Abstract
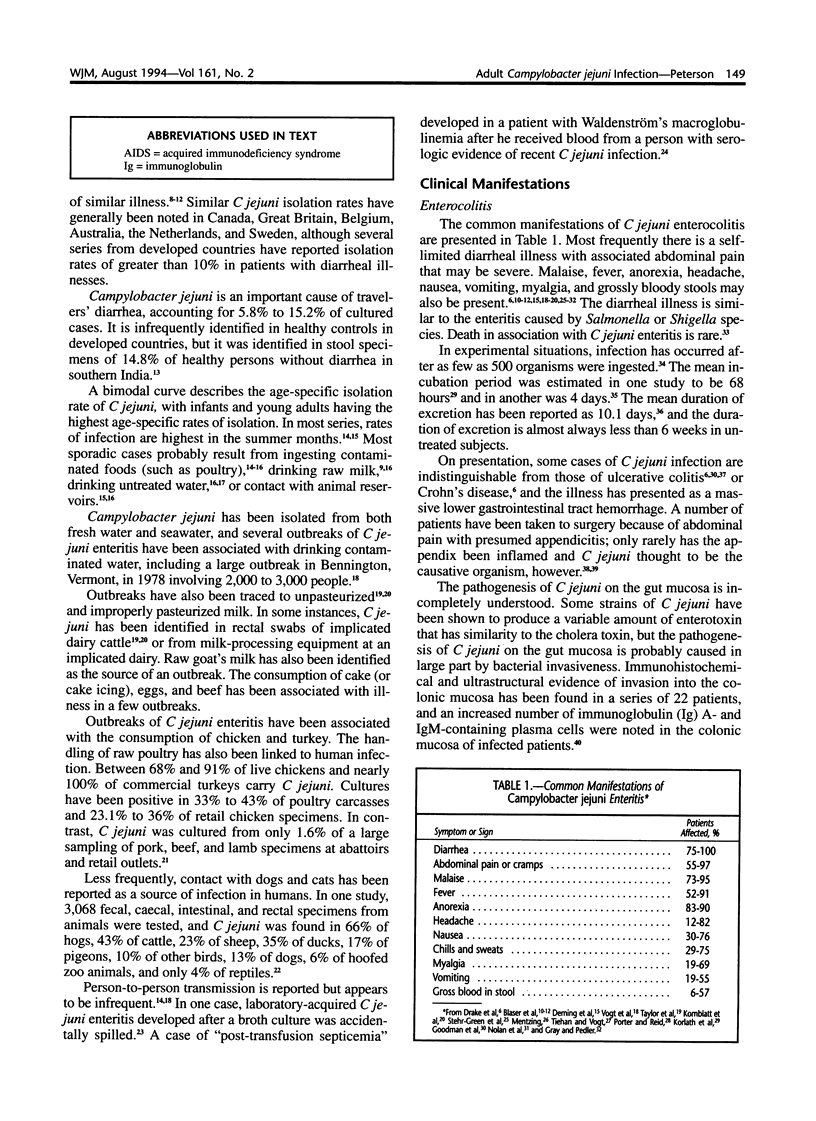
Campylobacter jejuni is an almost ubiquitous, microaerophilic, gram-negative rod. Outbreaks have been associated with drinking raw milk or contaminated water and eating poultry. Campylobacter jejuni accounts for 3.2% to 6.1% of cases of diarrheal illness in the general population of the United States, and infected patients frequently present with abdominal pain and fever. Less frequently, C jejuni is responsible for bacteremia, septic arthritis, septic abortion, and other extraintestinal infections. Reactive arthritis, Reiter's syndrome, the Guillain-Barré syndrome, and pancreatitis may accompany or follow C jejuni enterocolitis. Campylobacter jejuni is an important cause of diarrheal illness and is a more commonly identified stool organism than Salmonella or Shigella species. Recurrent and chronic infection is generally reported in immunocompromised hosts.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Black R. E., Levine M. M., Clements M. L., Hughes T. P., Blaser M. J. Experimental Campylobacter jejuni infection in humans. J Infect Dis. 1988 Mar;157(3):472–479. doi: 10.1093/infdis/157.3.472. [DOI] [PubMed] [Google Scholar]
- Blaser M. J., Berkowitz I. D., LaForce F. M., Cravens J., Reller L. B., Wang W. L. Campylobacter enteritis: clinical and epidemiologic features. Ann Intern Med. 1979 Aug;91(2):179–185. doi: 10.7326/0003-4819-91-2-179. [DOI] [PubMed] [Google Scholar]
- Blaser M. J., Hardesty H. L., Powers B., Wang W. L. Survival of Campylobacter fetus subsp. jejuni in biological milieus. J Clin Microbiol. 1980 Apr;11(4):309–313. doi: 10.1128/jcm.11.4.309-313.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaser M. J., Reller L. B., Luechtefeld N. W., Wang W. L. Campylobacter enteritis in Denver. West J Med. 1982 Apr;136(4):287–290. [PMC free article] [PubMed] [Google Scholar]
- Blaser M. J., Smith P. F., Kohler P. F. Susceptibility of Campylobacter isolates to the bactericidal activity of human serum. J Infect Dis. 1985 Feb;151(2):227–235. doi: 10.1093/infdis/151.2.227. [DOI] [PubMed] [Google Scholar]
- Blaser M. J., Wells J. G., Feldman R. A., Pollard R. A., Allen J. R. Campylobacter enteritis in the United States. A multicenter study. Ann Intern Med. 1983 Mar;98(3):360–365. doi: 10.7326/0003-4819-98-3-360. [DOI] [PubMed] [Google Scholar]
- Brodey P. A., Fertig S., Aron J. M. Campylobacter enterocolitis: radiographic features. AJR Am J Roentgenol. 1982 Dec;139(6):1199–1201. doi: 10.2214/ajr.139.6.1199. [DOI] [PubMed] [Google Scholar]
- Colgan T., Lambert J. R., Newman A., Luk S. C. Campylobacter jejuni enterocolitis. A clinicopathologic study. Arch Pathol Lab Med. 1980 Nov;104(11):571–574. [PubMed] [Google Scholar]
- Dekeyser P., Gossuin-Detrain M., Butzler J. P., Sternon J. Acute enteritis due to related vibrio: first positive stool cultures. J Infect Dis. 1972 Apr;125(4):390–392. doi: 10.1093/infdis/125.4.390. [DOI] [PubMed] [Google Scholar]
- Deming M. S., Tauxe R. V., Blake P. A., Dixon S. E., Fowler B. S., Jones T. S., Lockamy E. A., Patton C. M., Sikes R. O. Campylobacter enteritis at a university: transmission from eating chicken and from cats. Am J Epidemiol. 1987 Sep;126(3):526–534. doi: 10.1093/oxfordjournals.aje.a114685. [DOI] [PubMed] [Google Scholar]
- Drake A. A., Gilchrist M. J., Washington J. A., 2nd, Huizenga K. A., Van Scoy R. E. Diarrhea due to Campylobacter fetus subspecies jejuni. A clinical review of 63 cases. Mayo Clin Proc. 1981 Jul;56(7):414–423. [PubMed] [Google Scholar]
- Fujimoto S., Amako K. Guillain-Barré syndrome and Campylobacter jejuni infection. Lancet. 1990 Jun 2;335(8701):1350–1350. doi: 10.1016/0140-6736(90)91234-2. [DOI] [PubMed] [Google Scholar]
- Goodman L. J., Kaplan R. L., Trenholme G. M., Landau W., Kwiatkowski-Barrett J. E. Campylobacter fetus subsp. jejuni: experience in a large Chicago medical center. Am J Med Sci. 1981 Nov-Dec;282(3):125–130. doi: 10.1097/00000441-198111000-00005. [DOI] [PubMed] [Google Scholar]
- Gray J., Pedler S. J. Management of Campylobacter enteritis in hospitalized patients. J Hosp Infect. 1991 Apr;17(4):314–316. doi: 10.1016/0195-6701(91)90282-d. [DOI] [PubMed] [Google Scholar]
- Griffiths P. L., Park R. W. Campylobacters associated with human diarrhoeal disease. J Appl Bacteriol. 1990 Sep;69(3):281–301. doi: 10.1111/j.1365-2672.1990.tb01519.x. [DOI] [PubMed] [Google Scholar]
- Hopkins R. S., Olmsted R., Istre G. R. Endemic Campylobacter jejuni infection in Colorado: identified risk factors. Am J Public Health. 1984 Mar;74(3):249–250. doi: 10.2105/ajph.74.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Istre G. R., Blaser M. J., Shillam P., Hopkins R. S. Campylobacter enteritis associated with undercooked barbecued chicken. Am J Public Health. 1984 Nov;74(11):1265–1267. doi: 10.2105/ajph.74.11.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KING E. O. Human infections with Vibrio fetus and a closely related vibrio. J Infect Dis. 1957 Sep-Oct;101(2):119–128. doi: 10.1093/infdis/101.2.119. [DOI] [PubMed] [Google Scholar]
- Kaldor J., Pritchard H., Serpell A., Metcalf W. Serum antibodies in Campylobacter enteritis. J Clin Microbiol. 1983 Jul;18(1):1–4. doi: 10.1128/jcm.18.1.1-4.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaldor J., Speed B. R. Guillain-Barré syndrome and Campylobacter jejuni: a serological study. Br Med J (Clin Res Ed) 1984 Jun 23;288(6434):1867–1870. doi: 10.1136/bmj.288.6434.1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keat A. Reiter's syndrome and reactive arthritis in perspective. N Engl J Med. 1983 Dec 29;309(26):1606–1615. doi: 10.1056/NEJM198312293092604. [DOI] [PubMed] [Google Scholar]
- Kerstens P. J., Endtz H. P., Meis J. F., Oyen W. J., Koopman R. J., van den Broek P. J., van der Meer J. W. Erysipelas-like skin lesions associated with Campylobacter jejuni septicemia in patients with hypogammaglobulinemia. Eur J Clin Microbiol Infect Dis. 1992 Sep;11(9):842–847. doi: 10.1007/BF01960888. [DOI] [PubMed] [Google Scholar]
- Korlath J. A., Osterholm M. T., Judy L. A., Forfang J. C., Robinson R. A. A point-source outbreak of campylobacteriosis associated with consumption of raw milk. J Infect Dis. 1985 Sep;152(3):592–596. doi: 10.1093/infdis/152.3.592. [DOI] [PubMed] [Google Scholar]
- Kornblatt A. N., Barrett T., Morris G. K., Tosh F. E. Epidemiologic and laboratory investigation of an outbreak of Campylobacter enteritis associated with raw milk. Am J Epidemiol. 1985 Nov;122(5):884–889. doi: 10.1093/oxfordjournals.aje.a114171. [DOI] [PubMed] [Google Scholar]
- Kuroki S., Saida T., Nukina M., Haruta T., Yoshioka M., Kobayashi Y., Nakanishi H. Campylobacter jejuni strains from patients with Guillain-Barré syndrome belong mostly to Penner serogroup 19 and contain beta-N-acetylglucosamine residues. Ann Neurol. 1993 Mar;33(3):243–247. doi: 10.1002/ana.410330304. [DOI] [PubMed] [Google Scholar]
- Lambert J. R., Karmali M. A., Newman A. Campylobacter enterocolitis. Ann Intern Med. 1979 Dec;91(6):929–930. doi: 10.7326/0003-4819-91-6-929_2. [DOI] [PubMed] [Google Scholar]
- Lambert J. R., Tischler M. E., Karmali M. A., Newman A. Campylobacter ileocolitis: an inflammatory bowel disease. Can Med Assoc J. 1979 Nov 17;121(10):1377–1379. [PMC free article] [PubMed] [Google Scholar]
- Lambert M. E., Schofield P. F., Ironside A. G., Mandal B. K. Campylobacter colitis. Br Med J. 1979 Mar 31;1(6167):857–859. doi: 10.1136/bmj.1.6167.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lior H., Woodward D. L., Edgar J. A., Laroche L. J., Gill P. Serotyping of Campylobacter jejuni by slide agglutination based on heat-labile antigenic factors. J Clin Microbiol. 1982 May;15(5):761–768. doi: 10.1128/jcm.15.5.761-768.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKendrick M. W., Geddes A. M., Gearty J. Campylobacter enteritis: a study of clinical features and rectal mucosal changes. Scand J Infect Dis. 1982;14(1):35–38. doi: 10.3109/inf.1982.14.issue-1.07. [DOI] [PubMed] [Google Scholar]
- McKinley M. J., Taylor M., Sangree M. H. Toxic megacolon with campylobacter colitis. Conn Med. 1980 Aug;44(8):496–497. [PubMed] [Google Scholar]
- McNeil N. I., Buttoo S., Ridgway G. L. Spontaneous bacterial peritonitis due to Campylobacter jejuni. Postgrad Med J. 1984 Jul;60(705):487–488. doi: 10.1136/pgmj.60.705.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megraud F., Tachoire C., Latrille J., Bondonny J. M. Appendicitis due to Campylobacter jejuni. Br Med J (Clin Res Ed) 1982 Oct 23;285(6349):1165–1166. doi: 10.1136/bmj.285.6349.1165-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mentzing L. O. Waterborne outbreaks of campylobacter enteritis in central Sweden. Lancet. 1981 Aug 15;2(8242):352–354. doi: 10.1016/s0140-6736(81)90658-9. [DOI] [PubMed] [Google Scholar]
- Mishu B., Ilyas A. A., Koski C. L., Vriesendorp F., Cook S. D., Mithen F. A., Blaser M. J. Serologic evidence of previous Campylobacter jejuni infection in patients with the Guillain-Barré syndrome. Ann Intern Med. 1993 Jun 15;118(12):947–953. doi: 10.7326/0003-4819-118-12-199306150-00006. [DOI] [PubMed] [Google Scholar]
- Morlet N., Glancy R. Campylobacter jejuni appendicitis. Med J Aust. 1986 Jul 7;145(1):56–57. doi: 10.5694/j.1326-5377.1986.tb113754.x. [DOI] [PubMed] [Google Scholar]
- Nolan C. M., Johnson K. E., Coyle M. B., Faler K. Campylobacter jejuni enteritis: efficacy of antimicrobial and antimotility drugs. Am J Gastroenterol. 1983 Oct;78(10):621–626. [PubMed] [Google Scholar]
- Oates J. D., Hodgin U. G., Jr Laboratory-acquired Campylobacter enteritis. South Med J. 1981 Jan;74(1):83–83. doi: 10.1097/00007611-198101000-00031. [DOI] [PubMed] [Google Scholar]
- Paisley J. W., Mirrett S., Lauer B. A., Roe M., Reller L. B. Dark-field microscopy of human feces for presumptive diagnosis of Campylobacter fetus subsp. jejuni enteritis. J Clin Microbiol. 1982 Jan;15(1):61–63. doi: 10.1128/jcm.15.1.61-63.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner J. L., Hennessy J. N. Passive hemagglutination technique for serotyping Campylobacter fetus subsp. jejuni on the basis of soluble heat-stable antigens. J Clin Microbiol. 1980 Dec;12(6):732–737. doi: 10.1128/jcm.12.6.732-737.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepersack F., Prigogyne T., Butzler J. P., Yourassowsky E. Campylobacter jejuni post-transfusional septicaemia. Lancet. 1979 Oct 27;2(8148):911–911. doi: 10.1016/s0140-6736(79)92738-7. [DOI] [PubMed] [Google Scholar]
- Perlman D. M., Ampel N. M., Schifman R. B., Cohn D. L., Patton C. M., Aguirre M. L., Wang W. L., Blaser M. J. Persistent Campylobacter jejuni infections in patients infected with the human immunodeficiency virus (HIV). Ann Intern Med. 1988 Apr;108(4):540–546. doi: 10.7326/0003-4819-108-4-540. [DOI] [PubMed] [Google Scholar]
- Pines A., Goldhammer E., Bregman J., Kaplinsky N., Frankl O. Campylobacter enteritis associated with recurrent abortions in agammaglobulinemia. Acta Obstet Gynecol Scand. 1983;62(3):279–280. doi: 10.3109/00016348309155809. [DOI] [PubMed] [Google Scholar]
- Pitkanen T., Pettersson T., Pomka A., Kosunen T. U. Effect of erythromycin on the fecal excretion of Campylobacter fetus subspecies jejuni. J Infect Dis. 1982 Jan;145(1):128–128. doi: 10.1093/infdis/145.1.128. [DOI] [PubMed] [Google Scholar]
- Porter I. A., Reid T. M. A milk-borne outbreak of Campylobacter infection. J Hyg (Lond) 1980 Jun;84(3):415–419. doi: 10.1017/s0022172400026942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajan D. P., Mathan V. I. Prevalence of Campylobacter fetus subsp. jejuni in healthy populations in southern India. J Clin Microbiol. 1982 May;15(5):749–751. doi: 10.1128/jcm.15.5.749-751.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes K. M., Tattersfield A. E. Guillain-Barre syndrome associated with Campylobacter infection. Br Med J (Clin Res Ed) 1982 Jul 17;285(6336):173–174. doi: 10.1136/bmj.285.6336.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley L. W., Finch M. J. Results of the first year of national surveillance of Campylobacter infections in the United States. J Infect Dis. 1985 May;151(5):956–959. doi: 10.1093/infdis/151.5.956. [DOI] [PubMed] [Google Scholar]
- Robinson D. A. Infective dose of Campylobacter jejuni in milk. Br Med J (Clin Res Ed) 1981 May 16;282(6276):1584–1584. doi: 10.1136/bmj.282.6276.1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ropper A. H. Campylobacter diarrhea and Guillain-Barré syndrome. Arch Neurol. 1988 Jun;45(6):655–656. doi: 10.1001/archneur.1988.00520300075022. [DOI] [PubMed] [Google Scholar]
- Schmid G. P., Schaefer R. E., Plikaytis B. D., Schaefer J. R., Bryner J. H., Wintermeyer L. A., Kaufmann A. F. A one-year study of endemic campylobacteriosis in a midwestern city: association with consumption of raw milk. J Infect Dis. 1987 Jul;156(1):218–222. doi: 10.1093/infdis/156.1.218. [DOI] [PubMed] [Google Scholar]
- Skirrow M. B. Campylobacter enteritis: a "new" disease. Br Med J. 1977 Jul 2;2(6078):9–11. doi: 10.1136/bmj.2.6078.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G. S., Blaser M. J. Fatalities associated with Campylobacter jejuni infections. JAMA. 1985 May 17;253(19):2873–2875. [PubMed] [Google Scholar]
- Sorvillo F. J., Lieb L. E., Waterman S. H. Incidence of campylobacteriosis among patients with AIDS in Los Angeles County. J Acquir Immune Defic Syndr. 1991;4(6):598–602. [PubMed] [Google Scholar]
- Spelman D. W., Davidson N., Buckmaster N. D., Spicer W. J., Ryan P. Campylobacter bacteraemia: a report of 10 cases. Med J Aust. 1986 Nov 17;145(10):503–505. doi: 10.5694/j.1326-5377.1986.tb139451.x. [DOI] [PubMed] [Google Scholar]
- Tauxe R. V., Pegues D. A., Hargrett-Bean N. Campylobacter infections: the emerging national pattern. Am J Public Health. 1987 Sep;77(9):1219–1221. doi: 10.2105/ajph.77.9.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor D. N., Blaser M. J., Echeverria P., Pitarangsi C., Bodhidatta L., Wang W. L. Erythromycin-resistant Campylobacter infections in Thailand. Antimicrob Agents Chemother. 1987 Mar;31(3):438–442. doi: 10.1128/aac.31.3.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor D. N., McDermott K. T., Little J. R., Wells J. G., Blaser M. J. Campylobacter enteritis from untreated water in the Rocky Mountains. Ann Intern Med. 1983 Jul;99(1):38–40. doi: 10.7326/0003-4819-99-1-38. [DOI] [PubMed] [Google Scholar]
- Taylor D. N., Porter B. W., Williams C. A., Miller H. G., Bopp C. A., Blake P. A. Campylobacter enteritis: a large outbreak traced to commercial raw milk. West J Med. 1982 Nov;137(5):365–369. [PMC free article] [PubMed] [Google Scholar]
- Vesterby A., Baandrup U., Jacobsen N. O., Albertsen K. Campylobacter enterocolitis. An important differential diagnosis in ulcerative colitis. Acta Pathol Microbiol Immunol Scand A. 1983 Jan;91(1):31–33. [PubMed] [Google Scholar]
- Vogt R. L., Sours H. E., Barrett T., Feldman R. A., Dickinson R. J., Witherell L. Campylobacter enteritis associated with contaminated water. Ann Intern Med. 1982 Mar;96(3):292–296. doi: 10.7326/0003-4819-96-3-292. [DOI] [PubMed] [Google Scholar]
- Wood C. J., Fleming V., Turnidge J., Thomson N., Atkins R. C. Campylobacter peritonitis in continuous ambulatory peritoneal dialysis: report of eight cases and a review of the literature. Am J Kidney Dis. 1992 Mar;19(3):257–263. doi: 10.1016/s0272-6386(13)80007-8. [DOI] [PubMed] [Google Scholar]
- van Spreeuwel J. P., Duursma G. C., Meijer C. J., Bax R., Rosekrans P. C., Lindeman J. Campylobacter colitis: histological immunohistochemical and ultrastructural findings. Gut. 1985 Sep;26(9):945–951. doi: 10.1136/gut.26.9.945. [DOI] [PMC free article] [PubMed] [Google Scholar]


