Abstract
Objective
Seated exercises could prove a safe alternative to traditional weight-bearing exercises in stroke, but its effects on mobility and modifiable risk factors of stroke are limited. The objective is to investigate the effects of seated exercises on balance, mobility, and cardiometabolic health in individuals living with a stroke.
Data sources
Medline, EMBASE, CINAHL, and Cochrane library were searched up to October 2022, in addition to the 2018 Evidence-Based Review of Stroke Rehabilitation.
Methods
Trials that incorporated predominantly seated exercises and outcomes of balance, mobility, or cardiometabolic health in those living with a stroke were included. Quality assessments of randomized controlled trials were done using the Cochrane Risk-of-Bias Tool.
Results
Seven trials were included in the review (n = 337) with five trials including participants < 6 months post-stroke. Seated exercises improved balance (standard mean difference (SMD) = 0.76; 95% confidence interval (CI), 0.50, 1.02) and mobility (SMD = 0.68; 95% CI, 0.24,1.13) outcomes compared with control. Sensitivity analysis of gait speed found no significant change (mean difference (MD) = 0.33 m/s; 95% CI, −0.23, 0.89) following seated exercises compared with control. One trial found no significant changes in blood pressure. Most trials (78%) were assessed as having some concern for bias.
Conclusion
These findings suggest beneficial effects of seated exercises on balance and mobility outcomes in those with a stroke, compared with standard therapy or an attention control. However, there is limited evidence on the effects of seated exercises on outcomes of cardiometabolic health, particularly prominent modifiable risk factors for stroke.
PROSPERO registration number
CRD42022307426.
Keywords: Mobility, balance, stroke, exercise
Introduction
Stroke is a leading cause of disability worldwide, with over 143 million living with a stroke-related disability. 1 While most stroke survivors will regain components of physical function, impairments in balance and mobility may persist or deteriorate in the chronic stages of stroke.2–4 This can lead to a reduced independence in daily living and quality of life,5,6 and increased sedentary lifestyle. 7 However, improvements in balance and mobility are a top priority for people living with stroke8,9 and a key motivator for engaging in exercise. 10
Walking and resistance exercises are demonstrated to improve outcomes of balance and gait in stroke.11,12 However, some individuals living with the consequences of stroke may be less inclined to participate in walking or resistance exercises due to functional impairments and limited access to supervised exercise sessions. In older adults, seated exercises are found to reduce the risk of falls following hospital discharge 13 and improve physical function and quality of life.14–16 However, reviews in older adults (with or without a chronic condition) have found no change in balance (Berg Balance Scale) or mobility (gait speed) outcomes following chair-based exercises,15,16 contrasting with trials in stroke.17,18 In stroke, Dean et al. 17 found improvements in reach distance following 2 weeks of seated exercises and Park et al. 18 found improvements in Berg Balance Scale and gait speed following 6 weeks of seated boxing. The contrasting findings identify the need to better understanding the effects of seated exercises in those living with stroke.
Within the first five years of a stroke, up to 32% (12% to 32%) of stroke survivors will have a recurrent stroke.19–21 Exercise interventions have shown beneficial effects on modifiable risk factors of stroke, with improvements observed in blood pressure, lipid profiles, and glucose. 22 However, evidence on seated exercises has predominately focused on physical function in older adults,14–16 with limited focus on modifiable risk factors in stroke.
With limited access to rehabilitation services, seated exercises may provide those with stroke a safe alternative to walking exercises, which may be delivered in home through telerehabilitation. In stroke, this systematic review will address the following question: Do seated exercises improve balance, mobility, and outcomes of cardiometabolic health?
Methods
This systematic review was registered with PROSPERO (International database for prospectively registered systematic reviews; CRD42022307426) and followed PRISMA specifications 23 (Supplemental Table 1).
Search strategy
The search strategy was developed in Ovid Medline. Databases Ovid Medline, EMBASE, Cumulative Index to Nursing and Allied Health Literature, and the Cochrane library (CENTRAL) were searched from inception to 28 January 2022. In addition, the 2018 updated version of the Evidence-Based Review of Stroke Rehabilitation was searched for present evidence in stroke rehabilitation. An updated search was completed on 25 October 2022 (Figure 1). The search strategy incorporated search terms from previous systematic reviews on chair-based and seated exercises15,16 (Supplemental Table 2). Medical Subject Headings and keywords relating to “sitting position,” “chair-based exercises,” or “seated exercises” were included in the search strategy. Limits to the search strategy included English language.
Figure 1.
PRISMA flow chart. *Additional articles identified at updated search on 25 October 2022.
Eligibility criteria
All articles (title, abstract, and full text screening) were screened independently by two reviewers (PM and JE). Title, abstract, and full text screening were reviewed against the inclusion and exclusion criteria detailed in Table 1. Eligibility criteria were determined using the Population, Intervention, Comparison, and Outcomes format and included study design and publication type to refine the inclusion and exclusion criteria. Relevant systematic reviews and scoping reviews were hand searched to identify additional eligible articles. Conflicts were resolved by authors (PM and JE).
Table 1.
Inclusion and exclusion criteria.
| Parameter | Inclusion | Exclusion |
|---|---|---|
| Population | - Adults living with a stroke | |
| Intervention | - Exercises completed primarily while
seated Exercises must be predominantly completed in a seated position Warm-ups and cool-downs could be completed in other positions - Interventions taking place for a minimum of 2 weeks A minimum of 4 sessions to be completed - Group-based or 1:1 exercise sessions |
- Exercise sessions continuously alternating between
different positions, e.g. sitting and standing - Exercises not completed on a chair or wheelchair, e.g. yoga ball, bike, floor - Technology based interventions (e.g. video games) - Non-exercise related training, e.g. cognitive tasks - Wheelchair training, e.g. wheeling training, arm-cycle ergometer |
| Comparison | - Any | |
| Outcomes | - Interventions must include a mobility, balance, or
cardiometabolic health outcome Mobility or balance outcome (objective or subjective), e.g. Berg Balance Scale, gait, activities of daily living etc. Cardiometabolic health outcome, e.g. blood pressure, glucose etc. - Outcomes can be secondary or exploratory |
|
| Study design and publication type | - Randomized controlled trials - Original research articles - Full text publications - Articles published in English |
- Systematic reviews and meta-analyses* - Scoping reviews* - Literature reviews* - Non-randomized trials - Pre-post trials - Abstracts (conference abstracts) - Trial protocols - Theses |
*References from relevant systematic reviews and meta-analysis, scoping reviews or literature reviews were hand searched.
Data extraction
Data was extracted by the lead author (PM) and verified independently by the second author for accuracy. Data extraction included: participant characteristics, study design, condition (experimental/intervention, control), intervention (number of sessions, types of exercises, intensity, duration), adherence, delivery method, outcomes. The Template for Intervention Description and Replication guidelines was used to report the interventions of included studies. 24
Quality assessment
Two reviewers independently assessed the methodological quality of included studies. The Cochrane Risk-of-Bias Tool (version 2.0) was used to assess the methodological quality of randomized controlled trials included in the meta-analysis. 25 Randomized control trials were judged as yes, probably yes, no, or probably no with the Cochrane Risk-of-Bias Tool and determined as low, high, or some concerns for risk of bias. Low risk of bias was determined when all domains were judged as having a low risk of bias. High risk was determined when at least one domain was judged as a high risk of bias, or multiple domains were judged as some concern.
Data syntheses
A meta-analysis was performed using Cochrane Review Manager (RevMan, Version 5.4.1, the Cochrane Collaboration 2020) where two or more studies reported an outcome (Ryan, 2016). Continuous data were calculated using mean differences (MDs) and 95% confidence intervals (95% CIs) when outcomes were measured and reported the same way or standard mean difference (SMD) and 95% CIs when outcomes were measured or reported in a different way. Median data were converted to mean ± standard deviation using standard formulas. 26 Fixed effect and random effects models were used and determined by statistical heterogeneity (I2). An I2 > 50% suggests considerable heterogeneity 27 and thus a random effect model was used when considerable heterogeneity was identified. Data collected immediately following the experimental condition or reported as the data set nearest the end of the experimental condition were included. Trials not included in the meta-analysis were reported descriptively.
Results
Initially, 1393 articles were identified at database searching and three articles were identified from additional sources. A final search on 25 October 2022, identified an additional 74 articles for screening. In total, 46 full-text articles were screened and seven articles were included in the review. Six trials were included in the meta-analysis. Figure 1 details the PRISMA chart.
Trials were predominately based in Australia (n = 2) and conducted in participants <6 months post-stroke (N = 5; inpatient and rehabilitation units). There were 337 participants across the seven studies (range, 12–160), of which 45% were female. Participants were predominately older adults (average 66 years old), with a mean age range of 60–74 years.
Seated exercises included mostly reaching and trunk balance tasks (n = 4). One trial included seated boxing training 18 and one included seated Tai Chi training. 28 Control groups included routine care or physical therapy,18,29–31 an attention control,28,32 or a combined attention control with routine physical therapy. 17 Interventions lasted from 2 to 12 weeks, with 57% of sessions completed five times a week. Sessions were 30–120 min in duration (mean: 50 min) and were mostly supervised (n = 5 trials). One trial included 1 week of supervised inpatient sessions, followed by 11 weeks of self-guided practice using pre-recorded videos. 28 Exercise intensity was reported in only one trial, 30 with exercises completed at a moderate intensity (Borg Rating of Perceived Exertion, 3-5). Two trials measured adherence, reporting on average 79% adherence rate to the interventions. Dropout rates were reported between 0% and 14% (Table 2).
Table 2.
Characteristics of included studies.
| Author (Country) | Study design | Participant characteristics | Experimental condition | Control condition | Mobility, balance, or cardiometabolic health outcomes |
|---|---|---|---|---|---|
| Büyükavcı et al., 2016 Turkey |
RCT |
N = 65 Inpatient stroke BBS: Exp: 17.8 ± 14.7 Con: 14.6 ± 10.7 Age: Exp: 62.6 ± 10.5 Con: 63.6 ± 10.4 Sex (F/M): 33/32 |
Seated trunk training in addition to standard stroke rehabilitation | Standard stroke rehabilitation |
Balance: Berg Balance Scale, Trunk Impairment Scale Mobility: Functional Independence Measurement (motor score), Rivermead Mobility Index Cardiometabolic health: Not measured |
| Dean et al, 2007 Australia |
RCT |
N = 12 First stroke (<3 months post-stroke) MAS: ≥ 3 (Item 3) Age: Exp: 60 ± 7 Con: 74 ± 12 Sex (F/M): 3/9 |
Sitting training (reaching) in addition to routine physiotherapy | Attention training (sham sitting) in addition to routine physiotherapy |
Balance: Maximum reach distance while sitting Mobility: Peak vertical force through affected foot (sit-to-stand), 10 m walk test Cardiometabolic health: Not measured |
| Dean et al, 1997 Australia |
RCT |
N = 20 Chronic stroke (≥ 1-year post-stroke) able to sit unsupported (≥ 20 min) Age: Exp: 68.2 ± 8.2 Con: 66.9 ± 8.2 Sex (F/M): 6/14 |
Sitting balance training | Attention training (sham sitting) |
Balance: Maximum reach distance while sitting Mobility: Peak vertical ground reaction force through affected foot (sit-to-stand), 10 m walk test Cardiometabolic health: Not measured |
| Gambassi et al, 2019 Brazil |
RCT |
N = 22 Chronic (>6 months) independent in ADL. Barthel index: Exp: 87.3 ± 11.9 Con: 90.0 ± 6.3 Age: Exp: 66.4 ± 10.1 Con: 60.5 ± 13.2 Sex (F/M): 13/9 |
Predominately seated resistance training in addition to Physical therapy (neurological) | Physical therapy (neurological) |
Balance: Not measured Mobility: 10 m walk test, timed up and go, 5 time sit-to-stand test Cardiometabolic health: Blood pressure |
| Park et al, 2017 Korea |
RCT |
N = 30 Stroke survivors (<6 months) independent in walking (10 m) BBS: Exp: 30.15 ± 12.75 Con: 26.62 ± 12.23 Age: NR Sex (F/M): NR |
Seated boxing exercises in addition to physical therapy | Physical therapy |
Balance: Berg Balance Scale, Good balance system (static balance) Mobility: 10 m walk test Cardiometabolic health: Not measured |
| Pollock et al, 2002 United Kingdom |
Pilot RCT |
N = 28 Inpatient (<6 weeks) Independent in sitting balance for 60 s Age: Exp: 73.1 ± 10.3 Con: 68.4 ± 13.4 Sex (F/M): 16/12 |
Independent practice of sitting balance (reaching tasks) in addition to standard physiotherapy | Standard physiotherapy |
Balance: Balance components (symmetry of weight distribution, maximum weight transference) Mobility: Not measured Cardiometabolic health: Not measured |
| Zhao et al, 2022 China |
RCT |
N = 160 Stroke survivor-caregiver dyads. Subacute stroke independent in sitting. NIHSS: Exp: 3.93 ± 2.02 Con: 4.16 ± 2.59 Age: Exp: 62.61 ± 12.88 Con: 63.35 ± 12.90 Sex (F/M): 79/81 |
Seated Tai Chi | Attention control |
Balance: Berg Balance Scale, Trunk Impairment Scale Mobility: Barthel Index (ADL) Cardiometabolic health: Not measured |
Data are presented as mean ± SD.
ADL: activities of daily living; BBS: Berg Balance Scale; Con: control condition; Exp: experimental condition; MAS: motor assessment scale; NIHSS: National Institutes of Health Stroke Scale; NR: not reported; RCT: randomized controlled trial; F: female; M: male.
Results of meta-analysis
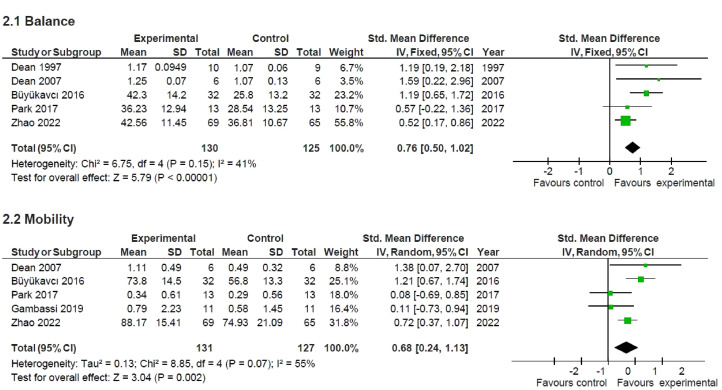
A meta-analysis of five trials for balance outcomes, including 255 participants was conducted (Figure 2 (2.1)). Overall, balance significantly improved (SMD = 0.76; 95% CI, 0.50, 1.02) following seated exercises compared with control. Two trials had data available on Berg Balance Scale (n = 224), two trials on sitting ability (n = 31; maximum reach distance), and two on Trunk Impairment Scale (n = 198). Individual forest plots show significant improvements in Berg Balance Scale (MD = 9.84; 95% CI 2.53, 17.14), reach distance (MD = 0.12; 95% CI, 0.06, 0.18), and Trunk Impairment Scale (MD = 4.32; 95% CI, 3.14, 5.49) following seated exercises (Figure 3 (3.1, 3.2 and 3.3, respectively)).
Figure 2.
Meta-analysis forest plots of balance and mobility. Standard mean difference and 95% CI of seated exercises compared with control on balance outcomes (2.1) and mobility outcomes (2.2).
Figure 3.
Meta-analysis forest plots of balance and mobility outcomes. Mean difference and 95% CI of seated exercises compared with control on Berg Balance Scale (3.1), maximum reach distance (3.2), Trunk Impairment Scale (3.3), gait speed (3.4), and sensitivity analysis of gait speed (3.5).
A meta-analysis of five trials for mobility outcomes, including 258 participants was conducted (Figure 2 (2.2)). Overall, mobility significantly improved (SMD = 0.68; 95% CI, 0.24, 1.13) following seated exercise compared with control. A trend for significant improvement was found for gait speed (MD = 0.32; 95% CI, 0.00, 0.64), as assessed by the 10 m walk test (n = 60; Figure 3 (3.4)). Two of the three trials were conducted in participants < 6 months post-stroke (n = 38). Sensitivity analysis (Figure 3 (3.5)) was conducted removing one trial reporting median data 30 and identified no significant difference in gait speed following seated exercise compared with control (MD = 0.33, 95% CI, −0.23, 0.89).
Trials reporting more than one balance or mobility outcome tended to show significant improvements in balance and mobility following seated exercises compared with control (Table 3). Insufficient trials were available on cardiometabolic health outcomes to be included in the meta-analysis. Only one trial 30 reported cardiometabolic health outcomes and found 8 weeks of seated resistance exercises (moderate intensity) did not significantly change systolic or diastolic blood pressure compared with physical therapy. However, following the 8-week trial, systolic and diastolic blood pressure were 10.4 and 8.2 mmHg lower, respectively, in the exercise group compared to control. 30
Table 3.
Characteristics and results of seated exercises used as the experimental condition.
| Author | Description of intervention | Intervention length (weeks) | Number of sessions | Duration of sessions (min) | Intensity | Adherence Dropouts | Intervention delivery | Results |
|---|---|---|---|---|---|---|---|---|
| Büyükavcı et al, 2016 | Trunk balance tasks completed at five stations. Upper and lower extremity tasks (reaching and pushing) with a task including use of a games console (Wii fit). | 3 | Daily | 120 | NR | Adherence: NR Dropouts: 1 |
Supervised (by author) individual session within inpatient rehabilitation unit | Significant ↑ in BBS, FIM, and RMI at 3 months
post-assessment, compared with control. Significant ↑ BBS, TIS, FIM, and RMI at 3 months compared to pre-assessment. |
| Dean et al 2007 | Seated reaching tasks (beyond arm's length) with a focus on co-ordinated movements and loading through the affected foot during tasks. | 2 | 10 | 30 | NR | Adherence: NR Dropouts: 0 |
Supervised (by author) individual coaching | Significant ↑ in reach distance (immediately post and 6
months post) compared with control Significant ↑ in peak vertical force compared with control Trend for ↑ in walking speed (non-significant) |
| Dean et al, 1997 | Seated reaching tasks (beyond arm's length) with a focus on co-ordinated movements and loading through the affected foot during tasks. | 2 | 10 | 30 | NR | Adherence: NR Dropouts: 1 |
Home-based individual coaching supervised by author | Significant ↑ in reach distance (all directions) compared
with control and following the sitting balance
intervention Significant ↑ in peak vertical force following sitting balance intervention ↔ 10 m walk test |
| Gambassi et al, 2019 |
Predominately seated resistance exercises (squats, seated row, knee extensions, seated vertical chest press) with resistance bands and weights. | 8 | 2/week |
NR | Moderate intensity (RPE, 3-5 on 1-10 Borg scale) | Adherence: NR Dropouts: 0 |
Researcher lead | Resistance training significantly improved 5STS and TUG
compared to control. 10 m walk test, TUG, and 5STS significantly improved following resistance training. ↔ in blood pressure. |
| Park et al, 2017 | Predominately seated boxing exercises against a sandbag and mitt. During final 2 weeks, boxing exercises were completed in a seated and standing position | 6 | 3/week | 30 | NR | Adherence: NR Dropouts: 2 |
Group exercises in rehabilitation settings | Significant ↑ in BBS following 6 weeks boxing training and
compared with control Significant ↓ in 10 m walk duration (s) following 6 weeks boxing training and compared with control Significant ↓ in static balance sway and velocity (mm/s; eyes open) following 6 weeks boxing training Significant ↓ in static balance sway (mm/s; eyes closed) following 6 weeks boxing training |
| Pollock et al, 2002 | Independent practice of reaching tasks with guided instructions. Tasks involved constructing vertical poles, stacking, color-coded placement tasks. | 4 | 5/week | NR | NR | Adherence: 80%
a
Dropouts: 4 |
Independent practice | ↔ between groups in symmetry of weight
distribution Significantly ↓ participants achieved normal weight distribution when reaching on the affected side (in sitting) compared with control |
| Zhao et al, 2022 | Seated Tai Chi, 10-form for stroke. | 12 | 36 3/week |
40 | NR | Adherence: 78.8% Dropouts: 11 (13.8%) |
Inpatient with Tai Chi master (3 sessions) followed by self-guided with pre-recorded videos | Significant ↑ in BBS following 12 weeks seated Tai Chi
compared with control Significant ↑ in TIS following 12 weeks seated Tai Chi compared with control Significant ↑ in BI following 12 weeks seated Tai Chi compared with control |
BBS: Berg Balance Scale; BI: Barthel Index; FIM: Functional Independence Measure; RMI: Rivermead Mobility Index; TIS: Trunk Impairment Scale; TUG: timed up and go; 5STS: 5 × sit-to-stand; NR: not reported; RPE: rating of perceived exertion.
↔ = no change; ↑ = increase; ↓ = decrease.
Median percentage sessions attended.
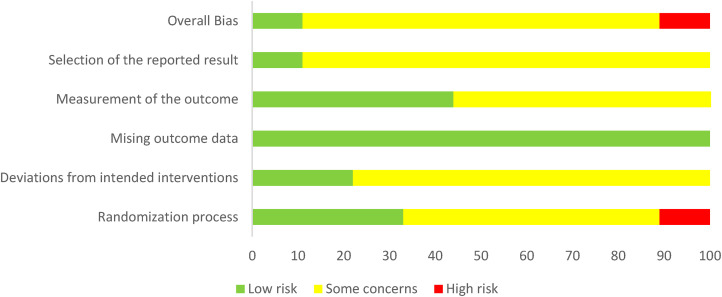
Risk of bias in trials
Of the trials included in the meta-analysis, approximately 78% were assessed as having some concerns for bias and 11% as high risk of bias (Figure 4). There was some concern for bias in 89% of trials in the “selection of the reported results” domain, as no pre-defined analysis was identified. One trial had high risk of bias due to reduced clarity in the randomization procedure. 30 There was low risk of bias in all trails in the “missing outcome data” domain.
Figure 4.
Risk of bias of studies using Cochrane Risk of Bias Tool (V2).
Discussion
The results from this systematic review demonstrate that seated exercises improve outcomes of balance and mobility in stroke survivors (n = 337) compared with physical therapy or an attention control. However, one trial reported outcomes of cardiometabolic health, demonstrating no improvement in blood pressure compared with physical therapy. Although balance and mobility outcomes improved with seated exercises, trials (78%) were deemed to have some concern for bias.
Seated exercises are reported to be safe and effective at improving physical function in nursing home residents 33 and reduce the risk of falls following hospital discharge in older adults. 13 This review found self-guided and supervised in-home seated exercise sessions to improve balance and mobility outcomes in those with an acute or chronic stroke. As many living with stroke may have limited access to rehabilitation services, seated exercises may be a safe alternative to weight-bearing exercises that could be incorporated into home settings and delivered via telerehabilitation.
The improvements in balance and mobility contrast with previous systematic reviews investigating the effects of seated exercises in older adults with or without a chronic condition.15,16 Though Klempel et al. 16 and Sexton and Taylor 15 did not report baseline function, a greater capacity for change in the current review due to balance deficits (Berg Balance Scale score 18–30) and time post stroke (n = 5 trials < 6 months) could reflect the difference in findings. This was further identified by the large increase in Berg Balance Scale score (MD, 9.84) following seated exercises in the current review. This increase exceeds the benefits found following walking (MD, 2.99) and resistance exercises (MD, 3.27) in those with stroke. 12 Thus, incorporating seated exercises in the early stages of stroke could benefit balance outcomes.
Improvements in gait speed following upper extremity seated exercises are suggested to be associated with improvements in weight-bearing capacity and trunk mobility. 34 While seated reaching tasks have been found to sufficiently increase peak vertical force and muscle activation in the lower extremities post-stroke, increased activation did not convert into changes in gait.17,32 Sensitivity analysis in this review found no significant change in gait speed following seated exercises, which is consistent with findings in older adults (with or without a chronic condition). 16 These findings could be reflected by the absence of task-specific training, 35 with most seated exercises (75%) including trunk training or reaching tasks. However, the 0.33 m/s increase in gait speed exceeds the minimum for clinical change in subacute stroke patients (0.16 m/s), 36 identifying potential clinical importance. Thus, incorporating seated exercises with explicit weight-bearing activities may better transfer to improvements in gait speed.
Outcomes of cardiometabolic health are vital in managing stroke risk, with hypertension the foremost modifiable risk factor in stroke. 37 In this review, one trial found no improvement in blood pressure following moderate intensity seated exercises compared with physical therapy. 30 However, after 8 weeks, Gambassi et al. 30 observed lower systolic (−10.4 mmHg) and diastolic blood pressure (−8.2 mmHg) in the exercise group than control. Similar findings have been reported following aerobic exercise (systolic, −4.3 mmHg; diastolic, −2.6 mmHg 38 ) and pharmacological treatments in stroke (systolic, −5.1 mmHg; diastolic, −2.5 mmHg 39 ). Therefore, incorporating seated exercises in stroke management plans could improve blood pressure control, particularly in those with limited mobility and at increased risk of falls.
A key strength of this review was the inclusion of modifiable risk factors of stroke that have not been included in previous reviews investigating seated exercises.15,16 However, some limitations need to be considered. Most trials did not report the intensity of and adherence to seated exercise sessions. Small samples sizes and limited number of trials included in the meta-analysis may result in an underestimation of effects of seated exercises. Further, the concern for bias in trials could lead to an overstatement in findings. Lastly, excluding technology-based interventions (e.g. video games) may have limited the number of eligible trials, particularly due to the increase in technology-based interventions since the COVID-19 Pandemic in 2020.
The findings from this review suggest seated exercises may improve outcomes of balance and mobility in those living with stroke. While seated exercises did not improve cardiometabolic health, the changes observed following seated exercises could suggest clinical importance. Thus, seated exercises when compared with physical therapy or an attention control could show clinical importance on balance, mobility, and cardiometabolic health in those living with a stroke.
Clinical messages.
Seated exercises can be beneficial on balance and mobility in acute and chronic stroke.
Reaching tasks and trunk balance training improve balance, while task-specific training may be more beneficial for mobility outcomes.
Supplemental Material
Supplemental material, sj-docx-1-cre-10.1177_02692155221150002 for The influence of seated exercises on balance, mobility, and cardiometabolic health outcomes in individuals living with a stroke: A systematic review and meta-analysis by Paul Mackie and Janice J Eng in Clinical Rehabilitation
Supplemental material, sj-docx-2-cre-10.1177_02692155221150002 for The influence of seated exercises on balance, mobility, and cardiometabolic health outcomes in individuals living with a stroke: A systematic review and meta-analysis by Paul Mackie and Janice J Eng in Clinical Rehabilitation
Footnotes
Author contributions: PM and JE completed all stages of the review: conception, design, screening and extraction, quality assessments, analysis and interpretation, manuscript development and finalization.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Michael Smith Foundation for Health Research (Fellowship to PM); Canadian Institutes of Health Research Foundation Grant (FDN 143340 to JE); and the Canada Research Chairs Program (to JE).
ORCID iDs: Paul Mackie https://orcid.org/0000-0001-5840-4348
Janice J Eng https://orcid.org/0000-0001-9783-7568
Supplemental material: Supplemental material for this article is available online.
References
- 1.Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 2021; 20: 795–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van de Port IGL, Kwakkel G, van Wijk I, et al. Susceptibility to deterioration of mobility long-term after stroke: a prospective cohort study. Stroke 2006; 37: 167–171. [DOI] [PubMed] [Google Scholar]
- 3.Mayo NE, Wood-Dauphinee S, Côté R, et al. Activity, participation, and quality of life 6 months poststroke. Arch Phys Med Rehabil 2002; 83: 1035–1042. [DOI] [PubMed] [Google Scholar]
- 4.Stig Jørgensen H, Nakayama H, Raaschou HO, et al. Stroke: neurologic and functional recovery the Copenhagen stroke study. Phys Med Rehabil Clin N Am 1999; 10: 887–906. [PubMed] [Google Scholar]
- 5.Schmid AA, Van Puymbroeck M, Altenburger PA, et al. Balance is associated with quality of life in chronic stroke. Top 2013; 20: 340–346. [DOI] [PubMed] [Google Scholar]
- 6.Buvarp D, Rafsten L, Sunnerhagen KS. Predicting longitudinal progression in functional mobility after stroke. Stroke 2020; 51: 2179–2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallanagh S, Quinn TJ, Alexander J, et al. Physical activity in the prevention and treatment of stroke. ISRN Neurol 2011; 2011: 953818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eng JJ, Bird M-L, Godecke E, et al. Moving stroke rehabilitation research evidence into clinical practice: consensus-based core recommendations from the stroke recovery and rehabilitation roundtable. Neurorehabil Neural Repair 2019; 33: 935–942. [DOI] [PubMed] [Google Scholar]
- 9.Rudberg A-S, Berge E, Laska A-C, et al. Stroke survivors’ priorities for research related to life after stroke. Top 2021; 28: 153–158. [DOI] [PubMed] [Google Scholar]
- 10.Simpson LA, Eng JJ, Tawashy AE. Exercise perceptions among people with stroke: barriers and facilitators to participation. Int J Ther Rehabil 2011; 18: 520–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saunders D, Greig C, Mead G. Physical activity and exercise after stroke: review of multiple meaningful benefits. Stroke 2014; 45: 3742–3747. [DOI] [PubMed] [Google Scholar]
- 12.Saunders DH, Sanderson M, Hayes S, et al. Physical fitness training for stroke patients. Cochrane Database Syst Rev 2020; 3: CD003316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vogler CM, Sherrington C, Ogle SJ, et al. Reducing risk of falling in older people discharged from hospital: a randomized controlled trial comparing seated exercises, weight-bearing exercises, and social visits. Arch Phys Med Rehabil 2009; 90: 1317–1324. [DOI] [PubMed] [Google Scholar]
- 14.Anthony K, Robinson K, Logan P, et al. Chair-based exercises for frail older people: A systematic review. Biomed Res Int 2013; 2013: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sexton BP, Taylor NF. To sit or not to sit? A systematic review and meta-analysis of seated exercise for older adults. Australas J Ageing2019; 38: 15-27. [DOI] [PubMed] [Google Scholar]
- 16.Klempel N, Blackburn NE, McMullan IL, et al. The effect of chair-based exercise on physical function in older adults: a systematic review and meta-analysis. Int J Environ Res Public Health 2021; 18: 1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dean CM, Channon EF, Hall JM. Sitting training early after stroke improves sitting ability and quality and carries over to standing up but not to walking: a randomised trial. Australian J Physiotherapy 2007; 53: 97–102. [DOI] [PubMed] [Google Scholar]
- 18.Park J, Gong J, Yim J. Effects of a sitting boxing program on upper limb function, balance, gait, and quality of life in stroke patients. NeuroRehabilitation 2017; 40: 77–86. [DOI] [PubMed] [Google Scholar]
- 19.Stahmeyer JT, Stubenrauch S, Geyer S, et al. The frequency and timing of recurrent stroke: an analysis of routine health insurance data. Dtsch Arztebl Int 2019; 116: 711–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hardie K, Hankey GJ, Jamrozik K, et al. Ten-year risk of first recurrent stroke and disability after first-ever stroke in the Perth community stroke study. Stroke 2004; 35: 731–735. [DOI] [PubMed] [Google Scholar]
- 21.Flach C, Muruet W, Wolfe CDA, et al. Risk and secondary prevention of stroke recurrence. Stroke 2020; 51: 2435–2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.D’Isabella NT, Shkredova DA, Richardson JA, et al. Effects of exercise on cardiovascular risk factors following stroke or transient ischemic attack: a systematic review and meta-analysis. Clin Rehabil 2017; 31: 1561–1572. [DOI] [PubMed] [Google Scholar]
- 23.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev 2021; 10: 89. DOI: 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Br Med J 2014; 348: g1687. [DOI] [PubMed] [Google Scholar]
- 25.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Br Med J 2019; 366: I4898. [DOI] [PubMed] [Google Scholar]
- 26.Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014; 14: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deeks Jj HJPTADG. Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins Jpt TJCJCMLTPMJWVA (ed) Cochrane Handbook for Systematic Reviews of Interventions version 63 (updated February 2022). Cochrane, 2022.
- 28.Zhao J, Chau JPC, Chan AWK, et al. Tailored sitting Tai Chi Program for subacute stroke survivors: a randomized controlled trial. Stroke 2022; 53: 2192–2203. [DOI] [PubMed] [Google Scholar]
- 29.Buyukavci R, Sahin F, Sag S, et al. The impact of additional trunk balance exercises on balance, functional condition and ambulation in early stroke patients: randomized controlled trial. Turkiye Fiziksel tip ve Rehabilitasyon Dergisi 2016; 62: 248–256. [Google Scholar]
- 30.Gambassi BB, CoelhoJunior HJ, Paixao Dos Santos C, et al. Dynamic resistance training improves cardiac autonomic modulation and oxidative stress parameters in chronic stroke survivors: a randomized controlled trial. Oxid Med Cell Longevity 2019; 2019: 5382843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pollock AS, Durward BR, Rowe PJ, et al. The effect of independent practice of motor tasks by stroke patients: a pilot randomized controlled trial. Clin Rehabil 2002; 16: 473–480. [DOI] [PubMed] [Google Scholar]
- 32.Dean CM, Shepherd RB. Task-related training improves performance of seated reaching tasks after stroke. A randomized controlled trial. Stroke 1997; 28: 722–728. [DOI] [PubMed] [Google Scholar]
- 33.Cordes T, Schoene D, Kemmler W, et al. Chair-based exercise interventions for nursing home residents: a systematic review. J Am Med Dir Assoc 2021; 22: 733–740. [DOI] [PubMed] [Google Scholar]
- 34.Eng JJ, Tang P-F. Gait training strategies to optimize walking ability in people with stroke: a synthesis of the evidence. Expert Rev Neurother 2007; 7: 1417–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bayona NA, Bitensky J, Salter K, et al. The role of task-specific training in rehabilitation therapies. Top 2005; 12: 58–65. [DOI] [PubMed] [Google Scholar]
- 36.Tilson JK, Sullivan KJ, Cen SY, et al. Meaningful gait speed improvement during the first 60 days poststroke: minimal clinically important difference. Phys Ther 2010; 90: 196–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O'Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 2016; 388: 761–775. [DOI] [PubMed] [Google Scholar]
- 38.Wang C, Redgrave J, Shafizadeh M, et al. Aerobic exercise interventions reduce blood pressure in patients after stroke or transient ischaemic attack: a systematic review and meta-analysis. BJSM online 2019; 53: 1515–1525. [DOI] [PubMed] [Google Scholar]
- 39.Liu L, Wang Z, Gong L, et al. Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res 2009; 32: 1032–1040. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-cre-10.1177_02692155221150002 for The influence of seated exercises on balance, mobility, and cardiometabolic health outcomes in individuals living with a stroke: A systematic review and meta-analysis by Paul Mackie and Janice J Eng in Clinical Rehabilitation
Supplemental material, sj-docx-2-cre-10.1177_02692155221150002 for The influence of seated exercises on balance, mobility, and cardiometabolic health outcomes in individuals living with a stroke: A systematic review and meta-analysis by Paul Mackie and Janice J Eng in Clinical Rehabilitation