Dear Editor,
SARS-CoV-2 predisposes patients to thrombotic disease due to excessive inflammation, platelet activation, endothelial dysfunction, and stasis [1]. The infection was recognized as an independent risk factor for acute myocardial infarction (AMI), which is considered part of the clinical picture of the COVID-19 disease [2]. Cardiovascular disease increases both the susceptibility to SARS-COV-2 and the risk of death in patients with COVID-19 [3]. Among those who died and were COVID PCR-positive, almost one-third (30%) suffered from ischemic heart disease [4].
Viral infections in general and SARS-Cov-2, even more so, increase the risk of atherosclerotic plaque destabilization and atherothrombosis [2,3]. The most significant reduction in the risk of cardiovascular events associated with influenza vaccinations was observed in patients post-MI, with an average reduction in the risk of subsequent MI by two-thirds and a decrease in the risk of cardiovascular death of more than a half [5].
Behavior changes, conditioned by fear of contact with health care facilities, led to patients neglecting care and treatment of diseases other than COVID-19 [6]. At the same time, the burden posed by the pandemic, in terms of increased numbers of patients, had the power to paralyze medical services, thus fundamentally affecting the overall functionality and availability of healthcare. There was an across-the-board decline in the utilization of in-person patient care [7]. In the Czech Republic, a significant decrease in hospital admissions for AMI was documented with an incidence ratio of 0.949 (0.911;0.989) for acute STEMI and 0.949 (0.911;0.989) for NSTEMI [8].
The changes caused by the COVID-19 pandemic led to the presumption of a higher incidence of cardiogenic shock complicating acute myocardial infarction. The presumption was primarily based on the higher risk of (repeated) atherothrombotic events in consequence to the infection- and pandemic-related stress, longer time to search- and impaired availability of health care, including reperfusion therapy, which plays a strategic role in patient prognosis. This study aimed to assess the impact of the COVID-19 pandemic on the incidence and prognosis of acute myocardial infarction complicated by cardiogenic shock (CS-AMI).
The analysis is based on data from the National Registry of Cardiovascular Surgery and Interventions (NRCSI) in the Czech Republic combined with data from other registries of the National Health Information System (NHIS), namely the registry of deaths for mortality analysis and the Information System of Infectious Diseases (ISID) for COVID-19 data. NHIS data were collected by the Institute of Health Information and Statistics in the Czech Republic and provide data on the health status of the population, and on activities of healthcare providers. Data in the ISID are collected in compliance with Act No. 258/2000 Coll. on Protection of Public Health, and data in the NHIS are collected under Act No. 372/2011 Coll., on Health Services and Conditions of Their Provision. Due to this legal mandate, the retrospective analyses did not require either approval by an ethics committee or informed consent from participants.
Standard descriptive statistics were applied in the analysis; absolute and relative frequencies for categorical variables and means supplemented with standard deviations or medians supplemented with IQR for continuous variables. Statistical significance of differences among groups of patients was computed using the Fisher exact test for categorical variables, and odds ratios supplemented with 95% confidence intervals were adopted to describe changes in risk events occurring between the studied periods. Linear regression was used for the prediction of the expected number of CS-STEMI. The level of statistical significance was set at 0.05 in all analyses. Statistical computations were done using SPSS 27.0.0.0. (IBM Corporation 2022).
From 1/2016 to 12/2020, 50,745 AMI patients were included in the NRCSI all-comers registry, and 2822 (5.6%) were complicated by CS.
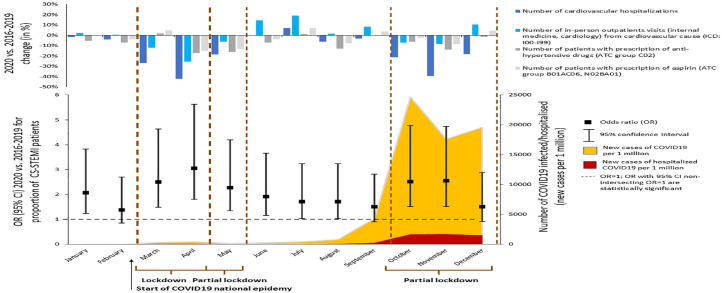
The mean incidence of CS-AMI was significantly higher during the COVID period (2020) than the incidence from 2016 to 2019 (6% vs. 5.5%, p = 0.032, odds ratio (OR) for CS-AMI in 2020 was 1.118 (95% C.I. 1.019; 1.227)). The difference was caused by significant increase in acute STEMI complicated by CS (8.7% vs. 7.6%, p = 0.011, OR for CS-STEMI in 2020 was 1.166 (1.039; 1.309)); it was 7.1% in 2016, 7.8% (2017), 7.6% (2018), 7.8% (2019), and 8.7% (2020). NSTEMI complicated by CS was 2.3% (2016), 2.7% (2017), 2.7% (2018), 2.8% (2019), and 2.8% (2020). The observed rise in the incidence of CS-STEMI during each month of the pandemic (compared to the average incidence in non-pandemic years) correlated with national lockdowns and the substantial increase in the number of COVID infected/hospitalized patients (Fig. 1 ).
Fig. 1.
The COVID-19 and the occurrence of cardiogenic shock (CS) complicating acute myocardial infarction (AMI).
- The upper part of the figure: The number of hospitalizations for cardiovascular diseases; in-person outpatient visits to cardiologists or internal medicine specialists, patients with prescriptions for anti- hypertensive drugs and aspirin (with a cardiovascular indication), in relation to lockdowns and the number of COVID-19 infected/hospitalized patients
- The lower part of the figure: Impact of national lockdowns and numbers of COVID-19 infected/hospitalized patients as it relates to the risk of CS-STEMI.
A significant prolongation in time delay to reperfusion (from the onset of symptoms to balloon/reperfusion) was only observed in October 2020, compared to non-COVID Octobers in 2016–2019. October 2020 saw (1) a peak in the national epidemic with the highest growth of infected and hospitalized patients and (2) a partial lockdown (Fig. 1). During the partial lockdown (October–December), measures affecting schools, shopping malls, and restaurants were in place (starting on October 5, 2020). However, no complete lockdown was implemented, and most measures ended before Christmas. In other months of the COVID year, no significant changes in the onset of symptoms to reperfusion time were observed in CS-STEMI patients.
Except for a less frequent history of previous PCI (13.9% vs. 8.2%, p<0.001), we found no significant differences in CS-STEMI patient characteristics in 2016–2019 vs. 2020; men 72.7% vs. 75.4%, mean age (SD) 66.3 (12.3) years vs. 66.3 (12.2) years, diabetes 20.9% vs. 19.1%, chronic kidney disease 5.4% vs. 5.7%, previous CABG 4.5 vs. 4.2%, left main disease 14.3% vs. 16%, one vessel disease 24.9% vs. 32.1%, pre-PCI TIMI flow 0 64.4% vs. 66.2%, and post- PCI TIMI flow 3 76.7% vs. 76.9%. PCR positivity for COVID-19 infection within 30 days before hospitalization for CS-AMI was confirmed in 3.6% (21) of patients.
The COVID pandemic did not influence the proportions of pre-hospital resuscitated CS-AMI patients (57.5% vs. 58.7%, p = 0.6) nor the number of patients on mechanical ventilation (67.8% vs. 68.3%, p = 0.8).
CS-AMI 30-day mortality was 53.7% in 2016, 51.6% (2017), 49.7% (2018), 49.3% (2019), and 47.9% (2020). For CS-STEMI it was 50.8%, 47.1%, 46.4%, 44.1%, and 45.3%, respectively (P for 2019 vs. 2020 = 0.8). Odds ratios for 30-day mortality in 2020 vs. 2016–2019 was 0.929 (0.738; 1.170), p = 0.534 for CS-AMI and 0.915 (0.541; 1.548), p = 0.740 for CS-STEMI.
During the national COVID epidemic, there was a meaningful decline in the number of hospitalizations for cardiovascular diseases (an absolute reduction of 4.606 per million population above 18 years), in-person outpatient visits to cardiologists or internal medicine specialists (fell by 5.207 per million population above 18 years), and prescription medications to prevent the risk of major cardiovascular events (anti-hypertensives fell by 2.549 and aspirin (for cardiovascular reasons) fell by 4.261 per million population above 18 years) (Fig. 1). This was especially true during lockdown periods, where the absolute reductions in the mentioned cardiovascular care parameters were −27.8%, −8.7%, −8.4%, and −5%, respectively.
Cardiogenic shock is the leading cause of death in AMI. Therefore, analyzing its incidence is essential to identifying preventable factors that diminish survival probabilities in AMI, which is the leading cause of cardiovascular death worldwide.
Our national all-commers registry data collected over the years showed no impact of the pandemic, across all societal and regulatory levels, on the mortality of patients admitted to hospital with STEMI complicated by CS. We found no differences in patient cardiovascular risk profiles, time to reperfusion, angiographic findings, and procedural results. We also failed to observe a significant increase in prehospital resuscitations.
We found a significant decline in the number of patients receiving in-hospital and out-of- hospital cardiovascular care and the number of patients taking prescription medication to prevent major cardiovascular events, i.e., hypertensives and aspirin (Fig. 1). We noted that adherence to outpatient care, lifestyle recommendations, and drug treatment was severely compromised during the pandemic [7]. Cardiovascular pharmacotherapy was linked to both greater susceptibility to coronavirus infection and higher mortalities after infection [9]. This appeared to be the case because patients with cardiovascular disease were more vulnerable to both these aspects [3,4]. Although randomized trials have not confirmed a relationship between drugs that interfere with neurohumoral regulation of the renin-angiotensin-aldosterone system [9] and antithrombotic agents [10]; however, alarming messages in media [11] led patients to distrust these medications and ultimately affected adherence.
The availability of comprehensive health care information makes it possible to present a detailed analysis of the incidence of CS-AIM during the COVID-19 pandemic [8]. We were able to document an increase in the proportion of patients admitted to hospitals with STEMI complicated by CS in 2020, the year of the COVID pandemic. The rise in CS correlated with lockdown periods and increases in the number of people infected. Considering the presented results, we concluded that the pandemic substantially impacted the availability of health care and patient treatment adherence. We found no evidence that the survival of those admitted to the hospital was affected by the specific and unusual circumstances created by the COVID-19 pandemic.
What are the implications of our findings? There is an essential need to prevent an unjustified violation of the patient's trust in treatment and thus their adherence to evidence-based recommendations, especially those impacting survival. In periods of social isolation, should mass and social media, with their power and close cooperation with cardiovascular care experts, take responsibility for building confidence in the health care system. Furthermore, it is also imperative for informing the public about the dangers and consequences of misinformation.
Funding
The work was supported by the Ministry of Health of the Czech Republic, Grant No. NV19- 02–00086. All rights reserved. The work was further supported by the project National Institute for Research of Metabolic and Cardiovascular Diseases (Program EXCELES, ID Project No. LX22NPO5104) - Funded by the European Union – Next Generation EU, and by the Charles University Research Program COOPERATIO – Cardiovascular Science.
Conflict of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that can influence the work reported in this paper.
Acknowledgments
Data availability statement
Anonymized data are available on request from the Institute of Health Information and Statistics of the Czech Republic (IHIS).
Acknowledgment
The authors of the present work express respect and acknowledge the work of all colleagues who contributed to the creation of the registries. It is necessary to acknowledge the efforts of the Institute of Health Information and Statistics of the Czech Republic for the development of national information systems enabling the analysis of quality data.
References
- 1.Bonaventura A., Vecchié A., Dagna L., Martinod K., Dixon D.L., Van Tassell B.W., et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol. 2021;21:319–329. doi: 10.1038/s41577-021-00536-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katsoularis I., Fonseca-Rodríguez O., Farrington P., Lindmark K., Connolly A.M. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study. Lancet. 2021;398:599–607. doi: 10.1016/S0140-6736(21)00896-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E., et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Card. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323:1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 5.Behrouzi B., Bhatt D.L., Cannon C.P., Vardeny O., Lee D.S., Solomon S.D., et al. Association of influenza vaccination with cardiovascular risk: a meta-analysis. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.8873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pedrosa A.L., Bitencourt L., Fróes A.C.F., Cazumbá M.L.B., Campos R.G.B., de Brito S.B.C.S., et al. Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.566212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cransac-Miet A., Zeller M., Chagué F., Faure A.S., Bichat F., Danchin N., et al. Impact of COVID-19 lockdown on lifestyle adherence in stay-at-home patients with chronic coronary syndromes: towards a time bomb. Int J Cardiol. 2021;323:285–287. doi: 10.1016/j.ijcard.2020.08.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Motovska Z.J., Jarkovsky J., Hlinomaz O., Kala P., Hromadka M., Mrozek J., et al. Impact of COVID-19 pandemic on the incidences of hospitalizations for acute myocardial infarction and out-of-hospital cardiac death. a nation-level analysis. Circulation. 2022;146(Suppl_1):A12101. [Google Scholar]
- 9.Savoia C., Volpe M., Kreutz R. Hypertension, a moving Target in COVID-19: current views and perspectives. Circ Res. 2021;128:1062–1079. doi: 10.1161/CIRCRESAHA.121.318054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santi R.L., Márquez M.F., Piskorz D., Saldarriaga C., Lorenzatti A., Wyss F., et al. Ambulatory patients with cardiometabolic disease and without evidence of COVID-19 during the pandemic. The CorCOVID latam study. Glob heart. 2021;16(1):15. doi: 10.5334/gh.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nelson D.J. Health Care & Pharma; 2020. Blood-pressure drugs are in the crosshairs of COVID-19 research.https://www.reuters.com/article/us-health-conoravirus-blood-pressure-ins-idUSKCN2251GQ Available from: (Accessed March 2023) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data are available on request from the Institute of Health Information and Statistics of the Czech Republic (IHIS).