Abstract
Sacubitril/valsartan (Sac/Val) reduces mortality in patients with heart failure with reduced ejection fraction (HFrEF) compared to enalapril. However, its effects on functional capacity remain uncertain; consequently, we sought to compare Sac/Val vs. standard medical therapy, in terms of effects on prognostically significant CPET parameters, in HFrEF patients during a long follow-up period. We conducted a single-center, observational study in an HF clinic; specifically, we retrospectively identified that 12 patients switched to Sac/Val and 13 patients that managed with standard, optimal medical therapy (control group). At each visit, baseline, and follow-up (median time: 16 months; IQ range: 11.5–22), we collected demographic information, medical history, vital signs, cardiopulmonary exercise testing, standard laboratory data, pharmacological treatment information, and echocardiographic parameters. The study’s primary end-point was the change from baseline in peak VO2 (adjusted to body weight). We did not observe significant differences between the two study groups at baseline. Similarly, we did not observe any significant differences during the follow-up in mean values of peak VO2 corrected for body weight: Sac/Val baseline: 12.2 ± 4.6 and FU: 12.7 ± 3.3 vs. control group: 13.1 ± 4.2 and 13.0 ± 4.2 mL/kg/min; p = 0.49. No significant treatment differences were observed for changes in VE/VCO2 slope: Sac/Val baseline: 35.4 ± 7.4 and FU: 37.2 ± 13.1 vs. control group: 34.6 ± 9.1 and 34.0 ± 7.3; p = 0.49. In conclusion, after a median follow-up period of 16 months, there was no significant benefit of Sac/Val on peak VO2 and other measures of CPET compared with standard optimal therapy in patients with HFrEF.
Keywords: sacubitril/valsartan, heart failure, HFrEF, CPET, exercise capacity, peak VO2
1. Introduction
Sacubitril/Valsartan (Sac/Val) significantly reduced heart failure (HF) hospitalizations and mortality in the PARADIGM-HF trial [1]. It also showed an essential role in improving the quality of life in patients with chronic HF [2,3]. However, its effects on functional capacity remain uncertain, with controversial results emerging from the studies currently available in the literature [4,5,6].
The cardiopulmonary exercise test (CPET) is a valuable tool in HF with reduced ejection fraction (HFrEF). CPET allows the assessment of relevant parameters for functional capacity and prognostic evaluation (e.g., peak VO2 and minute ventilation/carbon dioxide production relationship [VE/VCO2 slope]) [7,8,9,10,11,12,13].
The previous studies investigating the Sac/Val effects on cardiopulmonary testing parameters are mainly characterized by a short-term follow-up (3–6 months).
On this clinical background, we evaluated prognostically significant CPET parameters in a population with chronic HFrEF and its effect on prognosis, comparing Sac/Val vs. standard medical therapy in a more extended follow-up period.
2. Materials and Methods
2.1. Study Design and Participants
We conducted a single-center, observational study in a HF clinic of a tertiary cardiac center in Italy (Salerno). We retrospectively identified 12 patients who switched to Sac/Val, according to the European guidelines [14], and 13 patients managed with standard, optimal medical therapy (control group). With this sample size, assuming a study power of 80%, with a 2-sided type I error of 0.05, we accepted that only a large treatment effect of sacubitril/valsartan in comparison to standard therapy would have been significantly detectable in terms of change in peak VO2 from baseline, in patients affected by HFrEF.
To be included in the study, participants had to meet the following criteria: (a) have a left ventricular ejection fraction (LVEF) < 40%; (b) have a stationary New York Heart Association (NYHA) functional class of at least II; (c) capability to carry out a valid CPET, and d) have undergone prior treatment with an ACE inhibitor or AR blocker.
Exclusion criteria for the patients that met the inclusion criteria were: (1) hospitalization 90 days prior to evaluation due to HF, (2) myocardial revascularization 180 days prior to the evaluation, (3) concomitant initiation during study follow-up or in the previous 6 months of cardiac resynchronization therapy (CRT) and/or percutaneous mitral valve treatment, (d) had congenital heart disease, (e) failure to execute CPET, and (f) severe renal/hepatic impairment or medical history of tumors.
All patients provided informed consent, and the research ethics committee approved the protocol in accordance with the principles of the Declaration of Helsinki and national regulations.
At each visit, baseline, and follow-up (median time: 16 months; IQ range: 11.5–22), we collected demographic information, medical history, vital signs, 12-lead electrocardiogram, cardiopulmonary exercise testing, standard laboratory data, pharmacological treatments information, and echocardiographic parameters. Doses of Sac/Val were prescribed and titrated to the maximally tolerated doses, according to established recommendations [14]. The primary end-point consisted of the changes from baseline in peak VO2 (adjusted to body weight). The secondary end-point included changes in ventilatory efficiency during exercise (VE/VCO2 slope), in percent predicted VO2, and in main echocardiographic (ejection fraction, left ventricle and left atrium volumes, E/e’ ratio, tricuspid annular plane systolic excursion, systolic pulmonary artery pressure) and hemodynamic (systolic blood pressure) parameters.
2.2. Cardiopulmonary Exercise Testing
All CPETs were conducted on a cycle ergometer, with the pedaling rate set to 60 rpm. A ramp exercise protocol was systematically followed, with the workload starting at 10 watts for a warm-up period of 2 min and increasing by 6 watts every 60 s thereafter. The patients were encouraged to exercise to the point of feeling unable to continue due to dyspnea or fatigue. The peak VO2 was calculated by determining the highest 30 s average within the final minute of the exercise, as recommended by Mezzani et al. [15]. To assess the ventilatory efficiency, we calculated the relationship between minute ventilation and carbon dioxide production (VE/VCO2 slope) over the entire exercise duration, as previously recommended [16].
The percentage of predicted VO2 represented the achieved peak VO2 adjusted for age, weight, and height and expressed as a percentage. We used the equations by Wasserman and Hansen to measure the percentage of predicted VO2 [17].
2.3. Echocardiographic Measurements
To perform echocardiographic examinations, a 3.5 MHz monoplane ultrasound probe of Vivid E-9 (GE-Vingmed Ultrasound, Horten, Norway) was used, following international guidelines [18]. To avoid bias, two expert operators blinded to clinical data assessed all the parameters offline. LVEF was calculated by the Simpson biplane method according to the following formula: LVEF = [left ventricular end-diastolic volume (LVEDV)-LV end-systolic volume (LVESV)]/LVEDV × 100 as the mean of two measures in four and two apical chambers. A biplane method was used for left atrial volume (LAV) assessment, as well. For the evaluation of early-diastolic filling (E), in the apical long-axis view, the pulsed-wave Doppler sample volume was placed at the extremeness of the tenting area of the mitral valve. In the apical 4-chamber view using Tissue Doppler Imaging (TDI), mean e’ was assessed in the basal inferoseptal and lateral LV region. Consequently, the ratio of mitral E peak velocity and averaged e’ velocity (E/e’) was calculated. Furthermore, by sampling the systolic trans-tricuspid pressure gradient, calculated by the modified Bernoulli equation, the tricuspid regurgitant jet velocity was determined. Subsequently, the systolic pulmonary artery pressure (sPAP) was calculated from the sum of the tricuspid regurgitant jet velocity with the estimated right atrial pressure, according to inferior vena cava dimension and inspiratory collapsibility. Finally, in the apical four-chamber view, by aligning the M-mode linear cursor to the lateral tricuspid annulus and evaluating the tricuspid annular plane systolic excursion (TAPSE), the right ventricular function was determined.
2.4. Statistical Analysis
Continuous variables were reported as mean ± standard deviation or median and interquartile (IQ) range if the data did not follow a normal distribution. Numbers and percentages were used for categorical variables. To check for normal distribution, the Shapiro–Wilk test was used. Baseline characteristics were analyzed using either the Student t-test or the Mann–Whitney test for parametric or nonparametric variables, respectively. To assess categorical variables, the chi-square and Fisher’s exact tests were used. For data analysis, a two-way repeated measures ANOVA was employed, with time (baseline, follow-up) and treatment (Sac/Val vs. standard optimal therapy) as factors. In the case of nonparametric variables, a Friedman test was applied. Bonferroni post hoc correction was applied when a significant time × treatment interaction was found. For all tests, a p-value <0.05 was considered statistically significant. Statistical analysis was performed using SPSS software version 23.0 (SPSS Inc., Chicago, Illinois) and R version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria) [19]. Sample size analysis was performed considering the main statistical study analysis, ANOVA with repeated measures and between factors difference, with the G-power 3.1 software.
3. Results
At baseline, demographic and clinical data, according to the main treatment (Sac/Val vs. control group), are described in Table 1, while echocardiographic and cardiopulmonary test data are depicted in Table 2. We did not observe significant differences between the two study groups at baseline.
Table 1.
Baseline characteristics of study population according to treatment.
| Variables | Sacubitril/Valsartan (n = 12) | Control Group (n = 13) | p Value |
|---|---|---|---|
| Demographic and clinical data | |||
| Age (years) | 66.1 ± 7.9 | 60.8 ± 7.4 | 0.1 |
| Female Gender N (%) | 2 (16.7) | 2 (15.4) | 0.9 |
| BMI (Kg/m2) | 28.4 ± 4.3 | 27.4 ± 3.0 | 0.5 |
| SBP (mmHg) | 110 (110–130) | 115 (110–125) | 0.8 |
| HR (beats/min) | 70 (60–74) | 60.5 (57.2–68.5) | 0.2 |
| NYHA Class | |||
| 2 | 8 (66.7) | 9 (69.2) | 0.6 |
| 3 | 4 (33.3) | 3 (23.1) | |
| 4 | 0 | 1 (7.7) | |
| Laboratory data | |||
| Haemoglobin (g/dL) | 14.7 (11.8–15.5) | 14.3 (10.6–14.8) | 0.3 |
| Fasting glucose (mg/dL) | 110 (92–121) | 103 (93.5–111.5) | 1 |
| Creatinine (mg/dL) | 1 (0.9–1.19) | 1.06 (0.94–1.21) | 0.7 |
| Potassium (mEq/L) | 4.36 ± 0.8 | 4.4 ± 0.74 | 0.8 |
| eGFR (mL/min) | 70.1 ± 20.6 | 72.5 ± 32.0 | 0.8 |
| LDL (mg/dL) | 86.4 ± 32.0 | 87.5 ± 33.4 | 0.9 |
| Tryglicerides (mg/dL) | 156.5 ± 74.3 | 104.7 ± 36.7 | 0.1 |
| Comorbidities | |||
| Coronary artery disease N (%) | 8 (66.7) | 5 (38.5) | 0.2 |
| Primitive dilated cardiomyopathy N (%) | 3 (25) | 6 (46.2) | 0.4 |
| Hypertension N (%) | 10 (83.3) | 9 (69.2) | 0.6 |
| Dyslipidemia N (%) | 12 (100) | 11 (84.6) | 0.5 |
| Atrial fibrillation N (%) | 5 (41.7) | 2 (15.4) | 0.2 |
| Diabetes N (%) | 5 (41.7) | 2 (15.4) | 0.2 |
| Chronic Kidney Disease N (%) | 6 (50) | 8 (61.5) | 0.7 |
| Chronic obstructive pulmonary disease N (%) | 0 | 5 (38.5) | 0.04 |
| Thyroid disorders N (%) | 4 (33.3) | 2 (15.4) | 0.4 |
| Previous implantation of ICD/CRT N (%) | 11 (91.7) | 10 (76.9) | 0.6 |
| Medications N (%) | |||
| β-blockers (bisoprolol) | 12 (100) | 13 (100) | - |
| Furosemide | 11 (91.7) | 12 (92.3) | 0.95 |
| Mineralcorticoid receptor antagonist (MRA) | 11 (91.7) | 12 (92.3) | 0.95 |
| Medications dose (mg) | |||
| Bisoprolol | 2.5 (2.5–3.75) | 2.5 (1.25–4.37) | 0.79 |
| Furosemide | 50 (25–68.7) | 50 (25–75) | 0.84 |
| MRA | 37.5 (25–50) | 25 (25–50) | 0.63 |
BMI: body mass index; SBP: systolic blood pressure; HR: heart rate; NYHA: New York Heart Association; eGFR: estimated glomerular filtration rate; LDL: low-density lipoproteins; ICD: implantable cardioverter defibrillator; CRT: cardiac resynchronization therapy; MRA: mineralocorticoid receptor antagonist. We have reported in bold the statistically significant p-value.
Table 2.
Baseline echocardiographic and cardiopulmonary exercise test data, according to treatment.
| Variables | Sacubitril/Valsartan (n = 12) | Control Group (n = 13) | p Value |
|---|---|---|---|
| Echocardiographic parameters | |||
| LVEF (%) | 30.7 ± 4.0 | 32.3 ± 5.1 | 0.4 |
| LVEDVi (mL/m2) | 116.0 ± 36.9 | 129.6 ± 32.4 | 0.4 |
| LVESVi (mL/m2) | 80.6 ± 27.9 | 86.0 ± 33.7 | 0.7 |
| TAPSE (mm) | 17.5 (16.2–21.2) | 18 (16–21.5) | 0.8 |
| sPAP (mmHg) | 32.1 ± 8.7 | 39.2 ± 9.6 | 0.1 |
| LAVi (mL/m2) | 44.2 ± 15.4 | 46.8 ± 15.6 | 0.7 |
| E/e’ ratio | 16.0 ± 7.5 | 15.2 ± 9.5 | 0.9 |
| Cardiopulmonary exercise test data | |||
| PeakVO2 (mL/kg/min) | 12.2 ± 4.6 | 13.1 ± 4.2 | 0.6 |
| VE/VCO2 slope | 35.4 ± 7.4 | 34.6 ± 9.1 | 0.8 |
| Predicted peak VO2, % | 61.5 ± 25.7 | 59.2 ± 20.7 | 0.8 |
LVEF: left ventricular ejection fraction; LVEDVi: left ventricular end-diastolic volume index; LVESVi: left ventricular end-systolic volume index; E: early-wave transmitral diastolic velocity; e’: early-diastolic velocity at tissue Doppler imaging; TAPSE: tricuspid annular plane systolic excursion; sPAP: pulmonary artery systolic pressure; LAVi: left atrial volume index; VO2: oxygen consumption; VE/VCO2: minute ventilation to carbon dioxide production.
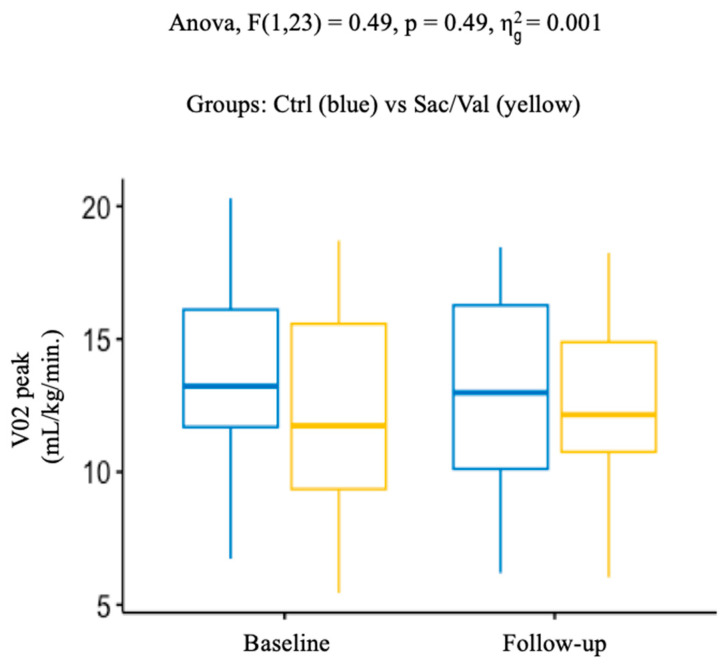
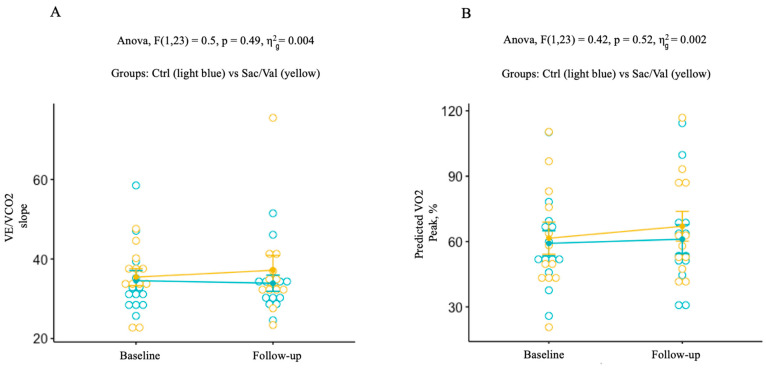
Similarly, we did not observe any significant differences during the follow-up, in terms of main CPET parameters, between the Sac/Val and the control group (Table 3, and Figure 1 and Figure 2A,B). Primary outcome analysis revealed, indeed, no differences in mean values of peak VO2 corrected for body weight between baseline and follow-up: Sac/Val 12.2 ± 4.6 and 12.7 ± 3.3 vs. 13.1 ± 4.2 and 13.0 ± 4.2 mL/kg/min, in the control group; p = 0.49. During the follow-up, no significant treatment differences were observed for changes in VE/VCO2: Sac/Val 35.4 ± 7.4 and 37.2 ± 13.1 vs. 34.6 ± 9.1 and 34.0 ± 7.3 in the control group; p = 0.49, as well as for predicted peak VO2: Sac/Val 61.5 ± 25.7 and 67.0 ± 23.7 vs. 59.2 ± 20.7 and 61.1 ± 23.9 %; p = 0.53. It is noted that, despite the lack of statistical significance in the other secondary outcomes analyzed, we observed a trend of improvement in main echocardiographic parameters in the Sac/Val group (Table 3). Moreover, the Sac/Val group showed a trend towards lower systolic blood pressure values during the follow-up (Table 3).
Table 3.
Primary and secondary outcomes.
| Variables | Baseline | Follow-Up | p Value |
|---|---|---|---|
| PRIMARY OUTCOME | |||
| PeakVO2 (mL/kg/min) | |||
| Sac/Val | 12.2 ± 4.6 | 12.7 ± 3.3 | 0.49 |
| Control group | 13.1 ± 4.2 | 13.0 ± 4.2 | |
| SECONDARY OUTCOMES | |||
| VE/VCO2 slope | |||
| Sac/Val | 35.4 ± 7.4 | 37.2 ± 13.1 | 0.49 |
| Control group | 34.6 ± 9.1 | 34.0 ± 7.3 | |
| Predicted VO2 peak (%) | |||
| Sac/Val | 61.5 ± 25.7 | 67.0 ± 23.7 | 0.53 |
| Control group | 59.2 ± 20.7 | 61.1 ± 23.9 | |
| LVEF (%) | |||
| Sac/Val | 30.7 ± 4.0 | 36.1 ± 4.8 | 0.06 |
| Control group | 32.3 ± 5.1 | 33.1 ± 7.8 | |
| LVEDVi (mL/m2) | |||
| Sac/Val | 116.0 ± 36.9 | 80.3 ± 19.1 | 0.09 |
| Control group | 129.6 ± 32.4 | 125.0 ± 37.2 | |
| LVESVi (mL/m2) | |||
| Sac/Val | 80.6 ± 27.9 | 51.5 ± 15.8 | 0.08 |
| Control group | 86.0 ± 33.7 | 89.2 ± 31.0 | |
| E/e’ ratio | |||
| Sac/Val | 16.0 ± 7.5 | 13.0 ± 10.0 | 0.07 |
| Control group | 15.2 ± 9.5 | 13.9 ± 10.0 | |
| LAVi (ml/m2) | |||
| Sac/Val | 44.2 ± 15.4 | 42.8 ± 5.3 | 0.7 |
| Control group | 46.8 ± 15.6 | 43.8 ± 14.7 | |
| TAPSE (mm) | |||
| Sac/Val | 17.5 (16.2–21.2) | 20 (19–22) | 0.4 |
| Control group | 18 (16.0–21.5) | 20.5 (17.8–22.2) | |
| sPAP (mmHg) | |||
| Sac/Val | 32.1 ± 8.7 | 33.9 ± 10.4 | 0.17 |
| Control group | 39.2 ± 9.6 | 36.7 ± 12.3 | |
| SBP (mmHg) | |||
| Sac/Val | 110 (110–130) | 100 (925–110) | 0.07 |
| Control group | 115 (110–125) | 110 (100–125) | |
Sac/Val: sacubitril/valsartan; VO2: oxygen consumption; VE/VCO2: minute ventilation to carbon dioxide production; LVEF: left ventricular ejection fraction; LVEDVi: left ventricular end-diastolic volume index; LVESVi: left ventricular end-systolic volume index; E: early-wave transmitral diastolic velocity; e’: early-diastolic velocity at tissue Doppler imaging; LAVi: left atrial volume index; TAPSE: tricuspid annular plane systolic excursion; sPAP: pulmonary artery systolic pressure; SBP: systolic blood pressure.
Figure 1.
Changes of peak VO2, from baseline to follow-up, in the control group (blue) and the Sac/Val group (yellow) (p 0.49). VO2: oxygen consumption.
Figure 2.
Figure 2. (A) Changes of VE/VCO2 slope, from baseline to follow-up, in the control group (blue) and in the Sac/Val group (yellow) (p 0.49). (B) Changes of predicted peak VO2 from baseline to follow-up in the control group (blue) and in the Sac/Val group (yellow) (p 0.53). VE/VCO2: minute ventilation to carbon dioxide production; VO2: oxygen consumption.
During the follow-up, none of the patients in the Sac/Val group interrupted the treatment; however, only three patients were able to tolerate the maximum dose. No deaths or rehospitalizations were recorded during the study.
4. Discussion
In our study, we found no significant differences between the Sac/Val and control groups in various measures of CPET. Although we did observe from the baseline a small improvement in peak VO2 in the Sac/Val group, it was lower than the clinically meaningful change of 1.5 mL/min/kg [20,21]. According to the literature, as shown by the HF-ACTION trial, even modest increases as low as 6% in peak VO2 can be associated with better clinical outcomes in HF patients (NYHA class II–IV) over a 3-month period [22]. In the Sac/Val group, we observed only a 4% increase between baseline and follow-up; however, the longer follow-up period considered in our analysis, along with the small sample size, could represent valuable reasons for such a small variation.
Currently, the CPET is considered the ‘gold standard’ for assessing functional capacity in HFrEF patients [23,24,25]. Few studies have investigated the effects of Sac/Val on improving the exercise capacity of patients affected by HFrEF, with discordant results [4,5,6,26,27,28]. Positive effects of Sac/Val on exercise capacity were often observed in retrospective, single-arm studies during short follow-up periods. Our study, with a longer follow-up period, confirms the lack of Sac/Val effects on exercise capacity, similar to the most recent trials [5,6,28]. Although Sac/Val is superior when compared with enalapril in reducing mortality and morbidity [1], it may have a limited impact on improving exercise capacity in patients with HFrEF. It should be noted that even other HF pharmacotherapies showed no benefit in improving exercise capacity [29]. As pointed out in the recent trial by Halle et al. [6], a possible explanation of our results is that the mean baseline values of VO2 peak in the Sac/Val and the control group were, respectively, 12.2 ± 4.6 and 13.1 ± 4.2 mL/kg/min, indicative therefore of a very limited exercise capacity, potentially refractory to further improvement. However, even with better baseline values of VO2 peak (19 mL/Kg/min), a recently published study showed similar negative results [5].
The positive trends showed in terms of main echocardiographic findings in the Sac/Val group during the follow-up means that our population, despite being limited in terms of sample size, is still representative of a real-world population of patients affected by HFrEF. The absence of significant results in both primary and secondary end-points, despite a longer follow-up, may also be related to the study design, where the timings of data entry and follow-up visits are different for each patient. Moreover, a dose effect cannot be ruled out as a possible further cause of unsuccessful improvement in CPET parameters (only three patients in our study achieved the maximum Sac/Val dose).
5. Limitations
There are several limitations to our study that should be acknowledged, which may restrict the generalizability of our results. First, we evaluated a small sample size in a retrospective, single-center study. In addition, the effects of Sac/Val on surrogate markers of efficacy (such as N-terminal pro-B-type natriuretic peptide levels) and functional capacity (NYHA class) were not evaluated [30]. At baseline, 74% of our patients were in NYHA class II. It is possible that an analysis performed in more severe HF patients (Class III) may bring different results. A larger sample size is required to increase the robustness of the results. However, it is challenging to identify a control group since the PARADIGM-HF established the long-term superiority of Sac/Val over enalapril in reducing the risk of cardiovascular death or HF hospitalization and all-cause death. Therefore, despite several limitations, our study provides a real-world population, including a control group and an extended follow-up period, thus supporting our findings.
6. Conclusions
After a median follow-up period of 16 months, there was no significant benefit of Sac/Val on peak VO2 and other measures of CPET compared with standard optimal therapy in patients with HFrEF.
Author Contributions
Conceptualization, V.V. and M.C..; methodology, V.V., A.C. and M.C.; data curation, V.V., A.C., S.D.C., G.J.F., C.M., C.I., F.M., P.D.P., N.V., A.R., D.B. and M.C.; writing—original draft preparation, V.V., A.C. and M.C.; writing—review and editing, V.V., A.C., C.V. and M.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The protocol was approved by the research ethics committee in accordance with the principles of the Declaration of Helsinki and national regulations.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data available on request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.McMurray J.J., Packer M., Desai A.S., Gong J., Lefkowitz M.P., Rizkala A.R., Rouleau J.L., Shi V.C., Solomon S.D., Swedberg K., et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 2014;371:993–1004. doi: 10.1056/NEJMoa1409077. [DOI] [PubMed] [Google Scholar]
- 2.Zhang R., Sun X., Li Y., He W., Zhu H., Liu B., Zhang A. The Efficacy and Safety of Sacubitril/Valsartan in Heart Failure Patients: A Review. J. Cardiovasc. Pharmacol. Ther. 2022;27:10742484211058681. doi: 10.1177/10742484211058681. [DOI] [PubMed] [Google Scholar]
- 3.Song Y., Zhao Z., Zhang J., Zhao F., Jin P. Effects of sacubitril/valsartan on life quality in chronic heart failure: A systematic review and meta-analysis of randomized controlled trials. Front. Cardiovasc. Med. 2022;9:922721. doi: 10.3389/fcvm.2022.922721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malfatto G., Ravaro S., Caravita S., Baratto C., Sorropago A., Giglio A., Tomaselli M., Parati G., Villani A. Improvement of functional capacity in sacubitril-valsartan treated patients assessed by cardiopulmonary exercise test. Acta Cardiol. 2020;75:732–736. doi: 10.1080/00015385.2019.1669317. [DOI] [PubMed] [Google Scholar]
- 5.Dos Santos M.R., Alves M.N.N., Jordao C.P., Pinto C.E.N., Correa K.T.S., de Souza F.R., da Fonseca G.W.P., Tomaz Filho J., Costa M., Pereira R.M.R., et al. Sacubitril/valsartan versus enalapril on exercise capacity in patients with heart failure with reduced ejection fraction: A randomized, double-blind, active-controlled study. Am. Heart J. 2021;239:1–10. doi: 10.1016/j.ahj.2021.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Halle M., Schobel C., Winzer E.B., Bernhardt P., Mueller S., Sieder C., Lecker L.S.M. A randomized clinical trial on the short-term effects of 12-week sacubitril/valsartan vs. enalapril on peak oxygen consumption in patients with heart failure with reduced ejection fraction: Results from the ACTIVITY-HF study. Eur. J. Heart Fail. 2021;23:2073–2082. doi: 10.1002/ejhf.2355. [DOI] [PubMed] [Google Scholar]
- 7.Malhotra R., Bakken K., D’Elia E., Lewis G.D. Cardiopulmonary Exercise Testing in Heart Failure. JACC Heart Fail. 2016;4:607–616. doi: 10.1016/j.jchf.2016.03.022. [DOI] [PubMed] [Google Scholar]
- 8.Sarullo F.M., Fazio G., Brusca I., Fasullo S., Paterna S., Licata P., Novo G., Novo S., Di Pasquale P. Cardiopulmonary Exercise Testing in Patients with Chronic Heart Failure: Prognostic Comparison from Peak VO2 and VE/VCO2 Slope. Open Cardiovasc. Med. J. 2010;4:127–134. doi: 10.2174/1874192401004010127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sinagra G., Iorio A., Merlo M., Cannata A., Stolfo D., Zambon E., Di Nora C., Paolillo S., Barbati G., Berton E., et al. Prognostic value of cardiopulmonary exercise testing in Idiopathic Dilated Cardiomyopathy. Int. J. Cardiol. 2016;223:596–603. doi: 10.1016/j.ijcard.2016.07.232. [DOI] [PubMed] [Google Scholar]
- 10.Corra U., Giordano A., Marcassa C., Gambarin F.I., Gnemmi M., Pistono M. Prognostic value of 6-min walk test compared to cardiopulmonary exercise test in patients with severe heart failure. J. Cardiovasc. Med. 2022;23:379–386. doi: 10.2459/JCM.0000000000001322. [DOI] [PubMed] [Google Scholar]
- 11.Myers J., Gullestad L., Vagelos R., Do D., Bellin D., Ross H., Fowler M.B. Clinical, hemodynamic, and cardiopulmonary exercise test determinants of survival in patients referred for evaluation of heart failure. Ann. Intern. Med. 1998;129:286–293. doi: 10.7326/0003-4819-129-4-199808150-00004. [DOI] [PubMed] [Google Scholar]
- 12.Corra U., Agostoni P.G., Anker S.D., Coats A.J.S., Crespo Leiro M.G., de Boer R.A., Harjola V.P., Hill L., Lainscak M., Lund L.H., et al. Role of cardiopulmonary exercise testing in clinical stratification in heart failure. A position paper from the Committee on Exercise Physiology and Training of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018;20:3–15. doi: 10.1002/ejhf.979. [DOI] [PubMed] [Google Scholar]
- 13.Paolillo S., Veglia F., Salvioni E., Corra U., Piepoli M., Lagioia R., Limongelli G., Sinagra G., Cattadori G., Scardovi A.B., et al. Heart failure prognosis over time: How the prognostic role of oxygen consumption and ventilatory efficiency during exercise has changed in the last 20 years. Eur. J. Heart Fail. 2019;21:208–217. doi: 10.1002/ejhf.1364. [DOI] [PubMed] [Google Scholar]
- 14.McDonagh T.A., Metra M., Adamo M., Gardner R.S., Baumbach A., Bohm M., Burri H., Butler J., Celutkiene J., Chioncel O., et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021;42:3599–3726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 15.Mezzani A., Agostoni P., Cohen-Solal A., Corra U., Jegier A., Kouidi E., Mazic S., Meurin P., Piepoli M., Simon A., et al. Standards for the use of cardiopulmonary exercise testing for the functional evaluation of cardiac patients: A report from the Exercise Physiology Section of the European Association for Cardiovascular Prevention and Rehabilitation. Eur. J. Cardiovasc. Prev. Rehabil. 2009;16:249–267. doi: 10.1097/HJR.0b013e32832914c8. [DOI] [PubMed] [Google Scholar]
- 16.Arena R., Myers J., Aslam S.S., Varughese E.B., Peberdy M.A. Technical considerations related to the minute ventilation/carbon dioxide output slope in patients with heart failure. Chest. 2003;124:720–727. doi: 10.1378/chest.124.2.720. [DOI] [PubMed] [Google Scholar]
- 17.Wasserman K., Hansen J.E., Sue D.Y., Stringer W., Whipp B.J. In: Normal Values. Principles of Exercise Testing and Interpretation. 4th ed. Weinberg R., editor. Lippincott Williams and Wilkins; Philadelphia, PA, USA: 2005. pp. 160–182. [Google Scholar]
- 18.Lang R.M., Badano L.P., Mor-Avi V., Afilalo J., Armstrong A., Ernande L., Flachskampf F.A., Foster E., Goldstein S.A., Kuznetsova T., et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging. 2015;16:233–270. doi: 10.1093/ehjci/jev014. [DOI] [PubMed] [Google Scholar]
- 19.R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. 2020. [(accessed on 10 January 2022)]. Available online: https://www.R-project.org/
- 20.Guazzi M., Palermo P., Pontone G., Susini F., Agostoni P. Synergistic efficacy of enalapril and losartan on exercise performance and oxygen consumption at peak exercise in congestive heart failure. Am. J. Cardiol. 1999;84:1038–1043. doi: 10.1016/S0002-9149(99)00495-6. [DOI] [PubMed] [Google Scholar]
- 21.Lewis G.D., Shah R., Shahzad K., Camuso J.M., Pappagianopoulos P.P., Hung J., Tawakol A., Gerszten R.E., Systrom D.M., Bloch K.D., et al. Sildenafil improves exercise capacity and quality of life in patients with systolic heart failure and secondary pulmonary hypertension. Circulation. 2007;116:1555–1562. doi: 10.1161/CIRCULATIONAHA.107.716373. [DOI] [PubMed] [Google Scholar]
- 22.Swank A.M., Horton J., Fleg J.L., Fonarow G.C., Keteyian S., Goldberg L., Wolfel G., Handberg E.M., Bensimhon D., Illiou M.C., et al. Modest increase in peak VO2 is related to better clinical outcomes in chronic heart failure patients: Results from heart failure and a controlled trial to investigate outcomes of exercise training. Circ. Heart Fail. 2012;5:579–585. doi: 10.1161/CIRCHEARTFAILURE.111.965186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guazzi M., Adams V., Conraads V., Halle M., Mezzani A., Vanhees L., Arena R., Fletcher G.F., Forman D.E., Kitzman D.W., et al. EACPR/AHA Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2012;126:2261–2274. doi: 10.1161/CIR.0b013e31826fb946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mazaheri R., Sadeghian M., Nazarieh M., Niederseer D., Schmied C. Performance of Heart Failure Patients with Severely Reduced Ejection Fraction during Cardiopulmonary Exercise Testing on Treadmill and Cycle Ergometer; Similarities and Differences. Int. J. Environ. Res. Public Health. 2021;18:12958. doi: 10.3390/ijerph182412958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giannitsi S., Bougiakli M., Bechlioulis A., Kotsia A., Michalis L.K., Naka K.K. 6-minute walking test: A useful tool in the management of heart failure patients. Ther. Adv. Cardiovasc. Dis. 2019;13:1753944719870084. doi: 10.1177/1753944719870084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beltran P., Palau P., Dominguez E., Faraudo M., Nunez E., Guri O., Mollar A., Sanchis J., Bayes-Genis A., Nunez J. Sacubitril/valsartan and short-term changes in the 6-minute walk test: A pilot study. Int. J. Cardiol. 2018;252:136–139. doi: 10.1016/j.ijcard.2017.10.074. [DOI] [PubMed] [Google Scholar]
- 27.Vitale G., Romano G., Di Franco A., Caccamo G., Nugara C., Ajello L., Storniolo S., Sarullo S., Agnese V., Giallauria F., et al. Early Effects of Sacubitril/Valsartan on Exercise Tolerance in Patients with Heart Failure with Reduced Ejection Fraction. J. Clin. Med. 2019;8:262. doi: 10.3390/jcm8020262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piepoli M.F., Hussain R.I., Comin-Colet J., Dosantos R., Ferber P., Jaarsma T., Edelmann F. OUTSTEP-HF: Randomised controlled trial comparing short-term effects of sacubitril/valsartan versus enalapril on daily physical activity in patients with chronic heart failure with reduced ejection fraction. Eur. J. Heart Fail. 2021;23:127–135. doi: 10.1002/ejhf.2076. [DOI] [PubMed] [Google Scholar]
- 29.von Haehling S., Arzt M., Doehner W., Edelmann F., Evertz R., Ebner N., Herrmann-Lingen C., Garfias Macedo T., Koziolek M., Noutsias M., et al. Improving exercise capacity and quality of life using non-invasive heart failure treatments: Evidence from clinical trials. Eur. J. Heart Fail. 2021;23:92–113. doi: 10.1002/ejhf.1838. [DOI] [PubMed] [Google Scholar]
- 30.Ferreira J.P., Duarte K., Graves T.L., Zile M.R., Abraham W.T., Weaver F.A., Lindenfeld J., Zannad F. Natriuretic Peptides, 6-Min Walk Test, and Quality-of-Life Questionnaires as Clinically Meaningful Endpoints in HF Trials. J. Am. Coll. Cardiol. 2016;68:2690–2707. doi: 10.1016/j.jacc.2016.09.936. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request.