Abstract
The coronavirus disease 2019 (COVID-19) pandemic has restricted many medical practices. We aimed to investigate the impact of the COVID-19 pandemic on the number of bronchoscopies, outpatients, and hospital admissions. We retrospectively analyzed the number of outpatients, admissions, and bronchoscopies performed between March 2020 and May 2022. We defined “Peak month of the pandemic,” “Wave of the pandemic,” “Month in the wave,” and “Period of a state of emergency” for each analysis. In the first year of the COVID-19 pandemic, analysis of variance (ANOVA) in linear mixed models indicated significant effects of “month in each wave” on the number of bronchoscopies (P = .003), outpatients (P = .041), and admissions (P = .017). The number of outpatients, admissions, and bronchoscopies was significantly influenced by the first wave of the COVID-19 pandemic. In contrast, in the second year of the COVID-19 pandemic, a mixed-ANOVA indicated significant effects of “month in each wave” only on the number of outpatients (P = .020) but no significant effects on the number of bronchoscopies (P = .407) and admissions (P = .219). During the second year of the pandemic, the number of bronchoscopies and admissions was not significantly affected by the waves of the pandemic. There were no significant differences in the number of admissions and bronchoscopies between the fourth and sixth waves. Although the number of bronchoscopies was found to be significantly affected in the early stages of the COVID-19 pandemic, the impact of the pandemic was much more limited thereafter.
Keywords: admission, bronchoscopy, COVID-19, outpatient
1. Introduction
Coronavirus disease 2019 (COVID-19) pandemic continues to have a serious impact on healthcare systems, economies, and social systems worldwide.[1,2] Many healthcare professionals and institutions were forced to respond to the COVID-19 pandemic, and nonessential consultations and examinations were largely curtailed.[3] Therefore, the COVID-19 pandemic caused a decline in outpatient and inpatient admissions, as well as a curtailment of surgeries and tests, with serious consequences such as delays in the diagnosis and treatment of serious diseases.[4] In the US, it has been reported that the COVID-19 pandemic has led to significant delays in the diagnosis and treatment of cancer.[5] In Japan, delays in cancer detection owing to the discontinuation of annual health checkup services have also become a problem.[6] In the respiratory field, the discontinuation of lung cancer screening has caused delays in the detection of lung cancer.[7]
Bronchoscopy is an important procedure in the diagnosis of respiratory diseases, particularly lung cancer. However, it is a droplet-inducing procedure that is considered high risk for severe acute respiratory syndrome coronavirus 2 transmission due to droplet exposure of healthcare workers during the COVID-19 pandemic.[8–10] For this reason, it was assumed that bronchoscopy was avoided during the COVID-19 pandemic. However, the impact of COVID-19 on bronchoscopy in general community hospitals is not well understood. In the present study, we aimed to examine the impact of the COVID-19 pandemic on the number of outpatients, admissions, and bronchoscopies.
2. Materials and methods
This was a retrospective observational cohort study. All patients who visited the Department of Respiratory Medicine between March 2020 and May 2022 were included. The number of outpatients, admissions, and bronchoscopies was examined from the electronic medical record data. This study was approved by the institutional ethical review board of our institution (approval number: 21-061).
Since this study only dealt with statistical data and did not collect individual patient data, written informed consent from the patients was not required. We defined “Peak month of the pandemic,” “Wave of the pandemic,” “Month in the wave,” and “Period of a state of emergency” as follows:
Peak month of the pandemic: the month which includes the day when the number of new COVID-19 patients nationwide was the largest in the 2 months before and after the month. The peaks of new COVID-19 patients nationwide were observed on April 11, 2020, August 7, 2020, January 8, 2021, May 8, 2021, August 20, 2021, and February 1, 2022.
Wave of the pandemic: the period from the month prior to the peak to the month prior to the next peak. Thus, each wave contained 1 peak month of the pandemic.
Month in the wave: we defined month 0 as the first month of each wave and month 1 as the peak month of the wave. Thereafter, the months in the wave were named months 2, 3, 4, etc in that order. We indicated the peak of the pandemic and the time from the peak in each wave as indicators of the impact of the COVID-19 pandemic, denoted as “month in each wave.”
Period of a state of emergency: Between March 2020 and May 2022, the Government of Japan declared a state of emergency in Kyoto City 4 times (first time: April 16, 2020, to May 21, 2020; second time: January 14, 2021, to February 28, 2021; third time: April 25, 2021, to June 20, 2021; fourth time: August 20, 2021, to September 30, 2021).[11]
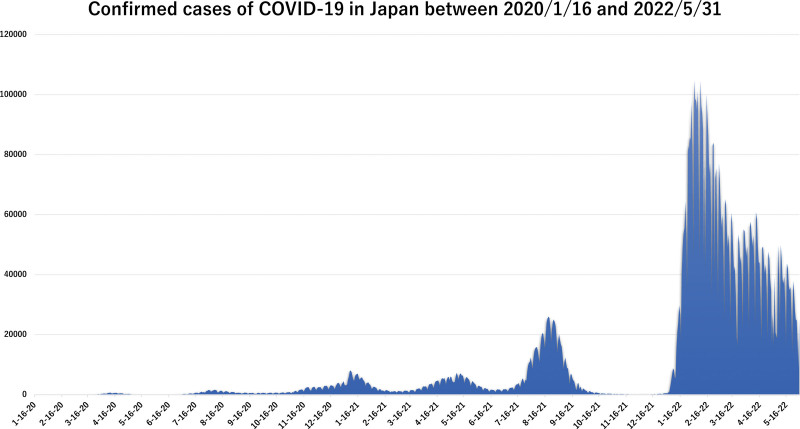
We used COVID-19 statistical data published by the Japanese Ministry of Health, Labour and Welfare to identify peaks and waves (Fig. 1).[2] For statistical analysis, a month (0–6) setting was used for each wave. Specific dates and times were set for each wave and peak month, and statistical analysis was performed using the number at that point in time. We also defined “fiscal year” as follows: the first year of the COVID-19 pandemic as March 2020–March 2021 and the second year as April 2021–May 2022 (Table 1). We assumed the “fiscal year” to be an effect modifier of the COVID-19 pandemic.
Figure 1.
The peaks and waves of the number of COVID-19 patients in Japan extracted from statistical data published by the Japanese Ministry of Health, Labour and Welfare. COVID-19 = coronavirus disease 2019.
Table 1.
Peak months and waves of the COVID-19 pandemic and month in the wave.
| Year* | Wave | Month | ||||||
|---|---|---|---|---|---|---|---|---|
| 0† | 1† | 2 | 3 | 4 | 5 | 6 | ||
| 1st | Mar 2020 | Apr 2020 | May 2020 | Jun 2020 | Jul 2020 | |||
| 1st (2020) | 2nd | Jul 2020 | Aug 2020 | Sep 2020 | Oct 2020 | Nov 2020 | Dec 2020 | |
| 3rd | Dec 2020 | Jan 2021 | Feb 2021 | Mar 2021 | Apr 2021 | |||
| 4th | Apr 2021 | May 2021 | Jun 2021 | Jul 2021 | ||||
| 2nd (2021) | 5th | Jul 2021 | Aug 2021 | Sep 2021 | Oct 2021 | Nov 2021 | Dec 2021 | Jan 2022 |
| 6th | Jan 2022 | Feb 2022 | Mar 2022 | Apr 2022 | May 2022 | |||
COVID-19 = coronavirus disease 2019.
1st year: Mar 2020 to Mar 2021 , 2nd year: Apr 2021 to May 2022 .
Month 0: A month before the peak month (reference); month 1: peak month.
2.1. Statistical analyses
We used linear multi-model with repeated measures (LMMRM) for evaluating the impact of the COVID-19 pandemic on the number of bronchoscopies, outpatients, and admissions per month stratified by “wave of the pandemic” and “fiscal year.” In the LMMRM analysis, “month in each wave” was a fixed effect with repeated measures, “fiscal year” was a fixed effect, and “wave of the pandemic” was a random effect. Fixed effects were analyzed using a mixed model analysis of variance (ANOVA). Post hoc intramonth differences were assessed using t tests, in which multiplicity was adjusted by the Bonferroni method, with month 0 as a reference. The covariance structure of the residuals was set to composite symmetry.
We performed a 3-step analysis to evaluate the association between “fiscal year” and “month in each wave.” First, we performed an LMMRM including only “month in each wave” and “wave of the pandemic.” Second, we added the fixed effect of “fiscal year” and the interaction of “fiscal year” and “month in each wave” effect in the LMMRM model. Finally, we conducted the LMMRM analysis separately for each fiscal year when there was a significant interaction between “fiscal year” and “month in each wave.”
Missing data among some waves in months 4 to 6 were due to the shorter interval between the wave and the next wave. In the LMMRM analysis, missing data were permitted under the assumption that the length of each wave was randomly varied. Throughout the analysis, all tests were 2-sided, and the alpha value was set to 0.05. All statistical analyses were performed using IBM SPSS Statistics for Windows version 28.0 (IBM Corp. Armonk, NY).
3. Results
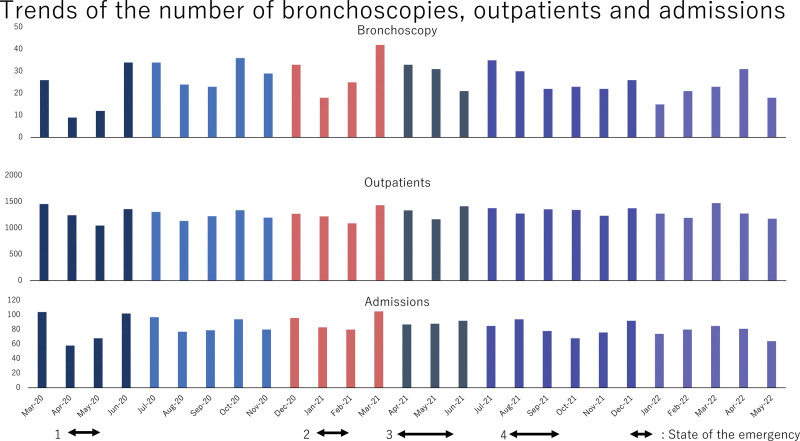
Table 2 shows the number of bronchoscopies, outpatients, and hospital admissions per year before (2017–2019) and during (2020–2021) the COVID-19 pandemic. Figure 2 shows the trajectory of the number of bronchoscopies, outpatients, and hospital admissions per month during the COVID-19 pandemic. The numbers fell the most during the first wave of the COVID-19 pandemic. The general trend is that the number of bronchoscopies decreased during the first and second states of emergency declarations but was unaffected by the third and fourth states.
Table 2.
The number of bronchoscopies, outpatients, and admissions before (2017–2019) and during (2020–2021) the COVID-19 pandemic.
| Year | Bronchoscopy | Outpatients* | Admissions* | |
|---|---|---|---|---|
| Before the COVID-19 pandemic | 2017 | 329 | 16,803 | 1094 |
| 2018 | 367 | 17,783 | 1239 | |
| 2019 | 336 | 18,079 | 1173 | |
| During the COVID-19 pandemic | 2020 | 322 | 15,414 | 1059 |
| 2021 | 280 | 15,623 | 1028 | |
Data are shown as numbers.
COVID-19 = coronavirus disease 2019.
Data are shown as the total number of patients each year.
Figure 2.
The trajectory of the number of bronchoscopies, outpatients, and admissions during the COVID-19 pandemic. Both arrows indicate when a state of emergency should be declared (first to fourth times). COVID-19 = coronavirus disease 2019.
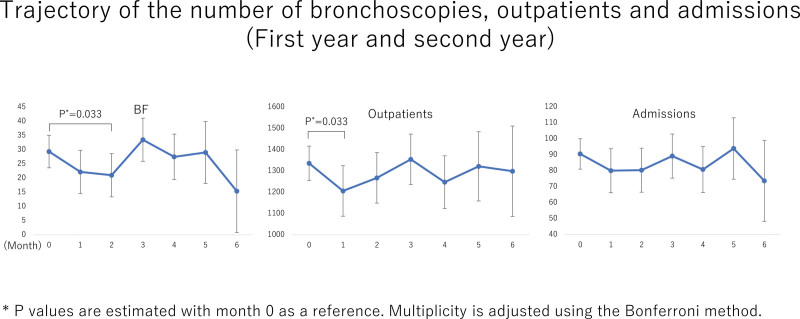
In the first step of LMMRM, mixed-ANOVA indicated significant effects of “month in each wave” on the number of bronchoscopies (P = .021) but no significant effects on the number of outpatients (P = .192) and admissions (P = 348). Figure 3 shows the mean number of bronchoscopies, outpatients, and admissions estimated by the first step of LMMRM. Intramonth multiple comparisons adjusted by the Bonferroni method for the whole study period (first and second year) showed a significant decrease in the number of bronchoscopies between months 0 and 2 (29.3 vs 22.0, P = .033) and the number of outpatients between months 0 and 1 (1336 vs 1206, P = .033).
Figure 3.
The trajectory of the number of bronchoscopies, outpatients, and admissions estimated by the first step of the linear multi-model with repeated measures.
In the second step of LMMRM, the mixed-ANOVA indicated significant interactions of “month in each wave” and “fiscal year” in the number of bronchoscopies (P = .045), outpatients (P = .004), and admissions (P = .005). Therefore, we performed the third step of LMMRM.
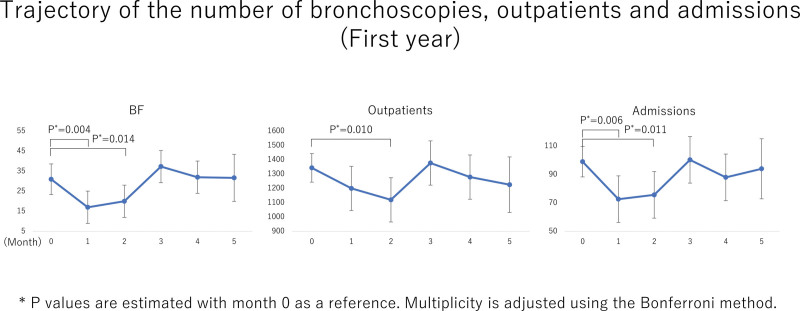
The third step was conducted separately for the first (Fig. 4) and second years (Fig. 5) of the COVID-19 pandemic. In the first year, a mixed-ANOVA indicated significant effects of “month in each wave” on the number of bronchoscopies (P = .003), outpatients (P = .041), and admissions (P = .017). Figure 4 shows the mean number of bronchoscopies, outpatients, and admissions estimated by the third step of LMMRM in the first year. Significant decreases were observed in the number of bronchoscopies between months 0 and 1 (31.0 vs 17, P = .004) or 2 (31.0 vs 20.0, P = .014), outpatients between months 0 and 2 (1344 vs 1120, P = .010), and admissions between months 0 and 1 (99.0 vs 72.7, P = .006) or 2 (99.0 vs 75.7, P = .011). The decrease in the number of outpatients was the greatest in the second month after the first wave. These timings coincided with the first declaration of a state of emergency.
Figure 4.
The third step of linear multi-model with repeated measures conducted for the first year.
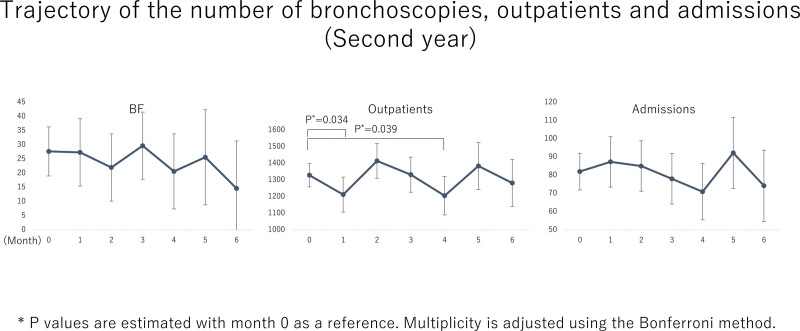
Figure 5.
The third step of linear multi-model with repeated measures conducted for the second year.
In contrast, in the second year of the COVID-19 pandemic (Fig. 5), a mixed-ANOVA indicated a significant effect of “month in each wave” only on the number of outpatients (P = .020), but no significant effects on the number of bronchoscopies (P = .407) and admissions (P = .219). We found that the number of bronchoscopies and admissions was not significantly affected by the waves during the second year of the COVID-19 pandemic. As shown in Figure 5, there were no significant differences in the number of admissions and bronchoscopies between the fourth and sixth waves in the second year. A decrease in the number of outpatients was observed in months 1 (1329 vs 1212, P = .034) and 4 (1329 vs 1205, P = .039).
4. Discussion
In the present study, we identified trends in the number of outpatients, admissions, and bronchoscopies during the COVID-19 pandemic. We found that the numbers were significantly influenced by the first wave of the COVID-19 pandemic, which coincided with the time when the first declaration of a state of emergency was issued. Moreover, the impact of the COVID-19 pandemic, represented by the surge in nationwide COVID-19 incidence, persisted for 1 to 2 months. The time remaining for the impact of the surge was close to the time between the declaration of a state of emergency and its lifting due to a nationwide decline in the incidence of COVID-19.
In Japan, the impact can be seen in the fact that the disastrous situation in Europe and the US was widely reported prior to the first declaration of a state of emergency, which, combined with the fact that COVID-19 is an unknown disease state, fueled public anxiety and fear.[12–14] The psychological impact of information panic (so-called infodemics) in the early stages of the COVID-19 pandemic led to a reduction in visits to medical institutions, leading to a decrease in the number of outpatients, admissions, and bronchoscopies. The number of bronchoscopies and hospital admissions was linked to the number of bronchoscopies performed at our hospital because all bronchoscopies were performed on an admission basis. It has been pointed out that in the early stages of the COVID-19 pandemic, many medical institutions were forced to suspend their health-screening services, which delayed the early detection of cancer.[7] A report from South Korea indicates that the COVID-19 pandemic has led to fewer people being screened for lung cancer and lower detection rates.[15] Also in New York City, it has been reported that lung cancer staging at diagnosis has progressed.[16]
Therefore, it is likely that referrals of patients requiring bronchoscopy decreased around the time health screening ceased.
However, the impact tended to decrease as the number of emergency declarations increased in the latter half of the year. This is thought to be the result of reduced fear of the disease owing to a better understanding of the condition and the public’s familiarity with the disease. It is possible that the public grew tired of the repeated declarations of a state of emergency, making them less effective. In the second year of the COVID-19 pandemic, patients requiring bronchoscopy were also likely to have recovered, as health-screening services reopened in response to the epidemic situation. Despite a decrease in the effect of the COVID-19 pandemic in the second year, only the number of outpatients decreased after the peak month of the pandemic. This may be because the decision to visit an outpatient clinic reflected the patients’ fear of the COVID-19 pandemic more intensively than the decisions of hospital admissions and bronchoscopies. The decision of admission or bronchoscopy is made only when the physician deems it necessary; medical professionals are less fearful of COVID-19 than the general patient population.
Recently, the Japanese Respiratory Society (JRS) published the results of a large survey of its member hospitals.[17] According to this survey, the number of bronchoscopies performed in hospitals with respiratory specialists has decreased by approximately 15% since the COVID-19 pandemic era. The reasons for the decrease were reported to be a decrease in the number of patients, followed by procedural restrictions from institutions. As our hospital does not restrict bronchoscopy, and the number of bronchoscopies is linked to the number of admissions, we believe that the decrease in the number of admissions had a significant impact.
The JRS survey also showed that the main reasons for the decrease in the number of outpatients were longer follow-up intervals and fewer referrals.[17] The factors contributing to the decrease in the number of admissions included the limited number of admission beds due to the acceptance of COVID-19 patients and a decrease in referred patients. As our study only dealt with statistical data and did not examine the circumstances of individual patients, the reasons for this decrease are unknown, but we suspect it was due to a previously reported trend.
In the field of gastroenterology, a prominent decrease in the number of gastroscopy and colonoscopy cases has been reported. As with bronchoscopy, gastrointestinal endoscopy has been reported to be significantly affected by the COVID-19 pandemic.[18] Therefore, the COVID-19 pandemic had a significant impact on endoscopy and bronchoscopy. We believe that understanding the impact of the COVID-19 pandemic on the number of bronchoscopies is crucial for the management of patients with respiratory diseases. This is also a good opportunity to consider how to respond to similar pandemics in the future.
This study has several limitations. The study used statistical data on the number of outpatients, admissions, and bronchoscopies, but it did not examine individual patient characteristics. Hence, it is not possible to analyze the pathological conditions of patients, their psychological situation, or the factors contributing to behavioral change. As this was a single-center study and our hospital treats a large number of malignant tumor cases, there may be gaps in the patient population and age groups compared to other hospitals. The prevalence of COVID-19 varies widely between countries and regions; therefore, the results from our hospital cannot be immediately applied to other regions. In a series of LMMRM analyses, we set the covariance structure of the residuals to composite symmetry, that is, we assumed a normal distribution of residuals. We should have analyzed the validity of this assumption as a sensitivity analysis by performing a series of analyses without making any assumptions about the covariance structure of the residuals. However, we could not perform a sensitivity analysis because of insufficient research duration. To make up for the lack of sensitivity analysis, we strictly adjusted the multiplicity in the post hoc analyses using the Bonferroni method.
In conclusion, we evaluated the impact of the COVID-19 pandemic on the number of outpatients, admissions, and bronchoscopies. The number of bronchoscopies was the most affected by the first wave of the COVID-19 pandemic. Although the number of bronchoscopies was found to be significantly affected in the early stages of the pandemic, the impact of the pandemic was much more limited thereafter. In the early stages of the COVID-19 pandemic, when the pathogenesis and dynamics of the pandemic are not well understood, important tests such as bronchoscopy will inevitably be suppressed. Therefore, it is important to take preventive measures during normal times to respond to future pandemics.
Acknowledgments
The authors thank Kumiko Sano for her assistance in data collection.
Author contributions
Conceptualization: Kohei Fujita.
Data curation: Kohei Fujita, Osamu Kanai, Takanori Ito, Zentaro Saito, Takuma Imakita, Issei Oi, Yuki Yamamoto, Masayuki Hashimoto, Satoru Sawai, Hiroaki Hata, Takao Odagaki, Tadashi Mio.
Formal analysis: Kohei Fujita, Osamu Kanai, Tadashi Mio.
Funding acquisition: Kohei Fujita, Osamu Kanai, Tadashi Mio.
Investigation: Kohei Fujita, Osamu Kanai, Tadashi Mio.
Methodology: Kohei Fujita, Osamu Kanai, Tadashi Mio.
Project administration: Kohei Fujita, Osamu Kanai, Takanori Ito, Zentaro Saito, Takuma Imakita, Issei Oi, Yuki Yamamoto, Masayuki Hashimoto, Satoru Sawai, Takao Odagaki, Tadashi Mio.
Resources: Kohei Fujita, Osamu Kanai.
Software: Kohei Fujita, Osamu Kanai, Tadashi Mio.
Supervision: Kohei Fujita, Osamu Kanai, Hiroaki Hata, Takao Odagaki, Tadashi Mio.
Validation: Kohei Fujita, Osamu Kanai.
Visualization: Kohei Fujita, Osamu Kanai.
Writing – original draft: Kohei Fujita.
Writing – review & editing: Kohei Fujita, Osamu Kanai, Takanori Ito, Zentaro Saito, Takuma Imakita, Issei Oi, Yuki Yamamoto, Masayuki Hashimoto, Satoru Sawai, Hiroaki Hata, Takao Odagaki, Tadashi Mio.
Abbreviations:
- ANOVA
- analysis of variance
- COVID-19
- coronavirus disease 2019
- JRS
- Japanese Respiratory Society
- LMMRM
- linear multi-model with repeated measures
KF and OK contributed equally to this work.
The authors have no funding to disclose.
This study was approved by the National Hospital Organization Kyoto Medical Center institutional review board (approval number: 21-061).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
How to cite this article: Fujita K, Kanai O, Ito T, Saito Z, Imakita T, Oi I, Yamamoto Y, Hashimoto M, Sawai S, Hata H, Odagaki T, Mio T. Impact of the COVID-19 pandemic on the trajectory of the number of bronchoscopies performed in a tertiary hospital in Kyoto city. Medicine 2023;102:21(e33918).
Contributor Information
Osamu Kanai, Email: okanai.kmc@gmail.com.
Takanori Ito, Email: takai.med.23@gmail.com.
Zentaro Saito, Email: szsghaj7@gmail.com.
Issei Oi, Email: isseioi@kuhp.kyoto-u.ac.jp.
Yuki Yamamoto, Email: zyuki@hilung.com.
Masayuki Hashimoto, Email: mhashi77@gmail.com.
Satoru Sawai, Email: ssawai456059@gmail.com.
Hiroaki Hata, Email: hhata-kyt@umin.ac.jp.
Takao Odagaki, Email: takao-odagaki@umin.ac.jp.
Tadashi Mio, Email: tmio.kmc@gmail.com.
References
- [1].World Health Organization COVID-19 situation reports. 2021. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. [access date November 22, 2022]
- [2].diseases situation in Japan. 2021. Available at: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000164708_00079.html. [access date November 22, 2022]
- [3].Mehta S, Machado F, Kwizera A, et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med. 2021;9:226–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Reschen ME, Bowen J, Novak A, et al. Impact of the COVID-19 pandemic on emergency department attendances and acute medical admissions. BMC Emerg Med. 2021;21:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020;1059:1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Okuyama A, Watabe M, Makoshi R, et al. Impact of the COVID-19 pandemic on the diagnosis of cancer in Japan: analysis of hospital-based cancer registries. Jpn J Clin Oncol. 2022;52:1215–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Terashima T, Tsutsumi A, Iwami E, et al. Delayed visit and treatment of lung cancer during the coronavirus disease 2019 pandemic in Japan: a retrospective study. J Int Med Res. 2022;50:030006052210973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lentz RJ, Colt H. Summarizing societal guidelines regarding bronchoscopy during the COVID‐19 pandemic. Respirology. 2020;25:574–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wahidi MM, Shojaee S, Lamb CR, et al. The use of bronchoscopy during the coronavirus disease 2019 pandemic. Chest. 2020;158:1268–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Luo F, Darwiche K, Singh S, et al. Performing bronchoscopy in times of the COVID-19 pandemic: practice statement from an international expert panel. Respiration. 2020;99:417–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Information about 2019 novel coronavirus (COVID-19) infection in Kyoto City. Available at: https://www.pref.kyoto.jp/kikikanri/coronamatome.html.
- [12].Jia H, Guerin RJ, Barile JP, et al. National and state trends in anxiety and depression severity scores among adults during the COVID-19 pandemic – United States, 2020–2021. MMWR Morb Mortal Wkly Rep. 2021;70:1427–32. [DOI] [PubMed] [Google Scholar]
- [13].Kujawa A, Green H, Compas BE, et al. Exposure to COVID‐19 pandemic stress: associations with depression and anxiety in emerging adults in the United States. Depress Anxiety. 2020;37:1280–8. [DOI] [PubMed] [Google Scholar]
- [14].Awano N, Oyama N, Akiyama K, et al. Anxiety, depression, and resilience of healthcare workers in Japan during the coronavirus disease 2019 outbreak. Intern Med. 2020;59:2693–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Duong TL, Lee N, Kim Y, et al. Assessment of the fear of COVID-19 and its impact on lung cancer screening participation among the Korean general population. Transl Lung Cancer Res. 2021;10:4403–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Flores R, Alpert N, McCardle K, et al. Shift in lung cancer stage at diagnosis during the COVID-19 pandemic in New York City. Transl Lung Cancer Res. 2022;11:1514–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Yamane M, Yokoyama A. Impact of coronavirus disease 2019 on respiratory care in Japan: a nationwide survey by the Japanese Respiratory Society. Respir Investig. 2022;60:640–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Castonguay M, el Sayed R, Richard C, et al. COVID-19 impact on diagnosis and staging of colorectal cancer: a single tertiary canadian oncology center experience. Curr Oncol. 2022;29:3282–90. [DOI] [PMC free article] [PubMed] [Google Scholar]