Figure 3: Pressure volume (PV) loop basics.
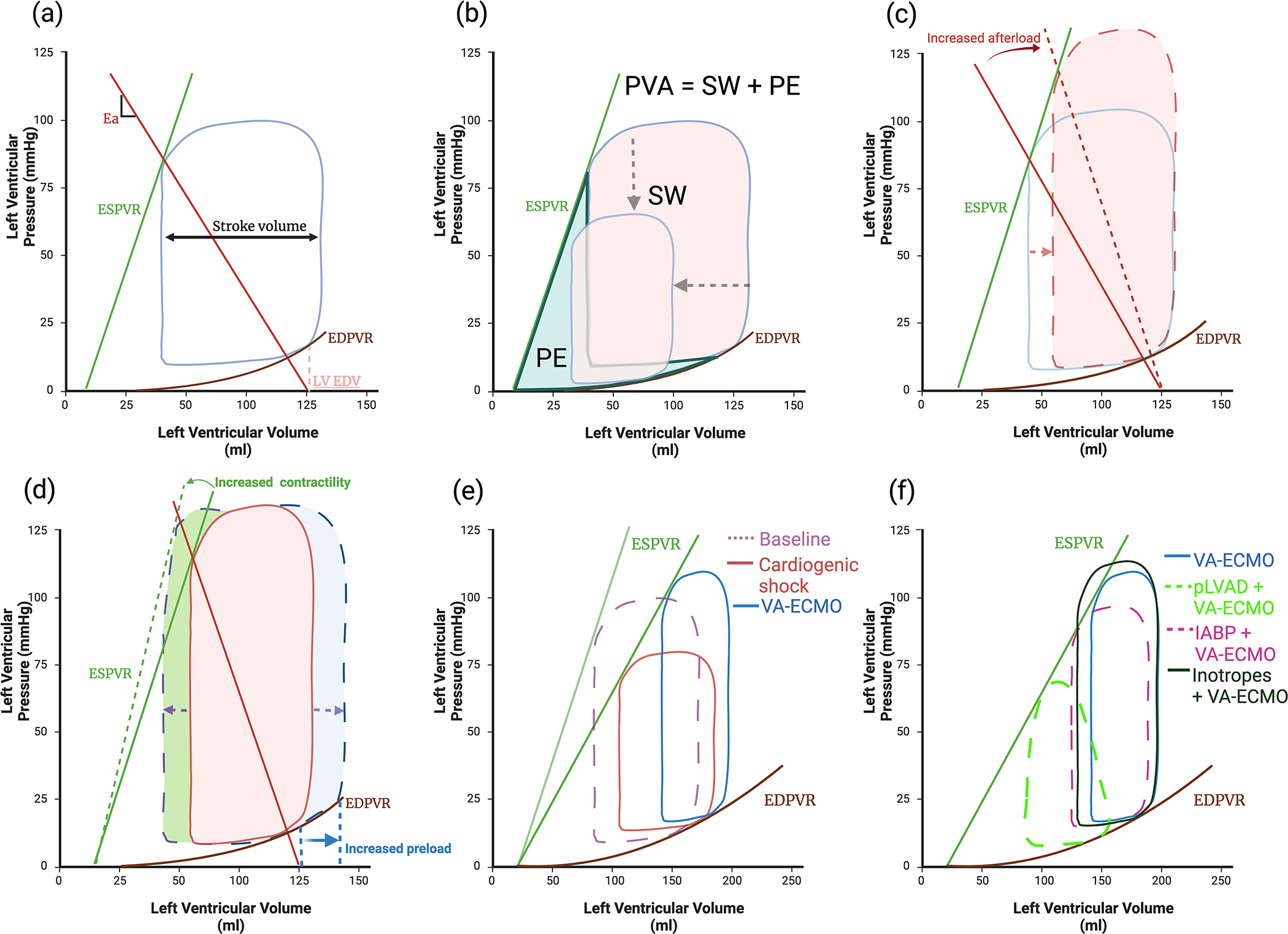
(a) Normal PV loop, boundaries are created by the end systolic pressure volume relationship (ESPVR) and the non-linear end diastolic pressure volume relationship (EDPVR). Effective arterial elastance (Ea) reflects afterload and is the slope of the line between the end diastolic volume (LV EDV) and the ESPVR. (b) Stroke work (SW) is the work required to eject blood, Potential energy (PE) is energy generated during contraction but not converted to SW. Pressure volume area (PVA) correlates linearly with myocardial oxygen consumption (MVO2) and is the sum of the SW and PE. Ventricular unloading is defined by a reduction in the PVA. (c) Increased afterload whilst maintaining the same level of contractility and preload reduces stroke volume (SV) (d) SV can be increased by either increasing preload, however in a dilated ventricle this will cause a significant rise in end diastolic pressure due to the non-linear EDPVR or by increasing contractility but this also increases MVO2. (e) Cardiogenic shock results in loss of contractility and increases end diastolic pressure (EDP) and volume (EDV). (b) VA-ECMO raises systolic pressure, EDP and afterload thereby increasing pressure volume area (PVA), whilst further reducing SV (f) IABP reduces afterload, increasing SV without significantly reducing EDP, EDV or PVA. In contrast pLVAD actively unloads the ventricle reducing afterload, EDV and EDP thereby significantly reducing PVA. Inotropes increase contractility improving SV; however, this increases PVA.
