Abstract
While maintaining an active lifestyle and engaging in regular exercise are known to promote cardiovascular (CV) health, increasing evidence has emerged to indicate that these lifestyle behaviors also can promote psychological health and well-being. This has led to research to determine if exercise can serve as a potential therapeutic modality for major depressive disorder (MDD), which is a leading cause of mental-health impairment and overall disability worldwide. The strongest evidence to support this use comes from an increasing number of randomized clinical trials (RCTs) that have compared exercise to usual care, placebo controls, or established therapies in healthy adults and in various clinical populations. The relatively large number of RCTs has led to numerous reviews and meta-analyses, which generally have been concordant in indicating that exercise ameliorates depressive symptoms, improves self-esteem, and enhances various aspects of quality of life. Together, these data indicate that exercise should be considered as a therapeutic modality for improving CV health and psychological well-being. The emerging evidence also has led to a new proposed subspecialty of “lifestyle psychiatry”, which promotes the use of exercise as an adjunctive treatment for patients with MDD. Indeed, some medical organizations have now endorsed lifestyle-based approaches as foundational aspects of depression management, with adoption of exercise as a treatment option for MDD. This review summarizes research in the area and provides practical suggestions for the use of exercise in clinical practice.
Keywords: Cardiovascular disease, Exercise, Depression, Lifestyle medicine, Cardiac rehabilitation
Lifestyle medicine is an evolving medical specialty that uses therapeutic lifestyle interventions as a primary modality to treat chronic, noncommunicable diseases. Lifestyle medicine focuses on health behaviors and psychological factors that promote health and decrease disease risk (Fig. 1). For instance, poor diet, obesity, physical inactivity, substance abuse, and smoking are negative health behaviors that contribute to chronic medical conditions, such as coronary heart disease (CHD), type 2 diabetes, and hypertension.1 Psychological determinants of disease include depression, anxiety, social isolation and poor social support, various forms of chronic stress, pessimism, and vital exhaustion.2–6
Fig. 1.
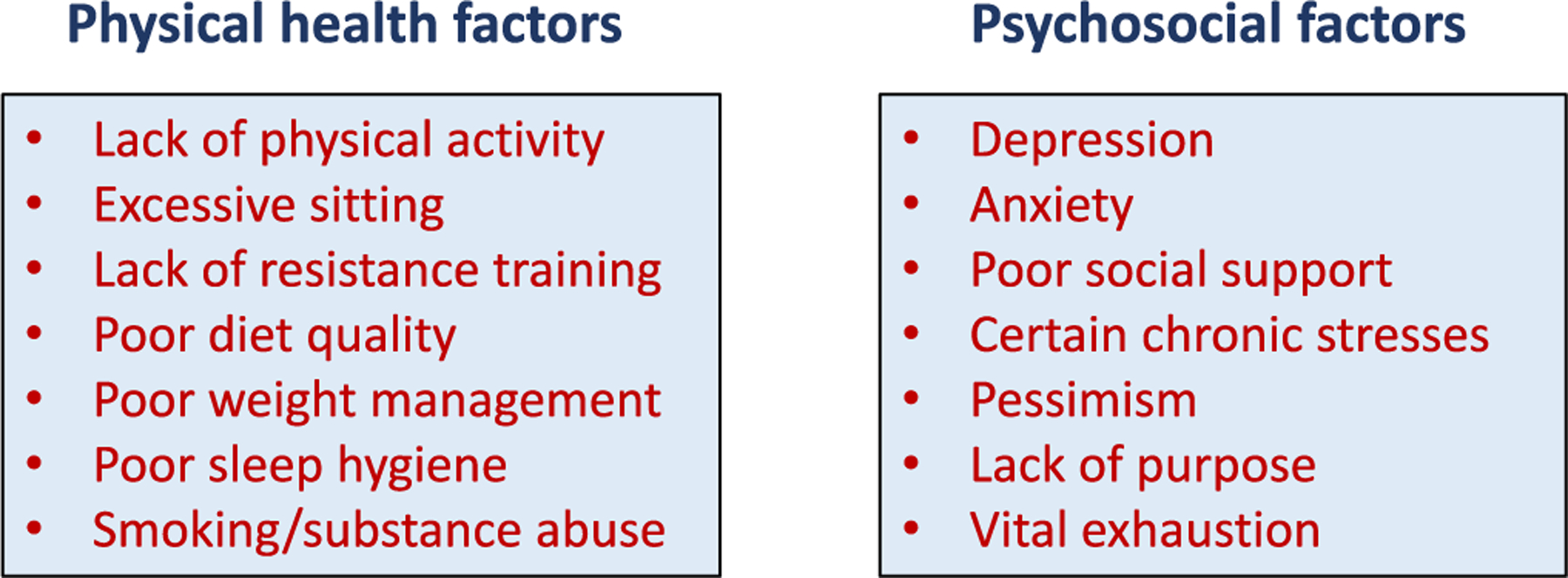
Physical health and psychosocial risk factors for disease.
A central tenet of lifestyle medicine is the bi-directional relationship between physical health behaviors and psychological well-being. Substantial evidence indicates that health-damaging behaviors can lead to a decrease in psychological well-being. Conversely, negative psychological states such as depression, anxiety and anger can adversely impact health-promoting behaviors. Indeed, common negative moods such as depression, anxiety, and anger along with low social support are commonly associated with a higher concentration of poor health habits.
The present review will briefly discuss the assessment of depression and distinguish between physical activity (PA) and exercise. Next, we will summarize available evidence regarding the amelioration of depression with physical activity and exercise in general and cardiac populations, with specific emphasis on the conduct of randomized clinical trials (RCTs), which have compared the efficacy of exercise versus standard of care, placebo controls, or established treatments for major depressive disorder (MDD). We will then overview emerging data regarding how the combination of exercise and other lifestyle interventions may be used as a treatment modality for depressive symptoms in medical practice. Finally, we will evaluate how these new findings can be incorporated into the current practice of clinical medicine and may be leading to a new sub-specialty of ‘lifestyle psychiatry’.
Definition and assessment of depression
Depression is a term that has been used to describe a mood state that may range from mild unhappiness to intense sadness and despair. It also may refer to a clinical syndrome or cluster of symptoms, or to a diagnosed clinical disorder. Major depressive disorder is one of the most common psychiatric conditions in the United States and worldwide. It is estimated that 21 million adults in the United States will have at least one major depressive episode during their lifetimes. This number represents 8.4% of all U.S. adults.7 The prevalence of MDD is higher among adult females (10.5%) compared to males (6.2%) and also is consistent across high, middle and low income countries, emphasizing the global burden of this condition.8
Clinical depression is relatively common in patients with CHD, with estimates of 15% to 20% of cardiovascular disease (CVD) patients meeting criteria for MDD and an additional 20% reporting elevated depressive symptoms.9–11 A number of studies have reported that the presence of clinical depression is associated with more than a doubling of risk for mortality and nonfatal CVD events12,13 and that even subclinical elevations in depressive symptoms are associated with a worse prognosis in patients with established CHD.10,11
According to the most recent Diagnostic and Statistical Manual of Mental Disorders (DSM-V), MDD is one of a number of depressive disorders. The common feature of these disorders is feeling of sadness, loss of interest, and/or irritable mood, accompanied by related changes that significantly affect the individual’s capacity to function (including somatic symptoms and impaired cognition). The severity of depression is typically based on three considerations: 1) the presence of symptoms (which may vary in frequency and intensity); 2) the duration of the disorder; and 3) the impact on personal and social functioning. The general criteria for MDD diagnosis are provided in Table 1.
Table 1.
Diagnosis of major depression based on DSM-5 criteria.⁎
|
A. Required symptoms. At least one of the following:
B. Associated symptoms. ≥4 of the following additional symptoms during the same 2-week period that are a change from previous functioning:
|
When symptoms not attributable to effects of substance abuse, underlying medical condition, or better explained by other psychiatric conditions.
MDD is formally diagnosed by clinical interview, while symptom severity is typically quantified by clinical ratings or psychometric questionnaires. The more commonly used questionnaires are listed in Table 2. Among these, the Patient Health Questionnaire (PHQ)-2 has been suggested by the American Heart Association as a screening tool for depression among CVD patients.14
Table 2.
Common psychometric instruments used to assess depression.
| Instrument | # of items |
|---|---|
| Beck Depression Inventory-II (BDI-II) | 21 |
| Center for Epidemiological Studies-Depression Scale (CES-D) | 20 |
| Hamilton Rating Scale for Depression (HAM-D)⁎ | 17 |
| Hospital Anxiety and Depression Scale-Depression (HADS-D) | 7 |
| Patient Health Questionnaire-9 (PHQ-9) | 9 |
| PHQ-2 subscale of PHQ-9 | 2 |
| Symptom Checklist-90 Depression scale (SCL-90 D) | 12 |
| Zung Self-Rating Depression Scale (SDS) | 20 |
Note: The HAM-D scale is administered and scored by a health care professional and contains 21 items, but the score is based on 17 items.
Exercise, physical activity and depression
Although the terms physical activity and exercise are often used interchangeably, physical activity and exercise are considered distinct constructs.15 PA is defined as any bodily movement that requires energy expenditure, while exercise is defined as structured PA that aims to maintain or improve physical fitness; PA defined in this manner is broader in scope, and includes such activities as gardening, housework, physical labor, and leisure type activities such as bowling, golf, and pickleball. Exercise, on the other hand, is a subcategory of physical activity and is considered more purposeful in that it is designed to improve or maintain aerobic capacity, muscular strength and endurance, and/or flexibility.
The beneficial impact that PA and exercise have upon mental health is well-documented. The earliest studies were observational and examined the relationship between physical activity and incidence of depression within communities. An example of an early epidemiologic study was conducted in Alameda County California in 1965.16 A PA index was computed based upon the frequency and presumed intensity of self-reported PA (e.g., playing sports, swimming, walking, and gardening). Men and women who reported low levels of PA at baseline were more likely to be depressed and were twice as likely to subsequently develop depression compared to those individuals who reported high PA at baseline. Interestingly, persons who were active but who subsequently became sedentary also were more likely to become depressed. As an extension of these findings, recent Mendelian randomization research has demonstrated that people who are more active and are genetically predisposed to MDD are less likely to develop MDD compared to people of equal genetic risk for MDD and low PA levels.17 Because these observational studies are correlational in nature, such studies cannot be used to establish causal relationships. For example, factors such as illness and declining health could also be responsible for these associations. People who are sick and disabled are less likely to engage in PA and are more likely to get depressed.
The study of the relationship between exercise and depression in general populations has led to subsequent investigations as to whether promotion of PA and exercise can be used as therapy for the prevention and treatment of psychiatric disorders. This is particularly important insofar as it has been estimated that mental, neurological and substance-use disorders (i.e. schizophrenia, mood and anxiety disorders, epilepsy, dementia, alcohol dependence) account for 13% of the global burden of disease, placing mental illness as the greatest burden, exceeding both heart disease and cancer.18 The potential use of exercise therapy for treating depression is especially relevant insofar as MDD and CHD are both highly prevalent and each is considered a risk factor for the other.
RCTs of exercise in depressed populations
The most convincing evidence for the causal effects of exercise in reducing depressive symptoms can be derived from RCTs. Over the past two decades, the number of RCTs of exercise on depression has accrued substantially.19,20 In the most recent Cochrane review of the literature by Cooney et al.,19,21 39 trials (2326 participants) fulfilled inclusion criteria, of which 37 provided data for the meta-analyses. For the 35 trials (1356 participants) comparing exercise versus no treatment or a control intervention, the pooled standardized mean difference (SMD) for the primary outcome of depression at the end of treatment was −0.62, indicating a moderate clinical effect. However, when only the six trials (464 participants) with adequate allocation concealment, intention-to-treat analysis, and blinded outcome assessment were considered, the pooled SMD for this outcome was no longer statistically significant.
A subsequent meta-analysis by Schuch et al.22 of 25 RCTs compared exercise to a number of control or comparison groups, with adjustment for publication bias. Nine of the trials included participants with MDD. Exercise was associated with a large and significant reduction in depression (Fig. 2). The anti-depressant effect of exercise was greater for studies that included individuals diagnosed with MDD. Adjusted analyses found that publication bias generally resulted in an underestimation of the beneficial effects of exercise upon depression. Further, larger effect sizes were observed for studies involving supervision of exercise by qualified exercise professionals. However, it also should be noted that many studies suffer from methodological shortcomings, which detract from the strength of these findings.
Fig. 2.
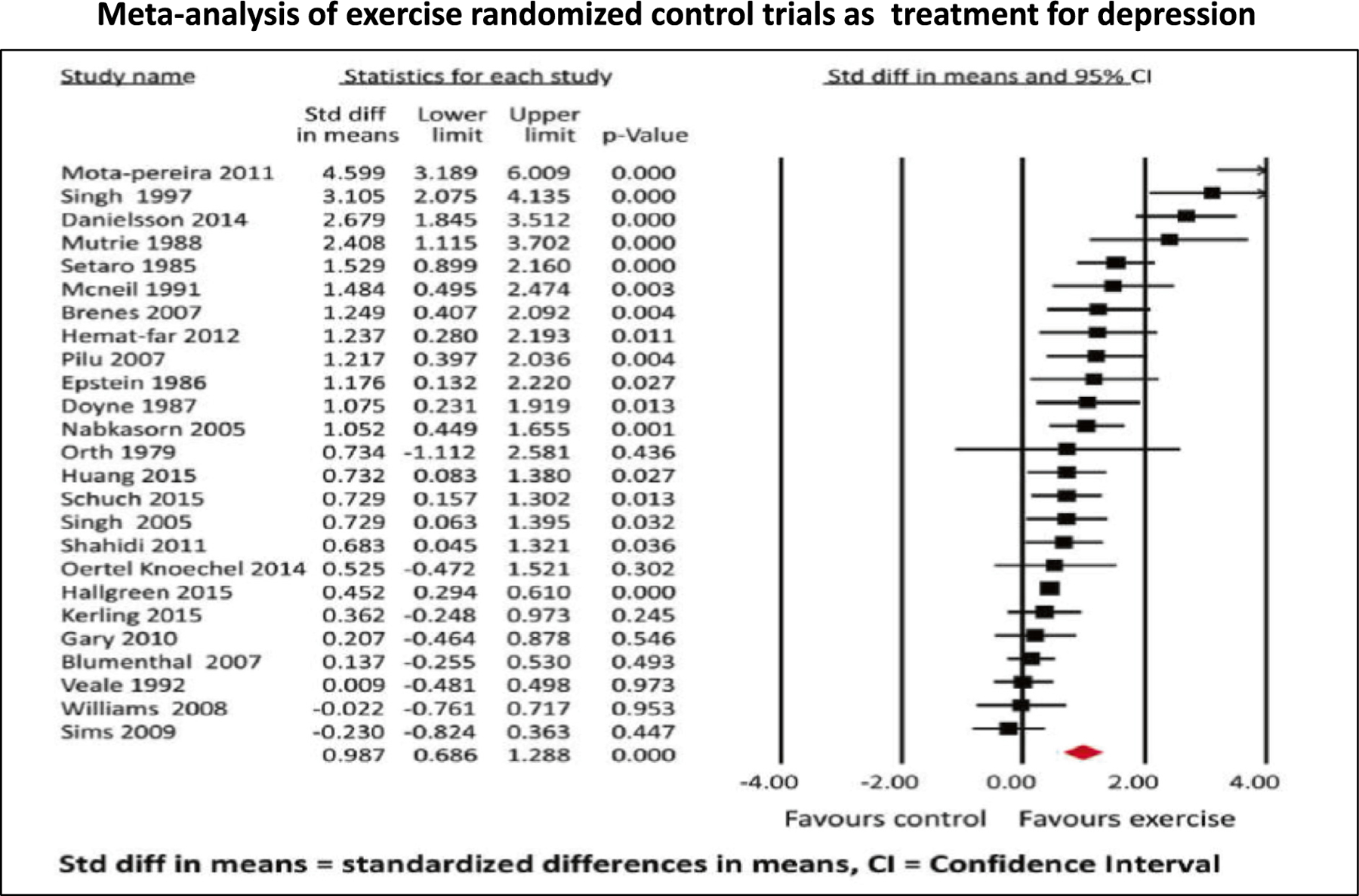
Results of meta-analysis of 25 randomized controlled trials of exercise interventions versus control conditions among individuals with major depressive disorder or depressive symptoms, indicating a large treatment effect. (Reprinted with permission from Schuch et al.22).
RCTs of exercise for depression compared to established antidepressant medications
A series of studies at Duke University have examined the benefits of exercise compared to established pharmacotherapy for depression. In 1999, researchers conducted the first in a series of RCTs designed to examine the effects of exercise in patients with MDD compared to standard antidepressant medication.23 Initially, there was a great deal of skepticism among those in the mental health field: Would sufficient numbers of patients with MDD volunteer for an exercise study? Could patients with MDD engage in exercise and stick to it? And of course, would exercise help ease depression? The answer to each of these questions was a resounding ‘yes’!
In the first RCT, 156 patients with MDD were recruited and randomized to one of three conditions: aerobic exercise, antidepressant medication (sertraline) or a combination of exercise and sertraline. Results revealed that all three groups showed significant, and comparable, improvements in depressive symptoms. Remission rates (i.e., no longer met criteria for MDD) were 60.4% of patients in the exercise group, 65.5% in the medication group, and 68.8% in the combined group. Surprisingly, even patients with more severe depression appeared to benefit from exercise as much as those who received the medication, and there was no advantage for those who received both exercise and sertraline compared to those who received either sertraline or exercise alone—even in those with more severe depression.
Interestingly, in a 6-month follow up report,24 participants in the exercise group exhibited lower rates of depression (30%) compared to participants in the sertraline (52%) and combined group (55%). Moreover, only 8% of those patients who were remitted after treatment in the exercise condition suffered a relapse, compared to 31% in the sertraline condition and 38% in the combination sertraline and exercise condition.
The study provided some answers, but also raised other questions. Because most patients improved, the improvements could be attributed to any number of explanations–a placebo effect, spontaneous remission, demand characteristics (i.e., trying to ‘please’ the researchers), regression to the mean, or due simply to the increased attention provided by study staff. Because participants exercised in a group setting, there was a possibility that social support provided to participants during their exercise workouts further enhanced the benefits of exercise. A second study attempted to address these concerns.25 In this study, 202 adults with MDD were randomly assigned to supervised exercise in a group setting; home-based exercise; antidepressant medication (sertraline, 50–200 mg daily); or placebo pill. After 4 months of treatment, 41% of the participants achieved remission, defined as no longer meeting the criteria for MDD and a score of <8 on the Hamilton Rating Scale for Depression. Both exercise and medication groups achieved higher remission rates compared with placebo; 45% of MDD patients undergoing supervised exercise, 40% undergoing home-based exercise, and 47% receiving medication were in remission after 16 weeks of treatment, compared with only 31% receiving placebo. The efficacy of exercise in patients was generally comparable to those patients receiving antidepressant medication, and medication and exercise tended to be better than the placebo. Not surprisingly, placebo response rates were high, suggesting that some of the therapeutic response was due to patient expectations, ongoing symptom monitoring, attention, and other nonspecific factors.
These studies involved patients with MDD, but did not specifically target patients with CHD, for whom the presence of comorbid depression has important prognostic significance. Subsequently, 101 patients with stable CHD and elevated depressive symptoms, in a study known as UPBEAT,26 were randomized to aerobic exercise (3 times/week), sertraline (50–200 mg/day), or placebo. After 4 months, participants in the aerobic exercise program and those who received sertraline had larger reductions in depressive symptoms compared to patients in the placebo group (Fig. 3). In addition, exercise and antidepressant medication tended to result in greater improvements in heart rate variability compared with placebo, and exercise tended to result in greater improvements in heart rate variability compared with sertraline. This study was important because it demonstrated that the improvements in depression from exercise training were comparable to an established antidepressant medication and had the added benefit of also improving some CHD biomarkers that could improve clinical outcomes.
Fig. 3.
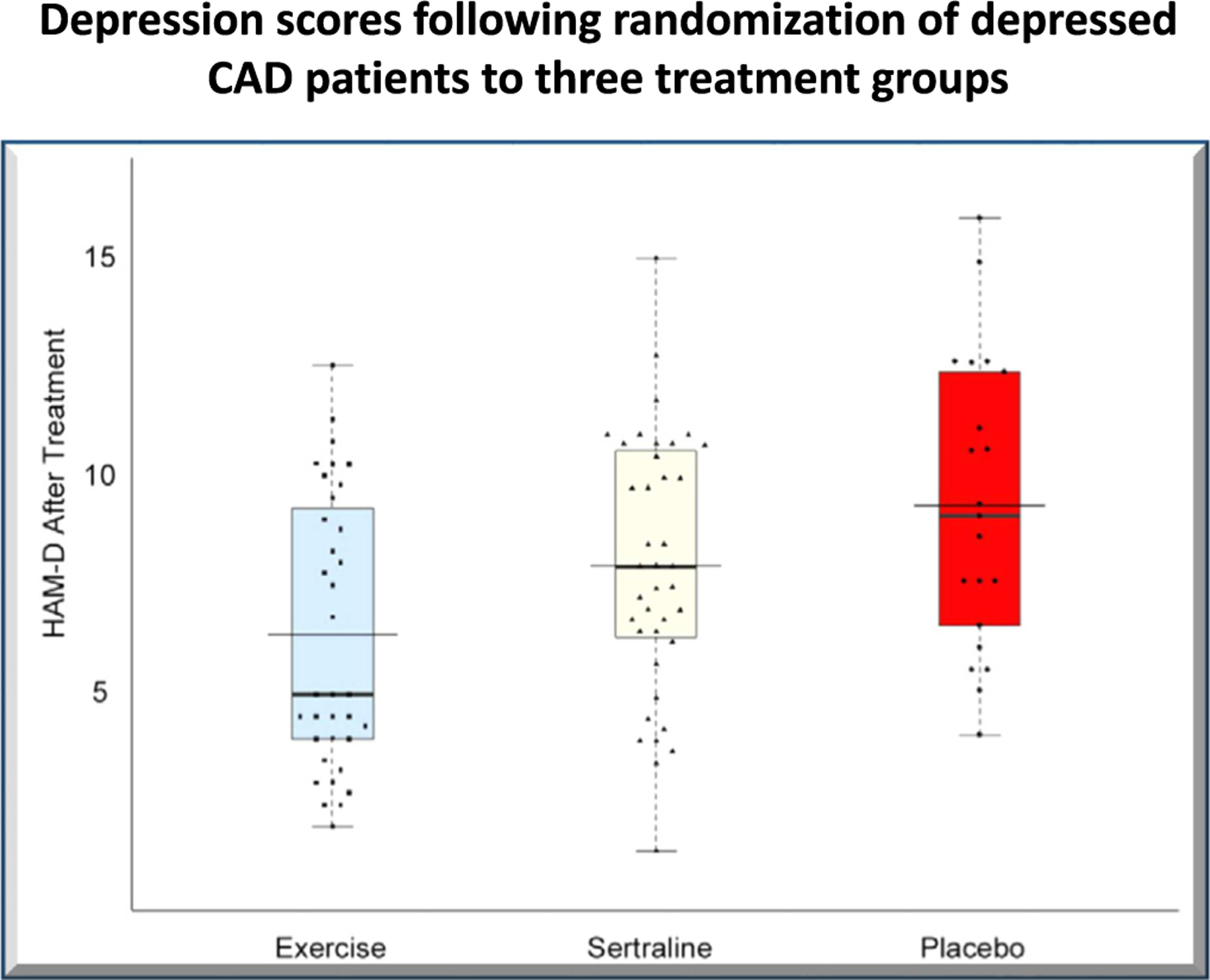
Hamilton-D (HAM—D) scores for depression among 101 cardiac patients with elevated depression symptoms, randomized to three groups, after completion of their randomized treatments. The exercise group had the lowest depression scores. (Reprinted with permission from Blumenthal et al.26).
RCTs of aerobic exercise for depression in heart failure (HF)
While depression is common among CHD patients, its presence is accentuated among patients with HF. Depression among heart failure patients is associated with both diminished quality of life (QoL) and a higher risk for adverse clinical outcomes, especially if depression worsens over time.27,28 A systematic review and meta-analysis of 16 RCTs involving 3226 patients with HF found that exercise training was associated with a significant decrease in depressive symptoms compared to patients with HF who did not undergo exercise training.29,101 In perhaps the largest, multi-site RCT of exercise in HF patients, known as HF-ACTION, participants randomized to exercise reported lower levels of depression after 3 and 12 months compared to usual care controls. Findings were similar among patients undergoing exercise training in center-base, home-based, or combined settings.
RCTs of resistance training for depression
Most studies of exercise and depression focus on aerobic exercise. However, an important aspect of physical fitness involves muscular strength and endurance, which is improved by resistance training. There is now evidence that resistance training can also improve mental health. In a meta-analysis of 33 RCTs, involving 1877 participants,30 resistance exercise training was associated with a moderate-sized mean effect upon reduction of depressive symptoms. There was significant heterogeneity in the findings, however, due in part to small samples and disparate baseline conditions. Accordingly, more studies regarding the impact of resistance training upon depression are needed.
Impact of cardiac rehabilitation (CR) on depression
Although CR was initially introduced primarily as an exercise intervention, it has subsequently expanded in scope to become a more comprehensive lifestyle intervention, with aerobic exercise as the core and four additional elements including dietary modification, risk factor management (including smoking cessation), stress reduction, and patient education (Fig. 4). This development is relevant because there is increasing evidence that besides exercise, dietary modification,31–34 smoking cessation,35–37 and sleep hygiene,38–41 either alone or acting additively42 or synergistically43–45 with exercise can contribute to improvements in depression.
Fig. 4.
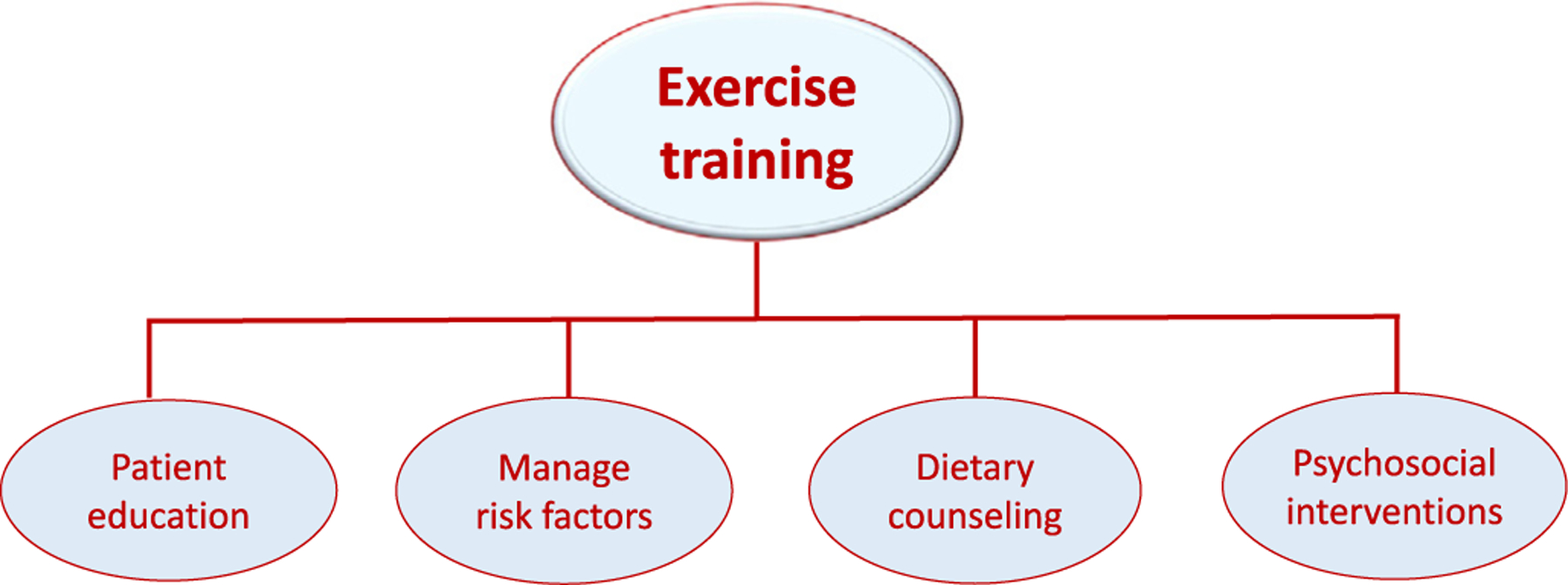
Cardiac rehabilitation is based on the promotion of exercise training and the inclusion of four other core components, including stress management and psychotherapy (e.g., interpersonal therapy or cognitive behavior therapy) specifically for patients with depression when indicated.
In a series of reports from the Ochsner Clinic, participation in exercise-based CR has been shown to be associated with reduced depression in women,46 older adults,47 and in patients with risk factors for CHD such as diabetes.48 In one study of 338 consecutive patients who were referred for exercise-based CR,49 69 patients were depressed at study entry. After 12 weeks of CR and exercise training (CRET), depression was reduced significantly in two thirds of patients and improvements on several measures of QoL were noted. In a subsequent study of 522 consecutive CHD patients enrolled in CRET and a control group of 179 CHD patients who did not complete CRET, the prevalence of depression decreased 63% after CRET (from 17% to 6%).50 Depressed patients who completed cardiac rehabilitation also had a 73% lower mortality rate.
To assess the relative benefit of each of the core components of CR, Kabboul et al.51 performed a meta-analysis of 148 RCTs, involving 50,965 participants, which evaluated the comparative effectiveness of each of the core components on mortality and morbidity. The two components that had the most significant impact on reducing all cause-mortality were exercise training and psychosocial interventions (Table 3). In an important RCT of patients referred for exercise-based CR, Blumenthal et al.52 reported that stress management provided added value to traditional exercise-based CR on depression and a composite measure of stress, as well as on major adverse CVD events.
Table 3.
Estimates of the effects of the five core components of cardiac rehabilitation upon all-cause mortality according to meta-analysis by Kabboul et al.51
| Core component | Estimate and 95% CI |
|---|---|
| Exercise training | 0.74 (0.60–0.92) |
| Nutritional counseling | 1.07 (0.78–1.46) |
| Risk factor modification | 0.87 (0.66–1.15) |
| Patient education | 0.98 (0.78–1.20) |
| Psychosocial management | 0.68 (0.54–0.85) |
There also are emerging data that suggest that dietary interventions also may reduce the risk of MDD,32 whereas diets high in ultra-processed foods may be associated with an increased risk of depressive symptoms.53 Meta-analyses of clinical trials that use whole food diet interventions have provided preliminary evidence that they significantly reduced depressive symptoms and several small RCTs have reported improvements in depressive symptoms when randomized to receive Mediterranean-style dietary intervention compared to controls.33,54–56 Clearly, a promising area for future research is to further assess the impact of dietary interventions upon depression as well as the combined effects of diet and exercise.
Mechanisms of beneficial effects of exercise on depression
A growing literature suggests that exercise can reduce depression through both biological and psychological mechanisms. However, these mechanisms are complex and not yet fully elucidated. For instance, some early investigations focused rather narrowly on beta endorphins and it was thought that the release of beta endorphins during exercise might explain the anti-depressant effects of exercise.57 However, this notion was subsequently considered overly simplistic since endorphin levels measured in the periphery are not necessarily reflective of levels in the brain.
A current understanding of the mechanistic relationship between exercise and depression, including the influence of potential moderators and confounders has been summarized by Kandola et al.58 (Fig. 5). Some of the principal biological derangements associated with depression include disruptions in the neuroplasticity pathways of the brain, the effects of chronic low grade inflammation, vulnerability of the brain to oxidative stress, and the impact of neuroendocrine dysfunction. There is supportive evidence that exercise can favorably retard each of these mechanistic pathways toward depression.
Fig. 5.
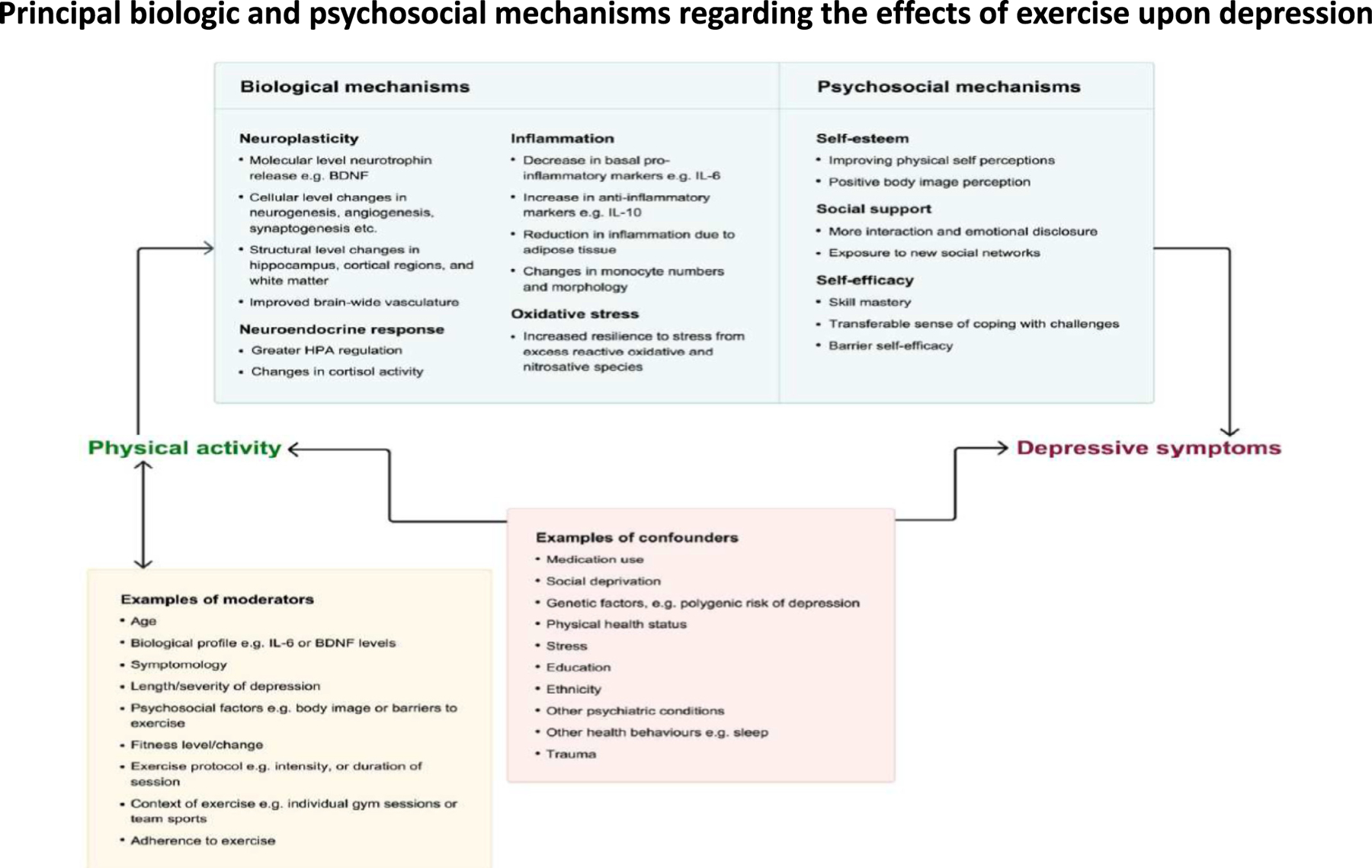
Biological and psychosocial mechanisms that may contribute to the anti-depressant effects of exercise, along with examples of moderators and cofounding factors that may influence the study of these mechanistic relationships. (Reprinted with permission from Kendola et al.58).
Some of the plausible biological and psychological mechanisms that could be responsible for the beneficial effects of exercise include stimulation of brain-derived neurotrophic factor (BDNF),59,60 increased core body temperature,61 reduced inflammation,62,63 stimulation of the pre-frontal cortex and hippocampus,64 enhanced aminergic transmission including alterations in central norepinephrine activity,65–68 enhanced activity of the hypothalamic-pituitary-adrenocortical axis, including structural brain changes that can be induced by prolonged cortisol exposure,69 and reductions in oxidative stress.70
The psychological benefits of exercise are broad-based, including evidence that exercise can promote one’s sense of self-efficacy and mastery, and lead to improved self-esteem.58 Exercise also can provide a greater sense of hope, purpose and meaning, and can serve as a method for coping with stress. In addition, exercise, particularly in a group setting such as the programs offered through cardiac rehabilitation, can increase social support by providing opportunities to socialize and interact with others. It is likely that the improvement in mood that can follow from the initiation of exercise involve a synergistic interplay of the biological, psychological, and social pathways that are promoted by regular exercise and increased PA.
Clinical implications
Evidence accumulated over the past two decades indicates that physically active individuals and individuals who engage in regular exercise are less likely to be depressed at the time of baseline measurements and less likely to become depressed when followed over time. As reviewed herein, the results of numerous RCTs generally indicate that exercise improves depressive symptoms even among people with MDD. Meta-analyses of RCTs also demonstrate that exercise can significantly improve other psychological domains including self-esteem, quality of life, neurocognition,71 and sleep.72,73 Therefore, based upon available evidence, exercise has become increasingly considered as a viable treatment option for patients with mild to moderate MDD and it can be combined with other established therapies such as cognitive behavior therapy, interpersonal psychotherapy, and/or pharmacotherapy in particular for more severe MDD.
These psychological benefits raise practical questions as to how to use exercise as a therapeutic modality for the prevention and treatment of depression. First, what is the “therapeutic dose” of exercise that aids its anti-depressive effects? Second, how can one best motivate depressed patients to exercise? And third, what are useful strategies to help patients maintain exercise, especially those who may be depressed? The following sections will briefly address these practical concerns.
Exercise “dose” for treating depression.
The issue of exercise dose has recently been evaluated by Pearce et al. in a meta-analysis of exercise activity and depression among 15 studies, involving 191,130 participants.74 An inverse curvilinear association between PA and incident depression was observed. This dose response relationship was similar among patients diagnosed with MDD versus patients with depressive symptoms with steeper gradients at lower PA volumes (Fig. 6). Relative to those adults not reporting any activity, those accumulating half the recommended volume of PA (i.e., ~ 75 min of moderate intensity of exercise/week) had 18% lower risk of depression, while those reportedly engaged in the recommended volume of exercise (i.e., ~ 150 min of moderate intensity exercise per week) had 25% lower risk, with diminishing benefits beyond that exposure level. Importantly, the greatest differences in risk for depression were observed among those who were totally sedentary versus those engaging in low doses of PA. This parallels the general finding that clinical health benefits accrue most dramatically among patients who shift from being sedentary to initiating even low levels of PA.75,76 One relatively small RCT of depressed patients determined that the optimal dose of exercise was 150 min/wk. of aerobic exercise,77 but because the methodologies of exercise RCTs generally tend to be of lower quality compared to drug trials78 there remains uncertainty as to the optimal dose of exercise to treat depression in clinical populations.
Fig. 6.
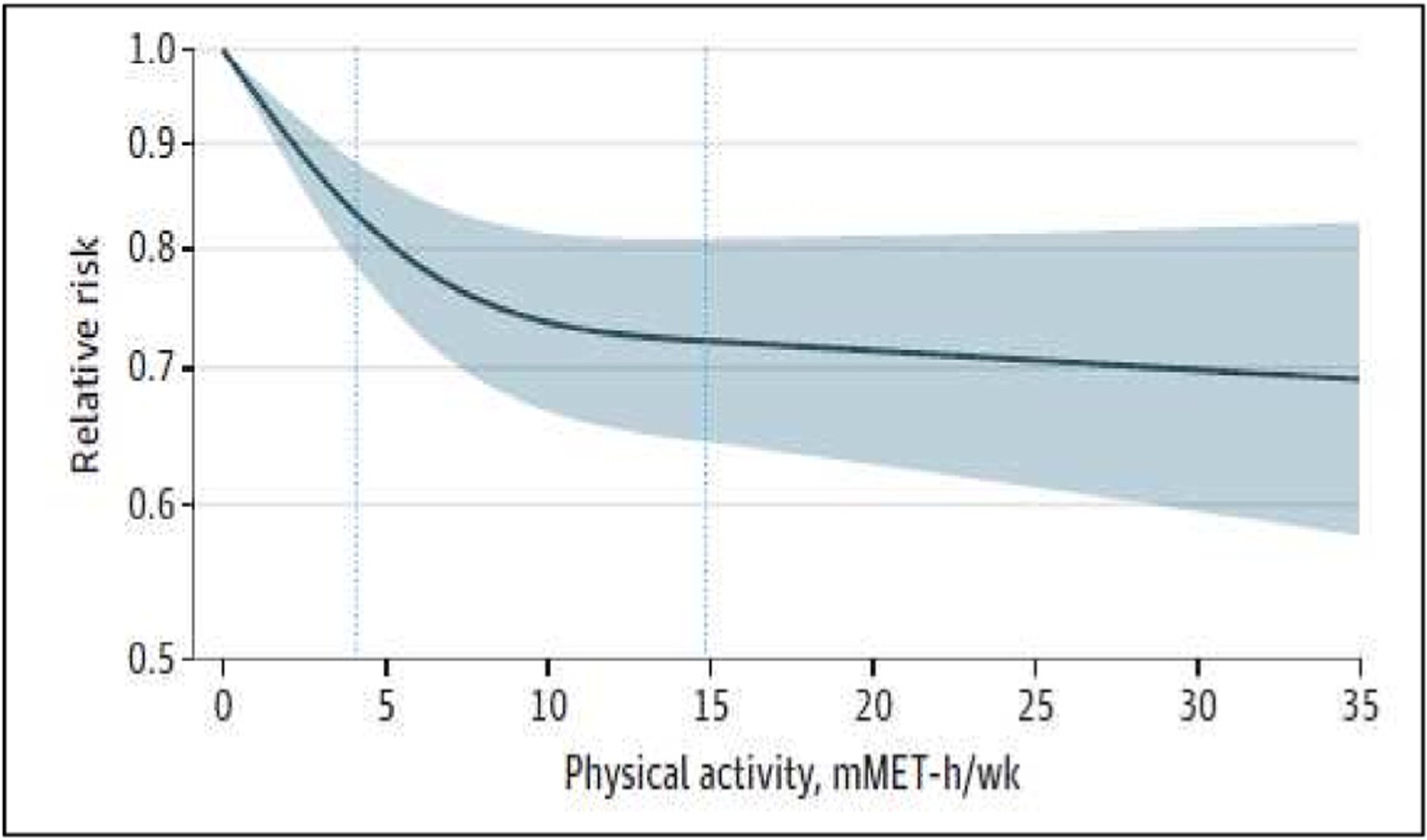
Association between physical activity level and risk for depression, from meta-analysis of 119,130 participants in 15 studies. An inverse curvilinear relationship between dose of physical activity and depression is noted, with the greatest reduction occurring at low levels of physical activity. (Reproduced with permission from Pearce et al.74).
Motivating Patients with Clinical Depression to Exercise.
One of the pressing challenges in clinical practice is how to motivate patients who are depressed and sedentary to initiate an exercise regimen. A full discussion of this issue is beyond the scope of this review, but we favor using principles applied from motivational interviewing,79 action planning concepts,80,81 and the transtheoretical model of health behavior change.82 Among these principles, it is best to look for opportunities to assess patients’ willingness to consider initiating exercise. This might involve asking patients open-ended questions about their PA habits or garnering the same information from questionnaires, such as the two-item exercise vital sign that is recommended by the American Academy of Sports Medicine.83 Using such information, patients can then be asked if they are willing to consider the benefits of exercise. If so, then the present and future-oriented benefits of exercise can be shared with patients, followed by querying patients as to their thoughts about this information.
A related counseling principle is helping patients to make action plans according to their sense of “self-efficacy”. This principle is based on the well-demonstrated recognition that patients are less likely to initiate goals if they believe they are beyond their capability. Thus, the goal with depressed sedentary patients should be to achieve “small wins” or psychological successes by encouraging them to engage in whatever level of exercise or PA that the feel they can initiate. This is best accomplished by setting modest goals to maximize the likelihood of success and providing patients with encouragement. This could mean as little as 5–10 min of walking every day or a few days per week, which is consistent with a new directive within the 2018 Physical Activity Guidelines for Americans that suggests that any amount of exertion, regardless of duration, can count toward one’s weekly total of physical activity.84
In our experience, movement begets movement and the first goal among patients who are sedentary is to get them to take the first step—literally and figuratively. This is particularly helpful because many depressed patients may be easily fatigued, have unrealistic fears about being able to exercise safely, and/or have little confidence that they can succeed.
It is important that providers not just prescribe exercise but follow-up at regular intervals to reinforce patients’ exercise behaviors so that it becomes a habit. If the physician provides an exercise prescription but never follows up, the unintended message to the patient may be that exercise is just not that important. Ultimately, we have found that patients who exercise regularly will transition from considering exercise as a means to an end (i.e., increased fitness, greater survival) to an end in itself.85 Other guidelines for incorporating exercise as a treatment for patients with depression are listed in Table 4.
Table 4.
Guidelines for exercise prescription for depressed patients.
|
Barriers to Begin and Sustain an Exercise Regimen.
In anticipation of difficulty sustaining an exercise program, it can be useful for patients to identify potential barriers to exercise, to anticipate obstacles to exercise, and to brainstorm potential solutions. External factors may include inclement weather, unsafe neighborhoods, and time demands of family and work. Internal factors include low motivation (e.g., low energy, belief that exercise may not be helpful or is beyond the person’s abilities), unpleasant sensations from exercise (e.g., pain, fatigue, shortness of breath), or fear of injury or of a catastrophic event (e.g., myocardial infarction or stroke). The presence of significant anxiety is another factor that can diminish the effectiveness of exercise in reducing depression. In one exercise RCT of depressed patients, Herman and colleagues86 showed that high anxiety levels at study entry predicted early dropout from exercise programs and the presence of comorbid anxiety has also been shown to diminish the effectiveness of exercise in reducing depression.87,88 Therefore, anxious patients with comorbid depression may require more attention to initiate and maintain an exercise program.
Summary and conclusions
Based upon the available evidence, a number of medical organizations, such as the American Heart Association, American College of Sports Medicine, and American College of Lifestyle Medicine have called for the routine assessment of PA in healthcare settings. However, the emerging evidence regarding the psychological benefits of exercise for depressed patients suggests that there is also fertile opportunity for mental health professionals to use exercise therapy and other lifestyle interventions in their management of patients with depression and related disorders in what may be considered a new subspecialty of “lifestyle psychiatry”. This emerging field recognizes the important contribution of health behaviors on mental, as well as physical health, including the benefits derived from healthy nutrition,89,90 smoking abstinence,91,92 sleep,93,94 and physical activity.95,96
Notably in this regard, a number of organizations including the Royal Australia and New Zealand Royal College of Psychiatrists97 now endorse lifestyle-based approaches as foundational aspects of depression management. Furthermore, exercise is also now recommended as a treatment option for MDD by a number of mental health organizations, including the European Psychiatric Association,98 and the World Federation of Societies for Biological Psychiatry suggest that exercise be considered as an adjunctive treatment to supplement pharmacotherapy.99
The National Institute for Health and Care Excellence (NICE) guidelines, which set forth evidence-based recommendations for health and care in England, also endorse exercise and physical activity as a treatment modality for mild depression. According to the NICE Guidelines,100 doing any form of physical activity on a regular basis could help enhance feelings of wellbeing and further suggest that the benefits could be enhanced if this activity is performed outdoors.
In summary, accumulated evidence from both observational studies and RCTs indicate that exercise diminishes depressive symptoms, even among individuals with MDD. These findings add to the extant literature suggesting that exercise can enhance self-esteem, increase self-confidence, and improve QoL. Thus, in addition to the cardiovascular benefits of exercise, exercise now may be considered an effective therapeutic modality for aiding in the prevention and treatment of depression.
Acknowledgments
The authors wish to thank Stephanie Mabe, MS for her assistance in the preparation of this manuscript.
Funding support
Grant HL125522 from the National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD.
Abbreviations:
- CHD
coronary heart disease
- CR
cardiac rehabilitation
- CRET
cardiac rehabilitation and exercise training
- CVD
cardiovascular disease
- HF
heart failure
- MDD
major depressive disorder
- NICE
National Institute for Health and Care Excellence
- PA
physical activity
- PHQ
Patient Health Questionnaire
- QoL
quality of life
- RCTs
randomized clinical trials
- SMD
Standard mean difference
Footnotes
Declaration of Competing Interest
None.
References
- 1.Kushner RF, Mechanick JI. Lifestyle Medicine : A Manual for Clinical Practice 1st ed. Springer International Publishing: Imprint: Springer. 2016.1 online resource (XVI, 363 pages 40 illustrations, 20 illustrations in color. [Google Scholar]
- 2.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation Apr 27 1999;99(16):2192–2217. 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 3.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol Mar 1 2005;45(5): 637–651. 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Cohen R, Bavishi C, Haider S, Thankachen J, Rozanski A. Meta-analysis of relation of vital exhaustion to cardiovascular disease events. Am J Cardiol Apr 15 2017;119(8): 1211–1216. 10.1016/j.amjcard.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Rozanski A, Bavishi C, Kubzansky LD, Cohen R. Association of optimism with cardiovascular events and all-cause mortality: a systematic review and meta-analysis. JAMA Netw Open Sep 4 2019;2(9), e1912200. 10.1001/jamanetworkopen.2019.12200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lett HS, Blumenthal JA, Babyak MA, et al. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med May-Jun 2004;66(3):305–315. 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- 7.NIH. Accessed July 21, 2022: https://www.nimh.nih.gov/health/statistics/major-depression 2022.
- 8.Malhi GS, Mann JJ. Depression. Lancet Nov 24 2018;392(10161):2299–2312. 10.1016/S0140-6736(18)31948-2. [DOI] [PubMed] [Google Scholar]
- 9.Thombs BD, Bass EB, Ford DE, et al. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med Jan 2006;21(1):30–38. 10.1111/j.1525-1497.2005.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lesperance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation Mar 5 2002;105(9):1049–1053. 10.1161/hc0902.104707. [DOI] [PubMed] [Google Scholar]
- 11.Bush DE, Ziegelstein RC, Tayback M, et al. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol Aug 15 2001;88 (4):337–341. 10.1016/s0002-9149(01)01675-7. [DOI] [PubMed] [Google Scholar]
- 12.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA Oct 20 1993;270(15):1819–1825. [PubMed] [Google Scholar]
- 13.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med Nov-Dec 2004;66(6):802–813. 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 14.Lichtman JH, Bigger JT Jr, Blumenthal JA, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation Oct 21 2008;118(17):1768–1775. 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 15.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep Mar-Apr 1985;100(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- 16.Camacho TC, Roberts RE, Lazarus NB, Kaplan GA, Cohen RD. Physical activity and depression: evidence from the Alameda County study. Am J Epidemiol Jul 15 1991;134 (2):220–231. 10.1093/oxfordjournals.aje.a116074. [DOI] [PubMed] [Google Scholar]
- 17.Choi KW, Zheutlin AB, Karlson RA, et al. Physical activity offsets genetic risk for incident depression assessed via electronic health records in a biobank cohort study. Depress Anxiety Feb 2020;37(2):106–114. 10.1002/da.22967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry Feb 2016;3(2):171–178. 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 19.Cooney GM, Dwan K, Greig CA, et al. Exercise for depression. Cochrane Database Syst Rev Sep 12 2013;9, CD004366. 10.1002/14651858.CD004366.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Josefsson T, Lindwall M, Archer T. Physical exercise intervention in depressive disorders: meta-analysis and systematic review. Scand J Med Sci Sports Apr 2014;24(2): 259–272. 10.1111/sms.12050. [DOI] [PubMed] [Google Scholar]
- 21.Cooney G, Dwan K, Greig C, et al. Exercise for depression. Advn Psychiatr Treatm 2014;20(1):2. 10.1192/apt.20.1.2. [DOI] [Google Scholar]
- 22.Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res Jun 2016;77:42–51. 10.1016/j.jpsychires.2016.02.023. [DOI] [PubMed] [Google Scholar]
- 23.Blumenthal JA, Babyak MA, Moore KA, et al. Effects of exercise training on older patients with major depression. Arch Intern Med Oct 25 1999;159(19):2349–2356. 10.1001/archinte.159.19.2349. [DOI] [PubMed] [Google Scholar]
- 24.Babyak M, Blumenthal JA, Herman S, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med Sep-Oct 2000;62 (5):633–638. 10.1097/00006842-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Blumenthal JA, Babyak MA, Doraiswamy PM, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med Sep-Oct 2007;69 (7):587–596. 10.1097/PSY.0b013e318148c19a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blumenthal JA, Sherwood A, Babyak MA, et al. Exercise and pharmacological treatment of depressive symptoms in patients with coronary heart disease: results from the UPBEAT (understanding the prognostic benefits of exercise and antidepressant therapy) study. J Am Coll Cardiol Sep 18 2012;60(12):1053–1063. 10.1016/j.jacc.2012.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol Oct 17 2006;48(8):1527–1537. 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 28.Sherwood A, Blumenthal JA, Hinderliter AL, et al. Worsening depressive symptoms are associated with adverse clinical outcomes in patients with heart failure. J Am Coll Cardiol Jan 25 2011;57(4):418–423. 10.1016/j.jacc.2010.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tu RH, Zeng ZY, Zhong GQ, et al. Effects of exercise training on depression in patients with heart failure: a systematic review and meta-analysis of randomized controlled trials. Eur J Heart Fail Jul 2014;16(7):749–757. 10.1002/ejhf.101. [DOI] [PubMed] [Google Scholar]
- 30.Gordon BR, McDowell CP, Hallgren M, Meyer JD, Lyons M, Herring MP. Association of efficacy of resistance exercise training with depressive symptoms: meta-analysis and meta-regression analysis of randomized clinical trials. JAMA Psychiatry Jun 1 2018;75(6):566–576. 10.1001/jamapsychiatry.2018.0572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marx W, Moseley G, Berk M, Jacka F. Nutritional psychiatry: the present state of the evidence. Proc Nutr Soc Nov 2017;76(4):427–436. 10.1017/S0029665117002026. [DOI] [PubMed] [Google Scholar]
- 32.Firth J, Solmi M, Wootton RE, et al. A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry Oct 2020;19(3):360–380. 10.1002/wps.20773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Francis HM, Stevenson RJ, Chambers JR, Gupta D, Newey B, Lim CK. A brief diet intervention can reduce symptoms of depression in young adults - a randomised controlled trial. PloS One 2019;14(10), e0222768. 10.1371/journal.pone.0222768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lassale C, Batty GD, Baghdadli A, et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry Jul 2019;24(7):965–986. 10.1038/s41380-018-0237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taylor GM, Lindson N, Farley A, et al. Smoking cessation for improving mental health. Cochrane Database Syst Rev Mar 9 2021;3, CD013522. 10.1002/14651858.CD013522.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fluharty M, Taylor AE, Grabski M, Munafo MR. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob Res Jan 2017;19(1): 3–13. 10.1093/ntr/ntw140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stepankova L, Kralikova E, Zvolska K, et al. Depression and smoking cessation: evidence from a smoking cessation clinic with 1-year follow-up. Ann Behav Med Jun 2017;51(3):454–463. 10.1007/s12160-016-9869-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev Dec 2021;60, 101556. 10.1016/j.smrv.2021.101556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bei B, Asarnow LD, Krystal A, Edinger JD, Buysse DJ, Manber R. Treating insomnia in depression: insomnia related factors predict long-term depression trajectories. J Consult Clin Psychol Mar 2018;86(3):282–293. 10.1037/ccp0000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Henry AL, Miller CB, Emsley R, et al. Insomnia as a mediating therapeutic target for depressive symptoms: a sub-analysis of participant data from two large randomized controlled trials of a digital sleep intervention. J Sleep Res Feb 2021;30(1), e13140. 10.1111/jsr.13140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gee B, Orchard F, Clarke E, Joy A, Clarke T, Reynolds S. The effect of non-pharmacological sleep interventions on depression symptoms: a meta-analysis of randomised controlled trials. Sleep Med Rev Feb 2019;43:118–128. 10.1016/j.smrv.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 42.Wong VW, Ho FY, Shi NK, Sarris J, Chung KF, Yeung WF. Lifestyle medicine for depression: a meta-analysis of randomized controlled trials. J Affect Disord Apr 1 2021;284:203–216. 10.1016/j.jad.2021.02.012. [DOI] [PubMed] [Google Scholar]
- 43.Opie RS, O’Neil A, Itsiopoulos C, Jacka FN. The impact of whole-of-diet interventions on depression and anxiety: a systematic review of randomised controlled trials. Public Health Nutr Aug 2015;18(11):2074–2093. 10.1017/S1368980014002614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Imayama I, Alfano CM, Kong A, et al. Dietary weight loss and exercise interventions effects on quality of life in overweight/obese postmenopausal women: a randomized controlled trial. Int J Behav Nutr Phys Act Oct 25 2011;8:118. 10.1186/1479-5868-8-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abbenhardt C, McTiernan A, Alfano CM, et al. Effects of individual and combined dietary weight loss and exercise interventions in postmenopausal women on adiponectin and leptin levels. J Intern Med Aug 2013;274(2):163–175. 10.1111/joim.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lavie CJ, Milani RV, Cassidy MM, Gilliland YE. Effects of cardiac rehabilitation and exercise training programs in women with depression. Am J Cardiol May 15 1999;83(10):1480–1483.A7: 10.1016/s0002-9149(99)00127-7. [DOI] [PubMed] [Google Scholar]
- 47.Milani RV, Lavie CJ. Prevalence and effects of cardiac rehabilitation on depression in the elderly with coronary heart disease. Am J Cardiol May 15 1998;81(10):1233–1236. 10.1016/s0002-9149(98)00121-0. [DOI] [PubMed] [Google Scholar]
- 48.Milani RV, Lavie CJ. Behavioral differences and effects of cardiac rehabilitation in diabetic patients following cardiac events. Am J Med May 1996;100(5):517–523. 10.1016/s0002-9343(96)00020-4. [DOI] [PubMed] [Google Scholar]
- 49.Milani RV, Lavie CJ, Cassidy MM. Effects of cardiac rehabilitation and exercise training programs on depression in patients after major coronary events. Am Heart J Oct 1996;132(4):726–732. 10.1016/s0002-8703(96)90304-x. [DOI] [PubMed] [Google Scholar]
- 50.Milani RV, Lavie CJ. Impact of cardiac rehabilitation on depression and its associated mortality. Am J Med Sep 2007;120(9):799–806. 10.1016/j.amjmed.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 51.Kabboul NN, Tomlinson G, Francis TA, et al. Comparative effectiveness of the Core components of cardiac rehabilitation on mortality and morbidity: a systematic review and network Meta-analysis. J Clin Med Dec 4 2018;7(12). 10.3390/jcm7120514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blumenthal JA, Sherwood A, Smith PJ, et al. Enhancing cardiac rehabilitation with stress management training: a randomized, clinical efficacy trial. Circulation Apr 5 2016;133(14):1341–1350. 10.1161/CIRCULATIONAHA.115.018926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lane MM, Davis JA, Beattie S, et al. Ultraprocessed food and chronic noncommunicable diseases: a systematic review and meta-analysis of 43 observational studies. Obesity Reviews 2021;22, e13146. 10.1111/obr.13146b. [DOI] [PubMed] [Google Scholar]
- 54.Forsyth A, Deane FP, Williams P. A lifestyle intervention for primary care patients with depression and anxiety: a randomised controlled trial. Psychiatry Res Dec 15 2015;230(2):537–544. 10.1016/j.psychres.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 55.Jacka FN, O’Neil A, Opie R, et al. A randomised controlled trial of dietary improvement for adults with major depression (the “SMILES” trial). BMC Med Jan 30 2017;15(1):23. 10.1186/s12916-017-0791-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Parletta N, Zarnowiecki D, Cho J, et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: a randomized controlled trial (HELFIMED). Nutr Neurosci Jul 2019;22(7):474–487. 10.1080/1028415X.2017.1411320. [DOI] [PubMed] [Google Scholar]
- 57.Hoffmann P Physical Activity and Mental Health 1st ed. Taylor & Francis. 1997:302. [Google Scholar]
- 58.Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. Physical activity and depression: towards understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev Dec 2019;107:525–539. 10.1016/j.neubiorev.2019.09.040. [DOI] [PubMed] [Google Scholar]
- 59.Kerling A, Kuck M, Tegtbur U, et al. Exercise increases serum brain-derived neurotrophic factor in patients with major depressive disorder. J Affect Disord Jun 2017;215:152–155. 10.1016/j.jad.2017.03.034. [DOI] [PubMed] [Google Scholar]
- 60.Voss MW, Vivar C, Kramer AF, van Praag H. Bridging animal and human models of exercise-induced brain plasticity. Trends Cogn Sci Oct 2013;17(10):525–544. 10.1016/j.tics.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.deVries HA. Tranquilizer effect of exercise: a critical review. Phys Sportsmed Nov 1981;9(11):46–55. 10.1080/00913847.1981.11711206. [DOI] [PubMed] [Google Scholar]
- 62.Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol Aug 5 2011;11(9):607–615. 10.1038/nri3041. [DOI] [PubMed] [Google Scholar]
- 63.Beavers KM, Brinkley TE, Nicklas BJ. Effect of exercise training on chronic inflammation. Clin Chim Acta Jun 3 2010;411(11−12):785–793. 10.1016/j.cca.2010.02.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lin K, Stubbs B, Zou W, et al. Aerobic exercise impacts the anterior cingulate cortex in adolescents with subthreshold mood syndromes: a randomized controlled trial study. Transl Psychiatry May 18 2020;10(1):155. 10.1038/s41398-020-0840-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ransford CP. A role for amines in the antidepressant effect of exercise: a review. Med Sci Sports Exerc 1982;14(1):1–10. 10.1249/00005768-198201000-00001. [DOI] [PubMed] [Google Scholar]
- 66.Rubin RT. Pharmacoendocrinology of major depression. Eur Arch Psychiatry Neurol Sci 1989;238(5–6):259–267. 10.1007/BF00449807. [DOI] [PubMed] [Google Scholar]
- 67.Sothmann MS, Ismail AH. Relationships between urinary catecholamine metabolites, particularly MHPG, and selected personality and physical fitness characteristics in normal subjects. Psychosom Med Nov-Dec 1984;46(6):523–533. 10.1097/00006842-198411000-00005. [DOI] [PubMed] [Google Scholar]
- 68.Sothmann MS, Ismail AH. Factor analytic derivation of the MHPG/NM ratio: implications for studying the link between physical fitness and depression. Biol Psychiatry May 1985;20(5):579–583. 10.1016/0006-3223(85)90032-0. [DOI] [PubMed] [Google Scholar]
- 69.Galbo H, Kjaer M, Stallknecht B, et al. Discussion: hormonal adaptation to physical activity. Exercise, Fitness and Health: A Consensus of Current Knowledge Champaign, Ill: Human Kinetics Publishers; 1990. p. 259–263. [Google Scholar]
- 70.Schuch FB, Vasconcelos-Moreno MP, Borowsky C, et al. The effects of exercise on oxidative stress (TBARS) and BDNF in severely depressed inpatients. Eur Arch Psychiatry Clin Neurosci Oct 2014;264(7):605–613. 10.1007/s00406-014-0489-5. [DOI] [PubMed] [Google Scholar]
- 71.Smith PJ, Blumenthal JA, Hoffman BM, et al. Aerobic exercise and neurocognitive performance: a meta-analytic review of randomized controlled trials. Psychosom Med Apr 2010;72(3):239–252. 10.1097/PSY.0b013e3181d14633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lederman O, Ward PB, Firth J, et al. Does exercise improve sleep quality in individuals with mental illness? A systematic review and meta-analysis. J Psychiatr Res Feb 2019;109:96–106. 10.1016/j.jpsychires.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 73.Schuch F, Vancampfort D, Firth J, et al. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis. J Affect Disord Mar 1 2017;210:139–150. 10.1016/j.jad.2016.10.050. [DOI] [PubMed] [Google Scholar]
- 74.Pearce M, Garcia L, Abbas A, et al. Association between physical activity and risk of depression a systematic review and meta-analysis. JAMA Psychiatry Jun 2022;79 (6):550–559. 10.1001/jamapsychiatry.2022.0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moore SC, Patel AV, Matthews CE, et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med 2012;9 (11), e1001335. 10.1371/journal.pmed.1001335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wen CP, Wai JP, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet Oct 1 2011;378(9798):1244–1253. 10.1016/S0140-6736(11)60749-6. [DOI] [PubMed] [Google Scholar]
- 77.Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med Jan 2005;28(1):1–8. 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 78.Hansford HJ, Wewege MA, Cashin AG, et al. If exercise is medicine, why don’t we know the dose? An overview of systematic reviews assessing reporting quality of exercise interventions in health and disease. Br J Sports Med Jun 2022;56(12): 692–700. 10.1136/bjsports-2021-104977. [DOI] [PubMed] [Google Scholar]
- 79.Miller WR, Rollnick Stephen. Motivational Interviewing: Helping People Change 3rd ed. The Guildford Press. 2013. [Google Scholar]
- 80.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med Aug 2003;26(1):1–7. 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 81.Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation Jul 27 2010;122(4):406–441. 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot Sep-Oct 1997;12(1):38–48. 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 83.Coleman KJ, Ngor E, Reynolds K, et al. Initial validation of an exercise “vital sign” in electronic medical records. Med Sci Sports Exerc Nov 2012;44(11):2071–2076. 10.1249/MSS.0b013e3182630ec1. [DOI] [PubMed] [Google Scholar]
- 84.2018 Physical Activity Guidelines Advisory Committee Scientific Report 2018.
- 85.Blumenthal JA, Rose S, Chang JL. Anorexia nervosa and exercise. Implications from recent findings. Sports Med Jul-Aug 1985;2(4):237–247. 10.2165/00007256-198502040-00001. [DOI] [PubMed] [Google Scholar]
- 86.Herman S, Blumenthal JA, Babyak M, et al. Exercise therapy for depression in middle-aged and older adults: predictors of early dropout and treatment failure. Health Psychol Nov 2002;21(6):553–563. [PubMed] [Google Scholar]
- 87.Blumenthal JA, Babyak MA, Craighead WE, et al. The role of comorbid anxiety in exercise and depression trials: secondary analysis of the SMILE-II randomized clinical trial. Depress Anxiety Feb 2021;38(2):124–133. 10.1002/da.23088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Blumenthal JA, Smith PJ, Jiang W, et al. Effect of exercise, escitalopram, or placebo on anxiety in patients with coronary heart disease: the understanding the benefits of exercise and escitalopram in anxious patients with coronary heart disease (UN-WIND) randomized clinical trial. JAMA Psychiatry Nov 1 2021;78(11):1270–1278. 10.1001/jamapsychiatry.2021.2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jacka FN, Mykletun A, Berk M, Bjelland I, Tell GS. The association between habitual diet quality and the common mental disorders in community-dwelling adults: the Hordaland health study. Psychosom Med Jul-Aug 2011;73(6):483–490. 10.1097/PSY.0b013e318222831a. [DOI] [PubMed] [Google Scholar]
- 90.Klimova B, Dziuba S, Cierniak-Emerych A. The effect of healthy diet on cognitive performance among healthy seniors - a mini review. Front Hum Neurosci 2020;14:325. 10.3389/fnhum.2020.00325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mykletun A, Overland S, Aaro LE, Liabo HM, Stewart R. Smoking in relation to anxiety and depression: evidence from a large population survey: the HUNT study. Eur Psychiatry Mar 2008;23(2):77–84. 10.1016/j.eurpsy.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 92.Breslau N, Novak SP, Kessler RC. Daily smoking and the subsequent onset of psychiatric disorders. Psychol Med Feb 2004;34(2):323–333. 10.1017/s0033291703008869. [DOI] [PubMed] [Google Scholar]
- 93.Baglioni C, Nanovska S, Regen W, et al. Sleep and mental disorders: a Meta-analysis of polysomnographic research. Psychol Bull Sep 2016;142(9):969–990. 10.1037/bul0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang S, Wu Y, Ungvari GS, et al. Sleep duration and its association with demographics, lifestyle factors, poor mental health and chronic diseases in older Chinese adults. Psychiatry Res Nov 2017;257:212–218. 10.1016/j.psychres.2017.07.036. [DOI] [PubMed] [Google Scholar]
- 95.Zschucke E, Gaudlitz K, Strohle A. Exercise and physical activity in mental disorders: clinical and experimental evidence. J Prev Med Public Health Jan 2013;46(suppl 1): S12–S21. 10.3961/jpmph.2013.46.S.S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Noordsy DL. Lifestyle Psychiatry 1st ed. American Psychiatric Association Publishing. 2019. [Google Scholar]
- 97.Malhi GS, Bell E, Bassett D, et al. The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry Jan 2021;55(1):7–117. 10.1177/0004867420979353. [DOI] [PubMed] [Google Scholar]
- 98.Stubbs B, Vancampfort D, Hallgren M, et al. EPA guidance on physical activity as a treatment for severe mental illness: a meta-review of the evidence and position statement from the European Psychiatric Association (EPA), supported by the International Organization of Physical Therapists in Mental Health (IOPTMH). Eur Psychiatry 2018;54:124–144. [DOI] [PubMed] [Google Scholar]
- 99.Bauer M, Pfennig A, Severus E, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: update 2013 on the acute and continuation treatment of unipolar depressive disorders. World J Biol Psychiatry Jul 2013;14(5):334–385. 10.3109/15622975.2013.804195. [DOI] [PubMed] [Google Scholar]
- 100.NICE. Depression in adults: treatment and management. 2023. www.nice.org.uk/guidance/ng222. [PubMed]
- 101.Blumenthal JA, Babyak MA, O’Connor C, Keteyian S, Landzberg J, Howlett J, Kraus W, Gottlieb S, Blackburn G, Swank A, Whellan DJ. Effects of exercise training on depressive symptoms in patients with chronic heart failure: the HF-ACTION randomized trial. JAMA 2012. Aug 1;308(5):465–474. 10.1001/jama.2012.8720. Erratum in: JAMA. 2012 Nov 7;308(17):1742. [DOI] [PMC free article] [PubMed] [Google Scholar]


