Abstract
An increase in life expectancy leads to a greater impact of chronic non-communicable diseases. This is even more remarkable in elder populations, to whom these become main determinants of health status, affecting mental and physical health, quality of life, and autonomy. Disease appearance is closely related to the levels of cellular oxidation, pointing out the importance of including foods in one’s diet that can prevent oxidative stress. Previous studies and clinical data suggest that some plant-based products can slow and reduce the cellular degradation associated with aging and age-related diseases. Many plants from one family present several applications that range from the food to the pharmaceutical industry due to their characteristic flavor and scents. The Zingiberaceae family, which includes cardamom, turmeric, and ginger, has bioactive compounds with antioxidant activities. They also have anti-inflammatory, antimicrobial, anticancer, and antiemetic activities and properties that help prevent cardiovascular and neurodegenerative diseases. These products are abundant sources of chemical substances, such as alkaloids, carbohydrates, proteins, phenolic acids, flavonoids, and diarylheptanoids. The main bioactive compounds found in this family (cardamom, turmeric, and ginger) are 1,8-cineole, α-terpinyl acetate, β-turmerone, and α-zingiberene. The present review gathers evidence surrounding the effects of dietary intake of extracts of the Zingiberaceae family and their underlying mechanisms of action. These extracts could be an adjuvant treatment for oxidative-stress-related pathologies. However, the bioavailability of these compounds needs to be optimized, and further research is needed to determine appropriate concentrations and their antioxidant effects in the body.
Keywords: antioxidant activity, Elettaria cardamomum L. Maton (cardamom), Curcuma longa L. (turmeric), Zingiber officinale Roscoe (ginger), bioactive compounds
1. Introduction
The use of natural bioactive compounds to prevent and improve health is widely accepted. Traditional medicine has always found in nature an important source of remedies for numerous pathologies. This is the basis for the use of nutraceuticals as adjuvants in these conditions. The Zingiberaceae family, comprising more than 1400 species distributed in tropical and subtropical areas, has been widely used in traditional Chinese and Indian medicine to prevent and treat numerous pathologies [1,2]. Plants of this family are also used as foods (spices and herbs) and to produce natural dyes [3].
To this family belongs cardamom, turmeric, and ginger. These plants are among the most active natural remedies due to their numerous biological properties. The following activities are attributed to them: antioxidant, anti-inflammatory, anticancer, antigrowth, antiarthritic, antiatherosclerotic, antidepressant, antiaging, antidiabetic, antimicrobial, wound healing, and memory enhancing [4,5].
The most used varieties of cardamom are green and black. The main bioactive compounds of cardamom are terpenes and phenolic compounds, which exhibit powerful antioxidant properties. Their main bioactive compounds are as follows: 1,8-cineole, α-terpinyl acetate, nerolidol, sabinene, g-terpinene, α-pinene, methyl linoleate, α-terpineol, β-pinene, n-hexadecanoic acid, and limonene [6]. 1,8-cineole and α-terpinyl acetate are the principle bioactive components in black and green cardamom (Table 1). These compounds aid in safeguarding against chronic diseases and oxidative stress (OS) [6,7]. Additionally, cardamom has been found to improve insulin sensitivity and glucose uptake [8], which may help to reduce the risk of type 2 diabetes [9].
Turmeric has a very complex and diverse composition; principally containing terpenoids and phenolic compounds, it also contains other compounds, such as carbohydrates (sugars and fiber), proteins, minerals, and resin [10]. Mainly, turmeric bioactive compounds are curcuminoids (curcumin I, II, and III) and non-curcuminoid compounds [11] (Table 1). Curcumin has been shown to possess strong antioxidant activities that help protect against OS and various chronic diseases [12,13,14]. Curcumin is a powerful scavenger of free radicals (FR), which are unstable molecules that damage cells and contribute to the development of chronic diseases such as cancer, heart disease, and diabetes [15,16,17]. Non-curcuminoid compounds [11] also present significant biological activity and have been attributed with anti-inflammatory, antioxidant, and anticancer properties [10].
The main bioactive compounds of ginger are phenolic compounds and terpenes (Table 1). In addition to these it contains polysaccharides, such as fiber, lipids, and organic acids [18]. Its most bioactive phenolic compounds are gingerols, shogaols, and paradols. The first ones are found in ginger and from them the others are obtained by heat treatment and hydrogenation, respectively. Many beneficial properties have been attributed to ginger, including treatments for arthritis, muscular aches, pain, sore throat, cramps, hypertension, dementia, fever, infectious diseases, cough, nervous diseases, gingivitis, asthma, and gastric disorders, among others [19,20,21]. Both gingerols and shogaols exhibit a host of biological activities, ranging from anticancer, antioxidant, antimicrobial, anti-inflammatory, and anti-allergic to various central nervous system activities [22].
Table 1.
| Plants | Dose | Phytochemicals | Bioactive Compounds |
|---|---|---|---|
| Cardamom | 1–3 g/d | Terpenes | 1,8-cineole, α-terpinyl acetate, nerolidol, sabinene, g-terpinene, α-pinene, methyl linoleate, α-terpineol, β-pinene, n-hexadecanoic acid, and limonene |
| Phenolic compounds | Curcumin I (1,7-bis(4-hydroxy-3-methoxyphenyl)-1,6-heptadiene-3,5-dione) | ||
| Turmeric | 0.5–2 g/d | Curcuminoid (polyphenolic compounds) |
Curcumin II (demethoxycurcumin, 1-(4-hydroxy-3-methoxyphenyl)-7-(4-hydroxyphenyl)-1,6-heptadiene-3,5-dione, and curcumin III (bisdemethoxycurcumin, 1,7-bis(4-hydroxyphenyl)-1,6-heptadiene-3,5-dione) |
| Non-curcuminoids (terpenoids and phenolic compounds) |
Turmerones, elemene, bisacurone, curdione, cyclocurcumin, germacrone, furanodiene, curcumol, and calebin A | ||
| Ginger | 1–3 g/d | Phenolics compounds | Gingerols, shogaols, paradols, quercetin, zingerone, and gingerenone-A |
| Terpene components | β-bisabolene, α-curcumene, zingiberene, α-farnesene, β-sesquiphellandrene, and zingiberene |
Overall, the Zingiberaceae family offers a wealth of health benefits, which turns into a valuable addition to a healthy diet, as its beneficial effects are enhanced by its culinary use as a spice, making it a tasty and convenient way to add antioxidants to one’s diet [24].
Regarding the bioavailability of these compounds, curcumin has a poor pharmacokinetic profile and low bioavailability in humans, even at high doses. It is chemically unstable, poorly soluble in water, and degrades at an alkaline pH. Therefore, curcumin is poorly absorbed in the small intestine, combined with a high hepatic reductive and conjugative metabolism that clears curcumin components quickly by biliary and urine excretion [25]. Only a small amount of curcumin is distributed from blood to tissue [26]. Several authors [27] have observed that a dose of 8 g of turmeric has no adverse effects in humans.
The bioavailability of curcumin depends on the types of molecular complexes it creates. It forms them with carbohydrates, proteins (such as whey proteins, bovine serum albumin, and β-lactoglobulin), lipids (phospholipids), and bioactive compounds, such as resveratrol, quercetin, and piperine, and the formation of these contributes to increasing the bioavailability of curcumin [27].
The absorption of curcumin is multiplied by 10 times when ingested together with piperine [28]. Piperine is the alkaloid responsible for the pungency of black pepper that inhibits glucuronidation processes by the enzyme UDP-glucuronosyltransferase in the small intestine and liver [12].
The amount of curcumin distributed from the blood to the tissues is very small, below the detection limit. Liposomes, capable of carrying lipophobic and hydrophobic particles, are being used to improve the bioavailability of curcumin. Curcumin analogues can also be used, modifying their chemical structure to improve absorption. Curcumin analogues include the following: bis-o-hydroxycinnamoylmethane, bis-1.7-(2-hydroxyphenyl)-hepta-1.6-diene-3.5-dione (BDMC), tetrahydrocurcumin (THC) analogs, and two new curcumin derivatives, B06 and C66, which have been shown in studies to have higher bioavailability [29].
Gingerols (the main compounds of ginger) have the problem of low solubility, especially 6-gingerol. It is important to optimize them through different techniques, such as nanotechnology, to increase their bioavailability [30,31,32].
With respect to the metabolization of the main compounds of ginger root (6-, 8-, and 10-gingerol and 6-shogaol), it is observed that glucuronide-conjugated metabolites are the major metabolites, and sulfate-conjugated metabolites are also detected [17]. These authors have observed that these metabolites are detected in blood samples after 15 min of consumption. These authors did not detect 6-shogaol or free 6-8-10 gingerols.
Several authors have observed that the main metabolic pathway of shogaols and gingerols is ketone reduction, with gingerdiols being the main metabolites. Conjugation with cysteine is one of the main metabolic pathways of 6-shogaol (90%). We could consider these metabolites as responsible for the beneficial effects of gingerols and shogaols [25].
Zhang et al. 2022 have observed in asthmatic patients that 33% of 6-gingerol is metabolized to its reducing metabolites, which are the 6-girgerdiols. 6-shogaol is metabolized to its phase I metabolites and conjugated to cysteine. The half-life of these compounds ranges from 0.6 to 2.4 h [26]. Chen et al. [33] showed that hydrogenation, oxidation, and demethylation metabolisms of gingerols are the main metabolic types in microsomes. However, there are differences in metabolic kinetics and the metabolic types of different species of liver microsomes. CYP2C19 and CYP1A2 are the main enzymes involved in the oxidation and demethylation metabolism of these gingerols, but the affinity of the gingerols is not balanced.
Bioactive compounds in cardamom also have low bioavailability due to complex molecular structure [34]. Their pharmaceutical and food applications are limited by the low solubility of their active components in aqueous media. Encapsulation could be a solution to improve their bioavailability and stability [6].
The objective of this review is to establish and unify in a single comprehensive review how the antioxidant capacity of the Zingiberaceae family, particularly turmeric, ginger, and cardamom, could contribute to health-associated benefits by the intake of their bioactive compounds through diet.
2. Relationship between Oxidative Stress and Health
OS is known as an imbalance between oxidizing agents and antioxidants in favor of the first [35]. This imbalance may be due to a low intake of antioxidants, depletion of endogenous antioxidants, or an increase in reactive species (RS) [36]. Consequently, it can induce damage to lipids, proteins, and DNA [37].
Among RS [38] are highlighted those of oxygen (ROS) [39], synthesized in cells during mitochondrial oxidative metabolism, and those of nitrogen (RNS), synthesized under hypoxia conditions [40]; there are also RS of sulfur (RSS) [41], of carbonyl (RCS) [42], and of selenium (RSeS) [43]. It is known that under physiological conditions, the organism can synthesize ROS in small quantities, which is afterwards neutralized. ROS are involved in vital processes for the organism, such as cellular homeostasis, gene expression, receptor activation, or signal transduction. Excessive and prolonged production of ROS and RNS may turn into damage to cell structure and function, which can lead to irreparable changes. For instance, lipid peroxidation of membrane lipids can impair membrane function, inactivate membrane receptors and enzymes, increase permeability to ions, decrease membrane fluidity, and ultimately rupture the membrane [39].
There are different types of SRs, and whenever possible it is convenient to use the name of the specific chemical species instead of using the term FR, since depending on their origin, some are radical (they have an unpaired electron) and others are non-radical (they are the product of the reduction of two electrons), as shown in Table 2 [38].
Table 2.
Classification of the most common reactive species. Adapted from Sies and collaborators [38].
| Free Radicals | No Radicals |
|---|---|
| Reactive Oxygen Species | |
| Superoxide anion radical (O2¯˙) | Hydrogen peroxide (H2O2) |
| Hydroxyl radical (OH˙) | Singlet molecular oxygen (O21 ∆g) |
| Peroxyl radical (ROO˙) | |
| Reactive Nitrogen Species | |
| Nitric oxide (NO˙) | Nitrite (NO2¯) |
| Nitrogen dioxide (NO2˙) | Peroxynitrite (ONOO¯) |
FRs are highly unstable molecules due to the presence of one or more unpaired electrons, and as we have seen they can come from oxygen and nitrogen, among other elements [44]. They have a short lifespan, ranging from milliseconds to nanoseconds, and in order to stabilize they seek coupling with electrons from contiguous biological molecules, with donating or accepting electrons being the genesis of OS [45].
When the production of ROS is excessively high and the organism is not able to neutralize them, harmful effects begin to appear in vital cellular structures such as proteins, lipids, and nucleic acids [46], producing OS. OS is responsible for the appearance and progression of different types of diseases, such as atherosclerosis, cardiovascular diseases, diabetes, cancer, and metabolic disorders [47].
ROS production originates from enzymatic and non-enzymatic reactions. Once O2¯˙ is synthesized, it is involved in certain reactions that produce radical and non-radical RS, such as the following: H2O2, OH˙, ONOO¯, etc. OH˙ is the most reactive among all FR species in vivo. FRs are synthesized from endogenous and exogenous sources and their sources are summarized in Table 3 [48].
Table 3.
Endogenous and exogenous sources that generate FRs [48].
| Endogenous Sources | Exogenous Sources |
|---|---|
| Inflammation | Exposure to contaminants |
| Ischemia | Exposure to heavy metals (Hg, Cd, Pb, Fe, and As) |
| Infection | Chemical solvents |
| Cancer | Food cooking (smoked meat and used oil) |
| Activation of immune cells | Medications (cyclosporine, tacrolimus, bleomycin, and gentamicin) |
| Excessive exercise | Cigarette smoke |
| Mental stress | Alcohol |
| Aging | Radiation |
Hg: mercury; Cd: cadmium; Pb: lead; Fe: iron; As: arsenic.
As mentioned above, an uncontrolled excess of RL will produce OS. For example, an excess of OH˙ and ONOO¯ could cause lipid peroxidation, damaging cell membranes and lipoproteins and creating malondialdehyde (MDA) and conjugated diene compounds, which are cytotoxic and mutagenic [48]. As a radical chain reaction, lipid peroxidation propagates extremely rapidly, affecting a large number of lipid molecules [49]. OS can also cause DNA damage through the formation of 8-oxo-2′-deoxyguanosine (8-OHdG), responsible for mutagenesis [50] as well as loss of epigenetic information [51]. Oxidative DNA damage is also a stimulus in the development of cancer [52]. OS is also considered a primary or secondary cause of a large number of CVDs [53], as circulating LDL oxidized by ROS contributes to foam cell formation and lipid accumulation, resulting in the formation of atheromatous plaques. OS has also been associated with various neurological diseases, such as Alzheimer’s disease (AD), Parkinson’s disease, amyotrophic lateral sclerosis, multiple sclerosis, depression, and memory loss [54]. OS is implicated in renal diseases, such as renal failure, proteinuria, and uremia [55,56], as well as respiratory diseases, such as asthma and chronic obstructive disease [57], and delayed sexual maturation and onset of puberty [58]. Thus, the excess of FRs and consequently OS affect different tissues, being responsible for the onset and progression of different pathological conditions that affect human health.
Several biomarkers have been employed and exhaustively examined to evaluate OS in reference to different diseases [35,59], among the most important of which are carbonyl groups and xanthine oxidase (XO) in proteins, advanced glycation end products (AGEs) in carbohydrates, 8-OHdG in DNA and MDA, and oxidized low-density protein (OxLDL) and F2-isoprotans in lipids.
Antioxidants are used to combat oxidation. Antioxidants are stable molecules that have the capacity to donate an electron to an FR in order to neutralize it, reducing its potential damage [60]. Antioxidant systems can be produced endogenously in the organism or introduced exogenously [61]. Regarding the endogenous form, the organism possesses mechanisms of action to neutralize RS through enzymatic and non-enzymatic mechanisms [44]. Among the enzymatic mechanisms, referred to as high-molecular-weight mechanisms, are as follows: superoxide dismutase (SOD), the main antioxidant enzyme of the organism, catalyzes the superoxide anion into oxygen (O2) and H2O2 and in turn interacts with different enzymes that help neutralize SRs; catalase (CAT), which catalyzes H2O2 in water and O2 in the presence of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase; glutathione peroxidase (GPx), which reduces H2O2 and organic peroxides in water or alcohol whenever selenium is present; and peroxiredoxin (Prx), which shows the lowest efficiency in H2O2 metabolization [44,60,62]. As for low-molecular-weight or non-enzymatic mechanisms, they include vitamin E, vitamin C, bilirubin, biliverdin, uric acid, ascorbic acid, glutathione, and flavonoids [44,63].
3. Antioxidant Activity of Zingiberaceae Family
3.1. Antioxidant Activity of Ginger
Ginger has been extensively studied for its antioxidant properties. The underlying mechanism of action lies in the fact that ginger possesses bioactive compounds with two or more hydroxyl groups attached to an aromatic ring that confer on them the antioxidant capacity to neutralize unpaired electrons of FRs and donate hydrogens or chelate metal ions, thus reducing OS [18]. If not neutralized, these FRs, such as ROS or RNS, interact with cells, causing oxidative damage, which can contribute to cellular aging and the development of chronic diseases, such as cancer [64], inflammatory diseases [65], neurodegenerative diseases [66], and cardiovascular diseases [67]. This antioxidant property of ginger is due to the presence of antioxidant compounds, such as gingerols (6-gingerol, 8-gingerol, and 10-gingerol), shogaols (6-shogaol, 8-shogaol, and 10-shogaol), flavonoids, and phenolic acids [68].
As previously mentioned, oxidative damage can affect proteins and cell membrane lipids [69]. Proteins can be oxidized by the formation of FR groups in their component amino acids, which can alter their structure and function; this can also damage the structure of the cell membrane and increase its permeability. It has been observed that ginger may have a protective effect against this oxidation in several studies. This has been investigated in the study conducted by Romero et al., where it was observed that a ginger extract decreased AKT-phosphorylation, thus protecting cells from hydrogen peroxide-induced oxidative damage in human hepatocyte cell cultures [70]. In another study carried out by Carnuta et al., it was shown that a Zingiber officinale extract reduced lipid accumulation in hamsters’ livers, caused by a decrease in endoplasmic reticulum stress (ERS) markers [71].
Cells employ antioxidant mechanisms, such as MDA, or enzymes, such as SOD, CAT, and GPx, to compensate for oxidative damage. These antioxidants can neutralize FRs and reduce OS in cells. For example, a meta-analysis of clinical trials has shown that ginger supplementation decreases MDA values and increases total antioxidant capacity [72]. This is consistent with the findings of the study conducted by Sheikhhossein et al., in which there was also a significant reduction in MDA; in addition, an increase in GPx was observed [73].
In addition to ROS, reactive nitrogen species, including nitric oxide (NO), are known to contribute to the development of diseases by influencing signal transduction and causing DNA damage. The production of NO is regulated by inducible nitric oxide synthase (iNOS), which is upregulated in response to various stressors [74]. Oxidative damage to DNA can lead to mutations and activation of cell signaling pathways that may contribute to the development of chronic diseases, such as cancer, because FRs can cause strand breaks and oxidation of DNA’s nitrogenous bases, which can lead to errors in replication and the formation of mutations. Studies have demonstrated that 6-gingerol can effectively inhibit XO, which is responsible for catalyzing the oxidation of hypoxanthine to xanthine and then xanthine to uric acid. This process occurs during the final stage of purine metabolic degradation and results in the production of ROS [21].
In addition, other studies have shown that 6-gingerol inhibits NO production and reduces iNOS expression in lipopolysaccharide (LPS)-stimulated mouse macrophages [75]. 6-gingerol was found to effectively suppress oxidative damage mediated by peroxynitrite. Other ginger derivatives, such as 6-shogaol, 1-dehydro-10-gingerdione, and 10-gingerdione, were also found to decrease LPS-induced NO production, with 6-shogaol and 1-dehydro-10-gingerdione effectively reducing iNOS expression [76].
During an inflammatory response, leukocytes and macrophages release ROS to destroy invading microorganisms. However, ROS can also damage surrounding cells and tissues, which can lead to a chronic inflammatory response and contribute to the development of chronic inflammatory diseases, such as arthritis, inflammatory bowel disease, or systemic lupus erythematosus, among others [77].
Chronic inflammation causes the elevation of pro-inflammatory markers, such as nuclear factor-kappaB (NF-κB), the mechanistic target of rapamycin (mTOR) pathways, interleukin (IL)-6, total antioxidant capacity (TAC), c-reactive protein (CRP), and tumor necrosis factor alpha (TNF-α). Several studies have shown that ginger can reduce the concentrations of these markers, and this has been supported by several studies, such as the systematic review and meta-analysis carried out by Jalali et al. [72]. In another study, it was demonstrated that 6-gingerol enhances the expression of Beclin1, which promotes autophagy in human endothelial cells. It also hinders signaling in the PI3K/AKT/mTOR pathway without affecting the cell cycle [78]. In addition, it has been shown that ginger extract can inhibit NF-κB activation and decrease the level of IL-1β [79]. The anti-inflammatory effects of 6-shogaol were achieved through the inhibition of the production of PGE2 and pro-inflammatory cytokines (IL-1β, IL-6, TNF-α, and cyclooxygenase-2 (COX-2)). This was accomplished by downregulating the expression of p38MAPK and NF-κB [80].
The anticancer properties of phenolic compounds present in ginger have also been demonstrated. Some studies have shown that 6-gingerol and 6-shogaol produce cell cycle arrest, inducing growth suppression and a decrease in tumor volume and tumor burden through the increase in CKDIs p21 (Cyclin-Dependent Kinase Inhibitors), which are involved in the control of the transition of cells from the G1 to the S phase of the cell cycle [81,82,83]. In addition, the benefits of ginger as an antiemetic have been described in several controlled studies. A systematic review and meta-analysis realized by Kim at al. showed that ginger or its bioactive compounds diminish acute and delayed phases of chemotherapy-induced nausea and vomiting nausea in breast cancer patients [84], producing inhibition of 5-hydroxytryptamine type3 (5-HT3) receptors in the central and peripheral nervous systems. The efficacy of ginger on postoperative nausea and vomiting [85] and on nausea and vomiting of pregnancy [86] has also been demonstrated.
Inflammation and ROS are closely related to the pathogenesis of cardiovascular disease (CVD). Chronic inflammation can trigger the production of ROS, activate several inflammatory signaling pathways, and promote the expression of pro-inflammatory molecules. This is why the use of ginger has been extensively studied in this type of disease [87]. Studies have shown that several bioactive compounds found in ginger exhibit hypolipidemic, anti-inflammatory, and antioxidant effects in vivo. For example, El-Seweidy et al. conducted a study that revealed that 10-dehydrogingerdione possesses a proprotein convertase subtilisin/kexin type 9 (PCSK9) lowering effect, which may be responsible for its cardiovascular protective effect against dyslipidemia through a mechanism that modulates lipid levels [88].
Neurodegenerative diseases are also related to increased ROS production in the brain. This increase can cause damage to cells and tissues, which has been linked to brain cell death and neuronal dysfunction in neurodegenerative diseases [66].
Ginger has been studied in these types of diseases. It has been observed that 6-shogaol inhibited some components of the inflammatory pathway, such as TNF-α, NO, COX-2, and iNOS, in patients with Parkinson’s disease [89]. In addition, it has been suggested that this compound may inhibit glial cell activation and reduce memory impairment in animal models of dementia [90], as well as exert a protective effect against amyloid-β in AD [91].
The antimicrobial properties of ginger have been well documented in recent years, with various studies highlighting its effectiveness against a range of pathogens [92]. Bioactive compounds present in ginger are believed to target the cell membrane and cell wall of microorganisms, leading to the disruption of their structural integrity and eventual cell death [93]. Ginger has demonstrated broad-spectrum antimicrobial activity against Gram-positive and Gram-negative bacteria, as well as fungi and viruses [92]. This can be attributed to its ability to inhibit bacterial protein synthesis, DNA replication, and cell division [94]. Furthermore, ginger has been found to be synergistic with conventional antibiotics in combating resistant strains of bacteria [95].
In addition to its direct antimicrobial effects, ginger also possesses anti-inflammatory and immunomodulatory properties, which can boost the host’s immune response against infections [94]. This makes ginger a promising candidate for the development of new antimicrobial agents, particularly in the face of increasing antibiotic resistance [92].
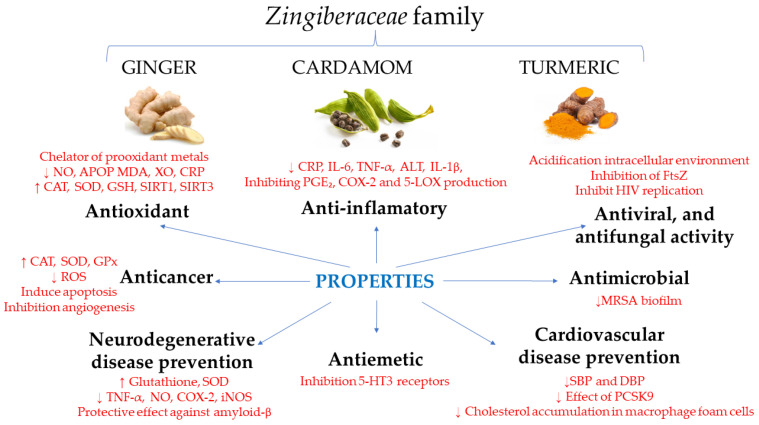
Table 4 and Figure 1 summarize the properties and mechanisms of action of ginger.
Table 4.
Summary of product characteristics of ginger.
| Extract | Function | Mechanism | References |
|---|---|---|---|
| Ginger | Antioxidant | Decreased AKT-phosphorylation | [70] |
| Decreased ERS markers | [71] | ||
| Decreased MDA and increased GPx levels | [72,73] | ||
| Inhibition of XO | [21] | ||
| Inhibition of NO production and reduction in iNOS | [75,76] | ||
| Anti-inflammatory | Increased Beclin1 expression and obstruction of signaling in the PI3K/AKT/mTOR pathway | [78] | |
| Inhibition of NF-κB activation and decrease in the level of IL-1β | [79] | ||
| Inhibition of the production of PGE2 and pro-inflammatory cytokines (IL-1β, IL-6, TNF-α, and COX-2) | [80] | ||
| Anticancer | Decrease in tumor volume and tumor burden by increasing p21 CKDIs | [81,82,83] | |
| Antiemetic | Inhibition of 5-HT3 receptors in the central and peripheral nervous systems | [84,85,86] | |
| Antimicrobial | Inhibition of bacterial protein synthesis, DNA replication and cell division. | [94] | |
| Cardiovascular disease prevention | Reducing effect of PCSK9 through a modulatory mechanism of lipid levels | [88] | |
| Neurodegenerative disease prevention | Inhibition of TNF-α, NO, COX-2, and iNOS | [89] | |
| Inhibition of glial cell activation | [90] | ||
| Protective effect against amyloid-β | [91] |
AKT: protein kinase B; ERS: endoplasmic reticulum stress; MDA: malondialdehyde; GPx: glutathione peroxidase; XO: xanthine oxidase; NO: nitric oxide; iNOS: inducible nitric oxide synthase; PI3K/AKT/mTOR: phosphoinositide 3 kinase (PI3K)/AKT/mammalian target of rapamycin (mTOR); NF-κB: nuclear factor κB; 5-HT3: 5-hydroxytryptamine type3; PGE2: prostaglandin E2; IL-1β: interleukin-1 beta; IL-6: interleukin-6; PCSK9: proprotein convertase subtilisin/kexin type 9; TNF-α: tumor necrosis factor alpha; COX-2: cyclooxygenase-2; CKDIS: cyclin-dependent kinase inhibitors.
3.2. Antioxidant Activity of Turmeric
Antioxidants inhibit the formation of FRs and their propagation; they prevent the formation of peroxides and interfere in the FR chain reaction [96]. Antioxidants counteract OS and promote healthy aging. The organism presents endogenous enzymatic antioxidant defenses: GPx, CAT, and SOD and non-enzymatic antioxidant defenses, such as vitamin C, vitamin E, β-carotene, zinc, selenium, and uric acid [97,98].
Curcumin is an effective antioxidant that reduces OS levels. It can act as a chelator of pro-oxidant metals and regulate the activity of numerous enzymes [99]. It can reduce ROS generation, scavenge FRs, and act as a strong inhibitor of advanced glycation end products and lipid peroxidation [100]. There are several mechanisms by which curcumin prevents OS. Curcumin acts as an activator of sirtuin (SIRT)1 and SIRT3, but as an inhibitor of SIRT2. SIRT1 and SIRT3 inhibit OS in cells, whereas SIRT 2 triggers it [100]. SIRT1 prevents the expression and production of iNOS and ROS. This action occurs through p65, leading to the suppression of the NF-ĸB signaling pathway [101]. SIRT 1 is primarily located in the nucleus and activates FOXO 3a protein transcription factors (Forkhead box O) that regulate antioxidant genes (CAT and SOD) by reducing FR levels [102]. Mitochondrial SIRT3 deacetylates and activates several enzymes that are critical in maintaining cellular ROS levels. One of these enzymes is SOD2, which is an important antioxidant enzyme located in the mitochondria. SIRT3 deacetylates two important lysine residues in SOD2, which enhances its catalytic activity. It has also been observed that the catalytic activity of SOD2 decreases when SIRT3 is suppressed [103].
Turmeric/curcumin supplementation might be used as a viable intervention for improving the inflammatory/oxidative status of individuals. In addition, turmeric/curcumin supplementation significantly improved antioxidant activity through reducing MDA levels and SOD activity and enhancing TAC [104]. Panahi et al. [105] observed that the supplementation with a curcuminoid–piperine combination significantly reduced MDA and CRP concentrations and improved serum SOD activities compared with placebo. Short-term supplementation with a curcuminoid–piperine combination significantly improves oxidative and inflammatory status in patients with metabolic syndrome.
Curcumin stimulates peroxisomal enzymes with high antioxidant activity, such as CAT and SOD. These enzymes reduce OS through the peroxisome proliferator-activated receptor alpha/gamma (PPAR) pathway [27]. The reduction of reactive nitrogen and oxygen species is essential for maintaining normal neuronal functions.
Neurodegenerative diseases are associated with increased OS and inflammatory processes. This increased OS is associated with mitochondrial dysfunction, calcium overload, and excitotoxicity.
AD is a neurodegenerative disorder of the elderly. As the prevalence of AD rises in the 21st century, there is an urgent need for the development of effective pharmacotherapies. Physical exercise and healthy diets have been reported to have implications to delay disease progression of AD in elderly individuals and improve cognitive functions in subjects with mild cognitive impairment and in early AD patients. Neuroinflammation and OS have been considered as hallmarks of AD, playing crucial roles in neurotoxicity. For this reason, an adequate antioxidant strategy may improve the treatment of neurodegenerative diseases and dementia [106]. Curcumin inhibits the formation and promotes the disaggregation of amyloid-β plaques, attenuates the hyperphosphorylation of tau and enhances its clearance, binds copper, lowers cholesterol, modifies microglial activity, inhibits acetylcholinesterase, mediates the insulin signaling pathway, and is an antioxidant. In conclusion, curcumin has the potential to be more efficacious than current treatments [107].
Curcumin prevents the aggregation of new existing amyloid deposits, promotes disaggregation of amyloid deposits, and reduces their size in patients with AD. It also binds to redox active metals (copper and iron) by preventing the metal induction of Nf-kB, reducing the inflammatory process associated with the disease. Curcumin prevents cognitive decline associated with aging and dementia [108].
Curcumin suppresses the differentiation of Th17 cells, cells that are an important factor in the development of multiple sclerosis. It also causes the degradation of the myelin sheath of neurons in these patients and decreases inflammation, reducing inflammatory cytokines, NF-kB, and JAK-STAT, AP-1, and AP-1 signaling pathways [5].
Any circumstance harmful to health, such as infections and tissue lesions, leads to an inflammatory process, related to numerous pathological and physiological comorbidities, and produced by a series of responses triggered by the immune system. Inflammation is related to an increase in lipid peroxides, products resulting from lipid peroxidation, and an increase in FRs and inflammatory markers, such as cytokines [109]. Curcumin decreases OS and inflammation by acting through the Nrf2-keap1 pathway; it blocks TNF-α-mediated cell signaling and TFN production by suppressing pro-inflammatory pathways associated with chronic diseases [110]. Curcumin regulates NF-κB, MAPK, AP-1, JAK/STAT, and other signaling pathways, and inhibits the production of inflammatory mediators.
OS is closely related to inflammatory processes by activating transcription factors associated with inflammation. Curcumin increases antioxidant activity due to its effect on NADPH oxidase and increasing the activity of antioxidant enzymes (SOD, CAT, and GPx), and is related to the Nrf2-Keap1 pathway [111,112], which could potentially promote cell survival.
Curcumin, as an antioxidant, reduces lipid peroxidation, a risk factor for cardiovascular disease and atherosclerosis. Curcumin also improves the lipid profile by influencing the same mediators as statins. Additionally, curcumin has the ability to prevent endothelial dysfunction and smooth muscle cell proliferation and migration, which may be beneficial in the treatment of atherosclerosis [17]. Moreover, curcumin may exert antidiabetic effects by increasing the gene expression of PPAR-γ, which has a pleiotropic impact on glucose homeostasis and insulin sensitivity and controls gene expression in glucose metabolism and lipids [113].
Curcumin has also been shown to protect against atherosclerosis in mice lacking apolipoprotein E by inhibiting Toll-like receptor 4 expression [114], in addition to its ability to suppress cholesterol accumulation in macrophage foam cells and atherosclerosis [115].
Curcumin has been shown to have anti-proliferative and anti-metastatic properties [116]. These properties may contribute to preventing the onset and development of cancer. Some of the mechanisms by which curcumin may act to prevent cancer include the following: (a) reduction in OS, as it may reduce the production of ROS that damage DNA and other cellular structures, which may prevent the occurrence of genetic mutations that contribute to the development of cancer; (b) anti-inflammatory action by inhibiting the production of inflammatory molecules, such as TNF-α and IL-6, as chronic inflammation has been linked to the development of some types of cancer, and curcumin’s ability to reduce inflammation may help prevent cancer; (c) induction of apoptosis by cell death programming, known as apoptosis, in cancer cells, which may help prevent cancer cell proliferation, as the induction of apoptosis is linked to the action of curcumin on the proteasome; (d) inhibiting angiogenesis by blocking the formation of new blood vessels that nourish tumors, which may prevent tumor formation and growth acting on transcription factors AP-1 and NF-kB; inhibiting COX-2 and 5-lipooxygenase (5-LOX); limiting the expression of IL-8 in pancreatic cancer and head and neck cancer cell lines; and inhibiting angiogenesis mediated by NO and iNOS. Curcumin can also regulate various cell signaling pathways that are involved in cell proliferation, differentiation, and cell survival, which may help prevent cancer [117].
In summary, curcumin may act in several ways to prevent cancer, including reducing OS, inhibiting inflammation, inducing apoptosis, inhibiting angiogenesis, and regulating cell signaling pathways. However, further studies are needed to fully understand the mechanisms of action of curcumin and its efficacy in cancer prevention and treatment [116,117].
Curcumin has antimicrobial activity against a wide range of microorganisms, including bacteria, such as Escherichia coli, Staphylococcus aureus, Pseudomonas aeruginosa, Streptococcus pyogenes, and Helicobacter pylori. In addition, curcumin can inhibit the formation of bacterial biofilms, which can increase the efficacy of antimicrobial treatments. A possible antibacterial mechanism of action produced by curcumin is the inhibition of cell division protein FtsZ assembly on the Z-ring and the suppression of bacterial cells [118]; in addition, regarding viruses, it has been found to interfere with virus entry into host cells and reduce viral replication. Among the most important effects produced against viruses is the effect of curcumin against human immunodeficiency virus (HIV). Due to effects on the function of some viral proteins, counting viral integrase, protease, and transactivate of transcription protein (Tat), curcumin can inhibit HIV replication and has also demonstrated antifungal activity.
Curcumin treatment of Candida species results in cell death. A possible mechanism to explain cell death could be the acidification of the intracellular environment by inhibiting thymidine 1 and proton extrusion causing the inhibition of hyphal development [119].
Table 5 and Figure 1 summarize the properties and mechanisms of action of turmeric.
Table 5.
Summary of product characteristics of turmeric.
| Extract | Function | Mechanism | References |
|---|---|---|---|
| Turmeric | Antioxidant | Chelates of pro-oxidant metals | [99] |
| Strongly inhibits advanced glycation end products and lipid peroxidation | [100] | ||
| Reduces lipid peroxidation | |||
| Acts as an activator of SIRT1 and SIRT3 | [100,101,102,103] | ||
| Reduces MDA levels and CRP | [104] | ||
| Improves serum SOD and CAT activities | [100,105] | ||
| Enhances TAC | [105] | ||
| Anti-inflammatory | Inhibits the production of inflammatory mediators | [111,112] | |
| Inhibits the production of inflammatory molecules, such as TNF-α and IL-6 | |||
| Inhibits COX-2 and 5-LOX | |||
| Anticancer | Reduces the production of ROS that damage DNA and other cellular structures | [116,117] | |
| Has anti-inflammatory action | |||
| Induces apoptosis | |||
| Inhibits angiogenesis | |||
| Antimicrobial, antiviral and antifungal activity | Increases the efficacy of antimicrobial treatments | [118,119] | |
| Inhibitions FtsZ assembly on the Z-ring and the suppression of bacterial cells | |||
| Inhibits HIV replication | |||
| Acidifies the intracellular environment | |||
| Cardiovascular disease prevention | Has ability to prevent endothelial dysfunction and smooth muscle cell proliferation and migration | [114,115] | |
| Inhibits Toll-like receptor 4 expression | |||
| Has ability to suppress cholesterol accumulation in macrophage foam cells and atherosclerosis | |||
| Neurodegenerative disease prevention | Inhibits the formation and promotes the disaggregation of amyloid-β plaques | [106,107,108] | |
| Attenuates the hyperphosphorylation of tau and enhances its clearance | |||
| Modifies microglial activity | |||
| Inhibits acetylcholinesterase | |||
| Binds to redox active metals (copper and iron) | |||
| Suppresses the differentiation of Th17 cells | [5] | ||
| Exhibits antioxidant activity | [111,112] |
SIRT: sirtuin; CRP: C-reactive protein; MDA: malondialdehyde; SOD: superoxide dismutase; CAT: catalase; TAC: total antioxidant capacity; TNF-α: tumor necrosis factor alpha; IL-6: interleukin-6; COX-2: cyclooxygenase-2; 5-LOX: 5-lipo-oxygenase; HIV: human immunodeficiency virus.
3.3. Antioxidant Activity of Cardamom
The natural process of oxidation in living organisms is mediated by the reaction of molecular oxygen with other molecules and leads to the enhancement of FRs and ROS. These ROS and FRs, along with further oxidation products, are associated with an arousal of some degenerative diseases, such as atherosclerosis or cancer, to name a few.
Reports indicate that cardamom (Elettaria cardamomum) contains biologically active antioxidant metabolites which render the capacity of scavenging those previously mentioned FRs and provide a defense against oxidation and its damages. The literature describes that it is in seeds and pods where the highest amount of antioxidant molecules is stored. Among the antioxidant components, we can find some phenolic components, such as gallic acid equivalents, with the capacity of avoiding the peroxidation of the linoleic acid system, proving its greater antioxidant activity [120]. Cardamom is a good source of volatile oils, fixed oils, phenolic acids, and sterols [121]. Cardamom’s antioxidant effect is manifested as a reduction in MDA, advanced protein oxidation products (APOP), and nitric oxide (NO) detected in the liver and in plasma [8]. Furthermore, CAT, SOD, and GSH are cellular antioxidants which reduce OS. The activity of CAT was significantly depleted in the cardamom group, as in SOD and GSH.
The most dominant bioactive substances in cardamom are 1,8-cineol (20–60%) and α-terpinyl acetate (20–55%) [34]. Given those components, publications described this extract as an antioxidant and a synergistic agent to favor the skin permeation of certain drugs [122,123], but also as a bacterial inhibitor [124].
OS plays a pivotal role in diabetes complications, both microvascular and cardiovascular. The evolution of diabetes causes mitochondrial superoxide overproduction in vessel endothelial cells, and in the myocardium. Increased levels of intracellular ROS cause defective angiogenesis in response to ischemia, activate a number of pro-inflammatory pathways, and cause long-lasting epigenetic changes which drive persistent expression of pro-inflammatory genes after glycemia is normalized (‘hyperglycemic memory’) [125]. A study in 80 pre-diabetic subjects, who randomly took the cardamom supplement (n = 40) or placebo (n = 40) during 8 weeks, described that cardamom improved parameters of inflammation and OS (decreasing serum CRP (p = 0.02), hs-CRP:IL-6 ratio (p = 0.008), and MDA (p = 0.009)) compared with the placebo group [126].
Several publications have proven role of OS in obesity and its comorbid factors [127]: triggering the accumulation of white adipose tissue (WAT) and altering food intake, and causing an increase in preadipocyte proliferation, its differentiation, and size [128]. Obesity per se can also induce systemic OS through multiple biochemical mechanisms, such as superoxide generation from NADPH oxidases (NOX), oxidative phosphorylation, glyceraldehyde auto-oxidation, protein kinase C (PKC) activation, and polyol and hexosamine pathways [129]. A randomized study of eighty-seven obese patients [130] with nonalcoholic fatty liver disease (NAFLD) were allocated in two matching arms of a trial, taking 3 g of cardamom or placebo with meals through six capsules 3-times/day, and cardamom (n = 43) and placebo (n = 44) for 3 months. Green cardamom significantly increased (p < 0.05) antioxidant markers (Sirt1) and decreased inflammatory markers (e.g., TNF-α, IL-6, alanine aminotransferase (ALT), and fatty liver status) [131]. Further results of this group determined that when compared with placebo, GC significantly increased endocrine activation factors of brown fat tissue and the sensitivity index to insulin and decreased glycemic and blood lipidic levels (p < 0.05) [132]. Similarly, a parallel, double-blind randomized [9], placebo-controlled study carried out in 83 participants with overweight, obesity, and/or type 2 diabetes, proved that 10 weeks of taking 3 g of green cardamom daily favored an increase in antioxidants, such as SIRT1. Unfortunately, no significant changes in other serum lipidic indices (TC, HDL-c, and LDL-c) were found [133]. Furthermore, other studies have also described the capacity of cardamom to reduce inflammation seen by TNF-α, IL-6, and CRP serum levels, and thus also the expression levels of TNF-α and CRP genes (p < 0.001) [134].
There is a key background mechanism in hypertension manifested as an increment in OS and alterations in the total antioxidant capacity, commonly described in other cardiovascular diseases [67,135]. In one study, twenty participants [136] recently diagnosed with stage 1 primary hypertension received 3 g of cardamom in two doses during 12 weeks to link the administration of cardamom with decreased systolic, diastolic, and mean blood pressure, together with an increase in fibrinolytic activity and total antioxidant status (p < 0.05).
ROS can damage lipids, nucleic acids, and proteins, thereby altering their functions, leading to many pathologies. There is some evidence in different types of cancer about low antioxidative enzyme levels or higher rates of products of lipid peroxidation, such as MDA, as biomarkers to assess the level of OS. Some of the studies proposed their potential in defining the stage of tumor progression. Preliminary results in animal models have described that cardamom compared against benzo(α)pyrene reduced tumor incidence and multiplicity significantly (p < 0.001). Moreover, biochemical assays described an enhancement in the hepatic activities of oxidation preventing hormones (such as glutathione-S-transferases, SOD, GPx, and CAT) in mice models treated with cardamom (p < 0.01). Furthermore, the non-enzymatic antioxidant glutathione was increased in the cardamom-treated group significantly (p < 0.001), whereas the lipid peroxidation level along with lactate dehydrogenase activity exhibited a significant reduction with cardamom treatment compared to the control (p < 0.01). These results suggest that cardamom has the potential to become a pivotal chemo preventive agent against forestomach cancer [137].
In a couple of studies in 142 healthy volunteers (age of 55 years or above) selected for a relatively low baseline NK cell activity and a history of recurrent coughs, regular consumption of tea with ginger and cardamom enhanced NK cell activity [138].
When the effect of aromatherapy on postoperative nausea after ambulatory surgery was examined in 301 participants, the groups who inhaled a blend of different compounds including cardamom and ginger essential oils showed significant results in the reduction in nausea levels [139].
A recent study with single-blind, randomized, placebo-controlled design used cardamom inhalation for postoperative nausea and vomiting after spinal anesthesia [140]. The intervention had 70 participants who were distributed in placebo and cardamom groups, and regarding nausea, after controlling the initial severity, the declining extent was more noticeable in the intervention group than in the placebo group.
Recent studies have described the capacity of cardamom to suppress bacterial activity, especially its essential oil against methicillin-resistant Staphylococcus aureus (MRSA) [122,141]. However, currently the mechanism of action that cardamom exerts on MRSA biofilm is unclear. Notwithstanding, some studies have deeply assessed cardamom anti-MRSA biofilm activity by destroying the barrier of the biofilm and causing bacterial loss of metabolic activity. Secondly, some studies have avoided MRSA’s adhesion ability and therefore inhibited the formation of extracellular polymers. Finally, there is a suggestion that points out the ability of cardamom to downregulate MRSA biofilm-forming genes [124].
Cardamom is involved in treating AD with the following mechanisms: anti-cholinesterase activity, induction of endogenous antioxidants, such as glutathione and superoxide dismutase, impeding the production of reactive hydroxyl radicals, preventing the formation of Aβ42 deposits, and protecting cells from iron-induced death [142]. Gomaa et al. [143] observed that the effect of 25 mg/kg cardamom supplementation on AD-induced alterations in an animal model could be positive via ameliorating the alterations produced by decreasing OS and neuroinflammation and through the activation of blunted insulin signal transduction in the brain.
Table 6 and Figure 1 summarize the properties and mechanisms of action of cardamom.
Table 6.
Summary of product characteristics of cardamom.
| Extract | Function | Mechanism of Action | References |
|---|---|---|---|
| Cardamom | Antioxidant | Decreased NO, APOP, and MDA | [8,122,123,126] |
| Increased activity of CAT, SOD, and GSH | [8,122,123] | ||
| Increased Sirt1 | [122,132] | ||
| Anti- inflammatory |
Decreased serum CRP | [126] | |
| Decreased hs-CRP:IL-6 ratio | |||
| Inhibited the production of inflammatory markers (IL-6, TNF-α, ALT, and fatty liver status) | [131] | ||
| Anticancer * | Enhanced the hepatic activities of oxidation-preventing hormones (such as glutathione-S-transferases, SOD, GPx, and CAT) | [137] | |
| Antiemetic | Volatile compounds from essential oil were significantly efficient to reduce nausea level | [139,140] | |
| Antimicrobial | Enhanced NK cell activity and anti-MRSA biofilm activity and avoided MRSA adhesion ability; cardamom may downregulate MRSA biofilm-forming genes |
[122,123,124,141] | |
| Cardiovascular disease prevention | Decreased systolic, diastolic, and mean blood pressure, and increased fibrinolytic activity | [136] | |
| Neurodegenerative disease prevention | Exhibited anti-cholinesterase activity, induced endogenous antioxidants, such as glutathione and superoxide dismutase, impeded the production of reactive hydroxyl radicals, prevented the formation of Aβ42 deposits, and protected cells from iron-induced death | [142] |
*: Mice model, ALT: alanine aminotransferase; Apop: advanced protein oxidation products; CAT: catalase; CRP: C-reactive protein; GSH: glutathione reduced; GPx: glutathione peroxidase; IL-6: interleukin-6; MDA: malondialdehyde; MRSA: methicillin-resistant Staphilococus Aureus; NO: nitric oxide; NF-κB: nuclear factor κB; SOD: superoxide dismutase; TNF-α: tumor necrosis factor alpha.
Figure 1.
Summary of the functions and mechanisms of action of the 3 products of the Zingiberaceae family. Bold color refers to the functions and red color refers to the mechanisms of action.↑: increases; ↓: decreases; NO: nitric oxide; APOP: advanced protein oxidation products; MDA: malondialdehyde; XO: xanthine oxidase; CRP: C-reactive protein; CAT: catalase; SOD: superoxide dismutase; GPx: glutathione peroxidase; ROS: reactive oxygen species; TNF-α: tumor necrosis factor alpha; COX-2: cyclooxygenase-2; iNOS: inducible nitric oxide synthase; 5-HT3: 5-hydroxytryptamine type3; IL-6: interleukin-6; ALT: alanine aminotransferase; IL-1β: interleuikin-1beta; PGE2: prostaglandin E2; 5-LOX: 5-lypooxygenase; FtsZ: cell division protein FtsZ; MRSA: methicillin-resistant Staphylococcus aureus; SBP: systolic blood pressure; DBP: diastolic blood pressure; PCSK9: proprotein convertase subtilisin/kexin type 9.
4. Conclusions and Future Research Lines
Cardamom, turmeric, and ginger are among the most active natural remedies due to their numerous biological properties. They have bioactive compounds with important antioxidant activities. Ginger’s antioxidant capacity is proved by its capacity to decrease AKT-phosphorylation, ERS markers, and MDA and GPx levels, to inhibit XO and NO levels, and to produce PGE2 and pro-inflammatory cytokines (IL-1β, IL-6, TNF-α, and COX-2), as well as via the presence of 5-HT3 receptors in the central and peripheral nervous system. Turmeric improves serum SOD and CAT activity; inhibits the production of inflammatory molecules, such as TNF-α, IL-6, COX-2, and 5-LOX; prevents endothelial dysfunction; and suppresses cholesterol accumulation in macrophage foam cells and atherosclerosis. Cardamom decreases NO, APOP, MDA, CAT, SOD, and GSH activity; induces endogenous antioxidants, such as glutathione and superoxide dismutase; enhances NK cell activity; and inhibits the production of inflammatory markers. Due to all of these properties, cardamom, turmeric, and ginger could be a coadjuvant treatment in different pathologies where oxidative stress plays an important role.
However, the bioavailability of these compounds needs to be optimized, and further research is needed to determine the optimal concentration ranges for these compounds to have effects as antioxidants in the body.
Author Contributions
Conceptualization, P.Z., P.B., B.C. and R.A.; writing—original draft preparation, P.Z., P.B., B.C., A.M.G.-M., J.M. and R.A.; writing—review and editing, P.Z., P.B., B.C., A.M.G.-M., J.M. and R.A.; visualization, P.Z., P.B., B.C., A.M.G.-M., J.M. and R.A.; supervision, P.Z., P.B., B.C., A.M.G.-M., J.M. and R.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Lakhan S.E., Ford C.T., Tepper D. Zingiberaceae extracts for pain: A systematic review and meta-analysis. Nutr. J. 2015;14:50. doi: 10.1186/s12937-015-0038-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peng W., Li P., Ling R., Wang Z., Feng X., Liu J., Yang Q., Yan J. Diversity of Volatile Compounds in Ten Varieties of Zingiberaceae. Molecules. 2022;27:565. doi: 10.3390/molecules27020565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rachkeeree A., Kantadoung K., Suksathan R., Puangpradab R., Page P.A., Sommano S.R. Nutritional Compositions and Phytochemical Properties of the Edible Flowers from Selected Zingiberaceae Found in Thailand. Front. Nutr. 2018;5:3. doi: 10.3389/fnut.2018.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kunnumakkara A.B., Bordoloi D., Padmavathi G., Monisha J., Roy N.K., Prasad S., Aggarwal B.B. Curcumin, the golden nutraceutical: Multitargeting for multiple chronic diseases. Br. J. Pharmacol. 2017;174:1325–1348. doi: 10.1111/bph.13621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kocaadam B., Şanlier N. Curcumin, an active component of turmeric (Curcuma longa), and its effects on health. Crit. Rev. Food Sci. Nutr. 2017;57:2889–2895. doi: 10.1080/10408398.2015.1077195. [DOI] [PubMed] [Google Scholar]
- 6.Abdullah, Ahmad N., Tian W., Zengliu S., Zou Y., Farooq S., Huang Q., Xiao J. Recent advances in the extraction, chemical composition, therapeutic potential, and delivery of cardamom phytochemicals. Front. Nutr. 2022;9:1024820. doi: 10.3389/fnut.2022.1024820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kandikattu H.K., Rachitha P., Jayashree G.V., Krupashree K., Sukhith M., Majid A., Amruta N., Khanum F. Anti-inflammatory and anti-oxidant effects of Cardamom (Elettaria repens (Sonn.) Baill) and its phytochemical analysis by 4D GCXGC TOF-MS. Biomed. Pharmacother. 2017;91:191–201. doi: 10.1016/j.biopha.2017.04.049. [DOI] [PubMed] [Google Scholar]
- 8.Rahman M.M., Alam M.N., Ulla A., Sumi F.A., Subhan N., Khan T., Sikder B., Hossain H., Reza H.M., Alam M.A. Cardamom powder supplementation prevents obesity, improves glucose intolerance, inflammation and oxidative stress in liver of high carbohydrate high fat diet induced obese rats. Lipids Health Dis. 2017;16:151. doi: 10.1186/s12944-017-0539-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aghasi M., Koohdani F., Qorbani M., Nasli-Esfahani E., Ghazi-Zahedi S., Khoshamal H., Keshavarz A., Sotoudeh G. Beneficial effects of green cardamom on serum SIRT1, glycemic indices and triglyceride levels in patients with type 2 diabetes mellitus: A randomized double-blind placebo controlled clinical trial. J. Sci. Food Agric. 2019;99:3933–3940. doi: 10.1002/jsfa.9617. [DOI] [PubMed] [Google Scholar]
- 10.Nair A., Amalraj A., Jacob J., Kunnumakkara A.B., Gopi S. Non-Curcuminoids from Turmeric and Their Potential in Cancer Therapy and Anticancer Drug Delivery Formulations. Biomolecules. 2019;9:13. doi: 10.3390/biom9010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aggarwal B.B., Yuan W., Li S., Gupta S.C. Curcumin-free turmeric exhibits anti-inflammatory and anticancer activities: Identification of novel components of turmeric. Mol. Nutr. Food Res. 2013;57:1529–1542. doi: 10.1002/mnfr.201200838. [DOI] [PubMed] [Google Scholar]
- 12.Abrahams S., Haylett W.L., Johnson G., Carr J.A., Bardien S. Antioxidant effects of curcumin in models of neurodegeneration, aging, oxidative and nitrosative stress: A review. Neuroscience. 2019;406:1–21. doi: 10.1016/j.neuroscience.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 13.Garza G.R.C., Luévano J.H.E., Rodríguez A.F.B., Montes A.C., Hernández R.A.P., Delgado A.J.M., Villarreal S.M.L., Rodríguez J.R., Casas R.M.S., Velázquez U.C., et al. Benefits of Cardamom (Elettaria cardamomum (L.) Maton) and Turmeric (Curcuma longa L.) Extracts for Their Applications as Natural Anti-Inflammatory Adjuvants. Plants. 2021;10:1908. doi: 10.3390/plants10091908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang H.A., Kitts D.D. Turmeric and its bioactive constituents trigger cell signaling mechanisms that protect against diabetes and cardiovascular diseases. Mol. Cell. Biochem. 2021;476:3785–3814. doi: 10.1007/s11010-021-04201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ming T., Tao Q., Tang S., Zhao H., Yang H., Liu M., Ren S., Xu H. Curcumin: An epigenetic regulator and its application in cancer. Biomed. Pharmacother. 2022;156:113956. doi: 10.1016/j.biopha.2022.113956. [DOI] [PubMed] [Google Scholar]
- 16.Gupta N., Verma K., Nalla S., Kulshreshtha A., Lall R., Prasad S. Free Radicals as a Double-Edged Sword: The Cancer Preventive and Therapeutic Roles of Curcumin. Molecules. 2020;25:5390. doi: 10.3390/molecules25225390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jabczyk M., Nowak J., Hudzik B., Zubelewicz-Szkodzińska B. Curcumin in Metabolic Health and Disease. Nutrients. 2021;13:4440. doi: 10.3390/nu13124440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mao Q.-Q., Xu X.-Y., Cao S.-Y., Gan R.-Y., Corke H., Beta T., Li H.-B. Bioactive Compounds and Bioactivities of Ginger (Zingiber officinale Roscoe) Foods. 2019;8:185. doi: 10.3390/foods8060185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haniadka R., Saldanha E., Sunita V., Palatty P.L., Fayad R., Baliga M.S. A review of the gastroprotective effects of ginger (Zingiber officinale Roscoe) Food Funct. 2013;4:845–855. doi: 10.1039/c3fo30337c. [DOI] [PubMed] [Google Scholar]
- 20.Marx W., Ried K., McCarthy A.L., Vitetta L., Sali A., McKavanagh D., Isenring L. Ginger-Mechanism of action in chemotherapy-induced nausea and vomiting: A review. Crit. Rev. Food Sci. Nutr. 2017;57:141–146. doi: 10.1080/10408398.2013.865590. [DOI] [PubMed] [Google Scholar]
- 21.Rondanelli M., Fossari F., Vecchio V., Gasparri C., Peroni G., Spadaccini D., Riva A., Petrangolini G., Iannello G., Nichetti M., et al. Clinical trials on pain lowering effect of ginger: A narrative review. Physiol. Res. 2020;34:2843–2856. doi: 10.1002/ptr.6730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Semwal R.B., Semwal D.K., Combrinck S., Viljoen A.M. Gingerols and shogaols: Important nutraceutical principles from ginger. Phytochemistry. 2015;117:554–568. doi: 10.1016/j.phytochem.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 23.Ajanaku C.O., Ademosun O.T., Atohengbe P.O., Ajayi S.O., Obafemi Y.D., Owolabi O.A., Akinduti P.A., Ajanaku K.O. Functional bioactive compounds in ginger, turmeric, and garlic. Front. Nutr. 2022;9:1012023. doi: 10.3389/fnut.2022.1012023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang T.A. Health Benefits of Culinary Herbs and Spices. J. AOAC Int. 2019;102:395–411. doi: 10.5740/jaoacint.18-0418. [DOI] [PubMed] [Google Scholar]
- 25.Li R., Wang Y., Liu Y., Chen Q., Fu W., Wang H., Cai H., Peng W., Zhang X. Curcumin Inhibits Transforming Growth Factor-β1-Induced EMT via PPARγ Pathway, Not Smad Pathway in Renal Tubular Epithelial Cells. PLoS ONE. 2013;8:e58848. doi: 10.1371/journal.pone.0058848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang S., Dimango E., Zhu Y., Saroya T.K., Emala C.W., Sang S. Pharmacokinetics of Gingerols, Shogaols, and Their Metabolites in Asthma Patients. J. Agric. Food Chem. 2022;70:9674–9683. doi: 10.1021/acs.jafc.2c03150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Racz L.Z., Racz C.P., Pop L.C., Tomoaia G., Mocanu A., Barbu I., Sárközi M., Roman I., Avram A., Tomoaia-Cotisel M., et al. Strategies for Improving Bioavailability, Bioactivity, and Physical-Chemical Behavior of Curcumin. Molecules. 2022;27:6854. doi: 10.3390/molecules27206854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bi X., Yuan Z., Qu B., Zhou H., Liu Z., Xie Y. Piperine enhances the bioavailability of silybin via inhibition of efflux transporters BCRP and MRP2. Phytomedicine. 2019;54:98–108. doi: 10.1016/j.phymed.2018.09.217. [DOI] [PubMed] [Google Scholar]
- 29.Sohn S.-I., Priya A., Balasubramaniam B., Muthuramalingam P., Sivasankar C., Selvaraj A., Valliammai A., Jothi R., Pandian S. Biomedical Applications and Bioavailability of Curcumin-An Updated Overview. Pharmaceutics. 2021;13:2102. doi: 10.3390/pharmaceutics13122102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taghipour Y.D., Bahramsoltani R., Marques A.M., Naseri R., Rahimi R., Haratipour P., Panah A.I., Farzaei M.H., Abdollahi M. A systematic review of nano formulation of natural products for the treatment of inflammatory bowel disease: Drug delivery and pharmacological targets. DARU J. Pharm. Sci. 2018;26:229–239. doi: 10.1007/s40199-018-0222-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Q., Yang Q., Cao X., Wei Q., Firempong C.K., Guo M., Shi F., Xu X., Deng W., Yu J. Enhanced oral bioavailability and anti-gout activity of [6]-shogaol-loaded solid lipid nanoparticles. Int. J. Pharm. 2018;550:24–34. doi: 10.1016/j.ijpharm.2018.08.028. [DOI] [PubMed] [Google Scholar]
- 32.Yücel Ç., Karatoprak G.Ş., Açıkara Ö.B., Akkol E.K., Barak T.H., Sobarzo-Sánchez E., Aschner M., Shirooie S. Immunomodulatory and anti-inflammatory therapeutic potential of gingerols and their nanoformulations. Front. Pharmacol. 2022;13:902551. doi: 10.3389/fphar.2022.902551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen C., Chen X., Mo Q., Liu J., Yao X., Di X., Qin Z., He L., Yao Z. Cytochrome P450 metabolism studies of [6]-gingerol, [8]-gingerol, and [10]-gingerol by liver microsomes of humans and different species combined with expressed CYP enzymes. RSC Adv. 2023;13:5804–5812. doi: 10.1039/D2RA06184H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ashokkumar K., Murugan M., Dhanya M.K., Warkentin T.D. Botany, traditional uses, phytochemistry and biological activities of cardamom [Elettaria cardamomum (L.) Maton]—A critical review. J. Ethnopharmacol. 2020;246:112244. doi: 10.1016/j.jep.2019.112244. [DOI] [PubMed] [Google Scholar]
- 35.Frijhoff J., Winyard P.G., Zarkovic N., Davies S.S., Stocker R., Cheng D., Knight A.R., Taylor E.L., Oettrich J., Ruskovska T., et al. Clinical Relevance of Biomarkers of Oxidative Stress. Antioxid. Redox Signal. 2015;23:1144–1170. doi: 10.1089/ars.2015.6317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scalbert A., Manach C., Morand C., Rémésy C., Jiménez L. Dietary polyphenols and the prevention of diseases. Crit. Rev. Food Sci. Nutr. 2005;45:287–306. doi: 10.1080/1040869059096. [DOI] [PubMed] [Google Scholar]
- 37.Ďuračková Z. Some current insights into oxidative stress. Physiol. Res. 2010;59:459–469. doi: 10.33549/physiolres.931844. [DOI] [PubMed] [Google Scholar]
- 38.Sies H., Berndt C., Jones D.P. Oxidative Stress. Annu. Rev. Biochem. 2017;86:715–748. doi: 10.1146/annurev-biochem-061516-045037. [DOI] [PubMed] [Google Scholar]
- 39.Hussain T., Tan B., Yin Y., Blachier F., Tossou M.C.B., Rahu N. Oxidative Stress and Inflammation: What Polyphenols Can Do for Us? Oxid. Med. Cell. Longev. 2016;2016:7432797. doi: 10.1155/2016/7432797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Del Río L.A. ROS and RNS in plant physiology: An overview. J. Exp. Bot. 2015;66:2827–2837. doi: 10.1093/jxb/erv099. [DOI] [PubMed] [Google Scholar]
- 41.Giles G.I., Tasker K.M., Jacob C. Hypothesis: The role of reactive sulfur species in oxidative stress. Free Radic. Biol. Med. 2001;31:1279–1283. doi: 10.1016/S0891-5849(01)00710-9. [DOI] [PubMed] [Google Scholar]
- 42.DeLeon E.R., Gao Y., Huang E., Arif M., Arora N., Divietro A., Patel S., Olson K.R. A case of mistaken identity: Are reactive oxygen species actually reactive sulfide species? Am. J. Physiol. Regul. Integr. Comp. Physiol. 2016;310:R549–R560. doi: 10.1152/ajpregu.00455.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Labunskyy V.M., Hatfield D.L., Gladyshev V.N. Selenoproteins: Molecular pathways and physiological roles. Physiol. Rev. 2014;94:739–777. doi: 10.1152/physrev.00039.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carvajal Carvajal C. Especies reactivas del oxígeno: Formación, funcion y estrés oxidativo. Med. Leg. Costa Rica. 2019;36:91–100. [Google Scholar]
- 45.Kumar S., Pandey A.K. Free radicals: Health implications and their mitigation by herbals. Br. J. Med. Med. Res. 2015;7:438–457. doi: 10.9734/BJMMR/2015/16284. [DOI] [Google Scholar]
- 46.Wu J.Q., Kosten T.R., Zhang X.Y. Free radicals, antioxidant defense systems, and schizophrenia. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2013;46:200–206. doi: 10.1016/j.pnpbp.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 47.Taniyama Y., Griendling K.K. Reactive oxygen species in the vasculature: Molecular and cellular mechanisms. Hypertension. 2003;42:1075–1081. doi: 10.1161/01.HYP.0000100443.09293.4F. [DOI] [PubMed] [Google Scholar]
- 48.Pizzino G., Irrera N., Cucinotta M., Pallio G., Mannino F., Arcoraci V., Squadrito F., Altavilla D., Bitto A. Oxidative Stress: Harms and Benefits for Human Health. Oxid. Med. Cell. Longev. 2017;2017:8416763. doi: 10.1155/2017/8416763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Frei B. Reactive oxygen species and antioxidant vitamins: Mechanisms of action. Am. J. Med. 1994;97:S5–S13. doi: 10.1016/0002-9343(94)90292-5. [DOI] [PubMed] [Google Scholar]
- 50.Nishida N., Arizumi T., Takita M., Kitai S., Yada N., Hagiwara S., Inoue T., Minami Y., Ueshima K., Sakurai T., et al. Reactive oxygen species induce epigenetic instability through the formation of 8-hydroxydeoxyguanosine in human hepatocarcinogenesis. Dig. Dis. 2013;31:459–466. doi: 10.1159/000355245. [DOI] [PubMed] [Google Scholar]
- 51.Yasui M., Kanemaru Y., Kamoshita N., Suzuki T., Arakawa T., Honma M. Tracing the fates of site-specifically introduced DNA adducts in the human genome. DNA Repair. 2014;15:11–20. doi: 10.1016/j.dnarep.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 52.Valko M., Izakovic M., Mazur M., Rhodes C.J., Telser J. Role of oxygen radicals in DNA damage and cancer incidence. Mol. Cell. Biochem. 2004;266:37–56. doi: 10.1023/B:MCBI.0000049134.69131.89. [DOI] [PubMed] [Google Scholar]
- 53.Pacher P., Beckman J.S., Liaudet L. Nitric oxide and peroxynitrite in health and disease. Physiol. Rev. 2007;87:315–424. doi: 10.1152/physrev.00029.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Halliwell B. Role of free radicals in the neurodegenerative diseases: Therapeutic implications for antioxidant treatment. Drugs Aging. 2001;18:685–716. doi: 10.2165/00002512-200118090-00004. [DOI] [PubMed] [Google Scholar]
- 55.Dröge W. Free radicals in the physiological control of cell function. Physiol. Rev. 2002;82:47–95. doi: 10.1152/physrev.00018.2001. [DOI] [PubMed] [Google Scholar]
- 56.Galle J. Oxidative stress in chronic renal failure. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2001;16:2135–2137. doi: 10.1093/ndt/16.11.2135. [DOI] [PubMed] [Google Scholar]
- 57.MacNee W. Oxidative stress and lung inflammation in airways disease. Eur. J. Pharmacol. 2001;429:195–207. doi: 10.1016/S0014-2999(01)01320-6. [DOI] [PubMed] [Google Scholar]
- 58.Interdonato M., Pizzino G., Bitto A., Galfo F., Irrera N., Mecchio A., Pallio G., Ramistella V., De Luca F., Santamaria A., et al. Cadmium delays puberty onset and testis growth in adolescents. Clin. Endocrinol. 2015;83:357–362. doi: 10.1111/cen.12704. [DOI] [PubMed] [Google Scholar]
- 59.Rotariu D., Babes E.E., Tit D.M., Moisi M., Bustea C., Stoicescu M., Radu A.-F., Vesa C.M., Behl T., Bungau A.F., et al. Oxidative stress—Complex pathological issues concerning the hallmark of cardiovascular and metabolic disorders. Biomed. Pharmacother. 2022;152:113238. doi: 10.1016/j.biopha.2022.113238. [DOI] [PubMed] [Google Scholar]
- 60.Lobo V., Patil A., Phatak A., Chandra N. Free radicals, antioxidants and functional foods: Impact on human health. Pharmacogn. Rev. 2010;4:118–126. doi: 10.4103/0973-7847.70902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alkadi H. A Review on Free Radicals and Antioxidants. Infect. Disord. Drug Targets. 2020;20:16–26. doi: 10.2174/1871526518666180628124323. [DOI] [PubMed] [Google Scholar]
- 62.Von Dentz K.E., Silva B.S., Queiroz E.A.I.F., Bomfim G.F., Nascimento A.F., Sugizaki M.M., Luvizotto R.A.M. Hibiscus sabdariffa ethanolic extract modulates adipokine levels, decreases visceral fat and improves glycemic profile in high-fat/sugar diet-induced obese rats. Nutr. Food Sci. 2021;51:222–233. doi: 10.1108/NFS-03-2020-0092. [DOI] [Google Scholar]
- 63.Rahal A., Kumar A., Singh V., Yadav B., Tiwari R., Chakraborty S., Dhama K. Oxidative stress, prooxidants, and antioxidants: The interplay. Biomed. Res. Int. 2014;2014:761264. doi: 10.1155/2014/761264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Srinivas U.S., Tan B.W.Q., Vellayappan B.A., Jeyasekharan A.D. ROS and the DNA damage response in cancer. Redox Biol. 2019;25:101084. doi: 10.1016/j.redox.2018.101084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Forrester S.J., Kikuchi D.S., Hernandes M.S., Xu Q., Griendling K.K. Reactive Oxygen Species in Metabolic and Inflammatory Signaling. Circ. Res. 2018;122:877–902. doi: 10.1161/CIRCRESAHA.117.311401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Singh A., Kukreti R., Saso L., Kukreti S. Oxidative stress: A key modulator in neurodegenerative diseases. Molecules. 2019;24:1583. doi: 10.3390/molecules24081583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Senoner T., Dichtl W. Oxidative Stress in Cardiovascular Diseases: Still a Therapeutic Target? Nutrients. 2019;11:2090. doi: 10.3390/nu11092090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Alolga R.N., Wang F., Zhang X., Li J., Tran L.S.P., Yin X. Bioactive Compounds from the Zingiberaceae Family with Known Antioxidant Activities for Possible Therapeutic Uses. Antioxidants. 2022;11:1281. doi: 10.3390/antiox11071281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kang Q., Yang C. Oxidative stress and diabetic retinopathy: Molecular mechanisms, pathogenetic role and therapeutic implications. Redox Biol. 2020;37:101799. doi: 10.1016/j.redox.2020.101799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Romero A., Forero M., Sequeda-Castañeda L.G., Grismaldo A., Iglesias J., Celis-Zambrano C.A., Schuler I., Morales L. Effect of ginger extract on membrane potential changes and AKT activation on a peroxide-induced oxidative stress cell model. J. King Saud Univ. Sci. 2018;30:263–269. doi: 10.1016/j.jksus.2017.09.015. [DOI] [Google Scholar]
- 71.Carnuta M.G., Deleanu M., Barbalata T., Toma L., Raileanu M., Sima A.V., Stancu C.S. Zingiber officinale extract administration diminishes steroyl-CoA desaturase gene expression and activity in hyperlipidemic hamster liver by reducing the oxidative and endoplasmic reticulum stress. Phytomedicine. 2018;48:62–69. doi: 10.1016/j.phymed.2018.04.059. [DOI] [PubMed] [Google Scholar]
- 72.Jalali M., Mahmoodi M., Moosavian S.P., Jalali R., Ferns G., Mosallanezhad A., Imanieh M.H., Mosallanezhad Z. The effects of ginger supplementation on markers of inflammatory and oxidative stress: A systematic review and meta-analysis of clinical trials. Phyther. Res. 2020;34:1723–1733. doi: 10.1002/ptr.6638. [DOI] [PubMed] [Google Scholar]
- 73.Sheikhhossein F., Borazjani M., Jafari A., Askari M., Vataniyan E., Gholami F., Amini M.R. Effects of ginger supplementation on biomarkers of oxidative stress: A systematic review and meta-analysis of randomized controlled trials. Clin. Nutr. ESPEN. 2021;45:111–119. doi: 10.1016/j.clnesp.2021.07.010. [DOI] [PubMed] [Google Scholar]
- 74.Cinelli M.A., Do H.T., Miley G.P., Silverman R.B. Inducible nitric oxide synthase: Regulation, structure, and inhibition. Med. Res. Rev. 2020;40:158–189. doi: 10.1002/med.21599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ippoushi K., Azuma K., Ito H., Horie H., Higashio H. [6]-Gingerol inhibits nitric oxide synthesis in activated J774.1 mouse macrophages and prevents peroxynitrite-induced oxidation and nitration reactions. Life Sci. 2003;73:3427–3437. doi: 10.1016/j.lfs.2003.06.022. [DOI] [PubMed] [Google Scholar]
- 76.Eun M.K., Hye J.K., Kim S., Woo H.C., Yeon H.C., Shi Y.R., Young S.K., Woo S.K., Park S.Y. Modulation of macrophage functions by compounds isolated from Zingiber officinale. Planta Med. 2009;75:148–151. doi: 10.1055/S-0028-1088347. [DOI] [PubMed] [Google Scholar]
- 77.Ballester P., Cerdá B., Arcusa R., Marhuenda J., Yamedjeu K., Zafrilla P. Effect of Ginger on Inflammatory Diseases. Molecules. 2022;27:7223. doi: 10.3390/molecules27217223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang S., Sun X., Jiang L., Liu X., Chen M., Yao X., Sun Q., Yang G. 6-Gingerol induces autophagy to protect HUVECs survival from apoptosis. Chem. Biol. Interact. 2016;256:249–256. doi: 10.1016/j.cbi.2016.07.020. [DOI] [PubMed] [Google Scholar]
- 79.Hsiang C.Y., Lo H.Y., Huang H.C., Li C.C., Wu S.L., Ho T.Y. Ginger extract and zingerone ameliorated trinitrobenzene sulphonic acid-induced colitis in mice via modulation of nuclear factor-κB activity and interleukin-1β signalling pathway. Food Chem. 2013;136:170–177. doi: 10.1016/j.foodchem.2012.07.124. [DOI] [PubMed] [Google Scholar]
- 80.Han S.J., Kim M., D’Agati V.D., Lee H.T. 6-Shogaol protects against ischemic acute kidney injury by modulating NF-κB and heme oxygenase-1 pathways. Am. J. Physiol. Renal Physiol. 2019;317:F743–F756. doi: 10.1152/ajprenal.00182.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mansingh D.P., Sunanda O.J., Sali V.K., Vasanthi H.R. [6]-Gingerol-induced cell cycle arrest, reactive oxygen species generation, and disruption of mitochondrial membrane potential are associated with apoptosis in human gastric cancer (AGS) cells. J. Biochem. Mol. Toxicol. 2018;32:e22206. doi: 10.1002/jbt.22206. [DOI] [PubMed] [Google Scholar]
- 82.Kim Y.J., Jeon Y., Kim T., Lim W.C., Ham J., Park Y.N., Kim T.J., Ko H. Combined treatment with zingerone and its novel derivative synergistically inhibits TGF-β1 induced epithelial-mesenchymal transition, migration and invasion of human hepatocellular carcinoma cells. Bioorg. Med. Chem. Lett. 2017;27:1081–1088. doi: 10.1016/j.bmcl.2016.12.042. [DOI] [PubMed] [Google Scholar]
- 83.Zadorozhna M., Mangieri D. Molecular Sciences Mechanisms of Chemopreventive and Therapeutic Proprieties of Ginger Extracts in Cancer. Int. J. Mol. Sci. 2021;22:6599. doi: 10.3390/ijms22126599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kim S.D., Kwag E.B., Yang M.X., Yoo H.S. Efficacy and Safety of Ginger on the Side Effects of Chemotherapy in Breast Cancer Patients: Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2022;23:11267. doi: 10.3390/ijms231911267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Maroufi S.S., Moradimajd P., Moosavi S.A.A., Imani F., Samaee H., Oguz M. Dose Ginger Have Preventative Effects on PONV-Related Eye Surgery? A Clinical Trial. Anesthesiol. Pain Med. 2019;9:e92072. doi: 10.5812/AAPM.92072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sharifzadeh F., Kashanian M., Koohpayehzadeh J., Rezaian F., Sheikhansari N., Eshraghi N. A comparison between the effects of ginger, pyridoxine (vitamin B6) and placebo for the treatment of the first trimester nausea and vomiting of pregnancy (NVP) J. Matern. Fetal. Neonatal Med. 2018;31:2509–2514. doi: 10.1080/14767058.2017.1344965. [DOI] [PubMed] [Google Scholar]
- 87.Roudsari N.M., Lashgari N.A., Momtaz S., Roufogalis B., Abdolghaffari A.H., Sahebkar A. Ginger: A complementary approach for management of cardiovascular diseases. Biofactors. 2021;47:933–951. doi: 10.1002/biof.1777. [DOI] [PubMed] [Google Scholar]
- 88.El-Seweidy M.M., sarhan Amin R., Husseini Atteia H., El-Zeiky R.R., Al-gabri N.A. Dyslipidemia induced inflammatory status, platelet activation and endothelial dysfunction in rabbits: Protective role of 10-Dehydrogingerdione. Biomed. Pharmacother. 2019;110:456–464. doi: 10.1016/j.biopha.2018.11.140. [DOI] [PubMed] [Google Scholar]
- 89.Angelopoulou E., Paudel Y.N., Papageorgiou S.G., Piperi C. Elucidating the Beneficial Effects of Ginger (Zingiber officinale Roscoe) in Parkinson’s Disease. ACS Pharmacol. Transl. Sci. 2022;5:838–848. doi: 10.1021/acsptsci.2c00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Moon M., Kim H.G., Choi J.G., Oh H., Lee P.K., Ha S.K., Kim S.Y., Park Y., Huh Y., Oh M.S. 6-Shogaol, an active constituent of ginger, attenuates neuroinflammation and cognitive deficits in animal models of dementia. Biochem. Biophys. Res. Commun. 2014;449:8–13. doi: 10.1016/j.bbrc.2014.04.121. [DOI] [PubMed] [Google Scholar]
- 91.Reddy P.H., Manczak M., Yin X., Grady M.C., Mitchell A., Tonk S., Kuruva C.S., Bhatti J.S., Kandimalla R., Vijayan M., et al. Protective Effects of Indian Spice Curcumin Against Amyloid-β in Alzheimer’s Disease. J. Alzheimers. Dis. 2018;61:843–866. doi: 10.3233/JAD-170512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ahmed N., Karobari M.I., Yousaf A., Mohamed R.N., Arshad S., Basheer S.N., Peeran S.W., Noorani T.Y., Assiry A.A., Alharbi A.S., et al. The Antimicrobial Efficacy Against Selective Oral Microbes, Antioxidant Activity and Preliminary Phytochemical Screening of Zingiber officinale. Infect. Drug Resist. 2022;15:2773. doi: 10.2147/IDR.S364175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Park M., Bae J., Lee D.S. Antibacterial activity of [10]-gingerol and [12]-gingerol isolated from ginger rhizome against periodontal bacteria. Phyther. Res. 2008;22:1446–1449. doi: 10.1002/ptr.2473. [DOI] [PubMed] [Google Scholar]
- 94.Zorofchian Moghadamtousi S., Abdul Kadir H., Hassandarvish P., Tajik H., Abubakar S., Zandi K. A review on antibacterial, antiviral, and antifungal activity of curcumin. Biomed Res. Int. 2014;2014:186864. doi: 10.1155/2014/186864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Karuppiah P., Rajaram S. Antibacterial effect of Allium sativum cloves and Zingiber officinale rhizomes against multiple-drug resistant clinical pathogens. Asian Pac. J. Trop. Biomed. 2012;2:597. doi: 10.1016/S2221-1691(12)60104-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gaschler M.M., Stockwell B.R. Lipid peroxidation in cell death. Biochem. Biophys. Res. Commun. 2017;482:419–425. doi: 10.1016/j.bbrc.2016.10.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tan B.L., Norhaizan M.E., Liew W.P.P., Rahman H.S. Antioxidant and oxidative stress: A mutual interplay in age-related diseases. Front. Pharmacol. 2018;9:1162. doi: 10.3389/fphar.2018.01162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Espinosa-Diez C., Miguel V., Mennerich D., Kietzmann T., Sánchez-Pérez P., Cadenas S., Lamas S. Antioxidant responses and cellular adjustments to oxidative stress. Redox Biol. 2015;6:183–197. doi: 10.1016/j.redox.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jakubczyk K., Drużga A., Katarzyna J., Skonieczna-Żydecka K. Antioxidant Potential of Curcumin-A Meta-Analysis of Randomized Clinical Trials. Antioxidants. 2020;9:1092. doi: 10.3390/antiox9111092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Alizadeh M., Kheirouri S. Curcumin reduces malondialdehyde and improves antioxidants in humans with diseased conditions: A comprehensive meta-analysis of randomized controlled trials. BioMedicine. 2019;9:23. doi: 10.1051/bmdcn/2019090423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lee J.H., Song M.Y., Song E.K., Kim E.K., Moon W.S., Han M.K., Park J.W., Kwon K.B., Park B.H. Overexpression of SIRT1 protects pancreatic β-cells against cytokine toxicity by suppressing the nuclear factor-κB signaling pathway. Diabetes. 2009;58:344–351. doi: 10.2337/db07-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lai L., Yan L., Gao S., Hu C.L., Ge H., Davidow A., Park M., Bravo C., Iwatsubo K., Ishikawa Y., et al. Type 5 adenylyl cyclase increases oxidative stress by transcriptional regulation of manganese superoxide dismutase via the SIRT1/FoxO3a pathway. Circulation. 2013;127:1692–1701. doi: 10.1161/CIRCULATIONAHA.112.001212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Qiu X., Brown K., Hirschey M.D., Verdin E., Chen D. Calorie restriction reduces oxidative stress by SIRT3-mediated SOD2 activation. Cell Metab. 2010;12:662–667. doi: 10.1016/j.cmet.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 104.Dehzad M.J., Ghalandari H., Nouri M., Askarpour M. Antioxidant and anti-inflammatory effects of curcumin/turmeric supplementation in adults: A GRADE-assessed systematic review and dose–response meta-analysis of randomized controlled trials. Cytokine. 2023;164:156144. doi: 10.1016/j.cyto.2023.156144. [DOI] [PubMed] [Google Scholar]
- 105.Panahi Y., Hosseini M.S., Khalili N., Naimi E., Majeed M., Sahebkar A. Antioxidant and anti-inflammatory effects of curcuminoid-piperine combination in subjects with metabolic syndrome: A randomized controlled trial and an updated meta-analysis. Clin. Nutr. 2015;34:1101–1108. doi: 10.1016/j.clnu.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 106.Spagnuolo C., Napolitano M., Tedesco I., Moccia S., Milito A., Russo G.L. Neuroprotective Role of Natural Polyphenols. Curr. Top. Med. Chem. 2016;16:1943–1950. doi: 10.2174/1568026616666160204122449. [DOI] [PubMed] [Google Scholar]
- 107.Tang M., Taghibiglou C. The Mechanisms of Action of Curcumin in Alzheimer’s Disease. J. Alzheimers. Dis. 2017;58:1003–1016. doi: 10.3233/JAD-170188. [DOI] [PubMed] [Google Scholar]
- 108.Belwal T., Nabavi S.M., Nabavi S.F., Dehpour A.R., Shirooie S. Naturally Occurring Chemicals against Alzheimer’s Disease. Academic Press; Cambridge, MA, USA: 2020. [Google Scholar]
- 109.He Y., Yue Y., Zheng X., Zhang K., Chen S., Du Z. Curcumin, inflammation, and chronic diseases: How are they linked? Molecules. 2015;20:9183–9213. doi: 10.3390/molecules20059183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Peng Y., Ao M., Dong B., Jiang Y., Yu L., Chen Z., Hu C., Xu R. Anti-Inflammatory Effects of Curcumin in the Inflammatory Diseases: Status, Limitations and Countermeasures. Drug Des. Devel. Ther. 2021;15:4503–4525. doi: 10.2147/DDDT.S327378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yousefian M., Shakour N., Hosseinzadeh H., Hayes A.W., Hadizadeh F., Karimi G. The natural phenolic compounds as modulators of NADPH oxidases in hypertension. Phytomedicine. 2019;55:200–213. doi: 10.1016/j.phymed.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 112.Lin X., Bai D., Wei Z., Zhang Y., Huang Y., Deng H., Huang X. Curcumin attenuates oxidative stress in RAW264.7 cells by increasing the activity of antioxidant enzymes and activating the Nrf2-Keap1 pathway. PLoS ONE. 2019;14:e0216711. doi: 10.1371/journal.pone.0216711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Jamilian M., Foroozanfard F., Kavossian E., Aghadavod E., Shafabakhsh R., Hoseini A., Asemi Z. Effects of curcumin on body weight, glycemic control and serum lipids in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Clin. Nutr. ESPEN. 2020;36:128–133. doi: 10.1016/j.clnesp.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 114.Zhang S., Zou J., Li P., Zheng X., Feng D. Curcumin Protects against Atherosclerosis in Apolipoprotein E-Knockout Mice by Inhibiting Toll-like Receptor 4 Expression. J. Agric. Food Chem. 2018;66:449–456. doi: 10.1021/acs.jafc.7b04260. [DOI] [PubMed] [Google Scholar]
- 115.Zhao J.F., Ching L.C., Huang Y.C., Chen C.Y., Chiang A.N., Kou Y.R., Shyue S.K., Lee T.S. Molecular mechanism of curcumin on the suppression of cholesterol accumulation in macrophage foam cells and atherosclerosis. Mol. Nutr. Food Res. 2012;56:691–701. doi: 10.1002/mnfr.201100735. [DOI] [PubMed] [Google Scholar]
- 116.Meiyanto E., Putri H., Arum Larasati Y., Yudi Utomo R., Istighfari Jenie R., Ikawati M., Lestari B., Yoneda-Kato N., Nakamae I., Kawaichi M., et al. Anti-proliferative and Anti-metastatic Potential of Curcumin Analogue, Pentagamavunon-1 (PGV-1), Toward Highly Metastatic Breast Cancer Cells in Correlation with ROS Generation. Adv. Pharm. Bull. 2019;9:445–452. doi: 10.15171/apb.2019.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mansouri K., Rasoulpoor S., Daneshkhah A., Abolfathi S., Salari N., Mohammadi M., Rasoulpoor S., Shabani S. Clinical effects of curcumin in enhancing cancer therapy: A systematic review. BMC Cancer. 2020;20:791. doi: 10.1186/s12885-020-07256-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Rai D., Singh J.K., Roy N., Panda D. Curcumin inhibits FtsZ assembly: An attractive mechanism for its antibacterial activity. Biochem. J. 2008;410:147–155. doi: 10.1042/BJ20070891. [DOI] [PubMed] [Google Scholar]
- 119.Sharma M., Manoharlal R., Puri N., Prasad R. Antifungal curcumin induces reactive oxygen species and triggers an early apoptosis but prevents hyphae development by targeting the global repressor TUP1 in Candida albicans. Biosci. Rep. 2010;30:391–404. doi: 10.1042/BSR20090151. [DOI] [PubMed] [Google Scholar]
- 120.Saeed A., Sultana B., Anwar F., Mushtaq M., Alkharfy K.M., Gilani A.-H. Antioxidant and antimutagenic potential of seeds and pods of green cardamom (Elettaria cardamomum) Int. J. Pharmacol. 2014;10:461–469. doi: 10.3923/ijp.2014.461.469. [DOI] [Google Scholar]
- 121.Bhaswant M., Poudyal H., Mathai M.L., Ward L.C., Mouatt P., Brown L. Green and black cardamom in a diet-induced rat model of metabolic syndrome. Nutrients. 2015;7:7691–7707. doi: 10.3390/nu7095360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jamil B., Abbasi R., Abbasi S., Imran M., Khan S.U., Ihsan A., Javed S., Bokhari H., Imran M. Encapsulation of Cardamom Essential Oil in Chitosan Nano-composites: In-vitro Efficacy on Antibiotic-Resistant Bacterial Pathogens and Cytotoxicity Studies. Front. Microbiol. 2016;7:1580. doi: 10.3389/fmicb.2016.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Preedy V.R., Watson R.R. Nuts and Seeds in Health and Disease Prevention. Academic Press; Cambridge, MA, USA: 2020. [Google Scholar]
- 124.Cui H., Zhang C., Li C., Lin L. Inhibition mechanism of cardamom essential oil on methicillin-resistant Staphylococcus aureus biofilm. LWT. 2020;122:109057. doi: 10.1016/j.lwt.2020.109057. [DOI] [Google Scholar]
- 125.GiaccoF B. Oxidativestressanddiabetic complications. Circ. Res. 2010;107:1058. [Google Scholar]
- 126.Kazemi S., Yaghooblou F., Siassi F., Rahimi Foroushani A., Ghavipour M., Koohdani F., Sotoudeh G. Cardamom supplementation improves inflammatory and oxidative stress biomarkers in hyperlipidemic, overweight, and obese pre-diabetic women: A randomized double-blind clinical trial. J. Sci. Food Agric. 2017;97:5296–5301. doi: 10.1002/jsfa.8414. [DOI] [PubMed] [Google Scholar]
- 127.Savini I., Catani M.V., Evangelista D., Gasperi V., Avigliano L. Obesity-associated oxidative stress: Strategies finalized to improve redox state. Int. J. Mol. Sci. 2013;14:10497–10538. doi: 10.3390/ijms140510497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Higuchi M., Dusting G.J., Peshavariya H., Jiang F., Hsiao S.T.-F., Chan E.C., Liu G.-S. Differentiation of human adipose-derived stem cells into fat involves reactive oxygen species and Forkhead box O1 mediated upregulation of antioxidant enzymes. Stem Cells Dev. 2013;22:878–888. doi: 10.1089/scd.2012.0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Manna P., Jain S.K. Obesity, oxidative stress, adipose tissue dysfunction, and the associated health risks: Causes and therapeutic strategies. Metab. Syndr. Relat. Disord. 2015;13:423–444. doi: 10.1089/met.2015.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Daneshi-Maskooni M., Keshavarz S.A., Mansouri S., Qorbani M., Alavian S.M., Badri-Fariman M., Jazayeri-Tehrani S.A., Sotoudeh G. The effects of green cardamom on blood glucose indices, lipids, inflammatory factors, paraxonase-1, sirtuin-1, and irisin in patients with nonalcoholic fatty liver disease and obesity: Study protocol for a randomized controlled trial. Trials. 2017;18:260. doi: 10.1186/s13063-017-1979-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Daneshi-Maskooni M., Keshavarz S.A., Qorbani M., Mansouri S., Alavian S.M., Badri-Fariman M., Jazayeri-Tehrani S.A., Sotoudeh G. Green cardamom increases Sirtuin-1 and reduces inflammation in overweight or obese patients with non-alcoholic fatty liver disease: A double-blind randomized placebo-controlled clinical trial. Nutr. Metab. 2018;15:63. doi: 10.1186/s12986-018-0297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Daneshi-Maskooni M., Keshavarz S.A., Qorbani M., Mansouri S., Alavian S.M., Badri-Fariman M., Jazayeri-Tehrani S.A., Sotoudeh G. Green cardamom supplementation improves serum irisin, glucose indices, and lipid profiles in overweight or obese non-alcoholic fatty liver disease patients: A double-blind randomized placebo-controlled clinical trial. BMC Complement. Altern. Med. 2019;19:59. doi: 10.1186/s12906-019-2465-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Aghasi M., Ghazi-Zahedi S., Koohdani F., Siassi F., Nasli-Esfahani E., Keshavarz A., Qorbani M., Khoshamal H., Salari-Moghaddam A., Sotoudeh G. The effects of green cardamom supplementation on blood glucose, lipids profile, oxidative stress, sirtuin-1 and irisin in type 2 diabetic patients: A study protocol for a randomized placebo-controlled clinical trial. BMC Complement. Altern. Med. 2018;18:18. doi: 10.1186/s12906-017-2068-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Cheshmeh S., Ghayyem M., Khamooshi F., Heydarzadeh N., Hojati N., Mosaieby E., Moradi S., Pasdar Y. Green Cardamom Plus Low Calorie Diet Can Decrease Inflammatory Genes Expression among Obese Women with Poly Cystic Ovarian Syndrome, A Double Blind Randomized Clinical Trial. Eat Weight Disord. 2021;27:821–830. doi: 10.1007/s40519-021-01223-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wu Y., Ding Y., Ramprasath T., Zou M.-H. Oxidative stress, GTPCH1, and endothelial nitric oxide synthase uncoupling in hypertension. Antioxid. Redox Signal. 2021;34:750–764. doi: 10.1089/ars.2020.8112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Verma S.K., Jain V., Katewa S.S. Blood pressure lowering, fibrinolysis enhancing and antioxidant activities of cardamom (Elettaria cardamomum) Indian J. Biochem. Biophys. 2009;46:503–506. [PubMed] [Google Scholar]
- 137.Qiblawi S., Dhanarasu S. Chemopreventive effect of cardamom (Elettaria cardamomum L.) against benzo (α) pyrene-induced forestomach papillomagenesis in swiss albino mice. J. Environ. Pathol. Toxicol. Oncol. 2015;34:95–104. doi: 10.1615/JEnvironPatholToxicolOncol.2015010838. [DOI] [PubMed] [Google Scholar]
- 138.Bhat J., Damle A., Vaishnav P.P., Albers R., Joshi M., Banerjee G. In vivo enhancement of natural killer cell activity through tea fortified with Ayurvedic herbs. Phyther. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2010;24:129–135. doi: 10.1002/ptr.2889. [DOI] [PubMed] [Google Scholar]
- 139.Hunt R., Dienemann J., Norton H.J., Hartley W., Hudgens A., Stern T., Divine G. Aromatherapy as treatment for postoperative nausea: A randomized trial. Anesth. Analg. 2013;117:597–604. doi: 10.1213/ANE.0b013e31824a0b1c. [DOI] [PubMed] [Google Scholar]
- 140.Khatiban M., Mirzaie M., Fazeli A., Tapak L., Khalili Z. Effect of Cardamom Inhalation Therapy on Intra-and Postoperative Nausea and Vomiting of Mothers Undergoing Spinal Anesthesia for Elective Cesarean Section. J. PeriAnesthesia Nurs. 2022;37:452–457. doi: 10.1016/j.jopan.2021.09.008. [DOI] [PubMed] [Google Scholar]
- 141.Teneva D., Denkova Z., Denkova R., Atanasova T., Nenov N., Merdzhanov P. Antimicrobial activity of essential oils and extracts from black pepper, cumin, coriander and cardamom against some pathogenic and saprophytic microorganisms. Bulg. J. Vet. Med. 2015;18:373–377. doi: 10.15547/bjvm.881. [DOI] [Google Scholar]
- 142.Paul K., Ganguly U., Chakrabarti S., Bhattacharjee P. Is 1,8-Cineole-Rich Extract of Small Cardamom Seeds More Effective in Preventing Alzheimer’s Disease than 1,8-Cineole Alone? Neuromol. Med. 2020;22:150–158. doi: 10.1007/s12017-019-08574-2. [DOI] [PubMed] [Google Scholar]
- 143.Gomaa A.A., Makboul R.M., El-Mokhtar M.A., Abdel-Rahman E.A., Ahmed I.A., Nicola M.A. Terpenoid-rich Elettaria cardamomum extract prevents Alzheimer-like alterations induced in diabetic rats via inhibition of GSK3β activity, oxidative stress and pro-inflammatory cytokines. Cytokine. 2019;113:405–416. doi: 10.1016/j.cyto.2018.10.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.