Abstract
Background
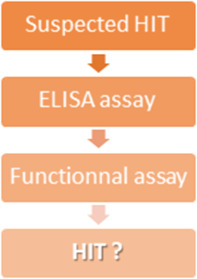
Heparin‐induced thrombocytopenia (HIT) is a severe complication of heparin therapy associated with thrombosis that requires a quick diagnosis. Therefore, laboratory assays must provide an accurate and swift answer. This work aims to evaluate the performances of an ELISA assay, especially when combined with 4T risk score, and a functional assay.
Methods
Data were collected for 894 patients treated by heparin who underwent anticoagulant switch because of HIT suspicion and were examined by a multidisciplinary expert team who confirmed or ruled out HIT diagnosis. All patients were tested for anti‐PF4 IgG with Asserachrom HPIA IgG (ELISA), and 307 were tested with a platelet aggregation test done on platelet‐rich plasma (PRP‐PAT). The 4T risk score was available for 607 of them.
Results
HIT was diagnosed in 232 patients. 4T risk score had a 94.2% negative predictive value (NPV) for risk scores ≤3 and 77.3% for risk scores ≤5. The sensitivity of ELISA was 90.9%, its specificity 79.0%, and its NPV 96.1%. When combined with 4T risk score, its NPV reached 100% and 97% for risk scores ≤3 and ≤5, respectively. PRP‐PAT sensitivity was 70.4%, and its specificity was 92.3%. Combination of ELISA and PRP‐PAT had a 0.7% false‐negative rate.
Conclusion
This study shows that ELISA can rule out HIT with an excellent NPV, especially when combined with the 4T risk score. Nonetheless, it has low specificity; hence, it needs to be associated with a functional assay.
Keywords: adverse effects, heparin, platelet factor 4, thrombocytopenia, thrombosis
Heparin‐induced thrombocytopenia (HIT) is life‐threatening and requires an accurate diagnosis. Therefore, data were examined for 894 patients to determine the performances of laboratory diagnosis of HIT. ELISA had an excellent negative predictive value for low and intermediate (100% and 97.0%) 4T risk scores and the functional assay had a 70.4% sensitivity and 92.7% specificity. These findings support the combination of ELISA and functional assay, with a 0.7% false‐negative rate.
1. INTRODUCTION
Heparin‐induced thrombocytopenia (HIT) is a severe complication of heparin treatment with a significant incidence. Indeed, a meta‐analysis estimated HIT in about 2.6% of unfractionated heparin (UFH) and 0.2% of low‐molecular‐weight heparin (LMWH) treatments. 1 It is mainly caused by IgG antibodies against the complex platelet factor 4 (PF4)/heparin. When those antibodies bound PF4/heparin complexes on platelet surface, their Fc domains activate platelet FCγRIIA receptors, which leads to platelet activation: This may be life‐threatening due to induced thrombotic risk.
Therefore, even though it is recommended to swiftly substitute heparin for another anticoagulant when HIT is suspected, a rapid diagnostic test is desirable. The 4T risk score has an excellent negative predictive value (NPV) for low risk scores (≤3) (NPV ranged from 85% to 99.8% 2 , 3 , 4 , 5 ), but its positive predictive value (PPV) for intermediate or high risk scores remains insufficient 2 , 3 , 5 . Thus, it seems necessary in many cases to confirm or rule out HIT with laboratory assays, such as immunoassays (detection of anti‐PF4 antibodies) or functional assays (detection of platelet activation).
Although immunoassays (ELISA for instance) may rapidly highlight anti‐PF4 antibodies with high sensitivity, they lack specificity 6 , 7 , 8 , 9 as they may detect clinically irrelevant antibodies and are subject to interferences such as antiphospholipid antibodies 10 . Therefore, their use is usually limited to screening tests.
Functional assays are usually regarded as gold‐standard for HIT diagnosis such as Serotonin Release Assay (SRA), platelet aggregation test with platelet‐rich plasma (PRP‐PAT) or with washed platelets (WP‐PAT), heparin‐induced platelet activation test, and so on. Unfortunately, they are time‐consuming, restricted to specialized laboratories, require platelets from healthy donors, and cannot provide quick results. Despite their excellent specificity, functional assays are usually confirmation assays due to their low sensitivity 11 , 12 , 13 , 14 , 15 .
Here, we retrospectively evaluated the performances of the 4T risk score, an ELISA assay, and an in‐house PRP‐PAT.
2. MATERIALS AND METHODS
2.1. Study design and patients
This retrospective study was approved by the institutional ethics board (CE‐2022‐76). Data were collected by the Regional Center of Pharmacovigilance from medical files of patients hospitalized at the University Hospital of Strasbourg between January 2009 and December 2019. Heparin was substituted for another anticoagulant for 1101 patients due to suspected HIT during this period. Patients without complete medical information or laboratory results were excluded from this study.
A multidisciplinary expert group, comprised of clinicians, pathologists, and pharmacists, evaluated the probability of HIT based on clinical (platelet kinetics—including after discontinuation of heparin, sepsis or severe infection, contemporaneous treatments, comorbidities, 4T risk score, 16 etc.) and laboratory results (ELISA, PAT, SRA sent out to another laboratory). HIT was assessed based on consensual decision, and patients were assigned to the HIT or non‐HIT groups.
All 4T risk score, ELISA and PRP‐PAT results were confronted to the expert conclusion and classified as true positive (TP), true negative (TN), false positive (FP) and false negative (FN). Sensitivity, specificity, PPV and NPV of each test were computed.
2.2. Plasma samples
Patient blood was drawn into BD Vacutainer® glass citrated tubes with 0.129 M of trisodium citrate (Becton Dickinson). Platelet‐Poor Plasma (PPP) was then prepared by double centrifugation each at 2500 g for 10 min at 20°C. Plasma aliquots were stored in polypropylene tubes at −20°C.
Platelets from selected healthy donors, previously identified to have platelets reactive to HIT antibodies, were used for the PAT‐PRP. Blood was drawn into BD Vacutainer® glass citrated tubes with 0.129 M of trisodium citrate. Platelet‐Rich Plasma (PRP) was then prepared by centrifugation at 200 g for 10 min at 20°C.
2.3. ELISA
ELISA was systematically performed for every sample sent to our laboratory, regardless of the 4T risk score.
Anti‐PF4 IgG were detected by Asserachrom HPIA IgG ELISA (Diagnostica Stago) according to the manufacturer recommendations. Absorbances were measured using Sunrise microplate reader (Tecan) at 450 nm. ELISA assay positivity was determined by comparison to internal standard absorbances.
2.4. PRP‐PAT
PRP‐PAT was done solely when ELISA was positive and/or in case of strong HIT suspicion. PRP‐PAT was not performed when PPP volume was not sufficient. Briefly, 75 μL of patient PPP and 150 μL of healthy donor PRP were mixed, then platelet aggregation was monitored for 20 min at 37°C with constant stirring on APACT 4004 (LABiTec).
Patients PPPs were tested with two different donor PRPs and with increasing heparin concentrations: 0.5 IU and 1.0 IU/mL of UFH, 0.5 and 1.0 IU/mL of LMWH (Enoxaparin). When significant aggregation (maximal amplitude ≥20%) occurred with any heparin concentration, samples were further tested with 100 IU/mL UFH and physiological serum to confirm the specificity towards heparin.
Healthy donor platelet reactivity was assessed using arachidonic acid at 500 mg/mL. They were also tested with UFH 1 UI/mL and LMWH 1 IU/mL with the donor's own PPP to verify their anergy toward heparin, as well as their reactivity toward in‐house positive control (PPP from HIT‐positive patient).
2.5. Statistical analyses
Contingency tables were established with RP, RN, FN, and FP parameters to determine sensitivity, specificity, NPV, and PPV. ELISA absorbances of HIT and no‐HIT groups were compared with the Student's t‐test.
Analyses were performed with Prism version 6.05 (GraphPad Software).
3. RESULTS
After the exclusion of patients with incomplete information or no available laboratory results, 894 patients were included in this study. The complete cohort description is presented in Table 1. HIT was assessed by the expert group for 232 patients (26.0%).
TABLE 1.
Demographic data
| Demographic data | |
|---|---|
| Age (years) | 0–105 (median: 67.8) |
| Male | 505 (56.5%) |
| Female | 389 (43.5%) |
| Surgery Unit | 149 (16.7%) |
| Medical Unit | 439 (49.1%) |
| Intensive Care Unit | 297 (33.2%) |
| Obstetrics and Gynecology Unit | 9 (1%) |
3.1. 4T risk score
4T risk scores were available within 607 patient's medical records: 207, 322, and 78 had a low, intermediate, and high 4T risk scores, respectively. Based on recommendations from the multidisciplinary expert group, 170 (28%) were assigned to the HIT group.
A strong association was found between 4T risk score and HIT group assignment. Indeed, 6%, 36%, and 64% of patients with low, intermediate, or high 4T risk score had HIT diagnosed, respectively. 4T risk score had 94.2% and 77.3% NPV for score ≤3 and ≤5, respectively, and 64.1% PPV for score ≥6 (see Table 2).
TABLE 2.
Performances of 4T score, IgG anti‐PF4 ELISA assay, and PRP‐PAT
| Criteria | Number +/Total (%) | Sensitivity (95% CI) | Specificity (95% CI) | NPV (95% CI) | PPV (95% CI) |
|---|---|---|---|---|---|
| IgG anti‐PF4+ | 350/894 (39) | 90.9% (86.5–94.3) | 79.0% (75.7–82.1) | 96.1% (94.2–97.6) | 60.3% (CI: 55.0–65.5) |
| 4T ≤ 3 | 207/607 (34) | 92.9% (88.0–96.3) | 44.6% (39.9–49.4) | 94.2% (90.1–97.0) | 39.5% (34.7–44.5) |
| 4T ≤ 5 | 529/607 (87) | 29.4% (22.7–36.9) | 93.6% (90.9–95.7) | 77.3% (75.5–79.0) | 64.1% (53.8–73.2) |
| 4T ≤ 3: IgG anti‐PF4+ | 47/207 (23) | 100% (73.5–100) | 82.1% (75.9–87.2) | 100% (97.8–100) | 25% (13.6–39.6) |
| 4T 4–5: IgG anti‐PF4+ | 158/322 (49) | 95.4% (89.5–98.5) | 74.3% (67.9–80.0) | 97.0% (93.0–99.0) | 65.2% (57.2–72.6) |
| 4T ≥ 6: IgG anti‐PF4+ | 52/78 (67) | 86.0% (73.2–94.2) | 67.9% (47.7–84.1) | 73.1% (52.2–88.4) | 82.7% (69.7–91.8) |
| PRP‐PAT+ | 112/307 (36) | 70.4% (62.2–77.8) | 92.7% (87.6–96.2) | 78.5% (73.8–86.5) | 89.3% (82.7–93.6) |
3.2. ELISA
ELISA was performed for 894 patients. HIT was assessed by the expert group for 232 patients (26.0%), while 346 (39%) had a positive ELISA. ELISA had 90.9% sensitivity, 79.0% specificity, and 96.1% NPV.
4T risk scores combined with ELISA results improved performances: indeed, NPV of 4T risk score ≤5 combined with negative anti‐PF4 IgG was 97% and reached 100% for 4T risk score ≤3 combined with negative anti‐PF4 IgG (see Table 2).
In addition, a strong correlation between ELISA absorbances and HIT diagnosis was found. HIT group mean absorbance was 1.580 (0.198–3.32) compared with only 0.653 (0.164–2.804) in the non‐HIT group (p < 0.001).
3.3. PRP‐PAT
Three hundred and seven patients out of the 894‐patient cohort were tested with PRP‐PAT, and 142 (46.3%) of them were assigned to the HIT group.
PRP‐PAT was positive for 100 HIT patients with 70.4% sensitivity, 92.7% specificity, and 89.3% PPV (see Table 2).
Interestingly, out of the 12 ELISA‐negative HIT patients, 11 were positive when tested with PRP‐PAT. Only one HIT patient was negative with both assays.
Of note, twelve patients had PRP‐PAT false‐positive result. Seventy‐five percent of them had sepsis or severe infections and 25% had disseminated intravascular coagulation (DIC) (Table 3).
TABLE 3.
Conditions of patients having a false‐positive PRP‐PAT result
| Patient | Diagnosis |
|---|---|
| 1 | Low‐grade lymphoma with monoclonal IgM |
| 2 | Staphylococcus aureus pneumonia with mechanical ventilation |
| 3 | Severe sepsis due to Candida tropicalis |
| 4 | Infectious pneumonia (undocumented). Patient had chemotherapy and radiotherapy for pulmonary adenocarcinoma |
| 5 | Rectal neoplasm. Chemotherapy was discontinued 1 month earlier due to cerebral venous thrombosis. |
| 6 | Septic shock (Staphylococcus aureus) with DIC |
| 7 | Metastatic pancreatic adenocarcinoma with DIC |
| 8 | Infectious endocarditis with septic shock due to Streptococcus dysgalactiae and DIC. The patient also underwent aortic surgery |
| 9 | Pneumonia due to Staphylococcus aureus |
| 10 | Sepsis due to Escherichia coli |
| 11 | Hemorrhagic stroke followed by ischemic stroke |
| 12 | Staphylococcus aureus and Klebsiella oxytoca infection on pacemaker with sepsis. |
4. DISCUSSION
Within our monocentric retrospective study on a cohort of 894 patients, we investigated the benefits of laboratory assays to rule out HIT when suspected. We confronted laboratory results to multidisciplinary expert group conclusions based on both clinical and laboratory data and demonstrated the benefit of laboratory assays to rule out HIT. Although low 4T risk‐score NPV was 94.2%, NPV dropped to 77.3% for 4T risk scores ≤5, while ELISA NPV alone remained at 96.1%. Interestingly, a combination of 4T risk scores with ELISA results had a NPV of 100% for low 4T risk scores and 97% for 4T risk score ≤5, which is consistent with previous data. 3 Therefore, we demonstrated that ELISA results are useful to rule out HIT for low and intermediate 4T risk scores.
ELISA also exhibited a good sensitivity (90.9%) but a low specificity (79.0%) as anticipated. Indeed, previous studies demonstrated that immunoassays such as ELISA are prone to false‐positive results, which are usually caused by clinically irrelevant antibodies. Such irrelevant antibodies may be found in autoimmune disorders such as antiphospholipid syndrome or systematic erythematous lupus, 10 , 17 , 18 or even in monoclonal gammopathy of undetermined significance. 19 Likewise, many patients who underwent cardiac surgery develop anti‐PF4 antibodies without any evidence of HIT. 20 , 21 , 22 Therefore, clinicians and pathologists must be aware of those interferences.
ELISA assay had a mediocre NPV (73.1%) for high 4T risk scores with a 9% false‐negative rate. However, we cannot exclude that these patients had anti‐PF4 IgM or IgA, 23 or anti‐IL8 or anti‐NAP1 antibodies. 24 Thus, it appears relevant to systematically perform functional assays for patients with a high 4T risk score but a negative ELISA.
PRP‐PAT performances were appropriate as confirmatory assay. Its specificity was 92.7% with a low sensitivity (70.4%) and 89.3% PPV. Although there is no standardization for PRP‐PAT (selection and number of healthy donors, heparin concentration, duration of the assay, patient PPP / donor PRP ratio, etc.), our results are consistent with two previous studies, which estimated its sensitivity from 39% to 81% 12 , 14 with a specificity between 82 and 100%.
In this study, PAT‐PRP had 10.7% false‐positive rate. This may be explained by several causes. 25 , 26 , 27 , 28 , 29 , 30 Patient's PPP may contain residual thrombin that leads to platelet aggregation. This situation might occur when patients suffer from DIC, 26 , 28 as it was the case for 3 out of 12 patients in our cohort. Furthermore, platelet activation through FCγRIIA may occur in presence of immune complexes 27 , 28 or autoantibodies, for instance in autoimmune disorders such as systematic erythematous lupus. 25 , 27 , 29 Platelet activation may also result from antibodies against class I HLA antigens, 26 , 30 as well as from pathogens (either directly or after IgG opsonization). 27 Of note, in this study, 8 out of 12 patients with PRP‐PAT false‐positive results had a severe infection, most of the time due to Gram‐positive bacteria. Platelet aggregation test with PRP instead of WP might cause decreases in both sensitivity 11 and specificity. WP‐PAT, however, is time‐consuming and more complex to implement, therefore requires a trained staff.
Finally, a combination of screening assay (ELISA) with confirmatory assay (PRP‐PAT)—performed regardless of ELISA results when strong clinical HIT suspicion—seems highly relevant. In our cohort, only one out of 142 (0.7%) HIT patients tested with both assays was not positive for both tests.
Limitations of this study are its retrospective nature, as well as the sole inclusion of patients who underwent anticoagulant switch. HIT prevalence may therefore be higher.
In conclusion, these findings highlight the benefit of combining 4T risk scores with ELISA results to rule out HIT when risk scores are low or intermediate. In addition, confirmatory assays seem to be required because of ELISA low specificity and the risk of nondetection of non‐IgG anti‐PF4 antibodies.
AUTHOR CONTRIBUTIONS
A.H. designed the study, collected and interpreted data, and wrote the article. M.D. collected and interpreted data. J.W. collected data and revised the intellectual content. D.R. provided a critical writing and revised the intellectual content. M.T. collected data and revised the intellectual content. A.L. collected data and revised the intellectual content. C.L. collected data and revised the intellectual content. M.C. collected data. X.D. collected data. T.K. collected data. D.P. collected data. M.S. collected data. L.M. revised the intellectual content. L.S. collected data and revised the intellectual content.
CONFLICT OF INTEREST STATEMENT
The authors have no relevant conflict of interest to declare.
Herb A, Depierreux M, Wimmer J, et al. Laboratory diagnosis of heparin‐induced thrombocytopenia: A retrospective experience. J Clin Lab Anal. 2023;37:e24884. doi: 10.1002/jcla.24884
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Martel N, Lee J, Wells PS. Risk for heparin‐induced thrombocytopenia with unfractionated and low‐molecular‐weight heparin thromboprophylaxis: a meta‐analysis. Blood. 2005;106(8):2710‐2715. [DOI] [PubMed] [Google Scholar]
- 2. Cuker A, Gimotty PA, Crowther MA, Warkentin TE. Predictive value of the 4Ts scoring system for heparin‐induced thrombocytopenia: a systematic review and meta‐analysis. Blood. 2012;120(20):4160‐4167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thawani R, Nannapaneni S, Kumar V, et al. Prediction of heparin induced thrombocytopenia (HIT) using a combination of 4Ts score and screening immune assays. Clin Appl Thromb. 2020;26:1076029620962857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Matsumura Y, Nakada T, Oda S. Relationship between the 4Ts scoring system and the antiplatelet factor 4/heparin antibodies test in critically ill patients. Acute Med Surg. 2013;1(1):37‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Younis M, Ya'qoub L, Ali Z, Grover P, Ya'acoub R, Hamarshi MS. Comparison of a clinical‐laboratory algorithm, 4t and heparin‐induced thrombocytopenia expert probability scores in the diagnosis of heparin‐induced thrombocytopenia in the critical care setting. Am J Blood Res. 2019;9(3):25‐33. [PMC free article] [PubMed] [Google Scholar]
- 6. Nellen V, Sulzer I, Barizzi G, Lämmle B, Alberio L. Rapid exclusion or confirmation of heparin‐induced thrombocytopenia: a single‐center experience with 1,291 patients. Haematologica. 2012;97(1):89‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Warkentin TE, Sheppard JAI, Linkins LA, Arnold DM, Nazy I. High sensitivity and specificity of an automated IgG‐specific chemiluminescence immunoassay for diagnosis of HIT. Blood. 2018;132(12):1345‐1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vianello F, Sambado L, Scarparo P, et al. Comparison of three different immunoassays in the diagnosis of heparin‐induced thrombocytopenia. Clin Chem Lab Med CCLM. 2015;53(2):257‐263. [DOI] [PubMed] [Google Scholar]
- 9. Mardovina T, Chromczak JG, Riley PW. Comparison of two different ELISA Methods for heparin‐induced thrombocytopenia (HIT) screening on an automated ELISA platform. Blood. 2019;134:4935. [Google Scholar]
- 10. Pauzner R, Greinacher A, Selleng K, Althaus K, Shenkman B, Seligsohn U. False‐positive tests for heparin‐induced thrombocytopenia in patients with antiphospholipid syndrome and systemic lupus erythematosus. J Thromb Haemost. 2009;7(7):1070‐1074. [DOI] [PubMed] [Google Scholar]
- 11. Vayne C, Guéry EA, Charuel N, et al. Evaluation of functional assays for the diagnosis of heparin induced thrombocytopenia using 5B9, a monoclonal IgG that mimics human antibodies. J Thromb Haemost. 2020;18(4):968‐975. [DOI] [PubMed] [Google Scholar]
- 12. Brodard J, Alberio L, Angelillo‐Scherrer A, Nagler M. Accuracy of heparin‐induced platelet aggregation test for the diagnosis of heparin‐induced thrombocytopenia. Thromb Res. 2020;185:27‐30. [DOI] [PubMed] [Google Scholar]
- 13. Greinacher A, Amiral J, Dummel V, Vissac A, Kiefel V, Mueller‐Eckhardt C. Laboratory diagnosis of heparin‐associated thrombocytopenia and comparison of platelet aggregation test, heparin‐induced platelet activation test, and platelet factor 4/heparin enzyme‐linked immunosorbent assay. Transfusion (Paris). 1994;34(5):381‐385. [DOI] [PubMed] [Google Scholar]
- 14. Chong BH, Burgess J, Ismail F. The clinical usefulness of the platelet aggregation test for the diagnosis of heparin‐induced thrombocytopenia. Thromb Haemost. 1993;69(4):344‐350. [PubMed] [Google Scholar]
- 15. Samama MM, Elalamy I, Lecrubier C, Potevin F, Horellou MH, Conard J. Heparin‐induced thrombopenia: significance and difficulties of precise identification of the immunologic mechanism. Bull Acad Natl Med. 1998;182(7):1517‐1533. discussion 1534–1536. [PubMed] [Google Scholar]
- 16. Lo GK, Juhl D, Warkentin TE, Sigouin CS, Eichler P, Greinacher A. Evaluation of pretest clinical score (4T's) for the diagnosis of heparin‐induced thrombocytopenia in two clinical settings. J Thromb Haemost. 2006;4(4):759‐765. [DOI] [PubMed] [Google Scholar]
- 17. McRae HL, Moore JW, Ifthikharuddin JJ, Refaai MA. False‐positive heparin‐PF4 latex immunoturbidimetric assay due to lupus anti‐coagulant interference: a case report. Br J Haematol Juill. 2021;194(1):211‐213. [DOI] [PubMed] [Google Scholar]
- 18. Satoh T, Tanaka Y, Okazaki Y, Kaburaki J, Ikeda Y, Kuwana M. Heparin‐dependent and ‐independent anti‐platelet factor 4 autoantibodies in patients with systemic lupus erythematosus. Rheumatol Oxf Engl Sept. 2012;51(9):1721‐1728. [DOI] [PubMed] [Google Scholar]
- 19. Markovic I, Debeljak Z, Bosnjak B, Marijanovic M. False positive immunoassay for heparin‐induced thrombocytopenia in the presence of monoclonal gammopathy: a case report. Biochem. Medica. 2017;27(3):030801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yusuf AM, Warkentin TE, Arsenault KA, Whitlock R, Eikelboom JW. Prognostic importance of preoperative anti‐PF4/heparin antibodies in patients undergoing cardiac surgery. A systematic review. Thromb Haemost Janv. 2012;107(1):8‐14. [DOI] [PubMed] [Google Scholar]
- 21. Everett BM, Yeh R, Foo SY, et al. Prevalence of heparin/platelet factor 4 antibodies before and after cardiac surgery. Ann Thorac Surg. 2007;83(2):592‐597. [DOI] [PubMed] [Google Scholar]
- 22. Bauer TL, Arepally G, Konkle BA, et al. Prevalence of heparin‐associated antibodies without thrombosis in patients undergoing cardiopulmonary bypass surgery. Circulation. 1997;95(5):1242‐1246. [DOI] [PubMed] [Google Scholar]
- 23. Amiral J, Wolf M, Fischer AM, Boyer‐Neumann C, Vissac AM, Meyer D. Pathogenicity of IgA and/or IgM antibodies to heparin–PF4 complexes in patients with heparin‐induced thrombocytopenia. Br J Haematol. 1996;92(4):954‐959. [DOI] [PubMed] [Google Scholar]
- 24. Amiral J, Marfaing‐Koka A, Wolf M, et al. Presence of autoantibodies to interleukin‐8 or neutrophil‐activating peptide‐2 in patients with heparin‐associated thrombocytopenia. Blood. 1996;88(2):410‐416. [PubMed] [Google Scholar]
- 25. Stricker H, Lämmle B, Furlan M, Sulzer I. Heparin‐dependent in vitro aggregation of normal platelets by plasma of a patient with heparin‐induced skin necrosis: specific diagnostic test for a rare side effect. Am J Med. 1988;85(5):721‐724. [DOI] [PubMed] [Google Scholar]
- 26. Minet V, Dogné JM, Mullier F. Functional assays in the diagnosis of heparin‐induced thrombocytopenia: a review. Mol Basel Switz. 2017;22(4):E617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Arman M, Krauel K. Human platelet IgG fc receptor FcγRIIA in immunity and thrombosis. J Thromb Haemost. 2015;13(6):893‐908. [DOI] [PubMed] [Google Scholar]
- 28. Moore JC, Arnold DM, Warkentin TE, Warkentin AE, Kelton JG. An algorithm for resolving ‘indeterminate’ test results in the platelet serotonin release assay for investigation of heparin‐induced thrombocytopenia. J Thromb Haemost. 2008;6(9):1595‐1597. [DOI] [PubMed] [Google Scholar]
- 29. Duffau P, Seneschal J, Nicco C, et al. Platelet CD154 potentiates interferon‐α secretion by Plasmacytoid dendritic cells in systemic lupus erythematosus. Sci Transl Med. 2010;2(47):47ra63. [DOI] [PubMed] [Google Scholar]
- 30. Rijkers M, Saris A, Heidt S, et al. A subset of anti‐HLA antibodies induces FcγRIIa‐dependent platelet activation. Haematologica. 2018;103(10):1741‐1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


