Abstract
Background:
Hypertension is one of the most important causes of cardiovascular diseases. Patients with hypertension have a lower quality of life. We aimed to evaluate the effects of mindfulness meditation on blood pressure, mental health, and quality of life in patients with hypertension.
Methods:
This randomized clinical trial was performed in 2019 in Isfahan. Eighty adult women with Stage I or II hypertension were included and assigned randomly to 2 groups: 12 weeks of mindfulness-based stress reduction (MBSR) and routine care. At baseline and 1 week after the end of the intervention, blood pressure, stress, depression, anxiety, and quality of life of the studied participants were measured using the Depression, Anxiety, and Stress Scale-21 (DASS-21) and 36-Item Short Form Survey (SF-36) questionnaires. The data were analyzed using the independent t-test, the paired t-test, and the MANCOVA test.
Results:
After the intervention, the mean systolic and diastolic blood pressures decreased significantly in the intervention group compared with the baseline (142.82±11.01 mmHg vs 133.7±510.43 mmHg for systolic pressure and 86.12±8.24 mmHg vs 79.15±6.26 mmHg for diastolic pressure) and the control group (140.18±14.27 mmHg vs 142.15±10.23 mmHg for systolic pressure and 84.62±9.22 vs mmHg 88.51±8.54 mmHg for diastolic pressure; P=0.001). There was also a significant increase in quality of life, stress, anxiety, and depression scores in the intervention group (P<0.05).
Conclusion:
The 12-week MBSR program resulted in a significant reduction in the mean systolic and diastolic blood pressures and improvement in mental health and different aspects of quality of life.
Keywords: Mindfulness, Mental health, Hypertension, Quality of life
Introduction
Hypertension is one of the most significant causes of cardiovascular diseases. Research has shown that the prevalence of hypertension is on the rise in all countries, especially Iran, with the disease accounting for 7.1 million deaths annually worldwide. Based on epidemiologic studies, the prevalence of hypertension in the adult population of Iran is 23.2%.1,2 Hypertension, like most chronic diseases, is closely related to lifestyle, mental health, and quality of life, and if not controlled appropriately, it can cause various issues, including disability, reduced productivity, and ultimately diminished mental health.3
Recent studies have shown that patients with hypertension have a lower quality of life than individuals with normal blood pressure.4,5 Quality of life is an issue that determines the level of satisfaction with daily life because it affects different life aspects, including physical, mental, social, and spiritual.6 In most previous studies, individuals with hypertension had low scores in all aspects, including physical strength, social function, mental health, mental function, and energy, compared with healthy subjects.7,8
In addition to chronic disease, individuals’ quality of life is also affected by stress. It increases emotions and behavioral changes and interferes with cognition and biological mechanisms.9 Stress could also be a major cause of mental diseases. Mental health, one of the most significant aspects of health in populations, is affected by different factors, such as age and stress.10 Recent decades are synonymous with lifestyle changes, endangering many aspects of physical and mental health and leading to more physical and mental illnesses. According to statistics released by the World Health Organization (WHO), mental illness affects about 250 million people, of whom 52 million suffer from severe mental illness.11
A psychological intervention to alleviate stress is mindfulness-based stress reduction (MBSR). Mindfulness meditation has the potential for the treatment of clinical disorders and might facilitate the cultivation of a healthy mind and increased well-being.12 Mindfulness practice improves emotion regulation and ameliorates stress. Research has shown that practicing mindfulness alters the physical structure of the brain.13 Investigations have indicated that the fronto-limbic network involved in these processes shows various patterns of engagement by mindfulness meditation.14 Some studies have investigated the effectiveness of mindfulness training in reducing stress and blood pressure and increasing quality of life and mental health.15,16
The principal mechanism of the effectiveness of mindfulness meditation is stress alleviation. Various studies have evaluated the effectiveness of stress reduction in lowering blood pressure, which could lead to enhanced quality of life.17 These changes have been evaluated separately in previous studies. Nonetheless, given the significance of hypertension and its impact on quality of life and stress, we aimed to assess the effects of mindfulness meditation on blood pressure, mental health, and quality of life in patients with hypertension.
Methods
The present randomized clinical trial was performed in 2019 in Isfahan, a central city in Iran. The study population consisted of hypertensive adult women (age =30–59 y) visiting Imam Ali Health Care Center in 2019. The study protocol was approved by the Research Committee and was confirmed by the Ethics Committee of Isfahan University of Medical Sciences (ethics code:
IR.MUI.MED.REC.1399.653, Iranian Registry of Clinical Trials [IRCTID]: IRCT20190410043230N1). All the patients signed an informed consent form.
The inclusion criteria were composed of physician-diagnosed Stage I or II hypertension with or without medical treatments, a history of regular visits to the health center during the preceding 6 months, age between 30 to 59 years, and the ability to participate in treatment sessions. The exclusion criteria consisted of pregnancy, lactation, receiving psychological treatments in the past year, alcohol or drug abuse, chronic diseases, including cancer, failure to follow the designed study protocol, participation in any exercise program or psychotherapy sessions outside the protocol of the current study, and hypertension crisis.
The sample size was 40 patients for each group, based on a statistical power of 80%, a significance level of 5%, and a 20% drop rate. Eighty patients were selected from the entire covered population of Imam Ali Health Care Center via electronic health records based on the inclusion and exclusion criteria. The participants were allocated randomly to 2 groups, intervention and control, using a random allocation software tool (developed by Mahmoud Saghaei).
Demographic data, including age, education level, occupation, and marital status, as well as blood pressure, were noted for all the patients. The method of blood pressure measurement was the same as that before study commencement. Blood pressure was assessed twice at 5-minute intervals, and the mean value was recorded as blood pressure. Stress, depression, and anxiety were measured using the Depression, Anxiety, and Stress Scale-21 (DASS-21) questionnaire. This questionnaire assesses negative emotional symptoms using a 4-point Likert scale, ranging from 0 to 3. DASS-21 has 3 subscales, depression, anxiety, and stress, with 7 items in each subscale. These subscales are scored by adding the total item scores, which can range from 0 to 21. The summed number in each subscale needs to be multiplied by 2 because DASS 21 is the short form of the scale. Accordingly, a higher score indicates worse status. The validity and reliability of this questionnaire in the Iranian population were confirmed by Sahebi et al18 in 2005. The quality of life of the patients was also measured using a 36-Item Short Form Survey (SF-36) questionnaire. It has 36 questions and consists of 8 subscales, with each subscale consisting of 2 to 10 items. The subscales are composed of physical functioning, role limitations due to physical health, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems, and mental health. One question covers changes in health status over the past year and is not counted in scoring the 8 dimensions. The total score on each SF-36 subscale ranges between 0 and 100, with greater scores indicating a better health-related quality of life. The validity and reliability of this questionnaire have also been confirmed in Iran.19,20
The intervention group received 8 weekly 120-minute sessions of MBSR training by a psychologist skilled in this field. Afterward, home exercises were given to the participants for 4 weeks, and they recorded the results on a weekly basis at home. They learned different mindfulness skills, such as body scan exercises, sitting meditation, and yoga. They were advised to practice these skills at home for at least 45 minutes per day, 6 days per week. Training sessions were implemented based on the fundamental concepts and specific techniques provided in the MBSR manual by Kabat-Zinn.20
The control group received routine care in the health care center throughout the study. For the purposes of compliance with ethical considerations, after the end of the study, the control group was given the printed and audio contents of the mindfulness training. At week 13 (1 week after the end of the intervention), blood pressure, stress, depression, anxiety, and quality of life were measured using the same measuring tools.
The data were analyzed using the SPSS 24 software with descriptive statistics, including the t, paired t, and χ2 tests. The assumption of the analysis was checked by evaluating the normality of the dependent variables via the Kolmogorov–Smirnov test. Additionally, linear relationships between the dependent variable and the covariates were evaluated using a scatter plot. A confidence level of less than 0.05 was considered statistically significant.
Results
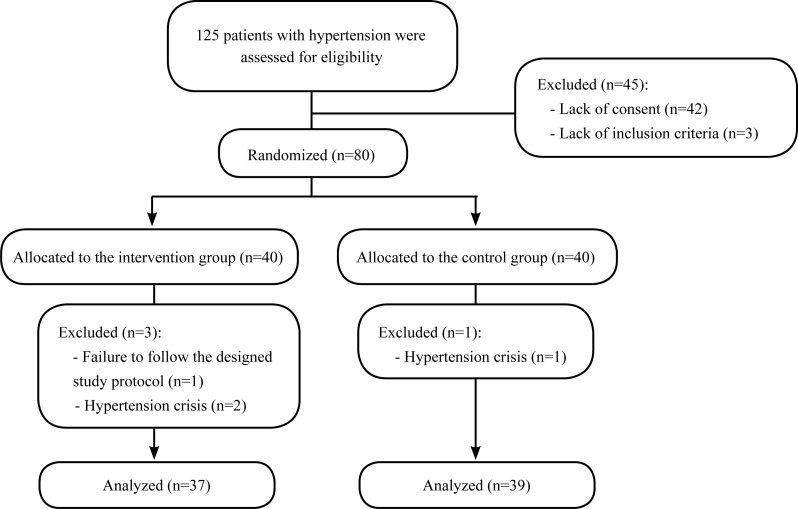
The present study enrolled 80 patients and randomly allocated them to 2 groups of 40 patients. One patient in the control group and 3 patients in the intervention group were excluded due to failure to follow the designed study protocol and hypertension crisis. The CONSORT flow diagram of the study is illustrated in Figure 1.
Figure 1.
The image depicts the CONSORT flow diagram.
The mean age was 48.67±1.42 years in the intervention group and 49.32±2.31 years in the control groups (P=0.343). No significant differences were detected between the 2 groups regarding marital status, education level, and occupation (P>0.05 for all items). These results are summarized in Table 1. No significant differences were observed between the 2 groups concerning antihypertensive drug use, and none of the patients received any treatment for psychological issues.
Table 1.
Comparison of the baseline characteristics between the intervention and control groups
| Variables | Intervention (n=37) | Control (n=39) | P* |
|---|---|---|---|
| Marital status (married) | 30 (81.1%) | 34 (87.2%) | 0.513 |
| Educational level (literate) | 29 (78.4%) | 33 (84.6%) | 0.321 |
| Occupation (unemployed) | 36 (97.3%) | 36 (94.7%) | 0.546 |
Using the χ2 test
The mean systolic and diastolic blood pressures at baseline were not significantly different between the groups (P=0.373) (Table 2). After the intervention, the mean systolic and diastolic blood pressures dropped significantly in the intervention group compared with the baseline and the control group (P<0.001). These results are presented in Table 3.
Table 2.
Comparison of pre-intervention blood pressure, quality of life, and mental health between the intervention and control groups*
| Intervention (n=37) | Control (n=39) | P** | |
|---|---|---|---|
| Systolic blood pressure | 142.82±11.01 | 140.18±14.27 | 0.373 |
| Diastolic blood pressure | 86.12±8.24 | 84.62±9.22 | 0.491 |
| Total quality of life score | 47.22±2.13 | 49.81±2.53 | 0.381 |
| Physical functioning | 61.71±4.12 | 60.80±4.81 | 0.732 |
| Bodily pain | 52.62±3.45 | 63.12±4.55 | 0.024 |
| Role limitations due to physical health | 45.55±6.74 | 53.25±6.03 | 0.483 |
| General health | 50.16±1.66 | 51.01±12.27 | 0.792 |
| Vitality | 38.18±2.98 | 38.90±2.53 | 0.891 |
| Social functioning | 51.39±1.72 | 50.12±1.91 | 0.791 |
| Role limitations due to emotional problems | 48.94±6.60 | 48.77±5.90 | 0.905 |
| Mental health | 43.52±2.89 | 49.01±2.05 | 0.184 |
| Change in health status over the past year | 37.20±3.15 | 40.44±3.88 | 0.502 |
| Stress | 14.1±15.34 | 10.49±5.68 | 0.014 |
| Depression | 13.61±5.66 | 9.67±6.64 | 0.009 |
| Anxiety | 11.14±4 5.89 | 8.81±5.54 | 0.015 |
Data are presented as mean±SD or n (%).
Using the independent t test
Table 3.
Comparison of post-intervention blood pressure, quality of life, and mental health between the intervention and control groups*
| Intervention (n=37) | Control (n=39) | P** | |
|---|---|---|---|
| Systolic blood pressure | 133.7±510.43 | 142.15±10.23 | 0.001 |
| Diastolic blood pressure | 79.15±6.26 | 88.51±8.54 | 0.001 |
| Total quality of life score | 55.99±2.32 | 48.43±2.32 | 0.004 |
| Physical functioning | 77.87±3.00 | 63.45±5.11 | 0.009 |
| Bodily pain | 65.27±3.82 | 62.11±3.90 | 0.534 |
| Role limitations due to physical health | 56.24±6.01 | 40.33±6.23 | 0.071 |
| General health | 52.11±1.73 | 48.48±1.82 | 0.562 |
| Vitality | 39.52±2.62 | 37.85±2.13 | 0.672 |
| Social functioning | 48.65±1.67 | 50.67±2.74 | 0.518 |
| Role limitations due to emotional problems | 72.59±5.74 | 40.19±6.56 | 0.001 |
| Mental health | 57.11±1.96 | 47.68±1.94 | 0.001 |
| Change in health status over the past year | 51.04±3.74 | 40.66±3.68 | 0.021 |
| Stress | 9.15±5.87 | 11.45±5.72 | 0.124 |
| Depression | 9.44±6.86 | 10.51±5.69 | 0.651 |
| Anxiety | 7.35±5.41 | 9.23±4.73 | 0.137 |
Data are presented as mean±SD or n (%).
Using the independent t test
The results also demonstrated a significant improvement in different aspects of quality of life in the intervention group (P<0.001). These data are summarized in Table 3 and Table 4.
Table 4.
Comparison of changes in blood pressure, quality of life, and mental health from before to after the intervention time*
| Intervention (n=37) | Control (n=39) | P** | |
|---|---|---|---|
| Systolic blood pressure | −9.11±0.85 | 1.59±0.91 | <0.001 |
| Diastolic blood pressure | −7.22±0.67 | 3.89±0.48 | <0.001 |
| Total quality of life score | 8.92±0.05 | −1.65±0.07 | <0.001 |
| Physical functioning | 16.11±1.52 | 2.22±0.04 | <0.001 |
| Bodily pain | 9.36±0.05 | 1.14±0.023 | 0.321 |
| Role limitations due to physical health | 10.47±1.14 | 12.05±1.22 | 0.194 |
| General health | 2.41±0.001 | −2.32±0.004 | 0.163 |
| Vitality | 1.85±0.20 | −1.01±0.11 | 0.963 |
| Social functioning | −2.27±0.04 | 0.26±0.001 | 0.524 |
| Role limitations due to emotional problems | 24.10±1.22 | −8.36±0.72 | <0.001 |
| Mental health | 13.66±1.24 | −1.75±0.02 | <0.001 |
| Change in health status over the past year | 14.52±1.26 | 0.54±0.002 | 0.055 |
| Stress | −4.76±2.25 | 0.26±0.31 | 0.013 |
| Depression | −4.62±2.11 | 0.14±0.12 | <0.001 |
| Anxiety | −3.85±0.15 | 1.32±0.42 | 0.007 |
Data are presented as mean±SD or n (%).
Using the independent t test
The stress, depression, and anxiety scores in the 2 groups before and after intervention are summarized in Table 2 and Table 3.
Discussion
The present study showed a significant reduction in the mean blood pressure, stress, depression, and anxiety scores, as well as a significant improvement in different aspects of quality of life in patients who received MBSR.
Abbott et al21 performed a systematic review and meta-analysis on the effectiveness of MBSR and mindfulness-based cognitive therapy in patients with cardiovascular disease. They reviewed 9 articles from 8 original randomized controlled trials including 578 patients and reported that mindfulness could lead to decreased stress levels in patients. Nevertheless, they also mentioned that the effects of mindfulness on blood pressure were not yet established. Another study conducted by Hughes et al22 in 2014 on 56 patients diagnosed with unmedicated blood pressure in the prehypertensive range showed that 8 weeks of the MBSR program led to a significant reduction in the mean systolic and diastolic pressures. Niazi et al23 concluded that mindfulness training could improve the condition of patients suffering from chronic illnesses, especially cardiovascular disease, and help them cope with various clinical problems. These data are in line with our findings. It can be argued that mindfulness practices affect biological, psychosocial, and spiritual features of life. On the other hand, mindfulness practices can improve patients’ skills to tolerate negative emotional states by emotion regulation. This could result in an improvement in the quality of life.
Consistent with our results, Márquez et al24 concluded that mindfulness meditation alleviated stress and blood pressure. A reduction in stress, anxiety, and hypertension in patients could lead to enhanced quality of life, chiming in with several studies that encourage physicians to increase patients’ quality of life by using mindfulness meditation.25–27
The salient aspect of the current study is that our evaluation of the effects of MBSR on blood pressure, quality of life, stress, depression, and anxiety in patients confirms the ability of mindfulness training to influence the different aspects of health concurrently.
Paradoxical reports also exist regarding the effectiveness of mindfulness. Blom et al28 evaluated the effects of an 8-week MBSR program on stress and hypertension among 101 adults with untreated Stage I hypertension. They measured the ambulatory blood pressure of the patients and showed the inability of the program to reduce it. Sangprasert et al29 in 2019 evaluated the effects of mindfulness-based health education practice on different aspects of life among patients with hypertension and reported that mindfulness training could increase the quality of life and lessen hypertension; still, they observed no evidence of a blood pressure reduction in adults. We assume that these inconsistencies could be due to differences in the studied populations.
A systematic review and meta-analysis was conducted by Conversano et al30 in 2021. Based on their data, lowering the stage of hypertension and controlling the situation could significantly increase the effectiveness of mindfulness training, but altogether, the training sessions could reduce blood pressure.
In the current study, we observed a significant increase in diastolic blood pressure in the control group after the intervention. (The rise in systolic blood pressure was not statistically significant.) The finding could be justified based on the seasonal effects on blood pressure. Our study began in the early fall and ended in the winter. Many studies on the relationship between seasons and blood pressure have shown higher blood pressure in winter than in summer.31,32
The present study had some limitations. First, the participants were not blind to the assigned group due to the educational nature of the intervention. Second, men and highly educated women were not included in the study due to low referral to the health center, which could affect the generalizability of the results. Third, financial constraints precluded the use of Holter monitoring, and blood pressure was measured only at the beginning and end of the study, while blood pressure can fluctuate at different times of the day. Therefore, we suggest that future investigations replicate this study with samples consisting of both sexes, assess blood pressure with more reliable instruments, and compare MBSR with other gold-standard therapies, instead of routine care.
Conclusion
A 12-week MBSR program resulted in a significant reduction in mean blood pressure and improvements in different aspects of quality of life and mental health. Health care providers could use the results of this study regarding MBSR to furnish hypertensive patients with better care.
Acknowledgments
We hereby appreciate the assistance of all the participants in this study and all the staff members of Imam Ali Health Care Center. This study was approved and supported by Isfahan University of Medical Sciences, Isfahan, Iran.
Notes:
This paper should be cited as: Babak A, Motamedi N, Mousavi SZ, Ghasemi Darestani N. Effects of Mindfulness-Based Stress Reduction on Blood Pressure, Mental Health, and Quality of Life in Hypertensive Adult Women: A Randomized Clinical Trial Study. J Teh Univ Heart Ctr 2022;17(3):127-133.
References
- 1. Baharvand-Ahmadi B, Asadi-Samani M. A mini-review on the most important effective medicinal plants to treat hypertension in ethnobotanical evidence of Iran. J Nephropharmacol 2016; 6: 3– 8. [PMC free article] [PubMed] [Google Scholar]
- 2. Mirzaei M, Moayedallaie S, Jabbari L, Mohammadi M. Prevalence of Hypertension in Iran 1980–2012: A Systematic Review. J Tehran Heart Cent 2016; 11: 159– 167. [PMC free article] [PubMed] [Google Scholar]
- 3. Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, Harris KC, Nakhla M, Cloutier L, Gelfer M, Lamarre-Cliche M, Milot A, Bolli P, Tremblay G, McLean D, Padwal RS, Tran KC, Grover S, Rabkin SW, Moe GW, Howlett JG, Lindsay P, Hill MD, Sharma M, Field T, Wein TH, Shoamanesh A, Dresser GK, Hamet P, Herman RJ, Burgess E, Gryn SE, Grégoire JC, Lewanczuk R, Poirier L, Campbell TS, Feldman RD, Lavoie KL, Tsuyuki RT, Honos G, Prebtani APH, Kline G, Schiffrin EL, Don-Wauchope A, Tobe SW, Gilbert RE, Leiter LA, Jones C, Woo V, Hegele RA, Selby P, Pipe A, McFarlane PA, Oh P, Gupta M, Bacon SL, Kaczorowski J, Trudeau L, Campbell NRC, Hiremath S, Roerecke M, Arcand J, Ruzicka M, Prasad GVR, Vallée M, Edwards C, Sivapalan P, Penner SB, Fournier A, Benoit G, Feber J, Dionne J, Magee LA, Logan AG, Côté AM, Rey E, Firoz T, Kuyper LM, Gabor JY, Townsend RR, Rabi DM, Daskalopoulou SS, Hypertension Canada . Hypertension Canada's 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children. Can J Cardiol 2018; 34: 506– 525. [DOI] [PubMed] [Google Scholar]
- 4. Trevisol DJ, Moreira LB, Kerkhoff A, Fuchs SC, Fuchs FD. Health-related quality of life and hypertension: a systematic review and meta-analysis of observational studies. J Hypertens 2011; 29: 179– 188. [DOI] [PubMed] [Google Scholar]
- 5. Carvalho MV, Siqueira LB, Sousa AL, Jardim PC. The influence of hypertension on quality of life. Arq Bras Cardiol 2013; 100: 164– 174. [DOI] [PubMed] [Google Scholar]
- 6. Turner-McGrievy G, Davidson CR, Billings DL. Dietary intake, eating behaviors, and quality of life in women with polycystic ovary syndrome who are trying to conceive. Hum Fertil (Camb) 2015; 18: 16– 21. [DOI] [PubMed] [Google Scholar]
- 7. Ha NT, Duy HT, Le NH, Khanal V, Moorin R. Quality of life among people living with hypertension in a rural Vietnam community. BMC Public Health 2014; 14: 833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zadeh AR, Eghbal AF, Mirghazanfari SM, Ghasemzadeh MR, Nassireslami E, Donyavi V. Nigella sativa extract in the treatment of depression and serum Brain-Derived Neurotrophic Factor (BDNF) levels. J Res Med Sci 2022; 27: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wen J, Shi YK, Li YP, Yuan P, Wang F. Quality of life, physical diseases, and psychological impairment among survivors 3 years after Wenchuan earthquake: a population based survey. PLoS One 2012; 7: e43081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Keller A, Litzelman K, Wisk LE, Maddox T, Cheng ER, Creswell PD, Witt WP. Does the perception that stress affects health matter? The association with health and mortality. Health Psychol 2012; 31: 677– 684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016; 3: 171– 178. [DOI] [PubMed] [Google Scholar]
- 12. Creswell JD. Mindfulness Interventions. Annu Rev Psychol 2017; 68: 491– 516. [DOI] [PubMed] [Google Scholar]
- 13. Lu H, Song Y, Xu M, Wang X, Li X, Liu J. The brain structure correlates of individual differences in trait mindfulness: a voxel-based morphometry study. Neuroscience 2014; 272: 21– 28. [DOI] [PubMed] [Google Scholar]
- 14. Engen HG, Bernhardt BC, Skottnik L, Ricard M, Singer T. Structural changes in socio-affective networks: Multi-modal MRI findings in long-term meditation practitioners. Neuropsychologia 2018; 116( Pt A): 26– 33. [DOI] [PubMed] [Google Scholar]
- 15. Addington EL, Javandel S, De Gruttola V, Paul R, Milanini B, Ances BM, Moskowitz JT, Valcour V. Mindfulness-based stress reduction for HIV-associated neurocognitive disorder: Rationale and protocol for a randomized controlled trial in older adults. Contemp Clin Trials 2020; 98: 106150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Campbell TS, Labelle LE, Bacon SL, Faris P, Carlson LE. Impact of Mindfulness-Based Stress Reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer: a waitlist-controlled study. J Behav Med 2012; 35: 262– 271. [DOI] [PubMed] [Google Scholar]
- 17. Palta P, Page G, Piferi RL, Gill JM, Hayat MJ, Connolly AB, Szanton SL. Evaluation of a mindfulness-based intervention program to decrease blood pressure in low-income African-American older adults. J Urban Health 2012; 89: 308– 316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sangsefidi ZS, Mirzaei M, Hosseinzadeh M. The relation between dietary intakes and psychological disorders in Iranian adults: a population-based study. BMC Psychiatry 2020; 20: 257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peipert JD, Bentler PM, Klicko K, Hays RD. Psychometric Properties of the Kidney Disease Quality of Life 36-Item Short-Form Survey (KDQOL-36) in the United States. Am J Kidney Dis 2018; 71: 461– 468. [DOI] [PubMed] [Google Scholar]
- 20. Motamed N, Ayatollahi AR, Zare N, Sadeghi-Hassanabadi A. Validity and reliability of the Persian translation of the SF-36 version 2 questionnaire. East Mediterr Health J 2005; 11: 349– 357. [PubMed] [Google Scholar]
- 21. Abbott RA, Whear R, Rodgers LR, Bethel A, Thompson Coon J, Kuyken W, Stein K, Dickens C. Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. J Psychosom Res 2014; 76: 341– 351. [DOI] [PubMed] [Google Scholar]
- 22. Hughes JW, Fresco DM, Myerscough R, van Dulmen MH, Carlson LE, Josephson R. Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosom Med 2013; 75: 721– 728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Niazi AK, Niazi SK. Mindfulness-based stress reduction: a nonpharmacological approach for chronic illnesses. N Am J Med Sci 2011; 3: 20– 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ponte Márquez PH, Feliu-Soler A, Solé-Villa MJ, Matas-Pericas L, Filella-Agullo D, Ruiz-Herrerias M, Soler-Ribaudi J, Roca-Cusachs Coll A, Arroyo-Díaz JA. Benefits of mindfulness meditation in reducing blood pressure and stress in patients with arterial hypertension. J Hum Hypertens 2019; 33: 237– 247. [DOI] [PubMed] [Google Scholar]
- 25. Thiermann UB, Sheate WR, Vercammen A. Practice Matters: Pro-environmental Motivations and Diet-Related Impact Vary With Meditation Experience. Front Psychol 2020; 11: 584353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nyklícek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med 2008; 35: 331– 340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fortney L, Luchterhand C, Zakletskaia L, Zgierska A, Rakel D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: a pilot study. Ann Fam Med 2013; 11: 412– 420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Blom K, Baker B, How M, Dai M, Irvine J, Abbey S, Abramson BL, Myers MG, Kiss A, Perkins NJ, Tobe SW. Hypertension analysis of stress reduction using mindfulness meditation and yoga: results from the HARMONY randomized controlled trial. Am J Hypertens 2014; 27: 122– 129. [DOI] [PubMed] [Google Scholar]
- 29. Hofmann SG, Gómez AF. Mindfulness-Based Interventions for Anxiety and Depression. Psychiatr Clin North Am 2017; 40: 739– 749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Conversano C, Orrù G, Pozza A, Miccoli M, Ciacchini R, Marchi L, Gemignani A. Is Mindfulness-Based Stress Reduction Effective for People with Hypertension? A Systematic Review and Meta-Analysis of 30 Years of Evidence. Int J Environ Res Public Health 2021; 18: 2882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Modesti PA, Morabito M, Massetti L, Rapi S, Orlandini S, Mancia G, Gensini GF, Parati G. Seasonal blood pressure changes: an independent relationship with temperature and daylight hours. Hypertension 2013; 61: 908– 914. [DOI] [PubMed] [Google Scholar]
- 32. Stergiou GS, Palatini P, Modesti PA, Asayama K, Asmar R, Bilo G, de la Sierra A, Dolan E, Head G, Kario K, Kollias A, Manios E, Mihailidou AS, Myers M, Niiranen T, Ohkubo T, Protogerou A, Wang J, O'Brien E, Parati G. Seasonal variation in blood pressure: Evidence, consensus and recommendations for clinical practice. Consensus statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens 2020; 38: 1235– 1243. [DOI] [PubMed] [Google Scholar]