Cigarette smoking is the leading preventable cause of cancer worldwide and associated with substantial morbidity. Here, we chronicle how the relationship between smoking and the development of bladder cancer came to be understood. We describe the evidence that established the causal effect of smoking cigarettes on bladder cancer and highlight the scientists involved in these discoveries. Using Surgeon General’s Reports, from the mid-1900’s to 2020, we provide a historical narrative of the discovery of the link between cigarette smoking and bladder cancer.
THE RISE OF CIGARETTES
Mechanization of the cigarette rolling machine coupled with commercial marketing in the late 1800s popularized cigarette smoking. Cigarettes were being made at a rate of 200/min and the annual per capita cigarette consumption increased from 54 cigarettes in 1900 to 4345 cigarettes in 1963.1 This dramatic rise in smoking resulted in a global epidemic of lung cancer, a disease which until then had been rare. The association of tobacco smoking and lung tumors was suspected in the 1890s, and cigarettes were finally recognized as the cause of the lung cancer epidemic in the 1950s. Despite the recognition of lung cancer risks, the link between cigarettes and bladder cancer occurred much slower. There was growing evidence that bladder cancer was linked to the exposure of occupational dyes, but not until the mid-1900s did a link emerge between smoking and bladder cancer and another 40 years until a causal relationship was established.2,3
THE LINK BETWEEN BLADDER CANCER AND SMOKING
ANIMAL EXPERIMENTATION
Animal studies provided initial key evidence to link bladder cancer with smoking (Figure 1). Dr. Angel Roffo of Argentina, founding director of the Instituto de Medicina Experimental para el Estudio y Tratamiento del Cancer established in 1922 in Buenos Aires, was one of the first scientists to publish detailed accounts of animal experiments demonstrating the development of tumors by exposure to tobacco. He treated a large population of cancer patients, from whom he had learned that smoking was linked to a wide scope of cancers. Roffo dedicated his career to studying the effects of tobacco on what he called the “smoking highway” (lips, tongue, throat, cheek, bronchial passages, etc.), and subsequently postulated that smoking could cause bladder cancer (further extending the smoking highway).4 Lars Holsti MD and Pentti Ermala MD, both Finnish physicians, were also among the first to establish a link between smoking tobacco and bladder cancer. To investigate the effect of tobacco tar on tissues of the oral cavity, they swabbed the lips and oral cavities of mice with tobacco tar daily for 140 days and then observed them for 12 months. Instead of finding changes in the oral cavity, the researchers unexpectedly found benign and malignant papillary tumors of the bladder at autopsy.5 Four years later in 1959, a second study by Moore and Dipaolo also found that the application of cigarette smoke condensate to the oral mucosa of mice induced bladder hyperplasia and one mouse developed anaplastic sarcoma.6 These initial mice studies laid the ground work for clinical and epidemiologic studies on smoking and bladder cancer and would be key citations in the landmark 1964 Surgeon’s General’s Report. Unfortunately, Dr. Moore, a surgeon and oncologist who directed Roswell Park from 1952 to 1973, died of bladder cancer in 2008.
Figure 1.
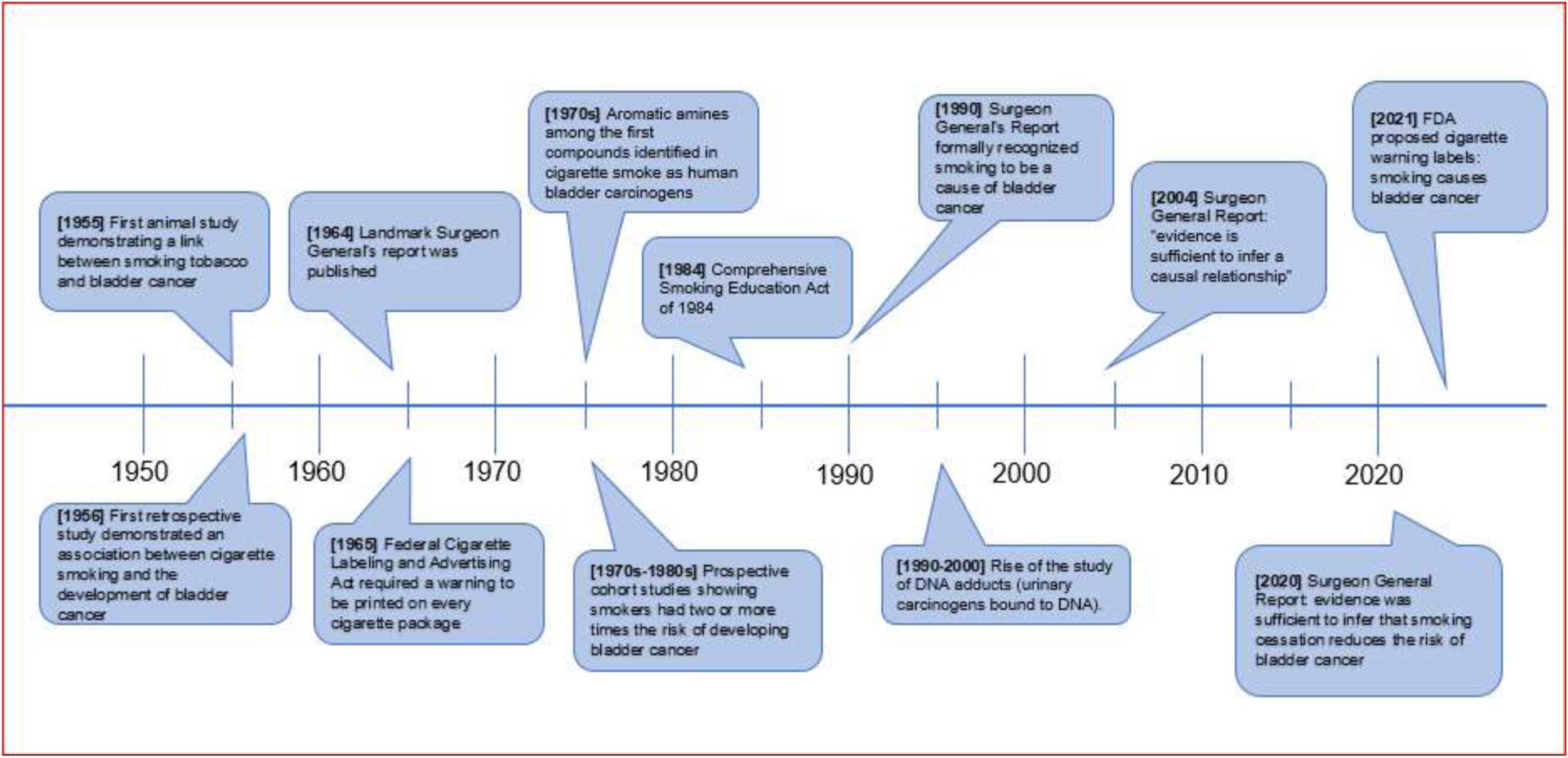
Timeline of evidence supporting the association of smoking and bladder cancer.
POPULATION STUDIES
A second line of evidence came from population human studies which evaluated the association between cigarette use and bladder cancer (Figure 1). The first population study on the link between cigarettes and bladder cancer was published in 1956 by Lilienfeld, Moore and Levin (Figure 1). This retrospective case-control study investigated the history of cigarette smoking in patients with bladder cancer compared to smokers with other malignancies. The authors included 1290 men and 1323 females from 1945–1955, controlling for sex, type of tobacco, residence, socioeconomic status, and smoking duration. They found a significant association between cigarette smoking and the development of bladder cancer among men however they notably concluded “it is clear there is no association of cigarette smoking and bladder cancer in women”.7 The molecular epidemiology driving gender differences in bladder cancer is complex and not until 20 years later was there an understanding that bladder cancer risk may be influenced from the interplay of sex hormones.8 Abraham Lilienfeld, who is considered the “father of contemporary chronic disease epidemiology,” worked along with Moore and Levin at Roswell Park, a key institution in the discovery of the smoking-bladder cancer association.
Following Lilienfeld’s et al. findings, several retrospective and prospective population studies began to lay the groundwork for the first United States Surgeon General’s Report.
SURGEON GENERAL’S REPORT OF 1964 LINKS SMOKING AND BLADDER CANCER
On January 11, 1964, Luther L. Terry, MD, Surgeon General of the United States, released Smoking and Health: Report of the Advisory Committee of the Surgeon General of the Public Health Service. This report was famous for establishing the initial link between cigarette smoking with dangerous health effects including lung cancer and heart disease.9 Dr. Terry, a previous smoker himself until about 3 months prior to the published report, was appointed to the post as the Surgeon General by President John F. Kennedy. At the time of the report, surveys indicated up to half of all physicians smoked, and the Surgeon General advisory committee reflected this culture: half of its 10 members were cigarettes smokers. In the 1964 report, which summarized results from four case–control studies and seven prospective cohort studies, bladder cancer was included as one of the deleterious effects of cigarette smoking. Relative risks (RR) of individual studies of bladder cancer in smokers compared to non-smokers were stratified by sex. Males had a RR of up to 2.9 while 2 studies of females found no relationship with smoking, others found a RR of up to 1.5, and a single outlier showed a RR of 3.9. The Surgeon General’s Report concluded “available data suggest an association between cigarette smoking and urinary bladder cancer in the male but are not sufficient to support a judgment on the causal significance of this association.” Several inconsistent study findings and lack of stratification by tobacco dose and sex of the user precluded causality determination.
CONGRESSIONAL REACTION TO THE 1964 SURGEON GENERAL’S REPORT
Congress reacted to the Surgeon General’s Report by passing multiple acts to decrease cigarette consumption. Senator Warren G. Magnuson (D-WA) introduced the Federal Cigarette Labeling and Advertising Act of 1965 which required the warning “Caution: cigarette smoking may be hazardous to your health” to be printed on all cigarette packages (Figure 2). In 1969, the Public Health Cigarette Smoking Act was passed and signed into law in 1970, which escalated the language required on cigarette packages and read “Warning: the surgeon general has determined that cigarette smoking is dangerous to your health” (Figure 2). On April 1, 1970 President Richard Nixon signed legislation banning cigarette advertisements on television and radio. The last televised cigarette ad ran at 11:50 p.m. during The Johnny Carson Show on January 1, 1971. Subsequent studies have shown that cigarette advertising bans did not have a significant effect of cigarette consumption, however, a widely read article in Reader’s Digest in 1952 titled “Cancer by the Carton,” contributed to the largest drop in cigarette consumption since the Depression.10
Figure 2.
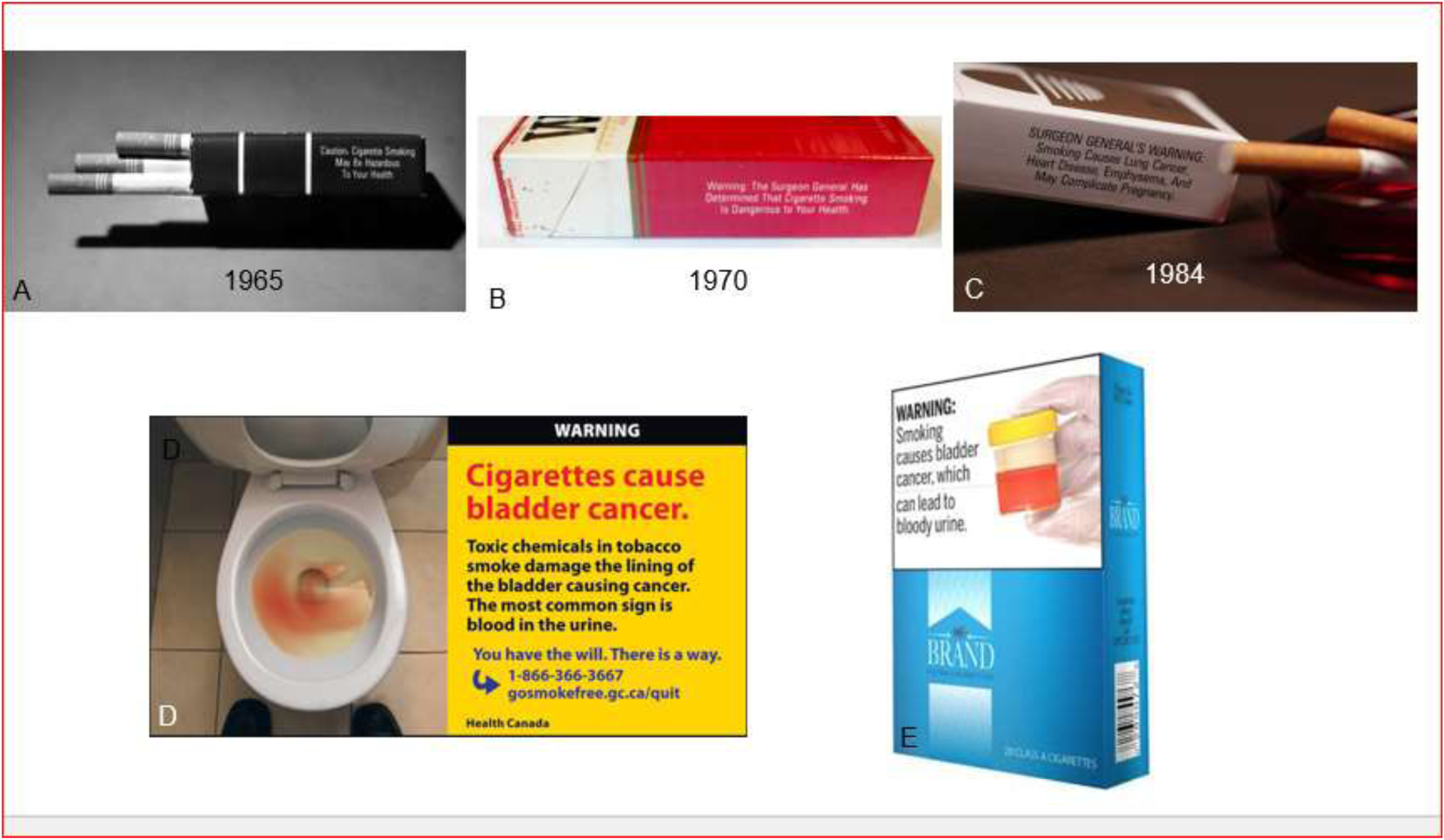
A) Federal Cigarette Labeling and Advertising Act of 1965 which required the warning “Caution: cigarette smoking may be hazardous to your health” to be printed on every cigarette package, B) Public Health Cigarette Smoking Act of 1970 escalated the language required on cigarette packages, which read “Warning: the Surgeon General has determined that cigarette smoking is dangerous to your health”, C) Comprehensive Smoking Education Act of 1984 requiring four specific health warnings on all cigarette packages, D) Canadian Cigarette Package stating smoking causes bladder cancer, E) FDA proposed new warning label on cigarette packaging highlighting smoking causes bladder cancer.
BLADDER CANCER CAUSING CARCINOGENS
After a link between cigarette smoking and bladder cancer had been established in the 1964 Surgeon General’s Report, the biological basis for this relationship was investigated. The next line of evidence linking smoking with bladder cancer was the discovery of carcinogens in the urine of cigarette smokers (Figure 1). Aromatic amines including 4-Aminobiphenyl and 2-naphthylamine were among the first compounds identified in cigarette smoke as human bladder carcinogens.11 In addition to carcinogenic activity of the urine of smokers, the mutagenicity of the urine of smokers was also being investigated. In 1977, Yamasaki and Ames investigated the concentrations of mutagens and carcinogens in the urine of smokers and nonsmokers and found no mutagenic biomarkers in non-smokers, while the urine of all the smokers in their study had significant mutagenic activity.12 To further understand the sex hormone effects of bladder cancer carcinogenesis, male mice, when treated with the carcinogen N-butyl-N-(4-hydroxybutyl) nitrosamine which is similar to the carcinogens in cigarettes smoke, developed bladder on average 63 days earlier than did female mice. These sex difference could be eliminated by castrating the male mice prior to carcinogen treatment, or treating the female mice with testosterone.13 This led to an understanding that gender difference in bladder was associated with effects of sex hormones (particularly androgens and estrogens) and their respective receptors in the urothelium (androgen and estrogen receptors—including a protective effect of ER alpha signaling and a facilitating effect of ER beta signaling). The disparity in bladder cancer incidence has now persisted over many decades of study.
SURGEON GENERAL’S REPORTS OF 1979 AND 1982 CITE SMOKING AS A CONTRIBUTORY FACTOR IN BLADDER CANCER
The toxic effects of smoking on the lungs and oral cavity were in the forefront of epidemiological studies during the next several decades. It was not until the Surgeon General’s Reports of 1979 and 1982, led by Julius B. Richmond, MD a pediatrician and C. Everett Koop, MD a pediatric surgeon respectively, that there was further elucidation on the relationship between cigarette smoking and the development of bladder cancer. Based on 17 case–control and eight prospective cohort studies, the reports concluded that cigarette smoking was a contributory factor in the development of bladder cancer. Compared with nonsmokers, smokers had two or more times the risk of developing or dying from bladder cancer. Moreover, the evolving data illustrated a dose–response relationship which showed that bladder cancer risk increased with more substantial smoking histories. “Cigarette smoking is a contributory factor in the development of bladder cancer …. The term ‘contributory factor’ by no means excludes the possibility of a causal role for smoking”.14
CONGRESSIONAL REACTION TO THE 1979 AND 1982 SURGEON GENERAL’S REPORTS
As a response to the growing body of evidence, Congress enacted the Comprehensive Smoking Education Act of 1984 which was sponsored by Henry Waxman (D-CA). This act required four specific health warnings on all cigarette packages and advertisements which were rotated every 3 months. The warnings did not specifically address bladder cancer but clearly stated the causative relationship with lung cancer: “SURGEON GENERAL’S WARNING: Smoking Causes Lung Cancer, Heart Disease, Emphysema, and May Complicate Pregnancy” (Figure 2).
SURGEON GENERAL REPORT OF 1990: SMOKING CAUSES BLADDER CANCER
“In the 1990 Surgeon General’s Report smoking was formally recognized to be a cause of bladder cancer.15 At the time the surgeon general was Antonia C. Novella, MD, the first woman and first Hispanic to serve as Surgeon General. The report additionally found that smoking cessation could reduce the risk of bladder cancer by 50% after only a few years of cessation, when compared to those who continued to smoke.15 Multiple scientists and studies contributed data demonstrating relative risks with a dose-dependent relationship between smoking development of bladder cancer. Dunn and Weir reported a relative risk of bladder cancer of 2.89 among all smokers and noted a dose-dependent relationship when the data were stratified based on packs smoked per day: a relative risk of 1.52 among those who smoked less than a half pack per day, 2.81 among those who smoked one pack per day and 5.41 among those who smoked more than a pack and a half per day.16 The finding that smoking cessation could reduce the risk of bladder cancer was consistent with the concept that environmental bladder carcinogens that are inhaled or ingested can be modified (activated, inactivated, etc.) by other organs before they are excreted into the urine where they sit for hours while in contact with the urothelium. Opposed to organs along the “smoking highway” that are in direct contact with carcinogens in cigarette smoke where risks decrease rapidly to close to those of “never smokers”, the decline in risk for bladder cancer after quitting smoking is far more gradual and takes many years to reach those of never smokers”.17
MODERN ERA AND THE 2020 SURGEON GENERAL’S REPORT ON SMOKING CESSATION
Towards the end of the 1900s and into the 2000s there were further endeavors to describe the biological basis for a smoking-bladder cancer causal relationship, where the study of DNA adducts, urinary carcinogens bound to DNA, arose. There was evolving evidence to suggest that DNA adducts are risk factors in the development of tobacco related cancers including bladder cancer. Recent studies have shown that nicotine-derived nitrosamine ketone and Benzo[a]pyrenrom in cigarette smoke induce DNA adducts in bladder cancer.18 These basic science studies gave additional support to the 2004 Surgeon General’s Report which cited 30 case–control and 10 cohort studies that strengthened the causal association between cigarette smoking and bladder cancer. The report, under surgeon general Richard Carmona MD, concluded “The evidence is sufficient to infer a causal relationship between smoking and… bladder cancer.”
The Surgeon General’s Report of 2020, under the office of Jerome Adams MD, focused on the health benefits of smoking cessation and quitting strategies. The report concluded “The evidence is sufficient to infer that smoking cessation reduces the risk of bladder cancer. ”19 However, the evidence was insufficient to infer that smoking cessation decreases mortality due to bladder cancer. The report additionally highlighted the rapid growth of e-cigarette use and raised questions about the potential impact that such products could have on disease and death caused by tobacco use.
Multiple public health efforts continued to address the link between bladder cancer and smoking while promoting smoking cessation. Canada introduced pictorial health warning labels on cigarette packages in 2001 and a new set of 16 health warnings were implemented in 2012, including a label that cigarettes cause bladder cancer (Figure 2). Not until 2020 did the US FDA begin requiring new health warnings related to bladder cancer on cigarette packages. In 2021, the FDA planned a set of 11 health warnings accompanied by a photograph to be required on cigarette packages, one of which was a warning that smoking cigarettes can cause bladder cancer (Figure 2).20 As a result of a lawsuit brought forth in Texas, the new warnings have been postponed. A final court ruling is expected in April of 2023.
CONCLUSION
Over the last century, data have evolved from the suggestion of a link between cigarette smoking and bladder cancer, to clear evidence demonstrating causality and the ability to decrease the risk of bladder cancer by smoking cessation. The evidence has influenced public health laws including banning cigarette advertisements on television and the escalation of warnings required on cigarette packages. In spite of these efforts, the delay in definitively recognizing the relationship between smoking and bladder cancer may contribute to less awareness among both physicians and the general public as compared to other smoking-related cancers. Further disseminating knowledge about the urologic risks of tobacco use may help promote cessation and primary prevention.
Footnotes
Conflict of Intrest: No conflict
REFERENCES
- 1.From the Centers for Disease Control and Prevention. Tobacco use--United States, 1900–1999. JAMA. 1999. Dec 15;282(23):2202–4. [PubMed] [Google Scholar]
- 2.Nabavizadeh B, Amend GM, Breyer BN. Workers Died of Dyes: The Discovery of Occupational Bladder Cancers. Urology. 2021. Aug;154:4–7. doi: 10.1016/j.urology.2021.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Freedman ND, Silverman DT, Hollenbeck AR, Schatzkin A, Abnet CC. Association between smoking and risk of bladder cancer among men and women. JAMA. 2011;306(7):737–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Proctor RN. Angel H Roffo: the forgotten father of experimental tobacco carcinogenesis. Bull World Health Organ. 2006;84(6):494–496. doi: 10.2471/blt.06.031682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holsti LR, Ermala P. Papillary carcinoma of the bladder in mice, obtained after peroral administration of tobacco tar. Cancer. 1955;8(4):679–682. doi: [DOI] [PubMed] [Google Scholar]
- 6.Dipaolo Joseph A., Moore George E., Effect on Mice of Oral Painting of Cigarette-Smoke Condensate, JNCI: Journal of the National Cancer Institute, Volume 23, Issue 3, September 1959, Pages 529–534, 10.1093/jnci/23.3.529 [DOI] [PubMed] [Google Scholar]
- 7.Levin ML, Lilienfeld AM, Moore GE. The association of smoking with cancer of the urinary bladder in humans. AMA Arch Intern Med. 1956;98(2):129–135. doi: 10.1001/archinte.1956.00250260001001 [DOI] [PubMed] [Google Scholar]
- 8.Okajima E, Hiramatsu T, Iriya K, Ijuin M, Matsushima S. Effects of sex hormones on development of urinary bladder tumours in rats induced by N-butyl-N-(4-hydroxybutyl) nitrosamine. Urol Res. 1975;3:73–79. [DOI] [PubMed] [Google Scholar]
- 9.Bayne-Jones S. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. US Department of Health, Education, and Welfare, Public Health Service; 1964. [Google Scholar]
- 10.Capella ML, Taylor CR, & Webster C (2008). The effect of cigarette advertising bans on consumption: A meta-analysis. Journal of Advertising, 37(2), 7–18. 10.2753/joa0091-3367370201 [DOI] [Google Scholar]
- 11.Radomski JL, Brill E. Bladder cancer induction by aromatic amines: role of N-hydroxy metabolites. Science. 1970. Feb 13;167(3920):992–3. doi: 10.1126/science.167.3920.992. [DOI] [PubMed] [Google Scholar]
- 12.Yamasaki E, Ames BN. Concentration of mutagens from urine by absorption with the nonpolar resin XAD-2: cigarette smokers have mutagenic urine. Proc Natl Acad Sci U S A. 1977. Aug;74(8):3555–9. doi: 10.1073/pnas.74.8.3555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bertram JS, Craig AW. Specific induction of bladder cancer in mice by butyl-(4-hydroxybutyl)-nitrosamine and the effects of hormonal modifications on the sex difference in response. Eur J Cancer. 1972;8:587–594. [DOI] [PubMed] [Google Scholar]
- 14.Shopland DR The Health Consequences of Smoking: Cancer: A Report of the Surgeon General. US Department of Health, Education, and Welfare, Public Health Service; 1982 [Google Scholar]
- 15.Samet JM. The 1990 report of the surgeon general: the health benefits of smoking cessation. Am Rev Respir Dis. 1990;142(5):993–994. doi: 10.1164/ajrccm/142.5.993 [DOI] [PubMed] [Google Scholar]
- 16.Weir JM, Dunn JE. Smoking and mortality: a prospective study, Cancer, 1970, vol. 25 (pg. 105–12) [DOI] [PubMed] [Google Scholar]
- 17.Welty CJ, Wright JL, Hotaling JM, et al. Persistence of urothelial carcinoma of the bladder risk among former smokers: results from a contemporary, prospective cohort study. Urologic Oncology. 2014. Jan;32(1):25.e21–5. DOI: 10.1016/j.urolonc.2012.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jin F, Thaiparambil J, Donepudi SR, et al. Tobacco-Specific Carcinogens Induce Hypermethylation, DNA Adducts, and DNA Damage in Bladder Cancer. Cancer Prev Res (Phila Pa). 2017;10(10):588–597. doi: 10.1158/1940-6207.CAPR-17-0198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.United States. Public Health Service. Office of the Surgeon General, issuing body. | National Center for Chronic Disease Prevention and Health Promotion (U.S.). Office on Smoking and Health, issuing body. Smoking Cessation: A Report of the Surgeon General. A Report of the Surgeon General. Published online 2020. [Google Scholar]
- 20.Commissioner, O. of the. (2020, March 17). FDA requires new health warnings for cigarette packages and advertisements. U.S. Food and Drug Administration. Retrieved March 31, 2022, from https://www.fda.gov/news-events/press-announcements/fda-requires-new-health-warnings-cigarette-packages-and-advertisements [Google Scholar]


