Abstract
Background and aim
Age-related hearing loss has potential effects on communication, cognitive, emotional, and social aspects of the older person’s life. Evaluating the role of hearing aids in reducing these difficulties is important. This study aimed to evaluate communication difficulties, self-perceived handicaps, and depression in hearing-impaired older adults who are either hearing aid users or non-users.
Methods
A total of 114 older adults in the age range of 55–85 years with moderate to moderately severe hearing loss (two hearing-matched groups; hearing aid users: n = 57; hearing aid non-users: n = 57) took part in this study during the COVID-19 pandemic. Self-perceived hearing handicaps and communication were evaluated using the Hearing Handicap Inventory in the Elderly-Screening (HHIE-S) and Self-Assessment Communication (SAC) questionnaires. Depression was assessed using the geriatric depression scale (GDS).
Results
The average score of HHIE-S was significantly higher in the hearing aid users than the non-users (16.61 ± 10.39 vs. 12.49 ± 9.84; p = 0.01). Differences between groups were not significant for SAC or GDS scores (p ≥ 0.05). There were strong positive correlations between HHIE-S and SAC scores in both groups. Moderate correlations were found between SAC and GDS scores in the hearing aid users and between the duration of using hearing aid with SAC and HHIE-S scores.
Conclusion
It seems that self-perceived handicaps, communication difficulties and depression are affected by many factors, and only receiving hearing aids without subsequent support such as auditory rehabilitation and programming services cannot bring the expected output. The effect of these factors was clearly observed due to reduced access to services in the COVID-19 era.
Keywords: Age-related hearing loss, Communication problems, Self-perceived handicaps, Depression
Introduction
Age-related hearing loss or presbycusis is a prevalent sensory disorder among geriatrics. Approximately one-third of the elderly population experience moderate to severe hearing loss [1, 2]. The consequences of ineffective communication in hearing-impaired people are not unexpected. It has been established that age-related hearing loss may impact the communication, cognitive, emotional, and social aspects of the elderly population’s life [2, 3]. These people might experience additional psychological problems such as social isolation, loneliness, and depression, which reduce their quality of life as a result of hearing loss, as well as communication disorders [4]. Nonetheless, this situation appears to be variable among a geriatric population of diverse cultures. The subjective experience of hearing problems seems to be a crucial factor, and hearing loss itself does not necessarily parallel the self-perception of a social or an emotional disability or handicap in the everyday lives of the older adults [1]. It has been demonstrated that several factors affect self-perceived handicap, such as marital status (widowed) and self-perceived general health. Therefore, in addition to hearing impairments, information on self-perceived hearing handicaps is essential for identifying older individuals who require supplementary hearing rehabilitation services [1].
The primary management option for hearing loss in older adults is the use of hearing aids. However, it appears that not everyone pursues effective communication troubleshooting. In Jalilvand et al.’s (2008) study, only two of 59 older adults with hearing loss used hearing aids [5] despite having a self-perceived disability. Several studies have investigated the role of hearing aids on self-perceived handicap and presented contradictory findings about the effectiveness of hearing aids in reducing handicaps [6–17]. It appears that self-perceived handicap, rather than hearing loss, is an important factor in hearing aid utilization and demand. In a study by Chang et al. (2007) on subjects with moderate to profound hearing impairment, 45.4% of those with a self-perceived hearing handicap used hearing aids or felt the need to use hearing aids, whereas only 5% of those without a hearing handicap used or needed hearing aids. Screening for self-perceived hearing handicaps, therefore, is an important part of hearing screening tests for identifying older adults with a high need for further hearing evaluation and/or rehabilitation [1].
Meanwhile, a number of research studies have investigated the impact of hearing aids on self-perceived handicap and communication difficulties. In a 2009 study conducted by Lotfi et al. on 350 hearing-impaired individuals using the Hearing Handicap Inventory in the Elderly-Screening (HHIE-S) to measure self-perceived handicap, it was revealed that hearing aid use significantly enhanced HHIE-S scores after at least three months of use. The overall HHIE-S score was 65.88% before using hearing aids, which decreased to 22.1% following three months of hearing aid use. The degree of hearing loss in 95% of this population was moderate to severe. Regarding communication difficulties, in a study on 30 disabled hearing aid users and 10 control participants, it was concluded that if people use hearing aids for at least one month, their communication problems, as measured by the SAC/SOAC questionnaire, will decrease significantly. Within six months of utilizing appropriate hearing aids, the communication abilities of older adults with moderate hearing loss are comparable to those of their contemporaries [18]. However, among this large body of evidence, some studies failed to provide evidence that hearing aid use reduces handicaps [6–8, 17]. A systematic review also revealed low- to very-low-quality evidence supporting the use of hearing aids for the management of auditory rehabilitation in adults. There was evidence of a statistically, but not clinically, significant long-term effect; however, there was no evidence of a short- to medium-term effect [19].
In addition to handicaps, the role of hearing aid in minimizing the emotional and psychological consequences of hearing loss has also been extensively investigated [9–11, 14, 15, 20–25]. A study on 192 older adults, showed that sustained use of hearing aid for 12 months significantly improved self-perceived handicap, communication problems and depression [15]. Some suggest that hearing disability and handicap are associated with reduced well-being and depression in the geriatric population, and hearing aid helps alleviate the older adults’ difficulties [9]. However, in a clinical trial, Metselaar et al. (2009) found that in contrast to the long-term effect of hearing aid on handicaps, the incidence of depression did not alter following hearing-aid fitting [24]. This study aimed to compare the self-perceived handicap, communication problems, and depression between older adults who are hearing aid users and non-users.
Methods
Participants
Overall, 114 participants between the ages of 55 and 85 (57 hearing aid users and 57 non-users) who were referred to a public or private audiological clinic were invited to participate in this cross-sectional study. They were selected based on our inclusion criteria of having symmetrical sensorineural hearing loss, inter-aural threshold differences smaller than 10 dB and no other otological disease. The degree of hearing loss was determined based on the average of the four main frequencies (500, 1000, 2000 and 4000 Hz), and its classification was considered based on the conventional classification, including moderate to moderately severe hearing loss [26]. Therefore, only individuals with an average hearing loss between 41 and 70 dB and a speech recognition score of at least 70% were included in the study. Since the degree of hearing loss and speech recognition affects the degree of disability and communication [27], a limited range was carefully considered. Hearing aid users were selected based on whether they had at least six months of unilateral or bilateral usage.
Data collection
Questionnaires
Demographic and clinical information was gathered using standardized self-questionnaires and interviews. Demographic data about age, gender, the duration of hearing aid use, and daily hours of hearing aid use were collected. The SAC and HHIE-S were used to assess communication and handicap problems, and the Geriatric Depression Scale (GDS) was used to evaluate depression. The order in which the questionnaires were filled out was random.
Self-assessment communication questionnaire
The SAC questionnaire consists of 10 questions designed to assess the communication, emotional and social effects of hearing loss. The frequency of problems for each question is scored on a five-point scale. Items 1–6 are related to communication problems in various situations, items 7 and 8 are related to the person’s general feelings about their hearing problem, and items 9 and 10 measure the person’s perceptions of what others think about their communication abilities [28]. On a five-point Likert scale, with responses ranging from “almost never” (one point) to “almost always,” the participants were asked to rate the frequency of various behaviors or feelings for each topic (five points). The higher the score, the greater the communication difficulty.
Hearing handicap inventory in the elderly screening
The HHIE-S is a shortened version of the HHIE, which consists of five social or situational items and five emotional response items [5]. The HHIE-S was employed to assess how an individual perceives the social and emotional effects of hearing loss; thus, it is an index of self-perceived hearing handicap. The questionnaire consists of 10 items—five social/situational items and five emotional response items—with a total score range of 0–40. A “YES” response receives four points, a “NO” response receives zero points, and a “SOMETIMES” response receives two points. The HHIE-S total scores were used to classify the results into three categories: 0 to 8 (no self-perceived hearing handicap), 10–24 (mild to moderate handicap), and 26–40 (severe handicap). According to the American Speech-Language-Hearing Association’s proposed recommendations, a total HHIE-S score of 8 indicates the presence of a hearing handicap [29].
GDS questionnaire
The geriatric depression scale (GDS) short form was employed to investigate depression in the older adults. Each item requires a dichotomous response (yes or no) that is scored as 1 or 0, respectively. The GDS was designed to reflect the characteristics of geriatric depression, such as cognitive decline, while also considering the frequent somatic symptoms or insomnia present in the non-depressed geriatric population [30].
Statistical analysis
The data were analyzed using SPSS version 20.0. Software. A one-sample Kolmogorov–Smirnov test was performed to assess whether each parameter follows a parametric or nonparametric distribution. In addition to the descriptive statistics, significant differences among groups were assessed through a Mann–Whitney U test to analyze the difference between users, and non-users for communication, handicap and depression scales. In addition, Spearman’s rank correlation coefficient was used to analyze the relationship between the variables. P ≤ 0.05 was considered statistically significant.
Results
The population studied in this research consisted of older adults over 55 years of age (age range 55–85) who were suffering from moderate to severe hearing loss. A total of 114 people participated in this study, 57 of whom had used a hearing aid for at least six months and 57 of whom were not hearing aid users. Age and pure tone average (PTA) were not significantly different between the two groups (p > 0.05). The hearing aids of most of the participants were smart and made by different brands. None of participant had received auditory rehabilitation after hearing aid prescription. Further demographic details are described in Table 1.
Table 1.
Demographic information of the participants
| Group/variables | Hearing aid users | Hearing aid non-users |
|---|---|---|
| Age (years) | 70.22 (8.78) | 68 (8.83) |
| Gender | ||
| Female | 26 | 19 |
| Male | 31 | 38 |
| PTA (dB) | ||
| Right ear | 57.77 (12.69) | 50.78 (10.57) |
| Left ear | 56.68 (13.30) | 50.71 (12.18) |
| WRS (%) | ||
| Right ear | 88 (8.48) | 88.81 (7.22) |
| Left ear | 88.20 (8.89) | 89.69 (7.54) |
| Duration of using hearing aid (months) | ||
| 6–12 | 12 | NA |
| 12–24 | 13 | |
| More than 24 M | 32 | |
| Daily hours of hearing aid use (hours) | ||
| 1 < | 2 | NA |
| 2–4 | 14 | |
| 4–8 | 27 | |
| > 8 | 14 | |
| Type of hearing aid fitting | ||
| Unilateral | 30 | NA |
| Bilateral | 27 | |
| Refer to hearing aid fine tuning | 4 (7.01%) | |
| Hearing aid repair | 5 (8.77%) | NA |
PTA pure tone average, WRS word recognition score, NA not applicable
Comparison between user and non-user groups
The results showed that severe handicap was low in both groups according to their HHIE-S scores. In the hearing aid user group, more than half of the participants expressed having a moderate handicap (61.40%), whereas, in the non-user group, a lower percentage of people expressed having a moderate handicap (45.62%). In the non-user group, the number of people with a moderate handicap (45.62%) was almost equal to the number of people with no handicap (43.85%). The statistical analysis revealed significant differences between the two groups, as hearing aid users had worse scores on HHIE-S than non-users (P = 0.01). Regarding communication problems based on SAC scores, the majority of participants had communication problems at frequencies of about 40% or less in both hearing aid users (54.37%) and non-users (59.64%). Approximately 45.25% of hearing aid users and 40.36% of non-users had greater than 40% communication problems, although the number of patients with the lowest communication problems (0–20%) was nearly twice as low in the non-user group compared to the user group. However, there is no significant difference in the SAC scores between groups (P > 0.05). An investigation of depression in both groups revealed that the majority of people did not have depression (52.63% in the user group and 66.66% in the non-user group), and the number of participants with severe depression was low in both groups. No significant difference was found in the GDS scores between groups (P > 0.05). The average HHIE-S, SAC and GDS scores are shown in Table 2.
Table 2.
Handicap, communication difficulty, and depression in hearing aid users and non-users
| Variable/group | User (n-57) | Non-user (n = 57) | All (n = 114) |
|---|---|---|---|
| HHIE-S | |||
| 0–8 without handicap | 14 (24.56%) | 25 (43.85%) | 40 (35.08%) |
| 9–24 moderate handicap | 35 (61.40%) | 26 (45.62%) | 60 (52.63%) |
| 25–40 severe handicap | 8 (0.04%) | 6 (10.53%) | 14 (12.29%) |
| Mean | 16.61 (10.39) | 12.49 (9.84) | |
| Mean rank | 76.47 | 59.70 | |
| Z | − 2.46 | ||
| P-value | 0.01* | ||
| SAC | |||
| 0–20 | 10 (17.53%) | 21 (36.84%) | 31 (27.19%) |
| 21–40 | 21 (36.84%) | 13 (22.80%) | 36 (31.58%) |
| 41–60 | 12 (21.04%) | 10 (17.54%) | 23 (20.18%) |
| 61–80 | 11 (18.29%) | 12 (21.05%) | 22 (19.30%) |
| 81–100 | 3 (6.3%) | 1 (1.77%) | 2 (1.75%) |
| Mean | 42.08 (23.60) | 35.16 (25.20) | |
| Mean rank | 74.95 | 63.67 | |
| Z | − 1.64 | ||
| P-value | 0.10 | ||
| GDS | |||
| 0–4 without depression | 30 (52.63%) | 38 (66.66%) | 56 (49.12%) |
| 5–8 mild depression | 18 (31.58%) | 13 (8.22%) | 35 (30.80%) |
| 9–11 moderate depression | 6 (10.52%) | 4 (7.03%) | 14 (12.28%) |
| 12–15 severe depression | 3 (5.27%) | 2 (3.51%) | 9 (7.80%) |
| Mean | 4.72 (3.80) | 4.13 (3.71) | |
| Mean rank | 70.09 | 64.04 | |
| Z | − 0.91 | ||
| P-value | 0.36 |
HHIE-S Hearing Handicap Inventory for the Elderly-screening, SAC Self- Assessment of Communication, GDS Geriatric Depression Scale
In addition, the HHIE-S (Z = − 0.61, p = 0.53), SAC (Z = − 0.77, p = 0.43), and GDS (Z = − 1.79, p = 0.07) scores did not differ significantly between the two types of fittings (unilateral and bilateral). For the bilateral and unilateral fitting, the HHIE-S scores were 16.45 and 16.64, and the SAC scores were 39.73 and 45.83, respectively. Regarding gender differences, males’ scores were higher (worse) than females’ scores on handicap, communication difficulties, and depression in both groups. In older adults who use hearing aids, there is a gender difference in terms of depression, as males have significantly lower depression levels compared with females (P = 0.02, t = 2.25). However, no significant gender difference was found for HHIE-S or SAC scores in hearing aid users. In contrast, in non-users, gender differences were observed in HHIE-S and SAC scores, with males presenting lower HHIE-S (P = 0.01, Z = 2.54) and SAC scores (P = 0.000, Z = 4.10) than females; no gender difference was found for GDS score.
Correlation results
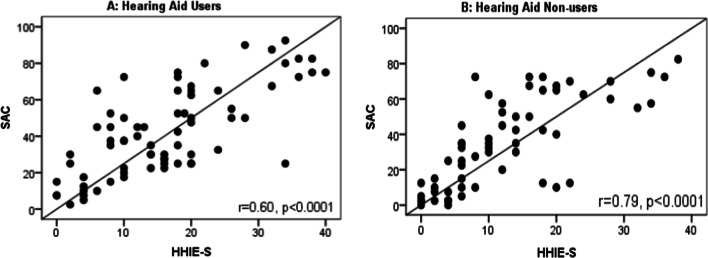
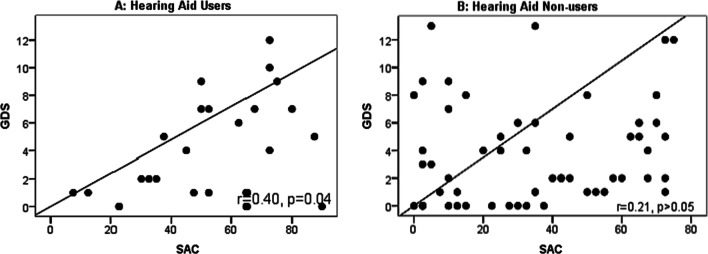
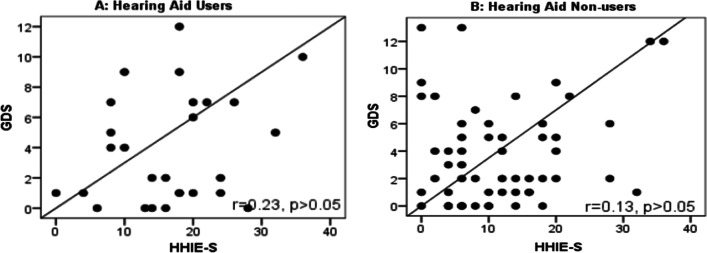
Figures 1, 2, and 3 depict the correlation results between the questionnaire scores of both groups separately. Regarding the correlations between questionnaires, the results of the HHIE-S and SAC questionnaires were highly correlated in both groups (users: r = 0.60, p < 0.0001, non-users: r = 0.79, p < 0.0001) (Fig. 1). In addition, there was a statistically significant and moderately positive correlation between the SAC score and the GDS scores (communication and depression) in geriatric hearing aid users (r = 0.40, P = 0.04) (Fig. 2) but not in non-users (P > 0.05). There was no correlation between HHIE-S scores and GDS scores (disability and depression) within any of the groups (P > 0.05) (Fig. 3).
Fig. 1.
Correlation between HHIE and SAC
Fig. 2.
Correlation between SAC and GDS
Fig. 3.
Correlation between HHIE-S and GDS
As shown in Table 3, there is a positive and statistically significant correlation between the time course of hearing aid use and the scores of the HHIE-S and SAC questionnaires (r = 0.61; r = 0.70, p < 0.01, respectively), such that the longer the use of HAs, the higher the level of self-perceived handicap and communication problems. There was no correlation between the time course of hearing aid usage and depression, nor between the daily hours of HA use and the HHIE-S and SAC scores (P > 0.05).
Table 3.
Correlation of the study variables
| Variable | Group | Correlation (r) | p value |
|---|---|---|---|
| HHIE-S*PTA | Users | 0.49 | < 0.02* |
| Non-users | 0.61 | < 0.0001* | |
| HHIE-S *WRS | Users | − 0.29 | 0.21 |
| Non-users | − 0.16 | 0.23 | |
| SAC*PTA | Users | 0.50 | 0.02* |
| Non-users | 0.66 | < 0.0001* | |
| SAC *WRS | Users | − 0.15 | 0.52 |
| Non-users | − 0.09 | 0.48 | |
| GDS*PTA | Users | 0.38 | 0.08 |
| Non-users | 0.15 | 0.25 | |
| GDS *WRS | Users | 0.16 | 0.51 |
| Non-users | − 0.10 | 0.47 | |
| HHIE-S*Age | Users | − 0.09 | 0.65 |
| Non-users | − 0.01 | 0.93 | |
| SAC*Age | Users | − 0.04 | 0.82 |
| Non-users | 0.002 | 0.99 | |
| GDS*Age | Users | 0.25 | 0.21 |
| Non-users | 0.07 | 0.60 | |
| Duration of hearing aid use*HHIE-S | Users | 0.61 | 0.003* |
| Duration of hearing aid use *SAC | Users | 0.70 | < 0.0001* |
| Duration of hearing aid use*GDS | Users | 0.04 | 0.85 |
| Daily hours of hearing aid use*HHIE-S | Users | − 0.22 | 0.25 |
| Daily hours of hearing aid use*SAC | Users | − 0.06 | 0.76 |
| Daily hours of hearing aid use*GDS | Users | − 0.23 | 0.24 |
*P ≤ 0.05
Because there was no significant difference between ears in the correlation between PTA and HHIE-S, SAC, and GDS scores, both ears’ data were merged. As shown in Table 3, the results revealed a significant association between PTA and HHIE-S scores, both in HA users (r = 0.49, p < 0.05) and non-users (r = 0.61; p < 0.0001), as well as between PTA and SAC scores (r = 0.50 and r = 66 in users and non-users, respectively). However, none of the groups demonstrated correlations between HHIE-S, SAC, and WRS (p > 0.05). Likewise, PTA and WRS were not found to be correlated with GDS scores. In both groups, age was not correlated with HHIE-S, SAC or GDS (P > 0.05).
Discussion
The results showed that in the hearing aid group, the average self-score of handicap (as measured by HHIE-S) was significantly higher than in the non-hearing aid group. Regarding communication difficulties (measured by SAC) and depression (measured by GDS), however, there were no differences between groups. Both groups exhibited a significant positive correlation between HHIE-S and SAC scores. However, no correlation was observed between GDS and HHIE-S scores in either group. A moderate correlation between SAC and GDS scores was observed only in the hearing aid group. The duration of hearing aid use was moderately correlated with SAC and HHIE-S scores but not with the daily hearing aid usage hours.
This result indicates that although there are no significant differences in communication difficulties between the two groups, the group that uses hearing aids felt more handicapped than those without hearing aids despite possessing the same degree of hearing loss. In the present study, findings from the HHIE-S score suggest that 52.63% of the older adults in both groups reported a moderate handicap, and 35.08% reported no handicap. Only 12.29% expressed a severe handicap. In detail, 61.40% of the participants in the group that uses hearing aids expressed moderate handicaps, and 24.56% expressed no handicap; meanwhile, in the group that does not utilize hearing aids, nearly the same number of people reported having a moderate handicap (42.62%) or no handicap (43.85%). The number of individuals with a severe handicap was similarly low in both groups. These data indicate that the average handicap score of non-users is lower than that of hearing aid users. In addition, the proportion of non-users who reported no impairment (43.85%) was greater than that of users (24.56%).
According to the HHIE-S scores in users and non-users, those with hearing aids experience a greater level of self-perceived handicap than those without hearing aids. The findings of this study disagree with a 2007 Iranian study conducted by Jalilvand et al. on 52 older adults with mild to severe hearing loss. In their study, 61.5% of participants had no handicap, 27% had a mild to moderate handicap, and 11.5% had a severe handicap. However, just two people used hearing aids [5]. Meanwhile, in the current study, the majority of participants reported a mild to moderate handicap, and the frequency of no handicap was lower than in Jalilvand’s study. In both investigations, however, the number of patients suffering from severe disabilities was nearly identical and minimal. The current study’s findings are consistent with our earlier research on elderly individuals conducted in 2020. Previous research revealed that only 20% of respondents had no self-perceived handicap, while 80% felt handicapped to varying degrees [31]. Varying degrees of handicap have been reported in different countries; some of these differences may be attributable to the cultural acceptance of diminished hearing sensitivity as a normal part of the aging process [1]. In addition to cultural effects, it appears that other factors strongly influence self-perceived handicap. For instance, it has been shown that the degree of perceived handicap is associated with hearing status, general health, and marital status [1]. Studies have also indicated the impact of psychological factors, such as depression, on self-perceived handicap [32, 33].
In the present study, hearing threshold, age, gender, communication problems, duration of hearing aid use, and daily hours of hearing aid use, as well as depression, were investigated in relation to self-perceived handicap and compared between two groups that either use or do not use hearing aids. No correlation was detected between age and HHIE-S score. Even though females had a greater level of handicap than males and despite the significant difference between females and males in terms of self-perceived handicap, interestingly, this difference was only detected in non-users and not in hearing aid users. Other studies have demonstrated gender differences in hearing aid outcomes. For instance, gender differences were observed in improved life quality after hearing aid fitting [34]. In the present study, however, there was no difference in self-perceived handicap between men and women who use hearing aids. In contrast, a gender difference in depression among elderly hearing aid users was revealed, with males having significantly lower depression levels than females. This study also showed a moderately significant correlation between hearing thresholds and handicaps for both groups. This is consistent with the findings of Chang et al., who reported a moderate correlation (r = 0.52) between hearing impairment and self-perceived handicap in a study of 1220 older adults [1]. In the present study, there was no connection between daily hours of hearing aid use and self-perceived disability. Unlike other research in which higher scores for the perception of hearing impairment were significantly associated with longer hours of daily hearing-aid use, we observed no such correlation [1, 35].
In addition, using the SAC questionnaire, we also evaluated the communication difficulties of individuals with hearing loss. In this study, there was a strong correlation between the HHIE-S score and the SAC score in both groups, indicating that those who feel more handicapped tend to have more communication difficulties. The average communication problem was higher in hearing aid users (42.08%) compared with non-users (35.16%). However, in contrast to self-perceived handicap, we did not find any significant difference between hearing aid users and non-users in terms of SAC score. Interestingly, the findings of the current study related to the SAC questionnaire indicated that mild communication problems (less than 50%) were reported in both groups. In contrast, one study suggested that if a person uses hearing aid for at least one month, their SAC/SOAC-assessed communication difficulties are significantly reduced. However, the study lacked a control group [18]. One of the reasons for this result could be that only 7% of the participants during the COVID-19 era had referred for hearing aid fine tuning, which could have affected the effectiveness of hearing aids, and ultimately affected communication abilities. Ghahraman et al. (2021) also detected a significant correlation between self-perceived handicap and communication problems [31]. Similar to self-perceived handicap, we discovered that communication problems were moderately significantly positively correlated with hearing thresholds but not with age. Similarly, although communication problems handicap was significantly higher in females compared with males, this difference was only detected in non-users and not in users.
The absence of significant communication problems between people with and without hearing aids, coupled with the significant difference in self-perceived handicap, implies that hearing aids were not very effective in alleviating communication problems in the participants, whose communication problems and perceived handicaps were worse than those of the group without hearing aids. It is unclear how hearing aids affect handicaps. As mentioned, some studies suggest that the use of hearing aids is effective in reducing perceived handicap, while others do not. In fact, there are contradictory findings about the effectiveness of hearing aids in reducing handicaps. A recent investigation on the influence of hearing aids on handicaps in a cohort design found that the average HHIE-S scores following hearing aid provision were considerably lower at six months, 12 months, and five years compared to baseline [36]. In another study, the mean HHIE-S score decreased substantially after four months of hearing aid use [12]. In a separate study, the mean HHIE-S score reduced from 28.7 to 12.7 following six months of hearing aid use [14]. Some clinical trials that have directly studied the effect of hearing aids on handicaps have indicated a reduction relative to baseline measurements [9–11]. In a study by Lotfi et al. on 350 individuals with moderate to severe hearing loss (age and hearing level did not differ between the two groups), hearing aids significantly improved HHIE-S scores after at least three months of use. Before using the hearing aid, the overall score of HHIE-S was 65.88%, and it dropped to 22.1% after hearing aid use [11]. In a study in China in 2020, the effect of an intervention with hearing aid on handicap features revealed that the average HHIE-S score among hearing-impaired individuals was 33.49 before hearing aid use and roughly 31.50 after two years [16].
However, in agreement with the current study, a previous study indicated no significant difference in handicap scores between participants who had recently acquired a hearing aid and those who had utilized a hearing aid in the past [37]. Cross-sectional investigations, such as that conducted by Dawes et al. (2015), revealed that self-reported disability was greater among hearing aid users than among non-users. According to HHIE questionnaire scores, after five and 11 years of follow-up, although the difference between the two groups narrowed, those who used hearing aids felt more handicapped than those who did not use hearing aids [6]. In a study by Gopinath et al. (2011), the rate of self-reported disability was higher among those who used hearing aids than those who did not [7]. In another study, those who used hearing aids had a higher rate of handicap than those who did not, but those who used hearing aids also had more severe hearing loss in this case [17]. A notable aspect about the handicaps is the attention that must be paid to hearing loss. This is due to the fact that the degree of hearing loss correlates directly with the degree of handicap [27, 38]. Intriguingly, in the study by Maeda et al. (2016), the mean HHIE-S was not statistically different between two groups of older adults with moderate hearing loss, one of which used hearing aids and the other did not. Nevertheless, those who used hearing aids were more likely to feel handicapped than non-users. The two groups were comparable in terms of hearing loss, age, speech differentiation, and dynamic range [8], which is consistent with the present study.
As previously stated, psychological variables may also contribute to self-perceived handicap. Depression is one of the consequences of hearing loss in the older adults, according to the majority of studies [39]. Hearing loss in the older adults, in particular, has been shown to induce frustration, loneliness, and communication disorders, all of which degrade their quality of life [4]. According to a number of studies, those who report significant hearing impairment are more likely to suffer from depression compared with normal hearing individuals [9]. Depression was not significantly different between hearing aid users and non-users in the present study. Some reports indicate that hearing aids can also alleviate the psychological effects of hearing loss, such as depression [21, 22], while other reports do not show this [23, 24]. According to the results of the Depression Inventory, over half of all older adults were depression-free (49.12%), followed by those with mild (30.80%), moderate (12.28%), and severe depression (7.80%). Both groups followed this pattern, and there was no statistically significant difference between the group with hearing aids and those without hearing aids in terms of GDS scores, as the mean depression score for both groups was less than 5. The average GDS scores for those with and without hearing aids were 4.72 and 4.13, respectively. In agreement, the mean GDS scores of individuals with hearing aids, without hearing aids, and without hearing loss were evaluated in a study. It was determined that these scores were 1.2, 2.6, and 2.1, without a significant difference between the three groups [25]. In the current study, more than half of the participants in both groups did not experience depression; specifically, 52.63% of hearing aid users, and 66.66% of non-users did not have depression.
In agreement with our findings, a recent study with a two-month follow-up indicated that depression after hearing aid use was worse than before hearing aid use, possibly due to aging or the commencement of the COVID-19 pandemic. In this study, out of 385 participants, 140 (36.36%) experienced depression, and 63.64% did not, with the number of those without depression increasing to 154 after two months of follow-up [16]. Another study reported a lack of an association between hearing aid use and depression, perhaps because hearing aids impede participation in social engagements by enhancing the adverse background noise common in social venues such as coffee shops, salons, and restaurants [23]. In the study conducted by Shukla et al. (2021), there were no statistically significant associations between hearing aid use and depressive symptoms. However, they stated that the role of several characteristics connected to hearing aid use, such as frequency of use and the user’s perceptions of benefits or satisfaction, which were not included in their analysis, may also be relevant [21]. In this study, there was no correlation between depression and self-perceived handicap; however, there was a moderate positive correlation between depression and communication difficulties among hearing aid users. In other words, in those with hearing aids, the greater the communication problem, the more severe the depression. Another study found that offering free hearing aids improved outcomes SPS:refid::bib16(16). This finding could be related to the expectations from the hearing aid in these people resulted in depression. In other words, people with hearing aids, when having communication problems, may have become frustrated because they paid a significant amount of money for their hearing aids. In addition, there appears to be a bidirectional connection between hearing aid satisfaction and self-perceived handicap. This implies that self-perceived handicap can impact hearing aid satisfaction and that contentment with hearing aid can influence self-perceived handicap. This is presumably because, like self-perceived handicap, multiple factors also affect hearing aid satisfaction. Thus, hearing aid satisfaction may have a role in self-perceived handicap. One of the factors that play an important role in hearing aid satisfaction in the older adults is post-prescription support [40], which can also be influenced by pandemic limitations. As seen in the results of our study, the reduction of timely referral for hearing aid fine tuning as well as not receiving auditory rehabilitation can worsen the outcome of handicaps and communication abilities even with the existence of hearing aids. According to a systematic review, there are audiological and non-audiological determinants of hearing aid effectiveness. Other determinants of hearing-aid usage include expectations, self-perceived benefits, and satisfaction with the hearing aid being used, with extended daily hours of use of hearing aids associated with increased satisfaction [41]. In addition, research indicates that although effective hearing aid use affects a person’s perceived handicap, constant use of hearing aid does not guarantee a positive patient outcome [42]. Another study compared the administration of hearing aids in groups with and without auditory rehabilitation and found that HHIE-S scores improved significantly from baseline to follow-up in the group that received hearing training. In contrast, no change was observed in the group that received hearing aids without a rehabilitation plan [43]. In another study, self-assessments were used to investigate the prevalence of hearing difficulties, and it was discovered that older adults, including those with hearing aids, had numerous hearing problems and that the majority of them did not use their hearing aids. In addition, the older a person is, the less often they use their hearing aids, usually due to improper administration and maintenance of the hearing device, as well as annoyance with the hearing aid [25]. In fact, a portion of the feeling of disability may be attributable to unhappiness with the hearing aid, which is influenced by numerous factors, including auditory and non-auditory aspects reliant on the individual and the hearing aid [44]. In our study, the incidence of the COVID-19 pandemic and restrictions may have reduced the frequency with which people go for hearing aid fitting or servicing. Consequently, the user’s satisfaction with the hearing aid may have decreased, and he or she may have endured communication difficulties and a heightened sense of disability. Increasing hearing aid satisfaction may be a crucial factor in self-perceived handicap. People used hearing aids less during the pandemic due to hearing-related constraints, such as restricted access to battery purchases, resetting or repairing hearing aids, and impediments to accessing hearing training programs [45]. Recent research by Nuess et al. (2021) revealed that participants who indicated a willingness to use hearing aids were more likely to have higher HHIE/A scores than normal-hearing participants and those unwilling to use hearing aids [33].
There are a few contradictory findings regarding the effects of hearing aid parameters, such as daily duration, the duration of hearing aid usage, and hearing aid type, on handicaps or communication difficulties. It has been indicated that individuals with better ear PTA thresholds and those who used their hearing aids more frequently reported a greater improvement in the disability domain. Self-reported hearing disabilities may be a stronger predictor of hearing aid uptake than PTA thresholds [46]. In the present study, the majority of participants (56.14%) used hearing aids for at least 24 months and for an average of 36.25 months, and neither the duration of hearing aid use nor the hours of daily use were correlated with depression scores. In contrast, we demonstrated that there is a positive and significant correlation between the duration of hearing aid use (but not the amount of daily use) with HHIE-S and SAC questionnaire scores, such that the longer hearing aids are used, the greater the degree of disability and perceived communication difficulties. However, some reports have indicated a significant association between hearing aid use time and pre- and post-treatment audiological and distress-related indices [47]. In addition, none of the other characteristics in this study were associated with the type of hearing aid (unilateral or bilateral). In other words, there was no significant difference in disability, depression, or communication difficulties between unilateral and bilateral hearing aid users. Little is known about this effect.
The limitations of this study include the facts that participants with varying types of hearing aids were included and that satisfaction with hearing aids was not investigated. Another limitation was that in our country, rehabilitation is not routinely performed after receiving hearing aids in the elderly, and this made us unable to examine the effects of simultaneous use of hearing aids and rehabilitation which could affect our results. It would be preferable if the hearing aid was adjusted uniformly by an institution or an individual so that individual satisfaction cannot be guaranteed. Despite this, the majority of patients in the present study utilized smart hearing aids. Additional research is required to demonstrate the role of auditory rehabilitation facilities in overcoming communication challenges and decreasing the self-perceived handicap and depression associated with communication failure.
Conclusion
It seems that self-perceived handicap, communication difficulties and depression are affected by many factors, and only receiving hearing aids without subsequent support such as auditory rehabilitation and programming services cannot bring the expected output. The effect of these factors was clearly observed due to reduced access to services in the COVID- 19 era. In fact, it appears that to hearing aids have beneficial effects on the feeling of handicap and depression, first of all, patients should be satisfied with it, which itself is affected by several factors. Further investigation is required to fully comprehend the effects of hearing aids on handicaps and depression, as well as the relationship between hearing aid satisfaction with self-perceived handicap or depression together with simultaneous effects of hearing aids and auditory rehabilitation.
Author contributions
ET and VR collaborated in designing of the study, performing all statistical analyses and writing the paper. SHJ supervised the data analyses. MEK, ZS, MAG, NR helped to plan the report and contributed in writing and revising the paper. All authors approved the final version.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Elham Tavanai, Email: etavanai@sina.tums.ac.ir.
Vida Rahimi, Email: v-rahimi@sina.tums.ac.ir.
References
- 1.Chang HP, Ho CY, Chou P. The factors associated with a self-perceived hearing handicap in elderly people with hearing impairment–results from a community-based study. Ear Hear. 2009;30(5):576–583. doi: 10.1097/AUD.0b013e3181ac127a. [DOI] [PubMed] [Google Scholar]
- 2.Lee KY. Pathophysiology of age-related hearing loss (peripheral and central) Korean J Audiol. 2013;17(2):45–49. doi: 10.7874/kja.2013.17.2.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang HP, Chou P. Presbycusis among older Chinese people in Taipei, Taiwan: a community-based study. Int J Audiol. 2007;46(12):738–745. doi: 10.1080/14992020701558529. [DOI] [PubMed] [Google Scholar]
- 4.Ciorba A, Bianchini C, Pelucchi S, Pastore A. The impact of hearing loss on the quality of life of elderly adults. Clin Interv Aging. 2012;7:159–163. doi: 10.2147/CIA.S26059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jalilvand Karimi L, Ashrafi M, Khosravi E, Shahidipour Z, Vafaei F. Hearing screening in the elderly and evaluating the need for hearing aid. Auditory Vestibular Res. 2008;16(2):38–45. [Google Scholar]
- 6.Dawes P, Cruickshanks KJ, Fischer ME, Klein BE, Klein R, Nondahl DM. Hearing-aid use and long-term health outcomes: hearing handicap, mental health, social engagement, cognitive function, physical health, and mortality. Int J Audiol. 2015;54(11):838–844. doi: 10.3109/14992027.2015.1059503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gopinath B, Schneider J, Hartley D, Teber E, McMahon CM, Leeder SR, et al. Incidence and predictors of hearing aid use and ownership among older adults with hearing loss. Ann Epidemiol. 2011;21(7):497–506. doi: 10.1016/j.annepidem.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Maeda Y, Sugaya A, Nagayasu R, Nakagawa A, Nishizaki K. Subjective hearing-related quality-of-life is a major factor in the decision to continue using hearing aids among older persons. Acta Otolaryngol. 2016;136(9):919–922. doi: 10.1080/00016489.2016.1183817. [DOI] [PubMed] [Google Scholar]
- 9.Tolson D, Swan I, Knussen C. Hearing disability: a source of distress for older people and carers. Br J Nurs. 2002;11(15):1021–1025. doi: 10.12968/bjon.2002.11.15.10529. [DOI] [PubMed] [Google Scholar]
- 10.Mulrow CD, Aguilar C, Endicott JE, Tuley MR, Velez R, Charlip WS, et al. Quality-of-life changes and hearing impairment. A randomized trial Ann Intern Med. 1990;113(3):188–194. doi: 10.7326/0003-4819-113-3-188. [DOI] [PubMed] [Google Scholar]
- 11.Lotfi Y, Mehrkian S, Moossavi A, Faghih-Zadeh S. Quality of life improvement in hearing-impaired elderly people after wearing a hearing aid. Arch Iran Med. 2009;12(4):365–370. [PubMed] [Google Scholar]
- 12.Chang W-H, Tseng H-C, Chao T-K, Hsu C-J, Liu T-C. Measurement of hearing aid outcome in the elderly: comparison between young and old elderly. Otolaryngology-Head and Neck Surgery. 2008;138(6):730–734. doi: 10.1016/j.otohns.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 13.Newman CW, Weinstein BE. The Hearing Handicap Inventory for the Elderly as a measure of hearing aid benefit. Ear Hear. 1988;9(2):81–85. doi: 10.1097/00003446-198804000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Vuorialho A, Karinen P, Sorri M. Effect of hearing aids on hearing disability and quality of life in the elderly. Int J Audiol. 2006;45(7):400–405. doi: 10.1080/14992020600625007. [DOI] [PubMed] [Google Scholar]
- 15.Mulrow CD, Tuley MR, Aguilar C. Sustained benefits of hearing aids. J Speech Hear Res. 1992;35(6):1402–1405. doi: 10.1044/jshr.3506.1402. [DOI] [PubMed] [Google Scholar]
- 16.Ye X, Zhu D, Chen S, Shi X, Gong R, Wang J, et al. Effects of providing free hearing aids on multiple health outcomes among middle-aged and older adults with hearing loss in rural China: a randomized controlled trial. BMC Med. 2022;20(1):124. doi: 10.1186/s12916-022-02323-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Popelka MM, Cruickshanks KJ, Wiley TL, Tweed TS, Klein BE, Klein R. Low prevalence of hearing aid use among older adults with hearing loss: the Epidemiology of Hearing Loss Study. J Am Geriatr Soc. 1998;46(9):1075–1078. doi: 10.1111/j.1532-5415.1998.tb06643.x. [DOI] [PubMed] [Google Scholar]
- 18.Sahin D, Başar FS, Güven AG. Self and significant other assessment of hearing device aided communication skills in the elderly with hearing loss. Kulak Burun Bogaz Ihtis Derg. 2012;22(3):153–159. doi: 10.5606/kbbihtisas.2012.029. [DOI] [PubMed] [Google Scholar]
- 19.Barker F, Mackenzie E, Elliott L, Jones S, de Lusignan S. Interventions to improve hearing aid use in adult auditory rehabilitation. Cochrane Database Syst Rev. 2014(7):Cd010342 [DOI] [PubMed]
- 20.Stark P, Hickson L. Outcomes of hearing aid fitting for older people with hearing impairment and their significant others. Int J Audiol. 2004;43(7):390–398. doi: 10.1080/14992020400050050. [DOI] [PubMed] [Google Scholar]
- 21.Shukla A, Reed NS, Armstrong NM, Lin FR, Deal JA, Goman AM. Hearing loss, hearing aid use, and depressive symptoms in older adults-findings from the atherosclerosis risk in communities neurocognitive study (ARIC-NCS) J Gerontol B Psychol Sci Soc Sci. 2021;76(3):518–523. doi: 10.1093/geronb/gbz128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marques T, Marques FD, Miguéis A. Age-related hearing loss, depression and auditory amplification: a randomized clinical trial. Eur Arch Otorhinolaryngol. 2022;279(3):1317–1321. doi: 10.1007/s00405-021-06805-6. [DOI] [PubMed] [Google Scholar]
- 23.Dawes P, Emsley R, Cruickshanks KJ, Moore DR, Fortnum H, Edmondson-Jones M, et al. Hearing loss and cognition: the role of hearing AIDS, social isolation and depression. PLoS ONE. 2015;10(3):e0119616. doi: 10.1371/journal.pone.0119616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Metselaar M, Maat B, Krijnen P, Verschuure H, Dreschler WA, Feenstra L. Self-reported disability and handicap after hearing-aid fitting and benefit of hearing aids: comparison of fitting procedures, degree of hearing loss, experience with hearing aids and uni- and bilateral fittings. Eur Arch Otorhinolaryngol. 2009;266(6):907–917. doi: 10.1007/s00405-008-0847-x. [DOI] [PubMed] [Google Scholar]
- 25.Öberg M, Marcusson J, Nägga K, Wressle E. Hearing difficulties, uptake, and outcomes of hearing aids in people 85 years of age. Int J Audiol. 2012;51(2):108–115. doi: 10.3109/14992027.2011.622301. [DOI] [PubMed] [Google Scholar]
- 26.Clark JG. Uses and abuses of hearing loss classification. ASHA. 1981;23(7):493–500. [PubMed] [Google Scholar]
- 27.Purnami N, Mulyaningsih EF, Ahadiah TH, Utomo B, Smith A (2020) Score of hearing handicap inventory for the elderly (HHIE) compared to whisper test on presbycusis. Ind J Otolaryngol Head Neck Surg 1–5 [DOI] [PMC free article] [PubMed]
- 28.English KM editor (2010) Reliability of the self-assessment of communication adolescent
- 29.(1989) Guidelines for the identification of hearing impairment/handicap in adult/elderly persons. Asha 31(8):59–63 [PubMed]
- 30.Malakouti K, Fathollahi P, Mirabzadeh A, Salavati M, Kahani S. Validation of Geriatric Depression Scale (GDS-15) in Iran. Pejouhesh dar Pezeshki (Research in Medicine) 2006;30(4):361–369. [Google Scholar]
- 31.Fatemeh H, Mansoureh Adel G, Elham T, Shohreh J, Farzaneh Zamiri A, et al. Self-assessed hearing handicap in the elderly: a pilot study on Iranian population. Auditory Vestibular Res. 2021;30(1):33–41. [Google Scholar]
- 32.Saito H, Nishiwaki Y, Michikawa T, Kikuchi Y, Mizutari K, Takebayashi T, et al. Hearing handicap predicts the development of depressive symptoms after 3 years in older community-dwelling Japanese. J Am Geriatr Soc. 2010;58(1):93–97. doi: 10.1111/j.1532-5415.2009.02615.x. [DOI] [PubMed] [Google Scholar]
- 33.Nuesse T, Schlueter A, Lemke U, Holube I. Self-reported hearing handicap in adults aged 55 to 81 years is modulated by hearing abilities, frailty, mental health, and willingness to use hearing aids. Int J Audiol. 2021;60(sup2):71–79. doi: 10.1080/14992027.2020.1858237. [DOI] [PubMed] [Google Scholar]
- 34.Joanovič E, Kisvetrová H, Nemček D, Kurková P, Švejdíková B, Zapletalová J, et al. Gender differences in improvement of older-person-specific quality of life after hearing-aid fitting. Disabil Health J. 2019;12(2):209–213. doi: 10.1016/j.dhjo.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 35.Mizutari K, Michikawa T, Saito H, Okamoto Y, Enomoto C, Takebayashi T, et al. Age-related hearing loss and the factors determining continued usage of hearing aids among elderly community-dwelling residents. PLoS ONE. 2013;8(9):e73622. doi: 10.1371/journal.pone.0073622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim AS, Betz JF, Nieman CL, Hoyer MR, Applebaum J, Lin FR, et al. Long-term impact of hearing aid provision or cochlear implantation on hearing handicap. Laryngoscope. 2021;131(5):1122–1126. doi: 10.1002/lary.29175. [DOI] [PubMed] [Google Scholar]
- 37.Kelly-Campbell RJ, McMillan A. The relationship between hearing aid self-efficacy and hearing aid satisfaction. Am J Audiol. 2015;24(4):529–535. doi: 10.1044/2015_AJA-15-0028. [DOI] [PubMed] [Google Scholar]
- 38.Wiley TL, Cruickshanks KJ, Nondahl DM, Tweed TS. Self-reported hearing handicap and audiometric measures in older adults. J Am Acad Audiol. 2000;11(2):67–75. doi: 10.1055/s-0042-1748012. [DOI] [PubMed] [Google Scholar]
- 39.Cosh S, Helmer C, Delcourt C, Robins TG, Tully PJ. Depression in elderly patients with hearing loss: current perspectives. Clin Interv Aging. 2019;14:1471–1480. doi: 10.2147/CIA.S195824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Solheim J, Kværner KJ, Sandvik L, Falkenberg E-S. Factors affecting older adults' hearing-aid use. Scand J Disabil Res. 2012;14(4):300–312. doi: 10.1080/15017419.2011.640411. [DOI] [Google Scholar]
- 41.Ng JH, Loke AY. Determinants of hearing-aid adoption and use among the elderly: a systematic review. Int J Audiol. 2015;54(5):291–300. doi: 10.3109/14992027.2014.966922. [DOI] [PubMed] [Google Scholar]
- 42.Aazh H, Moore BCJ. Audiological rehabilitation for facilitating hearing aid use: a review. J Am Acad Audiol. 2017;28(3):248–260. doi: 10.3766/jaaa.16035. [DOI] [PubMed] [Google Scholar]
- 43.Tesch-Römer C. Psychological effects of hearing aid use in older adults. J Gerontol B Psychol Sci Soc Sci. 1997;52(3):P127–P138. doi: 10.1093/geronb/52B.3.P127. [DOI] [PubMed] [Google Scholar]
- 44.Mahsa Hamidi P, Reza H. Factors influencing the hearing aids use and satisfaction: a review study. J Modern Rehabilit. 2020;13(3):137–146. doi: 10.32598/JMR.13.3.137. [DOI] [Google Scholar]
- 45.Alqudah S, Zaitoun M, Alqudah O, Alqudah S, Alqudah Z. Challenges facing users of hearing aids during the COVID-19 pandemic. Int J Audiol. 2021;60(10):747–753. doi: 10.1080/14992027.2021.1872806. [DOI] [PubMed] [Google Scholar]
- 46.Ho EC, Li K, Ong WMW, Bei YTE, Seneviratna A. Factors Influencing Hearing disability and reduction in disability among first-time hearing aid users in Singapore. Ann Acad Med Singap. 2020;49(12):978–989. doi: 10.47102/annals-acadmedsg.2020376. [DOI] [PubMed] [Google Scholar]
- 47.Boecking B, Psatha S, Nyamaa A, Dettling-Papargyris J, Funk C, Oppel K, et al. Hearing aid use time is causally influenced by psychological parameters in mildly distressed patients with chronic tinnitus and mild-to-moderate hearing loss. J Clin Med. 2022;11(19):5869. doi: 10.3390/jcm11195869. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.