Abstract
Purpose:
There are few data on the relationship between health literacy and discharge disposition. We hypothesized that patient discharge needs after radical cystectomy are affected by health literacy.
Materials and Methods:
We identified 504 patients who underwent radical cystectomy and completed the validated BHLS (Brief Health Literacy Screen) after November 2010. Bivariate and logistic regression analyses were performed to determine whether health literacy is associated with the use of discharge resources after radical cystectomy.
Results:
Of patients treated with radical cystectomy 50.6% required discharge services and had lower health literacy (BHLS 11.9 vs 12.5, p = 0.016) than patients discharged home without services. On multivariable analysis older age (OR 1.1, 95% CI 1.0–1.1, p = 0.002), female gender (OR 2.3, 95% CI 1.2–4.4, p = 0.019), body mass index (OR 1.1, 95% CI 1.0–1.1, p = 0.034), Charlson comorbidity index score (OR 1.1, 95% CI 1.0–1.2, p = 0.037) and length of stay (OR 1.1, 95% CI 1.0–1.2, p = 0.019) were significantly associated with the use of discharge resources. Patients with continent vs incontinent urinary diversion were less likely to require discharge services (OR 0.4, 95% CI 0.2–0.8, p = 0.013).
Conclusions:
Older age, female gender, body mass index, comorbidities, length of stay and incontinent diversion are associated with increased use of discharge resources after radical cystectomy. Low health literacy may affect patient discharge disposition but it was not significant on multivariable analysis. Factors that influence the complex self-care required of patients after cystectomy should be considered during discharge planning.
Keywords: urinary bladder, cystectomy, self care, health literacy, health resources
Radical cystectomy with bilateral pelvic lymph node dissection remains the standard of care for muscle invasive bladder cancer.1 This complex, costly and time intensive operation can involve substantial morbidity with reported postoperative complication rates as high as 64% in contemporary series.2 In addition to removal of the bladder and pelvic lymph nodes, urinary diversion is required, which is most commonly constructed using a portion of ileum to create an ileal conduit.
This incontinent diversion, which is similar to a colostomy, requires daily management of a stoma and its required supplies, such as a skin barrier device and a collection bag. Most patients undergo detailed teaching by wound, ostomy and continence nurses in the immediate postoperative period to ensure successful long-term care of the stoma.3 Continent urinary diversions, including the orthotopic neobladder and the Indiana pouch, are also available for appropriately selected patients. These diversions necessitate intermittent catheterization for urinary drainage, which requires an understanding of basic urological anatomy and strict catheterization regimens. Regardless of the diversion choice, patients with cystectomy require resource intensive postoperative care and detailed discharge teaching, which includes verbal and written self-care instructions.4
To understand and execute these complex selfcare routines after RC patients must have some degree of health literacy. As defined by IOM (Institute of Medicine) health literacy is the ability to obtain, comprehend and act on medical information.5 Urological surgeons and other health care providers may overestimate patient health literacy, which can impact patient education and contribute to health care disparities.6,7 Additionally, health literacy is an independent predictor of health outcomes in patients with chronic health conditions and lower health literacy is associated with poorer global health status.7–9
While the impact of health literacy on chronic medical conditions and overall health is well studied, there are few data on health literacy and its relationship to the discharge disposition, which is a critical transition point in the postoperative care of patients treated with RC that may be influenced by health literacy. Prior groups have examined factors affecting discharge placement after RC but they did not specifically examine patient health literacy.10
To better understand the discharge needs of patients who underwent RC, we examined the relationship of health literacy and other clinicodemographic factors to discharge disposition. We hypothesized that patients who underwent RC and had low health literacy were more likely to use home health care, a skilled nursing facility or other rehabilitation services in the immediate postoperative period.
MATERIALS AND METHODS
Since November 2010, all patients admitted to our institution have been administered the validated BHLS (fig. 1). This screening tool consists of 3 questions, which are verbally administered by nursing staff and added to the EHR. The questions are 1) “How confident are you filling out medical forms by yourself?” 2) “How often do you have someone help you read hospital materials?” and 3) “How often do you have problems learning about your medical condition because of difficulty understanding written information?”11
Figure 1.
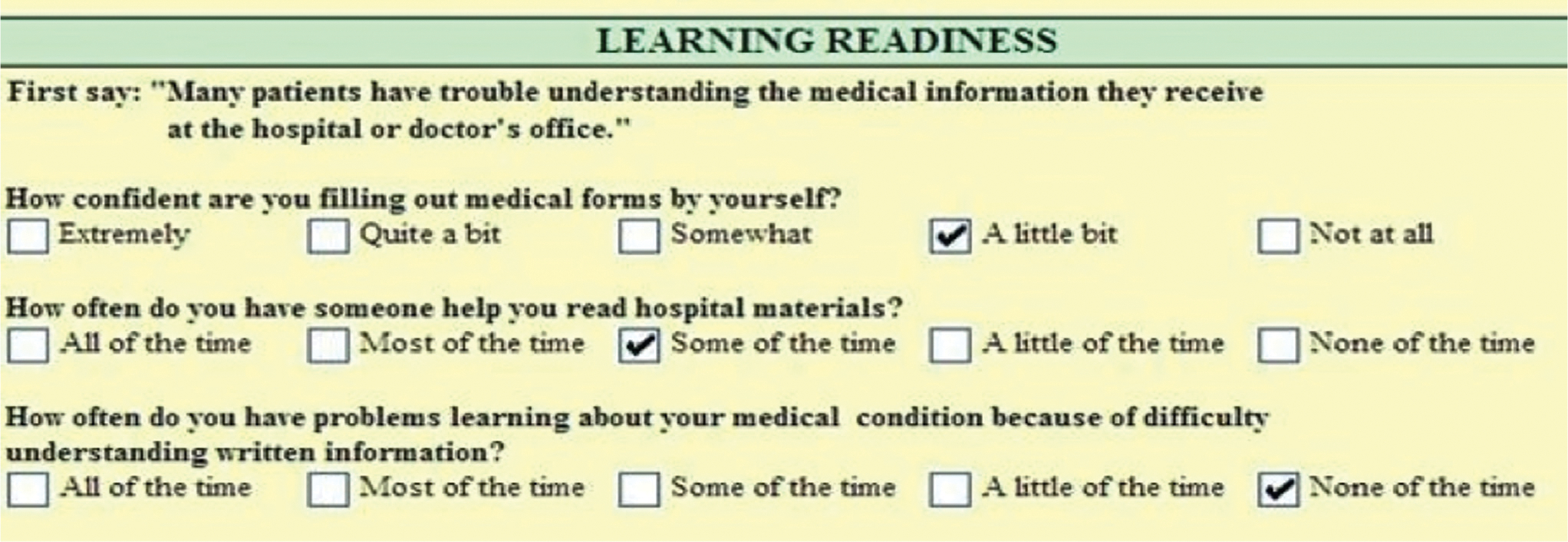
Patient responses are evaluated using a 5-point Likert-type scale with the total score ranging from 3–lowest score to 15–highest score. These questions have been previously shown to correlate with other measures of health literacy, including S-TOFHLA (Short Test of Functional Health Literacy in Adults) and REALM (Rapid Estimate of Adult Literacy in Medicine).12 Because to our knowledge there is no defined threshold delineating adequate or high literacy from inadequate or low literacy, we used the mean health literacy score of all patients in the study population to facilitate relative literacy comparisons between patient groups.
Demographic and clinical characteristics of all RC cases from November 2010 to August 2015 were abstracted by key study personnel from the Vanderbilt University RC database stored in REDCap (Research Electronic Data Capture).13 These data are prospectively maintained by dedicated research staff and can be accessed by key study personnel with appropriate institutional review board training. Health literacy data and educational status were abstracted from EHRs by the health services research core staff according to medical record numbers provided from the REDCap RC database.
In addition to discharge disposition (home, home health care, skilled nursing facility or inpatient rehabilitation), the patient characteristics examined included age, gender, race, educational attainment, marital status, insurance, BMI, preoperative albumin, CCI score and use of neoadjuvant chemotherapy. Furthermore, we analyzed operative details such as an open vs a robot-assisted laparoscopic approach and urinary diversion type (ileal conduit, neobladder or Indiana pouch), length of stay and pathological tumor classification based on the AJCC (American Joint Committee on Cancer), 7th edition.
We first performed bivariate analysis to compare patients who were discharged home without services to those who required discharge services such as home health care, a skilled nursing facility or inpatient rehabilitation. This was done to identify possible associations of demographic and clinical characteristics with the use of discharge resources after RC. We then performed logistic regression analysis adjusted for select clinical and demographic characteristics to determine whether health literacy was associated with the use of discharge resources.
All tests of significance were 2-tailed with p <0.05 considered significant. IBM® SPSS®, version 22.0 was used for statistical analysis. All methods were approved by the Vanderbilt University Medical Center institutional review board.
RESULTS
Health literacy data were available on 504 patients who underwent RC during the study period (table 1). Literacy data were missing on 34 patients (6%). The mean ± SD BHLS score was 12.2 ± 2.9. The patient population was older (mean age 67.1 ± 8.6 years), 95.4% were white and 83.5% were male. The mean education attainment was13.3 ± 3.3 years and more than three-quarters of the patients were married. Patients carried a mix of insurance types, including private in 33.5% and Medicaid/Medicare in 63.3% while 3.2% were uninsured. Patients were overweight (mean BMI 28.6 ± 5.4 kg/m2) with baseline medical comorbidities (mean CCI score 3.7 ± 2.9). Of the patients 70.4% underwent open surgery with an ileal conduit in 82.1% while 29.6% were treated via a robot-assisted laparoscopic approach and 17.9% underwent continent diversion.
Table 1.
Demographics and clinical characteristics by use of discharge services
| Discharge Services |
||||
|---|---|---|---|---|
| Overall | Yes | No | p Value | |
|
| ||||
| No. pts (%) | 504 (100.0) | 255 (50.6) | 249 (49.4) | — |
| Mean ± SD BHLS score | 12.2 ± 2.9 | 11.9 ± 2.9 | 12.5 ± 2.8 | 0.016 |
| Mean ± SD age | 67.1 ± 8.6 | 70.1 ± 8.6 | 64.1 ± 9.6 | <0.001 |
| No. male (%) | 421 (83.5) | 202 (79.2) | 219 (88.0) | 0.008 |
| No. white (%) | 481 (95.4) | 242 (95.7) | 239 (96.0) | 0.681 |
| Mean ± SD education (yrs)* | 13.3 ± 3.3 | 12.9 ± 3.2 | 13.7 ± 3.4 | 0.035 |
| Mean ± SD No. married | 379 ± 76.4 | 180 ± 71.4 | 199 ± 81.6 | 0.008 |
| No. insurance (%): | <0.001 | |||
| Self-pay | 16 (3.2) | 0 | 16 (6.5) | |
| Medicaid/Medicare | 316 (63.3) | 198 (78.3) | 118 (48.0) | |
| Private | 167 (33.5) | 55 (21.7) | 112 (45.5) | |
| Mean ± SD BMI (kg/m2) | 28.6 ± 5.4 | 29.0 ± 5.4 | 28.2 ± 5.4 | 0.118 |
| No. preop albumin (%)† | 4.1 (0.3) | 4.1 (0.3) | 4.1 (0.4) | 0.038 |
| Mean ± SD Charlson comorbidity index | 3.7 ± 2.9 | 4.0 ± 3.0 | 3.4 ± 2.7 | 0.008 |
| No. neoadjuvant chemotherapy (%): | 0.282 | |||
| Yes | 155 (30.8) | 84 (32.9) | 71 (28.5) | |
| No | 349 (69.2) | 171 (67.1) | 178 (71.5) | |
| No. procedure (%): | 0.043 | |||
| Open | 355 (70.4) | 190 (74.5) | 165 (66.3) | |
| Robotic | 149 (29.6) | 65 (25.5) | 84 (33.7) | |
| No. urinary diversion (%): | <0.001 | |||
| Incontinent (ileal conduit) | 414 (82.1) | 237 (93.3) | 177 (71.7) | |
| Continent (neobladder or Indiana pouch) | 90 (17.9) | 18 (6.7) | 72 (28.3) | |
| Mean ± SD length of stay (days) | 6.8 ± 3.0 | 7.3 ± 3.4 | 6.3 ± 2.5 | <0.001 |
| No. pathological stage (%): | 0.631 | |||
| Muscle invasive (pT2 or greater) | 299 (60.4) | 149 (59.4) | 150 (61.5) | |
| Nonmuscle invasive (pT0, pTis, pTa, pT1) | 205 (39.6) | 106 (40.6) | 99 (38.5) | |
Data missing on 85 of 504 patients (16.9%).
Data missing on 137 of 504 patients (27.2%).
Of all patients who underwent RC 50.6% required home health care, a skilled nursing facility or other rehabilitation services at the time of discharge. Compared to patients discharged home without services, those who required discharge services had a lower BHLS score on bivariate analysis (11.9 vs 12.5, p = 0.016). Patients who needed discharge services were older (age 70.1 vs 64.1 years, p <0.001) and more likely to be female (20.8% vs 12.0%, p = 0.008), unmarried (28.6% vs 18.4%, p = 0.008) and less educated (12.9 vs 13.7 years, p = 0.035). Patients who used additional services after discharge were never uninsured and they more commonly had Medicare or Medicaid than private insurance. These patients also had more comorbidities at baseline (mean CCI score 4.0 vs 3.4, p = 0.008), were more likely to undergo ileal conduit urinary diversion (93.3% vs 71.7%, p <0.001) and had a longer length of stay (7.3 vs 6.3 days, p <0.001).
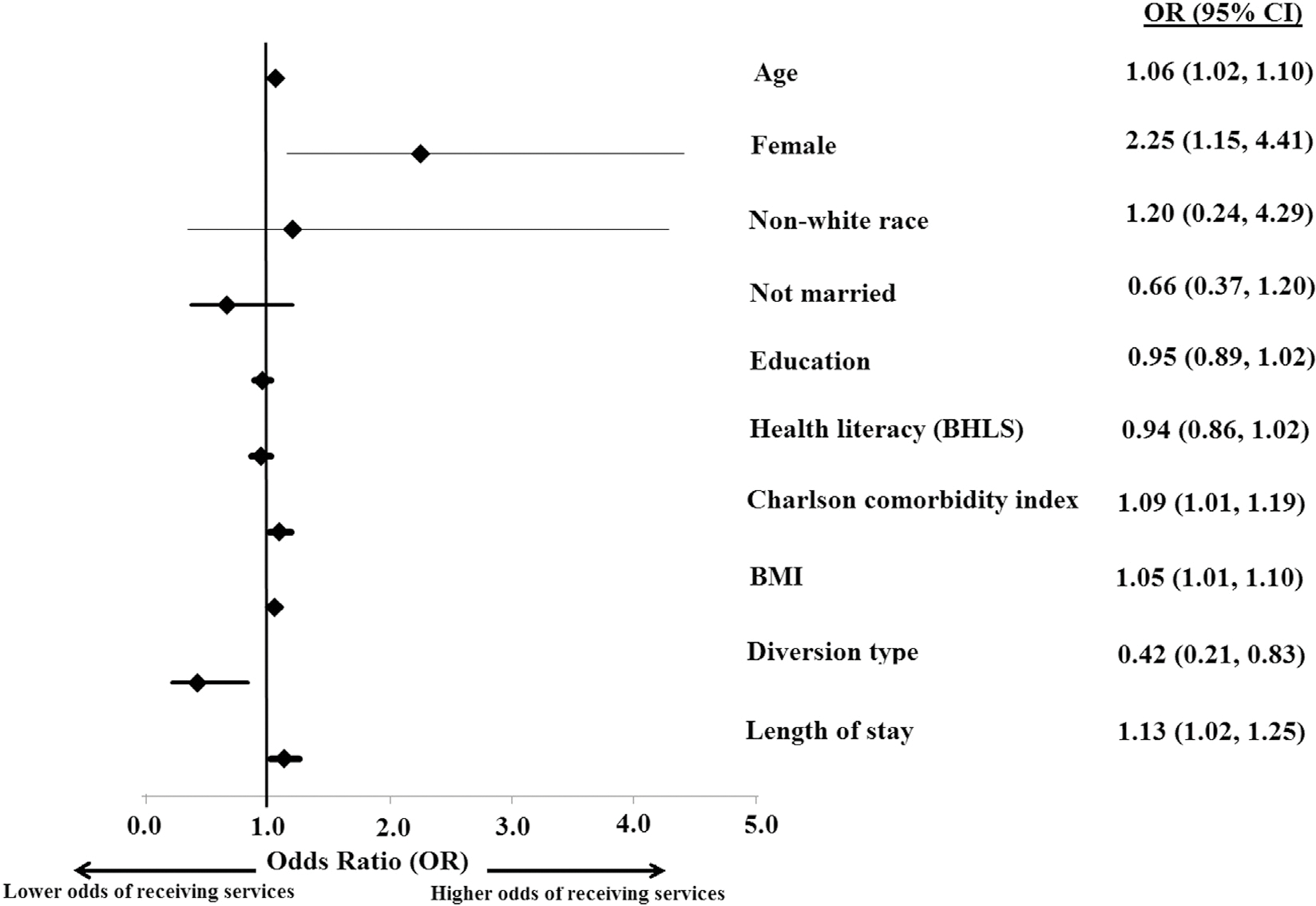
On multivariable analysis older age (OR 1.1, 95% CI 1.0–1.1, p = 0.002), female gender (OR 2.3, 95% CI 1.2–4.4, p = 0.019), BMI (OR 1.1, 95% CI 1.0–1.1, p = 0.034), CCI score (OR 1.1, 95% CI 1.0e1.2, p = 0.037) and length of stay (OR 1.1, 95% CI 1.0–1.2, p = 0.019) were significantly associated with the use of discharge resources. Patients with a continent urinary diversion (a neobladder or an Indiana pouch) were less likely to require discharge services than patients with an ileal conduit (OR 0.4, 95% CI 0.2–0.8, p <0.05, table 2 and fig. 2). BHLS score was not associated with the use of services after discharge on multivariable analysis, nor was race, education, marital status, insurance, receipt of neoadjuvant chemotherapy, procedure approach (robotic vs open) or pathological stage.
Table 2.
Multivariable logistic regression model of use of discharge services
| OR (95% CI) | p Value | |
|---|---|---|
|
| ||
| BHLS | 0.935 (0.859–1.017) | 0.117 |
| Age | 1.057 (1.020–1.095) | 0.002 |
| Gender (female vs male as referent) | 2.246 (1.146–4.405) | 0.019 |
| Race (nonwhite vs white as referent) | 1.204 (0.338–4.285) | 0.774 |
| Education | 0.951 (0.885–1.022) | 0.173 |
| Marital status (married vs not married as referent) | 0.663 (0.367–1.196) | 0.172 |
| Insurance (private vs other as referent) | 0.636 (0.346–1.167) | 0.144 |
| BMI | 1.051 (1.004–1.100) | 0.034 |
| Charlson comorbidity index score | 1.093 (1.005–1.188) | 0.037 |
| Neoadjuvant chemotherapy (yes vs no as referent) | 1.364 (0.789–2.360) | 0.266 |
| Procedure (robotic vs open) | 1.280 (0.730–2.244) | 0.389 |
| Continent urinary diversion (neobladder or Indiana pouch vs ileal conduit as referent) | 0.419 (0.211–0.830) | 0.013 |
| Length of stay (days) | 1.128 (1.020–1.247) | 0.019 |
| Pathological stage (muscle vs nonmuscle invasive as referent) | 0.736 (0.443–1.224) | 0.237 |
Figure 2.
DISCUSSION
Patients require resource intensive care after RC, including inpatient teaching by ostomy nurses if they elect incontinent urinary diversion or instructions on catheterization if they elect continent diversion. At hospital discharge, which is a critical transition point in post-cystectomy care, patients review this self-care teaching and receive a multitude of other verbal and written instructions. This is a process requiring a certain level of health literacy. Beyond its effect on discharge teaching, health literacy may be one of many factors that influence the patient discharge disposition after RC.
In this study approximately half of the patients who underwent RC required home health care, a skilled nursing facility or other rehabilitation services at the time of discharge. On bivariate analysis patients treated with RC who required discharge services had lower health literacy than those discharged home without services. Patients who needed home health care, a skilled nursing facility or other rehabilitation services were older and more likely to be female, unmarried, less educated and insured. These patients also had more baseline comorbidities and a longer length of stay, and were more likely to undergo ileal conduit urinary diversion. However, many of these differences were attenuated when controlling for select covariates on multivariable analysis. Ultimately, older age, female gender, higher BMI, higher CCI score, longer length of stay and the selection of incontinent urinary diversion were significantly predictive of the use of discharge services.
Previous groups have examined the impact of health literacy at the time of hospital discharge. Patient survey data reveal a perceived lack of knowledge of discharge instructions in patients with marginal or inadequate health literacy and medical terminology has been identified as a barrier to care.14,15 Choudhry et al reviewed their institutional trauma discharge instructions and found that they were written well above a sixth grade reading level, which is too advanced for many patients.16 Alberti and Nannini similarly found poor comprehension of patient discharge instructions and observed that clinicians seldom clarify patient comprehension in practice.17 In a large study of geriatric patients Albrecht et al noted that complete noncomprehension of discharge instructions among older adults was prevalent, including 5% for followup appointments, 27% for medications, 48% for exercise recommendations and 50% for diet recommendations.18
Factors associated with noncomprehension included older age, depression and social isolation. Given the many challenges in facilitating patient understanding of discharge instructions and the adverse outcomes associated with poor patient understanding of these instructions, IOM recently published a report summarizing the impact of discharge instructions on outcomes to highlight the importance of transitions of care, identify quality improvement opportunities and encourage further research.19
Few studies have examined health literacy and discharge disposition among patients undergoing RC. We recently reported health literacy and postoperative complications, having found that higher health literacy is associated with lower odds of complications after cystectomy.20 However, in that study we did not specifically evaluate discharge status. In an earlier study Aghazadeh et al from our institution evaluated discharge status after radical cystectomy.10 Older age, poor nutritional status, unmarried status and comorbidities predicted the need for home health care. Older age, poor exercise tolerance and longer length of stay predicted discharge to a facility with the significant finding that patients discharged to facilities have higher mortality rates. However, that study did not hypothesize that health literacy impacts the discharge disposition, and those data were not available during this earlier study period. Many other groups have assessed discharge practice patterns as well as readmissions after RC but they did not examine health literacy as a factor driving the use of post-discharge services or readmissions.21–26
To our knowledge this is the first report of the association between health literacy and the use of post-discharge resources after cystectomy. Additionally, by demonstrating specific demographic and clinical characteristics that predict the use of discharge services, this study identifies a patient population at risk that may benefit from targeted interventions. These interventions could include early identification of high risk populations by administration of the BHLS questionnaire during a preoperative visit, more intensive postoperative teaching or anticipatory clinical care pathways that facilitate care transitions and communication between inpatient teams and discharge facilities.
Several factors may explain why this study did not demonstrate a predictive association between low health literacy and the use of discharge services after RC. With increasing age there is a higher risk of low health care literacy.27 Thus, the influence of literacy on the discharge disposition may be attenuated by the older age of this patient population. Also, toward the end of the study period the clinical care pathway at our institution changed to default many patients to receive discharge services, given the high readmission rates of this patient population. This demonstrable shift toward increased use of discharge services regardless of patient risk factors may have influenced the outcomes.
This study has strengths. 1) It identifies clinically relevant risk factors for use of discharge services in a contemporary patient population treated with RC. These risk factors provide targets for improved patient counseling and perioperative clinical care pathways. 2) This study contains significant clinical granularity, given our thorough database and EHR chart abstraction, which allowed for examination of a variety of potential predictors of the use of discharge services after RC.
A limitation of this study is its retrospective nature. Consequently our conclusions must be weighed carefully and primarily considered as hypothesis generating. Also, our study cohort is racially homogenous. The fact that such a small percent of our patient population was nonwhite limits the generalizability of these results. Another limitation is that other confounding factors that were excluded from analysis may have influenced the patient discharge disposition, including performance and frailty status, which are associated with outcomes after cystectomy.28,29 Lastly, a potential limitation of this study is that patients with lower literacy scores may receive more teaching and attention, attenuating the relationship. However, our staff does not use health literacy scores to direct clinical care, nor were there targeted interventions as part of this study.
Despite these limitations, this study identifies key risk factors (age, comorbidities and incontinent diversion) which influence the complex self-care and ultimate discharge dispositions of patients who undergo RC. Targeting patients with these and other risk factors, including health literacy, may improve the discharge care of these patients in a cost-effective manner, as demonstrated in large health systems.30
CONCLUSIONS
The discharge process after RC is a resource intensive, critical transition point after which approximately half of patients require home health care, a skilled nursing facility or other inpatient rehabilitation services. Low health literacy may affect the patient discharge disposition while older age, female gender, BMI, comorbidities, length of stay and incontinent urinary diversion significantly predict the use of discharge services after RC. These risk factors and other clinical characteristics which may influence the complex self-care required of patients after cystectomy should be considered in the perioperative period with increased focus on discharge planning.
Abbreviations and Acronyms
- BHLS
brief health literacy screen
- BMI
body mass index
- CCI
Charlson comorbidity index
- EHR
electronic health record
- RC
radical cystectomy
Contributor Information
Stephen F. Kappa, Department of Urologic Surgery, Vanderbilt University Medical Center, Nashville, Tennessee
Kristen R. Scarpato, Department of Urologic Surgery, Vanderbilt University Medical Center, Nashville, Tennessee
Kathryn M. Goggins, Center for Health Services Research, Vanderbilt University Medical Center, Nashville, Tennessee
Sunil Kripalani, Department of Medicine, Vanderbilt University Medical Center, Nashville, Tennessee.
Kelvin A. Moses, Departments of Urologic Surgery, Vanderbilt University Medical Center, Nashville, Tennessee
REFERENCES
- 1.Montie JE: Against bladder sparing: surgery. J Urol 1999; 162: 452. [PubMed] [Google Scholar]
- 2.Shabsigh A, Korets R, Vora KC et al. : Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol 2009; 55: 164. [DOI] [PubMed] [Google Scholar]
- 3.Golden TM and Ratliff C: Development and implementation of a clinical pathway for radical cystectomy and urinary system reconstruction. J Wound Ostomy Continence Nurs 1997; 24: 72. [DOI] [PubMed] [Google Scholar]
- 4.Yeung C, Dinh T and Lee J: The health economics of bladder cancer: an updated review of the published literature. Pharmacoeconomics 2014; 32: 1093. [DOI] [PubMed] [Google Scholar]
- 5.Nielsen-Bohlman L, Panzer AM and Kindig DA: Health Literacy: A Prescription to End Confusion. Washington, D.C.: National Academies Press; 2004. [PubMed] [Google Scholar]
- 6.Kelly PA and Haidet P: Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns 2007; 66: 119. [DOI] [PubMed] [Google Scholar]
- 7.Safeer RS and Keenan J: Health literacy: the gap between physicians and patients. Am Fam Physician 2005; 72: 463. [PubMed] [Google Scholar]
- 8.Cavanaugh KL, Wingard RL, Hakim RM et al. : Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol 2010; 21: 1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson PN, Shetterly SM, Clarke CL et al. : Health literacy and outcomes among patients with heart failure. JAMA 2011; 305: 1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aghazadeh MA, Barocas DA, Salem S et al. : Determining factors for hospital discharge status after radical cystectomy in a large contemporary cohort. J Urol 2011; 185: 85. [DOI] [PubMed] [Google Scholar]
- 11.Chew LD, Bradley KA and Boyko EJ: Brief questions to identify patients with inadequate health literacy. Fam Med 2004; 36: 588. [PubMed] [Google Scholar]
- 12.Chew LD, Griffin JM, Partin MR et al. : Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 2008; 23: 561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R et al. : Research electronic data capture (REDCap)da metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wallace AS, Perkhounkova Y, Bohr NL et al. : Readiness for hospital discharge, health literacy, and social living status. Clin Nurs Res 2016; 25: 494. [DOI] [PubMed] [Google Scholar]
- 15.Samuels-Kalow M, Rhodes K, Uspal J et al. : Unmet needs at the time of emergency department discharge. Acad Emerg Med 2015; 23: 279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choudhry AJ, Baghdadi YM, Wagie AE et al. : Readability of discharge summaries: with what level of information are we dismissing our patients? Am J Surg 2016; 211: 631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alberti TL and Nannini A: Patient comprehension of discharge instructions from the emergency department: a literature review. J Am Assoc Nurse Pract 2013; 25: 186. [DOI] [PubMed] [Google Scholar]
- 18.Albrecht JS, Gruber-Baldini AL, Hirshon JM et al. : Hospital discharge instructions: comprehension and compliance among older adults. J Gen Intern Med 2014; 29: 1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Facilitating Patient Understanding of Discharge Instructions: Workshop Summary. Roundtable on Health Literacy, Board on Population Health and Public Health Practice, Institute of Medicine. Washington, D.C.: National Academies Press; 2014. [PubMed] [Google Scholar]
- 20.Scarpato KR, Kappa SF, Goggins KM et al. : The impact of health literacy on surgical outcomes following radical cystectomy. J Health Commun 2016; 21: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nayak JG, Gore JL, Holt SK et al. : Patient-centered risk stratification of disposition outcomes following radical cystectomy. Urol Oncol 2015; 34: 235. [DOI] [PubMed] [Google Scholar]
- 22.Minnillo BJ, Maurice MJ, Schiltz N et al. : Few modifiable factors predict readmission following radical cystectomy. Can Urol Assoc J 2015; 9: 439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taub DA, Dunn RL, Miller DC et al. : Discharge practice patterns following cystectomy for bladder cancer: evidence for the shifting of the burden of care. J Urol 2006; 176: 2612. [DOI] [PubMed] [Google Scholar]
- 24.Skolarus TA, Jacobs BL, Schroeck FR et al. : Understanding hospital readmission intensity after radical cystectomy. J Urol 2015; 193: 1500. [DOI] [PubMed] [Google Scholar]
- 25.James AC, Izard JP, Holt SK et al. : Root causes and modifiability of 30-day hospital readmissions after radical cystectomy for bladder cancer. J Urol 2016; 195: 894. [DOI] [PubMed] [Google Scholar]
- 26.Hu M, Jacobs BL, Montgomery JS et al. : Sharpening the focus on causes and timing of readmission after radical cystectomy for bladder cancer. Cancer 2014; 120: 1409. [DOI] [PubMed] [Google Scholar]
- 27.Kripalani S, Gatti ME and Jacobson TA: Association of age, health literacy, and medication management strategies with cardiovascular medication adherence. Patient Educ Couns 2010; 81: 177. [DOI] [PubMed] [Google Scholar]
- 28.Mayr R, May M, Martini T et al. : Comorbidity and performance indices as predictors of cancer-independent mortality but not of cancer-specific mortality after radical cystectomy for urothelial carcinoma of the bladder. Eur Urol 2012; 62: 662. [DOI] [PubMed] [Google Scholar]
- 29.Revenig LM, Canter DJ, Taylor MD et al. : Too frail for surgery? Initial results of a large multidisciplinary prospective study examining preoperative variables predictive of poor surgical outcomes. J Am Coll Surg 2013; 217: 665. [DOI] [PubMed] [Google Scholar]
- 30.Haun JN, Patel NR, French DD et al. : Associationbetween health literacy and medical care costs in an integrated healthcare system: a regional population based study. BMC Health Serv Res 2015; 15: 249. [DOI] [PMC free article] [PubMed] [Google Scholar]


