Abstract
Purpose
Non-communicable diseases (NCDs) have become a global health priority with a great need for prompt evidence-based preventing and managing interventions. Here, we describe the development of a comprehensive cohort study that provides the most accurate results for NCDs’ risk factors, named the Iran Cohort Study (ICS) to estimate the effect size of the risk factors associated with major NCDs.
Methods
This cohort is an observational prospective study, which its baseline data was gathered through the Iran STEPwise Approach to NCD Risk Factor Surveillance (STEPs) survey in 2016. Following the STROBE criteria, the protocols for investigation of several areas were developed. The follow-up phase began through telephone calls to estimate the effect size of socio-demographic, behavioral, and metabolic risk factors on the incidence of or death due to major NCDs during the three years of study period.
Delinerables
The main deliverables of ICS are planned to be as following; a comprehensive bank of primary data and follow-up data, national and subnational reports on estimation of the effect size of various risk factors, and a policy brief on the policy options and recommendations for promotion of ongoing programs and designing new interventions. Also, the collected data on the individuals’ health status will be sent to the participants as an electronic health record.
Conclusion
The present study is the first comprehensive national and sub-national representative cohort study on NCDs’ risk factors in Iranian adults. The results could be used for promotion of health planning and also future complementary studies and programs.
Keywords: Noncommunicable diseases, NCD, Population surveillance, Risk factors, Protocol, Cohort, STEPs, Iran
Introduction
The aging of population and the increasing exposure to non–communicable diseases’ (NCDs) risk factors have led to the raised burden of NCDs during the last three decades. It is remarkable that the slope of changes is steeper in developing countries [1–3]. The World Health Organization (WHO) recommended a comprehensive program for reducing 25% of unconditional probability of deaths due to four major NCDs including cardiovascular diseases (CVDs), diabetes mellitus, cancers, and chronic respiratory diseases (CRDs) by 2025. This reduction happens through effective management of tobacco use, unhealthy diet, lack of physical activity, and harmful alcohol use which urges countries to be aware of exposure to NCDs’ risk factors [4–7].
With an aim to a better prevention and control of adverse health outcomes of various risk factors, policymakers and health authorities need reliable evidence on the mortality and morbidity attributable to NCDs’ risk factors [8–10]. However, the absence of reliable information on the distribution of NCDs’ risk factors and their attributable burden remains a major concern in the developing countries [2, 11, 12]. The concern seems to be major in Iran considering its ambition to estimate NCDs risk factors distribution at the subnational levels [5, 7, 13, 14].
Addressing the superiority of the cohort studies in accurate detection of risk factors, we planned for a comprehensive cohort study to provide scientific evidence. In Iran, there have been many cross-sectional and cohort studies. However, most of them are limited to specific sub-populations that cannot be generalized to all country [15–18]. The WHO STEPwise approach to risk factor Surveillance (STEPs) provides a simple and standardized method for collecting, analyzing, and disseminating information on NCDs’ risk factors. The previous conducted STEPs survey in Iran (STEPs 2016) provided the baseline data of a nationally representative sample of Iranian adults including 30,541 participants [13]. The specific design and sampling method of Iran STEPs 2016 provided the maximum possibility to estimate the prevalence of NCDs and related risk factors [13].
Based on the developed capacities and benefiting from the unique large-scale database in STEPs survey 2016 [18], we planned for a comprehensive well-designed cohort study that provides the most accurate results for NCDs and risk factors, named the Iran Cohort Study (ICS). This manuscript provides the details of study design and implementation of the ICS cohort.
Material and methods
Study design
This cohort is an observational prospective study, which its baseline data was gathered through the Iran STEPs survey in 2016 [13]. After development of protocols covering several areas (information technology (IT), questionnaires and guide for interviewers, capacity building and training, supervision, sampling, feasibility assessment, statistical analyses, and ethical considerations), follow-up phase began through telephone calls to estimate the effect size of socio-demographic factors (age, sex, socio-economic situation, etc.), behavioral risk factors (physical inactivity, nutritional habits, smoking, etc.), and metabolic risk factors (diabetes, overweight/obesity, hypertension, high total cholesterol, etc.) on the incidence of or death due to cancers, ischemic heart diseases, cerebrovascular accidents, diabetes mellitus, and hypothyroidism during the three years of study period.
Study population
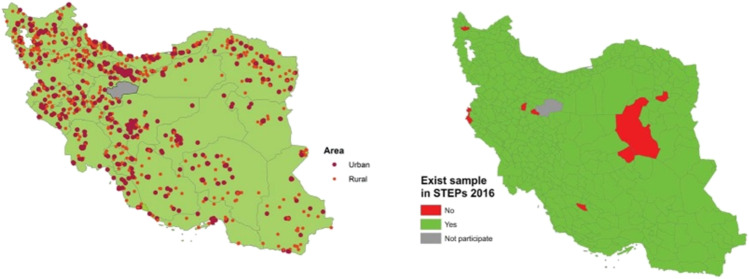
The ICS was designed to recruit the community-living individuals who participated in STEPs 2016 (Fig. 1). The eligibility criteria for the cohort were the Iranian nationality, age ≥ 18 years-old, living in the current place of residence for at least 6 months of year, being able to articulate their own opinion regarding participation in study, and self-report absence of pregnancy in women. The only exclusion criteria was unwillingness to continue collaboration. General characteristics of the participants in the baseline survey of the Iran STEPs 2016 are presented in Table 1.
Fig. 1.
The distribution of sampling point according to the participants’ residential areas
Table 1.
General characteristics of participants of the Iran Cohort Study in the baseline survey of Iran STEPs 2016
| Iran Cohort Participants | ||
|---|---|---|
| Male | Female | |
| Sex | 14,566 (48%) | 15,975 (52%) |
| Age (year) | ||
| 18–24 | 1261 (45%) | 1542 (55%) |
| 25–34 | 3426 (47%) | 3865 (53%) |
| 35–44 | 3137 (48%) | 3358 (52%) |
| 45–54 | 2638 (47%) | 2935 (53%) |
| 55–64 | 2100 (48%) | 2279 (52%) |
| 65–69 | 647 (45%) | 791 (55%) |
| 70≤ | 1357 (53%) | 1205 (47%) |
| Marital status | ||
| Never married | 18.0% (17.4–18.7) | 12.8% (12.3–13.4) |
| Married | 80.1% (79.4–80.8) | 73.6% (72.8–74.3) |
| Divorced | 0.8% (0.7–1.0) | 2.7% (2.4–2.9) |
| Widowed | 1.1% (0.9–1.3) | 10.9% (10.4–11.4) |
| Educational status | ||
| Illiterate | 9.7% (9.2–10.1) | 19.1% (18.5–19.7) |
| Primary school | 23.4% (22.7–24.1) | 25.1% (24.4–25.8) |
| Middle or high school | 43.8% (43.0–44.6) | 36.2% (35.5–37.0) |
| ≥ College | 23.2% (22.5–23.9) | 19.6% (19.0–20.3) |
| Occupation | ||
| Unemployed | 9.7% (9.2–10.2) | 3.2% (2.9–3.5) |
| Government employee | 8.4% (8.0–8.9) | 3.0% (2.7–3.3) |
| Government workers | 1.9% (1.6–2.1) | 0.2% (0.1–0.3) |
| Non-Government employee | 3.6% (3.3–3.9) | 1.9% (1.6–2.1) |
| Non-Government workers | 10.0% (9.5–10.6) | 0.8% (0.7–1.0) |
| Self-employee | 46.1% (45.2–46.9) | 3.6% (3.3–3.9) |
| Unpaid | 20.2% (19.5–20.9) | 87.2% (86.7–87.8) |
| Behavioral and metabolic risk factors | ||
| Current daily cigarette smoker | 20.1% (19.4–20.7) | 0.9% (0.8–1.1) |
| Lifetime alcohol drinker | 15.3% (14.6–15.9) | 1.3% (1.2–1.5) |
| Overweight and Obesity a | 53.6% (52.7–54.4) | 64.7% (63.9–65.5) |
| Hypertension b | 25.2% (24.4–25.9) | 27.6% (26.9–28.3) |
| Diabetes mellitus c | 9.9% (9.2–10.7) | 11.5% (10.7–12.2) |
| Hypercholesterolemia d | 19.2% (18.2–20.1) | 25.3% (24.3–26.3) |
| Hypertriglyceridemia e | 31.4% (30.3–32.5) | 25.1% (24.1–26.1) |
| Low HDL cholesterol f | 64.7% (63.6–65.9) | 73.7% (72.6–74.7) |
Values are presented as % or mean
aObesity was defined as a body mass index ≥25.0 kg/m2
bHypertension as treatment with medication or a systolic blood pressure reading of ≥140 mmHg or a diastolic blood pressure of ≥90 mmHg
cDiabetes mellitus as treatment with medication or fasting glucose level ≥ 126 mg/dL
dHypercholesterolemia as treatment with medication or a serum cholesterol level ≥ 200 mg/dL
eHypertriglyceridemia as a serum triacylglycerol level ≥ 150 mg/dL
flow HDL cholesterol as an HDL cholesterol level ≤ 40 mg/dL among males and ≤ 50 mg/dL among females
Study aim
To estimate the effect size of the risk factors of NCDs associated with CVDs, metabolic diseases, mental disorders, cancers, and injuries during the three years of study period.
Interested outcomes
The defined outcomes of interest are as following; cancers assessed by national cancer registry data and pathology data (ICD-10 codes C00-D46), ischemic heart diseases assessed by documents of inpatient/outpatient healthcare (ICD codes I20-I25), cerebrovascular accidents assessed by documents of inpatient/outpatient healthcare (ICD codes I60.00-I63.9), diabetes mellitus assessed by patient-provided laboratory results or assessment of anti-diabetic medications use (ICD-10 codes E10 and E11), hypothyroidism assessed by patient-provided laboratory results or investigation of Levothyroxine or Liothyronine use (ICD-10 code E03.9).
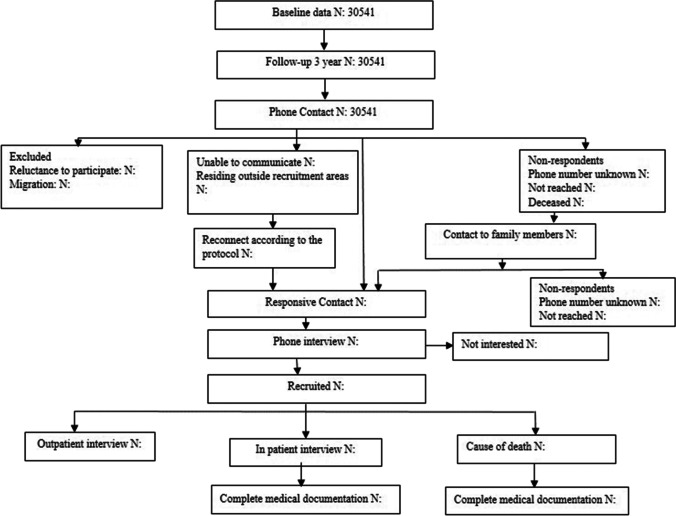
Data collection
Participants will be contacted using three levels of contacts information (participants, relatives, and their friends) that already have been collected through a designed algorithm (Fig. 2). After reaching out the participant and receiving the informed consent and verifying the individual, data collection will happen in three steps including; completion of the rapid target questionnaire via phone interviews, follow-up of participants with a positive response to the interested outcomes via a face to face interview, and complementary data gathering based on hospital or outpatient documents that are searched and attached by interviewers. These results will be reviewed by a multi-disciplinary scientific/adjudication committee to categorize events wisely. In addition to the direct follow-up, indirect follow-ups using secondary data sources such as the National Health Insurance claims database, National Death Statistics, and the National Cancer Registry are planned to obtain further information on health services utilization and mortality statistics.
Fig. 2.
The flowchart of study and recruitment of participants (The number of participants in the following steps of the cohort will be completed as the cohort goes on)
Measurements
Each participant will be contacted through on-time intervals to check for changes in address and phone number and to record measurements according to a predesigned protocol. For a period of three years, starting from the time of basic data gathering in 2016, interested variables will be gathered through the electronic questionnaires. Information about outpatient visits, hospitalization, and death due to study’s defined outcomes will be completed. Details of these three main measures are provided in Table 2.
Table 2.
Main outcome measures included in the study and the items included in each follow-up
| Main outcome measures | Interested variables | Items |
|---|---|---|
| Death | Place of death | Within home |
| Outdoor | ||
| Hospital | ||
| Cause of death | ||
| Outpatient visits of doctors and health centers | Diabetes and its complications | Kidney problems caused by diabetes |
| Eye problems caused by diabetes | ||
| Diabetic foot | ||
| Peripheral nerve problems caused by diabetes | ||
| Asthma and respiratory diseases | ||
| Hypothyroidism | ||
| Heart disease | Myocardial infarction | |
| Heart failure | ||
| Angina | ||
| High blood pressure | ||
| Stroke | ||
| Kidney problems | Dialysis | |
| Transplantation | ||
| Liver problems | Fatty liver | |
| Cirrhosis | ||
| Cancers | Bone, joints, and articular cartilage, Breast, Connective, subcutaneous and other soft tissues, Intestine and anus, Stomach, Liver, Other gastrointestinal cancers, Eyes, brain and other parts of the central nervous system, Cervix, Ovary, Other female genital cancers, Lips, oral cavity, pharynx, Lymph nodes (Hodgkin’s lymphoma) Lymph nodes (non-Hodgkin’s lymphoma), Testicles, Prostate, Other male genital cancers, Secondary and unidentified locations of leukemia, Other types of malignant neoplasms, expressed or presumably related to lymphoid, blood and tissue, Peripheral nerves and autonomic nervous system, Lung, Other parts of the respiratory system and organs inside the chest, Retroperitoneal and peritoneal melanoma, Other types of skin cancer, Thyroid, Other endocrine glands, Bladder, Kidney, Other parts of the urinary tract, Cancers with unknown Initial location | |
| Accidents and injuries | Fracture of one limb | |
| Fracture of several limbs | ||
| Internal injuries | ||
| Bruises and skin injuries | ||
| Brain injuries | ||
| Mental health | Depressive disorder | |
| Anxiety | ||
| Bipolar disorder | ||
| Obsessive-compulsive disorder | ||
| Schizophrenia | ||
| Nervous system | Parkinson’s | |
| Alzheimer’s or dementia | ||
| Musculoskeletal problems | Knee osteoarthritis | |
| Pelvic osteoarthritis | ||
| Hand osteoarthritis | ||
| Osteoarthritis of the neck | ||
| Back pain | ||
| Other related complications | ||
| Falling problem or falling due to old age and imbalance | Fracture | |
| Dislocation of limbs | ||
| Muscle contusion | ||
| Hospitalization | Causes of hospitalization | |
| Number of hospitalizations |
Quality control and supervision
Quality control and supervision processes of study are planned for different steps and stages of study to ensure the accuracy of data collection and the results. Survey monitoring and evaluation will be conducted directly and indirectly. To evaluate the performance of the questioners and the accuracy of the answers, we aim to re-ask a number of quality control questions.
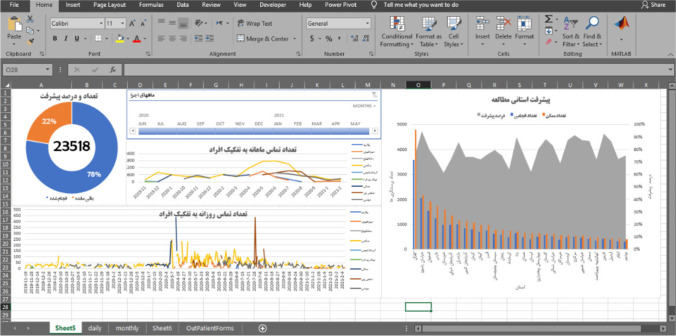
Some important selected parts of questions will be randomly chosen and the questionnaires will be compared with the recorded voices. In case of any discrepancies, the reason of the differences will be followed up and resolved by the study supervisor. Also, as the telephone interview is recorded with informed consent, a subset of each interviewer’ records will be randomly assigned to quality control. Overall progress monitoring and equipment management will be another part of the supervision process (Fig. 3).
Fig. 3.
Online supervision panel
Dissemination of findings
In all future publications, data will be reported according to the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) criteria [19]. The main deliverables of ICS are planned to be as following; a comprehensive bank of primary data and follow-up data, national and subnational reports on estimation of the effect size of demographic, socio-economic, behavioral, and metabolic risk factors on the incidence and death of CVDs, cancers, metabolic diseases, mental disorders, and injuries during the three years of study period, and a policy brief on the policy options and recommendations for promotion of ongoing programs and designing new required interventions and action plans. Also, the collected data on the individuals’ health status will be sent to the participants as an electronic health record (EHC), during the data collection and at the end of the follow-up process, with the aim of maintaining motivation and encourage of study participants and making a better monitoring of health status possible.
Ethical considerations
Ethical approval for the study was obtained from the Ethical Committee of National Institute for Medical Research Development (NIMAD). Participation in the study was voluntary. Prior to participation in study, the objectives and methods of the study will be described for all eligible individuals and verbal informed consent will be obtained from all those who accepted to participate. Their agreements for participation in the study will be recorded in the electronic follow-up system. Participants will be informed that they can withdraw from the study at any time.
Discussion
ICS is a comprehensive national and subnational representative cohort on NCDs risk factors in Iranian adults, estimating the effect size of the risk factors of major NCDs in Iran. In this cohort we have used a comprehensive approach which enables us to study the interactions between NCD risk factors that underlie the attributed health outcomes of Iranian adult population. The results of this study have the potential to contribute to improvements in strategies to prevent progression of NCDs’ adverse outcomes.
The United Nations (UN) and the WHO have called for a 25% reduction in mortality from NCDs in age groups of 30–70 years old, by 2025 compared to 2010, adopting the slogan “25 by 25” to comply with the Sustainable Development Goals (SDGs) set for 2030 [20]. In order to achieve these goals, one of the effective strategies is to focus on the public health interventions [21]. It is predicted that without any interventions, NCDs will impose a substantial human and economic burden in the next two decades [5, 15, 22–25].
Iran, as an in-transition country, tackled communicable diseases and now is confronting emerging challenges of NCDs in the path to reach health for everyone by 2030 [3, 13]. Available results of investigations in Iran confirmed that the incidence and prevalence of NCDs have increasing trends and account for nearly 80% of deaths and attributable disabilities [15, 22, 26–28]. To plan and conduct these interventions, we need an exact vision of distribution of metabolic and life style risk factors [5].
Considering the gap between research-based evidence in NCDs’ control policies and clinical decision making in many developing countries, designing and implementing reliable cohort studies could be very helpful to provide the required data for health decision makers. The comprehensive well-developed longitudinal prospective NCDs’ cohort is a unique resource for both descriptive and analytical studies, in the population undergoing control of NCDs. Therefore, the ICS was designed and conducted to contribute to evidence-based health policies [4, 13, 29].
As a matter of comprehensive approach and national and sun-national representativeness, the implementation of ICS, may be a considerable achievement of this STEPs follow up in Iran. Some specification of this experience could be pointed as its’ initiatives. Based on the software provisions of the study, it will be possible to send EHC, for all of study participation. EHC as an incentive for more participation, provides online access to biological tests results and anthropometric information besides relevant interpretations and suggestions for follow-up. The link to this EHC will be sent, automatically¸ to participants’ smart phones, through texts to allow them to access their record by visiting the SEPID system. For the participants without access to internet, reports will be mailed .
One of the main strengths of present cohort is its focus on the standard executive follow-up protocols proposed in the form of a comprehensive online regulatory. This package covers all required standards designed for different phases of the study. As a novelty, we should mention that yet no previous cohort study in Iran has been conducted based on this large-scale well-developed infrastructure of electronic survey. Additional to the comprehensive scientific and executive protocols that have been compiled from up-to-date scientific evidence, the web-based platform is a strong point of this study.
There are also some limitations we planned to control them. Probable levels of the lost to follow-up can lead to bias. We will use three levels of contact information to reach the participants actively. There is a chance of recall bias for the considerable time period between measurements and follow-up, which makes us consider death and hospitalization as main outcomes of our cohort. This approach enables us to reduce the levels of recall bias since we are going to use death certificate and hospital documents.
Conclusion
The present study introduces the first nationally and subnationally representative cohort study on NCDs’ risk factors in Iranian adults. Undoubtedly, development and management of the health programs require comprehensive evidence-based documents. So, future policies and health programming regarding NCDs could benefit from the findings of this investigation.
Acknowledgments
The authors would like to thank the research experts and staff of the Non-Communicable Diseases Research Center (NCDRC) for their valuable efforts in this study. We also thank for cooperation of all of participants who made this experience possible. The authors would like to thank NIMAD for providing the financial support of this study.
Authors’ contributions
Conceptualization: FF and SD. Writing – original draft: SD, SA, and FF. Writing – review & editing: SD, SA, NeR, and FF. Data curation and analysis: MRM, EG, MY, and SSM. Project administration: NaR, SN, AG, RH, and YF. All of the authors have read and approved the final manuscript. FF was the corresponding author of this manuscript and supervised all stages of the project and study conduction.
Funding
This study was supported by Grant No. 973048 from the National Institutes for Medical Research Development (NIMAD), Tehran, Iran.
Data availability
Not applicable.
Code availability
Not applicable.
Declarations
Ethics approval
Ethical approval for the study was obtained from the Ethical Committee of National Institute for Medical Research Development (NIMAD) (code: IR.NIMAD.REC.1397.513).
Consent to participate
All participants provided informed consent prior to participation in this study.
Consent for publication
All participants provided informed consent about publishing the results of this study anonymously.
Conflict of interest
The authors declare that they have no conflicts of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2013;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.Peykari N, Sepanlou SG, Djalalinia S, Kasaeian A, Parsaeian M, Ahmadvand A, et al. National and sub-national prevalence, trend, and burden of metabolic risk factors (MRFs) in Iran: 1990–2013, study protocol. Arch Iran Med. 2014;17(1):54–61. [PubMed] [Google Scholar]
- 3.Aminorroaya A, Fattahi N, Azadnajafabad S, Mohammadi E, Jamshidi K, Rouhifard Khalilabad M, et al. Burden of non-communicable diseases in Iran: past, present, and future. J Diabetes Metab Disord. 2020. 10.1007/s40200-020-00669-z.
- 4.NCD Risk Factor Collaboration Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19· 1 million participants. Lancet (London, England) 2017;389(10064):37. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peykari N, Hashemi H, Dinarvand R, Haji-Aghajani M, Malekzadeh R, Sadrolsadat A, et al. National action plan for non-communicable diseases prevention and control in Iran; a response to emerging epidemic. J Diabetes Metab Disord. 2017;16:3. doi: 10.1186/s40200-017-0288-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Azadnajafabad S, Mohammadi E, Aminorroaya A, Fattahi N, Rezaei S, Haghshenas R, et al. Non-communicable diseases' risk factors in Iran; a review of the present status and action plans. J Diabetes Metab Disord. 2021:1–9. 10.1007/s40200-020-00709-8. [DOI] [PMC free article] [PubMed]
- 8.Djalalinia S, Kelishadi R, Qorbani M, Peykari N, Kasaeian A, Saeedi Moghaddam S, et al. Suggestions for better data presentation in papers: an experience from a comprehensive study on national and sub-national trends of overweight and obesity. Arch Iran Med. 2014;17(12):830–836. [PubMed] [Google Scholar]
- 9.Varmaghani M, Sharifi F, Mehdipour P, Sheidaei A, Djalalinia S, Gohari K, et al. Prevalence of smoking among Iranian adults: findings of the national STEPs survey 2016. Arch Iran Med. 2020;23(6):369–377. doi: 10.34172/aim.2020.29. [DOI] [PubMed] [Google Scholar]
- 10.Global Burden of Disease Study 2019 (GBD 2019) Results [database on the Internet]: Institute for Health Metrics and Evaluation (IHME); 2020 [3 May 2021]. Available from: http://ghdx.healthdata.org/gbd-results-tool.
- 11.Farzadfar F, Danaei G, Namdaritabar H, Rajaratnam JK, Marcus JR, Khosravi A, et al. National and subnational mortality effects of metabolic risk factors and smoking in Iran: a comparative risk assessment. Popul Health Metrics. 2011;9(1):55. doi: 10.1186/1478-7954-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gakidou E, Afshin A, Abajobir AA, Abate KH, Abbafati C, Abbas KM, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1345–1422. doi: 10.1016/S0140-6736(17)32366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Djalalinia S, Modirian M, Sheidaei A, Yoosefi M, Zokaiee H, Damirchilu B, et al. Protocol Design for Large-Scale Cross-Sectional Studies of surveillance of risk factors of non-communicable diseases in Iran: STEPs 2016. Arch Iran Med. 2017;20(9):608–616. [PubMed] [Google Scholar]
- 14.Danaei G, Farzadfar F, Kelishadi R, Rashidian A, Rouhani OM, Ahmadnia S, et al. Iran in transition. Lancet. 2019;393(10184):1984–2005. doi: 10.1016/S0140-6736(18)33197-0. [DOI] [PubMed] [Google Scholar]
- 15.Nikbakht H-A, Rezaianzadeh A, Seif M, Ghaem H. Prevalence of metabolic syndrome and its components among a population-based study in south of Iran, PERSIAN Kharameh cohort study. Clinical Epidemiology and Global Health. 2020;8(3):678–83. doi: 10.1016/j.cegh.2020.01.001. [DOI] [Google Scholar]
- 16.Najafi F, Rezaei S, Hajizadeh M, Soofi M, Salimi Y, Kazemi Karyani A, et al. Decomposing socioeconomic inequality in dental caries in Iran: cross-sectional results from the PERSIAN cohort study. Arch Public Health. 2020;78:75. doi: 10.1186/s13690-020-00457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mansour-Ghanaei F, Joukar F, Naghipour M, Sepanlou S, Poustchi H, Mojtahedi K, et al. The PERSIAN Guilan cohort study (PGCS) Arch Iran Med. 2019;22(1):39. [PubMed] [Google Scholar]
- 18.Azadnajafabad S, Saeedi Moghaddam S, Mohammadi E, Rezaei N, Haghshenas R, Ghasemi E, et al. Importance of population-wide studies in controlling noncommunicable diseases: achievements of non-communicable diseases research center, endocrinology and metabolism research institute. J Diabetes Metab Disord 2020;20(1 (Special Issue, 25th Anniversary of the Foundation) #HD00276):25–34.
- 19.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):1–5. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.NCD Risk Factor Collaboration Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmidt H, Gostin L, Emanuel E. Public health, universal health coverage, and sustainable development goals: can they coexist? Lancet (London, England). 2015;386(9996):928. doi: 10.1016/S0140-6736(15)60244-6. [DOI] [PubMed] [Google Scholar]
- 22.Eghtesad S, Mohammadi Z, Shayanrad A, Faramarzi E, Joukar F, Hamzeh B, et al. The PERSIAN cohort: providing the evidence needed for healthcare reform. Arch Iran Med. 2017;20(11):691–695. [PubMed] [Google Scholar]
- 23.Djalalinia S, Saeedi Moghaddam S, Sheidaei A, Rezaei N, Naghibi Iravani SS, Modirian M, et al. Patterns of obesity and overweight in the Iranian population: findings of STEPs 2016. Front Endocrinol (Lausanne) 2020;11:42. doi: 10.3389/fendo.2020.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Djalalinia S, Kelishadi R, Qorbani M, Peykari N, Kasaeian A, Nasli-Esfahani E, et al. A systematic review on the prevalence of overweight and obesity, in Iranian children and adolescents. Iran J Pediatr. 2016;26(3):e2599. doi: 10.5812/ijp.2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Djalalinia S, Mehdipour P, Mohajer B, Mohebi F, Larijani B, Sepanlou SG, et al. Levels and trends of BMI, obesity, and overweight at national and sub-national levels in Iran from 1990 to 2016; a comprehensive pooled analysis of half a million individuals. Arch Iran Med. 2021;24(5):344–353. doi: 10.34172/aim.2021.51. [DOI] [PubMed] [Google Scholar]
- 26.Djalalinia S, Moghaddam SS, Peykari N, Kasaeian A, Sheidaei A, Mansouri A, et al. Mortality attributable to excess body mass index in Iran: implementation of the comparative risk assessment methodology. Int J Prev Med. 2015;6:107. doi: 10.4103/2008-7802.169075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fattahi N, Azadnajafabad S, Mohammadi E, Aminorroaya A, Rezaei S, Ghasemi E, et al. Geographical, gender and age inequalities in non-communicable diseases both at national and provincial levels in Iran. J Diabetes Metab Disord. 2021. 10.1007/s40200-020-00713-y.
- 28.Mohammadi E, Aminorroaya A, Fattahi N, Azadnajafabad S, Rezaei N, Farzi Y, et al. Epidemiologic pattern of cancers in Iran; current knowledge and future perspective. J Diabetes Metab Disord. 2021;20(1):825–829. doi: 10.1007/s40200-020-00654-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharifi A, Farzi Y, Roshani S, Ghamari A, Tabatabaei-Malazy O, Djalalinia S, et al. A new model for optimization of diabetes clinics with the case study in Iran. J Diabetes Metab Disord. 2022;21(1):817–22. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.