Abstract
Plasmodium vivax malaria continues to cause a significant burden of disease in the Asia-Pacific, the Horn of Africa, and the Americas. In addition to schizontocidal treatment, the 8-aminoquinoline drugs are crucial for the complete removal of the parasite from the human host (radical cure). While well tolerated in most recipients, 8-aminoquinolines can cause severe haemolysis in glucose-6-phosphate dehydrogenase (G6PD) deficient patients. G6PD deficiency is one of the most common enzymopathies worldwide; therefore, the WHO recommends routine testing to guide 8-aminoquinoline based treatment for vivax malaria whenever possible. In practice, this is not yet implemented in most malaria endemic countries. This review provides an update of the characteristics of the most used G6PD diagnostics. We describe the current state of policy and implementation of routine point-of-care G6PD testing in malaria endemic countries and highlight key knowledge gaps that hinder broader implementation. Identified challenges include optimal training of health facility staff on point-of-care diagnostics, quality control of novel G6PD diagnostics, and culturally appropriate information and communication with affected communities around G6PD deficiency and implications for treatment.
Keywords: P. vivax, G6PD testing, radical cure, malaria elimination, policy, treatment guidelines, implementation, point of care diagnostics
1. Introduction
Approximately 2.5 billion people are at risk of a Plasmodium vivax (P. vivax) infection. Between 5 and 14 million cases are recorded annually, the majority of which are reported in Southeast Asia [1,2,3]. Increased efforts of national malaria control programs (NMCPs) have led to a reduction of the global P. vivax burden. According to the World Health Organisation (WHO), cases decreased from 24.5 million in 2000 to 4.9 million in 2021 [3]; while Battle et al. estimated a reduction of 41.6% between 2000 and 2017, from 24.5 to 14.3 million cases [2].
Despite these advances, the control and elimination of vivax malaria is challenging, largely due to the parasite’s biology and ability to survive in the human host. P. vivax gametocytes develop before the onset of symptoms, resulting in asymptomatic but infectious patients who cannot be identified by passive surveillance [4,5,6]. Secondly, the sensitivity of most point-of-care (PoC) tests for P. vivax is lower than for P. falciparum due to lower parasite densities [7,8,9]. Thirdly, P. vivax forms dormant liver stages (hypnozoites) that can reactivate weeks to months after a primary infection [10], resulting in recurrent episodes of malaria (relapse) [2,11]. In some areas, up to 80% of clinical cases are due to relapse [12], causing long-term morbidity and significant health and economic burdens [13].
The 8-aminoquinoline (8-AQ) class of antimalarial compounds are the only available drugs with good efficacy against hypnozoites. The treatment of vivax malaria requires killing both the peripheral blood stage parasites with a blood schizontocidal and the dormant liver stages with an 8-AQ drug—together, this is referred to as radical cure. Primaquine (PQ) is the most widely used 8-AQ [14], and is usually administered over 14 days as a total dose of 3.5 mg/kg when used for radical cure in line with WHO recommendations [15]. More recently, the WHO Treatment Guidelines were updated to include a 7-day treatment regimen with the same total dosage [16]. The anti-relapse efficacy of primaquine is related to the total dose administered, and higher doses are sometimes recommended in patients at high risk of relapse [15,17]. The long treatment duration is often associated with poor adherence and low effectiveness [18,19]. Novel, short-course, PQ-based regimens with higher daily doses [20] and the recently introduced single-dose 8-AQ tafenoquine (TQ) [21] both have the potential to improve adherence.
Whilst well tolerated in most recipients, 8-AQs can cause severe haemolysis in individuals with the common enzymopathy glucose-6-phosphate dehydrogenase (G6PD) deficiency, necessitating G6PD testing to reduce this risk and guide radical cure. The degree of drug-induced haemolysis is dose-dependent, and since shorter PQ regimens require a higher daily dose to achieve the same total dose, these regimens are associated with a higher risk of drug-induced haemolysis. PQ is rapidly eliminated (half-life 4 to 9 h), whereas TQ is more slowly eliminated (half-life ~14 days), allowing it to be administered as a single dose [22]. Due to TQ’s long half-life, patients are continuously exposed to the oxidative effects of the drug, underlining the need for reliable G6PD testing to guide treatment.
2. G6PD Deficiency
G6PD is a ubiquitous enzyme [23] and the rate-limiting component of the pentose phosphate pathway (PPP). In red blood cells (RBCs), G6PD is essential to maintain the cells’ redox potential by producing reduced nicotinamide adenine dinucleotide phosphate (NADPH) [24]; NADPH is a key electron donor for the conversion of oxidised glutathione (GSSG) into reduced glutathione (GSH). GSH, in turn, captures free radicals that could cause oxidative damage. Human RBCs contain neither a nucleus nor mitochondria and cannot replenish G6PD levels. Reticulocytes and young RBCs therefore have up to a 10-fold higher G6PD activity compared to older RBCs [25].
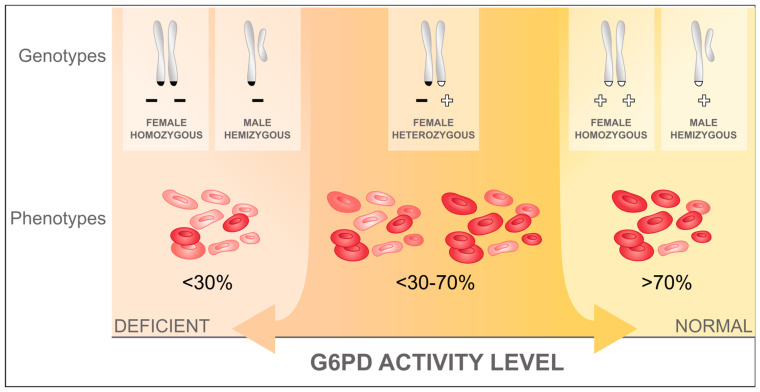
G6PD deficiency is among the most common enzymopathies affecting 400 to 500 million people [26], and it is most prevalent in current and historically malaria endemic areas [27,28,29], suggesting some form of protective effect of G6PD deficiency against malaria or a Plasmodium species infection [30,31]. The G6PD gene is located on the X-chromosome (Xq28), so males are either hemizygous deficient or normal. Females have two X-chromosomes, one of which is randomly deactivated at the cellular level at an early embryonic stage through a process called lyonization [32]. Accordingly, females can be homozygous deficient or normal, or heterozygous for the G6PD gene. Heterozygous females have two distinct RBC populations, a G6PD normal and a G6PD deficient one, with proportions differing depending on the degree of lyonization (Figure 1 [33]). In hemizygous, homozygous, and heterozygous deficient individuals, the risk for drug-induced haemolysis depends on the underlying G6PD genetic variant, the degree of lyonization in heterozygous females, the degree of oxidant exposure, and the age of the RBC population [23].
Figure 1.
RBC populations in individuals with different G6PD alleles. RBCs with normal G6PD activity are coloured in red, while RBCs with deficient G6PD activity are pale red; adapted from Domingo et al. (2019) [33].
Phenotypic G6PD activity is measured in units per gram haemoglobin (U/g Hb). The gold standard is spectrophotometry; however, measures can differ significantly between assays, populations, and locations, confounding direct comparison [34]. Instead, activities are normalized and expressed in the percentage of normal activity, defined by the site-specific adjusted male median (AMM) calculated from quantitatively measured G6PD activity of the male population [35]. Most hemi- and homozygous individuals have G6PD activities below 30% (G6PD deficient) or above 70% to 80% of normal activity (G6PD normal) [36]. Conversely heterozygous females have enzyme activities ranging from close to 0% to almost normal activities, with activities of the majority of heterozygous females clustering around the 50% mark [37].
3. Overview of G6PD Test Formats and Products
There are multiple methods to diagnose G6PD deficiency [38], including molecular tests for population screening and genotyping [39], flow cytometry based methods to quantify degree of lyonization in heterozygous females [40,41], and phenotypic tests (both qualitative and quantitative) used in clinical settings for case management and reference testing.
Molecular methods identify polymorphisms of the G6PD gene that have been associated with enzyme activity [42]. Sequencing methods are able to identify known and novel G6PD variants, while variant-specific genotyping methods such as the PCR-RFLP, PCR-SSCP, or hybridisation arrays are only suitable for areas where the most common variants are known. Current molecular methods require good laboratory infrastructure and well-trained staff, and the interpretation of the final result requires specialised tools [43]. No existing molecular method can provide results within a timeframe that would render the method suitable for testing to support radical cure treatment decisions at the bedside [44]. Furthermore, even between individuals carrying the same G6PD genetic variants, G6PD activity varies [36], and it may be further confounded by changes in G6PD activity associated with acute malaria [45,46,47]. These molecular methods are employed for the surveillance of populations and research purposes only.
Cytochemical assays do not measure G6PD residual activity but can distinguish individual G6PD deficient RBCs from G6PD normal RBCs to determine the proportion of G6PD deficient cells in heterozygous females [40,41]. The method requires a costly flow cytometer, with protocols involving hazardous chemicals [40].
Phenotypic methods measure G6PD activity from blood samples by measuring NADPH production, either directly or indirectly, and either qualitatively or quantitatively. Most phenotypic assays require a laboratory (Table 1) and specialized training or experience in interpreting the results.
Table 1.
Common phenotypic laboratory and PoC assays to detect G6PD deficiency.
| Diagnostic to Detect G6PD Deficiency (Year First Reported) |
Output | Blood Volume Required |
Time to Result |
Pipetting Steps in Sample Preparation |
Cost * | Performance ** |
|---|---|---|---|---|---|---|
| Laboratory Assays | ||||||
| Spectrophotometry (1967) [48] | Quantitative | 10 µL | 15 min + calculation time | 4–5 + sample or buffer preparation steps | Trinity Biotech (Ireland) USD 3.6 Pointe Scientific (USA) USD 2.0 [49] |
Used as diagnostic reference; substantial inter-lab variability [34] |
| Fluorescent Spot Test (1966) [50,51] | Qualitative | 10 µL | 15 min + drying time | 5 | USD 0.1–3.0 [52] |
|
| WST-8/1-methoxy PMS (2003) [57,58] | Quantitative or qualitative | 5 µL | 15–60 min | 4 | USD 0.1–3.2 [55,58] |
|
| Flow Cytometry (1989) [40,41,59] | Cytochemical | 1 mL [59] | 3 h | At least 14 + buffer preparation steps | USD 20 [60] |
|
| Point-of-care Assays | ||||||
| CareStart G6PD RDT (2011; AccessBio, Somerset, NJ, USA) [61] | Qualitative (2.7 U/g Hb threshold) | 2 µL | 10 min | 2 | USD 1.5 [62] |
|
| BinaxNOW G6PD Test (2010; Alere, Waltham, MA, USA) [64,65] | Qualitative (4.0 U/g Hb threshold) | 10 µL | 7 min | 3 | USD 15 [66] |
|
| CareStart G6PD Biosensor (2017; AccessBio, Somerset, NJ, USA) |
Quantitative | 5 µL | 4 min | 0 | USD 670 (device) + USD 3.4 (test strip) [68] USD 500 (device) + 2.5 (test strip) [58] |
|
| STANDARD G6PD Test (2018; SD Biosensor, Suwon, Republic of Korea) | Quantitative | 10 µL | 2 min | 2 | USD 380 (device) + USD 3 (test device) [68] |
|
Sens. = sensitivity; Spec. = specificity; AMM = adjusted male median; RDT = rapid diagnostic test. * Cost refers to manufacturer price recommendations and may vary significantly for different countries. ** Based on non-systematic literature review of commercial assays for which performance has been evaluated in the field, considering spectrophotometry as reference method. $ Performance considering direct sequencing as reference method.
Current PoC phenotypic assays require minimal resources, low expertise in handling, and a short time to show a result. In recent years, several G6PD PoC tests have been developed, including lateral flow qualitative tests to identify G6PD deficiency at around 30% of normal G6PD activity as well as quantitative handheld devices (biosensors) that can identify individuals with intermediate activity (Table 1).
To guide future development of G6PD diagnostics, the WHO has created two target product profiles (TPPs) [74]; one is for screening G6PD at point of care to guide individual treatment decisions (TPP #1), and the other is a one-time quantitative assay that is meant to classify individuals as deficient, intermediate, or G6PD normal once in order to guide any future treatment decisions (TPP #2). The main acceptable and desirable characteristics of TPP #1 and TPP #2 are summarized in Table 2.
Table 2.
Key performance/agreement, storage requirement, and pricing characteristics as guided by the WHO’s TPP for future development of G6PD diagnostics [74].
| Characteristics | Acceptable | Desirable |
|---|---|---|
| TPP #1: PoC Screening Test for G6PD | ||
| Performance in percent positive agreement (PPA) or percent negative agreement (PNA) |
|
|
| Kit storage |
|
|
| Pricing |
|
|
| TPP #2: One-time Quantitative Test for G6PD | ||
| Agreement | Systematic difference (bias):
|
Systematic difference (bias):
|
| Kit storage |
|
|
| Pricing |
|
|
4. Policy and Practice of G6PD Testing
G6PD testing is recommended as part of a ‘good practice statement’ by the WHO [75]. In practice, testing has not been implemented in endemic countries, leading to a disconnect between international guidelines and national policy and practice [76]. Barriers to implementation include the perceived low risk of drug-induced haemolysis, low prioritisation of radical cure treatment because of the perception that vivax malaria is benign, additional costs and financing of implementation, lack of clear guidance on how to provide treatment to G6PD deficient patients, and concerns over additional workload for health staff [77,78,79]. This has changed in recent years, with an increasing number of countries implementing PoC testing.
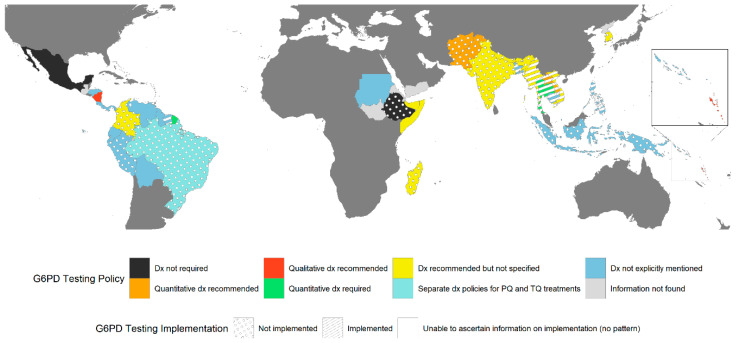
A review of current policy on G6PD testing and treatment (Text S1) is presented according to region: Asia-Pacific (Table S1 [80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110]), Africa and the Middle East (Table S2 [111,112,113,114]), and the Americas (Table S3 [115,116,117,118,119,120,121,122,123,124,125,126,127,128]). Where possible, the current status of practice and implementation was confirmed with local stakeholders (Tables S1–S3). There continues to be a disconnect between policy and practice (Figure 2). More than two thirds of the available national malaria treatment guidelines across the Asia-Pacific (13/17) include a statement on the need for G6PD testing, while testing is only implemented in four of those countries (Lao PDR, Thailand, and Myanmar using a PoC diagnostic (STANDARD G6PD, SD Biosensor, ROK), and centralized testing in South Korea). Despite the absence of a clear recommendation to test, PoC testing using the STANDARD G6PD is rolled out in Bangladesh, Cambodia, Vietnam, and the Solomon Islands, and is planned for 2023 in Bhutan. In addition, large feasibility studies including the use of the STANDARD G6PD are planned in Indonesia and Papua New Guinea.
Figure 2.
G6PD testing policies and their implementation in vivax endemic countries in the Asia-Pacific, the Horn of Africa and Madagascar, and the Americas. Different policies are indicated by different colours in the map, while the policy implementation status is indicated by the overlaying patterns.
In the Americas, only 4 of the 14 vivax endemic countries with available national antimalarial guidelines explicitly recommend G6PD testing (Brazil [116], Colombia [117], French Guiana [120] and Nicaragua [124]). Of these four countries with G6PD testing recommendations, only Brazil is implementing testing with the STANDARD G6PD in the context of the rollout of TQ. They are doing so with temporary approval of the device in two municipalities while it is under review by the National Committee for Health Technology Incorporation (Conitec). No information was ascertained for current implementation in French Guiana and Nicaragua, while Peru and Colombia are planning or conducting feasibility studies to inform the potential rollout.
Out of the five available guidelines in Africa and the Middle East, only two (Somalia [112] and Madagascar [114]) recommend testing, although neither have implemented this in routine practice yet.
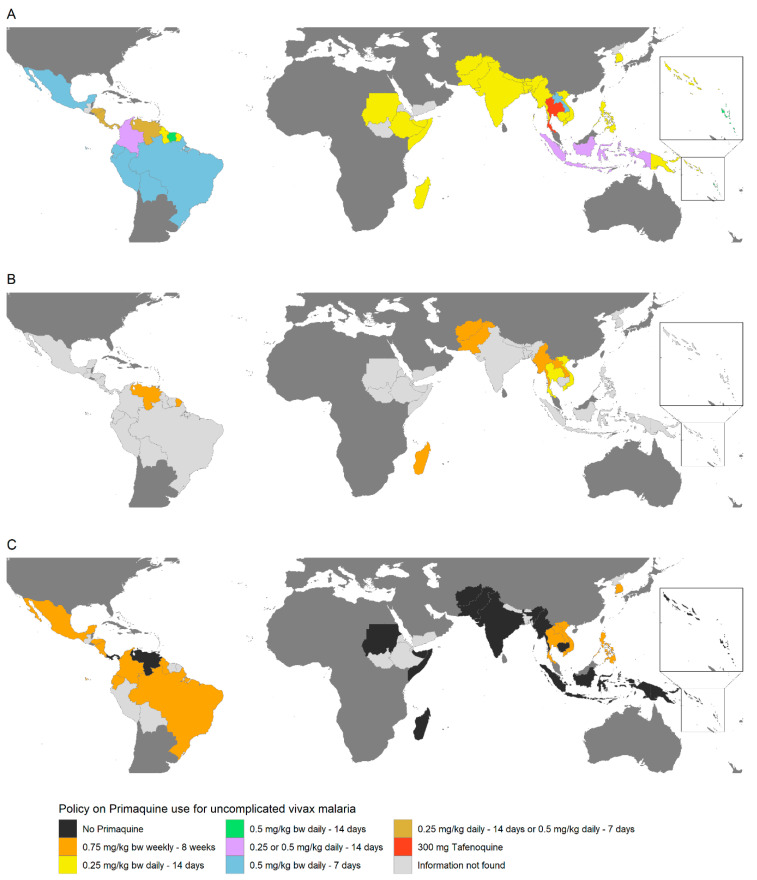
Treatment recommendations based on G6PD status vary between countries, and in most cases, there is a lack of guidance on how to treat patients with intermediate deficiency (Figure 3) or what to do if testing is unavailable.
Figure 3.
Policies on radical cure treatment for uncomplicated vivax malaria according to G6PD testing results in vivax endemic countries in the Asia-Pacific, the Horn of Africa and Madagascar, and the Americas. Treatment regimens are indicated by the country colour on the map. PQ treatment policies for G6PD normal, G6PD intermediate or mildly deficient, and G6PD deficient or severely deficient are shown in maps (A–C), respectively. bw = body weight. In Cambodia, G6PD normal individuals may also be given 0.75 mg/kg bw PQ weekly for 8 weeks. In Vanuatu and Panama, G6PD deficient individuals may also be given 0.75 mg/kg bw PQ weekly for 8 weeks, if access to supervision or blood transfusion is available.
Only a few of the guidelines reviewed included details on whether the deployed assay should be a PoC or laboratory-based assay, and whether the respective diagnostic should return a qualitative or quantitative result. Guidance on the latter was only indicated in Afghanistan [80,81], Lao PDR [91,92,93], Pakistan [98,99], Thailand [106], Vanuatu [107,108], Brazil [116], French Guiana [120], and Nicaragua [124]. Most guidelines do not provide the G6PD activity thresholds to define G6PD normal or deficient status. Some guidelines (11/17 from the Asia-Pacific and 8/14 from the Americas) use terminology such as “G6PD normal”, “intermediate”, and “deficient” without further clarification, while others (4/19 in the Asia-Pacific and 2/14 in the Americas) refer to the older nomenclature of “mild”, “moderate”, and “severe” status, again without a precise definition [129]. Only guidelines from Afghanistan [80,81], Lao PDR [91,92,93], Thailand [106], Vietnam [109,110], Brazil [116], Colombia [117], and Nicaragua [124] state what enzyme activity thresholds determine normal G6PD status either in percent activity or as an absolute value. Vietnam’s guidelines [109,110] provide thresholds but allow for qualitative or quantitative testing. None of the guidelines state what assay those thresholds are based on or how 100% G6PD activity is defined.
5. Early Experiences with the Implementation of PoC G6PD Testing
Several countries have begun implementing PoC diagnostics into routine care or plan to do so in the near future; most are using or considering the STANDARD G6PD. To date, the vast majority of STANDARD G6PD analysers and consumables (Figure 2) are distributed within the Asia-Pacific (58%) region, followed by the Americas (15%), Africa (14%), and the Middle East (11%), compared to only 2% in Europe (SD Biosensor, personal communication). Feedback from early experience with the use and implementation of the STANDARD G6PD in endemic countries (including Brazil, Bangladesh, Cambodia, Lao PDR, Thailand, and Vietnam) can be broadly divided into four types of considerations for the wider rollout: (i) the need for technical improvements of the device itself, (ii) logistical considerations, (iii) the training and supervision required, and (iv) the level of the healthcare system where the test can be performed [130,131,132,133,134,135,136].
Based on their experience with the STANDARD G6PD in Bangladesh, Cambodia, Lao PDR, and Vietnam, users identified required technical improvements and logistical considerations relevant to the wider rollout [130,131,132,133,134,137].
5.1. Technical Challenges
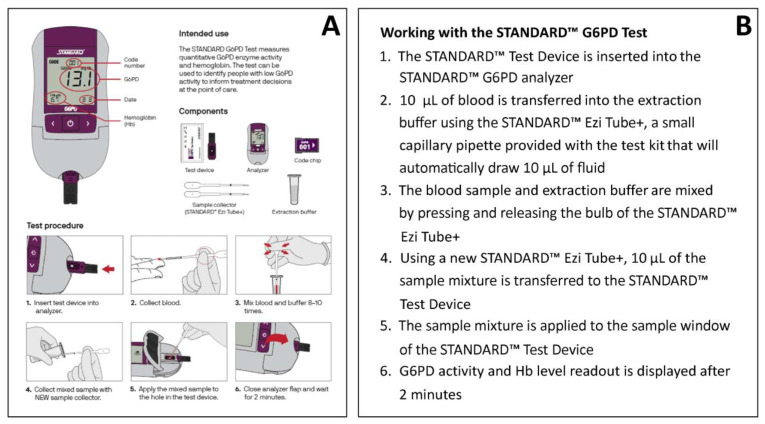
In some areas, healthcare staff have prior experience with qualitative G6PD rapid diagnostic tests (RDTs), specifically the previously WHO-prequalified, qualitative CareStart G6PD lateral flow assay (Access Bio/CareStart, Somerset, NJ, USA) and the quantitative STANDARD G6PD (Table 1). These users appreciated the STANDARD G6PD’s easier result interpretation based on a numeric output and additional haemoglobin reading [130,131]. However, end users also indicated that the STANDARD G6PD testing procedure (Figure 4 [132]) was more complicated than the qualitative CareStart G6PD RDT, which is based on colorimetric principles (Table 1) [130,131]. Some end users reported difficulties with the required two pipetting steps, while others described difficulties with mixing the buffer with the blood sample [130,131,132]. In comparing procedural errors between regular test use and control runs, some users found running controls more difficult [137].
Figure 4.
STANDARD G6PD Test Procedure: (A) Illustrated instructions for the use of the STANDARD G6PD Test from Adhikari et al. (2022) [132], and (B) Step-by-step detailed description of procedures.
5.2. Logistical Considerations
End users commented that the number of included pipettes (n = 50 for 25 test devices) was insufficient to allow for procedural errors [130,133]. In malaria elimination settings with low case numbers, the original shelf life of the test devices (12 months) and original package sizes (25 strips per box) would result in a significant number of expired strips, wasting resources [130]. The shelf life of the test devices and buffer was regarded as being too short to accommodate local logistics, including import processes and customs clearances [130,131]. In response to this feedback, the manufacturer has increased the shelf life of the test devices to 18 months and now offers package sizes of 10 test devices per box (SD Biosensor, personal communication). Additionally, end users suggested making the machine rechargeable rather than being reliant on single-use batteries [130,131,132]. Feedback from community level users suggested that a percentage battery indicator on the screen would help identify devices with a low battery [132]. Community level feedback also recommended including a tube rack for the test kit buffer vials so that they do not fall over when working at village level without laboratory infrastructure [132]. Finally, the appropriate place and time for running controls is an important consideration. As a result of difficulties performing the quality control steps, in Lao, PDR controls have been phased out of district and health centre levels and are only conducted by the national program lab team during supervision visits [137]. In contrast, Cambodia maintains its practice of conducting control runs at the health centre level [130].
5.3. Training and Supervision
Adequate training and supervision are likely to be essential to the successful rollout of the STANDARD G6PD [77,138], especially in areas with low case numbers [134]. Standardised training materials [139] that include background information on the G6PD enzyme, G6PD deficiency, and test and control procedures as well as a practical training agenda have been developed [140]. Generally, NMCPs and pilot projects, such as those in Brazil, Vietnam, Lao PDR, and Bangladesh, have adapted these standardized training materials to varying degrees based on their country context [130,133,135]. National trainings have largely involved the trainings-of-trainers model, while in Lao PDR a training-of-trainers and cascade model starting with central level laboratory technicians was employed due to time and budgetary constraints [141].
Some key considerations for training are the ratio of trainee-to-trainer, time, and resource allocation, and the availability of qualified trainers [130]. An ideal trainer-to-trainee ratio has not been identified to date and varies by program. For the national rollout training in Cambodia, the ratio was 1 to 10, while in Lao PDR it was 1 to 8 at the provincial and district level [130]. In comparison, in research or pilot program contexts, Vietnam’s ratio was one to three and Brazil’s and Thailand’s were one to five [130,135,142]. Ensuring that sufficient time is allocated to individual practice is an important part of training [130,133,142]. Most training workshops of the STANDARD G6PD were delivered over half a day to a day, and in some cases were embedded into larger NMCPs case management training. Early experiences from Vietnam suggest that training at participants’ work sites would be more beneficial compared to centralised training, while in Cambodia, training laboratory technicians on the use of the G6PD test to act as facilitators during training was found to make the process easier [130]. During training, there were benefits to having a demonstration with visual aids, including using G6PD testing process video and an A3 size job aid [130,133,135].
Although users’ practical testing proficiency was the focus of most trainings, conducting formal practical assessments was dependent on time and capacity [133,135,136]. In some cases, formal practical assessments were conducted during supervision visits [136]. In Cambodia, the NMCP highlighted the need to have enough facilitators and time for the competency assessments during training—noting that not all trainees could be assessed [130]. These assessments are based on standardized materials tailored to a country’s needs to varying degrees [139].
Training of health care workers likely requires not only focusing on how to use the diagnostic but also how to interpret G6PD and haemoglobin readings and translate them into treatment decisions. The ongoing TQ Roll-out Study (TRuST) in Brazil and a pilot study in Lao PDR are currently assessing the provision of appropriate treatment according to a patient’s G6PD status, gender, and age [137,143].
In addition to training, adequate supervision of end users is critical, especially during the initial phases of the G6PD testing rollout [78,130,144,145]. Regular supervision visits are crucial for assessing and strengthening the capacity of health workers to conduct the test [130,134,145]. In Cambodia, the national program plans to conduct three supervision visits per year for 15 health centres with low scores in the post-training assessment [136]. In Lao PDR, an assessment is conducted during supervision visits, after which refresher training is provided if required [136]. The number of supervision visits are limited to regular case management supervision visits due to budgetary constraints. However, there is no clear guidance on what level of supervision is required, and this is likely dependent on overall health system capacity. In addition to regular supervision visits, refresher trainings are likely required with varying frequency, especially in areas with low malaria caseloads where trained health professionals use the test infrequently. In an operational study in Brazil implementing the STANDARD G6PD, the study location with the lowest case load had the lowest assessment score at 6 months after initial training. As such, the authors suggest refresher training every 6 months in such locations [146].
5.4. Considerations about Level of Health Care System
Currently, most testing with the STANDARD G6PD is occurring at the health facility level; however, in most endemic settings, patients with malaria are diagnosed at the community level [147,148]. Hence current strategies for G6PD testing require referral of patients diagnosed with malaria at the community level to the health facility for G6PD testing and radical cure treatment. Successful routine referral from community health workers to health facilities with G6PD testing has proven to be challenging and limits the access to adequate treatment [130,136]. The proportion of vivax patients referred to health facilities for G6PD testing and radical cure treatment who subsequently present for testing at the referral site has been shown to be low [141,145]. In Cambodia between February and December 2021, 34% of patients referred by village malaria workers (VMWs) to health facilities for G6PD testing did not reach the health facility [149]. Similarly, in Lao PDR in 2021, only around a third of patients eligible for G6PD testing actually underwent testing, a discrepancy mostly attributed to challenges with patient referral [141]. Referral rates are likely to improve through enhanced training, outreach, patient education, and referral support [150]. This was demonstrated in Cambodia, where the use of qualitative and quantitative PoC G6PD testing was piloted before the wider rollout. In this study, all patients who were referred by VMWs completed referral and received G6PD testing at a health centre. Training of VWMs, community sensitisation, and VMWs often accompanying patients to the health centre aided in completing referrals [150].
An alternative strategy to referral is to conduct G6PD testing at community level. A pilot study from Cambodia found that VMWs have the capacity to perform G6PD testing if given appropriate training and supervision [132]. In the same study, VMWs received a one-day training course, including theoretical and practical components on how to use the STANDARD G6PD. Throughout the study, they were supported by a study coordinator and received refresher training during their monthly visit to the health centre. Comparison of VMW measurements with measurements conducted by laboratory technicians indicated no significant difference in absolute readings and a very good and significant correlation. Such findings are in line with Gerth-Guyette et al. (2021) who found that there was no significant difference in proficiency based on the level of laboratory experience [80]. However, there were differences in how G6PD results were interpreted between VMWs and laboratory technicians [151]. Although this study does show promise for VMWs conducting G6PD testing, quality of measurement and translation of STANDARD G6PD readings into treatment decisions warrants further investigation to inform the operationalisation of VMWs conducting G6PD testing.
Based on these combined early experiences, several key themes need to be addressed as the rollout is progressing (Table 3).
Table 3.
Key themes for G6PD test roll out that require further research.
|
Themes to be
addressed |
|
6. Other Considerations for the Update of Novel Diagnostics
The early experiences with the STANDARD G6PD are encouraging, but reports are primarily focused on technical and logistical considerations. The slow uptake of similar PoC or RDTs such as those for malaria, HIV, and tuberculosis (TB) provide important lessons on the broader societal considerations that are often neglected, including economic implications for widescale implementation of the STANDARD G6PD or other PoC G6PD diagnostics [152].
Uptake of novel diagnostics is influenced by the regard for modern medicine in the community [152]. Apprehensions of new test formats likely contributes to users’ (patients and health workers) poor adherence to diagnostic results, as illustrated by the non-adherence to negative malaria RDT results and the over-prescription of anti-malarials seen in the early days of RDT introduction [152]. Additionally, social acceptance of a new technology is influenced by the perception of its risks and benefits by end users [153]. For example, the belief that blood is sacred influenced patients’ aversion to testing in the context of malaria diagnosis, a phenomenon likely to impact acceptance of any G6PD PoC as well [152]. Information and education communication therefore needs to be locally and culturally appropriate to address negative community perceptions of new diagnostic tests before they present a barrier, as well as provide relevant information on the benefits of the new technology (Table 3).
A shortage of qualified health workers and poorly developed medical infrastructure can contribute to test misuse, misdiagnosis, and test failure [152,154], ultimately leading to the erosion of user confidence in a new diagnostic device [152]. Supply chain issues are also an important infrastructural consideration that NMCPs have raised repeatedly [155] as a potential limiting factor for the widespread adoption of novel PoC diagnostics [152,154,156,157]. Reasons for interruptions of supply lines for diagnostics include inaccurate estimation of new shipment deliveries, insufficient preparation for seasonal demand, difficult transport conditions due to damaged roads, and inadequate compliance with inventory management practices at the local level [152]. In the context of introducing G6PD testing, it is therefore important to also consider supply chain and stock management as part of capacity building efforts, rather than singularly focusing on the end user performance of the test.
Historically, the absence of universal regulation and a standard evaluation process has slowed the uptake of new diagnostic tools such as malaria RDTs [152]. The WHO prequalification process is designed to provide adequate guidance for countries and donors to purchase quality assured products. As such, the Notice of Concern issued by the WHO Prequalification Team for the CareStart RDT has resulted in an interim halt of its rollout [158]. While the STANDARD G6PD is not yet WHO pre-qualified [159], it has received interim approval from the Expert Review Panel for Diagnostics (ERPD) [160], a mechanism aimed to review diagnostics that may have a high public health impact. The device has also received the Conformité Européene (CE) Mark (2017) and approval from the Australian Therapeutic Goods Administration (TGA; 2021) (SD Biosensor, personal communication). The ERDP approval has facilitated the purchase and rollout of the STANDARD G6PD in many countries (Tables S1–S3) through the Global Fund.
Finally, though PoC tests tend to be more affordable than alternative, more complex diagnostics [161], the cost per person screened with the STANDARD G6PD is relatively high (Table 1) [162,163]. These costs are unlikely to be covered by consumers, but rather by the health system and, by extension, external donors such as the Global Fund. Of particular concern is the cost of the STANDARD G6PD analyser per person screened, as this will be dependent on the device’s expected lifetime before it needs to be replaced and the number of patients screened per year. This means that the cost per person screened for G6PD deficiency will be higher at facilities that see fewer patients. In the context of the end stages of malaria elimination, it is unlikely that G6PD screening will be cost-effective in the short-term. Accordingly, the focus needs to shift to the longer-term benefits of malaria elimination. It is also important to note that the indicative price will not be the final cost, which may decrease after negotiation with the supplier after country-level regulatory approval but will need to include shipping, taxes, and other distribution expenses. Another related consideration when evaluating the economic impact of G6PD testing is deciding at what level(s) of the health system STANDARD G6PD might be placed. For example, placing STANDARD G6PD at hospitals that see more vivax malaria patients will result in lower costs per test administered than placing them at community facilities where fewer patients are seen. One option is to refer patients to higher level facilities, but this will be a challenge to balance with ensuring uptake given the findings from Cambodia that a third of patients did not use referrals to higher facilities [149].
The cost effectiveness of implementing G6PD screening with the STANDARD G6PD will vary significantly with heterogeneity in the underlying case burden and severity and the prevalence of G6PD deficiency. For example, in a country with mild variants and low prevalence of G6PD deficiency, the costs of screening may outweigh the benefits since haemolysis would be rare and unlikely to be severe. In places where primaquine is currently prescribed without G6PD screening, a value of information analysis could be conducted in order to help decide whether it is a better use of funding to conduct surveys to determine the prevalence of G6PD deficiency or whether G6PD screening should be implemented without this information.
Current malaria policies usually reflect associated funding by the Global Fund, so it is unclear whether the cost-effectiveness of G6PD testing is an important driver in country-level decision making. However national malaria control programs have ranked cost effectiveness of new approaches as a key area for further research [164], suggesting that this has some impact on policy decisions. Whether an intervention such as G6PD testing is considered cost-effective will also depend on the budget available, which could be a national health budget or a budget specifically for malaria control [165].
7. Conclusions
A range of G6PD PoC are now available, and some of these are likely to be WHO prequalified in the near future. Current experiences with the ongoing implementation of the STANDARD G6PD should inform the optimisation of the broader rollout of this test and will be crucial to facilitate the introduction of alternative diagnostic options. In many cases, policy guidance will need to incorporate the reality of implementation.
Acknowledgments
We extend our gratitude to the National Malaria Control Programs and their partners for sharing their respective country’s malaria treatment guidelines. We also thank them for sharing current G6PD testing practices.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/pathogens12050650/s1, Text S1: Methodology for policy review; Table S1: Radical cure and G6PD testing policy in in the Asia-Pacific; Table S2: Radical cure and G6PD testing policy in countries in Africa and the Middle East; Table S3: Radical cure and G6PD testing policy in Central and South America.
Author Contributions
A.S., S.C.-S., M.M. and B.L. wrote the first draft. A.S., S.C.-S., S.A., M.M. and K.T. collated treatment guidelines and extracted data. A.S., S.C.-S., S.A., A.D., R.N.P., M.M., K.T. and B.L. contributed to writing the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethical approval was not required for this review.
Informed Consent Statement
Informed consent was not required for this review.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
A.S.: S.C.-S. and M.M. are funded through Charles Darwin International PhD Scholarships (CDIPS). K.T. is a CSL Centenary fellow. R.N.P. is funded by NHMRC Leadership Investigator Grants (2008501).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Howes R.E., Battle K.E., Mendis K.N., Smith D.L., Cibulskis R.E., Baird J.K., Hay S.I. Global Epidemiology of Plasmodium vivax. Am. J. Trop. Med. Hyg. 2016;95:15–34. doi: 10.4269/ajtmh.16-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Battle K.E., Lucas T.C.D., Nguyen M., Howes R.E., Nandi A.K., Twohig K.A., Pfeffer D.A., Cameron E., Rao P.C., Casey D., et al. Mapping the global endemicity and clinical burden of Plasmodium vivax, 2000–2017: A spatial and temporal modelling study. Lancet. 2019;394:332–343. doi: 10.1016/S0140-6736(19)31096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . World Malaria Report 2022. World Health Organization; Geneva, Switzerland: 2022. [Google Scholar]
- 4.Nguitragool W., Mueller I., Kumpitak C., Saeseu T., Bantuchai S., Yorsaeng R., Yimsamran S., Maneeboonyang W., Sa-angchai P., Chaimungkun W., et al. Very high carriage of gametocytes in asymptomatic low-density Plasmodium falciparum and P. vivax infections in western Thailand. Parasites Vectors. 2017;10:512. doi: 10.1186/s13071-017-2407-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rovira-Vallbona E., Contreras-Mancilla J.J., Ramirez R., Guzman-Guzman M., Carrasco-Escobar G., Llanos-Cuentas A., Vinetz J.M., Gamboa D., Rosanas-Urgell A. Predominance of asymptomatic and sub-microscopic infections characterizes the Plasmodium gametocyte reservoir in the Peruvian Amazon. PLoS Negl. Trop. Dis. 2017;11:e0005674. doi: 10.1371/journal.pntd.0005674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Motshoge T., Ababio G.K., Aleksenko L., Read J., Peloewetse E., Loeto M., Mosweunyane T., Moakofhi K., Ntebele D.S., Chihanga S., et al. Molecular evidence of high rates of asymptomatic P. vivax infection and very low P. falciparum malaria in Botswana. BMC Infect. Dis. 2016;16:520. doi: 10.1186/s12879-016-1857-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Almeida A.C.G., Kuehn A., Castro A.J.M., Vitor-Silva S., Figueiredo E.F.G., Brasil L.W., Brito M.A.M., Sampaio V.S., Bassat Q., Felger I., et al. High proportions of asymptomatic and submicroscopic Plasmodium vivax infections in a peri-urban area of low transmission in the Brazilian Amazon. Parasites Vectors. 2018;11:194. doi: 10.1186/s13071-018-2787-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng Q., Cunningham J., Gatton M.L. Systematic Review of Sub-microscopic P. vivax Infections: Prevalence and Determining Factors. PLoS Negl. Trop. Dis. 2015;9:e3413. doi: 10.1371/journal.pntd.0003413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ding X.C., Ade M.P., Baird J.K., Cheng Q., Cunningham J., Dhorda M., Drakeley C., Felger I., Gamboa D., Harbers M., et al. Defining the next generation of Plasmodium vivax diagnostic tests for control and elimination: Target product profiles. PLoS Negl. Trop. Dis. 2017;11:e0005516. doi: 10.1371/journal.pntd.0005516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Battle K.E., Karhunen M.S., Bhatt S., Gething P.W., Howes R.E., Golding N., Van Boeckel T.P., Messina J.P., Shanks G.D., Smith D.L., et al. Geographical variation in Plasmodium vivax relapse. Malar. J. 2014;13:144. doi: 10.1186/1475-2875-13-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mueller I., Galinski M.R., Baird J.K., Carlton J.M., Kochar D.K., Alonso P.L., del Portillo H.A. Key gaps in the knowledge of Plasmodium vivax, a neglected human malaria parasite. Lancet Infect. Dis. 2009;9:555–566. doi: 10.1016/S1473-3099(09)70177-X. [DOI] [PubMed] [Google Scholar]
- 12.Commons R.J., Simpson J.A., Watson J., White N.J., Price R.N. Estimating the Proportion of Plasmodium vivax Recurrences Caused by Relapse: A Systematic Review and Meta-Analysis. Am. J. Trop. Med. Hyg. 2020;103:1094–1099. doi: 10.4269/ajtmh.20-0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chu C.S., White N.J. Management of relapsing Plasmodium vivax malaria. Expert Rev. Anti-Infect. Ther. 2016;14:885–900. doi: 10.1080/14787210.2016.1220304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edgcomb J.H., Arnold J., Yount E.H., Alving A.S., Eichelberger L., Jeffery G.M., Eyles D., Young M.D. Primaquine, SN 13272, a new curative agent in vivax malaria; a preliminary report. J. Natl. Malar. Soc. 1950;9:285–292. [PubMed] [Google Scholar]
- 15.World Health Organization . WHO Guidelines for Malaria, 13 July 2021. World Health Organization; Geneva, Switzerland: 2021. (WHO/UCN/GMP/2021.01 Rev.1) License: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 16.World Health Organization . WHO Guidelines for Malaria, 14 March 2023. World Health Organization; Geneva, Switzerland: 2023. (WHO/UCN/GMP/2023.01) License: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 17.Baird J.K. 8-Aminoquinoline Therapy for Latent Malaria. Clin. Microbiol. Rev. 2019;32:e00011-19. doi: 10.1128/CMR.00011-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Douglas N.M., Poespoprodjo J.R., Patriani D., Malloy M.J., Kenangalem E., Sugiarto P., Simpson J.A., Soenarto Y., Anstey N.M., Price R.N. Unsupervised primaquine for the treatment of Plasmodium vivax malaria relapses in southern Papua: A hospital-based cohort study. PLoS Med. 2017;14:e1002379. doi: 10.1371/journal.pmed.1002379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thriemer K., Bobogare A., Ley B., Gudo C.S., Alam M.S., Anstey N.M., Ashley E., Baird J.K., Gryseels C., Jambert E., et al. Quantifying primaquine effectiveness and improving adherence: A round table discussion of the APMEN Vivax Working Group. Malar. J. 2018;17:241. doi: 10.1186/s12936-018-2380-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor W.R.J., Thriemer K., Seidlein L.v., Yuentrakul P., Assawariyathipat T., Assefa A., Auburn S., Chand K., Chau N.H., Cheah P.Y., et al. Short-course primaquine for the radical cure of Plasmodium vivax malaria: A multicentre, randomised, placebo-controlled non-inferiority trial. Lancet. 2019;394:929–938. doi: 10.1016/S0140-6736(19)31285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shanks G.D., Oloo A.J., Aleman G.M., Ohrt C., Klotz F.W., Braitman D., Horton J., Brueckner R. A New Primaquine Analogue, Tafenoquine (WR 238605), for Prophylaxis against Plasmodium falciparum Malaria. Clin. Infect. Dis. 2001;33:1968–1974. doi: 10.1086/324081. [DOI] [PubMed] [Google Scholar]
- 22.Brueckner R.P., Lasseter K.C., Lin E.T., Schuster B.G. First-time-in-humans safety and pharmacokinetics of WR 238605, a new antimalarial. Am. J. Trop. Med. Hyg. 1998;58:645–649. doi: 10.4269/ajtmh.1998.58.645. [DOI] [PubMed] [Google Scholar]
- 23.Cappellini M., Fiorelli G. Glucose-6-phosphate dehydrogenase deficiency. Lancet. 2008;371:64–74. doi: 10.1016/S0140-6736(08)60073-2. [DOI] [PubMed] [Google Scholar]
- 24.Mason P.J., Bautista J.M., Gilsanz F. G6PD deficiency: The genotype-phenotype association. Blood Rev. 2007;21:267–283. doi: 10.1016/j.blre.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Luzzatto L., Ally M., Notaro R. Glucose-6-phosphate dehydrogenase deficiency. Blood. 2020;136:1225–1240. doi: 10.1182/blood.2019000944. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization . Control and Elimination of Plasmodium vivax Malaria: A Technical Brief. World Health Organization; Geneva, Switzerland: 2015. [Google Scholar]
- 27.Howes R.E., Piel F.B., Patil A.P., Nyangiri O.A., Gething P.W., Dewi M., Hogg M.M., Battle K.E., Padilla C.D., Baird J.K., et al. G6PD Deficiency Prevalence and Estimates of Affected Populations in Malaria Endemic Countries: A Geostatistical Model-Based Map. PLoS Med. 2012;9:e1001339. doi: 10.1371/journal.pmed.1001339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Howes R.E., Battle K.E., Satyagraha A.W., Baird J.K., Hay S.I. Chapter Four—G6PD Deficiency: Global Distribution, Genetic Variants and Primaquine Therapy. In: Hay S.I., Price R.N., Baird J.K., editors. Advances in Parasitology. Volume 81. Academic Press; Cambridge, MA, USA: 2013. pp. 133–201. The Epidemiology of Plasmodium vivax. [DOI] [PubMed] [Google Scholar]
- 29.Howes R.E., Dewi M., Piel F.B., Monteiro W.M., Battle K.E., Messina J.P., Sakuntabhai A., Satyagraha A.W., Williams T.N., Baird J.K., et al. Spatial distribution of G6PD deficiency variants across malaria-endemic regions. Malar. J. 2013;12:418. doi: 10.1186/1475-2875-12-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mbanefo E.C., Ahmed A.M., Titouna A., Elmaraezy A., Trang N.T.H., Phuoc Long N., Hoang Anh N., Diem Nghi T., The Hung B., Van Hieu M., et al. Association of glucose-6-phosphate dehydrogenase deficiency and malaria: A systematic review and meta-analysis. Sci. Rep. 2017;7:45963. doi: 10.1038/srep45963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Awab G.R., Aaram F., Jamornthanyawat N., Suwannasin K., Pagornrat W., Watson J.A., Woodrow C.J., Dondorp A.M., Day N.P., Imwong M., et al. Protective effect of Mediterranean-type glucose-6-phosphate dehydrogenase deficiency against Plasmodium vivax malaria. eLife. 2021;10:e62448. doi: 10.7554/eLife.62448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beutler E., Yeh M., Fairbanks V.F. The normal human female as a mosaic of X-chromosome activity: Studies using the gene for G-6-PD-deficiency as a marker. Proc. Natl. Acad. Sci. USA. 1962;48:9–16. doi: 10.1073/pnas.48.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Domingo G.J., Advani N., Satyagraha A.W., Sibley C.H., Rowley E., Kalnoky M., Cohen J., Parker M., Kelley M. Addressing the gender-knowledge gap in glucose-6-phosphate dehydrogenase deficiency: Challenges and opportunities. Int. Health. 2019;11:7–14. doi: 10.1093/inthealth/ihy060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pfeffer D.A., Ley B., Howes R.E., Adu P., Alam M.S., Bansil P., Boum Y., Brito M., Charoenkwan P., Clements A., et al. Quantification of glucose-6-phosphate dehydrogenase activity by spectrophotometry: A systematic review and meta-analysis. PLoS Med. 2020;17:e1003084. doi: 10.1371/journal.pmed.1003084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Domingo G.J., Satyagraha A.W., Anvikar A., Baird K., Bancone G., Bansil P., Carter N., Cheng Q., Culpepper J., Eziefula C., et al. G6PD testing in support of treatment and elimination of malaria: Recommendations for evaluation of G6PD tests. Malar. J. 2013;12:391. doi: 10.1186/1475-2875-12-391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pfeffer D.A., Satyagraha A.W., Sadhewa A., Alam M.S., Bancone G., Boum Y., Brito M., Cui L., Deng Z., Domingo G.J., et al. Genetic Variants of Glucose-6-Phosphate Dehydrogenase and Their Associated Enzyme Activity: A Systematic Review and Meta-Analysis. Pathogens. 2022;11:1045. doi: 10.3390/pathogens11091045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Satyagraha A.W., Sadhewa A., Panggalo L.V., Subekti D., Elyazar I., Soebianto S., Mahpud N., Harahap A.R., Baird J.K. Genotypes and phenotypes of G6PD deficiency among Indonesian females across diagnostic thresholds of G6PD activity guiding safe primaquine therapy of latent malaria. PLoS Negl. Trop. Dis. 2021;15:e0009610. doi: 10.1371/journal.pntd.0009610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.von Seidlein L., Auburn S., Espino F., Shanks D., Cheng Q., McCarthy J., Baird K., Moyes C., Howes R., Ménard D., et al. Review of key knowledge gaps in glucose-6-phosphate dehydrogenase deficiency detection with regard to the safe clinical deployment of 8-aminoquinoline treatment regimens: A workshop report. Malar. J. 2013;12:112. doi: 10.1186/1475-2875-12-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization . Guide to G6PD Deficiency Rapid Diagnostic Testing to Support P. vivax Radical Cure. World Health Organization; Geneva, Switzerland: 2018. p. 26. [Google Scholar]
- 40.Shah S.S., Diakite S.A.S., Traore K., Diakite M., Kwiatkowski D.P., Rockett K.A., Wellems T.E., Fairhurst R.M. A novel cytofluorometric assay for the detection and quantification of glucose-6-phosphate dehydrogenase deficiency. Sci. Rep. 2012;2:299. doi: 10.1038/srep00299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peters A.L., Noorden C.J.F.V. Glucose-6-phosphate Dehydrogenase Deficiency and Malaria: Cytochemical Detection of Heterozygous G6PD Deficiency in Women. J. Histochem. Cytochem. 2009;57:1003–1011. doi: 10.1369/jhc.2009.953828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Minucci A., Giardina B., Zuppi C., Capoluongo E. Glucose-6-phosphate dehydrogenase laboratory assay: How, when, and why? IUBMB Life. 2009;61:27–34. doi: 10.1002/iub.137. [DOI] [PubMed] [Google Scholar]
- 43.Kaplan M., Hammerman C. Neonatal Screening for Glucose-6-Phosphate Dehydrogenase Deficiency: Biochemical Versus Genetic Technologies. Semin. Perinatol. 2011;35:155–161. doi: 10.1053/j.semperi.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 44.Rumaseb A., Marfurt J., Kho S., Kahn M., Price R.N., Ley B. A fluorometric assay to determine the protective effect of glucose-6-phosphate dehydrogenase (G6PD) against a Plasmodium spp. infection in females heterozygous for the G6PD gene: Proof of concept in Plasmodium falciparum. BMC Res. Notes. 2022;15:76. doi: 10.1186/s13104-022-05952-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ley B., Alam M.S., Kibria M.G., Marfurt J., Phru C.S., Ami J.Q., Thriemer K., Auburn S., Jahan N., Johora F.T., et al. Glucose-6-phosphate dehydrogenase activity in individuals with and without malaria: Analysis of clinical trial, cross-sectional and case–control data from Bangladesh. PLoS Med. 2021;18:e1003576. doi: 10.1371/journal.pmed.1003576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ley B., Alam M.S., Satyagraha A.W., Phru C.S., Thriemer K., Tadesse D., Shibiru T., Hailu A., Kibria M.G., Hossain M.S., et al. Variation in Glucose-6-Phosphate Dehydrogenase activity following acute malaria. PLoS Negl. Trop. Dis. 2022;16:e0010406. doi: 10.1371/journal.pntd.0010406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taylor W.R.J., Kim S., Kheng S., Muth S., Tor P., Christophel E., Mukaka M., Kerleguer A., Luzzatto L., Baird J.K., et al. Dynamics of G6PD activity in patients receiving weekly primaquine for therapy of Plasmodium vivax malaria. PLoS Negl. Trop. Dis. 2021;15:e0009690. doi: 10.1371/journal.pntd.0009690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organization . Standardization of Procedures for the Study of Glucose-6-Phosphate Dehydrogenase. Volume 366. World Health Organization; Geneva, Switzerland: 1967. pp. 1–53. (Report of a WHO Scientific Group. World Health Organization Technical Report Series). [PubMed] [Google Scholar]
- 49.Alam M.S., Kibria M.G., Jahan N., Price R.N., Ley B. Spectrophotometry assays to determine G6PD activity from Trinity Biotech and Pointe Scientific G6PD show good correlation. BMC Res. Notes. 2018;11:855. doi: 10.1186/s13104-018-3964-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beutler E., Mitchell M. Brief Report: Special Modifications of the Fluorescent Screening Method for Glucose-6-Phosphate Dehydrogenase Deficiency. Blood. 1968;32:816–818. doi: 10.1182/blood.V32.5.816.816. [DOI] [PubMed] [Google Scholar]
- 51.Beutler E., Halasz A. A Series of New Screening Procedures for Pyruvate Kinase Deficiency, Glucose-6-Phosphate Dehydrogenase Deficiency, and Glutathione Reductase Deficiency. Blood. 1966;28:553–562. doi: 10.1182/blood.V28.4.553.553. [DOI] [PubMed] [Google Scholar]
- 52.Henriques G., Phommasone K., Tripura R., Peto T.J., Raut S., Snethlage C., Sambo I., Sanann N., Nguon C., Adhikari B., et al. Comparison of glucose-6 phosphate dehydrogenase status by fluorescent spot test and rapid diagnostic test in Lao PDR and Cambodia. Malar. J. 2018;17:243. doi: 10.1186/s12936-018-2390-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roca-Feltrer A., Khim N., Kim S., Chy S., Canier L., Kerleguer A., Tor P., Chuor C.M., Kheng S., Siv S., et al. Field Trial Evaluation of the Performances of Point-of-Care Tests for Screening G6PD Deficiency in Cambodia. PLoS ONE. 2014;9:e116143. doi: 10.1371/journal.pone.0116143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bancone G., Chu C.S., Chowwiwat N., Somsakchaicharoen R., Wilaisrisak P., Charunwatthana P., Bansil P., McGray S., Domingo G.J., Nosten F.H. Suitability of Capillary Blood for Quantitative Assessment of G6PD Activity and Performances of G6PD Point-of-Care Tests. Am. J. Trop. Med. Hyg. 2015;92:818–824. doi: 10.4269/ajtmh.14-0696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Espino F.E., Bibit J.-A., Sornillo J.B., Tan A., Seidlein L.v., Ley B. Comparison of Three Screening Test Kits for G6PD Enzyme Deficiency: Implications for Its Use in the Radical Cure of Vivax Malaria in Remote and Resource-Poor Areas in the Philippines. PLoS ONE. 2016;11:e0148172. doi: 10.1371/journal.pone.0148172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Oo N.N., Bancone G., Maw L.Z., Chowwiwat N., Bansil P., Domingo G.J., Htun M.M., Thant K.Z., Htut Y., Nosten F. Validation of G6PD Point-of-Care Tests among Healthy Volunteers in Yangon, Myanmar. PLoS ONE. 2016;11:e0152304. doi: 10.1371/journal.pone.0152304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tantular I.S., Kawamoto F. An improved, simple screening method for detection of glucose-6-phosphate dehydrogenase deficiency. Trop. Med. Int. Health. 2003;8:569–574. doi: 10.1046/j.1365-3156.2003.01055.x. [DOI] [PubMed] [Google Scholar]
- 58.Ley B., Alam M.S., O’Donnell J.J., Hossain M.S., Kibria M.G., Jahan N., Khan W.A., Thriemer K., Chatfield M.D., Price R.N., et al. A Comparison of Three Quantitative Methods to Estimate G6PD Activity in the Chittagong Hill Tracts, Bangladesh. PLoS ONE. 2017;12:e0169930. doi: 10.1371/journal.pone.0169930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Van Noorden C.J., Dolbeare F., Aten J. Flow cytofluorometric analysis of enzyme reactions based on quenching of fluorescence by the final reaction product: Detection of glucose-6-phosphate dehydrogenase deficiency in human erythrocytes. J. Histochem. Cytochem. 1989;37:1313–1318. doi: 10.1177/37.9.2768805. [DOI] [PubMed] [Google Scholar]
- 60.Thedsawad A., Wanachiwanawin W., Taka O., Hantaweepant C. Cut-off values for diagnosis of G6PD deficiency by flow cytometry in Thai population. Ann. Hematol. 2022;101:2149–2157. doi: 10.1007/s00277-022-04923-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim S., Nguon C., Guillard B., Duong S., Chy S., Sum S., Nhem S., Bouchier C., Tichit M., Christophel E., et al. Performance of the CareStart™ G6PD Deficiency Screening Test, a Point-of-Care Diagnostic for Primaquine Therapy Screening. PLoS ONE. 2011;6:e28357. doi: 10.1371/journal.pone.0028357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baird J.K., Dewi M., Subekti D., Elyazar I., Satyagraha A.W. Noninferiority of glucose-6-phosphate dehydrogenase deficiency diagnosis by a point-of-care rapid test vs the laboratory fluorescent spot test demonstrated by copper inhibition in normal human red blood cells. Transl. Res. 2015;165:677–688. doi: 10.1016/j.trsl.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ley B., Satyagraha A.W., Rahmat H., Fricken M.E.v., Douglas N.M., Pfeffer D.A., Espino F., Seidlein L.v., Henriques G., Oo N.N., et al. Performance of the Access Bio/CareStart rapid diagnostic test for the detection of glucose-6-phosphate dehydrogenase deficiency: A systematic review and meta-analysis. PLoS Med. 2019;16:e1002992. doi: 10.1371/journal.pmed.1002992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Osorio L., Carter N., Arthur P., Bancone G., Gopalan S., Gupta S.K., Noedl H., Kochar S.K., Kochar D.K., Krudsood S., et al. Performance of BinaxNOW G6PD Deficiency Point-of-Care Diagnostic in P. vivax-Infected Subjects. Am. J. Trop. Med. Hyg. 2015;92:22–27. doi: 10.4269/ajtmh.14-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tinley K.E., Loughlin A.M., Jepson A., Barnett E.D. Evaluation of a Rapid Qualitative Enzyme Chromatographic Test for Glucose-6-Phosphate Dehydrogenase Deficiency. Am. J. Trop. Med. Hyg. 2010;82:210–214. doi: 10.4269/ajtmh.2010.09-0416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Baird J.K. Point-of-care G6PD diagnostics for Plasmodium vivax malaria is a clinical and public health urgency. BMC Med. 2015;13:296. doi: 10.1186/s12916-015-0531-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.LaRue N., Kahn M., Murray M., Leader B.T., Bansil P., McGray S., Kalnoky M., Zhang H., Huang H., Jiang H., et al. Comparison of Quantitative and Qualitative Tests for Glucose-6-Phosphate Dehydrogenase Deficiency. Am. J. Trop. Med. Hyg. 2014;91:854–861. doi: 10.4269/ajtmh.14-0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Alam M.S., Kibria M.G., Jahan N., Thriemer K., Hossain M.S., Douglas N.M., Phru C.S., Khan W.A., Price R.N., Ley B. Field evaluation of quantitative point of care diagnostics to measure glucose-6-phosphate dehydrogenase activity. PLoS ONE. 2018;13:e0206331. doi: 10.1371/journal.pone.0206331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Weppelmann T.A., von Fricken M.E., Wilfong T.D., Aguenza E., Philippe T.T., Okech B.A. Field Trial of the CareStart Biosensor Analyzer for the Determination of Glucose-6-Phosphate Dehydrogenase Activity in Haiti. Am. J. Trop. Med. Hyg. 2017;97:1262–1270. doi: 10.4269/ajtmh.16-0714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bancone G., Gornsawun G., Chu C.S., Porn P., Pal S., Bansil P., Domingo G.J., Nosten F. Validation of the quantitative point-of-care CareStart biosensor for assessment of G6PD activity in venous blood. PLoS ONE. 2018;13:e0196716. doi: 10.1371/journal.pone.0196716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pengboon P., Thamwarokun A., Changsri K., Kaset C., Chomean S. Evaluation of quantitative biosensor for glucose-6-phosphate dehydrogenase activity detection. PLoS ONE. 2019;14:e0226927. doi: 10.1371/journal.pone.0226927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zobrist S., Brito M., Garbin E., Monteiro W.M., Clementino Freitas S., Macedo M., Soares Moura A., Advani N., Kahn M., Pal S., et al. Evaluation of a point-of-care diagnostic to identify glucose-6-phosphate dehydrogenase deficiency in Brazil. PLoS Negl. Trop. Dis. 2021;15:e0009649. doi: 10.1371/journal.pntd.0009649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pal S., Myburgh J., Bansil P., Hann A., Robertson L., Gerth-Guyette E., Ambler G., Bizilj G., Kahn M., Zobrist S., et al. Reference and point-of-care testing for G6PD deficiency: Blood disorder interference, contrived specimens, and fingerstick equivalence and precision. PLoS ONE. 2021;16:e0257560. doi: 10.1371/journal.pone.0257560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.World Health Organization . Tests for Glucose-6-Phosphate Dehydrogenase Activity: Target Product Profiles. World Health Organization; Geneva, Switzerland: 2022. [Google Scholar]
- 75.World Health Organization . Guidelines for the Treatment of Malaria. 3rd ed. World Health Organization; Geneva, Switzerland: 2015. [Google Scholar]
- 76.Recht J., Ashley E.A., White N.J. Use of primaquine and glucose-6-phosphate dehydrogenase deficiency testing: Divergent policies and practices in malaria endemic countries. PLoS Negl. Trop. Dis. 2018;12:e0006230. doi: 10.1371/journal.pntd.0006230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ley B., Thriemer K., Jaswal J., Poirot E., Alam M.S., Phru C.S., Khan W.A., Dysoley L., Qi G., Kheong C.C., et al. Barriers to routine G6PD testing prior to treatment with primaquine. Malar. J. 2017;16:329. doi: 10.1186/s12936-017-1981-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Adhikari B., Awab G.R., von Seidlein L. Rolling out the radical cure for vivax malaria in Asia: A qualitative study among policy makers and stakeholders. Malar. J. 2021;20:164. doi: 10.1186/s12936-021-03702-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Berte C.J., Lorenzo P.J., Espino F.E. Perceived challenges in implementing point-of-care testing for glucose-6-phosphate-dehydrogenase for malaria patients before primaquine treatment in the Philippines. Res. Sq. Platf. LLC. 2022:preprint. doi: 10.21203/rs.3.rs-2137623/v1. [DOI] [Google Scholar]
- 80.National Malaria and Leishmaniasis Control Program . National Malaria Treatment Guideline. Ministry of Public Health Islamic Republic of Afghanistan; Kabul, Afghanistan: 2017. [Google Scholar]
- 81.National Malaria and Leishmaniasis Control Program . National Strategic Plan “From Malaria Control to Elimination in Afghanistan” 2018–2022. Ministry of Public Health Islamic Republic of Afghanistan; Kabul, Afghanistan: 2017. [Google Scholar]
- 82.National Malaria Elimination and Aedes Transmitted Diseases Control Program . Revised Malaria Treatment Regimen. 6th ed. Ministry of Health and Family Welfare People’s Republic of Bangladesh; Dhaka, Bangladesh: 2019. [Google Scholar]
- 83.National Malaria Elimination Programme . National Strategic Plan for Malaria Elimination in Bangladesh: 2021–2025. Ministry of Health and Family Welfare Bangladesh; Dhaka, Bangladesh: 2020. [Google Scholar]
- 84.Vector-borne Disease Control Programme . National Guidelines on Diagnosis and Treatment of Malaria in Bhutan. 5th ed. Department of Public Health Bhutan; Gelephu, Bhutan: 2019. [Google Scholar]
- 85.Vector-borne Disease Control Programme . Strategic Plan for Elimination of Malaria and Prevention of Re-Introduction in Bhutan 2020–2025. Ministry of Health Kingdom of Bhutan; Thimphu, Bhutan: 2020. [Google Scholar]
- 86.Ministry of Health . National Treatment Guidelines for Malaria in Cambodia. Ministry of Health Kingdom of Cambodia; Phnom Penh, Cambodia: 2014. [Google Scholar]
- 87.National Vector Borne Disease Control Programme . Guidelines for Diagnosis and Treatment of Malaria in India 2011. National Institute of Malaria Research; New Delhi, India: 2011. [Google Scholar]
- 88.National Vector Borne Disease Control Programme . Operational Manual for Malaria Elimination in India 2016 (Version 1) Ministry of Health and Family Welfare Government of India; New Delhi, India: 2016. [Google Scholar]
- 89.National Vector Borne Disease Control Programme . National Framework for Malaria Elimination in India 2016–2030. Ministry of Health and Family Welfare Government of India; New Delhi, India: 2016. [Google Scholar]
- 90.Directorate General of Disease Prevention and Control . Buku Saku Tatalaksana Kasus Malaria 2020 (Malaria Case Management Pocket Book) Ministry of Health Republic of Indonesia; Jakarta, Indonesia: 2019. [Google Scholar]
- 91.Center of Malariology Parasitology and Entomology . Malaria Treatment Guideline (Updated Nov 2017) Ministry of Health Lao People’s Democratic Republic; Vientiane, Laos: 2017. [Google Scholar]
- 92.Center of Malariology Parasitology and Entomology . Malaria NSP 2021–2025. Ministry of Health Lao People’s Democratic Republic; Vientiane, Laos: 2020. [Google Scholar]
- 93.Center of Malariology Parasitology and Entomology . National Guidelines for the Treatment of Malaria. Ministry of Health Lao People’s Democratic Republic; Vientiane, Laos: 2022. [Google Scholar]
- 94.National Malaria Control Programme . Guidelines for Malaria Diagnosis and Treatment in Myanmar. Ministry of Health Republic of the Union of Myanmar; Naypyidaw, Myanmar: 2015. [Google Scholar]
- 95.National Malaria Control Programme . Addendum—Guidelines for Malaria Diagnosis and Treatment in Myanmar. Ministry of Health Republic of the Union of Myanmar; Naypyidaw, Myanmar: 2018. [Google Scholar]
- 96.Epidemiology and Disease Control Division . National Malaria Treatment Protocol. Ministry of Health and Population Government of Nepal; Kathmandu, Nepal: 2019. [Google Scholar]
- 97.Epidemiology and Disease Control Division . National Malaria Strategic Plan 2014–2025. Ministry of Health and Population Government of Nepal; Kathmandu, Nepal: 2018. [Google Scholar]
- 98.Directorate of Malaria Control . National Malaria Case Management Guidelines. Ministry of National Health Services Regulations and Coordination Islamic Republic of Pakistan; Islamabad, Pakistan: 2018. [Google Scholar]
- 99.Directorate of Malaria Control . National Strategic Plan for Malaria Elimination in Pakistan 2021–2035. Directorate of Malaria Control Islamic Republic of Pakistan; Islamabad, Pakistan: 2020. [Google Scholar]
- 100.National Department of Health . National Malaria Treatment Protocol. National Department of Health Independent State of Papua New Guinea; Port Moresby, Papua New Guinea: 2009. [Google Scholar]
- 101.National Malaria Control Program . National Malaria Strategic Plan 2014–2018. National Department of Health Independent State of Papua New Guinea; Port Moresby, Papua New Guinea: 2014. [Google Scholar]
- 102.National Malaria Control and Elimination Program . Philippines Clinical Practice Guidelines for the Diagnosis, Treatment, Prevention, and Control of Malaria in Adults and Special Risk Groups. Department of Health Republic of the Philippines; Manila, Philippines: 2018. [Google Scholar]
- 103.National Vectorborne Disease Control Programme . Solomon Islands Strategic Plan for Malaria Control and Elimination 2021–2025. Ministry of Health and Medical Services Solomon Islands; Honiara, Solomon Islands: 2020. [Google Scholar]
- 104.Ministry of Health and Medical Services . Solomon Islands 2018 Malaria Case Management Guideline. Ministry of Health and Medical Services Solomon Islands; Honiara, Solomon Islands: 2018. [Google Scholar]
- 105.Korea Centers for Disease Control and Prevention . 2019년 말라리아 진료 가이드 (Malaria Practice Guide 2019) Ministry of Health and Welfare Government of South Korea; South Chungcheong, Republic of Korea: 2019. [Google Scholar]
- 106.Division of Vector-Borne Diseases . Medical Practice Guidelines for Malaria Disease Treatment 2021. Ministry of Public Health Kingdom of Thailand; Nonthaburi, Thailand: 2021. [Google Scholar]
- 107.National Malaria and Vector Borne Diseases Control Program . Malaria Diagnosis and Treatment Guidelines 2021. Republic of Vanuatu Ministry of Health; Port Villa, Vanuatu: 2021. [Google Scholar]
- 108.National Malaria and Vector Borne Diseases Control Program . National Strategic Plan for Malaria Elimination 2021–2026. Republic of Vanuatu Ministry of Health; Port Vila, Vanuatu: [Google Scholar]
- 109.National Malaria and Vector Borne Diseases Control Program . Guidelines for Malaria Diagnosis, Treatment and Prevention: MOH Decision No. 4845/QD-BYT. Ministry of Health Socialist Republic of Viet Nam; Hanoi, Viet Nam: 2016. [Google Scholar]
- 110.National Malaria and Vector Borne Diseases Control Program . National Strategic Plan on Malaria Control and Elimination 2021–2025. Ministry of Health Socialist Republic of Viet Nam; Hanoi, Viet Nam: 2020. [Google Scholar]
- 111.Ministry of Health . National Malaria Guidelines. 5th ed. Ministry of Health Federal Democratic Republic of Ethiopia; Addis Ababa, Ethiopia: 2022. [Google Scholar]
- 112.National Malaria Control Program . Guidelines for the Diagnosis and Treatment of Malaria in Somalia 2016. Ministry of Health Federal Government of Somalia Puntland and Somaliland; Mogadishu, Somaliland: 2016. [Google Scholar]
- 113.Directorate of Communicable and Non-communicable Diseases Control . Sudan Malaria Diagnosis and Treatment Protocol 2017. Federal Ministry of Health Republic of Sudan; Khartoum, Sudan: 2017. [Google Scholar]
- 114.Directorate for the Fight against Malaria . Prise en charge des cas de paludism—Manuel de Référence (Malaria Case Management Reference Manual) Ministry of Public Health Republic of Madagascar; Antananarivo, Madagascar: 2015. [Google Scholar]
- 115.Pharmacotherapeutic Committee of the Malaria Program . Manual de Tratamiento de la Malaria (Malaria Treatment Manual) Ministry of Health and Sports Bolivian Plurinational State; La Paz, Bolivia: 2013. [Google Scholar]
- 116.Department of Immunization and Communicable Diseases . Guia de Tratamento da Malária no Brasil (Malaria Treatment guidelines for Brazil) Ministry of Health Federative Republic of Brazil; Brasilia, Brazil: 2020. [Google Scholar]
- 117.Ministry of Health and Social Protection . Guía de Práctica Clínica Diagnóstico y Tratamiento de la Malaria (Clinical Practice Guidelines Diagnosis and Treatment of Malaria) Ministry of Health and Social Protection Republic of Colombia; Bogotá, Colombia: 2022. [Google Scholar]
- 118.Costa Rican Social Security Fund . Protocolo Para La Atención de la Persona Con Malaria Según Nivel de Atención (Protocol for the Care of the Person with Malaria by Level of Attention) Directorate of Development of Health Services Republic of Costa Rica; San José, Costa Rica: 2020. [Google Scholar]
- 119.Ministry of Public Health . Diagnóstico y Tratamiento de Malaria (Diagnosis and Treatment of Malaria) Ministry of Public Health Republic of Ecuador; Quito, Ecuador: 2019. [Google Scholar]
- 120.Regional Health Agency . Plan de Lutte Contre le Paludism en Guyane 2015–2018 (Plan against Malaria in Guiana 2015–2018) Regional Health Agency Territorial Collectivity of French Guiana; Cayenne, French Guiana: 2015. [Google Scholar]
- 121.National Malaria Control Program . Malaria Treatment Guideline for Health Facilities in Guyana 2015. Ministry of Public Health Co-Operative Republic of Guyana; Georgetown, Guyana: 2015. [Google Scholar]
- 122.Ministry of Health . Protocolo De Atención Integral a la Malaria (Comprehensive Malaria Care Protocol) Ministry of Health Republic of Honduras; Tegucigalpa, Honduras: 2018. [Google Scholar]
- 123.National Center for Disease Control and Preventive Programs . Manual de Tratamientos Medicos para la Atención de Casos Confirmados de Paludismo en México (Manual of Medical Treatments for the Care of Confirmed Cases of Malaria in Mexico) Secretariat of Health Mexico; Mexico City, Mexico: 2022. [Google Scholar]
- 124.Ministry of Health . Guía para el Manejo Clínico de la Malaria (Guide to the Clinical Management of Malaria) Ministry of Health Republic of Nicaragua; Managua, Nicaragua: 2022. [Google Scholar]
- 125.Directorate General of Public Health . Guía de Abordaje Integral para la Eliminación de la Malaria en la República de Panamá (Integral Approach Guide for the Elimination of Malaria in the Republic of Panama) Ministry of Health Republic of Panama; Panama City, Panama: 2022. [Google Scholar]
- 126.Directorate General of People’s Health . Norma Tecnica de Salud Para la Atencion de la Malaria y Malaria Grave en el Peru (Technical Health Standard for Malaria Care and Severe Malaria in Peru) Ministry of Health Republic of Peru; Lima, Peru: 2015. [Google Scholar]
- 127.National Malaria Board . Malaria Preventie en Therapie Protocol 2018 (Malaria Prevention and Therapy Protocol 2018) Ministry of Health Republic of Suriname; Paramaribo, Suriname: 2018. [Google Scholar]
- 128.Ministry of Popular Power for Health . Pautas de Tratamiento en Casos de Malaria (Treatment Guidelines in Malaria Cases) Ministry of Popular Power for Health Bolivarian Republic of Venezuela; Caracas, Venezuela: 2017. [Google Scholar]
- 129.Yoshida A., Beutler E., Motulsky A.G. Human glucose-6-phosphate dehydrogenase variants. Bull. World Health Organ. 1971;45:243–253. [PMC free article] [PubMed] [Google Scholar]
- 130.Vanisaveth V.C.K., Vongviengxay S., Cassidy-Seyoum S., Nguyen H., Tsai Y. GORCoP: Early Experiences with Point-of-Care G6PD Testing in Malaria Case Management. [(accessed on 18 October 2022)];GORCoP Zoom. 2021 Available online: https://www.youtube.com/watch?v=Up9oVdYvG60. [Google Scholar]
- 131.Engel N., Ghergu C., Matin M.A., Kibria M.G., Thriemer K., Price R.N., Ding X.C., Howes R.E., Ley B., Incardona S., et al. Implementing radical cure diagnostics for malaria: User perspectives on G6PD testing in Bangladesh. Malar. J. 2021;20:217. doi: 10.1186/s12936-021-03743-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Adhikari B., Tripura R., Dysoley L., Callery J.J., Peto T.J., Heng C., Vanda T., Simvieng O., Cassidy-Seyoum S., Ley B., et al. Glucose 6 Phosphate Dehydrogenase (G6PD) quantitation using biosensors at the point of first contact: A mixed method study in Cambodia. Malar. J. 2022;21:282. doi: 10.1186/s12936-022-04300-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Alam M.S. GORCoP: A Training for Health Service Providers on the SD Biosensor STANDARD G6PD Test in Bangladesh. [(accessed on 24 October 2022)];GORCoP Zoom. 2020 Available online: https://www.youtube.com/watch?v=Cze6OeHYQXk. [Google Scholar]
- 134.Gerth-Guyette E., Cassidy-Seyoum S., Nguyen H. Integrating G6PD Point-of-Care Testing into Malaria Case Management to Support Radical Cure: An Assessment of Health Worker Skills and Knowledge in Laos and Vietnam; Proceedings of the 70th ASTMH Annual Meeting 2021 Poster Presentation; Virtual. 17–21 November 2021. [Google Scholar]
- 135.Brito-Sousa J.D. GORCoP: Training Healthcare Providers for Point of Care G6PD Testing in Brazil. [(accessed on 14 October 2022)];GORCoP Zoom. 2020 Available online: https://www.youtube.com/watch?v=TmJI67YNb_U. [Google Scholar]
- 136.CHAI Cambodia and Laos . G6PD Testing in Cambodia and Laos—Piloting and Implementation. P. vivax Information Hub; Phnom Penh, Cambodia: 2021. [Google Scholar]
- 137.Finn T. Expanding access to safe radical cure: A study to assess the operational feasibility of reactive case detection and integrating quantitative G6PD testing into P. vivax malaria case management in Lao PDR; Proceedings of the International Congress for Tropical Medicine and Malaria 2022; Bangkok, Thailand. 24–28 October 2022. [Google Scholar]
- 138.Kitchakarn S., Lek D., Thol S., Hok C., Saejeng A., Huy R., Chinanonwait N., Thimasarn K., Wongsrichanalai C. Implementation of G6PD testing and primaquine for P. vivax radical cure: Operational perspectives from Thailand and Cambodia. WHO South-East Asia J. Public Health. 2017;6:60. doi: 10.4103/2224-3151.213793. [DOI] [PubMed] [Google Scholar]
- 139.Gerth-Guyette E., Adissu W., Brito M., Garbin E., Macedo M., Sharma A., Das S., Lacerda M.V.G., Pereira D., Talukdar A., et al. Usability of a point-of-care diagnostic to identify glucose-6-phosphate dehydrogenase deficiency: A multi-country assessment of test label comprehension and results interpretation. Malar. J. 2021;20:307. doi: 10.1186/s12936-021-03803-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.PATH G6PD Operational Research Community of Practice (GORCOP) G6PD Training Materials. [(accessed on 7 December 2022)]. Available online: https://www.path.org/programs/diagnostics/gorcop-g6pd-test-training-materials/
- 141.Chindavongsa K. Paving the way to elimination by optimizing P. vivax radical cure: Roll-out of Point of Care G6PD Testing in Lao PDR; Proceedings of the 71st ASTMH Annual Meeting; Seattle, WA, USA. 30 October–3 November 2022. [Google Scholar]
- 142.Bancone G. G6PD Tests Training; Proceedings of the APMEN Vivax Working Group Annual Meeting 2022; Hilton, Bangkok. 12–14 December 2022. [Google Scholar]
- 143.Lacerda M.V.G. TRuST: Assess operational feasibility of providing appropriate radical cure after G6PD testing; Proceedings of the APMEN Vivax Working Group Annual Meeting 2022; Hilton, Bangkok. 12–14 December 2022. [Google Scholar]
- 144.VivAccess Compliance and Adherence to Primaquine Treatment in Myanmar: A Brief of Available Evidence. 2021. [(accessed on 24 October 2022)]. Available online: https://www.vivaxmalaria.org/resources/compliance-and-adherence-to-primaquine-treatment-in-myanmar-%E2%80%94-a-brief-of-available.
- 145.Dysoley L. From evidence to nationwide policy: The rollout of P. vivax radical cure with G6PD testing in Cambodia, November 2019 to June 2021; Proceedings of the APMEN Vivax Working Group 2021 Poster Presentation; Online. 9–11 August 2021; [(accessed on 18 October 2022)]. Available online: https://www.vivaxmalaria.org/resources/poster-from-evidence-to-nationwide-policy-the-rollout-of-p-vivax-radical-cure-with-g6pd. [Google Scholar]
- 146.Brito-Sousa J.D., Murta F., Vitor-Silva S., Sampaio V., Mendes M., Souza B., Batista T., Santos A., Marques L., Barbosa L., et al. Quantitative G6PD Deficiency Screening in Routine Malaria Diagnostic Units in the Brazilian Amazon (SAFEPRIM): An Operational Mixed-Methods Study. Pathogens. 2022;11:1328. doi: 10.3390/pathogens11111328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Chhim S., Piola P., Housen T., Herbreteau V., Tol B. Malaria in Cambodia: A Retrospective Analysis of a Changing Epidemiology 2006–2019. Int. J. Environ. Res. Public Health. 2021;18:1960. doi: 10.3390/ijerph18041960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.World Health Organization . How Village Malaria Workers Lead the Fight against Malaria in Purworejo. World Health Organization; Geneva, Switzerland: 2021. [Google Scholar]
- 149.Dysoley L., Iqubal S., Chhun B., Samphor N.T., Nguon S., Peng S., Dunn J.C., Cheung H.C., Tsai Y., Sovannaroth S., et al. Applying an effective coverage cascade to measure gaps in case management of P. vivax malaria, improve coverage, and maximize impact in Cambodia; Proceedings of the 71st ASTMH Annual Meeting 2022; Seattle, WA, USA. 30 October–3 November 2022. [Google Scholar]
- 150.Kheang S.T., Ridley R., Ngeth E., Ir P., Ngor P., Sovannaroth S., Lek D., Phon S., Kak N., Yeung S. G6PD testing and radical cure for Plasmodium vivax in Cambodia: A mixed methods implementation study. PLoS ONE. 2022;17:e0275822. doi: 10.1371/journal.pone.0275822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Adhikari B., Tripura R., Dysoley L., Peto T.J., Callery J.J., Heng C., Vanda T., Simvieng O., Cassidy-Seyoum S., Thriemer K., et al. Glucose-6-Phosphate Dehydrogenase (G6PD) Measurement Using Biosensors by Community-Based Village Malaria Workers and Hospital Laboratory Staff in Cambodia: A Quantitative Study. Pathogens. 2023;12:400. doi: 10.3390/pathogens12030400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Miller E., Sikes H.D. Addressing Barriers to the Development and Adoption of Rapid Diagnostic Tests in Global Health. Nanobiomedicine. 2015;2:2–6. doi: 10.5772/61114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Starr C. Social benefit versus technological risk. Science. 1969;165:1232–1238. doi: 10.1126/science.165.3899.1232. [DOI] [PubMed] [Google Scholar]
- 154.Engel N., Ochodo E.A., Karanja P.W., Schmidt B.M., Janssen R., Steingart K.R., Oliver S. Rapid molecular tests for tuberculosis and tuberculosis drug resistance: A qualitative evidence synthesis of recipient and provider views. Cochrane Database Syst. Rev. 2022;4:CD014877. doi: 10.1002/14651858.CD014877.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Averilla L. Supply chain issues—Why did stock data come up as such a high priority across so many countries?; Proceedings of the APMEN Vivax Working Group Annual Meeting 2022; Hilton, Bangkok. 12–14 December 2022. [Google Scholar]
- 156.Mwaura M., Engel N. Constructing confidence: User perspectives on AlereLAM testing for tuberculosis. Int. J. Infect. Dis. 2021;112:237–242. doi: 10.1016/j.ijid.2021.09.018. [DOI] [PubMed] [Google Scholar]
- 157.Engel N., Wolffs P.F.G. Aligning diagnostics to the point-of-care: Lessons for innovators, evaluators and decision-makers from tuberculosis and HIV. BMJ Glob. Health. 2020;5:e003457. doi: 10.1136/bmjgh-2020-003457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.World Health Organization WHO Information Notice for Users 2020/1. [(accessed on 15 December 2022)]; Available online: https://www.who.int/news/item/13-02-2020-who-information-notice-for-users-2020-1.
- 159.World Health Organization . WHO List of Prequalified In Vitro Diagnostic Products. World Health Organization; Geneva, Switzerland: 2023. [Google Scholar]
- 160.The Global Fund . List of Rapid Diagnostic Test (Rdt) Kits for Malaria Classified According to the Global Fund Quality Assurance Policy. The Global Fund; Geneva, Switzerland: 2022. [Google Scholar]
- 161.Devine A., Pasaribu A.P., Teferi T., Pham H.-T., Awab G.R., Contantia F., Nguyen T.-N., Ngo V.-T., Tran T.-H., Hailu A., et al. Provider and household costs of Plasmodium vivax malaria episodes: A multicountry comparative analysis of primary trial data. Bull. World Health Organ. 2019;97:828–836. doi: 10.2471/BLT.18.226688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Devine A., Howes R.E., Price D.J., Moore K.A., Ley B., Simpson J.A., Dittrich S., Price R.N. Cost-Effectiveness Analysis of Sex-Stratified Plasmodium vivax Treatment Strategies Using Available G6PD Diagnostics to Accelerate Access to Radical Cure. Am. J. Trop. Med. Hyg. 2020;103:394–403. doi: 10.4269/ajtmh.19-0943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Brito-Sousa J.D., Peixoto H.M., Devine A., Silva-Neto A.V., Balieiro P.C.S., Sampaio V.S., Vitor-Silva S., Mendes M.O., Souza B.K.A., Lacerda M.V.G., et al. Real-life quantitative G6PD screening in Plasmodium vivax patients in the Brazilian Amazon: A cost-effectiveness analysis. PLoS Negl. Trop. Dis. 2022;16:e0010325. doi: 10.1371/journal.pntd.0010325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ruwanpura V.S.H., Nowak S., Gerth-Guyette E., Theodora M., Dysoley L., Haile M., Peeters Grietens K., Price R.N., Lynch C.A., Thriemer K. Further evidence needed to change policy for the safe and effective radical cure of vivax malaria: Insights from the 2019 annual APMEN Vivax Working Group meeting. Asia Pac. Policy Stud. 2021;8:208–242. doi: 10.1002/app5.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Paulden M., O’Mahony J., McCabe C. Determinants of Change in the Cost-effectiveness Threshold. Med Decis. Mak. 2017;37:264–276. doi: 10.1177/0272989X16662242. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.