating | 16S V4, pyrosequencing | No | No | No | [32] |
| Hsieh | 2018 | Taiwan | Tissue | 16S V3-4, MiSeq | - | - | - | [33] |
| Coker | 2018 | China | Tissue | 16S V4, N-W algorithm | No | No | No | [34] |
| Shao | 2019 | China | Tissue | 16S V4 + miniseq | - | - | - | [35] |
| Gunathilake | 2019 | South Korea | Tissue | 16S V3-4 + MiSeq | - | - | - | [36] |
| Liang | 2019 | China | Faeces | 16S +MiSeq | No | No | No | [37] |
| Kageyama | 2019 | Japan | Saliva | 16S V1-2 + Ion PGM Hi-Q Seq | No | - | No | [38] |
| Chen | 2019 | China | Tissue | 16S V4-5 HiSeq | No | No | No | [39] |
| Dong | 2019 | China | Serum | 16S V1-2 HiSeq | - | No | No | [40] |
| Liu | 2019 | China | Tissue | 16S V3-4 MiSeq | No | No | No | [16] |
| Qi | 2019 | China | Faeces | 16S V3-4 MiSeq | No | - | No | [41] |
| Wang | 2020 | China | Tissue | 16S V4 MiSeq | No | No | No | [42] |
| Wang | 2020 | China | Tissue | 16S V3-4 HiSeq | - | No | No | [43] |
| Spiegelhauer | 2020 | Denmark | Tissue | Culture + 16S V3-4 HiSeq | No | No | No | [44] |
| Gantuya | 2020 | Mongolia | Tissue | 16S V3-4 + MiSeq | - | No | No | [45] |
| Wu | 2020 | China | Tissue | 16S + HiSeq | No | No | No | [46] |
| Xu | 2020 | China | Tongue coating | 16S V3-4 + MiSeq | No | No | No | [47] |
| Dang | 2020 | China | Tissue | 16S V3-4 + MiSeq | - | - | - | [48] |
| Park | 2021 | Korea | Faeces, serum, urine | 16S V3-4 + MiSeq | No | No | No | [66] |
| Pimenetel-Nunes | 2021 | Portugal | Tissue | 16S V1-8 | - | No | - | [67] |
| Yu | 2021 | China | Faeces | 16S V3-4 + TruSeq nano | No | - | No | [63] |
| Yang | 2021 | USA | Buccal | Shotgun | - | - | No | [68] |
| Dai | 2021 | China | Tissue | 16S V3-4 + Ion plus fragment | - | - | - | [69] |
| Li | 2021 | China | Tissue | 16S V3-4 + MiSeq | - | No | No | [70] |
| Gunathilake | 2021 | Korea | Tissue | 16S V4 + MiSeq | - | - | - | [71] |
| Huang | 2021 | China | Saliva | 16S V3-4 + MiSeq | No | No | No | [72] |
| Oliveira | 2021 | North Brazil | Saliva, dental plaque | qPCR | No | - | No | [73] |
| Sarhadi | 2021 | Finland | Faeces | 16S V2-4, V6-9 + Ion Chip | No | - | No | [74] |
| Zhang | 2021 | China | Tissue | 16S V3-4 + MiSeq | - | - | - | [75] |
| Liu | 2021 | China | Faeces | 16S V3-4 + 454 GS-FLX | - | - | - | [76] |
| Zhang Y | 2021 | China | Faeces | 16S V4 + HiSeq | No | No | No | [77] |
| Abate | 2022 | FFPE tissue | MSKCC and TCGA | - | - | - | [64] | |
| Liu | 2022 | China | Tissue | 10 public datasets 16S | - | No | No | [65] |
| Zhang C | 2022 | China | Faeces, tissue, oral mucosal | 16S V4 + Novoseq/MiSeq | No | - | No | [78] |
| He | 2022 | China | Tissue, gastric juice | 16S V4 + MiSeq | - | No | No | [79] |
| Ding | 2022 | China | Faeces, gastric juice | 16S V4 + NovoSeq | - | - | No | [80] |
| Park | 2022 | China | Gastric juice | 16S V3-4 + MiSeq | - | - | No | [81] |
| Zhou | 2022 | China | Tissue, faeces | 16S V3-4 + MiSeq | No | No | No | [82] |
| Sun | 2022 | China | Tissue | 16S V3-4 | No | No | No | [83] |
| Png | 2022 | Singapore | Tissue | 16S V3-4 + MiSeq | - | - | - | [84] |
| Shu | 2022 | China | Saliva | 16S V3-4 + Ion S5TM XL | No | - | No | [85] |
| Zhang Z | 2022 | China | Faecal | 16S V3-4 + MiSeq | No | No | No | [86] |
| Shi | 2022 | China | Tissue | 16S V3-4 + MiSeq | No | - | No | [87] |
OG, oesophagogastric. SP, subgingival plaque. B, benign. HC, healthy control. AHT, adjacent healthy tissue. 16S, 16S rRNA. N-W, Needleman–Wunsch. NAT, neoadjuvant therapy. PPI, proton pump inhibitor therapy. Abx, antibiotic therapy. Y, yes. N, no.
Sample type: Microbial assessment was performed in various biological matrices, including upper gastrointestinal tract tissue (n = 34, 61%); faeces (n = 11, 19%); oral samples (saliva, n = 6, 10%; tongue coating, n = 3, 5%; plaque, n = 2, 3%); gastric/oesophageal fluid (n = 5, 9%); serum (n = 2, 3%); and urine (n = 1, 2%).
Method for bacterial identification: Significant heterogeneity was observed in the sequencing technique used to examine the microbiome. The majority of studies (n = 48, 86%) used 16S rRNA gene sequencing predominantly targeting the V3-4 hypervariable region. Four studies that utilised 16S rRNA gene sequencing did not specify which variable region was targeted [22,23,29,37,46]. Two studies employed primary bacterial culture from acquired tissue samples with subsequent 16S rRNA V3-4 sequencing [12,20], and two studies utilised shotgun sequencing and terminal restriction fragment length polymorphism [21,31]. Public datasets including The Cancer Genome Atlas and Memorial Sloan Kettering Cancer Center have been used to pool samples for big dataset analysis.
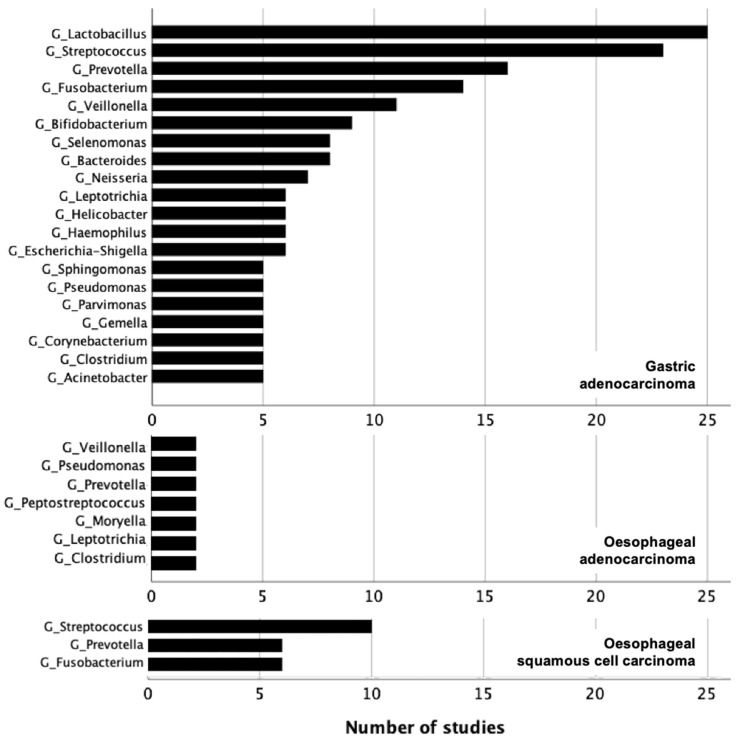
Bacteria enriched in gastric adenocarcinoma: Taxonomic classifications to the genus level were reported by the majority of studies. A total of 352 bacteria were enriched in gastric cancer at the following levels: 18 phyla, 15 classes, 31 orders, 50 families, 149 genera, 87 species and 2 strains. Bacteria that were reported by ten or more studies (36/357, including all taxonomic levels) are shown in Figure 2. Full details of bacteria identified in association with gastric adenocarcinoma are provided in Supplementary Table S2.
Figure 2.
Bacteria enriched in oesophagogastric carcinoma across all included 89 studies. G = genus.
All five genera observed to be enriched in gastric adenocarcinoma belonged to the three predominant phyla: Lactobacillus (Phyla: Firmicutes) was reported in 25 studies (45%) in multiple biological matrices: tumour tissue (n = 16), faeces (n = 5), gastric/oesophageal fluid (n = 3), tongue coating (n = 1). Streptococcus (Phyla: Firmicutes) was identified in 23 studies (41%): tumour tissue (n = 13), faeces (n = 8), gastric/oesophageal fluid (n = 2), tongue coating (n = 1), saliva (n = 1). Prevotella (Phyla: Bacteroidetes) was present in 16 studies (29%): tumour tissue (n = 13), faeces (n = 2), saliva (n = 1). Fusobacterium (Phyla: Fusobacteria) was reported in 14 studies (25%), including tumour tissue (n = 10), faeces (n = 2), gastric/oesophageal fluid (n = 1) and urine (n = 1). Veillonella (Phyla: Firmicutes) was found in 11 studies (20%) and was reported in various biological matrices, including tumour tissue (n = 5), faeces (n = 3), gastric/oesophageal fluid (n = 2) and subgingival plaque (n = 1).
Bacteria enriched in benign gastric conditions: The benign group demonstrated an enrichment of 218 bacteria reported at the following levels: 12 phyla, 12 classes, 20 orders, 30 families, 93 genera, 47 species and 4 strains. No bacteria were reported in more than 10 studies.
Bacteria enriched in healthy control group: The healthy control group showed enrichment of 129 bacteria reported at the following levels: 13 phyla, 3 classes, 5 orders, 13 families, 62 genera and 33 species. No bacteria were reported in more than 10 studies.
Microbial diversity metrics: 51 studies (91%) assessed microbial diversity. The majority of studies employed more than one metric. Alpha diversity, a measure of the number (richness) of species within a sample and the distribution of abundances of the individual species (evenness), was reported in 50 studies (89%). Richness and evenness indices reported included: the Shannon index (n = 46); Chao1 (n = 28); OTUs (n = 21); the Simpson Index (n = 17); ACE (n = 9); the Phylogenetic Diversity tree (n = 9). All alpha diversity metrics reported different outcomes with either an increase, decrease or no change in the species richness. Overall, 13 studies demonstrated an increase in alpha diversity, 11 studies reported a decrease, 13 studies showed no difference, and 15 studies reported at least two opposing changes. Beta diversity, a measure of the species diversity between two communities or ecosystems, was measured in 42 studies (75%); principal coordinate analysis was used in 36 studies, weighted and unweighted UniFrac distance was employed in 23 studies, and Bray Curtis in 21 studies. Twenty-eight studies reported a significant difference between cancer and benign/control samples. Ten studies showed no significant difference, and two studies reported conflicting outcomes. Evaluation of diversity metrics has shown conflicting results for alpha diversity but trends towards a significant difference in beta diversity between cancer and non-cancer samples.
3.3. Oesophageal Adenocarcinoma
Study characteristics: Fourteen studies included the analysis of the oesophageal adenocarcinoma microbiome, including one combined SCC/OAC group (Table 2; detailed study characteristics are provided in Table S1). A total of 1223 patients were included in the analysis: 623 OAC (51%); 532 healthy controls (43%); and 68 with benign disease (6%). Half of the studies originated from Asian populations. All studies, except one, were prospective case-control studies.
Table 2.
Study characteristics of articles reporting on the microbiome of oesophageal adenocarcinoma compared to a non-cancer group.
| Author | Year | Country | Specimen Type | Microbiome Assessment Method |
NAT | PPI | Abx | Ref. |
|---|---|---|---|---|---|---|---|---|
| Yamamura | 2016 | Japan | Tissue | qPCR | No | - | No | [51] |
| Elliott | 2017 | UK | Tissue | 16S V1-2 + MiSeq | Mixed | - | - | [52] |
| Peters | 2017 | USA | Mouthwash | 16S V4 + MiSeq | - | - | - | [53] |
| Kageyama | 2019 | Japan | Saliva | 16S V1-2 + Ion PGM Hi-Q Seq | No | - | No | [38] |
| Yuda | 2020 | Japan | Saliva | Culture | Mixed | - | No | [12] |
| Peter | 2020 | USA | Tissue | 16S V4 + Miseq | - | Mixed | No | [57] |
| Li | 2020 | China | Tissue | 16S V3-4 + Miseq | No | - | No | [58] |
| Zhou | 2020 | Australia | Tissue | 16S V1-3 + Miseq | No | - | No | [60] |
| Lopetsu | 2020 | Italy | Tissue | 16S V3-4 + Miseq | No | N | No | [61] |
| Kawasaki | 2020 | Japan | Subgingival plaque | RT-PCR | No | - | No | [62] |
| Ishaq | 2021 | China | Faeces | 16S V3-4 + Hiseq, qPCR | - | - | No | [88] |
| Wang | 2021 | - | Tissue | TCMA database | - | - | - | [89] |
| Deng | 2021 | China | Faeces | 16S V4 + Miseq | No | No | No | [90] |
| Hao | 2022 | USA | Tissue, oral mucosal | - | - | - | No | [91] |
16S, 16S rRNA. NAT, neoadjuvant therapy. PPI, proton pump inhibitor therapy. Abx, antibiotic therapy. Y, yes. N, no.
Sample type: Primary sites for sample collection were from the upper gastrointestinal tract and the oral cavity. Tissue biopsy (n = 8), saliva (n = 3) and faecal (n = 2) samples were the most common, with a single study using mouthwash samples.
Method for bacterial identification: Nine of the fourteen studies identified bacteria by 16S rRNA sequencing with different targeted variable regions, V3-4 being the most common (n = 7). Other methods employed were q-PCR, RT-PCR and bacteria culture methods.
Bacteria enriched in oesophageal carcinoma: No common trend was observed at any taxonomic level for studies that evaluated bacteria related to oesophageal adenocarcinoma. A maximum of two studies shared similar bacterial identification. With relative paucity in data related to oesophageal adenocarcinoma, robust conclusions could not be drawn.
3.4. Oesophageal Squamous Cell Carcinoma
Study characteristics: Twenty-eight studies included the analysis of the oesophageal squamous cell carcinoma, with one combining SCC/OAC samples (Table 3; detailed study characteristics are provided in Table S1). A total of 3262 patients were included in the analysis: 2346 patients with SCC (72%); 884 healthy controls (27%); and 32 with benign disease (1%). Twenty-four of the twenty-eight studies originated from Asian populations. Three studies were retrospective in nature, evaluating publicly available datasets. The remainder of the studies were prospective case-control design.
Table 3.
Study characteristics of articles reporting on the microbiome of oesophageal squamous cell carcinoma compared to a non-cancer group.
| Author | Year | Country | Specimen Type | Microbiome Assessment Method |
NAT | PPI | Abx | Ref. |
|---|---|---|---|---|---|---|---|---|
| Chen | 2015 | China | Saliva | 16S V3-4 + pyrosequencing | No | - | No | [49] |
| Nasrollahzadeh | 2015 | Iran | Tissue | 16S V3-4 + GS-FLX | - | - | - | [50] |
| Yamamura | 2016 | Japan | Tissue | qPCR | No | - | No | [51] |
| Shao | 2019 | China | Tissue | 16S V4 + miniSeq | - | - | - | [35] |
| Kageyama | 2019 | Japan | Saliva | 16S V1-2 + Ion PGM Hi-Q Seq | No | - | No | [38] |
| Wang | 2019 | China | Saliva | 16S V3-4 + MiSeq | No | - | No | [54] |
| Yamamura | 2019 | Japan | Tissue | qPCR | Mixed | - | - | [55] |
| Xu | 2020 | China | Oral mucosal swab | 16S V3-4 + Ion S5 TM XL | Yes | - | No | [56] |
| Yuda | 2020 | Japan | Saliva | Culture | Mixed | - | No | [12] |
| Li | 2020 | China | Tissue | 16S V3-4 + Miseq | No | - | No | [58] |
| Zhao | 2020 | China | Saliva | 16S V3-4 + Miseq | No | - | No | [59] |
| Kawasaki | 2020 | Japan | Subgingival plaque | RT-PCR | No | - | No | [62] |
| Li Z | 2021 | China | Tissue | 16S V3-4 + Miseq, qPCR | - | - | - | [92] |
| Li Z | 2021 | China | Saliva, tissue | 16S V4 + Ion S5TM XL | - | No | No | [93] |
| Wei | 2021 | China | Saliva | 16S V4 + Hiseq | - | No | No | [94] |
| Ishaq | 2021 | China | Faeces | 16S V3-4 + Hiseq, qPCR | - | - | No | [88] |
| Jiang | 2021 | China | Tissue | 16S V3-4 | No | No | No | [95] |
| Wang | 2021 | - | Tissue | TCMA database | - | - | - | [89] |
| Shen | 2021 | China | Tissue | 16S + qPCR | - | - | - | [96] |
| Chen | 2021 | China | Oral mucosal swab | 16S V3-4 | - | - | - | [97] |
| Kovaleva | 2021 | Russia | FFPE tissue | 16S V3-4 + qPCR | - | - | - | [98] |
| Yang | 2021 | China | Tissue | 16S V4 | - | No | No | [99] |
| Deng | 2021 | China | Faeces | 16S V4 + Miseq | No | No | No | [90] |
| Cheung | 2022 | Hong Kong | Faeces | 16S V4 + Miseq | No | No | No | [100] |
| Wu | 2022 | China | Faeces | - | No | No | No | [101] |
| Lin | 2022 | China | Tissue | 16S V3-4 + Hiseq | No | No | No | [102] |
| Shen | 2022 | China | Tissue | 16S V1-9 + Miseq | No | - | - | [103] |
FFPE, formalin-fixed paraffin-embedded. 16S, 16S rRNA. NAT, neoadjuvant therapy. PPI, proton pump inhibitor therapy. Abx, antibiotic therapy. Y, yes. N, no.
Sample type: Primary sites for sample collection were from the upper gastrointestinal tract, tissue biopsy (n = 14), and the oral cavity, saliva (n = 8). Other bio-sample included, faecal samples (n = 4).
Method for bacterial identification: Twenty-two of the twenty-eight studies identified bacteria by 16S rRNA sequencing with different targeted variable regions, V3-4 being the most common (n = 19). Other methods employed were q-PCR, RT-PCR and bacteria culture methods.
Bacteria enriched in oesophageal squamous cell carcinoma: A total of 146 oesophageal SCC specific taxa were reported: 7 phyla, 5 classes, 10 orders, 19 families, 74 genera and 31 species. Full details of bacteria identified in association with oesophageal SCC are provided in Supplementary Table S2. Three bacterial genera were identified in six or more studies, demonstrating an enrichment of Streptococcus (n = 10 studies) [49,56,58], Fusobacteria and Prevotella in tissue and saliva samples [49,56,59]. No significant abundances were identified in the comparison groups.
4. Evaluation of Diagnostic Performance
The diagnostic performance of the microbiome was assessed by Sun et al., who reported a 97% sensitivity of saliva and subgingival plaque for gastric cancer screening [3]. No other clinically relevant applications of the microbiome were determined from studies presented herein.
5. Influence of Sample Origin
There was insufficient data to compare the relationship between the tumour tissue and oral microbiome of patients with oesophagogastric cancer. However, three studies showed a similarity in bacterial abundance across the orodigestive tract. Li et al. demonstrated common biomarkers, Bosea, Solobacterium, Gemella and Peptostreptococcus, in saliva and cell brush tissue in oesophageal squamous cell carcinoma patients [93]. Hao et al. identified a depletion of Streptococcus and an enrichment of Veillonella, alongside several other bacteria in the oesophageal adenocarcinoma saliva and tissue specimens [91]. Similarly, Zhang et al. supported the notion that the oral and tissue microbiome have a similar shared network [78].
6. Quality of Assessment
The Newcastle Ottawa Scale for case-control and cohort studies assessed the quality of reporting [104]. A total of 41 (47%) studies scored the maximum of nine stars; Ten studies 11%) scored eight stars, and 35 (40%) scored seven stars. All studies reported patient selection representative of the community population, apart from one study that enrolled hospitalized patients. Microbiome results were reported accurately in accordance with the outcome measures. Although age and gender were provided for all groups, comparability between groups, including statistical analysis of baseline characteristics, were poorly reported. No study scored less than six, suggesting overall good study design, assessment and reporting of primary outcomes.
The STORMS checklist demonstrated clear reporting of the rationale of the study (100%), detailed sample collection (91%), DNA extraction strategies (87%) and storage (61%). Few studies used positive controls (mock communities, 4%), discussed batch effects (10%) or reported contamination within DNA extraction kits/reagents, which are prevalent in low biomass samples (21%). Important microbial influencing factors such as antibiotic use (61%) and matching criteria (35%) were not reported in all studies as potential confounding factors. Although it is strongly encouraged to deposit sequence reads in an established publicly available repository such as NCBI, this was done in only 44% of studies. Full details of quality assessment scoring are provided in Supplementary Tables S3 and S4.
7. Discussion
This systematic review summarises the current published literature concerning the association between the microbiome and oesophagogastric cancer. The principal findings were: (i) the enrichment of select bacteria in gastric adenocarcinoma compared to benign disease and healthy controls, with distinctive bacterial profiles observed at all taxonomic levels; (ii) enrichment of the genera Lactobacillus and Streptococcus in gastric adenocarcinoma; (iii) higher abundances of Firmicutes in various bio-samples including tumour tissue, saliva and gastric fluid; and (iv) significant methodological heterogeneity in standards of reporting.
The microbiome has received increasing attention for its potential role in disease pathogenesis, including carcinogenesis within the gastrointestinal tract [42]. As such, intestinal bacteria may have a role in early cancer detection [3,4] and, with advancements in immunotherapy, in personalised therapeutics [7]. Early detection by profiling the salivary microbiome has been reviewed by Muszyński et al., demonstrating a distinct alteration in cancer compared to healthy controls. However, a link between the salivary and tumour microbiome is yet to be established [105]. There is also evidence suggesting the microbiome can provide prognostic information, related to a post-operative change in the microbiome linked with complications and survival [12,51,106]. Compared to the lower gastrointestinal tract, characterisation of the upper gastrointestinal microbiome remains, however, in a very preliminary stage.
Enrichment of the genera Lactobacillus and Streptococcus were common findings in 34 studies (61%) evaluating gastric adenocarcinoma. Although this review supports an important alteration in species composition, there is disagreement between species diversity. Most studies used more than one alpha diversity metric, producing conflicting results. Although it is becoming increasingly evident that microbial alteration in disease is important, assessment of the functional capabilities is deemed to provide more valuable information. The functional ecology describes the active contribution of microbes to a system but may not reflect the species composition. Species may be present; however, they can be functionally redundant.
In recent years, metagenomic analysis has transformed the understanding of cancer pathogenesis within the cancer–microbe–immune axis. PD-L1, expressed in half of all gastric cancers, are potentially responsible for suppressing killer T cells and activating regulatory T cells to promote carcinogenesis. In this setting, bacteria-enriched cancer pathways and their associated metabolites may be critical in directing tumour immunity to induce carcinogenesis [107]. Hu et al. described cancer-specific metabolites generated from pathways related to amino acid metabolism (L-arginine, L-ornithine) and the pentose phosphate pathways in gastric cancer compared to superficial gastritis [31]. Functional prediction of the microbiome using software such as PICRUSt, Tax4Fun and KEGG databases have been utilised with 16S rRNA data to explore potential cancer-mediated pathways. Barrett’s oesophagus and oesophageal adenocarcinoma are linked to the nitric oxide pathway in the context that nitrate is reduced by bacterial metabolism in the digestive tract. Downstream metabolites have been associated with oesophagogastric cancer [91]. Genomic analyses have identified the presence of bacterial genes expressing these pathways of interest. Other amino acid metabolic pathways such as cysteine and methionine metabolism have been identified in gastric cancer and shown to play a pivotal role in cancer cell growth [108]. Their end metabolites are responsible for localised inflammation, an important step in the progression to cancer. Several amino acid metabolism pathways evidenced in gastric cancer can be predictive of increased metabolism driven by the gastric microbiome.
Identification of these pathways can lead to better understanding of tumour biology and mechanisms, offering a platform for targeted therapeutics. Microbial functional analysis showed modulation of the tumour microenvironment by inflammation and cell cycle regulation. An increased functional microbial abundance of arachidonic acid, oxidative phosphorylation and the tricarboxylic acid cycle was shown in gastrointestinal cancers [109]. The pro-inflammatory effects of bacteria may be a key mechanism driving the host–microbe interactions to promote carcinogenesis through DNA replication or DNA repair [81]. Park et al. showed the enrichment of cancer pathways linked to DNA replication and mismatch repair, which are crucial to cell growth and survival [81]. Functional pathway analysis may reveal the role of the cancer microbiome in therapeutic monitoring and response.
The role of the microbiome in the pathogenesis of gastric cancer was reported by Wang et al., who identified characteristic bacterial variation that was related to disease progression from chronic gastritis to intestinal metaplasia to gastric cancer [42]. Specifically, Actinobacteria, Bacteroides, Firmicutes and Fusobacteria were enriched in premalignant and cancer states, with candidate OTUs demonstrating an area under the curve >0.9 for gastric cancer detection [42]. Firmicutes were also reported in higher abundances in different biological matrices including the tissue, gastric fluid and saliva of gastric cancer patients. Similarities in bacterial taxa found in different biological samples may support future non-invasive methods for characterising the microbiome in oesophagogastric cancer. Sun et al. reported that saliva and the subgingival plaque microbiome could detect gastric cancer with 97% sensitivity [3].
A limited number of studies with variable methodologies meant that fewer trends were observed in the oesophageal adenocarcinoma microbiome. Of 14 studies, only three studies identified the same seven genera, Veillonella, Pseudomonas, Prevotella, Peprostreptococcus, Moryella, Leptotrichia and Clostridium [58,61,91]. No bacterial changes were consistently observed in more than two studies.
A total of 41 of the 87 studies (47%) identified by this review were published since 2021, highlighting how interest in the upper gastrointestinal cancer microbiome is a relatively recent occurrence. During the emergence of this field, there has been significant heterogeneity between the methodologies used by individual studies. Though 16S rRNA gene sequencing was the most common method for defining the microbiome used in studies identified by this review, there were differences in the variable regions targeted. As different variable regions amplify different bacteria, there is a risk of taxonomic bias. Studies that also included culture methods introduce further selection bias. It is therefore recommended that a standardised methodology for sample acquisition and microbiome assessment, including DNA extraction and sequencing, should be considered. The diversity of methods used may explain the observed variation in results.
Existing checklists for the assessment of study reporting and quality do not encompass specific aspects of study design that are important to human microbiome research. Many checklists, including the Newcastle Ottawa Scale that was used to assess studies included in this review, fail to assess both patient-specific (e.g., diet, co-morbidity, medications) and analytical (e.g., sample handling, analysis and data processing) factors that have the potential to influence findings. Recently, a consortium of researchers have proposed a standardised checklist to improve reporting of human microbiome research [110]. Though the STORMS checklist has not yet been validated, it can serve as a guide to researchers within the field. The checklist comprises key features that are considered to be important in reporting high-quality and reproducible microbiome research. For this reason, the STORMS checklist was selected as the most relevant and accurate representation for quality assessment. For studies included in this review, it highlighted: (i) deficiencies in eliminating sources of contamination by using controls and assessing DNA extraction kits; (ii) the need to control for patient factors influencing the microbiome; and (iii) heterogeneity in laboratory methods used, including target variable regions. Though it is beyond the scope of the current review to establish similar guidance, important considerations for the specific analysis of the upper gastrointestinal microbiome are presented in Table 4 and are intended to serve as a guide to future investigators.
Table 4.
Specific considerations for designing a microbiome assessment study in upper gastrointestinal disease.
| Workflow | Considerations | |
|---|---|---|
| Study design | Prospective case-control | Cross-sectional observational studies to determine microbial–disease associations Longitudinal studies: premalignant conditions to identify causative factors for diagnostic purposes, therapeutic response, prognostication |
| Patient factors influencing the microbiome | Neoadjuvant treatment naive Use of proton pump inhibitors and/or histamine-2 antagonists Use of antibiotics (consider time interval between use and microbiome assessment) Immunosuppressive states Synchronous cancer Smoking status Previous gastrointestinal surgery |
|
| Geographical location | Genetic and lifestyle factors such as diet and exercise | |
| Matching groups | Matched age and gender as a minimum | |
| Sample size calculation | ||
| Sub-group analysis | E.g., tumour stage, ethnicity, geographical location and its association with therapeutic response and prognostication—homogeneity will allow for a more accurate microbiome assessment. | |
| Sampling process | Sample weight | Endoscopic tissue biopsies can be of variable size. Establish a minimum weight of tissue for adequate analysis. |
| Positive control | Consider adjacent healthy tissue. | |
| Negative control | Consider storing an empty tube and/or storage medium at the same time as the sample. | |
| Replicates | (where possible) | |
| Minimise freeze–thaw cycles | ||
| Laboratory techniques | This is comprehensively covered by the STORMS reporting checklist [110]. |
This review suffers from a number of acknowledged limitations. As previously mentioned, wide methodological variation meant that it was not possible to draw robust conclusions from the combined outcomes of selected studies. Over three quarters of included studies recruited less than eighty cancer patients, suggesting that they may have been underpowered to draw definitive conclusions. No study presented a formal sample size calculation. Furthermore, only 31 studies out of 87 (36%) used multiple comparison correction. Studies were predominantly from Far Eastern centres and, as such, have poor external validity; hence, it is uncertain how translatable results may be for patients from other global regions. Microbial profiles are influenced by many environmental factors, and geographical location encompasses many of these. With the recent increase in the incidence of oesophageal adenocarcinoma in Western countries, more studies are encouraged to define the microbial profile in the these populations [111]. A meta-analysis of the datasets of studies identified in this review was not possible due to a lack of publicly deposited datasets and associated metadata. An attempt to retrieve this information from corresponding authors was not successful. Other features of the microbiome, including the virome and the mycobiome, have not been explored, as they remain outside the scope of this work.
In conclusion, the primary limitation in microbiome research of oesophagogastric cancer is the lack of standardisation in study methodology. This heterogeneity limits the comparability of data. As a relatively new field, there is a wide scope to investigate the alterations in the human ecological system to identify cancer-related markers. The causal link between microbiome and disease and the correlative relationship between the oral cavity and the tumour tissue have not been fully explored. The results provide an insight into the importance of investigating the oesophagogastric cancer microbiome and the crucial role it plays in carcinogenesis and personalised therapeutics. Furthermore, understanding the functionality and metabolic capabilities of cancer-specific bacteria with a multi-omics approach could support improved early diagnostics and personalised treatment strategies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers15102668/s1, Table S1: Detailed study characteristics of articles reporting on the microbiome of gastric adenocarcinoma, oesophageal adenocarcinoma and oesophageal squamous cell carcinoma compared to a non-cancer group; Table S2: Full data extraction worksheet from identified studies in this review; Table S3: Detailed Newcastle Ottawa Scale workflow; Table S4: Detailed STORMS checklist workflow.
Author Contributions
Conception: P.R.B. and G.B.H.; Study design/search strategy: M.T. and B.V.; Data acquisition: B.V. and M.T.; Data analysis: B.V.; Interpretation of data: B.V. and M.T.; Writing of the manuscript: B.V. and M.T.; Critical revision of the manuscript: all authors. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding. The APC was funded by Imperial College London.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1. [(accessed on 21 March 2021)]. Available online: https://gco.iarc.fr/today/fact-sheets-cancers.
- 2.Flemer B., Warren R.D., Barrett M.P., Cisek K., Das A., Jeffery I.B., Hurley E., O‘Riordain M., Shanahan F., O’Toole P.W. The oral microbiota in colorectal cancer is distinctive and predictive. Gut. 2018;67:1454–1463. doi: 10.1136/gutjnl-2017-314814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun J., Li X., Yin J., Li Y., Hou B., Zhang Z. A screening method for gastric cancer by oral microbiome detection. Oncol. Rep. 2018;39:2217–2224. doi: 10.3892/or.2018.6286. [DOI] [PubMed] [Google Scholar]
- 4.Fan X., Alekseyenko A.V., Wu J., Peters B.A., Jacobs E.J., Gapstur S.M., Purdue M.P., Abnet C.C., Stolzenberg-Solomon R., Miller G., et al. Human oral microbiome and prospective risk for pancreatic cancer: A population-based nested case-control study. Gut. 2018;67:120–127. doi: 10.1136/gutjnl-2016-312580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hosgood H.D., Cai Q., Hua X., Long J., Shi J., Wan Y., Yang Y., Abnet C., Bassig B.A., Hu W., et al. Variation in oral microbiome is associated with future risk of lung cancer among never-smokers. Thorax. 2020;76:256–263. doi: 10.1136/thoraxjnl-2020-215542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu L., Qi Y., Jiang Y., Ji Y., Zhao Q., Wu J., Lu W., Wang Y., Chen Q., Wang C. Crosstalk between the gut microbiome and clinical response in locally advanced thoracic esophageal squamous cell carcinoma during neoadjuvant camrelizumab and chemotherapy. Ann. Transl. Med. 2022;10:325. doi: 10.21037/atm-22-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu X., Lv J., Guo F., Li J., Jia Y., Jiang D., Wang N., Zhang C., Kong L., Liu Y., et al. Gut Microbiome Influences the Efficacy of PD-1 Antibody Immunotherapy on MSS-Type Colorectal Cancer via Metabolic Pathway. Front. Microbiol. 2020;11:814. doi: 10.3389/fmicb.2020.00814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jin Y., Dong H., Xia L., Yang Y., Zhu Y., Shen Y., Zheng H., Yao C., Wang Y., Lu S. The Diversity of Gut Microbiome is Associated with Favorable Responses to Anti–Programmed Death 1 Immunotherapy in Chinese Patients with NSCLC. J. Thorac. Oncol. 2019;14:1378–1389. doi: 10.1016/j.jtho.2019.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Routy B., Gopalakrishnan V., Daillère R., Zitvogel L., Wargo J.A., Kroemer G. The gut microbiota influences anticancer immunosurveillance and general health. Nat. Rev. Clin. Oncol. 2018;15:382–396. doi: 10.1038/s41571-018-0006-2. [DOI] [PubMed] [Google Scholar]
- 10.Peng Z., Cheng S., Kou Y., Wang Z., Jin R., Hu H., Zhang X., Gong J.F., Li J., Lu M., et al. The Gut Microbiome Is Associated with Clinical Response to Anti-PD-1/PD-L1 Immunotherapy in Gastrointestinal Cancer. Cancer Immunol. Res. 2020;8:1251–1261. doi: 10.1158/2326-6066.CIR-19-1014. [DOI] [PubMed] [Google Scholar]
- 11.Reddy R.M., Weir W.B., Barnett S., Heiden B., Orringer M.B., Lin J., Chang A., Carrott P.W., Lynch W.R., Etherton-Beer C., et al. Increased Variance in Oral and Gastric Microbiome Correlates with Esophagectomy Anastomotic Leak. Ann. Thorac. Surg. 2018;105:865–870. doi: 10.1016/j.athoracsur.2017.08.061. [DOI] [PubMed] [Google Scholar]
- 12.Yuda M., Yamashita K., Okamura A., Hayami M., Fukudome I., Toihata T., Imamura Y., Mine S., Ishizuka N., Watanabe M. Influence of Preoperative Oropharyngeal Microflora on the Occurrence of Postoperative Pneumonia and Survival in Patients Undergoing Esophagectomy for Esophageal Cancer. Ann. Surg. 2020;272:1035–1043. doi: 10.1097/SLA.0000000000003287. [DOI] [PubMed] [Google Scholar]
- 13.Pimentel M., Saad R.J., Long M.D., Rao S.S.C. ACG Clinical Guideline: Small Intestinal Bacterial Overgrowth. Am. J. Gastroenterol. 2020;115:165–178. doi: 10.14309/ajg.0000000000000501. [DOI] [PubMed] [Google Scholar]
- 14.Ianiro G., Rossi E., Thomas A.M., Schinzari G., Masucci L., Quaranta G., Settanni C.R., Lopetuso L.R., Armanini F., Blanco-Miguez A., et al. Faecal microbiota transplantation for the treatment of diarrhoea induced by tyrosine-kinase inhibitors in patients with metastatic renal cell carcinoma. Nat. Commun. 2020;11:4333. doi: 10.1038/s41467-020-18127-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans . Schistosomes, Liver Flukes and Helicobacter pylori. Volume 61. IARC; Lyon, France: 1994. pp. 1–241. [PMC free article] [PubMed] [Google Scholar]
- 16.Liu X., Shao L., Liu X., Ji F., Mei Y., Cheng Y., Liu F., Yan C., Li L., Ling Z. Alterations of gastric mucosal microbiota across different stomach microhabitats in a cohort of 276 patients with gastric cancer. Ebiomedicine. 2019;40:336–348. doi: 10.1016/j.ebiom.2018.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pittayanon R., Lau J.T., Leontiadis G.I., Tse F., Yuan Y., Surette M., Moayyedi P. Differences in Gut Microbiota in Patients with vs. without Inflammatory Bowel Diseases: A Systematic Review. Gastroenterology. 2020;158:930–946.e1. doi: 10.1053/j.gastro.2019.11.294. [DOI] [PubMed] [Google Scholar]
- 18.Zhang X., Liu Q., Liao Q., Zhao Y. Pancreatic Cancer, Gut Microbiota, and Therapeutic Efficacy. J. Cancer. 2020;11:2749–2758. doi: 10.7150/jca.37445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mirzayi C., Renson A., Genomic Standards Consortium. Massive Analysis and Quality Control Society. Zohra F., Elsafoury S., Geistlinger L., Kasselman L.J., Eckenrode K., van de Wijgert J., et al. Reporting guidelines for human microbiome research: The STORMS checklist. Nat. Med. 2021;27:1885–1892. doi: 10.1038/s41591-021-01552-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sjöstedt S., Heimdahl A., Kager L., Nord C.E. Microbial colonization of the oropharynx, esophagus and stomach in patients with gastric diseases. Eur. J. Clin. Microbiol. Infect. Dis. 1985;4:49–51. doi: 10.1007/BF02148660. [DOI] [PubMed] [Google Scholar]
- 21.Dicksved J., Lindberg M., Rosenquist M., Enroth H., Jansson J., Engstrand L. Molecular characterization of the stomach microbiota in patients with gastric cancer and in controls. J. Med. Microbiol. 2009;58:509–516. doi: 10.1099/jmm.0.007302-0. [DOI] [PubMed] [Google Scholar]
- 22.Seo I., Jha B.K., Suh S.-I., Suh M.-H., Baek W.-K. Microbial Profile of the Stomach: Comparison between Normal Mucosa and Cancer Tissue in the Same Patient. J. Bacteriol. Virol. 2014;44:162–169. doi: 10.4167/jbv.2014.44.2.162. [DOI] [Google Scholar]
- 23.Aviles-Jimenez F., Vazquez-Jimenez F., Medrano-Guzman R., Mantilla A., Torres J. Stomach microbiota composition varies between patients with non-atrophic gastritis and patients with intestinal type of gastric cancer. Sci. Rep. 2014;4:4202. doi: 10.1038/srep04202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eun C.S., Kim B.K., Han D.S., Kim S.Y., Kim K.M., Choi B.Y., Song K.S., Kim Y.S., Kim J.F. Differences in Gastric Mucosal Microbiota Profiling in Patients with Chronic Gastritis, Intestinal Metaplasia, and Gastric Cancer Using Pyrosequencing Methods. Helicobacter. 2014;19:407–416. doi: 10.1111/hel.12145. [DOI] [PubMed] [Google Scholar]
- 25.Hu J., Han S., Chen Y., Ji Z. Variations of Tongue Coating Microbiota in Patients with Gastric Cancer. BioMed Res. Int. 2015;2015:173729. doi: 10.1155/2015/173729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang L., Zhou J., Xin Y., Geng C., Tian Z., Yu X., Dong Q. Bacterial overgrowth and diversification of microbiota in gastric cancer. Eur. J. Gastroenterol. Hepatol. 2016;28:261–266. doi: 10.1097/MEG.0000000000000542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yu G., Torres J., Hu N., Medrano-Guzman R., Herrera-Goepfert R., Humphrys M.S., Wang L., Wang C., Ding T., Ravel J., et al. Molecular Characterization of the Human Stomach Microbiota in Gastric Cancer Patients. Front. Cell. Infect. Microbiol. 2017;7:302. doi: 10.3389/fcimb.2017.00302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li T.H., Qin Y., Sham P.C., Lau K., Chu K.-M., Leung W.K. Alterations in Gastric Microbiota after H. Pylori Eradication and in Different Histological Stages of Gastric Carcinogenesis. Sci. Rep. 2017;7:44935. doi: 10.1038/srep44935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Castaño-Rodríguez N., Goh K.-L., Fock K.M., Mitchell H.M., Kaakoush N.O. Dysbiosis of the microbiome in gastric carcinogenesis. Sci. Rep. 2017;7:15957. doi: 10.1038/s41598-017-16289-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferreira R.M., Pereira-Marques J., Pinto-Ribeiro I., Costa J.L., Carneiro F., Machado J.C., Figueiredo C. Gastric microbial community profiling reveals a dysbiotic cancer-associated microbiota. Gut. 2017;67:226–236. doi: 10.1136/gutjnl-2017-314205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu Y.-L., Pang W., Huang Y., Zhang Y., Zhang C.-J. The Gastric Microbiome Is Perturbed in Advanced Gastric Adenocarcinoma Identified through Shotgun Metagenomics. Front. Cell. Infect. Microbiol. 2018;8:433. doi: 10.3389/fcimb.2018.00433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu J., Xu S., Xiang C., Cao Q., Li Q., Huang J., Shi L., Zhang J., Zhan Z. Tongue Coating Microbiota Community and Risk Effect on Gastric Cancer. J. Cancer. 2018;9:4039–4048. doi: 10.7150/jca.25280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hsieh Y.-Y., Tung S.-Y., Pan H.-Y., Yen C.-W., Xu H.-W., Lin Y.-J., Deng Y.-F., Hsu W.-T., Wu C.-S., Li C. Increased Abundance of Clostridium and Fusobacterium in Gastric Microbiota of Patients with Gastric Cancer in Taiwan. Sci. Rep. 2018;8:158. doi: 10.1038/s41598-017-18596-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coker O.O., Dai Z., Nie Y., Zhao G., Cao L., Nakatsu G., Wu W.K., Wong S.H., Chen Z., Sung J.J.Y., et al. Mucosal microbiome dysbiosis in gastric carcinogenesis. Gut. 2017;67:1024–1032. doi: 10.1136/gutjnl-2017-314281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shao D., Vogtmann E., Liu A., Qin J., Chen W., Abnet C.C., Wei W. Microbial characterization of esophageal squamous cell carcinoma and gastric cardia adenocarcinoma from a high-risk region of China. Cancer. 2019;125:3993–4002. doi: 10.1002/cncr.32403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gunathilake M.N., Lee J., Choi I.J., Kim Y.-I., Ahn Y., Park C., Kim J. Association between the relative abundance of gastric microbiota and the risk of gastric cancer: A case-control study. Sci. Rep. 2019;9:13589. doi: 10.1038/s41598-019-50054-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liang W., Yang Y., Wang H., Wang H., Yu X., Lu Y., Shen S., Teng L. Gut microbiota shifts in patients with gastric cancer in perioperative period. Medicine. 2019;98:e16626. doi: 10.1097/MD.0000000000016626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kageyama S., Takeshita T., Takeuchi K., Asakawa M., Matsumi R., Furuta M., Shibata Y., Nagai K., Ikebe M., Morita M., et al. Characteristics of the Salivary Microbiota in Patients with Various Digestive Tract Cancers. Front. Microbiol. 2019;10:1780. doi: 10.3389/fmicb.2019.01780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen X.-H., Wang A., Chu A.-N., Gong Y.-H., Yuan Y. Mucosa-Associated Microbiota in Gastric Cancer Tissues Compared with Non-cancer Tissues. Front. Microbiol. 2019;10:1261. doi: 10.3389/fmicb.2019.01261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dong Z., Chen B., Pan H., Wang D., Liu M., Yang Y., Zou M., Yang J., Xiao K., Zhao R., et al. Detection of Microbial 16S rRNA Gene in the Serum of Patients with Gastric Cancer. Front. Oncol. 2019;9:608. doi: 10.3389/fonc.2019.00608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Qi Y.-F., Sun J.-N., Ren L.-F., Cao X.-L., Dong J.-H., Tao K., Guan X.-M., Cui Y.-N., Su W. Intestinal Microbiota Is Altered in Patients with Gastric Cancer from Shanxi Province, China. Dig. Dis. Sci. 2019;64:1193–1203. doi: 10.1007/s10620-018-5411-y. [DOI] [PubMed] [Google Scholar]
- 42.Wang Z., Gao X., Zeng R., Wu Q., Sun H., Wu W., Zhang X., Sun G., Yan B., Wu L., et al. Changes of the Gastric Mucosal Microbiome Associated with Histological Stages of Gastric Carcinogenesis. Front. Microbiol. 2020;11:997. doi: 10.3389/fmicb.2020.00997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang L., Xin Y., Zhou J., Tian Z., Liu C., Yu X., Meng X., Jiang W., Zhao S., Dong Q. Gastric Mucosa-Associated Microbial Signatures of Early Gastric Cancer. Front. Microbiol. 2020;11:1548. doi: 10.3389/fmicb.2020.01548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spiegelhauer M.R., Kupcinskas J., Johannesen T.B., Urba M., Skieceviciene J., Jonaitis L., Frandsen T.H., Kupcinskas L., Fuursted K., Andersen L.P. Transient and Persistent Gastric Microbiome: Adherence of Bacteria in Gastric Cancer and Dyspeptic Patient Biopsies after Washing. J. Clin. Med. 2020;9:1882. doi: 10.3390/jcm9061882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gantuya B., El Serag H.B., Matsumoto T., Ajami N.J., Uchida T., Oyuntsetseg K., Bolor D., Yamaoka Y. Gastric mucosal microbiota in a Mongolian population with gastric cancer and precursor conditions. Aliment. Pharmacol. Ther. 2020;51:770–780. doi: 10.1111/apt.15675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu Z.-F., Zou K., Wu G.-N., Jin Z.-J., Xiang C.-J., Xu S., Wang Y.-H., Wu X.-Y., Chen C., Xu Z., et al. A Comparison of Tumor-Associated and Non-Tumor-Associated Gastric Microbiota in Gastric Cancer Patients. Dig. Dis. Sci. 2020;66:1673–1682. doi: 10.1007/s10620-020-06415-y. [DOI] [PubMed] [Google Scholar]
- 47.Xu S., Xiang C., Wu J., Teng Y., Wu Z., Wang R., Lu B., Zhan Z., Wu H., Zhang J. Tongue Coating Bacteria as a Potential Stable Biomarker for Gastric Cancer Independent of Lifestyle. Dig. Dis. Sci. 2020;66:2964–2980. doi: 10.1007/s10620-020-06637-0. [DOI] [PubMed] [Google Scholar]
- 48.Dang Y.-N., Dong Y., Mu Y.-Z., Yan J., Lu M., Zhu Y.-L., Zhang G.-X. Identification of gastric microbiota biomarker for gastric cancer. Chin. Med. J. 2020;133:2765–2767. doi: 10.1097/CM9.0000000000001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen X., Winckler B., Lu M., Cheng H., Yuan Z., Yang Y., Jin L., Ye W. Oral Microbiota and Risk for Esophageal Squamous Cell Carcinoma in a High-Risk Area of China. PLoS ONE. 2015;10:e0143603. doi: 10.1371/journal.pone.0143603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nasrollahzadeh D., Malekzadeh R., Ploner A., Shakeri R., Sotoudeh M., Fahimi S., Nasseri-Moghaddam S., Kamangar F., Abnet C.C., Winckler B., et al. Variations of gastric corpus microbiota are associated with early esophageal squamous cell carcinoma and squamous dysplasia. Sci. Rep. 2015;5:8820. doi: 10.1038/srep08820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yamamura K., Baba Y., Nakagawa S., Mima K., Miyake K., Nakamura K., Sawayama H., Kinoshita K., Ishimoto T., Iwatsuki M., et al. Human Microbiome Fusobacterium Nucleatum in Esophageal Cancer Tissue Is Associated with Prognosis. Clin. Cancer Res. 2016;22:5574–5581. doi: 10.1158/1078-0432.CCR-16-1786. [DOI] [PubMed] [Google Scholar]
- 52.Elliott D.R.F., Walker A.W., O’Donovan M., Parkhill J., Fitzgerald R.C. A non-endoscopic device to sample the oesophageal microbiota: A case-control study. Lancet Gastroenterol. Hepatol. 2017;2:32–42. doi: 10.1016/S2468-1253(16)30086-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peters B.A., Wu J., Pei Z., Yang L., Purdue M.P., Freedman N.D., Jacobs E.J., Gapstur S.M., Hayes R.B., Ahn J. Oral Microbiome Composition Reflects Prospective Risk for Esophageal Cancers. Cancer Res. 2017;77:6777–6787. doi: 10.1158/0008-5472.CAN-17-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang Q., Rao Y., Guo X., Liu N., Liu S., Wen P., Li S., Li Y. Oral Microbiome in Patients with Oesophageal Squamous Cell Carcinoma. Sci. Rep. 2019;9:19055. doi: 10.1038/s41598-019-55667-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yamamura K., Izumi D., Kandimalla R., Sonohara F., Baba Y., Yoshida N., Kodera Y., Baba H., Goel A. Intratumoral Fusobacterium Nucleatum Levels Predict Therapeutic Response to Neoadjuvant Chemotherapy in Esophageal Squamous Cell Carcinoma. Clin. Cancer Res. 2019;25:6170–6179. doi: 10.1158/1078-0432.CCR-19-0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu L., Li Y., Sun S., Yue J. Decrease of oral microbial diversity might correlate with radiation esophagitis in patients with esophageal cancer undergoing chemoradiation: A pilot study. Precis. Radiat. Oncol. 2020;4:81–88. doi: 10.1002/pro6.1098. [DOI] [Google Scholar]
- 57.Peter S., Pendergraft A., VanDerPol W., Wilcox C.M., Baig K.R.K.K., Morrow C., Izard J., Mannon P.J. Mucosa-Associated Microbiota in Barrett’s Esophagus, Dysplasia, and Esophageal Adenocarcinoma Differ Similarly Compared with Healthy Controls. Clin. Transl. Gastroenterol. 2020;11:e00199. doi: 10.14309/ctg.0000000000000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li D., He R., Hou G., Ming W., Fan T., Chen L., Zhang L., Jiang W., Wang W., Lu Z., et al. Characterization of the Esophageal Microbiota and Prediction of the Metabolic Pathways Involved in Esophageal Cancer. Front. Cell. Infect. Microbiol. 2020;10:268. doi: 10.3389/fcimb.2020.00268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhao Q., Yang T., Yan Y., Zhang Y., Li Z., Wang Y., Yang J., Xia Y., Xiao H., Han H., et al. Alterations of Oral Microbiota in Chinese Patients with Esophageal Cancer. Front. Cell. Infect. Microbiol. 2020;10:541144. doi: 10.3389/fcimb.2020.541144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhou J., Shrestha P., Qiu Z., Harman D.G., Teoh W.-C., Al-Sohaily S., Liem H., Turner I., Ho V. Distinct Microbiota Dysbiosis in Patients with Non-Erosive Reflux Disease and Esophageal Adenocarcinoma. J. Clin. Med. 2020;9:2162. doi: 10.3390/jcm9072162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lopetuso L.R., Severgnini M., Pecere S., Ponziani F.R., Boskoski I., Larghi A., Quaranta G., Masucci L., Ianiro G., Camboni T., et al. Esophageal microbiome signature in patients with Barrett’s esophagus and esophageal adenocarcinoma. PLoS ONE. 2020;15:e0231789. doi: 10.1371/journal.pone.0231789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kawasaki M., Ikeda Y., Ikeda E., Takahashi M., Tanaka D., Nakajima Y., Arakawa S., Izumi Y., Miyake S. Oral infectious bacteria in dental plaque and saliva as risk factors in patients with esophageal cancer. Cancer. 2020;127:512–519. doi: 10.1002/cncr.33316. [DOI] [PubMed] [Google Scholar]
- 63.Yu D., Yang J., Jin M., Zhou B., Shi L., Zhao L., Zhang J., Lin Z., Ren J., Liu L., et al. Fecal Streptococcus Alteration Is Associated with Gastric Cancer Occurrence and Liver Metastasis. mBio. 2021;12:e0299421. doi: 10.1128/mBio.02994-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abate M.M., Vos E., Gonen M., Janjigian Y.Y., Schattner M., Laszkowska M., Tang L., Maron S.B., Coit D.G., Vardhana S., et al. A Novel Microbiome Signature in Gastric Cancer. Ann. Surg. 2022;276:605–615. doi: 10.1097/SLA.0000000000005587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu D., Zhang R., Chen S., Sun B., Zhang K. Analysis of gastric microbiome reveals three distinctive microbial communities associated with the occurrence of gastric cancer. BMC Microbiol. 2022;22:184. doi: 10.1186/s12866-022-02594-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Park J.-Y., Kang C.-S., Seo H.-C., Shin J.-C., Kym S.-M., Park Y.-S., Shin T.-S., Kim J.-G., Kim Y.-K. Bacteria-Derived Extracellular Vesicles in Urine as a Novel Biomarker for Gastric Cancer: Integration of Liquid Biopsy and Metagenome Analysis. Cancers. 2021;13:4687. doi: 10.3390/cancers13184687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pimentel-Nunes P., Barros A., Pita I., Miranda I., Conceição G., Borges-Canha M., Leite-Moreira A.F., Libânio D., Dinis-Ribeiro M. Gastric microbiome profile throughout gastric carcinogenesis: Beyond helicobacter. Scand. J. Gastroenterol. 2021;56:708–716. doi: 10.1080/00365521.2021.1902560. [DOI] [PubMed] [Google Scholar]
- 68.Yang Y., Long J., Wang C., Blot W.J., Pei Z., Shu X., Wu F., Rothman N., Wu J., Lan Q., et al. Prospective study of oral microbiome and gastric cancer risk among Asian, African American and European American populations. Int. J. Cancer. 2021;150:916–927. doi: 10.1002/ijc.33847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dai D., Yang Y., Yu J., Dang T., Qin W., Teng L., Ye J., Jiang H. Interactions between gastric microbiota and metabolites in gastric cancer. Cell Death Dis. 2021;12:1104. doi: 10.1038/s41419-021-04396-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li F., Zhu H., Tao K., Xia Y., Liu M., Wang Y., Sun Y., Cao T., Chai J., Ni F., et al. Mucosal microbial microenvironment in early gastric neoplasia and non-neoplastic gastric disease. J. Gastroenterol. Hepatol. 2021;36:3092–3101. doi: 10.1111/jgh.15565. [DOI] [PubMed] [Google Scholar]
- 71.Gunathilake M., Lee J., Choi I.J., Kim Y., Kim J. Association between bacteria other than Helicobacter pylori and the risk of gastric cancer. Helicobacter. 2021;26:e12836. doi: 10.1111/hel.12836. [DOI] [PubMed] [Google Scholar]
- 72.Huang K., Gao X., Wu L., Yan B., Wang Z., Zhang X., Peng L., Yu J., Sun G., Yang Y. Salivary Microbiota for Gastric Cancer Prediction: An Exploratory Study. Front. Cell. Infect. Microbiol. 2021;11:640309. doi: 10.3389/fcimb.2021.640309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Oliveira G.R.D.C., Anna C.D.C.S., Lamarão L.M., Guimarães A.C., da Rocha C.M., Bahia M.D.O., de Souza C.R., Calcagno D.Q., de Assumpção P.P., Burbano R.R. Quantitative difference of oral pathogen between individuals with gastric cancer and individuals without cancer. Oncotarget. 2021;12:1677–1686. doi: 10.18632/oncotarget.28034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sarhadi V., Mathew B., Kokkola A., Karla T., Tikkanen M., Rautelin H., Lahti L., Puolakkainen P., Knuutila S. Gut microbiota of patients with different subtypes of gastric cancer and gastrointestinal stromal tumors. Gut Pathog. 2021;13:11. doi: 10.1186/s13099-021-00403-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang X., Li C., Cao W., Zhang Z. Alterations of Gastric Microbiota in Gastric Cancer and Precancerous Stages. Front. Cell. Infect. Microbiol. 2021;11:559148. doi: 10.3389/fcimb.2021.559148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu S., Dai J., Lan X., Fan B., Dong T., Zhang Y., Han M. Intestinal bacteria are potential biomarkers and therapeutic targets for gastric cancer. Microb. Pathog. 2021;151:104747. doi: 10.1016/j.micpath.2021.104747. [DOI] [PubMed] [Google Scholar]
- 77.Zhang Y., Shen J., Shi X., Du Y., Niu Y., Jin G., Wang Z., Lyu J. Gut microbiome analysis as a predictive marker for the gastric cancer patients. Appl. Microbiol. Biotechnol. 2021;105:803–814. doi: 10.1007/s00253-020-11043-7. [DOI] [PubMed] [Google Scholar]
- 78.Zhang C., Hu A., Li J., Zhang F., Zhong P., Li Y., Li Y. Combined Non-Invasive Prediction and New Biomarkers of Oral and Fecal Microbiota in Patients with Gastric and Colorectal Cancer. Front. Cell. Infect. Microbiol. 2022;12:830684. doi: 10.3389/fcimb.2022.830684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.He C., Peng C., Shu X., Wang H., Zhu Z., Ouyang Y., Yang X., Xie C., Hu Y., Li N., et al. Convergent dysbiosis of gastric mucosa and fluid microbiome during stomach carcinogenesis. Gastric Cancer. 2022;25:837–849. doi: 10.1007/s10120-022-01302-z. [DOI] [PubMed] [Google Scholar]
- 80.Ding J., Man Y.-G., Deng X., Chen T. Differences in community structure of gastrointestinal tract between Helicobacter pylori positive patients and negative patients with gastric cancer. J. Cancer. 2022;13:1905–1913. doi: 10.7150/jca.69873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Park J.Y., Seo H., Kang C.-S., Shin T.-S., Kim J.W., Park J.-M., Kim J.G., Kim Y.-K. Dysbiotic change in gastric microbiome and its functional implication in gastric carcinogenesis. Sci. Rep. 2022;12:4285. doi: 10.1038/s41598-022-08288-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhou C.-B., Pan S.-Y., Jin P., Deng J.-W., Xue J.-H., Ma X.-Y., Xie Y.-H., Cao H., Liu Q., Xie W.-F., et al. Fecal Signatures of Streptococcus anginosus and Streptococcus constellatus for Noninvasive Screening and Early Warning of Gastric Cancer. Gastroenterology. 2022;162:1933–1947.e18. doi: 10.1053/j.gastro.2022.02.015. [DOI] [PubMed] [Google Scholar]
- 83.Sun Q.-H., Zhang J., Shi Y.-Y., Fu W.-W., Ding S.-G. Microbiome changes in the gastric mucosa and gastric juice in different histological stages of Helicobacter pylori-negative gastric cancers. World J. Gastroenterol. 2022;28:365–380. doi: 10.3748/wjg.v28.i3.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Png C.W., Lee W.J.J., Chua S.J., Zhu F., Gastric Consortium. Yeoh K.G., Zhang Y. Mucosal microbiome associates with progression to gastric cancer. Theranostics. 2022;12:48–58. doi: 10.7150/thno.65302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shu J., Yu H., Ren X., Wang Y., Zhang K., Tang Z., Dang L., Chen W., Li B., Xie H., et al. Role of salivary glycopatterns for oral microbiota associated with gastric cancer. Int. J. Biol. Macromol. 2022;209:1368–1378. doi: 10.1016/j.ijbiomac.2022.04.133. [DOI] [PubMed] [Google Scholar]
- 86.Zhang Z., Zhu L., Ma Y., Wang B., Ci C., Zhang J., Zhou Y., Dou C., Gu Q., An Y., et al. Study on the Characteristics of Intestinal Flora Composition in Gastric Cancer Patients and Healthy People in the Qinghai-Tibet Plateau. Appl. Biochem. Biotechnol. 2022;194:1510–1526. doi: 10.1007/s12010-021-03732-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Shi L., Fan Q., Zhou B., Wu J., Jin M., Yu D., Zhang T., Song J., Liu H. The composition and functional profile of the microbial communities in human gastric cancer tissues and adjacent normal tissues. Acta Biochim. Biophys. Sin. 2021;54:47–54. doi: 10.3724/abbs.2021010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ishaq H.M., Mohammad I.S., Muhammad K.S., Li H., Abbas R.Z., Sindhu Z.U.D., Ullah S., Fan Y., Sadiq A., Raza M.A., et al. Gut microbial dysbiosis and its association with esophageal cancer. J. Appl. Biomed. 2021;19:1–13. doi: 10.32725/jab.2021.005. [DOI] [PubMed] [Google Scholar]
- 89.Wang Y., Guo H., Gao X., Wang J. The Intratumor Microbiota Signatures Associate with Subtype, Tumor Stage, and Survival Status of Esophageal Carcinoma. Front. Oncol. 2021;11:754788. doi: 10.3389/fonc.2021.754788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Deng Y., Tang D., Hou P., Shen W., Li H., Wang T., Liu R. Dysbiosis of gut microbiota in patients with esophageal cancer. Microb. Pathog. 2021;150:104709. doi: 10.1016/j.micpath.2020.104709. [DOI] [PubMed] [Google Scholar]
- 91.Hao Y., Karaoz U., Yang L., Yachimski P.S., Tseng W., Nossa C.W., Ye W., Tseng M., Poles M., Francois F., et al. Progressive dysbiosis of human orodigestive microbiota along the sequence of gastroesophageal reflux, Barrett’s esophagus and esophageal adenocarcinoma. Int. J. Cancer. 2022;151:1703–1716. doi: 10.1002/ijc.34191. [DOI] [PubMed] [Google Scholar]
- 92.Li Z., Shi C., Zheng J., Guo Y., Fan T., Zhao H., Jian D., Cheng X., Tang H., Ma J. Fusobacterium nucleatum predicts a high risk of metastasis for esophageal squamous cell carcinoma. BMC Microbiol. 2021;21:301. doi: 10.1186/s12866-021-02352-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li Z., Dou L., Zhang Y., He S., Zhao D., Hao C., Song G., Zhang W., Liu Y., Wang G. Characterization of the Oral and Esophageal Microbiota in Esophageal Precancerous Lesions and Squamous Cell Carcinoma. Front. Cell. Infect. Microbiol. 2021;11:714162. doi: 10.3389/fcimb.2021.714162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wei J., Li R., Lu Y., Meng F., Xian B., Lai X., Lin X., Deng Y., Yang D., Zhang H., et al. Salivary microbiota may predict the presence of esophageal squamous cell carcinoma. Genes Dis. 2021;9:1143–1151. doi: 10.1016/j.gendis.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jiang Z., Wang J., Shen Z., Zhang Z., Wang S. Characterization of Esophageal Microbiota in Patients with Esophagitis and Esophageal Squamous Cell Carcinoma. Front. Cell. Infect. Microbiol. 2021;11:774330. doi: 10.3389/fcimb.2021.774330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shen W., Tang D., Deng Y., Li H., Wang T., Wan P., Liu R. Association of gut microbiomes with lung and esophageal cancer: A pilot study. World J. Microbiol. Biotechnol. 2021;37:128. doi: 10.1007/s11274-021-03086-3. [DOI] [PubMed] [Google Scholar]
- 97.Chen M.-F., Lu M.-S., Hsieh C.-C., Chen W.-C. Porphyromonas gingivalis promotes tumor progression in esophageal squamous cell carcinoma. Cell. Oncol. 2021;44:373–384. doi: 10.1007/s13402-020-00573-x. [DOI] [PubMed] [Google Scholar]
- 98.Kovaleva O., Podlesnaya P., Rashidova M., Samoilova D., Petrenko A., Mochalnikova V., Kataev V., Khlopko Y., Plotnikov A., Gratchev A. Prognostic Significance of the Microbiome and Stromal Cells Phenotype in Esophagus Squamous Cell Carcinoma. Biomedicines. 2021;9:743. doi: 10.3390/biomedicines9070743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yang W., Chen C.-H., Jia M., Xing X., Gao L., Tsai H.-T., Zhang Z., Liu Z., Zeng B., Yeung S.-C.J., et al. Tumor-Associated Microbiota in Esophageal Squamous Cell Carcinoma. Front. Cell Dev. Biol. 2021;9:641270. doi: 10.3389/fcell.2021.641270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cheung M.K., Yue G.G.L., Lauw S., Li C.S.Y., Yung M.Y., Ng S.C., Yip H.C., Kwan H.S., Chiu P.W.Y., Lau C.B.S. Alterations in gut microbiota of esophageal squamous cell carcinoma patients. J. Gastroenterol. Hepatol. 2022;37:1919–1927. doi: 10.1111/jgh.15941. [DOI] [PubMed] [Google Scholar]
- 101.Wu C., Wang M., Zhou Q., Shi H. Associations of Changes in Intestinal Flora and Inflammatory Factors with Prognosis of Patients with Esophageal Cancer. J. Health Eng. 2022;2022:2426301. doi: 10.1155/2022/2426301. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 102.Lin Z., Rao W., Xiang Z., Zeng Q., Liu S., Yu K., Zhou J., Wang J., Chen W., Chen Y., et al. Characteristics and interplay of esophageal microbiota in esophageal squamous cell carcinoma. BMC Cancer. 2022;22:696. doi: 10.1186/s12885-022-09771-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shen W., Tang D., Wan P., Peng Z., Sun M., Guo X., Liu R. Identification of tissue-specific microbial profile of esophageal squamous cell carcinoma by full-length 16S rDNA sequencing. Appl. Microbiol. Biotechnol. 2022;106:3215–3229. doi: 10.1007/s00253-022-11921-2. [DOI] [PubMed] [Google Scholar]
- 104.Wells G.A., Shea B., O-Connell D., Peterson J., Welch V., Losos M., Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. [(accessed on 30 September 2022)]. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 105.Muszyński D., Kudra A., Sobocki B.K., Folwarski M., Vitale E., Filetti V., Dudzic W., Kaźmierczak-Siedlecka K., Połom K. Esophageal cancer and bacterial part of gut microbiota—A multidisciplinary point of view. Front. Cell. Infect. Microbiol. 2022;12:1057668. doi: 10.3389/fcimb.2022.1057668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tarazi M., Jamel S., Mullish B.H., Markar S.R., Hanna G.B. Impact of gastrointestinal surgery upon the gut microbiome: A systematic review. Surgery. 2022;171:1331–1340. doi: 10.1016/j.surg.2021.10.014. [DOI] [PubMed] [Google Scholar]
- 107.Arai J., Niikura R., Hayakawa Y., Suzuki N., Hirata Y., Ushiku T., Fujishiro M. Clinicopathological Features of Gastric Cancer with Autoimmune Gastritis. Biomedicines. 2022;10:884. doi: 10.3390/biomedicines10040884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Duncan S.H., Iyer A., Russell W.R. Impact of protein on the composition and metabolism of the human gut microbiota and health. Proc. Nutr. Soc. 2021;80:173–185. doi: 10.1017/S0029665120008022. [DOI] [PubMed] [Google Scholar]
- 109.Li N., Bai C., Zhao L., Ge Y., Li X. Characterization of the fecal microbiota in gastrointestinal cancer patients and healthy people. Clin. Transl. Oncol. 2022;24:1134–1147. doi: 10.1007/s12094-021-02754-y. [DOI] [PubMed] [Google Scholar]
- 110.Mirzayi C., Renson A., Zohra F., Elsafoury S., Kasselman L., van de Wijgert J., Segata N., Beghini F., Eckenrode K., Dowd J., et al. Strengthening The Organizing and Reporting of Microbiome Studies (STORMS) bioRxiv. 2020 doi: 10.1101/2020.06.24.167353. [DOI] [Google Scholar]
- 111.Arnold M., Soerjomataram I., Ferlay J., Forman D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut. 2015;64:381–387. doi: 10.1136/gutjnl-2014-308124. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.