Abstract
Background and objectives: Local anesthetic systemic toxicity (LAST) in children is extremely rare, occurring at an estimated rate of 0.76 cases per 10,000 procedures. However, among reported cases of LAST in the pediatric population, infants and neonates represent approximately 54% of reported LAST cases. We aim to present and discuss the clinical case of LAST with full clinical recovery due to accidental levobupivacaine intravenous infusion in a healthy 1.5-month-old patient, resulting in cardiac arrest necessitating resuscitation. Case presentation: A 4-kilogram, 1.5-month-old female infant, ASA I, presented to the hospital for elective herniorrhaphy surgery. Combined anesthesia was planned, involving general endotracheal and caudal anesthesia. After anesthesia induction, cardiovascular collapse was noticed, resulting in bradycardia and later cardiac arrest with EMD (Electromechanical Dissociation). It was noticed that during induction, levobupivacaine was accidentally infused intravenously. A local anesthetic was prepared for caudal anesthesia. LET (lipid emulsion therapy) was started immediately. Cardiopulmonary resuscitation was carried out according to the EMD algorithm, which lasted 12 min until spontaneous circulation was confirmed and the patient was transferred to the ICU. In ICU, the girl was extubated the second day, and the third day she was transferred to the regular pediatric unit. Finally, the patient was discharged home after a total of five days of hospitalization with full clinical recovery. A four-week follow-up has revealed that the patient recovered without any neurological or cardiac sequelae. Conclusions: The clinical presentation of LAST in children usually begins with cardiovascular symptoms because pediatric patients are already under general anesthesia when anesthetics are being used, as was the case in our case. Treatment and management of LAST involve cessation of local anesthetic infusion, stabilization of the airway, breathing, and hemodynamics, as well as lipid emulsion therapy. Early recognition of LAST as well as immediate CPR if needed and targeted treatment for LAST can lead to good outcomes.
Keywords: local anesthetic systemic toxicity, anesthesia adverse event, pediatric
1. Introduction
Local anesthetic systemic toxicity (LAST) in children is extremely rare, occurring at an estimated rate of 0.76 cases per 10,000 procedures [1]. However, among reported cases of LAST in the pediatric population, infants and neonates represent approximately 54% of reported cases [2]. Systemic absorption of local anesthetic can occur during bolus infusion or inadvertent intravenous injection, resulting in neurological and cardiovascular complications and death. Methemoglobinemia can also be present in some cases of LAST [3,4].
The mechanism of action of local anesthetics is mainly described by the blockage of voltage-gated Na+ channels, which leads to the prevention of further nerve impulse conduction in the membrane. The therapeutic goal of this mechanism is usually to block the nerve tissues involved in pain transmission; however, if anesthetic enters systemic circulation, local anesthetic blockage has an effect on any tissue containing sodium channels, including cardiac and CNS tissues, which leads to these systems’ functional derangement [5,6].
We present a case report that demonstrates LAST with full clinical recovery due to an accidental levobupivacaine intravenous infusion in a healthy 1.5-month-old patient, resulting in cardiac arrest necessitating resuscitation. The described occurrence is unexpected and novel since there have not been previously published accidental local anesthetic intravenous injections in infants.
2. Case Presentation
A 4-kg, 1.5-month-old female, ASA I, without any medical history, presented for elective one-sided hernia repair. A review of the systems did not reveal any problems. Combined anesthesia was planned, involving general endotracheal and caudal anesthesia. The infant presented to the operating room in a calm, nonagitated state with a heart rate (HR) of 135 bpm and a blood pressure (BP) of 105/60 mmHg.
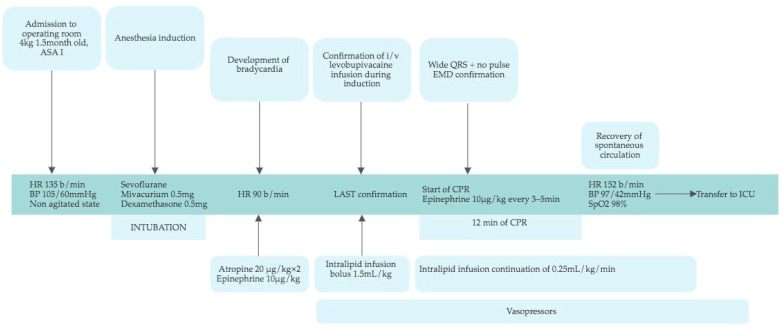
The infant underwent sevoflurane induction with mivacurium (0.5 mg) and dexamethasone (0.5 mg) and was intubated. Immediately after that, bradycardia at 90 bpm occurred. Atropine (20 μg/kg) was administered two times, as was epinephrine (10 μg/kg), without any effect. Displacement of the endotracheal tube and pneumothorax were excluded by patient lung auscultation; moreover, all artificial lung ventilation parameters were in normal ranges according to patient age and weight. Cardiovascular diseases were considered; however, previous medical history and the patient’s clinical condition before anesthesia did not demonstrate any symptoms or signs that could indicate congenital cardiovascular abnormalities. The nurse confessed that during induction, levobupivacaine was accidentally infused intravenously. The mentioned medication was prepared for caudal anesthesia. Presently, intralipid infusion of 1.5 mL/kg bolus was started with continuation of 0.25 mL/kg/min and administration of epinephrine 10 μg/kg to treat bradycardia. The call for a resuscitation team was made. The bone marrows were punctured, and intravenous dobutamine administration was started following a NaHCO3 4.2% 4 mL infusion because, in the arterial blood gas test, severe acidosis was observed (pH 6.9, base excess −15.9 mEq/L). In the cardiac monitor, wide QRS complexes were seen and no pulse was identified; consequently, electromechanical dissociation (EMD) was confirmed, and cardio-pulmonary resuscitation (CPR), including chest compression and epinephrine administration, was started according to the algorithm. CPR continued for 12 min, and i/v epinephrine was repeated three times. Finally, the recovery of spontaneous circulation was confirmed. After resuscitation, HR was 152 bpm, and BP was 97/42 mmHg with continued dobutamine infusion. While continuing artificial lung ventilation, the observed SpO2 value was 98%, and the patient was transferred to the pediatric ICU with continuous intralipid and dobutamine infusions (Figure 1).
Figure 1.
Schematic representation of the case from admission to the operating room to the ICU. HR—heart rate; BP—blood pressure; LAST—local anesthetic systemic toxicity; i/v—intravenously; EMD—electromechanical dissociation; CPR—cardiopulmonary resuscitation; ICU—intensive care unit.
Intralipid was stopped after reaching a total infusion of 60 mL. Vasopressors were discontinued the next day. A transthoracic echocardiogram (TTE) was performed the following day, showing a structurally normal heart. The second day, the patient was extubated, and the third day, she was transferred to a regular pediatric unit. Finally, the patient was discharged home after a total of five days of hospitalization. Later on, any blood test abnormalities, including methemoglobinemia, were not observed.
A four-week follow-up has revealed that the patient recovered without any neurological or cardiac sequelae. Consequently, elective surgery was performed without any adverse events. Further neurological assessment of the patient mentioned is planned within the next two years.
3. Discussion
Local anesthetic systemic toxicity (LAST) in the pediatric population is an understudied complication of regional anesthesia, but it may differ in some aspects when compared with adults’ LAST. The incidence of LAST in children is counted at around 8/100,000 procedures [1], whereas the risk in adults is much higher at 27/100,000 [5]. A recent literature review performed by Ramesh and Boretsky found 31 case reports of LAST among children reported from 2014 to 2019. Surprisingly, no deaths or long-term morbidity have been reported among them, contrary to adults’ mortality rate of LAST, which varies between 4.3% and 10% [7,8].
The clinical presentation of LAST can vary, but mostly it involves CNS and cardiovascular symptoms. Even though CNS signs and symptoms mostly present first, children can develop cardiotoxicity prior to neurological manifestation [3,9]. This is explained by the fact that usually pediatric patients are already under general anesthesia when local anesthetics are administered, so infants are unable to communicate changes in the CNS such as dizziness, tinnitus, taste alterations, paresthesia, tremors, etc. Cardiovascular manifestations of LAST involve arrhythmias and myocardial depression. The range of arrhythmias is wide and can vary from bradyarrhythmias to reentry tachyarrhythmias and wide-complex arrhythmias. If a large dose of local anesthetic is injected into the systemic circulation, it can provoke immediate cardiac arrest [6]. Early symptoms are not specific only to LAST; therefore, caregivers administering or preparing local anesthetics for a particular patient should always keep in mind the possibility of LAST.
In our case, the patient first presented bradycardia, which was refractory to atropine and epinephrine, and later it progressed to wide QRS complexes with no pulse-EMD with the necessity of resuscitation, which lasted 12 min. It is important to note that the development of acute hemodynamic depression in infants after induction of anesthesia, as in our case, has a broad differential diagnosis, including ETT displacement, myocardial depression caused by anesthetics, pneumothorax, undiagnosed congenital diseases, and, finally, LAST. Therefore, to identify this complication requires vigilance and clinical susceptibility.
Management and treatment of LAST start with early identification of the signs and symptoms noted before stabilizing the airway, breathing, and circulation. The cessation of local anesthetic infusions should take place immediately. Secondly, airway security to assure oxygenation and ventilation should be made in order to prevent hypoxia, hypercarbia, or acidosis. Our patient was already intubated, so we just checked the ETT position. Treatment depends on present symptoms—if cardiovascular changes are present, such as bradycardia, as it was in our case—and the administration of atropine 20 μg/kg (repeated once) and/or epinephrine 10 μg/kg (repeated every 3–5 min) according to PALS guidelines (Pediatric Advances Life Support) [10], although according to ASRA guidelines on LAST (American Society of Regional Anesthesia and Pain Medicine), they suggest a lower dose of epinephrine by 1 μg/kg, but there is no explanation why they reduce this dose [5]. Speaking of present CNS symptoms, such as convulsions (which happen less frequently in the pediatric population because they are already under general anesthesia), benzodiazepines should be given. If cardiac arrest is present, CPR with effective chest compression and administration of epinephrine (10 μg/kg) have to be started according to the PALS algorithm. LET (lipid emulsion therapy) should be started immediately after suspicion of the LAST event. Although the specific ILE’s mechanism of action is unclear, some authors explain the theory of “lipid sink”. A LA concentration gradient is formed between the tissues and the blood, due to which the LA are removed from the heart or brain tissue, where there are high concentrations of them, into the “lipid sink”. In this way, the amount of free LA decreases and causes less harm to organs sensitive to the effects of local anesthetics [5]. Hence, ILE binds LA molecules and increases the volume of distribution of LA, thereby reducing the unwanted effects of LA. The recommendations for dosage remain the same for adults as for children, starting with a 1.5 mL/kg bolus over 2–3 min with continuous infusion of 0.25 mL/kg/min and not exceeding the maximum lipid dose of 12 mL/kg [5]. If cardiovascular stability is reached, LET should be continued for 10 min. In our case, we started lipid therapy as soon as a probable diagnosis of LAST was made, approximately 2–3 min after accidental infusion, with recommended doses, but the patient remained hemodynamically unstable and was transferred to the ICU with continuous infusion of LET and dobutamine. The total dose of infused lipid was 60 mL, which means 15 mL/kg. However, it did not contribute to the patients’ outcomes. Furthermore, it is noted that some patients in LAST can develop methemoglobinemia, which is reported only with four types of anesthetics: prilocaine, benzocaine, lidocaine, and tetracaine. However, in laboratory findings, methemoglobinemia can occur due to the infusion of lipid emulsion, which disrupts blood analysis [4].
The presented case report illustrates LAST event provoked by an accidental levobupivacaine direct intravenous infusion in a 1.5-month-old infant with full clinical recovery. Even though LAST manifested with cardiovascular depression resulting in bradycardia and cardiovascular arrest necessitating resuscitation, early recognition of LAST as well as immediate CPR and targeted treatment for LAST led to good outcomes. The mentioned situation was challenging as the infant deteriorated very fast due to LA intravenous injection. When medical staff faces a similar situation during central or peripheral nerve block performance, the LAST can be recognized without delay.
We performed a PubMed search of other reported pediatric LAST cases and case series between 2016 and 2022 and found a total of 16 published cases; most of them were published in the US, with a few in Europe and Asia. Most of the described LAST cases happened in the operating room and mostly involved cardiovascular signs and symptoms. Five out of sixteen cases included cardiac arrest with CPR. Although no sequels due to LAST were mentioned in any case (Table 1).
Table 1.
Summary of published pediatric LAST cases between 2016 and 2022.
| No. | Author | Country | Patient’s Age | Type of Surgery | Place of LAST Event | Intended Site of Administration | Accidental i/v Injection | Local Anesthetic | Cardiovascular | CNS | CPR | Medications Used | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Najafi N., Veyckemans et al. [11] | USA | 4.5 years | Circumcision | Operating room | Penile block | Ropivacaine | Bradycardia | - | - | Atropine | No sequels | |
| 2 | Yu R.N., Houck C.S., Casta A., et al. [12] | USA | 9 months | Circumcision | Operating room | Penile block | Bupivacaine | ECG changes: wide QRS and peaked T waves | - | No sequels | |||
| 3 | Yu R.N., Houck C.S., Casta A., et al. [12] | USA | 3 years and 2 months | Revision circumcision | Operating room | Penile block | Bupivacaine | ECG changes: ST-segment depression and inverted T waves | - | No sequels | |||
| 4 | Yu R.N., Houck C.S., Casta A., et al. [12] | USA | 14 months | Distal hypospadias repair | Operating room | Penile block | Bupivacaine | Hypotension ECG changes: wide QRS and peaked T waves |
- | No sequels | |||
| 5 | Yu R.N., Houck C.S., Casta A., et al. [12] | USA | 9 months | Revision circumcision | Operating room | Penile block | Bupivacaine | Hypotension and atrial flutter |
- | Adenosine | No sequels | ||
| 6 | Yu R.N., Houck C.S., Casta A., et al. [12] | USA | 10 months | Distal hypospadias repair | Operating room | Penile block | Bupivacaine | Hypotension ECG changes: ST-segment depression and QRS widening |
- | No sequels | |||
| 7 | Yu R.N., Houck C.S., Casta A., et al. [12] | USA | 6 months | Circumcision | Operating room | Penile block | Bupivacaine | Hypotension ECG changes: wide QRS and peaked T waves |
- | 4 min CPR | Intralipid | No sequels | |
| 8 | Yu R.N., Houck C.S., Casta A., et al. [12] | USA | 6 months | Circumcision | Operating room | Penile block | Bupivacaine | Hypotension ECG changes: QRS widening and peaked T waves |
- | 3–4 min CPR | Intralipid | No sequels | |
| 9 | Hernandez M.A., Boretsky et al. [13] | USA | 9 months | Pyeloplasty | Intensive care unit | Paravertebral catheter | Probable | Chloroprocaine | Hypotension | Alerted consciousness and seizures | No sequels | ||
| 10 | Musielak M. and McCall J. [14] | USA | 6 years | Skin autography due to burn | Operating room | Local infiltration | Probable | Bupivacaine | Bradycardia, asystole, and hypotension |
30 min CPR | Intralipid and vasopressors |
No sequels | |
| 11 | Shapiro P. and Schroeck H. [15] | USA | 12 months | Repair of the omphalocele and abdominal surgery | Intensive care unit | Epidural catheter 3rd day | Bupivacaine | Agitation and seizures |
Lorazepam | No sequels | |||
| 12 | Yamane Y. and Kagawa T. [16] | Japan | 6 years | Thoracotomy and pacemaker implantation | Operating room | Paravertebral catheter | Ropivacaine | Asystole | 2 min CPR | Adrenaline, intralipid, and vasopressors |
No sequels | ||
| 13 | Torres L.M., Figueroa et al. [17] | Brazil | 6 years | Hypospadias repair | Operating room | Caudal block | Bupivacaine | Ventricular tachycardia 3 x EMD |
1 min 4 min 9 min CPR |
Amiodarone, intralipid, and adrenaline |
No sequels | ||
| 14 | Eizaga Rebollar R., García Palacios et al. [18] | Spain | 17 months | Colostomy close and bowel anastomose | Operating room | Caudal block | Levobupivacaine | ECG changes: ST severe depression and T increase | Intralipid | No sequels | |||
| 15 | Hsieh X.-X., Hsu et al. [19] | Taiwan | 10 years | Tenectomy | Operating room | Intravenously | Lidocaine | Tonic-clonic seizures | Finding a diagnosis of epilepsy | ||||
| 16 | McMahon K., Paster et al. [20] | USA | 15 months | Emergency room | Topical | Lidocaine and prilocaine cream | Tonic-clonic seizures | Lorazepam and intralipid |
No sequels |
We want to emphasize not only the importance of strategies to reduce LAST but also the high importance of implementing effective preventive strategies to improve medication errors.
4. Conclusions
Local anesthetic systemic toxicity is a life-threatening complication that in children usually begins with cardiovascular symptoms because the pediatric patient is already under general anesthesia when anesthetics are being used, as it was in our case. Treatment and management of LAST involve stabilization of the airway, breathing, and hemodynamics, as well as LET therapy. Early recognition of LAST as well as immediate CPR if needed and targeted treatment for LAST can lead to good outcomes. A cornerstone of the presented clinical case is continuous improvement based on learning from errors and adverse events.
Author Contributions
J.J. and I.R. managed the case, wrote, and revised the manuscript. D.E.G., V.G., L.L. and A.M. assisted with the preparation and revision of the manuscript. All authors take full responsibility for the integrity of the study and final manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical review and approval were waived for this retrospective case report by the Kaunas Regional Biomedical Research Ethics Committee because it did not impact the management of the patient.
Informed Consent Statement
The Kaunas Regional Biomedical Research Ethics Committee, according to the law, waived the need for a patient’s consent because this manuscript neither directly nor indirectly identified the person. The written statement from the Ethics Committee is available for review by the Journal editor.
Data Availability Statement
The data presented in the present study is available from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The study received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Walker B.J., Long J.B., Sathyamoorthy M., Birstler J., Wolf C., Bosenberg A.T., Flack S.H., Krane E.J., Sethna N.F., Suresh S., et al. Complications in Pediatric Regional Anesthesia. Anesthesiology. 2018;129:721–732. doi: 10.1097/ALN.0000000000002372. [DOI] [PubMed] [Google Scholar]
- 2.Singaravelu Ramesh A., Boretsky K. Local Anesthetic Systemic Toxicity in Children: A Review of Recent Case Reports and Current Literature. Reg. Anesth. Pain Med. 2021;46:909–914. doi: 10.1136/rapm-2021-102529. [DOI] [PubMed] [Google Scholar]
- 3.Christie L.E., Picard J., Weinberg G.L. Local Anaesthetic Systemic Toxicity. BJA Educ. 2015;15:136–142. doi: 10.1093/bjaceaccp/mku027. [DOI] [Google Scholar]
- 4.Guay J. Methemoglobinemia Related to Local Anesthetics: A Summary of 242 Episodes. Anesth. Analg. 2009;108:837–845. doi: 10.1213/ane.0b013e318187c4b1. [DOI] [PubMed] [Google Scholar]
- 5.Neal J.M., Barrington M.J., Fettiplace M.R., Gitman M., Memtsoudis S.G., Mörwald E.E., Rubin D.S., Weinberg G. The Third American Society of Regional Anesthesia and Pain Medicine Practice Advisory on Local Anesthetic Systemic Toxicity. Reg. Anesth. Pain Med. 2018;43:113–123. doi: 10.1097/AAP.0000000000000720. [DOI] [PubMed] [Google Scholar]
- 6.Berde C.B. Toxicity of Local Anesthetics in Infants and Children. J. Pediatr. 1993;122:S14–S20. doi: 10.1016/S0022-3476(11)80004-1. [DOI] [PubMed] [Google Scholar]
- 7.Gitman M., Barrington M.J. Local Anesthetic Systemic Toxicity. Reg. Anesth. Pain Med. 2018;43:1. doi: 10.1097/AAP.0000000000000721. [DOI] [PubMed] [Google Scholar]
- 8.Vasques F., Behr A.U., Weinberg G., Ori C., Di Gregorio G. A Review of Local Anesthetic Systemic Toxicity Cases Since Publication of the American Society of Regional Anesthesia Recommendations. Reg. Anesth. Pain Med. 2015;40:698–705. doi: 10.1097/AAP.0000000000000320. [DOI] [PubMed] [Google Scholar]
- 9.Maxwell L.G., Martin L.D., Yaster M. Bupivacaine-Induced Cardiac Toxicity in Neonates: Successful Treatment with Intravenous Phenytoin. Anesthesiology. 1994;80:682–686. doi: 10.1097/00000542-199403000-00028. [DOI] [PubMed] [Google Scholar]
- 10.Dontukurthy S., Tobias J.D. Update on Local Anesthetic Toxicity, Prevention and Treatment During Regional Anesthesia in Infants and Children. J. Pediatr. Pharmacol. Ther. 2021;26:445–454. doi: 10.5863/1551-6776-26.5.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Najafi N., Veyckemans F., Du Maine C., van de Velde A., de Backer A., Vanderlinden K., Poelaert J. Systemic toxicity following the use of 1% ropivacaine for pediatric penile nerve block. Reg. Anesth. Pain Med. 2016;41:549–550. doi: 10.1097/AAP.0000000000000415. [DOI] [PubMed] [Google Scholar]
- 12.Yu R.N., Houck C.S., Casta A., Blum R.H. Institutional policy changes to prevent cardiac toxicity associated with bupivacaine penile blockade in infants. A&A Case Rep. 2016;7:71–75. doi: 10.1213/XAA.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 13.Hernandez M.A., Boretsky K., Polaner D. Chloroprocaine: Local anesthetic systemic toxicity in a 9-month infant with paravertebral catheter. Paediatr. Anaesth. 2016;26:665–666. doi: 10.1111/pan.12912. [DOI] [PubMed] [Google Scholar]
- 14.Musielak M., McCall J. Lipid rescue in a pediatric burn patient. J. Burn Care Res. 2016;37:380–382. doi: 10.1097/BCR.0000000000000263. [DOI] [PubMed] [Google Scholar]
- 15.Shapiro P., Schroeck H. Seizure after abdominal surgery in an infant receiving a standard-dose postoperative epidural bupivacaine infusion. A A Case Rep. 2016;6:238–240. doi: 10.1213/XAA.0000000000000286. [DOI] [PubMed] [Google Scholar]
- 16.Yamane Y., Kagawa T. Cardiac arrest after thoracic paravertebral block with ropivacaine in a 6-year-old child. JA Clin. Rep. 2015;1:4–7. doi: 10.1186/s40981-015-0015-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Torres de Araújo Azi L.M., Figueroa D.G., Simas A.A.S. Cardiac arrest after local anaesthetic toxicity in a paediatric patient. Case Rep. Anesthesiol. 2016;7:826–828. doi: 10.1155/2016/7826280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eizaga Rebollar R., García Palacios M.V., Morales Guerrero J., Morera L.M.T. Lipid rescue in children: The prompt decision. J. Clin. Anesth. 2016;32:248–252. doi: 10.1016/j.jclinane.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 19.Hsieh X.-X., Hsu Y.-C., Cherng C.-H., Lin C.C., Huang G.S., Lin S.L., Wu Z.F., Yeh C.C. Grand mal seizure induced by low-dose fentanyl and lidocaine in a young child. Acta Anaesthesiol. Taiwanica. 2015;53:105–108. doi: 10.1016/j.aat.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 20.McMahon K., Paster J., Baker K.A. Local anesthetic systemic toxicity in the pediatric patient. Am. J. Emerg. Med. 2022;54:325. doi: 10.1016/j.ajem.2021.10.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in the present study is available from the corresponding author.