On May 5th 2023, the World Health Organisation declared that COVID-19 does not constitute a Public Health Emergency of International Concern (PHEIC) anymore, advising that it is time to transition to long-term management of the COVID-19 pandemic. In these three years of the COVID-19 PHEIC in Europe, almost 250 million infections have been confirmed, and more than 2 million people have died from the disease—this is more than the population of Vienna.
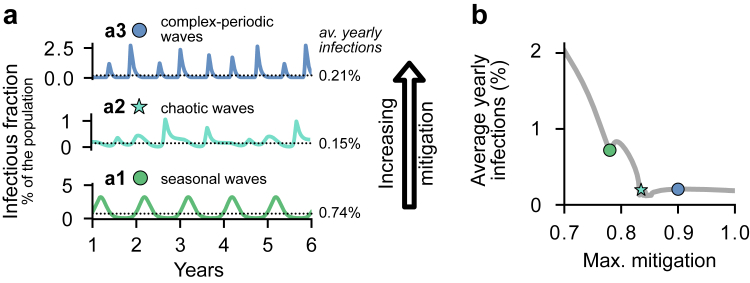
With the PHEIC being over, will COVID-19 become endemic, and what does that imply? As SARS-CoV-2 is highly transmissible and immunity against it wanes, one expects that COVID-19 incidence worldwide will settle to a nonzero level. The precise “endemic equilibrium” is determined by the waning immunity and transmission rate of the predominant variants, vaccination rates, seasonality, and human behaviour (including active mitigation responses). In other words, the endemic equilibrium is a result of an implicit balance between the maximum incidence that societies accept and the maximum feasible extent of mitigation they tolerate.1 Classically, one expects for endemicity either relatively constant incidence, or seasonal waves (Fig. 1a1). However, if moderate mitigation responses remain necessary and interact with seasonality, complex and even chaotic dynamics can emerge even in the endemic state2 (Fig. 1a2 and a3). That means that we might not see the classic steady state or seasonal waves but highly complex and potentially irregular wave patterns. These complex dynamics reduce long-term predictability but have the advantage of reducing the total number of infections2 (Fig. 1b).
Fig. 1.
The many faces of endemic disease spread. a. Depending on the maximum mitigation required, vastly different dynamics for the endemic incidence can emerge. a1. Classically (without any mitigation), seasonal outbreaks are expected. a2, a3. However, complex oscillatory dynamics can arise when mitigation and seasonality are comparable, featuring complex-periodic waves (e.g., 3 waves in 2 years), or chaos. b. The average number of infections observed for chaotic dynamics (a2.) is substantially lower than that for unmitigated seasonal waves (a1.) and is comparable to when mitigating too strongly (a3.). This implies that societies might have to trade off predictability for reductions in the average number of infections, and that above a certain point, over-mitigation does not pay off. Figure modified from.2
The average incidence of the endemic equilibrium matters: with high incidence, we accept high morbidity, and higher economic and societal costs due to sick leave, severe course, and post-COVID, besides having higher chances of generating new variants with undesirable properties.3 On the other hand, ongoing mild exposure to the virus might refresh immunity and protect individuals against a severe course.4 Given the available information, it is not clear yet how these factors equilibrate. It is thus an ongoing task for societies to weigh the consequences of high COVID-19 incidence against the cost of mitigation.5
If some non-pharmaceutical interventions (NPIs) are necessary in case of pandemics, what can Europe do to avoid some of their negative consequences?
The COVID-19 pandemic taught us, by example, a lot for future pandemics. From the perspective of dynamics, we here summarize five basic mechanistic principles that can inform the design of interventions. The principles apply if mitigation is considered necessary, e.g., to bridge the time until vaccination is broadly available: (I.) Act early. As disease spread at the early stage is typically exponential, a few days of delay can double the incidence.6,7. (II.) To be able to act early, active surveillance for novel outbreaks is critical. (III.) Even under uncertainty, it is often better to act than not to act.8. (IV.) Act strongly; if the aim is to lower the incidence, then stronger interventions are over-proportionally more effective: To illustrate this, for COVID-19, reducing the incidence by half takes one week if the reproduction number R is lowered to R = 0.7; the same reduction takes one month if only R = 0.9 is achieved.6,7 Finally, (V.) low case numbers allow for more freedom, because then test-trace-and-isolate interventions have more capacity and are faster to break infection chains. Thus, overall, the mitigation measures required to equilibrate incidence (i.e. reach R = 1) at low case numbers are milder than those needed to equilibrate an outbreak at high incidence, again at the limit where the overall immunity levels in the population are low.6
A key challenge for the future relates to making NPIs equitable across countries and segments of society, making them fair, consistent and effective, and to communicate them clearly.5,8, 9, 10 Targeted interventions for those disproportionately impacted by NPIs can substantially reduce the NPIs’ collateral damage.10 Implementing these flanking measures alongside broader strategies will not only help reduce the overall burden of NPIs but also foster a more inclusive and resilient society during challenging times.
As COVID-19 transitions from epidemic to endemic state, we appreciate the positive aspects of regaining normalcy in our lives. People are finally resuming activities and social interactions that were restricted during the pandemic, enriching their well-being and fostering a sense of community. As scientists also recover from the intense research efforts during COVID-19, we only start to systematically evaluate past actions to be better prepared for the next pandemic. Thus, in terms of research tasks, our work in understanding the COVID-19 pandemic has not concluded.
Contributors
All authors contributed equally to this comment.
Conceptualization: all.
Writing - Original Draft: all.
Writing - Review & Editing: all.
Declaration of interests
VP was a member of the ExpertInnenrat of the German federal government on COVID and an advisor for other governmental and non-governmental entities. The remaining authors declare no competing interests.
Acknowledgements
All authors received support from the Max-Planck-Society. SC and VP received funding by the German Federal Ministry for Education and Research for the RESPINOW project (031L0298), and ENI and VP for the infoXpand project (031L0300A). VP was supported by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Germany's Excellence Strategy - EXC 2067/1-390729940.
References
- 1.Medley G.F., Vassall A. When an emerging disease becomes endemic. Science. 2017;357(6347):156–158. doi: 10.1126/science.aam8333. [DOI] [PubMed] [Google Scholar]
- 2.Wagner J., Bauer S., Contreras S., Fleddermann L., Parlitz U., Priesemann V. Societal feedback induces complex and chaotic dynamics in endemic infectious diseases. arXiv. 2023 arXiv:2305.15427. [Google Scholar]
- 3.Katzourakis A. COVID-19: endemic doesn't mean harmless. Nature. 2022;601(7894):485. doi: 10.1038/d41586-022-00155-x. [DOI] [PubMed] [Google Scholar]
- 4.De Angelis M.L., Francescangeli F., Rossi R., Giuliani A., De Maria R., Zeuner A. Repeated exposure to subinfectious doses of SARS-CoV-2 May promote T cell immunity and protection against severe COVID-19. Viruses. 2021;13(6):961. doi: 10.3390/v13060961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lazarus J.V., Romero D., Kopka C.J., et al. A multinational Delphi consensus to end the COVID-19 public health threat. Nature. 2022:1–14. doi: 10.1038/s41586-022-05398-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Contreras S., Dehning J., Mohr S.B., Bauer S., Spitzner F.P., Priesemann V. Low case numbers enable long-term stable pandemic control without lockdowns. Sci Adv. 2021;7(41) doi: 10.1126/sciadv.abg2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dehning J., Zierenberg J., Spitzner F.P., et al. Inferring change points in the spread of COVID-19 reveals the effectiveness of interventions. Science. 2020;369(6500) doi: 10.1126/science.abb9789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Priesemann V., Balling R., Brinkmann M.M., et al. An action plan for pan-European defence against new SARS-CoV-2 variants. Lancet. 2021;397(10273):469–470. doi: 10.1016/S0140-6736(21)00150-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore S., Hill E.M., Dyson L., Tildesley M.J., Keeling M.J. Retrospectively modeling the effects of increased global vaccine sharing on the COVID-19 pandemic. Nat Med. 2022:1–8. doi: 10.1038/s41591-022-02064-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iftekhar E.N., Priesemann V., Balling R., et al. A look into the future of the COVID-19 pandemic in Europe: an expert consultation. Lancet Reg Health Eur. 2021;8 doi: 10.1016/j.lanepe.2021.100185. [DOI] [PMC free article] [PubMed] [Google Scholar]