Abstract
Objective
This study was aimed at identifying the potential subgroups of supportive care needs among Chinese patients with colorectal cancer (CRC) through latent class analysis (LCA) and clarifying the characteristics of patients with high needs.
Methods
From January to September 2020, a cross-sectional survey was conducted in the Oncology Department and Radiotherapy Department of four tertiary grade A hospitals in Suzhou by using the general information questionnaire and Comprehensive Needs Assessment Tool for patients with cancer. Potential subgroups of supportive care needs were identified through LCA, and the association between the subgroups and statistical variables was analyzed with chi-square tests to clarify the demographic characteristics of the high-need group. This study was not registered.
Results
A total of 403 patients with CRC were included in the survey. LCA indicated two subgroups of supportive care needs in patients with CRC: a high-need group (51.86% of patients) and a low-need group (48.14% patients). In both groups, the probability of healthcare staff and information needs was high (> 50%). Single/divorced/widowed patients had greater supportive care needs than married patients, and patients with rectal cancer had greater supportive care needs than those with colon cancer.
Conclusions
Patients’ healthcare staff and information needs are of critical importance. Focus should be placed on unmarried, patients with rectal cancer, as well as those receiving chemotherapy plus radiotherapy or palliative treatment.
Keywords: Colorectal cancer patients, Supportive care, Needs assessment, Population characteristics, Latent class analysis
1. Introduction
Colorectal cancer (CRC) poses an enormous disease burden and has become a major public health problem. According to the global cancer burden data from the International Agency for Research on Cancer, in 2020, the number of new CRC cases was 1.93 million, and the number of CRC deaths was 0.94 million.1 With the continuing development of China's economy, diet structures and eating habits have substantially changed. People in China have shifted toward consuming more high-fat food (red meat, fried food, pastries, etc.), and more alcohol and tobacco, thereby increasing CRC incidence and mortality.2, 3, 4 According to the most recent Chinese cancer data, the number of new CRC cases was 0.56 million, accounting for one-third of the global population with CRC, and the number of deaths was 0.29 million.1
With advances in diagnosis and treatment technology, the 5-year survival rate of patients with CRC continues to increase. This rate is approximately 64% in the United States and >60% in European countries; in recent years, this rate has increased by more than 10% in China, to approximately 58% for colon cancer and 57% for rectal cancer.5 CRC is usually treated by surgery supplemented with radiotherapy and chemotherapy. Surgical treatments remove the primary tumor and the affected lymphatic drainage area and may cause pelvic nerve damage, abnormal intestinal activity, and changes in sexual function; moreover, radiotherapy and chemotherapy frequently result in fatigue, pain, diarrhea, numbness, alopecia, and other toxic adverse effects.6 Pathophysiological changes caused by various clinical factors can lead to changes in physical function, mental state, and social function among CRC survivors. Meanwhile, in long-term treatment and rehabilitation, survivors have multiple and critical supportive care needs. Supportive care needs are defined as various types of help and services required by individuals coping with the effects experienced during multiple treatment stages, such as cancer diagnosis, treatment, remission, and deterioration. Their scope includes “needs beyond surgery, radiotherapy and chemotherapy, drugs, and other treatments.”7,8 On the basis of the existing literature, the primary supportive care needs of patients with cancer can be broadly categorized into physical, psychological, informational, social, and practical needs.9
Unmet supportive care needs are closely associated with poor health condition and can cause psychological distress and decrease patients' quality of life.10, 11, 12 According to the supportive care needs of patients with cancer, the development and provision of corresponding care plans will help make better use of limited medical resources and achieve patient-centered care.13 However, at present, research on supportive care needs in China has focused on patients with comprehensive types of cancer, gynecological malignancies, breast cancer, lung cancer, and esophageal cancer,14, 15, 16, 17, 18 whereas patients with CRC have received relatively little attention. In view of the large number of CRC survivors and the various problems that the patients may experience in the course of disease, identifying and analyzing the supportive care needs of patients with CRC is necessary.
In addition, when the Chinese researchers have analyzed the supportive care needs of patients with cancer, they have often studied patients as a whole, without considering the heterogeneity among individuals. In fact, even if two individuals in the same group share the same needs assessment score, they may respond differently to each item, and these differences may be critical for effective intervention. Latent class analysis (LCA) is a well-validated statistical technique designed to identify potential subgroups in a population, on the basis of individual responses to multiple observed binary variables, and to provide an estimate of the number and proportion of people in each subgroup.19 In contrast to traditional regression analyses, whose goal is to understand the relationship of prespecified independent variables to a known outcome, the LCA model considers whether a subgroup of patients might be defined by the combination of similar baseline variables and does not need to consider the outcome.20 LCA has been demonstrated to be an essential and widely used statistical tool in sociology, education, health science, and other fields.21
Therefore, the purpose of this study was to identify the potential subgroups of supportive care needs in Chinese patients with CRC by using LCA, and to clarify the characteristics of high-need patients, to provide a basis for the development of nursing measures that meet the needs of patients with CRC.
2. Methods
We conducted a cross-sectional, anonymous survey. This study was not registered.
2.1. Sample and setting
Through convenience sampling, four tertiary grade A hospitals in Suzhou were selected, where patients with CRC were recruited consecutively from the oncology department and radiotherapy departments from January to September of 2020. The inclusion criteria were (1) patients older than 18 years, (2) patients with a CRC diagnosis, (3) patients currently receiving treatment, and (4) patients agreeing to participate in the study. The exclusion criteria were (1) patients unable to communicate properly; (2) patients not knowing their diagnoses; (3) patients with serious cognitive or psychological difficulties, who were too unwell to participate; and (4) patients participating in interventions associated with supportive care needs. Before the survey, patients were required to sign an informed consent form.
The sample size was determined according to the number of items in the needs assessment scale used in the survey. The sample size has been suggested to be 5–10 times the number of items.22 Given that the Comprehensive Needs Assessment Tool in cancer for patients (CNAT) used in the survey contained 59 items, and assuming a 10% rate of invalid responses, we estimated that a sample size of 328–656 participants would be required.
2.2. Tools
2.2.1. General information questionnaire
The general information questionnaire was designed after review of a large body of relevant literature.23, 24, 25 The questionnaire included age, sex, nationality, marital status, education, occupation, religious beliefs, monthly per capita household income, payment method of medical expenses, CRC family history, knowledge of CRC, cancer types, metastasis, current treatment, and other diseases.
2.2.2. Comprehensive Needs Assessment Tool in cancer for patients (CNAT)
The CNAT was developed by Korean researchers in 2011.26 This questionnaire contains 59 items in seven dimensions (physical symptoms, psychological problems, healthcare staff, information, social/religious/spiritual support, hospital facilities and services, and practical support). Each item is divided into four levels: 0 = no need, 1 = low need, 2 = moderate need, and 3 = high need. Zhao Xinshuang translated it into Chinese in 2017,27 and the domain scores were calculated by averaging the score for each domain with subsequent linear transformation to a scale of 0–100, according to the European Organization for Research and Treatment of Cancer scoring guidelines.28 The specific scoring method is the score of each dimension= (actual score of each dimension × 100)/(number of items × 3). The Cronbach's α coefficient of the total scale was 0.95, the split-half coefficient was 0.81, and the test-retest reliability was 0.82. Eight factors were extracted, which explained 70.33% of the total variance.27 The Chinese version of the CNAT differs from the original version in that it divides the need dimension of healthcare staff into two subdimensions: physicians and nurses. However, given the content of the questionnaire and the actual clinical situation, dividing the healthcare staff needs into needs for physicians and needs for nurses is difficult, because some items involve both physicians and nurses, such as item 24, “being involved in the decision-making process in choosing tests or treatment that I receive,” and item 25, “collaboration and communication among healthcare staff.” Therefore, this study conducted statistical analyses according to the dimensions of the original version of the CNAT.
2.3. Procedures
Seven nursing postgraduates with data collection experience in nursing research were recruited as research assistants. After being trained by the principal investigator of this study, they collected data in the inpatient departments of the study sites. The research assistants recruited patients with CRC, assessed their eligibility, and explained the study procedure. After providing informed consent, the participants completed the questionnaires. Participants’ questions about the items in the survey were answered by the research assistants. If the participants had difficulty in reading the written questions, the research assistants read the questions and options to the participants without making any implications. After participants submitted the questionnaires, the research assistants verified the questionnaires and reminded the participants to respond to unanswered questions on a voluntary basis.
2.4. Data analysis
Analyses were performed in IBM SPSS Statistics 24 and Mplus 8.3. Participant characteristics and need scores were presented as descriptive statistics.
LCA was used to identify potential subgroups of supportive care needs in patients with CRC. To adapt the data to the LCA of the potential subgroups of total needs, if the total score of each dimension was < 50, it was counted as 0, whereas a score ≥ 50 was counted as 1. In analysis of the needs in each dimension, an original item score of 0 was counted as 0, whereas a score of 1–3 was counted as 1. After grouping, the chi-square test was used to analyze the associations between subgroups and statistical variables. The best LCA model was selected with the following indicators: log-likelihood, Akaike information criterion, Bayesian information criterion, and sample size adjusted Bayesian information criterion; the smaller the values, the better the model fit.29 Entropy can also be used to evaluate model classification accuracy: when the entropy is between 0 and 1, the higher the value, the higher the accuracy; when the entropy is approximately 0.80, the accuracy of classification exceeds 90%.30 In addition, model fitting differences can be assessed with a likelihood ratio test, such as the Lo Mendel Rubin adjusted likelihood ratio test or bootstrap-based likelihood ratio test. P < 0.05 indicated statistically significant differences, representing the K-class model is significantly better than the (k-1)-class model. Previous studies have shown that the best fitting model corresponds to the lowest Bayesian information criterion and entropy ≥0.80.31
2.5. Ethical approval
The study was approved by the Ethics Committee of Soochow University (IRB No. SUDA20200225H08). The research request form clearly stated the study purpose and methods. All participants provided written informed consent. Furthermore, it stated that participants' addresses would be obtained only after their consent and that the researchers should be contacted in the event of psychological distress caused by participation in the study. Returning of questionnaires was considered to constitute consent to participate in the study. The collected data were anonymized to maintain confidentiality.
3. Results
A total of 416 questionnaires were distributed in this study, and 13 participants quit the survey for reasons such as being unavailable at the time of the survey or physical discomfort. A total of 403 valid questionnaires were recovered, with an effective recovery rate of 96.9%.
3.1. Participant characteristics
The average age of the 403 participants (257 men and 146 women) was 58.83 ± 10.86; 381 were married, 22 were single, divorced, or widowed; 256 were patients with colon cancer, and 147 were patients with rectal cancer. Details regarding the socio-demographic and clinical characteristics of the participants are shown in Table 1.
Table 1.
The characteristics of patients with CRC participating in the study (n = 403).
| Characteristics | n (%) | Characteristics | n (%) |
|---|---|---|---|
| Age, years ( ± s) | 58.83 ± 10.86 | Monthly per capita household income (RMB) | |
| Gender | < 1000 | 32 (7.94) | |
| Male | 257 (63.77) | 1000–1999 | 62 (15.38) |
| Female | 146 (36.23) | 2000–2999 | 107 (26.55) |
| Nationality | 3000–4000 | 98 (24.32) | |
| Han nationality | 401 (99.50) | > 4000 | 104 (25.81) |
| Others | 2 (0.50) | Cancer type | |
| Marital status | Colon cancer | 256 (63.52) | |
| Married | 381 (94.54) | Rectal cancer | 147 (36.48) |
| Single/Divorced/Widowed | 22 (5.46) | Metastasis | |
| Occupation | Yes | 328 (81.39) | |
| Farmer/Worker | 188 (46.65) | No | 50 (12.41) |
| Cadre/Teacher | 20 (4.96) | Unclear | 25 (6.20) |
| Self-employed laborer | 34 (8.44) | Current treatment | |
| Retired | 161 (39.95) | Chemotherapy | 378 (93.80) |
| Religious belief | Chemotherapy + Radiotherapy | 16 (3.97) | |
| Yes | 45 (11.17) | Palliative treatment | 9 (2.23) |
| No | 358 (88.83) | CRC family history | |
| Education | Have | 59 (14.64) | |
| ≤Primary school | 71 (17.62) | Not have | 344 (85.36) |
| Junior high school | 143 (35.48) | Knowledge of CRC | |
| Senior high school or technical secondary school | 118 (29.28) | Fully understand | 110 (27.30) |
| Junior college | 48 (11.91) | Partially understand | 248 (61.54) |
| ≥ Bachelor | 23 (5.71) | Do not understand | 45 (11.17) |
| Payment method of medical expenses | Other diseases | ||
| Self-paid | 19 (4.71) | Yes | 192 (52.36) |
| Full reimbursement | 6 (1.49) | No | 211 (37.47) |
| Partial reimbursement | 378 (93.80) | ||
3.2. Level of supportive care needs
The average score of total needs was 39.56 ± 18.58. The average score of healthcare staff needs was highest, followed by information needs. The detailed scores are shown in Table 2.
Table 2.
The need scores of each dimension in patients with CRC (n = 403).
| Need dimension | ± s |
|---|---|
| Physical symptoms | 15.78 ± 18.69 |
| Psychological problems | 18.12 ± 24.27 |
| Healthcare staff | 71.75 ± 31.65 |
| Information | 67.07 ± 26.54 |
| Social/Religious/Spiritual support | 26.91 ± 26.78 |
| Hospital facilities and services | 48.34 ± 29.80 |
| Practical support | 32.95 ± 27.35 |
| Total∗ | 39.56 ± 18.58 |
The scores of each dimension need and total need range from 0 to 100.
3.3. LCA of supportive care needs
A series of models were fitted to ensure the validity of the classification hypothesis, and the fitting index values were compared. The fitting index of the total needs and needs for each dimension is shown in Table 3. In addition, the probability graph was carefully assessed, and each subgroup was named as appropriately as possible according to the characteristics of actual needs in each dimension/item.
Table 3.
Model fitting indexes for LCA in supporting care needs.
| Need dimension/Model | LL | AIC | BIC | ABIC | ALMR LRT(p) | BLRT (p) | Entropy |
|---|---|---|---|---|---|---|---|
| Total needs | |||||||
| 1 | −1416.71 | 2847.42 | 2875.41 | 2853.20 | – | – | – |
| 2a | −1213.10 | 2456.20 | 2516.18 | 2468.59 | < 0.01 | < 0.01 | 0.82 |
| 3 | −1162.50 | 2371.01 | 2462.98 | 2390.00 | < 0.01 | < 0.01 | 0.77 |
| 4 | −1145.12 | 2352.24 | 2476.21 | 2377.84 | < 0.01 | < 0.01 | 0.77 |
| 5 | −1142.16 | 2362.32 | 2518.27 | 2394.52 | 0.12 | 1.00 | 0.79 |
| Physical symptoms needs | |||||||
| 1 | −2680.25 | 5384.50 | 5432.49 | 5394.41 | – | – | – |
| 2 | −2219.35 | 4488.70 | 4588.67 | 4509.35 | < 0.01 | < 0.01 | 0.87 |
| 3a | −2111.15 | 4298.29 | 4450.25 | 4329.68 | < 0.01 | < 0.01 | 0.84 |
| 4 | −2091.37 | 4284.74 | 4488.69 | 4326.86 | 0.74 | < 0.01 | 0.83 |
| 5 | −2073.82 | 4275.63 | 4531.57 | 4328.49 | 0.15 | 0.03 | 0.80 |
| Psychological problems needs | |||||||
| 1 | −2463.80 | 4947.60 | 4987.59 | 4955.86 | – | – | – |
| 2 | −1755.46 | 3552.93 | 3636.91 | 3570.27 | < 0.01 | < 0.01 | 0.91 |
| 3 | −1606.53 | 3277.05 | 3405.02 | 3303.48 | < 0.01 | < 0.01 | 0.91 |
| 4 | −1569.98 | 3225.95 | 3397.90 | 3261.46 | < 0.01 | < 0.01 | 0.91 |
| 5a | −1536.71 | 3181.42 | 3397.36 | 3226.01 | <0.01 | < 0.01 | 0.93 |
| 6 | −1513.14 | 3156.29 | 3416.22 | 3209.97 | 0.01 | < 0.01 | 0.92 |
| Healthcare staff needs | |||||||
| 1 | −1278.80 | 2573.60 | 2605.59 | 2580.21 | – | – | – |
| 2 | −906.86 | 1847.71 | 1915.69 | 1861.75 | < 0.01 | < 0.01 | 0.94 |
| 3a | −856.63 | 1765.26 | 1869.23 | 1786.73 | < 0.01 | < 0.01 | 0.86 |
| 4 | −839.23 | 1748.46 | 1888.42 | 1777.36 | < 0.01 | < 0.01 | 0.87 |
| 5 | −821.33 | 1730.66 | 1906.61 | 1766.99 | 0.08 | < 0.01 | 0.92 |
| Information needs | |||||||
| 1 | −1685.90 | 3391.79 | 3431.78 | 3400.05 | – | – | – |
| 2a | −1341.74 | 2725.47 | 2809.45 | 2742.81 | < 0.01 | < 0.01 | 0.92 |
| 3 | −1288.68 | 2641.36 | 2769.32 | 2667.78 | 0.10 | < 0.01 | 0.84 |
| 4 | −1266.76 | 2619.52 | 2791.47 | 2655.03 | 0.60 | < 0.01 | 0.74 |
| 5 | 1250.93 | 2609.87 | 2825.81 | 2654.46 | < 0.01 | < 0.01 | 0.78 |
| Social/Religious/Spiritual support needs | |||||||
| 1 | −1165.16 | 2340.32 | 2360.32 | 2344.45 | – | – | – |
| 2 | −914.17 | 1850.34 | 1894.33 | 1859.43 | < 0.01 | < 0.01 | 0.95 |
| 3a | −880.62 | 1795.24 | 1863.22 | 1809.28 | < 0.01 | < 0.01 | 0.81 |
| 4 | −866.85 | 1779.70 | 1871.68 | 1798.70 | < 0.01 | < 0.01 | 0.82 |
| 5 | −864.84 | 1787.68 | 1903.65 | 1811.63 | 0.15 | 1.00 | 0.85 |
| Hospital facilities and services needs | |||||||
| 1 | −1890.98 | 3797.95 | 3829.94 | 3804.56 | – | – | – |
| 2 | −1573.48 | 3180.97 | 3248.95 | 3195.00 | < 0.01 | < 0.01 | 0.81 |
| 3a | −1503.26 | 3058.53 | 3162.50 | 3080.00 | < 0.01 | < 0.01 | 0.82 |
| 4 | −1493.24 | 3056.48 | 3196.44 | 3085.38 | 0.51 | 0.238 | 0.80 |
| 5 | −1486.16 | 3060.31 | 3236.27 | 3096.65 | 0.66 | 1.00 | 0.77 |
| Practical support needs | |||||||
| 1 | −1486.14 | 2984.27 | 3008.27 | 2989.23 | – | – | – |
| 2a | −1238.08 | 2502.17 | 2554.15 | 2512.90 | < 0.01 | < 0.01 | 0.84 |
| 3 | −1216.52 | 2473.04 | 2553.01 | 2489.55 | < 0.01 | < 0.01 | 0.71 |
| 4 | −1201.70 | 2457.41 | 2565.38 | 2479.70 | 0.49 | < 0.01 | 0.80 |
| 5 | −1194.90 | 2457.80 | 2593.76 | 2485.88 | 0.02 | 0.13 | 0.82 |
LL, Log Likelihood; AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion; ABIC, sample-size Adjusted Bayesian Information Criterion; ALMR LRT, Lo-Mendell-Rubin Adjusted Likelihood Ratio Test; BLRT, Bootstrapped Likelihood Ratio Test.
Optimal model.
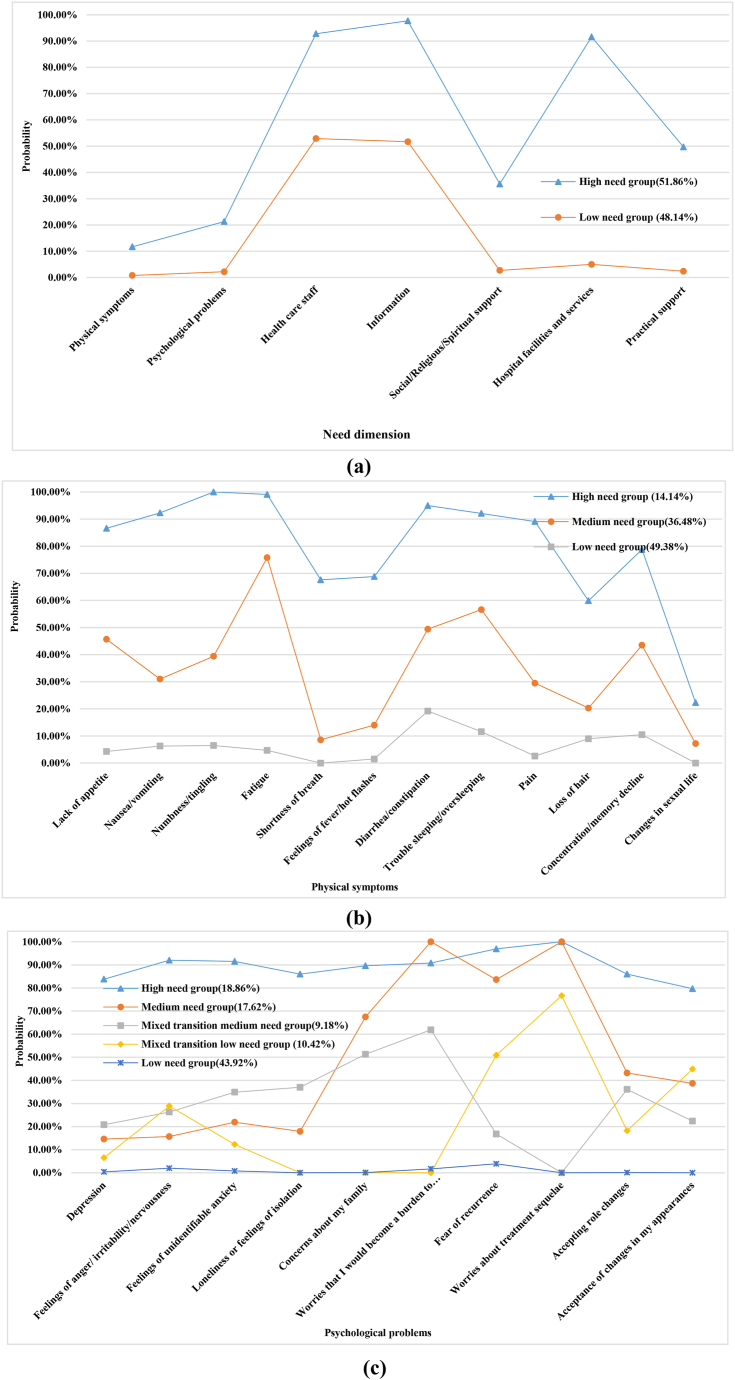
3.3.1. Total needs
Fig. 1 shows two subgroups regarding total needs: 51.86% of the patients belonged to the high-need group and 48.14% belonged to the low-need group. In the high-need group, the probability of needs for the dimensions of healthcare staff, information, and hospital facilities and services exceeded 90%, whereas the probability of needs for the other four dimensions was lower than 50% but still higher than that of the low-need group. Chi-square tests indicated that single/divorced/widowed patients and patients with rectal cancer had relatively higher needs (Table 4).
Fig. 1.
Probabilities of each need dimension/needs for each latent class: a: Needs dimension; b: Physical symptoms; c: Psychological problems.
Table 4.
Chi-square test for latent subgroups and statistical variables of supportive care needs (n = 403).
| Statistical variables | High need group, n (%) | Medium need group, n (%) | Mixed transition medium needs group, n (%) | Mixed transition low need group, n (%) | Low need group, n (%) | P |
|---|---|---|---|---|---|---|
| Total needs | ||||||
| Marital status | ||||||
| Married | 193 (50.66) | – | – | – | 188 (49.34) | 0.04 |
| Single/Divorced/Widowed | 16 (72.73) | – | – | – | 6 (27.27) | |
| Cancer type | ||||||
| Colon cancer | 119 (46.48) | – | – | – | 137 (53.52) | < 0.01 |
| Rectal cancer | 90 (61.22) | – | – | – | 57 (38.78) | |
| Physical symptoms need | ||||||
| Other diseases | ||||||
| Have | 36 (18.75) | 73 (38.02) | – | – | 83 (43.23) | 0.01 |
| Not have | 21 (9.95) | 74 (35.07) | – | – | 116 (54.98) | |
| Metastasis | ||||||
| Yes | 54 (16.46) | 123 (37.50) | – | – | 151 (46.04) | 0.02 |
| No | 1 (2.00) | 17 (34.00) | – | – | 32 (64.00) | |
| Unclear | 2 (8.00) | 7 (28.00) | – | – | 16 (64.00) | |
| Current treatment | ||||||
| Chemotherapy | 48 (12.70) | 137 (36.24) | – | – | 193 (51.06) | < 0.01 |
| Chemotherapy + Radiotherapy | 4 (25.00) | 8 (50.00) | – | – | 4 (25.00) | |
| Palliative treatment | 5 (55.56) | 2 (22.22) | – | – | 2 (22.22) | |
| Psychological problems need | ||||||
| Current treatment | ||||||
| Chemotherapy | 66 (17.46) | 65 (17.20) | 33 (8.73) | 40 (10.58) | 174 (46.03) | < 0.01 |
| Chemotherapy + Radiotherapy | 5 (31.25) | 5 (31.25) | 1 (6.25) | 2 (12.50) | 3 (18.75) | |
| Palliative treatment | 5 (55.56) | 1 (11.11) | 3 (33.33) | 0 (0.00) | 0 (0.00) | |
| Social/religious/spiritual support needs | ||||||
| Gender | ||||||
| Male | 66 (25.68) | 39 (15.18) | – | – | 152 (59.14) | 0.02 |
| Female | 54 (36.99) | 27 (18.49) | – | – | 65 (44.52) | |
| Marital status | ||||||
| Married | 106 (27.82) | 64 (16.80) | – | – | 211 (55.38) | < 0.01 |
| Single/Divorced/Widowed | 14 (63.64) | 2 (9.09) | – | – | 6 (27.27) | |
| Hospital facilities and services needs | ||||||
| Cancer type | ||||||
| Colon cancer | 92 (35.94) | 127 (49.61) | – | – | 37 (14.45) | 0.03 |
| Rectal cancer | 71 (48.30) | 64 (43.54) | – | – | 12 (8.16) | |
| Metastatic | ||||||
| Yes | 144 (43.90) | 147 (44.82) | – | – | 37 (11.28) | 0.03 |
| No | 10 (20.00) | 31 (62.00) | – | – | 9 (18.00) | |
| Unclear | 9 (36.00) | 13 (52.00) | – | – | 3 (12.00) | |
| Current treatment | ||||||
| Chemotherapy | 146 (38.62) | 186 (49.21) | – | – | 46 (12.17) | 0.02 |
| Chemotherapy + Radiotherapy | 10 (62.50) | 3 (18.75) | – | – | 3 (18.75) | |
| Palliative treatment | 7 (77.78) | 2 (22.22) | – | – | 0 (0.00) | |
| Practical support needs | ||||||
| Marital status | ||||||
| Married | 117 (30.71) | – | – | – | 264 (69.29) | 0.02 |
| Single/Divorced/Widowed | 12 (54.55) | – | – | – | 10 (45.45) | |
| Cancer type | ||||||
| Colon cancer | 72 (28.13) | – | – | – | 184 (71.88) | 0.03 |
| Rectal cancer | 57 (38.78) | – | – | – | 90 (61.22) | |
| Current treatment | ||||||
| Chemotherapy | 115 (30.42) | – | – | – | 263 (69.58) | 0.02 |
| Chemotherapy + Radiotherapy | 10 (62.50) | – | – | – | 6 (37.50) | |
| Palliative treatment | 4 (44.44) | – | – | – | 5 (55.56) | |
3.3.2. Needs in the dimension of “physical symptoms”
Three subgroups were identified in this dimension: high-, moderate-, and low-need groups included 14.14%, 36.48%, and 49.38% of patients, respectively. In the high-need group, except for “changes in sexual life,” the probability of other needs exceeded 55%, in which the need probability for five items exceeded 90%. In the moderate-need group, the probability of most needs was in the range of 30%–60%, and only that of “fatigue” exceeded 75%. The probability of all needs in the low-need group was less than 20% (Fig. 1). Chi-square tests indicated that other diseases, metastasis, and current treatment had significant effects on the needs in the dimension of “physical symptoms” (Table 4).
3.3.3. Needs in the dimension of “psychological problems”
The “psychological problems” dimension comprised five needs: high-, moderate-, mixed-to-moderate, mixed-to-low, and low-need groups, with 18.86%, 17.62%, 9.18%, 10.42%, and 43.92% of patients, respectively. The probability of all needs in the high-need group exceeded 75%. In the moderate-need group, the need probability of four items was high (> 65%), whereas that of other needs was in the range of 10–45%. In the mixed-to-moderate need group, the need probability of “fear of recurrence” and “worries about treatment sequelae” was less than 20%, and those of the other eight needs were between 20% and 65%. The mixed-to-low need group had relatively high need probability in only four items (25–80%), whereas those of other needs were in the range of 0–20%. The probability of all needs in the low-need group was less than 10% (Fig. 1). Chi-square tests indicated that current treatment had a significant influence on needs in the “psychological problems” dimension in patients with CRC (Table 4).
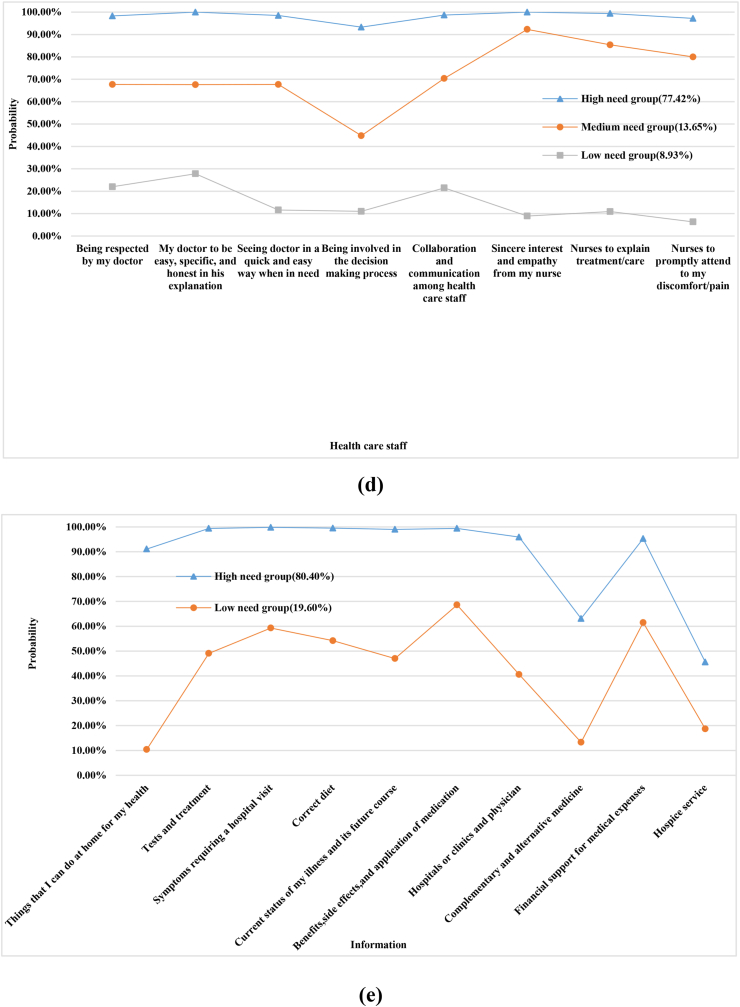
3.3.4. Needs in the dimension of “healthcare staff”
The dimension of healthcare staff contained three subgroups: high -, moderate-, and low-need groups, which included 77.42%, 13.65%, and 8.93% of patients, respectively. The probability of all needs in the high-need group exceeded 90%. In the moderate-need group, the probability of all needs was between 40% and 95%; and in the low-need group, the probability of all needs was less than 30% (Fig. 2). Chi-square tests did not indicate statistically significant indicators. Thus, the results are not presented.
Fig. 2.
Probabilities of needs for each latent class: d Healthcare staff; e Information.
3.3.5. Needs in the dimension of “information”
Needs in the “information” dimension included two subgroups: high-need and low-need groups, accounting for 80.40% and 19.60% of patients, respectively. In the high-need group, the need probability of “complementary and alternative medicine,” and “hospice service” was lower than 90%, and that of other needs exceeded 90%; the probability of all needs in the low-need group was lower than that in the high-need group, ranging from 10% to 70% (Fig. 2). Chi-square tests did not reveal statistically significant indicators, and thus the results are not shown.
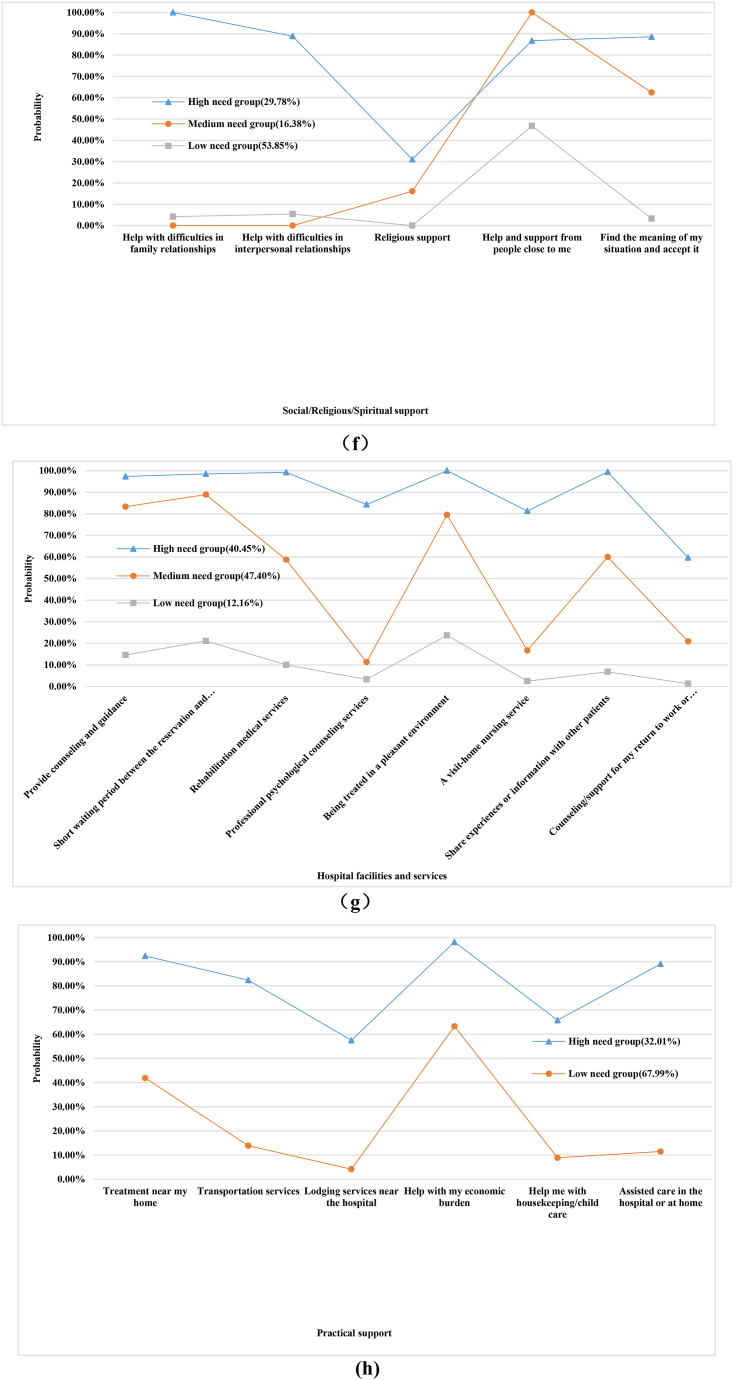
3.3.6. Needs in the dimension of “social/religious/spiritual support”
The “social/religious/spiritual support” dimension contained three subgroups: high -, moderate-, and low-need groups, accounting for 29.78%, 16.38%, and 53.85% of patients, respectively. In the high-need group, the need probability of four items exceeded 80%. In the moderate-need group, the need probability of “help and support from people close to me” and “find the meaning of my situation and accept it” was 100% and 62.50%, respectively, whereas that of other needs was less than 20%. In the low-need group, the need probability of four items was less than 10% (Fig. 3). Chi-square tests indicated that female and single/divorced/widowed patients had comparatively higher social/religious/spiritual support needs (Table 4).
Fig. 3.
Probabilities of needs for each latent class: f: Social/Religious/Spiritual support; g: Hospital facilities and services; h: Practical support.
3.3.7. Needs in the dimension of “hospital facilities and services”
Needs in the “hospital facilities and services” dimension included three subgroups: high -, moderate-, and low-need groups, accounting for 40.45%, 47.40%, and 12.16% of patients, respectively. In the high-need group, the probability of all other needs exceeded 80% except for “counseling and support for my return to work or reemployment” (59.70%). The moderate-need group had a high need probability for three items (> 75%), whereas those of other needs were between 10% and 60%. The probability of all needs in the low-need group was less than 30% (Fig. 3). Chi-square tests indicated that cancer type, metastasis, and current treatment significantly affected the needs in the “hospital facilities and services” dimension (Table 4).
3.3.8. Needs in the dimension of “practical support”
Needs in the “practical support” dimension included two subgroups: high-need and low-need groups, accounting for 32.01% and 67.99% of patients, respectively. In the high-need group, the need probability for “lodging services near the hospital I was treated in” and “someone to help me with housekeeping and/or child care” was 57.50% and 65.80%, whereas that of other needs exceeded 80%. In the low-need group, except for “help with my economic burden caused by cancer” (63.30%), the probability of other needs was less than 45% (Fig. 3). Chi-square tests indicated significant differences in practical support needs among patients with CRC with different marital statuses, cancer type, and current treatment (Table 4).
4. Discussion
4.1. More than half of Chinese patients with colorectal cancer have high supportive care needs
This study used LCA for statistical analysis, and the results revealed two potential subgroups of supportive care needs in Chinese patients with CRC: 51.86% of patients were in the high-need group, and 48.14% of patients were in the low-need group. A cross-cultural LCA study (involving Japan, Canada, and the United States) on patients with cancer has indicated that the supportive care needs in these three countries can be classified into two subgroups: the Japanese sample was most likely to be classified in the “high-need” group (51%, as compared with 44% in the Canadian sample and 30% in the U.S. sample).32 Possibly because of minor differences in culture or lifestyles may exist between China and Japan, the identified need subgroups were similar, with more than 50% of patients with high needs.
4.2. More needs in the dimensions of “healthcare staff” and “information”
On the basis of the conditional probabilities for the two subgroups regarding supportive care total needs across the seven dimensions (Fig. 1), the “high-need” group exhibited the highest conditional probability for information (97.70%) and healthcare staff (92.80%). In the “low-need” group, the conditional probabilities for healthcare staff (52.90%) and information (51.70%) were also higher than those for other dimensions. This result suggests that Chinese patients with CRC have a high demand for these two dimensions, in agreement with the results of a Japanese study also indicating that patients’ information needs were high.32 Furthermore, LCA was used to identify potential subgroups of information needs and healthcare staff needs separately. A large proportion of patients belonged to the high-need group in these two dimensions (77.42% for healthcare staff and 80.40% for information). However, no statistically significant features were identified in the chi-square test results for either dimension, probably because patients with CRC had high needs in both dimensions, regardless of their characteristics. More studies with larger sample sizes are needed to validate this aspect. Nonetheless, the results indicated that for Chinese patients with CRC, the needs for information and healthcare staff should be a focus, and continuing improvement in professional competence of healthcare staff, and provision of relevant information should also be priorities.
Notably, the conditional probability for psychological problems in both the “high-need” group and “low-need” group (21.30% and 2.20%, respectively) was lower than those reported for other countries.32 Several reasons may explain this difference. First, in Jennifer's study,32 the study population included mixed cancer types, whereas our study focused on patients with CRC. However, whether the psychological needs of patients are dependent on cancer type must be confirmed in further studies. In addition, the different research tools used between studies may also explain the difference in psychological needs: psychological items accounted for the largest portion of the total variance in the tool used in Jennifer's study33 but not in our tool,26 thus potentially explaining why the results from other countries were more sensitive to psychological problems. Moreover, in accordance with traditional Chinese culture, many Chinese patients may be reserved and reluctant to reveal their true internal feelings to researchers, but more inclined to express their needs for external support, such as healthcare staff and information. This aspect may also explain why the supportive care needs of Chinese patients with CRC are high in terms of healthcare staff and information. However, when assessing and meeting these needs, healthcare staff should not underestimate the psychological needs of patients.34 Establishing a trusting relationship with patients, encouraging them to express themselves, and providing proper psychological counseling are particularly important.
4.3. Higher supportive care needs in patients who are unmarried, with rectal cancer, receiving chemotherapy plus radiotherapy or palliative treatment
On the basis of the results of the LCA for each dimension individually, the people in the “high-need” groups all appeared to have similar characteristics. The findings of this study indicated that single/divorced/widowed participants had higher total needs as well as higher needs in certain need dimensions, including social/religious/spiritual support needs and practical support needs. A survey on patients with acute leukemia has also shown similar results, indicating higher psychological needs and supportive care needs in unmarried patients than married patients.35 Single/divorced/widowed patients are more likely to lack a close person to share the treatment burden, provide emotional support, and share their concerns about deterioration due to illness.35,36
Our research showed that compared with patients with colon cancer, patients with rectal cancer had higher total needs as well as higher hospital facility and service needs, and practical support needs. Similarly, Wang's study has suggested that “information,” “physical and daily living,” and “sexuality and stoma” needs among patients with rectal cancer, particularly those without anal sphincter preservation, are significantly higher than those of patients with colon cancer.37 Patients with rectal cancer are more physically and mentally burdened than patients with colon cancer, thus affecting their daily lives and posing difficulties in stoma care. These aspects might explain the relatively greater support needed by these patients.38,39
In this study, we observed statistically significant differences in the levels of physical symptom needs, psychological problems needs, social/religious/spiritual support needs, hospital facility and service needs, and practical support needs among patients undergoing different current treatments. Patients who underwent chemotherapy plus radiotherapy had greater needs in the “practical support needs” dimension, and those receiving palliative treatment had higher needs in the other three dimensions. Yang has also found that compared with patients receiving single treatment, patients receiving multiple treatments have greater needs.40 Because patients receiving multiple anticancer treatments and palliative care are likely to have more severe symptoms and poorer emotional status,41 attention should be paid to the needs of these patients. In summary, the above three characteristics of the “high-need” groups together indicate that greater attention should be paid to unmarried patients, those with rectal cancer, and those receiving chemotherapy plus radiotherapy or palliative treatment.
4.4. Limitations
This study has several limitations. First, it was not a cross-regional survey, and it was conducted in four hospitals in the same city. Second, the distribution of samples was relatively unbalanced in terms of nationality, marital status, religious beliefs, and so on, and multivariate analysis was not conducted to control the influence of confounding factors. Finally, this study had a cross-sectional design, in which the dynamic variability of supportive care needs was not considered. Cross-regional longitudinal surveys with larger sample sizes remain necessary to further analyze the potential subgroups of supportive care needs in Chinese patients with CRC and identify the characteristics of high-need patients, to provide a basis for formulating effective scientific interventions in the future.
5. Conclusions
In conclusion, a considerable proportion of patients with CRC have a high level of supportive care needs in China. Although needs in the dimensions of “healthcare staff” and “information” should be prioritized, the psychological needs of patients with CRC should not be ignored. Focus should be placed on unmarried patients, patients with rectal cancer, and patients receiving chemotherapy plus radiotherapy or palliative treatment.
CRediT author statement
Bei Dong: Conceptualization, Methodology, Data curation, Formal analysis, Writing. Jiyin Zhang: Methodology, Data collection, Writing – Original draft preparation. Fen Wang: Formal analysis, Writing – Revised draft preparation, Data curation. Congyan Xie: Methodology, Data collection. Yishu Qi: Methodology, Data collection. Lu Lin: Writing – Original and revised draft preparation, Article polishing. Li Tian: Conceptualization, Writing – Original and revised draft preparation, Article polishing. All authors had full access to all the data in the study, and the corresponding author had final responsibility for the decision to submit for publication. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Declaration of competing interest
The authors declare no conflict of interest. The corresponding author, Dr. Lin LU, is an associate editor of Asia-Pacific Journal of Oncology Nursing. The article was subject to the journal’s standard procedures, with peer review handled independently of Dr. Lu and their research groups.
Funding
This study was funded by the Humanity and Social Science Youth Foundation of Ministry of Education of China (No. 18YJCZH164) and the National Natural Science Foundation of China (Grant No. 81801098). The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Ethics statement
The study was approved by the Ethics Committee of Soochow University (IRB No. SUDA 20200225H08).
Contributor Information
Lu Lin, Email: linlu@suda.edu.cn.
Li Tian, Email: tianlisz@suda.edu.cn.
References
- 1.World Health Organization (WHO) 2020. World Cancer Report.https://www.iarc.fr/cards_page/world-cancer-report/ [Google Scholar]
- 2.Zhang Y., Shi J., Huang H., et al. Burden of colorectal cancer in China. Chin J Epidemiol. 2015;36(7):709–714. [PubMed] [Google Scholar]
- 3.Yan T., Su L., Zhang X.G. Epidemiological characteristics and risk factors of colorectal cancer. Journal of Diseases Monitor & Control. 2015;9(4):241–243. [Google Scholar]
- 4.Luo P.F., Yu H., Han R.Q., et al. Study of disease burden and related risk factors of colorectal cancer in Jiangsu Province, 1990—2019. China Cancer. 2022;31(12):967–974. [Google Scholar]
- 5.Allemani C., Matsuda T., Carlo V.D., et al. Global surveillance of trends in cancer survival: analysis of individual records for 37,513,025 patients diagnosed with one of 18 cancers during 2000-2014 from 322 population-based registries in 71 countries (CONCORD-3) Lancet. 2018;391(10125):1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cunningham C., Lindsey I. Colorectal cancer: management. Medicine. 2007;35(5):306–310. [Google Scholar]
- 7.Fitch M. vol. 23. Ontario Cancer Treatment and Research Foundation; Toronto: 1994. (Providing Supportive Care for Individuals Living with Cancer). [Google Scholar]
- 8.Simonelli L.E. Understanding the support needs of women with gynecologic cancer. Del Med J. 2010;82(3):93–96. [PubMed] [Google Scholar]
- 9.Shang Y.L., Wang L., Peng L.H., et al. Research progress on supportive care needs of patients with colorectal cancer. Chin Nurs Res. 2021;35(4):634–638. [Google Scholar]
- 10.Sodergren S.C., Wheelwright S.J., Permyakova N.V., et al. Supportive care needs of patients following treatment for colorectal cancer: risk factors for unmet needs and the association between unmet needs and health-related quality of life-results from the ColoREctal Wellbeing (CREW) study. J Cancer Surviv. 2019;13(6):899–909. doi: 10.1007/s11764-019-00805-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oberoi D., White V.M., Seymour J.F., et al. The influence of unmet supportive care needs on anxiety and depression during cancer treatment and beyond: a longitudinal study of survivors of hematological cancers. Support Care Cancer. 2017;25(11):3447–3456. doi: 10.1007/s00520-017-3766-9. [DOI] [PubMed] [Google Scholar]
- 12.Hansen D.G., Larsen P.V., Holm L.V., et al. Association between unmet needs and quality of life of cancer patients: a population-based study. Acta Oncol. 2013;52(2):391–399. doi: 10.3109/0284186X.2012.742204. [DOI] [PubMed] [Google Scholar]
- 13.Richardson A., Medina J., Brown V., Sitzia J. Patients' needs assessment in cancer care: a review of assessment tools. Support Care Cancer. 2007;15(10):1125–1144. doi: 10.1007/s00520-006-0205-8. [DOI] [PubMed] [Google Scholar]
- 14.Zhao X.S., Wang H.Y., Zhang L.L., et al. Prevalence and risk factors associated with the comprehensive needs of cancer patients in China. Health Qual Life Outcome. 2019;17(1) doi: 10.1186/s12955-019-1171-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cao S., Xie L.L., Zhang Z.W. Analysis of the influencing factors and current status of supportive care needs in patients with preliminary diagnosed gynecological cancer. Military Nursing. 2015;32(16):16–19. [Google Scholar]
- 16.Cai Y.J., Shi T.Y., Li Y.J., et al. A longitudinal study on the supportive care needs and quality of life of patients with breast cancer. Chinese Nursing Management. 2018;18(1):134–139. [Google Scholar]
- 17.Zhang T., He H., Liu Q., et al. Supportive care needs of patients with lung cancer in Mainland China: a cross-sectional study. J Nurs Res. 2019;27(6):e52. doi: 10.1097/jnr.0000000000000338. [DOI] [PubMed] [Google Scholar]
- 18.Ren J.Y., Zhong Z.D., Yuan J., et al. Symptom distress and supportive care needs among esophageal cancer patients after esophagectomy in recovery stage. Journal of Nursing Science. 2020;35(11):87–90. [Google Scholar]
- 19.Zeng X.H., Xiao L., Zhang Y.B. Principle and case analysis of latent class analysis. Chin J Health Statistics. 2013;30(6):815–817. [Google Scholar]
- 20.Calfee C.S., Delucchi K., Parsons P.E., et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2(8):611–620. doi: 10.1016/S2213-2600(14)70097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dziak J.J., Lanza S.T., Tan X. Effect size, statistical power and sample size requirements for the bootstrap likelihood ratio test in latent class analysis. Struct Equ Model. 2014;21(4):534–552. doi: 10.1080/10705511.2014.919819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang J.L. Shanghai Science and Technology Press; Shanghai: 2014. Clinical Epidemiology. [Google Scholar]
- 23.Hu Y. Anhui Medical University; 2017. Development and Psychometric Testing of Two Disease-specific Instrument to Measure Supportive Care Needs for Patients with Esophageal/colorectal Cancer. [Google Scholar]
- 24.Dau H., Safari A., Saad El Din K., et al. Assessing how health information needs of individuals with colorectal cancer are met across the care continuum: an international cross-sectional survey. BMC Cancer. 2020;20(1):1031. doi: 10.1186/s12885-020-07539-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miniotti M., Bassino S., Fanchini L., et al. Supportive care needs, quality of life and psychological morbidity of advanced colorectal cancer patients. Eur J Oncol Nurs. 2019;43 doi: 10.1016/j.ejon.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Shim E.J., Lee K.S., Park J.H., et al. Comprehensive needs assessment tool in cancer (CNAT): the development and validation. Support Care Cancer. 2011;19(12):1957–1968. doi: 10.1007/s00520-010-1037-0. [DOI] [PubMed] [Google Scholar]
- 27.Zhao X.S., Zhang L.L., Li Z.Z. Validation of Chinese version of the comprehensive needs assessment tool for cancer patients. Chin J Nurs. 2017;52(1):34–39. [Google Scholar]
- 28.Shin D.W., Park J.H., Shim E.J., et al. The development of a Comprehensive Needs Assessment Tool for cancer-caregivers in patient-caregiver dyads. Psycho Oncol. 2011;20(12):1342–1352. doi: 10.1002/pon.1857. [DOI] [PubMed] [Google Scholar]
- 29.Xie S. Shandong University; 2019. Study on Resilience of Latent Class Analysis of Elderly Diabetic Patients in Shandong Province. [Google Scholar]
- 30.Carragher N., Adamson G., Bunting B., et al. Subtypes of depression in a nationally representative sample. J Affect Disord. 2009;113(1-2):88–99. doi: 10.1016/j.jad.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 31.Celeux G., Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. J Classif. 1996;13(2):195–212. [Google Scholar]
- 32.Reese J.B., Blackford A., Sussman J., et al. Cancer patients' function, symptoms and supportive care needs: a latent class analysis across cultures. Qual Life Res. 2015;24(1):135–146. doi: 10.1007/s11136-014-0629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goździewicz B., Strugała M., Talarska D., Stanisławska J., Bączyk G. Functioning of people with colorectal cancer during chemotherapy. Demographic and clinical determinants of quality of life of patients with colorectal cancer receiving chemotherapy. Pilot study. Eur J Cancer Care. 2017;26(3) doi: 10.1111/ecc.12616. [DOI] [PubMed] [Google Scholar]
- 34.Bonevski B., Sanson-Fisher R., Girgis A., Burton L., Cook P., Boyes A. Evaluation of an instrument to assess the needs of patients with cancer. Supportive Care Review Group. Cancer. 2000;88(1):217–225. doi: 10.1002/(sici)1097-0142(20000101)88:1<217::aid-cncr29>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 35.Yan J. Fujian Medical University; 2018. Status of Supportive Care Needs and Construction of a Supportive WeChat Platform Program for Acute Leukemia Patients and Their Caregivers. [Google Scholar]
- 36.Smith T.G., Troeschel A.N., Castro K.M., et al. Perceptions of patients with breast and colon cancer of the management of cancer-related pain, fatigue, and emotional distress in community oncology. J Clin Oncol. 2019;37(19):1666–1676. doi: 10.1200/JCO.18.01579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang H.R., Yuan C.S., Qiu F.B. An investigation of the difference in supportive care needs between postoperative patients with colon cancer and those with rectal cancer. Chinese Nursing Management. 2014;14(6):641–644. [Google Scholar]
- 38.Downing A., Morris E.J., Richards M., et al. Health-related quality of life after colorectal cancer in England: a patient-reported outcomes study of individuals 12 to 36 months after diagnosis. J Clin Oncol. 2015;33(6):616–624. doi: 10.1200/JCO.2014.56.6539. [DOI] [PubMed] [Google Scholar]
- 39.Niu H.H. Lanzhou University; 2020. Analysis of the Current Situation and Influencing Factors of Supportive Care Needs of Colorectal Cancer Patients with Stoma. [Google Scholar]
- 40.Yang P., Zhu J.H., Xiao W.H., et al. Supportive care needs of intermediate or advanced cancer patients and its influencing factors. Acad J Chin PLA Med Sch. 2016;37(5):452–456. [Google Scholar]
- 41.Fan G., Filipczak L., Chow E. Symptom clusters in cancer patients: a review of the literature. Curr Oncol. 2007;14(5):173–179. doi: 10.3747/co.2007.145. [DOI] [PMC free article] [PubMed] [Google Scholar]