Abstract
Objective:
To determine longitudinal outcomes and contributors to parental stress and coping in mothers of very low-birth-weight (VLBW) children.
Design:
Prospective cohort follow-up of high-risk VLBW children (n=113), low-risk VLBW children (n=80), and term children (n=122) and their mothers from birth to 14 years.
Setting:
Recruitment from level III neonatal intensive care and term nurseries in a large Midwestern region with follow-up at an academic medical center.
Participants:
A total of 315 mother-infant dyads enrolled from November 8, 1989, to February 22, 1992.
Main Exposures:
High-risk VLBW infants had bronchopulmonary dysplasia. Comparison groups were demographically similar low-risk VLBW children (without bronchopulmonary dysplasia) and term children.
Main Outcome Measures:
Child IQ and self-report measures of parenting stress, family impact, maternal coping, education, and social support.
Results:
After VLBW birth, mothers attained fewer additional years of education than term mothers (P=.04). Mothers of high-risk VLBW children felt more personal stress (P=.006) and family stress (P=.009) under conditions of low social support and had greater child-related stress than term mothers; however, they also expressed the highest levels of parenting satisfaction at 14 years. They became less likely to use denial (P=.02) and mental disengagement (P=.03) as coping mechanisms over time. Except for education attainment, mothers of low-risk VLBW infants did not differ from mothers of term children and at 14 years reported the lowest stress.
Conclusions:
Parenting a VLBW child had both positive and negative outcomes, dependent on child medical risk, child IQ, social support, and maternal coping mechanisms, suggesting that mothers experience posttraumatic growth and resilience after significant distress post partum.
Very Low-Birth-Weight (VLBW) and extremely low-birth-weight births continue to increase world-wide due to medical care advances. They number more than 63 000 annually in the United States.1 Long-term outcome studies indicate persistent functional disabilities in a significant proportion of children, leading to research interest in parental stress and adaptation to preterm birth and their effects on the family.2–4 Understanding the experiences of parents of VLBW children is important for medical decision making and the design of intervention programs to improve child outcomes.5 Children’s behavioral and cognitive outcomes are known to be related to maternal psychological status, family stress, financial burden, and maternal coping strategies all of which have been shown to be affected by VLBW birth.4,6–8
While there are a small number of studies of parental outcomes of VLBW children beyond the immediate postpartum period, there is little information on the longitudinal trajectory of parental coping and stress or on factors contributing to stress over time. In a prospective, longitudinal study from birth to 3 years, severity of child medical risk, child age, and developmental delay were related to maternal psychological status, the mother’s child-related stress, personal strain, and family financial impact but not to parenting competence or coping.9 At school age, maternal coping strategies but not psychological symptoms were related to high-risk (HR) VLBW birth.3 Maternal education, coping style, socioeconomic status, and social support have all been related to stress associated with parenting a VLBW infant.3,4,6,9 Longitudinal studies that assess changes in these factors and their effects over time are needed to understand the impact of VLBW birth on the family.10
To our knowledge, this study is the first to address longitudinal changes in maternal stress related to parenting a VLBW infant from birth to early adolescence. In addition to child medical risk and cognitive outcome, the roles of protective factors such as social support, maternal intelligence, education, coping strategies, and family socioeconomic status were assessed in relation to stress.
METHODS
Mothers were interviewed as part of a longitudinal study of the outcomes of infants with bronchopulmonary dysplasia (BPD), a chronic lung disease of prematurity and VLBW.9 Infants with VLBW admitted to the level III neonatal intensive care units of hospitals in the Cleveland, Ohio, region were eligible for the study and were prospectively, consecutively enrolled between November 8, 1989, and February 22, 1992. Mothers and children were seen at 7 points, ie, when the children were aged 1 and 8 months and 1, 2, 3, 8, and 14 years.
The HR children with VLBW (HR-VLBW) had all of the following characteristics: (1) diagnosis of BPD11,12; (2) birth weight less than 1500 g; (3) supplementary oxygen requirement for more than 28 days because of lung immaturity at birth; and (4) radiographic evidence of chronic lung disease. A partial stratification sampling strategy was adopted to enroll adequate numbers of subjects without socioeconomic disadvantage or severe neurologic risk so that the impact of social class and medical risk factors on outcome could be investigated. Infants with BPD who were free of neurologic problems other than grades I or II intraventricular hemorrhage and were not socially disadvantaged (ie, Hollingshead classification IV and V)13 were exhaustively recruited. The remainder was recruited by approaching the family of the next available infant with BPD who could be accommodated in the follow-up schedule. Parents of infants with BPD were approached by a research assistant in the hospital as soon as possible after the diagnosis by the neonatologist, and they were informed of the longitudinal study investigating child outcomes and family stressors associated with VLBW birth.
Low-risk (LR) children with VLBW (LR-VLBW) did not have a diagnosis of BPD, weighed less than 1500 g at birth, and required oxygen supplementation for less than 25 days. For each infant with BPD, the next available comparison VLBW infant without BPD of the same race and socioeconomic status and born during the same period was recruited.
As a comparison group, term children were drawn from the neonatal nurseries. Term infants had no diagnosed medical illnesses or abnormalities at birth, were more than 36 weeks’ gestation, and, for singleton births, weighed more than 2500 g at birth. Information about the study and return-addressed postcards were provided to all mothers in the term nurseries. For each infant with BPD and VLBW enrolled, the next eligible term infant equivalent in race and socioeconomic status with a returned postcard indicating parental willingness to participate was recruited.
For all groups, infants with major congenital malformations, with drug or heavy alcohol exposure, or whose mothers had major psychiatric or physical illness, human immunodeficiency virus, or mental retardation or lived more than 2 hours’ driving distance were excluded. At follow-up, 4 children with diagnoses of cancer (n=2), fragile X syndrome (n=1), or mosaic trisomy 22 (n=1) were excluded. The total sample size included 315 children (113 HR-VLBW children, 80 LR-VLBW children, and 122 term children) with at least 1 visit. Seventy-eight percent (n=245) of the cohort were seen at 4 or more visits. Seventeen completed 1 visit and 19 completed 2 visits. There was no differential attrition based on demographic or medical characteristics.
MEASURES
Mothers completed the following standardized self-report measures at all visits.
The Parenting Stress Index (PSI)14 assesses parental perceptions of the degree of stress related to dimensions of the parenting role. The parent domain of the PSI measures 7 dimensions of stress (attachment, depression, role restriction, health, sense of competence, social isolation, and spousal/partner support) with higher scores indicating greater stress. Under the child domain of the PSI, 6 child characteristics (adaptability, acceptability, distractibility-hyperactivity, mood, demandingness, and reinforces parent) are rated. Normative data were derived from 534 families with children from ages 1 month to 19 years. The PSI has acceptable reliability, has demonstrated validity in studies of parents of sick children, and was used for measurements from birth to 8 years. The Stress Index for Parents of Adolescents,15 which is the adolescent version of the PSI, was given at 14 years. This measure produces the child domain and parent domain scores and has also been shown to be valid and reliable.
The Impact on Family Scale16 measures maternal perceptions of the degree of the child’s negative and positive impact on the family. Designed to assess the impact of a child with a chronic illness or disability, statements were modified to also apply to healthy children. The scale includes 1 factor assessing total impact and 1 factor assessing financial impact, with higher scores indicating higher negative impact. A mastery (coping) set was also retained from the original test. For our study, higher scores indicate higher mastery. The impact was measured from 2 to 14 years. For birth to 1 year, adjusted means were derived from the regression model.
The Multidimensional Scale of Perceived Social Support,17 measured at 2 to 14 years, assesses perceptions of social support from 3 sources: family, friends, and significant other. This scale is a self-report measure of 12 items rated on a 7-point scale from low to high support. The Social Isolation Scale of the PSI, measured at all points, was also used as a measure of social support and was reverse coded to indicate positive social support.
Mothers were administered the Peabody Picture Vocabulary Test—Revised18 at infant birth as a measure of overall verbal IQ, with education level (years of education) measured at all visits.
The Coping Orientation to Problems Experienced scale19 is a self-report questionnaire consisting of 60 items that assess conceptually distinct, theoretically derived dimensions of coping. Internal consistency coefficients range from 0.45 to 0.92 and test-retest reliability coefficients range from 0.46 to 0.86.19 A 4-point scale indicates the degree to which behaviors are used to cope with stressful situations. Three subscales (behavioral disengagement, mental disengagement, and denial) were selected for this study because at 8 years mothers of HR-VLBW children were found to differ from mothers of LR-VLBW and term children on these coping mechanisms. Factor analyses20 indicate that items from these 3 subscales loaded as a factor identified as avoidant coping mechanisms. Item examples include “I pretend that (the stressor) really hasn’t happened,” “I daydream about things other than (the stressor),” and “I give up the attempt to get what I want.” Avoidant coping strategies have been consistently associated with higher maternal stress.6,21,22
All children were administered standardized, normative IQ and developmental assessments at each visit, including the Bayley Scales of Infant Development23 at 8 months to 2 years, the Bayley Scales of Infant Development, second edition24 at 3 years, the Wechsler Intelligence Scale for Children, third edition25 at 8 years, and the Wechsler Intelligence Scale for Children, fourth edition26 at 14 years, all standardized, widely used, normative assessments of child intellectual ability with well-established reliability and validity. Because a developmental quotient was not attained at 1 month, the values at 8 months were used for this point.
This study was approved by the institutional review boards of the hospitals that participated. Informed consent from parents and assent from children were also obtained. Mothers were given a stipend of $50 to $150 for participation, and transportation costs were covered for each visit.
DATA ANALYSES
The generalized estimating equations method27,28 is used to analyze correlated data that otherwise could be modeled as a generalized linear model, an important strategy in the analysis of correlated data sets arising from longitudinal studies in which subjects are measured at different points and share a common characteristic.
The generalized estimating equations method has advantages over conventional methods such as multivariable repeated-measures analyses because it accounts for correlation between outcomes across time within the same individuals and allows for specification of both time-varying and individual-difference variables. It includes data from all assessments regardless of the number of completed follow-up sessions. The generalized estimating equations method was used for linear regression models to determine the association of birth group (HR-VLBW, LRVLBW, or term) with parenting stress (parent domain and child domain of the PSI) and family impact (total, financial, and mastery) over the 7 points while also measuring the contribution of predictors. A test for nonlinear slope for the outcome trajectories indicated that the parent domain of the PSI had a quadratic trajectory; thus, covariates were evaluated with age-squared terms. The same set of analyses was conducted for predictors (maternal education, coping mechanisms, and social support) to assess whether these changed by group over time as there were no differences in these factors across groups at the time of enrollment. To determine whether covariates varied with age, we created a data set that contained the regression slope for each outcome and subject with the independent factor as child age, creating parameter estimates for child age and each outcome. The regression slope was correlated with covariates to determine which might interact with age in the model (P<.20). Covariates were retained at P<.10, interactions at P<.05. Child IQ was evaluated as a potential mediator of the effects of HR-VLBW birth on parenting outcomes.
RESULTS
SAMPLE CHARACTERISTICS
The HR-VLBW children had lower birth weights and gestational ages, more neurologic and medical risk factors at birth, and lower IQ scores at age 8 years than LR-VLBW and term children (Table). There were more multiple births among VLBW children. The IQ scores were in the range of intellectual disability (<70) for 22% of the HR-VLBW group, 10% of the LR-VLBW group, and less than 3% of the term group (; ), reflecting the overall medical risk status and functional outcomes of the groups. The groups did not differ in sex, race, social class, maternal marital status, or maternal verbal IQ, which was in the average range for all groups.
Table.
Maternal and Child Characteristics
| Risk Group |
|||||
|---|---|---|---|---|---|
| Characteristic | HR-VLBW (n=113) | LR-VLBW (n=80) | Term (n=122) | Statistica | P Value |
|
| |||||
| Baseline Measures | |||||
| Male, No. (%) | 60 (53) | 33 (41) | 60 (49) | 0.32 (1)b | .57 |
| African American, No. (%) | 50 (44) | 41 (51) | 57 (47) | 0.13 (1)b | .72 |
| Multiple births, No. (%)c,d,e | 26 (23) | 36 (45) | 12 (10) | 6.14 (1)b | .01 |
| Low socioeconomic status, No. (%) | 63 (56) | 49 (61) | 75 (61) | 0.78 (1)b | .38 |
| Peabody Picture Vocabulary Test–Revised standard score, mean (SD) | 91.06 (17.22) | 88.77 (16.38) | 90.59 (18.15) | 0.42 (2,304) | .66 |
| Birth weight, mean (SD), gc,d,e | 957.37 (246.09) | 1252.56 (178.37) | 3448.79 (527.43) | 1538.39 (2,314) | <.001 |
| Gestational age, mean (SD), wkc,d,e | 27.26 (2.12) | 30.10 (2.24) | 39.75 (1.27) | 1412.64 (2,314) | <.001 |
| Maternal age at child’s birth, mean (SD), y | 27.87 (5.48) | 28.22 (6.06) | 26.91 (6.11) | 1.46 (2,312) | .23 |
|
| |||||
| Time-Varying Measures | |||||
| Maternal education level, mean (SD), yd | 13.48 (0.26) | 13.49 (0.28) | 13.85 (0.43) | 2.94 (2,18) | .08 |
| Social support, mean (SD)f | |||||
| PSI score, 1 mo to 1 y | 16.61 (0.74) | 16.98 (1.30) | 16.75 (0.65) | 0.24 (2,15) | .79 |
| MSPSS score, 2–14 y | 68.20 (1.03) | 67.23 (3.18) | 67.67 (1.59) | 0.21 (2,9) | .82 |
| Child IQ, mean (SD)f | |||||
| MDI score, 8 mo to 3 ye | 90.18 (3.77) | 99.48 (6.65) | 107.06 (7.58) | 7.40 (2,9) | .01 |
| WISC score, 8–14 yc,d,e | 84.30 (2.24) | 92.54 (1.17) | 100.03 (2.70) | 27.14(2,3) | .01 |
| COPE scale score, mean (SD) | |||||
| Denial c,d | 5.14(0.21) | 5.56 (0.24) | 5.60 (0.16) | 10.58 (2,18) | .001 |
| Behavioral disengagement | 5.73 (0.17) | 5.72 (0.28) | 5.93 (0.16) | 2.22 (2,18) | .14 |
| Mental disengagementd | 7.55 (0.49) | 7.68 (0.25) | 8.02 (0.16) | 3.75 (2,18) | .04 |
| Stress score, mean (SD)f | |||||
| Child domain | |||||
| PSI, 1 mo to 8 y | 104.10(4.14) | 101.28(6.11) | 98.81 (3.86) | 1.81 (2,15) | .20 |
| SIPA, 14 y c,e | 45.47 (27.33) | 35.62 (29.21) | 48.44 (30.56) | 3.67 (2,235) | .03 |
| Parent domain | |||||
| PSI, 1 mo to 8 y | 119.93 (4.46) | 119.60 (9.41) | 118.51 (5.19) | 0.07 (2,15) | .93 |
| SIPA, 14 ye | 26.87 (23.11) | 25.30 (23.14) | 34.23 (29.15) | 2.79 (2,235) | .06 |
| Impact score, mean (SD) | |||||
| Mastery | 9.01 (0.13) | 9.27 (0.67) | 9.80 (0.82) | 1.73 (2,9) | .23 |
| Financiald | 6.97 (0.71) | 6.46 (0.62) | 6.00 (0.35) | 2.80 (2,9) | .11 |
| Total | 13.57(1.41) | 12.25 (1.40) | 12.00 (1.02) | 1.68 (2,9) | .24 |
Abbreviations: COPE, Coping Orientation to Problems Experienced; HR, high-risk; LR, low-risk; MDI, Mental Development Index; MSPSS, Multidimensional Scale of Perceived Social Support; PSI, Parenting Stress Index; SIPA, Stress Index for Parents of Adolescents; VLBW, very low-birth-weight; WISC, Wechsler Intelligence Scale for Children.
Statistics are Fscore (df) unless otherwise indicated.
Statistics are χ2 (df).
Significant difference for HR-VLBW children vs LR-VLBW children (P≤.05).
Significant difference for HR-VLBW children vs term children (P≤.05).
Significant difference for term children vs LR-VLBW children (P≤.05).
Owing to changes in questionnaires over time, the following measures were standardized: (1) for child IQ, Bayley MDI (months 8–36) and WISC full-scale IQ (months 96 and 168); (2) for social support, MSPSS total score (months 24–168) and PSI reverse-coded social isolation (measured at months 1–12); and (3) for stress (child domain and parent domain), PSI (months 1–96) and SIPA (month 168).
EFFECTS OF BIRTH RISK ON MATERNAL EDUCATION, COPING, AND SOCIAL SUPPORT
First, we examined the trajectories over time of those factors conceptualized in the study design as impacting maternal stress, ie, maternal education level, avoidant coping mechanisms, and social support, all of which were equivalent across risk groups at birth.
There were significant child age effects for maternal education, indicating an increase in years of education over time for all groups. However, a significant age×group interaction indicated that mothers of term infants increased their education level after their child’s birth at a faster rate than both VLBW groups and by 14 years had attained significantly more years of education (mean education, 14.51 vs 13.82 years, respectively; t239=2.11; P=.04).
Although mothers did not differ in the extent or type of coping mechanisms used at birth through 3 years, their use of 2 coping mechanisms (denial and mental disengagement) differentially changed over time to an extent that significant group differences emerged. At 8 through 14 years, mothers of HR-VLBW children reduced their use of mental disengagement and denial, resulting in lower use compared with mothers of LR-VLBW and term children (Figure 1). Groups did not differ in social support at any time.
Figure 1.
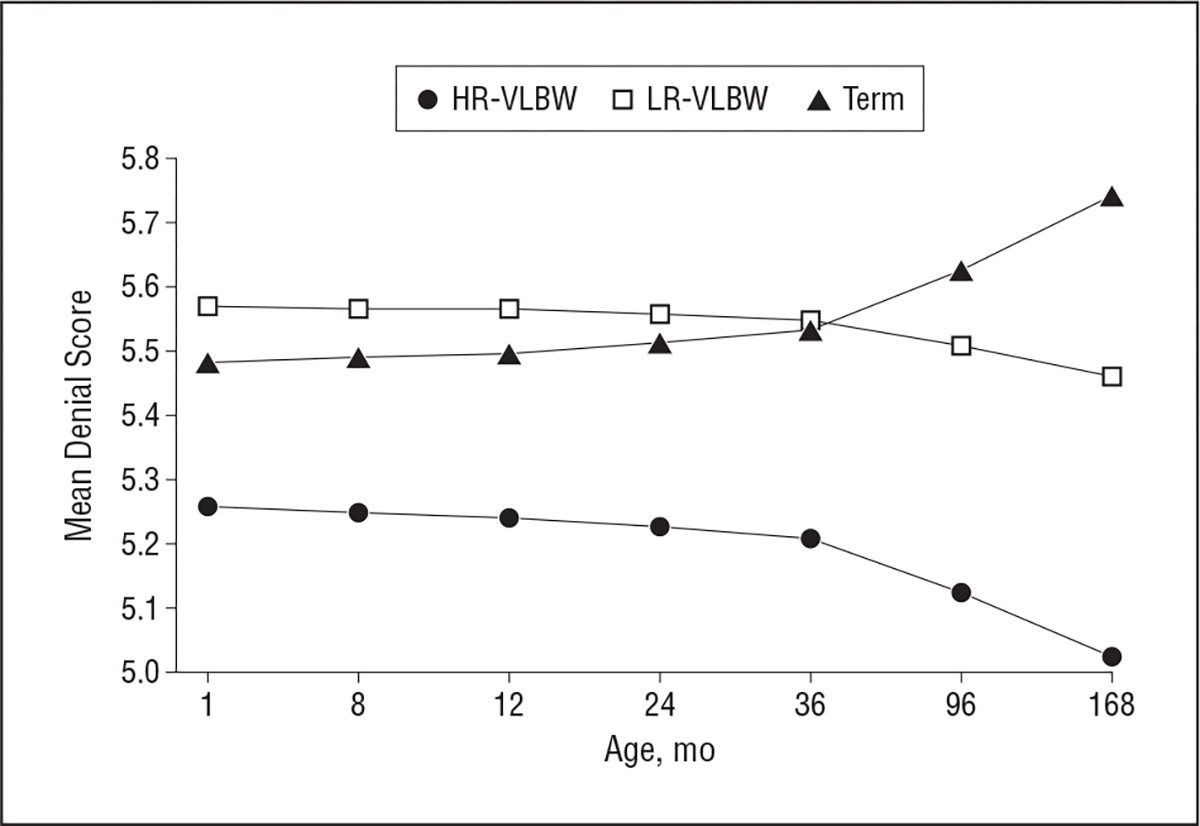
Denial coping on the Coping Orientation to Problems Experienced scale by risk group at each age. P=.02 at 96 months and P=.03 at 168 months for high-risk (HR)–very low-birth-weight (VLBW) vs term children. LR indicates low risk.
EFFECTS OF BIRTH RISK
All outcomes (child domain on the PSI, parent domain on the PSI, total impact, financial impact, and mastery) were predicted by birth risk group and child age after controlling for covariates of maternal vocabulary and education, social support, and copy skills when relevant. For all mothers, older child age was related to decreasing financial strain, lower total and financial impact of the child, and decreasing feelings of positive mastery based on the Impact on Family Scale.16
Birth group had significant effects on financial strain, contributing to the total negative impact of the child on the family. Mothers of HR-VLBW children endorsed feeling more negative financial impact (P<.001) and total impact (P=.01) than the other groups at all points. A significant risk group×social support interaction indicated that social support buffered these negative effects, as mothers of HR-VLBW children with high levels of social support (>75th percentile) did not differ from mothers of LR-VLBW or term children (Figure 2).
Figure 2.
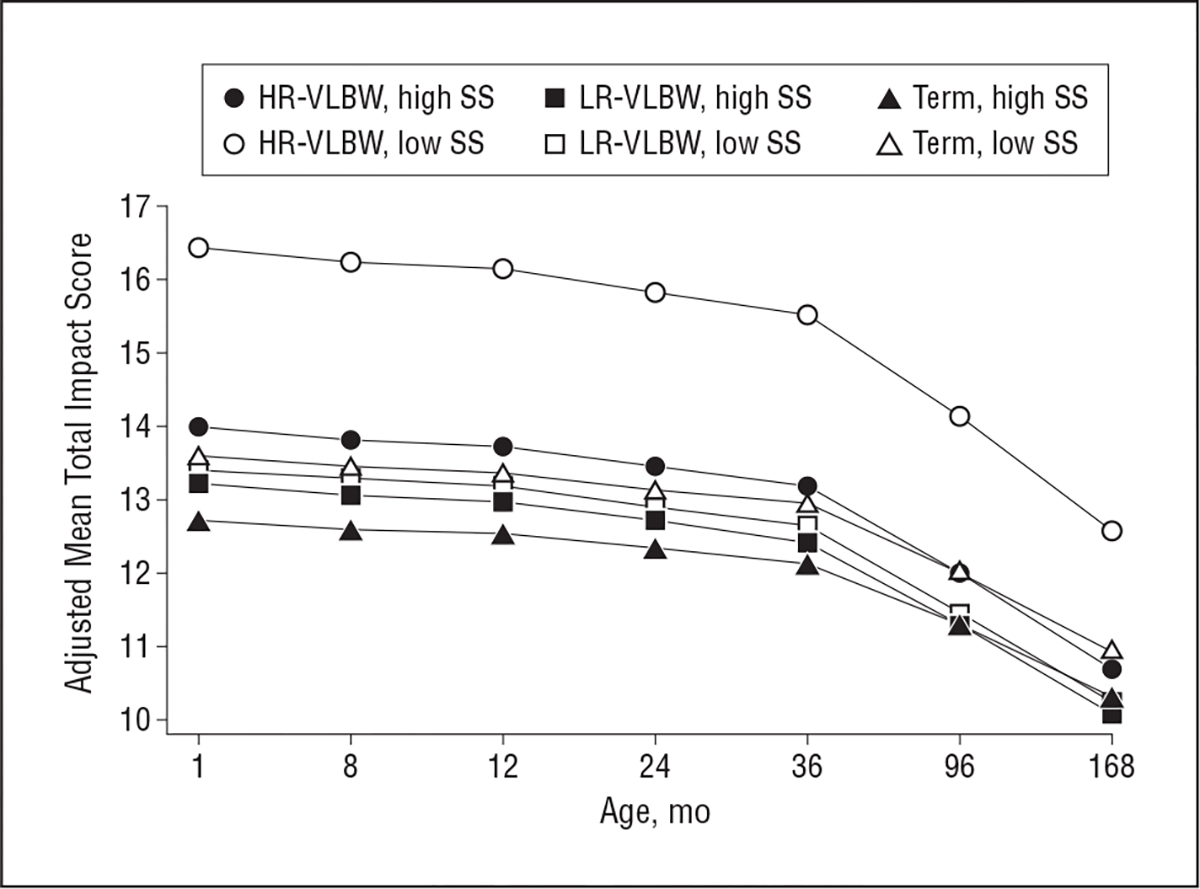
Means of total impact on the Impact on Family Scale by risk group and social support (SS) at each age, adjusted for child’s IQ and maternal mental disengagement. HR indicates high risk; VLBW, very low birth weight; and LR, low risk.
All mothers of VLBW children endorsed feeling more positive mastery than mothers of term children (Figure 3).
Figure 3.
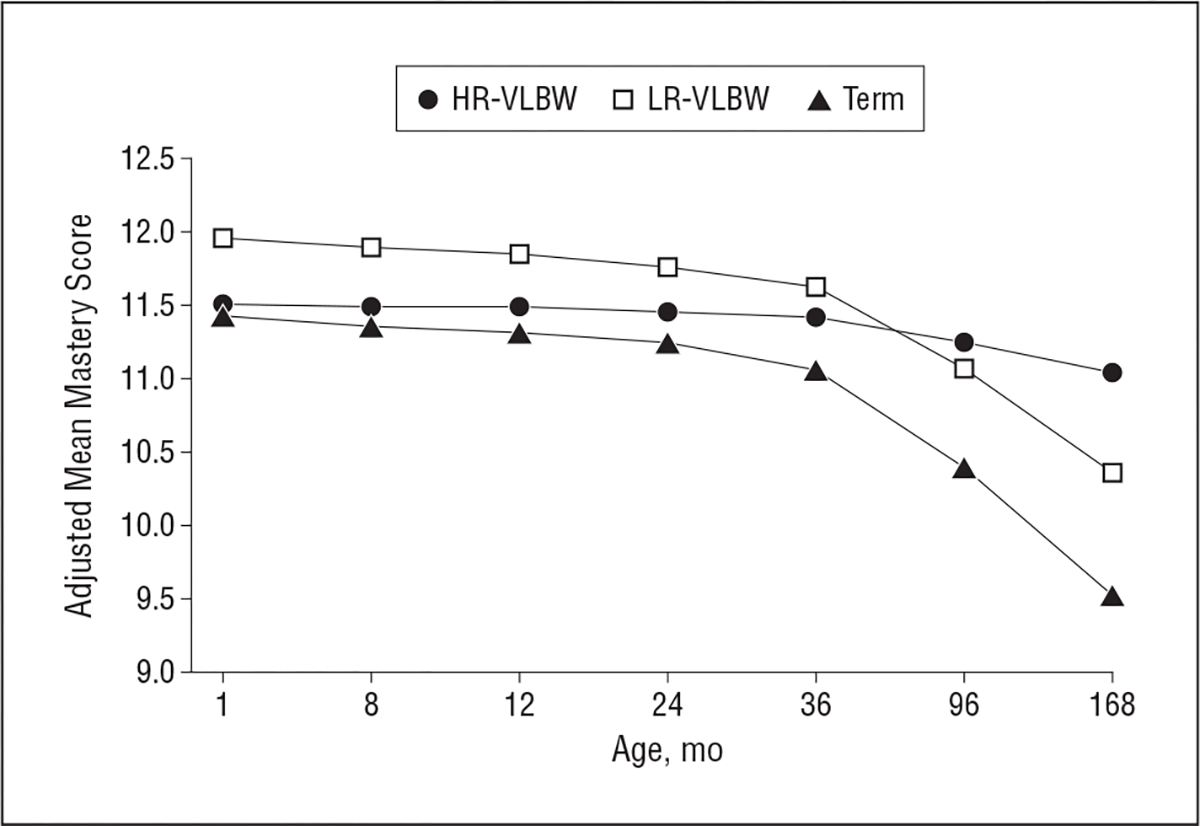
Means of mastery by risk group at each age, adjusted for age, maternal Peabody Picture Vocabulary Test–Revised standard score, social support, mental disengagement, and child IQ. Mastery scores were reverse coded before graphing; thus, higher scores indicate higher mastery. P=.04 at 24 months, P=.03 at 36 months, and P=.03 at 96 months for low-risk (LR)–very low-birth-weight (VLBW) vs term children; P=.008 at 96 months and P<.001 at 168 months for high-risk (HR)–VLBW vs term children.
High-risk VLBW birth was associated with higher child-related stress, with lower child IQ mediating this effect. Mothers of HR-VLBW children reported greater child-related stress overall than mothers of term children, but the effects of birth risk group on child domain stress varied with child age (Figure 4). Mothers of LR-VLBW children reported that their child-related stress decreased at a faster rate than the stress of mothers of HR-VLBW children such that by 14 years, mothers of LR-VLBW children had lower child-related stress than mothers of both HR-VLBW and term children (; ), who did not differ from each other.
Figure 4.
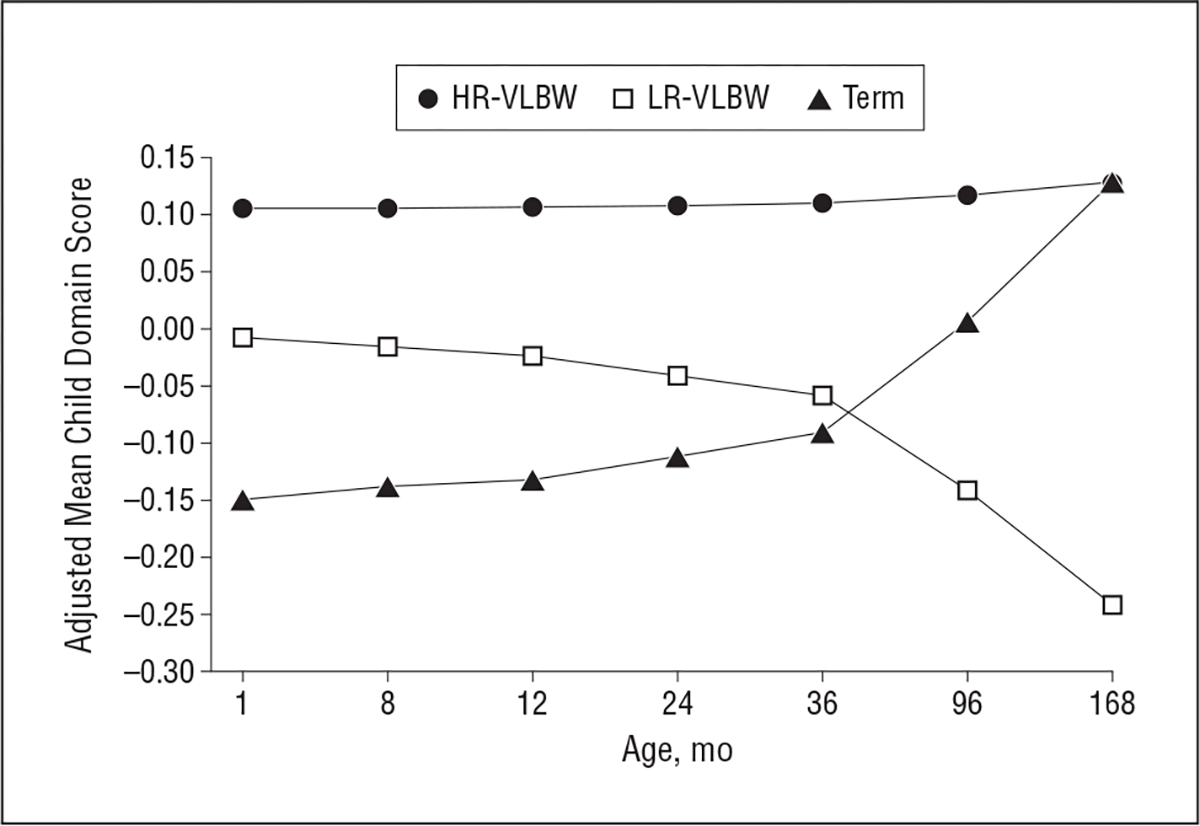
Means of standardized child domain scores on the Parenting Stress Index by risk group at each age, adjusted for child age, maternal Peabody Picture Vocabulary Test–Revised standard score, social support, and mental disengagement. P=.005 at 1 month, P=.005 at 8 months, P=.005 at 12 months, P=.006 at 24 months, and P=.008 at 36 months for high-risk (HR)–very low-birth-weight (VLBW) vs term children; P=.006 at 96 months and P=.007 at 168 months for HR-VLBW vs low-risk (LR)–VLBW children; and P=.01 at 168 months for LR-VLBW vs term children.
Parent domain stress of birth risk groups differed only at 14 years, when mothers of LR-VLBW children reported lower stress than term mothers (; ) (Figure 5), similar to the pattern for child domain stress at the same age.
Figure 5.
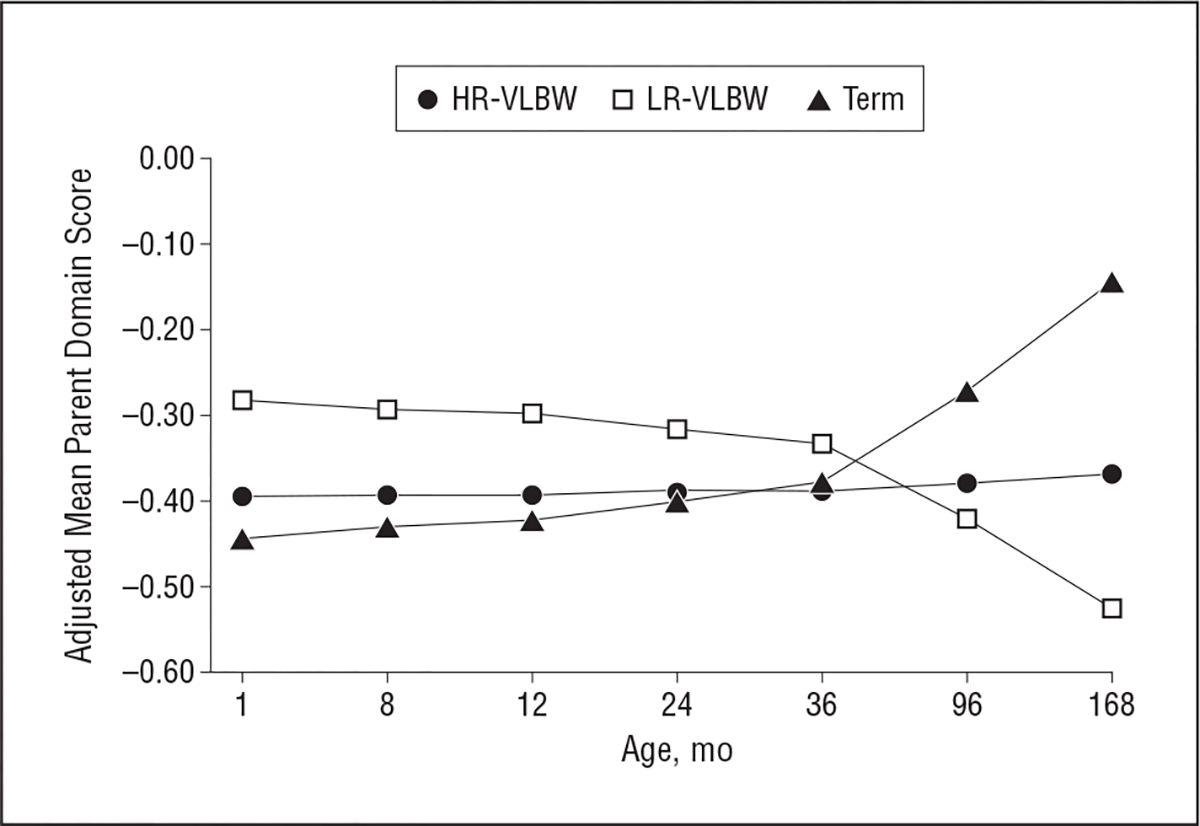
Means of parent domain scores on the Parenting Stress Index by risk group at each age, adjusted for child age, maternal Peabody Picture Vocabulary Test–Revised standard score, and mental disengagement. P=.02 at 168 months for low-risk (LR)–very low-birth-weight (VLBW) vs term children. HR indicates high risk.
COMMENT
In the first longitudinal controlled study from birth to adolescence, VLBW birth was found to have significant effects on several maternal outcomes, including education attainment; financial, child, and parenting stress and satisfaction; and use of coping mechanisms. Several of these maternal outcomes were also affected by contextual factors, ie, VLBW risk status, child IQ, and social support.
EDUCATION ATTAINMENT
Mothers of VLBW infants, regardless of child medical risk, were less likely to advance in schooling after their infants’ birth and had slower and eventually lower education attainment than mothers of term infants. Because the 3 groups of mothers did not differ from each other in education level at enrollment or on other measured factors related to education achievement, it is reasonable to consider their lower attainment to be a sequela of VLBW birth. Education achievement is associated with a host of corollary benefits such as higher occupational and socioeconomic status, personal self-esteem, and wages29 as well as lower child and parenting stress; it also correlates with the use of coping mechanisms related to lower stress.4 Thus, the negative effects of this differential in education achievement should be considered in future analyses of the economic and psychological impact of VLBW birth.
IMPACT ON FAMILY STRESS
Financial stress and the total stressful impact of the child on the family decreased over time for all mothers but were greater for mothers of HR-VLBW children under conditions of low social support. In contrast, mothers of LR-VLBW children had stress similar to that of term mothers independent of social support. Thus, the buffering effects of social support on psychological distress symptoms found at infant birth for all mothers of VLBW infants30 persisted for mothers of HR-VLBW children through early adolescence.
Mothers of HR-VLBW children experienced greater parenting stress due to child characteristics than mothers of term children in the first 3 years of life, but these differences narrowed by school age as the stress of parents of term children increased. In contrast, divergent, significantly lower stress levels were reported by mothers of LR-VLBW children at adolescence, continuing a pattern first seen at 3 years.9 Several factors may contribute to these differences over time. Early adolescence is often considered a challenging period for parents as children seek greater independence and become behaviorally more difficult. Children with VLBW have been characterized as being less involved in parent-child conflict4 and as more risk avoidant than term children,31 potentially reducing parental stress. In addition, mothers of LR-VLBW children may experience relief at their children’s positive outcomes after their traumatic birth experience and subsequent maternal distress9 since they are well within normal limits of intelligence and functional outcomes.
COPING MECHANISMS
Mothers of HR-VLBW infants demonstrated significant changes in their use of certain coping mechanisms over time that suggest adaptation to their initial parenting stress. By 3 years and through 14 years, they became less likely than the other 2 groups to use coping strategies of denial and mental disengagement, coping strategies characterized as efforts to avoid dealing with the reality of a problem or of stressful events.19 It is likely that because HR-VLBW children had lower IQs, more physical disabilities, and more chronic illness than the other 2 groups,32 mothers of HR-VLBW children were confronted with caregiving and medical needs that demanded their attention to a degree that precluded their continued use of avoidant coping strategies. Because initial decline in use of these coping mechanisms appeared at 3 years, when their children’s long-term developmental outcomes could be more reliably predicted, the change in coping for mothers of HR-VLBW children can reasonably be inferred to be related to their parenting of HR-VLBW children.9,33 Moreover, these coping differences from mothers of term and LR-VLBW children increased over time.
MASTERY
Contrary to expectation, term mothers’ experience of mastery and satisfaction in parenting decreased over time to an extent that they reported lower mastery levels than mothers of HR-VLBW children at 14 years. Mothers of HR-VLBW children maintained high levels of mastery over the course of the study, expressing higher satisfaction in parenting than term parents at 14 years. While counterintuitive, these findings are consistent with studies of parents with children diagnosed with life-threatening illnesses; these parents experienced posttraumatic growth and stress and developed new perspectives and coping mechanisms in the face of traumatic life experiences.34–36 Posttraumatic growth is a term that has been used to acknowledge the complexity of adjustment to traumatic stress, which may lead to adaptive coping in addition to the well-defined negative effects.35 Similarly, our findings support those of Saigal et al3 in which parents of 12- to 18-year-old, extremely low-birth-weight children acknowledged negative effects and higher mental stress compared with parents of term children but also felt greater self-esteem and family satisfaction.
Limitations of our study include its restrictions to mothers’ self-report of stress and coping and its lengthy intervals between follow-up visits. However, the prospective, longitudinal, controlled design, the high retention of families, the assessment of multiple aspects of stress and coping, and the differentiation of VLBW risk status advance current knowledge.
For a significant proportion of mothers of VLBW children, long-term adaptation to parenting appears to be no different from that of mothers of term children despite an initial traumatic reaction of postpartum distress.9,10 These mothers can be identified in the neonatal period as their infants have lower risk for chronic illness and neurologic complications. However, our findings also indicate that even mothers of HR-VLBW children, despite their children’s high rate of disability and related parenting stress, demonstrate significant adaptation apparent in their satisfaction in parenting and expressed feelings of mastery. This study indicates that their positive outcomes are related to a number of factors, including high levels of social support, higher education attainment, lower use of avoidant coping strategies, and their children’s better developmental outcomes.
Although mothers of VLBW children demonstrate significant resilience through their children’s early adolescence on the whole, mothers with low social support, with avoidant coping styles, and whose children have significant disabilities should continue to be monitored by health care and education professionals. It will be important to educate health care providers about the role of coping mechanisms and social support in modifying stress. More research is needed into the best ways to support parents of VLBW children and to help them develop adaptive coping mechanisms.
Funding/Support:
This work was supported by grants MCJ-390592, MC-00127, MC-00334, and R40MC089661 from the Maternal and Child Health Program, Health Resources and Services Administration, Department of Health and Human Services, Rockville, Maryland.
Footnotes
Additional Contributions: Terri Lotz-Ganley assisted with manuscript preparation, and Nancy Klein, PhD, George Asaad, MA, Elizabeth H. Lottig, MEd, José Coenraads, MS, and Nicole Herbst, BA, assisted with data collection, coding, and analysis. We extend our thanks to the participating families and hospitals.
Contributor Information
Lynn T. Singer, Department of General Medical Sciences, Ohio; Department of Psychiatry, Ohio; Department Pediatrics, Ohio; Department Psychology, Ohio.
Sarah Fulton, Department Pediatrics, Ohio.
H. Lester Kirchner, Geisinger Health System, Danville, Pennsylvania.
Sheri Eisengart, Department Pediatrics, Ohio.
Barbara Lewis, Department Communication Sciences, Ohio.
Elizabeth Short, Department Psychology, Ohio.
Meeyoung O. Min, Department Pediatrics, Ohio.
Sudtida Satayathum, Department Pediatrics, Ohio.
Carolyn Kercsmar, Case Western Reserve University, Cleveland, and Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio.
Jill E. Baley, Department Pediatrics, Ohio.
References
- 1.Martin JA, Kung H-C, Mathews TJ, et al. Annual summary of vital statistics: 2006. Pediatrics. 2008;121(4):788–801. [DOI] [PubMed] [Google Scholar]
- 2.Majnemer A, Shevell M, Rosenbaum P, Law M, Poulin C. Determinants of life quality in school-age children with cerebral palsy. J Pediatr. 2007;151(5):470–475. [DOI] [PubMed] [Google Scholar]
- 3.Saigal S, Burrows E, Stoskopf B, Rosenbaum P, Streiner D. Impact of extreme prematurity on families of adolescent children. J Pediatr. 2000;137(5):701–706. [DOI] [PubMed] [Google Scholar]
- 4.Singer LT, Fulton S, Kirchner HL, et al. Parenting very low birth weight children at school age: maternal stress and coping. J Pediatr. 2007;151(5):463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marlow N Parenting stress and childhood impairment. J Pediatr. 2007;151(5):448–449. [DOI] [PubMed] [Google Scholar]
- 6.Eisengart SP, Singer LT, Fulton S, Baley JE. Coping and psychological distress in mothers of very low birth weight young children. Parent Sci Pract. 2003;3(1):49–72. doi: 10.1207/S15327922PAR0301_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dodge KA. Developmental psychopathology in children of depressed mothers. Dev Psychol. 1990;26(1):3–6. doi: 10.1037/0012-1649.26.1.3. [DOI] [Google Scholar]
- 8.McCormick MC, Brooks-Gunn J, Workman-Daniels K, Turner J, Peckham GJ. The health and developmental status of very low-birth-weight children at school age. JAMA. 1992;267(16):2204–2208. [PubMed] [Google Scholar]
- 9.Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281(9):799–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warfield ME, Krauss MW, Hauser-Cram P, Upshur CC, Shonkoff JP. Adaptation during early childhood among mothers of children with disabilities. J Dev Behav Pediatr. 1999;20(1):9–16. [DOI] [PubMed] [Google Scholar]
- 11.Northway WH Jr, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. N Engl J Med. 1967;276(7):357–368. [DOI] [PubMed] [Google Scholar]
- 12.Martin RJ, Walsh-Sukys MC. Bronchopulmonary dysplasia: no simple solution. N Engl J Med. 1999;340(13):1036–1038. [DOI] [PubMed] [Google Scholar]
- 13.Hollingshead AB. Two Factor Index of Social Position. New Haven, CT: Yale University; 1957. [Google Scholar]
- 14.Abidin RR. Parenting Stress Index. 2nd ed. Charlottesville, VA: Pediatric Psychology Press; 1986. [Google Scholar]
- 15.Sheras PT, Abidin RR, Konold TR. Stress Index for Parents of Adolescents (SIPA). Lutz, FL: Psychological Assessment Resources; 1998. [Google Scholar]
- 16.Stein REK, Jessop D. The Impact on Family Scale revisited: further psychometric data. J Dev Behav Pediatr. 2003;24(1):9–16. [PubMed] [Google Scholar]
- 17.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52(1):30–41. [DOI] [PubMed] [Google Scholar]
- 18.Dunn L, Dunn L. Peabody Picture Vocabulary Test–Revised. Circle Pines, MN: American Guidance Service; 1981. [Google Scholar]
- 19.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283. [DOI] [PubMed] [Google Scholar]
- 20.Eisengart SP, Singer LT, Kirchner HL, et al. Factor structure of coping: two studies of mothers with high levels of life stress. Psychol Assess. 2006;18(3):278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barakat LP, Linney JA. Optimism, appraisals, and coping in the adjustment of mothers and their children with spina bifida. J Child Fam Stud. 1995;4(3):303–320. doi: 10.1007/BF02233965. [DOI] [Google Scholar]
- 22.Thompson RJ Jr, Oehler JM, Catlett AT, Johndrow DA. Maternal psychological adjustment to the birth of an infant weighing 1500 grams or less. Infant Behav Dev. 1993;16(4):471–485. doi: 10.1016/0163-6383(93)80005-S. [DOI] [Google Scholar]
- 23.Bayley N Manual for the Bayley Scales of Infant Development. New York, NY: Psychological Corp; 1969. [Google Scholar]
- 24.Bayley N Manual for the Bayley Scales of Infant Development. 2nd ed. San Antonio, TX: Psychological Corp; 1993. [Google Scholar]
- 25.Wechsler D Wechsler Intelligence Scale for Children. 3rd ed. San Antonio, TX: Psychological Corp; 1991. [Google Scholar]
- 26.Wechsler D Wechsler Intelligence Scale for Children. 4th ed. San Antonio, TX: Psychological Corp; 2003. [Google Scholar]
- 27.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. doi: 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- 28.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 29.Baum S, Payea K. Education Pays 2004: The Benefits of Higher Education for Individuals and Society. Rev ed. New York, NY: College Board; 2005:23–52. [Google Scholar]
- 30.Singer LT, Davillier M, Bruening P, Hawkins S, Yamashita TS. Social support, psychological distress, and parenting strains in mothers of very low birthweight infants. Fam Relat. 1996;45(3):343–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hack M, Cartar L, Schluchter M, Klein N, Forrest CB. Self-perceived health, functioning and well-being of very low birth weight infants at age 20 years. J Pediatr. 2007;151(6):635–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Short EJ, Klein NK, Lewis BA, et al. Cognitive and academic consequences of bronchopulmonary dysplasia and very low birth weight: 8-year-old outcomes. Pediatrics. 2003;112(5):e359. doi: 10.1542/peds.112.5.e359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singer L, Yamashita T, Lilien L, Collin M, Baley J. A longitudinal study of developmental outcome of infants with bronchopulmonary dysplasia and very low birth weight. Pediatrics. 1997;100(6):987–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turner de S, Cox H. Facilitating post traumatic growth. Health Qual Life Outcomes. 2004;2:34. doi: 10.1186/1477-7525-2-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barakat LP, Alderfer MA, Kazak AE. Posttraumatic growth in adolescent survivors of cancer and their mothers and fathers. J Pediatr Psychol. 2006;31(4):413–419. [DOI] [PubMed] [Google Scholar]
- 36.Ribi K, Vollrath ME, Sennhauser FH, Gnehm HE, Landolt MA. Prediction of posttraumatic stress in fathers of children with chronic diseases or unintentional injuries: a six-months follow-up study. Child Adolesc Psychiatry Ment Health. 2007;1(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]


