Abstract
Background and Aims:
Inguinal hernia repair is a common surgical procedure. We compared the analgesic efficacy of ultrasound-guided anterior quadratus lumborum (QL) block versus ilioinguinal/iliohypogastric (II/IH) nerve block in pediatric patients undergoing open inguinal hernia repair.
Material and Methods:
It was a prospective randomized study in which 90 patients of 1-8 years of age were randomly assigned into control (general anesthesia only), QL block, and II/IH nerve block groups. Children’s Hospital Eastern Ontario Pain Scale (CHEOPS), perioperative analgesic consumptions, and time to first analgesic request were recorded. The normally distributed quantitative parameters were analyzed by one-way ANOVA with post-hoc Tukey’s HSD test while parameters that did not follow a normal distribution and the CHEOPS score were analyzed using the Kruskal-Wallis test followed by the Mann-Whitney U test with Bonferonni correction for post-hoc analysis.
Results:
In the 1st 6h postoperative, the median (IQR) CHEOPS score was higher in the control group than II/IH group (P = 0.000) and QL group (P = 0.000) while comparable between the latter two groups. CHEOPS scores were significantly lower in the QL block group than the control group and II/IH nerve block group at 12 and 18h. The intraoperative fentanyl and postoperative paracetamol consumptions in the control group were higher than II/IH and QL groups while lower in QL than II/IH group.
Conclusion:
Ultrasound-guided QL and II/IH nerve blocks provided effective postoperative analgesia in pediatric patients undergoing inguinal hernia repair with lower pain scores and less perioperative analgesic consumptions in the QL block group compared to II/IH group.
Keywords: Hernia, inguinal, pain, postoperative
Introduction
Inguinal hernia repair is one of the most commonly performed surgical procedures in children.[1] Ilioinguinal/iliohypogastric (Il/IH) nerve block is a frequently used analgesic modality following such procedures.[2] The escalation in the use of ultrasound guidance has led to performing this technique with greater success rates, smaller volumes, and lower risk of potential complications.[3,4]
Quadratus lumborum (QL) block; originally described by Blanco[5] as a posterior approach to transversus abdominis plane (TAP) block; has experienced several modifications and currently, four types of the block are described depending on the site of local anesthetic administration. Anterior QL block involves the injection of local anesthetic in the fascial plane between the psoas major (PM) muscle and QL muscle[6] with subsequent cranial spread under the medial and lateral arcuate ligaments posterior to the fascia transversalis and thereby into the thoracic paravertebral space posterior to the endothoracic fascia.[7] QL block has gained popularity as one of the perioperative regional analgesic techniques in patients undergoing abdominal and hip surgery.[8,9]
We hypothesized that the QL block would be a more effective analgesic technique than the II/IH nerve block in pediatric patients undergoing open unilateral inguinal hernia repair.
We compared the effects of ultrasound-guided anterior QL block to that of the ultrasound-guided II/IH nerve block on the 1st 24 h postoperative CHEOPS score as a primary outcome and on the total postoperative rescue analgesic consumption as a secondary outcome.
Material and Methods
After obtaining approval from the Hospital Ethics Committee (32214/03/18), registration in PACTR trials registry (PACTR201807311514045,) and informed written parental consent, this prospective controlled randomized double-blinded study was conducted. The patients were recruited between September 2019 and April 2020. Every patient’s parents received an explanation for the purpose of the study during the pre-anesthetic consultation.
Children aged 1-8 years, of either gender, ASA I-II, undergoing elective unilateral open inguinal hernia repair were enrolled in the study. The exclusion criteria were parental refusal, children with any contraindications to regional anesthesia e.g. coagulation disorders or skin infection at the planned injection site, patients with a developmental or mental delay, or known hypersensitivity to the study drug. The patients were randomly allocated into three groups. Randomization was performed using computer-generated sequences and concealed in sealed opaque envelopes.
In the control group, patients received general anesthesia only. In QL block group, the patients received ipsilateral ultrasound-guided QLblock after induction of general anesthesia while in the IL/IH nerve block group, the patients received ipsilateral ultrasound-guided II/IH nerve block after induction of general anesthesia.
All children were premedicated orally with midazolam 0.5 mg/kg 30 min prior to surgery and monitored by 5 lead ECG, pulse oximetry, non-invasive blood pressure, capnography, and temperature. The technique of general anesthesia and postoperative analgesia was standardized for all patients. General anesthesia was induced using 8% sevoflurane in an air-oxygen mixture. After intravenous (IV) atracurium 0.5 mg/kg, orotracheal intubation was performed. Anesthesia was maintained with a mixture of air- oxygen (50-50%), and 2% sevoflurane inhalation. After induction of general anesthesia, all blocks were performed by the same anesthesiologist experienced in the ultrasound-guided regional anesthetic techniques who had no further role in the study. The surgical incision was allowed about 15 min after block administration. Muscle relaxation was maintained during the procedure with atracurium. Patients were mechanically ventilated with the ventilatory parameters adjusted to maintain ETCO2 at 4.6 ± 0.25 kPa. IV fentanyl 0.5 m/kg was administered in case of inadequate analgesia as detected by more than 20% increase in heart rate (HR) or mean arterial blood pressure. Total intraoperative fentanyl consumption was recorded. The inhalational anesthetic was discontinued at the end of the surgical procedure. Extubation was performed when spontaneous breathing is adequate and following prompt reversal.
After the end of the surgery, patients were transferred to the PACU where HR, respiratory rate, SpO2 and systolic, diastolic, and mean arterial blood pressures were monitored, and any changes were recorded immediately. Quality of analgesia was assessed using the Children’s Hospital Eastern Ontario Pain Scale (CHEOPS).[10] Routine postoperative analgesia was administered in the form of diclofenac suppository 25 mg starting at the end of surgery and repeated/8 hourly thereafter. Paracetamol (perfalgan) 15 mg/kg IV was given as rescue analgesia if CHEOPS score >6. Any adverse events as hypotension, nausea, vomiting, or local anesthetic toxicity were recorded. All intraoperative and postoperative parameters were assessed by a dedicated anesthesiologist blinded to group allocation. The primary outcome was postoperative pain score in the 1st 24 h. CHEOPS score was assessed immediately after transfer to PACU, at 1h, 2h, 4h, 6h, 12h, 18h, and 24 h. The secondary outcomes included the total postoperative rescue analgesic consumption in the 1st 24h.
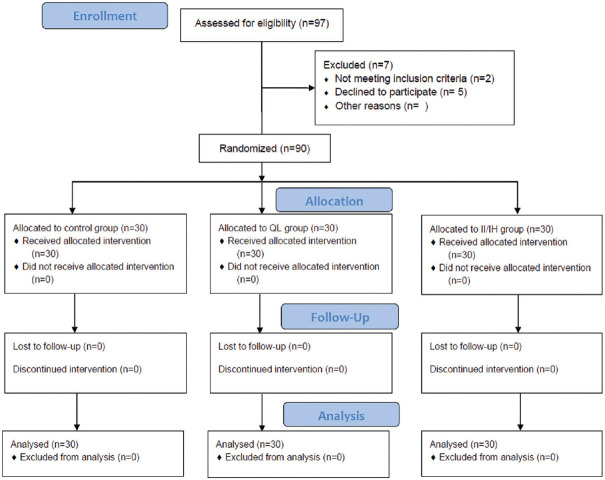
To perform the QL block, with the patient in the lateral decubitus position and under aseptic conditions, a linear 6–13 MHz ultrasound probe (Sono Site Edge, Bothell, Washington) was placed transversely to the abdominal flank. QL muscle, PM muscle, erector spinae muscle, and transverse process of L4 vertebra are identified through visualization of the Shamrock sign where the three muscles form the leaves and the transverse process forms the stem of clover. As previously described by Børglum et al.[11] a 22G, 50 mm needle (Visioplex, Vygon, France) was inserted using the in-plane technique and preceded further into the fascia between the QLM and PM muscle. After confirmation of needle tip position using hydrolocation with 1 ml local anesthetic solution, 0.3 ml/kg bupivacaine 0.25% was injected. The total dose of bupivacaine would not exceed 2 mg/kg [Figure 1].
Figure 1.
Ultrasound-guided demonstration of the quadratus lumborum block. (a) Ultrasonographic anatomy: QL (quadratus lumborum muscle), PM (psoas major muscle), ES (Erector Spinae muscle), LD (latissimus dorsi muscle), EO (external oblique muscle), TP (Transverse processes of the L4 vertebra). (b) needle location indicated by arrows with local anesthetic (LA) deposited into the fascia between the QLM and PM muscle
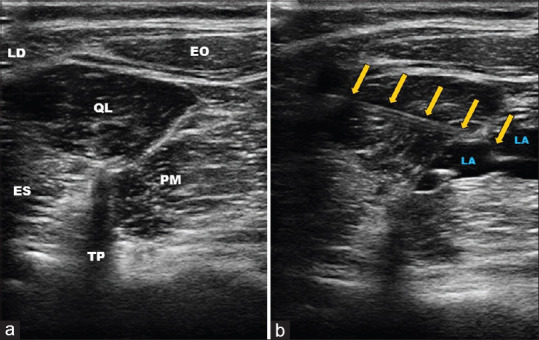
To perform the II/IH nerve block, under aseptic conditions, a linear 6–13 MHz ultrasound probe (Sono Site Edge, Bothell, Washington) was placed at the level of the anterior superior iliac spine to identify the targeted nerves and surrounding anatomical structures. A 22G, 50mm needle (Visioplex, Vygon, France) was advanced using an in-plane technique till the tip of the needle became into a position immediately adjacent to the nerves in the space between the internal oblique and the transverse abdominis muscle.[4]At this position, 0.3 ml/kg of 0.25% bupivacaine was injected under direct visualization.The total dose of bupivacaine would not exceed 2 mg/kg [Figure 2].
Figure 2.
Ultrasound-guided demonstration of the ilioinguinal/iliohypogastric nerve block.(a) ultrasonographic anatomy: EO (externaloblique muscle), IO (internal oblique muscle), TA (transversus abdominis muscle), ASIS (anterior superior iliac spine). Arrow represents the ilioinguinal/iliohypogastric nerves.(b) needle location indicated by arrows with local anesthetic (LA) deposited adjacent to the nerves in the space between the internal oblique and the transverse abdominis muscle
The sample size was calculated using G* Power3 program (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). Postoperative pain score in the 1st 24h in our pilot study (performed on 15 patients) was 7.08 ± 2.68 in the control group, 6.18 ± 1.96 in the Ilioinguinal/iliohypogastric group and 5.05 ± 1.06 in the QLB group. The sample size calculation was based on a One-way ANOVA test of postoperative pain score. Assuming the difference of postoperative pain score means, a pooled SD of 2.01 and effect size of 0.41, at least 26 patients were needed in each group at α error 0.05 and power of the study 90%.
Statistical analysis
We used SPSS 16 software (SPSS Inc., Chicago, IL, USA) for statistical analysis. The Shapiro-Wilk test and the visualization of the histogram were utilized to verify the assumption of normality. The quantitative parameters that were normally distributed were expressed as mean ± SD and analyzed by One-way ANOVA with post-hoc Turkey’s HSD Test while the parameters that didn’t follow the normal distribution (intra-operative fentanyl consumption, postoperative rescue analgesic consumption, and the time to 1st rescue administration) and the CHEOPS score were expressed as median with interquartile range and analyzed using the Kruskal-Wallis test followed by the Mann–Whitney U test with Bonferonni correction for post-hoc analysis (for pairwise comparisons). Categorical data were described as numbers or frequencies (%) and the Chi-square test was used for comparison between groups. The mean time to first analgesic administration was analyzed by Kaplan–Meier survival analysis and log-rank statistics. The nature of the hypothesis testing was 2-sided, and P value <0.05 was considered significant.
Results
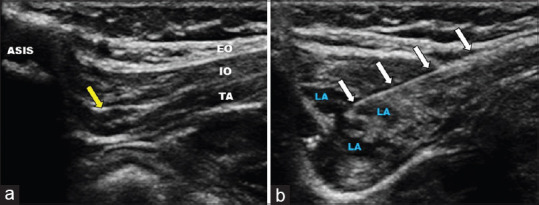
Ninety-seven children were evaluated for eligibility; 2 patients didn’t match the inclusion criteria and 5 patients’ parents refused to participate. 90 patients were enrolled in the study and allocated in three groups of 30 patients each [Figure 3].
Figure 3.
CONSORT flow diagram of participants through each stage of the randomized trial
Demographic data regarding the age, weight, and gender were comparable between the three groups (P = 0.632, 0.585, and 0.227 respectively) [Table 1].
Table 1.
Demographic data, duration of surgeryand perioperative analgesic consumption in the studied groups
| Control group | Ilioinguinal/Iliohypogastric nerve block | Quadratus lumborum block | P | P1 | P2 | P3 | |
|---|---|---|---|---|---|---|---|
| Age (years) | 3.67±1.71 | 3.40±1.75 | 3.80±1.45 | ||||
| Gender M/F | 28/2 | 27/3 | 30/0 | ||||
| Weight (Kg) | 15.90±3.73 | 15.20±3.81 | 16.13±3.32 | ||||
| Duration of surgery (min) | 51.93±7.31 | 50.67±7.21 | 48.80±6.23 | ||||
| Intraoperative Fentanyl consumption (µg) | 8 (4.5-9.25) | 0.0 (0.0-9.0) | 0.0 (0.0-0.0) | <0.001 | 0.027 | <0.001 | 0.021 |
| Postoperative paracetamol consumption (mg/kg) | 30 (15-45) | 0.0 (0.0-30.0) | 0.0 (0.0-0.0) | <0.001 | 0.006 | <0.001 | 0.009 |
| Time to first rescue analgesia requirement (min) | 60 (5-120) | 380 (330-457.5) | 860 (720-1080) | <0.001 | <0.001 | <0.001 | 0.003 |
Data presented as mean±SD, patient number (%) or median (interquartile range). P presented the comparison among the three groups. P1 presented the comparison between the control group and the ilioinguinal/iliohypogastricgroup. P2 presented the comparison between the control group and the quadratus lumborum group. P3 presented the comparison between the ilioinguinal/iliohypogastricgroup and quadratus lumborumgroup. P<0.05 denotes statistical significance
On admission to PACU, postoperative CHEOPS score was significantly higher in the control group than the II/IH nerve block group (P = 0.003) and the QL block group (P = 0.000) without a significant difference between the II/IH nerve block group and the QL block group (P = 0.999). For the 1st six-hour postoperative, the median postoperative CHEOPS score was higher in the control group [6.0 (5.0-7.25)] than the II/IH nerve block group [5.0 (5.0-6.0)] (P = 0.000) and the QL block group [5.0 (5.0-5.0)], (P = 0.000) at the same times, the median postoperative CHEOPS score was comparable between the II/IH nerve block group and the QL block group (P = 0.135) [Figure 4].
Figure 4.
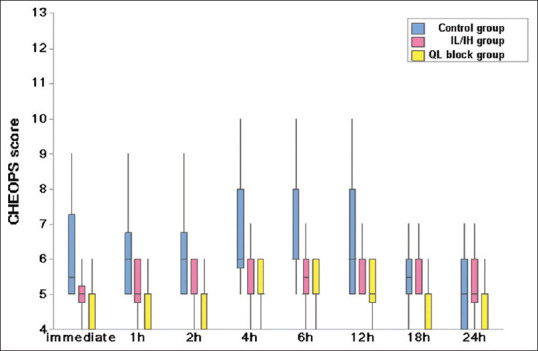
Children’s Hospital Eastern Ontario Pain Scale (CHEOPS) in the studied groups
At 12 and 18 h postoperative, the postoperative CHEOPS scores were significantly lower in the QL block group than the control group and the II/IH nerve block group while the comparison of the postoperative CHEOPS scores was insignificantly different between the control group and the II/IH nerve block group at these times (P = 0.21 and 0.717 respectively). At 24h postoperative, the postoperative CHEOPS score was comparable among the three groups [refer to Figure 4].
Twenty-six patients in the control group received postoperative rescue analgesic versus 14 patients in the II/IH nerve block group (P = 0.003) and 5 patients in the QL block group (P = 0.000). The median (IQR) postoperative rescue analgesic consumption in the control group [30 (15-45)] was significantly higher than that in II/IH nerve block group [0.0 (0.0-30.0)] (P = 0.006) and that in the QL block group [0.0 (0.0-0.0)] (P = 0.000). The postoperative rescue analgesic consumption was significantly higher in the II/IH nerve block group than theQL blockgroup (P = 0.009) [refer to Table 1].
The median (IQR) time to the 1st rescue analgesia administration was significantly longer in the QL blockgroup [860 (720-1080)] than that of the control group [60 (5-120)] and the II/IH nerve block group[380 (330-457.5)] (P = 0.000, P = 0.003 respectively). The median time to the 1st rescue analgesia administration was significantly longer in the II/IH than in the control group (P = 0.000) refer to Table 1 and Figure 5.
Figure 5.
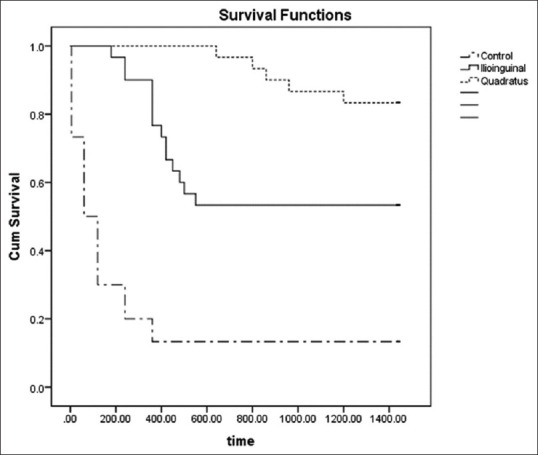
Kaplan-Meier curve for the time to 1st rescue analgesic administration
Twenty-three patients in the control group, 10 patients in the II/IH nerve block group, and 2 patients in the QL block group received intraoperative fentanyl. The median (IQR) intraoperative fentanyl consumption in the control group [8 (4.5-9.25)] was significantly higher than that in the II/IH nerve block group [0.0 (0.0-9.0)] (P = 0.027) and that in the QL block group [0.0 (0.0-0.0)] (P = 0.000). The intraoperative fentanyl consumption was lower in the QL block group than the II/IH nerve block group (P = 0.021) refer to Table 1.
Five patients developed postoperative nausea and vomiting in the control group compared to 3 patients in II/IH nerve block group and 3 patients in the QL block group (P = 0.661).
Discussion
The results of the present study revealed that the QL block provided lower pain scores, longer duration of analgesia, and less consumption of postoperative paracetamol in the first 24 postoperative hours and intraoperative fentanyl compared to the II/IH nerve block. Both techniques provided better analgesia than the control group.
Various regional anesthesia techniques have been investigated for hernia repair in pediatric age groups, such as the caudal block,[12] TAP block,[13] QL block,[14] and II/IH nerve block.[2]
QL blocks have been proven to provide analgesia for pediatric patients undergoing abdominal and hip surgery.[8,9,14] Aksu et al.[8] compared the analgesic efficacy of the ultrasound-guided QL block to that of the ultrasound-guided erector spinae plane block in children undergoing lower abdominal surgeries and they stated that both techniques provided similar postoperative analgesia that extended for more than 24 h postoperative. The longer duration noted by Aksu et al.[8] compared to our trial may be explained by the different local anesthetic volumes and the different types of surgery involved in their study. Öksüz et al.[14] demonstrated that the QL block provided more effective and prolonged postoperative analgesia than the TAP block in children undergoing unilateral inguinal hernia repair or orchiopexy. They, however, used a different approach to QL block. Compared to the anterior approach used in our study which involves the injection of local anesthetic in the fascial plane between the psoas major (PM) muscle and QL muscle, they used the QL2 block (posterior QL block) in which the point of injection was moved from the anterolateral side of the QL muscle to the posterior wall and positioned between the posterior edge of the QL and the thoracolumbar fascia.
Ultrasound-guided QL block provided more effective and prolonged analgesia than ultrasound-guided II/IH nerve block with respect to the pain scores during the 1st 24 postoperative hours and postoperative and intraoperative analgesic consumption. This more effective analgesia may be attributed to blockage of the genital branch of the genitofemoral nerve needed during inguinal herniorrhaphy to decrease the pain induced by traction of the hernia sac[15] as well as the more extensive sensory block obtained with the QL block.
The true mechanism of analgesia provided by QL block remains a matter of debate. The anterior QL block approach targets injection of local anesthetic between the QL and PM muscles with subsequent cranial spread beneath the medial and lateral arcuate ligaments posterior to the fascia transversalis (anterior layer of the thoracolumbar fascia (TLF)), hence, spreading into the thoracic paravertebral space posterior to the endothoracic fascia.[7,16] However, other Cadaveric studies of the anterior approach of QL block demonstrated injectate spread either confined to the lumbar paravertebral spaces alone or together with the lumbar nerve roots within the psoas muscle compartment, implying probable efficacy for hip procedures.[17,18] Thus, the anterior QL block can produce T10 to L4 analgesia.[18] However, another cadaveric model examined the injection of contrast into the area around QL muscle and found that it did not spread into the paravertebral space and that the contrast injected into the paravertebral space did not spread around QL muscle.[19] An additional mechanism of action can be explained by the anatomical–histological features of the TLF as in the superficial layer of the TLF, there is a thick network of sympathetic neurons. In the fascia, there are high-threshold and low-threshold mechanoreceptors as well as pain receptors. These receptors play a role in the development of both acute and chronic pain. The QL block analgesia could be, at least partially, explained by the blockade of these receptors.[20,21] Those data indicate that the QL block can provide both somatic and visceral analgesia.[6]
Ultrasound-guided II/IH nerve block has gained popularity for pediatric patients undergoing inguinal hernia repair owing to its efficacy and safety.[2-4,22] However, Ohashi et al.[1] found that ultrasound-guided II/IH nerve block reduced the amount of required intra-operative sevoflurane but did not reduce postoperative pain. Contrary to other studies that reported the postoperative analgesic efficacy of ultrasound-guided II/IH nerve block, they reported that the primary outcome of their study was to evaluate the emergence delirium at 30 min after the emergence of general anesthesia and explained that the calculated sample size was not sufficient to detect differences in postoperative pain.
No block-related complications were observed in our studied groups.Complications such as colonic puncture[23] and inadvertent femoral block[24,25] have been reported in the II/IH nerve block, and the use of the ultrasound guidance for block performance has decreased these potential risks.
Limitations
Our study is limited by the relatively small sample size and the lack of sensory block assessment. In addition, we evaluated only one approach of the QL blockin which the local anesthetics were injected between the QLmuscle and the PM muscle.
Conclusions
Ultrasound-guided QL and II/IH nerve blocks provided effective postoperative analgesia compared to the control group with comparable pain scores between both groups during the first 6 postoperative hours. CHEOPS scores were significantly lower in the QL block group than II/IH nerve block group at 12 and 18 h postoperative. In addition, QL block was associated with less perioperative analgesic consumptions compared to II/IH nerve block group.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ohashi N, Denda S, Furutani K, Yoshida T, Kamiya Y, Komura R, et al. Ultrasound-guided ilioinguinal/iliohypogastric block did not reduce emergence delirium after ambulatory pediatric inguinal hernia repair:A prospective randomized double-blind study. Surg Today. 2016;46:963–9. doi: 10.1007/s00595-015-1280-6. [DOI] [PubMed] [Google Scholar]
- 2.Fredrickson MJ, Paine C, Hamill J. Improved analgesia with the ilioinguinal block compared to the transversus abdominis plane block after pediatric inguinal surgery:A prospective randomized trial. PaediatrAnaesth. 2010;20:1022–7. doi: 10.1111/j.1460-9592.2010.03432.x. [DOI] [PubMed] [Google Scholar]
- 3.Willschke H, Bosenberg A, Marhofer P, Johnston S, Kettner S, Eichenberger U, et al. Ultrasonographic guided ilioinguinal/iliohypogastric nerve block in pediatric anesthesia:What is the optimal volume? Anesth Analg. 2006;102:1680–4. doi: 10.1213/01.ane.0000217196.34354.5a. [DOI] [PubMed] [Google Scholar]
- 4.Willschke H, Marhofer P, Bosenberg A, Johnston S, Wanzel O, Cox SG, et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth. 2005;95:226–30. doi: 10.1093/bja/aei157. [DOI] [PubMed] [Google Scholar]
- 5.Blanco R. TAP block under ultrasound guidance:The description of a “non pops technique.”. Reg Anesth Pain Med. 2007;32:130. [Google Scholar]
- 6.Akerman M, Pejčić N, Veličković I. A review of the quadratus lumborum block and ERAS. Front Med (Lausanne) 2018;5:44. doi: 10.3389/fmed.2018.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dam M, Moriggl B, Hansen CK, Hoermann R, Bendtsen TF, Børglum J. The pathway of injectate spread with the transmuscular quadratus lumborum block:A cadaver study. Anesth Analg. 2017;125:303–12. doi: 10.1213/ANE.0000000000001922. [DOI] [PubMed] [Google Scholar]
- 8.Aksu C, Şen MC, Akay MA, Baydemir C, Gürkan Y. Erector spinae plane block vs quadratus lumborum block for pediatric lower abdominal surgery:A double blinded, prospective, and randomized trial. J Clin Anesth. 2019;57:24–8. doi: 10.1016/j.jclinane.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Sato M, Hara M, Uchida O. An antero-lateral approach to ultrasound-guided lumbar plexus block in supine position combined with quadrates lumborum block using single-needle insertion for pediatric hip surgery. Paediatr Anaesth. 2017;27:1064–5. doi: 10.1111/pan.13208. [DOI] [PubMed] [Google Scholar]
- 10.Honarmand A, Safavi MR, Jamshidi M. The preventive analgesic effect of preincisional peritonsillar infiltration of two low doses of ketamine for postoperative pain relief in children following adenotonsillectomy. A randomized, double-blind, placebo-controlled study. Paediatr Anaesth. 2008;18:508–14. doi: 10.1111/j.1460-9592.2008.02461.x. [DOI] [PubMed] [Google Scholar]
- 11.Børglum J, Moriggl B, Jensen K, Lønnqvist PA, Christensen AF, Sauter A, et al. Ultrasound-guided transmuscular quadratus lumborum blockade. Br J Anaesth. 2013;111 https://doi.org/10.1093/bja/el_9919. [Google Scholar]
- 12.Yao Y, Yu C, Zhang X, Guo Y, Zheng X. Caudal and intravenous dexmedetomidine similarly prolong the duration of caudal analgesia in children:A randomized controlled trial. Paediatr Anaesth. 2018;28:888–96. doi: 10.1111/pan.13469. [DOI] [PubMed] [Google Scholar]
- 13.Abu Elyazed MM, Mostafa SF, Abdullah MA, Eid GM. The effect of ultrasound-guided Transversus abdominis plane (TAP) block on postoperative analgesia and neuroendocrine stress response in pediatric patients undergoing elective open inguinal hernia repair. Paediatr Anaesth. 2016;26:1165–71. doi: 10.1111/pan.12999. [DOI] [PubMed] [Google Scholar]
- 14.Öksüz G, Bilal B, Gürkan Y, Urfalioğlu A, Arslan M, Gişi G, et al. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery a randomized controlled trial. Reg Anesth Pain Med. 2017;42:674–9. doi: 10.1097/AAP.0000000000000645. [DOI] [PubMed] [Google Scholar]
- 15.Sasaoka N, Kawaguchi M, Yoshitani K, Kato H, Suzuki A, Furuya H. Evaluation of genitofemoral nerve block, in addition to ilioinguinal and iliohypogastric nerve block, during inguinal hernia repair in children. Br J Anaesth. 2005;94:243–6. doi: 10.1093/bja/aei031. [DOI] [PubMed] [Google Scholar]
- 16.Elsharkawy H, El-Boghdadly K, Kolli S, Esa WAS, DeGrande S, Soliman LM, et al. Injectate spread following anterior subcostal and posterior approaches to the quadratus lumborum block:A comparative cadaveric study. Eur J Anaesthesiol. 2017;34:587–95. doi: 10.1097/EJA.0000000000000680. [DOI] [PubMed] [Google Scholar]
- 17.Adhikary SD, El-Boghdadly K, Nasralah Z, Sarwani N, Nixon AM, Chin KJ. A radiologic and anatomic assessment of injectate spread following transmuscular quadratus lumborum block in cadavers. Anaesthesia. 2017;72:73–9. doi: 10.1111/anae.13647. [DOI] [PubMed] [Google Scholar]
- 18.Carline L, McLeodGA , Lamb C. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. Br J Anaesth. 2016;117:387–94. doi: 10.1093/bja/aew224. [DOI] [PubMed] [Google Scholar]
- 19.Kumar A, Sadeghl N, Wahal C, Gadsden J, Grant SA. Quadratus lumborum spares paravertebral space in fresh cadaver injection. Anesth Analg. 2017;125:708–9. doi: 10.1213/ANE.0000000000002245. [DOI] [PubMed] [Google Scholar]
- 20.Benetazzo L, Bizzego A, De Caro R, Frigo G, Guidolin D, Stecco C. 3D reconstruction of the crural and thoracolumbar fasciae. Surg Radiol Anat. 2011;33:855–62. doi: 10.1007/s00276-010-0757-7. [DOI] [PubMed] [Google Scholar]
- 21.Tesarz J, Hoheisel U, Wiedenhofer B, Mense S. Sensory innervation of the thoracolumbar fascia in rats and humans. Neuroscience. 2011;194:302–8. doi: 10.1016/j.neuroscience.2011.07.066. [DOI] [PubMed] [Google Scholar]
- 22.Jagannathan N, Sohn L, Sawardekar A, Ambrosy A, Hagerty J, Chin A, et al. Unilateral groin surgery in children:Will the addition of an ultrasound-guided ilioinguinal nerve block enhance the duration of analgesia of a single-shot caudal block? Paediatr Anaesth. 2009;19:892–8. doi: 10.1111/j.1460-9592.2009.03092.x. [DOI] [PubMed] [Google Scholar]
- 23.Johr M, Sossai R. Colonic puncture during ilioinguinal nerve block in a child. Anesth Analg. 1999;88:1051–2. doi: 10.1097/00000539-199905000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Shivashanmugam T, Kundra P, Sudhakar S. Iliac compartment block following ilioinguinal iliohypogastric nerve block. Pediatr Anesth. 2006;16:1084–6. doi: 10.1111/j.1460-9592.2006.01925.x. [DOI] [PubMed] [Google Scholar]
- 25.Rosario DJ, Jacob S, Luntley J, Skinner PP, Raftery AT. Mechanism of femoral nerve palsy complicating percutaneous ilioinguinal field block. Br J Anaesth. 1997;78:314–6. doi: 10.1093/bja/78.3.314. [DOI] [PubMed] [Google Scholar]