OP01: Endoscopy in Spine Surgery
75
A001: Assessing the learning process of endoscopic surgery for sciatica
Pravesh Gadjradj 1 and Biswadjiet Harhangi 2
1 Neurological Surgery, Weill Cornell, New York, United States
2 Neurological Surgery, Erasmus MC, Rotterdam, The Netherlands
Objective: Percutaneous transforaminal endoscopic discectomy (PTED) is gaining popularity by both surgeons and patients as a less invasive treatment option for sciatica. Concerns, however, exist for its learning curve. No previous study has assessed the learning process of PTED. Hereby we present the learning process of three surgeons learning PTED. Methods: This analysis was conducted alongside a multicenter randomized controlled trial. After attending a cadaveric workshop, three spine dedicated surgeons started performing PTED, initially under supervision of a senior surgeon. After each 5 cases, and up to case 20, the learning process was evaluated using the validated questionnaires (OSATS, GOALS) and a 10-step checklist specifically developed for PTED. Results: In total, 3 learning curve surgeons performed a total of 161 cases. Based on self-assessment, surgeons improved mostly in the domains “Time and Motion”, “Respect for Tissue”, and “Knowledge and Handling of Instruments”. Learning curve surgeons were more able to detect differences in performances on the OSATS than the senior surgeon. Based on the GOALS, the biggest improvements could be seen in “depth-perception” and “autonomy”. Based on the 10-item specific checklist, all surgeons performed all 10 steps by case 10, while only one surgeon performed all steps adequately by case 15. Conclusions: Based on these study results, PTED appears to be successfully adopted stepwise by three spine dedicated surgeons. From 15 cases on, most steps of PTED are performed adequately. Validated tools, however, are needed to determine the cut-off when a surgeon should be able to perform PTED independently.
74
A002: Two-year outcomes of a RCT on full-endoscopic versus open discectomy for sciatica
Pravesh Gadjradj 1 and Biswadjiet Harhangi 2
1 Neurological Surgery, Weill Cornell, New York, United States
2 Neurological Surgery, Erasmus MC, Rotterdam, The Netherlands
Background: Open microdiscectomy (OM) is the current standard procedure to treat sciatica caused by lumbar disk herniation. Percutaneous transforaminal endoscopic discectomy (PTED) is an alternative procedure which is performed under local anesthesia. Here we report the long-term results. Methods: A pragmatic, multicenter, non-inferiority, randomized controlled trial was conducted in which patients were randomized between PTED or OM in a 1:1 ratio. The primary outcome is self-reported leg pain measured by the 0-100 Visual Analogue Scale (VAS) with a non-inferiority margin of 5. Secondary outcomes include self-reported ODI, back pain, costs, QALYs, health-related quality of life and self-perceived recovery. Outcomes were measured the day following surgery, at 2, 4, and 6 weeks, and at 3, 6, 9, and 12, 24 months. Results: A total of 613 were randomized to either PTED (n = 304) or OM (n = 309). At 24 months, 92% of the patients had follow-up data available. At 24 months, the adjusted between group difference of the VAS leg pain was 7.3 in favor of PTED (17.0 ± 22.4 vs. 24.3 ± 26.5). There was no difference in back pain at 24 months between both groups. All other secondary patient-reported outcomes showed small but statistically more favorable results for the PTED-group. Complications rates and rate of recurrent disc surgery (PTED 6.7%; OM 8.7%) appear similar between both groups. Except for costs of the surgery itself, all other costs were lower for PTED than OM. Cost-effectiveness acceptability curves indicated that the probability of PTED being cost-effective compared with OM was almost 100% for leg pain and QALYs, regardless of the willingness-to-pay. Conclusions: PTED is non-inferior and cost-effective to OM in the treatment of sciatica at 24 months of follow-up and clinical outcomes appear to be more favorable for PTED albeit not exceeding established MCIDs. Therefore, based on these study results, implementation of PTED as a treatment option for sciatica is warranted.
61
A003: Comparative cohort study of paraspinal muscle volume change between uniportal full endoscopic and minimally invasive open posterolateral transforaminal lumbar interbody fusion
Pang Hung Wu 1 and Hyeun Sung Kim 2
1 Orthopaedic Surgery, Ng Teng Feng General Hospital, Singapore, Singapore
2 Neurosurgery, Nanoori Gangnam Hospital, Seoul, South Korea
Background: Recent literature of uniportal full endoscopic posterolateral transforaminal lumbar interbody fusion demonstrates good clinical and radiological outcomes with minimally invasive benefits potentially preserving paraspinal muscle. There is no literature on paraspinal muscle volume change between the endoscopic and microscopic minimally invasive interbody fusion. Methods: We included patients who met the indication criteria for lumbar fusion and underwent either uniportal full endoscopic posterolateral transforaminal lumbar interbody fusion or open transforaminal lumbar interbody fusion. Clinical parameters of visual analog scale and Oswestry disability index were measured at preoperative, postoperative 1 week, 3 months postoperative and final follow up. Magnetic Resonance Imaging measurement of preoperative and postoperative Kjaer grade, right and left psoas muscle mass area, right and left paraspinal muscle mass area were performed. Results: 74 levels of Endo-TLIF and 42 patients with minimally invasive Open TLIF were included. There was statistically significant greater improvement in VAS and ODI in Endo-TLIF cohort at 1 week significant improvement of Kjaer grade at postoperative 1 year in Endo-TLIF compared to MIS-TLIF. There is statistically significant improvement in paraspinal muscle mass area in Endo-TLIF (104.83 ± 316.45) mm2 compared to MIS-TLIF (89.88 ± 185.14) mm2Conclusion: Uniportal Endoscopic Posterolateral Lumbar Transforaminal Interbody Fusion achieved improved paraspinal and psoas muscle bulk and less fatty infiltration in the operated level as compared to Minimally Invasive Open Transforaminal Lumbar Interbody Fusion while both cohorts achieved equivalent positive clinical outcomes.
1096
A004: Full endoscopic discectomy for thoracic disc herniations: a single arm meta-analysis of safety and efficacy outcomes
Jackson Daniel 1 , Luis Eduardo Carelli Texeira Da Silva 2 , Ricardo Araujo 3 , and Jose Alberto Oliveira 4
1 Neurosurgery, Hospital of Federal University of Piaui, Teresina, Brazil
2 Orthopedics and Spine Surgery, Instituto Nacional de Traumatologia e Ortopedia Jamil Haddad – INTO, Rio de Janeiro, Brazil
3 Neurosurgery, Universidade de São Paulo, São Paulo, Brazil
4 Orthopedics and Spine, Universidade Federal do Ceará, Fortaleza, Brazil
Introduction: Surgical intervention is the treatment of choice in patients with thoracic disc herniation (TDH) with refractory symptoms and progressive acute myelopathy. Due to high occurrence of complications from open surgery, minimally invasive approaches are desirable. Nowadays, endoscopic techniques have become increasingly popular and full endoscopic surgery can be performed in the thoracic spine with low complication rates. Methods: Cochrane Central, PubMed and EMBASE databases were systematically searched for studies that evaluated patients who underwent full endoscopic spine thoracic surgery. The outcomes of interest were dural tear, myelopathy, epidural hematoma, recurrent disc herniation and dysthesia. In the absence of comparative studies, a single arm meta-analysis was performed. Results: We included 16 studies with a total of 292 patients. Follow-up ranged from 6 to 89 months, age from 17 to 82 years, with 56.2% male. The procedure was performed under local anesthesia with sedation 228 (78.08) surgeries local anesthesia and sedation was applied. A transforaminal approach was used in 87.3% of the cases. There were no cases of infection or death reported. The data showed a pooled incidence of outcomes as follows, with their respective 95% confidence intervals (CI) - dural tear (1.4%; 95% CI 0 - 2.7%); myelopathy (2.2%; 95% CI 0.5 - 3.9%), epidural hematoma (1.1%; 95% CI 0.2 - 2.5%), dysesthesia (4.7%; 95% CI 2.0 - 7.3%), recurrent disc herniation (1.8%; 95% CI 0 - 3.7%) and reoperation (1.7%; 95% CI 0.1 - 3.4%). Conclusion: Full endoscopic discectomy has a low incidence of adverse outcomes in patients with thoracic disc herniations. Controlled studies, ideally randomized, are warranted to establish the comparative efficacy and safety of the endoscopic approach relative to open surgery.
494
A005: Outcomes collection and reoperation rates following lumbar tubular microdecompression: 6 year follow up using an in-house methodology
Garrett Bullock 1 , Evan Miller 1 , Christian Sangio 2 , Edward Beck 1 , Anirudh Gowd 1 , Kerry Danelson 1 , and Tadhg O'Gara 1
1 Atrium Health Wake Forest Baptist, Orthopaedic Surgery, Winston-Salem, United States
2 Wake Forest University School of Medicine, Orthopaedic Surgery, Winston-Salem, United States
Introduction: Long term data describing patient reported outcomes (PROs) and re-operation rates following lumbar tubular microdeompression (LTM) are lacking. The purpose of this present study was to to report re-operation rates following LTM as well as compare PROs 6 years after surgery between those who did and did not need revision to open laminectomy or fusion. Material and Methods: Patients with lumbar spinal stenosis underwent one or more of three LTM procedures. LTM techniques utilized were the unilateral laminotomy to address central and ipsilateral lateral recess stenosis, the unilateral laminotomy for bilateral decompression to address central pathology, bilateral lateral recess pathology and contralateral foraminal stenosis, and the far lateral (FLD) “transpedicular” decompression to address ipsilateral foraminal stenosis. Demographic, PROs [Oswestry Disability Index (ODI) and visual analog scale (VAS) for back and leg pain], and re-operation data were collected. Failure of an index LTM was defined as revision to open laminectomy or fusion. Failure and revision LTM incidence and cumulative incidence were prospectively collected up to 6 years. Mixed effects linear regressions with 95% confidence intervals (95% CI) were performed to assess potential differences in ODI and reported VAS back and leg pain between patients that reported failure and those that did not. Results: 418 patients were included with median follow up of 3.0 (1.9, 4.1) years. 25% had a reoperation by 6 years. 65 (15.5%) failed and 35 (9.0%) underwent a second LTM. Cumulative failure incidence was 9% within the first 2 years. Failure patients had a statistically higher ODI [12.1 (95% CI: 3.2, 20.1) and VAS back [2.3 (95% CI: 0.9, 3.8)] and leg pain [1.6 (95% CI: 0.2, 3.1)] throughout follow-up. The overall dural tear rate was 7.2%. Conclusion: LTM is an effective treatment for lumbar spinal stenosis with sustained 6 year PROs. Most failures occur within 2 years postoperatively and stabilize to 4% yearly incidence by year 5. The yearly incidence of re-operation with LTM stabilizes at 3% by year 6 post operatively.
600
A006: Full-endoscopic lumbar decompression versus minimally invasive transforaminal lumbar interbody fusion for stable, degenerative spondylolisthesis
Khanathip Jitpakdee 1 , Yanting Liu 2 , Weerasak Singhatanadgige 3 , Vit Kotheeranurak 3 , Worawat Limthongkul 3 , and Jin-Sung Kim 2
1 Orthopedics, Queen Savang Vadhana Memorial Hospital, Chonburi, Thailand
2 Neurosurgery, The Catholic University of Korea, Seoul St. Mary’s Hospital, College of Medicine, Seoul, South Korea
3 Department of Orthopaedics, Faculty of Medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand
Introduction: Minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) is generally considered an effective treatment for degenerative spondylolisthesis. Meanwhile, lumbar endoscopic unilateral laminotomy for bilateral decompression (LE-ULBD) is also emerging as a minimally invasive non-fusion procedure for this condition. However, a comparative analysis of outcomes between both techniques is still lacking. The aim of this study was to compare clinical, radiographic outcomes, and complications following LE-ULBD and MIS-TLIF for degenerative spondylolisthesis. Methods: We conducted a retrospective review including patients with single-level, low-grade, stable, degenerative spondylolisthesis who were treated with LE-ULBD or MIS-TLIF. Patient demographics, operative data, and complications were collected. Clinical outcomes including Oswestry Disability Index (ODI), visual analog scale of back (VAS-B) and leg pain (VAS-L), neurologic recovery rate, and MacNab criteria were evaluated. Radiographic parameters including disc height (DH), lumbar lordosis (LL), slip angle (SA), and slip percentage (SP) were recorded pre- and postoperatively to assess progression of spondylolisthesis. Patients were scheduled for a follow-up examination at 1, 3, 6, 12, and 24 months postoperatively. Results: A total of consecutive 141 patients were included, consisting of 68 patients in LE-ULBD group and 73 patients in MIS-TLIF group. Demographic characteristics were not different between both groups. LE-ULBD had significantly shorter operative time and hospital stay than MIS-TLIF group. Patient satisfactions and clinical outcomes including ODI, VAS-L, and neurologic recovery rates were improved postoperatively in both groups with no significant difference at all follow-up periods. Interestingly, LE-ULBD group had significantly higher VAS-B at 12 and 24 months than MIS-TLIF group (3.1 vs 1.2, p < 0.05 and 2.8 vs 0.4; p < 0.05, respectively). Moreover, MIS-TLIF group had significantly better improvement in radiographic parameters including the DH, SP, and SL at final follow-up, while the lumbar lordosis was not different between both groups. Overall complication rates were also similar but the reoperation rate was slightly higher following LE-ULBD than MIS-TLIF (4.8% vs 2.7%, p > 0.05). Conclusion: For stable, degenerative spondylolisthesis, LE-ULBD is an effective minimally invasive surgical treatment with comparable efficacy, safety, and patient satisfaction to MIS-TLIF. However, a further study is required to investigate back pain and instability following LE-ULBD at longer follow-up period.
1058
A007: Outpatient percutaneous endoscopic lumbar interbody fusion under local anaesthesia in an awake and aware patient - study of 54 patients
Varun Agarwal 1
1 Orthopedics, Rohilkhand Medical College and Hospital, Bareilly, India
Introduction: Many surgical approaches from conventional open TLIF, MIS TLIF etc have been used for spinal fusion. Endoscopic Lumbar interbody fusion through a Kambin triangle is a minimal invasive procedure which can be done under local anesthesia, without muscle splitting, with short hospital stay and minimal complications compared to other techniques used. The aim of this study was to evaluate the functional outcomes following EndoLIF under local anesthesia for lumbar fusions. Material and Methods: This Retrospective study was conducted between November 2020 and August 2022 in orthopaedics department of Rohilkhand medical college and hospitals, Bareilly, U.P. This study included 54 patients with radicular pain for at least three weeks with a positive nerve root compression sign and lumbar instability and underwent percutaneous EndoLIF under Local anesthesia. Visual analogue score (VAS) and Oswestry Disability Index (ODI) has been used for pre and post-operative clinical assessment of the patients, follow up was done at 6 weeks, 3 months, 6 months and 1 year postoperatively. Results: Maximum patients were in the age group of 61 to 70 years and 65.2% of the patients were males. 68.2% patients had lumbar instability at L4-L5 level. The mean operative time of EndoLIF was 50.6 minutes. Out of 16 cases of L5-S1 disc prolapse, 1 case was operated by making an iliac bone window due to inaccessibility of disc space because of highly placed iliac crest. The mean preoperative VAS and ODI scores were 8.1 and 56.6 respectively. The Post operative VAS and ODI scores were dramatically improved at each follow up interval (p < 0.0001). Out of 66 patients who underwent operation, 4 patients developed Surgical site infection and 2 were found to have dysesthesia, no serious complications were noted. Conclusion: Percutaneous EndoLIF has been shown to be a safe, effective and minimally invasive alternative for the treatment of lumbar instability requiring fusion. The procedure proved to be advantageous as it had shorter operative time, less blood loss, early recovery period, less postoperative work disability, lesser rate of complications, and epidural scarring, thus facilitating easy revision surgeries as and when indicated, clearly point toward a better acceptance of the endoscopic techniques and their potential large usage in the coming times.
1851
A008: Full-endoscopic versus microscopic unilateral laminotomy for bilateral decompression of lumbar spinal stenosis at L4-L5
Kuo-Tai Chen 1 , Kyung-Chul Choi 2 , Dong-Chan Lee 3 , Hyeong-Ki Shim 3 , and Jin-Sung Luke Kim 4
1 Neurosurgery, Chang Gung Memorial Hospital Chiayi Branch, Puzi City, Taiwan
2 Neurosurgery, Seoul Top Spine Hospital, Goyang, South Korea
3 Neurosurgery, The Leon Wiltse Memorial Hospital, Anyang, South Korea
5 Neurosurgery, Seoul St. Mary’s Hospital, Seoul, South Korea
Introduction: Full-endoscopic spine surgery for degenerative lumbar diseases is growing in popularity and has shown favorable outcomes. Lumbar endoscopic unilateral laminotomy for bilateral decompression (LE-ULBD) has been used to treat lumbar spinal stenosis (LSS). However, studies comparing LE-ULBD to microscopic ULBD are lacking. This study compared the clinical efficacy and radiological outcomes between the LE-ULBD and microscopic ULBD. Material and Methods: The study retrospectively enrolled patients undergoing either LE-ULBD or microscopic ULBD for spinal stenosis at the L4-L5 level. The demographic data, operative details, radiological images, clinical outcomes, and complications of patients from the two groups were compared through matched-pairs analysis. The minimum follow-up duration was 24 months. Results: There were 93 patients undergoing either LE-ULBD (n = 42) or microscopic ULBD (n = 51). The patient demographics were similar between the two groups. The LE-ULBD group had significantly less estimated blood loss, less analgesic use, and shorter hospitalization duration (p < .05). The endoscopic group had a significantly lower visual analog scale for back pain at all follow-up intervals compared with the microscopic group (p < .05). There were no significant differences in leg pain or Oswestry Disability Index. The cross-section area of the spinal canal was significantly wider after microscopic ULBD. There were no significant differences in postoperative degenerative changes in disc height, translational motion, or facet preservation rate. Conclusion: LE-ULBD is comparable in clinical and radiological outcomes with enhanced recovery for single-level LSS. The endoscopic approach might further minimize tissue injury and enhance postoperative recovery.
289
A009: Review of the vascular anatomy of the lower lumbar spine. An endoscopic spine surgeon's perspective
Yilun Huang 1 , Dae Jung Choi 2 , Jin-Ho Hwang 2 , and Moon-Chan Kim 2
1 Orthopaedic Surgery, Seng Kang General Hospital, Singapore, Singapore
2 Orthopaedic Surgery, Himanaera Hospital, Busan, South Korea
Study design: An analysis of the vascular anatomy in the lower lumbar spine that will be encountered by the everyday endoscopic spine surgeon. Objective: To better define the vascular anatomy of this region from the perspective of the endoscopic spine surgeon, thus improving surgical handling of bleeding spots intraoperatively and reducing post operative complications. Summary of background data: Limited study and papers have described the vascular anatomy of the lower lumbar spine that is faced by a posterior biportal endoscopic approach. The increase in popularity of endoscopic approach for spinal decompression in the last decade render this paper to be clinically useful. Methods: We reviewed previously recorded operating video clips of 50 cases of extraforaminal and 50 cases of interlaminar approach using biportal endoscopic spine surgery (BESS). Several bleeding foci were matched with previously known vascular anatomy and adapted to a biportal endoscopic view to give endoscopic spine surgeon a better understanding of the anatomy and the vasculature that they can possibly encounter during surgery. Results: There were four main arterial branches coming out from the lumbar segmental artery. Inferior articular artery, superior articular artery, inter-articular artery and radicular artery could be faced in order during extra-foraminal or inter-laminar approaches using BESS. To escape heavy bleeding from the inferior articular artery and superior articular artery, the dorso-distal surface of transverse process (TP) should be exposed to make a working space without scratching the proximal area of the TP and dorsal surface of the facet during extra-foraminal approach. Inter-articular artery was hidden and covered under the capsule overlying superior articular process. Radicular artery was running along the midline of the root under the foraminal ligamentum flavum. With a inter-laminar approach, endoscopic spine surgeon needs to pay attention to the contribution of vessels from inferior, superior and inter articular artery will be at a 5 7 and 9 o’clock positions on the superficial endoscopic view. Within the spinal canal, multiple branches from the radicular artery are also highlighted as potential bleeding spot during surgery. Conclusions: The information of the geometric location of the four arterial branches could help to escape heavy bleeding on various approaches and control the bleeding foci to prevent postoperative hematoma in biportal endoscopic spine surgery.
OP02: Adult Deformity 1
658
A010: Patient and procedural risk factors for deterioration in Lower Extremity Motor Scores (LEMS) following adult spinal deformity surgery
Sarthak Mohanty 1 , Fthimnir Hassan 2 , Lawrence Lenke 2 , Douglas Burton 3 , Alan Daniels 4 , Munish Gupta 5 , Richard Hostin 6 , Khaled Kebaish 7 , Michael Kelly 5 , Han Jo Kim 8 , Eric Klineberg 9 , Stephen Lewis 10 , Peter Passias 11 , Themistocles Protopsaltis 11 , Frank Schwab 12 , Christopher Shaffrey 13 , Justin Smith 13 , Renaud Lafage 14 , Virginie Lafage 14 , Shay Bess 15 , and International Spine Study Group (ISSG) 16
1 Perelman School of Medicine at the University of Pennsylvania, Philadelphia, United States
2 Department of Orthopaedic Surgery, Columbia University Medical Center, The Och Spine Hospital at New York-Presbyterian, New York, United States
3 Department of Orthopaedic Surgery, University of Kansas Medical Center, Kansas City, United States
4 Department of Orthopaedic Surgery, University Orthopedics, Providence, United States
5 Department of Orthopaedic Surgery, Washington University – SOM, St. Louis, United States
6 Department of Orthopaedic Surgery, Swedish Neuroscience Institute, Seattle, United States
7 Johns Hopkins Medical Institute, Department of Orthopaedic Surgery, Baltimora, United States
8 Hospital for Special Surgery, Department of Orthopaedic Surgery
9 Department of Orthopaedic Surgery, University of California, Davis, United States
10 Department of Surgery and Spine Program, University of Toronto, Canada
11 Department of Orthopaedic Surgery, NYU Hospital for Joint Diseases - Langone Medical Center, New York, United States
12 Department of Orthopaedic Surgery, Lenox Hill Hospital, New York, United States
13 Department of Neurosurgery, University of Virginia Medical Center, Charlottesville, United States
14 Department of Orthopaedic Surgery, Northwell Health, New York, United States
15 Department of Orthopaedic Surgery, Denver International Spine Center/Presbyterian St. Luke's Medical Center, Denver, United States
16 International Spine Study Group
Introduction: The prospective Scoli-Risk-1 study assessed neurological outcomes using lower extremity motor score (LEMS) following complex adult spinal deformity (ASD) surgery. That study, complete nearly a decade ago, reported a decline in LEMS in 22% of patients at hospital discharge. Furthermore, patients who developed a new motor deficit suffered the greatest negative changes in HRQOLs. A recent, prospective, multicenter ASD study has been initiated and the following two aims are being investigated: to delineate the association of clinical variables with decline in LEMS; and to discern risk factors for LEMS decline in the early (6-wks) postop time frame. Methods: ASD patients undergoing posterior spinal fusion with or without concomitant lumbar anterior spinal fusion (ASF) between 2018 and 2021 at 18 spinal deformity centers in North America were entered into a multicenter database. All patients had baseline and postop LEMS obtained prospectively. The primary outcome in this analysis was the change in LEMS from preop to 6 wks postop. Patients were enrolled had one of the following radiographic and/or procedural criteria: PI-LL ≥ 25°, TPA ≥ 30°, SVA ≥ 15 cm, thoracic scoliosis ≥ 70°, thoracolumbar scoliosis ≥50°, global coronal malalignment ≥ 7 cm, and/or having a 3-column osteotomy, or spinal fusion ≥12 levels. Univariate and multivariable logistic regression models with Bonferroni’s corrections were built to quantify the degree to which a patient's postoperative LEMS was related to clinical characteristics. Results: 205 patients, with an average age of 61 (SD:16.1), 67.3% females, were analyzed. Greater proportion of patients reported normal LEMS postoperatively (70.2% vs 65.4%, p < 0.0001). Of 134 patients with normal baseline LEMS, 18.7% had abnormal postoperative LEMS, declining by an average of -2.52 (−4.68 – −0.36) points, while 36/71 (50.8%) reported normalization of baseline abnormal LEMS. Of 19 patients who were observed to have neuromonitoring changes intraoperatively, 6 (31.6%) reported worsened LEMS post-operatively (p = 0.0158). However, no single measure was significantly associated with worsening postoperative LEMS: SSEP (p = 0.7542), MEP (p = 0.9551), dNEP (p = 0.1696), Wake-Up Test (p = 0.3748). Univariate regression revealed that older age (50-65yrs: 3.31 (1.07 - 12.56), > 65yrs: 5.03 (1.85 - 17.71)), male gender (2.6 3[1.41 - 4.96]), increased frailty (1.17 [1.05 - 1.33]), higher BMI (BMI < 25: 0.24 (0.11 - 0.51), BMI 25-30: 0.41 (0.19 - 0.85)), worse baseline LEMS [1.31 per point (1.17 - 1.49)], longer OR-time (1.15 per hour [1.01 - 1.32]), the presence of intraop neuromonitoring changes (3.84 [ 1.47 - 10.47]), and decompression (2.98 [1.54 - 6.07]) and PSO (2.25 [1.08 - 4.63]) were associated with a decline in LEMS postop. Of the variables associated with abnormal postoperative LEMS, pre-operative LEMS is the most prominent, independent driver of abnormal 6-week LEMS. Each point decrease in preoperative LEMS confers 1.27x higher odds of abnormal perioperative LEMS. Conclusion: This study demonstrated that 18.7% of patients undergoing ASD surgery had a decline in LEMS at the 6-week postop assessment. However, there was a normalization of baseline abnormal LEMS in 50.8% of patients. Elderly patients and those with higher BMI, greater EBL, and undergoing PSO and decompression may be more susceptible to a decline in LEMS. However, the presence, and magnitude of preoperative lower extremity motor deficit was the strongest predictor of a decline in perioperative LEMS.
248
A011: Increased pelvic implant density is associated with lower rates of acute pelvic fixation failure
Christopher Martin 1 , Kenneth Holton 1 , Rajiv Dharnipragada 1 , Paul Soriano 1 , Kristen Jones 1 , Jonathan N. Sembrano 1 , Nathan Hendrickson 1 , and David Polly 1
1 University of Minnesota, Minneapolis, United States
Introduction: Higher magnitude deformity corrections, particularly in the sagittal plane, are known to be higher risk for pelvic fixation failure, but the impact of increased pelvic fixation density has not been well studied. A previous study performed at our institution found an unexpectedly high rate (5%, 6/125) of acute pelvic fixation failure occurring within 6 months of the index procedure. This rate was confirmed by a multi-center study, 5% (37/779). Materials and Methods: Comparative consecutive cohort study of chronological time periods of multiple surgeons at a single intuition. Adult spinal fusions of 3 or more levels, and which included new pelvic fixation from 7/2019-12/2020 (subsequent) were compared to 3/2017-6/2019 (initial) cohort. Acute pelvic fixation failure was defined as occurring within 6 months of the index surgery and requiring revision. Radiographic and surgical parameters were compared between cohorts. Pelvic implants included iliac screws, S2AI screws, and triangular titanium rods. Results: Pelvic implant density was higher in the subsequent cohort (3.1 v. 2.1, p < 0.001) with multiple pelvic implants (≥ 3) occurring in 60/102 of the subsequent cohort and 8/125 in the initial cohort. The incidence of pelvic fixation failures in the subsequent cohort was 0% (0/101 cases), as compared to 5% (6/125 cases) in the initial cohort (p = 0.03). Across cohorts, no significant difference between age (p = 0.59), sex (p = 0.68), BMI (p = 0.49), and levels operated (p = 0.16) was found. The follow-up cohort had lower magnitude surgical corrections, particularly in the sagittal plane, mean change in lumbar lordosis (9.04 v. 18.23, p < 0.001) and TPA (5.6 v. 21.8, p < 0.001). Conclusion: Higher density of pelvic fixation and lower magnitude sagittal plane corrections were associated with decreased rates of acute pelvic fixation failure. This finding builds upon previous studies which reported on surgical correction and technical reasons for failure, and implicates the density of pelvic fixation as a potential protective factor.
335
A012: Post-operative bracing following adult spine deformity surgery: results from the AO Spine survey of post-operative management of adult spine deformity patients
So Kato 1 , Justin Smith 2 , Stephen Lewis 3 , Christopher Shaffrey 4 , Lawrence Lenke 5 , and AO Spine KF Deformity 6
1 The University of Tokyo, Japan
2 University of Virginia, Charlottesville, United States
3 University of Toronto, Canada
4 Duke University, Durham, United States
5 Columbia University, New York, United States
6 AO Foundation
Introduction: Mechanical failures, such as proximal junctional kyphosis (PJK) and rod fracture, are common after adult spine deformity (ASD) surgery. The etiologies of these adverse events are multifactorial, and post-operative management may play an important role. Some surgeons favor spine bracing after ASD surgery to help prevent these complications, while others disfavor brace usage and the evidence that supports its rationale has been scarce. The objective of the present study is to better understand the current trend in use of bracing following ASD surgery based on an international survey. Material and Methods: An e-mail-based online survey was conducted among AO Spine international members with regard to postoperative management of ASD patients. Details of brace prescription (type and duration) as well as its indications and influencing factors were solicited. Descriptive data were summarized and comparisons were made based on different demographic groups and fusion levels for the responding surgeons who annually perform at least 10 long-segment fusions of >5 levels extending to the pelvis. Results: A total of 116 responses were received, including 71 surgeons (61%) who use postoperative bracing for long fusion >5 levels (28% routinely and 33% only selectively), while the rest denied brace usage. Among 71 brace prescribers, 34% denied use for fusions not extending to pelvis. The majority (56%) use bracing for 6 to 12 weeks after the surgery, while 7% use for less than 4 weeks, and 6% use more than 20 weeks. The most typical reasons for bracing were pain management (55%), followed by construct protection (49%), PJK prevention (37%), and fusion enhancement (25%). Bone quality was the strongest influencing factor (69%), but age of the patient (42%), procedure performed (41%), level of fusion (39%), perceived patient activity (38%), intraoperative screw purchase (34%) and patient body habitus (31%) also affected use of bracing. Surgeons from Asia-Pacific had the highest rate of bracing (88%), and North American surgeons had the lowest rate (45%). The most common type of brace used was custom molded or prefabricated TLSO for cases with an upper-most instrumented vertebra (UIV) in the low- or mid-thoracic spine (47% for UIV at T7-12, 58% for UIV at T4-6, among valid responses), followed by hyperextension braces, such as Jewett, CASH and dorsolumbar brace (32% for T7-12 and 22% for T4-6). For UIV at T1-3, a cervical brace, such as a SOMI, cervical collar or CTLSO were the most commonly used (40%). Conclusion: Given the lack of robust scientific evidence to support the routine use of postoperative bracing in this cohort, as well as the diverse patient backgrounds, clinicians’ bracing practices seem to largely depend on experience and personal preference. The present survey demonstrates significant variability in postoperative bracing practice following ASD surgery in terms of prescription, duration, indication and type. Formal study of the role of bracing following ASD surgery is needed.
498
A013: Defining the quality of intraoperatively salvaged blood in spinal deformity surgery and its suitability for autologous transfusion: preliminary results of a prospective study
David Kurland 1 , Andrew Smith 1 , Daniel Alber 1 , Alexander Cheung 1 , Shah Ahmed 2 , Anthony Frempong-Boadu 1 , and Darryl Lau 1
1 Neurosurgery
2 Anesthesiology, NYU Langone Health, New York, United States
Introduction: Studies in the corpus of cardiac, vascular, transplant, and obstetrics surgery literature have shown clinical benefits and cost-effectiveness of utilizing red blood cell (RBC) salvage and autologous transfusions. Despite mixed supporting evidence, these positive effects are commonly assumed in the context of spinal deformity surgery. Studies in the spine literature suggest that RBC salvage reduces intraoperative allogeneic transfusions, but not postoperative transfusions, calling the quality and health of these salvaged RBCs into question. We postulate that electrocautery, exposure to foreign surgical materials and prolonged stasis prior to collection lead to irreversible cellular injury that decreases RBC survivability and oxygen carrying capacity. This is in contrast to other surgical subspecialities in which blood is often salvaged directly with low risk of cellular injury. Here, we present the initial results of an ongoing prospective study to define the quality, rheological profile, and clinical utility of intraoperatively salvaged RBCs in spinal deformity surgery. Material and Methods: Patients undergoing spinal deformity surgery booked with intraoperative RBC salvage (Cell Saver, HAEMONETICS®) were prospectively enrolled (N = 25). Patient characteristics and surgical details were collected. Baseline and Post-operative blood samples were drawn directly from the patient. When available, samples were drawn sterile from the autologous Cell Saver product and allogeneic RBCs (Blood Bank), immediately prior to administration to the patient. Laboratory testing was carried out on all samples [CBC, BMP, PT/INR, PTT, LDH, plasma free hemoglobin (pf-Hgb)]. Virtual blood smears were prepared from samples via Stimulated Raman Histology (NIO Laser Imaging System, Invenio) for morphological evaluation. Intra- and post-operative resuscitative measures (crystalloid, colloid, pressors, blood products, e.g.) were also tabulated for each patient. Results: There was a linear relationship between estimated blood loss (EBL) and volume of salvaged RBCs. The blood volume salvaged was sufficient for autologous transfusion in 63% of cases, with an average of 167 mL transfused. Reflecting differences in their storage solutions, both Cell Saver and Blood Bank samples differed significantly from Baseline on laboratory testing. Morphologically, Cell Saver samples had a high proportion of shrunken and irregularly spiculated RBCs (acanthocytes), consistent with alterations in membrane structure. LDH and pf-Hgb were significantly elevated in Cell Saver samples, suggestive of extravascular RBC lysis (p < 0.05). Notably, the hemolysis index (HI) was significantly elevated in Cell Saver samples, exceeding levels suitable for transfusion by FDA standards (p < 0.05). Additionally, in Post-operative samples, both LDH and pf-Hgb were significantly elevated in patients who received autologous transfusions, suggestive of ongoing intravascular RBC lysis (p < 0.05). Preliminary analysis suggested no difference in the need for intra- or post-operative resuscitative measures in patients who received autologous transfusions. Conclusion: Our preliminary results suggest that techniques commonly employed in modern spinal surgery cause irreversible injury to RBCs destined for autologous transfusion, and thus may decrease the suitability of salvaged RBCs as a blood replacement, and even offer a false sense of adequate resuscitation. Experiments to assess ex-vivo mechanical fragility as well as membrane deformability via ektacytometry are in process. Robust multivariate analysis is planned after additional patient enrollment (N = 200 anticipated).
458
A014: Validation of the MISDEF2 algorithm for adult spinal deformity: analysis of 2-year clinical and patient reported outcomes
Ibrahim Hussain 1 , Andrew Chan 2 , Nitin Agarwal 3 , Khoi Than 4 , Christopher Shaffrey 4 , Paul Park 5 , Juan Uribe 6 , Richard Fessler 7 , Adam Kanter 8 , David Okonkwo 8 , Gregory Mundis 9 , Robert Eastlack 9 , Pierce Nunley 10 , Neel Anand 11 , Michael Virk 1 , Jacob Goldberg 1 , Vivian Le 12 , Shay Bess 13 , Michael Wang 14 , Dean Chou 2 , Praveen Mummaneni 12 , and Kai-Ming Fu 1
1 Neurosurgery, Weill Cornell-New York Presbyterian Hospital, New York, United States
2 Columbia University, New York Presbyterian Hospital, New York, United States
3 Washington University in St. Louis, United States
4 Duke University, Durham, United States
5 University of Michigan, Ann Arbor, United States
6 Barrow Neurologic Institute, Phoenix, United States
7 Rush University, Chicago, United States
8 University of Pittsburgh, United States
9 Scripps Clinic, San Diego, United States
10 Spine Institute of Louisiana, Shreveport, United States
11 Cedars-Sinai Medical Center, Los Angeles, United States
12 University of California San Francisco, United States
13 Denver International Spine Center, Presbyterian St. Luke’s/Rocky Mountain Hospital for Children, Denver, United States
14 University of Miami, United States
Introduction: The Minimally Invasive Spinal Deformity Surgery Algorithm was developed to provide a framework for decision making in adult spinal deformity (ASD) and was updated in 2019 (MISDEF2) to incorporate more advanced techniques and interbody technologies. This study evaluated if application of the MISDEF2 was consistent with its radiographic components, degree of invasiveness, and if adherence to the algorithm resulted in successful clinical outcomes. Material and Methods: A retrospective review of a prospectively maintained database of patients undergoing minimally invasive surgery (MIS) for ASD was performed. Patients were stratified according to the MISDEF2 as Class I (fusion of a listhetic level), Class II (multi-level MIS), or Class III (circumferential MIS with anterior column release or hybrid MIS-open surgery). Baseline radiographic and perioperative variables were collected, as were 90-day postoperative complications, 1- and 2-year patient reported outcome measures (PROMs), and 2-year revision surgery rates. Results: 85 patients were enrolled and stratified as Class I (N = 7), II (N = 37), and III (N = 41). There were no significant differences in baseline age, American Society of Anesthesiologists (ASA) score, Frailty Index, Charlson Comorbidity Index, Oswestry Disability Index (ODI), EQ-5D, or SF-36 Physical Component Score (PCS). Statistically significantly differences among Classes were noted with lumbar lordosis-pelvic incidence (LL-PI) mismatch and pelvic tilt (PT), with a nonsignificant trend in sagittal vertical axis (SVA). There were significant incremental increases in number of osteotomy levels (0 vs. 0.1 vs. 1.2, p < 0.001), instrumented levels (1 vs. 3.7 vs. 6.1, p < 0.001), and number of interbodies (1 vs. 3.1 vs. 3.6, p < 0.001). 90-day overall and major complication rates were 25.9% and 7.1%, respectively, with the highest rates observed in Class II (35.1% and 13.5%, respectively). Overall 2-year revision rate was 15.3% (0% vs. 13.5% vs. 19.5%), mostly due to neurologic symptoms, radiographic imbalance/junctional pathology, and implant failure/pseudarthrosis. All Classes demonstrated statistically significant improvements in ODI, EQ-5D, and SF-36 PCS at 1-year postoperatively, and for Class II and III at 2-years postoperatively. Conclusion: Our data supports the MISDEF2 as a validated tool for surgical decision making and correlates with clinical outcomes in minimally invasive approaches for ASD surgery.
1416
A015: Comparison of multi-level low grade technique versus three column osteotomies in adult spinal deformity surgery: does harmonious correction matter?
Peter Passias 1 , Tyler Williamson 1 , Peter Tretiakov 1 , Kimberly McFarland 1 , Jamshaid Mir 1 , Pooja Dave 1 , Rachel Joujon-Roche 1 , Shaleen Vira 2 , Jordan Lebovic 1 , Stephane owusu-saprong 1 , Andrew Schoenfeld 3 , Bassel Diebo 4 , Renaud Lafage 5 , and Virginie Lafage 5
1 NYU Langone Medical Center, New York, United States
2 UT Southwestern Medical Center, Dallas, United States
3 Brigham and Women’s Hospital/Harvard Medical Center, Boston, United States
4 SUNY Downstate Medical Center, New York, United States
5 Lenox Hill Hospital, New York, United States
Introduction: Recent debate has arisen between whether to use a three-column osteotomy or multiple level, low-grade techniques to treat more rigid deformities in adult spinal deformity (ASD) surgery. Therefore, we examined the performance of three-column (3CO) osteotomies versus multi-level low-grade (MLG) techniques in ASD patients undergoing corrective surgery. Purpose: To compare the complication rates, radiographic and clinical outcomes of three-column osteotomies and multi-level low-grade techniques performed in ASD corrective surgeries. Study Design/Setting: Retrospective cohort study of a prospectively collected database. Patient Sample: 111 ASD patients. Outcome Measures: postoperative alignment; mechanical complication, PJK, reoperation; Smith et al. Best Clinical Outcome for ODI and SRS. Methods: Included: ASD pts with baseline PI-LL > 30° and 2Y data. Groups: 1) 3CO or 2) MLG (3+ Smith-Peterson osteotomies or 3+ ALIF interbodies between T12-S1 with no 3CO). Groups were propensity score matched (PSM) for BL PI-LL and prior fusion. Segmental Utility Ratio (SU Ratio) assessed relative segmental correction, defined as segmental correction divided by overall correction in lordosis divided by number of thoracolumbar interventions (IBF, SPO, 3CO). Paired t-test assessed lordotic distribution by differences in lordosis between adjacent lumbar disc spaces (i.e. L1-L2 to L2-L3, etc). Analysis of Variance (ANOVA) and binary logistic regression analysis evaluated the complication rates, radiographic and patient-reported outcomes between groups. Results: 111 ASD patients included. Of these patients, 44% underwent an MLG and 40% underwent a 3CO. Notably MLG had higher CCI and lower BMI (both p < .05). MLG pts underwent significantly less revisions than 3COs (31% vs. 80%, p < .001). MLG patients accrued 43% less blood loss (p < .001), but 22% greater operative time (511 min vs. 419, p = .015). Upon PSM for revision status and BL PI-LL (23 in each group), 3COs had greater segmental and relative correction at each level (SU Ratio means: 3CO 69% vs. MLG 23%, p < .001). However, 3COs had lordotic differences between two adjacent lumbar disc pairs (range: -0.5-8.4°, p = .015), while MLG was more harmonious (range: 2.4-5.4°, p>0.6). MLG were more often realigned to age-adjusted standards (OR: 5.6, [1.2-46.4]; p = .033). MLG were less likely to develop neurological complications or undergo reoperation (OR: 0.4, [0.1-0.9]; p = .041). MLG patients more often met SCB in ODI (OR: 5.3, [1.1-26.8]; p = .043). Conclusion: Multi-level low-grade techniques showed better utility in lumbar distribution and age-adjusted global correction, while minimizing neurological complications and reoperation rates by 2 years. In selective instances, these techniques may offer the spine deformity surgeon a safer alternative when correcting severe adult spinal deformity.
512
A016: How to use preoperative pelvic obliquity, leg length discrepancy, and lower extremity compensation as an intraoperative tool to predict postoperative coronal alignment for adult spinal deformity with 2 years follow up
Nathan Lee 1 , Michael Fields 1 , Gerard Marciano 1 , Matthew Simhon 1 , Cole Morrissette 1 , Fthimnir Hassan 1 , Christopher Mikhail 1 , Stephen Stephan 1 , Joshua Baksheshian 1 , Andrew Platt 1 , Joseph Lombardi 1 , Zeeshan Sardar 1 , Ronald A. Lehman 1 , and Lawrence Lenke 1
1 Orthopedic Surgery, Columbia University, Och Spine Hospital, New York, United States
Introduction: The major challenges with determining intraoperative coronal alignment for adult spinal deformity (ASD) surgery include the inability to quantify verticality in the prone position, pelvic obliquity (PO) changes between erect and prone films, leg length discrepancy (LLD), and lower extremity (LE) compensation (e.g. asymmetric knee bending, LE mechanical axis difference s[LMAD]). The horizontal distance from C7 to the central sacral pelvic line (C7-CSPL; CSPL = line bisecting the sacrum and perpendicular to the line touching the acetabular sourcils) was recently introduced as a potential target for intraoperative CVA; however, this may fail in the presence of LLD and PO. To account for this, we describe a system to better guide intraoperative coronal alignment. Material and Methods: Two lines are drawn on intraoperative prone films: CSPL (as described above) and “Proxy CSVL,” which is drawn relative to CSPL based on the preop erect PO. The C7-CSPL and iCVA (intraoperative distance from C7 to “Proxy CSVL”) are compared with actual immediate postop CVA and 2 year postop CVA. To account for LLD and preoperative LE compensation, patients were categorized into 4 preoperative groups: Type 1 = No LLD (<1 cm) and No LE compensation; Type 2 = No LLD with LE compensation (PO > 1 deg, asymmetric knee bending, LMAD > 2 deg); Type 3 = LLD and No LE compensation, and Type 4 = LLD with LE compensation (asymmetric knee bending, LMAD > 4 deg). A retrospective review of a consecutively collected cohort with ASD min 6 level fusion with pelvic fixation was performed to validate. Results: 102 patients (age 57.7 ± 13.7yrs, levels fused 14.0 ± 3.9) were reviewed. Mean preop/2 year postop CVA was 5.0 ± 2.0/2.2 ± 1.8cm. Type 1: both C7-CSPL and iCVA had similar error margins for immediate postop CVA (0.4 vs.0.4 cm, p = 0.962) and 2 yearr postop CVA (0.3 vs.0.4 cm, p = 0.187). Type 2: C7-CSPL was more accurate for immediate postop CVA (0.8 vs.1.8 cm, p < 0.01) and 2 year postop CVA (0.7 vs.2.1 cm, p < 0.01). Type 3: iCVA was more accurate for immediate postop CVA (0.3 vs. 1.9 cm, p < 0.01) and 2 year postop CVA (0.2 vs. 2.0 cm, p < 0.01). Type 4: iCVA was more accurate for immediate postop CVA (0.6 vs. 3.2cm, p < 0.01) and 2 year postop CVA (0.5 vs. 3.2 cm, p < 0.01). Conclusion: This system, which accounts for LLD and preop LE compensation, provides an intraoperative guide to optimize both immediate and 2 year postoperative CVA with high accuracy. For Type 1 and 2 (No LLD with or without LE compensation), C7-iCSPL accurately predicts postoperative CVA up to 2 year follow up (mean error = 0.5cm). For Type 3 and 4 (LLD with or without LE compensation), iCVA accurately predicts postoperative CVA up to 2 year follow up (mean error = 0.4 cm).
1006
A017: How would spino-pelvic fixation construct impact on the post-operative compensatory mechanisms in patients with adult spine deformity?
Maroun Rizkallah 1 , Ghassan Boubez 1 , Jesse Shen 1 , Frederic Lavoie 1 , Nicholas Newman 1 , Fidaa Al-Shakfa 2 , Daniel Shedid 3 , Sung-Joo Yuh 3 , Yousef Kamel 4 , Jia Liu 4 , and Zhi Wang 1
1 Orthopedic Surgery
2 Centre de Recherche
3 Neurosurgery Department, Centre Hospitalier de l'Universite de Montreal, Montreal, Canada
4 Ecole de Medecine, Universite de Montreal, Montreal, Canada
Introduction: Few papers have evaluated the reciprocal change of the body’s sagittal profile after spino-pelvic fusion in patients with adult spine deformity (ASD). This is the first study to compare the post-operative changes in the compensatory mechanisms of the sagittal balance according to the type of pelvic fixation: S2-Alar-iliac screws (S2AI) versus iliac screws (IS), in patients with ASD. Material and Methods: This retrospective monocentric study included ASD patients who underwent spino-pelvic fixation and remained with a PI-LL > 10⁰ mismatch post-operatively. Standing whole body lateral EOS imaging was performed pre-operatively and at the 6 months of post-operative follow-up for all included patients. Pre and post-operative PI, Lumbar lordosis (LL), pelvic tilt (PT), sacral slope (SS), thoracic kyphosis (TK), femur obliquity angle (FOA), knee flexion angle (KFA) and ankle flexion angle (AFA) were analyzed. Patients were categorized based on the type of pelvic fixation (S2AI vs IS), and the pre-operative to post-operative changes in the compensatory mechanisms were compared between both groups. Results: A total of 79 patients with a mean age of 67.8 ± 9 years were included. Mean PI went from 58.01 ± 15⁰ pre-operatively to 58.41 ± 12⁰ post-operatively (p = 0.86). Mean PI-LL decreased from 23.8 ± 14⁰ pre-operatively to 19.44 ± 10⁰ post-operatively (p = 0.03). Patients with S2AI (n = 53) and those with IS (n = 26) were comparable for the baseline pre-operative criteria, mainly PI (57.9⁰ vs 58.2⁰, p = 0.93) and PI-LL (27.1⁰ vs 28.1⁰, p = 0.56). The pre-operative to post-operative change in SS averaged 7.2⁰ in the S2AI group compared to 9.9⁰ in the IS group (p = 0.001), whereas the KFA pre-operative to post-operative change reached 6.1⁰ in the S2AI group as opposed to 3.5⁰ in the IS group (p = 0.02). The PT pre- to post-operative change was comparable between both groups (6.3⁰ for S2AI group vs 5.2⁰ for IS group, p = 0.42), together with the TK pre- to post-operative change (11.5⁰ for S2AI group vs 10.5⁰ for IS group, p = 0.59). The FOA pre- to post-operative change averaged 3.2⁰ in both groups (p = 1) whereas the AFA angle changed 3.1⁰ from pre-operatively to post-operatively in the S2AI group and 2.8⁰ in the IS group (p = 0.72). Conclusion: This study is the first to show that the type of pelvic fixation impacts significantly on the post-operative compensatory mechanisms of the body’s sagittal profile in patients with ASD. Patients with S2AI screws are more likely to compensate their remaining post-operative PI-LL mismatch through their knees and less likely through their sacrum compared to patients with IS. This could be explained by a lower resistance of the iliac connectors to the junctional mechanical stresses, allowing for some degrees of sacro-iliac joint motion, as opposed to the rigid sacro-iliac fixation offered by the S2AI screws constructs.
1097
A018: Thromboembolic disease following adult spinal deformity surgery: an analysis of over 8,500 spinal deformity patients
Daniel Gallagher 1 , Takshi Hirase 2 , Kevin Bondar 2 , Jacob Harris 3 , Darrell Hanson 2 , Rex Marco 2 , and Comron Saifi 2
1 Medical Education, Robert Wood Johnson Medical School, New Brunswick, United States
2 Spine Surgery, Houston Methodist Hospital, Houston, United States
3 Orthopaedic Surgery, University of Pennsylvania, Philadelphia, United States
Introduction: Deep vein thrombosis (DVT) and pulmonary embolism (PE), collectively referred to as venous thromboembolism (VTE), represents a major postoperative complication. Despite validated, evidence-based guidelines to prevent VTE, approximately 350,000-900,000 individuals in the United States develop VTE each year. Given the risk for bleeding complications following spinal surgery, particularly epidural hematoma, there remains no consensus regarding the use or timing of chemical prophylaxis. No prior studies have evaluated the incidence and risk factors for VTE following ASD surgery with ≥ 7 vertebral levels. The objectives of this study were to evaluate the 30-day incidence of and risk factors for VTE following ASD surgery with ≥ 7 levels of instrumentation. Materials and Methods: A retrospective observational study was conducted using the ACS-NSQIP database for patients undergoing ASD surgery from 2010 to 2019. The NSQIP database collects more than 150 variables from over 600 participating hospitals in the United States. Each participating site has a trained and certified surgical clinical reviewer to extract preoperative to 30-day postoperative data for randomly assigned patients. The NSQIP has developed multiple processes to optimize accuracy and reliability of data collection, including an inter-rater reliability audit of selected sites. Using the ACS-NSQIP participant user file, patients from participating institutions, aged 18 years and older having surgical correction of ASD with ≥7 levels of correction, were identified using Current Procedural Terminology (CPT) codes 22843 and 22844. Methods were conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. Results: 8,533 patients met the inclusion criteria, with a mean age of 62 years and a female predominance (55%). Postoperative venous thromboembolism (VTE) was identified in 325 (3.81%) cases. Of these, 201 (2.36%) involved DVTs, and 157 (1.84%) involved PEs. Independent predictors of postoperative DVT identified by multivariate logistic regression included disseminated cancer, steroid or immunosuppressant use for a chronic condition, and preoperative hematocrit. Independent predictors of postoperative PE identified by multivariate logistic regression included female patients, black patients, and disseminated cancer. Patients undergoing elective surgery were less likely to have postoperative DVT and PE. Conclusion: DVT and PE represent major postoperative complications after complex ASD surgery. Black patients, patients with disseminated cancer, patients on chronic steroid or immunosuppressive therapies, and patients with lower preoperative hematocrit levels were at increased risk for VTE following ASD surgery with ≥7 levels of posterior instrumentation. Physicians should be aware that patients with one or more of these risk factors may require closer monitoring for VTE.
OP03: Machine Learning Anfd Augmented Reality
549
A019: Outcomes of restorative neurostimulation in patients with refractory chronic low back pain secondary to multifidus dysfunction: clinical preliminary results
Carlos Lijo 1 , Michael Selby 1 , YH Yau 1,2 , Derek Yull 1 , and Ian Whittle 1,3
1 3D Research, The International Spine Centre, Adelaide, Australia
2 Spine Unit, Royal Adelaide Hospital, Adelaide, Australia
3 Health and Medical Sciences, The University of Adelaide, Adelaide, Australia
Introduction: Multifidus muscle impairment can contribute to chronic low back pain (CLBP). As the main spine segment stabilizer, multifidus plays a crucial role in providing direct stabilization to the lumbar spine in response to changes in posture and protection against abrupt movements. Implantable neurostimulators (Reactiv8, Mainstay Medical, Dublin, Ireland) aimed specifically at improving multifidus function are a promising novel therapy. A two-year study evaluated the effectiveness of this restorative neurostimulator system (ReActiv8-B study - Gilligan et al, 2021) and showed significant improvements in pain, disability or both, in 76% of the 206 initial participants. These positive results provide evidence of long-term effectiveness and compelling endorsement of the Reactiv8. Our study describes results for Reactiv8 therapy from an independent spinal clinic and compares such data with the previous clinical trials. Material and Methods: StudyType: Prospective cohort study. Setting: Multidisciplinary Independent Spinal Clinic in an Australian capital city. Cohort: 64 patients with CLBP implanted with restorative neurostimulator system (Reactiv8,). All patients were managed and assessed using the timelines and some PROMS from the Reactiv8 B Trial. Clinical pain intensity (Visual Analog Scale - VAS) and disability (Oswestry Disability Index – ODI) were the primary outcome measures. These were assessed at baseline, three months, six months and twelve months after implant activation. Results: The first patient had surgery in March 2021. To date a total of 64 patients have been implanted. Preliminary results in 26 patients at the three months mark after the device implantation show a statistically significant mean group VAS improvement (5.62 to 4.39, p = 0.010). Oswestry Disability Index had improved by -11.2 (37.62 to 26.43, p = 0.009). Longer term data and more patient data will be presented. One patient had the device removed because of infection. Conclusion: The preliminary results of this study are compatible with the two-year results of the ReActiv8-B trial aimed at CLBP, multifidus dysfunctional patients. This recovery trajectory is consistent with restoration of neuromuscular control and structural muscle changes. Our aim is to demonstrate medium and long term outcomes with clinical and functional outcome parameters. Currently further data is being collected and will be adjoined to this study in the upcoming months.
1304
A020: Positive feedback exoskeleton robots in spinal cord injury show improved neuroplasticity and function: A systematic review
Ka Ioi Argus Chiu 1 , Priyanshu Saha 1 , Zion Hwang 1 , Emily Tsang 1 , Bisola Ajayi 2 , Jason Bernard 2 , Timothy Bishop 2 , and Darren Lui 2
1 Complex Neurosurgery, St Georges University of London, London, United Kingdom
2 Complex Neurosurgery, St Georges Hospital, London, United Kingdom
Introduction: Exoskeletons are utilised in the rehabilitation of spinal cord injury (SCI) as an adjunct to physiotherapy. Robots aid rehabilitation utilising changes in body position and weight shifts and mechanical repetition. Newer, positive feedback exoskeletons have been designed to identify electrical signals in the paralysed limbs that actively initiate and drive limb movements. Positive feedback eventually increases the amplitude of cerebral signals to generate unassisted movements and inducing neuroplasticity. There have been no previous studies comparing Exoskeleton robots in SCI. Material and Methods: A systematic review searched for Exoskeleton robots in SCI between 2011 and 2021. Comorbidities studied were 4 categories. 1) Continence: Wexner Score, Cleveland Clinic Constipation Score and self reports. 2) Mobility: the 6 Minute Walking Test and 10 Meter Walking Test 3) Pain: VAS, NRS and McGill Pain Questionnaire 4) HRQoL: SF36 and SWLS. Results: 6 exoskeletons were identified that examined the 4 categories, 5 are categorised as passive robotic control: Ekso Bionics, ReWalk, Indego, KAFO and AIDER. 1 robot provides active rehabilitation: HAL 1) Continence: ReWalk, Indego and HAL assessed continence. HAL used the Wexner score and a decrease from 8.89 to 6.51 with p = 0.008 was observed showing an improvement in continence. 2) Mobility: 6MWT and 10MWD KAFO, ReWalk, AIDER and Ekso assessed mobility using the 6MWT. They all showed an increase in ambulatory distance with aid of the robot post rehabilitation. AIDER and Ekso also used the 10MWT to assess mobility. Completion time decreased by 15.4% and 82.4% respectively post rehabilitation with aid of the robot. HAL assessed 6MWT and 10MWT without aid of the robot. Post rehabilitation, there was an average increase in ambulatory distance of 105.2% across 3 studies in the 6MWT and an average decrease in completion time by 88.65% in the 10MWT across 4 studies. In addition, HAL had better 6MWT and 10MWT compared to all the other Exoskeletons despite not needing their aid. 3) Pain: Indego, HAL, Ekso assessed pain. Only Ekso showed statically significant reductions in pain from 6.0 (IQR = 4.5-7.0) to 2.0 (IQR = 0.0-4.0). 4) HRQoL: Indego and HAL assessed HRQoL but only HAL showed a statistically significant increases in HRQoL based on the SF-36. Conclusion: Improvements in comorbidities were consistent across all exoskeletons. Only HAL and Ekso has shown statistically significant improvements with HAL showing more statistically significant improvements. HAL was the only Exoskeleton that allowed patients to walk without aid of the robot and also showed better 6MWT and 10MWT results without the assistance of the robot due to the amplification of cerebral signals to allow for unassisted movements suggesting the new positive feedback robot is more effective in spinal rehabilitation in patients with an SCI than traditional robots focused on weight changes and repetition.
1228
A021: Investigating the effectiveness of using augmented reality headset in spinal facet joint injections on human cadaver model
Ali Ekrem Adiyaman 1
1 Neurosurgery Dep., Istanbul University Faculty of Medicine, Istanbul, Turkey
Introduction: Facet joint injections are often performed with c-arm fluoroscopy in clinical practice. The c-arm fluoroscopy device emits X-rays, and radiation exposure occurs in use. In addition, the process is performed by looking at a separate screen on a two-dimensional image. Operating by looking at the two-dimensional image on the screen requires experience and is not easy, and it may shift the doctor's focus. Augmented reality technology, interacting with the real world, can reflect three-dimensional images created in the computer environment to the user's eye. Our study aims to perform facet joint injections with augmented reality headset compared to c-arm fluoroscopy. Material and Methods: We used five human cadavers. After the cadavers were marked with unique markers for the procedure, spinal CT was performed. CT data were processed using open-source programs called 3D Slicer and Blender, and a 3D model of the cadaver spine was created. A separate program was developed for each injection using the Unity and Vuforia Engine SDK image target system. These programs were run on the Microsoft HoloLens 2 augmented reality headset. Next, in the experimental group, a total of 72 needles (20 G, Spinocan, Braun) at 18 levels from C7-T1 to L5-S1 for two cadavers and 36 needles for three cadavers at six levels from T12-L1 to L5-S1 were placed. After the needles were placed, no medication was injected, and we performed a spinal CT to test the accuracy of the needle placements. After the needles were removed from the cadavers, facet joint injections were performed using the c-arm fluoroscopy in the control group, and then we performed a spinal CT. Results: Neuroradiologists independently evaluated each needle placements in the experimental and control groups based on the following scoring: unsuccessful, successful, and excellent. The independent sample t-test indicated that the success rate in 108 injections in the experimental group (X ¯ = 2.25, SS = 0.68) was slightly higher compared to the 108 injections in the control group (X ¯ = 2.12, SS = 0.66) but there was no statistically significant difference among two groups, t(214) = 1.51, p = .13. Conclusion: Compared to the c-arm fluoroscopy, the facet joint injections performed with the augmented reality headset provided no statistically significant differences in the success and safety rate in human cadavers. The study can act as a proof of concept to show the feasibility of using AR in facet joint injections. Furthermore, the procedure can be facilitated by moving it from a two-dimensional image to a three-dimensional image. Benefiting from these advantages, AR headsets can effectively improve the quality of the procedure, reduce the dependence on the experience of surgeons by eliminating the problem of focus switching, and reduce the intensity of the radiation exposure of the patient and healthcare personnel.
693
A022: Automatic recognition of whole-spine sagittal alignment and curvature analysis through a deep learning technique
Yu-Cheng Yeh 1 , Chi-Hung Weng 2 , Chao-Yuan Yeh 2 , and Tsung-Ting Tsai 1
1 Orthopaedic Surgery, Chang Gung Memorial Hospital, Linkou, Taoyuan City, Taiwan
2 aetherAI Co., Ltd., Taipei City, Taiwan
Introduction: Artificial intelligence based on deep learning (DL) approaches enables the automatic recognition of anatomic landmarks and subsequent estimation of various spinopelvic parameters. The locations of inflection points (IPs) and apices (APs) in whole-spine lateral radiographs could be mathematically determined by a fully automatic spinal sagittal curvature analysis system. Material and Methods: We developed a DL model for automatic spinal curvature analysis of whole-spine lateral plain radiographs by using 1800 annotated images of various spinal disease etiologies. The DL model comprised a landmark localizer to detect 25 vertebral landmarks and a numerical algorithm for the generation of an individualized spinal sagittal curvature. The char- acteristics of the spinal curvature, including the IPs, APs, and curvature angle, could thus be analyzed using mathematical definitions. The localization error of each landmark was calculated from the predictions of 300 test images to evaluate the performance of the landmark localizer. The interrater reliability among a senior orthopedic surgeon, a radiologist, and the DL model was assessed using the intraclass correlation coefficient (ICC). Results: The accuracy of the landmark localizer was within an acceptable range (median error: 1.7-4.1 mm), and the interrater reliabilities between the proposed DL model and each expert were good to excellent (all ICCs > 0.85) for the measurement of spinal curvature characteristics. Conclusion: The interrater reliability between the proposed DL model and human experts was good to excellent in predicting the locations of IPs, APs, and curvature angles. Future applications should be explored to validate this system and improve its clinical efficiency.
1908
A023: Effect of non fusion anterior scoliosis correction on shoulder balance in Lenke type 1 adolescent idiopathic scoliosis patients - is it detrimental or beneficial?
Dr Sajan Hegde 1 , Vigneshwara Badikkilaya 1 , Sharan Achar T 1 , Umesh Kanade P 1 , and Harith Reddy 1
1 Orthopaedics, Apollo Hospitals Chennai India, Chennai, India
Introduction: Cosmesis of the back and shoulders with a coronally balanced spine are the critical factors for any Adolescent idiopathic scoliosis (AIS) patient. Achievement of shoulder balance is one of the most important factor for patient satisfaction, in-turn measure of a successful scoliosis surgery. All the existing literature reports the importance of post operative shoulder balance following posterior fusion surgery and factors to be considered for the same. There is an evident dreath in the clinical data describing the effect of Anterior Vertebral Body Tethering (AVBT) on shoulder balance. Furthermore, we in our center use a modified technique of VBT, termed as Non Fusion Anterior Scoliosis Correction (NFASC) where we use segmental compression, de-rotation, apical translation and sequential tensioning of cord to achieve maximum intraoperative correction. This differentiates it from the actual AVBT technique which is mere tethering of the cord. Thus objective of this study is to evaluate the effect of Non Fusion ion Anterior Scoliosis Correction (NFASC) on shoulder balance in Lenke type 1 AIS patients. Materials and Methods: Single center, single surgeon retrospective study of 40 patients with Lenke type 1 AIS curve treated with NFASC at 2 years postoperatively (follow-up range: 21-48 months). Clinical photographs were compared pre and post operatively and shoulder angle, axilla angle, inner and outer shoulder heights were analysed. Image analysis software such as Image J (National Institute of Health, Bethesda, Maryland) was used. Radiologically, changes in the curvature, clavicular angle, T1 tilt angle and radiographic shoulder height were investigated. Results: Of the 40 patients, 95.56% were female with preoperative age 14.96 ± 2.69 years. The mean thoracic Cobbs angle was corrected by 69% at last follow up, 52.11˚ ± 7.74˚ preoperative compared to 16.92˚ ± 5.06˚ post-operative Cobbs. Axilla and shoulder angle clinically were 6° ± 2.7° and 5.5° ± 1.8° pre-operatively and 2.1° ± 0.8° and 1.8° ± 0.5° post operatively respectively (p < 0.001). Inner and outer shoulder height also improved post op though statistically insignificant. Absolute clavicular angle and T1 tilt angle also showed a drastic improvement from 8.6° ± 2.1° and 10.7° ± 3.4° preoperatively to 1.8° ± 0.7° and 2.8° ± 1.7° at 2-year follow-up (p < 0.005). Preoperatively, absolute shoulder height averaged 19.6 ± 7.4 mm, and 18 (45%) patients had shoulder imbalance. At 2-year follow-up, absolute shoulder height averaged 5.2 ± 423 mm, and 4 (10%) patients had shoulder imbalance. Conclusion: NFASC offers promising curve correction and stabilization of curve progression in AIS cases with low risk of complications, preservation of spinal mobility, sagittal parameters and proves to be a favourable alternative to fusion modality. Shoulder balance improved in 66% of patients who had pre-operative shoulder imbalance. These results likely reflect that even though the proximal thoracic curve cannot be addressed due to technical difficulty, NFASC has a beneficial effect on shoulder balance.
757
A024: Predicting post-operative functional outcomes in spine surgery using machine learning algorithms and physical activity data
Daksh Chauhan 1 , Ali Hamade 1 , Hasan Ahmad 1 , Andrew Yang 1 , Michael Wang 2 , Gregory Basil 2 , Jang Yoon 1 , and Sai Mannam 3
1 Neurosurgery, University of Pennsylvania, Philadelphia, United States
2 Neurosurgery, University of Miami, Coral Gables, United States
3 Perelman School of Medicine at the University of Pennsylvania, Philadelphia, United States
Introduction: Smartphone activity data recorded through high-fidelity accelerometry has been shown to provide objective and accurate assessments of patient functional outcomes after spine surgery. Machine learning (ML) can be used to leverage these datasets and build data-driven predictive models and clinical decision-making tools. While logistic regression (LR) is an ML algorithm suited for linear and continuous data, more complex models including decision trees may be more effective for categorical variables in a larger dimensional space. This study compared the efficacy of LR, random forest (RF), and extreme gradient boosting (XGBoost) ML algorithms for predicting postoperative functional outcomes after spine surgery. Material and Methods: A total of 41 patients, 18 who received an LD procedure and 23 who received an LF procedure, were retrospectively included in the study. Activity data (steps-per-day) recorded in Apple Health (Apple Inc., Cupertino, CA) was collected. Our dataset encompassed over 69,000 datapoints over 2 years peri-operatively, and it was classified into 6 temporal epochs representing distinct functional states: (1) pre-operative baseline, (2) acute pre-operative decline, (3) pre-operative spontaneous recovery, (4) immediate post-operative recovery, (5) full recovery, and (6) post-recovery decline. Inputs into ML algorithms included patient age, BMI, duration of immediate postoperative recovery, and 1st/2ndderivatives of steps taken over time. The ML models were trained on 80% of the dataset and validated on the remaining 20%. Results: Following training, the XGBoost and LR models both achieved a predictive accuracy of 88.9%, while the RF model had an accuracy of 66.7%. Receiving operator characteristic curves showed an area under the curve, a measure of a classifier model's effectiveness, of 0.83 for both LR and XGBoost models and of 0.73 for the RF model. Conclusion: LR and XGBoost models predicted the direction of post-operative functional activity more accurately than an RF classifier model. The lower performance of the RF model may be due to the unbalanced nature of activity data, represented by the physiologically normal periods of increased and decreased activity (e.g., weekdays vs. weekends). Our study demonstrated that machine learning algorithms may be effective at predicting adverse clinical outcomes with a high accuracy of 88.9%. The information yielded by these models can be leveraged by surgeons and clinicians to provide highly personalized care to patients following surgery and improve clinical outcomes. While these models may be promising from the perspective of predictive analytics in spine surgery, they must be validated on larger datasets that include patients from backgrounds representative of the relevant populations.
1915
A025: Effect of enhanced recovery pathway (ERP) resulting in reduced length of stay (LOS) and opiod consumption after non fusion anterior scoliosis correction surgery for adolescent idiopathic scoliosis - a single centre experience
Dr Sajan Hegde 1 , Vigneshwara Badikkilaya 1 , Sharan Achar T 1 , Umesh Kanade P 1 , and Keyur Akbari 1
1 Orthopaedics, Apollo Hospitals Chennai India, Chennai, India
Introduction: There have been several reports on enhanced recovery pathway (ERP) in patients undergoing posterior spinal fusion (PSF) for Adolescent Idiopathic Scoliosis (AIS) resulting in early recovery and mobilization, decreased usage of opiods, early discharge and overall improved patient satisfaction. However, there is paucity of literature emphasizing its role in AIS patients undergoing non fusion anterior scoliosis correction surgery (NFASC). NFASC for AIS is a major surgical procedure and may be associated with significant postoperative pain and increased opioid consumption. ERP is a multidisciplinary approach aimed to expedite rapid recovery, reduced LOS, and minimizes morbidity associated with NFASC surgery. Material and Methods: Retrospective analysis of 35 AIS patients who underwent NFASC with Lenke 1 and Lenke 5 curves with a minimum of 1 year of follow up was done. Patient demographics, surgical details, postoperative analgesia, mobilization, length of stay (LOS), patient satisfaction survey score with respect to information and care, and 90 days complications were collected. Results: The cohort included 34 female and 1 male. The mean age at the time of surgery was 15.2 years (11-18 years). Mean Sanders score was 6.8 ± 0.6 and mean Risser score was 4.2 ± 0.5. There were 16 Lenke 1 and 19 Lenke 5 in the study. Mean pre operative major thoracic and thoracolumbar/lumbar Cobb’s angle were 52˚ ± 7.6˚ and 51˚ ± 4.5˚ respectively. All underwent tethering with upper intrumented vertebra being D5 and lower instrumented vertebra being L4. Average blood loss during surgery was 102 ± 6.4 ml and average surgical time was 168 ± 10.2 mins. The average time to commencing solid food was 6.5 ± 1.5 hrs. The average time to mobilization following surgery was 15.5 ± 4.3 hrs. The average duration to stopping of epidural was 42.5 ± 3.5 hrs. The average dose of opiod consumption intraoperatively was 600.5 ± 100.5 mcg of fentanyl i.v. and 12.5 ± 4.5 mg morphine i.v. Post operatively opiods were administered via an epidural catheter at a dose of 2 mg of morphine every 24 hours upto 2 days and an infusion of 2mcg/hr of fentanyl along with 0.12-0.15% ropivacaine. The average duration to transition to oral analgesia was 55.5 ± 8.5 hrs. 20 patients had urinary catheter and the average time to removal of catheter was 17.5 ± 1.4 hrs. 25 patients had chest tube and the average time to removal of chest tube was 25.5 ± 3.2 hrs. The average length of hospital stay was 3.1 ± 0.5 days. No patient had postoperative ileus or requirement of blood transfusion or any other complications. No correlation was found between LOS and initial cobb angle. The average patient satisfaction score for both information and care were 8.9 ± 0.5 and 9.1 ± 0.4 respectively. Conclusion: Our study shows promising results on application of ERP in AIS patients undergoing NFASC with reduced LOS and indirectly the cost, reduced post operative opiod use, early mobilization, enhance patient recovery, and overall improve patient satisfaction score.
305
A026: Closed cervical traction using a motorized robot: an AO Spine Young Investigators research grant funded study
Brandon Sherrod 1 , Haohan Zhang 2 , and Marcus Mazur 1
1 Neurosurgery
2 Mechanical Engineering, University of Utah, Salt Lake City, United States
Introduction: Closed cervical traction is commonly used to reduce subaxial cervical spine dislocation injuries and to distract the intervertebral space during cervical spine surgery. However, the standard weight-and-pulley cervical traction with cranial tongs relies on cumbersome and imprecise technology without any safeguard to prevent over-traction or weights being pulled/released inadvertently. To overcome the limitations of current methods, our goal was to demonstrate that robotic traction using novel safeguards can apply closed cervical traction more safely and efficiently than manual weight-and-pulley traction in extension spring and cadaveric models. Materials and Methods: A prototype robotic traction device was designed and manufactured with the following objectives: real-time tensile force measurement, ±1lb (5 N) force application accuracy, locking/non-backdriveable linear actuators with actuator position sensing, maximum force capability of 200 lbs (900 N), up to 20 degrees of flexion/extension manipulation, device weight <25 lbs (111 N), and compatibility with Gardner-Wells tongs or Mayfield head clamp. The device was tested using both an extension spring model and an intact fresh cadaver specimen to assess applied force and desired force over time as well as radiographic changes in the cervical spine as traction force increased. The cadaver was tested in manual traction and then robotic traction in 10 lbs (50 N) increments up to 80 lbs (400 N) to compare methods. Results: The prototype device met or exceeded all objectives. In extension spring testing, the device was able to reach prescribed forces of 111 N and 355 lbs accurately and maintain a desired weight. In cadaveric testing, radiographic outcomes were equivalent between the prototype and manual weight-and-pulley traction at 80 lbs (355 N) (disc space measurements within ±10% for all levels), and the device was able to reach the desired weight amount within ±1 lb (5 N) of accuracy at each weight interval. Conclusion: This preliminary work demonstrates that motorized robotic cervical traction can safely and effectively apply controlled traction forces that are more precise than weight-and-pulley traction. Novel applications of this device include closed cervical traction, open reduction of fracture-dislocations, and spinal realignment during deformity correction surgery.
468
A027: Educational potency of surgical simulation on high-fidelity spine model in spinal surgery
Haruki Ueda 1 , Satoshi Inami 1 , Hiroshi Moridaira 1 , Hidekazu Arai 1 , Satoshi Takada 1 , Tomoya Kanto 1 , and Hiroshi Taneichi 1
1 Orthopaedic Surgery, Dokkyo Medical University, Shimotsuga, Japan
Introduction: Along with the development of the spine surgery, the surgical procedures and techniques in this field have become more complicated. The surgeons and trainees are demanded to catch up with this advancement. However, both the safety of the patients and the efficiency of medical resources are two of the current important topics in healthcare, and it gets more difficult for the trainees to obtain abundant training time and experience in the daily operative theater. As one of the effective training methods, we would like to share our experience on surgical training with our high-fidelity spine model. Material and Methods: A simulated patient was created in electronic medical chart with diagnostic imaging studies from one of our real patients with cervical kyphotic deformity and corresponding fictional medical history. Four young spine surgeons, who have spinal instrumentation experience for relatively simple cases but not for complex deformities, were told to see this chart to make diagnosis and treatment plan in detail by their own, and to perform their surgery as planned after a month. 3D cervical spine model of MRT2 (Medtronic Japan) was created from the CT DICOM data of the patient. MRT2 is the newly developed high-fidelity radiograph-friendly bone model covered with sponge mimicking soft tissue. The procedures by those surgeons were performed one by one with slight assist by a senior surgeon in the real operative theater with the actual equipment including surgical tools and imaging devices, as they had ordered preoperatively. Their preparation and surgical time were recorded. The questionnaire which contained 5-point Likert scales and free comments were answered by the attendees. Results: The participants spent 308 minutes on average for pre-procedural learning, 75 minutes on average for making surgical plan, and 127 minutes on average for their procedures. Three planned anteroposterior surgery, and one planned anteroposteroanterior (3 stage) surgery. Three used image intensifiers for lateral mass screws, and one used CT Navigation for all-pedicle-screw construct. Preoperatively kyphotic C2-7 angle of -47 degrees was corrected to -9 degrees on average (-3.3 to -20 degrees). All the attendees said they could devote themselves to the procedure, and positively appreciated this simulation as excellent training method. Likert scales were more than 4 points on average in all items indicating both the model and this experience were accepted quite positively by the attendees. The positive points were including; that the radiographic outcome can be compared to the others, that the model provides sufficient quality of the hand feeling and imaging (X-ray, CT Navigation) appearance. Written feedback and comment added on their operative report were also favorably appreciated. All of them desired to participate again if the similar session would be held. Conclusion: The surgical simulation on the bone model can bring satisfying training experience for young surgeons if provided in the real operative environment with high-fidelity model with realistic medical background. This simulation seems valuable especially for the young surgeons to experience challenging cases for their hands.
OP04: Challenges in Cervical Spinal Trauma
1950
A028: Safety and efficacy of mesenchymal stem cells treatment in cervical spinal cord injury
Cene Kopač 1 and Marko Jug 1
1 Deparment of Traumatology, University Clinical Centre Ljubljana, Ljubljana, Slovenia
Background: Traumatic cervical spinal cord injury is a devastating event. Despite advances in research, current treatment options remain limited to early surgical treatment and minimizing secondary spinal cord injury. Spinal cord repair strategies are desperately needed. Mesenchymal stem cell (MSC) therapy is one of promising methods for cellular repair after spinal cord injury. Purpose of the study: The purpose of our study was to investigate safety, feasibility and efficacy of intravenous and intrathecal application of MSC after acute cervical spine injury. Neurologic recovery was evaluated. Methods: Eight patients with complete spinal cord injury from C3 – C7 and urgent spinal cord decompression and stabilisation were enrolled in the study. In the first month after injury, bone marrow (B) MSC were first harvested from patients iliac crests and cultivated, thereafter patients received an intravenous transplantation of 150 million allogeneic BMSC. One month after intravenous transplantation, patients received three intrathecal transplantations of 150 million autologous BMSC on a monthly basis. Before each transplantation one third of BMSC were radiolabeled and cell migration was evaluated with whole-body planar and hybrid (SPECT/CT) imaging of the spine at after transplantation. Intrathecal application was performed per lumbar puncture. According to ASIA, eurologic function was assessed before treatment and one month after each transplantation. Safety and feasibility of BMSC application and tracking was assessed. Results: Serious side effects after transplantation and cell labelling were not observed. However, most patients reported mild transient headaches and chills which resolved within one day with bed rest and acetaminophen. Neurologic improvement was observed in six out of the eight patients. All patients were classified as ASIA A prior BMSC application. In two patients we did not observe any neurological recovery, two patients improved to ASIA B, two patients improved to ASIA C and one improved to ASIA D after BMSC application. BMSC tracking with hybrid SPECT/CT imaging revealed that after intravenous administration BMSC were distributed in the reticuloendothelial system and in the lung parenchyma. BMSC retention at the site of spinal cord injury was unremarkable at any time frame. On the contrary, after intrathecal administration BMSC immediately migrated to the site of injury even several months after SCI. In one patient, cell migration was unremarkable, probably due to persistent severe spinal cord edema obliterating the spinal canal as shown on control MRI. Conclusion:Our study suggests that therapeutic application of allogenous and autologous mesenchymal stem cells is safe and feasible for treatment of spinal cord injury. No serious adverse events were associated with BMSC application. We found that BMSC may migrate to the site of SCI after transplantation even months after injury and that retention of cells after intrathecal administration at the injury site is superior to the retention after intravenous administration. Although neurologic recovery was observed it could not be attributed solely to BMSC transplantation. Due to small sample size and that this is unblinded study we can not exclude endogenous recovery or placebo effect.
235
A029: Comparison of posterior screw-rod-systems for the treatment of atlanto-axial instabilities: a biomechanical study
Titus Kuehlein 1 , Becker Christopher 1 , Kistler Manuel 1 , Greiner Axel 1 , Böcker Wolfgang 1 , and Adrian Cavalcanti Kußmaul 1
1 Department of Orthopaedics and Trauma Surgery, Musculoskeletal University Center Munich, LMU, University Hospital Munich, Munich, Germany
Introduction: The incidence of injuries of the atlanto axial joint is not only continuously increasing but aggravated due to the current demographic change. In the geriatric population, these injuries are mostly caused by an inadequate trauma and often require surgical treatment. Dorsal spondylodesis, such as the Harms or Magerl technique, have shown the highest fusion rates, however still display significant non-union rates and surgical complications, resulting in an ongoing debate about the optimum treatment for atlanto axial injuries. Recently, Harati developed a new procedure combining polyaxial transarticular screws with polyaxial atlas massae lateralis screws via a rod system with promising clinical results, yet biomechanical data is lacking. This study consequently evaluated and compared the biomechanical properties of the Harati and the Harms technique. Material and Methods: Two groups, each consisting of 7 cervical vertebral segments (C1/2), were formed. All specimens were provided with a dens axis type 2 fracture according to Alonzo. One group was then treated with the Harms and the other with the Harati technique. After embedding and mounting the specimens on a biomechanical testing machine, they were loaded via a lever arm. An initial weight of 50 N was placed on top for head simulation. To achieve a torque of 2 N/m, the lever was cyclically loaded with a force of ± 13,33 N. This resulted in cyclic extension/flexion in the sagittal plane and lateral flexion in the frontal plane. For rotation, ±2 N/m were applied directly to the upper vertebra via the testing machine. For statistical analysis, the dislocation (°) was measured and compared between the groups. Results: The Harati technique displayed a mean dislocation of 4.12 ± 2.36° in the sagittal plane, while the Harms technique displayed a dislocation of 8.48 ± 1.49° (p < 0.01). For lateral flexion, the dislocation was 0.57 ± 0.30° for the Harati and 1.19 ± 0.25° for the Harms group (p < 0.01). The mean dislocation for rotation was 1.09 ± 0.48° for the Harati and 2.10 ± 0.31° for the Harms group (p < 0.01). No implant failure occurred in any trial. Conclusion: This study confirmed the biomechanical stability of the spondylodesis described by Harati et al. and even displayed a significant increase in stability when compared to the technique by Harms et al. This can mainly be explained by the formation of a three-point-fixation based on the combination of the transarticular screws with massae lateralis screws. Based on the foundation of its biomechanical stability, this novel osteosynthesis as a combination technique furthermore facilitates the implantation of a transarticular screw by its unilateral use in case of an anomalous course of the vertebral artery. In detail, since an anomalous course of the vertebral artery, usually impeding the implementation of a transarticular screw, generally occurs unilaterally, this technique allows the implantation of an axis isthmus screw on the affected site while keeping the transarticular screw implantation contralaterally.
1628
A030: Operative versus nonoperative management of type II odontoid process fracture in octogenarians
Žiga Žigman 1 and Marko Jug 1
1 Department of Traumatology, University Medical Centre Ljubljana, Ljubljana, Slovenia
Introduction: Odontoid fractures are the most common fracture of the axis and the most common cervical fracture in patients over 80 years, with most classified as type II on the basis of the Anderson and D’Alonzo classification system. Despite their frequency, there is considerable controversy about the treatment. Material and Methods: A retrospective review of C2 fractures in patients 80 years of age or older who were admitted at University Medical Centre Ljubljana from 2011 to 2019 was performed. Demographics, mechanism of injury, date of injury, associated injuries, comorbidities, neurologic deficits, radiological measurements (fracture displacement and angulation), initial treatment modality (operative vs nonoperative), length of hospital stay and mortality were collected and analyzed. The subjects were followed with outcome, radiographic healing rates and complications. Results: We identified 44 patients with C2 fractures with 28 patients classified as Anderson–D’Alonzo Type-II odontoid fracture. Subjects were treated either surgically (n = 5) or initially nonsurgically (n = 23) as determined by the treatment preferred of the treating physicians and the patients. The mean age was 82.8 ± 2.4 years in the surgical and 85.7 ± 4.4 years in the nonsurgical group (p > 0.03); mean number of comorbidities was 3.2 ± 2.9 in the surgical and 3.6 ± 1.8 in the nonsurgical group (p > 0.38); mean fracture displacement was 5 mm ± 1 mm in the surgical group and 2.3 mm ± 1.8 mm in the nonsurgical (p > 0.0004). Acute in-hospital mortality rate was 20% ± 47% in the surgical group and 4% ± 21% in the nonsurgical group (p > 0.24). The percentage of patients experiencing complications was higher in the nonoperative group than the operative group (34% vs. 20% (p > 0.27)). In surgical group there was no nonunion in nonsurgical group there was 34% of nonunion (p > 0.001). One year survival rate in surgical group was 80% and in nonsurgical group 87% (p > 0.37). Five years survival rate was 60% in the surgical group and 39% in nonsurgical group (p > 0.23). Conclusion: Mean displacement was significant larger in group of patients that were operated. Operative treatment provides significant better fusion rate than external immobilization for acute odontoid Type ІІ fractures in the geriatric population. There was no significant difference between 1- and 5-year survival rates in patients treated operatively or nonoperatively. Type II odontoid fractures in the octogenarian population are associated with substantial morbidity and mortality, irrespective of management method.
922
A031: Anterior odontoid screw fixation following Anderson d’Alonzo type II and shallow type III fracture - Hounsfield unit prediction protocol of fusion rates
Petr Vachata 1 and Jan Lodin 1
1 Neurosurgery dpt., Spine Center Ústí nad Labem, Usti nad Labem 11, Czech Republic
Introduction: Main objective of this study was to determine whether Hounsfield units (HU) measured in the watershed area of the axis correlate with successful fusion in patients with type II and shallow type III C2 fractures undergoing anterior odontoid screw osteosynthesis (AOSF). Material and Methods: In the first retrospective part of study 45 patients with C2 fractures treated via AOSF were analyzed. Only bony fusion with bone trabeculations across the fracture line was considered a successful result. Preoperative HU values were measured in three zones- corpus, watershed and dens. Statistical analysis was performed to determine significant differences between HU of fused and unfused patients in all three zones of a complete and adjusted patient cohort. In the second prospective part of study, the new acquired protocol of indication limits of AOSF based on high bone quality (HU > 300) in the watershed area was applied on 17 consecutive patients with type II and shallow type III odontoid C2 fractures. Results: Statistically significant differences of HU values were retrospectively found between fused (corpus- 363.7, watershed - 327.9) and unfused (corpus - 279.5, watershed - 194.2) of the complete cohort and the adjusted cohort. Cut-off HU values in the watershed zone were calculated for the complete (250 and 300) and adjusted cohort (240 and 260), dividing patients into three groups of bone quality. Patients with high watershed bone quality (HU > 300) achieved successful fusion in 84.62%, patients with low bone quality (HU < 250) in 3.85% and patients with medium bone quality (HU 250-300) in 50%. In the prospective part of study, five patients with low bone quality were indicated for posterior C1-2 fusion with 100% fusion rate. Nine patients with high bone density were indicated for AOSF. In this group 7 of 8 patients with one year follow up fused. The fusion rate of AOSF changed from 36% to 88% (HU uncontrolled vs. HU controlled group). Conclusions: Preoperative measurement of HU can be used to predict the probability of successful fusion in patients undergoing AOSF for type II and shallow type III C2 fractures. AOSF is a highly effective treatment modality in patients with watershed HU >300, whereas alternatives should be considered in patients with lower bone quality.
809
A032: Awake cranial traction and isolated anterior cervical discectomy and fusion in the treatment of traumatic subaxial cervical facet joint dislocations (AO Type C F4 injuries): analysis of a cohort of 70 patients and predictors of surgical failure
Arnaldo Sousa 1 , Cláudia Rodrigues 1 Tiago Barbosa 1 , and Ricardo Rodrigues-Pinto 1
1 Spinal Unit/ Unidade Vertebro-Medular (UVM), Department of Orthopaedics, Centro Hospitalar e Universitário do Porto, Porto, Portugal
Introduction: Cervical facet dislocations are among the most common traumatic spinal injuries. The management of this type of lesions is still controversial. The objective of our work was to analyze the results of subaxial cervical facet dislocations submitted to an isolated anterior cervical discectomy and fusion (ACDF) after attempted closed reduction with cranial traction and to identify risk factors for treatment failure. Material and Methods: All patients operated in a tertiary trauma center during an 11-year period (2008-2018) for traumatic single-level cervical facet joint dislocation (AO C F4 injuries) were retrospectively reviewed. Age, use of cranial traction, dislocation characteristics, neurologic injury, surgical data and follow-up records were reviewed. A minimum of 18 months follow-up was required. Results: Seventy patients with a mean age of 56 years [18-90] (72% male) were identified. The C6-C7 level was the most frequently affected (36/70 cases). Spinal cord injury (SCI) was present in 34 % of the cases. Bilateral dislocations and rigid spines were risk factors for SCI. Cranial traction was performed in 59 cases with success in 52 cases (88%). There were 3 failures after anterior fusion, which required revision surgery with a 360 degrees fusion, all occurring at the C7-T1 level. Conclusion: Cranial traction of the cervical spine is an effective and fast way to achieve closed reduction of cervical facet dislocations. After successful reduction, ACDF, as a single procedure, offers an excellent surgical option. All cases of failure occurred at the C7-T1 level, suggesting that here, a 360-degree fusion may be needed.
793
A033: Mortality risk assessment in cervical spinal fractures in the elderly
Pedro Fernandes 1 , Carole Cruz 2 , Francisco Alves 1 , João Pedro 2 , Nuno Lança 1 , and Antonio Tirado 2
1 Orthopaedics, Centro Hopitalar Universitário Lisboa Norte, Lisboa, Portugal
2 Faculdade de Medicina de Lisboa, Lisboa, Portugal
Context: Because of their dismal prognosis, cervical spinal fractures in the aging population, represents a major challenge to both patients and health systems. Surgery is often performed although its added value may well be questioned in the future on a case base scenario. Objectives: Evaluate complications and mortality associated with cervical spinal fractures in the elderly and define risk factors related to bad prognosis. Methods: A retrospective study was designed to review patients over 65 years old admitted with a spinal fracture and surgically treated from 2007 to 2020. Fractures were divided between axial and subaxial, early surgery was set before 72 h. Complications, total length of stay and ICU stay and one-year mortality were registered. Data was collected in a Microsoft Excel database and SPSS IBM was used to evaluate relevant variables in the outcome and survival analysis. Multivariate logistic regression was performed to assess predictive factors on mortality. Results: 65 patients were included in the study. The mean age was 76.55 years. The most prevalent comorbidities were hypertension (69.2%) and diabetes (32.3%). 75.4% of patients had a subaxial spine fracture and 56,9% had neurological injury. Early surgery occurred in 22 patients (33.9%). 41 patients (63.1%) were operated through a posterior approach. There were 52 complications in 36 patients (55.38% of patients). One-year postoperative mortality was 35.19% (79% in the first post-operative trimester); neurological deficit (Odds = 7.0; p = 0.007), subaxial spine (Odds 6.538; p = 0.086); postoperative complications (p = 0.043; B = 2.051), age over 75 (Odds = 3.250; p = 0.059) were considered relevant and significant in a predictive model (R2 = 0.504). Conclusion: Early mortality in the very elderly patient with a cervical spinal fracture can be high. A predictive model including age, neurological injury, spine level, and number of postoperative complications is presented to help surgeons in the quite often difficult treatment decision.
Keywords: Cervical spine fracture; Elderly; Morbidity; Mortality; Treatment
748
A034: Differences in survivorship between elderly patients with odontoid and hip fractures: a retrospective cohort study
Zachary Crawford 1 , Jorge Figueras 2 , Nihar Shah 1 , Troy Holden 3 , Kristina Casos 3 , and Anthony Guanciale 1
1 Orthopaedic Surgery, College of Medicine, University of Cincinnati, Cincinnati, United States
2 Orthopaedic Surgery, Indiana University, Indianapolis, United States
3 College of Medicine, University of Cincinnati, Cincinnati, United States
Background Context: Both odontoid fractures and hip fractures often occur from a standing height and are thus categorized as fragility fractures. Studies have reported a one-year mortality rate of 37.5% for patients with odontoid fractures in comparison to a one-year mortality rate of 32% for those with hip fractures within the same age-matched cohort. However, an evaluation of comorbidities’ influence on the relative mortality of hip and odontoid fractures is lacking. Purpose: The purpose of this study is to compare the mortality and risk factors of isolated odontoid fractures to those with isolated hip fractures among the elderly population (> 65 years). Study Design/Setting: A single institution 14-year retrospective review of a level 1 trauma center with six fellowship trained spine surgeon. Patient Sample: This study included elderly patients (> 65 years at the time of injury) who sustained either an isolated hip fracture or isolated odontoid fracture. Outcome Measures: Primary outcomes were age at time of injury, comorbidities (Charlson Comorbidity Index (CCI)), and time from injury to mortality. Methods: Patients greater than 65 years with an isolated odontoid fracture or hip fracture from 2006 to 2020 were identified. Data collected include demographic information, time from injury to death, and living status. Death was assessed using a national social security database. Patients were matched on a 4:1 basis on both age and CCI. A Kaplan-Meier table was used to analyze survivorship from the date of fracture between age- and CCI score-matched patients with an odontoid fracture or hip fracture. A Cox regression analysis to assess the effect of age and CCI score on survival. Results: 1,234 patients with isolated hip fractures and 133 patients with isolated odontoid fractures were identified. After matching, a total of 532 hip fracture patients and 133 odontoid fracture patients were included in the analysis. A Kaplan-Meier estimate analysis revealed that survivorship for elderly patients with isolated odontoid fractures was longer compared to elderly patients with isolated hip fractures (p < 0.0001). Furthermore, patients with isolated hip fractures experienced an increased risk of death compared to patients with isolated odontoid fractures (hazard ratio [HR] = 1.47, p = 0.03), regardless of CCI score. Although risk of death was greater following hip fractures, CCI scores were independently associated with an increased risk of death in both patient groups (HR = 1.43, p = 0.004). Conclusion: Survivorship following isolated hip or odontoid fractures decreases substantially over time. Elderly patients who suffer isolated odontoid fractures have a lower risk of death compared to elderly patients who suffer isolated hip fractures. The presence of comorbidities significantly increases the risk of death in patients with isolated hip or odontoid fractures.
1822
A035: Cement-augmented direct anterior screw ostheosynthesis of the odontoid fracture in elderly patients
Petr Nesnídal 1,2 , Ondřej Teplý 1 , and Jiří Fiedler 1
1 Neurosurgical Department, Neurosurgical Department Hospital Ceske Budejovice a.s., České Budějovice, Czech Republic
2 Institute of Hygiene and Epidemiology, 1st Faculty of Medicine, Charles University, Prague, Czech Republic
Purpose of the Study: A retrospective study of prospectively collected data of a cohort of patients operated on with the same surgical technique over a 10-year period with a mean age of 81.7 years for odontoid fracture. Material And Methods: We performed cement-augmented direct anterior screw osteosynthesis in 37 patients between 2012 and 2021, a period of 10 years. We included 34 patients with a history of low-energy trauma and osteoporosis. The mean age was 81.7 years, with a 2:1 female to male predominance. The mean follow-up period was 2.7 years, with a minimum of 1 year. Results: The mean time of surgery after injury was 5.5 days (N = 34), median 2 days, and duration of surgery was 88 minutes. A total of 41 screws were inserted, 2 screws in 7 patients, mean length 41mm. Total of 33 patients (97%; N=34) odontoid type type II fracture, 1x type III (1%; N = 34), 29% within complex C1-C2 injury, no effect on fusion. 4x early death, 1x not observed. Radiologically on CT scans we found 20x fusion (69%; N = 29), 7x pseudoarthrosis stable (type I and II) (24.1%; N = 29), 2x loosening, failure (type III and IV) (7%; N = 29). We assessed as stable condition 27 times (93%; N = 29). On the flollow-ups with no major reported pain VAS 2 (6.9 to 2 postoperatively) (p < 0.05), 26 (90%; N = 29) of living patients return to original activities at 1 year postoperatively. Perioperatively, we experinced 16 times cement leakage (47%; N = 34), minimal leakage 10 times (29%; N = 34) (always asymptomatic, more severe type of leakage 6x (17%; N = 34), of which once (3%) symptomatic, leakage into the C1-C2 articular space (p < 0.05). Cement leakage in two screws 6/7 (86%) versus in one screw 10/27 (37%) (p < 0.05). 30-day mortality was 8.8%, 1-year mortality 14.7%, and overall mortality 26.5%. Late complications were once (3%; N = 34) reoperation for failure, instability and loosening at 6 months (Harms/Wright C1-C2), once (3%; N = 34) instability without intervention, good clinical condition of the patient. Late complications were 1x (3%; N = 34) reoperation for failure, instability and loosening at 6 months (Harms/Wright C1-C2), 1x (3%; N = 34) instability without intervention, good clinical condition of the patient. Discussion: Compared to posterior stabilization, it is less risky for the patient - time and position (88 min), blood loss, preservation of C1-C2 segment mobility, relatively less risk - injury to blood vessels, nerve structures (0%), similar stiffness of both stabilizations. Compared to non-augmented direct osteosynthesis, there is a significant increase in stiffness, less risk of failure. Reduction in the occurrence of a pseudoartrosis from 50% to 75%. In our cohort 69%, risk of cement leakage, up to 50%. Mostly asymptomatic. Conclusions: In our institution, now the method of first choice for type II dentoalveolar injuries in geriatric patients, which has a reasonable operative risk, preservation of rotations of the upper cervical spine, but a lower percentage of fusion (69%). On the other hand, less risk, preservation of stability (in our cohort 93%) and quality of life of these patients (satisfaction 90%).
1076
A036: Use of pedicular screws in the subaxial cervical spine: comparative analysis between tomographic positioning and clinical repercussion of 102 screws
Igor Ebert Cechin 1 , Gabriel Alves 1 , Alderico Girão Campos de Barros 1 , and Luis Eduardo Carelli Texeira da Silva 1
1 Coluna, Instituto Nacional de Traumatologia e Ortopedia Jammil Haddad (INTO), Rio de Janeiro, Brazil
Introduction: To compare clinical and radiological results and to assess the safety of applying pedicle screws in the subaxial cervical spine, a technique that is not widely used among spine surgeons. Material and Methods: We evaluated the results regarding the application of 102 subaxial pedicle screws in the treatment of cervical pathologies in 19 patients, 14 males and 5 females, aged between 16 - 76 years (mean 57.7) in the period between 2005 and 2021. The selected patients had favorable pedicular morphology demonstrated by preoperative computed tomography. The surgical technique used presented hybrid concepts between Abumi's original technique, the Funnel Technique and the Pedicle Axis View, without the use of three-dimensional navigation. Clinical evaluation was performed in the postoperative period, looking for signs and symptoms related to spinal cord, cervical nerve roots and vertebral artery injuries. The classification of screw positioning was performed independently by three spine surgeons, using an axial tomographic image along the axis of the screws, classifying according to the classification proposed by Neo et al. Results: Between 2005 and 2021, 102 pedicle screws were inserted from C3 to C6 in 19 patients undergoing surgical treatment of cervical pathologies. The initial diagnosis was spondylotic myelopathy in 9 patients, cervical trauma in 7, tumor pathologies in 2 patients and 1 central cord syndrome. It was evidenced that 81.4% of the screws did not show any deviation (Neo grade 0) and only 1.9% had Neo grade 3 deviation. The level most subject to critical deviations (grades 2 and 3) was C3, with C6 being the level with the best accuracy – 96.7% of the screws did not present any cortical perforation in this segment. Incorrect positioning was more often lateral, in 68.4% of cases with deviation. There were no screws classified as Grade 3 for medial deviation. As a complication, only one patient had a neurological radicular compromise consistent with inadequate positioning - medial grade 2, evolving positively without the need of revision. There was no need to return to the operating room for repositioning in any patient. One patient died on the seventh postoperative day due to an ischemic stroke in the territory of the anterior circulation, without anatomical correspondence with the possible complications of the procedure. There were no vascular complications related to the vertebral artery. Conclusion: Despite being technically demanding, the use of pedicle screws in the subaxial cervical spine proved to be safe, with a low rate of malpositioning in the postoperative tomographic analysis and relevant clinical complications.
OP05: Spinal Trauma
827
A037: AO Spine CROST (Clinician Reported Outcome Spine Trauma): reliability analysis and validation
Said Sadiqi 1 , Sander Muijs 1 , and Cumhur Oner 1
1 Department of Orthopaedics, University Medical Center Utrecht, The Netherlands
Introduction: Next to a patient reported outcome measure, there is also need for a simple, reliable and quick to administer tool that is completed by the treating surgeons and reflects their perspectives adequately. Consisting of the most relevant clinical and radiological assessment parameters, the AO Spine CROST (Clinician Reported Outcome Spine Trauma) was developed by the AO Spine Knowledge Forum Trauma. The development of the tool and initial reliability results are presented in the current study. Material and Methods: The development of the AO Spine CROST initiated by the identification of the most relevant parameters from the clinicians’ perspective for outcomes measurement of spine trauma patients. An iterative approach of multiple cycles of development, review and revision including an expert clinician panel was conducted. This was followed by a reliability study among an expert panel who were provided with 20 spine trauma cases, administered twice with a four-week interval. Descriptive statistics were used to analyze the developmental process. In the reliability analysis Kappa statistics was used to analyze the reliability per parameter. The inter-rater agreement was analyzed using Intraclass Correlation Coefficient (ICC). Finally, Cronbach’s alpha was used for the assessment of the internal consistency. Results: After completing the iterative approach in the initial phase the AO Spine CROST was developed, consisting of 10 parameters. Two of those 10 parameters are only applicable to surgically treated patients (‘Wound healing’ and ‘Implants’), the remaining 8 parameters are applicable to both surgically and conservatively treated patients. The scoring system includes a dichotomous ‘yes or no’-response which expresses expected problems for both the short-term and long-term. In the reliability study, 16 (84.2%) participated in the first round and 14 (73.7%) in the second. Fair to good intra-rater reliability was found for both time-points (κ = 0.40-0.80 and κ = 0.31-0.67). Results of inter-rater reliability per item were lower (κ = 0.18-0.60 and κ = 0.16-0.46). The inter-rater agreement for the total scores showed better results (ICC = 0.52-0.60). The internal consistency seemed acceptable (α = 0.76-0.82). Conclusion: Following a comprehensive approach led to the development of the AO Spine CROST. This tool is completed by the treating surgeons and enables them to evaluate and predict outcomes of spine trauma patients. Fair to moderate results and acceptable internal consistency were found in an initial reliability study. Currently, further studies are being performed to analyze the reliability and clinical evaluation of the tool in a prospective setting. Satisfactory results are expected from these studies which would contribute to increased value of the tool for the daily clinical practice and research, leading to improved care and outcomes for spine trauma patients.
1031
A038: Returning to work and narcotic use after traumatic spine fractures: current status in Saudi Arabia
Abdulrahman AlHabeeb 1 and Faisal Konbaz 2
1 College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyad, Arabia Saudita
2 King Faisal Specialist Hospital and Research Centre, Riyad, Arabia Saudita
Introduction: The consequences of spine fractures can be deleterious in many ways including the risk of spinal cord injuries, operative complications, and chronic pain. Not only do spine fractures affect patients from a health point of view, but it also affects patients’ financial status in many ways, one of which is returning to work. Hence, in this study, we aimed to assess the return to work and narcotic use in patients who had spine fractures. Material and Methods: A retrospective cohort study done at King Abdulaziz Medical City in Riyadh, Saudi Arabia. All patients with traumatic spine fractures who required surgical intervention from 2016 to 2021 were included. Variables regarding patients and injury characteristics, management, including post discharge narcotics use, and work status after the injury were collected that were subsequently analyzed using SPSS version 22. Results: Out of 750 cases, a total of 173 fulfilled our inclusion criteria. Male patients account for 82.7%, and motor vehicle accidents were the most common mechanism of injury accounting for 80.2%. The majority of the fractures were chance fractures (32.2%), and neurologically intact patients accounted for 78.6%. Out of 173 patients, 38.15% of the patients have returned to their jobs after their injury, and 24.24% of them had to change their work style, for example, desk job instead of field job, or had to change their university specialty due to the injury. On the other hand, patients who haven’t returned to work accounted for 27.1%. Majority of the patients didn’t use narcotics more than 1 week after discharge (93.1%). A significant difference was found between older age and not getting back to work (p = 0.005). Moreover, higher surgical blood loss, operation time, and hospital length of stay were significantly associated with not returning to work (p = 0.001, p = 0.003, p = 0.012, respectively). In the multivariant regression analysis, we found that every increase of 100 ml of blood loss during the operation decreases the chance of getting back to work by 25% (p = 0.04). Furthermore, every increase of one hour in operation time decreases the chance of getting back to work by 31% (p = 0.03). Lastly, those aged <20 have a 20 times higher chance to go back to work compared to those aged from 50-60 (p = 0.001). Conclusion: Returning to work is an important aspect that needs to be taken into consideration by healthcare providers. We found that age, longer surgery time, higher blood loss, and longer hospital stay are significantly impacting patients’ returning to work.
1347
A039: Spinal gunshot injuries: a Latin American multicenter retrospective study
Guillermo Ricciardi 1 , Oscar Martinez-Gutierrez 2 , Jorge Cabrera 3 , Javier Matta 4 , Victor Davila 5 , Jose Maria Jimenez 6 , Hugo Vilchis 7 , Victor Tejerina 8 , Jeasson Perez 9 , Juan P. Cabrera Cousiño 10 , and Ratko Yurac 11
1 Spine Team - Orthopaedics and Traumatology, Centro Médico Fitz Roy, Ciudad de Buenos Aires, Argentina
2 Hospital Universitario Dr. José E. González, Mexico City, Mexico
3 Hospital de Traumatología "Dr. Victorio de la Fuente Narvaez" IMSS, Mexico City, Mexico
4 Hospital Militar Central, Bogota, Colombia
5 Hospital Universitario Dr. Manuel Nuñez Tovar, Monagas, Venezuela
6 Instituto Mexicano del Seguro Social, Coahuila, Mexico
7 Unidad Médica de Alta Especialidad, Hospital de Traumatología y Ortopedia Lomas Verdes IMSS, Naucalpan de Juarez, Mexico
8 Hospital Traumatología y Ortopedia Magdalena de las Salinas, Mexico City, Mexico
9 Clínica de columna "Dr. Manuel Dufoo Olvera", Mexico City, Mexico
10 Hospital Clínico Regional de Concepción, Chile
11 Clínica Alemana de Santiago, University del Desarrollo, Santiago, Chile
Introduction: every day in Latin America new homicide victims are added to its statistical record. The American continent accounts for 37% of all homicides worldwide and most of them occurred across Latin America. Affecting, predominately young civilian population, firearms are involved in three quarters of homicides. There was registered a rate of 16.4 young people killed by others with firearms per 100,000 youth in Latin America. Spinal gunshot injuries represent 13-17% of all spinal injuries, with a great economic and social impact. These are the third most common cause of spinal injury in civilian populations, after fall from height and motor vehicle accident. Our objective is to describe demographic data, assessment and treatment of a multicenter retrospective case-series of patients with gunshot to the spine across Latin America. Material and Methods: retrospective multicenter case series study of patients treated for gunshot to the spine among 12 institutions from Latin America during the period from January 2015 to January 2022. Demographic and clinical data was registered considering injury time, initial assessment, vertebral gunshot injury and treatment. Results: We have included 423 patients with gunshot injuries to the spine treated at institutions from Mexico (80%), Argentina, Brazil, Colombia and Venezuela. Spine injuries mainly affected the thoracic and lumbar spine. Neurological injury was registered in 320 (76%) patients and spinal cord injuries in most of them (n = 269; 63%). Treatment was frequently conservative. Otherwise, 90 (21%) patients were surgically treated, principally by posterior conventional approach (79; 87%). Injury features associated with surgical cases were canal compromise (p = 0.000), dirty wounds (p = 0.000), remains of splinters in the canal (p = 0.000) and injuries that affects the posterior arch (p = 0.021), facets (p = 0.003) or disc (p = 0.008). Conclusion: This study described a large Latin American multicenter case series of gunshot to the spine. Including predominantly male, civilian, lower/middle social class population that suffered assaults with low-energy firearm.
831
A040: Applicability of the AO Spine Patient Reported Outcome Spine Trauma (PROST) in motor-complete spinal cord injury patients: a cognitive interview study
Aline J Hakbijl 1 , Tijn van Diermen 2 , Stephanie Dompeling 3 , Cumhur Oner 3 , Marcel Post 1 , and Said Sadiqi 3
1 Department of Spinal Cord Injury Rehabilitation, De Hoogstraat Rehabilitation, Utrecht, The Netherlands
2 Department of Orthopaedics, Sint Maartenskliniek, Ubbergen, The Netherlands
3 Department of Orthopaedics, University Medical Center Utrecht, The Netherlands
Introduction: A number of outcome measures are available to evaluate the function and health of people with spinal cord injury (SCI). However, none cover the whole spectrum of functional status, secondary problems, mood and social consequences with a single scale. The AO Spine Knowledge Forum Trauma initiated a project to develop such instrument for the spine trauma population: the Patient Reported Outcome Spine Trauma (AO Spine PROST). Previous studies have shown that the AO Spine PROST is reliable and valid among people with spine trauma, with no, transient or mild neurology. Data on its applicability for use in people sustaining AISA Impairment Scale (AIS) A and B and non-traumatic cause of injury are unavailable to date. The aim of this study was to examine the applicability of the AO Spine PROST in people with motor-complete traumatic or non-traumatic SCI. Material and Methods: Semi-structured cognitive interviews were conducted with 29 adults with a motor-complete SCI (AIS A or B). Participants were asked to complete the AO Spine PROST and four additional evaluation questions rated on a 1-5 point Likert scale (5 most positive), while verbalizing their thoughts about their answers. Interviews were audio recorded and transcribed. Codes were identified and linked to a coding schema. Qualitative data were used to interpret the quantitative results. Results: Almost three-quarters of the participants (71.4%) had a traumatic SCI. Positive ratings of the measure were obtained regards comprehensibility (mean 4.0), non-offensiveness (4.6), relevance (4.2) and completeness (3.6). A question about the emotional impact of SCI was indicated to be missing. A recurring topic found during the cognitive interviews included the importance to weight an assistive device in the score. The use of multiple examples per item raised uncertainty, mostly solved by patients through averaging their score. Some individuals indicated that the possibility to express even better function compared to pre-trauma would be valuable. Conclusion: Overall, the AO Spine PROST appeared to be applicable in adults with a motor-complete traumatic or non-traumatic SCI. Recommendations were made for improvement in instructions, terminology and used examples in the items. Only minor changes were proposed to make the tool applicable to spinal cord injured patients as well. This study forms an important milestone for the further development of the AO Spine PROST as well as its applicability to the entire spectrum of spine trauma and SCI patients, leading to improved care and research in this specific patient population.
755
A041: Neurological recovery after early versus delayed surgical decompression for acute, traumatic spinal cord injury: a prospective, observational, European multicentre (SCI-POEM) study
Allard Hosman 1 , Giuseppe Barbagallo 2 , Eugen Cezar Popescu 3 , Henk van de Meent 4 , Cumhur Oner 5 , Federico de Iure 6 , Jacopo Bonavita 7 , Kreinest Michael 8 , Richard Lindtner 9 , Nasir Quraishi 10 , Pradeep Thumbika 11 , Vide Bilic 12 , Jeremy Reynolds 13 , Maurizio Belci 14 , Alp Börcek 15 , Seamus Morris 16 , Christoph Hoffmann 17 , Francesco Signorelli 18 , Konstantin Uzuno 19 , and Joost van Middendorp 1
1 Orthopedic Surgery, Radboud University Medical Center, Nijmegen, The Netherlands
2 U.O. di Clinica Neurochirurgia, Universitaria Policlinico, Azienda Ospedaliero, Catania, Italy
3 “Prof. N. Oblu” Emergency Hospital, Iasi, Romania
4 Rehabilitation, Radboud University Medical Center, Nijmegen, The Netherlands
5 Orthopedic Surgery, Universitair Medisch Centrum Utrecht, Utrecht, The Netherlands
6 SD Chirurgia Vertebral, Ospedale Maggiore, Bologna, Italy
7 Spinal Unit, Montecatone Rehab Institute, Imola, Italy
8 BG Klinik Ludwigshafen, Ludwigshafen, Germany
9 Department of Orthopaedics and Traumatology, Medical University of Innsbruck, Innsbruck, Austria
10 Nottingham University Hospital NHS Trust, Nottingham, United Kingdom
11 Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom
12 Department of Traumatology, University Hospital Centre Sestre Milosrdnic, Zagreb, Croatia
13 Oxford University Hospitals NHS Trust, Oxford, United Kingdom
14 National Spinal Injury Centre Stoke Mandeville Hospital, Aylesbury, United Kingdom
15 Gazi Üniversitesi Tıp, Ankara, Turkey
16 Mater Misericordiae University Hospital, Dublin, Ireland
17 Center for Spinal Surgery and Neurotraumatology,Berufsgenossenschaftliche Unfallklinik Frankfuram Main, Frankfurt, Germany
18 Hôpital Neurologique et Neurochirurgical Pierre Wertheim, Lyon, France
19 University Multiprofile Hospital for Active Treatment and Emergency Medicien “N.I.Pirogov”, Sofia, Bulgaria
Aims: To determine whether early surgical treatment results in better neurological recovery 12 months after injury than late surgical treatment in patients with acute traumatic spinal cord injury (tSCI). Methods: Patients with tSCI requiring surgical spinal decompression presenting to 17 centres in Europe were recruited. Depending on the timing of decompression, patients were divided into early (≤ 12 hours after injury) and late (> 12 hours and < 14 days after injury) groups. The American Spinal Injury Association neurological (ASIA) examination was performed at baseline (after injury but before decompression) and 12 months. The primary endpoint was the change in lower extremity motor score (LEMS) from baseline to 12 months. Results: The final analyses included 159 patients in the early and 135 in the late group. Patients in the early group had significantly more severe neurological impairment before surgical treatment. For unadjusted complete-case analysis, mean (95% confidence interval [CI]) change in LEMS was 15·6 (12·1; 19·0) in the early and 11·3 (8·3; 14·3) in the late group, with a mean (95% CI) between-group difference of 4·3 (-0·3; 8·8). Using multiply imputed data adjusting for baseline LEMS, baseline ASIA Impairment Scale (AIS), and propensity score, the mean (95% CI) between-group difference in the change in LEMS decreased to 2·2 (-1·5; 5·9). Conclusion: Compared to late surgical decompression, early surgical decompression following acute tSCI did not result in statistically significant nor clinically meaningful neurological improvements 12 months after injury. These results, however, do not impact the well-established need for acute medical treatment following tSCI. This is the first study to highlight that a combination of baseline imbalances, ceiling effects, and attrition rates may yield an overestimate of the effect of early surgical decompression in unadjusted analyses, which underpins the importance of adjusted statistical analyses in acute tSCI research.
597
A042: Increased incidence of traumatic spine injury in elderly patients in the Netherlands
Chiara Bruggink 1 , Marc van de Ree 1 , Jan van Ditshuizen 2 , Max Reijman 1 , and Joost Rutges 1
1 Orthopedic Surgery and Sports Medicine
2 Trauma Surgery, Erasmus MC, Rotterdam, The Netherlands
Introduction: The global elderly population is growing rapidly and will increase to an estimated 30% in Europe by 2050. In addition, elderly patients are increasingly active despite their comorbidities. Consequently, more elderly patients with traumatic spine injury are seen in emergency departments worldwide. In the Netherlands, where currently 18.5% of the population is >65 years, the incidence of traumatic spine injury among elderly patients has significantly increased between 1994-2010. However, it is currently unknown how the incidence of traumatic spine injury has evolved during the past decade. Moreover, little is known regarding the differences of sociodemographic and clinical characteristics between young and older patients. Therefore, the aim of this study was to determine the incidence and characteristics of traumatic spine injury among patients <65 and >65 years in three time periods, 2009/2010, 2014/2015 and 2019/2020. Methods and materials: All patients with traumatic spine injury in the Netherlands from three periods 2009-2010, 2014-2015 and 2019-2020 were identified from the Dutch National Trauma Registry (DNTR). Patient and injury characteristics were obtained for the subgroup of patients that were treated in our level 1 trauma center. Details regarding the treatment, complications and 1 year mortality were retrieved from the electrotonic patient files. Results: On a national level 25.737 patients with traumatic spine injury were identified. When compared to 2009/2010 the percentage of elderly significantly increased from 37% (n = 2482) to 43% (n = 4077) in 2014/2015 (p < 0.0001), and 47% in 2019/2020 (n = 4422, p < 0.0001). In our level 1 trauma center 1.054 patients with traumatic spine injury were seen. When compared to 2009/2010 the percentage of elderly increased from 26.1% (n = 67) to 30.9% (n = 116) in 2014/2015 (p = 0.185 NS) and 33.9% (n = 143) in 2019/2020 (p = 0.033).The most common trauma mechanism in patients > 65 years was a low energy fall (64.1%, n = 209), the cervical spine was most frequently injured (50.6%, n = 165), and the AO Spine type A fracture pattern was most prevalent (64.7%, n = 211). Patients > 65 years had a higher 1-year mortality rate compared to patients < 65 years 22.7% vs 9.2% respectively, OR [95%CI] 2.9 [2.0 - 4.2]). Conclusion: The incidence of traumatic spine injury in elderly patients in the Netherlands has significantly increased the past decade. In 2019/2020 almost half of all patients with traumatic spine injury was > 65 years. Based on the predicted growth of the elderly population in Europe, the majority of patients with traumatic spine injury will be > 65 years in the upcoming 10-20 years. The increased incidence and high mortality rate of spinal injury in elderly emphasizes the need of specifically developed treatment protocols for this patient category.
1355
A043: Outcomes in spine trauma with a dedicated spine surgeon versus general neurosurgeon on-call: a retrospective review
Edward Floyd 1 , Amanda Mathies 2 , Rebecca Baird 3 , Tyler Sang 4 , Alycia Abler 3 , Adam Jackson 5 , and Mentor Ahmeti 3
1 Sanford Orthopedics & Sports Medicine University of North Dakota School of Medicine and Health Sciences, Orthopedic Surgery, Fargo, United States
2 Medical School
3 General Surgery, University of North Dakota School of Medicine and Health Sciences, Grand Forks, United States
4 Sanford Medical Center Fargo, Research, Fargo, United States
5 Neurosurgery, Sanford Brain and Spine Center Fargo, Fargo, United States
Introduction: The timely and appropriate management of traumatic spine injuries is a cornerstone of neurological and orthopedic trauma surgery. Nearly half of polytrauma patients may present with acute spine pathology, and appropriate intervention within 24 hours, with early decompression when indicated, is critical to ameliorating life-altering sequelae. The availability of spine surgeons varies in hospitals in the U.S. and globally and the medical safety net may include fellowship-trained spine surgeons of orthopedic or neurosurgical background, or general neurosurgeons without fellowship training. This report investigates whether management and outcomes of acute spinal injuries may differ based on the training of the on-call spine team. Materials and Methods: This study was a retrospective cohort reviewing patients over 18 years old with acute cervical or thoracolumbar trauma presenting to a level-I trauma center in the Upper Midwestern United States. Patients with previous spine trauma or hardware, those with uncomplicated spinous or transverse process fractures alone, and those who had no documented evaluation from a neurosurgeon or spinal surgeon, or who left against medical advice were excluded. Age, sex, race, BMI, and comorbidities were collected. Outcomes examined included 30-day mortality and readmission, complications (constipation, ileus, deep vein thrombosis/pulmonary embolism, infection, skin breakdown), length of time from presentation to intervention/surgery, consult to charted final plan, and length of surgery. Demographics, comorbidities, and outcomes were compared between patients seen by both provider types. Statistical comparisons were conducted using R version 4.2.1 to perform Kruskal-Wallis rank sum test for continuous variables and Chi-squared test for categorical variables, with a level of significance at α = 0.05. Results: After exclusion, 447 patient charts were examined. Of the outcomes examined, time to operating room and time to charted final plan were significantly longer (p < 0.05) for patients seen by a general neurosurgeon than by a fellowship-trained spine surgeon. Mean time to surgery was 58.39 versus 48.88 hours, and time to charted plan was 34.83 versus 21.36 hours for general versus spine fellowship trained, respectively. The number of complications was not sufficient to detect a difference by provider type. Length of hospital and intensive care stay were not significantly different by type of provider. Interestingly, this study also detected a significant increase in 30-day mortality by age (> 65), coexisting diabetes, congestive heart failure (CHF), and hypertension. Conclusions: This study examined the effect of type of provider, whether general neurosurgeon or fellowship-trained spine surgeon, on time to intervention, length of stay, duration of intensive care, and 30-day mortality in spine trauma patients in a major rural hospital system in the U.S. Of these, the only significant difference was a roughly 10-hour longer time to intervention with general neurosurgeons. These results suggest that equivalent patient outcomes may be obtained by general neurosurgeons as opposed to spine fellowship-trained providers in caring for acute traumatic injuries to the spine, a finding which may be of interest particularly in rural or resource-limited healthcare settings. We also found worsened 30-day mortality in patients with a number of preexisting conditions, reinforcing the benefits of medical co-management for these patients.
1004
A044: Systematic review of clinical prediction models of outcomes in spinal cord injury
Ali Moghaddamjou 1 , Zaid Salaheen 2 , Ayesha Quddusi 2 , Saman Arfaie 3 , Alex Bak 2 , and Michael Fehlings 1
1 Neurosurgery, University of Toronto, Canada
2 University of Toronto, Canada
3 McGill University, Montréal, Canada
Introduction: Traumatic Spinal Cord Injury (tSCI) imposes a significant clinical and economical burden on patients and the health care system. Despite its importance, clinical prediction of outcomes based on factors present in the initial presentation is difficult. Having accurate prediction models of outcomes is not only important for the expectation setting of patients and their families but can help guide management and the design of clinical trials on emerging therapies. The goal of this project was to perform a systematic review of the literature on clinical prediction models of tSCI based on factors known at the time of initial presentation. With this review, we aim to identify potential clinical predictors and assess the strength of current clinical prediction models. Material and Methods: We included studies that had prediction models of tSCI in patients above the age of 14. We excluded those studies that did not document any factors present within 72 hours of the initial injury. We also excluded those studies that had less than 40 patients and had less than 3 months follow-up post-injury. We excluded studies that only included the prediction of complications. Our review plan was registered a-prior on PROSPERO (CRD42021231278). The MEDLINE and EMBASE clinical databases were searched for studies that included terms associated with tSCI and outcome measures replicating previous Cochrane review search strategies. A piloted search was conducted, and 500 abstracts were reviewed to ensure an adequate search strategy. Covidence software was used for screening and de-duplication and EndNote was used for reference management. Abstracts were screened by a minimum of 2 reviewers and disagreements were resolved by the primary author. Data extraction was carried out using the validated PROBAST tool and the CHARMS checklist for risk of bias assessment. The AOSpine Knowledge Forum, AANS website, AAO website, and the European Spine Association website were also searched for grey literature review. Results: Overall identified 10,100 articles for review. After abstract review 24 articles were selected for full-text review. The results of the PROBAST indicated that the majority of the studies had a low risk of bias when it came to the selection of the model participants, predictors, and outcomes. Furthermore, all the studies were graded to be applicable. Most of the studies (80%) were graded to have a high risk of bias when it came to the analytical plan. We were also able the isolate 37 predictors of outcomes. Of these predictors, 30% were from the patient exam and only 10.8% were related to the treatment. The main outcome modeled in these studies was the AIS grade conversion (42.31%). Almost all the studies used a multivariate logistic regression model. Conclusion: From the results of this systematic review, we can conclude that there are many potential predictors of tSCI that need to be explored further. Some of these predictors include age, surgical decompression, and MRI findings such as intramedullary lesion length and presence of hemorrhage). Furthermore, there is a need for more robust and diverse modeling techniques and outcome measures.
1828
A045: Validity of the short musculoskeletal function assessment questionnaire in spinal fractures
Simon Blixt 1,2 and Paul Gerdhem 1,3,4
1 Department of Clinical Science Intervention and Technology, Division Orthopedics and Biotechnology, Karolinska Institutet, Stockholm, Sweden
2 Department of Reconstructive Orthopaedics, Karolinska University Hospital, Stockholm, Sweden
3 Department of Surgical Sciences, Uppsala University, Uppsala, Sweden
4 Department of Orthopaedics and Handsurgery, Uppsala University Hospital, Uppsala, Sweden
Introduction: Patient-reported outcome measures (PROMs) play an important role in assessing the impact of spinal fractures and their treatment. To date, there is no widely accepted PROM specifically designed for spinal fractures. The Oswestry Disability Index (ODI) is often used for this purpose, as it is designed to measure disability related to lower back pain. One of the more frequently used PROMs for fractures in general in Sweden, is the Short Musculoskeletal Function Assessment (SMFA). The SMFA, not being specific for a particular body part, has the advantage of being able to compare outcomes between different types of musculoskeletal injuries. SMFA is divided in 2 parts, the 1st part assessing the level of dysfunction the patient is experiencing and the 2nd part assessing the how much the patient is bothered by their disability. The purpose of this study was to compare the SMFA with the commonly used ODI in patients with a spinal fracture. Materials and Methods: This was a prospective observational cohort of patients admitted to the Karolinska University Hospital in Huddinge between January 1st 2016 and October 31st 2017 with a spinal fracture (C1-L5). Patients were asked to fill out ODI, SMFA and EQ-5D-3L questionnaires approximately 1 year after their injury. All questionnaires were collected by paper. Spearman’s rank correlation coefficient (rho) was used to assess convergent validity for each PROM. Bland-Altman plots were used to assess agreement between PROMs. Results: 82 patients completed all questionnaires in their entirety. The SMFA dysfunction index and bother index was highly correlated with ODI (rho = 0.89, rho = 0.86 respectively), as well as with EQ-5D-3L (rho = 0.89, rho = 0.80 respectively). The correlation for separate categories of the SMFA dysfunction index (daily activities, emotional status, arm and hand function, mobility) with ODI and EQ-5D-3L was good to excellent (rho range 0.71-0.87 and 0.72-0.84 respectively). The agreement on Bland-Altman plots were good, with a mean difference of -2.6 between ODI and SMFA dysfunction index with 93% of the scores within 95% limits of agreement (18.0 and -23.1) and -3.6 between ODI and SMFA bother index with 96% within 95% limits of agreement (18.6 and -25.7). A modified index of SMFA was generated by selecting the 10 items of SMFA with the highest correlations with the 10 items of ODI. This modified SMFA index correlated highly with ODI (r = 0.92). Conclusion: The SMFA dysfunction index and bother index, or selected SMFA items, may be used to assess outcome in patients with spinal fractures as an alternative to ODI.
OP06: Biological Therapies
141
A046: Standarized method for lumbar fusion techniques using p-15/ABM in addition to autologous BMA, measured by clinical and radiological outcomes
Alberto Perez 1 and Diana Chavez 1
1 Neurosurgery, Hospitales Angeles, Mexico, Mexico
Introduction: Multiple lumbar fusion techniques and materials available to treat low-back pain. Techniques include: Transforaminal (TLIF), Lateral (LLIF, XLIOF, OLIF) and Anterior (ALIF) interbody fusion. Fusion rates are enhanced through bone graft materials, as i-FACTOR/P-15, bound to anorganic bone mineral (ABM); plus the use of autologous bone marrow aspirate (BMA) that increases the benefits of the bone graft, by the osteogenic, osteo-inductive and osteoconductive stimuli. Main objective is to standardize lumbar fusion process on any technique to achieve more efficient and predictable fusion, evaluating results with radiological and clinical scales. Other objectives are to find the amount of graft needed to achieve spinal fusion and determine if its necessary in all cases to perform bone marrow aspirate (BMA). Material and Methods: Prospective study, data during May 2021 to December 2022. Inclusion Criteria includes every ALIF, TLIF and LLIF procedures with complete follow up at 6 weeks with radiograph and complete follow up and 3, 6 and 12 months with Computed Tomography. Exclusion Criteria are revision procedures, less than 1 year of follow-up and lack of the specified CT imaging. Patients will be divided in Group A - Using I-Factor bone graft and subdivided into three groups: TLIF 2.5 cc in the cage and 2.5 cc in the space, LLIF 5 cc in the cage, ALIF 5 cc in the cage. And Group B - Using I-Factor bone graft mixed with bone marrow aspirate concentrate. (1:1) subdivided into three groups: TLIF 2.5 cc in the cage and 2.5 cc in the space, LLIF 5 cc in the cage, ALIF 5 cc in the cage. Radiological outcomes includes fusion rates per the Lenke scale, CTUH. Clinical outcomes will be evaluated via the Oswestry Disability Index (ODI), Short Form Performance (SPF-36) and Visual Analog Scale (VAS and VASS) for pain and satisfaction. Results: Data analysis by now, with 26 patients completed 6 months follow up. Group A (19 patients), Group B (7 patients), shows no difference at Lenke scale with every patient on LENKE A at 6 months. CTUH measures shows more differences between 3 and 6 months in patients with use of mixed ABM/p-15 + BMA (Group B) than just ABM/P-15 (Group A). No differences in clinical outcomes in both groups. Conclusion: No differences between techniques used, therefore the quantities used seem to be sufficient to achieve fusion. Fusion rates seems to be slightly improved at Group B (p15/ABM + BMA) and non dependent on the technique. Long-term follow-up is required, this is 6 months preliminary report.
1329
A047: AOGO guideline: changing the landscape of the osteobiologic use in ACDF
Hans-Jörg Meisel 1 , Nancy Santesso 2 , Yabin Wu 3 , Amit Jain 4 , Timothy S. Yoon 5 , Jeffrey C. Wang 6 , Viswanadha Arun-Kumar 7 , Gianluca Vadalá 8 , Juan P. Cabrera 9 , Ricardo Rodrigues-Pinto 10 , Sathish Muthu 11 , Christopher Martin 12 , Pieter-Paul A. Vergroesen 13 , Chris Arts 14 , Waeel Hamouda 15 , Patrick Hsieh 6 , Andreas Demetriades 16 , Zorica Buser 17 , and AO Spine Knowledge Forum Degenerative
1 BG KlinikumBergmannstrost, Halle, Germany
2 Department of Health Research Methods, Evidence & Impact, McMaster University, Ontario, Canada
3 AO Spine, Davos, Switzerland
4 Johns Hopkins University, United States
5 Emory University, United States
6 Keck School of Medicine, United States
7 Reva Spine Centre, India
8 Campus Bio-Medico University of Rome, Italy
9 Hospital Clínico Regional de Concepción, Chile
10 Spinal Unit (UVM), Department of Orthopaedics, Centro Hospitalar Universitário do Porto, Portugal
11 Government Medical College, India
12 University of Minnesota, United States
13 The University Medical Center Utrecht, The Netherlands
14 Department Orthopaedic Surgery, Maastricht University Medical Centre, The Netherlands
15 Kasr Alainy School of Medicine, Research, and Teaching Hospitals - Cairo University, Egypt
16 Royal Infirmary Edinburgh, United Kingdom
17 Gerling Institute, Brooklyn, United States
Introduction: Osteobiologics are widely used in spinal surgery for a variety of indications. However, the clinical use of the several available osteobiologics is not very well defined. Several factors are responsible for the current situation. Firstly, there is a lack of robust clinical evidence for the use of biologics, which provides limited information to foster their knowledge and to guide their use. Secondly, regulations about the use of biologics vary across different countries. In most cases, a specific osteobiologic is chosen based on surgeon’s interest and/or because it is available in the hospital catalog. There is a need to develop an international guideline to provide evidence-based guidance to the spinal community on how and when to use osteobiologics in spine surgery. Therefore, the AO Spine Knowledge Forum Degenerative conducted an internationally led initiative to develop a guideline (AOGO) for the use of osteobiologics in Anterior Cervical Spine Fusion (ACDF) procedures. Material and Methods: The AO policies and the Guideline International Network (GIN)-McMaster Guideline Development Checklist directed the overall guideline development. The guideline group consisted of 71 participants with expertise in degenerative spine diseases and surgery from 22 countries. Meetings were held to discuss evidence and recommendations and were attended by the guideline panel, a methodologist to facilitate the process, and AO Spine representatives. The guideline panel determined the topics for evidence review and the outcomes to be assessed, including benefits, harms and the effects of comorbidities and costs. Systematic reviews of the evidence were conducted for each topic and are published separately. The methodologist compiled the evidence from the systematic reviews into GRADE Evidence-to-Decision (EtD) frameworks, using the GRADEpro Guideline Development Tool. Guideline panel members made the final recommendations through consensus. Results: The guideline group agreed on five recommendations. A conditional recommendation for the use of allograft, autograft or a cage with an osteobiologic in primary ACDF surgery was made. There was also a conditional recommendation for the use of an osteobiologic in single or multi-level ACDF and in ACDF/cervical total disc replacement (TDR) hybrid construct surgery. However, the guideline group suggested that surgeons use other osteobiologics rather than human bone morphogenetic protein-2 (rhBMP-2) in common clinical situations. A conditional recommendation means that surgeons can choose to use one graft over another or one osteobiologic over another primarily based on the clinical situation, and the costs and availability of the materials. Clinicans will need to be informed of their local situation when making decisions. Due to the lack of data, no recommendation was made for the use of ostebiologics in people with comorbidities or for revision surgery. Conclusion: With a rigorous evaluation process and systematic review of the literature utilizing the GRADE approach, the AOGO guideline was developed. Despite, the comprehensive searches for evidence, there were often few studies, primarily non-randomised studies and case series, with small sample sizes and inherent risks of bias. Therefore, the certainty of the evidence for the benefits and harms, and the costs associated with osteobiologics in ACDF, was either low or very low.
1627
A048: Elucidating the potential therapeutic mechanisms underlying distriction spinal cord injury-associated neuroinflamation and apoptosis
Bo Han 1 , Weishi Liang 1 , Yong Hai 1 , and Peng Yin 1
1 Department of Orthopedic Surgery, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: The incidence of distraction spinal cord injury (DSCI), which results from spinal cord ischemia due to vascular compromise and spinal cord tract disturbances, remains high. Furthermore, because no animal model that mimics DSCI in clinical settings is available thus far, the cytological and molecular mechanisms underlying DSCI remain unclear. Thus, this study aimed to establish a porcine model of DSCI and investigate the apoptosis and neuroinflammation in these pigs. Material and Methods: Before surgery, all pigs were randomly divided into three groups: sham group, osteotomy surgery only (control); the incomplete distraction spinal cord injury (IDSCI) and complete distraction spinal cord injury (CDSCI) groups, osteotomy plus DSCI surgery with a motor-evoked potential (MEP) amplitude decreased by >75% and >100%, respectively. After surgery, modified Tarlov scoring and MRC muscle strength scoring were used to evaluate neurologic function in each group. We observed the distracted spinal cord using magnetic resonance imaging (MRI), and all the pigs were sacrificed. We used immunofluorescence staining to assess the neuroinflammatory responses and neuronal survival in the DSCI lesions. Inflammatory cytokine levels in the spinal cord and cerebrospinal fluid (CSF) were also analyzed. Western blotting and immunohistochemistry were used to determine the expression of apoptosis-related proteins. Results: The modified Tarlov scoring and MRC muscle strength decreased significantly in the DSCI groups. T2-MRI showed a relative enhancement at the center of the DSCI lesions. H&E and Lxol fast blue staining revealed that spinal cord distraction destroyed the normal structure of spinal cord tissues and nerve fiber tracts, exacerbating inflammatory cell infiltration, hyperemia, and edema. Immunofluorescence staining indicated impaired neuronal and microglial structure and function and astrocyte hyperplasia after DSCI. The IL-1β, IL-6, and TNF-α levels increased in the spinal cord and CSF of the DSCI groups. Moreover, DSCI promoted the protein expression of p53, Bax, and caspase-3 in the spinal tissues, but reduced the Bcl-2 expression. Conclusion: This study successfully established a porcine DSCI model that closely mimics DSCI in clinical settings and clarified the mechanisms underlying DSCI-associated apoptosis and neuroinflammation; thus, our findings highlight potential DSCI-treatment strategies for establishing suitable drug therapies.
1922
A049: The intersection of spinopelvic deformity and spine oncology
Eric Sankey 1 , Harrison Hockenberry 1 , Brandon Bishop 1 , Meghan Price 1 , Jacob Sperber 1 , Edwin Owolo 1 , Antoinette Charles 1 , Dana Rowe 1 , Emily Luo 1 , Eli Johnson 1 , Alexia Bwensa 1 , Ali Ahmed 1 , Zachary Pennington 1 , Melissa Erickson 1 , Daniel Sciubba 2 , and C. Rory Goodwin 1
1 Duke University School of Medicine, Department of Neurosurgery, Durham, United States
2 Northwell, Department of Neurosurgery
Introduction: Spinopelvic alignment, particularly in the context of sagittal balance, significantly impacts health-related quality of life and postoperative outcomes. Despite the fact that spine tumors are known to cause significant vertebral body destruction and focal kyphotic deformity, the influence of global spinal alignment in the context of spine oncology remains unknown. As such, we conducted a retrospective cohort review of adult patients with spine tumors and investigated the incidence and association of spinopelvic deformity on outcomes after spine surgery. Methods: A multi-institutional retrospective cohort study was conducted on patients with spine tumors who received one or more full-length spinal (scoliosis) x-rays at two, large tertiary medical centers over a period of 7 years. Local and global spinopelvic parameters were measured on all available pre- and initial postoperative scoliosis x-rays, including pelvic tilt, sacral slope, pelvic incidence (PI), thoracic kyphosis, T1 slope, lumbar lordosis (LL), global tilt, sagittal vertical axis, coronal alignment, PI-LL mismatch, and global alignment and proportion (GAP) score. Patients were then compared between a PI-LL mismatch of ≤ 10 (appropriately aligned) or >10 degrees (positive sagittal imbalance) in terms of baseline characteristics, postoperative outcomes, and mortality. Continuous, nonparametric variables are expressed as median (interquartile range) and categorical data is expressed as frequency (%). Fisher’s exact test was used to compare categorical data and Wilcoxon rank-sum test was used for continuous data. A p-value < 0.05 was considered statistically significant. Results: Between 2012 and 2019, 82 adult patients with one or more spinal tumors received pre- and/or postoperative full-length spinal (scoliosis) x-rays at the authors’ institutions. Of these patients, 38 (46%) were found to have a PI-LL mismatch ≤10 degrees and 44 (54%) patients had a mismatch > 10 degrees, denoting positive sagittal imbalance. Patients with sagittal imbalance were more frequently male (n = 35 (80%); p = 0.001), had extra-vertebral osseous metastasis (n = 33 (75%), p = 0.04), and presented with pain (n = 44 (100%), p = 0.018). However, other characteristics including age, functional status (i.e., mRS and KPS), pathological vertebral body collapse, treatment approach and modalities, hospital length of stay and discharge location, postoperative complication rates, mortality and survival rates were relatively similar between groups over a follow-up duration of 20 (7-33.5) months. Conclusions: The incidence and impact of spinopelvic deformity on patients with spinal tumors has been previously unknown. This is the first study to demonstrate that the majority of patients with spine tumors may develop spinal deformity during the course of their disease process. While previous investigations have shown a negative correlation between positive sagittal imbalance and patient outcomes in the degenerative spine population, we did not find a significant difference in our spine oncology cohort. Ultimately, larger, prospective studies with standardized imaging and follow-up protocols are needed to further elucidate the impact of spinopelvic deformity on outcomes in patients with spine tumors.
196
A050: Do the use of autograft influence the fusion and complication rate in patients undergoing 1 or 2-level ACDF surgery? A PRISMA-compliant network meta-analysis
Sathish Muthu 1,2 , Vibhu Krishnan Viswanathan 2,3 , Ricardo Rodrigues-Pinto 4,5 , Juan P. Cabrera 6 , Stipe Corluka 7,8 , Christopher Martin 9 , Michael Collins 10,11 , Neha Agarwal 12 , Yabin Wu 13 , Jeffrey C. Wang 14,15 , Meisel Hans-Jorg 16 , Zorica Buser 17,18 , and AO Spine Knowledge Forum Degenerative
1 Department of Orthopaedics, Government Medical College, Dindigul, India
2 Department of Spine Surgery, Orthopaedic Research Group, Coimbatore, India
3 Department of Musculoskeletal Oncology, University of Calgary, Alberta, Canada
4 Department of Orthopaedics, Centro Hospitalar Universitário do Porto, Portugal
5 Universidade do Porto, Portugal Instituto de Ciências Biomédicas Abel Salazar, Portugal
6 Department of Neurosurgery, Hospital Clínico Regional de Concepción, Chile
7 Spinal Surgery Division, Department of Traumatology, University Hospital Centre Sestre Milosrdnice, Zagreb, Croatia
8 University of Applied Health Sciences, Department of Anatomy and Physiology, Zagreb, Croatia
9 Department of Orthopaedic Surgery, University of Minnesota, Minneapolis, United States
10 Department of Orthopaedic Surgery, Tulane University, New Orleans, United States
11 Department of Neurosurgery, Tulane University, New Orleans, United States
12 P95 Epidemiology and Pharmacovigilance, Leuven, Belgium
13 AO Foundation, Research Department, AO Spine, Davos, Switzerland
14 Department of Orthopaedic Surgery, Keck School of Medicine, University of Southern California, California, United States
15 Department of Neurosurgery, Keck School of Medicine, University of Southern California, California, United States
16 Department of Neurosurgery, BG Klinikum Bergmannstrost Halle, Germany
17 Gerling Institute, New York, United States
18 Department of Orthopedic Surgery, NYU Grossman School of Medicine, New York, United States
Introduction: To date, there exists significant ambiguity regarding the benefits and pitfalls of the use of autograft, other bone graft substitutes, and different constructs for reconstruction in patients undergoing ACDF. The current study was conducted to compare the fusion outcomes and complications for different 1 or 2-level anterior cervical decompression and fusion (ACDF) constructs performed with and without the application of autologous bone graft. Methods: We performed an independent and duplicate search in electronic databases including PubMed, Embase, Web of Science, Cochrane, and Scopus for relevant articles published between 2000 and 2020. We included comparative studies reporting fusion rate and complications with and without the use of autografts in ACDF across 5 different fusion constructs. A network meta-analysis was performed with the included studies in Stata, categorized based on the type of fusion constructs utilized. Available fusion constructs were ranked based on the p-score approach and surface under cumulative ranking curve (SUCRA) scores. The confidence of results from the analysis was appraised with Cochrane’s CINeMA approach. Results: A total of 2,216 patients from 22-studies including 6 Randomized Controlled Trials (RCTs) and 16 non-RCTs were included in the network analysis. The mean age of included patients was 49.3 (±3.62) years. Based on our meta-analysis, we could conclude that the use of autograft in 1- or 2-level ACDF did not affect the achievement of final fusion and mechanical implant-related complications. The final fusion and mechanical complication rates were also not significantly different across the five different ACDF fusion constructs. The use of plated constructs was associated with a significant increase in the post-ACDF dysphagia rates [OR 3.42; 95% CI (0.01,2.45)], as compared to stand-alone procedures but were associated with the lowest rates of graft collapse and subsidence. Conclusion: The choice of fusion constructs and use of autografts does not significantly affect the fusion and overall complication rates following 1 or 2-level ACDF.
1878
A051: An investigation of the potential of the human skeletal stem cell to replace mesenchymal stromal cells in bone tissue engineering
Daniel Ahern 1 , Mathieu Riffault 1 , Barry Moran 2 , David Hoey 1 , and Joseph Butler 3
1 Trinity Centre for Biomedical Engineering
2 School of Biochemistry and Immunology, Trinity College Dublin, Dublin, Ireland
3 Department of Trauma and Orthopaedics, Mater Misericordiae University Hospital, Dublin, Ireland
Introduction: Mesenchymal stromal cells (MSCs) have long been considered as one of the key cellular precursors in bone formation and have been the subject of several pre-clinical and clinical studies exploring their role in spinal fusion. However, the clinical application of MSCs is currently limited by significant variability, which could potentially be explained by the heterogeneous nature of MSC samples. Recently, a skeletal stem cell (SSC), and its progeny, were identified in adult human long bones. We sought to identify the presence of these cells within human vertebral body (VB) bone marrow and examine their osteogenic potential, in order to identify a cellular candidate for bone tissue engineering (TE). Methods: Bone marrow aspirates were obtained from the vertebral body bone marrow of patients undergoing posterior spinal fusion. Flow cytometric analysis was used to identify proportions of SSC populations within the marrow isolate, with the remaining undergoing traditional plastic adherent cell culture expansion. Serial flow cytometry was performed to identify trends in SSC cell surface marker expression over time. At Passage (P)3, PA MSCs underwent cell sorting and the SSC, BCSP, OP and CP cell populations were isolated individually from the main MSC fraction. These in turn, were culture expanded to P7 in tandem with the MSC, at which point all populations underwent flow cytometry and osteogenic and adipogenic assays. Results: 6 donors were recruited to this study (3 male and 3 female). The SSC and progenitors were present in varying proportions of each donor: SSC 0.0542%, BCSP 0.9%, OP 10.868%, CP 5.553%. Following culture expansion, significant changes over time were demonstrated between the proportions of the SSC and progenitors within the total cell fraction. Following culture expansion, a significant reduction in cell surface marker expression was found in all groups. For individual donors, the OP demonstrated superior osteogenic potential compared to the SSC (3-fold greater, p < 0.05) but not compared to the MSC. Conclusion: Here, we describe the presence of the SSC within the VB BM. The low presence of the SSC or progenitors within BM precludes their use from immediate cell sorting and reimplantation following BM aspiration. Therefore, cell culture expansion of MSCs is necessary to obtain a viable number of cells. While the SSC has demonstrated great promise as a pure stem cell, here, the OP cell demonstrated superior osteogenic capacity to the SSC with equivalent osteogenic capacity to the MSC. While this study is primarily limited by a small sample size, this is the first study directly comparing the SSC to the traditional MSC.
1949
A052: Allograft cellular bone matrix as an alternative to iliac crest autograft in anterior cervical discectomy and fusion
Samuel Goldman 1 , Gregory Paschal 1 , Frederik Abel 1 , Philip Paschal 1 , Celeste Abjornson 1 , Andrew Sama 2 , and Frank Cammisa 2
1 Integrated Spine Research Program
2 Spine Surgery, Hospital For Special Surgery, New York, United States
Introduction: Anterior Cervical Discectomy and Fusion (ACDF) is a commonly used surgical procedure to alleviate pain related to symptomatic cervical degenerative disc disease (DDD). There are many graft material options and interbody cage designs available. Iliac crest autograft has conventionally been considered the gold standard. Due to reported complications and pain associated with iliac crest harvest for ACDF, cellular allogenic bone grafts with mesenchymal stem cells (MSCs) and osteoprogenitor cells (OPCs), known as cellular bone matrices (CBMs), have been investigated as a possible alternative. Many CBMs are commercially available but vary greatly by processing methods. The objective was to assess the radiographic and clinical outcomes of ACDF procedures with anterior cage and plate fixation that were supplemented with CBM. Material and Methods: Under IRB approval, a retrospective review of all patients who underwent an ACDF with placement of CBM (Trinity Elite, Orthofix, Lewisville, TX) was conducted. Patient charts were reviewed for demographics, medical co-morbidities, pain assessments, radiographic findings, and physical exam findings at the following time points: preoperative, perioperative, and post-operatively at 6 weeks, 6 months, and at 12 months. Intra-operative data such as instrumentation used, cage sizes, numbers of levels fused, length of surgery, amount of bone graft material used, autologous graft used, and blood loss were collected. Radiographic images were assessed for fusion status. Clinical outcome measures included complication(s) and reoperation rates. Results: Ninety-seven patients underwent an ACDF procedure at single or multiple levels with CBM. Average age was 62.68 (range 18-87). The average fusion length was 1.18 levels (range 1-3); 5cc per level were used on average in each patient. There were no surgical complications with the placement of the cage/CBM. Pre-operative pain assessment averaged an 8 visual analogue score (VAS; range 5-10) and was significantly reduced to 2.26 (range 0-6: p < 0.05) at last follow up. There was radiographic evidence of bone remodeling and bridging bone in 70% of patients by 3 months; in 85% by 6 months and 94% by one year. No loosing of hardware was documented by the last follow up. Conclusion: The use of cellular bone matrix is safe and provides a high fusion rate. This type of graft material provides an ideal graft with osteoinductive, osteoconductive, and osteogenic properties.
502
A053: Preliminary results of biphasic calcium phosphate with submicron surface topography as standalone alternative to autograft in posterolateral fusion: a prospective, multi-center, randomized, intra-patient controlled trial
Luuk van Dijk 1 , Diyar Delawi 2 , Eric Hoebink 3 , Diederik Kempen 4 , Job van Susante 5 , and Moyo Kruyt 6
1 Kuros Biosciences BV, The Netherlands
2 St. Antonius Ziekenhuis, The Netherlands
3 Amphia Ziekenhuis, Breda, The Netherlands
4 OLVG Amsterdam, The Netherlands
5 Rijnstate Ziekenhuis, Arnhem, The Netherlands
6 University Medical Center Utrecht, Utrecht, The Netherlands
Introduction: Iliac Crest Bone Graft is considered the gold standard for spinal fusion, but with limited availability and an extra procedure for harvesting, spine surgeons often utilize alternatives. Synthetic calcium phosphate bone grafts with submicron surface topographies have demonstrated promising results in preclinical studies. We initiated a large multicenter trial to determine non-inferiority of a biphasic calcium phosphate with submicron needle-shaped surface topography (BCP<µm) as compared to autograft in instrumented posterolateral spinal fusion (PLF). For registration purposes we analyzed the safety and fusion rate in the first 50 patients. Methods: Adult patients indicated for instrumented PLF of one to six levels from T10-S2 were enrolled at five participating centers. After instrumentation and preparation of the bone bed, the randomized allocation side of the graft type was disclosed. One side was grafted with 10 cc of autograft per level containing a minimum of 50% iliac crest bone. The other side was grafted with 10 cc of BCP<µm granules standalone (without autograft or bone marrow aspirate). In total, 71 levels were treated (average 1.4 per patient). Prospective follow-up included adverse events, the Oswestry Disability Index (ODI), and a fine-cut (< 1 mm) Computerized Tomography (CT) at one year. Fusion per level and per side was systematically scored as ‘fusion’, ‘doubtful fusion’, or ‘no fusion’ by two spine surgeons blinded for the allocation. Disagreements were resolved by panel discussion. Only levels scored with ‘fusion’ were considered fused, whereas levels with ‘doubtful fusion’ and ‘no fusion’ were considered not fused. Results: The inclusion period spanned two years and follow up of these patients is one year. Average age was 57 years old (27-79 years), with 60% female and 40% male. The diagnoses included deformity (56%), structural instability (28%), and instability from decompression (20%). The fusion rate determined by fine-cut (< 1 mm) CT for BCP<µm was 76.1% (54/71 levels), which compared favorably to the fusion rate of 43.7% for autograft (31/71 levels). Fusion of the BCP<µm side was not contingent upon fusion of the autograft side, as 36.6% (26/71) of levels fused on the BCP<µm side but did not fuse on the autograft side. In contrast, 4.2% (3/71) of levels fused on the autograft side but not on the BCP<µm side. Moreover, 39.4% (28/71) of levels had complete fusion of both sides, while 19.7%% (14/71) did not have fusion on either side. BCP<µm performed better than autograft in single-level fusions, achieving a 73.5% (25/34 levels) fusion rate, compared to 47.1% (16/34 levels) for autograft. In two-level fusions, the fusion rate for BCP<µm was 73.1% (19/26 levels), compared to 38.5% (10/26 levels) for autograft. Oswestry Disability Index (ODI) score decreased from a mean of 46.0 (±15.0) to a mean of 31.7 (±16.9), and 52.4% of patients improved with at least 15-point decrease. Discussion and Conclusion: This data, aiming to determine non-inferiority of standalone BCP<µm as compared to autograft for posterior spinal fusions, is promising. Ongoing studies to increase the power of the statistics with more patients is forthcoming.
1464
A054: The potential risk of neurological deterioration while on neo-adjuvant denosumab in patients with spinal giant cell tumor and epidural mass extension causing neurological or impending deficit: a meta-analysis of the literature
Humaid Al Farii 1 and Justin Bird 1
1 Orthopedics, MD Anderson Cancer Center, Houston, United States
Purpose: GCT is a benign but locally aggressive primary bone tumor and spinal GCTs accounted for 2.7-6.5% of all GCTs in bone. En bloc resection which the standard treatment for GCT of the spine might not feasible because of unresectable tumor at presentation, however, neoadjuvant denosumab has been proved recently with its effectiveness to downstaging the tumor. So, the aim of this study primarily to identify the potential risk of neurological deterioration while patients on neoadjuvant denosumab for spinal GCT with epidural mass extension, and also aimed to have secondary outcomes included radiographic features, surgical/technical complexity and histological features after patients received neoadjuvant denosumab. Methods: Using predetermined inclusion and exclusion criteria, PubMed and Embase electronic databases were searched in August 2022 for relevant articles relating to surgical spinal GCTs with neoadjuvant denosumab. Keywords used were “Spine” AND “Giant Cell Tumor” AND “Denosumab”. Results: 428 articles were identified and screened. A total of 22 patients from 12 studies were included for review. 17 patients were female (17/22, 77%), mean age of the patients was 32 years (18-62 years) and average follow up was 21 months. Most GCTs occurred in the thoracic and thoracolumbar spine (11 patients, 50%), followed by 36% in lumbar spine and lowest 14% in cervical spine. Almost half of the patients had neurological deficit at presentation (45%), and more than 60% had epidural mass extension of type 2 and 3 on Bilsky grading system. Although there were four patients underwent initial spinal stabilization with neoadjuvant denosumab, none of the other cases deteriorate neurologically irrespective to their neurological status at presentation. All twenty-two neither had local recurrence or metastasis except one patient who found to have lung nodules post operatively. More than 90% of cases had decreased overall tumor size and increased bone formation, and technically facilitated surgical dissection in more than 85% among those who had documented their definitive procedures. Also, denosumab was able to remarkably deplete giant cells in about 95% of cases, however, some authors reported residual RANKL-positive stromal cells especially remained around the woven bone in 27% (6 cases). Conclusions: In spinal GCTs and specifically inoperable tumors at presentation, neoadjuvant denosumab showed its efficacy to downstage the tumor radiographically and surgically, and furthermore its safety with no potential risk of neurological deterioration irrespective to presence of epidural mass extension and/or neurological deficit at presentation. However, there is still uncertainty about the treatment protocol for denosumab therapy in term of duration and dosage, and we recommended further well-designed studies to support our findings and make more consensus conclusions.
OP07: Surgical Biomechanics 2
562
A055: Influence of the facet joint tissues on lumbar segmental range of motion in the sagittal plane: a finite element approach
Adi Mithani 1 , Ahmed Aoude 2 , and Mark Driscoll 3
1 Biological and Biomedical Engineering
2 Health Centre, Department of Surgery
3 Mechanical Engineering, McGill University, Montreal, Canada
Introduction: Facet joints (FJ) play a biomechanical role in the kinematic behaviour of the lumbar spine. They are located posteriorly and contain the facet cartilage (FC) surrounded by the facet capsular ligament (FCL). Patients with FJ degeneration show non-significant changes in intervertebral rotations (IVR), whereas those with added disc degeneration have increased IVR. Under flexion-extension loading, the FCL undergoes superior-inferior strain, suggesting its role in contributing to spinal stiffness. However, no biomechanical modelling has been conducted to evaluate the influence of the FCL-FC complex on lumbar IVR. The primary objective of this research was to develop a validated and representative finite element (FE) spine model to evaluate the contribution of the FCL-FC complex to lumbar IVR in the sagittal plane under extension loading. Material and Methods: In this study, a FE spine model was developed and validated against in-vivo published findings of IVRs at lumbar spine levels L2-S1. The model included the thoracolumbar vertebrae, rib cage, intervertebral disc, FC, FCL, pelvis, and spinal ligaments (iliolumbar, supraspinous, intertransverse, and interspinous ligaments). The FC and FCL were modelled as compression-only and tension-only spring elements, respectively, connecting adjacent facets of the superior and inferior vertebra. A follower load of 1000N was applied perpendicularly to the surface of the T1 vertebra’s superior endplate to S1 using pre-loaded springs, increasing by 2.4% at each vertebral level. The perpendicular orientation of loading ensured the resultant forces remained tangential to the spinal profile. The FJ primarily carries compressive forces in extension, thus a -55˚ remote rotation was applied to the body of the T1 vertebra to simulate maximum extension with the pelvis as the fixed support. Case scenarios were executed and IVRs were calculated based on the intersection between lines running parallel to the superior and inferior endplate at an intervertebral level. Results: The application of extension generated IVRs values within a 20% margin of the in-vivo mean values acquired from Lin et al. (1994), remaining within the standard deviation of each intervertebral segment. Extension loading following bilateral L4-L5 FCL removal increased L4-L5 IVR by 23.63%. Similarly, L5-S1 FCL removal increased L5-S1 IVR by 30.08%. Bilateral L4-L5 FC removal increased L4-L5 IVR by 41.86%, while L5-S1 FC removal increased L5-S1 IVR by 16.69%. Finally, removal of the L4-L5 FC-FCL complex increased L4-L5 IVR by 23.18%, while L5-S1 FC-FCL removal increased L5-S1 IVR by 51.42%. Conclusion: Removal of the FCL-FC complex increased instability significantly at L4-L5 and L5-S1. Clinically, this may suggest a role for FJ tissues in mediating the mechanical effects of FJ osteoarthritis (OA) through a positive-feedback loop. Repeated loading of the FCL at physiologic strains reduces FCL stiffness, contributing to increased IVR and lumbar instability. Increased segmental movement causes stress at the FJ, which promotes FC degeneration. This may impart additional strain on the FCL, increasing segmental instability and the risk of FJ OA. The FCL-FC complex is involved in controlling the mobility of the FJ and the magnitude of contact forces, a delicate interplay required to preserve normal segmental movement and prevent spinal pathology.
765
A056: Segmental range of motion is an independent determinant of spinal cord stress and strain in degenerative cervical myelopathy
Aditya Vedantam 1 , Balaji Harinathan 1 , Ali Warraich 2 , Yuvaraj Purushothaman 1 , Matthew Budde 1 , and Narayan Yoganandan 1
1 Neurosurgery, Medical College of Wisconsin, Milwaukee, United States
2 University of Chicago, Chicago, United States
Introduction: Spinal cord stress and strain during cervical flexion and extension is a known contributor to the pathophysiology of DCM, yet direct measurement of these forces is not feasible in humans. The factors contributing to spinal cord stress and strain in DCM patients have not been elucidated. Determining the association between segmental range of motion and spinal cord stress/strain can help choose surgical strategies that address adverse spinal cord tension. The aim of this study was to measure spinal cord stress/strain using patient-specific 3D finite element models (FEM), and determine the relationship between range of motion and spinal cord stress/strain. Material and Methods: Three-dimensional patient-specific FEMs were created for 6 DCM patients (mild [n = 2], moderate [n = 2] and severe [n = 2]). FEMs were developed using MRI-derived geometries of the spine and spinal cord and incorporated material properties from human spinal cord tissue that have been reported previously. Flexion and extension of the cervical spine was simulated with a pure moment load of 2 Nm. The model was constrained at the inferior surface of the T1 vertebra in all degrees-of-freedom, and the sagittal moment loads were applied at the superior vertebra. An additional follower force of 75N to simulate the head mass and muscle force was applied. Von Mises stress and maximum principal strain of the spinal cord was calculated at each segment during flexion and extension. Spinal cord area, spinal cord compression and range of motion at each segment was measured and regression analysis was performed to determine predictors of spinal cord stress and strain. Results: A total of 36 segmental measurements were made. The mean segmental Von Mises stress was 34.7 ± 19.9 kPa and the mean segmental MPS was 20.7 ± 10.7%. Segmental Von Mises stress (p < 0.001) and maximum principal strain (p=0.027) was significantly higher in extension compared to flexion. The mean segmental range of motion was 4.8 ± 2.8 degrees, the mean spinal cord area was 62.9 ± 10.2 mm2 and the mean spinal cord compression ratio was 0.77 ± 0.02. Segmental range of motion was independently associated with spinal cord stress (b = 0.81, p < 0.001) and strain (b = 0.6, p < 0.001). Segmental range of motion was a stronger determinant of stress and strain as compared to spinal cord compression ratio (b = 0.49, p < 0.001; b = 0.47, p = 0.003) or spinal cord area (b = 0.03, p = 0.8; b = 0.29, p = 0.046). Conclusion: Using patient-specific cervical spinal cord FEM, we estimated patient-specific spinal cord stress and strain during flexion and extension. Neck extension is associated with greater stress and strain in the cervical spinal cord. Segmental range of motion is the primary determinant of spinal cord stress and strain, and this association is independent of the severity of spinal cord compression. Further study is necessary to confirm these findings and determine the effect of surgical intervention on spinal cord stress and strain.
1261
A057: A biomechanical approach to predict proximal junctional kyphosis development
Fatemeh Alavi 1 , Christopher J. Nielsen 2 , Stephen Lewis 2 , Raja Rampersaud 2 , and Angela Cheung 1
1 Osteoporosis and Women's Health, University Health Network (UHN), Toronto General Hospital, Toronto, Canada
2 Orthopaedic Surgery, University Health Network (UHN), Toronto Western Hospital, Canada
Introduction: Proximal junctional kyphosis (PJK) remains one of the most common complications of adult spinal deformity surgery. Interventions proposed to limit the rate of PJK include tethering, cementing upper instrumented vertebra (UIV) +/- UIV +1, as well as sagittal alignment parameters which are still debated in adult spinal deformity. The aim of this research is to identify patients at the risk of PJK pre-operatively using a novel biomechanical approach based on mathematical, musculoskeletal, and finite element (FE) analyses to define loading forces on the UIV and UIV + 1. We hypothesis that PJK occurs as a result of excessive vertebral loading at UIV and/or UIV+1, with low bone mineral density (BMD) increasing risk. Material and Methods: Twenty consecutive patients with UIV of T10 fused to sacrum, and no previous fusion surgery were retrospectively reviewed. We used patient-specific thoracolumbar full-body musculoskeletal models to calculate vertebral forces. The models were created by using the generic model scaled for height and weight. We developed custom MATLAB scripts to identify the location and orientation of the intervertebral discs (IVDs) from the preoperative EOS images and adjusted the orientation of the vertebral bodies in the model accordingly. We employed Bezier curve fit to simulate postoperative alignments by changing control points of the curve fitted to preoperative EOS image, based on radiological parameters of postoperative EOS image. After constructing patient-specific pre- and postoperative models, musculoskeletal analysis was performed using OpenSim software in the upright standing position to calculate vertebral loading at all levels. For patients with opportunistic CT scans, FE modeling of UIV or UIV+1 was carried out under their corresponding calculated vertebral loading. The location of failure at UIV or UIV+1 was specified by elements with high risk factor (defined as strain energy density to yield strain energy density). Results: PJK developed in 10 out of 20 patients. Average shear force at UIV + 1 in non-PJK patient was 36.2N, while average shear force at UIV + 1 was 152N in patients with PJK. Utilizing a cut-off value of 100N of shear force at UIV + 1, the sensitivity and specificity of our approach were 0.8 and 0.9, respectively. The FE analysis showed the location of compression fracture occurrence in UIV and/or UIV+1, which perfectly agreed with postoperative images. Conclusion: Utilizing a novel biomechanical approach of mathematical, musculoskeletal, and finite element analyses, we were able to determine a cut-off value of 100N for shear force at the UIV + 1 to predict the risk of PJK after adult spinal deformity surgery. Further research needs to identify modifiable alignment variables which can be used for pre-operative planning to lessen shear forces at the UIV + 1.
1860
A058: The effect of semirigid fixation techniques on the development of proximal junctional kyphosis - a finite element study
Máté Turbucz 1,2 , Ágoston Jakab Pokorni 1,3 , Jennifer Fayad 1,4 , Peter Pal Varga 5 , Peter Eltes 1,3 , and Aron Lazary 3,5
1 National Center for Spinal Disorders, Buda Health Center, In Silico Biomechanics Laboratory, Budapest, Hungary
2 School of PhD Studies
3 Department of Spine Surgery, Semmelweis University, Budapest, Hungary
4 Department of Industrial Engineering, Alma Mater Studiorum, Universita di Bologna, Bologna, Italy
5 National Center for Spinal Disorders, Buda Health Center, Budapest, Hungary
Introduction: Proximal junctional kyphosis (PJK) is a common complication following long posterior spinal fixations in patients undergoing adult spine deformity correction. Its incidence rate varies between 20 and 40 %, causing functional instability at the cranial end of the instrumented spine. Numerous patient-specific and biomechanics-related factors have been reported in the literature that have been shown to contribute to the development of PJK. Sudden change in the range of motion (ROM) between the healthy and fixed spinal segments were identified as one of the main biomechanical causes. Accordingly, in the current study, we investigated different semirigid fixation techniques (SFT) that could form a damping zone at the cranial end of spinal fixations. Material and Methods: Four osseoligamentous 3D finite element (FE) models have developed: the intact T7-L5 spine; the titanium rod fixation (TRF) technique, which included a 5.5 mm titanium rod fixation from T8 to L5; the multiple rod fixation (MRF) technique, which included a 5.5 mm titanium rod fixation from T9 to L5 connected with multiple 1.9 mm thin titanium rods from T8 to T9, and the PEEK rod fixation (PRF) technique, which included a 5.5 mm titanium rod fixation from T9 to L5 connected with 5.5 mm polyetheretherketone rods from T8 to T9. A modified multidirectional hybrid testing protocol was used in the current study. First, in the load-controlled step, a pure bending moment of 5 Nm was applied to measure the intervertebral rotation (IVR) in the three anatomical planes, normalized by the TRF technique. Second, in the motion-controlled step, the displacement of the TRF technique from the first step was applied to the instrumented FE models to analyze the pedicle screw stress distributions in the upper instrumented vertebra (UIV). Results: In the load-controlled step, at the most cranial instrumented segment, the IVR values increased by 46.8% and 99.2% in flexion, by 43.2% and 87.7% in extension, by 90.1% and 137% in lateral bending, and by 407.1% and 585.2% in axial rotation, in the case of MRF and PRF, respectively. In the displacement-controlled step, the maximum pedicle screw stress values for the TRF at the UIV level were 37.26 MPa, 42.13 MPa, 44.4 MPa and 44.59 MPa for flexion, extension, lateral bending and axial rotation, respectively. Compared to TRF, MRF and PRF lowered the maximum screw stress values by 17.3% and 27.7% for flexion, by 26.6% and 36.7% for extension, by 6.8% and 34.3% for lateral bending, and by 49.1% and 59.8% for axial rotation. Conclusion: FE analysis has revealed that semirigid spinal fixation techniques allow higher mobility at the most cranial instrumented segment and provide a more gradual transition in motion between the instrumented and healthy segments of the cranial spine. Accordingly, using semirigid spinal instruments decreases the load in the pedicle screws at the UIV level and therefore reduces the risk of developing PJK.
1299
A059: Evaluating the active apex correction (APC) technique in early onset scoliosis (EOS) with simulated spinal growth using patient-specific finite element modelling
Alaa Azmi Ahmad 1,2 , Daksh Jayaswal 2 , Manoj Kodigudla 2 , Amey Kelkar 2 , Aakash Agarwal 2 , and Vijay Goel 2
1 Palestine Polytechnic University, Hebron, Palestine
2 Department of Biomedical Engineering, University of Toledo, Toledo, United States
Introduction: New techniques like the Active Apex Correction (APC) technique have the potential to be effective surgical alternates to traditional treatments methods in EOS. The APC actively remodulates the most-wedged vertebra via a compressive force applied on convex side. While recent studies have reported the efficacy of the technique as a proof of concept, there is limited biomechanical data to understand the remodulation of the vertebra and its associated parameters. Designed as a modified SHILLA technique, the APC aims to overcome key complications with SHILLA: crank-shafting & adding-on. The current study builds on earlier clinical studies on the APC technique, aiming to quantify and understand the vertebral remodulation across 5 patient-specific FE models with simulated growth. Material and Methods: Five ligamentous, representative patient-specific models were developed from clinical radiographic data. These pre-op models were then used to simulate the APC intra-surgical processes. Finally, the effect of gravity forces and spinal growth were simulated. Parameters such as Cobb, AVT, vertebral wedging etc. were recorded for these models. To ensure clinical relevance, the model inputs and processes were confirmed with a surgeon. Results: The correction in the ratio of convex to concave-side vertebral height for the 3 vertebrae in the tethered area averaged at 2.25% compared to 0.5% in the control vertebrae. Data also showed excellent correction post-surgery; reduction of the primary curve was 45% (27 degrees), kyphosis reduced by 27% (7.1 degrees) and the AVT reduced by 46% (2.3 cm) on average. Additionally, at the 6-month follow-up, the same parameters indicated a maintenance of correction for all patient models. Conclusion: The results clearly indicate the correction of the vertebral wedging, with the correctional effect being transferred beyond the most-wedged vertebrae. This coupled with indications of maintained correction over the spinal growth augurs well for long-term outcomes for APC. While this study is limited in terms of follow-up time, it indicates the potential of this technique and paves the way for additional research.
1346
A060: Assessment of elasticity changes on abdominal compliance and spinal stability: a numerical spine model approach inclusive of intra-abdominal pressure
Ibrahim El Bojairami 1,2 and Mark Driscoll 1,2
1 Mechanical Engineering, McGill University, Montreal, Canada
2 Montreal General Hospital, McGill University Health Center, Canada
Introduction: Abdominal compliance ( ) is the measure of ease of abdominal expansion, to which high compliance indicates that the abdomen can expand relatively freely, while low compliance restricts abdominal expansion. This is known to influence abdominal intra-abdominal pressure which is believed to influence spinal stability. The global objective of the present work was to evaluate the effect of abdominal elasticity changes on and equilibrium spinal stability, using a fully validated and representative finite element (FE) spine model inclusive of an accurate fluid-structure intra-abdominal pressure (IAP) model. Material and Methods: The developed spine model comprised 273 spinal tissues, developed from MRI-scans, governing the thoracic and lumbar vertebrae, intervertebral discs (IVDs), spinal muscles, thoracolumbar fascia (TLF), and a fluid-filled pressurized model of the IAP. The overall biomechanical behavior of the model was previously validated against six different ex vivo, in vivo, and in situ investigations. In the present study, was evaluated using: , to which compliance results were first validated against. Based on collected physiological data, abdominal elasticity ( ) was varied between 10 to 60 kPa and IAP was activated between 1.5 and 30 mmHg. results were then collected, along spinal supportive abdominal and TLF forces ( and ) in efforts of assessing resultant spinal stability by means of spinal displacements ( ) from the equilibrium initial position. Results: Validation results against literature showed average discrepancies of 6.9% and 13.1% in , but with all simulated data points falling within reported standard deviations. Thereafter, the increase in led to a decrease in abdominal volumes, and thus an accompanied decrease in passive . On the other hand, this abdominal activation subjected the spine to and with average forces of 20-42.7N and 15.4-34.5N, respectively. Correspondingly, this decrease in active was accompanied with imposing spinal displacements , from the original position, increasing mean from 7.05 to 25.83 mm. Conclusion: The purpose of this study was to exploit and validate a representative FE spine model, inclusive of an abdominal representation, to evaluate the effect of physiological elasticity changes on abdominal compliance and equilibrium stability. Although validation results were in good agreement with reported data, variations were observed, which may be indicative of patient-to-patient physiological differences. Also, findings suggested that is inversely related to elasticity. The nonlinearities in results suggested that if there is a greater baseline volume, for the same applied IAP levels, the abdomen is unable to inflate as much as its smaller counterparts. Clinically, this may relate to obesity whereby thickening fat layers cause a stiffer abdomen, and thus yield dangerously low levels of passive . Conversely, a reduction in , related to active augmentation of abdominal elasticity, subjected the spine to high supportive and forces. Based on these results, individuals who show improved active abdominal compliance may further benefit from spinal stability effects as reported herein.
1038
A061: 'Smart' interbody cages for assessing fusion progression: a proof-of-concept
Vivek Ramakrishna 1,2,3 , Uphar Chamoli 2,4 , Subhas Mukhopadhyay 3 , Ashish Diwan 2,5 , and Gangadhara Prusty 1
1 School of Mechanical and Manufacturing Engineering, University of New South Wales, Kensington, Australia
2 Spine Labs, University of New South Wales, Sydney, St. George & Sutherland Clinical School, Kogarah, Australia
3 School of Engineering, Faculty of Engineering and Science, Macquarie University, Macquarie Park, Australia
4 School of Biomedical Engineering, Faculty of Engineering and IT, University of Technology, Sydney, Ultimo, Australia
5 Spine Service, Department of Orthopaedic Surgery, St. George Hospital Campus, Kogarah, Australia
Introduction: There are several complications associated with lumbar interbody fusion (LIF) surgery however, pseudarthrosis presents a multifaceted challenge in the postoperative management of the patient. Rates of pseudarthrosis at least one year after LIF surgery range from 3-20% in patients with healthy bone and 20-30% in patients with osteoporosis. Plain radiographs and fine-cut CT have high false positive rates and poor agreement between the two modalities. The aim of this study was to develop a proof-of-concept load-sensing interbody cage to determine whether it may be used to monitor fusion progression. Material and Methods: Amphenol P122 pressure sensors were bonded to printed circuit boards (PCBs), which connected to a microcontroller to convert and transmit the sensor outputs. The sensors were individually calibrated within their overload limits. A polyether ether ketone (PEEK) interbody cage was manufactured with CNC milling to fit the PCBs within. Silicone and poly (methyl methacrylate) (PMMA) were inserted in the graft regions to simulate early and full fusion. The load-sensing cage was loaded with distributed and eccentric loads up to 900N at 0.6mm/min between two pieces of synthetic bone with dimensions of lumbar vertebral bodies. A finite element analysis model was developed with identical conditions to the experimental setup. Results: Under maximum load, the anterior sensors recorded a 56-58% reduction in pressure in the full fusion state compared to early fusion. Lateral regions measured a 36-37% stress reduction while the central location reduced by 45%. The two graft states were similarly distinguishable by sensor-recorded pressure at lower loads. The experimental results generally fell within the range of the average and maximum values obtained from simulation. The sensors more effectively detected left and right eccentric loads compared to anterior and posterior. Further, the load-sensing cage was able to detect changes in endplate stiffness. Conclusion: The proof-of-concept load-sensing interbody cage is able to detect differences in fusion state, endplate stiffness, and loading conditions in this in vitro experimental setup. Future research should aim to improve the implantability of the device by reducing the number of sensors, improving durability, and optimising the sensing configuration.
770
A062: Vertebral bone quality score independently predicts proximal junctional kyphosis following adult spinal deformity surgery
Cathleen Kuo 1 , Mohamed Soliman 1,2 , Alexander Aguirre 1 , Nicco Ruggiero 1 , Marissa Kruk 1 , Asham Khan 1 , Moleca Ghannam 1 , Patrick Jowdy 1 , David Smolar 1 , John Pollina 1 , and Jeffrey Mullin 1
1 Neurosurgery, University at Buffalo, Buffalo, United States
2 Neurosurgery, Cairo University, Cairo, Egypt
Introduction: Proximal junctional kyphosis (PJK) can be a catastrophic complication associated adult spinal deformity (ASD) surgery. One mechanism of PJK is fracture of the upper instrumented vertebra or the level above, in which osteoporotic patients are at an increased risk. Recently, a novel magnetic resonance imaging (MRI)-based vertebral bone quality (VBQ) score has been shown to correlate with dual-energy x-ray absorptiometry (DEXA) T-score. This study aimed to investigate the ability of the VBQ score in predicting PJK in patients undergoing ASD correction. Material and Methods: A retrospective chart review identified patients older than 50 years of age who had received ASD surgery of five or more levels. Demographic, spinopelvic parameters, and procedural-related variables were collected. For each patient, VBQ score was calculated using preoperative T1-weighted MRI. PJK was defined as a change in proximal junctional angle of at least 10° between the immediate postoperative and final follow-up standing radiograph. Univariate analysis followed by multivariate logistic regression analysis were performed to determine the potential risk factors of PJK. Results: A total of 116 patients (40 males and 76 females) were included, with a mean age 64.1 ± 6.8 years and a mean follow-up of 25.6 ± 13.4 months. Among them, 34 patients (29.3%) developed PJK. The mean VBQ score for patients without PJK was 2.5 ± 0.5 and 3.1 ± 0.5 for patients with PJK, which was significantly different between the two groups (p < .001). On multivariate logistic regression, a higher VBQ score was significantly associated with an increased risk of PJK (OR = 1.745, 95% confidence interval = 1.558-1.953, p < .001) and was the only significant independent predictor of PJK after ASD surgery. Conclusion: In patients undergoing long-segment thoracolumbar spinal reconstruction, a higher VBQ score was independently associated with PJK. The measurement of VBQ score on preoperative MRI may be a useful adjunct to ASD surgery planning.
1054
A063: Computed tomography morphometric analysis for C1 lateral mass screw placement
Francisco Fasano 1 , Pablo Jalón 1 , Alfredo Guiroy 2 , and Sofia Beltrame 3
1 Neurosurgery, Hospital de Clínicas José de San Martín, Buenos Aires, Argentina
2 Orthopedics, Hospital Español, Mendoza, Argentina
3 Orthopedics, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina
Introduction: There is a significant interpersonal variability in the morphological aspects of the atlas, and given its proximity to neurovascular structures (vertebral artery, cervical medulla, C2 root), it is mandatory to make an exhaustive presurgical planning for the choice of the arthrodesis technique, type of screws to be used, and their trajectory; thus, reducing the possible complications inherent in the surgical procedure. Objectives: 1. Perform a morphometric analysis by computed tomography of the lateral masses of the atlas, determining the average, median, and variability values of said vertebra for the correct choice of the arthrodesis technique and dimensions of the screws to be used. 2. Taking as "entry point" the cephalo-caudal and latero-medial midpoint of the lower portion of the lateral masses, estimate the different possible trajectories based on latero-medial angulation in the axial plane and cephalo-caudal angulation in the sagittal plane. Material and Methods:Population.
Inclusion criteria.
Patients attended on an outpatient basis by the Neurosurgery and/or Diagnostic Imaging Services of the Hospital de Clínicas ´ ´José de San Martín ´ ´ during the period August 2021 – August 2022 who have had indication of the realization of a computed axial tomography of the cervical spine.
Exclusion criteria
1. Patients under 18 years of age.
2. Patients with a history of spinal surgery.
3. Patients with a history or findings of vertebral fractures, tumor, vascular or malformities pathology of the spine.
Elimination criteria
Patients whose computed axial tomography has been absent or misplaced.
Design: An exploratory, descriptive, observational, retrospective, cross-sectional design study was conducted. The present research protocol was carried out by reviewing CT scans of the cervical spine of those patients who meet the previously developed criteria. The measurements of the parameters to be studied were made with the Radiant DICOM Viewer program (64-bit) and later dumped into an Excel spreadsheet. Results: We reviewed 107 CT scans of the cervical spine, of which 8 had to be discarded according to the exclusion criteria (4 incomplete studies, 2 axis fractures, 1 gunshot wound, and 1 congenital bone malformation), leaving a total of 99 CT scans. The distribution by gender was 34 males and 65 females. The mean, median and standard deviation parameters were obtained for each variable analyzed. A statistically significant difference has been found not only in relation to the gender (male vs female) of the measured parameters (Parameters A, B, C, D, F, G, H p-value < 0.05), but also according to laterality (right vs left; Parameters C, E, F, G p-value < 0.05). Conclusion: There is significant variability in the morphological properties of the atlas, both in terms of gender (male vs female) and laterality (right vs left). That is why the present study emphasizes the importance of the presurgical realization of a computed tomography of the upper cervical spine to guarantee an effective and safe instrumentation at this level, according to the length, width, and trajectory of the screws to be used.
OP08: Cervical Arthroplasty
811
A064: Titanium trabecular 3D electron beam melting printed cervical cages to promote rapid healing in cervical fusion: from bench to bedside. A prospective study with over 2 years of follow-up
Nermine Habib 1 , Renato Gondar 1 , Daniele Valsecchi 1 , and Gianluca Maestretti 1
1 Unité Neuro Spinale, Service Orthopedie, HFR Université de Fribourg, Switzerland
Introduction: Anterior cervical discectomy and fusion (ACDF) is a widely implemented procedure in treating degenerative cervical disc disease. Porous trabecular titanium (PTT) has an open-cell metal structure with a low modulus of elasticity similar to human subchondral and cancellous bone leading to better load transfer and minimizing the stress-shielding phenomenon. In vitro studies on PTT cages, manufactured by the electron beam melting (EBM) technology, showed excellent results with the ability to trigger osteogenic differentiation. A great capacity for osteoinduction and bone regeneration is also suggested by the results of these in vitro studies. However, in vivo osteointegration and osteoinduction capabilities remain unknown. The aim is to determine the radiological fusion rate, as well as the clinical outcome associated with the use of titanium trabecular 3D EBM printed cervical cages. Material and Methods: We performed a prospective analysis of 16 consecutive patients with at least two years of clinical and/or radiological follow-up; suffering from degenerative cervical spine conditions and benefiting from one- to three-level ACDF. Specially designed 3D printed cages made of PTT and modelled by CAD/CAM technology by means of EBM (MT Ortho, Aci Sant' Antonio, Sicily, Italy) are implanted with or without an anterior plate support depending on the pre-operative findings and presence or absence of myelopathy. Bone grafts are avoided. Fusion rate, segmental height and alignment are assessed via computed tomography (CT) scan at three months. The visual analogue scale (VAS) pain score and Neck Disability Index (NDI) are recorded preoperatively and at 3 months, 6 months, 1 and 2 years postoperatively. Results: At over two years of follow-up (average 31 months), 2 of the 16 patients were lost to follow up. The CT-scan results at three months showed signs of bony growth through the cage in 87.5% of the patients. At two years, the average VAS pain score for axial pain and radicular pain was very low at 1 ± 3 and 1 ± 3. The average NDI score was 5/50. Subsidence or device failure was not observed. One patient required revision surgery for an epidural hematoma on the 3rd postoperative day, and another presented with facet joint degeneration in the adjacent level. Otherwise, no significant complications are documented. Conclusion: Special designed 3D EBM printed PTT cages give the bone matrix the possibility to adhere and grow in the cage in order to stabilize the implant rapidly. This faster bony ingrowth seems independent from the diagnosis or additional plating. The cells prove to early colonize the central cavity of the cage, improving the bone fusion confirming the data obtained by recent in vitro studies. Their clinical application in cervical arthrodesis appears to be safe and efficient.
1344
A065: 4-year outcomes in patients undergoing artificial disc replacement vs anterior cervical discectomy and fusion in Asian patients for one-level symptomatic cervical disc disease
Naresh Kumar 1 , Sirisha Madhu 1 , and Liang Shen 2
1 Orthopaedic Surgery
2 Medical Statistics, National University of Singapore, Singapore, Singapore
Objectives: The aim of our study was to evaluate the hypothesis that ProDisc-C may be non-inferior to ACDF in terms of clinical outcomes, with lower incidence of adjacent segment disease (ASD) at 48-months post-surgery in Asian patients with SCDD. Methods: This multicenter, prospective, randomized controlled trial was initiated in January-2008, after obtaining ethical approval at nine centres (in China/Hong Kong/Korea/Singapore/Taiwan). Patients with single-level SCDD involving C3-C7-vertebral segments were enrolled and randomized in 2:1 ratio into: group A treated with ProDisc–C and group B with ACDF. A protocol modification (January-2010) allowed patients with cervical myelopathy also to be included. Assessments were conducted at baseline, 6-weeks, 3/6/12/18/24-months post-surgery and annually thereafter out to 84-months. Primary endpoint was overall success, defined as the composite of: 1) improvement in neck disability index (NDI) by 20% from baseline; 2) maintained/improved neurologic parameters; 3) no implant removal/revision/re-operation/additional fixation at index-level; 4) no adverse events related to implant/surgery and no severe/life-threatening events. Secondary endpoints included: 1) incidence of ASD at 24-months; 2) individual endpoints of primary outcome; 3) outcomes of short-form survey (SF-36), visual analogue scale (VAS) score(neck/arm-pain intensity/frequency; patient’ satisfaction); 4) radiological parameters [range of motion(ROM)]. Results: Of the 120 enrolled/treated patients (80 ProDisc-C, 40 ACDF), 76 with ProDisc-C and 37 with ACDF were treated as per protocol (PP). Overall success [PP, last observation carried forward (LOCF)] was 79% in group-A and 83.8% in group-B at 24-months (p = 0.10). ProDisc-C demonstrated non-inferiority to ACDF at 18-months (81.6% versus 83.8%, p = 0.0398) with borderline non-inferiority at 3-months (76.3% versus 78.4%, p = 0.054). In intent-to-treat-LOCF analysis, overall success at 24-months was 78.2% with ProDisc-C and 81.6% with ACDF (p = 0.06). ProDisc-C demonstrated non-inferiority to ACDF at both 3-months (75.6% versus 76.3%, p = 0.0396) and 18-months (80.8% versus 81.6%, p = 0.0284). Secondary outcomes improved after 24-months for both groups with no significant differences between groups for percentage change from baseline. Occurrence of ASD was higher in ACDF versus ProDisc-C, with no statistical significance. The ROM was sustained with ProDisc-C at 24-months when compared to preoperative ROM. Whilst, loss of ROM was noted in group-B. Conclusions: Cervical TDR with ProDisc-C is feasible, safe, and effective for treatment of SCDD in Asians. ProDisc-C was non-inferior to ACDF at 3 and 18 months after index-surgery with no clear non-inferiority at 24-months. Patients treated with ProDisc-C demonstrated significant improvement in terms of NDI, neurologic success, VAS-pain scores, and SF-36, along with preservation of ROM at 24-months post-surgery. Incidence of ASD was comparable between the two groups at 24-months.
Keywords: Anterior cervical discectomy and fusion; Total disc replacement; ProDisc-C; Randomized controlled trial; Cervical disc disease; Degenerative disc disease; Asians
1663
A066: Fatty infiltration into cervical paraspinal muscle undergoing hybrid surgery and its relationship with cross-sectional area
Junbo He 1 , Tingkui Wu 1 , Beiyu Wang 1 , and Hao Liu 1
1 Orthopedic Surgery, West China Hospital, Sichuan University, Chengdu, China
Introduction: The cervical paraspinal muscle (CPM) has an essential role in positioning, stabilizing and directing the cervical spine. However, information is lacking regarding the influence of CPM on outcomes following anterior cervical surgery. This study aims to evaluate the association of fatty infiltration (FI) of CPM with postoperative outcomes in patients undergoing hybrid surgery (HS) and analyze the relationship between FI and cross-sectional area (CSA) of CPM. Material and Methods: A retrospective analysis was performed on 110 consecutive patients undergoing continuous 2-level HS. According to Goutallier classification of multifidus FI, the patients were divided into normal, moderate, and severe groups. Image J software was employed to outline and analyze CPM. Clinical outcomes and radiographic parameters were collected and evaluated for relevant comparisons. Results: Visible FI was identified in 69.1% of patients (76/110), with a propensity in elderly patients (p = 0.053). No statistically significant differences were presented among the three groups regarding pre- and postoperative clinical evaluation scores. The cervical lordosis was significantly higher in the normal group before surgery (p = 0.029). Likewise, the sagittal vertical axis (SVA) was significantly higher in the severe group than the normal group at the final follow-up (p = 0.046). The function spine unit angle and disc angle of arthroplasty levels were significantly lower in the severe group than the normal group at follow-ups. Moreover, after correction according to vertebral body area, no statistically significant relationship existed between CSA ratio and FI grade. Conclusion: CPM degeneration is common and age-related in patients with cervical disc degenerative disease. More importantly, there was a significant positive correlation between severe FI of CPM and postoperative sagittal balance disorder, particularly in C2-7 SVA and segmental alignment of arthroplasty level. Meanwhile, FI of CPM appears to have no impact on clinical outcomes and reveals small correlations to CSA.
791
A067: The influence of the degree of preoperative cervical degeneration on the formation of heterotopic ossification following cervical disc replacement
Yi-Wei Shen 1 and Hao Liu 1
1 Department of Orthopedics, Orthopedic Research Institute, West China Hospital, Sichuan University, Department of Orthopedics, Chengdu, China
Introduction: The occurrence of heterotopic ossification (HO) is an intractable issue after cervical disc replacement (CDR) because it may decrease the motion of index level and even develop to complete intervertebral fusion, which is against the design philosophy of disc replacement with motion-preserving. Preoperative cervical degenerative is considered one of the contributors to HO formation after CDR. This study aimed to explore the influence of the degree of preoperative cervical degeneration on HO formation in different locations after CDR. Material and Methods: The degree of preoperative cervical degeneration was evaluated on radiographs and computed tomography (CT), including the intervertebral disc, uncovertebral joints, facet joints, and ligaments. The effects of preoperative cervical degeneration on the HO formation after CDR were analyzed according to the location of HO. Multivariate logistic regression was performed to identify the independent factors. Results: 149 patients with a total of 196 arthroplasty segments were involved in this study. HO, anterior HO (AHO), and posterior HO (PHO) developed in 59.69%, 22.96%, and 41.84% levels, respectively. The significant factors in univariate analysis for PHO after CDR included disc height loss, anterior osteophytes, preoperative uncovertebral joint osteophytes, and facet joint degeneration. The incidence of adjacent segment degeneration (ASD) was significantly higher in the PHO group compared to that without PHO at the last follow-up (p = 0.003). The disc height loss in the high-grade HO was significantly more than that in the low-grade group (p = 0.039). Multivariate analysis identified disc height loss as the only independent factor for PHO (p = 0.009). No significant degenerative factors related to the formation of AHO were found. Conclusion: Preoperative cervical degeneration predominantly affected the HO formation in the posterior disc space after CDR. The disc height loss was an independent risk factor for PHO formation. Rigorous criteria for the extent of preoperative disc height loss should be used when selecting appropriate candidates for CDR.
124
A068: Operative treatment outcomes for adult cervical deformity: a prospective multicenter assessment with mean 3-year follow up
Elias Elias 1 , Shay Bess 2 , Breton Line 3 , Virginie Lafage 4 , Renaud Lafage 5 , Eric Klineberg 6 , Han Jo Kim 5 , Peter Passias 7 , Zeina Nasser 8 , Jeffrey Gum 9 , Khaled Kebaish 10 , Robert Eastlack 11 , Alan Daniels 12 , Gregory Mundis 11 , Richard Hostin 13 , Themistocles Protopsaltis 7 , Alex Soroceanu 14 , Kojo Hamilton 15 , Michael Kelly 16 , Munish Gupta 17 , Robert Hart 18 , Frank Schwab 4 , Douglas Burton 19 , Christopher Ames 20 , Christopher Shaffrey 21 , and Justin Smith 22
1 Neurosurgery, University of Texas Southwestern, Dallas, United States
2 Denver International Spine Center/Presbyterian St. Luke's Medical Center, Denver, United States
3 Presbyterian St Lukes Medical Center, Denver, United States
4 Department of Orthopedic Surgery, Lennox Hill Hospital, New York, United States
5 Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, United States
6 Department of Orthopaedic Surgery, University of California, Davis, Sacramento, United States
7 Department of Orthopaedic Surgery, NYU Hospital for Joint Diseases, New York, United States
8 Neuroscience Research Center, Faculty of Medical Sciences, Lebanese University, Hadath, Beirut, Lebanon
9 Leatherman Spine Center, Louisville, United States
10 Department of Orthopedic Surgery, Johns Hopkins Hospital, Baltimore, United States
11 Scripps Clinic, San Diego, United States
12 Department of Orthopedic Surgery, Brown University, Providence, United States
13 Department of Orthopaedic Surgery, Baylor Scoliosis CenterPlano, United States
14 Department of Orthopedic Surgery, University of Calgary, Alberta, Canada
15 Department of Neurosurgery, University of Pittsburgh, Pittsburgh, United States
16 Department of Orthopedic Surgery, Rady Children’s Hospital, San Diego, United States
17 Department of Orthopedic Surgery, Washington University, St. Louis, United States
18 Department of Orthopaedic Surgery, Swedish Medical Center, Seattle, United States
19 Department of Orthopaedic Surgery, University of Kansas Medical Center, Kansas, United States
20 Department of Neurological Surgery, University of California, San Fransisco, United States
21 Departments of Neurosurgery and Orthopedic Surgery, Duke University, Durham, United States
22 University of Virginia, Neurosurgery, Charlottesville, United States
Introduction: Adult cervical deformity (ACD) has high complication rates due to surgical complexity and patient frailty. Very few studies have focused on longer-term outcomes of operative ACD treatment. The objective of this study was to assess minimum 2-year outcomes and complications of ACD surgery. Material and Methods: A multicenter, prospective observational study was performed at 13 centers across the United States to evaluate surgical outcomes for ACD. Demographics, complications, radiographic parameters, and patient-reported outcome measures (PROMs; Neck Disability Index, modified Japanese Orthopaedic Association, EuroQol-5D [EQ-5D], and numeric rating scale [NRS] for neck and back pain) were evaluated, and analyses focused on patients with ≥2-year follow-up. Results: Of 169 patients with ACD who were eligible for the study, 102 (60.4%) had a minimum 2-year follow-up (mean 3.4 years, range 2-8.1 years). The mean age at surgery was 62 years (SD 11 years). Surgical approaches included anterior-only (22.8%), posterior-only (39.6%), and combined (37.6%). PROMs significantly improved from baseline to last follow-up, including Neck Disability Index (from 47.3 to 33.0) and modified Japanese Orthopaedic Association score (from 12.0 to 12.8; for patients with baseline score ≤ 14), neck pain NRS (from 6.8 to 3.8), back pain NRS (from 5.5 to 4.8), EQ-5D score (from 0.74 to 0.78), and EQ-5D visual analog scale score (from 59.5 to 66.6) (all p ≤ 0.04). More than half of the patients (n = 58, 56.9%) had at least one complication, with the most common complications including dys-phagia, distal junctional kyphosis, instrumentation failure, and cardiopulmonary events. The patients who did not achieve 2-year follow-up (n = 67) were similar to study patients based on baseline demographics, comorbidities, and PROMs. Over the course of follow-up, 23 of the total 169 enrolled patients were reported to have died. Notably, these represent all-cause mortalities during the course of follow-up. Conclusion: This multicenter, prospective analysis demonstrates that operative treatment for ACD provides sig-nificant improvement of health-related quality of life at a mean 3.4-year follow-up, despite high complication rates and a high rate of all-cause mortality that is reflective of the overall frailty of this patient population. To the authors’ knowledge, this study represents the largest and most comprehensive prospective effort to date designed to assess the intermedi-ate-term outcomes and complications of operative treatment for ACD.
752
A069: Characterizing the effect of surgical approach and the success of deformity correction on the perioperative quality of swallowing in patients undergoing corrective surgery for cervical deformity
Peter Passias 1 , Tyler Williamson 1 , Bailey Imbo 1 , Pooja Dave 1 , Rachel Joujon-Roche 1 , Stephane owusu-saprong 1 , Jordan Lebovic 1 , Kimberly McFarland 1 , Jamshaid Mir 1 , and Shaleen Vira 2
1 NYU Langone Medical Center, New York, United States
2 UT Southwestern, Dallas, United States
Clinical Relevance: There remains a paucity of literature evaluating the perioperative quality of swallowing among the various approaches to the cervical spine, as well as the success of cervical deformity (ACD) correction. Purpose: Determine the impact of surgical approach and deformity correction on quality of swallowing following ACD surgery. Study Design: Retrospective cohort. Methods: ACD patients with three-month (3M) data were included. Dysphagia was defined as any complication related to patient-reported difficulty swallowing, that required: evaluation from a speech language pathologist and/or otolaryngologist and lengthened hospital stay. Clinical deterioration was defined as scoring an MCID of 8 points higher in SWAL-QOL by 3M. Patients were stratified based on surgical approach. Univariate analysis assessed patient characteristics, dysphagia rates, SWAL-QOL scores/improvement at baseline and 3M. ANCOVA and multivariable regression analysis controlling for age, gender, levels fused, baseline deformity (cSVA and TS-CL) and delayed extubation, evaluated the groups based on the 3M difference in SWAL-QOL scores, along with correlation with radiographic improvement. Results: 219 ACD patients included. By surgical approach, 26% anterior-only, 35% posterior-only, and 36% combined. Patients with delayed extubation were more likely to develop dysphagia and require evaluation (OR: 4.7, 95% CI [1.9-11.7]; p < .001). A total of 22 patients (10.0%) reported dysphagia postoperatively (3 anterior, 1 posterior, 18 combined; p < .001). Patients developing dysphagia also had higher operative times and more superior upper-instrumented vertebra (UIV), although levels fused and EBL was not different. Adjusted analysis revealed patients undergoing a combined approach were still more likely to develop dysphagia than either posterior or anterior approaches. However, timing to resolution of dysphagia was shortest for patients undergoing a combined procedure (7.9 days vs. average of 14.9 days). When examining patients with low and high SWAL-QOL scores at three months, cSVA, C2-T3, and C2-slope showed significant differences between groups. Correlation between improvement in McGregor’s slope and the Fear Swallow domain, as well as TS-CL and Mental and Fatigue domains. Binary logistic regression analysis revealed the Burden domain was correlated with improvement in 5 of the 6 radiographic parameters analyzed (C2-slope, cSVA, C2-C7 Lordosis, MGS, and TS-CL). Conclusion: The combined anterior-posterior approach was associated with higher rates of dysphagia, but much faster recovery (7.9 days on average) compared to the dysphagia reported in anterior and posterior approaches. Preliminary data suggests more successful deformity correction, using improved radiographic markers as a surrogate, may be associated with improved quality of perioperative swallowing.
1867
A070: Cranio-cervical decompression associated with non-instrumented occipito-C2 fusion in children with mucopolysaccharidosis
Nessrine Nessib 1 , Mohamed Zairi 2 , Sliti Firas 1 , Sofiene Bouali 1 , Ahmed Msakni 2 , Mohsni Ahmed Amine 2 , Rim Boussetta 2 , and NESSIB Mohamed Nabil 2
1 Neurosurgery, Mongi ben Hamida Institute of Neurology, Tunis, Tunisia
2 Orthopedics, Bechir Hamza Children's Hospital, Tunis, Tunisia
Introduction: Mucopolysaccharidosis (MPS) is a multisystemic storage disorder of glycosaminoglycan deposits. Infiltration of the dura mater and supporting ligaments caused spinal cord compression and consecutive myelopathy, predominantly at the cranio-cervical junction (CCJ). Craniocervical instability and posterior decompression often poses the problem of fixation in children. The main purpose of this work was to present the result of an original technique of occipito-cervical arthrodesis using halo-cast system in pediatric population. Materials and Methods: 21 patients with cervical myelopathy. All patients had spinal cord decompression by enlargement of foramen magnum and C1 laminectomy, and occipito-C2 fusion by corticocancellous bone. Only one child had an extended laminectomy from C1 to C3. The occipito-C2 arthrodesis is stabilized by the halo-cast system. This immobilisation was performed preoperatively and kept for three months then switched to minerva. Clinical evaluations, including the Goel grade and mJOA. Radiographs and magnetic resonance imaging were performed before surgery. The occipito-cervical arthrodesis is controlled by standard X-rays and CT scan. Results: According to the type of mucoplosaccharidosis, the patients were divided into MPS type I n = 3, II: n = 7, IV: n = 11. The mean age of patients at surgery was 6.76 years. All mucopolysaccharidoses cases required a foramen magnum decompression by craniectomy, C1 laminectomy and occipito-C2 arthrodesis. As major complications, a child had immediate post-operative paraplegia due to spinal cord ischemia. The postoperative follow-up ranged from 1.5 to 4 years, with an average of 3.3 years. The average preoperative mJOA score was 8.9, and it improved to 14 points at the most recent follow-up. Conclusions: Satisfactory fusion and good clinical results were obtained with the 2-stage approach to CCJ anomalies.
584
A071: A 5-year cost-utility analysis comparing synthetic cage vs allograft use in anterior cervical discectomy and fusion surgery for cervical spondylotic myelopathy
Micheal Raad 1 , Amy Xu 1 , Carlos Ortiz-Babilonia 1 , Majd Marrache 1 , Welsey Durand 1 , Marc Greenberg 1 , and Amit Jain 1
1 Orthopedic Surgery, Johns Hopkins Hospital, Baltimore, MD, United States
Introduction: Synthetic cage (SC) and allograft (Allo) are two commonly used interbody choices for anterior cervical discectomy and fusion (ACDF) surgery. Previous comparative analyses have reached mixed conclusions regarding their cost-effectiveness. In recent years, several large database studies comparing outcomes between the two techniques have suggested a higher revision rate with SC and may provide estimates for an improved and updated cost-utility analysis. The purpose of this study was to conduct a cost-analysis comparing SC vs. Allo over a five-year time horizon. Material and Methods: A decision-analysis model comparing the use of Allo vs SC was developed for a hypothetical 60-year-old patient with cervical spondylotic myelopathy (CSM) undergoing single-level ACDF surgery. A comprehensive literature review was performed to estimate probabilities, costs (2020 USD) and Quality-Adjusted Life Years (QALYs) gained over a 5-year period. A probabilistic sensitivity analysis using a Monte Carlo Simulation of 10,000 patients was carried out to calculate incremental cost effectiveness ratio (ICER) and net monetary benefits (INMB). One-way deterministic sensitivity analysis was performed to estimate the contribution of individual parameters to uncertainty in the model. Results: The use of Allo was favored in 81.6% of the iterations at a societal willing-to-pay threshold (WTP) of 50,000 USD/QALY. Allo dominated (higher net QALYs and lower net costs) in 67.8% of the iterations. The INMB in the Allo group was 2,650 USD at a WTP threshold of 50,000 USD/QALY. The average cost per QALY gained was 75,110 USD/QALY and 83,400 USD/QALY in the Allo and SC groups respectively. Based on the simulation results, the mean cost was 24,800 USD (SD = 1,960) in the Allo group and 27,380 USD (SD = 2,210) in the SC group. Mean effectiveness was 0.33 QALYs gained (SD = 0.03) for Allo and 0.33 QALYs (SD = 0.03) for SC. One-way deterministic sensitivity analysis revealed that the cost of the index surgery was the only factor which significantly contributed to uncertainty and result in significant ICER changes. Conclusion: The present study utilizes a Monte Carlo simulation with robust probabilistic sensitivity analysis and suggests that Allo is a more cost-effective interbody option for ACDF surgery over a 5-year time horizon. Our analysis suggests that this is a result of lower costs and slightly higher QALYs seen in the Allo group. The additional cost for SC is substantial and may be amplified for number of levels fused. Thus, while SC is widely used, it is cost-ineffective with higher monetary costs without providing additional benefit. Future research should continue to assess drivers of cost variability in spine surgery to identify potential targets for the reduction of healthcare expenditure.
780
A072: A novel Cervical Vertebral Bone Quality (C-VBQ) score independently predicts cage subsidence following anterior cervical discectomy and fusion
Mohamed Soliman 1,2 , Alexander Aguirre 2 , Cathleen Kuo 2 , Nicco Ruggiero 2 , Shady Azmy 2 , Asham Khan 2 , Moleca Ghannam 2 , Patrick Jowdy 2 , Jeffrey Mullin 2 , and John Pollina 2
1 Neurosurgery, Cairo University, Cairo, Egypt
2 Neurosurgery, University at Buffalo, Buffalo, United States
Introduction: Surgeons can preoperatively assess bone quality using dual-energy X-ray absorptiometry or computerized tomography (CT), however, this is not feasible for all patients. Recently, a magnetic resonance imaging (MRI)-based scoring system was used to evaluate the lumbar spine's vertebral bone quality (VBQ). We aimed to create a similar scoring system for the cervical spine (C-VBQ), correlate C-VBQ to CT-Hounsfield units (CT-HU), and evaluate the utility of this scoring system to independently predict cage subsidence following anterior cervical discectomy and fusion (ACDF). Material and Methods: Demographic, procedure-related, and radiographic data were collected for study patients. Pearson correlation test was utilized to determine the correlation between C-VBQ and CT-HU. Cage subsidence was defined as ≥ 3 mm loss of fusion segmental height. A multivariate logistic regression model was built to determine the correlation between potential risk factors for subsidence.Results: Among 59 patients undergone single-level ACDF, subsidence was found in 17 (28.8%) patients. The mean C-VBQ score for no subsidence levels was 2.22 ± 0.36 and for subsidence levels was 2.83 ± 0.38 (p < .001). On multivariate analysis, a higher C-VBQ score was significantly associated with subsidence (odds ratio = 1.85, 95% confidence interval = 1.39-2.46, p < .001) and was the only significant independent predictor of subsidence after ACDF. There was significant negative correlation between CT-HU and C-VBQ (r2 = -0.49, p < .001). Conclusion: We found that a higher C-VBQ score was significantly associated with cage subsidence following ACDF. Furthermore, there was significant negative correlation between C-VBQ and CT-HU. The C-VBQ score may be a valuable tool for assessing preoperative bone quality and independently predicting cage subsidence following ACDF.
OP09: Surgical Techniques for the Lumbar Spine
1812
A073: Adding sacral anchors through S1 alar screw and multi-rod construct as a strategy for lumbosacral junction augmentation
Aixing Pan 1 , Yong Hai 1 , and Yuzeng Liu 1
1 Orthopedic, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: Achieving solid fusion of the lumbosacral junction continues to be a challenge in long-segment instrumentation to the sacrum. The purpose of this study was to test the condition of adding sacral anchors through an S1 alar screw (S1AS) and multirod construct relative to using S1 pedicle screws (S1PSs) alone with sacroiliac fixation in lumbosacral junction augmentation. Material and Methods: Seven fresh-frozen human lumbar-pelvic spine cadaveric specimens were tested under nondestructive moments (7.5 Nm). The ranges of motion (ROMs) in extension, flexion, left and right lateral bending (LB), and axial rotation (AR) of instrumented segments (L3-S1); the lumbosacral region (L5-S1); and the adjacent segment (L2-3) were measured, and the axial construct stiffness (ACS) was recorded. The testing conditions were 1) intact; 2) bilateral pedicle screw (BPS) fixation at L3-S1 (S1PS alone); 3) BPS and unilateral S2 alar iliac screw (U-S2AIS) fixation; 4) BPS and unilateral S1AS (U-S1AS) fixation; 5) BPS and bilateral S2AIS (B-S2AIS) fixation; and 6) BPS and bilateral S1AS (B-S1AS) fixation. Accessory rods were used in testing conditions 3-6. Results: In all directions, the ROMs of L5-S1 and L3-S1 were significantly reduced in B-S1AS and B-S2AIS conditions, compared with intact and S1PS alone. There was no significant difference in reduction of the ROMs of L5-S1 between B-S1ASs and B-S2AISs. Greater decreased ROMs of L3-S1 in extension and AR were detected with B-S2AISs than with B-S1ASs. Both B-S1ASs and B-S2AISs significantly increased the ACS compared with S1PSs alone. The ACS of B-S2AISs was significantly greater than that of B-S1ASs, but with greater increased ROMs of L2-3 in extension. Conclusion: Adding sacral anchors through S1ASs and a multirod construct was as effective as sacropelvic fixation in lumbosacral junction augmentation. The ACS was less than the sacropelvic fixation but with lower ROMs of the adjacent segment. The biomechanical effects of using S1ASs in the control of long-instrumented segments were moderate (better than S1PSs alone but worse than sacropelvic fixation). This strategy is appropriate for patients requiring advanced lumbosacral fixation, and the risk of sacroiliac joint violation can be avoided.
878
A074: Influence of multi-level trans foraminal lumbar interbody fusion on spino-pelvic parameters and clinical outcome in degenerative lumbar disc diseases
Dr Sajan Hegde 1 , Sharan Achar T 1 , Vigneshwara Badikkilaya 1 , and Umesh Kanade P 1
1 Orthopaedics, Apollo Hospitals Chennai India, Chennai, India
Introduction: Trans Foraminal Lumbar Interbody Fusion (TLIF) is the gold standard procedure for Degenerative lumbar disc diseases. Restoration of lumbar lordosis, thus improving the sagittal balance is of paramount importance for Health related quality of life (HrQOL) after multilevel TLIF because it improves fusion rate, reduces the rate of adjacent segment disease and incidence of persistent low back pain. Existing literature reported good functional outcomes with 1 or 2 level TLIFs. With anecdotal evidence of poor outcome, there is evident dearth in clinical data specifically on the change of spinal alignment, its effect on spino-pelvic parameters and its clinical significance with 3 or more level TLIF. The objective of this study is to investigate the clinical and radiological outcomes of multi-level (3 or more) TLIF in degenerative lumbar canal stenosis (LCS) patients. Materials and Methods: Single center, retrospective observational study with minimum 2-year follow up. 27 patients who underwent Multi-level TLIF were retrospectively reviewed. Standing x-rays were assessed for changes in lumbar lordosis and segmental lordosis, improvement in pelvic parameters, global sagittal and coronal balance improvement. Fusion was assessed in serial follow up period based on Bridwell grading. Clinical assessment parameters included Visual Analog Score (VAS), Oswestry Disability Index (ODI) and Short Form 36 (SF-36). Statistical analysis was done using SPSS for Windows Version 22.0. Results: The average age of the patients were 42yrs (27 to 71). The mean follow up was 25.1 months (2-4 years). Among the 27 patients, 7 had 4 level, 20 had 3 level TLIF surgeries. Lumbar lordosis improved from 20.5˚ ± 4.6° to post-operative 42.1˚ ± 6.4°. Disc height and segmental lordosis at fusion levels significantly increased post operatively (p < 0.05 and p < 0.001). Pelvic tilt was significantly reduced (p < 0.01) post op with improved global sagittal balance (p = 0.07). ODI scores improved from 48.9 to 35.4 (27.5%) (p < 0.001). SF36 scales also had significant improved in all scales except role emotional scores. 1 case each had post operative foot drop, cage back out but not necessitating revision surgery and 1 case of significant persistant chronic back pain. Conclusion: Multi-level TLIF for Lumbar Degenerative Disc disease with proper patient selection and precise technique can provide significant improvement in ODI by improving the segmental spinal and pelvic balance.
167
A075: Five-year outcomes of cortical bone trajectory screws versus traditional pedicle screws in patients with single-level lumbar degenerative spondylolisthesis
Kwon Ji Won 1 , Yung Park 2 , Byung Ho Lee 2 , Si Young Park 2 , Jae Ho Yang 2 , Joong-Won Ha 1 , Kyung-Soo Suk 2 , Seong-Hwan Moon 2 , Hak-Sun Kim 2 , and Yong Ho Lee 1,3
1 Department of Orthopedic Surgery, Yonsei University College of Medicine, Seoul, South Korea
2 National Health Insurance Service Ilsan Hospital, Department of Orthopedic Surgery, Goyang, South Korea
3 Department of Orthopedic Surgery, Yonsei Baro Chuk Hospital, Seoul, South Korea
Introduction: Few studies have compared 5-year follow-up outcomes between CBT screws and TP screws in TLIF. This study investigated the clinical and radiological results of using cortical bone trajectory (CBT) screws versus traditional pedicle (TP) screws in transforaminal lumbar interbody fusion (TLIF) during a 5-year follow-up of patients with single-level lumbar degenerative spondylolisthesis. Material and Methods: We reviewed outcome data of patients with single-level lumbar degenerative spondylolisthesis who underwent TLIF procedures with CBT screws (131 patients) or TP screws (80 patients) between 2011 and 2015. Patient-reported clinical outcome data included Oswestry Disability Index (ODI) scores and visual analog scale (VAS) scores for back and leg pain at baseline, 6 months, and 1 year, 2 years, and 5 years postoperatively. The radiographic fusion rate and prevalence of secondary surgery for adjacent segment disease were also measured. Results: During the follow-up over 5 years, the CBT group had significantly lower VAS scores for back pain (p < .0001, respectively). At 2 years after surgery, the CBT group had significantly higher VAS scores for leg pain (p = .007). At 5 years postoperatively, no significant differences existed in the VAS score for leg pain or in the ODI score between the two groups. Radiographic fusion rates (CBT vs. TP: 95.5% vs. 95.9%; p = 0.881) and adverse events during the 5 years after surgery were not significantly different. At 2 years postoperatively, the prevalence of secondary surgery to treat adjacent segment disease was significantly different between the two groups (CBT vs. TP: 13.7% vs. 5.0%; p = 0.044). Conclusion: Our results suggest that, during a 5-year follow-up, CBT screws for TLIF were an effective treatment, compared to TP screws, for patients with single-level lumbar degenerative spondylolisthesis. However, when performing CBT screws for TLIF, surgeons should consider a symptomatic adjacent segment disease requiring surgery.
1440
A076: Mini-incision oblique lumbar interbody fusion (OLIF) and anterolateral screws rod fixation for surgical treatment of lumbar spine spondylolisthesis
YuTong Gu 1
1 Orthopedic Surgery, Zhongshan Hospital Fudan University, Shanghai, China
Introduction: Compared with PLIF or TLIF, OLIF has some advantages including less trauma, less blood loss, faster recovery and bigger cage with better distraction ability, better reduction of spondylolisthesis and higher fusion rate. And OLIF has the efficacy of indirect neurologic decompression. However, OLIF usually needs posterior screws fixation for biomechanical stability, which sharply reduces the advantages of OLIF due to longer operative time under general anesthesia and more invasiveness. Additionally, OLIF of L5/S1 is generally performed through the approach between bilateral iliac vessels and some patients are not suitable for OLIF of L5/S1 because the entrance is obstructed by the great vessels. In this study, mini-incision OLIF and anterolateral screws rod fixation through the corridor between the great vessel or iliac vessels and psoas major muscle were used to treat lumbar spine spondylolisthesis including L5. The purpose is to evaluate the feasibility, efficacy and safety of this method. Materials and Methods: 29 cases of 1-level, 2-level or 3-level lumbar spondylolisthesis (L2-L5) (Meyerding[16] I° or II°) were included in this study. The patients underwent OLIF for L2/3, L3/4, L4/5 or L5/S1 in a right lateral position under general anesthesia. Through mini-incision, the OLIF25 cage is placed into the intervertebral space including L5/S1 through the corridor between the great vessel or iliac vessels and psoas major muscle. Then, the pedicle screws are inserted into adjacent vertebrae from the anterolateral side close to the endplate with one screw for one vertebra, and the rod is fixed over the screws. If the neurologic symptoms are not relieved, second-stage percutaneous transforaminal endoscopic surgery (PTES) is used to treat the neurologic compression. Back and leg pain VAS, ODI, radiologic paraments and complications are recorded. Results: There were 26 cases of 1-level lumbar spondylolisthesis, 2 cases of 2-level and 1 case of 3-level. The mean operative duration was 76.2 (65-150) minutes. The mean frequency of intraoperative fluoroscopy was 7 (5-15) times. There was a mean blood loss of 25 (10-80) ml, and the average incision length was 39.6 ± 3.1 mm. The mean drainage removal was 2 (1-3) days and the mean hospital stay was 4 (3-6) days. The average follow-up duration was 33 (24-45) months. For the clinical evaluation, the VAS pain index of back and leg, the ODI showed excellent outcomes after surgery. No second-stage PTES was needed. The intervertebral space height, lumbar lordotic angle and operative segmental lordotic angle significantly improved postoperatively, and no significant difference change was observed during the follow-up. Fusion grades based on the Bridwell grading system at 2-year follow-up were grade I in 22 segments (66.7%, 22/33), grade II in 11segments (33.3%, 11/33). No patients had any form of permanent iatrogenic nerve damage and a major complication. No failure of instruments was observed. Conclusion: Mini-incision OLIF and anterolateral screws rod fixation is a good choice of minimally invasive surgery for lumbar spine spondylolisthesis including L5, which can get easy reduction, rigid fixation and good fusion, indirect neurologic decompression and hardly destroy the paraspinal muscles and bone structures.
1727
A077: OLIF is less invasive compared to TLIF - a matched case-control study on 1-, 2-level lumbar fusions
Aron Lazary 1 , Kristof Koch 1 , László Horváth 2 , Marton Ronai 1 , and Zoltan Hoffer 1
1 Buda Health Center, National Center for Spinal Disorders, Budapest, Hungary
2 Faculty of Medicine, Semmelweis University, Budapest, Hungary
Introduction: Oblique lumbar interbody fusion (OLIF) is a safe and effective anterior approach alternative of posterior fusion procedures, especially at the L2-5 levels. Beyond their mechanical advantages, anterior procedures are often called as less invasive fusions but only few studies are found in the literature publishing comparative analysis of complications. The goal of this study is to compare the complication pattern of homogenous OLIF and TLIF cohorts operated because of lumbar degenerative disorders. Materials and Methods: Intra- and postoperative clinical data of 67 patients operated with 1- or 2-level OLIF and matched cohort of 201 1-, 2-level TLIF subjects were analyzed. All patients were operated in the same institution because of a lumbar degenreative pathology. Perioperative parameters and all types of complications appeared within 40 days after discharge were collected systematically. ANOVA and chi-square tests were applied and p < 0.05 was conisdered as significant difference between OLIF and TLIF groups. Results: Mean age in both cohorts was 65.9y. Male/female ratio as well as distribution of surgeries were same in both cohorts (30% males, 78% single-level surgeries). Overall complication rate was significantly lower in OLIF cohort (19% vs 33%). Most of the complications were minor ones but length of hospital stay and ICU time were longer in TLIF cohort (LOS: 6.9 vs. 6.1 days, ICU: 1.9 vs 1 days, p < 0.05). Intraoperative blood loss was lower in the OLIF cohort (180 ml vs 383ml, p < 0.05) despite the longer surgeries (180 min vs 130 min, p < 0.05). In the OLIF cohort, none of the procedure-specific major complications of OLIF (vessel-, ureter-, bowel injury) was appeared despite the fact that patients operated during our learning curve were not excluded from the analysis. Early readmission because of need for a reoperation was also less common in OLIF cohort (1.5% vs 3.5%, p < 0.05). Conclusions: 1-, 2-level OLIF surgeries are characterized with a lower complication rate compared to TLIF procedures in a general lumbar degenerative cohort. OLIF is less invasive also demonstrated by shorter ICU and LOS as well as less blood loss and lower early reoperation rate.
288
A078: Are osteopenia and sarcopenia risk factors for surgical site infection after posterior lumbar fusion? A retrospective study
Marco Manzetti 1 , Francesca Barile 1 , tosca cerasoli 1 , Giovanni Viroli 1 , Marco Ialuna 1 , matteo traversari 1 , alberto rinaldi 1 , fabio vita 1 , Alberto Ruffilli 1 , and Cesare Faldini 1
1 Clinica Ortopedica e Traumatologica I, IRCCS - Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Surgical Site Infection (SSI) following spine surgery leads to significant patient morbidity and increased health care costs. For this reason, interest has grown in identifying associated risk factors. Among them, sarcopenia and osteopenia have recently been attracting a lot of interest. Central sarcopenia, defined as a “syndrome of progressive and generalized loss of muscle mass and strength”, is related to higher complication rates, longer length of stay, higher perioperative morbidity and mortality in both spinal and prosthetic surgery. Osteopenia, defined as decreased bone mineral density and bone mass, is associated with vertebral fractures and postoperative mechanical complications. To the best of the Authors’ knowledge, there are currently no studies that correlate both sarcopenia and osteopenia with the rate of SSI after lumbar fusion. Thus, the aim of this article is to evaluate the influence of sarcopenia and osteopenia on the postoperative infection rate in patients treated with posterior fusion for degenerative diseases of the lumbar spine. Material and Methods: Patients aged 50-85 treated with a short (3 levels or less) posterior arthrodesis for degenerative lumbar spine disease over a 15-year period (2005-2020) were included. Minimum follow-up was 2 years. Baseline characteristics, Charlston Comorbidity Index (CCI), ASA score and length of stay were collected. Postoperative infectious complications were recorded. Through preoperative MRI, central sarcopenia and osteopenia were quantified with the Psoas Lumbar Vertebral Index (PLVI) and the M-score, respectively. Patients were initially stratified into high/low PLVI with the mean value (0.71) to identify baseline; the same stratification was performed for M-score values, with the mean value 0 as a baseline. Results: A total of 308 patients were included (mean age 63.8 years, range 51-82; mean follow-up 45.6 months, range 24-124). Postoperative SSI was diagnosed in 26/308 patients (8.4%) after an averge time of 30 days after surgery (14-43). Low PLVI was associated with older age (p < 0.01), female gender (p = 0.016) and higher CCI (p = 0.015); however, it was not associated with higher risk of postoperative SSI (p=0.68). On the other hand, low M-score was associated to older age (p = 0.04) and diabetes (p = 0.04); moreover, low M-score patients were at higher risk of developing SSI (p=0.04). However, they did not show a low-PLVI value (p = 0.5) and were homogeneously distributed between low and high PLVI groups (p = 0.6). Conclusion: Our results indicated that a low M-score is a risk factor for surgical site infection, while a low PLVI is not. This confirms that osteopenia could have a great impact on spine surgery outcomes.
951
A079: Early compensatory segmental angle changes at L3-4 and L4-5 following a L5-S1 anterior versus transforaminal lumbar interbody fusions
Bailey O’Connor 1 , Gina Canlas 1 , Caroline Drolet 1 , Jesse Shen 1,2 , Venu Nemani 1 , Jean Christophe Leveque 1 , Katie Krause 1 , Rajiv Sethi 1 , and Philip Louie 1
1 Neurosurgery, Virginia Mason Franciscan Health, Seattle, United States
2 Université de Montréal, Canada
Introduction: As degenerative and chronic isthmic spondylolistheses progress over time at L5-S1, a decrease in the segmental lordosis at this level is often observed. This often progresses to lordotic overcompensation at the adjacent levels in an attempt to maintain spinopelvic balance. The fate of the adjacent angles following interbody fusion has not been well described. Our goal was to compare the early reciprocal changes seen at the L3-4 and L4-5 adjacent levels 6 months following an anterior (ALIF) or transforaminal (TLIF) lumbar interbody fusion at L5-S1. Material and Methods: Patients who underwent a L5-S1 ALIF or TLIF with posterior pedicle screw instrumentation for a grade 1 spondylolisthesis between January 1, 2018 and November 1, 2021 were included in this study. Preoperative and 6-month postoperative measurements were made on sagittal standing radiographs: segmental lordosis (L3-4, L4-5, and L5-S1), lumbar lordosis, and pelvic incidence. We performed preliminary t-tests for descriptive purposes and multiple regression for our main hypothesis testing. Results: We identified 70 patients who met our inclusion criteria (35 ALIF and 35 TLIF). For both the overall lordosis (ALIF 4.6 deg, TLIF -4.3 deg) and at L5-S1 (ALIF 10.5 deg and TLIF -2.2 deg), ALIF procedures led to greater lordotic change than TLIF procedures (p < .001). A greater amount of lordosis achieved at L5-S1 was associated with a greater reduction of segmental lordosis at L4-5 and L3-4 (p = 0.02). In fact, a greater change in the compensatory lordosis (return to neutral) at L4-5 predicted a similar change at L3-4 (p = .02). Thus, patients that underwent an ALIF at L5-S1 demonstrated greater amounts of compensatory loss of segmental lordosis at L4-5 and L3-4 compared to those that underwent a TLIF. Conclusion: In patients who underwent a L5-S1 ALIF or TLIF with posterior pedicle screw instrumentation for a grade 1 spondylolisthesis, we observed greater segmental L5-S1 lordosis in those that underwent an ALIF compared to those undergoing a TLIF. Six months following surgery, greater compensatory changes (lordosis reduction) are observed at the L4-5 and L3-4 adjacent levels in patients undergoing an ALIF at L5-S1. Interestingly, the amount of lordosis correction at L5-S1, directly impacts the amount of compensatory loss of lordosis (return to neutral) at L4-5, which in turn affects the change in segmental lordosis at L3-4. This is suggestive of an indirect effect of the operative L5-S1 segmental angle change and procedure interaction through L4-5 angle change on L3-4.
1482
A080: Comparison of the clinical and radiologic outcomes between T9 vs T10 vertebra in the midthoracic spine as upper instrumented vertebra in the long fusion down to sacrum for adult spinal deformity
Azmi Hamzaoglu 1 , Hamisi Mraja 1 , Tunay Sanli 1 , Halil Gok 1 , Celaleddin Bildik 1 , Onur Levent Ulusoy 1 , Ayhan Mutlu 1 , Selhan Karadereler 1 , and Meric Enercan 1
1 Scoliosis-Spine Center Istanbul, Istanbul, Turkey
Introduction: T10 has been accepted as the lowest immobile thoracic vertebra at midthoracic region and ideal upper instrumented vertebra (UIV) for many years. Previous studies reported high rates of PJK/PJF when T10 vertebra was selected as upper instrumented vertebra in long fusions for ASD. Above T10 level ribs articulate with two adjacent vertebra through costovertebral joints indicating that T10 vertebra still belongs to the mobile transitional zone. T9 vertebra anatomically provides better rib cage support than T10 vertebra and will be a more stable fixation point. Aim of this study is to compare clinical and radiological outcomes of surgically treated ASD patients in which T9 or T10 vertebra were selected as the upper instrumented vertebra. Methods: 88 ASD patients, >60 years, underwent posterior long fusion down to sacrum were reviewed. T9 Group (T9G) included 45 patients (27F, 18M) and T10 Group (T10G) included 43 (30F, 13M). Cement augmented pedicle fixation was performed at UIV and prophylactic vertebroplasty was performed at the UIV-1 in all patients. Preop, postop & f/up radiologic parameters were measured. ODI score was used for clinical evaluation. Results: Mean age was 69 (60-79) years and f/up was 47 (24-182) month in T9G. Mean age was 67 (60-80) years and f/up was 61 (24-144) month in T10G. Radiologically, no patient had PJK/PJF in T9G, and 8 patients had PJK (18.6%), 4 patients had PJF in T10G (9.3%). Patients with PJF were revised and fixation was extended up to T4. Mean ODI score at f/up was better in T9G (23) than T10G (33). Conclusion: Patients with upper instrumented vertebra at T9 (none PJK/PJF) showed better radiologic and clinical outcomes when compared to patients with upper instrumented vertebra at T10 (PJK 18.6%, PJF 9.3%) in long fusions down to the sacrum. Due to the anatomic transition of facet joint orientation and stiffer rib cage support above the T10 level, T9 vertebra is better and safer than T10 vertebra to prevent proximal junctional problems. T9 vertebra should be selected as upper instrumented vertebra unless this level is the apex of kyphosis or T9 does not contribute to the upper thoracic curve in ASD cases. Mean ODI score was better in T9G.
1962
A081: Are there any differences in the rate of distal junctional pathology between L3 vs L4 PSO?
Saman Shabani 1 , Vardhaan Ambati 2 , Timothy Chryssikos 2 , Anthony di Giorgio 2 , alma rechav ben natan 2 , Jeremy Huang 2 , Alysha Jamieson 2 , Jeremy Guinn 2 , Hao-Hua Wu 2 , Wang Minghao 2 , Pingguo Duan 2 , Zhuo Xi 2 , Joshua Rivera 2 , Parishkrita Srivastava 2 , Shane Burch 3 , Sigurd Berven 3 , Praveen Mummaneni 2 , Dean Chou 2 , and Lee Tan 2
1 Department of Neurological Surgery, Medical College of Wisconsin, Milwaukee, United States
2 Department of Neurological Surgery
3 Department of Orthopaedic Surgery, University of California, San Francisco, United States
Introduction: Pedicle subtraction osteotomy (PSO) is a powerful technique for correction of severe spinal deformities. L3 and L4 are two common PSO sites; however, the differences in radiographic outcomes and complication profile are still unclear. In this study, we aim to determine if there are differences in radiographic outcomes and rates of distal junctional pathology between L3 and L4 PSO. Material and Methods: Retrospective analysis was conducted on patients who underwent either L3 or L4 PSO between 2005 and 2021 with at least 1-year of follow-up. Distal junctional pathology is defined as either hardware failure or pseudarthrosis at or distal to PSO site. Univariate and multivariate analysis were performed for statistical analysis. Results: A total of 121 patients were included in the study; 89 (73.6%) patients underwent L3 PSO, while 32 (26.4%) underwent L4 PSO. The average follow-up length was 4.0 years (1.0-10.9 years). There were no significant differences in age, sex, BMI, operation time, and estimated blood loss between the cohorts. There were no significant differences in spinopelvic parameters preoperatively except that L3 versus L4 PSO cohort had lower pelvic incidence (49.08 ± 11.52 vs. 57.38 ± 14.91, p = 0.002). Postoperatively, L4 versus L3 PSO cohort had larger L4-S1 segmental lordosis (38.2 ± 13.4 vs. 22.1 ± 10.7 vs., p < 0.001) and lower rates of low lordosis distribution index (LDI) (18.2% vs 60.0%, p < 0.001). The L4 PSO cohort had lower total rates of distal junctional pathology (15.2% vs. 47.8%, p = 0.001), including hardware failure (15.2% vs. 41.1%, p = 0.007) and pseudarthrosis (6.1% vs. 34.4%, p = 0.002). Multivariate analysis found that L4 PSO results in a 30% reduced risk for developing distal junctional pathology. Conclusion: L4 PSO cohort experienced lower rate of distal junctional pathology, compared to L3 PSO cohort. This could be related to more physiological distribution of lumbar lordosis by performing L4 PSO, compared to L3 PSO.
OP10: Surgical Outcomes
1507
A082: Analysis of the individual impacts of comorbidities that compose the modified 5-factor frailty index in elective spine surgery. Should all factors be weighted equally?
Gaston Camino-Willhuber 1 , Henryk Haffer 2 , Erika Chiapparelli 1 , Soji Tani 1 , Maximilian Muellner 2 , Yusuke Dodo 1 , Jennifer Shue 1 , Michele Sarin 3 , William Zelenty 1 , Gbolabo Sokunbi 1 , Darren Lebl 1 , Federico Girardi 1 , Frank Cammisa 1 , Alexander Hughes 1 , and Andrew Sama 1
1 Department of Orthopaedic Surgery
2 Universitätsmedizin Berlin, Center of Musculoskeletal Surgery, Germany
3 Department of Epidemiology and Biostatistics, Hospital for Special Surgery, United States
Introduction: Preoperative risk stratification is essential to assess the patient’s risk of postoperative complications. In this regard, the modified 5-factor index score has shown to effectively predict complications in Spine surgery. Each factor from the score equals “1” point and patients are considered frail if they have two or more factors. However, the individual impact of each factor is unknown. Therefore, the objective of this study is to analyze and compare the individual influence of the variables that compose the modified 5-factor frailty index score (mFI-5) in terms of complications, reoperation, readmission, and mortality after elective spine surgery. Material and Methods: The American College of Surgeons - National Surgical Quality Improvement Program (ACS-NSQIP) Database 2005- 2018 was used to identify patients who underwent elective spine surgery. The mFI-5 score was calculated based on the presence of the 5 comorbidities: Congestive heart failure within 30 days prior to surgery, insulin-dependent or non-insulin-dependent Diabetes mellitus, chronic obstructive pulmonary disease or Pneumonia, partially dependent or totally Dependent functional health status at time of surgery, and Hypertension requiring medication. Multivariable analysis was used to assess the independent impact of each comorbidity in the mFI-5 score on the risk of complications, reoperation, readmission and mortality. Results: A total of 169,125 patients were included with a mean age of 59.9 ± 13.7. The number suffering complications was 15,683 (9.3%), 3,061 suffered surgical complications (1.8%), 4,659 required reoperations (2.8%), 7,971 were readmitted (4.7%), and 386 died (0.2%) within 30 days after surgery. Multivariable analysis showed that Chronic heart failure and Dependent status had significantly higher risk of complications (OR = 3.1 and 2.9, respectively), compared with Diabetes (OR = 1.4), Hypertension (OR = 1.7), and Chronic obstructive pulmonary disease (OR = 1.5). Similar results were observed for reoperation, readmission and mortality. Conclusion: Individual impact of each comorbidity composing the mFI-5 score is different. For this reason, the frailty status definition based on the presence of two or more comorbidities should be reconsidered in elective spine surgery. The definition of frailty status should not only rely on a quantitative analysis but also in a qualitative manner.
1168
A083: Fourteen-year long trends analysis on surgery for degenerative spinal disease in Canada: a retrospective cohort study
Charlotte Dandurand 1 , Pedram Laghaei Farimani 1 , Tamir Ailon 1 , Raphaële Charest-Morin 1 , Nicolas Dea 1 , Marcel Dvorak 1 , Charles Fisher 1 , Brian Kwon 1 , Scott Paquette 1 , and John T. Street 1
1 Vancouver, University of British Columbia, Canada
Introduction: Despite degenerative spinal pathologies being a growing burden on healthcare systems, very little is known about variations in surgical care for this disease. An analysis of these trends is crucial as there is a worldwide shift in the epidemiological profile with an increasing elderly population. This new knowledge will be invaluable for healthcare decision makers and future resource allocation planning. The main goal of this study was to provide an essential portrait of surgical trends for degenerative spinal pathologies within Canada. Material and Methods: This is a retrospective analysis of prospectively collected data from a rigorously maintained national registry, the Canadian Institute for Health Information (CIHI). CIHI is an independent non-profit organization that collects comparable data across all Canadian healthcare systems. We identified patients who received surgical intervention for a degenerative spinal condition from 2006 to 2019. The trends in number of spinal interventions, emergent vs elective hospitalizations, in-hours vs out-of-hours interventions, resource utilization, discharge disposition and adverse events were analyzed using linear regression models. Results: Over the fourteen-year period, this study analyzed a total of 338,658 spinal interventions that occurred in Canada. The number of spinal interventions increased over time 2.5 % per year (95%CI 1.023-1.028, p < 0.001) or 609.47 interventions (95% CI 535.64 - 683.30, p < 0.001). This growth is more rapid than the average Canadian population growth rate from 2006 to 2019 of 1.1 %. This study analyzed a total of 256,351 hospitalizations for degenerative spinal disease from 2006 to 2019. There were 192,018 elective hospitalizations (74.9%) and 64,333 emergent hospitalizations (25.1%). In Canada, the number of elective hospitalizations increased overtime on average 2% yearly (95%CI 1.017 – 1.023, p < 0.001) or 275.56 elective hospitalizations (95% CI 228.32-322.80, p < 0.001). A more rapid increase in the number of emergent hospitalizations was observed with an average 3.4% yearly increase (95%CI 1.027 – 1.040, p < 0.001). The average resource utilization per emergent hospitalization has decreased on average 5.7% per year (95% CI 0.01-0.11, p = 0.033). The average resource utilization per elective hospitalization has not changed over time. The number of spinal interventions associated with an adverse event increased on average 6.3% per year (95%CI 1.049-1.077, p < 0.001). Trends in discharge disposition were presented. Conclusion: This study presented a fourteen-year long report on 338,658 spinal interventions taking a rigorous look at Canadian surgical trends for degenerative spinal disease. Our findings highlight the increasing demand for surgical treatment for degenerative spinal disease with a growth rate of 2.5% per year. Secondarily, we observed a shift from elective in-hours procedures to emergent out-of-hours procedures suggesting an overload of the Canadian healthcare system. We hypothesize that the overall increase in surgical load and hospitalizations associated with an adverse event is likely related to the growing elderly population receiving spinal surgical care. This new knowledge is crucial for healthcare decision makers to minimize the burden on the healthcare system due to the changing spinal care environment and the growing population, especially in the elderly.
1508
A084: Frailty stratification using the modified 5-factor index, proposal of mild and severe frailty statuses in elective spine surgery
Gaston Camino-Willhuber 1 , Henryk Haffer 2 , Erika Chiapparelli 1 , Maximilian Muellner 2 , Soji Tani 1 , Yusuke Dodo 1 , Jennifer Shue 1 , Michele Sarin 3 , William Zelenty 1 , Gbolabo Sokunbi 1 , Darren Lebl 1 , Frank Cammisa 1 , Federico Girardi 1 , Ellen Soffin 4 , Alexander Hughes 1 , and Andrew Sama 1
1 Department of Orthopaedic Surgery
2 Universitätsmedizin Berlin, Center of Musculoskeletal Surgery, Germany
3 Department of Epidemiology and Biostatistics
4 Department of Anesthesiology, Hospital for Special Surgery, United States
Introduction: Frailty is a clinical condition characterized by a decline in the physiological reserve and has been associated with higher risk of postoperative complications. The modified 5-factor index frailty score is a good predictor of complications and mortality after Spine surgery in patients with two or more comorbidities (mFI-5≥ 2). However, the frailty status encompasses a range of two, three, four and five comorbidities, moreover, the combination of different comorbidities might result in heterogeneous risk of complications. Therefore, the objective of this study is to analyze and compare the combinations of variables that compose the modified 5-factor frailty index score (mFI-5) based on the number and type of comorbidities in terms of complications, reoperation, readmission, and mortality after elective spine surgery. Material and Methods: The American College of Surgeons - National Surgical Quality Improvement Program (ACS-NSQIP) Database 2005- 2018 was used to identify patients who underwent elective spine surgery. The mFI-5 score was calculated based on the presence of the 5 comorbidities: Congestive heart failure within 30 days prior to surgery, insulin-dependent or non-insulin-dependent Diabetes mellitus, Chronic obstructive pulmonary disease or Pneumonia, partially dependent or totally Dependent functional health status at time of surgery, and Hypertension requiring medication. Multivariable analysis was used to assess the independent impact of each combination of comorbidities in the mFI-5 score on the risk of complications, reoperation, readmission and mortality. Results: A total of 169,125 patients were included with a mean age of 59.9 ± 13.7. The number suffering complications was 15,683 (9.3%), 3,061 suffered surgical complications (1.8%), 4,659 required reoperations (2.8%), 7,971 were readmitted (4.7%), and 386 died (0.2%) within 30 days after surgery. The risk of complications ranged from the lowest risk observed in patients with Diabetes + Hypertension (OR = 1.5) to the highest risk from combination of CHF, Diabetes, COPD, and Dependent Status (OR = 8.3) with a high variation of complication rate based on different combinations, patients with a relative risk less than 5 were classified as mild frail and patients with higher risk were considered severe frail. Conclusion: There is a high variability in terms of relative risk of complications based on the presence and combination of some comorbidities. Therefore, frailty status encompasses a heterogeneous group and sub-stratification of frailty status in mild and severe forms can be useful to discriminate a subgroup of frailty patients with significantly higher risk of complications.
1089
A085: Timing of pregnancy and childbirth after lumbar discectomy: a retrospective study
David Felzensztein 1 , Eilat Sapirstein 1 , and Eyal Itshayek 1
1 Neurosurgery, Rabin Medical Center, Holon, Israel
Introduction: Lumbar radiculopathy affects 1.6% to 13.4% of the population. Low back pain (LBP) and leg pain (LP) are common complaints during pregnancy, affecting around half the pregnant population. LBP associated with true radiculopathy caused by disc herniation affects around 1% of women during pregnancy. Risk factors that increase LBP and LP include excessive weight gain, previous low back pain and a history of pelvic girdle pain. Joints can shift and press on different nerves causing motor and sensory deficits. The pain's pathophysiology remains unclear but is most likely due to biomechanical and hormonal changes that occur during pregnancy. This study aims to identify the optimal timing for pregnancy and childbirth after lumbar discectomy and to identify the risk factors for lumbar back pain during or after pregnancy in women who have had a previous lumbar discectomy. Material and Methods: Query was made through the Clalit Health Services database of beneficiaries who received care in Clalit health facilities between 2010 and 2019. The population in question included women aged 18-45 who underwent lumbar discectomy up to 10 years before giving birth. Demographic data and timing from index procedure to pregnancy, and time from pregnancy to the second event (ie radiculopathy, lumbar back pain, sciatica, etc) were included in the search query. Patients were excluded if found without sufficient documentation. The obtained data were anonymised and randomly collected. Data was extracted from Clalit Health Services (CHS) using Clalit Data Sharing platform powered by MDClone** Results: Overall, 112 patients were included (age 32.2 ± 5.29 years old). Out of the 112 patients, 12 experienced a second event. The average time from the first disc herniation to pregnancy was 1357.01 days. Our analysis showed the median time from the first disc herniation to pregnancy was 1207 days. Using Kaplan Mayer survival model, a trend toward reduced risk for disc herniation was found; the longer the time from first disc herniation to pregnancy (p = 0.0597). No statistically significant relationship was found between the time from first back pain until pregnancy and the reoccurrence of back pain after pregnancy. Conclusion: Our findings suggest an increased risk of lumbar back pain after birth the shorter the time interval between discectomy and pregnancy. Patients should be advised a year's rest prior to pregnancy to reduce the likelihood of worsening lumbar symptomatology.
1637
A086: Variability in postoperative activity restrictions after thoracolumbar spine surgery depending on surgical complexity and surgeon geographics: a multi-national cross-sectional survey
Dae-Woong Ham 1 , Ohsang Kwon 2 , Timothy S. Yoon 3 , Yabin Wu 4 , Matthew Gary 3 , Ho-Joong Kim 5 , and AO Spine Knowledge Forum Degenerative
1 Department of Orthopaedics, Chung-Ang University Hospital, Seoul, South Korea
2 Department of Orthopaedics, Armed Force Capital Hospital, Seng-Nam, South Korea
3 Emory Orthopaedics & Spine Center, Atlanta, United States
4 AO Spine International, Research Department, Davos, Switzerland
5 Department of Orthopaedics, Seoul National University Bundang Hospital, Seng-Nam, South Korea
Introduction: Activity restriction after thoracolumbar spine surgery is of great interest to patients. The enhancement of fixation technologies and fusion techniques are diminishing the need for long-term restriction of range of motion or return to sports. Clinical practice is currently based on unchanged guidelines or personal experience. Here we present the results of a multinational cross-sectional survey on activity restriction from spine surgeons with different specialties and geographics. Material and Methods: AO Spine sponsored survey was performed. Two hundred and eighty surgeons annually performing more than ten cases of fusion surgeries responded to the survey. The survey items were the postoperative period until 1) unrestricted range of motion (ROM), 2) return to noncontact sports, 3) return to contact sports. The results were sub-analyzed by surgical complexity (minimal invasive surgery [MIS] vs. open surgery / one- or two-level fusion vs. three- to five-level fusion vs. deformity correction involving more than five-level fusion), specialties (orthopedic surgeon vs. neurosurgeon) and geographic region (North America, Latin America, Europe & Southern Africa, Middle East and North Africa, or Asia Pacific). Results: The duration until returning to daily activities, from unrestricted ROM to non-contact or contact sports, were not significantly different across various complexity of the fusion surgery for degenerative spinal stenosis. The most common responses and their percentages are as follows. Duration until 1) unrestricted ROM: immediately after surgery (31.3%, 30.9%, and 30.2% for minimal invasive one- or two-level fusion, open one- or two-level fusion, and open three- to five-level fusion, respectively), 2) non-contact sports: 12 to 16 weeks (28.6%, 27.5%, and 28.0%), and 3) contact sports: 6 to 12 months (26.8%, 30.0%, and 23.8%). The trend of activity restriction in the deformity surgeries involving more than five-level fusion was stricter than the degenerative spinal stenosis setting with statistical significance. Geographically, surgeons from Europe, South Africa, and Latin America tended to allow unrestricted ROM earlier than other regions. The return to non-contact and contact sports tended to be allowed earlier by surgeons from North American region. Neurosurgeons allowed their patients to return to noncontact and contact sports earlier than the orthopedic surgeons (p = 0.03 and 0.02 respectively). Conclusion: The variance of surgical complexity in the degenerative spinal stenosis setting did not significantly influence on when the patients were told to return to unrestricted ROM, noncontact sports, or contact sports. However, the trend of activity restriction was significantly different according to the geographic regions and specialty of the surgeons.
1289
A087: The predictive potential of nutritional and metabolic burden: development of a novel validated metric predicting increased post-operative complications in adult spinal deformity surgery
Peter Tretiakov 1 , Zach Thomas 1 , Pooja Dave 1 , Jamshaid Mir 1 , Kimberly McFarland 1 , Bailey Imbo 1 , Rachel Joujon-Roche 1 , Tyler Williamson 1 , Shaleen Vira 2 , Andrew Schoenfeld 3 , and Peter Passias 1
1 Neurological and Orthopaedic Surgery, NYU Langone Health, New York City, United States
2 Department of Orthopedic Surgery, UT Southwestern, Dallas, United States
3 Department of Orthopedic Surgery, Brigham and Women's Center for Surgery and Public Health, Boston, United States
Introduction: Endocrine and metabolic disease burden has been previously identified to significantly influence patient outcomes, and may play a significant role in predicting increased peri and post-operative complications. Such effects have not been well studied in adult spinal deformity (ASD) surgery. Material and Methods: ASD patients ≥18 years with baseline (BL) and two-year (2Y) data were included. An internally cross-validated weighted equation using pre-operative laboratory and comorbidity data correlating to peri-operative complications was developed via backstep logistic regression. BMI categorization (normal, over/underweight, obese) was established per USA CDC guidelines. Diabetes classification (normal, prediabetic, diabetic) was stratified per 2010 American Diabetes Associates (ADA) cutoffs. A novel spine surgery-specific metabolic burden score was calculated via Beta-Sullivan adjustment, and Conditional Inference Tree (CIT) determined score threshold for experiencing ≥1 complication. Cohorts were ranked into halves for comparison (LOW vs HIGH). Linear regression assessed correlations between increasing burden score and complications. Means comparison analysis assessed groups differences in BL and post-operative factors. Results: 201 ASD patients were included (mean age: 58.60 ± 15.4, sex: 48% female, BMI: 29.95 ± 14.31, CCI: 3.75 ± 2.40). Significant demographic, nutritional and metabolic factors were determined to be: age (+1/year), hypertension (+18), peripheral vascular disease (+37), smoking status (+21), anemia (+1), VitD hydroxyl (+1 per ng/mL), hemoglobin (+1 per g/dL), BMI categorization (+13/cat), and diabetes categorization (+4/cat) correlating to occurrence of post-operative complications (model: p < .001). CIT determined scores above 175 correlated with ≥ 1 post-op complication (p < .001). At baseline, LOW patients were more likely to be younger (p = .002), have less total comorbidities (both p < .001), and report lower SF-36 Physical Role scores (p = .037), though groups did not differ by regional or global deformity (p > .05). Surgically, HIGH patients had higher ASA grades (p = .021), and were more likely to require PSO (p = .031). Post-operatively, HIGH patients reported significantly worse SF-36 Physical Functioning scores by 2Y (p = .042) than their LOW counterparts. Furthermore, HIGH patients reported higher rates of post-operative cardiac complications (p = .045), and were more likely to require reoperation (p = .024) compared to LOW patients. Conclusion: Nutritional and metabolic related factors play a tremendous impact on the peri- and post-operative course of adult spinal deformity patients undergoing corrective surgery, speaking potentially to a diminished physiology reserve and resilience. Development of a validated novel nutritional and metabolic burden score demonstrated that patients with higher scores are at greater risk of increased post-operative complications and course. As such, surgeons should consider reduction of nutritional and metabolic burden pre-operatively to enhance outcomes and reduce complications in ASD patients.
843
A088: Spine deformitise 33 analisys of association of genetic markers
Egor Filatov 1 , Dmitry Klyuchnikov 2 , Ivan Tyumi 2 , Olga Tyumina 3 , and Alex Evsukov 1
1 Iizarov centre, Kurgan, Russian Federation
2 Medical Centre “Dynas, Samara, Russian Federation
Introduction: To study the associations of single-nucleotide polymorphisms: rs6570507 in GPR126 gene, rs1800795 in IL-6 gene, rs1800469 in TGFB1 gene, rs731236 in VDR gene, rs625039 and rs11598564 polymorphisms in LBX1 gene, and rs12946942 in SOX9 gene with congenital scoliosis. Material and Methods: The study included 90 patients with verified congenital anomalies of the spine (single and multiple malformations of the spine, ICD-10 Code: Q76.3) and 157 clinically healthy volunteers without diagnosed spinal deformity and without family history of spinal malformations or osteoarticular system diseases. Molecular genetic testing was performed by PCR with real-time registration of a signal from the developed oligonucleotides used to determine rs6570507, rs1800795, rs1800469, rs625039, rs11598564, rs12946942, and rs731236 polymorphisms. Reference sequences were selected from the dbSNP database, and sequence design was performed on the BLAST platform. Data analysis was performed using the R free software computing environment. Data were compared using Pearson’s χ2 test, and 95 % confidence interval limits were calculated to assess the significance of OR. Results: Statistically significant association of the G allele and GG genotype of the rs1800795 polymorphism in the interleukin-6 gene with congenital scoliosis was found in group of Russian patients (p < 0.001). No significant association of alleles and genotypes of polymorphic variants of rs6570507, rs1800469, rs625039, rs11598564, rs12946942, and rs731236 with congenital scoliosis was found. Conclusion: The rs1800795 polymorphism can be considered as a promising marker for molecular genetic diagnostics of congenital scoliosis.
1209
A089: Scoliosis in pediatric neuromuscular myopathy - a Retrospective national Cohort
Alexandra Satanovsky 1 , Sharon Eylon 2 , Leon Kaplan 1 , and Josh Schroeder 1
1 Orthopedic Surgery, Hadassah Medical Center, Jerusalem, Israel
2 Orthopedic Surgery, Alyn Rehabilitation Hospital for Children & Adolescents, Jerusalem, Israel
Introduction: Neuromuscular scoliosis if a deformity of the coronal plane of patients with abnormal myoneural pathway. In these disorders poor head and trunk control is seen, also, they suffer from impaired ADL and in progressive disorders may become wheelchair and ventilator dependent. Scoliosis in myopathic disorders in prevalent in up to 90%, and may progress rapidly in peak growth period as much as 16-24 degrees per year, resulting in reduction in lung function (4-8% Vital Capacity for every 10% in COBB angle). Progression of the long C shaped curve may result in disruption of the pelvic obliquity and inability to seat in a wheelchair or proper nursing of these patient. Contribution of surgical spinal fusion to improvement in respiratory status of curve progression is controversial. Also, the available data of the effect of surgery on quality of life and change in disease’s natural course is limited. Due to the rare nature of these disorders data available is scarce and most studies lack adequate control group. Our adolescent and pediatric rehabilitation hospital is a national reference center for diagnosis, treatment and rehabilitation of neuromuscular patients. In this hospital a multidisciplinary approach is used. In our study, we set to evaluate the natural course of neuromuscular scoliosis in myopathic disorders under optimal modern treatment. Material and Methods: Patients admitted to a single hospital’s neuromuscular clinic, with diagnosis of Myopathy and scoliosis, age 18 years old and less on the first visit were initially identified for this retrospective cohort. Hospitalized children were included. Both archived and computerized data was obtained from 1976-2020. Demographic data, medical history, ambulation, respiratory and nutritional status was documented in the first and last visit. Scoliosis progression was evaluated via of COBB angle and pelvic obliquity on radiograph of first and last visit, pre and post surgery. Surgical data was obtained. Patients with missing data were excluded. All calculations were performed by as single researcher. Results: Of 290 patients initially identified 131 were included in the cohort. 159 patients were excluded due to missing data. Male to female 73:58. On last follow up 113 living patients were found. Age at first visit ranged from 2 months to 52 years (median 4.5 SD 8.68). Congenital (29%) and other muscular dystrophy (25%) were the most frequent diagnosis, followed by Nemaline myopathy (13%) and fiber type myopathy (8%). Delta in COBB angle was similar in surgical and non surgical group, with 23 degrees of average correction. Delta in pelvic obliquity was smaller in the surgical group (2.6 and 7.3). Progression in motor disability was seen in non surgical group only, as respiratory deterioration was more progressive in the surgical group. Conclusion: To our knowledge, this is the largest database of pediatric myopathic scoliosis published. With limitations, surgical correction halts progression and showed better functional independence, though it did not improve respiratory status comparing to the non surgical group. This comprehensive data allows to better understand the natural course of these rare disorders, under modern multidisciplinary treatment, especially in the non-surgically treated group.
568
A090: Is “sarcopenia” a hype??? or does it really affect the outcome of spine surgeries?
Manojkumar Gaddikeri 1 and Abhay Nene 1
1 Lilavati Hospital and Research Center, We Are Spine, Mumbai, India
Introduction: Sarcopenia, defined as progressive impairment of muscle function secondary to loss of skeletal muscle mass has prevalence of 24%- 56% in patients > 60 years. 44% of elderly patients undergoing orthopaedic surgery are found to be sarcopenic. It is a known risk factor for fall, fractures, disability, increased post-operative morbidity and mortality. If diagnosed pre-operatively, it can help prepare the patient and surgical team to foresee complications and thereby reduce morbidity and mortality. In the present study, we evaluated and correlated sarcopenia with the surgical outcome of operated patients with lumbar spine pathology. Materials and Methods: A prospective, observational study was conducted on 108 patients > 40 yrs undergoing lumbar spine surgeries, who were studied and followed up for 3-months. They were segregated into 5 groups based on age (40-49 yr, 50-59 yr, 60-69 yr, 70-79 yr, ≥ 80 yr) and were assessed separately. Data on demography, grip-strength analysis, 30s chair stand test, Psoas muscle index (calculated on pre-operative MRI), pre and post-operative ODI (Oswestry Disability Index) scores at 2 weeks and 3 months, Dindo-Clavien Classification of peri-operative complications, 90-day readmission rates and mortality (if any) were included. Patients were segregated into sarcopenic & non-sarcopenic groups based on the definition and set parameters as per the European Working Group on Sarcopenia in Older People (EWGSOP). A comparative analysis between these groups was performed. Results: Of 108 patients, there were 18 patients in 40-49 yrs, 24 in 50-59yrs, 27 in 60-69 yrs, 30 in 70-79 yrs and 9 in > 80 yrs age group. Statistically significant difference in peri-operative ODI scores was seen in sarcopenic vs non-sarcopenic patients in all age groups (p < 0.05) except 40-49 yrs. Results showed that sarcopenic group had higher rate of peri-operative complications, delayed mobilisation, longer stay and mortality compared to non-sarcopenic group. Conclusion: We conclude that sarcopenic patients have poor outcome in lumbar spine surgery compared to those without. So, by diagnosing sarcopenia using tests routinely done as pre-operative requirement, one can reduce radiation exposure and cost of treatment. The management can be revolutionized by predicting those who are at high risk of developing post-operative complications and poor surgical outcomes by mere diagnosis of sarcopenia. This knowledge will benefit both the patients and the surgeons.
Keywords: Sarcopenia, EWGSOP, Grip strength, chair stand test, Dindo-Clavien Classification, Oswestry Disability Index
OP11: Infections in Spine Surgery
385
A091: Osteoradionecrosis and acute infection after needle aspiration of the upper pharynx result in pathological fracture of C1 vertebra and formation of a fistula in a young patient with history of cervical chordoma. A rare case with lots of diagnostic and therapeutic dillemas and chalenges
Thomas Repantis 1 , Panagiotis Korovessis 1 , Andreas Baikousis 1 , and Ioannis Papaioannou 1
1 Orthopaedic, General Hospital Agios Andreas, Patra, Greece
Introduction: Chordoma is a low-grade malignant tumor thought to be relatively radioresistant with a high rate of local recurrence. The use of modern radiotherapy (proton or carbon ion therapy) is advocated for patients undergoing surgery for the treatment of primary and recurrent chordomas but radionecrosis, among other complications, may occur. Radionecrosis can be aggravated by secondary infection which may lead to devastating results. Material and Methods: A 36-year old woman with clival chordoma and recurrence to C2–lateral mass vertebra, had been operated and had received post-operative radiation twice, 13 and 7 years ago respectively. The patient presented ten months ago with a neck infection after a needle aspiration of the upper oropharynx, accompanied by a pathological fracture of the anterior arch of C1 vertebra. She was clinically improved after 3 weeks of IV antibiotics, reporting no complaints apart from torticollis. Nevertheless a fistula was clinically and radiographically detected between the upper oropharynx wall (initial aspiration site) and C1, C2 lateral mass, while atlantoaxial instability signs were evident. Clinical decision regarding what procedure to follow was thoroughly discussed. Occipitocervical stabilization followed by closure of the fistula or vice versa or both procedures at the same time, were all suggested options. Results: Osteoradionecrosis of the C1 and C2 vertebrae due to radiation treatment for chordoma was thought to be the reason for spontaneous fracture of C1, along with the post-aspiration infection of the area. Treatment with the PENTOCLO protocol (pentoxifylline, tocopherol, clodronate) was suggested and followed for three months. Then, due to deterioration of the spinal instability (increasing neck pain, occasional extremities dysesthesia and numbness and worsening of torticollis) occipitocervical fusion was performed with autologous iliac bone graft. The histology did not disclose any malignancy or osteomyelitis. Signs of postoperative infection (fever, elevated CRP, local pain) led to surgical debridement at the 18th postoperative day. Intraoperative cultures from the cervical spine disclosed Klebsiella pneumoniae, Serratia odorifera and Enterococcus faecium. Klebsiela and Serratia had also been found in cultures taken from the retropharynx fistula. The patient received postoperatively IV antibiotics for 4 weeks and another 8 weeks orally. At the latest follow-up of 4 months she is neurologically intact, still wearing a Minerva brace and no signs of infection exist. The fistula at the retropharynx still exists though, making necessary a close follow-up for signs of recurrence of the infection and presenting a therapeutic challenge. Conclusion: Radionecrosis after radiotherapy for treatment of head and neck tumors threatens the viability of the soft tissues and the bone. We present a case of pathological post-radiation fracture of the atlas after an iatrogenic infection and formation of a fistula, connecting retropharynx and upper cervical spine. There is no consensus on therapeutic strategies on such a bad biological environment. We provided stability to the cervical spine despite the risk of infection, securing thus neurological integrity of the patient and promoting healing of the surrounding structures. Close follow-up of such patients as well as multi-disciplinary approach are necessary for the best possible results in such demanding cases.
1333
A092: Risk factors of surgical site infection after spinal surgery in a low income population
Ahmed Zendeoui 1 , Mohamed Amine Gharbi 1 , Houssem Eddine Chahed 1 , Mahdi Bouzidi 1 , and Mouadh Nefiss 1
1 Orthopedic and Trauma Surgery, Mongi Slim Marsa University Hospital Center, Tunis, Tunisia
Introduction: The awareness and identification of risk factors predisposing to surgical site infection after spinal surgery allows us to anticipate them and to take them into consideration in preoperative planning. Consequently, the incidence of postoperative infections can be reduced, Materials and Methods: In our study, we studied anthropometric data, lifestyle habits, patient history, as well as intraoperative incidents and postoperative follow-up that may interfere with the occurrence of a surgical site infection. Result: The results of our study are concordant with those of the literature and show that the major risk factors are multitarred patients with an ASA score greater 2, especially those with diabetes and hypertension, a history of spinal surgery, obesity and smoking also interfered, but alcoholism did not show a significant impact, a postoperative pulmonary or urinary infection, a long operating time with a lot of blood loss and the necessity of transfusion, a stay in intensive care, and dural tear. On the other hand, the gender of the patient, his age, the surgical approach and the number of fused segments did not significantly increase the rate of postoperative infections. Conclusion: In the strategy for control of postoperative infections in spinal surgery especially in low income populations knowledge of these risk factors is an important pillar of the treatment, the surgeon's experience with less debridement and the new technologies of minimally invasive surgery are also important, these parameters should be considered in further studies.
243
A093: Functional outcome and quality of life of conservative versus surgical management of adult Potts disease: a prospective cohort study
Mark Maranon 1 and David Endriga 2
1 Orthopedics, Asian Hospital and Medical Center, Muntinlupa, Philippines
2 Orthopedics, Philippine Orthopedic Center, Quezon City, Philippines
Introduction: The Philippines is currently ranked eighth in the top 20 countries with the highest number of tuberculosis. The country alone contributes to 3% of the global census having 1,379,390 cases from 2003 to 2011. In developing countries like the Philippines, access to surgery is difficult given that Potts disease more commonly affects people in the low-income group. Thus, patients who are candidates for surgery sometimes end up being managed conservatively with anti-Kochs medications alone. Although there is improvement in symptoms in patients treated with conservative management, there is still paucity of literature comparing the functional outcomes and quality of life of patients with Potts disease who have been treated with surgery and non-operatively. This study aims to determine the differences in functional outcome and quality of life of adult patients with Potts disease who have undergone surgical versus non-surgical management. Material and Methods: In this prospective cohort study, 45 patients were followed up for 1 year after undergoing pharmacologic treatment alone versus a combination of anti-Kochs and surgery for Potts disease. Oswestry Disability Index (ODI) and Short Form-36 (SF-36) were obtained on initiation of treatment, after three months, six months and one year. Results: ASIA scores from onset of treatment and after 1 year significantly improved (p < 0.001) for both non-surgical and surgical patients. ODI scores significantly improved after 6 months of treatment for both surgical and non-surgical patients. Both surgical and non-surgical patients showed significant improvement in their SF-36 scores but scores were noted to be higher in patients who underwent surgery. Conclusion: Significant improvement with regards to functional outcome and quality of life was noted from both surgical and non-surgical patients after 1 year of treatment, with earlier improvements and better final scores in SF 36 and ODI in patients who underwent surgery.
1596
A094: Trends in topical antibiotic use after posterior lumbar fusion: a global survey of AOSpine members
Paul Al-Attar 1 , Eric Geng 1 , Calista Dominy 1 , Jonathan Markowitz 1 , Jared Doan 1 , Matthew Gary 2 , Ho-Joong Kim 3 , Timothy S. Yoon 4 , Samuel Cho 1 , and (on behalf of) AO Spine Knowledge Forum Degenerative
1 Orthopaedic Surgery, Icahn School of Medicine at Mount Sinai, New York, United States
2 Neurosurgery
3 Orthopedic Surgery, Seoul National University, Seoul, South Korea
4 Orthopaedic Surgery, Emory School of Medicine, Atlanta, United States
Introduction: Although there are conflicting conclusions in the literature, studies have shown antibiotic powders reduce the risk of infection following lumbar spine fusion. However, the practice patterns of spine surgeons worldwide vary regarding actual use, dose, antibiotic, and type of procedure. We present a survey of topical antibiotic use in 1-2 level open, 1-2 level minimally invasive (MIS), and 3-5 level open posterior lumbar fusion surgeries among surveyed AO spine members. Materials and Methods: 280 responses from over 5000 surveyed AOSpine members were obtained. Only those who performed more than 10 cases of 1-2 level open, MIS, and 3-5 level open posterior lumbar fusion were included in this study. Surgeons were asked about their usage (not used, deep to fascia, superficial to fascia, on the bone graft) and dosage (< 1 g, > 1 g up to 2 g, > 2 g up to 3 g, > 3 g up to 4 g, > 4 g) of topical vancomycin and tobramycin. Results were compared between groups and regions (Asia Pacific, North America, South America, Europe and Southern Africa, Middle East and Northern Africa) using chi-squared with level of significance set at p < 0.05. Results: There were 233 respondents for open 1-2 level fusion, 112 for MIS 1-2 level fusion, and 194 for open 3-5 level fusion. Among open 1-2 level, 54.94% did not use vancomycin powder, 36.91% applied it deep to the fascia, 13.30% superficial to the fascia, and 12.45% on the bone graft. 92.46% used 2g or less. Among MIS, 60.71% did not use vancomycin, 33.93% applied it deep to fascia, 14.29% superficial to fascia, and 7.14% on the bone graft with 95.45% using 2g or less. For 3-5 level, 52.58% did not use vancomycin, 35.57% applied it deep to fascia, 14.95% superficial to fascia, and 14.43% on the bone graft with 91.30% using 2g or less. There was no significant difference in vancomycin usage (p = 0.62) or dosage (p = 0.65) between groups. For open 1-2 level, only 1.72% of respondents used tobramycin powder and applied it deep to fascia. The majority applied 2g or less. For MIS, 0.89% used tobramycin, applying it deep to the fascia for 1 g or less. For open 3-5 level, 1.03% used tobramycin, applying it deep to fascia for 2g or less. There was no significant difference in tobramycin usage (p = 0.77) or dosage (p = 0.67) between groups. There was significant variation in vancomycin usage by region for 1-2 level (p = 0.003) and MIS (p = 0.002) but not open 3-5 level fusion (p = 0.16). Conclusion: Most surgeons did not use vancomycin powder and a minority used tobramycin. Application was typically deep to fascia for less than 2g. Vancomycin use varied by region for MIS and 1-2 level fusion, but not open 3-5 level fusion. There were no differences in usage and dosage between procedures. Our results illustrate global trends in topical antibiotic use, which may be valuable in updating guidelines.
1062
A095: Percutaneous pedical screw fixation in caries spine - Does early MIS fixation has advantage over conservative?
Varun Agarwal 1
1 Orthopedics, Rohilkhand Medical College and Hospital, Bareilly, India
Introduction: Tuberculous (TB) spine with spondylodiscitis has conventionally been treated with medical management and prolonged immobilization in bed. Surgical intervention is only indicated for progressive deformity or neurological deficit, preventing spinal cord compression and its complications. However, prolonged bed rest has its own set of complications and poor acceptability by the patient. We performed this study to investigate the role of fixation by percutaneous pedicle screw fixation (PPSF) in spondylodiscitis secondary to TB origin for pain relief and rapid early mobilization of the patient. Material and Methods: Thirty-two cases of tuberculous spondylodiscitis were managed from March 2017 to 2019. Clinical assessment, radiological evaluation, and laboratory studies with over a year follow-up after PPSF without decompression. Visual analog scale (VAS score) and Oswestry disability indices (ODI scale, Hindi version) were used for outcome measure. Results: Female-to-male ratio was 19:13. The average follow-up was 14 months ±6 days and the duration for fusion was around 6 months. The mean duration of hospital stay was 4.006 ± 1.17 days. The average blood loss was 27.18 ml ± 17.71. The mean surgical time was 121.25 ± 14.59 min. ATT was continued for 12–18 months. Mean 48 days after surgery, and 1 year at follow-up, C-reactive protein, erythrocyte sedimentation rate, pain scores (VAS score), and ODI returned to their baseline. No failure of instrumentation or decline in neurovascular condition was reported after operative intervention. Conclusion: Primary treatment of TB spine has been chemotherapy with limited indications for surgery. Severe pain in the presence of spondylodiscitis without neurological deficit or deformity projects as an unclear situation and a temporary surgical fixation gives stability to prevent uneventful neurological injury and promote early healing with faster rehabilitation in contrast to strict bed rest and external bracing.
1701
A096: Effects of COVID19 on mental health of patients awaiting elective spine surgery in the UK
Purnajyoti Banerjee 1 and Amr Elbahi 1
1 Orthopaedic Spine, Kettering General Hospital, United Kingdom
Introduction: Novel Coronavirus (COVID19) outbreak in early 2020 has led to significant changes to the waiting list for elective spine surgery. Patients in the National Health Service (NHS) had to wait longer with increasing uncertainty on when and if they will have their surgery undertaken. This apprehension has possibly led to increased stress and mental health issues amongst patients waiting for elective spine surgery in the UK. Our aim is to determine if patients were depressed whilst waiting longer for their spine surgery during the pandemic. Methods: Elective spine patients booked before outbreak of COVID19 were included. Patients with pathologies other than degenerative spine diseases were excluded as were spine injections. Validated depression screening score (patient health questionnaire2; PHQ2) was used to screen patients for depression before and after the outbreak. Oswestry disability scores (ODI) were calculated prospectively. Results: 42 patients were included M:F = 24:18). Mean age was 62.57 years). There was no significant differences between age and PHQ2 (p = 0.89); sex and depression (Fischer exact test = 1; p > 0.05); ODI (p = 0.41) and type of procedure (decompression, two level decompression, fusion and disc surgery; p = 0.05) when related to diagnosis of depression. However the PHQ2 was significantly in favour of depression (score > 3) in 71.4% patients compared to pre COVID19 outbreak (Fisher exact test = 0.02; p < 0.05). Conclusion: This study reports the mental health effects on patients awaiting elective spine surgery in the NHS secondary to delays and uncertainties surrounding elective surgery services related to outbreak of COVID19 patients.
1684
A097: Trends in postoperative intravenous antibiotic use after posterior lumbar fusion: a global survey of AOSpine members
Eric Geng 1 , Paul Al-attar 1 , Calista Dominy 1 , Jonathan Markowitz 1 , Jared Doan 1 , Matthew Gary 2 , Ho-Joong Kim 3 , Timothy S. Yoon 4 , and Samuel Cho 1
1 Orthopaedic Surgery, Icahn School of Medicine at Mount Sinai, New York, United States
2 Neurosurgery, Emory School of Medicine, Atlanta, United States
3 Orthopedic Surgery, Seoul National University, Seoul, South Korea
4 Orthopedic Surgery, Emory School of Medicine, Atlanta, United States
Introduction: IV Antibiotic prophylaxis is commonly utilized after posterior lumbar fusion to reduce risk of surgical site infection. Generally, guidelines have supported the use of a first generation cephalosporin. However, this is not necessarily universal, and patterns of usage may differ by region, institution, and spine surgeon. Recently, a study by AO Spine surveyed 5000 + members (280 full responses) across the globe regarding their perioperative management of posterior lumbar fusion. In this study, we present the survey results of antibiotic type. Materials and Methods: Data were obtained from online surveys of AO Spine members who performed more than 10 cases of 1-2 level open, 1-2 level MIS, and 3-5 level open posterior lumbar fusion. Surgeons were asked about their postoperative IV antibiotic type (cephalosporin, cloxacillin, ciprofloxacin, aminoglycoside, vancomycin, clindamycin, or other). Results were compared between procedures and regions (Asia Pacific, North America, South America, Europe and Southern Africa, Middle East and Northern Africa) using chi-squared with level of significance set at p < 0.05. Results: There were 233, 112, and 194 respondents for open 1-2 level, MIS, and open 3-5 level fusion respectively. 94.85%, 97.32%, 95.77% of respondents reported using IV antibiotics postoperatively for open 1-2 level, MIS, and open 3-5 level fusion respectively. For open 1-2 level, responses for antibiotic type were: cephalosporin (86.27%), cloxacillin (1.72%), ciprofloxacin (3%), aminoglycoside (3%), vancomycin (6.01%), clindamycin (5.15%), and other (3.43%). For MIS, responses for antibiotic type were cephalosporin (91.07%), cloxacillin (0%), ciprofloxacin (4.46%), aminoglycoside (0%), vancomycin (2.68%), clindamycin (3.57%), and other (1.79%). For open 3-5 level, responses were: cephalosporin (86.08%), cloxacillin (1.03%), ciprofloxacin (4.12%), aminoglycoside (2.58%), vancomycin (5.67%), clindamycin (5.15%), and other (2.58%). There was no statistically significant difference in antibiotic type between groups (p = 0.70). Cephalosporin usage differed significantly by region for open 1-2 level (p < 0.001), MIS (p = 0.02), and open 3-5 level (p < 0.001) fusions. Conclusion: Consistent with the standard of practice, most surgeons used cephalosporins. However, there was significant variation by region. Antibiotic type was not significantly different between procedures. The results from our study illustrate global trends in antibiotic prophylaxis after posterior lumbar fusion, which may be used to inform further studies and contribute to updated guidelines.
1724
A098: Four easily implemented infection prevention procedures might reduce deep surgical site infections
Aldemar Andres Hegewald 1
1 Department of Neurosurgery and Spine Surgery, VAMED Baltic Sea Hospital Damp, Damp, Germany
Introduction: The purpose of this study is to investigate the incidence of surgical site infection and wound dehiscence requiring surgical intervention before and after the implementation of a bundle of infection prevention procedures, including (1) wound and disc space irrigation with a modern antiseptic (sodium hypochlorite/hypochlorous acid), (2) change of outer gloves at least every 3 hours and before implant manipulation, (3) covering of implants and instruments when not used, and (4) prolonged wound drainage in complex cases. Material and Methods: We performed a retrospective review of patients in our institution that underwent dorsal spinal surgery for degenerative spinal diseases from March 2019 to June 2020 (Group A) and after implementation of new preventive measures from July 2020 to October 2021 (Group B). The primary outcome was surgical site infection and wound dehiscence requiring surgical intervention, and more specific, discitis/infectious spondylitis, as well as epifascial and subfascial wound problems. Fisher's exact test was used for statistical analysis. Results: 1001 patients were included, 524 in Group A and 477 in Group B. In both groups 20% instrumented fusions were performed. Overall, rates of surgical site infections and wound dehiscences requiring surgical interventions were not significantly reduced from 2.2% to 1.1% (p = 0.21), in the subgroup of instrumented fusions from 6.2% to 2.2% (p = 0.17). The incidence of discitis/infectious spondylitis was reduced from 0.5% to 0% (p = 0.06). The ratio of discitis/infectious spondylitis to other wound problems was 45% to 55% in Group A, whereas it was 0% to 100% in group B (p = 0.12). The ratio of subfascial to epifascial wound problems was 91% to 10% in Group A, whereas it was 20% to 80% in group B (p = 0.01). No adverse effects of the antiseptic sodium hypochlorite/hypochlorous acid was observed. Conclusion: Our results suggest a potential benefit of easily implemented preventive measures in reducing the risk for postoperative discitis/infectious spondylitis and shifting postoperative wound problems toward more benign epifascial complications. We hypothesize that the antiseptic (sodium hypochlorite/hypochlorous acid) considerably reduces potential intraoperative infectious contaminations and warrants further studies as an alternative to widely used local antibiotics that have shown problematic alterations in wound microorganisms.
799
A099: Experiences with the treatment of cervical spine infections from a level 1 trauma center: a retrospective cohort study
Zachary Crawford 1 , Jorge Figueras 2 , Cameron Thomson 3 , and Anthony Guanciale 1
1 Orthopaedic Surgery, University of Cincinnati College of Medicine, Cincinnati, United States
2 Orthopaedic Surgery, Indiana University, Indianapolis, United States
3 Orthopaedic Surgery, Brown University, Providence, United States
Introduction: Cervical spine infections are a rare disease, representing about 1% of skeletal infections (3-6% of which cervical spine infections). Despite the rarity of the disease, there has been an increase in incidence in recent years due to the increase in susceptible populations and the increase in accuracy in diagnosing cervical spine infections [2-3]. The purpose of this study was to report the treatment, results, and overall complication rates of patients treated for cervical spine infection at a Level-I trauma center. Methods: We retrospectively reviewed all patients with a cervical spine infection from 2012 to 2021 at a Level-I trauma center. Patients with infection due to previous spine surgery (i.e., surgical site infections and postoperative spinal implant infections) were excluded. Patients’ demographics, comorbidities (using the Charlson Comorbidity Index), white blood cell count (WBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) at time of presentation, neurologic deficit, and management (operative versus nonoperative). The incidences of reoperation, recurrent infection, and unresolved neurologic deficit were recorded. Patients treated surgically were subdivided by whether they had a fusion during their index procedure. The change in American Spinal Cord Injury Association (ASIA) motor scores from presentation to final follow-up was recorded, as well as the length of stay (LOS). Results: 163 patients with a spine infection were identified, of which 47 patients had cervical spine involvement and met the inclusion and exclusion criteria. Thirty-three (70.2%) patients had infections isolated in the cervical region. The mean age was 51.3[23-76] years old and there were thirty (63.8%) males. Thirty-nine (83.0%) patients were treated operatively, of which twenty-seven (31.0%) were treated with a cervical fusion. Of the patients that had a WBC (n = 41), ESR (n = 46), and CRP (n = 43) prior to admission, thirty-four (73.9%) patients had an elevated WBC, thirty-eight (92.7%) patients had an elevated ESR, and thirty-six (83.7%) had an elevated CRP. From the operative cohort, five (12.8%) patients had a reoperation, of which four (10.2%) patients had undergone fusion during their index procedure. Of the patients treated nonoperatively, none had a recurrent infection. Of the patients treated operatively, six (15.4%) had a recurrent infection. The average initial ASIA motor score was 90.5, the average ASIA motor score at follow-up was 96.4, and the average change in ASIA motor score was 8.8. The average LOS was 17.9 [2-55] days. Conclusion: Cervical spine infections are rare; however, early diagnosis and treatment are critical considering the morbidity and potential neurologic complications. Elevated inflammatory markers may be elevated in patients with a cervical spine infection; however, patients may still have an infection with normal lab values. Recurrent infections and reoperation are complications to consider when treating patients with cervical spine infections.
OP12: Treatment Updates in Thoracolumbar Trauma
376
A100: Analysis of radiological and functional results between long and mixed fixation for thoracolumbar junction fractures
Jlidi Mohamed 1 , Mouldi Lamouchi 1 , Mohamed Hedi Gharbi 1 , Walid Bouaicha 1 , Ayachi Montassar 1 , and Selim Daas 1
1 Orthopedics and Traumatology Department, Hospital of Mohamed Taher Maamouri, Nabeul, Tunisia
Introduction: Fractures of the thoracolumbar junction (T12-L1) are the most frequent lesions of the spine. These fractures occur at the level of transition from the rigid and fixed thoracic spine to the mobile and more dynamic lumbar spine. This biomechanical particularity makes this region vulnerable to trauma and constitutes a therapeutic challenge for spine surgeons. Therapeutic modalities for thoracolumbar junction fractures remain controversial. Our aim is to compare two types of posterior fusion assembly: long assembly versus mixed assembly. Material and Methods: This is a descriptive and analytical single centre retrospective study over a 10-year-span. Two groups have been identified:
• Group A including 53 patients treated with a long assembly (2 levels above the fracture and 2 levels below)
• Group B including 28 patients treated with a mixed assembly (2 levels above the fracture and one level below)
The evaluation of the results was done by calculating the variation of radiological parameters between the postoperative radiographs and the last follow-up radiographs. The Oswestry score and the Dallas self-questionnaire were used to assess the functional results. Results: Differences were significant between the two groups in operating time with 112.32 min (group A) versus 88.18 min (group B), and in blood loss estimation with 836.16 ml (group A) and 550 ml (group B). Radiologically, for group A, the mean postoperative and last follow-up vertebral kyphosis angles (VKA) were 12.52° and 12.95° respectively. The postoperative and last follow-up regional kyphosis angles (RKA) were 11.72° and 12.36° respectively. The mean regional traumatic angulation (RTA) was 9.14° postoperatively and 9.75° at the last follow-up examination. For group B, the mean postoperative and last follow-up VKA were 11.94° and 12.82° respectively. The mean postoperative and last follow-up RKA were 12.73° and 13.42° respectively. The mean RTA was 8.64° postoperatively and 9.33° at the last follow-up examination. There was no statistically significant difference. At the last follow-up, the loss of reduction in RKA, VKA and RTA was 0.64°, 0.61° and 0.625 respectively for group A. and 0.91°, 0.75° and 0.875° respectively for group B. These differences were not statistically significant. Functionally, there were no significant differences between the two groups. The Oswerty score was 22.78 for group A and 22.84 for group B, the Dallas score was 14.25 for group A and 13.48 for group B. Conclusion: A mixed fixation method with instrumentation of 2 levels above and 1 below for the thoracolumbar junction fractures showed better similar radiological and functional results when compared to the traditional methods of fixation with minimal blood loss and shorter surgical time.
65
A101: A comparative enaluation of the interobserverreliability of AO Magerl, TLICS and the new AOSpine Classifications
Fady Khamis 1 , Phillip Schleicher 2 , and Frank Kandziora 2
1 Klinikum Ingolstadt, Ingolstadt, Germany
2 BGU Frankfurt, Germany
Introduction: In order to determine the efficiency or reliability of a new classification system, a direct comparison with existing classification systems should be performed. The aim of this Study is to compare the interobserver reliability of three international classification systems for thoracolumbar spine injuries (AO Magerl, Thoracolumbar Injury classification score ``TLICS``, Thoracolumbar AO Spine classification “TL AOSpine”) and to determine the reliability of their treatment recommendations. Material and Methods: This is a monocentric, prospective analysis of Radiological and clinical data of 100 patients with fractures of the thoracolumbar region. Only cases with traumatic fractures were included, pathological fractures were excluded. Five spine surgeons with different degrees of experience classified the available x-rays, CT and MRT images using the three classification systems AOSpine, AO Magerl and TLICS, and the associated treatment recommendation according to Thoracolumbar AO Spine classification injury score`` TL AOS IS``, the German society for trauma surgery ``DGU`` and TLICS. For the statistical evaluation, the interobserver reliability, according to Cohen's kappa, was calculated. Results: AO Magerl showed moderate interobserver reliability (κ = 0.46) for morphological classification and substantial agreement (κ = 0.71) for DGU treatment recommendations. TLICS showed fair interobserver reliability (κ = 0.35) for morphological classification, substantial agreement (κ = 0.69) for therapy recommendations according to TLICS. TL AOS showed substantial interobserver reliability (κ = 0.69) for morphological classification and a substantial agreement (κ = 0.77) for treatment recommendations (TL AOS IS). Conclusion: The TL AOS is a reliable classification, with superior interobserver reliability compared to AO Magerl and TLICS. The treatment recommendations of TL AOSIS have higher interobserver reliability compared to other treatment recommendations (DGU and TLICS).
1249
A102: Thoracolumbar Fracture Management - Does It Follow the Surgical Algorithm Proposed by the AO Spine Thoracolumbar Injury Classification?
Khoa Tran 1 , Mark Lambrechts 1 , Yunsoo Lee 1 , Sandy Li 1 , Angela Huang 1 , Justin Chu 1 , Brian Karamian 1 , Jose Canseco 1 , Alan Hilibrand 1 , Christopher Kepler 1 , Alexander Vaccaro 1 , and Gregory Schroeder 1
1 Rothman Orthopedic Institute at Thomas Jefferson University, Philadelphia, United States
Introduction: The AO Spine Thoracolumbar Injury Classification was ultimately designed to guide injury management. To achieve this, thoracolumbar injuries progress in a hierarchical fashion based on fracture severity. Along with neurologic injury severity and classification modifiers, an injury severity score is calculated. This score can then be compared to pre-established surgical thresholds to dictate if initial conservative management or surgical intervention is appropriate. Therefore, our aim was to determine if historical management of thoracolumbar spine fractures were treated based on the current recommendations proposed by the AO Spine Thoracolumbar Injury Classification surgical algorithm. Material and Methods: Patients > 18 years of age with a thoracolumbar fracture or ligamentous disruption between 2006-2021 were retroactively identified from a prospectively collected database. All patients with a preoperative MRI or CT scan were included. Patients were excluded if the fracture was due to tumor or infection. Each injury was assigned points based on the injury severity score previously established by AO Spine with hierarchical progression from Type A0 to Type C. In addition, the patient's neurologic status (N0 to N4 and Nx, unknown) injury severity score was assigned, and an additional point was added to the TL AOSIS if the status of ligamentous integrity was indeterminate. The thoracolumbar surgical threshold algorithm was then applied to determine if the patient met criteria for initial non-operative or operative management. Injuries with a TL AOSIS of three or less should undergo a trial of conservative treatment, and injuries with a TL AOSIS of more than five should undergo initial surgical intervention. Either initial operative or non-operative treatment is considered appropriate for injuries with a TL AOSIS of four or five. Modified frailty index (mFI) scores were collected for each patient to assess for appropriate surgical treatment based on clinical indications and existing comorbidities. Univariate statistics compared cohort demographics, treatment decision, and mFI scores. Statistical significance was set at p < 0.05. Results: A total of 815 patients (TL AOSIS 0-3: 486, TL AOSIS 4-5: 150, TL AOSIS 6+: 179) were included. Patients with a TL AOSIS of 0-3 were more likely to undergo non-operative management compared to those with TL AOSIS of 4-5 or 6+ (99.0% vs 74.7% vs 13.4% respectively, p < 0.001) resulting in appropriate treatment based on the surgical threshold algorithm (99.0% vs 100% vs 86.6% respectively, p < 0.001). Most TL AOSIS 4-5 patients (74.7%) were treated non-operatively. Based on the treatment algorithm, 97.5% of patients who received operative treatment and 96.1% who received non-operative treatment were treated appropriately. Of the 29 patients who did not receive appropriate treatment, 5 patients (17.2%) were treated surgically. There was no difference in mFI scores among groups. Conclusion: Most patients were treated according to the treatment algorithm proposed by the AO Spine Thoracolumbar Injury Classification. Only 5 patients who should have received conservative management were initially treated operatively, while 24 patients who met the threshold for initial operative management were treated non-operatively. Injuries identified as “surgeon preference” (i.e. TL AOSIS of 4-5) were predominantly treated with non-operative management.
316
A103: Analysis of factors affecting postoperative loss of reduction in unstable thoracolumbar fractures performed posterior surgery
Jaewan Soh 1 and Chung-Su, Hyun 2
1 Orthopaedic Surgery
2 Department of Orthopaedic Surgery, Sahmyook Seoul Medical Center, Seoul, South Korea
Introduction: Unstable thoracolumbar fractures require surgical intervention to achieve adequate reduction and restore spinal stability. However, loss of reduction can causes the kyphotic deformity, which results in several complications. The authors studied the factors influencing the postoperative loss of reduction. Methods: Of fifty-two patients who were treated by posterior surgery and had completed a minimum follow-up of 1 year, we excluded nine patients who had multiple level fractures or underwent combined anterior-posterior surgery, which yielded forty-one patients. Postoperative loss of reduction was defined as 30% or more loss of vertebral body height as measured on lateral radiography at 1-year follow-up compared to lateral radiograph taken immediate after surgery. The associations between the patients’ gender, age, level of fracture, injury of posterior column, initial loss of fractured vertebral body height, the load-sharing score, TLICS score, number of fixed segments above and below the fracture, type of pedicle screws, the degree of postoperative reduction, the degree of postoperative corrected kyphotic angle, the changes in insertion angle of the upper and lower pedicle screws of the fractured vertebral body at 1 year follow-up and postoperative loss of reduction were analyzed. The SPSS 14.0 was used for analysis of data. Results: Among forty-one patients, seven patients had postoperative loss of reduction. The number of fixed segments above and below the fracture (p = 0.045), initial loss of fractured vertebral body height (p = 0.013), the changes in insertion angles of the lower pedicle screws (p = 0.007) were significantly associated with postoperative loss of reduction. Conclusion: In patients with posterior surgery for thoracolumbar unstable fractures, loss of reduction occurred when single segments fixation above and below the fracture was used, 50% or more loss of initial fractured vertebral body height, and 5 degrees or more changes in insertion angles of the lower pedicle screws of the fractured vertebral body. This result indicates that two segments pedicle screw fixation is more stable than single segment fixation when 50% or more loss of vertebral body height at the initial fracture, and loss of fracture reduction is predicted when insertion angles of the lower pedicle screw of the fractured vertebral body changes. Further studies are needed with more cases and long-term follow-up of patients.
750
A104: Which percutaneous augmentation technique is more effective in preventing recompression of the augmented osteoporotic vertebral fracture? Mid-term follow-up
Fikret Şahintürk 1 , Erkin Sönmez 1 , Selim Ayhan 1 , Salih Gülşen 1 , and Cem Yılmaz 1
1 Neurosurgery, Başkent University, Ankara, Turkey
Purpose: To determine mid-term effects of percutaneous vertebroplasty (PVP) and balloon kyphoplasty (BK) on the structural integrity of previously augmented vertebrae. Methods: 351 patients underwent BK and PVP due to osteoporotic vertebral compression fractures between the years 2010 and 2020. The demographical, surgical and radiological characteristics of the patients were retrospectively analyzed. A total of 55 patients who met the inclusion criteria of underwent only one level PVP or BK filled with at least 6 cc polymethylmethacrylate (PMMA) for T11-L5 levels and 3 cc PMMA for T6-T10 levels via bilateral approach with mid or long-term follow-up were included to our study. Patients were divided into two groups: BK (n: 40) and PVP (n: 15). All measurements were performed on standing lateral X-rays from the postoperative first day and the last ones that were obtained during the latest follow-up. Anterior (VHa) and posterior (VHp) heights of the index vertebrae and local kyphosis angle (LKA) were measured. Results: The decrease in the vertebral height and increasing kyphosis developing from early to late postoperative periods were found to be statistically significant in the BK group (p < 0.05). Furthermore, anterior parts of the vertebral bodies are much more affected in terms of the percentage of change. Conclusion: Our study is unique since it has the longest follow-up in the literature comparing BK and PVP in terms of recompression of the augmented vertebrae. Our study demonstrate that BK does not prevent height loss of the augmented vertebral bodies in mid-long term.
2036
A105: Thoracolumbar burst fractures (AO Spine A3, A4) in neurologically intact patients achieve minimal disability more quickly when treated surgically versus non-surgically
Marcel Dvorak 1 , Cumhur Oner 2 , Alexander Vaccaro 3 , Lorin Michael Benneker 4 , Shanmuganathan Rajasekaran 5 , Mohammad El-Sharkawi 6 , Eugen Cezar Popescu 7 , Jin Tee 8 , Jerome Paquet 9 , John France 10 , Richard Allen 11 , William Lavalle 12 , Miguel Hirschfeld 13 , and Spyros Pneumaticos 14
1 Department of Orthopaedic Surgery, University of British Columbia, Vancouver, Canada
2 University Medical Center, Utrecht, The Netherlands
3 Rothman Institute, Thomas Jefferson University Hospital, Philadelphia, United States
4 Spine Unit, Sonnenhof Spital, University of Bern, Bern, Switzerland
5 Department of Orthopaedics and Spine Surgery, Ganga Hospital, Coimbatore, India
6 Department of Orthopaedic and Trauma Surgery, Assiut University Medical School, Assiut, Egypt
7 Prof. Dr. N. Oblu” Emergency Hospital, Iasi, Romania
8 Department of Neurosurgery, National Trauma Research Institute (NTRI), The Alfred Hospital, Melbourne, Australia
9 Department of Neurosciences, CHU de Québec - Université Laval Research center, Quebec, Canada
10 Department of Orthopaedic Surgery, West Virginia University, Morgantown, United States
11 Department of Orthopaedic Surgery, University of California, San Diego, United States
12 Department of Orthopedics, SUNY Upstate Medical University, Syracuse, United States
13 Orthopedic Surgery and Traumatology, HC Marbella, Marbella, Spain
14 Department of Orthopaedic Surgery, KAT Hospital, Kifisia, Greece
Introduction: A prospective multi-center cohort analysis investigated the clinical outcomes of surgical (Sx) and non-surgical (NSx) treatment alternatives for patients with A3/A4 thoracolumbar fractures in neurologically intact patients. Although Sx and NSx treatments are both acknowledged to yield generally comparable mid to long term clinical outcomes, we hypothesized that Sx may achieve earlier clinically relevant improvement in the Oswestry Disability Index (ODI) during the first year after injury than NSx. Although individual investigators expressed preference for either Sx or NSx treatment, a true state of equipoise existed within the community and investigators recruiting to this study. Material and Methods: The study included AO Type A3 or A4 acute fractures on CT scan from T10 to L2 in patients aged 18 to 65 years. Patients with and without suspected PLC injury or type B injuries were included, while necessarily having an A3 or A4 fracture. Patients with any neurological deficit or other significant injuries were excluded. A patient diary assessed the ODI and indirect costs every 2 weeks until 6 month and then every second month until 2 years post-injury. Results: 14 Centres from North America, Europe, Middle East, India and Australia recruited a total of 213 patients with 130 (61%) patients treated surgically and 83 (39%) treated non-surgically. L1 was the most frequently injured level 49%. 58% of injuries were A3 while 41% were A4. As expected, some centres treated more than 90% of their recruited patients surgically, while other centres treated 90 to 100% non-surgically. Injury characteristics did not differ between centres. Patient demographics were similar in both Sx and NSx groups although females were more likely to be treated NSx (45%) than males (36%), however, the differences were statistically not significant (p value: 0.160). A Kaplan Meier analysis of time to achieve improvement in ODI to a value of less than or equal 20 (minimal disability on the ODI) was performed. Sx patients achieved this at a median of 66 days while NSx patients at 75 days. The adjusted hazard ratio of 1.33 expresses the increase in the Sx group achieving minimal disability as compared to the NSx group. At discharge 91% of surgical patients reported being somewhat, very or extremely satisfied with treatment while 81% of NSx patients were similarly satisfied. 85% of all patients were extremely or very satisfied at 2 years. Surgical patients returned to work at a mean (SD) of 90.8 (69.7) days while NSx patients returned to work at 116.5 (132.7) days. Conclusion: Surgery can shorten the time to minimal disability on ODI by an adjusted hazard ratio of 1.33. Reduced disability in the surgical group is evident at discharge up until 22 weeks postop. NSx patients report greater pain and disability at discharge and for up to 8 months after injury.
1421
A106: Traumatic thoracic fractures: how often MRI changes the fracture classification or clinical decision-making compared to CT alone?
Khulood AlRaddadi 1,2 and Mohamed Ali 2,3
1 Neurosurgery, National Neuroscience Institute, Riyadh, Saudi Arabia
2 Neurosurgery, Prince Mohammed Bin Abdulaziz Hospital, Riyadh, Saudi Arabia
3 Neurosurgery, Mansoura University, Egypt
Introduction: To determine the impact of magnetic resonance imaging (MRI) on fracture classification for thoracic spine fractures (TSFs) compared to CT alone. Material and Methods: This study was a retrospective review of 63 consecutive patients with TSFs who underwent CT and MRI within ten days of injury. Three reviewers classified all fractures according to AOSpine Classification and the Thoracolumbar Injury Classification (TLISS). Posterior ligamentous complex (PLC) injury in MRI was defined by black stripe discontinuity and in CT by the presence of vertebral body translation, facet joint malalignment, horizontal laminar or spinous process fracture, and interspinous widening. The proportion of patients with AO type A/B/C and with TLISS < 5 and ≥ 5 was compared between CT and MRI. We examined the overall accuracy and individual CT findings for PLC injury. Results: AO classification using CT was as follows: type A in 35 patients (55%), type B in 18 patients (28.5%), and type C in 10 patients (16%). Thirty-two patients (51%) had a TLISS ≥ 5, while the remaining 31 (49%) had TLISS < 5. The addition of MRI after CT changed the AO classification in 10 patients; which all were upgraded from type A to type B and all have changed TLISS from <5 to ≥5. Conclusion: CT was highly accurate (89%) for diagnosing of PLC injury in TSFs. The addition of MRI after CT changed the AO classification and/or TLISS, compared to CT alone, thus suggesting a high added value of MRI for PLC assessment for TSFs classification.
500
A107: The impact of construct length on outcomes for Type B and C cervical and thoracolumbar fractures
Jeremy Heard 1 , Mark Lambrechts 1 , Yunsoo Lee 1 , Nicholas D'Antonio 1 , Delano Trenchfield 1 , Parker Brush 1 , Tariq Issa 1 , Azra Dees 1 , Bright Wiafe 1 , Jose Canseco 1 , Christopher Kepler 1 , Alan Hilibrand 1 , Alexander Vaccaro 1 , Klaus Schnake 2 , and Gregory Schroeder 1
1 Department of Orthopedic Surgery, The Rothman Orthopedic Institute at Thomas Jefferson University Hospital, Philadelphia, United States
2 Center for Spinal and Scoliosis Surgery, Malteser Waldkrankenhaus St. Marien, Erlangen, Germany
Introduction: The AO Spine Classification was developed to provide a common language for discussing traumatic spinal injuries and addressing the pitfalls of previous classification systems. For patients undergoing operative management, construct length plays a vital role in patient outcomes. Although older literature has demonstrated that short constructs do not ensure adequate stability, this conclusion is limited by inadequate sample sizes and recent advancements in instrumentation. Hence, our study objectives are to (1) identify if construct length affects the rate of surgical complications and instrumentation revision following surgical reduction and fixation of subaxial and thoracolumbar Types B and C fractures; (2) determine the impact of fracture type B or C on surgical outcomes; (3) determine the impact of a diagnosis of AS/DISH on surgical outcomes. Methods: Patients were divided based on the number of vertebrae instrumented above and below the injured level (spanning > 5 vertebrae versus < 5 vertebrale). All operations were a posterior or combined anterior-posterior approach. Patient demographics, surgical characteristics, clinical outcomes, and changes in kyphosis were collected and compared. Independent t-tests or Mann-Whitney U tests compared continuous variables, while Pearson’s chi-square tests compared categorical variables. Bivariate logistic regression measured the effect of fixation construct length on the likelihood of having a surgical complication and reoperation for instrumentation revision and/or exchange. Alpha was set at p < 0.05. Results: 63 cervical and 45 thoracolumbar fractures were treated with constructs spanning < 5 vertebrae, while 28 cervical and 41 thoracolumbar were treated with constructs spanning > 5 vertebrae. For cervical fractures patients treated with constructs spanning < 5 vertebrae were younger than patients treated with constructs spanning > 5 vertebrae (52.4 ± 20.9 vs. 68.2 ± 17.0, p < 0.001). There were no significant differences in age for thoracolumbar fracture patients (p = 0.069). For cervical fractures, construct length did not impact magnitude of kyphotic angle change (3.98 ± 5.08 vs. 3.96 ± 4.26, p = 0.994), surgical complications (4.76% vs. 7.14%, p = 0.641), or surgical hardware revision/exchange (3.17% vs. 10.7%, p = 0.167). For thoracolumbar fractures, construct length did not impact magnitude of kyphotic angle change (6.04 ± 10.6 vs. 5.16 ± 5.13, p = 0.777), surgical complications (8.89% vs. 14.6%, p=0.508), or surgical hardware revision/exchange (0.00% vs. 4.88%, p = 0.224). Cervical Type B fractures had a significantly higher increase in kyphosis than type C fractures (5.26 ± 4.32 vs. 0.80 ± 3.58, p = 0.008). For cervical and thoracolumbar fractures, a diagnosis of AS/DISH was unrelated to an increase in kyphosis (p = 0.390 and p = 0.508, respectively), surgical complications (p = 0.621 and p = 1.000, respectively), or surgical hardware revision/exchange (p = 0.139 and p = 1.000, respectively). The multivariable analysis determined that constructs spanning >5 levels were not significantly predictive (p = 0.114, p = 0.191, and 0.989) of surgical complications, surgical hardware revision/exchange, or an increase in kyphosis. Conclusion: Unstable spinal fractures, type B and C, are treated with surgical reduction and fixation. Constructs spanning <5 vertebrae have similar surgical outcomes and change in kyphosis to those spanning >5 vertebral segments. Type B cervical fractures are less likely to maintain sagittal radiographic alignment than type C cervical fractures.
531
A108: Predictive algorithm to guide decision making in thoracolumbar burst fracture without neurological deficits
Charlotte Dandurand 1 , Nader Fallah 1 , Cumhur Oner 2 , Klaus Schnake 3 , and Marcel Dvorak 1
1 University of British Columbia, Vancouver, Canada
2 The University Medical Center Utrecht, The Netherlands
3 Malteser Waldkrankenhous St Marien, Erlangen, Germany
Introduction: Artificial intelligence (AI) has gained a lot of recent interest in the medical community. However, the use of predictive modeling remains an emerging field. Predictive analytic algorithms use complex modeling to interpret data to identify correlations, which would not be perceived by researchers using typical statistical models. A recent literature review summarized the use of predictive analytic modeling in spine surgery for complications, opioid usage and patient-reported outcomes1. Predictive analytic modeling has not previously been used to guide treatment decision-making in thoracolumbar burst fractures. Building such model is crucial in reducing the variability in decision making. The goal of this study was to build a mathematical prediction rule to guide treatment consensus in thoracolumbar burst fractures without neurological deficits. The purpose of this new model would be to define new scoring system to aid decision making. Material and Methods: The AO Spine Knowledge Forum Trauma completed recruitment for a prospective observational study of TL Fractures; the AO Spine A3/A4 study. The baseline CT scans and plain radiographs of 183 patients who were recruited to participate in this study were available. All patients were neurologically intact and had injuries between T11 and L2. Twenty-two expert surgeon from the AO Knowledge Forum Trauma reviewed the 183 cases. For each case, the expert spine trauma surgeons were asked to classify the fracture, provide a degree of certainty of posterior ligamentous complex (PLC) injury, evaluate the degree of comminution and provided treatment recommendation. Classification and regression trees were used to create predictive models. The methods used here are machine-learning methods for developing predictive models. We applied the decision tree model which accounts for the possibility of non-normal distributions of data. Several cross-validation techniques were used to validate the multivariate analyses. P-values of 0.05 were considered statistically significant. Results: Variables included in the algorithm were certainty of PLC injury, degree of comminution (%) and the use of M1 modifier. The algorithm suggested that a patient with a certainty of PLC injury over 57.5% had a 97.0% chance of receiving surgery. A patient with degree of comminution over 47.5%, certainty of PLC injury over 47.5% and the use of M1 modifier had 88.0% chance of receiving surgery. A patient with degree of comminution less than 17.5%, certainty of PLC injury less than 57.5% and absence of M1 modifier had 97.4% chance of being treated non surgically. Conclusion: This study presents a predictive analytic algorithm to guide decision-making in the treatment of thoracolumbar burst fractures without neurological deficits. The model identified cut-off points used by expert spinal trauma surgeons for treatment recommendation. This new knowledge will be key to the creating of new scoring system and guidelines.
OP13: MIS Lateral Approach
1138
A109: Reproducibility of implant positioning during prone lateral interbody fusion (LIF): does bed rotation result in increased variability of interbody placement?
Ashish Patel 1 , Michael Rogers 2 , Samantha Leide 3 , Jahangir Asghar 2 , Alfredo Guiroy 4
1 Spine Surgery, Duly Health and Care, Naperville, United States
2 Spine Surgery, Elite Spine Health and Wellness, Plantation, United States
Introduction: Performing a LIF in the prone position (p-LIF) has recently gained interest. Visualization of the surgical corridor may be difficult when in the perfectly orthogonal position. Several tools exist to mitigate this issue, including navigation, endoscopic cameras, and rotating the bed. During p-LIF, the bed can be rotated for better ergonomics and improved visualization. Although beneficial, bed rotation introduces variability that can cause implant malpositioning in the disc space or injury to neurovascular structures. Materials and Methods: Bed rotation was implemented with the surgeon in the seated position until optimal visualization was obtained. By our 25th case, we implemented a process to anchor the retractor in a perfectly orthogonal position prior to bed rotation. The retractor handles were placed 90degs to the vertebra as confirmed on AP and lateral fluoroscopy. The handles were then used as the referencing tool for all disc prep and final implant positioning. Postoperatively, all patients obtained a fine CT scan to assess the implant position within the disc space. Results: There were 92 patients with 126 levels treated. Implants were placed at L1-2 (6%), L2-3 (31%), L3-4 (51%), and L4-5 (66%) of the time. Average bed rotation was 7.5degs (min-max 5-10 degs) away from the surgeon to optimize line of sight. Average implant position was 3.6degs (min-max 0.1-18.1 degs) relative to orthogonal. There was a significant reduction in implant rotation with increasing experience (4.8degs 1st ⅓, 3.6 degs 2nd ⅓ 2.8 degs 3rd ⅓) (p < 0.05). In the first 25 levels, there were two incidents of unintentional anterior longitudinal ligament (ALL) rupture and one revision surgery performed for implant malposition causing contralateral nerve root irritation. After implementation of the new process to anchor the retractor, there were no further ALL ruptures or revisions for implant malposition. There were no incidents of vascular injury, bowel injury, or permanent nerve injury. Conclusion: Our findings demonstrate an initial learning curve for optimal implant position in the disc space during a p-LIF when rotating the operative bed. After developing a referencing system to aid in maintaining orthogonal alignment to the disc space, there was a significant improvement in satisfactory implant position and a reduction in technical complications. The average margin of error improved to less than ± 3 degs. Our study describes a reproducible fluoro-based technique to ensure orthogonal interbody work during prone-LIF while rotating the table.
1747
A110: Minimally invasive lateral retropleural approach for giant calcified thoracic disc herniation
Chun-Po Yen 1 , Peter Christiansen 2 , Juan Pablo Sardi 1 , Tolga Sursal 1 , and Justin Smith 1
1 Neurological Surgery, University of Virginia, Charlottesville, United States
2 Neurosurgery, Southern California Permanente Medical Group, Charlottesville, United States
Introduction: Minimally invasive lateral retropleural approach to remove symptomatic thoracic disc herniations (TDH) has gained popularity recently. However, its role in treating giant calcified TDH remains to be investigated. Material and Methods: Giant calcified TDH are defined as thoracic disc herniations with a calcified component occupying more than 40% of the anteroposterior diameter of the spinal canal. These disc herniations are notorious for their high risk of spinal cord damage and cerebrospinal fluid (CSF) leakage when surgical removal is conducted. Sixteen patients who underwent minimally invasive lateral retropleural diskectomy for giant calcified TDH comprised this study. Efforts were made to remove the disc herniations in entirety. However, if there was a lack of separable plane between the disc and dura due to severe adhesion, the calcified disc was debulked, and a high-speed burr was used to shave the disc leaving a thin shell of the calcified disc to prevent spinal cord injury or CSF leak. Results: Eight males and eight females with a mean age of 56.7 years (mean 40 to 72 years) comprised the clinical cohort. Five patients presented with medically intractable axial back pain and radicular chest wall pain, and 11 with myelopathy. All patients underwent lateral diskectomy with the techniques described earlier. All disks were adequately removed. The mean hospital stay was 5 days. There was no mortality or new neurological deficits. The mean follow-up was 16 months. Nurick grades improved on average from 3.4 to 1.1 in patients with myelopathy. Patients with back and radicular pain resolved completely (4 patients) or improved significantly (1 patient). In 12 patients, the disc was removed entirely. In 4 patients, a thin shell of the calcified disc was left attached to the dura. In one patient, there was a large dural defect following the disc removal. The defect was repaired with muscle graft and tissue sealant, and a lumbar drain was placed. No CSF leak was encountered in this patient postoperatively. One patient developed pneumonia that required treatment; one had temporary pleural effusion that resolved without intervention. Two patients developed post-thoracotomy chest pain that required an intercostal nerve block. Conclusion: Surgical treatment of giant calcified TDH poses a unique challenge to spine surgeons. The minimally invasive lateral retropleural approach is safe and effective to address giant calcified TDH with good outcomes and a low complication rate.
333
A111: Prospective study to compare the outcomes of TLIF vs OLIF in treatment of degenerative lumbar pathologies
Ayush Sharma 1
1 Spine Surgeries, Dr B R Ambedker Hospital, Mumbai, India
Introduction: Oblique lumbar interbody fusion (OLIF) and minimally invasive transforaminal interbody lumbar fusion (MIS-TLIF) are the two most popular minimally invasive fusion techniques for lumbar spine. The aim of the study was to compare the radiological and functional outcomes of OLIF vs MIS-TLIF in fusion surgery for degenerative lumbar pathology. Results: 46 OLIF and 156 MIS-TLIF patients with more than one year follow up were included in final analysis. On comprising the VAS and ODI scores both OLIF and MIS-TLIF group shows significant improvement without any significant statistical difference at 3 months, 6 months and one year follow up. Similar no difference was observed between the two groups in terms of hospital stay, Duration of surgery and intraoperative blood loss. While comparing the correction in coronal and sagittal imbalance OLIF groups showed significant better correction in scoliosis and PI-LL (Pelvic incidence and lumbar lordosis) mismatch .The mean correction in scoliosis was 12 degrees in OLIF group com compared to 4 degrees in MIS-TLIF (p = 0.01) similarly the mean correction in PI-LL mismatch was 10.09 degrees for OLIF patients compared to 6.8 for MIS-TLIF (p = 0.03).Return to work after surgery in days was significant faster for OLIF group with p = 0.002. Conclusion: Both OLIF and MIS-TLIF can result in significant improvement in VAS and ODI scores after lumbar interbody fusion for degenerative lumbar pathology. OLIF surgery results in better correction of sagittal and coronal imbalance and faster return to work compared to MIS-TLIF.
1127
A112: A retrospective review of 145 prone lateral lumbar interbody fusion cases: a single surgeon experience
Ashish Patel 1 , Michael Rogers 1 , and Eshan Doshi 1
1 Spine Surgery, Duly Health and Care, Naperville, United States
Introduction: Lateral lumbar interbody fusion (LLIF) allows for indirect decompression of central and foraminal stenosis, restoration of lordosis, and anterior fusion during surgical treatment of lumbar degenerative pathologies. Performing a LLIF in the prone position (p-LLIF) has recently gained popularity due to the substantial improvement in time under anesthesia and cost efficiency of avoiding the flip from the traditional lateral decubitus to the prone position for decompression/osteotomy or placement of screws. We performed a retrospective look at our data and report complications. Material and Methods: A retrospective chart review was conducted including intraoperative and perioperative data from patients who underwent p-LLIF from May 2019 to September 2022. Results: Our experience included a total of 233 interbody levels in 145 patients with an average age of 66.7 years. There were 86 single-level (59%), 34 two-level (23%), 21 three-level (14%), and 4 four-level (2%) surgeries performed. The average BMI for single-level surgery was 30.3 kg/m2 (min-max 17.2-50.3). Ninety-four patients (40%) underwent a prone lateral lumbar interbody fusion (p-LLIF) inclusive of the L4-5 level. Four corpectomies and four anterior column reconstructions were performed. One hundred and forty-one (141) patients had concomitant posterior work completed. The average surgical time for a single-level surgery was 89mins (min-max 40-185), with an average length of hospital stay of 1.8days (min-max 0-7; SD = 1.5), and an average estimated blood loss of 61 mL (min-max 20-300). There were 2 cases of an unintentional anterior longitudinal ligament (ALL) rupture requiring interbody with plate fixation and 3 cases of femoral nerve palsy, 2 of which recovered fully at 6weeks, and a single case that improved to 4/5 at one-year post-op. There was 1 case of revision for implant malposition impinging on the contralateral foramen. There were no cases of vascular, bowel, or complete spinal cord/root/plexus injury. Conclusion: Our single surgeon experience data demonstrates the utilization of the p-LLIF technique in treating single and multilevel degenerative disease of the lumbar spine. In addition, our data demonstrates a length of hospital stay and complication profile like that of a traditional LLIF performed in the lateral decubitus position. Further long-term studies are required to understand the complete utility of this approach and the benefits of widespread adoption. Nevertheless, early data demonstrates a substantial improvement in surgical time by avoiding the need for prone repositioning.
1034
A113: Clinical outcomes, MRI evaluation and prognostic factors of indirect decompression with lateral transpoas approach for lumbar interbody fusion: a multicenter experience
Salvatore Petrone 1 , Marco Ajello 2 , Nicola Marengo 2 , Marco Bozzaro 1 , Alessandro Fiumefreddo 2 , Alessandro Pesaresi 2 , Mario Allevi 2 , Fulvio Tartara 3 , giuseppe di perna 4 , Daniele Armocida 5 , Alessandro Pesce 6 , Alessandro Frati 5 , francesco zenga 2 , Diego Garbossa 2 , and Fabio Cofano 2
1 Spine Surgery Unit, Humanitas Gradenigo, Turin, Italy
2 Unit of Neurosurgery, AOU Città della Salute e della Scienza, Turin, Italy
3 Neurosurgery, Istituto Clinico Città Studi, Milan, Italy
4 Spine Surgery Unit, Casa di Cura Città di Bra, Bra, Italy
5 Neurosurgery Unit, University Sapienza of Rome, Rome, Italy
6 Neurosurgery Unit, Ospedale Santa Maria Goretti, Latina, Italy
Introduction: The effect of indirect LLIF decompression through the improvements of radiographic parameters is demonstrated. However, some cases which required second surgery due to insufficient indirect decompression due to central residual canal stenosis or lateral bone recess stenosis are reported. The goals of the study are to evaluate effect of LLIF indirect decompression by radiological parameters on MRI-scans and find a correlation between indirect decompression and clinical improvements and to identify predictors of better decompression and clinical outcome. Material and Methods: Radiological signs of indirect decompression were obtained evaluating modifications in preoperative and follow-up MRI studies and were subsequently correlated to clinical data, expressed as axial/radicular pain (VAS back/leg), index of disability (Oswestry Disability Index) and clinical severity of lumbar stenosis (Swiss Spinal Stenosis Questionnaire). Results: 72 patients were enrolled. The mean follow-up period was 24 months. Significantly differences in the vertebral canal (p < 0.001), area and height of the foramina (p < 0.001), thickness of the yellow ligament (p = 0.001) and anterior height of the interbody space (p = 0.02) were observed. Older age (p = 0.042), presence of spondylolisthesis (p = 0.042), presence of facetary intra-articular effusion (p = 0.003) and the posterior height of the interbody fusion cage (p = 0.020) positively affected the increase of the canal area. Change in root canal area (p < 0.001), the height of the implanted cage (p = 0.020) and younger age (p = 0.035) were predictive factors of improvement of root pain, while improvement of vertebral canal area (p = 0.020) and height of the interbody fusion cage (p = 0.023) positively affected the severity of clinical stenosis. Conclusion: The indirect decompression obtained by LLIF showed both clinical and radiological improvements in patients with stenosis. The presence and degree of spondylolisthesis, the presence of intra-articular facetary effusion, the age of the patient and the height of the cage were predictive factors of major clinical improvements.
1134
A114: A magnetic resonance imaging (MRI) analysis of nerve location within anterior psoas muscles in patients who underwent LLIF at L4-L5
Michael Rogers 1 , Ashish Patel 1 , Jonathon Garrett 1 , Jahangir Asghar 2 , and Alfredo Guiroy 2
1 Spine Surgery, Duly Health and Care, Naperville, United States
2 Spine Surgery, Elite Spine Health and Wellness, Plantation, United States
Introduction: The lateral lumbar interbody fusion (LLIF) technique accesses the anterior column through a retroperitoneal transpsoas corridor. Understanding the location of relevant neurovascular structures, foremost the lumbar plexus, as they course through the psoas muscle can reduce the risk of surgical complications and patient morbidity. The researchers in this study analyzed psoas and plexus morphology in patients who underwent LLIF at L4-L5 and discussed relevant clinical applications and complications. Material and Methods: We retrospectively reviewed preoperative lumbar spine MRIs on 78 patients who underwent LLIF at the L4-L5 level. Starting cranially, the L2 nerve was traced caudally through the psoas until the L4-L5 level. The distance from the anterior aspect of the nerve to the posterior vertebral body was measured. The location of the nerve was reported as a percentage of the vertebral body. The most posterior aspect of the vertebral body was labeled 0% and the anterior aspect 100%. Vertebral rotation was taken into account for all measurements. Results: Seventy-eight (78) patients (37.2% male, 62.8% female) with an average age of 67 years were included. The average vertebral rotation was 0.4deg clockwise (-7.6-8.7deg). The average psoas muscle stretched 105.5% anteriorly from the posterior edge of the vertebral body (min-max: 70-153%). On average, the nerve in the plexus was at 34.8% (3-67%). Forty-six (46/78 = 59%) patients had a psoas muscle extending anterior to the vertebral body with an average distance of 116% (100-153%). The average location of the nerve in an anterior psoas was 37.6% (12-67%) vs. not anterior psoas 30.9% (7.6-48%; p < 0.05). Three patients in this study presented with postoperative neuropraxia, two of which resolved to normal preoperative strength at 6 weeks while one resolved to 4/5 strength at one-year postoperative. For the complication group, the average psoas stretched 115% of the vertebral body (102-133%), and the average nerve location was 41% (39-43%). Conclusion: The foremost clinical application to understanding the anatomy of the lumbar plexus as it courses through the psoas muscle is to minimize surgical complications and patient morbidity when performing a LLIF. The results of this study show a statistically significant difference in nerve location in patients with and without an anterior psoas, although the authors argue its clinical application due to the relatively small average ventral increase (2.8mm) between the two groups. Postoperative neuropraxia was exclusively seen in patients with an anterior psoas (3/46 = 6.5%). However, more patients with an anterior psoas who underwent LLIF did not present with neuropraxia (43/46 = 93.5%). Further studies are underway to delineate the timing of these injuries during surgery by utilizing transabdominal muscle action potentials (TMAP).
2038
A115: Clinical and Radiologic Outcomes of Single and Double Level O-arm versus C-arm Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS-TLIF) for Degenerative Spondylolisthesis
Kia Teng Lim 1 , Alagan Gnanam 1 , Youheng Ou Yang 2 , Rui Xiang Toh, and Reuben Soh 2
1 Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
2 Department of Orthopaedic Surgery, Singapore General Hospital, Singapore, Singapore
Introduction: O-arm navigated minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) has been shown to increase both interbody cage and pedicle screw placement accuracy compared to C-arm guided placement. However, patient reported outcome measures (PROMs), clinical and radiologic outcomes have not been compared in a head to head fashion. This study aims to compare long-term clinical and radiologic outcomes between O-arm and C-arm MIS-TLIF. Material and Methods: This was a single-site, single-surgeon retrospective study. 95 patients with spondylolisthesis who underwent single or double level MIS-TLIF were included (n = 79 O-arm, n = 16 C-arm). Surgical outcomes, functional and radiographic changes over 2 years were analysed. Results: No significant differences were shown for operative time per level in O-arm (3.06 ± 0.86h) versus C-arm (2.82 ± 0.70h) (p = 0.30). C-arm patients had a shorter time to ambulation (1.08 ± 0.277 days versus 1.329 ± 0.614 days, p = 0.02). Differences in intraoperative blood loss (231.41 ± 171.96mLs versus 130.00 ± 115.95mLs, p = 0.08), drop in haemoglobin levels from pre-operative to post-operative day 1 (1.99 ± 1.12g/dL versus 1.69 ± 1.08g/dL, p = 0.33), duration of hospitalization stay (5.96 ± 3.96 days versus 6.38 ± 4.99 days, p = 0.73) and time to stairs (4.67 ± 7.58 days versus 2.75 ± 0.89 days, p = 0.48) were similar between O-arm and C-arm. O-arm demonstrated lower superficial infection rates (n = 3, 3.85%) versus C-arm (n = 4, 25%, p < 0.01). There were no deep infections. 4 O-arm patients underwent revision surgeries. O-arm patients showed significantly greater improvement in VAS lower limb pain at 1,3,6 months post-surgery (p < 0.01), leg pain symptom frequency at 1,3,6 months post-surgery (p = 0.01) and RAND-36 Social Function 24 months after surgery (p < 0.01). The improvement in VAS lower back pain and back pain were higher in C-arm than O-arm 3 months post-surgery (2.36 ± 1.55 versus 2.09 ± 2.26, p < 0.01; 5.29 ± 3.25 versus 4.23 ± 4.12, p < 0.01) but changes were insignificant at 24 months. Both groups demonstrated largely equal maintenance of post-operative sagittal alignment across all time points, except for change in L4/5 lordosis at 3 months (0.85° ± 5.40 in O-arm versus -13.00° in C-arm, p = 0.01). The most significant mean difference in L3/4 lordosis were found to be at the immediate post-operative period for both O-arm (-6.04° ± 6.46) and C-arm (-8.81°). For L4/5 lordosis, O-arm patients experienced most significant change around the 3 months (0.85°±5.40) to 6 months period (-0.71° ± 6.03). Changes in lordosis in C-arm patients remained relatively constant from immediate post-operative period (-2.53° ± 6.74) to 1 year (-2.04° ± 11.54) before decreasing at 2 years (0.77° ± 6.05). For L5/S1 lordosis, O-arm patients had most significant change at the immediate post-operative period (-0.79° ± 6.62), which remained similar at 2 years follow-up (-0.51° ± 11.41). C-arm patients showed a gradual decrease in L5/S1 lordosis from immediate post-operative period (1.04° ± 8.19) to 1 year post-surgery (3.12° ± 9.36). The incidences of cage migration and subsidence were significantly lower in O-arm patients than C-arm (0.00% versus 12.50%, p < 0.01; 1.35% versus 18.75%, p < 0.01). End-plate perforation rates were insignificant (3.80% versus 18.75%, p = 0.19). Radiographic fusion was achieved in 74.00% for O-arm by 2 years and 85.71% C-arm (p = 0.36). Conclusion: O-arm MIS-TLIF is superior in the area of PROMs, post-operative complications and functional outcomes compared to C-arm. Accuracy of implant placement aided by intra-operative navigation ensures reduced cage subsidence rates, but lordosis restoration was equal in both groups.
1584
A116: Lateral lumbar interbody fusion with percutaneous pedicle screw fixation: are we getting the sagittal alignment right?
Breana Siljander 1 , Nicholas Dick 1 , Austin DeBoer 1 , Jason Haselhuhn 1 , Paul Soriano 1 , J. Alex Thomas 2 , and Jonathan N. Sembrano 1
1 University of Minnesota, Minneapolis, United States
2 Atlantic Neurosurgical and Spine Specialists,, Wilmington, United States
Objective: This study evaluated the efficacy of lateral lumbar interbody fusion with percutaneous pedicle screw fixation (LLIF-PPS) in restoring or maintaining optimal sagittal alignment. The aim of this study was to compare pre- and post-operative standing lateral radiographs of patients who underwent LLIF-PPS to determine if sagittal alignment goals were met, including (1) PI-LL < 10°, (2) PT < 20°, and (3) L4-S1 > 60% of PI. Methods: 84 patients who were treated with LLIF for degenerative spinal conditions using the extreme lateral interbody fusion system were retrospectively reviewed. Standing lateral radiographs obtained between 6 and 12 weeks pre- and postoperatively were analyzed. Standard sagittal measurements were made and compared to the following alignment goal criteria: (1) PI-LL < 10°, (2) PT < 20°, and (3) L4-S1 > 60% of PI. The frequency that each of three sagittal alignment criteria was met in pre- and postoperative radiographs was recorded. Demographic data including age, sex, body mass index, and spinal diagnosis was also collected. Results: A total of 115 levels were treated. There was no significant difference between the proportions of patients meeting each alignment goal preoperatively versus postoperatively after LLIF-PPS (p > 0.05). The mean number of alignment goals met was higher preoperatively (1.7, SD 1.1) than postoperatively (1.5, SD 1.2) (p = 0.03). Compared to the preoperative state, 42 patients (51%) met the same number of alignment goals, 14 patients (17%) met more goals, and 26 patients (31%) met fewer goals. Conclusions: Our results show no difference in the number of patients who met specific alignment goals before and after LLIF-PPS surgery. These findings suggest that patients with preoperative sagittal malalignment may require additional procedures such as a posterior column/3-column osteotomy, involvement of L5-S1, or proximal extension to the thoracic spine if more significant correction of lordosis is desired. Thus, a mal-aligned spine cannot be reliably corrected to optimal sagittal alignment by LLIF-PPS alone.
397
A117: Does posterior column osteotomies increases segmental lordosis vs prone lateral lumbar interbody fusion without osteotomy?
Alfredo Guiroy 1 , Daniel Benson 2 , and Jahangir Asghar 1
1 Spine Surgery, Elite Spine Health and Wellness Center, Fort Lauderdale, United States
2 Elite Spine Health and Wellness Center, Fort Lauderdale, United States
Introduction: Prone lateral lumbar interbody fusion (pLLIF) offers a minimally invasive (MIS) option to achieve indirect decompression, disc height restoration, coronal correction, and fusion in degenerative pathologies with potential for improved lordosis restoration compared to a traditional LLIF. Posterior column osteotomies (PCO) are often used as a mechanism for lordosis restoration by shortening the posterior elements. However, the simultaneous use of PCO with LLIF in the prone position has not been studied yet. To evaluate the amount of lordosis correction with pLLIF with and without posterior column osteotomies. Material and Methods: We reviewed the charts of the patients operated on for degenerative pathologies using an LLIF in a single prone position from January 2019 to July 2021. Demographics, radiological and surgical variables were explored in order to evaluate the amount of lordosis obtained in both groups (with and without PCO) and complications. Results: 94 levels in 58 patients underwent an LLIF with posterior screws (n = 38, single level; n = 16, 2-levels; n = 8, 3-levels) in prone lateral single position over a course of 18 months. The pLLIF were divided into 2 groups: 69 Levels with PCO and 25 without it. All patients with PCO had prior posterior surgery. In both groups, there were no significant differences in mean implant sizes, and length of stay was similar in both groups. Overall segmental lordosis correction of both groups was an average of 8.8 degrees. However, the PCO group was significantly greater than the none PCO group (5.4 degrees vs 10.6: p = 0.037). Complications for the LLIF + PCO were one anterior longitudinal ligament rupture that required lateral plating and one return to OR for secondary stenosis secondary to angular correction. The overall rate of thigh dysesthesias was 12.7%, with no differences in the groups. Conclusion: We found that navigated pLLIF with simultaneous PCO significantly increased segmental lordosis and can be utilized as an intermediate adjunct to anterior column realignments (ACR) and pedicle subtraction osteotomies (PSO). As with all osteotomies, it is important to recognize the capacity to destabilize or create a secondary stenosis.
OP14: Adult Deformity 2
1000
A118: Comparing the post-operative changes in sacro-pelvic parameters after adult spine deformity surgery according to the type of pelvic fixation
Zhi Wang 1 , Ghassan Boubez 1 , Daniel Shedid 2 , Sung-Joo Yuh 2 , Jesse Shen 1 , Bilal Tarabay 2 , Fidaa Al-Shakfa 3 , Yousef Kamel 4 , Jia Liu 4 , and Maroun Rizkallah 1
1 Orthopedic Surgery
2 Neurosurgery Department
3 Centre de Recherche, Centre Hospitalier de l'Universite de Montreal, Montreal, Canada
4 Ecole de Medecine, Universite de Montreal, Montreal, Canada
Introduction: Recent studies suggest that changes occur to the previously assumed fixed pelvic incidence (PI) after spino-pelvic fixation and fusion. However, the differential impact of the type of pelvic fixation: S2-alar-iliac screws (S2AI) versus iliac screws (IS) on the PI and subsequently on the remaining pelvic parameters and sagittal balance was never evaluated. Material and Methods: This retrospective monocentric study included adult spine deformity (ASD) patients who underwent surgical correction and spino-pelvic fixation with ≥ 3 levels fusion. Standing whole body lateral EOS imaging was performed pre-operatively and within 3 months post-operatively for all included patients. Pre-operative and post-operative PI, lumbar lordosis (LL), thoracic kyphosis (TK), pelvic tilt (PT), sacral slope (SS), PI-LL mistmatch and the Sagittal Vertical Axis (SVA) were analyzed. A significant PI change was established a priori at ≥ 6⁰. Patients were categorized based on the type of pelvic fixation (S2AI vs IS). Results: A total of 142 patients with a mean age of 67.18 ± 11 years and a mean BMI of 29.98 ± 5 kg/m2 were included. Of these patients, 68 (48%) had a > 6⁰ change in their PI post-operatively. In the 50 patients with high pre-operative PI (> 60⁰), 31 (62%) had a significant PI change compared to 34 (37%) patients from the 92 patients with normal and low pre-operative PI (< 60⁰) (p = 0.01). When PI changed, it was likely to decrease in patients with high baseline PI and to increase in patients with low baseline PI. Patients in the S2AI group (n = 99) and those in the IS group (n = 43) were comparable at baseline for their pelvic and sagittal balance parameters. In the S2AI group, 46 (46%) patients had >6⁰ change in their PI compared to 23 (53%) patients in the IS group (p = 0.65). In both groups, patients with high pre-operative PI were more prone to significant post-operative change (p = 0.02 in IS, p = 0.01 in S2AI). Mean change in pre-operative to post-operative LL reached 16.8⁰ in S2AI group and 17.3⁰ in IS group (p = 0.89). Post-operative change in TK averaged 10.76⁰ in S2AI group compared to 9.89⁰ in IS group (p = 0.62). Preoperative to post-operative change in SS and PT did not differ between both groups (p = 0.23 and 0.49 respectively). Post-operative PI-LL mismatch averaged 8.8⁰ in S2AI group and 10.2⁰ in IS group (p = 0.79); while post-operative SVA reached 47mm in S2AI group and 53 mm in IS group (p = 0.83). Conclusion: This study confirms the PI could change significantly is as much as 50% of patients after spino-pelvic fixation for ASD, especially in those patients with high pre-operative PI. This occurs similarly in patients with S2AI and those with IS used for pelvic fixation. The type of pelvic fixation was not found to affect post-operative pelvic parameters nor post-operative sagittal balance despite changes in PI. Spine surgeons should keep in mind the possible post-operative significant PI change while planning the ideal LL for their patient pre-operatively as this might impact the post-operative PI-LL mismatch.
2018
A119: Geographic variation in the philosophy of adult spinal deformity management and patient outcomes: a propensity score matching analysis from the Prospective Evaluation Deformity Surgery (PEEDS) study
Kenny Yat Hong Kwan 1 , Stephen Lewis 2 , Marinus De Kleuver 3 , Yong Qiu 4 , Yukihiro Matsuyama 5 , Lawrence Lenke 6 , Ahmet Alanay 7 , Ferran Pellisé 8 , Maarten Spruit 9 , David Polly 10 , Jonathan N. Sembrano 10 , Christopher Shaffrey 11 , Justin Smith 12 , Michael Kelly 13 , Benny Dahl 14 , Sigurd Berven 15 , and Kenneth Man Chee Cheung 1
1 University of Hong Kong, Hong Kong
2 University of Toronto, Canada
3 Radboud University Medical Center, The Netherlands
4 Nanjing University Medical School, China
5 Hamamatsu University School of Medicine, Japan
6 Columbia University Medical Center, New York, United States
7 Acibadem Mehmet Ali Aydinlar University, Istanbul, Turkey
8 Hospital Universitari de la Vall d’Hebron, Barcelona, Spain
9 Sint Maartenskliniek Nijmegen, The Netherlands
10 University of Minnesota, Minneapolis, United States
11 Duke University, Durham, United States
12 University of Virginia, Charlottesville, United States
13 Rady Children’s Hospital, San Diego, United States
14 National University of Denmark, The Netherlands
15 University of California, San Francisco, United States
Introduction: Variations in radiographic disability thresholds and outcomes exist in geographical populations after adult spinal deformity surgeries. However, geographic variation in how surgeons manage these patients and how this affects outcome is unknown. Material and Methods: A total of 219 patients who had undergone surgery for adult spinal deformity were enrolled in the Prospective Evaluation of Elderly Deformity Surgery (PEEDS) study. Patients from Europe consisting of the fewest patients (14%; 31 of 219), and those in North America and Asia with incomplete baseline parameters for matching (17%; 37 of 219) were excluded, leaving 151 patients (69%) for analysis in this study from the original trial. From these 151 patients, a 1:1 propensity score matched between patients from North America and Asia was conducted using age, gender, Charlson Comorbidity Index, lumbar lordosis (LL), pelvic incidence (PI)-LL mismatch, sagittal vertical axis (SVA), absolute lumbar cobb angle, and sacral slope. The matched cohort included 41 patients in each group for a total of 82 patients (37%). Surgical details, radiological parameters, clinical outcomes using standardised HRQoL questionnaires, and occurrence of adverse events were compared between matched pairs. Results: Significant differences between regions were identified for surgical staging (p < 0.001). A greater proportion of patients in North America underwent a single stage procedure compared with those in Asia (88% versus 44%). Posterior approach with a combination of transforaminal and/or posterior interbody fusion and instrumentation was more commonly used in North America than Asia (85% versus 51%), whereas combined lateral and posterior approaches were more common in Asia than North America (49% versus 5%). Patients treated in North America had higher mean number of levels fused throughout all stages (11.5 ± 3.9 versus 9.1 ± 2.3; p < 0.004) than in Asia. No statistical difference was found in matched pairs at 2-year postoperative sagittal alignment parameters. For HRQoL scores, matched pair patients in North America had higher SRS-22r sub-total (3.8 ± 0.7 versus 3.6 ± 0.7; p = 0.03) and total scores (3.8 ± 0.7 versus 3.6 ± 0.7; p = 0.01), higher mean EQ-5D VAS (76.3 ± 17.3 versus 68.8 ± 20.0; p = 0.015). and lower mean leg pain NRS scores (1.8 ± 2.5 versus 3.3 ± 2.9; p = 0.009) at 2 year post-operatively compared with those in Asia. No difference was found in mean ODI and back pain NRS scores. The incidence of adverse events occurrence was similar in the matched pairs, except for a higher rate of deep venous thrombosis in North America (7 versus 0; p = 0.016). Conclusion: In matched pairs of patients with comparable baseline demographic and radiologic parameters, there was marked geographic variation in the surgical management of adult spinal deformity between North America and Asia. However, postoperative radiographic parameters, clinical outcomes and occurrence of adverse events were similar between the two regions. Efforts toward a deeper understanding on variation in surgical management observed between geographical regions will help to develop clearer guidelines and consensus on the management of adult spinal deformity globally.
782
A120: Resuming activity and sports after long segment fusions to the pelvis for adult spinal deformity: survey results of AO spine members
Alekos Theologis 1 , Daniel Cummins 1 , So Kato 2 , Stephen Lewis 3 , Christopher Shaffrey 4 , Lawrence Lenke 5 , Sigurd Berven 1 , and AO Spine KF Deformity 6
1 Department of Orthopaedic Surgery, University of California, San Francisco (UCSF), United States
2 Department of Orthopaedic Surgery, The University of Tokyo, Tokyo, Japan
3 Department of Surgery and Spine Program, University of Toronto, Toronto, Canada
4 Department of Orthopaedic Surgery, Duke University, Durham, United States
5 Department of Orthopaedic Surgery, Columbia University Medical Center, The Spine Hospital, New York City, United States
6 AO Spine Knowledge Forum Deformity, Switzerland
Introduction: Surgical correction of adult spinal deformity (ASD) provides meaningful improvements in quality of life. While operative strategies and associated postoperative outcomes and complications have been areas of comprehensive investigation, recommendations for when ASD patients may return to athletic activities after surgery have not been evaluated. This study aims to address this question. Materials and Methods: A web-based survey was administered to AO Spine’s members. The survey consisted of surgeon demographic information and questions asking when patients undergoing a long thoracolumbar fusion (>5 levels) with pelvic fixation for ASD would be allowed to resume unrestricted range of motion (ROM), non-contact sports, and contact sports postoperatively. Ordinal logistic regression was used to determine predictors for time to resume each activity. Results: 164 responses were included for analysis. The majority of respondents were male (98%) with fellowship training (70%) in orthopaedic surgery (80%). Respondents were mixed with regards to years in practice (< 5 yrs: 13%; 5-10 yrs: 21%; 11-15 yrs: 20%; 16-20 yrs: 19%; > 20 yrs: 27%), location of practice (North America-20%, Latin America-13%; Europe/Southern Africa-35%; Middle East/Northern Africa-10%; Asia Pacific-22%), and type of practice (Academic-56%; Public/Military-22%; Private-22%). The majority of respondents would allow unrestricted ROM within 3 months post-op [< 3 months: “immediately after surgery” (30%), “1-2 months” (25%), and “2--3 months” (24%) versus > 3 months: “3-4 months” (19%) and “> 4 months” (17%)]. Asian-Pacific region responders recommended later return to unrestricted ROM compared to European (OR = 0.28), Latin-American (OR = 0.27), and North American (OR = 0.30) respondents, p < 0.05. Other predictors of shorter return to unrestricted ROM were being fellowship trained (OR = 0.36; p < 0.05). For when to return to non-contact sports, the most common responses were “3-4 months” (29%), “6-12 months” (22%), “2-3 months” (21%), and “4-6 months” (17%). Infrequent responses were “1-2 months” (12%), “immediately after surgery” (7%), ">12 months” (5%), and “never” (2%). Asian-Pacific responders recommended later return to non-contact sports compared to European (OR = 0.33), Latin-American (OR = 0.12), and North American (OR = 0.27) respondents (p < 0.05). For when to return to contact sports, the majority advised > 6 months post-op [> 6 months: “6-12 months” (31%), “> 12 months” (34%) versus < 4 months: “1-2 months” (4%), “2-3 months” (0%), “3-4 months” (7%), “4-6 months” (19%)]. 19% responded they would “never” allow resumption of contact sports. Respondents from Asian-Pacific regions recommended later return to contact sports compared to European (OR = 0.13), Latin-American (OR = 0.04), and North American (OR = 0.08) respondents (p < 0.05). Conclusion: In this survey of AO Spine’s members, there is significant variation between surgeons’ recommendations for resumption of unrestricted range of motion and sports following long fusion with pelvic fixation for ASD. Asian-Pacific responders had the most conservative approach to return to activities following surgery. An evidence-based approach to activity recommendations will require information on outcomes and complications.
735
A121: Does coronal alignment affect patient reported outcomes for adult spinal deformity surgery? The key may be lower extremity compensation vs. decompensation
Nathan Lee 1 , Michael Fields 1 , Gerard Marciano 1 , Matthew Simhon 1 , Cole Morrissette 1 , Fthimnir Hassan 1 , Christopher Mikhail 1 , Stephen Stephan 1 , Joshua Baksheshian 1 , Andrew Platt 1 , Joseph Lombardi 1 , Zeeshan Sardar 1 , Ronald A. Lehman 1 , and Lawrence Lenke 1
1 Orthopedic Surgery, Columbia University, Och Spine Hospital, New York, United States
Introduction: Although sagittal alignment goals for adult spinal deformity (ASD) surgery and their association with patient reported outcomes (PROs) are well described, coronal alignment goals are less well understood. Some studies suggest a coronal vertical axis (CVA) goal of < 3 cm; however, there are conflicting results in regards to the association with PROs. Lower extremity changes (e.g. asymmetric knee bending, lower extremity mechanical axis differences) for coronal malalignment have yet to be described and may be important factors to consider. To the authors knowledge, this is the first study to quantify lower extremity changes in ASD patients with coronal malalignment and determine their contribution to PRO’s at 2 years postop. Material and Methods: A consecutive cohort of ASD patients with preoperative coronal malalignment (CVA ≥ 3 cm) and minimum 6 level fusion with pelvic fixation were reviewed. Excluded patients with leg length discrepancy (LLD > 1 cm) and < 2 year follow up. Patient demographics, comorbidities, baseline PROs, surgical factors, and radiographic factors (both coronal and sagittal) were collected. The outcome of interests included the minimum clinically important difference (MCID) for ODI and SRS (function, appearance, and pain). MCID threshold values were set in accordance with prior studies: −12.8 for ODI, +0.375 for SRS-function, +0.587 for SRS-pain, and +0.800 for SRS-appearance. To account for postoperative lower extremity (LE) changes, patients were categorized into 4 postoperative groups: Type 1a = No LE change AND CVA < 3 cm; Type 1b = No LE change AND CVA ≥ 3 cm; Type 2a = LE change (pelvic obliquity > 1°, asymmetric knee bending, LE mechanical axis difference (LMAD) > 2 deg) AND CVA < 3 cm; Type 2b = LE change AND CVA ≥ 3 cm. Bivariate and multivariate logistic regression were performed to determine the independent factors for the outcomes of interest. Results: 76 patients (age 58.3 ± 13.7, female 77.6%, levels fused 14.1 ± 3.9) were reviewed. Mean preop/2yr CVA 5.0 ± 1.9/2.1 ± 1.8 cm and SVA 5.7 ± 6.0/3.0 ± 3.9 cm. Patients with preop LE changes (N = 44, 57.9%) had a mean preop pelvic obliquity PO = 2.4⁰, LMAD = 4.2⁰, and 27% had asymmetric knee bending. Baseline/2yr ODI 39.3 ± 17.5 / 18 ± 17, SRS function 3.2 ± 0.9 / 3.8 ± 0.8, SRS pain 2.7 ± .9/3.8 ± 1.1, SRS appearance 2.4 ± 0.8/4.0 ± 0.9. At 2 years postop, patients with Type 2b had the lowest rate of achieving ODI MCID (1.8% vs. Type 1a = 72.7%, Type 1b = 10.9%, Type 2a: 14.6%, p < 0.01). Similarly, Type 2b had the lowest rate of SRS function MCID (10.7% vs. Type 1a = 46.6%, Type 1b = 21.4%, Type 2a = 21.4%, p < 0.01), SRS pain MCID (8.8% vs. Type 1a = 58.8%, Type 1b = 14.7%, Type 2a = 17.6%, p = 0.015), and SRS appearance MCID (5.3% vs. Type 1a = 55.3%, Type 1b = 15.8%, Type 2a = 23.7%, p = 0.016). In multivariate analysis, Type 2b was independently associated with worse ODI MCID (OR 64.6, p = 0.011). Other factors including baseline factors and 2 yr CVA, SVA, PI-LL mismatch did not remain in the final multivariate model. Conclusion: Understanding LE changes is essential in ASD patients with coronal malalignment. Postop CVA alone was not associated with PRO’s in the multivariate analysis; however, patients with LE decompensation (Type 2b = LE change with CVA ≥ 3 cm) was found to be an independent risk factor for worst PRO’s at 2 years postop.
798
A122: Does the use of monoaxial pedicle screws in caudal vertebra make a difference in management of lumbar spondylolisthesis? A propensity-matched study
Yogesh Pithwa 1 and Barath Kumar 2
1 Spine Surgery, Sattvik Spine and Scoliosis Center, Bengaluru, India
2 Orthopaedics, HOSMAT Hospital, Bengaluru, India
Introduction: Reduction of spondylolisthesis, when indicated, has been proposed using various techniques and various constructs. Though there is some literature to underscore the superiority of mono-axial pedicle screws in the management of scoliosis, there is a dearth of literature to enunciate the relative advantages of use of mono-axial screws in the management of spondylolisthesis. Material and Methods: Prospectively collected database of two groups of patients were analyzed. The study group [group 1] involved patients with single segment fixation for lumbar spondylolisthesis, with use of mono-axial pedicle screws into the caudal vertebra and polyaxial screws in the cranial listhesed vertebra. The control group [group 2] consisted of patients with single segment fixation for lumbar spondylolisthesis with use of only polyaxial screws in the entire construct. One-is-to-two nearest neighbour propensity score matching was done for multiple confounding factors including age, sex, BMI, presence of osteoporosis, smoking status, presence of disc height reduction >50% at the involved level, type of spondylolisthesis [degenerative or lytic] and length of follow-up. Statistical analysis was done for immediate postoperative correction of segmental translation as well as angulation at the involved level; loss of correction of segmental translation and angulation at last follow-up as compared to immediate postoperative status; improvement in VAS scores for leg and back pains; improvement in ODI and lastly, Odom’s criteria. Results: Fifteen patients were selected in study group while thirty were selected in the propensity-matched group. In the immediate postoperative period, statistical analysis revealed better correction of translation [p = 0.012] in the study group without any such similar advantage in improvement in lordosis. However, it was notable that the study group had better maintenance of correction of translation [p = 0.007] as well as lordosis [p = 0.003] over an identical follow-up period [mean-10.67 months], as compared to the propensity-matched group. This also reflected in better improvement in ODI scores [p = 0.02], VAS-back pain [p = 0.02], VAS-radicular pain [p = 0.02] and Odom’s criteria [p = 0.046] at last follow-up. Conclusion: In addition to better immediate intraoperative correction of translation, use of monoaxial pedicle screws in the caudal vertebra of a listhesed lumbar motion segment can allow for better maintenance of correction of translation as well as lordosis in the postoperative period. This is also likely to lead to better functional outcomes in patients. A larger multi-center study may help further validate these findings.
1871
A123: Long-term outcome of prospective evaluation of elderly deformity (PEEDS): a multi-center prospective international study on patients over 60 years of age
Stephen Lewis 1 , Lawrence Lenke 2 , Marinus De Kleuver 3 , Christopher Shaffrey 4 , Kenneth Man Chee Cheung 5 , Yong Qiu 6 , Yukihiro Matsuyama 7 , Ferran Pellisé Urquiza 8 , David Polly 9 , Jonathan N. Sembrano 9 , Benny Dahl 10 , Michael Kelly 11 , Maarten Spruit 12 , Ahmet Alanay 13 , Justin Smith 14 , and Sigurd Berven 15
1 Orthopaedic Surgery, Toronto Western Hospital, University Health Network, Toronto, Canada
2 Orthopaedic Spine, Columbia University, United States
3 Orthopaedics, Radboud University Medical Center, The Netherlands
4 Duke University, Durham, United States
5 University of Hong Kong, Hong Kong
6 Drum Tower Hospital of Nanjing University, China
7 Hamamatsu University, Japan
8 Hospital Universitari de la Vall d'Hebron, Barcelona, Spain
9 University of Minnesota, Minneapolis, United States
10 Rigshospitalet, University of Copenhagen, Denmark
11 University of San Diego, United States
12 Sint Maartenskliniek, Nijmegen, The Netherlands
13 Mehmet Ali Aydınlar University School of Medicine, Istanbul, Turkey
14 University of Virginia, Charlottesville, United States
15 University of California, San Francisco, United States
Introduction: The rate of multilevel fusion surgery for spinal deformity is increasing internationally. Understanding the outcomes of measured change in patient reported health related quality of life is important to determine the appropriateness of multilevel fusion in older adults with spinal deformity. Material and Methods: Patients ≥ 60 years undergoing ≥ 5 levels of spinal fusion from 12 international centers were prospectively enrolled and followed at 10 weeks, 1 year, 2 years, and 5 years. Indications for surgery and surgical procedures were performed at the discretion of the treating surgeon. Patient reported outcomes were analyzed using unadjusted and adjusted mixed effects regression models. Results: 219 patients of 255 enrolled met the inclusion and exclusion criteria for this study. 80.4% of patients were female with a mean age of 67.5 (60.0-83.0) years at time of index surgery. 44.3% of patients were treated in North America, 41.6% in Asia, and 14.2% in Europe. 179 (82%) patients completed 2-year and 118(54%) completed 5-year follow-up. Comparing baseline measurements to 2-years and 5-years, patients showed significant improvements in unadjusted least square means of SRS-22r (2.79 vs 3.69 vs 3.70), ODI (46.3% vs 27.0% vs 28.3%), NRS back (6.1 vs 2.6 vs 2.9), NRS leg (4.3 vs 2.3 vs 2.6), and EQ-5D (0.53 vs 0.74 vs 0.74). There were 275 recorded adverse events of which 26 occurred between 2 and 5 years. The majority of the adverse events between 2 and 5 years were implant related (n = 16). There were two peri-operative deaths, and three patients died of unrelated causes prior to the 2-year follow-up. 1 further death was recorded between 2 and 5 years. Conclusion: In this series of older patients, significant benefit was observed in multiple general and spine specific patient reported outcome scores following multilevel spinal fusions. Maximum improvement was seen at 1-year and was maintained at 2 and 5-year follow-up. Difficulties are noted in maintaining high levels of long-term follow-up data in multicenter studies even with dedicated contract research organization support.
2004
A124: Radiographic assessment following the utilization of Schwab-Grade-I posterior column osteotomy (PCO) in severe rigid kyphoscoliosis patients with curves 80 degrees or greater: two-year clinical results
Nicholas Van Halm-Lutterodt 1,2,3 , Ziyang Ye 3,4 , Aixin Pan 2 , Yangpu Zhang 2 , Lijin Zhou 2 , Jincai Yang 2 , Yuzeng Liu 2 , Tie Liu 2 , Sunny Kim 2 , and Yong Hai 2
1 School of Professional Studies, Brown University, Providence, United States
2 Department of Orthopedics Surgery, Beijing Chaoyang Hospital Affiliated Capital Medical University, Beijing, China
3 Department of Orthopedic and Neurosurgery, Inspired Spine Health, Burnsville, United States
4 Department of Analytics and Data Science, University of Chicago, Chicago, United States
Background: Frank Schwab et al. recently classified posterior column osteotomies (PCOs) into six different grades with increasing degree of aggressiveness. The Schwab-grade-1 PCO is the least aggressive osteotomy which includes Smith-Petersen osteotomy (SPO), chevron or extension osteotomies that can be used to lengthen the anterior column during spinal reconstruction. This osteotomy type has been used for mild-to-moderate forms of spinal curves and exploits primarily on anterior disc spaces for correction following posterior release and partial facetectomies. The clinical and radiographic effectiveness of this lowest osteotomy grade in the management of severe rigid kyphoscoliosis patients with curves ≥ 80o will inform spine deformity experts of the value-based impacts of its application in treating severe rigid deformities. Methods: Following approval by the institutional review board (IRB) of Beijing Chaoyang Hospital-Affiliated Capital Medical University in Beijing, a pool of 22 adult (≥18 years) severe rigid scoliosis or kyphoscoliosis patients (curves ≥ 80o) who had Schwab-grade-1 PCO as a primary corrective surgical technique from 2009 to 2014 were retrospectively evaluated. The primary outcomes included the perioperative clinical, radiographic patient-reported outcomes were evaluated at minimum 2-year, final follow-up (FFU) period. Secondary outcomes included preoperative and final follow-up ODI and SRS-22 scores. Statistical analyses were carried out by Student t-test, Mann-Whitney test, and Pearson’s Chi-squared test (Fisher’s Exact Test), through Python statistical software package. Statistical significance was set at (p < 0.05). Results: A total of 22 Schwab-grade-I treated patients were observed. The average age was 20.2 years with a female incidence of 72.73%. The etiologies were approximately 54.6% idiopathic and 45.4% congenital patients. The average body mass index (BMI) was 19.4 kg/m2. The average fusion length was 13.2 and the surgical duration was 295.5 minutes with a median blood loss volume of 750 ml. The average follow-up time was 2.8 years. The preoperative major curve Cobb angle of 102.9o was corrected to 53.6o at immediate postoperative and 53.0o at FFU, (p < 0.001). The preoperative compensatory curve Cobb angle of 53.3o was corrected to 31.85o at immediately postoperative and 31.3o at FFU, (p < 0.001). The average preoperative apical vertebral translation (AVT) of 10.28-cm was corrected to 4.6-cm at FFU, (p < 0.001). The averages of preoperative thoracic kyphotic (TK) and lumbar lordotic (LL) angles of 65.9o and 67.9o were corrected to 39.7o and 52.4o at FFU, respectively, (p < 0.001). The average vertical axes of coronal (CVA) and sagittal (SVA) outcomes demonstrated that normal alignment was achieved in these patients. Major curve corrective rate was 51.5% at FFU. The ODI and SRS-22 scores significantly improved from baseline at FFU, (p < 0.01). Conclusion: In this current study, we clearly appreciate Schwab-grade-I PCO as an effective posterior-only surgical approach for spinal reconstruction in patients with severe rigid scoliosis and kyphoscoliosis phenotypes. The clinical and patient-reported outcomes depicted in this study highlight the clinical value and patient benefits associated with Schwab-grade-I PCO for complex spine reconstruction. Clinical studies from larger patient cohorts employing Schwab-grade-I PCO are therefore warranted to delineate granular outcomes in spinal deformity patients.
1983
A125: Radiographic results in severe rigid kyphoscoliosis patients who were surgically treated with Schwab-Grade-I or Grade-II posterior column osteotomies (PCOs): a minimum 2-year comparative outcome
Nicholas Van Halm-Lutterodt 1,2,3 , Ziyang Ye 3,4 , Aixin Pan 2 , Yangpu Zhang 2 , Jincai Yang 2 , Tie Liu 2 , Lijin Zhou 2 , Yuzeng Liu 2 , Sunny Kim 3 , and Yong Hai 2
1 School of Professional Studies, Brown University, Providence, United States
2 Orthopedics Surgery, Beijing Chaoyang Hospital Affiliated Capital Medical University, Beijing, China
3 Department of Orthopedic and Neurosurgery, Inspired Spine Health, Burnsville, United States
4 Department of Analytics and Data Science, University of Chicago, Chicago, United States
Background: Smith-Petersen osteotomy, [SPO], (Schwab-grade-I) and Ponte osteotomy, [PO], (Schwab-grade-II) are very frequently used in spine deformity patients where aggressive osteotomy techniques are not required. Nevertheless, they are used in patients with mild to moderate deformities which are easy to maneuver. Reports on the application of these low-grade osteotomies in severe and rigid kyphoscoliosis with curves ≥ 80o are highly lacking. We aimed to compare between the radiographic, clinical, and patient-reported outcomes of severe rigid scoliosis or kyphoscoliosis patients surgically treated with Schwab-grade-I or Schwab-grade-II posterior column osteotomies (PCOs) and to determine their effectiveness. Methods: Following approval by the institutional review board (IRB) of Beijing Chaoyang Hospital-Affiliated Capital Medical University in Beijing, a pool of 28 propensity-score-matched, (PSM) adult (≥ 18 years) severe rigid scoliosis or kyphoscoliosis patients (curved ≥ 80o) who underwent spinal deformity primary corrective surgery were retrospectively evaluated. The patients were dichotomized into two (2) osteotomy technique groups: Smith-Petersen osteotomy (SPO-treated), (i.e., Schwab-grade-I PCO) and Ponte osteotomy, (PO-treated), (i.e., Schwab-grade-II PCO). The minimum follow-up period was 2 years. Primary outcomes included baseline and clinical features between the two osteotomy groups. Secondary outcomes included perioperative radiographic parameters [preoperative and minimum 2-year postoperative coronal and sagittal parameters]. Tertiary outcomes included preoperative and final follow-up ODI and SRS-22 scores. Statistical analyses were carried out by Student t-test, Mann-Whitney test, and Pearson’s Chi-squared test (Fisher’s Exact Test), through Python statistical software package. Statistical significance was set at (p < 0.05). Results: Of the 28 age- and gender-matched patients, 50.0% (n = 14) were SPO-treated and 50.0% (n = 14) were PO-treated patients, respectively. The overall average age of patients was 23.68 years, with a female incidence of 60.71%. Approximately 46.4% and 53.6% were idiopathic and congenital kyphoscoliosis, respectively. The average preoperative major curve Cobb angles of 98.4o and 105.2o in the SPO-treated and PO-treated patients were corrected to 50.0o and 45.5o at 2-year postoperative, respectively. The average preoperative thoracic kyphotic (TK) angles of 60.0o and 75.5o in the SPO-treated and PO-treated patients were corrected to 43.6o and 43.3o at 2-year postoperative, respectively. The average preoperative lumbar lordosis (LL) angles of 63.3o and 67.4o in the SPO-treated and PO-treated patients were corrected to 52.4o and 56.1o at 2-year postoperative, respectively. The average preoperative apical vertebral translation (AVT) of 10.4cm and 9.7cm in the SPO-treated and PO-treated patients were corrected to 3.9cm and 3.4cm at 2-year postoperative, respectively. The average vertical axes of coronal (CVA) and sagittal (SVA) showed that normal alignment was achieved in these patients. Major curve corrective rates were 51.7% and 56.4% in the SPO-treated and PO-treated patients, respectively. The ODI score was significantly superior at minimum 2-year follow-up, (p < 0.05), while preoperative and postoperative SRS-22 scores were comparable, (p > 0.05). Conclusion: In the current study, we have demonstrated that both Schwab-grade-I or Schwab-grade-II PCOs are surgically effective for correction of severe rigid kyphoscoliosis curves. The need to use less aggressive (low-grade) and safe osteotomies should be emphasized, especially if satisfactory curve corrective rates can be achieved while enhancing value-based outcomes in severe rigid kyphoscoliosis patients.
430
A126: Use of a kickstand rod improves coronal alignment and maintains correction compared to control at two-year follow-up
Anson Bautista 1 , Varun Puvanesarajah 2 , Fthimnir Hassan 3 , Josephine Coury 3 , Lawrence Lenke 2 , and Zeeshan Sardar 2
1 Orthopaedic Surgery, Dwight D. Eisenhower Army Medical Center, Fort Gordon, United States
2 Spinal Surgery
3 Orthopaedic Surgery, Columbia University Irving Medical Center, New York, United States
Introduction: Coronal malalignment (CM) often leads to significant disability and immobility. CM is difficult to correct intraoperatively and maintain over time. However, usage of the “kickstand rod” (KSR) technique has demonstrated significant CM correction with long-term corrective maintenance. However, no single-center studies have compared the long-term outcomes of KSR constructs to those without KSRs. The goal of the present study was to assess and compare coronal alignment correction at two-year follow-up in patients treated with and without KSRs. Materials and Methods: Consecutive adult patients who underwent posterior spinal fusion for adult spinal deformity at a single center with a preoperative coronal vertical axis (CVA) of at least 3 cm and a minimum of two-year clinical and radiographic follow-up were identified. Patients were divided into two groups: those treated with a KSR and those who were not (control). Patient characteristics, radiographic parameters, and patient-reported outcomes (PROs), such as the Oswestry Disability Index (ODI) and Scoliosis Research Society-22R (SRS-22r), were collected at the preoperative visit, one-year follow-up, and two-year follow up. The aforementioned parameters were analyzed and compared using standard statistical tests at each time point of interest using SAS software version 9.2, with significance set at p < 0.05. Results: 47 patients were identified: 20 in the KSR group and 27 in the control group. There were no differences in age (53.7 vs 56.9 years, p = 0.40); sex (85.0% vs. 70.4% female, p = 0.31); or number of revision cases (65.0% vs. 48.2%, p = 0.25). Similarly, there was no difference in maximum Cobb angle (50.5° vs. 44.9° p = 0.44) or sagittal vertical axis (SVA) (6.3 vs. 8.2 cm, p = 0.33). Patients treated with a KSR had a greater CVA preoperatively (5.9 vs. 4.4 cm, p = 0.03). The KSR group demonstrated greater absolute CVA correction at both one year (4.8 vs 2.8 cm, p = 0.01) and two years (5.0 vs. 2.9 cm, p = 0.01) postoperatively. Furthermore, the KSR group had lower CVA at both one year (1.5 vs. 2.5 cm, p = 0.03) and two years (1.5 vs. 2.5 cm, p = 0.01). Mechanical complications were defined as failures of the construct identified on imaging. Three patients (11%) in the control cohort returned to the operating room for mechanical complications, all of which were rod fractures resulting in revision surgeries for pseudoarthrosis and removal/replacement of instrumentation, compared to no patients in the KSR cohort (p = 0.18). Two patients (10%) from the KSR cohort had asymptomatic S2 alar-iliac (S2AI) screw fractures that did not return to the operating room compared to five patients (19%) in the control cohort, who had asymptomatic mechanical complications including three rod fractures and two S2AI screw fractures (p = 0.24). There was no significant difference in PROs between the cohorts at either one or two years postop. Conclusions: Patients treated with a KSR tended to have higher preop CVA, experienced more coronal correction than those not treated with a KSR, and this correction was maintained at a two-year follow-up. There was no difference in mechanical complications between the cohorts. While CVA radiographic improvement using a KSR was superior, no significant difference in PROs was identified.
OP15: Surgical Complications 1
192
A127: "XX" Sacroplasty - A noval technique for managment of "H-Type" sacral insufficiency fractures
Oded Hershkovich 1 and Raphael Lotan 1
1 Edith Wolfson Medical Center, Holon, Israel
Objective: Examine the feasibility, safety and results of a novel sacral percutaneous injection technique ("XX") addressing both the vertical and horizontal aspects of Sacral Insufficiency Fractures (SIF). Methods: Prospective cohort study. Eight consecutive SIF patients with immobility and pain investigated using CT, and nuclear imaging confirmed "H" type fracture. Demographics, pain level, and ambulation status were recorded. The long term quality of life was evaluated using the ODI questionnaire and pain VAS scores. Sacroplasty procedures in prone positioning using fluoroscopy were used to insert two bone trochars through the S1 Pedicles and two trochars through the sacral ale aiming towards the SIJ, thus forming two 'X' trochar formations. Balloon kyphoplasty was done through the trocars, and PMM was injected. Postoperative ambulation and VAS were recorded. Results: Average age 81.5 (±3.4 years). The time from presenting symptoms to hospital admission was two days to 4 months. All patients were significantly limited with ambulation. None had a neurologic compromise. Sacroplasty was performed with 2 cases that required additional lumbar Kyphoplasty. The mean operative time was 54 min (±14). The average exposure was 19mGy (±12mGy). Two patients had cement leaks. CT and X-rays revealed good cement filling of the fractures sacral alae and body of S1. The average postoperative hospitalization was ten days. All patients reported postoperatively pain relief immediately and were able to walk better. Follow up time was 17 ± 12months. Follow up VAS was 2.7 (±2), ODI was 57.3% (±21%). Conclusion: "XX" technique showed good outcomes for patients with higher complexity SIF, using the same principles as for lumbar VPL/KPL, and was found to be safe and effective.
Level of evidence – III
Keywords: Sacral Insufficiency Fracture, Sacroplasty, Osteoporosis, Balloon Kyphoplasty.
Elderly Sacral insufficiency fractures = SIF
569
A128: Giant calcified thoracic disc herniation - analysis of long term outcome of posterolateral approach
Manojkumar Gaddikeri 1 and Sudhir Srivastava 2
1 Lilavati Hospital and Research Center, We Are Spine, Mumbai, India
2 Orthopaedics, K J Somaiya Medical College and Hospital, Mumbai, India
Introduction: Thoracic disc herniation (TDH) though a rare occurrence (0.15-4%) causes significant neurological deficit. Labelled as Giant if herniated disc occupies > 40% of canal. Calcification is seen in 42% of herniations and intradural extension in 70%. Incidence of myelopathy in Giant TDH ranges from 70-95%. There is a lot of confusion regarding surgical approach and technique to be used in treating these cases. We present our experience of using a unique technique through posterolateral approach for extracting giant calcified thoracic disc. Material and Methods: The study included 24 patients of Giant calcified TDH who were operated by posterolateral approach (trans-facetal/trans-pedicular/costo-transversectomy approach) and with a post-operative follow up of at least 2years. We retrospectively reviewed the clinico-radiological aspects from the records of these 24 patients who were operated at our institute and were followed up with serial clinical examination and radiographs taken at 1, 3, 6months, 1year and 2years to assess the progress. Clinical parameters taken into account were age, sex, diagnosis and neurological assessment using Frankel grading system, surgical approach, instrumentation, surgical time, post-operative mobilization and peri-operative complications. Radiological assessment included taking pre-operative X-ray, CT and MRI scans and post-operative radiographs taken immediate post op, at 1, 3, 6 months ,1year and 2years. Radiological parameters studied were location, number of levels affected and percentage canal encroachment. The study was conducted after taking consent from all participants and has been approved by the ethics committee of our institute. The study included only those patients with calcified thoracic disc herniations and patients with non-calcified soft disc herniations were excluded from the study. Results: Of 24 patients 18 were male and 6 were female. Mean age was 39.62 years. Most common level was T11-12. Mean canal occupancy was 58.2%. Neurological improvement was seen in 22 patients with no worsening in any of them. There were total 6 complications with 3 dural tears and 3 with suture site infections which were managed appropriately. Mean level of instrumentation was 4.25 levels. Mean duration of surgery was 3.708 hours with mean blood loss of 1.17litres. Conclusion: Calcified thoracic disc herniations though a rare entity if not properly diagnosed and treated in time can cause irreversible damage. Study was done to show the method of approaching giant calcified TDH and its long-term outcome. Anterior approach is technically difficult and not everyone can master it as compared to posterolateral approach which is a commonly used approach in most surgeries. Since easy to master, with few modifications as shown above can be used effectively in resecting giant calcified TDH thereby minimizing the complications. The above study is done to promote and encourage surgeons to safely carry out resection of Giant TDH using the modified posterolateral approach technique.
Keywords: Giant Thoracic disc herniation, calcified disc, posterolateral approach
210
A129: Better teamwork made simple? Digital preoperative huddle improves quality and efficiency in neurosurgery cases
Roee Ber 1 , David Kurland 1 , Alexander Eremiev 2 , Samya Senan 3 , Shah Ahmed 4 , and Donato Pacione 1
1 Neurosurgery
2 NYU Grossman School of Medicine, New York, United States
3 Perioperative Services
4 Anesthesia,NYU Langone Health, New York, United States
Introduction: What if we could improve patient safety and save time and money by improving communication? We could. Numerous studies have shown that simply by implementing team communication practices such as preoperative huddles we can reduce complications and adverse events, increase efficiencies and reduce costs. But how do we make it easy? How do we make it sustainable?We evaluated the effect of a structured digital preoperative huddle through a mobile app among the surgeons, anesthesiologists, nurses and operating room staff on quality, efficiency and team collaboration. We report the results of this effort. Materials and Methods: We implemented a workflow which included a asynchronous digital huddle through a mobile app in neurosurgery cases. We used non-participating surgeons working at the same operating rooms as controls for the surgeons who were compliant with the workflow and compared objective and subjective outcomes in the pre- (March 2021 to February 2022) and post- (March 2022 to August 2022) intervention periods for each group. Primary quality outcomes included morbidity and mortality, as defined by the department’s criteria, and readmissions rate. Primary efficiency outcomes included the differences in time to incision, rate of delays in case starts, rate of cases that overrun by >30 minutes, and rate of accurate case time prediction within 15% and 30 minutes. Secondary subjective outcomes measures included surveys filled out by the anesthesia and nursing staff. Results: Participating surgeons performed 1554 and 689 cases in the pre- and post-intervention periods respectively. Compliance rate with the workflow among participating surgeons was 77%. Non-participating surgeons performed 985 and 409 cases in the pre- and post-intervention periods respectively. Among participating surgeons, there was a statistically significant decrease in readmissions rate (8.16% to 5.48%, p = 0.028) before and after intervention, while it did not change for non-participating surgeons (5.89% to 6.6%, p = 1). Rate of morbidity and mortality decreased more for participating (from 5.08% to 3.63%, p = 0.09) than for non-participating surgeons (from 3.21% to 2.79%, p = 0.76) but did not reach statistical significance for both groups. There was a significant decrease in time to incision (66 mins to 63 mins, p = 0.02) and rate of cases that overrun by > 30 minutes (41.5% to 36.22%, p = 0.02). There was a significant increase in the rate of accurate case time prediction within 15% and 30 minutes (34.6% to 43.1%, p = 0.0005) for participating surgeons. All the above efficiency outcomes did not change for non-participating surgeons. Rate of delayed starts was lower for participating surgeons in the post-intervention, but it did not reach statistical significance (6.94% to 5.34%, p = 0.15). The rate of delayed starts for non-participating surgeons remained the same (7.10% to 7.54%, p = 1). Nursing and anesthesia staff subjectively reported improvement across numerous domains of quality and efficiency. The average rate for the digital huddle ease of use was 4.3/5. Conclusion: Implementation of structured digital preoperative huddles resulted in significant decrease in readmission rates and improved efficiency outcomes within 5 months. Technology is key for a scalable and sustainable adoption of these game changing practices.
193
A130: Robustness of results of RCTs in spine surgery - A fragility analysis
Sathish Muthu 1,2 and Girinivasan Chellamuthu 2
1 Department of Orthopaedics, Government Medical College, Dindigul, India
2 Quality Appraisal Committee, Orthopaedic Research Group, Coimbatore, India
Introduction: Many trials in Spine surgery were characterised by fewer outcome events along with a small sample size. Fragility Index helps us identify the robustness of the results from such studies with statistically significant dichotomous outcomes. To assess the robustness of statistically significant outcomes from randomised control trials(RCTs) in spine surgery using Fragility Index(FI) which is a novel metric measuring the number of events upon which statistical significance of the outcome depends. Materials and Methods: We conducted independent and in duplicate, a systematic review of published RCTs in spine surgery from PubMed Central, Embase and Cochrane Database. RCTs with 1:1 prospective study design and reporting statistically significant dichotomous primary or secondary outcomes were included. FI was calculated for each RCT and its correlation with various factors was analysed. Results: 43 trials met inclusion criteria with a median sample size of 139 (IQR:80-319) and median reported events per trial was 48 (IQR:24-112). The median FI score was two (IQR 1-7), which means if we switch 2 patients from non-event to event, the statistical significance of the outcome is lost. The FI score was less than the number of patients lost to follow-up in 18/43 trials. The FI score was found to positively correlated with sample size (r = 0.491, p = 0.001), total number of outcome events (r = 0.416, p = 0.006) and journal impact factor (r = 0.348, p = 0.022) while negatively correlated with p-value (r = -0.417, p = 0.005). Funding and year of publication did not have a significant correlation. Conclusion: Statistically significant dichotomous outcomes reported in spine surgery RCTs are more often fragile and outcomes of the patients lost to follow-up could have changed the significance of results and hence it needs caution before transcending their results into clinical application. The addition of FI in routine reporting of RCTs would guide readers on the robustness of the statistical significance of outcomes.
1116
A131: Lymphopenia is a poor predictor of postoperative mortality and major complications in metastatic spinal tumor surgery
Jessica Ryvlin 1 , Mousa Hamad 1 , Justin Langro 1 , Benjamin Wang 1 , Pavan Patel 1 , Rafael De La Garza Ramos 1 , Saikiran Murthy 1 , Yaroslav Gelfand 1 , and Reza Yassari 1
1 Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, United States
Introduction: Lymphopenia can be seen in advanced metastatic disease for a range of primary tumor types and has been shown to be independently associated with poor outcomes in the setting of surgical intervention. Limited research has been done to validate this oncologic metric in patients with spinal metastases. The objective of this study was to evaluate the capability of preoperative lymphopenia to predict 30-day mortality, overall survival (OS), and major complications in the metastatic spine tumor population. Methods: This was a single-institution retrospective cohort study. A total of 153 patients who underwent metastatic spinal tumor surgery between 2012 and 2022 and met inclusion criteria were examined. Electronic medical record (EMR) chart review was conducted to obtain patient demographics, comorbidities, preoperative lab values, survival time, and postoperative complications. Preoperative lymphopenia was defined as < 1.0k/µL based on our institution’s lab cutoff. The primary outcome was 30-day mortality. Secondary outcomes were OS and 30-day postoperative major complication development. Outcomes were assessed with multivariate logistic regression. Survival analyses were done using the Kaplan-Meier method with log-rank test and multivariate cox regression. Receiver operating characteristic (ROC) curves were plotted to classify the predictive ability of lymphocyte count on outcome measures. Results: Lymphopenia was identified in 47% of patients (72 of 153). The overall 30-day mortality rate in our sample was 8.5% (13 of 153). After controlling for potential confounders such as BMI, ECOG status, and primary cancer type, lymphopenia was not associated with 30-day mortality (OR = 1.80, 95% CI 0.46-7.05, p = 0.405). The median OS for the group was 25.9 months (95% CI 11.8-40.0 months). The multivariate Cox regression model controlling for ECOG status, primary cancer type, hypoalbuminemia, and tobacco use did not show an association between lymphopenia and survival (HR = 1.21, 95% CI 0.72-2.03, p = 0.484). The major complication rate was 25.5% (39 of 153). After controlling for variables such as ECOG status, primary cancer type, and hypoalbuminemia, lymphopenia was not associated with the development of major complication (OR = 1.33, 95% CI 0.59-2.98, p = 0.487). Finally, ROC curves generated poor discrimination between lymphocyte count and all outcomes, including 30-day mortality (AUC = 0.600, p = 0.232). Conclusion: This study refutes prior research that had shown an independent association between low preoperative lymphocyte level and poor postoperative outcomes following metastatic spine tumor surgery. While lymphopenia may be used to predict outcomes in other tumor related surgeries, this metric may not hold a similar predictive capability in the metastatic spine population. Further research into reliable prognostic tools is needed.
635
A132: Analysis of complications and revisions after spine surgery in multiple myeloma patients with spinal involvement
Hester Zijlstra 1,2,3,4 , Robert-Jan Pierik 1 , Nienke Wolterbeek 2 , Diyar Delawi 2 , Diederik Kempen 3 , Jorrit-Jan Verlaan 4 , and Joseph Schwab 1
1 Department of Orthopedic Surgery, Massachusetts General Hospital/Harvard Medical School, Boston, United States
2 Department of Orthopedic Surgery, St. Antonius Hospital, Utrecht, The Netherlands
3 Department of Orthopedic Surgery, OLVG Amsterdam, Amsterdam, The Netherlands
4 Department of Orthopedic Surgery, UMC Utrecht, Utrecht, The Netherlands
Introduction: Multiple myeloma (MM) is the most common primary bone malignancy and typically affects the spine, ribs, skull, and pelvis, with the majority of patients having vertebral involvement at the time of diagnosis. MM patients are at an increased risk of infection and suffer from poor bone quality due to their disseminated malignant bone disease. In this study, we aimed to determine the incidence of complications after spinal surgery in MM patients and sought to identify predictors for such complications. Material and Methods: We retrospectively assessed the data of 270 patients surgically treated for spinal involvement due to multiple myeloma or plasmacytoma between 2008 and 2021. Data on demographics, clinical presentation, radiographical- and surgical factors, prior treatments, perioperative complications, reoperations, and survival was collected through manual chart review. We analyzed the incidence of perioperative complications and survival and factors associated with these complications. We used multivariate logistic regression to identify risk factors for complications within 6 weeks and reoperations. Results: The median age of our cohort was 65 and 58.1% were males. Almost all patients experienced back pain at presentation, were capable of all self-care (ECOG scores 0-2) (87.1%) and 33.7% presented with grade D or worse paralysis on the American Spinal Injury Association (ASIA) classification scale. Severe spinal cord compression (Bilsky grade 2-3) was present in 53.1% and 24.2% had unstable vertebrae according to the Spinal Instability Neoplastic Score (SINS). Surgical procedures performed were mainly vertebral augmentations (48.3%) and decompressions (with or without fusion) (29.5%). Twenty-four patients (8.9%) had an intra-operative complication. The overall short-term complication rate after surgery was 33.3%. Unplanned post-operative radiation therapy (within 2 years) because of new or persisting symptoms was indicated for 12.2% of the patients. The following variables were significantly (independently) associated with 60-day complications: age (OR 1.02, 95% CI = 1.00-1.05), ECOG score (OR 1.44, 95% CI = 1.10-1.90), baseline ASIA score (OR 1.69, 95% CI = 1.22-2.33), duration of neurologic symptoms (OR 1.13, 95% CI = 1.00-1.27), whether a steroid booster was given prior to surgery (OR 3.43, 95% CI = 1.97-5.99), Calcium (OR 0.52, 95% CI = 0.31-0.86, p = .011), Hemoglobin (OR 0.78, 95% CI = 0.63-0.96) and White Blood Cell count (OR 1.1, 95% CI = 0.98-1.22). A secondary surgery was indicated for 49 patients (17.8%), of which 40 took place within 2 years after initial surgery, and 13 within 2 weeks. Neurologic status worsened in 11 (4.4%), did not improve (excluding ASIA E) in 19 (7.5%), and improved in 58 (23.0%) patients after surgery. Median survival time was 37 months for patients who had a post-op complication, and 68 for patients without complications. Conclusion: The goal of surgical treatment for MM bone disease is to enhance patient quality of life and symptomatology. However, surgical complication rates remain high after spine surgery in patients with MM, likely attributable to inherent characteristics of the disease. Patient risk for complications and subsequent surgery should be explored and multidisciplinary therapy including other medical disciplines is crucial.
331
A133: Operative intervention for spine diseases in very old patients, an analysis of the indications, surgical techniques, and early postoperative results in 100 above 90 years old patients
Mohamed Alhashash 1,2 , Heinrich Boehm 1 , Reza Bahrami 1 , and Mootaz Shousha 1
1 Spine surgery, Zentralklinik Bad Berka, Bad Berka, Germany
2 Orthopedics and Trauma, Alexandria University, Alexandria, Egypt
Introduction: There is a continuous increase of the life expectancy of the population. Due to the improvement of the medical care, the spine surgeons are facing an increased number of old patients with spine pathologies. These patients are medically labile and frail because of the associated medical diseases and the prevalence of osteoporosis, this led to a higher rate of complications. Material and Methods: In a DWG (Deutsche Wirbelsäulengesellschaft) level-1 center, the data of all patients are collected prospectively in an extensive database including, pre-, intra-, and post-operative profile. In this work the data of all patients aged 90 years and above who were surgically managed for spine pathologies between 1997 and 2021 is analyzed including the indication of the surgical intervention, the surgical technique, peri-operative medical and surgical complications, and the readmission and reoperation rates. Results: The study included 100 patients, 74 females and 26 males. The mean age was 91.73 ± 1.03 years (90-97). The first indication of surgery was trauma in75 patients. Odontoid fractures type 2 in 20 patients, sub axial cervical spine fractures in 6 patients, thoracic Fractures in 16 patients, and lumbar fractures in 33 patients. In 15 patients there were multiple thoracic and lumbar fractures (2 to 5 levels). Osteoporosis was the most common cause of thoracic and lumbar spine fractures in 35 cases (10 thoracic and 25 lumbar). The second indication was degenerative disease in 15 patients with spinal canal stenosis, disc prolapse and instability. The third diagnosis was metastasis with pathological fractures or spinal canal infiltration in 6 patients. The fourth indication of surgery was spondylodiscitis in 4 patients. A minimal invasive surgical approach was used in most cases. Percutaneous cement augmentation for the Osteoporotic fractures, percutaneous C1-C2 fixation for the odontoid fractures, microscopic-assisted decompression for the spinal canal stenosis in degenerative and metastatic diseases, percutaneous screw stabilization for the posttraumatic and the degenerative Instability, and minimally invasive thoracoscopic surgery for the spondylodiscitis in the thoracic spine. The mean VAS improved from 7.6 ± 1.4 preoperative to 3.2 ± 2.5 postoperatively (p = 0.01) and the NDI and ODI improved from a mean of 26.3 ± 13.7 to 12.8 ± 6.4 postoperatively (p = 0.02). Postoperative pulmonary and cardiac complications occurred in 6 patients and required a short stay in the intensive unit for 2- 4 days. There were no in-hospital mortalities. Reoperation was necessary in 9 patients; in 6 patients the cause was an osteoporotic fracture in an adjacent or a distant segment. One patient had a wound healing problem after a posterior decompression for a metastatic spinal canal stenosis. One patient had a pseudarthrosis after 2 years of C1-C2 fusion for an odontoid fracture. One patient had a recurrent lumbar disc prolapse after a micro-discectomy. Conclusion: The main indication of surgery in the very old patients is fractures, especially odontoid fractures. A proper selection of the surgical approach and the use of minimal invasive techniques reduce the surgical complications. The surgical intervention significantly improved the clinical conditions of the patients.
662
A134: Medium to long term outcomes of magnetically controlled growing rods in an early onset scoliosis population
Henry Turner 1 , Robin McManus 1 , Flavia Alberghina 1 , Jim Kennedy 1 , Jacques Noel 1 , and Patrick Kiely 1
1 Trauma and Orthopaedic Surgery, Children's Health Ireland (CHI) at Crumlin, Dublin, Ireland
Introduction: There has recently been controversy around the safety and efficacy of magnetically controlled growing rods (MCGR) for the treatment of patients with early onset scoliosis (EOS). We present our findings from a single-centre prospective study analyzing EOS patients who underwent MCGR insertion. Material and Methods: All patients who had MCGR inserted in our institution and had a minimum follow-up time of 2 years were included. The outcomes measured included complications, pre- and post-operative Scoliosis Major Cobb (MCA) and Major Kyphosis (MKA) angles, space available for lung ratios (SALR), T1- T12 and T1-S1 heights, rod length changes and radiographic evidence of actuator pin or endcap failure. Results are presented as means with standard deviation (SD) and 95% Confidence interval (CI). Results: 83 patients (40 Females and 43 Males) were included. C-EOS classification included 18 Congenital, 23 Idiopathic, 14 Syndromic and 28 Neuromuscular patients. 5 patients were excluded due to insufficient follow-up time. The mean age at surgery was 8.12 years (SD ±2.74, CI 7.53 - 8.72) and follow-up after surgery was 4.38 years (SD ±1.2, CI 4.12 - 4.65). 20/83 (24.1%) patients needed unplanned additional surgery due to complications. The mean pre- and postoperative MCAs were 75 ° (SD ±21, CI 70-80) and 35° (SD ±18, CI 31 - 39), respectively. The latest mean MCA was 48 ° (SD ±23, CI 43 - 54). The mean pre- and postoperative MKAs were 42° (SD ± 27, CI 36 - 48) and 28° (SD ±15, CI 24 - 31), respectively. The latest mean MKA is 35° (SD ±16, CI 33 - 40). This is a significant decrease of 36% (p < 0.001) in the MCA with insignificant change in the MKA (41%, p = 0.06). The mean pre- and postoperative SALRs were 86% (SD ±14, CI 83-89) and 95% (SD ±11, CI 93-98) respectively. The latest mean SALR is 96% (SD ±9, CI 94-98), a significant increase of 10% (p < 0.001). The mean pre- and postoperative T1- T12 heights were 168 mm (SD ±30, CI 162 - 175) and 194 mm (SD ±30, CI 187-200) respectively. The latest mean T1- T12 height is 216 mm (SD ±34, CI 209-223), a final increase of 29% (p < 0.001). The mean pre- and postoperative T1-S1 heights were 276 mm (SD ±48, CI 266-287) and 317 mm (SD ±50, CI 306 - 328) respectively. The latest mean T1- S1 height is 342. (SD ±56, CI 329 - 354), a total increase of 24 % (p < 0.001). The mean increase in rod lengths was 21mm (SD ±12, CI 18-23) and 23mm (SD ±12, CI 20-26) for right and left side rods, respectively. 2/83 (2.4%) patients had radiographic evidence of bilateral actuator pin failure. There was no evidence of end cap failure. Conclusion: Our findings show that MCGR can achieve good outcomes over the medium to long term, but additional surgery may be needed before final fusion. Issues related to the mechanical limitations of the MCGR construct are important and should be discussed with patients and their parents before proceeding with surgery.
586
A135: Comparison between posterior lumbar decompression and fusion and transforaminal lumbar interbody fusion in degenerative spondylolisthesis as assessed by the CARDS Classification System
Tariq Issa 1 , Yunsoo Lee 1 , Mark Lambrechts 1 , Khoa Tran 1 , Parker Brush 1 , Jeremy Heard 1 , Delano Trenchfield 1 , Justin Chu 1 , Griffin Gilmore 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alexander Vaccaro 1 , Gregory Schroeder 1 , and Christopher Kepler 1
1 Division of Spine Surgery, Rothman Orthopaedic Institute, Philadelphia, United States
Introduction: Degenerative spondylolisthesis (DS) is heterogenous and broadly encompasses clinical symptoms due to vertebral translation, intervertebral disc collapse, sagittal alignment, and mobility with flexion and extension. The CARDS classification was created to provide clarity to the different radiographic findings and guide treatment approach for DS. However, the optimal fusion approach for each subtype of DS is unclear. Our primary objective was to compare clinical outcomes among CARDS subtypes in patients undergoing posterior lumbar decompression and fusion (PLDF) with or without additional TLIF, and to evaluate the CARDS system as a prognostic tool to guide clinical decisions regarding the treatment of degenerative spondylolisthesis (DS). Material and Methods: A retrospective study was conducted of patients who underwent PLDF or TLIF for a primary diagnosis of DS from 2010-2020. Patients were grouped by preoperative CARDS classification: Type A – disc space collapse (advanced) with no evidence of kyphosis; Type B – disc space preserved (partially) with ≤ 5.0 mm of translation; Type C – disc space preserved (partially) with > 5.0 mm of translation; and Type D – kyphotic alignment pattern. Multivariate analysis was utilized to determine the independent effects of treatment approach on one-year PROMs and 90-day surgical outcomes. Results: A total of 1,056 patients were included:148 patients with Type A DS, 323 Type B, 525 Type C, and 60 Type D. Patients with CARDS Type A and Type C who underwent PLDF were more likely to experience longer hospital length of stay (LOS) and were less likely to be discharged home. There were no differences in revision rates, perioperative complications, or 90-day readmission rates between PLDF and TLIF for any CARDS subtype. CARDS Type A patients who underwent PLDF were less likely to achieve MCID for VAS Back (36.8% vs 76.7%, p = 0.013) compared to those who underwent TLIF. There were no other significant differences in PROMs among CARDS subtypes. On multivariate regression analysis, TLIF was an independent predictor of better VAS Leg pain improvement at one-year follow-up (β = -2.92, p = 0.017) for patients with CARDS Type A. However, multivariate analysis demonstrated no significant difference in PROMs by surgical approach for patients with CARDS Types B, C, or D. Conclusion: Patients with disc space collapse and vertebral endplate apposition (CARDS Type A) appear to benefit from TLIF. However, patients with lumbar spondylolisthesis without disc space collapse or kyphotic angulation (CARDS Type B and C) may not benefit from additional interbody placement.
OP16: Cervical Myelopathy
130
A136: Deterioration after surgery for degenerative cervical myelopathy: an observational study from the canadian spine outcomes and research network
Lukas Burger 1,2 , Nathan Evaniew 1,2 , Nicolas Dea 2,3 , David Cadotte 1,2 , Greg McIntosh 2,4 , and Bradley Jacobs 1,2
1 Combined Spine Program, University of Calgary, Calgary, Canada
2 CSORN Inverstigators, Canada
3 Combined Neurosurgical and Orthopedic Spine Program, University of British Columbia, Vancouver, Canada
4 Canadian Spine Society, Markdale, Canada
Introduction: Post-operative neurological deterioration is one of the most undesirable complications that can occur after surgery for Degenerative Cervical Myelopathy (DCM). Our primary objective was to investigate the incidence, etiology, and outcomes of patients who experience this problem. Material and Methods: We analyzed data from the Canadian Spine Outcomes and Research Network (CSORN) DCM prospective cohort study. We defined post-operative neurological deterioration as a decrease in modified Japanese Orthopaedic Association (mJOA) score by at least one point from baseline to 3 months after surgery. Adverse events were collected using the Spinal Adverse Events Severity (SAVES) protocol with additional validation. Secondary outcomes included patient-reported pain, disability, and health-related quality of life. Results: Among a study cohort of 428 patients, 50 (12%) deteriorated by at least one point on the mJOA after surgery for DCM (21 by 1 point, 15 by 2 points, and 14 by 3 points or more). Significant risk factors after adjusting for potential confounders included older age, female sex, and milder pre-operative disease. Among those who deteriorated, 13 (3% of 428) experienced contributing intra- or post-operative adverse events, 6 (1%) had alternative non-DCM diagnoses, and 31 (7%) did not have an identifiable etiology. Patients who deteriorated had significantly lower mJOA scores at one year after surgery (13.5 (SD 2.7) versus 15.2 (SD 2.2), p < 0.01) and those with larger deteriorations were less likely to recover their mJOA to at least their pre-operative baseline, but most secondary measures of pain, disability, and health-related quality of life were unaffected. Conclusion: The incidence of mJOA deterioration after surgery for DCM was approximately one in ten, but many deteriorations were small, some were unrelated to actual spinal cord impairment, and most secondary outcomes were unaffected. These findings can inform patient and surgeon expectations during shared decision-making, and they demonstrate that interpretation of mJOA scores without clinical context can sometimes be misleading.
1515
A137: Timing of recovery after surgery for degenerative cervical myelopathy: an observational study from the canadian spine outcomes and research network
Nathan Evaniew 1 , Matthew Coyle 1 , Raja Rampersaud 2 , Chris Bailey 3 , Bradley Jacobs 1 , David Cadotte 1 , Ken Thomas 1 , Najmedden Attabib 4 , Jerome Paquet 5 , Andrew Nataraj 6 , Sean Christie 7 , Michael Weber 8 , Philippe Phan 9 , Raphaële Charest-Morin 10 , Charles Fisher 10 , Hamilton Hall 2 , Greg McIntosh 2 , and Nicolas Dea 10
1 Calgary, Canada
2 Toronto, Canada
3 London, Canada
4 Saint John, Canada
5 Laval, Canada
6 Edmonton, Canada
7 Halifax, Canada
8 Montreal, Canada
9 Ottawa, Canada
10 Vancouver, Canada
Introduction: The time course over which post-operative neurological recovery occurs after surgery for Degenerative Cervical Myelopathy (DCM) occurs is poorly understood. Our primary objective was to determine the timepoint at which patients experience significant neurological improvement. Material and Methods: We reviewed data from an ongoing prospective multicenter cohort study. We measured neurological function at 3 months, 1 year, and 2 years after surgery using the modified Japanese Orthopaedic Association scale (mJOA) scale. We implemented Minimal Clinical Important Differences (MCIDs) to guide interpretation of mJOA scores, and we used one-way Analysis of Variance to compare changes between follow-up intervals. Results: Among 330 patients, mean overall mJOA improved from 12.9 (Standard Deviation, SD 2.6) to 14.6 (SD 2.4) at 3 months, 14.7 (SD 2.4) at one year, and 14.8 (SD 2.5) at two years. The difference in means was statistically significant (p < 0.01) at the interval from baseline to 3 months post-op, but not from 3 months to one year or one year to two years. The MCID was reached by 161 patients at 3 months, 32 more at 1 year, and 15 more at 2 years, with a statistically significant difference only at 3 months. Patients with moderate or severe disease reached the MCID more frequently than those with mild disease. Conclusion: Among patients who underwent surgery for DCM, most significant neurological improvement occurred by 3 months after surgery. These findings will facilitate valid discussions about post-operative expectations during shared clinical decision-making between patients and their surgeons.
273
A138: K-line differences between extension and neutral radiographs with application to treatment of degenerative cervical myelopathy
Sagar Telang 1 , Zabiullah Bajouri 2 , Zoe Fresquez 1 , Michael Kim 1 , Zachary Gilbert 1 , Trevor Pickering 3 , Zorica Buser 1,4,5 , Raymond Hah 1 , Jeffrey C. Wang 1,2 , and Ram Alluri 1
1 Department of Orthopaedic Surgery
2 Department of Neurological Surgery
3 Southern California Clinical and Translational Science Institute, Keck School of Medicine of the University of Southern California, Los Angeles, United States
4 Gerling Institute, New York City, United States
5 Department of Orthopedic Surgery, NYU Grossman School of Medicine, New York City, United States
Introduction: The modified K-line is a radiological tool used in surgical planning of the cervical spine. It is defined as a line connecting the midpoints of the spinal canal at the C2 and C7 level on lateral radiographs. K-lines have been traditionally measured with neutral radiographs. However, a K-line measured in the extended position may offer better utility for patients undergoing cervical fusion which attempts to restore lordosis of the cervical spine. Little is known regarding extension K-lines for treatment of degenerative cervical myelopathy (DCM). Given the dynamic properties of the spine, it is reasonable to anticipate that the pathological features of DCM will change when patients are positioned in extension. Therefore, our group sought to describe changes to measurements provided by the modified K-line in neutral compared to extension to better characterize patients who undergo posterior cervical decompression and fusion with increased postoperative lordosis. Material and Methods: 97 patients with upright cervical MRIs taken in neutral and extension were included. For each patient, the K-line was drawn for both neutral and extension radiographs. The distance from the most posterior portion of each disc (between C2-C7) to the K-line was measured. Each disc to K-line distance was classified as K-line negative (< 4 mm) or K-line positive (>4 mm). The difference in distance measured at each level between neutral and extension was calculated. Additionally, we measured the Cobb Angle, C2-C7 SVA, the T1 slope, and the disc heights in both neutral and extension between the C2-T2 level. Cervical lordosis and disc height (in neutral and extension) were measured using a program called MRAnalyzer. A paired t-test was used to assess significant differences. Results: Across all levels between C2-C7 there was an increase in the distance between the dorsal aspect of the disc and K-line when comparing neutral and extension radiographs. The average change in difference (extension minus neutral) at each cervical spinal level was 0.9 mm (C2-C3), 2.5 mm (C3-C4), 2.6 mm (C4-C5), 2.0 mm (C5-C6), and 0.9 mm (C6-C7). A paired t-test showed that the K-line increase from neutral to extension was statistically significant across all disc levels (p < 0.001). Using logistical regression, high values for CL and T1 slope were found to have less odds of K-line conversion (negative to positive) - in particular, between C4-C6 (p = .02 to .001). Conclusion: When positioned in extension, patients experience a significant increase in distance from the disc to the K-line compared to when positioned in neutral, especially between C3-C6. Intuitively, this makes sense as the greatest change should occur at apical regions of the cervical spine lordotic angle. These findings suggests that there is a degree of additional disc-to-cord space that is being unconsidered in a neutral-drawn K-line in patients that undergo posterior cervical decompression and fusion and postoperatively are fused in an increased lordotic position compared to the preoperative neutral MRI. This is clinically relevant for surgeons considering a posterior cervical decompression and fusion as these patients may have enough cervical cord drift back when fused in an extended position, maximizing likelihood of improving postoperative CSM functional outcomes.
953
A139: Patient reported outcomes following surgical treatment for multilevel cervical myelopathy
Parker Brush 1 , Yunsoo Lee 1 , Mark Lambrechts 1 , Charles Lawall 1 , Amit Syal 1 , Jasmine Wang 1 , Tariq Issa 1 , Jeremy Heard 1 , Delano Trenchfield 1 , Jose Canseco 1 , Alan Hilibrand 1 , Christopher Kepler 1 , Alexander Vaccaro 1 , and Gregory Schroeder 1
1 Rothman Orthopaedic Institute at Thomas Jefferson University, Philadelphia, Unites States
Introduction: Rates of spinal fusion for degenerative cervical myelopathy are increasing. Surgeons can choose an anterior or posterior approach to decompress the spinal cord, and patient specific factors may favor one approach over the other. However, the optimal surgical treatment for the majority of patients with multilevel disease has yet to be elucidated. We aim to compare surgical and patient-reported outcomes between patients undergoing anterior cervical discectomy and fusion (ACDF) and posterior cervical decompression and fusion (PCDF) for multilevel disease. Material and Methods: We retrospectively identified patients at our institution from 2014-2021 for those treated by three- to four-level ACDF or PCDF for myelopathy or myeloradiculopathy with complete preoperative and one-year postoperative outcome measures by neck disability index (NDI). Patients between these two groups were compared by demographic variables and health history, as well as surgical, radiographic, and patient reported outcome measures (NDI, short from-12 survey, visual analog scale neck and arm pain, and the modified Japanese Orthopaedic Association score). Delta values were calculated for all patient reported outcome measures by subtracting the preoperative from the postoperative value. A univariate analysis between the groups and multivariate linear regression to identify factors independently associated with delta NDI and delta neck pain by visual analog scale (VAS) were performed. Results: We identified 153 patients who underwent ACDF and 31 patients who underwent PCDF. The ACDF group was younger (p < 0.001), had a lower BMI (p = 0.005), were less likely to have diabetes (p < 0.001), had a lower overall comorbidity burden by Charlson Comorbidity Index (p = 0.001), and were more likely to receive a three-level fusion (p < 0.001). Preoperative radiographs showed patients receiving an ACDF had less C2-C7 lordosis (7.8˚ vs 15.6 ˚, p = 0.014), and were more likely to have a kyphotic curve (25.7% vs 3.9%, p = 0.028). There were no differences in complication rates, risk of revision surgery, or readmission rates between groups. Patients in both groups experienced similar improvement in arm pain by VAS, quality of life by short form-12 survey, and myelopathy symptoms by the modified Japanese Orthopaedic Association score. However, the ACDF group experienced significantly greater improvement by NDI (-14.3 vs -2.2, p = 0.004) and neck pain by VAS neck (-2.9 vs -1.1, p = 0.011) on unadjusted analysis. On multivariate analysis, ACDF showed greater symptomatic improvement as measured by delta NDI (estimate, 8.75; 95% CI, -0.88-18.39; p = 0.075) and delta VAS neck pain variables (estimate 1.54, 95% CI, -0.20-3.28; p = 0.083) with large estimated effect sizes but high variability that did not meet statistical significance. Conclusion: Our data show that patients receiving an ACDF for multi-level degenerative cervical myelopathy may have improved quality of life by NDI and less neck pain compared to those who receive a PCDF. The findings are likely underpowered given the large effect sizes identified by multivariate analysis, but lack of statistical significance. The patient cohorts in our study were not similar, but our data supports multi-level ACDFs in the appropriate patient population. Despite the potential stability concerns from a multi-level ACDF, we identified no differences in postoperative complications or need for revision surgery.
872
A140: Classifying the trajectory of neurological recovery after surgery for degenerative cervical myelopathy
Anjishu Banerjee 1 , Marjorie C. Wang 2 , and Aditya Vedantam 2
1 Biostatistics
2 Neurosurgery, Medical College of Wisconsin, United States
Introduction: Patients with DCM exhibit complex patterns of functional recovery after surgery and accurate prediction of post-surgical neurological recovery for the individual DCM patient remains a challenge. Standard statistical learning to predict outcomes are limited by temporal changes and lack of flexibility to model individual patient patterns, especially with repeated patient observations. Multilevel computational models of recovery trajectories can overcome these challenges and identify groups of patients with similar phenotypes and recovery profiles. The aim of this study was to incorporate clinical and radiographic (conventional MRI and diffusion tensor imaging (DTI)) in the construction of recovery trajectory models for DCM patients undergoing surgery. Material and Methods: A prospective single-center non-randomized study of 66 consecutive DCM patients undergoing elective cervical spine decompression for DCM between 2010-2015 was performed. Baseline clinical and radiographic data was recorded, which included diffusion tensor imaging (DTI, n = 63) metrics of the cervical spinal cord. Functional status was recorded using the modified Japanese Orthopedic Association (mJOA) and neck disability index (NDI). The short form 36 physical component score (SF36 PCS) was used to measure quality of life. Post-surgical functional status and quality of life was recorded at 3, 6, 12 and 24 months. We constructed recovery trajectories based on a latent class Bayesian model, which identifies latent, unobserved clusters in patient phenotypes and estimates the clusters using Markov models. We identified baseline clinical and radiographic features that predict recovery trajectories. Additionally, we determined if early post-surgical function was predictive of future recovery trajectories. Statistical significance was set at p < 0.05. Results: Neurological recovery based on the mJOA scores during the first 24 months was modeled using 3 recovery trajectories in this cohort. The 3 trajectories were stagnation (initial improvement, worsening and then improvement again to baseline function at 24 months), sustained improvement (steady improvement in function in the first 6 months which was maintained at 24 months) and worsening (decline in function from surgery till 24 months postop). The four strongest predictors of recovery trajectory were age, mean diffusivity, anisotropy index and transverse apparent diffusion co-efficient at the level of maximum compression (p < 0.01). Early changes in mJOA and SF36 (within the first 6 months) were found to be most predictive of future recovery trajectory. Conclusion: Using prospective data, we demonstrate 3 trajectory models for functional recovery in DCM during the first 24 months after surgery. The models can predict potential post-surgical recovery paths for DCM patients, accounting for both population level and individual level trends. This is one of the first computational models to flexibly model variability in individual patient phenotypes while measuring association. While these models require external validation with larger datasets, this approach can enhance clinical prognostication and clinical trial design for DCM.
997
A141: Clinical courses of pain in degenerative cervical myelopathy: a pooled analysis of CSM-NA, CSM-I and CSM-protect trials
Ali Moghaddamjou 1 , Alex Bak 2 , Jefferson Wilson 1 , and Michael Fehlings 1
1 Neurosurgery, University of Toronto, Canada
2 University of Toronto, Canada
Introduction: Pain is a significant contributor to quality of life in degenerative cervical myelopathy (DCM). However, its trajectory and factors associated with chronic pain and resolution is poorly understood. Material and Methods: DCM patients with severe pain were queried using a harmonized dataset of the AOSpine North America, AOSpine International, and CSM-Protect clinical trials. Severe pain was characterized as a Neck Disability Index pain intensity (NDI-PI) score of 3 or greater. Latent class trajectory modelling (LCTM) was applied to classify patients into distinct trajectories based on their NDI-PI score over the initial 24 months postinjury. Optimal number of trajectories were chosen based on i) least Bayesian Information Criterion (BIC); ii) posterior probability > 0.70; iii) odds of correct classification > 5; and concordance between estimated and actual proportion of patients assigned to class. Predictors of recovery trajectories were identified using descriptive statistics and multivariate multinomial logistic regression on demographic and surgical variables. Results: Three distinct recovery trajectories were discovered from our analysis of 305 patients. Their parabolic course was classified as: 1) complete resolution (n = 128, 42.0%), 2) moderate recovery (n = 105, 34.4%), and 3) marginal recovery (n = 72, 23.6%). Complete resolution trajectory was characterized with severe pain at baseline that rapidly reduced to mild or painless levels within 12 months. Moderate recovery was described by severe pain that plateaued to moderate pain in 12 months. Marginal recovery was described by severe pain with little recovery and ended with severe pain in 12 months. Complete resolution was independently associated with anterior graft with autograft (RRR: 5.49, 95% CI[1.47–20.54]; p = 0.011), cage (RRR: 21.07, 95% CI[1.64-270.95]; p = 0.019), and allograft (RRR: 7.0, 95% CI[1.34-36.49]; p = 0.021); older age (RRR: 1.08, 95% CI[1.04-1.13]; p < 0.001); being married (RRR: 2.27, 95% CI[1.03–5.04]; p = 0.043); higher baseline MJOA score (RRR: 1.33, 95% CI[1.08-1.64]; p = 0.006), and baseline Nurick score (RRR: 1.70, 95% CI[1.06-2.73]; p = 0.026). Anxiety and depression was inversely associated with complete resolution (RRR: 0.39, 95% CI[0.16-0.98]; p = 0.044) and moderate recovery (RRR: 0.21, 95% CI[0.08-0.53]; p = 0.001). Posterior autograft was associated with inversely associated with complete and moderate recovery (RRR: 0.31, 95% CI[0.00-0.30]; p = 0.002; RRR: 0.06, 95% CI[0.01-0.50], p = 0.010). Conclusion: Severe acute pain prior to surgery for DCM can be classified into one of three distinct subpopulations with fundamentally differing clinical courses. There is greater than 50% of unresolved pain that becomes chronic in DCM patients over the course of 12 months. Given the high prevalence of chronic pain and impact to quality of life, factors associated with pain trajectories may be avenues for improvement or questions for futures studies.
673
A142: Management of mild degenerative cervical myelopathy and asymptomatic spinal cord compression: an international survey
Jamie Brannigan 1 , Aria Nouri 2 , Ratko Yurac 3 , Vishal Kumar 4 , Rory Murphy 5 , Enrico Tessitore 2 , Granit Molliqaj 2 , Joost Dejaegher 6 , Juan Jose Zamorano 7 , Guy Wynne-Joes 8 , Oliver Mowforth 9 , and Benjamin Davies 9
1 School of Clinical Medicine, University of Cambridge, Cambridge, United Kingdom
2 Department of Neurosurgery, Geneva University Hospitals, Geneva, Switzerland
3 University Hospital of Chile, Chile
4 Nehru Hospital, PGIMER, Chandigarh, India
5 Barrow Neurological Institute, Phoenix, United States
6 Faculty of Medicine KU Leuven, Leuven, Belgium
7 Clinica Alemania de Santiago, Santiago, Chile
8 The Newcastle Upon Tyne Hospitals NHS Foundation Trust, Newcastle, United Kingdom
9 University of Cambridge, Cambridge, United Kingdom
Introduction: Currently there is limited evidence and guidance on the management of mild degenerative cervical myelopathy (DCM) and asymptomatic spinal cord compression (SCC). Anecdotal evidence suggest variance in clinical practice. The objectives of this study were to assess current practice in the assessment and management of mild DCM and asymptomatic SCC and to quantify the variability in clinical practice. Material and Methods: Neurosurgeons, spinal orthopaedic surgeons, and some additional health professionals completed a web-based survey distributed by email to members of AOSpine and the CSRS North American Society. Questions captured experience with DCM, frequency of DCM patient encounters, and standard of practice in the assessment of DCM. Further questions assessed the definition and management of mild DCM, and the management of asymptomatic spinal cord compression. Results: A total of 699 respondents, mostly surgeons, completed the survey. Every world region was represented in the responses. Half (50.14%, n = 359) had greater than 10 years of caring for patients with DCM. A process of standardised follow-up for non-operative patients was reported by 488 respondents (69.52%). At follow-up for mild DCM, there was a heterogeneous mix of investigations reported, and this most often occurred at 6 months (32.92%, n = 158). There was some conflict regarding which clinical features would cause a surgeon to counsel a patient towards surgery. Practice for asymptomatic SCC aligned closely with mild DCM. Finally, there were some contradictory definitions of mild DCM provided in the form of free text. Conclusion: Professionals typically offer outpatient follow up for patients with mild DCM and/or asymptomatic SCC. However, what this constitutes varies widely. Further research is needed to define best practice.
613
A143: Surgical complications or neurologic decline? A patient discrete-choice experiment for cervical myelopathy
Mohamed Sarraj 1 , Meerab Majeed 2 , Daipayan Guha 3 , and Markian Pahuta 1
1 Orthopedic Surgery
2 Faculty of Health Sciences, Hamilton, Canada
3 Neurosurgery, McMaster University, Hamilton, Canada
Introduction: The burden of Degenerative Cervical Myelopathy (DCM) is growing internationally. Although cervical spine surgery is effective at halting the progression of DCM, surgery affects a small and unpredictable neurologic improvement. Concurrently, it may involve serious risks such as dysphagia, C5 palsy, and the risk of undergoing revision surgery. Given the uncertainty of benefit from surgery and high risks involved, value assessments of treatments for DCM should include outcomes that are most important to patients. This study aimed to quantify and compare the relative importance of neurologic function, risk of future surgery, and complications to patients with cervical stenosis in Canada. Material and Methods: Patients with cervical stenosis presenting for surgical evaluation, or post-operative cervical decompression patients, were recruited to participate in the study. Institutional Research Ethics Board approval was obtained (HiREB #13703). Demographic information including mJOA score, type of surgery, and complications were recorded and anonymized to the study ID. Patients then completed an online discrete-choice experiment survey. In a series of 10 questions, respondents chose between two hypothetical health states defined in terms of five attributes, or “decision factors”: upper extremity neurologic function, lower extremity neurologic function, risk of revision surgery, dysphagia, and C5 palsy. Differences in these attributes were highlighted between “Life A” and “Life B” and participants were asked to choose which ‘life’ they preferred. Health state choices were analyzed using a mixed multinomial-logit regression model to quantify the importance of each decision factor to patients in relation to other factors. Results: Overall, 100 patients completed the survey. Fifty-five patients had undergone cervical surgery, while 45 were either awaiting surgery, or not surgical candidates. In our population, neurologic function was the attribute with the greatest relative importance, and this was statistically significant. In all subgroups, lower extremity function was considered more important than upper extremity function. We also found that there was no statistically significant difference in the undesirability of neurologic decline and dysphagia. Differences in importance scores varied between patients who had undergone surgery and those who hadn’t. The post-operative group considered revision surgery more important than a C5 palsy, while non-operative patients valued the opposite. Additionally, when scaled to the least important attribute, non-surgical patients valued lower extremity function as 30-times more important than the least important attribute (revision surgery). In contrast, the surgical group only valued lower extremity function as 4-times more important than the least important attribute (C5 palsy). Conclusion: This study shows that patients consider neurology as the most important factor and hence treatment indications to preserve neurology are justifiable. However, neurology does not trump all other considerations in the treatment decisions, and not all complications should be considered equally. Potential complications should be carefully weighed against the benefits of surgery; especially given the high risks of surgery. Additionally, the experience of surgery does influence patients’ values and preferences, and must be incorporated into the decision making process. Ultimately, surgical decision making involves a variety of factors, but clear communication of specific complication profiles and risks remains critical for patient-centered care.
329
A144: Screening for degenerative cervical myelopathy (SCREEN-DCM): preliminary results of an ongoing multicenter, prospective study
Aria Nouri 1 , Granit Molliqaj 1 , alexandre lave 1 , Gianpaolo Jannelli 1 , Benjamin Davies 2 , Mark Kotter 2 , Allan Martin 3 , Justin Virojanapa 4 , Joseph Cheng 4 , Teresa Somma 5 , Paolo Cappabianca 5 , Carmen Vleggeert-Lankamp 6 , Valerie ter Wengel 6 , Karl Schaller 1 , and Enrico Tessitore 1
1 Neurosurgery, Geneva University Hospitals, Switzerland
2 Neurosurgery, University of Cambridge, United Kingdom
3 University of California, Davis, United States
4 Neurosurgery, University of Cincinnati, United States
5 University of Naples Federico II, Italy
6 Neurosurgery, Leiden University, The Netherlands
Introduction: Degenerative Cervical Myelopathy (DCM) is the most common cause of spinal cord impairment. Unfortunately, the condition remains poorly recognized and underdiagnosed. To better identify these patients, screening tests that target individuals at high risk such as those with known comorbidities would be helpful. One group in particular known to have a high prevalence of DCM are patients with lumbar degenerative disease (LDD), with the combined presentation referred to as tandem stenosis. It is estimated that tandem stenosis presents in 10-20% of patients with LDD. Given that LDD is one of the most common presentations in neurosurgical practice and primary care, it is the objective of the proposed study to administer a screening test to these patients as well as those with risk factors or symptoms which raise the suspicion of underlying DCM. Materials and Methods: A screening test based on the number of clinical sign/symptoms and known patient risk factors of DCM was designed and performed in our neurosurgical consultations primarily for patients with LDD or those with any suspicion of myelopathy. A survey of 13 neurosurgeons was used to develop and modify screening criteria and to define the minimum threshold of factors present before undertaken a cervical MRI. Points are attributed based upon the presence of signs or symptom of DCM (e.g. Hoffman sign, Hyperreflexia) as well as for comorbidities that predispose or are frequently associated with cervical myelopathy (e.g. Rheumatoid arthritis, carpal tunnel syndrome). Patients with ≥ 3 points undergo cervical MRI examination. Patients with positive MRIs will be consulted and receive assessment via mJOA and NDI scores, and subsequent clinical management will be based on practice guidelines. An exploratory multivariate analysis of the effectiveness and efficiency of this proposed screening test will be evaluated after positively screening 50 patients for DCM. Results: Out of 130 patients screened, 41 screened positive (≥ 3 points) and 30 had a subsequent cervical MRI. Of the 30 patients, 11 (36.7%) were diagnosed with cervical myelopathy. Three of the 11 patients or 10% of the those who screen positive were operated. The average number of points for patients screening positive with a diagnosis of myelopathy was 5.36 vs 4.17. All patients with myelopathy were considered as mildly myelopathic. Nine out of the 11 positive patients (81.8%) had T2WI hyperintensity signal changes on MRI. An additional 7 out of the 30 (23.3%) patients presented with cervical canal stenosis without clear evidence of spinal cord compression or sufferance. Conclusions: Screening for DCM in patients with lumbar pathology appears to be effective with a rate of cervical myelopathy uncovered in nearly 40% of patients screening positive. Additionally, screening identified a significant additional group of patients with cervical stenosis without clear myelopathy. These are preliminary results and a complete and more extensive analysis from this multicenter study are expected later this year.
OP17: Novel Surgical Approach for Lumbar Spine Pathologies
85
A145: Safety and efficay of posterolateral approach for central thoracic disc herniation with or without calcification in 32 consecutive cases: a clinical study
Manish Kasliwal 1 , Mohit Patel 1 , and Rohit Mauria 1
1 Neurological Surgery, University Hospitals Cleveland Medical Center, United States
Aim: To report the safety and efficacy of posterolateral approach for central thoracic disc herniation (TDH) via a consecutive clinical case series of 32 central thoracic disc herniations with or without calcifications operated through a posterolateral approach. Methods: A retrospective review was conducted of all patients with symptomatic TDH who underwent surgical intervention from 2016 to 2021. A total of 25 patients comprising 32 central TDH were included in the study. Age, gender, location of the lesion, preoperative and post-operative Frankel and Nurick scores, surgical approach and instrumented vertebrae, and length of stay were recorded. Results: 25 patients with an average age of 60 were included in the study. These patients had a total of 34 TDH with 32 of the 34 symptomatic TDH located centrally. 10/32 central TDH were calcified while 24/32 TDH were non-calcified. Intraoperative navigation was utilized in all cases and intraoperative real-time ultrasound was used as an adjunct in cases with calcified central TDH for confirmation of spinal cord decompression. The unilateral and bilateral transpedicular approach was used in the treatment of 12/32 and 10/32 disc herniations respectively. A transfacet-pedicle sparing approach was used in 10/32 disc herniations. 21/25 (84%) of the patients had improvement in Nurick score while 14/25 (56 %) patients improved their Frankel scores. The average length of stay was 4.5 days. No significant complications were encountered. All patients underwent a short-segment instrumented construct with no need for revision surgery for same level thoracic disc recurrence/residual disc herniation, worsening myelopathy, or instrumentation failure. Conclusions: 84% of the patients who underwent a transfacet or transpedicular decompression for the treatment of symptomatic TDH had improvement in their myelopathy with no neurological deterioration in any of the patients. Given the familiarity and low morbidity associated with a transfacet or transpedicular approach, posterolateral-based approaches especially with the use of navigation and intraoperative ultrasound remains an excellent technique for surgical management of the majority of the patients with thoracic disc herniations.
1414
A146: Lumbar foraminal decompression with a novel flexible microblade shaver has a high revision rate
Taylor Shackleford 1 , Samuel Adams 2 , John France 1 , Reed Andrews 3 , and Scott Daffner 1
1 Department of Orthopaedics, West Virginia University, Morgantown, United States
2 Pioneer Peak Orthopaedic Surgery, Wasilla, United States
3 Department of Orthopaedic Surgery, University of Southern Florida, Tampa, United States
Introduction: Several surgical options exist for decompression of symptomatic lumbar foraminal stenosis that has failed nonoperative treatment. One technique for this is the use of a flexible microblade shaver device (iO-Flex; Spinal Elements, Inc.; Carlsbad, CA, USA). Although this device has been available for several years, clinical reports on its efficacy and complications are limited in the literature. The purpose of this study was to describe long-term clinical results, complications, and revision rates following use of this novel device. A secondary goal was to determine any radiographic predictors of clinical failure following surgery. Material and Methods: A retrospective chart review was conducted to identify all patients undergoing lumbar foraminal decompression with the novel device between 2013 and 2017. Demographic data (including prior spinal surgery), preoperative imaging, postoperative course, and need for revision surgery was collected. Patients were subsequently contacted by telephone during which time clinical status, Visual Analog Scale pain score (VAS, 1-10), and Oswestry Disability Index (ODI) were assessed. Preoperative magnetic resonance imaging (MRI) was analyzed for foraminal dimensions (superior-inferior height, anterior-posterior width, cross-sectional area) using the narrowest point of the neuroforamen. A ratio was created for height divided by width. Posterior height of the intervertebral disc was also measured. Statistical analysis included two-tailed t-tests or chi-squared tests. Results: Forty-three patients met inclusion criteria. Average age at surgery was 60.6 years, and average follow-up was 791 days. Twenty patients had isolated foraminotomy, 23 had another concurrent procedure. Nine patients had undergone previous spinal surgery (none with the novel device). Overall, 14 patients (32.6%) required revision surgery, including 6 of the 9 that had prior spinal surgery (66.7%). Only 8 of 34 patients who had not had prior surgery required revision (23.5%, p = 0.04). Twenty-three patients were successfully contacted for telephone follow-up. Of these, 8 patients (34.8%) required an ambulatory aid. Average VAS pain score was 6.1 (range 0-10). Average ODI was 26.5 (range 0-78). None of the scores correlated significantly with need for revision. Age and concurrent procedure did not correlate with need for revision or ODI. MRI measurements showed average foraminal height of 7.6mm, width of 6.6mm, and ratio (H/W) of 1.23. Average cross-sectional area of the foramen was 51.1mm2, and average posterior disc height was 4.48mm. None of these findings correlated with final ODI or need for revision. Conclusion: At over two-year follow-up, we found no correlation between multiple demographic factors, concurrent procedures, VAS pain, ODI, or preoperative foraminal dimensions with outcomes or need for revision surgery following decompression with the iO-Flex flexible microblade shaver. We did, however, note a high rate of revision, particularly among patients who had undergone previous lumbar surgery, of which 2/3 required revision. This was statistically greater than other patients. Patients should be counseled regarding the potential need for revision when surgery using this novel device is being considered. Surgeons should consider alternate approaches to treating foraminal stenosis in patients who have undergone prior lumbar surgery.
131
A147: Effect modifiers of outcomes after transforaminal endoscopic discectomy versus microdiscectomy for sciatica; subgroup analyses of the PTED-study
Pravesh Gadjradj 1 and Biswadjiet Harhangi 2
1 Weill Cornell, New York, United States
2 Erasmus University Medical Center, Rotterdam, The Netherlands
Objective: Full endoscopic procedures are becoming increasingly popular to treat spine pathology. Recently, we published the results of a randomized controlled trial comparing Percutaneous Transforaminal Endoscopic Discectomy (PTED) with microdiscectomy and showed non-inferiority of PTED in leg pain reduction. Based on previous studies and on the surgical route of PTED (transforaminal versus dorsal during microdiscectomy), some type of disc herniations and some patient groups are hypothesized to be more suitable for one technique over the other. Compelling evidence on this, however, is lacking. Therefore, subgroup analyses were performed with the following objectives: (1) identify which subgroups of patients have better clinical outcomes after lumbar discectomy; (2) which patient groups benefit more from PTED compared to microdiscectomy. Methods: Data were used from a pragmatic, multicenter, non-inferiority, randomized controlled trial comparing the effectiveness of PTED with microdiscectomy for sciatica. Patients with at least 6 weeks of radiating leg pain and an MRI-confirmed lumbar disc herniation, were randomized between PTED or microdiscectomy. The primary outcome was leg pain as measured from a 0 to 100 visual analogue scale (VAS). Secondary outcomes include the Oswestry Disability Index (ODI), VAS back pain and self-perceived recovery. Outcomes were measured longitudinally with the main evaluation point at 12 months. A priori three subgroups analyses were planned: (1) (para)median disc herniations; (2) (extra)foraminal disc herniations; and (3) disc herniations at L5-S1. Linear and logistic mixed model analyses were used to calculate mean differences between treatment and subgroups. Results: Twelve months after surgery, 96% of the 530 patients had follow-up data available according to the per protocol analysis. Regardless of the allocated treatment, patients with (extra)foraminal disc herniations tended to have a higher VAS leg pain (mean difference 7.4, 95%CI 1.4 to 13.3), higher ODI (5.1, 95%CI 1.3 to 8.7) and lower odds for recover (odds ratio 0.5, 95%CI 0.3 to 0.8) than patients with (para)median disc herniations at 12 months. Patients with disc herniations at L5-S1 had similar clinical outcomes as patients with disc herniations at other levels. When comparing treatment effects between PTED and microdiscectomy within these three subgroups, no statistically significant interaction was found meaning that PTED had similar outcomes across these subgroups. Conclusions: The hypothesis that PTED is less suitable than microdiscectomy to treat (para)median discs or disc herniations above L5-S1, are not supported by this data. (Extra)foraminal disc herniations, however, might have slightly worse outcomes than (para)median disc herniations. These differences were, however, small and may not be clinically relevant.
Trial registration: ClinicalTrials.gov number NCT02602093.
Funded by ZonMw, The Netherlands Organization for Health Research and Development;
1513
A148: Uniportal versus biportal endoscopic decompression for lumbar spinal stenosis
Brian Chin 1 , Shuxun Lin 1 , Gamaliel Tan Yu Heng 1 , and Pang Hung Wu 1
1 Department of Orthopaedic Surgery, National University Health System, Singapore, Singapore
Introduction: Endoscopic spine surgery has been established as a practical, minimally invasive technique for decompression in patients with lumbar spinal stenosis. However, there remains a paucity of studies comparing the efficacy of uniportal and biportal endoscopic decompression surgery – both viable techniques with satisfactory clinical outcomes in the treatment of lumbar spinal stenosis. The objective of the present study is to compare the efficacy of uniportal and biportal endoscopic decompression surgery for patients with lumbar spinal stenosis. Material and Methods: Patients with lumbar spinal stenosis and neurogenic claudication were randomized to either uniportal or biportal endoscopic decompression. Total enrolment period was 12 months. Baseline characteristics, initial clinical presentation, and operative details including complications were recorded for all included patients. Clinical outcomes, such as visual analogue scale (VAS) and Oswestry Disability Index (ODI), were recorded at preoperative, immediate postoperative, 2 weeks, 3, 6, and 12-month follow-up periods. Results: A total of 62 patients underwent endoscopic decompression surgery for lumbar spinal stenosis (29 uniportal, 33 biportal). No significant differences were found between uniportal and biportal decompression, when comparing operative duration (130 vs 140 mins; p = 0.30), intraoperative blood loss (5.4 vs 6mLs; p = 0.05), and length of hospital stay (23.6 vs 20.3 hours; p = 0.35). Two patients (7%) who underwent uniportal endoscopic decompression required conversion to open surgery due to inadequate decompression. VAS score (leg & back) and ODI improved significantly (p < 0.001) in both endoscopic decompression groups across all follow-up time points, with no appreciable statistical differences between both groups. Conclusion: Uniportal endoscopic technique has the safe efficacy as biportal technique for decompression surgery in the treatment of lumbar spinal stenosis. While uniportal endoscopic surgery enjoys added aesthetic benefits of only one wound, biportal endoscopic surgery had lesser risks of inadequate decompression and conversion to open surgery, albeit statistically non-significant.
1642
A149: Peri-operative and radiographic outcomes between static and expandable cage in patients undergoing minimal invasive transforaminal interbody fusion: meta-analysis
Gun Keorochana 1 and Jatupon Kongtharvonskul 1
1 Orthopedics Department, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Objective: Transforaminal lumbar interbody fusion (TLIF) is a widely used technique for the treatment of degenerative pathologies of the lumbar spine. The interbody device serves to provide a large fusion surface to optimize fixation. In addition, there are potential secondary benefits of device placement depending on the interbody spacer type and position, which may include restoration of disk height, segmental lordosis, and increased foraminal heigh. A wide variety of TLIF interbody devices are available on the market today, however, the effect of cage choice on postoperative clinical and radiographic parameters remains controversial. The static intervertebral fusion cage was introduced since1990s and has become the device of choice in TLIF. While Expandable cages (EC) are a relatively new invention hypothesized to provide greater restoration of disk height and foraminal height, along with improvement in segmental lordosis, compared with static interbody cage (SC). Therefore this meta-analysis of static and expandable cage in TLIF was conducted with the aim of updating the comparison of the two for post-operative outcomes (visual analog scores (VAS) of back and leg, Oswestry disabilities index (ODI), complications, subsidence, fusion and reoperations), intraoperative outcomes (blood loss, operative time and length of stay) and radiographic parameter (anterior disc height, posterior disc height change, Lumbar lordosis change, segmental lordosis and foraminal height) in patients undergoing minimal invasive lumbar transforaminal interbody fusion. Methods: This systematic review was conducted according to the PRISMA guidelines. Relevant studies that reported post-operative outcomes, intra-operative and radiographic parameter of either technique were identified from Medline and Scopus from inception to September 25th, 2022. Results: Total of fourteen studies there were 908 and 673 patients in SC and EC groups. The unstandardized mean difference (UMD) of VAS of back and leg, ODI, blood loss, operative time length of stay, anterior disc height, posterior disc height change, Lumbar lordosis change, segmental lordosis and foraminal height in SC were 0.21 (95%CI: -0.65 to 1.07) scores, 0.25 (95%CI: -0.32 to 0.82) scores, 0.61 (95%CI: -0.40 to 1.62) scores, 0.27 (95%CI: -0.02 to 0.55) cc, -0.08 (95%CI: -0.41 to 1.03) minutes, 0.08 (95%CI: -0.40 to 0.56) days, -2.68 (95%CI: -5.89 to 0.53) degree, -1.00 (95%CI: -2.25 to 0.24) degree, -5.02 (95%CI: -14.4 to 4.37) degree, -0.08 (95%CI: -0.41 to 0.25) degree and -2.99 (95%CI: -6.55 to 0.56) degree without statistically significant difference when compared to EC group. The chance of having complications, fusion, subsidence and reoperations in SC were 0.76 (95%CI: 0.43 to 1.32) times, 1.39 (95%CI: 0.72 to 2.69) times, 0.25 (95%CI: 0.07 to 0.89) and 1.60 (95%CI: 0.69 to 3.69) times when compared to EC. No significant differences were noted for complications, fusion and reoperations between two groups. Conclusion: This meta-analysis indicated that expandable cage has about 4 times higher risk of having post-operative subsidence when compared to static cage in patients undergoing TLIF. However there have no differences in term of intraoperative blood loss, operative time, length of stay, radiographic change, back and leg pain, disability score, complications, fusion and reoperation rates.
1912
A150: OLIF for revisison surgery and indirect decompression
Dimitar Haritonov 1
1 Nearosurgery and Spinal Surgery, Heart and Brain Hospital, Pleven, Bulgaria
Introduction: Clinical outcome of indirect decompression for a revision surgery, at the same level of a previous lumbar decompression, has not been reported. The purpose of this study was to investigate the efficacy of oblique lateral interbody fusion (OLIF) in revision surgery after decompression for degenerative lumbar spinal disease. Material and Methods: We included 72 patients who were preoperatively diagnosed with a recurrence of canal stenosis, foraminal stenosis, or intervertebral instability at the same level of a prior lumbar decompression. These patients underwent OLIF with supplemental pedicle screw fixation without additional posterior decompression. All patients completed a minimum 1-year follow-up. We compared the cross-sectional area (CSA) of the thecal sac on magnetic resonance imaging as well as clinical outcome scores (ODI and VAS score) preoperatively and at the final follow-up. Fusion status, intervertebral foramen width and disc height/angle were evaluated based on computed tomography scans. Results: The CSA expanded from 136.4 ± 57.9 mm2 preoperatively to 194.1 ± 58.6 mm2 at the final follow-up (mean: 27.4 months; p < 0.001). Clinical symptoms significantly improved (59.0% improvement rate of ODI and VAS score) at the average of a 17.1-month follow-up. The fusion rate was 93.0%. The disc height was restored (preoperative: 5.7 mm; postoperative: 8.3 mm; P < 0.001), and foraminal stenosis significantly improved postoperatively. There were no major vascular/ureteral injuries. Conclusion: OLIF at the same level of a prior lumbar decompression provided a successful indirect decompressive effect, including expansion of the thecal sac, restoration of disc height, and subsequent improvement of foraminal stenosis. Specifically, this procedure can prevent incidental durotomy and nerve root injury, which may occur in conventional revision surgeries for direct posterior fusion.
1575
A151: Stand-alone ALIF versus TLIF in patients with low back pain - a propensity-matched cohort study with two-year follow-up
Peter Udby 1,2 , Leah Carreon 2 , Mikkel Østerheden Andersen 2 , Ali Toma 1 , Dennis Hallager 1 , and Rune Dueholm 1 Bech 3
1 Spine Surgery and Research, Zealand University Hospital, Køge, Denmark
2 Spine Surgery and Research, Spine Center of Southern Denmark, Lillebaelt Hospital, Middelfart, Denmark
Introduction: Instrumented lumbar fusion performed by an anterior or a transforaminal approach has theoretically different advantages and disadvantages. Few studies have compared Patient Reported Outcomes (PROs) between standalone anterior lumbar interbody fusion (ALIF) and transforaminal lumbar interbody fusion (TLIF). The study aimed to compare Patient Reported Outcomes (PROs) at two-year follow-up after ALIF and TLIF in patients with lumbar degenerative spine conditions. Material and Methods: We performed a dual-center cohort study over a nine-year period (2010-19) on patients undergoing single-level ALIF or TLIF. All patients were registered in the Danish National spine registry (DaneSpine). Prospective data were collected preoperatively and at one and two-year follow-up. Propensity score matching was performed. Primary outcomes were the Oswestry Disability Index (ODI), visual analog scale (VAS), and quality of life measured by European Quality of Life-5 Dimensions (EQ-5D) index score. Patient satisfaction was measured as a secondary outcome. Results: A total of 92 patients were matched, 46 ALIF and 46 TLIF. Both groups obtained statistically significant improvement in the ODI. No significant difference was observed at two-year follow-up -ALIF 30 ± 19 vs TLIF 36 ± 23; p = 0.140. We found similar improvement with no significant difference for EQ-5D score between the groups - ALIF 0.65 ± 0.35 vs TLIF 0.59 ± 0.26; p = 0.250. Pain scores at two-year follow-up were - leg pain ALIF 40 ± 31 vs. TLIF 39 ± 33; p = 0.877 and back pain ALIF 45 ± 31 vs. TLIF 50 ± 28; p = 0.365. Patient satisfaction reported at two-year follow-up was 58% in the ALIF group vs 49% in the TLIF group, while 18% vs 27% were dissatisfied. Conclusion: Patients treated with ALIF and TLIF improved significantly in ODI, back and leg pain, and EQ5D index score at two years compared to baseline. We found no significant differences in improvement between the groups.
992
A152: Assessing the importance of radiographic and clinical parameters when choosing decompression without fusion for LDS: results from the CSORN prospective DS study
Renan Jose Rodrigues Fernandes 1,2 , Jennifer Urquhart 1 , Patrick Thornley 1,2 , Raja Rampersaud 3 , Andrew Glennie 4 , Charles Fisher 5 , and Chris Bailey 1,2
1 Spine Surgery, London Health Sciences Centre, London, Canada
2 Surgery, University of Western Ontario, London, Canada
3 Surgery - Spine, Toronto Western Hospital, Toronto, Canada
4 Surgery - Orthopaedics, Dalhousie University, Halifax, Canada
5 Department of Orthopaedics,University of British Columbia, Vancouver, Canada
Introduction: The decision to decompress without fuse in lumbar degenerative spondylolisthesis surgery is partially based on an assessment of stability. Traditionally, recognized indications for fusion included more than 25% slip (≥ grade II), dynamic instability defined by >3mm motion between pre-op standing versus supine or flexion extension views, significant pre-op back pain, facet effusion, and lordotic disc angle. Despite meeting those fusion indications, a subset of patients within a multi-centred prospective study have been treated without fusion. This study examines the correlation between radiographic instability (> 3 mm translation on lateral film) and patient-reported outcomes (PRO) and radiographic measures in decompressed patients. Methods: The CSORN multi-centred prospective study on the assessment and management of LDS database was retrospectively reviewed to identify patients who had decompression surgery. Out of a total of 567 patients enrolled across eight centres, 109 patients that underwent decompression alone between 2015 and 2020 and had radiographic measures were included in the present study. Subjects were defined as stable if there was less than 3mm of translation between supine and standing pre-operative lateral or unstable if equal or bigger than 3mm of translation. Demographic, clinical and radiographic characteristics were compared at baseline. Operative details were compared between the groups. Patient-reported outcome measures (ODI, SF36 PCS and MCS, back pain and leg pain) were compared between the groups at baseline and 3 months and 1 year after surgery. Results: Out of the 109 patients, 81 were considered stable and 28 unstable. At baseline, there were no radiographic differences between the groups. The stable group was older in relation to the unstable groups (70.6 vs 66.3, p = 0.045), and the number of patients with grade II spondylolisthesis was higher in the unstable group (25% vs 7.4%, p = 0.032). Surgical time was longer in the unstable group (103 vs 84 minutes, p = 0.011) despite the number of multilevel procedures being higher in the stable group (30.8% vs 10.7%, p = 0.007). Using a mixed-model repeated measures analysis for the PROMs, patients in the unstable group had worse SF36-MCS at baseline (46.2 vs 50.9, p = 0.047) but were not different at 3 months and 1 year after surgery. No differences were found between groups for ODI, SF36-PCS, and back and leg pain at any time point. Conclusion: Our study identified that surgeons are becoming more liberal in their decision not to utilize fusion, and despite some indication of instability, no major difference was found between the groups with preoperative radiographic parameters and PROMs.
1687
A153: The cortical bone trajectory versus traditional pedicle screw fixation in the treatment of osteoporotic lumbar degenerative patients: a prospective RCT study
Hongtao Ding 1 , Yuzeng Liu 1 , and Yong Hai 1
1 Spine Surgery, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: To elucidate the clinical and radiographic outcomes and complications of cortical bone trajectory (CBT) screw fixation in patients with osteoporosis at 24 months follow-up and to compare the results with those after transforaminal lumbar interbody fusion (TLIF) using traditional pedicle screw (PS) fixation. Material and Methods: We enrolled 124 patients and randomly assigned them to 2 groups (each group had 62 participants). The primary outcome: fusion rate, secondary outcome measures include 1) clinical outcomes: visual analog scale (VAS), Oswestry Disability Index (ODI), and Japanese Orthopaedic Association Score (JOA); 2) surgical parameters: operating duration, incision length, estimated blood loss, and drainage volume; 3) radiologic outcomes; 4) complications. Results: At the 6- and 12-month follow-up points, similar fusion rate was observed based on CT scan in both groups (p = 0.583 and 0.583). According to the clinical outcome, CBT provided significant better short-term functional status at 3 months post-operation regarding ODI and JOA score (p = 0.012 and 0.000), and similar improvements in pain intensity and functional status at other follow-up point. In addition, CBT resulted in significantly better surgical characteristic. Notably, CBT fixation led to lower incidence of screw loosing in osteoporotic population (p = 0.006). Conclusion: The CBT screw fixation for single-level lumbar fusion in patients with osteoporosis provided improvement of clinical symptoms comparable to that of TLIF using PS fixation. In addition, statistically significant lumbar stability was found in the CBT group. Since the present study, we suggest CBT screw fixation to be a reasonable and superior alternative to PS in TLIF for osteoporotic population.
OP18: Contemporary Cervical Surgery
548
A154: A randomized trial of cervical orthosis versus no orthosis following multi-level posterior cervical fusion
Renan Jose Rodrigues Fernandes 1,2 , Patrick Thornley 1,2 , Jennifer Urquhart 1 , Sean Kelly 1 , Nasser Alenezi 1 , Abdulmajeed Alahamari 1 , Kevin Gurr 1,2 , Fawaz Siddiqi 1,2 , Supriya Singh 1,2 , Parham Rasoulinejad 1,2 , and Chris Bailey 1,2
1 Spine Surgery, London Health Sciences Centre, London, Canada
2 Surgery Department, University of Western Ontario, London, Canada
Introduction: Temporary postoperative immobilization with cervical orthosis (CO) is commonly utilized following posterior cervical fusion (PCF). However, this practice predates modern fusion techniques, and there is a lack of evidence in the literature regarding the practice. The primary indication for CO likely is a reduction in postoperative pain, although other potential advantages include decreased wound dehiscence and patient reassurance. Potential disadvantages may include patient discomfort, inconvenience, functional limitation, and cost to the health care system. Given the lack of evidence surrounding cervical collar use in this indication, our study aims to determine whether postoperative neck pain following multi-level PCF with CO is equivalent to multi-level PCF without orthosis. Materials and Methods: We conducted a single-centre, prospective, randomized, non-blinded, equivalence trial. Between March 2020 and May 2022, patients requiring multi-level (2- or more level), open, posterior cervical fusion extending no further than the second thoracic vertebrae (C1-T2) were enrolled and randomly assigned by 1:1 allocation to cervical orthosis (Collar) or no orthosis (No Collar) after PCF. Randomization was stratified based on: 1. trauma vs degenerative indication; and 2. pre-operative opioid use. Exclusion criteria were traumatic spinal cord injury, infection, tumour, primary sagittal deformity, inability to provide consent or comprehend patient-rated outcome instruments, previous surgery involving the same level, dementia, substance abuse, and psychosis. Primary outcome measure was neck pain intensity during the first 4 weeks after surgery, using the numerical pain rating scale (0 to 10 with higher scores indicating more severe symptoms). The equivalence margin was set at δ = 2 points. Secondary outcome measures included NDI, SF12, arm pain, range of motion (ROM), compliance, length of hospital admission, and comparison of procedural details and outcomes/complications postoperatively. A mixed model of longitudinal regression for repeated measures was used to analyze the primary outcome, accounting for the correlation among the outcome score on the same patient at 2 days, 2 weeks, and 4 weeks. Treatment (collar vs no collar), time, treatment x time interaction and baseline scores were included as fixed variables. Results: Sixty-two patients were enrolled in the study, 31 in the collar group and 31 in the no collar group. At baseline, the Collar group had more neck pain than the No Collar group (5.3 vs 3.2, p = 0.013). Otherwise, baseline characteristics and procedural details were similar between the groups. For the primary outcome, neck pain intensity score was 4.6 ± 0.3 for the Collar group vs. 4.9 ± 0.3 for the No collar group. The 95% confidence interval (-1.4 to 0.2) was within the predetermined margin of equivalence. No differences were found between groups for NDI or SF12 at any of the time points. The collar group had reduced neck range of motion at 6 weeks, but there was no difference between groups after 12 weeks. No differences in postoperative complications or adverse events were observed. Conclusion: Compared with patients treated with a CO, patients treated without orthosis maintain similar pain scores during the early postoperative period without increasing the risk of adverse events.
1008
A155: Clinical impact for progression of ossification of the posterior longitudinal ligament after cervical laminoplasty
Kawaguchi Yoshiharu 1 , Taketoshi Yasuda 1 , Shoji Seki 1 , Kayo Suzuki 1 , Kenta Watanabe 1 , Hiroto Makino 1 , Hayato Futakawa 1 , Katsuhiko Kamei 1 , Tran Canh Tung Nguyen 1 , and Zhongyuan He 1
1 Department of Orthopaedic Surgery, University of Toyama, Toyama, Japan
Introduction: Laminoplasty is a standard operation for the treatment of cervical myelopathy caused by cervical ossification of the posterior longitudinal ligament (OPLL), as cervical OPLL often causes multi-level spinal cord compression. It has been reported that the long-term surgical outcome of laminoplasty is favorable in most of the patients with cervical OPLL.1 However, as OPLL is a progressive disease,2 neurological deterioration is frequently encountered due to the progression of the ossified lesion. However, the incidence and characteristics of neurological deterioration due to OPLL progression after the first posterior surgery have not yet been precisely elucidated. Aim: The purpose of this study was 2 fold: 1) To analyze the incidence of patients who required an additional second surgery for the neurological deterioration due to OPLL progression, and 2) To clarify the clinical characteristics and surgical outcome of the patients. Materials and Methods: This study was carried out in a single institute with a long-term follow-up. From 1981 to October 2015, 201 patients with myelopathy due to cervical OPLL underwent laminoplasty. One hundred sixty-seven patients who could be followed for more than 2 years were included. The neurological finding was graded by JOA score. If the patients had both neurological deterioration with clinical symptoms and OPLL progression, we judged as the neurological deterioration was caused by the OPLL progression. We retrospectively examined the incidence of the patients who required an additional second surgery. We also evaluated the clinical characteristics and the surgical outcome after second operation. In the patients who required a second surgery due to OPLL progression (the second surgery group), the period from laminoplasty to second surgery was checked. The symptoms requiring the second surgery were evaluated. Clinical characteristics, including sex and age at cervical laminoplasty, were compared with the patients who did not have a second surgery during follow-up (the control group). Results: Nine patients (5.4%) out of 167 patients had the second surgery by neurological deterioration due to OPLL progression. The age in the second surgery group was younger than that in the control. The mixed type of OPLL in the second surgery group was more than that in the control group. The symptoms of neurological deterioration were progressive cervical or thoracic myelopathy in 6 patients and radiculopathy in 3. The neurological recovery was achieved in 6 patients after the second surgery, however, 3 still had the neurological deficit. The patients who showed poor recovery had clear T2 high intensity by MR image in the spinal cord. Conclusion: Young age at laminoplasty and mixed type of OPLL were risk factors for OPLL progression. Revision surgery was effective, but if the patients had clear T2 high intensity in the spinal cord, the recovery was poor. Thus, revision surgery should be considered before irreversible neural damage occurs.
References:
1. Kawaguchi Y, et al. More than 20 years follow-up after en bloc cervical laminoplasty. Spine 2016; 41: 1570-1579.
2. Kawaguchi Y, et al. Progression of ossification of the posterior longitudinal ligament following en bloc cervical laminoplasty. J Bone Joint Surg Am 2001; 83-A: 1798-1802.
133
A156: Does preoperative T1 slope affect the revision rate of multilevel posterior cervical or cervical-thoracic fusions: multi-center analysis
Eeric Truumees 1 , Devender Singh 1 , Ashley Duncan 1 , William Lavelle 2 , Ron Riesenburger 3 , Matthew Geck 1 , Thomas Mroz 4 , and John Stokes 1
1 Spine, Ascension Texas Spine and Scoliosis, Austin, United States
2 Spine, State University of New York Upstate Medical University, Syracuse, United States
3 Spine, Tufts Medical Center, Boston, United States
4 Spine,Cleveland ClinicCleveland, United States
Introduction: Previous studies have highlighted the biomechanical effect of high T1 slopes on lordic force and the subsequent acceleration of kyphosis in postoperative cervical laminoplasties. While the data and collective opinion remain varied when determining whether the caudal end of a posterior cervical fusion should routinely be in the cervical or thoracic spine, adjacent level stenosis and non-union are leading precipitating factors of revision. Aim: This study examines if preoperative T1 slope should be used when planning the caudal instrumented vertebra in multilevel posterior cervical fusions. Materials/Methods: Analysis of multicenter radiographic and clinical databases of patients that underwent a three or more-level posterior cervical fusion for degenerative disease between January 2013 and May 2015, with at least two years of post-operative (post-op) data. Patients were divided into two groups: Group I (fusion ending within the cervical spine) and Group II (fusion extending into the thoracic spine). Multiple radiographic variables, including cervical lordosis, thoracic kyphosis and T1 slope, were measured preoperatively and post-operatively at two weeks, one month, three months, six months, one year and two-year intervals. All radiographic measurements were performed by an independent, experienced clinical researcher. Paired t-test were used to compare means with a level of significance set at ɑ = 0.05. Results: There were 168 and 96 patients in Group I and II, respectively. Overall revision rate was 10.4%. Index surgeries ending in the cervical spine (Group I) had a higher rate of revision than those extending into the thoracic spine (Group II), 11.3% and 9.4% respectively, but were not statistically significant. At two years post-op, cervical lordosis had improved in both groups (12.6° and 14.1°), but the difference between groups was not statistically significant. Though there was no significant difference in T1 slope from two-weeks to two years post-operative, it is noted that patients with a cervical caudal level consistently had higher T1 slopes than those that terminated in the thoracic spine, regardless of revision status. Both groups showed significant improvement in pain (Visual Analog Scale) and function (Oswestry Disability Index) outcomes at two years post-op, but there was no statistical advantage of one terminal level over the other. Conclusion: As with previous studies, this study did not reveal a clear advantage of a cervical or thoracic last instrumented vertebra (LIV) in multilevel posterior cervical fusion. There was no evidence that preoperative T1 slope had an effect on revision rate in either the cervical or thoracic groups. It is noted, however, that though not significant, the cervical group did have higher T1 slopes consistently throughout the analysis. While this individual measure may not be a singular determinant in end level selection, future studies may include preop T1 slope vs. cervical lordosis mismatch in decision making about both appropriate LIV and the need for concomitant anterior interbody or osteotomy procedures.
1268
A157: Effects of adverse childhood experiences in the subjective global health outcomes in anterior cervical decompression and fusion surgery
Yak Nak 1,2 , Angela Atkinson 1,2 , Amanda Faust 1,2 , Michaela Thomson 1,2 , and Theodore Choma 1,2
1 Orthopaedic Spine, Missouri Orthopaedic Institute, Columbia, United States
2 Orthopaedic Surgery, University of Missouri School of Medicine, Columbia, United States
Introduction: Adverse Childhood Experiences (ACEs) have been linked to health outcomes – mortality, readmission rates, and safety of care – across various specialties (e.g., family medicine, internal medicine), however, limited studies exist in surgical specialties (e.g., orthopaedics). The ACE score is a battery of ten questions that quantifies an individual’s exposure to adverse childhood experiences: smoking, severe obesity, physical inactivity, depressed mood, suicide attempts, alcoholism, drug abuse, parenteral drug abuse, a high number of sexual partners, and history of sexually transmitted infections. In general, patients with ACE risk factors who seek orthopaedic care have more complex injuries, decreased quality of life, prolonged post-surgical pain, and increased risk for postoperative complications. Patients with higher ACE scores are known to have more complex spinal injuries such as multi-level vertebral fractions and spinal cord injuries leading to increased rates of surgical management in these populations. While management of patients with increased ACE scores is known to be more complex, literature is sparse regarding correlations between ACE scores and outcomes following common orthopaedic spinal surgeries such as anterior cervical discectomy and fusion (ACDF). This study aims to identify the impact of ACE scores and postoperative outcomes for patients undergoing ACDF for surgical management of symptomatic cervical disk degeneration and stenosis. This study seeks to test the hypothesis that orthopaedic patients over the age of 18 with higher ACE scores will report lower global health patient-reported outcomes at 12 months following ACDF surgery. Material and Methods: Between Jan. 2019-Mar. 2022, adult patients (> = 18) undergoing primary ACDF with at least 6-months follow up were identified and approached for inclusion in a retrospective cohort analysis. Patients who consented to participate were administered a validated ACE Questionnaire, PROMIS Scale v1.2 – Global Health, and Pain Catastrophizing Scale Short-Form (PCS-4) to measure subjective global health outcomes. Patient demographics were obtained from the medical record and included in analysis. ACE scores and ACE impact scores, subjective ACE impact on one’s health, were analyzed as a categorical variable using ANOVA and KW Testing. Included and excluded survey responders were compared for outgroup differences. Significance was set at p < .05. Results: A total of 39 patients (n = 19 males) consented for study participation with mean follow-up of 11.38 months (range 6-12 months). Mean patient age was 62.86 years (range 56.03-71.82), with a mean ACE score of 2.05 + 1.89. When compared to patients with ACE scores 1 or below, patients with ACE scores 2 or above were significantly (p = .02) associated with both lower Global Physical Health scores (46.32 vs. 39.25) and significantly (p = .01) increased PSC-4 scores (9.5 vs. 22.2). Categorically, increased ACE impact scores were associated with increased PSC-4 scores (p = .03). Conclusion: ACE scores provide an important measure for assessing risk factors for decreased patient-reported outcomes up to 12 months following ACDF surgery. Patients with higher ACE scores were found to report lower PROMIS global health, mental health, and pain catastrophizing up to 12-months after ACDF. Further studies should seek to identify strategies for moderating suboptimal outcomes in patients with high ACE scores undergoing ACDF.
1589
A158: Prediction of outcome in patients with degenerative cervical myelopathy
Lovisa Gerdhem 1 , Anastasios Charalampidis 2 , and Paul Gerdhem 3
1 Dept. of Surgery, Danderyd Hospital, Sweden
2 Dept. of Acute Surgery,Karolinska University Hospital, Trauma and Orthopaedics, Sweden
3 Dept. of Surgical Sciences, Uppsala University, Uppsala, Sweden
Introduction: Degenerative cervical myelopathy is the most common cause of spinal cord compromise in adults. Surgery is often the treatment of choice. Identifying predictors may help to improve patient selection. Our aim was to investigate whether improvement after surgery for degenerative cervical myelopathy is associated with preoperative disease severity and to identify predictors of outcome. Material and Methods: This is a retrospectively designed study on prospectively collected registry data. We identified 901 patients treated surgically for degenerative cervical myelopathy in the Swedish spine registry (Swespine). To investigate improvement in different disease severity groups, the individuals were divided into quartiles based on their preoperative European Myelopathy scale (EMS) and EQ-5D index. Statistical analyses were made with analysis of variance, Chi-square, McNemar and t-tests. Multivariable linear or logistic regression was used to identify predictors for one-year improvement in EMS and EQ-5D index, and satisfaction at one year. In the regressions, the patient reported outcome measures were dichotomized at their median, except improvement in EMS which was used as a continuous variable. Results: All patient reported outcome measures improved significantly from baseline to the one-year follow-up (p < 0.001). Statistically significant outcome improvements were seen in all disease severity groups. Preoperative low EMS (Beta = -1.37, p < 0.001), long walking distance (< 500 m vs > 500 m; Beta = 0.44, p = 0.030), and low NDI (Beta = -0.43, p = 0.048) were independent predictors of improvement in EMS. R2 was 0.11 for the multivariable model. Preoperative low EQ-5D index (odds ratio 0.11; 95% confidence interval 0.07-0.16) and low NDI (0.56; 0.36-0.88) were independent predictors of improvement in EQ-5D index. Preoperative high EMS (1.86; 1.20-2.90) and shorter arm pain duration (< 12 months vs > 12 months (0.54; 0.33-0.88) were independent predictors of satisfaction. Conclusion: Postoperative improvement was seen over the whole range of disease severity. Disease severity, symptom duration, and walking distance were predictors of outcome in patients treated surgically for degenerative cervical myelopathy.
1231
A159: The degenerative cervical myelopathy subjective and objective score (DCM-SOS): a novel outcome measure
Khadija Soufi 1 , Tess Perez 1 , Patricia Balatbat 1 , and Allan Martin 1
1 Department of Neurological Surgery, University of California, Davis, Sacramento, United States
Introduction: Degenerative cervical myelopathy (DCM) is a common, debilitating, and treatable condition in which the discs, ligaments and vertebrae compress the cervical spinal cord causing neurological dysfunction. Clinical management of DCM is informed by clinical practice guidelines (CPGs) that recommend surgical treatment for patients categorized with moderate to severe neurological impairment, and patients with deteriorating mild impairment. However, categorization of DCM severity is based solely on the modified Japanese Orthopedic Association (mJOA) score, which is a simplistic tool that assesses 4 domains on ordinal scales (utilizing subjective terms such as “mild” or “severe”). In this study, we sought to develop and validate a novel outcome measure, the DCM Subjective and Objective Score (DCM-SOS) that combines subjective questions with brief objective scored neurological examination. Material and Methods: A prospective cohort study was conducted with extensive data collection that included demographics, medical history, symptom history (duration, severity, etc.), mJOA, NDI, QuickDASH, EQ-5D-5L, EQ-VAS, power testing in 22 myotomes, JAMAR grip dynamometer, 1-2, 1-5, and 2-3 digit pinch dynamometer, sensory testing (light touch - LT, pin prick - PP, monofilaments, proprioception, vibration) in upper extremities (UE) and lower extremities (LE), GRASSP-Myelopathy (UE strength, sensation, dexterity), Berg Balance, manual gait and balance testing, and quantitative gait and balance testing using an electronic Protokinetics Zeno Walkway (self-paced, fast-paced, tandem gait, tandem stance, Romberg, standing on one foot). Subjective questions were based on differences between DCM and healthy subjects, including those used in the mJOA but with more explicit scoring of levels. Objective physical measurements were selected for inclusion in the DCM-SOS based on the following criteria: significant differences between DCM and healthy controls, correlation with mJOA score, no correlation with age (in healthy subjects), and no requirement for specialized equipment. Results: 46 patients with DCM and 55 healthy subjects were enrolled. Subjective ordinal questions were developed for UE coordination, UE strength, LE ambulation, UE and LE sensation, urinary/bowel/sexual function, and overall pain (p = 6 x 10-11). Among 278 objective measurements that were considered for inclusion, the following showed strong differences and were selected based on the criteria above: manual power testing of 1st dorsal interosseous (p = 1 x 10-14), thumb opposition (p = 6 x 10-12), finger extension (p = 4 x 10-7), elbow flexion (p = 1 x 10-6), and elbow extension (3 x 10-6); sensory testing of UE PP (p = 1 x 10-7), and UE LT (1 x 10-7); tandem gait score (4 x 10-8); and reflex testing for Hoffman, Tromner, or Babinski (p = 6 x 10-7). A draft version of the DCM-SOS was developed with 6 subjective domains (/30 points) and 4 objective domains (/30 points). Conclusion: The DCM-SOS is a data-driven outcome measure that can be performed in 5-10 minutes without specialized equipment and incorporates focused subjective and objective data regarding neurological function. Validation of this tool in a large prospective cohort is promising, with the hope that this tool may help improve clinical management, inform future CPGs, and enhance clinical trials for patients with DCM.
1278
A160: Enhanced measures to quantify gait and balance impairment in degenerative cervical myelopathy: a prospective study
Tess Perez 1 , Allan Martin 1 , Khadija Soufi 1 , and Patricia Balatbat 1
1 Neurosurgery, University of California, Davis, Spine
Introduction: Degenerative cervical myelopathy (DCM) is a common, debilitating, and treatable condition where the discs, ligaments and vertebrae compress the cervical spinal cord causing neurological dysfunction. Clinical management of DCM is variable between practitioners and guidelines are based only on the subjective modified Japanese Orthopedic Association (mJOA) score. Gait and balance impairment are among the cardinal symptoms of DCM, but utilizing objective measurements of these functions is highly challenging. In this study, we sought to investigate a wide array of quantitative gait and balance parameters and subsequently validate a novel outcome measure that can be performed in routine practice. Material and Methods: A prospective cohort study was conducted with extensive gait and balance data collection and included demographics, medical history, symptom history, mJOA, EQ-5D-5L, EQ-VAS, myotome power testing, multimodal sensory testing), Berg Balance scale, manual gait and balance testing with scored assessments (counting wobbles as a visible trunk correction to maintain balance, and stumbles as a touch with hand or foot to stabilize balance), and quantitative gait and balance testing using a Protokinetics Zeno Walkway electronic pressure mat. Tasks included self-paced walk, fast-paced walk, tandem gait, tandem stance, Romberg, and standing on one foot, and quantitative measures included velocity, stability ratio (SR; single stance time/double stance time), and gait variability index (GVI; variability of a composite of parameters) for walking tests, and center of pressure (COP) standard deviation in left-right (L-R) and anterior-posterior (A-P) directions for balance and tandem gait tasks. Results were compared between DCM and healthy subjects and correlation analysis was performed between manual and electronic measurements. Results: 41 patients with DCM and 55 healthy control subjects (HCS) were enrolled. Metrics including velocity (p = 5x10-8, p = 3x10-7), GVI (p = 2x10-8, p = 0.002), and SR (p = 4x10-7, p = 1x10-5) differed between DCM patients and healthy controls for both self-paced and fast-paced gait assessments, respectively. The COP variability in L-R (p = 0.002) and A-P directions (p = 1x10-4) differed between DCM and healthy subjects. Standing on either the Left or Right foot also showed a difference in COP variability in both directions: L-R (p = 4x107 Left, p = 8x10-7 Right) and A-P (p = 7x10-4 Left, p = 1x10-4 Right). On manual assessments, DCM patients were worse or trended toward worse scores in all tasks including self-paced (p = 0.06), fast-paced (p = 0.06), tandem gait (p = 4x10-8), Romberg eyes open (p = 0.02), Romberg eyes closed (p = 0.02), L foot standing (p = 7x10-6), R foot standing (2x10-6), and tandem stance (p = 9x10-5). Conclusion: Quantitative parameters from an electronic pressure mat can be used to assess gait and balance impairment with high sensitivity and strong correlation with subjective measures. Manual scoring of tandem gait, standing on one foot, and tandem stance also provided robust differences between groups and correlated strongly with subjective measures of gait and balance. These can be completed in under 5minutes in a standard clinic setting and easily adopted into routine clinical assessment of DCM patients.
1735
A161: Intraoperative neuromonitoring for anterior cervical surgery. A multicenter experience and literature review
Giovanni Barbagli 1 , Paolo Di Russo 2 , Mariano Vitelli 1 , Nicoletta Gargiuoli 1 , Elisabetta Peppucci 1 , Giulio Wembagher 3 , Matteo Capozza 4 , Alexander Evins 5 , Alessandro DiChirico 1 , and Sandro Carletti 1
1 Neurosurgery, IFCA, Florence, Italy
2 Istituto Neurologico Mediterraneo - Neuromed, Neurosurgery, Pozzilli, Italy
3 Spine Surgery Unit, Azienda Ospedaliero Universitaria Careggi, Florenc, Italy
4 Neurosurgery, Azienda USL Toscana Nord-ovest - Spedali Riuniti, Livorno, Italy
5 Neurosurgery, Weill Cornell Medical College, New York, United States
Introduction: Anterior Cervical Discectomy and Fusion (ACDF) as well as Anterior Cervical Corpectomy and Fusion (ACCF) are among the most common surgical procedures for cervical spine pathologies with or without myelopathy. Even though, in other spinal procedures, the prognostic benefit of intraoperative neurophysiological monitoring (IONM) is well known, this method for detecting impending neurological compromise is not routinely used in the aforementioned surgeries. Moreover, in the current literature there are no prospective studies validating the efficacy of IONM for these procedures. The aim of the study is primary to assess there is a routinary use of the intraoperative neurophysiological monitoring in four main spine centers in our country and the procedure used to assess the neurological status pre-/intra and postoperatively; secondly, to evaluate the efficacy in the early detection of segmental injury as well as long tract injury and in reducing the rate of post-operative neurological complications. Material and Methods: The authors retrospectively selected four cohorts of patients that are comparable in terms of age, risk factors, male-to-female ratio, type of surgery and length. Authors include in the study both ACDF and ACCF procedures regardless of the number of levels treated, from January 2020 to January 2022. One hundred ninety-five patients, admitted without pre-existence myelopathy (regardless the number of level treated) from 15/07/2019 to 15/07/2021, were examined. Descriptive and inferential statistics were performed using IBM®SPSS® Statistics v.27.0.1.0 analysis software. Descriptive analyses were performed using the frequency for the nominal variables and the means (± standard deviation) for the continuous variables. The differences between before and after neuromonitoring for both sensory and motor neurological deficits were investigated with the McNemar test using the contingency table. Any differences between continuous variables, such as age and duration of intervention, and nominal variables were explored with the Mann-Whitney non-parametric U test for independent samples. An error α = 0.05 was considered for statistical significance. Furthermore, authors carried out a complete literature review and compared the results of the study with the current data on Pubmed and MEDLINE. Results: The gender distribution of our series was quite balanced, with 53.3% of patients being female and 46.7% male. The mean age of the patients was 55.1 (± 12.3) years, while the mean surgical time was 137.7 (± 59.9) minutes with a minimum of 60 and a maximum of 345 minutes. Regarding the differences between the frequency of both sensitive and motor neurological deficits before surgery and those after surgery, our data show that a certain impact of neuromonitoring on post-operative outcomes exists, with a statistically significant difference, in securing a better clinical outcome (p = 0.001). Conclusion: Our data suggests that the routinary use of IONM is an effective and safe tool in reducing neurological deficits rate following anterior cervical procedures, in particular in patients admitted without pre-existing myelopathy. However, prospective studies with a larger sample are needed to provide stronger evidence.
361
A162: A clinical model to predict postoperative improvement in sub-domains of the modified Japanese orthopedic association score for degenerative cervical myelopathy
Byron Stephens 1,2,3 , Lydia McKeithan 4 , William Waddell 1 , Joseph Romano 1 , Anthony Steinle 1 , Andrew Croft 1 , Wilson Vaughan 1 , Jacquelyn Pennings 1,3 , Hui Nian 5 , Inamullah Khan 1 , Mohamad Bydon 6 , Scott Lawrence Zuckerman 1,2 , Kristin Archer 1,3,7 , and Amir Abtahi 1,3
1 Department of Orthopaedic Surgery
2 Department of Neurological Surgery
3 Center for Musculoskeletal Research, Nashville
4 Department of General Surgery
5 Department of Biostatistics
6 Department of Neurosurgery, Mayo Clinic, Rochester, MN, United States
7 Department of Physical Medicine and Rehabilitation,Vanderbilt University Medical Center, Nashville, TN, United States
Introduction: Degenerative cervical myelopathy (DCM) is one of the most common disorders of the spinal cord, resulting from disc degeneration, facet hypertrophy, and in-folding of the ligamentum flavum. The modified Japanese Orthopedic Association (mJOA) score is a commonly used metric to quantify the severity of cervical myelopathy. The mJOA score is comprised of six domains that assess the impact of spinal cord compression on: 1) Ability to feed oneself, 2) Ability to walk, 3) Loss of feeling or numbness in arms, 4) Loss of feeling or numbness in legs, 5) Loss of feeling or numbness in body and 6) Ability to urinate. Multiple studies have reported on predictors that influence overall improvement in mJOA score; however, no study has assessed the predictors of the mJOA sub-domains after elective surgical management for patients with cervical myelopathy. In the present study, the primary objective was to construct a clinical prediction model for improvement of mJOA sub-domains at 12-months following surgery for DCM. Material and Methods: We conducted a retrospective review of data collected from the Quality Outcomes Database (QOD), a national database containing prospectively collected data. Patients were selected for inclusion in the current study if: 1) one of their predominant indications for cervical surgery was myelopathy or myelopathy was indicated as a spine-associated symptom, and 2) they completed one-year follow-up data. The outcomes of interest were the sub-domains or items of the mJOA at 12-months following surgery. A multivariable proportional odds ordinal regression model was developed for patients with cervical myelopathy. The model included patient demographic, clinical, and surgery covariates, along with baseline sub-domain scores. The model was internally validated using bootstrap resampling to estimate the likely performance on a new sample of patients. Results: The final patient sample included 5,000 patients. Patients had statistically significant improvement from baseline to 12-months post-surgery on all the mJOA sub-domains (p < 0.001). The model identified mJOA baseline sub-domains to be the strongest predictors of 12-month scores, with numbness in legs and ability to walk predicting 5 of the 6 mJOA items. Additional covariates predicting 3 or more items included age, preoperative anxiety/depression, gender, race, employment status, duration of symptoms, smoking status, and radiographic presence of listhesis. Surgical approach, presence of motor deficits, number of surgical levels involved, history of diabetes mellitus, worker’s compensation claim, and patient insurance had no impact on 12-month mJOA scores. The discriminative ability of the model regarding joint probabilities measured by unweighted generalized C-index was 0.753. Conclusion: We developed and validated a clinical prediction model for improvement in mJOA scores at 12-months following surgery for cervical myelopathy. Our results highlight the importance of assessing preoperative numbness, walking ability, and the modifiable variables of anxiety/depression and smoking status. Additional factors to consider when counseling patients preoperatively are age, gender, race, employment status, duration of symptoms, and presence of listhesis. This model has the potential to assist surgeons, patients, and families when considering surgery for cervical myelopathy. Future steps include prospective, external validation of the predictive model to assess reproducibility and clinical utility.
OP19: Contemporary Surgery for Adolescent Deformity
538
A163: A cost-utility analysis of multimodal intraoperative neuromonitoring utilization during adolescent idiopathic scoliosis surgery
Carlos Ortiz-Babilonia 1,2 , Daniel Badin 1 , Micheal Raad 1 , Miguel Cartagena 1,3 , and Amit Jain 1
1 Department of Orthopedic Spine Surgery, John Hopkins University, Baltimore, United States
2 Department of Orthopedic Surgery, University of Puerto Rico Medical Sciences Campus, San Juan, Puerto Rico
3 Department of Orthopedic Surgery, Ponce Health Sciences University, Ponce, Puerto Rico
Study Design: Cost-utility analysis. Objective: This study aimed to evaluate the cost-utility of utilizing multimodal intraoperative neuromonitoring (IONM) during surgery for adolescent idiopathic scoliosis (AIS) correction. Background: There are studies that have shown that IONM may lead to lower incidence of new neurologic deficits (NNDs) after spine surgery by providing the physician an opportunity to intervene intraoperatively. To our knowledge, a cost-benefit analysis evaluating the utilization of this modality in AIS have not been performed. Methods: A decision-analysis model comparing IONM use versus no IONM use was developed for a hypothetical 15-year-old girl with a 50° main thoracic curve requiring surgery. Chance nodes (probabilities) and terminal nodes (costs and quality-adjusted life years (QALYs)) were populated with comprehensive review of the literature. Probabilistic sensitivity analysis was performed with Monte Carlo simulations of 1,000 hypothetical patients. Mean costs, QALYs, and INMB were obtained from this analysis. Deterministic sensitivity analyses were also performed to evaluate the variables which independently accounted for the most uncertainty in our model. Results: Our decision-analysis model revealed that IONM was preferred over no IONM in AIS surgery in 99% of the simulations. The mean cost of IONM utilization was found to be $63,615 (SD = 5,957), while not utilizing IONM resulted in a cost of $65,039 (SD = 5,927). Mean lifetime QALYs were determined to be 22.94 (SD = 2.21) with IONM and 22.93 (SD = 2.21) without IONM. The mean difference in lifetime costs was $1,424 (SD = 755), and the mean difference in lifetime QALYs was 0.01 (SD = 0.01). IONM use was associated with a median incremental net monetary benefit of $1,791 (SD = 899) at a willingness to pay = $50,000/QALY compared to not utilizing IONM. Only variation of the baseline iatrogenic neurologic deficit probability in AIS surgery to a value of 0.2% or less resulted in IONM use being less cost effective than not utilizing IONM. Conclusions: Cost-utility analysis supports the use of IONM during AIS surgery. However, lower risk of neurologic injury significantly decreased the cost-utility of IONM.
605
A164: Prognostic factors regarding the return to daily activities and sports following posterior spinal fusion for adolescent idiopathic scoliosis: a single center experience of 194 cases
Tuna Pehlivanoglu 1 , Bahadir Gokcen 2 , Kursat Kara 1 , Tugay Yagci 1 , O. Nuri Eroglu 1 , and Cagatay Ozturk 1
1 Dept. of Orthopaedic Surgery, Liv Hospital Ulus, Liv Spine Center certified by AOSpine, Istanbul, Turkey
2 Dept. of Orthopaedic Surgery, Liv Hospital Vadi, Liv Spine Center certified by AOSpine, Istanbul, Turkey
Introduction: When to return to contact/non-contact sports and when to have which specific type of athletic activity in adolescent idiopathic scoliosis (AIS) patients after posterior spinal fusion (PSF) is solely dependent on the surgeon’s choice and clinical experience, while no consensus or guidelines exists regarding these aspects, but just recommendations or anectodal reports. The aim of the present study was to assess prognostic factors which might delay the return to sports, while presenting our experiences as a result of a remarkable number of AIS patients who underwent PSF with modern instrumentation. Methods: 194 consecutive AIS patients, who underwent high-density thoracolumbar PSF in a single institution with at least 5 years of follow-up duration were enrolled. They had a mean age at the surgery of 9.2, mean follow-up duration of 78.3 months, mean BMI of 18.7. Patients radiographic-operative data were recorded and they were applied custom made questionnaires regarding the time of return to daily activities and sports, together with the SRS-22 questionnaire. Results: Mean pre-op curve magnitude was reduced from 64.3° to 4.2° (93.5% of correction, p < 0.001) at the latest follow-up. They had average 10.4 levels of bilateral pedicle screw placement. Most common curve distributions according to the Lenke types were as: 1: 101 (52.1%), 6: 38 (19.6%), 3: 27 (13.9%). LIV was L3: 104 (53.6%), L1: 46(23.7%), L2: 29 (14.9%), L4: 15(7.8%). Pre-operative mean total SRS-score was 2.7 improved to 4.8 at the last follow-up (p < 0.001).187 patients (96.4%) were able to return to daily activities and go back to school at the end of the 1st month. 179 (92.2%) patients were able to run or jog, 81 patients (41.7%) were able to swim, and 64 patients (32.9%) were able to bend forward at the end of the 3rd month. 138 patients (71.1%) were able return to contact sports at the end of the 6th month. At the end of 6th month, 92.2% of patients performing non-contact sports and 90.1% of patients performing contract sports were detected to be able to perform with similar pre-operative sportive performance, while 192 patients (98.9%) declared to be at the same activity level as pre-operatively at the end of 1 year. A high BMI (>15), a high pre-op Curve magnitude (>60°), a LIV below L3, a Lenke type > 4 and a pre-op/post-op SRS-22 scores of < 3.2/4.1 were detected as prognostic criteria for the late return to sports and daily activities. Conclusion: As a result of PSF performed with modern instrumentation, almost all of the AIS patients were able to return to the same pre-operative level of activity at the end of the 1st post-operative year, while for more than 90% of patients who perform contact/non-contact sports, the same pre-operative performance was even possible at the end of the 6th post-operative month. The present study concluded, that a high pre-op BMI (>15), a high pre-op Curve magnitude (>60°), a LIV below L3, a Lenke type >4 and a pre-op/post-op SRS-22 scores of < 3.2/4.1 were defined as independent prognostic criteria for the late return to sport and daily activities.
778
A165: Coronal imbalance after selective fusion surgery and its outcome in adolescent idiopathoc scoliosis - A single center retrospective study
Saumyajit Basu 1 and Gowtham Jallipalli 1
1 Department of Spine Surgery, Kothari Medical Center, Kolkata, India
Introduction: Primary goal of scoliosis surgery is to attain a good coronal balance - defined as (C7PL - CSVL within 2 cm), but Coronal decompensation is a common complication in AIS after selective fusion. However, the majority who developed immediately postoperative coronal decompensation experienced improvement and the related factors are not fully understood. Aim and Objective: The aim of this retrospective study was to investigate the prevalence of coronal imbalance in patients with AIS and to explore radiological factors associated with coronal imbalance and its spontaneous correction of after selective spinal fusion surgery. Material and Methods: All patients with AIS who underwent selective fusion from Jan 2009 - Dec 2019 were included. 60 patients underwent selective spinal fusion with 40 patients (group A – Selective Thoracic) and 20 patients (group B – Selective Thoracolumbar/Lumbar). Demographic characteristics, preoperative, immediate postoperative, 3 and 24 months follow up coronal alignment data was obtained. Results: Coronal decompensation seen in 7 patients (17.5%) group A and 5 patients (25%) in group B. In group A the magnitude of lumbar curve and its rigidity was greater in decompensated group (19.5∘ vs. 12.6∘, p = 0.006; 25.5∘ vs. 13.7∘, p < 0.01). In group B coronal decompensation was correlated with less flexible Thoracolumbar/Lumbar curve (49.7% vs 51.2%, p = 0.041), greater T10-L2 kyphosis (9.8 vs 7.8 degree, p = 0.031). The Lower Instrumented Vertebra (LIV) tilt was more in the decompensation group at early postoperative period (7.9 vs 3.4, p = 0.007). This decompensation was spontaneously corrected because of distal adding-on phenomena. Conclusion: Coronal imbalance is common in early postoperative period in selective fusion and is observed more frequently in stiff compensatory curves and with thoracolumbar kyphosis- however most of them correct spontaneously.
186
A166: Rocket incision: a modified surgical approach for posterior correction of neuromuscular scoliosis. A case series with technical notes
Elie Najjar 1 , Masood Shafafy 1 , Naveen Pandita 1 , and Mohamed Hassanin 2
1 Queen's Medical Center, The Center for Spine Studies and Surgery, Nottingham, United Kingdom
2 Nottingham University Hospital, United Kingdom
Introduction: Neuromuscular Scoliosis (NMS) surgeries often involve distal extension of incision to the sacrum for spino-pelvic fixation. Such incisions in what already is an atrophic and fibrous tissue carry a high risk of infection by faecal contamination due to proximity to perineal area in patients with minimal or no bowel control. The Rocket incision; a semilunar musculocutaneous flap on either side of the midline incision is based on the Superior Gluteal Arteries and Lumbar perforators allowing for better implant coverage with vascularized tissue and keeping the distal end away from the perianal area thus decreasing the rates of wound complications. It additionally aids in pelvic obliquity correction by releasing the Iliolumbar fascia from the iliac crest in the concavity of the curve. Material and Methods: A cohort of 15 NMS patients (10 males and 5 females, average age 11.4 years (5-19)) Underwent this approach for correction of their progressive spinal deformity. 65% of the patients had Cerebral Palsy, 27% Muscular Dystrophies and 13% were Syndromic. 10 patients underwent standard posterior instrumentation from T2 to pelvis, 4 patients underwent MAGEC rods and 1 patient Luque’ trolley for Early Onset Scoliosis. A deep gravity drain was inserted in all cases and the wounds were closed using non-absorbable sutures for the fascia, and absorbable for the subcutaneous tissue and skin which was finally covered with suction dressing. Routine 3 doses of postoperative antibiotic were give. Data related to wound complications including infection and dehiscence and radiographic data regarding correction of the deformity and pelvic obliquity was collected. Results: The mean surgical time was 452 (320-720) minutes with average blood loss of 851 mls (250-1800). Average length of stay was 12.6 (7-35) days. The Wound was dry in all the patients after 14 days and the dressings were removed. At the latest follow up of 24 (4-43) months, no patient had had any complication related to the surgical wound, nor any metal work prominence. One patient developed late post-operative deep infection secondary to a dental abscess 17 months after her initial surgery. She underwent removal of metal work through the same approach. The wound healed for the second time with no complication. Pelvic obliquity had improved from 20.5 (95CI:2.03, 4.63) degrees to 3.3 (95CI: 14.8, 26.1) degrees with 86 % correction (p < 0.001), and main deformity had improved form 81.5 degrees (95CI:, 72.5,90.5) degrees to 21 degrees (95CI: 15, 27.1 ) degrees with 74% correction (p < 0.001). Conclusion: This new surgical approach in this cohort of patients appears to be safe and effective in posterior correction of neuromuscular scoliosis.
602
A167: Only posterior hemivertebrectomy with short-segment transpedicular fixation for congenital scoliosis: at least 10-years' results of 37 patients
Tuna Pehlivanoglu 1 , Bahadir Gokcen 2 , Kursat Kara 1 , Tugrul Ergun 3 , Gorkem Muratoglu 3 , and Cagatay Ozturk 1
1 Dept. of Orthopaedic Surgery, Liv Hospital Ulus, Liv Spine Center certified by AOSpine, Istanbul, Turkey
2 Dept. of Orthopaedic Surgery, Liv Hospital Vadi, Liv Spine Center certified by AOSpine, Istanbul, Turkey
3 Dept. of Orthopaedic Surgery, Istinye Uni. Liv Hospital, Liv Spine Center certified by AOSpine, Istanbul, Turkey
Introduction: The ideal treatment of congenital scoliosis caused by hemivertebra is challenging. Although mainly short-term studies regarding posterior hemivertebrectomy and transpedicular fixation reported promising results, long term data must be provided to assess the efficacy and safety of this method on growing spine. The aim of the present study was to report the minimum 10 years’ radiographic, clinical and functional results of hemivertebrectomy and bisegmental transpedicular fixation. Methods: Consecutive patients, who underwent posterior hemivertebrectomy combined with short-segment transpedicular fixation (PHSSTPF) for the management of congenital scoliosis resulting from fully segmented, non-incarcerated hemivertebra, with an age of < 10 (at the time of surgery) and a follow-up duration of at least 10 years, without any history of previous spinal surgery or intraspinal anomaly were enrolled and retrospectively analyzed regarding the radiographic, clinical and functional outcomes Results: 37 patients (22F,15M) with a mean age of 6.9 (5-12) and mean follow-up duration of 128.4 months (120-132) were enrolled. They had a mean total duration of operations and loss of blood of 162.7 mins (121-143) - 211 mL (110-350), respectively. All patients underwent one level hemivertebra resection combined with transpedicular fixation, while 26 patients (70.2%) underwent bisegmental fusion. Total main coronal curve was 48.1° pre-operatively, 6.3° post-operatively and 4.2° at the final follow-up (p < 0.001 for all) with an average rate of correction of 88.1%. Segmental kyphosis was 23.7° pre-operatively, 4.8° post-operatively and 3.6° at the final follow-up (p < 0.001 for all) with an average rate of correction of 82.2%. Cranial-Caudal compensatory curves were 14.2°-15.4° pre-operatively, 4.1°-4.7° post-operatively and 3.8°-3.3° at the final follow-up (p < 0.001 for all) with an average rate of correction of 72.2%-.73.9%. Pre-operative trunk shift of 23.4mm was improved to 3.4mm post-operatively and to 1.2mm at the latest follow-up (p < 0.001 for all). Pre-operative mean total SRS-22 score of 2.7 was improved to 4.3 (p = 0.003) at the final follow-up visit. No crankshaft or implant related complications were noted during the entire follow-up. Conclusion: Posterior hemivertebrectomy combined with short-segment transpedicular fixation (PHSSTPF) was detected to provide excellent correction of major scoliotic curve and segmental kyphosis, successful restoration of the spinal balance, preservation of the growth of the spine together with significantly improved functional outcomes at the end of the minimum 10 years. Hereby, the present study underlined the safety and efficacy of PHSSTPF for the excellent management of congenital scoliosis in the long term.
1455
A168: Clinical, radiological and HRQOL outcomes after selective thoracic fusion with minimum 20 years follow up: assessment of the degenerative changes of unfused lumbar spine with MRI study
Azmi Hamzaoglu 1 , Hamisi Mraja 1 , Tunay Sanli 1 , Halil Gok 1 , Onur Levent Ulusoy 1 , Ayhan Mutlu 1 , Celaleddin Bildik 1 , Selhan Karadereler 1 , and Meric Enercan 1
1 Scoliosis-Spine Center Istanbul, Istanbul, Turkey
Introduction: The aim of this study is to evaluate the clinical, radiological outcomes and long-term behavior of the lumbar curve in AIS patients treated with selective thoracic fusion and assess the disc degeneration (DD) and facet joint degeneration (FJD) of the unfused lumbar spine with MRI at the end of minimum 20 years follow up. Methods: AIS patients treated with selective thoracic fusion and having minimum 20 years follow up were included. Preoperative, postoperative, and final follow up radiographs were reviewed. All patients had lumbar MRIs at the final follow up in order to evaluate DD and FJD of the unfused lumbar spine. Clinical evaluation was done by using SRS22r and Numerical Rating Scale (NRS). Results: 21 AIS (21 F) patients with mean age 36.2 (32-45) years and mean follow up was 22.8 (20-30) years. MT was corrected from 53.8° to 16° (70.3% correction rate), spontaneous lumbar curve correction rate was 57.9% (38° to 16°). Coronal, sagittal parameters, residual lumbar curve and lowest instrumented vertebra (LIV) angulation were stable over time. Median grade of lumbar DD was 2 (1-4) and lumbar FJDs was 2 (1-4). Residual lumbar curve more than 20° (area = 0.734) was correlated with DD of unfused segments (r = 0.62; p < 0.01), decrease in total SRS22r score (U = 11.0; p < 0.05) and SRS pain domain (U = 0.0; p < 0.05). LIV angle more than 10° (area = 0.703) was correlated with FJD at LIV+1 level (r = 0.477; p < 0.05). Mean SRS22r sub-total score was 4.42 and NRS was 1.4 at final follow up. Mean patient satisfaction was 4.72 at final follow up. Conclusion: Selective thoracic fusion provides satisfactory clinical and radiological outcomes at minimum 20 years follow up. Spinal balance and spontaneous lumbar curve correction were well maintained over time. The degree of disc and facet joint degeneration in unfused segments was higher in patients who had residual lumbar curve > 20° and LIV angle > 10° compared to those with residual lumbar curve < 20° and LIV angle < 10°. Patient satisfaction (4.72/5) was high at the end of 20 years follow-up.
622
A169: Restoration of spinopelvic alignment after reduction of high-grade spondylolisthesis: myth or reality? A systematic review of the literature and meta-analysis
Giovanni Viroli 1 , Marco Ialuna 1 , Marco Manzetti 1 , Francesca Barile 1 , matteo traversari 1 , fabio vita 1 , alberto rinaldi 1 , giuseppe d'antonio 1 , Alberto Ruffilli 1 , and Cesare Faldini 1
1 1 st Orthopaedic and Traumatologic Clinic, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: High-grade spondylolisthesis (HGS) is defined as an anterior translation of a vertebra, over the underlying vertebra, greater than 50% according to the Meyerding Classification. The slippage of the vertebra, in HGS, is often associated with segmental kyphotic deformity of the involved level, which is almost invariably the L5-S1 level. This combination of translation and regional kyphosis, leads to secondary compensatory mechanisms in the adjacent spinal regions: increase in lumbar lordosis (LL), reduction of thoracic kyphosis (TK) and decrease of cervical lordosis (CL). Moreover, a retroversion of the pelvis, with an increase in pelvic tilt (PT) and a decrease in sacral slope (SS), is often seen in order to keep a globally balanced spine. While it is clear that performing a reduction surgery for spondylolisthesis leads to a partial or complete correction of translation and regional kyphosis, the effect of surgery on the sagittal spinal alignment and particularly on pelvic orientation is still uncertain. By a systematic review of literature and meta-analysis, the aim of the presented study is to assess if the reduction of HGS, through the correction of lumbosacral kyphosis, leads to a decrease in the sagittal spinopelvic compensatory mechanisms. Material and Methods: A systematic search of electronic databases was conducted. Inclusion criteria were: diagnosis of HGS (Meyerding > II, Slip% > 50%), partial or complete reduction surgery (with significant decrease in Slip%), report of spinopelvic parameters (Pelvic Incidence, Pelvic Tilt or Sacral Slope). Clinical and radiographic outcomes were extracted and summarized. Meta-analyses were performed to estimate the differences between pre- and post-operative spinopelvic alignment measures. A random effect model was applied as a conservative approach to account for different sources of variation among studies. p < 0.05 was considered significant. Results: 16 studies were included. The mean preoperative Slip % ranged between 60 and 94%, while the mean postoperative Slip % ranged between 11 and 65%. The mean slip angle ranged from 13.9° to 32° preoperatively and from 2.2° to 12.3° after surgery. PT showed a statistically significant decrease of -1.9024 (95% CI: -3.2602 to -0.5445; p = 0.006), while SS showed a significant increase of 4.7390 (95% CI: 2.5253 to 6.9527; p < 0.0001). Conversely, both LL and TK showed non-significant changes, -4.9148° (95% CI: -11.0731° to 1.2436°; p = 0.1178) and 6.9825° (95% CI: -1.5736° to 15.5385°; p = 0.1097) respectively. VAS significantly decreased by -3.3077 (95% CI: -5.8826 to -0.7328; p = 0.0118). Conclusion: The meta-analysis showed mild, yet statistically significant, decrease of PT and increase in SS after HGS reduction. Although statistically significant, the clinical significance of such mild improvements in sagittal spinopelvic alignment remains questionable. Conversely, non-statically significant decrease in LL and increase in TK occurred.
933
A170: Intermittent pedicle screw constructs provide better kyphosis restoration in Lenke type 1 curves
Alim Can Baymurat 1 , Aliekber Yapar 2 , Omer Kilicaslan 2 , Mehmet Tokgoz 1 , Huseyin Selcuk 2 , Semih Yas 1 , and Alpaslan Senkoylu 1
1 Department of Orthopedics and Traumatology, Faculty of Medicine, Gazi University, Ankara, Turkey
2 Department of Orthopedics and Traumatology, Health Sciences University, Antalya Education and Research Hospital Antalya, Turkey
Introduction: All pedicle screw constructs are the gold standard for adolescent idiopathic scoliosis (AIS) surgery. However, there is still no consensus on the optimum pedicle screw density required for the desired thoracic kyphosis restoration after scoliosis surgery. The aim of this study was to evaluate the clinical outcomes and the thoracic kyphosis restoration of the Lenke type 1 and 2 AIS curves corrected with pedicle screws inserted consecutively or intermittently. Hypothesis: Intermittent pedicle screw constructs for the treatment of Lenke type 1 and 2 AIS curves provide better thoracic kyphosis restoration compared to consecutive pedicle screw constructs. Study Design: Retrospective case-control study with a minimum of 2 years of follow-up. Material and Methods: The data of 106 patients who underwent corrective surgery for Lenke type 1 and 2 AIS between January 2005 and December 2019 were reviewed. Two groups were constituted according to the pedicle screw density: intermittent pedicle screw constructs (IPSC) (n = 52 patients) and consecutive pedicle screw construct (CPSC) (n = 54 patients) groups. The preoperative and minimum 24-month follow-up radiographs and SRS-22 scores were evaluated. The Cobb angle of the main and accompanying curves in the coronal plane, cervical lordosis (C2-C7), and thoracic kyphosis (T5-T12) in the sagittal plane were measured and compared. Results: The mean follow-up period for the IPSC and CPSC groups were 72.3 ± 37.2 and 62.9 ± 28.8 months, consequently. In the SRS-22 questionnaire, there was no significant difference between the two groups in terms of self-image/appearance domain scores (p = 0.466), but better results were obtained in the IPSC group in terms of treatment satisfaction domain scores (p = 0.010) and better thoracic kyphosis restoration was achieved in IPSC group radiologically for Lenke type 1 curves with -81.4 ± 81.4% in the IPSC group and 6.8 ± 83.8% in the CPSC group (p < 0.001). Conclusion: It was considered that better thoracic kyphosis restoration could be achieved with the less lordotic effect of IPSC in Lenke type 1 curves. Although the current situation had a significant impact on radiological outcomes, its effect on SRS-22 scores was limited.
564
A171: Anterior release & posterior spinal fusion vs. posterior-only fusion in ais patients with large magnitude thoracic curves
Anabelle Permutt 1 , Zacharia Silk 2 , Roozbeh Shafafy 2 , Chadi Ali 2 , MH Hilali Noordeen 2 , Julian Leong 2 , Sean Molloy 2 , Jan Lehovsky 2 , and Alexander Gibson 2
1 Medical School, University College London, London, United Kingdom
2 Spine, Royal National Orthopaedic Hospital, London, United Kingdom
Introduction: The treatment of large magnitude thoracic curves in patients with adolescent idiopathic scoliosis (AIS) remains a contentious source of debate amongst the surgical community. Whilst the literature demonstrates a shift towards posterior-only fusion (PF) techniques, the utilisation of an anterior release in combination with posterior fusion (ARPF) may still have an important role. Material and Methods: We present a retrospective cohort study comparing the clinical and radiological outcomes of PF vs. ARPF performed at a high-volume spinal deformity unit. The study groups comprise patients with AIS (10 – 18 years), a major thoracic curve ≥ 700 (Lenke 1 - 4) and a minimum of 2 years follow-up. Results: In total, 89 (PF = 51; ARPF = 38) patients were enrolled. Pre-operative baseline characteristics were similar across all parameters except age and skeletal maturity, where those undergoing ARPF were found to be younger (13.7 vs 14.8, p = 0.001) and more likely to be Risser 0 – 2 (60.5% vs 37.3%). Although baseline Cobb was statistically no different (p = 0.0634), those undergoing ARPF were stiffer (p = 0.0257), had less flexibility (p = 0.0408) and achieved a significantly higher correction index of 248.2% vs 168.1% (p = 0.0024) at final follow-up. Expectedly, Op-time, LOS and EBL were higher in ARPF, yet the rate of neuromonitoring alerts was greater in PF. Conclusion: Whilst ARPF offers a significantly greater opportunity for curve correction, its use may be limited to those with demonstrably stiffer curves and an ongoing risk of crankshaft phenomena due to skeletal immaturity.
OP20: Complexities in Primary Spine Tumors
1434
A172: Baseline metabolic aberrational status is significantly associated with increased comorbidity incidence and 2-year postoperative poorer disability and physical quality outcomes in primary intradural-extramedullary spinal cord tumor patients: prospective, propensity-matched outcomes
Nicholas Van Halm-Lutterodt 1,2,3 , Krishna Mandalia 4 , Nicholas Storlie 5 , Chenlong Yang 6 , Ziyang Ye 3,7 , Mohamed Mesregah 8 , Josh Gonzalez 3 , Andrew Mecum 9 , Wei-Hsun Huang 2 , Wei-Cheng Chen 2 , Roberta Kungulli 10 , Mercy Bartels-Mensah 11 , Wenju Jiang 2 , Yu Wang 2 , Sunny Kim 3 , and Yulun Xu 2
1 Department of Professional Studies and Public Health, Brown University, Providence, United States
2 Department of Neurosurgery, Beijing Tiantan Hospital, China
3 Department of Orthopedic and Neurosurgery, Inspired Spine Health, Burnsville, United States
4 Department of Orthopaedic Surgery, Tufts University School of Medicine, Boston, United States
5 School of Medicine, Creighton University School of Medicine, Omaha, United States
6 Department of Orthopedics and Neurosurgery, Peking University, China
7 Department of Data Science and Analytics, University of Chicago, United States
8 Department of Orthopaedic Surgery, Menoufia University, Shibin El Kom, Egypt
9 School of Medicine, University of Colorado Anschutz School of Medicine, Aurora, United States
10 School of Medicine, Capital Medical University, Beijing, China
11 Debrecen School of Medicine, University of Debrecen, Hungary
Background: Studies published in the spine literature have documented of how abnormal body mass index (BMI) impact spine patient outcomes. Recent cardio-metabolic studies indicate that BMI does not always significantly correlate with metabolic health status since some patients with abnormal BMI status may be metabolically healthy and vice-versa. Identifying the insidious entities in serum metabolic panel that dictate abnormal metabolic health status in spine patients would be a great fundamental step to addressing the negative impacts of metabolomics in our spine patient population. Materials and Methods: Following Institutional Review Board (IRB) of Beijing Tiantan Hospital approval, we prospectively obtained patient data from January 2017 through December 2017. The study design included: adult patients who were diagnosed with primary IDEM-SCTs and underwent tumor resection surgery as primary treatment. The IDEM-SCT patients who had ≥ 2 items of the following four metabolic criteria were considered metabolically unhealthy (MU_IDEM-SCT) while those with < 2 of the criteria were considered metabolically healthy (MH_IDEM-SCT): (i) high fasting blood glucose level (≥ 5.6 mmol/L or ≥ 100.8 mg/dL) or on diabetic medications (oral or intravenous), (ii) low high density lipoprotein cholesterol (HDL-c), (< 1.04 mmol/L or < 40.56 mg/dL for male patients and (< 1.29 mmol/L or <50.31 mg/dL for female patients), (iii) elevated systolic blood pressure (≥ 130 mmHg) or diastolic blood pressure (≥ 85 mmHg) or on anti-hypertensive drugs and (iv) high serum triglyceride (TG) level (≥ 1.7 mmol/L or ≥ 150.44 mg/dL) or on lipid-lowering drugs. Baseline metabolic profile and neurological, and 2-year postoperative neurological, and patient-reported outcomes (PROs) including: [Chinese Food Frequency Questionnaire (FFQ), SF-36, NDI or ODI and VAS scores] were analyzed by t-tests following Python-based ‘age and sex’ propensity score matching (PSM). Significance was set at p < 0.05. Results: Overall, 88 patients with IDEM-SCTs were matched in this study, [MH_IDEM-SCT]; n = 44 (50.0%) and [MU_IDEM-SCT]; n = 44 (50.0%) patients, respectively. The average body mass index (BMI) of patients in [MH_IDEM-SCT] and [MU_IDEM-SCT] groups were (25.17 ± 4.29) and (25.33 ± 2.58) kg/m2, respectively, (p > 0.05). At baseline, significant increase in the incidence of comorbid status [27.27% in MH group vs 56.82% in MU group] and average serum glucose and triglyceride (TG) levels, and cholesterol ratio (CR), (p < 0.01), as well as significant decrease in average high-density lipoprotein cholesterol (HDL-c) level, (p = 0.029) in the [MU_IDEM-SCT] patients were observed. At 2-year postoperative, the average Physical Function (PF), Role Physical (RP), Bodily Pain (BP), and Physical Component Summary (PCS) components of SF-36, as well as NDI or ODI significantly demonstrated inferior score outcomes in the [MU_IDEM-SCT] group compared to the [MH_IDEM-SCT] patient group, (p < 0.05). Conclusions: These findings confirm that an unhealthy metabolic status was not specific to BMI-only but also associated with higher baseline comorbid status in the [MU_IDEM-SCT] patient group. Further, these patients demonstrated inferior physical quality and increased disability outcomes at 2-year postoperative. It is pertinent to identify these patients within the spine population, as they may benefit more from well-structured nonoperative treatment modalities and ancillary health programs following spine surgery.
58
A173: Risk factors for sacral fracture following en bloc chordoma resection
Anthony Mikula 1 , Zachary Pennington 1 , Nikita Lakomkin 1 , Marc Prablek 2 , Behrang Amini 3 , Mohammed Karim 4 , Shalin Patel 5 , Daniel Lubelski 6 , Daniel Sciubba 7 , Christopher Alvarez-Breckenridge 8 , Rob North 8 , Claudio Tatsui 8 , Mohamad Bydon 1 , Jeremy Fogelson 1 , Benjamin D. Elder 1 , William Krauss 1 , Justin Bird 5 , Peter Rose 4 , Michelle Clarke 1 , and Laurence Rhines 8
1 Neurological Surgery
2 Neurological Surgery, Baylor College of Medicine, Houston, United States
3 Radiology
4 Orthopedics, Mayo Clinic, Rochester, United States
5 Orthopedics
6 Neurological Surgery, Johns Hopkins, Baltimore, United States
7 Neurological Surgery, Northwell, New York, United States
8 Neurological Surgery, MD Anderson Cancer Center, Houston, United States
Introduction: Sacral chordomas are rare malignant bone tumors, and en bloc resection has provided the highest rates of disease-free and overall survival. For cases of mid to low sacral chordomas, only partial sacral amputation may be required, and spinopelvic stability can be maintained without instrumentation. However, some of these patients may suffer sacral insufficiency fractures. The purpose of this study was to analyze risk factors for sacral fracture following non-instrumented partial sacral amputation for en bloc chordoma resection. Material and Methods: A multicenter retrospective chart review identified patients who underwent non-instrumented partial sacral amputation for en bloc chordoma resection with pre and post operative imaging. Hounsfield units (HU) were measured in the S1 level. Variables collected included basic demographics, patient comorbidities, surgical approach, sacral amputation level, pre-operative radiographic details, neoadjuvant and adjuvant radiation therapy, and post operative sacral fracture data. Results: One hundred and one patients (60 men, 41 women) were included with an average age of 69, BMI of 29 kg/m2, and follow-up of 60 months. Sacral amputation level was partial S1 (2%), S2 (37%), S3 (44%), S4 (9%), and S5 (9%). Patients had a posterior only approach (77%) or a combined anterior/posterior approach (23%) with ten patients (10%) having partial sacroiliac (SI) joint resection. Twenty-seven patients (27%) suffered a post operative sacral fracture, all occurring between one and seven months after the index surgery. Multivariable logistic regression analysis demonstrated S1-S2 sacral amputation (p = 0.001), combined anterior/posterior approach (p = 0.0064), and low superior S1 HU (p = 0.027) to be independent predictors of sacral fracture. The fracture rate for patients with superior S1 HU < 225, 225-300, and > 300 was 38%, 15%, and 9%, respectively. An optimal superior S1 HU cutoff of 300 was found to maximize sensitivity (89%) and specificity (42%) in predicting post-amputation sacral fracture. In addition, the fracture rate for patients who underwent partial SI joint resection was 100%. Conclusion: Patients with S1-S2 partial sacral amputations, a combined anterior/posterior surgical approach, low superior S1 HU, and partial SI joint resection are at higher risk for post-operative sacral fracture following en bloc chordoma resection and should be considered for spinopelvic instrumentation at the index procedure.
580
A174: Neurologic compromise and the need for re-treatments among multiple myeloma patients with high-grade spinal cord compression treated with radiotherapy or surgery
Hester Zijlstra 1,2,3,4 , Robert-Jan Pierik 1 , Alexander Crawford 1 , Brandon Striano 1 , Nienke Wolterbeek 2 , Diyar Delawi 2 , Diederik Kempen 3 , Jorrit-Jan Verlaan 4 , and Joseph Schwab 1
1 Department of Orthopedic Surgery, Massachusetts General Hospital/Harvard Medical School, Boston, United States
2 Department of Orthopedic Surgery, St. Antonius Hospital, Utrecht, The Netherlands
3 Department of Orthopedic Surgery, OLVG Amsterdam, Amsterdam, The Netherlands
4 Department of Orthopedic Surgery, UMC Utrecht, Utrecht, The Netherlands
Introduction: Multiple myeloma (MM) is a malignant plasma cell neoplasm and is the second most diagnosed hematological malignancy in developed countries. Up to 30% of MM patients are expected to experience Spinal Cord Compression (SCC) during the course of their disease. To prevent irreversible neurological damage due to continuous SCC, timely diagnosis and treatment are important. While according to the neurologic, oncologic, mechanical, and systemic (NOMS) framework, high-grade epidural spinal cord compression (ESCC) is not an indication for surgical decompression in MM patients without spinal instability, it is often perceived that way. With this study, we aim to investigate the neurological outcomes and frequency of re-treatments for high grade ESCC patients undergoing radiotherapy (RT) and compare that with those treated with surgical interventions. Material and Methods: This retrospective cohort study was approved by our institutional review board. Baseline clinical parameters and outcome measures were extracted with manual chart review. Assessment of neurological status was done using the American Spinal Injury Association (ASIA) impairment scale. ESCC was rated by three independent orthopedic residents using the Bilsky scale. Survival analysis was performed using Kaplan-Meier method and propensity score matching was done to control for confounding by indications. Results: Two-hundred-fifty-nine consecutive MM patients with high grade ESCC (grades 2 or 3) were included in this study, 154 (59.5%) receiving RT alone and 105 (40.5%) received surgery (with or without RT). After radiotherapy, 82 patients (53.2%) achieved full (ASIA E) recovery from neurologic function. Of all surgically treated patients, 67 (63.8%) achieved full neurologic function. ASIA E or improvement of motor function by at least 1 ASIA score at the end of follow-up occurred significantly more after surgery (63.0% vs. 78.1%, p = .009). Especially in the first 3-6 months, radiotherapy patients suffered significantly more from neurological deterioration and less patients improved neurologically. Thirty-six (23.4%) patients needed secondary treatment (surgery or radiotherapy) after initial radiotherapy and 22 (20.9%) surgically treated patients needed a retreatment. Overall survival was significantly better in the surgery group (median survival time radiotherapy group: 13.3 months, surgery group: 55.2 months, p < .001). After propensity score matching on possible surgical indications (age, ECOG, ASIA score, SINS and ESCC grade), this difference remained significant (p = .03). The median time from initial MM diagnosis to the intervention for ESCC was 345 days [IQR 10 - 1509] for patients getting radiotherapy and 7 days [IQR 0 - 128] for surgery. Conclusion: This study evaluated the differences in neurologic outcomes, the rate of retreatment and survival between radiotherapy and surgery. Using a strict evaluation, we reported favorable results for surgical management of myeloma related ESCC. Improvement of motor function occurred significantly more often after surgery, retreatment rate seems higher after initial radiotherapy and propensity score matched survival analysis showed significantly better survival after surgery versus radiotherapy. However, since there was an obvious selection bias, the results need to be carefully interpreted. Yet, the results of this study indicate that surgery could have certain benefits and could be considered as an appropriate treatment option more often.
1182
A175: Does the application of neoadjuvant high energy particle therapy change the local control in intentional Enneking inappropriate surgical treatment of Osteogenic sarcoma (OGS) of the spine?
Gisberto Evangelisti 1 , Luigi Falzetti 1 , Giovanni Barbanti Bròdano 1 , and Alessandro Gasbarrini 1
1 Department of Spine Surgery, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: OGS is a rare malignant bone tumor. Wide margins resection associated with chemotherapy is the gold standard of treatment. Advances in radiotherapy have provided another treatment consideration to complement surgery. Material and Methods: We retrospectively reviewed a series of 23 patients affected by primary OGS of the spine treated at tertiary referral hospital between 2009 and 2020. The clinical, pathologic, and radiographic data were reviewed in all cases. All cases were classified according to the classification proposed by Enneking and also by the Weinstein, Boriani, Biagini (WBB) classification. Results: 23 patients were initially included in the present study. Three patients were excluded because they were initially surgically treated at other institutions or because affected by low grade OGS. The median follow-up was 15.7 months (range 4-95) or until death. Thirteen of twenty patients were dead at final follow up (65%). The disease specific one- and five- year survival rate for the global cohort were 68.4% and 36.8% respectively. Four over 20 patients received high energy particles as adjuvant therapy after aggressive, extracapsular intralesional excision. In this group of patients, the disease specific survival rate was 100% at one year and 100% at five years. Four over 20 patients received adjuvant photons therapy. In this group of patients, the survival rate was 25% at one year and 0% at five years. Eight patients underwent a planned en-bloc spondylectomy. Five of the 8 patients who underwent en-bloc resection had a negative margin. The median survival for patient who underwent planned en-bloc resection was 26.4 months. The median overall survival for the five patients who underwent en-bloc resection with confirmed negative margins was 15.8 months. The one-year survival was 80% while the five-year survival was 40%. Twelve patients underwent planned intralesional resections. The median survival for all patient who underwent planned intralesional gross total resection was 14.3 months. Four out of this 12 patients received adjuvant high energy particle therapy, the median disease-specific survival for this subgroup of patients was 25.7 months. The other 8 patients had a median disease-specific overall survival of 8.6 months. Patients treated with intralesional gross total resection and particle therapy had a significant higher disease-specific survival (p = 0.029). Conclusion: Wide or marginal margins resection coupled with modern chemotherapy protocols is the gold standard approach to OGS.. From a technical point of view an en-bloc excision in terms of margin-free spondylectomy can be performed when the tumor extends to only one pedicle, i.e., it is centrally located and confined only to zone 4-8 or 5-9 according to the WBB system. However, a considerable number of cases of OGS of the spine fall in the group of planned inappropriate resection due to the extension of the tumor. This is the group of patients which mostly benefits of the advent of high energy particle radiotherapy. The concept of “separation surgery” is changing the surgical paradigms also for the treatment of primary tumors of the spine.
1123
A176: Median labiomandibular glossotomy approach for craniocervical pathologies and multilevel spine reconstruction: options
Jackson Daniel 1 , Luis Eduardo Carelli Texeira da Silva 2 , Alderico Girão Campos de Barros 2 , and Renato Tavares 2
1 Neurosurgery, Hospital Of Federal Universty of Piaui, Teresina / Piaui, Brazil
2 Orthopedics and Spine Surgery, Instituto Nacional de Traumatologia e Ortopedia - INTO, Rio de Janeiro, Brazil
Introduction: Exposure of the clivus and upper cervical spine should ideally provide an adequate surgical field in which the surgeon can safely decompress and stabilize the craniovertebral junction (CVJ). We present a series of 4 cases with narrative review of the literature in which the Labiomandibular approach with Medium Glossotomy was used for the treatment of pathologies of CVJ in order to expose the importance and indications of such access. Material and Methods: We performed a retrospective analysis of patients underwent to a MLMG for several pathologies. The group comprised 4 patients (2 men, 2 women). 5 approaches were accomplished (1 revision surgery). Results: The approach was suitable for all cases, clivus was achieved when necessary. Distally C4 was exposed obtained a satisfactory osteosynthesis. Laterally we had a good view of the tumor and vertebral artery control. As complications we had superficial wound infection, easily healed, a tardy pharyngeal wound dehiscence and pseudoartrosis, all in the same patient. There are 3 main anterior surgical techniques for managing lesions of the clivus, foramen magnum or upper cervical vertebrae. We choose the Median Labiomadibular Glossotomy (MLMG) as a primary option which provided us direct view of the clivus, C3 – C4 caudally and a wider surgical field. The main advantages of the MLMG technique include direct access to spinal pathology, avascular plane through the median pharyngeal raphe and a wider surgical field in both transverse and sagittal dimensions. Conclusion: This approach provides excellent exposure of the craniocervical junction and upper cervical spine.
1119
A177: Racial disparities in breast cancer patients with spinal metastases: an analysis of 1,072 patients over a decade
Alyssa Mixon 1 , William Huffman 2 , Takshi Hirase 3 , Rex Marco 3 , Francesca Taraballi 4 , and Comron Saifi 3
1 Physical Medicine and Rehabilitation, University of Virginia, Charlottesville, United States
2 Orthopaedic Surgery, University of Pennsylvania,Philadelphia, United States
3 Spine Surgery
4 Orthopedic Surgery and Sports Medicine, Houston Methodist, Houston, United States
Introduction: Metastatic breast cancer to the spine has become a progressively common diagnosis over the last two decades within the United States, largely due to the aging population as well as the increasingly prolonged survival after initial diagnosis of primary breast cancer. Recent studies have found increasingly favorable prognosis for patients undergoing surgery for metastatic breast cancer to the spine and is attributed to evolving adjuvant therapies and surgical techniques. However, recent literature demonstrates significant racial disparities associated with the proper diagnosis and treatment of breast cancer. For instance, black women have significantly higher mortality rates from breast cancer compared with non-Hispanic white women and has been largely attributed to substantial delays in diagnosis and treatment. The objective of this study was to evaluate racial disparities among women with metastatic breast cancer to the spine undergoing spine surgery. Materials and Methods: A retrospective cohort study was performed using data from the Surveillance Epidemiology and End Results (SEER)-Medicare database to evaluate racial disparities in the surgical quality of care among patients with spinal metastasis between 2007 and 2016. We describe this study in accordance with the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines. The study protocol was approved through the Institutional Review Board of the University of Pennsylvania with a waiver for informed consent due to the retrospective nature of the study. Inclusion criteria involved female patients aged 18 years and above with breast cancer metastatic to the spine registered in SEER-Medicare from 2007 to 2016. Outcomes of interest included time from diagnosis until the surgical intervention, complications, the number of ED visits, and mortality within 30 and 90 days after discharge. Process of care measures, including post-operative LOS, readmission rates, emergency department visits, and time to treatment were evaluated. Results: Of the 1,072 patients (mean age 63.6 years), 158 were African American (AA)/black and 914 were non-Hispanic white. AA/black patients had longer LOS (Marginal means [MM], 11 [95% CI, 9.31-12.6] vs 8.57 [95% CI, 7.43-9.71], p = .001), increased readmissions (Odds ratio [OR], 1.43 [95% CI, 0.98-2.11], p = .064), increased ED visits (OR, 1.57 [95% CI, 1.08-2.26], p = .016), higher frailty scores (MM, 1.34 [95% CI, 1.13-1.55] vs 1.91 [95% CI, 1.59-2.23], p < 0.001), and increased complications (respiratory: OR, 1.66 [95% CI, 1.12-2.44], p = .011, renal: OR, 1.65 [95% CI, 1.1-2.45], p = .014). There was no significant difference in surgical intervention rate for spinal metastasis within the first year of diagnosis (21.5% vs 19.5%) (OR, 1.42 [95% CI, 0.882-2.25], p = .141) or in cancer-specific (hazard ratio [HR], 1.09 [95% CI, 0.846-1.39], p = .519) and all-cause mortality (HR, 1.13 [95% CI, 0.912-1.4], p = .266). Conclusion: AA/black women undergoing spine surgery for metastatic breast cancer have higher risk for peri-operative complications, longer LOS, higher readmission rates, and more post-operative ED visits. Continued efforts to address and overcome these disparities are necessary.
1322
A178: The use of carbon fibre instrumentation versus titanium instrumentation in separation surgery with post adjuvant stereotactic ablative radiotherapy for spinal oligometastatic disease
Priyanshu Saha 1 , Kofi Cox 1 , Jemma Keefe 1 , Emily Tsang 1 , Zion Hwang 1 , Bisola Ajayi 2 , Mohamed Abdalla 2 , Varinder Singh Alg 2 , Ursalan Khan 2 , Shahnawaz Haleem 2 , Tesfaladet Kurban 2 , Jason Bernard 2 , Timothy Bishop 2 , Pawan Minhas 2 , and Darren Lui 2
1 St George's University of London, London, United Kingdom
2 Department of Complex Neurosurgery, St George's University Hospitals NHS Foundation Trust, London, United Kingdom
Introduction: Radical treatment for Spinal Oligometastatic Disease (OMD) and Oligo-progression (OPD) was often done with highly morbid Tomita En Bloc Spondylectomy. Now, Stereotactic Ablative Radiosurgery (SABR) provides curative tumour ablation without open surgery, reduced cord toxicity and better pain management. SABR delivered postoperatively to Separation Surgery (SS) has shown to have excellent mortality rates, infection control, maximum local control (MLC) and better pain management. Carbon fibre instrumentation (CFI) offers high heat tolerance, high tensile strength, resistance to corrosion and conductivity. Carbonaceous implants possess high resistance to ionizing radiation and low wear particles like biological tissues, which is better suited for postoperative SABR planning and surveillance imaging. There is reduced rate of infection due to the difficulty organisms have producing a biofilm over carbon fibre as opposed to conventional Titanium Instrumentation (TI). When SABR is contraindicated, other systemic therapy is explored before switching to palliative decompression (PD). Methods: Retrospective review of OMD/OPD cases that underwent separation surgery with post adjuvant SABR for the investigating: tumour histology, OMD type, instrumentation used for SS (CFI versus TI), mortality, local recurrence (LR), pain management, infection, complications, hospital length of stay, ICU length of stay and palliative outcomes in a quaternary level 1 spinal unit. Results: Out of 79 patients that were part of the OMD/OPD pathway, 36 patients underwent separation surgery with/without post adjuvant radiosurgery. 16 patients had SS with CFI and 20 patients had SS with TI. SS with TI± SABR: Overall (n = 20) 30 day mortality - 10% (n = 2; patient 1 and 2 died of SS demotion to PD because of no post-operative SABR), 12 month mortality – 15% (n = 3, patient 3 died of SS demotion to PD because of no post-operative SABR). SS with TI + SABR: 30-day mortality - 0 % 12-month mortality – 0%, 12-month LR – 0%. TI: There was a 4% (n=1) superficial surgical site infection 2 weeks post-surgery (washout debridement and implant retention satisfactory). SS with CFI ± SABR: Overall (n = 16) 30 day mortality - 6% (n = 1; patient 4 died of infection unrelated to surgery), 3 year mortality – 12.5% (patient 5 died of SS demotion to PD because of no post-operative SABR). SS with CFI + SABR: 30-day mortality - 0 % 12-month mortality – 0%, 12-month LR- 0%. CFI: Infection – 0%. Pain in both groups were associated with PD cases only. Conclusions: Separation surgery with post adjuvant SABR regardless of CFI or TI instrumentation for OMD radical treatment has demonstrated excellent outcomes for mortality, local recurrence, infection control, pain relief and overall systemic disease control. When post adjuvant SABR is absent from the hybrid treatment regime, that is when patients have met complications and have been demoted to palliative decompression and neurological symptom management. This highlights the importance of SABR in conjunction to SS. The benefit of using CFI over TI is shown by the overall mortality (CFI: 30 day: 6%,1 year:12.5%; TI:30day:10%, 1 year:15%). Other benefits of carbon are long-term surveillance, better suited for SABR/RT and its similarity to biological tissue making it less susceptible to infection and rejection.
1266
A179: Preoperative hypoalbuminemia is associated with longer length of stay and increased morbidity following posterior thoracolumbar fusion for spine tumor excision
Khaled Taghlabi 1 , Takshi Hirase 2 , Jesus Cruz-Garza 1 , Rex Marco 2 , Amir Faraji 1 , and Comron Saifi 3
1 Department of Neurosurgery
2 epartment of Orthopedics and Sports Medicine
3 Spine Surgery, Houston Methodist Hospital, Houston, United States
Introduction: Preoperative nutritional status is a key component in the care of spine oncology patients. Posterior thoracolumbar fusion for spine tumors is associated with high rates of perioperative complications. Preoperative hypoalbuminemia has been shown to be an important predictor of postoperative complications following elective spine surgeries. Our hypothesis is that preoperative hypoalbuminemia is associated with longer length of stay and higher risk of postoperative complications following posterior thoracolumbar fusion for spine tumor excision. Materials and Methods: A Retrospective analysis of prospectively collected data was conducted using the National Surgical Quality Improvement (NSQIP) database and was queried for all patients treated with posterior thoracolumbar fusion for spine tumor excision between 2010 and 2019. Patients with incomplete records were excluded. Demographics, preoperative albumin levels, operative data, hospital length of stay, 30-day reoperation, 30-day readmission, discharge disposition, and postoperative complications were collected. Logistic regression models were used to examine the relationship between preoperative serum albumin levels and perioperative outcome measures. Results: A total of 352 patients (194M, 158F) were included. The median age was 63 years, median BMI was 27.5 and 19% of patients were smokers. Preoperative hypoalbuminemia was associated with longer LOS (p < 0.001). There was a trend for a higher incidence of perioperative complications (p = 0.06). After multiple logistic regression modeling, for every unit decrease of preoperative serum albumin (g/dL), there was a 2.34 times higher chance of patient extending their length of stay by one week (95% CI: 1.72, 3.18; p < 0.001) and 1.36 times higher chance of incurring any perioperative complication (95% CI: 0.99, 1.88; p = 0.06). There was no significant association between preoperative serum albumin, operative time, intraoperative transfusion, 30-day reoperation, 30-day readmission, or discharge disposition. Conclusion: Preoperative hypoalbuminemia is associated with longer hospital length of stay and a trend for a higher incidence of perioperative complications in patients treated with posterior thoracolumbar fusion for spine tumors. Large multi-center prospective studies are required to further investigate preoperative hypoalbuminemia as a prognostic tool to detect the risk of adverse surgical outcomes.
1011
A180: Tubular retractor assisted transoral approach for irreducible ventral cranio cervical junction compressive pathologies: surgical technique and outcome
Mohd Hisam Muhamad Ariffin 1 and Azmi Baharudin 1
1 Orthopaedics, UKM Medical Centre, Kuala Lumpur, Malaysia
Study Design: Retrospective cohort study. Objective: To investigate the use of tubular retractor to provide access to the craniovertebral junction (CVJ) sparing the soft palate with the aim of reducing complications associated with traditional transoral approach but yet allowing adequate decompression of the CVJ. Methods: Twelve consecutive patients with severe myelopathy (JOA-score less than 11) from ventral CVJ compression were operated between 2014-2020 using tubular retractor assisted transoral decompression. Results: All patients improved neurologically statistically (p = 0.02). There were no posterior pharynx wound infections or rhinolalia. There was one case with incomplete removal of the lateral wall of odontoid and one incidental durotomy. Conclusions: Tubular retractor provide adequate access for decompression of the ventral compression of CVJ. As the tubular retractor pushed away the uvula, soft palate and pillars of the tonsils as it docked on the posterior pharyngeal wall, the traditional complications associated with traditional transoral procedures is completely avoided.
Keywords: Transoral approach, craniovertebral junction, myelopathy, tubular retractors, os odontoideum, odontoidectomy
The key surgical landmarks identified microsurgically were depicted
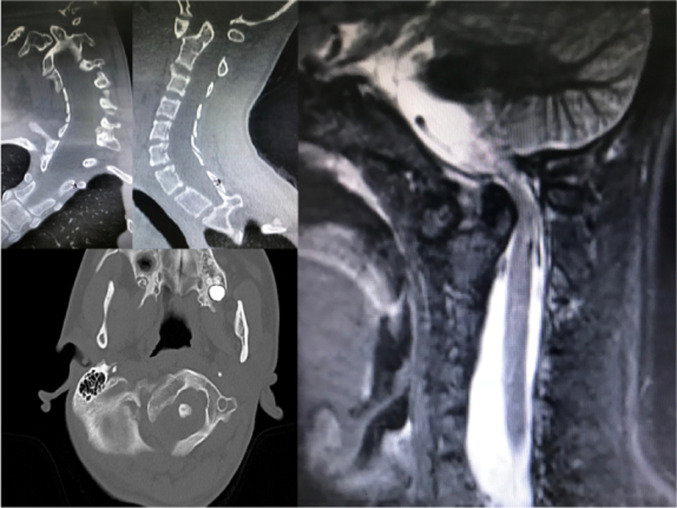
CT of the cervical spine with coronal (a), sagittal (b) and axial (c) reconstruction and MRI of the cervical spine in sagittal T2-weighted (d). CT demonstrates narrowing of the spinal canal of 50% with atlantoaxial dense interval (ADI) of 9mm, borderline basilar invagination where the tip of the odontoid process just touches the McRae line and type III atlantoaxial dislocation. MRI reveals an intramedullary high signal intensity at the region of compression indicating myelomalacia. The spinal canal is severely narrowed that the normal CSF anterior and posterior to the spinal cord is compromised.
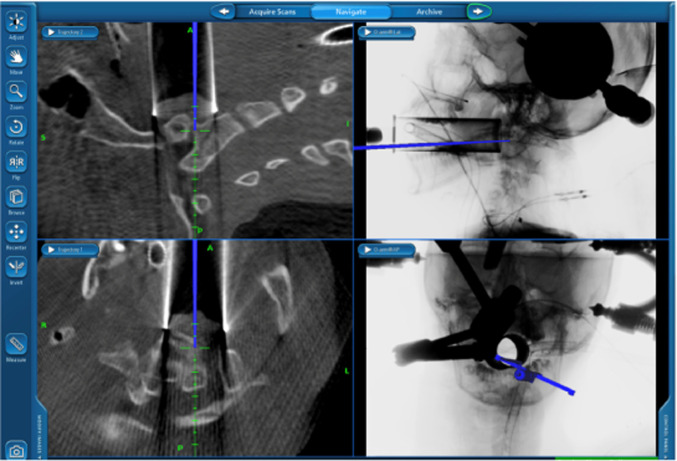
To identify the exact location, an intraoperative CT scan was performed with O-arm and the images were used for navigation. A passive planar blunt probe was used to point the exact location of the dislocated odontoid tip and the METRx tube was adjusted to centre on the probe.
The key surgical landmarks identified microsurgically were depicted
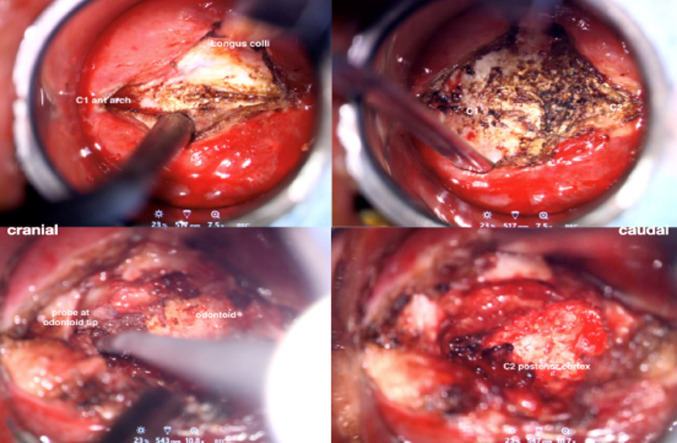
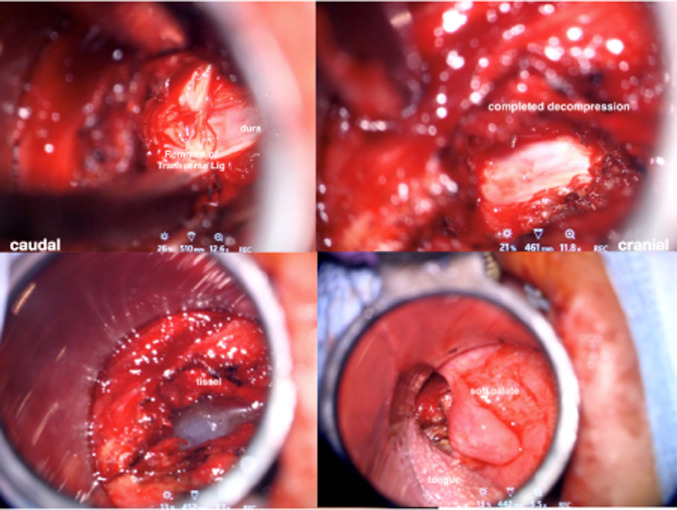
OP21: Lumbar Surgical Outcomes
1222
A181: Comparison of clinical outcome of conventional and endoscopic discectomy in prolapsed lumbar intervertebral disc disease
Ahsan Atta 1 , Usama Muhammad 1 , Ammar Dogar 1 , and Haseeb Hussain 1
1 Orthopedics, Ghurki Trust Teaching Hospital, Lahore, Pakistan
Background: The conventional open technique for excision of lumbar prolapsed inter vertebral disc (PIVD) has been associated with good clinical outcome. But the idea that it causes trauma to the spinal soft tissue; whereas, a less invasive technique like endoscopic surgery will avoid this, has led to more frequent use of endoscopic technique for discectomy. But this newer endoscopic technique requires more experienced surgical hand and advanced technology. This project is designed to compare the clinical outcome of both the techniques at our setup. Research Methodology: A total of 52 patients that underwent lumbar disc excision January 2019 onwards at GTTH Lahore were included in the study. Of these, those who underwent endoscopic discectomy (n = 19) constituted group A, while open discectomy cases were grouped into group B (n = 33). Clinical outcome was studied in terms of leg and back pain (visual analogue scale VAS), disability (Oswestry Disability Index) and patient satisfaction (the modified MacNab score). Results: The study cohort’s mean age was 52 ± 11.6 years and follow-up period was 7.9-2.95 months. 53.58% (n = 32) of the whole sample were females. Postoperatively, statistically significant improvement was noted in both the groups in terms of VAS and ODI (p < 0.05). However, comparison of pain on last follow-up showed no significant difference among the categories (Group A = 2.19 + 0.9, Group B = 2.31 + 1.1, p > 0.05). Similarly, disability comparison by Oswestry Disability Index at last follow up revealed statistically alike state (A = 14.9 + 8.7, B = 16.1 + 9.1, p > 0.05). The only statistically significant difference noted among the two groups was in degree of satisfaction postoperatively, as measured by modified MacNab score (p < 0.05 with Group A = 79.98 + 0.91, Group B = 61.09 + 0.79). Conclusion: Open surgical technique for discectomy has been reported to be an effective treatment option over the year; although, endoscopic discectomy has the advantage of early postoperative recovery, less trauma to soft tissue and lesser postoperative pain. Here it’s evident that the endoscopic discectomy provides equally good results in terms of clinical improvement with added benefit of higher patient satisfaction: that might be due to brisker and less painful postoperative recovery.
Keywords: Prolapsed lumbar intervertebral disc, endoscopic discectomy, open discectomy, clinical outcome
574
A182: Lumbar spinal fusion in elderly patients: a systematic review and meta-analysis of clinical outcomes
Sameer Rathore 1 , Maheswara Akula 1 , and Amr Fahmy 1
1 Spine, Basildon University Hospital, Basildon, United Kingdom
Introduction: Evaluate the morbidity of instrumented lumbar arthrodesis in elderly patients – primarily addressing perioperative complications, operative time and length of hospital stay. Material and Methods: We performed a systematic review of the literature using the PRISMA, searching the Medline/PubMed, Cochrane, EMBASE, and Scopus databases. Inclusion criteria included prospective and retrospective cohort studies with patients age > 65 years treated for degenerative lumbar spinal disorders such as spinal stenosis, spondylolisthesis, degenerative disc disease with posterior instrumented fusion. The articles were screened against established criteria for inclusion into this study and further screening done for extractable data as per our inclusion criteria. Clinical & functional outcomes data using Oswestry Disability Index (ODI), Japanese Orthopaedic Association scores (JOA) and pain intensity using Visual Analogue Scale (VAS) were extracted and analysed. Morbidity and mortality data from studies were incorporated into Excel, with event rates and confidence intervals analysed. Results: Our search strategy identified 1120 studies in total. An additional 38 studies were identified by screening the references of relevant articles. 580 duplicates were removed. 81 articles matched our inclusion criteria which went on to full-text analysis. 35 articles of these were excluded. 46 articles were subjected to qualitative and quantitative analysis. Mortality rate was 2.5% (95% Confidence interval 0.9 to 6.6%) and meta regression of mortality suggested direct relation between the age and mortality. Mean operative duration was 195.5 minutes. The incidence of spinal procedure related complications include: neurological deficit, 3.6%; proximal junctional kyphosis, 4.0%; pseudoarthrosis, 8.5%; seroma/dehiscence, 3.7%; and wound infection, 4.2%; adjacent segment degeneration, 5.4%; dural tear, 6.7%; hardware failure, 2.8%; epidural hematoma, 5.0%. Sub-group analysis was done to assess the impact of fusion technique on mortality and morbidity. Significant improvements in clinical outcome were shown, with a reduction in ODI by 37.1, reduction in pain by 3.7 on the VAS, and significant improvement in functional outcome by 10.6 on JOA scores. Conclusion: Such surgery may often be dismissed in the elderly, due to mortality and morbidity. However, our data sheds light on the relative morbidity, and shows significant clinical and functional outcomes. A shared decision-making process between healthcare professionals, patients and relatives is essential in offering lumbar arthrodesis to older patients. This study provides essential information to guide surgeons and anaesthetists in planning peri-operative care in this challenging demographic, whilst also informing healthcare policy makers considering the aging population.
1532
A183: Non-conformance to guidelines for bracing after degenerative lumbar fusion: international practice pattern
Timothy S. Yoon 1 , Yabin Wu 2 , Ho-Joong Kim 2 3 , Matthew Gary 4 , Samuel Cho 5 , Juan P. Cabrera 6 , Patrick Hsieh 7 , Gianluca Vadalá 8 , and AO Spine Knowledge Forum Degenerative
1 Orthopedic Surgery
2 AO Spine, Degenerative Knowledge Forum
3 Seoul National University Bundung Hospital, Orthopedic Surgery, Seoul, South Korea
4 Neurosurgery,Emory University, Atlanta, United States
5 Orthopedic Surgery, Mount Sinai Hospital, New York, United States
6 Department of Neurosurgery, Hospital Clínico Regional de Concepción, Concepción, Chile
7 Neurosurgery, University of Southern California, United States
8 Orthopedic Surgery, Università Campus Bio-Medico di Roma, Rome, Italy
Introduction: Since the introduction of internal instrumentation for posterior lumbar fusion, the usage of external bracing has decreased. Furthermore, guidelines have been developed that indicate bracing is not required after fusion with instrumentation. However, based on anecdotal information there is still quite high usage of bracing after spinal fusion. The purpose of a current study is to evaluate the current practice pattern of brace usage after lumbar fusion based on specialty and geography. Furthermore, we will compare clinical practice pattern to the current guideline. Materials and Methods: AOSpine sponsored survey was performed. Surveys were sent to all AOSpine members. Members who perform more than 10 cases per year of lumbar fusion (one or two levels) were asked to respond to the questions: 1) Do you use brace after 1 or 2 level open lumbar fusion surgery? What is the main purpose of bracing? What are the factors influencing brace use? The results were analyzed by specialty (neurosurgery vs orthopedic surgery) and geographic region (Asia Pacific, Europe and South Africa, Latin America, Middle East and North Africa, North America). Chi-square test was used to determine differences in proportions and p < 0.05 was used for significance. Results: The overall responses to the use of bracing were 28% yes, 30% occasionally, and 42% never. The responses to reason for bracing were 36% for pain management, 28% to protect the construct, 17% improve fusion rate, 10% to prevent PJK. The factors that influence the decision for brace use were 39% bone quality, 26% age of patient, 22% intraop screw purchase. Between orthopedic surgeons and neurosurgeon there was no difference between specialties on the use age of bracing p = 0.44 using Chi-squared test. Geographic distribution was different with Asia Pacific using bracing significantly more than other geographic regions 86% (yes or occ) compared to (44-60%) in the rest of the world. Conclusion: Brace usage after 1 or 2-levels posterior lumbar fusion is 58% (Yes and Occasional). The bracing decision is not affected by specialty. However, there is significant regional variation in bracing, with surgeons in the Asia Pacific prescribing post-operative bracing more than surgeons from the rest of the world. Despite the 2014 J Neurosurgery Spine guideline recommending "no bracing" after lumbar fusion, our study reveals a significant departure in clinical practice patterns from the 2014 clinical guidelines around the globe. As bracing incurs additional treatment costs and leads to patient discomfort, the use of a brace after lumbar spine fusion should be further studied.
1183
A184: Predictive factors for postoperative loss to follow-up after surgery for degenerative lumbar spondylolisthesis
Anna Filley 1 , Avionna Baldwin 1 , Khuzaima Rangwalla 1 , Faisal Bawahab 1 , Ashraf El Naga 1 , David Gendelberg 1 , and Sigurd Berven 1
1 Orthopaedic Surgery, University of California, San Francisco, United States
Introduction: Long-term, complete postoperative follow-up is essential for ensuring adequate clinical care and statistically sound research. Clinically, incomplete follow-up does not allow the provider to evaluate treatment efficacy, identify surgical complications, or provide additional recommendations. Low follow-up rates can also significantly compromise the internal validity of study outcomes by introducing biases to the data available for analysis. Identifying factors predictive of incomplete follow-up is a topic of high importance to both clinicians and researchers. Therefore, the purpose of this paper was to identify factors predictive of loss to follow-up after surgical treatment of degenerative lumbar spondylolisthesis. Material and Methods: Retrospective study of 184 consecutive patients who underwent elective surgical treatment of symptomatic degenerative spondylolisthesis at our institution between January 2016 and June 2020. Bivariate analysis was used to compare patients lost to follow-up and those with completed or ongoing care based on preoperative demographics, medical comorbidities, and surgical characteristics, in order to identify factors correlated with incomplete follow-up. Results: Ninety patients (48.9%) had incomplete care, defined as failure to return for a scheduled postoperative appointment, of which 58 patients (64%) and 78 patients (87%) were noted to be lost to follow-up at 12 months and 24 months postoperatively, respectively. The overall length of follow-up was significantly shorter for patients with incomplete care (50 ± 52.9 weeks vs 97.8 ± 86.8 weeks, p < 0.0001). Loss to follow-up was associated with younger patient age (OR: 2.74, p = 0.0011), psychiatric comorbidities (OR: 3.13, p = 0.0004), and Medicaid insurance (OR: 2.5, p = 0.03). The odds of incomplete care were also higher for patients who were unemployed (OR: 1.95, p = 0.13) and those with estimated median income below the poverty threshold (OR: 1.76, p = 0.0589), though these trends did not reach statistical significance. Factors including patient gender, race or ethnicity, primary language, marital status, distance from home to surgical facility, number and type of other medical comorbidities, and surgical procedure were not found to be significant. Conclusion: Psychiatric comorbidities, younger age, lower income, unemployment, and Medicaid insurance were associated with an increased risk of loss to follow-up after operative treatment of degenerative spondylolisthesis. Patients lost to follow-up often have a different overall prognosis than those who complete care, and a disproportionate lack of accounting for these cases in clinical outcomes research functions to further marginalize underrepresented subgroups. Recognition of identified risk factors may guide intervention strategies for ensuring continued routine follow-up in these groups.
647
A185: Clinical and neurophysiological outcome of randomized controlled trial for surgical vs non-surgical treatment of lumbar spinal stenosis: the Uppsala Spinal Stenosis Trial (UppSten)
Konstantinos Pazarlis 1 , Arne Sandberg 2 , Anna Rostedt Punga 2 , Nikos Schizas 1 , Bengt Sandén 1 , Karl Michaëlsson 1 , and Peter Försth 1
1 Surgical Sciences, Orthopaedics
2 Medical Sciences, Clinical Neurophysiology, Uppsala University, Sweden
Introduction: Lumbar spinal stenosis (LSS) is the most common indication for spinal surgery. However, only two-thirds of the patients undergoing surgery for LSS report satisfaction with the results, whereas non-surgical treatment has also shown positive results. Material and Methods: The Uppsala Spinal Stenosis Trial (UppSten) was a single center randomized controlled trial including 155 patients with symptomatic LSS who were randomized during 2018-2021 into surgery with decompression or structural physical training (PT). The study included a multidimensional follow-up, including clinical, neurophysiological, radiological and laboratory data. The current analysis included 154 baseline patients and 136 patients who have already passed their 6-month clinical follow-up (FU). The primary outcome was the Oswestry Disability Index (ODI). Secondary outcomes were the Numeric Rating Scale (NRS) for back and leg pain, the EuroQol Five-Dimensional descriptive system questionnaire (EQ-5D) and the six-minute walking test (6MWT). The electrodiagnostic analysis (EDX) included 70 patients; 36 underwent surgery and 34 performed PT. The focus of this analysis was on the segments L5 and S1. The denervation and reinnervation process was measured with motor nerve conduction studies (compound motor action potential; CMAP), concentric needle electromyography (EMG) and motor unit number index (MUNIX). Results: At baseline the two groups showed no significant difference (p > 0.05) for ODI, NRS for back and leg pain and EQ-5D. They differed however regarding the 6MWT. At six months FU, there was a significant difference (p < 0.05) in favor of surgery for all the above outcomes but for the 6MWT where the groups did not differ. In the surgical group there was a significant improvement from baseline for all outcomes including 6MWT (p < 0.05). In the non-surgical group, none of the outcomes showed significant improvement (p > 0.05). The neurophysiological analysis showed no correlation between worse baseline ODI and greater neurogenic involvement with MUNIX and EMG. However, worse baseline ODI related to low degree of possible central activation in the measurement of MUNIX in the S1 segment after intervention. MUNIX (L5) and EMG (S1), both worsened for the PT group but not after surgery. Moreover, there was an improvement of the low central activation after surgery for MUNIX in L5 segment. A significant correlation was found between baseline 6MWT and the MUNIX difference for abductor hallucis (AH) after surgery but not after PT. Conclusion: Our results support that the surgical treatment for LSS leads to superior clinical outcome compared to the non-surgical one when it comes to ODI, NRS for back and leg pain, EQ-5D and 6MWT. Regarding neurophysiology, the EDX cannot predict the clinical outcome measured with ODI when modest neurogenic involvement is present. Surgery preserves the neurogenic degree of involvement while non-surgical treatment seems to worsen the neurogenic EDX involvement. A possible explanation could be that the neural compression in the PT group have continued 6 months longer and thus timing of surgery is of importance. Furthermore, there are indications that decreased muscle activation improves after surgery, but not after training. Finally, we concluded that the 6MWT correlates with MUNIX difference for HA in the surgical group.
1090
A186: Lumbar decompression versus decompression and fusion in octogenarians: complications and clinical course with 3-years follow-up
Pavlina Lenga 1 , Guelec Gelo 1 , Karl L. Kiening 1 , Andreas W. Unterberg 1 , and Basem Ishak 1
1 Neurosurgery, Heidelberg University Hospital, Heidelberg, Germany
Introduction: Over the past years, the prevalence of degenerative disorders of the lumbar spine, such as spinal stenosis and spondylolisthesis, has rapidly increased worldwide in the geriatric population. However, there is still a paucity of data describing the risk factors as well as mortality and morbidity rates of geriatric lumbar spinal surgery. Therefore, we aimed to assess and compare the clinical outcomes and complications (between surgical decompression only versus decompression and fusion in the lumbar spine in patients aged ≥80 years. Material and Methods: A retrospective review of electronic medical records at a single institution was conducted between September 2005 and December 2021. Data of patient demographics, surgical characteristics, complications, hospital clinical course, and 90-day mortality were collected. Comorbidities were assessed using the age-adjusted Charlson comorbidity index (CCI). Logistic regression was used to identify potential risk factors for the occurrence of complications. Results: Over a 16-year period, 327 patients were allocated to the decompression only group, whereas 89 patients were allocated to the decompression and instrumented fusion group, with a mean follow-up duration of 36.7 ± 12.4 months. Patients of the instrumentation group were significantly younger than their counterparts (82.5 ± 2.5 years vs. 81.7 ± 1.4 years; p = 0.049). When assessing the CCI, patients of the instrumentation group had fewer comorbidities (CCI 6.2 ± 1.5 vs. 8.9 ± 0.5; p < 0.001), significantly longer surgical duration (290 ± 106 min vs. 145 ± 50.2 min; p < 0.001), significantly higher volume of intraoperative blood loss (791 ± 319.3 ml vs. 336.1 ± 150.8 ml; p < 0.001), more frequent intraoperative blood transfusion (7 ± 2.1% vs. 16 ± 18.0%; p < 0.001), and extended stays in the intensive care unit and hospitalization rates. However, the in-hospital and 90-day mortality rates were similar in both groups. In-hospital revision rates were significantly higher in the instrumentation group, whereas in the long-term follow-up, no additional surgery was performed in either group. Logistic regression analysis revealed that surgical duration and extent of surgery were unique risk factors for the occurrence of complications. Conclusion: Lumbar decompression only, and additional fusion in octogenarians can safely be performed. Older patients undergoing lumbar spine fusion have longer hospitalization rates and higher revision rates than those undergoing decompression only. However, the mortality rates and neurological outcomes were similar in both groups. Prolonged operative time and extent of surgery are associated with a higher risk of complications. Careful attention to patients’ comorbidities is critical, and use of an anesthetic and operative duration should be kept to a minimum.
76
A187: Surgeons learning curve of Full-endoscopic surgery for sciatica
Pravesh Gadjradj 1 and Biswadjiet Harhangi 1
1 Neurological Surgery, Erasmus MC, Rotterdam, The Netherlands
Objective: Full-endoscopic spine surgery is gaining interest as a less-invasive alternative to treat sciatica caused by a lumbar disc herniation. Concerns, however, exist with the learning curve as percutaneous transforaminal endoscopic discectomy (PTED) appears to be more difficult to be performed compared to other techniques. In this study, the clinical outcomes during and after the learning curve are presented of three surgeons naïve to PTED. Methods: In the first phase of a randomized controlled, non-inferiority trial comparing PTED with microdiscectomy, three surgeons were trained in the PTED-procedure by a senior surgeon. After performing up to 20 cases under supervision, they started performing PTED on their own. Results of the early cases were compared to the later cases (> 20). Furthermore, complications and reoperations were compared. Finally, differences in clinical outcomes between surgeons were compared. Results: At 12 months of follow-up, 87% of the patients had follow-up data available. In general, there were no significant differences in patient-reported outcomes between the early and later PTED-cases. Furthermore, outcomes of the early PTED cases were comparable to the outcomes of microdiscectomy, while the later PTED cases had small, but more favorable outcomes compared to microdiscectomy. Two learning curve surgeons had substantially higher rates of reoperations within 1 year, compared to the senior surgeon or the microdiscectomy group. Duration of surgery was also longer for all learning curve surgeons. Finally, when comparing clinical outcomes of patients undergoing PTED vs microdiscectomy, there appears to be some statistically significant differences in outcomes compared between the senior and three learning curve surgeons. Conclusion: PTED appears to be safe to be adopted by surgeons naïve to the procedure when they are initially supervised by an experienced senior surgeon. Duration of surgery and risk of repeated surgery are increased during the learning curve, but patient-reported outcomes of the early PTED cases are similar to the outcomes of later PTED cases, and similar to the outcomes of microdiscectomy cases. This study underlines the need for an experienced mentor for surgeons to safely adopt PTED.
1498
A188: A long-term follow-up study of the effects of intervertebral height index on clinical outcomes, imaging parameters, and degeneration of adjacent segments after single-level lumbar fusion with different fusion methods
Zhuojing Luo 1
1 Institute of Orthopaedics, Xijing Hospital, The Fourth Military Medical University, Xi’an, China
Purpose: To compare the effects of intervertebral height index on the clinical efficacy, imaging parameters, and adjacent segmental degeneration after single-level ALIF, TLIF or PLF. Methods: A total of 504 patients underwent single-level L4-5 surgery in our department from March 2003 to October 2007, of which 221 met the inclusion and exclusion criteria of this study. According to the different surgical methods used on the 221 patients, they were divided into the ALIF group (27), TLIF group (136), and PLF group (58). The previous research of our team recommends different reference values of the normal intervertebral height index for people of different ages and genders, so the patients of each group in this study were sub-divided into two parts: the restoration of intervertebral height index group and the non-restoration of intervertebral height index group. Basal parameters and clinical efficacy was evaluated at preoperative and final follow-up. Fusion rate and incidence of radiographic adjacent segmental degeneration (rASD) were assessed at follow-up. The changes of preoperative and postoperative clinical efficacy and imaging parameters in each group were compared, and the effects of intervertebral height index on the above parameters were analyzed. Results: All the 221 patients were enrolled and followed up for a mean of 93 months (61-120 months). In the ALIF group, 21 patients (77.7%) recovered the intervertebral height index, 95 patients (69.9%) in the TLIF group, and 6 patients (10.3%) in the PLF group, and there was a statistical difference between the three groups (p < 0.05). The clinical efficacy of each subgroup were improved compared with those before surgery, with statistical significance (p < 0.05). In the ALIF group, the proportion of PI-LL mismatch in the recovery group was significantly reduced (p < 0.05), while in the TLIF and PLF groups, the proportion of PI-LL mismatch in the recovery group and the non-recovery group were not statistically different from those before surgery (p > 0.05). In the ALIF and TLIF groups, the proportion of PI-LL mismatch in the recovery group was less than that in the non-recovery group, which was statistically significant (p < 0.05). The incidence of rASD in the recovery group was lower than that in the non-recovery group of the three groups, with a statistical difference (p < 0.05). Conclusion: The long-term clinical outcome of L4-5 single-level fusion were all satisfied with similar fusion rates no matter ALIF, TLIF, or PLF was employed. Among the three groups, the lowest incidence of ASD occurred in the ALIF group while the highest occurred in the PLF group, and the probability of PI-LL mismatch after PLF was higher. Restoring the intervertebral height index to the normal range can better improve SL and LL, reduce the proportion of PI-LL mismatch after surgery, and reduce the occurrence of ASD.
1075
A189: Does a high BMI affect patient reported outcome in single level spinal fusion surgery?
Muhammad Usman 1 and Silviu Sabou 2
1 Trauma and Orthopaedics, Torbay Hospital, Torquay, United Kingdom
2 Department of Spinal Surgery, Salford Royal Hospital, Manchester, United Kingdom
Introduction: Lumbar fusion for obese or morbidly obese has been shown to have a higher rate of complications compared to non-obese patients. However, there is a paucity of studies evaluating the correlation between functional and pain outcomes of single level lumbar fusion surgery and obesity. Materials and Methods: We analysed prospectively collected data on 240 patients who underwent single level Posterior/ Transforaminal Lumbar Interbody Fusion (TLIF/ PLIF) between 2012 to 2015. Data on patient characteristics including BMIs were collected, as well as outcomes in the form of COMI scores, VAS scores for Back and Leg pain at Preop, 3 months, 6 months, 12 months and 24 months postoperatively. Kruskal-Wallis test was used to determine correlation between patients grouped by BMI category and patient reported outcomes measures (PROMs). Results: No corelation between BMI and COMI scores (p = 0.44), BMI and VAS Back pain (p = 0.07), BMI and VAS Leg Pain scores (p = 0.35) was noted. Patients were then re-grouped into Obese and Non-Obese patients and the statistical analysis did not show any significant difference in outcomes. Conclusion: Obese patients have similar improvement in pain following lumbar surgery as measured by COMI, VAS leg and VAS back as non-obese patients. Although the literature has shown a higher complication rate in obese patients, our study suggest that high BMI does not negatively impact pain and functional outcomes of single level posterior interbody fusion in well selected individuals.
OP22: Clinical Basic Science
1742
A190: Microfluidic model of innervated vasculature for nociception using human dorsal root ganglia from spine patients
Annee Nguyen 1 , Cesar Baeta 2 , Harrison Hockenberry 1 , Vardham Kumar 3 , Sajeeshkumar Perikamana 1 , Antoinette Charles 1 , Brandon Bishop 1 , Edwin Owolo 1 , David Kingsley 1 , Shyni Varghese 3,4 , and C. Rory Goodwin 1
1 Department of Neurosurgery
2 Stanford University, Center for Population Health Sciences, Palo Alto, United States
3 Department of Biomedical Engineering
4 Department of Orthopedic Surgery, Duke University School of Medicine, Durham, United States
Introduction: The interaction between nociceptor sensory neurons and vasculature is fundamental in evoking pain responses, neurite growth, and angiogenesis and is essential in studying neurodegenerative disorders and related therapeutic explorations. However, in vitro models are still limited in their ability to mirror the neurite/vascular system crosstalk seen in animals and in humans. We present the development of a microfluidic-assisted tissue model of nociception in the presence of microvasculature, using human dorsal root ganglia (DRG) from two spine patients. Methods: The chip device was created by soft lithography using polydimethylsiloxane (PDMS) to construct two parallel hydrogel microchannels for human cell culture, each surrounded by channels containing growth media. Human umbilical vein endothelial cells (HUVECs) were first cultured on the chip device for 4-5 days to establish perfusable vasculature. Human DRG neurons were harvested from spine patients and either co-cultured with the HUVECs or cultured alone on the device. Cultures were imaged and probed at Day 0 and Day 5. To compare nerve morphology, average neurite length and density were quantified and innervated vasculature tissue and neurons were immune stained with VE-cadherin and B-tubulin, respectively. To compare neuronal function, DRG monocultures and co-cultures were immune stained with TRPV1. Statistical analysis between mono- and co-cultures was performed using a student’s T-test. Results: Human DRG co-cultured with HUVECs (N = 20 neurons) had significantly greater neurite sprouts per cell (p < 0.0001) than human DRG monoculture (N = 13 neurons) with no significant difference in neurite length. Functionally, human DRG co-cultured with HUVECs (N = 31 neurons) had significantly higher TRPV1 expression (p < 0.0001) compared to human DRG monocultures (N = 33 neurons). Conclusion: Generation of perfusable vasculature innervated with human DRG is feasible, even with low cell density. This human-specific model can be fundamental to investigate nociceptive mechanisms, to aid in the development of analgesics and non-opioid alternatives, and ultimately to explore the effects of spine-associated pain.
1728
A191: Dysregulated gene expression of the Hippo-pathway can be associated with the biological behaviour of sacral chordoma
Arpad Bozsodi 1 , Beáta Scholtz 2 , Gergő Papp 3 , Zoltán Sápi 3 , Ádám Biczó 1 , Peter Pal Varga 1 , and Aron Lazary 1
1 National Center for Spinal Disorders, Budapest, Hungary
2 Biochemistry and Molecular Biology, Genomic Medicine and Bioinformatic Core Facility, Debrecen, Hungary
3 1st Department of Pathology and Experimental Cancer Research, Semmelweis University, Budapest, Hungary
Introduction: Chordoma is the most frequent primary malignant spinal tumor. It is characterized with a relative resistance on conventional oncological therapies and a high rate of local recurrence. The molecular mechanism of its oncogenesis is still unclear. Recurrence of the tumor can be related to the dysregulation of the expression of hundreds of genes and their complex regulatory networks such as non-coding RNAs, especially miRNAs. The Hippo signaling pathway controls cell proliferation and apoptosis but has a critical role in cell renewal and expansion of tissues too. Methods: Next-generation RNA sequencing was made to analyse the molecular profile of chordoma in comparison with nucleus pulposus samples to detect the alterations in the traqnscriptom and regulatory networks. Advanced bioinformatics workflow was applied on data for the comparative, integrated analysis of the transcriptome. Results were validated by RT-qPCR. Results: A high number of miRNA/mRNA networks have been identified with significant regulatory potential. A gene set with differently expressed miRNAs including key elements of the Hippo pathway was also identified and validated by RT-qPCR like TAOK1/miR-142, MOB1B/miR-148a/miR-182, LCOR/miR-199a-5p, MITF/miR-182-5p/miR-101/miR-148a-3p, HIF3a/miR-485-5p, HMGA1/miR-142-3p, RASA1/miR-182-5p/miR-223-3p, RGS17/miR-182-5p and RICTOR/miR-142-3p. These newly identified miRNA/RNA interactions are supposed to have a role in the self-renewal process of chordoma stem-cells providing the high recurrence ability of this tumor. Conclusions: Results of this comparative, next-generation sequencing study can significantly contribute in the understanding the nature of chordoma and designation of possible molecular targets of further development of anti-chordoma therapies.
1258
A192: The relationship between glycosaminoglycan and water content in the intervertebral disc and its degeneration
Dominik Taterra 1,2 , Krzysztof Tomaszewski 3 , and Przemyslaw Pekala 2
1 Orthopedic Rehabilitation, University Hospital, Zakopane, Poland
2 Department of Anatomy, Jagiellonian University Medical College, Krakow, Poland
3 A. F. Modrzewski Krakow University, Poland
Introduction: The correct spatial distribution and high negative charge of glycosaminoglycan chains (GAG) within the extracellular matrix of the intervertebral disc (IVD) is responsible for discs’ water imbibition, proper osmotic pressure and as such IVD’s physiological swelling behaviors. The changes in the content of extracellular matrix of the IVD that occur with age and degeneration lead to a loss of its bearing properties. There were only few studies in the literature on the distribution of GAG content and water concentration in the lumbar IVDs. However, they were limited by a very small sample size. Therefore, there was a need for a more comprehensive study on a large sample size analyzing the role of GAG and water content in degeneration of lumbar IVDs. As such, the aim of this study was to investigate the association of the distribution of GAG and water concentration with IVD degeneration as measured by Pfirrmann et. al and Thompson et al. grading systems. Material and Methods: Full spinal columns (vertebrae L1-S1 and IVD between them) were harvested from fresh cadavers through an anterior dissection. MRI scans of all spinal columns were conducted and assessed using Pfirrmann grading system. All vertebral columns were cut in the midsagittal plane. The level of degeneration was assessed morphologically using Thompson et al. grading system. Grades 4-5 were included in cases group, while grades 1-3 were included as controls. Samples from 5 regions of the L5/S1 IVDs were taken for concentration analyses. Standard curve spectrophotometry was utilized for this purpose. GAG and water content was compared between degeneration and control groups. Results: One hundred lumbar spine columns (L1-S1) were harvested from male cadavers. Mean age of the donor was 42.2 ± 12.3 years. Radiologic assessment using the Pfirrmann grading system and morphological Thompson grading system classified majority of discs as grade 3 and 4. A total of 478 samples from 5 regions of L5/S1 IVDs were included in the analysis of GAG content. The samples from the nucleus pulposus showed on average the highest concentration of GAG, although the differences were not statistically significant. The analysis revealed that there was significant decrease of mean GAG content in the IVD with degeneration as assessed by Pfirmann grading system (Z = -2.87, p = 0.004). Subgroup analysis on the GAG content between degenerated and control IVDs from 5 different regions of the IVD showed no significant differences, except for posterior inner annulus fibrosus (t[78] = 2.72, p < 0.01). All samples were included in water content analysis. There was a significant decrease of mean water content percentage with degeneration as measured by Pfirrmann grading system (Z = -1.99, p = 0.046). No significant changes were shown when Thompson grading system was utilized. Conclusion: Our study showed that there was a significant decrease of mean GAG content and water content in the IVD with degeneration. Regional IVD differences were not prominent, except for posterior inner annulus fibrosus. No significant changes in GAG and water content were found when Thompson grading system was used in the analysis.
1170
A193: Molecular interactions between pattern recognition receptors and putative pathogenic effector proteins in degenerative disc disease. A predictive insilico approach
Shanmuganathan Rajasekaran 1 , Chitraa Tangavel 2 , Sharon Miracle Nayagam 2 , Sunmathi R 2 , Murugesh Easwaran 2 , Ganesh Selvaraj 2 , Sri Vijay Anand KS 1 , Chandhan Murugan 1 , Ajoy P Shetty 1 , and Rishi Kanna 1
1 Dept. of Spine Surgery, Ganga Hospital, Coimbatore, India
2 Ganga Research Centre, Coimbatore, India
Background: Sub-clinical infection has been hypothesized to play a role in etiopathogenesis disc disorders. Our earlier reports have provided definite evidence of the prevalence of host-defense responses within the intervertebral disc, which serves as the proof-of-evidence for infection-mediated inflammatory mechanisms. In order to understand the rewiring of host metabolism, interactions between effector proteins (secretory proteins of the microbial consortia) and host proteins were studied. Material and Methods: Proteome data of 36 nucleus pulposus tissues were considered for the study under three groups: 11 healthy NP tissues from voluntary organ donors (normal disc group (ND); Twenty five degenerated diseased group (DD)- 17 in modic and 8 in non-modic condition respectively. The proteome raw-data were mapped with the bacterial and human proteome database to identify the host and bacterial proteins. Human proteins were manually curated based on literature evidence to identify the Pathogen Recognition Receptor (PRR) proteins. Similarly, bacterial proteins were screened for the presence of effector proteins by mapping with the bacterial T3 Secretory System library. Insilico predictive analysis of molecular interactions between host proteins and putative pathogenic bacterial proteins was done to understand the host-pathogen regulatory mechanisms. Results: Out of 8746 identified human proteins, 23 proteins were manually curated as PRRs (Pathogen Recognition Receptor). Following stringent statistical parameters (25% sample prevalence and ≥ 5 PSM), only six proteins such as C-type lectin domain family 3 member A (CLEC3A), C-type lectin domain family 11 member A (CLEC11A), C-type lectin domain family 2 member D (CLEC2D), Interferon- Inducible protein (AIM2), Fibronectin (FN1) and Vitronectin (VTN) were selected for the interaction study. To validate the host-pathogen interactions, molecular interaction analysis were performed between host PRRs and bacterial T3 secretory effector proteins. As a result, thermodynamically stable interaction prevails between the bacterial effector proteins with chosen five PRRs except for AIM2. While no bacterial T3 secretory effector proteins were detected in ND group, Forty-nine bacterial proteins [38: DD-Modic, 11: DD- Non-modic] were identified in DD group. Six effector proteins such as ATP synthase subunit beta, Elongation factor Tu 1, Elongation factor Tu 2, Elongation factor G, Major outer membrane lipoprotein Lpp, and Outer membrane protein A were selected after mapping against the T3 Secretory System Library. Conclusion: Host PRR proteins such as CLEC3A, CLEC2D, CLEC11A, FN1, and VTN interacted with the bacterial secretory proteins such as 30S ribosomal protein S4, and UDP-glucose 6-dehydrogenase. Observed bacterial proteins indicate the bacterial presence in disc tissues, and observed PPR and its interactions indicate a possible host-microbiome interaction within NP tissues.
1206
A194: Are endplates the gateway for establishment of inter vertebral disc microbiome ? A comparative metagenomic analysis
Shanmuganathan Rajasekaran 1 , Sri Vijay Anand KS 1 , Chandhan Murugan 1 , Sharon Miracle Nayagam 2 , Sunmathi R 2 , Monica Steffi Matchado 2 , Chitraa Tangavel 2 , Raveendran M 3 , Rishi Kanna 1 , and Ajoy P Shetty 1
1 Dept. of Spine Surgery, Ganga Hospital, Coimbatore, India
2 Ganga Research Centre, Coimbatore, India
3 Department of Biotechnology, Tamilnadu Agricultural University, Coimbatore, India
Background: There is increasing evidence for subclinical infection by fastidious low, growing bacteria to be a cause of disc degeneration. Although the presence of bacteria in the Nucleus pulposus has been reported well in literature, the source of bacteria is not clearly proved as the disc is avascular in healthy condition. Documentation of similar bacterial populations in the EP and NP may add proof that bacterial inoculation of NP occurs via the Endplate. Materials and Methods: Sixteen NP and 16 EP tissues were excised from brain-dead voluntary organ donors with no history of back pain and 20 diseased discs collected from patients undergoing microdiscectomy/ fusion surgery were used for profiling microflora through 16S rRNA amplicon sequencing using primers specific for V1-V9 hypervariable regions. Changes in the bacterial diversity and abundance were analyzed to identify the key microbial populations that are significantly altered in DD. Results: NP and EP shared a similar spectrum of microbiome but with varying abundance. The five dominant phyla identified were Proteobacteria, Firmicutes, Actinobacteria, OD1, and Bacteroidetes. Proteobacteria was found to be the most abundant phyla in both NP (62%) and EP (53%) of the normal IVD. This was followed by Firmicutes (16%), Actinobacteriota (11%), OD1 (Parcubacteria) (7.6%), and Bacteroidetes (2%) in NP and Firmicutes (23.4%, OD1 (Parcubacteria) (17.6%), Actinobacteriota (2.8%), and Bacteroidetes (2.6%) in EP respectively. Under diseased conditions, Proteobacteria (68%) was dominant when compared with other phyla. However, there was no significant difference in the abundance of Proteobacteria between the normal and diseased discs. Interestingly, the other dominant phyla such as Firmicutes (Normal-NP: 16.2%; Diseased-NP: 4.02%) and Actinobacteria (Normal-NP: 11%; Diseased-NP: 0.99%) showed a significant reduction in degenerated discs. To understand the key microbial populations that are significantly altered during disease, correlation analysis was performed among the three phyla, which revealed a negative correlation in the ratio of Actinobacteria + Firmicutes vs. Proteobacteria (p = 0.001) in DD. Conclusion: Results of our study clearly demonstrated a similar bacterial diversity but with varying abundance between the EP and NP, suggesting that the endplate could indeed be the gateway for the entry of the microbiome into nucleus pulposus.
1393
A195: The anatomical relationship between the cervical nerve roots, intervertebral discs and bony cervical landmark for posterior endoscopic cervical foraminotomy and discectomy: a cadaveric study
Gun Keorochana 1 , Pilan Jaipanya 2 , and Chakkraphan Tantrakansakun 3
1 Department of Orthopedics, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
2 Department of Orthopedics, Chakri Naruebodindra Medical Institute, Thailand
3 Department of Orthopedics, Ramathibodi Hospital, Mahidol University, Thailand
Introduction: The development of minimally invasive spine surgery (MISS) using a full cervical endoscope enables spine surgeons to avoid approach-related complications or extensive tissue damages associated with open surgeries. Posterior endoscopic cervical foraminotomy or discectomy (PECF or PECD) is a well-established procedure. The objective of this study was to define the anatomical relationship between bony landmark “V point”, dural sac, nerve roots, and intervertebral disc for improving operative outcomes and decreasing post-operative complications. Material and Methods: 10 soft adult cadavers were studied. We measured the distance of the V point to the lateral margin of dural sac, V point to the inferior border of intervertebral disc, and the inferior border of cervical nerve root to the inferior border of intervertebral disc. Then we calculated the mean of distance from V point to the inferior border of cervical nerve root. The relationship between these distances at each cervical spine level was evaluated and analyzed. Results: The mean distance from the V point to the lateral margin of dural sac from C3/4 to C7/T1 ranged from 3.1 ± 1.38 mm to 3.37 ± 1.46 mm. The mean distances from V point to the inferior border of intervertebral disc from C3/4 to C7/T1 were 0.19 ± 1.16 mm at C3/4, 0.45 ± 1.23 mm at C4/5, 0.43 ± 1.01 at C5/6, -0.43 ± 1.86 mm at C6/7 and -1.5 ± 1.2 mm at C7/T1. The mean distance from the inferior border of cervical nerve root to the inferior border of intervertebral disc from C3/4 to C7/T1 ranges from 0.25 ± 1.07 mm to 2.97 ± 2.35 mm in an increasing manner from the cranial to caudal levels. The mean distance between V point and the inferior border of cervical nerve root from C3/4 to C7/T1 showed all positive value, ranging from 0.06 ± 1.18 mm to 4.45 ± 2.57 mm. This illustrate that the V point is located more inferiorly to the nerve root at all levels and the distance tends to increase at caudal levels of cervical spine. Conclusion: In performing PECF or PECD, a 3-4 mm radius of bone removal should be enough for exposure and neural decompression at C3/4 to C5/6. At C6/7 and C7/T1 a more extensive bone cut of more than 4 mm is recommended, especially in cranial direction. Surgeons should consider removing the inferior part of the upper lamina further than the superior border of inferior lamina, starting from the V point.
1635
A196: The role of microglia/macrophages activation and TLR4/NF-kB/mark pathway in distributional spinal cord injury
Weishi Liang 1 , Bo Han 1 , Yong Hai 1 , and Peng Yin 1
1 Department of Orthopedic Surgery, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Background: Distraction spinal cord injuries (DSCIs) often occur as the neurological complication of distraction forces following the implantation of internal fixation devices during scoliosis correction surgery. However, the underlying mechanism behind these injuries remains unclear. Purpose: The present study aimed to explore the activation of microglia and macrophages, as well as changes in TLR4-mediated NF-κB and MAPK pathway activity after DSCIs in Bama miniature pigs. Methods: Prior to surgical intervention, the pigs were randomly divided into three groups: the sham group, the complete distraction spinal cord injury (CDSCI) group, and the incomplete distraction spinal cord injury (IDSCI) group. After surgery, the Tarlov scale and individual limb motor scale (ILMS) were used to evaluate changes in the pigs' behavior. All pigs were euthanized 7 days after surgery, and histopathological examinations of the spinal cord tissues were performed. Immunohistochemistry was used to detect Caspase-3 expression in the anterior horn of spinal gray matter tissues. Immunofluorescence staining was utilized to assess the M1/M2 phenotype changes in microglia/macrophages and NF-κB P65 expression in central DSCI lesions, while western blotting was performed to determine the expression of TLR4/NF-κB/MAPK pathway-related proteins. Results: The results of the present study showed that the Tarlov and ILMS scores decreased significantly in the two DSCI groups compared with the sham group. Hematoxylin and eosin (HE) and Nissl staining revealed that the tissue structure and nerve fiber tracts in the distracted spinal cord tissues were destroyed. Both DSCI groups showed the number of survived neurons decreased and the Caspase-3 expression increased. The results of the immunofluorescence staining indicated that the CD16 and CD206 expression in the microglia/macrophages increased. Between the two DSCI groups, the CDSCI group showed increased CD16 and decreased CD206 expression levels. The intensity of the fluorescence of NF-κB P65 was found to be significantly enhanced in pigs with DSCIs. Moreover, western blot results revealed that the expression of TLR4, p-IκBα, NF-κB P65, p-JNK, p-ERK, and p-P38 proteins increased in spinal cord tissues following DSCI. Conclusion: The present study was based on a porcine DSCI model that closely mimicked clinical DSCIs while clarifying DSCI-associated neuroinflammation mechanisms, in turn providing evidence for identifying potential anti-inflammatory targets.
741
A197: Association of polymorphism in leptin receptor gene with susceptibility of adolescent idiopathic scoliosis
Antonio Eulalio Pedrosa Araujo Junior 1 , Renato Tavares 1 , gustavo azevedo 1 , Luis Antônio Moliterno 1 , Jessica Vilarinho Cardoso 2 , Helton Defino 3 , and Jamila Alessandra Perini 2
1 Spine Surgery Center, National Institute of Traumatology and Orthopedics (INTO), Rio de Janeiro, Brazil
2 Research Laboratory of Pharmaceutical Sciences, State University of Rio de Janeiro (UERJ), Rio de Janeiro, Brazil
3 University of Sao Paulo, Ribeirão Preto School of Medicine, Ribeirão Preto, Brazil
Introduction: Patients with AIS may have abnormal leptin bioavailability, which influence in the bone formation and resorption, hence result in the disorder of skeletal growth. Although genetic studies revealed numerous potential polymorphisms associated with AIS, the etiology continues unknown. This study aimed to evaluate the potential role of polymorphisms in the gene encoding leptin (LEP) and its main receptor (LEPR) in the development of AIS. Materials and Methods: A retrospective case-control study was conducted with 202 AIS patients and 555 healthy controls recruited in a reference center in orthopedics from Brazil. Polymorphisms LEP rs2167270 and LEPR rs2767485 were genotyped using a TaqMan validated assay. Associations were evaluated by a binary logistic regression model, using odds ratios (OR) and 95% confidence intervals (CI). Results: Among the AIS group there was a predominance of females (n = 189, 93.6% and 14.5:1), 150 (74.3%) under 18 years old (16.7 ± 5.4), 177 (87.6%) low or normal BMI (20.6 ± 4.4 kg/m2), 119 (58.9%) had a Cobb angle greater than 45º (49.1 ± 16.3° Cobb) and 140 (69.3%) were skeletally mature (Risser IV-V). The minor allele frequencies of LEP rs2167270 and LEPR rs2767485 were 35.9% and 18.3%, for AIS cases; 37.0% and 24.4% for controls, respectively. After adjustment for confounding factors (age, sex and BMI), LEPR rs2767485 C allele and CC genotype were associated with a lower risk of AIS susceptibility (OR = 0.69; 95% CI = 0.52-0.92 and OR = 0.71; 95% CI = 0.67–0.75, respectively). Moreover, the LEPR rs2767485 CC genotype was only present in the group without spinal disease (control). No significant differences were detected in LEP rs2167270 polymorphism distribution between AIS cases and controls (Pearson's Chi-square test). Conclusion:LEPR rs2767485 polymorphism was associated with the genetic susceptibility of AIS, which represents an advance in understanding etiology of disease. These data can contribute to the identification of genetic biomarkers and, thus, could assist in the accurate and timely diagnosis of disease, being able to monitoring the at-risk individual, avoiding frequent follow-up, poor health quality of life and high treatment costs.
1975
A198: Optimization analysis of 3D printed titanium surface morphology for stem cell attachment and differentiation
Gregory Paschal 1 , Philip Paschal 1 , Samuel Goldman 1 , Fedan Avrumova 1 , Gbolabo Sokunbi 2 , Darren Lebl 2 , Frank Cammisa 2 , and Celeste Abjornson 1
1 Hospital For Special Surgery, Integrated Spine Research Program, New York, United States
2 Hospital For Special Surgery, Spine Surgery , New York, United States
Introduction: Titanium is a commonly used material for orthopedic implants. While titanium does possess osteoconductive properties that promote bone growth, certain surface morphologies can promote this activity more than others. With current advancements in 3D printing technology, titanium implants can be made with specific morphologies that optimize osteoconductivity. Investigation of different surface morphologies in vitro can translate into the production of a biologically optimized implant for spine surgery patients. The purpose of this study is to evaluate the response of mesenchymal stem cells to titanium implants with different surface morphology (roughness). We hypothesize that a certain surface roughness will best promote bone formation. Material and Methods: Titanium coupons were 3D printed with different surface roughness (smooth, fine, medium, rough, and very rough) and cultured with human mesenchymal stem cells. After 7 days, a portion were fixed and imaged via scanning electron microscope (SEM). Cell lysate and media were collected at 7, 14, and 21 days and assayed for viability and indicators of cell signaling toward osteocyte differentiation. Fluorescent microscopy was used to determine cell viability. Cell differentiation was determined via ELISA for osteocalcin, alkaline phosphatase, vascular endothelial growth factor (VEGF), bone morphogenic proteins (BMP) 2,4, and 7, and interleukins (IL) 1 beta, 6, 8, and 10. Results: Cell viability tests showed that cells were able to grow on all surfaces. Electron microscopy showed cellular attachment and communication on all samples except smooth, and at a greater amount in the medium to rough groups. Cell protein assays showed that cells on all surfaces were expressing important targets towards bone formation, with some surfaces showing a stronger response. Conclusion: Cellular attachment and biological response are necessary for osteoblast differentiation and bone formation. Current 3D printing technology allows for the production of implants with surface morphology that optimized biological response. The results of our study can hopefully further our understanding of the specific characteristics that optimize bone formation for implants.
OP23: Management of Primary Spinal Infections
829
A199: Patient-specific risk factors for the need of surgical revision in the treatment of endogenous spondylodiscitis - a retrospective analysis of 130 patients
Friederike Schömig 1 , Zhao Li 1 , Luis Becker 1 , Maximilian Muellner 1 , Pumberger Matthias 1 , and Nima Taheri 1
1 Center for Musculoskeletal Surgery, Charité - Universitätsmedizin Berlin, Berlin, Germany
Introduction: Despite the rising incidence of spondylodiscitis, to date there are no coherent guidelines for the surgical management of spinal infections. In particular, there is a lack of studies investigating perioperative complications after the surgical treatment of spondylodiscitis. Thus, in our study, we analyzed risk factors for the occurrence of postoperative complications warranting surgical revision in patients treated for endogenous spondylodiscitis. Material and Methods: We retrospectively included patients with endogenous spondylodiscitis who were treated surgically at our center between January 2006 and December 2020. Clinical and radiological data were collected from electronic patient charts. Spondylodiscitis was defined by a combination of distinct radiological findings of the intervertebral disc in MRI and/or CT imaging and clinical findings. The performed surgeries were grouped into debridement and decompression alone versus debridement, decompression, and instrumentation. Causative pathogens were identified using CT-guided biopsy, open biopsy, intraoperative tissue sampling, and/or blood cultures. Results: A total of 130 patients with a mean age of 66.3 ± 12.5 years were included. In 35 cases (26.9%) surgical revision was necessary and was performed within 65.8 ± 105.9 days. The most frequent indications for revision were wound healing disorders (54.3%), followed by postoperative abscesses (17.1%), implant failure (11.4%), progressive neurological deficits (8.6%), hematomas (5.7%), and dural tears (2.9%). In the revision group, the infection was located significantly more frequently in the thoracic (22.1% vs. 34.3%) or in two or more parts (4.2% vs. 17.1%) of the spine (p = 0.013) compared with the group without surgical revision. We did not find significant differences in age, sex, body mass index, Charlson Comorbidity Index, comorbidities, laboratory parameters or symptoms at admission, or type or extent of surgery between patients with and without surgical revision. In patients requiring revision surgery, Staphylococcus aureus (20.0% vs. 40.0%, p = 0.020) was found significantly more frequently than in patients not requiring surgical revision. Multiple logistic regression analysis showed a significant influence of both smoking (B = 1.613, p = 0.017) and the detection of Staphylococcus aureus (B = 1.500, p = 0.013) on the necessity of surgical revision. Conclusion: While previous studies have focused mainly on patient outcome after surgical treatment of spondylodiscitis, we for the first time analyzed the association of several pre- and intraoperative parameters with the need for surgical revision in the treatment of endogenous spondylodiscitis. Our results show that smoking as well as the detection of Staphylococcus aureus as a causative pathogen are significantly associated with the performance of a revision surgery. When planning the optimal individual treatment for each patient, these factors need to be taken into consideration.
571
A200: Comparative analysis of long term outcome of anterior reconstruction in thoracic tuberculosis by anterior vs posterior approach
Dr. Manojkumar Gaddikeri 1 and Sudhir Srivastava 2
1 Lilavati Hospital and Research Center, We Are Spine, Mumbai, India
2 Orthopaedics, K J Somaiya Medical College and Hospital, Mumbai, India
Introduction: First described by Sir Percival Pott, tuberculosis is an age-old problem affecting millions worldwide with developing countries being affected the most. Thoracic spine is the most common site affected with anterior column involved more commonly leading to kyphotic deformity and neural compression. The selection of whether anterior or posterior approach is still a matter of debate. The above study was done to compare the long term outcome in these two approaches. Material and Methods: A total of 245 patients with proven tuberculosis of thoracic spine were included, of which 127 were operated by posterior-approach and 118 were operated by anterior-approach using versatile approach technique. Patients with at least 1-year of post-operative follow up were included and their data was retrospectively analyzed. Patients were assessed clinically, radiologically and data regarding demography, affected levels, surgical approach used, operative time, blood loss, neurology as per Frankel grade, pre & post-operative alignment, percentage correction of kyphosis, time for fusion, fusion grade using Bridwell criteria, percentage loss of correction at the end of 1year, time for mobilisation and complications if any were collected, analyzed and compared in anterior versus posterior approach. Results: Mean age of patients in anterior-approach was 36.03 years & 39.83 years in posterior approach. Mean operative time in anterior-approach was 6.11 hours & 5hours in posterior approach. Mean blood loss was 1.6litres in anterior approach & 1.11litres in posterior approach. Mean kyphosis angle in posterior-approach was 34.803° pre-operatively & 11.286° (p < 0.001) at 3 months post-operative follow up with percentage of correction being 67.216%. Mean loss of correction at 1year was 4.186°. Mean kyphosis angle in anterior-approach was 41.154° pre-operatively & 9.498° at 3months post-operative follow up with percentage of correction being 77.467% (p < 0.001). Mean loss of correction at 1year was 6.184°. Mean time for fusion was 4.69 months in anterior-approach and 6.34 months in posterior-approach with mass considered fused as per Bridwell criteria. Mean time for mobilisation in posterior-approach was 1.18 weeks & 2.51 weeks in anterior-approach. Significant improvement in neurology was seen in patients operated by either approach, but slightly better improvement was seen in those operated by anterior-approach. Complications were slightly more in posterior-approach. Conclusion: Decompression and deformity correction are the only answer to prevent progression of kyphosis, neurological deficit and late onset paraplegia in these complex cases. Single stage anterior reconstruction and posterior stabilization via anterior approach allows for thorough debridement, neural decompression and much better anterior column reconstruction and deformity correction than posterior approach. Direct visualization of cord while correcting kyphosis reduces chances of neurological complications significantly. Both approaches have their own unique advantages and limitations. The age old saying of increased morbidity and poorer results with anterior approach have been proven wrong in this study. Though posterior approach is easy to master but the results shown by anterior approach cannot be overseen. We would like to conclude that better functional outcome and significantly better kyphosis correction by the anterior approach are strong pointers favoring the anterior approach.
906
A201: Determination of drug resistance pattern and incidence of drug resistance in spinal tuberculosis
Md Nawaz 1 , Rehab Razi Khan 2 , and Anil K. Jain 3
1 Orthopaedics, Katihar Medical College, Katihar, India
2 Rama Medical College and Hospital, Delhi, India
3 Orthopaedics, University College of Medical Sciences, University of Delhi, Delhi, India
Introduction: There is paucity of data on drug resistance pattern in spinal TB. This prospective observational study was conducted to document incidence of drug resistance among primary and presumptive resistant cases. Material and Methods: 59 consecutive cases diagnosed clinico-radiologically (imaging) were grouped into: Group A (n = 51, primary cases) and Group B (n = 8, presumptive resistant cases) based on pre-defined criteria (INDEX-TB guidelines, 2017). Tissue samples obtained percutaneously (37.29%,22/59) and surgery (62.71%,37/59) were subjected to genotypic DST (CBNAAT, LPA 1stand 2nd line) and phenotypic DST (BACTEC MGIT 960 culture and sensitivity using fixed critical concentration of drugs). Results: Etiological diagnosis was ascertained in all. 13/51 (25.49%) in GroupA while 3/8 (37.5%) in GroupB and 16/59 (27.12%) overall demonstrated drug resistance. 12/16 (75%) had no prior history of ATT intake. 4 had INH (Isoniazid) mono-resistance, 12 with polydrug resistance demonstrated: 5MDR, 3pre-XDR while RIF+FQ (fluoroquinolones), FQ+Lz (linezolid), only SLID (second line injectable drugs) and only FQ resistance observed in 1 case each. Isolated RIF(Rifampicin) resistance and XDR pattern was not observed. Overall frequency of RIF resistance was 16.4% (9/55) and INH was 25% (12/48) with low level INH resistance in 2 and high in 10. Among second line drugs, prevalence of FQ resistance was more than SLID resistance and within FQ, levofloxacin resistance was more frequent than moxifloxacin. MGIT had positive growth in 16/59 samples, out of which 1 sample was positive for nontuberculous mycobacteria (M.chelonae) but on genotypic testing demonstrated MTB resistant to RIF and FQ. Conclusion: First report on drug resistance pattern in culture positive/negative cases. 25.49% primary drug resistance is serious observation necessitating changed strategies for our goals of TB elimination. INH resistance is more than RIF with isolated RIF resistance unreported.
1968
A202: Clinical outcomes of primary lumbar fusion patients who were culture positive
Philip Paschal 1 , Gregory Paschal 1 , Tucker Callanan 1 , Celeste Abjornson 1 , Andrew Sama 1 , Federico Girardi 1 , Darren Lebl 1 , and Frank Cammisa 1
1 Spine, Hospital for Special Surgery, New York, United States
Introduction: Occult bacteria have been linked to deep and chronic infections in spine surgery. These organisms are commensal to dermal and deeper tissue layers, including the intervertebral disc and bone. We hypothesize that standard surgical skin preparation nor preoperative antibiotics properly access and eradicate these organisms prior to primary spine surgery. These organisms can potentially adhere to the biofilm surrounding the hardware and limit bone formation. Aims/Objectives: To determine the colonization rate of occult bacteria in the superficial and deep tissue layers of healthy patients undergoing primary instrumented lumbar spine surgery. Methods: This prospective, consecutive cohort of fifty-four patients undergoing primary lumbar spine surgery at a single tertiary center. All patients met the inclusion/exclusion criteria which included between the ages of 18 and 80, undergoing a posterior approach with pedicle screw instrumentation with no evidence of a prior or current fracture, trauma, tumor, or an active systemic or local infection. Patients were also excluded if they were immunosuppressed or had received prior surgery at any lumbar level with hardware. All patients received preoperative antibiotics and skin preparation. Culture samples were subsequently obtained from the superficial skin, dermal wound-edge following incision, hypodermis, and the vertebral pedicle prior to instrumentation implantation. Control culture samples were taken from scalpel, tap, and suction prior to incision. The primary outcome was the rate of positive culture samples from the various layers traversed during standard surgical spine exposure. Clinical outcomes of fusion status and revision rate were collected. This study was approved by our institutional review board and ethics review panel. Results: A total of 525 culture samples were obtained, and samples were positive in 33.3% of patients (18/54). Culture-positive patients had on average 3.1 positive samples per case. Superficial skin samples were positive in 13.0% (n = 7), dermal layer samples in 16.7% (n = 9), hypodermis samples in 13.0% (n = 7), and vertebral samples in 20.4% (n = 11) of cases. All control samples taken were culture-negative. C. acnes was the most common organism isolated, in 83.3% of culture-positive cases. Significantly more males were culture-positive than females. Patients with positive cultures were treated with antibiotics. At one year post-op, patients in culture-positive group had similar fusion rates to culture-negative groups. However, delayed fusion was observed at a higher rate in the culture-positive group. Conclusions: Occult bacteria was detected in one third of patients undergoing primary instrumented posterior spine surgery. Deep culture samples of the vertebral pedicle were more often positive than dermal layer samples. The data collected supports our hypothesis that occult bacteria persist in the skin and deeper tissue layers regardless of the efforts made by preoperative skin preparation and prophylactic antibiotics. The clinical sequela for culture-positive patients, although addressed perioperatively, was a higher incidence of delayed fusion.
1807
A203: The role of silicate substituted calcium phosphate (Ca-SiP) in fusion in spinal infections: a prospective study
Mandar Borde 1 , K Venugopal Menon 1 , Akash Mane 1 , and Sangram Rajale 1
1 Spine Surgery, Bharati Vidyapeeth (deemed to be University) Medical College and Hospital, Pune, India
Introduction: Instability secondary to spinal infections frequently warrants stabilization with or without reconstruction of the spinal column. Fusion procedures with pedicular screws have revolutionized the field of spine surgery. The endpoint of spinal infections, usually, is fusion of the affected segments but debridement of the infective tissue with fusion using bone graft or interbody spacers is the standard practice. The significant cavity remaining after debridement needs filling up with bone graft. Iliac crest bone graft has been the universal source, but autograft harvesting can be associated with significant morbidity and complications. Bioactive ceramics have been used as bone graft substitutes and volume expanders to enhance bone fusion rates since a long time. These ceramics are usually used as a mixture with autologous bone graft or with laminectomy and spinous process bone. Material and Methods: Between January 2020 and January 2021, 20 patients with spinal instability secondary to infection underwent debridement, spinal instrumentation and fusion using autologous bone graft from the laminae and spinous processes and silicate- substituted Calcium Phosphate (Ca-SiP) granules mixed in equal volumes. In cases with suspicion of pyogenic infection, 1 gram Vancomycin was added to the graft and in cases where Tuberculosis was suspected, one gram Streptomycin was added to the mixture. In cases involving the lumbosacral region, cancellous bone graft from the posterior superior iliac spine was used with ceramic granules. Eleven males and nine females constituted the study population with their age ranges being 6 to 70 years. The lumbosacral junction involvement was seen in 3 patients, lumbar spine was affected in 10 patients, 3 patients had dorsolumbar junction involvement while the dorsal spine was involved in 4 patients. The organism isolated was Mycobacterium tuberculosis in 11 patients, Methicillin Sensitive Staphylococcus aureus in 5 patients, Klebsiella pneumoniae in 1 patient, Burkholderia pseudomallei in 1 patient and 2 patients had mixed infections with Klebsiella pneumoniae and Mycobacterium tuberculosis. All patients were put on appropriate antibiotic therapy according to the culture and sensitivity reports. Results: Clinical and radiological evaluation of all the patients was done at 6 weeks, 3 months, 6 months, and 12 months after the surgery. 19 patients showed significant improvement in their clinical symptoms and showed radiographic evidence of solid bony fusion between 6-9 months. The patient with Burkholderia infection progressed to fulminant septicemia with multiorgan failure and succumbed to the infection. The mean Visual Analogue Score (VAS) at the end of 1-year was 2. Radiological assessment involved anteroposterior and lateral radiographs. Conclusion: Silicate- substituted Calcium Phosphate, when used in equal volumes with autologous bone graft, demonstrates good fusion at the affected segments and can act as an efficient volume expander especially in cases with paucity of bone graft. The granules can be easily sterilized in an autoclave and reused with equal efficiency and are cost effective as compared to other bone substitutes; addition of antibiotics helps in increasing the local concentration of the drugs; its disadvantages being the lack of osteoinduction and the expertise needed to manufacture the same.
595
A204: Extensive thoracic and lumbar spine actinomycetes in an immunocompetent patient causing paraparesis -A case report
Rohan Parihar 1 , Samir Dalvie 1 , Kshitij Chaudhary 1 , Sourav Chatterjee 1 , Pramod NK 1 , and R . Dileepan Chakrawarthi 1
1 Spine, P.D. Hinduja Hospital, Mumbai, India
Introduction: Actinomyces, Gram + commensal bacteria. Immunocompromised patients any organ can be involved, this infection is extremely rare in immunocompetent individuals. Spinal cord compression with neurological deficit is rarer. We report one such case with extensive actinomycosis of the entire thoracic and lumbar spine who presented with paraparesis. Case Report: A case of 35/F with symptoms of bilateral lower limb weakness with difficulty in walking since 4 months associated with multiple discharging sinuses at back. Patient first noticed swelling in back associated with discharge 10 years back for which I&D was done following which she was asymptomatic for past 7 years. Later another I & D was done 3 years later because of recurrence of symptoms. After this intervention also, patient developed another swelling associated with multiple discharging sinuses, after which she referred to a tertiary care hospital. Culture from sinuses came positive for Actinomycetoma. Amoxycillin, doxycyclin, septran, ceftriaxone was tried without success. Because patient developed bilateral weakness in the lower limbs, T3-T9 decompression was done and the intraoperative specimen was sent for bacterial, fungal, mycobacterial cultures, histopathology. Actinomyces colonies were identified in culture and HPE showed Typical filamentous bacteria. Post operatively, patient was given three cycles of injection amikacin, with oral Cotrimoxazole and Rifampicin for 3 months (modified Welsh regimen). Postoperatively, the surgical wound healed well. Sinuses healed after 3 months. The patient's bilateral lower-extremity motor strength improved slowly in 1 year and at the final follow up is walking unsupported. Patient continues to be on chronic suppressive antibiotics (augmentin and rifampicin). Conclusion: Spinal Actinomycosis with diffuse involvement of thoracic and lumbar spine is extremely rare in an immunocompetent patient. We present the treatment for one such patient who has been successfully treated for neurological deficit and is on chronic suppressive antibiotics for this indolent infection.
1794
A205: Spinal tuberculosis: controversies of treatment modalities, experience of 774 patients
Shah Alam 1 , Sarwar Jahan 2 , Dr Sharif Ahmed Jonayed 2 , and Abdullah Al Mamun 2
1 Orthopedics & Spine, Bangladesh Spine & Orthopedic Hospital (BSOH), Dhaka, Bangladesh
2 Orthopedics & Spine, National Institute of Traumatology & Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
Introduction: Tuberculosis of the spine is a common form of TB infection for 50% to 60% of osseous tuberculosis. Although uncommon, spinal TB still occurs in both developed and developing countries. The diagnosis of spinal tuberculosis is difficult and it commonly presents at an advanced stage. Delays in establishing diagnosis and management result in complications such as spinal cord compression and spinal deformity. Material and Methods: Total of 774 patients with tuberculosis of the cervical, thoracic and lumbar spine with moderate to severe cord compression were studied. Variable degrees of neurological deficit with deformity were treated from January 2003 to July 2022. Thoracotomy along with anterolateral decompression and autogenous strut bone grafting with simultaneous fixation by screws and rods were done in 81 cases. Posterior decompression, posterior interbody and posterolateral fusion by bone graft with stabilization by transpedicular screws and rods were done in 608 cases, whereas 85 cases of cervical tuberculosis were operated by either anterior approach or both anterior and posterior approaches. Appropriate anti TB drugs were given to all patients for 12-18 months. The follow-up period was 3 months to 10 years. Results: The average age was 47 (9-85) years. All patients survived surgery. There were 10 cases of superficial infections (1.3%) whilst there were 5 cases (0.65%) of deep infections. Revision surgery was performed in 15 patients (1.94%). Implant failure occurred in 21 cases (2.7%) whilst malposition of screws occurred in 26 cases (3.4%). Perioperative excessive bleeding complications were reported for 5 patients (0.6%). Neurological improvement occurred in all patients except for 19 cases (2.5%). Preoperatively, the majority of patients (n = 287, 37%) were classified with Class B on the American Spinal Injury Association (ASIA) neurological impairment scale. This was significantly reduced postoperatively to 0.3%. Conclusion: For patients with spinal tuberculosis anterior debridement, autograft bone fusion, anterior or posterior fixation appears to be effective in arresting disease, correcting kyphotic deformity and maintaining correction until solid spinal fusion.
1037
A206: Implant selection in cervical spondylodiscitis does not alter the outcome - a single-center experience of a case series of 24 patients
Stefan Motov 1 , Bastian Stemmer 1 , Krauss Philipp 1 , Bonk Maximilian-Niklas 1 , Christina Wolfert 1 , Steininger Kathrin 1 , Björn Sommer 1 , and Ehab Shiban 1
1 Neurosurgery, Universitätsklinikum Augsburg, Augsburg, Germany
Introduction: Cervical spondylodiscitis is an uncommon entity, with an incidence of 0.5 to 2.5 per 100,000 population, but it is potentially hazardous. This type of vertebral and discogenic infection might cause the highest rate of neurological impairment, and poses a high threat for permanent clinical damage. Radical surgical debridement of the infected segment with fusion and intravenous antibiotic therapy remain the gold standard in most spine centers. Material and Methods: In this study, we retrospectively included all patients suffering from cervical spondylodiscitis between 01/2017 and 05/2022, treated at the university hospital of Augsburg. Clinical and radiological parameters were evaluated. Descriptive statistics were performed using SPSS, and relevant correlations were examined using the t-test for independent samples and the Chi-square test. Results: 24 patients were identified. 17 patients (71%) suffered from sepsis on admission, 17 patients (71%) were diagnosed with epidural abscess on primary imaging and 5 patients (21%) had more than one discitis focus in a distant spinal segment. The presence of epidural abscess was significantly associated with systemic sepsis (p = 0.03) and myelopathy symptoms (p = 0.00). Septic status was significantly associated with the occurrence of discitis in other segments (p = 0.02), higher CCI (p = 0.03) and Clavien Dindo scores (p = 0.01), as well as a longer ICU stay (p = 0.04) and the occurrence of nonunion (p = 0.06). Sixteen patients (67%) underwent an anterior approach only, five patients (21%) underwent a combined anterior and posterior surgery and only one patient (4%) a posterior surgery alone. Two patients (8%) denied surgical treatment. A total of six patients (25%) died after a median of 20 days despite antibiogram-accurate therapy. The follow-up data of 19 patients (79%) was available with the evidence of permanent neurological damage e.g. radiculopathy, myelopathy, or complete sensorimotor cross-section in 9 patients (38%).The type of osteosynthesis (anterior plating, intersomatic cage, expandable vertebral body cage or combined anterior plating and posterior cervical lateral mass and thoracic pedicle screw-rod osteosynthesis) was not significantly associated with subsidence (p = 0.13), nonunion (p = 0.21) or revision surgery (p = 0.20) in our cohort. However the extent of stabilization correlated significantly with the rate of nonunion (p = 0.05). Conclusion: Cervical spondylodiscitis presents a severe infectious disease that occurs in multimorbid elderly patients and, despite adequate surgical and antibiotic treatment, is often associated with permanent neurological damage and a fatal outcome. Implant selection is irrelevant for the overall surgical and clinical outcome.
1951
A207: Polymicrobial hematogenous vertebral osteomyelitis. incidence, risk factors and outcome
Hamdan Abdelrahman 1,2 , Mootaz Shousha 3 , and Heinrich Boehm 3
1 Orthopedics and Trauma, Asiut University Hospitals, Egypt
2 Helios-Hospitals Erfurt, Germany
3 Zentralklinik Bad Berka, Germany
Introduction: Haematogenous vertebral osteomyelitis (VO) is primarily monomicrobial. The incidence of polymicrobic form is underestimated. In the past, tuberculosis infection was the major cause of spinal infections (SI). Nowadays, the majority of VO is bacterial. The described incidence of polymicrobial SI is variable ranging (0%-10.8%) and is most likely to result from contiguous spread. Patients and Methods: Retrospective analysis of the prospectively collected data of 600 patients with SI (2005- 2015). The aim of this study is to identify the incidence, risk factors and outcomes of such form of SI caused by more than one organism isolated from the infected site with mean follow up (FU) of 24.8 months. Results: A causative organism could be identified from the site of infection in 405 patients (67.5%); commonly one organism in 378 patients (93.3%). In 27 individuals (6.7%), more than one pathogen could be identified. Fifteen males and 12 females with mean age of 66.8 ± 10.26 years (47-82). The intraoperative swabs revealed pyogenic infection in 21 patients and one individual with mixed pyogenic and fungal infection. Histopathological examination in the other 5 patients revealed tuberculous granuloma, however causative bacteria could be isolated through the microbiological tests (superimposed infection). Staph. aureus was the commonest isolate in 15 patients (55.6%). ASA-Score Class III&IV was found in (74%). The commonest comorbidities were cardiac in 18 patients, DM in 17 (p-value 0.004*), other site of infection in 22 (p-value 0.003*) and peripheral vascular insufficiency in 13 cases. Neurological deficit occurred in 16 patients (59%), fever in 12 cases. Lumbar spine was the commonest region affected in 15 patients (56%). Non-contiguous infection was found in 4 patients (14.8%), epidural abscess in 16 (59%) and psoas abscess in 7 individuals. The mean preop. CRP was 85.8 ± 71.98 (12.3 ± 14.90 at last FU), ESR of 83.98 ± 34.26 (45.5 ± 36.59 at FU) and WBC of 10 ± 3.72 (7.0 ± 2.61 at FU). Ventrodorsal approach was necessary in 21 patients, 13 had minimal invasive surgery. Four patients had to be re-operated due to recurrent infection in 3 cases (11%) and one patient for adjacent fracture. Three patients died with septic shock (in-hospital mortality of 11%). The neurological improvement rate of at least one ASIA-grade was 75%. The mean preop. VAS was 8 ± 0.84 and reduced to 3 ± 1.38 at last FU. The postop. Antibiotic therapy had to be taken more than 8 weeks in 22 patients, antituberculous treatment more than 6 months and in 16 cases a combination of antibiotics was necessary. Conclusion: Polymicrobial VO, occurred at least in 6.7% and must be considered when treating multimorbid patients with DM and other sites of infection. The frequency of isolation of multiple bacterial species is in large part dependant on the process of specimen collection and laboratory culturing techniques employed. Minimal invasive surgeries and combinations of antibiotics may be favourable in management of such cases.
OP24: Outcomes in Spine Tumor Patients
877
A208: Application of the NSE score (neurology-stability-epidural compression assessment) to establish the need for surgery in spinal metastases of elderly patients: a multicenter investigation
Fabio Cofano 1,2 , giuseppe di perna 1,3 , Marco Bozzaro 2 , Salvatore Petrone 2 , Lucio Buffoni 4 , Serena Badellino 5 , Fulvio Tartara 6 , Nicola Marengo 7 , Marco Ajello 7 , francesco zenga 7 , Daniele Armocida 8 , Alessandro Pesce 9 , Alessandro Frati 8 , Roberto Altieri 10 , Giuseppe Barbagallo 10 , and Diego Garbossa 1
1 Neuroscience, University of Turin, Turin, Italy
2 Humanitas Gradenigo Hospital, Italy
3 Spine Surgery Unit, Casa di Cura Città di Bra, Spine Surgery Unit, Italy
4 Oncology, Humanitas Gradenigo Hospital, Italy
5 Radiotherapy, Città della Salute e della Scienza, Italy
6 Neurosurgery, Istituto Clinico Città Studi, Italy
7 Neurosurgery, Città della Salute e della Scienza, Italy
8 Neurosurgery, Sapienza University of Rome, Italy
9 Neurosurgery, Santa Maria Goretti Hospital, Latina, Italy
10 Neurosurgery, University of Catania, Catania, Italy
Objective: Management of spinal metastases has evolved in the last decades with the development of new oncological strategies and technologies. New concepts of Separation Surgery, Minimally-invasive fixation techniques and radiosurgery changed the paradigm of treatment. The Neurology-Stability-Epidural compression score (NSE) was developed few years ago in order to promote the use of a practical tool to establish the need for surgery in spinal metastases according to available evidence. The aim of this study was to confirm the reliability in the elderly of the NSE score after a multidisciplinary multicenter evaluation. Patients and Methods: A total number of 5 Hospitals were included for the evaluation. Elderly patients (>70 years old) were analyzed according to the inclusion/exclusion criteria of the score which was developed by the main author of this investigation. Three main items were confirmed for the analysis: Neurological status (0-5 points), Stability of the spine according to the Spinal Instability Neoplastic Score (SINS) Score (0-5 points), and Epidural compression according to the Epidural Spinal Cord Compression (ESCC) scale (0-3 points). Patients were considered suitable for surgery with ASA score < 4 and ECOG score < 3. A retrospective clinical validation of the NSE score was made on patients that underwent surgical or non surgical treatment. Results: A total number of 102 patients was analyzed. Agreement between the undertaken treatment and the score (85.3% of patients), resulted in a strong association with improvement or preservation of clinical status (neurological functions and mechanical pain) (p < 0.001) at 3 and 6 months. In the non-agreement group no association was recorded at the 3 and 6 months follow-up (p 0.486 and 0.343 for neurological functions, 0.063 and 0.858 for mechanical pain). The score appeared to be reliable also for patients with more than 75 years old. Conclusion: Functional outcomes of the study group showed that the proposed NSE score represent a practical and reliable tool to establish the need for surgery also for elderly patients. Agreement between the score and the performed treatments resulted in better clinical outcomes, when compared with patients without agreement.
1433
A209: Significantly prolonged hospital stay and increased incidence of postoperative neck or back pain, radiculopathy, and poorer physical quality outcomes in primary intradural spinal cord tumor patients with unhealthy baseline metabolic status: a prospective, propensity score matched analysis
Nicholas Van Halm-Lutterodt 1,2,3 , Krishna Mandalia 4 , Nicholas Storlie 5 , Chenlong Yang 6 , Ziyang Ye 3,7 , Mohamed Mesregah 8 , Josh Gonzalez 3 , Andrew Mecum 9 , Wei-Hsun Huang 1 , Wei-Cheng Chen 1 , Roberta Kungulli 10 , Mercy Bartels-Mensah 11 , Wenju Jiang 1 , Yu Wang 1 , Sunny Kim 3 , and Yulun Xu 1
1 Department of Neurosurgery, Beijing Tiantan Hospital, Beijing, China
2 Department of Professional Studies and Public Health, Brown University, Providence, United States
3 Department of Orthopedics and Neurosurgery, Inspired Spine Health, Burnsville, United States
4 Orthopedic Surgery, Tufts University School of Medicine, Boston, United States
5 School of Medicine, Creighton University School of Medicine, United States
6 Department of Orthopedics and Neurosurgery, Peking University, Beijing, China
7 Department of Data Science and Analytics, University of Chicago, Chicago, United States
8 Department of Orthopaedic Surgery, Menoufia University, Menoufia, Egypt
9 School of Medicine, University of Colorado Anschutz School of Medicine, Aurora, United States
10 School of Medicine, Capital Medical University,Beijing, China
11 University of Debrecen, Debrecen School of Medicine, Debrecen, Hungary
Background: In spine patients, sometimes neurological symptoms refractorily persist even following various treatments with or without surgery. It becomes difficult to assess whether this sequela is due to these treatments or other patient factors. An unhealthy metabolic phenotype (MU) has been extensively researched in cardiometabolic specialty areas but little to no information has been documented in the spine literature on this premise. Having an MU status at baseline can negatively impact perioperative clinical and neurological outcomes (pain, radiculopathy and/or myelopathy) in spine patients. Materials and Methods: Following Institutional Review Board (IRB) of Beijing Tiantan Hospital approval, we prospectively obtained patient data from January 2017 through December 2017. The study design included: adult patients who were diagnosed with primary intradural spinal cord tumors (ID-SCTs) and underwent tumor resection surgery as primary treatment. The ID-SCT patients who had ≥2 items of the following four metabolic criteria were considered metabolically unhealthy (MU_ID-SCT) while those with <2 of the criteria were considered metabolically healthy (MH_ID-SCT): (i) high fasting blood glucose level (≥5.6 mmol/L or ≥100.8 mg/dL) or on diabetic medications (oral or intravenous), (ii) low high density lipoprotein cholesterol (HDL-c), (<1.04 mmol/L or <40.56 mg/dL for male patients and (<1.29 mmol/L or <50.31 mg/dL for female patients), (iii) elevated systolic blood pressure (≥130 mmHg) or diastolic blood pressure (≥ 85 mmHg) or on anti-hypertensive drugs and (iv) high serum triglyceride (TG) level (≥1.7 mmol/L or ≥150.44 mg/dL) or on lipid-lowering drugs. Baseline and 2-year postoperative neurological outcomes were analyzed by t-tests following Python-based ‘age and sex’ propensity score matching (PSM) of the [MH_ID-SCT] and [MU_ID-SCT] patients. Significance was set at p < 0.05. Results: Overall, 126 patients with ID-SCTs were matched in this study, [MH_ID-SCT]; n = 63 (50.0%) and [MU_ID-SCT]; n = 63 (50.0%) patients, respectively. The overall average age was 53.57 years and the average body mass index (BMI) of patients in [MH_ID-SCT] and [MU_ID-SCT] groups were (23.87 ± 3.41) and (25.44 ± 2.56) kg/m2, respectively, (p < 0.01). Baseline physical activity, serum metabolic-panel, neck, or back pain incidence, mean operative time, and hospital length of stay (HLoS) significantly showed negative outcomes for [MU_ID-SCT] patient group, (p < 0.05). At 2-year postoperative, the incidence of radiculopathy (34.92% in MH vs 65.08% in MU), McCormick’s classification grading, Role Physical (RP) and Physical Component Summary (PCS) of Short_Form-36 (SF-36) scores, were significantly inferior in the [MU_ID-SCT] patient group, (p < 0.05). No significance was observed for WHO tumor grading, (p > 0.05). Conclusion: Our study shows that MU status at baseline is associated with increased BMI, decreased physical activity and higher 2-year postoperative incidences of radiculopathy and neck or back pain, and inferior-physical function. It is clearly articulated in this study that an MU status is a notable culprit in postoperative poorer long-term neurological morbidity and lengthened HLoS. Future studies can delineate the impact(s) of metabolic aberration status across the different spectrums of spine pathologies to elucidate the value-based approaches to triage steps for quality improvement in spine patients while shortening HLoS.
1146
A210: Temporal validation of the SORG 90-day and 1-year machine learning algorithms for survival of patients with spinal metastatic disease
Hester Zijlstra 1,2,3,4 , Harmen Kuijten 1,2 , Anirudh Bhimavarapu 1 , Olivier Q. Groot 1,2 , Aditya Karhade 1 , Diyar Delawi 3 , Diederik Kempen 4 , Jorrit-Jan Verlaan 2 , and Joseph Schwab 1
1 Orthopedic Surgery, Massachusetts General Hospital, Harvard Medical School, Boston, United States
2 Orthopedic Surgery, University Medical Center Utrecht, Utrecht, The Netherlands
3 Orthopedic Surgery, St. Antonius Hospital, Nieuwegein, The Netherlands
4 Orthopedic Surgery, OLVG Amsterdam, Amsterdam, The Netherlands
Introduction: Since 2004, the incidence of spinal metastasis diagnoses has increased each year. The Skeletal Oncology Research Group machine learning algorithm (SORG-MLA) algorithm was developed for preoperative survival prediction of patients with spinal metastatic disease using 732 patients that received surgical treatment between 2000 and 2016. Because of the ever-changing treatment modalities and potential for diminished performance of the algorithms in current and future patient groups, there is a need for a temporal validation with a contemporary patient population. Materials and Methods: This retrospective validation study was conducted to assess survival and validate the SORG-MLA on patients that received surgical treatment for spinal metastases between January 2017 and - July 2021 in a tertiary center in the United States. Variables needed for the SORG-MLA were manually collected from electronic medical records. These included 18 variables including primary tumor, Eastern Cooperative Oncology Group (ECOG) Performance Status Scale, American Spinal Injury Association (ASIA) Impairment Scale, and laboratory values. Performance of the SORG-MLA on the validation cohort was assessed with calibration (calibration plot, intercept, and slope), discrimination (area under the receiver operating characteristic curve), overall performance (Brier score compared to the null-model Brier score), and decision curve analysis. Results: A total of 518 patients were included. Among them, 122 (23%) died within 90-days and 262 (48%) died within one year. The validation cohort differed significantly from the development cohort with older age, more slower and moderate growth tumors, more normal ASIA scores, less Charlson comorbidities, more visceral and brain metastases, and less presence of three or more spinal metastases, lower white blood cell, platelet, and absolute neutrophil count, and higher creatinine levels. Despite these differences, the SORG-MLA continued to perform well on calibration, discrimination (AUC 0.81 [95% confidence interval (CI), 0.72 - 0.88] for 90-day mortality, AUC 0.75 [95% CI, 0.67 - 0.81] for 1-year mortality), Brier score, and decision curve analyses. Conclusions: The SORG-MLA for survival in spinal metastatic disease performed well on temporal validation. Surprisingly, the model retained its performance despite recent advances in the treatment of spinal metastases such as immunotherapy, targeted therapy, and improvements in radiotherapy and surgery. Updating of the model using this contemporary patient cohort could further improve performance for patients treated with more modern treatment modalities. The updated model can then be used in prospective, multi-center trials to prospectively validate the model.
1149
A211: Survivorship prediction in spinal oncology patients by oncologists is reliable: data from a quaternery metastatic spinal cord compression MDT
Kofi Cox 1 , Hassam Ahmed 1 , Priyanshu Saha 1 , Zion Hwang 1 , Emily Tsang 1 , Wing-kin Liu 2 , Mehran Afshar 2 , Erlick Pereira 3 , Thamer Hamdan 3 , Bisola Ajayi 3 , Tesfaladet Kurban 3 , Mohamed Abdalla 3 , Ursalan Khan 3 , Varinder Alg 3 , Timothy Bishop 3 , Jason Bernard 3 , Dimitrios Teslios 3 , and Darren Lui 3
1 St. George's, University of London, London, United Kingdom
2 Department of Oncology, St. George's Hospital, London, United Kingdom
3 Atkinson Morley Wing, Department of Complex Neurosurgery, St. George's Hospital, London, United Kingdom
Introduction: Metastatic spinal cord compression (MSCC) is a debilitating condition, and the secondmost common neurological complication of cancer. Numerous studies have shown clinical outcomes are related to timing and type of treatment. The use of prognostic scoring systems, such as the revised Tokuhashi, Bauer and Tomita scores, are popular and are used commonly to help guide treatment. However, these scoring systems and algorithms have been criticized because of their lack of specificity to any one cancer type as well as their lack of accommodation for the survival benefits conferred by contemporary systemic therapy options. Indeed, advances in the genetic profiling of cancers and the development of increasingly effective systemic therapy options have, in some cases, dramatically changed the prognosis of certain cancers. For example, certain lung cancers traditionally thought to have carried a poor prognosis can, with the correct genetic profile, now have curative chemotherapy. Bilsky developed the Neurological, Oncological, Mechanical and Systemic (NOMS) framework which aims to be a timeless utility as opposed to algorithms or scores which are intrinsically disadvantaged by advances in medicine that cannot be reflected in the scores. Now more than ever we rely on the oncologists to predict prognosis, yet little data exists assessing the accuracy of the prognostic estimates provided by referring oncologists. We analyzed patients referred to our supra-regional multidisciplinary team for management of MSCC to assess accuracy of the oncologist-given prognosis versus actual survival outcomes. Material and Methods: Retrospective data, captured between January 2015 and December 2018, was reviewed for 1,572 patients referred with MSCC and 829 patients were included in the study. We compared Group 1 (patient prognosis assigned as <6 months survival) versus Group 2 (patient prognosis assigned as >6 months survival). Median overall survival (mOS) and hazard ratio for death (HR) was assessed. Receiver operator curve (ROC) analysis was performed to assess the accuracy of the oncologist’s prognosis. Results: mOS in Group 1 was 5.8 months (95% CI 4.2-7.4 m), and in Group 2 mOS was notreached. Log rank test gave a Chi 2 of 131 (p < 0.001). Cox regression analysis revealed a HR of 0.30 (p < 0.001). Area under the ROC curve was 78%. Conclusion: Prognosis given by oncologists as part of the multidisciplinary team is accurate for this cohort of unselected, consecutive ‘real world’ patients. Given the rapid progress in the management of malignant disease and the associated improvements in survival times, the oncologist’s prognostic estimate is integral in informing patient management and is likely more accurate than outdated scoring systems. The accurate prognosis provided by oncologists is crucial in guiding the optimal treatment of MSCC, enabling a higher quality of life for patients. Therefore, the importance of the oncologist-given prognosis should be reflected in both national and international guidelines pertaining to the management of patients with MSCC.
968
A212: Development of the Patient Expectations in Spine Oncology (PEPSO) Questionnaire
Anne Versteeg 1 , Roxanne Gal 2 , Raphaële Charest-Morin 3 , Jorrit-Jan Verlaan 2 , Charles Fisher 3 , and Lenny Verkooijen 2
1 Department of Orthopaedics, University of Toronto, Canada
2 University Medical Center Utrecht, The Netherlands
3 Vancouver General Hospital/ University of British Columbia, Canada
Introduction: Surgery and radiation therapy have shown to be effective treatments to improve pain and health related quality of life (HRQOL) in patients with spinal metastatic disease. Yet, a significant portion of the patients report dissatisfaction with the outcomes of their treatment. It is thought that a discrepancy between pre-treatment expectations and perceived outcomes of treatment is a significant source of dissatisfaction. Currently, no clinical tools exist to assess patient expectations in patients undergoing treatment for spinal metastases. The purpose of this study was therefore to develop a questionnaire to evaluate patient expectations in patients with spinal metastatic disease. Material and Methods: The new PEPSO questionnaire was developed through an international quality study. The study was conducted in 3 phases. In the first phase, semi-structured interviews were conducted with patients with spinal metastatic disease, patient relatives and physicians involved in the care of patients with spinal metastatic disease. In the second phase, the interviews were analyzed and a preliminary version of the questionnaire was developed with an extensive item pool. In phase 3, the preliminary version of the questionnaire was tested for language, content and structure with a select group of patients. Results: A total of 22 items were retained in the final version of the new PEPSO questionnaire. The questionnaire is divided in three sections. Section A covers the patient expectations regarding the outcomes of surgery and/or radiation therapy including physical functioning, pain and social activities; and requirements of analgesia. Section B covers expectations regarding goals of treatment and life expectancy. Section C covers patient understanding of the consultation with the physician. Conclusion: The new Patient Expectations in Spine Oncology (PEPSO) questionnaire was developed to evaluate patient expectations regarding the outcomes following treatment for spinal metastases. This new questionnaire will allow physicians to systematically assess patient expectations and will help physicians to counsel patients towards realistic patient expectations. A follow-up study is planned to further evaluate the reliability and construct validity of the questionnaire.
716
A213: Survival trends of spine metastasis surgery from 2008 to 2021 - NTU Spine Tumor Registry
Fon-Yih Tsuang 1,2
1 Spine Tumor Center
2 Division of Neurosurgery, Department of Surgery, National Taiwan University Hospital, Taipei City, Taiwan
Introduction: The advances in systemic therapy have increased the overall survival of advanced cancer patients, and the survivals of patients receiving surgery for metastasis spinal disease. However, the primary cancer entity of spine metastasis is different between countries. We are reporting the first large spine metastasis surgery registry of Asian populations. Material and Methods: Data were obtained from the spine tumor registry of single tertiary referral center in Taiwan, and 990 patients were included for analysis. Patient having surgery between 2017/01/01 and 2021/12/31 were recorded prospectively, but patients between 2008/01/01 and 2016/12/31 were recorded retrospectively. The patient’s death date was obtained from National Health Insurance Database. The primary outcomes are overall survivals. the survival curves of time to death were estimated by the Kaplan-Meier method. In univariate analysis, the unadjusted effect of each potential risk factor, prognostic factor, or predictor of the binary outcome, dead vs. alive, and the survival outcome of time to death, was examined using the Wilcoxon rank-sum test, Chi-squared test, and log-rank test, as appropriate for the data type. Next, multivariate analysis was performed by fitting Cox’s proportional hazards models with time-dependent covariates (called the ‘Cox model’ for simplicity) to estimate the adjusted effects of risk factors, prognostic factors, and predictors on the time-to-death hazard rate. Results: Patient with lung, liver, and breast cancer are the most common cancer requiring spine metastasis surgery, and all of them experience a significant improvement in survival over time. In multivariate analysis, surgery later than 2017, patients younger than 39 year-old, synchronous spine metastasis, Frankel E while metastasis, multidisciplinary spine tumor team, en bloc spondylectomy, time-dependent variables Frankel E and D, are correlated with better overall survival. Cervical cancer, skin cancer, gall bladder cancer, shorter time between primary cancer and metastasis diagnosis, higher Tomita score, and Tokuhashi Scores no more than 8, are correlated with worse prognosis. Conclusion: The survivorship dramatically improved over past decades due to molecular makers, and application of target therapy and immunotherapy. Multidisciplinary spine tumor team is crucial for the comprehensive evaluation of the spine metastasis patients, especially the prognosis evaluation, including the surgical risks and benefits.
523
A214: Spinal metastasis in multiple primary malignancies involving lung cancer: clinical characteristics and survival
Van Tri Truong 1,2 , Fidaa Al-Shakfa 1 , Nicholas Newman 1 , David Roberge 3 , Giuseppina Laura Masucci 3 , Thi Phuoc Yen Tran 4 , Ghassan Boubez 1 , Daniel Shedid 5 , Sung-Joo Yuh 5 , and Zhi Wang 1
1 Orthopedic Surgery, Centre Hospitalier de l'Universite de Montreal, Montreal, Canada
2 Neurosurgery, Vinmec Central Park International Hospital, Vinmec Healthcare System, Ho Chi Minh City, Viet Nam
3 Radiology and Oncology
4 Research Center
5 Neurosurgery, Centre Hospitalier de l'Université de Montréal (CHUM), University of Montreal, Montreal, Canada
Introduction: The incidence of multiple primary malignancies (MPM) has increased in recent decades. Our aim was to evaluate the incidence, clinical features, and survival in cases of spinal metastases from MPM where one of the malignancies is lung cancer. Material and Methods: We retrospectively reviewed an institutional database of lung cancer patients with spinal metastasis and extracted all cases of MPM. Results: Among 275 patients who had spinal metastasis with lung cancer as one of the diagnoses, 21 (7.6%) patients with MPM were identified. The mean age was 68.5 (95% CI 65.3-71.7) years old. The most common cancers diagnosed in addition to the lung cancer were breast cancer (5 patients, 24%), upper aerodigestive tract cancer (4 patients, 19%), and prostate cancer (4 patients, 19%). Eighteen (86%) patients walked independently, and 3 (14%) patients walked with help. Seventeen (80.9%) patients had a good Karnofsky Performance Scale. The median survivals from the date of the first cancer diagnosis, the last cancer diagnosis, and the spinal metastasis diagnosis were 109.8 (95% CI 23.5-196.1 months), 17.8 (95% CI 5.8- 29.8 months), and 10.3 (95% CI 5.4- 15.2 months), respectively. The actual rates of survival at 6 months, 12 months, and 24 months from the date of spinal metastasis diagnosis were 81%, 42.9%, and 23.8%, respectively. Conclusion: The present study is the first series showing survival of spine metastatic patients with MPM involving lung cancer is not clearly inferior to that of spinal metastasis patients with lung cancer alone.
659
A215: The 5-item Modified Frailty Index is a better predictor of outcomes compared to age and revised cardiac risk index following transpedicular decompression and fusion for metastatic epidural spinal cord compression
Rohit Mauria 1 , Manish Kasliwal 1 , Collin Labak 1 , Eric Herring 1 , Olindi Wijesekera 1 , Mohit Patel 1 , Adel Azghadi 1 , and Pranav Kumar 2
1 Department of Neurosurgery, University Hospitals Cleveland Medical Center, Cleveland, United States
2 Case Western University School of Medicine, Cleveland, United States
Introduction: Patients with thoracic metastatic epidural spinal cord compression (MESCC) undergo large surgeries to obtain spinal cord decompression and avoid functional decline. These patients are often prone to postoperative complications due to their preexisting disease burden and comorbidities. Scales such as Revised Cardiac Risk Index (RCRI) are used as a component of preoperative surgical risk stratification to minimize patient morbidity and mortality after surgery, though with little evidence to support it. As predictive models for surgical outcomes have become increasingly important, the 5-item Modified Frailty Index (mFI-5) has been shown to be a predictor for postoperative complications for those having degenerative spine surgery. However, there is little evidence behind the application of this scoring system in a cohort of surgical patients with high Bilsky scores. This study evaluates the utility of the MFI-5 as a predictor for outcomes following transpedicular decompression and fusion for high grade MECSS. Methods: A retrospective chart review was conducted of patients from 2014-2022 who underwent decompression and fusion for MESCC. Baseline demographic information were collected. SINS score, pre-and post-operative Bilsky score, and primary tumor type were elucidated. Levels of compression involving the thoracic spine down to the conus were included. Patients who only had laminectomy only, laminectomy and fusion without transpedicular decompression, involvement of cervical spine, and prior spine surgery were excluded. MFI-5 was calculated for each patient. Effect of the variables were each analyzed by univariate analyses using simple logistic regression for dichotomous outcomes or linear regression for continuous outcomes. Effect sizes were summarized by odds ratio (dichotomous outcomes) or beta coefficients (continuous outcomes) and associated 95% confidence intervals (95% confidence interval). RCRI was recorded from preoperative documentation by internal medicine staff. Primary outcomes were evaluated according to the following variables: length of stay (LOS), intraoperative estimated blood loss (EBL), readmission and reoperations within the first 90 days, and mortality within the first 90 days, and hospital disposition. Results: A total of 127 patients (ages 19-85) were included in this study with mFI-5 calculated. All patients underwent instrumentation and fusion with transpedicular decompression at the level of epidural compression with 5 patients also requiring cage placement. 63% of patients presented with Bilsky grade 3 epidural compression and 30% presented with Bilsky grade 2. An increasing frailty was found to be a significant predictor of longer LOS (1.19, 95% CI: 0.2- 2.1, p < 0.01) and 90-day mortality (OR 1.81, 95% CI 1.04-3.17, p < 0.05) in contrast to RCRI and age. Multivariate analysis adjusting for sex, BMI, and age confirmed statistical significance (p < 0.05). MFI-5 was not a significant predictor for reoperations and readmissions in the first 90 days postoperatively and intraoperative EBL. Age, and not mFI-5 or RCRI, was a significant predictor for non-home disposition (OR 1.07, 95% CI 1.02 - 1.12, p = 0.001). Conclusion: 5-item Frailty index has a larger effect size than age and Revised Cardiac Risk Index in predicting adverse events such as longer LOS and 90 day mortality. Age, in congruence with prior studies, is a significant predictor for non-home disposition.
1826
A216: Differences in inpatient and outpatient palliative care utilization based on race and interventions provided for patients with spine metastasis
Edwin Owolo 1 , Meghan Price 1 , Dana Rowe 1 , Isabel Prado 1 , Tara Dalton 1 , Jacob Sperber 1 , Antoinette Charles 1 , Brandon Bishop 1 , Harrison Hockenberry 1 , Emily Luo 1 , Melissa Erickson 1 , Margaret Johnson 1 , Anthony Galanos 1 , Elizabeth Fricklas 1 , Arif Kamal 1 , and C. Rory Goodwin 2
1 Department of Neurosurgery, Duke University School of Medicine, Durham, United States
Introduction: Patients with spine metastases (SM) often have significant symptom burden and poor prognoses- both of which can be effectively addressed with specialty Palliative Care. However, there is a dearth of literature on both inpatient and outpatient PC (IPPC and OPPC) utilization throughout the treatment course for this patient population. Objective: The purpose of this study is to characterize IPPC and OPPC utilization trends for patients with SM at the end of life (EoL). Methods: We identified 137 patients who were both presented at our institution’s Brain and Spine Metastasis Tumor Board from February 2018-February 2020 and died during this time. Data regarding demographics, clinical presentation, IPPC/OPPC utilization, EoL outcomes, and last admission were extracted via manual chart review. Statistical analyses summarized and compared outcomes between patients who did and did not receive IPPC/OPPC. Results: Of the 137 patients included, 116 (84.7%) had at least one admission in the last 6 months of life. Of these patients, 42 (36.2%) and 39 (33.4%) had an OPPC or IPPC encounter, respectively. Patients who had been previously seen by OPPC were more likely to have an admission (95.3% vs 75.3%, p = 0.04) but less likely to have ED visits (52.7% vs 45.5%; p = 0.43) at the EoL. Regarding discharge disposition and code status, patients seen by IPPC during their last admission were more likely to die in the hospital/hospice vs discharged home (43.6% vs 16.4%, p = 0.002) and have their code status changed to DNAR (53.1% vs 21.4%, p = 0.0014). Conclusion: This is the first study to assess the use of IPPC/OPPC for patients with SM at the end of life. Given the significant differences in EoL metrics for patients seen by OPPC or IPPC, we advocate for the ongoing integration of these services into the care of patients with SM, particularly during EoL.
OP25: Degenerative Lumbar – Novel Solutions
999
A217: Monocarboxylate transporter expression directly affects degeneration of the intervertebral disc (IVD) in mice
Mulati Mieradil 1 , Shambhavi Bhagwat 1 , Kya Vaughn 1 , Evan Polsky 1 , Matt Silva 1 , Regis O'keefe 1 , and Matthew Goodwin 2
1 Orthopedics, Saint Louis, Washington University, United States
Introduction: Disc degeneration is the central component involved in numerous common spinal pathologies, and lower back pain remains one of the leading causes of disability in the world. While degenerative disc disease affects millions, the mechanisms driving degeneration remain poorly understood. Previous work has shown that high levels of intracellular lactate are involved in this pathology. Here, we present a series of experiments utilizing mouse models of intervertebral disc (IVD) degeneration designed to elucidate the role of lactate transport in degenerative disc disease. The goal was to define the metabolic pathways and role of lactate transport in disc degeneration in different disc degeneration models. Methods: Three models of disc degeneration in female mice (C57BL/6J, n = 108) were studied: 1) lumbar-disc poke, 2) tail-disc poke, 3)spinal instability, and 4)sham. In group 1, a retroperitoneal approach exposed lumbar IVD, and a 27G needle injured the disc. In group 2, the needle injured the tail IVD. In group 3, instability was induced by resection of facet joints and supraspinous/interspinous ligaments. Group 4 was sham. Mice were euthanized at 2, 4, 8 weeks. IVD was evaluated by histological and immunofluorescence analysis. RNA extraction from disc-tissue was analyzed with RNA-seq/QPCR. Results: At 2, 4, and 8 weeks, groups 1, 2, and 3 demonstrated disc degeneration characterized by loss of nucleus pulposus (NP) cells and gradual increase in matrix components in the NP, the distinction between NP and annulus fibrosus (AF) was lost, with increased expression of collagen X and MMP13 in the NP. GLUT1/CA3 (NP markers) gradually decreased, as did PSR-stained collagen (thickness). We analyzed RNA-seq and constructed a PCA score map with five distinct sections. Tail-poke, lumbar-poke, and instability all differed from sham. RNA-seq results at the early stage of disc injury revealed DGEs in our target MCTs, with lactate transporter (MCT4/Slc16a3) gene expression increased in the three models. The RNA-seq data also revealed that gene expression of a rare lactate transporter (MCT3/Slc16a8) was unchanged in the early stages of disc injury and hexokinase 2 (HK2), a key enzyme in glycolysis, was reduced. QPCR in the middle stage of caudal disc injury revealed that expression of MCT4 was gradually decreased and MCT3 increased. The expression of HK2 was also reduced. Conclusion: The IVD degenerative process was characterized by loss of NP cells and gradual increase in matrix components. Our results introduce novel evidence to support a common molecular pathway whereby discs degenerate after direct injury or becoming unstable. When viewing gene expression profiles in response to injury, the lumbar poke and instability models were significantly different from the sham but similar to each other. Genes up/down regulated are likely related to the development of mechanical disc degeneration. Our new finding that significant loss of MCT4 expression occurs following disc injury suggests that this transporter may play a functional role in IVD degeneration, while MCT3 is rarely expressed and may act as a "rescue" lactate transporter. Decreased HK2 gene expression results in reduced glycolysis and may also be important in disc degeneration.
1696
A218: Perioperative intravenous nefopam on pain and ambulation after open lumbar spine surgery: a randomized double blind controlled trial
Weerasak Singhatanadgige 1 , poornpan Chalermkitpanit 1 , Vit Kotheeranurak 1 , Worawat Limthongkul 1 , and Wicharn Yingsakmongkol 1
1 Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
Introduction: To evaluate the effect of intravenous nefopam regarding the reduction of morphine consumption, postoperative pain, and enhanced recovery in patients undergoing open spine surgery. Material and Methods: One hundred patients undergoing lumbar decompressive laminectomy with fusion were randomized into two groups. Intravenous nefopam of 20 mg was delivered at the end of the operation for patients in the nefopam group, then followed by a continuous infusion of 80 mg of nefopam for 24 hours postoperatively. An identical infusion of normal saline was administered in the control group. Multimodal analgesia including oral non-opioid medications and patient-controlled analgesia (PCA) of intravenous morphine were given in both groups. The primary outcome was the amount of the first 24-hour morphine consumption. The intensity of postoperative pain, postoperative function, and hospital stays were collected as secondary outcomes. Results: At the PACU, patients in the nefopam group demonstrated lower pain scores both while at rest (p = 0.03) and upon movement (p = 0.02) compared to patients in the normal saline group. However, the intensity of postoperative pain between the two study groups was similar on postoperative day 1, day 2, and day 3. Morphine consumption between both groups was equivalent. The length of hospital stays in patients who received nefopam was significantly shorter than patients in the control group (p < 0.01). There were no significant differences in postoperative function and ambulation between the two study groups. Conclusion: Perioperative intravenous nefopam demonstrated significant pain reduction during the early postoperative period and shortened length of hospital stays. The role of the opioid-sparing effect needs to be elucidated. Nefopam is considered safe and effective as a part of multimodal analgesia in open spine surgery.
2031
A219: Comparisons of duration of intravenous antibiotics following short and long lumbar fusion: a worldwide survey from AOSpine
Xueyu Hu 1 , Fang Xie 1 , Timothy S. Yoon 2 , Matthew Gary 2 , Ho-Joong Kim 2 , Zhuojing Luo 1 , and (on behalf of) AO Spine Knowledge Forum Degenerative
1 Orthopaedics, The First Affiliated Hospital of Air Force Medical University, Xi´an, China
2 AO Spine Knowledge Forum Degenerative
Introduction: Surgical site infection (SSI) can lead to serious consequence after spinal surgeries, varied in incidence rate, up to 20%. A number of surgeons choose prophylactic intravenous antibiotic usage postoperatively with satisfying clinical results. However, duration of intravenous antibiotics use vary. In this study, we analyzed using time of postoperative prophylactic intravenous antibiotic after short (1-2 level) and long (3-5 level) lumbar fusion. Material and Methods: Results of a survey of 280 surgeons from AO Spine Knowledge Forum Degenerative were collected. We then enrolled those who had extensive experience in open 1-2 or 3-5 lumbar fusion for adult lumbar degenerative diseases for further analysis. For duration of intravenous antibiotics, we classified data into seven categories as < 24 h, 24 h,72 h, 96 h, > 96 h, until the drains are out and other. Comparisons between proportions were done with the Chi-square test. A p < 0.05 was considered statistically significant. Results: Answers were obtained from 233 surgeons performing short fusion and 189 performing long fusion. In 1-2 level group, 98.28% used prophylactic intravenous antibiotic, 57.51% used 24h or less, followed by up to 72h (19.31%) and until the drains are out (7.73%). In 3-5 level group, 96.83% used prophylactic intravenous antibiotic. 57.75% used 24 h or less, followed by used up to 72h (15.87%) and until the drains are out (10.05%). There was no significant difference in routine of intravenous antibiotic usage (p = 0.983) between short and long fusion. Conclusion: Most of respondents used prophylactic intravenous antibiotic after lumbar fusion. More than half of surgeons used intravenous antibiotic within 24h postoperatively. No significant differences were found in using time between short and long fusion. Consensus recommendations for standardized use of antibiotics deserve further studies.
1360
A220: Comparison of efficacy of leucocyte rich platelet rich plasma vs leucocyte poor platelet rich plasma via caudal epidural route in patients with low backache due to degenerative disc disease : A randomised controlled double blinded study
Prabhat Agrawal 1
1 AIIMS, India
Introduction: Degenerative disc disease (DDD) is one of the commonest problems with which a patient presents apart from medicine and physiotherapy, epidural injections are gaining popularity when it comes to the management. Steroids have traditionally been used as a remedy but literature is very less regarding the efficacy of Platelet Rich Plasma (PRP). Apart from reducing inflammation, PRP also has regenerative capability. Among the types of PRP which we normally observe and use mainly 2 broad types are there: leukocyte rich PRP (LR-PRP) and leukocyte poor PRP (LR-PRP). So in our study we tried to compare between these two and determine which one is better for patient. Materials and Methods: A total of 50 patients with chronic low back ache due to degenerative disc disease with or without radiculopathy attending the AIIMS Patna Orthopaedics OPD were selected for the study. In OPD visit their VAS, MODQ, and SF-36 were calculated and these were kept as scoring parameters for comparison. 20 patients did not turn up for the procedure and finally 30 patients were included in the study. Block randomisation technique was used to designate and randomise the patients who had been allotted the particular treatment. The patients who had been allotted as group A would receive LR-PRP whereas the patients in group B would receive LP-PRP. Both the investigator and patient were unaware of the group the patient was put into. This fact was only known by the technician of blood bank and the data analyser after observing the randomisation list which was generated by computer. Epidural injection was given under C arm guidance.All the 3 scoring parameters were determined at 1st, 3rd and 6th months follow-up and results were compared. Results: At 1st, 3rd and 6th month post caudal epidural injection it was observed that VAS, MODQ and SF-36 of patients were better in group A patients than group B patients. Moreover, it was observed that at 1 month the difference between the values of reducing VAS was most indicating the clear role of LR-PRP in short term benefits. Conclusion: While both groups of patients were overall satisfied with the result, patients who had been given LR-PRP were symptomatically better than the other group. This gave us a clue to point towards the fact that LR-PRP is better than LP-PRP in managing chronic low back ache in patients having DDD.
1015
A221: Is there consensus on best practices for lumbar wound closure or are we simply perpetuating regional dogma? A worldwide survey of 280 spine surgeons
James Malcolm 1 , Timothy S. Yoon 2 , Yabin Wu 3 , Ho-Joong Kim 4 , Matthew Gary 1 , and (on behalf of) AO Spine Knowledge Forum Degenerative
1 Department of Neurosurgery
2 Department of Orthopedics, Emory University School of Medicine, Atlanta, United States
3 AO Foundation
4 Spine Center and Department of Orthopedic Surgery, Seoul National University College of Medicine and Bundang Hospital, Seoul, South Korea
Introduction: There is a lack of evidence available for best practices when it comes to wound closure following lumbar degenerative spine surgery. Wound complications following surgery can have devastating consequences, especially when hardware is present. Is there an optimal technique for wound closure to prevent wound breakdown and improve cosmesis? All studies to date are retrospective and are limited by selection bias and the prevailing dogma of the surgeon themselves. One recent systematic review only found 6 lower quality retrospective evidence level III papers from Jan 2000 to December 2017. Here we present current practices for skin and deep fascial closure among 280 spine surgeons around the world. Material and Methods: AOSpine sponsored survey was performed. Surveys were sent to all AOSpine members and those who perform more than 10 cases per year of lumbar fusion were asked to respond to the questions. There were 280 respondents who completed the survey. A subset of the questions focused on skin and deep fascial closure preferences. The skin closure category included staples, absorbable sutures, nonabsorbable sutures, glue, and steri-strips. The deep closure category included absorbable sutures, nonabsorbable sutures, muscular layer closure, continuous vs interrupted sutures, and plastic surgery involvement. Results were stratified by region. Chi^2 testing was used to test for difference in the regional distribution of answers. Results: For skin closure, across all regions, respondents indicated that they use the following: subcuticular absorbable suture 51%, staples 39%, external nonabsorbable sutures 34%, glue 12%, steri-strips 12%. For fascial closure, across all regions, respondents indicated that they use the following: absorbable braded 73%, absorbable monofilament 16%, nonabsorbable braided 6%, nonabsorbable monofilament 8%, approximate the muscles 21%, utilized plastic surgery 1%. Stratified by region, there were significant differences (p < 0.0001), specifically subcuticular was more commonly utilized among North American (59%) and Asian Pacific (64%), compared to Latin America, Europe, the Middle East, and Africa (43-47%). External nonabsorbable sutures were more common in Latin America (68%) compared to other regions (23-34%). Muscle closure was more common in Latin America (32%) compared to other regions (16-24%). Conclusion: There is no consensus on best practices for lumbar degenerative wound closure. There is strong preference for subcuticular skin closure compared to staples and external nonabsorbable sutures but there are regional biases. For fascial closure there is a strong preference for absorbable braided sutures. While a minority of surgeons close the muscle, it was more commonly done in Latin America. Given the lack of evidence and the varied practices around the world, further clinical trials are warranted to determine optimal closure technique for prevention of wound dehiscence and subsequent infection. Until then, surgeons will continue perpetuating regional dogma.
712
A222: Abdominal aortic calcification as a screening tool for osteoporosis in spine surgery
Maximilian Muellner 1 , Haffer Henryk 1 , Erika Chiapparelli 1 , Yusuke Dodo 1 , Jennifer Shue 1 , Andrew Sama 1 , Frank Cammisa 1 , Federico Girardi 1 , and Alexander Hughes 1
1 Spine Care Institute, Hospital for Special Surgery, New York, United States
Introduction: Osteoporosis can lead to devastating postoperative complications in orthopedic surgery. However, there is no standardized preoperative osteoporosis workup prior to lumbar spine surgeries to date. The aim of this study was to determine whether the presence of abdominal aortic calcification (AAC) can predict patient bone status, represented by volumetric bone mineral density (vBMD) assessed with quantitative computed tomography (QCT). Material and Methods: Patients undergoing lumbar fusion surgery at a tertiary care center between 2014 and 2021 were retrospectively reviewed. A semi-quantitative measurement method for AAC (AAC 4, AAC 8 and AAC 24) was performed using preoperative lumbar radiographs. QCT measurements were made for L1 and L2 and were averaged. Patients were divided into two groups depending on whether AAC was present. A one-way analysis of covariance was conducted to adjust for age. The Spearman correlation coefficient was determined for vBMD and the AAC measurements. A multiple linear regression model was used to test if age, sex, BMI and presence of AAC could predict the vBMD. A receiver operating characteristic (ROC) analysis was conducted to determine the specificity and sensitivity of AAC for predicting osteoporosis. Results: 267 patients (55.8% female) with a median age of 65.1 years and BMI of 29.8 kg/m2 were analyzed. Overall, 59.6% of patients had AAC. The group comparison showed that vBMD was significantly lower in patients with the presence of AAC (97.8 mg/cm3 vs. 121.5 mg/cm3). Age (β = -0.367; p < 0.001) and presence of AAC (β = -0.151; p = 0.018) significantly predict vBMD (corrected R2 = 0.196) as independent variables. Osteoporosis could be discriminated using AAC 4, 8 and 24 (cut off value 0.5) with a sensitivity of 70.1% and a specificity of 60.2% with an AUC of 0.674, 0.673 and 0.672, respectively. Conclusion: The presence of calcification of the abdominal aorta may identify patients at risk for impaired bone status. Preoperative evaluation of standard lumbar radiographs could be used as a potential diagnostic tool in assessing bone status and surgical risk management.
1159
A223: An analysis of a decade of lumbar interbody cage malfunctions in the United States: A MAUDE Database study
Amit Piple 1 , Victor Ungurean 2 , Oluwatodimu Raji 23 , Andrea Rowland 3 , Adam Schlauch 3 , Dimitriy Kondrashov 3 , Ken hsu 3 , and James Zucherman 3
1 Orthopaedic Surgery, The Taylor Collaboration, San Francisco, United States
2 The Taylor Collaboration, San Francisco, United States
3 St. Mary's Medical Center, San Francisco, United States
Introduction: Perioperative lumbar interbody cage malfunctions are underreported events in the spine literature. Although the Food and Drug Administration (FDA) ensures the safety of these devices postoperatively, rates of intraoperative failure due to transient loading conditions may be overlooked. These failures are of particular concern as any undetected damage to the implant components during implantation may lead to subpar postoperative outcomes. Therefore, this study aims to assess rates of lumbar interbody cage failures based on their production material and manufacturer. Methods: The FDA’s Manufacturer and User Facility Device Experience (MAUDE) database was queried for all reports of lumbar interbody cage device failures from 2012 to 2021. Each report was manually analyzed and categorized on the basis of failure type (i.e. cage breakage, cage migration, screw failure, instrumentation failure, collapse, and assembly failure). The implants were then categorized by its core and surface material (i.e. poly-ether-ether-ketone [PEEK], titanium, and silicon nitride), which was obtained from 510(k) premarket notifications. Rates of failures were compared based on core and surface material type. A market analysis was performed by dividing the total number of failures per year for each manufacturer by their approximate yearly revenue from spinal implants in the U.S. (in hundreds of millions of dollars), generating “failure to revenue indices”. Outlier analysis was performed to generate a threshold value above which failure rates were defined as greater than the normal index. Results: In total, 1,875 lumbar cage malfunctions were identified. Of these, 1,230 (65.6%) were cage breakages, 257 (13.7%) were instrument malfunctions, 177 (9.4%) were cage migrations, 143 (7.6%) were assembly failures, 70 (4.5%) were screw-related failures, and 21 (1.1%) were due to cage collapse. Of the cage breakages, 923 (74.9%) occurred during implant insertion or impaction. While the majority of these breakages were resolved without incident, 8.5% of these cage breakages detailed an intraoperative or postoperative complication, such as retained foreign bodies, new/worsening radicular symptoms, back pain, revision lumbar fusion, dural tear, or vascular injury requiring transfusion. Of the cage migrations, 155 (88.6%) were identified postoperatively, of which 73 (47.1%) detailed postoperative complications and 52 (33.5%) required a revision procedure. These complications included tissue injury, pain, nerve damage, re-stenosis, fatigue fracture, and radicular symptoms. Market analysis demonstrated that Medtronic (from 2019 to 2021), Zimmer Biomet (in 2012 and 2014), Stryker (in 2013 and 2015), Seaspine (in 2013 and 2015), and K2M (in 2017) exceeded the calculated threshold. Discussion: Lumbar interbody cages manufactured using PEEK core material failed by breakage more frequently than by migration, whereas titanium surface cages failed by migration more frequently than by breakage. Failure rates varied depending on the manufacturer. Most of the cage breakages identified in the present study occurred intraoperatively during insertion and impaction. Most instrumentation malfunctions were due to inserter fracture, which, in some cases, introduced metal debris into the wound. Many of these malfunctions resulted in intra- and postoperative complications or required a future revision procedure. These findings call for a more detailed FDA evaluation of these intraoperative malfunctions prior to commercial approval.
2017
A224: A whole spine MRI based ambispective cohort study of the prevalance and clinico-radiological association of lumbosacral transitional vertebrae with degenerative disc disease
Shanmuganathan Rajasekaran 1 , Ajoy P Shetty 1 , Chandhan Murugan 1 , Chintan Bhagchandani 2 , Karthik Ramachandran 1 , and Rishi Kanna 1
1 Department of Spine Surgery
2 Department of Orthopedics,Ganga Hospital, Coimbatore, India
Background: Lumbosacral transitional vertebra (LSTV) results in numerical alterations of the lumbar and the sacral segments, and prompt recognition of the LSTV is crucial. Literature concerning the true incidence of LSTV based on whole spine MRI and its association with low back pain, radicular symptoms and disc degeneration is lacking. Materials and Methods: The study is an ambispective observational cohort study. The prevalence of LSTV was determined by studying the whole spine MRIs of 2011 poly-trauma patients. A prospective analysis of 2230 patients was done to determine the association of LSTV with low back pain, radicular symptoms, disc degeneration and/or facet tropism. Disc degeneration was measured at the level of three distal mobile segments by Pfirrmann’s grading while the total end plate score (TEPS) was evaluated in the last mobile segment (C). Results: The overall prevalence of LSTV was 11.6%. Eighty-two prevent of the LSTV patients had sacralization of L5, while the rest had a lumbarization of S1. Castellvi’s type 2A was the most common type (33.6%) of sacralization, while the O’Driscoll type 4 was the commonest sub-type (54.8%) of lumbarization. LSTV was found in almost 15% of patients who presented with low back pain without radiculopathy, while it was found in 17% of patients who presented with predominantly radicular symptoms. Sacralization accounted for more than 80% of the LSTV patients in both groups. LSTV patients demonstrated considerably advanced degeneration (Pfirmanns grade 3-5) at all three levels in comparison with non-LSTV patients (p = 0.001). The TEPS, as well as the presence of facet tropism, was significantly higher in the LSTV group as compared to the non-LSTV group. Conclusion: The overall prevalence of LSTV was 11.6%, with sacralization accounting for more than 80%. LSTV was found to have a significant association with low back pain, radicular symptoms, disc degeneration, and facet tropism.
297
A225: Influence of timing of elective lumbar surgery on total joint replacement outcomes
Anthony Steinle 1 , Alex Volkmar 1 , Andrew Croft 1 , Eric Dilbone 1 , Hui Nian 2 , Jeffrey Chen 1 , Emil Varas-Rodriguez 1 , Scott Lawrence Zuckerman 1,3 , Byron Stephens 1,2,3 , Ryan Martin 1 , and Amir Abtahi 1,2,3
1 Department of Orthopaedic Surgery
2 Center for Musculoskeletal Research
3 Department of Neurological Surgery, Vanderbilt University Medical Center, Nashville, TN, United States
Introduction: The association between degenerative spine conditions and hip/knee pathology is well documented in the literature. For patients requiring both total joint replacement (TJR) and lumbar spine surgery, it is unknown whether the timing of lumbar surgery in relation to TJR affects TJR outcomes. The current study sought to determine if TJR (specifically THA or TKA) outcomes differed between patients who underwent TJR before vs. after lumbar spine surgery. We hypothesized patients who undergo TJR after lumbar surgery will have better TJR outcomes due to a reduction in pain and improvement in overall function. Material and Methods: A prospectively collected registry from a single institution was queried for patients who underwent both THA/TKA and lumbar surgery within a 3-year timeframe. All THA/TKA revisions, lumbar disc herniations, lumbar revisions, and lumbar deformity cases were excluded. Patients were separated into 4 groups: 1.) Lumbar surgery before THA, 2.) Lumbar surgery after THA, 3.) Lumbar surgery before TKA, and 4.) Lumbar surgery after TKA. Covariates for both groups included age, gender, and BMI. Covariates specific to the hip cohort included hip implant sizes/types. THA outcomes included NRS hip pain scores, leg length, cup abduction, and complication and dislocation rates within 12 months. TKA outcomes included knee range of motion (ROM) and NRS knee pain scores, and rates of complications, reoperations, revisions, and occurrence of arthrofibrosis within 12 months of TKA. A variety of statistical tests were performed to compare groups. Results: Of 46 eligible THA patients, 28 underwent THA after lumbar surgery, while 18 underwent THA prior to lumbar surgery. Bivariate analysis showed no differences in any baseline variables, surgical variables, dislocation rates, or NRS pain scores at 2 wks/6 wks/12 mo. Bivariate analysis showed patients who underwent THA prior to lumbar surgery had more overall complications following THA (33.1% vs 3.6%, p = 0.007). Univariate and multivariate regression also demonstrated higher rates of complications following THA when performed prior to spine surgery. Complications included UTI, sepsis, anemia, trochanteric bursitis, intraoperative fracture, and delayed wound healing. Timing of spine surgery was not associated with a significant difference in any other outcome measure. Of 91 eligible TKA patients, 43 underwent lumbar surgery before TKA, and 48 underwent lumbar surgery after TKA. Bivariate analysis showed no differences in baseline variables between groups. There were no statistically significant differences in knee ROM or NRS knee pain scores at any time point, nor were there differences in reoperation or implant revision rates. Univariate analysis showed timing of surgery had no impact on any TKA outcome measure at any time point. Conclusion: We compared TJR outcomes in patients undergoing TJR before vs. after lumbar surgery and found those who undergo THA prior to lumbar surgery had more overall complications following THA. While the reasons for this are unclear, this finding warrants further investigation. TKA outcomes did not differ based on the timing of lumbar surgery. It is recommended that the severity of symptoms as well as patient preference dictate surgical order in patients with concomitant spinal pathology and knee arthritis.
OP26: Spinal Imaging
1330
A226: Improved productivity using deep learning assisted reporting for MRI lumbar spine
James Hallinan 1 , Jiong Hao Tan 2 , Andrew Makmur 1 , Balamurugan Vellayappan 3 , and Naresh Kumar 2
1 DDI
2 Orthopaedic Surgery
3 Radiation Oncology, National University Health Systems, Singapore, Singapore
Introduction: Lumbar spine MRI studies are widely used for back pain assessment. Interpretation involves grading lumbar spinal stenosis, which is repetitive and time consuming. Deep learning (DL) could provide faster and more consistent interpretation. The aim of this study was to evaluate the time taken and interobserver agreement for reporting lumbar spinal stenosis with and without a DL model. Materials and Methods: In this retrospective study, a DL model designed to assist radiologists in the interpretation of spinal canal, lateral recess, and neural foraminal stenoses on lumbar spine MRI scans was utilized. Randomly selected lumbar spine MRI studies obtained in adult patients with back pain over a 3-year period, from September 2015 to September 2018, were included in an internal test set. Studies with instrumentation and scoliosis were excluded. Eight radiologists reviewed studies with and without DL model assistance, and a 1-month washout period and crossover study design were used to limit recall bias. The radiologists included two musculoskeletal radiologists (7- and 11-years of experience), four general radiologists (2-, 5-, 12- and 13- years of experience), and two second year trainee radiologists, with limited exposure to spine MRI studies. Time to diagnosis (seconds) and interobserver agreement (Gwet’s kappa) were assessed for stenosis grading for each radiologist with and without the DL model and compared with an external musculoskeletal radiologist (32 years of experience) as the reference standard. Results: Overall, 444 images in 25 patients (mean age, 51 years ± 20[SD]; 14 women) were evaluated in a test set. DL assisted radiologists had a reduced interpretation time per spine MRI. Overall, the mean interpretation time per spine MRI study with the DL model (mean range = 47-71 seconds [SD = 24-29 seconds]) was lower than without the DL model (mean range = 124-274 seconds [SD = 25-88 seconds]) (p < 0.001). This difference was seen for all experience levels. Musculoskeletal radiologists had a mean time saving of 62% (77 of 124 seconds) using the model, with mean times of 47 seconds ± 24 and 124 seconds ± 25 with and without the model, respectively. General radiologists had a mean time saving of 69% (156 of 226 seconds) using the DL model, with mean times of 70 seconds ± 29 and 226 seconds ± 61 with and without the model, respectively. In-training radiologists had the largest mean time saving of 74% (203 of 274 seconds) using the model, with mean times of 71 seconds ± 28 and 274 seconds ± 88 with and without the model, respectively. DL-assisted radiologists had either superior or equivalent interobserver agreement for all stenosis gradings compared with unassisted radiologists. DL-assisted general and in-training radiologists improved their interobserver agreement for four-class neural foraminal stenosis, with kappas of 0.71 and 0.70 (with DL) versus 0.39 and 0.39 (without DL), respectively (both p < 0.001). Conclusion: Radiologists who were assisted by deep learning for interpretation of lumbar spinal stenosis on MRI scans showed a marked reduction in reporting time and superior or equivalent interobserver agreement for all stenosis gradings compared with radiologists who were unassisted by deep learning.
696
A227: A standardized imaging approach to improve the accuracy and reliability for detecting thoracolumbar posterior ligamentous complex in CT and MRI
Mohamed Ali 1
1 Neurosurgery, Prince Mohamed Bin Abdelaziz Hospital, Riyadh, Saudi Arabia
Introduction: Assessment of the Posterior Ligamentous Complex integrity has been cited as a significant factor in Thoracolimbar fracture classification. However, there is no systematic approach for image interpretation to diagnose PLC injury. Materials and Methods: A systematic review was conducted following PRISMA guidelines. The Scopus database was searched from its inception until July 21, 2022, for studies evaluating CT or MRI assessment of the PLC injury following thoracolumbar trauma. The studies extracted key findings, objectives, injury definitions, and radiographic modalities. Results: Twenty-three studies were included in this systematic review, encompassing 2,021 patients. Five studies evaluated the accuracy of MRI in detecting thoracolumbar PLC injury using intraoperative findings as a reference. These studies indicate that black stripe discontinuity due to supraspinous or ligamentum flavum rupture is a more specific criterion of PLC injury than high-signal intensity. Thirteen papers evaluated the accuracy or reliability of CT in detecting thoracolumbar PLC injury using MRI or intraoperative findings as a reference. The overall accuracy rate of CT in detecting PLC injury was 68-90%. Two studies evaluate the accuracy of combined CT, showing that ≥2 CT findings are associated with a positive predictive value of 88-91 %. Vertebral translation, facet joint malalignment, spinous process fracture, horizontal laminar fracture, and interspinous widening were independent predictors of PLC injury. Conclusion: We provided a comprehensive imaging algorithm for diagnosing PLC in CT and MRI based on available literature and our experience. The algorithm includes standard definitions for CT/MRI findings, the best imaging planes/sequences, and the pitfalls and pearls of image interpretation.
Keywords: Posterior ligamentous complex, thoracolumbar fractures, imaging algorithm, Computed tomography, Magnetic resonance imaging.
357
A228: Are biplanar projection radiographs sufficient to confirm intra-operative robotic pedicle screw placement?
George Gorgy 1 , Fedan Avrumova 1 , Philip Paschal 1 , John Carrino 1 , and Darren Lebl 1
1 Spine Surgery, Hospital for Special Surgery, New York, United States
Introduction: Two Dimensional Bi-Planar Radiography (BPR) has been the gold standard to assess pedicle screw position in spine fusion surgery for many years. However, 3-dimension intraoperative imaging systems are now available. Significant pedicle screw misplacement rates have been previously reported in the thoracic and lumbar spine when utilizing BPR. With the advent of advancement of technology and advanced 3-dimensional imaging techniques, it has been reported that there is an increased accuracy and safety in pedicle screw placement. The goal of this study was to evaluate the effect of an intraoperative 3-dimensional (3D) imaging system/(Ziehm, Nuremberg, Germany) and its accuracy to confirm intraoperative pedicle screw placement when compared to intraoperative biplanar fluoroscopic images. Material and Methods: A retrospective review of prospectively collected data consisting of 205 patients underwent degenerative spinal surgery by one spine surgeon and screw placement was compared between intraoperative x-rays (BPR) and intraoperative 3D fluoroscopic imaging. The M-line and Gertzbein-Robbins system (GRS) were used to confirm false positives or negatives in BPR. M-line was defined as a line connecting the upper and lower spinous processes through the fixed vertebrae within BPR. GRS measures pedicle screw accuracy and categorizes positions into 4 groups based on a clinical positioning grading used in 3D imaging. Results: We assessed total 204 patients who underwent degenerative instrumented lumbar fusion. 187 had saved intra-operative BPR and intra-operative 3D imaging. A total of 1044 pedicle screws were placed, in which 922 (88.3%) screws were placed robotically. 93 (49.7%) of these patients also had post-operative CT scans that were used to confirm 100% of our M-line and GRS findings. 10 patients (5.3%) had discrepancies between their M-line and GRS findings. 1 pedicle screw per patient had the discrepancies. 8 patients (5.3%) had positive M-lines (i.e a medial pedicle breach) and a GRS grade of A (i.e no pedicle breach), concluding that there was a false positive on the BPR. Similarly, 2 patients (1.0%) had negative M-lines and a GRS grade of B, leading to a false negative. Conclusion: A clinically significant number of patients had false-negative and false-positive screw confirmation on BPR. In 5.3% of patients and 0.8% of screws, a false-positive on BPR findings was found. Furthermore, 1% of patients and 0.2% of screws showed a false negative of pedicle screw mal-positioning. BPR may yield a false sense of security for misplaced screws and conversely may raise concern over screws that are in a satisfactory position. These findings may make 3D imaging a more desirable post-instrumentation intra-operative gold standard.
1323
A229: Deep learning model for granting metastatic epidural spinal cord compression on staging CT
Jiong Hao Tan 1 , James Hallinan 2 , Andrew Makmur 3 , Balamurugan Vellayappan 2 , and Naresh Kumar 1
1 Orthopaedic Surgery
2 Radiation Oncology
3 DDI, National University Health System, Singapore, Singapore
Introduction: Metastatic epidural spinal cord compression (MESCC) is a devastating complication of advanced cancer. MRI is the current gold standard imaging test, but it is expensive and not suitable for screening. Staging CT scans are commonly performed for cancer diagnosis and treatment follow-up, and represent a window of opportunity for earlier diagnosis of MESCC. Deep learning (DL) models for automated MESCC classification on staging CT were developed to aid earlier diagnosis. Materials and Methods: Retrospective collection of staging CT scans and corresponding MRI spines from patients with suspected MESCC was conducted from September 2007 to September 2020. Exclusion criteria were scans with instrumentation, no intravenous contrast, extensive motion artefacts and non-thoracic coverage. The internal CT dataset split was 84% for training/validation and 16% for testing. An external CT test set from a different institution was also utilised. Internal training and validation sets were labelled by radiologists with spine imaging specialization (6 and 11 years of experience), and were used to develop a DL model for MESCC classification on CT. The spine imaging specialist (11-years expertise) labelled the staging CT test sets (axial portal venous phase images) in conjunction with the matched MRI spines (axial T2-weighted images) to serve as the reference standard. MESCC was classified using a modified Bilsky MESCC scale; normal/no epidural disease, low-grade (epidural disease with no contact of the spinal cord), and high-grade disease (spinal cord contact or compression). For evaluation of the DL model performance, internal and external test sets were independently reviewed by four radiologists; two spine specialists (Rad1 and Rad2, 7 and 5 years of experience, respectively) and two body radiologists with experience in oncological CT scan assessment (Rad3 and Rad4, 3 and 5 years of experience, respectively). Inter-rater agreement (Gwet’s kappa) and sensitivity/specificity/AUCs were calculated. Results: Overall, 420 CT scans were evaluated from 225 patients (mean age = 60 ± 11.9[SD]); 354 (84%) CT scans were used for training/validation and 66 (16%) CT scans were used for internal testing. The external test set consisted of 43 CT scans from 32 patients (mean age = 60 ± 13[SD]). The DL model showed almost-perfect inter-rater agreement for three-class MESCC grading with kappas of 0.87 (p < 0.001) and 0.84 (p < 0.001) on the internal and external test sets, respectively. On the internal test set the DL model inter-rater agreement (κappa = 0.87) was superior to Rad 2, a spine imaging specialist (κ = 0.80) and Rad 3, a body radiologist (κ = 0.72) (both p < 0.001). The DL model kappa of 0.84 on the external test set was also superior to Rad 3 (κ = 0.72) (p < 0.001). For detection of high-grade MESCC the DL model showed high kappa/sensitivity/specificity/AUC of 0.94/93.4/95.47/0.94 on the internal test set and 0.95/96.6/96.0/0.96 on the external test set, respectively. Conclusion: A DL model for detection of metastatic epidural spinal cord compression (MESCC) on CT showed comparable or superior inter-rater agreement compared to radiologists on internal and external testing. This DL model could provide earlier diagnosis and treatment of MESCC, resulting in improved patient outcomes including preservation of ambulation.
1301
A230: Deep learning model for classifying metastatic epidural cord compression on MRI
James Hallinan 1 , Jiong Hao Tan 2 , Andrew Makmur 1 , Balamurugan Vellayappan 3 , and Naresh Kumar 2
1 DDI
2 Orthopaedic Surgery
3 Radiation Oncology, National University Health Systems, Singapore, Singapore
Introduction: Metastatic epidural spinal cord compression (MESCC) is a devastating complication of advanced cancer. A deep learning (DL) model for automated MESCC classification on MRI could aid earlier diagnosis and referral. The aim of this study was to train a DL model for the automated Bilsky classification of MESCC using axial T2W MRI. This could aid earlier diagnosis of MESCC and identify suitable candidates for radiotherapy versus emergent surgical decompression. Materials and Methods: Patients with known MESCC diagnosed on MRI between September 2007 and September 2017 were eligible. MRI studies with instrumentation, suboptimal image quality, and non-thoracic regions were excluded. Axial T2-weighted images were utilized, and the data was obtained using a range of MRI platforms and parameters to prevent overfitting and train a more generalizable DL model. The internal dataset split was 82% and 18% for training/validation and test sets, respectively. External testing was also performed. Internal training/validation data were labelled using the Bilsky MESCC classification by a musculoskeletal radiologist (10 years of experience) and a neuroradiologist (5 years of experience). These labels were used to train a DL model utilizing a prototypical convolutional neural network. Internal and external test sets were labelled by the musculoskeletal radiologist as the reference standard. For assessment of DL model performance and inter-rater agreement, test sets were labelled independently by a neuroradiologist (5 years of experience), spine oncology surgeon (5 years of experience), and a radiation oncologist (11 years of experience). Inter-rater agreement (Gwet’s kappa) and sensitivity/specificity were calculated. Results: Overall, 215 MRI spine studies were analyzed [164 patients, mean age = 62 ± 12 (SD)] with 177 (82%) for training/validation and 38 (18%) for internal testing. On an internal test set, the DL model showed almost-perfect agreement (kappa = 0.92, p < 0.001) for dichotomous Bilsky MESCC classification (low grade versus high grade), similar to specialist readers, which included a radiation oncologist (kappa = 0.97, p < 0.001), a neuroradiologist (kappa = 0.96, p < 0.001), and a spine oncology surgeon (kappa = 0.98, p < 0.001). Similar performance was seen for external testing on a set of 32 MRI spines from a different institution with the DL model (kappa = 0.94, p < 0.001), radiation oncologist (kappa = 0.94, p < 0.001), neuroradiologist (kappa = 0.95, p < 0.001), and spine oncology surgeon (kappa = 0.94, p < 0.001) all showing almost perfect agreement (kappas = 0.94-0.95, p < 0.001) compared to the reference standard. The DL model showed high sensitivity/specificity of 97.6/93.6 on the internal test set and 89.9/98.1 on the external test set, respectively. Conclusion: A DL model showed comparable agreement to a subspecialist radiologist and clinical specialists for the classification of malignant epidural spinal cord compression on MRI. The DL model could be used to triage MRI scans for urgent reporting, augment non-sub-specialized radiologists when they report out of hours, and improve the communication and referral pathways between specialties including oncology, radiation oncology, and surgery.
1626
A231: In-vivo dynamic 3D kinematics analysis and clinic study of cervical spine based on fluoroscopic imaging system
Yuxiang Chen 1 and Yong Hai 1
1 Department of Orthopedic Surgery, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: The surgical management of cervical degenerative disc degeneration (CDDD) has not reached a consensus. Both ACDF and ACDR are common procedures for CDDD, have their unavoidable serious complications, and the clinical choice is still controversial. Clarifying the kinetic mechanism of the cervical spine can enhance our understanding of the subtle changes in the normal anatomical structure of the spine, abnormal movements of the spine in pathological conditions, and precise surgical treatment. However, previous related research mainly carried out kinematics research on the cervical spine through traditional pure three-dimensional (3D) or two-dimensional (2D) measurement techniques and failed to achieve 3D dynamic kinematics research in vivo. Methods: Firstly, we included 47 patients with ACDR and 46 patients with ACDF, and compared them by cervical sagittal alignment parameters and associated patient-related outcomes. Subsequently, we validated the 3D model-based contour registration technology of the dual fluoroscopic imaging system (DFIS) by in vitro validation experiment of porcine cervical vertebrae and in vivo validation experiment of healthy adults, respectively. Finally, a dynamic in vivo 3D kinematics study of the cervical spine was conducted with a total of 18 healthy subjects using the DFIS based on the above-mentioned contour registration technology. Results: The two approaches, ACDR and ACDF, were similar in their ability to treat CDDD in terms of radiographic reconstruction and clinical improvement. In the ACDF group, the preoperative intervertebral space height (ISH) was less than 4 mm, and the postoperative Japanese Orthopaedic Association score (JOA) was significantly better than that in the ACDR group (p < 0.05); The postoperative range of motion (ROM) of patients younger than 45 years in the ACDR group was significantly greater than that of patients older than 46 years (P < 0.05). The in vitro verification experiment results of the contour registration technology based on the 3D model show that, for translational accuracy, ranging from 0.10 mm to 0.56 mm; the precision is within ± 0.15 mm, the overall dynamic accuracy is ± 0.56 mm. For rotation accuracy, ranging from -0.89° to 0.63°; the precision is within ± 0.26°, and overall dynamic accuracy is ± 0.61°. The in vivo dynamic three-dimensional kinematics analysis based on DFIS showed during the flexion-extension, the primary rotation was flexion-extension mode, and coupled rotation was lateral bending and axial rotation mode. During the lateral bending and/or axial rotation motion of the neck, the primary rotation was lateral bending mode, and coupled rotation was flexion-extension and axial rotation mode. In all neck directions, the rotation of IVD was significantly greater than that of FJs (p < 0.05). In terms of the rotation of cervical motion, we could mainly focus on the change of IVD. Conclusions: Specific concerns should be analyzed while choosing between an ACDR and an ACDF. The results of the three-dimensional dynamic in vivo kinematics analysis of the cervical spine based on DFIS show that the changes of IVD can be mainly concerned with the rotational changes of cervical spine motion. The changes of FJs can be mainly concerned with the translational changes of cervical spine motion.
1933
A232: Strong correlation between the vertebral bone quality score and the cervical vertebral bone quality score in operative spine patients
Mohamed Soliman 1,2 , Cathleen Kuo 2 , Alexander Aguirre 2 , Nicco Ruggiero 2 , Marissa Kruk 2 , Asham Khan 2 , Ryan Hess 2 , David Smolar 2 , Jeffrey Mullin 2 , and John Pollina 2
1 Neurosurgery, Cairo University, Cairo, Egypt
2 Neurosurgery, University at Buffalo, Buffalo, United States
Introduction: Osteoporosis is a burgeoning public health problem for over 44 million people in the United States. For spine surgeons, osteoporosis poses a unique clinical challenge, as it increases the risk of fragility fractures and iatrogenic instability in the postoperative period. Magnetic resonance imaging (MRI)-based vertebral bone quality (VBQ) score and cervical VBQ (C-VBQ) score are two novel approaches that use data routinely gathered during preoperative evaluation to assess bone quality. The goal of this study is to assess the relationship between the VBQ score and the C-VBQ score. Material and Methods: We performed a retrospective chart review on patients undergoing spine surgery for degenerative conditions between 2015 and 2022. Patients must have preoperative T1-weighted MRIs in both the lumbar spine and the cervical spine to qualify for inclusion. Demographic characteristics of each patient were collected. The VBQ score was determined by dividing the median signal intensity (SI) of L1-L4 vertebral bodies by the SI of the cerebrospinal fluid (CSF) at L3 level. The C-VBQ score was calculated by dividing the median SI of C3-C6 vertebral bodies by the SI of C2 CSF space. Pearson’s correlation test was utilized to evaluate the association between the VBQ score and the C-VBQ score. Results: One hundred and seventy-one patients were identified, with a mean age of 57.44 ± 11.79 years. The inter-observer reliability of the VBQ and C-VBQ measurements was good (intraclass correlation coefficient 0.89 and 0.84, respectively). A statistically significant, positive correlation was found between the VBQ score and the C-VBQ score (r = 0.757, p < 0.001). Conclusion: This is the first study to test the correlation between the newly developed C-VBQ score and VBQ score. We found a strong correlation between the C-VBQ score and the VBQ score.
1112
A233: Correlation of craniocervical parameters with the retropharyngeal space in posterior C1-C2 arthrodesis
Luis Eduardo Carelli Texeira da Silva 1 , Alderico Girão Campos de Barros 1 , Fábio Antônio Cabral de Araújo Fagundes 1 , Igor Ebert Cechin 1 , and Gamaliel Gonzalez Atencio 2
1 Instituto Nacional de Traumatologia e Ortopedia Jammil Haddad (INTO), ARCOL, Rio de Janeiro, Brazil
2 Chepo Regional Hospital, Chepo, Panama
Introduction: The craniovertebral junction (CVJ) requires a detailed evaluation, as the changes in alignment caused by surgery can affect adjacent structures in a secondary way. Examples of these effects are dyspnea or dysphagia after posterior occipitocervical arthrodesis, due to decreased caliber of the oropharynx. These changes can be identified perioperatively by several radiographic parameters that aim to predict possible postoperative respiratory complications. Such complications appear to be related to the narrowest oropharyngeal airway space (nPAS), and may also occur following atlantoaxial (C1-C2) arthrodesis. This study aims to correlate the variation in CVJ alignment parameters before and after C1-C2 arthrodesis with the variation in nPAS. Material and Methods: Cross sectional retrospective study of 26 patients who underwent posterior C1-C2 arthrodesis between 2011 and 2019. The parameters evaluated included cervical lordosis, C1-C2 angle, slope of C2, occipito-C2 angle (O-C2), pharyngeal inlet angle (PIA), pharyngeal tilt angle (PTA), occiput and external acoustic meatus to axis angle (O-EAa), cranial transverse motion against C2 angle (C2TA), axial tilt (AT) and the percentage of change in nPAS (%∆nPAS). The statistical analysis was performed using the software program R®, version 4.0.2. Multiple linear regression was performed by correlating the variation in radiographic parameters and the percentage variation in nPAS. Results: The mean age was 40.34 (6 to 62) years. Basilar invagination represented the most common diagnosis, present in 18 (69%) patients. 3 (11%) cases of neglected Grisel syndrome, 2 (8%) odontoid fractures, 1 (4%) atlantoaxial spondylodiscitis,1 Chiari malformation (4%) and 1 altas fracture (4%). The investigation of associated factors was carried out using multiple linear regression variables. Only the variation of C1-C2, OC2, PTA and C2TA showed a statistically significant correlation with %∆nPAS. ∆C1-C2: C1-C2 angle variation; ∆C2-C7: Cervical Lordosis variation; ∆CS: C2 slope variation; ∆OC2: occipito-C2 angle variation; ∆PIA: Pharyngeal inlet angle variation; ∆PTA: Pharyngeal tilt angle variation; ∆O-EAa: occiput and external acoustic meatus to axis angle variation; ∆C2TA: cranial transverse motion against c2 variation; ∆AT: axial tilt variation. Through graphical analysis (Figure 4) and through the Shapiro- -Wilk test (Value - p = 0.090), attributing a significance level of 5%, it is possible to obtain statistical evidence that the residuals have a normal distribution. Conclusion: The change in cervical alignment and CVJ parameters is correlated with %∆nPAS and should, therefore, be evaluated before and after atlantoaxial fusion as a means of predicting a possible respiratory complication.
182
A234: Osteosarcopenia in the spine beyond bone mineral density: association between paraspinal muscle impairment and advanced glycation endproducts
Henryk Haffer 1,2 , Maximilian Muellner 2 , Erika Chiapparelli 2 , Yusuke Dodo 2 , Jiaqi Zhu 2 , Yi Xin Han 3 , Eve Donnelly 3 , Ek Tsoon Tan 4 , Jennifer Shue 2 , Andrew Sama 2 , Frank Cammisa 2 , Federico Girardi 2 , and Alexander Hughes 2
1 Center for Musculoskeletal Surgery, Charité – Universitätsmedizin, Berlin, Germany
2 Spine Care Institute
3 Department of Materials Science and Engineering, Cornell University, Ithaca, United States
4 Radiology, Hospital for Special Surgery, New York, United States
Introduction: Impaired bone integrity and muscle function are commonly described as osteosarcopenia. Osteosarcopenia is associated with falls, physical disability, fragility fractures and reduced quality of life. Bone integrity is influenced by bone quantity (bone mineral density) and quality (turnover, microarchitecture and collagen). The accumulation of advanced glycation endproducts (AGEs) by non-enzymatic collagen cross-linking stiffens collagen fibers and increases bone fragility. Despite the increasing challenges osteosarcopenia poses on healthcare systems for aging societies, the relationship between lumbar muscle composition and bone collagen properties has not been evaluated. We hypothesized that an accumulation of AGEs, a marker of impaired bone quality, is associated with impaired muscle composition (increased intramuscluar fat) in patients undergoing spinal fusion surgery. Material and Methods: A cross-sectional analysis using prospectively collected data of patients undergoing posterior lumbar spinal fusion from from 2014 to 2021 for degenerative conditions was conducted. The study was approved by the institutional review board and informed consent was obtained from all patients. Preoperative MRI measurements at level L4 included the musculus (m.) psoas and combined m. multifidus and m. erector spinae (posterior paraspinal musculature, PPM). Manual muscle segmentation on axial T2-weighted images (cross-sectional area, CSA) using ITK-SNAP and subsequent calculation of an automated pixel intensity threshold method to differentiate muscle (functional cross-sectional area, fCSA) and intramuscular fat (FAT). Intraoperative bone biopsies from the posterior superior iliac spine were obtained and evaluated with multiphoton microscopy for fluorescent AGE crosslink density (fAGEs). Quantitative computed tomography (QCT) measurements were performed at the lumbar spine categorizing patients with volumetric bone mineral density (vBMD) 80 mg/cm3 ≤ vBMD ≤ 120 mg/cm3 as osteopenic and vBMD < 80 mg/cm3 as osteoporotic. Correlations between fAGEs (trabecular and cortical) and paraspinal muscle morphology parameters (CSA, FAT, fCSA) were assessed with Spearman’s ρ. Multivariable linear regression models with adjustments for age, sex, body mass index (BMI), race and diabetes mellitus were used to investigate associations between fAGEs and paraspinal musculature. Results: 107 prospectively enrolled patients (50.5% female, mean age 60.7 years, median BMI 28.9 kg/m2) were analyzed. 41.1% and 15.0% of the patients demonstrated osteopenia and osteoporosis in the lumbar spine, respectively. CSA and fCSA in psoas musculature and fCSA in PPM were significantly lower in females compared to males. Univariate linear regression analysis demonstrated a significant association between cortical fAGEs and CSA in the m. psoas (ρ = 0.220, p = 0.039), but not in the PPM. Trabecular fAGEs revealed no significant associations to PPM or psoas musculature. In the multivariable analysis, higher cortical fAGEs were associated with increased FAT (β = 1.556; p = 0.002) and CSA (β = 1.305; p = 0.005) in the PPM after adjusting for covariates. Conclusion: This is the first investigation demonstrating that an accumulation of non-enzymatic collagen cross-linking product fAGEs in cortical bone is associated with increased intramuscular fat in the lumbar paraspinal musculature. Our findings elucidate the relationship between bone collagen modifications and paraspinal muscle composition. This might reflect crucial interactions contributing to osteosarcopenia in the spine beyond bone mineral density.
OP27: Surgical biomechanics 1
411
A235: The role of trabecular, ligamentous-intervertebral disk and facet joints systems: a finite element analysis in The L4-S1 vertebrae
Alejandro Guerrero 1,2 , Pablo Sanchez Quinones 2,3 , Humberto Madrinan-Navia 2,3 , and Leonardo Laverde 2,3
1 Mechanical Engineering Department, Universidad ECCI, Bogotá, Colombia
2 Neurosurgery Department, Center for Research and Training in Neurosurgery CIEN, Bogotá, Colombia
3 Neurosurgery Department, Hospital Universitario de La Samaritana, Neurosurgery Department, Bogotá, Colombia
Introduction: The arrangement of trabecular bone in the vertebrae is critical for the distribution of load and stress throughout the neuroaxis, as well as the role of intervertebral disk, ligamentous complex and facet joints. The objective of this study was to assess the load and stress distribution of the L4-S1 vertebral segment by a finite element analysis (FEA) in neutral, flexion, and extension positions, by describing the role of a trabecular, ligamentous-intervertebral disk and facet joints systems. Material and Methods: A healthy lumbosacral spine (L4-S1) model was built based on a computed tomography through an assisted design program CAD - Materialisse (Belgium). The anatomic structures included in the model were the main components of the vertebrae with trabecular-to-cortical bone distribution, ligaments, intervertebral disk with both nucleus pulposus and annulus fibrosus, and facet joints (FJ) with cartilage. We simulated a perpendicular force applied over the upper terminal plate of the L4 vertebra of 300N, 460N and 600N, in neutral, flexion and extension moments of 5 Nm and 7.5 Nm. Both models were solved by means of FEA in ANSYS (USA). Maximum principal stress (MPS) and total deformation (TD) were the main studied variables. Results: The FEA in neutral, flexion and extension moments, showed higher values of load stress in the vertebral body (30%), followed by pedicles (18.5% each), pars interarticularis (8.5% each), facet joints (10%) and spinous process (6%). Overall, greater values of TD were achieved in trabecular bone model compared to only cortical bone model, as well as lower values in MPS. This phenomenon confers capacity of resistance to axial loads in the vertebrae by optimizing elastic capacity and stress distribution throughout the vertebral segment, without an early breaking point. Interestingly, MPS and TD showed axial stress attenuation in the nucleus pulposus and longitudinal ligaments, as well as load distribution capacity. Facet joints and discontinuous ligaments (Flavum, intertransverse and interspinous ligaments) showed greater TD values in flexion moments but greater MPS values in extension, both at 5 and 7.5 Nm, conferring stability capacity to the lumbosacral junction, as well as axial load distribution capacity by the facet joints. Conclusion: We propose three anatomical systems for axial load distribution and stress attenuation in the lumbosacral junction. Trabecular bone distributes loads in a sequential manner through the vertebrae, while the ligamentous-intervertebral disk is necessary for transmission and attenuation of axial stress. Facet joints and discontinuous ligaments act as stabilizers for flexion and extension postures. Overall, the relationship between trabecular bone, ligamentous-intervertebral disk complex and facet joints is necessary for an efficient load distribution and segmental axial stress reduction during neutral, flexion and extension moments.
1693
A236: The effect of screw PMMA augmentation on the primary stability of different implants used in OLIF surgery with normal, and osteoporotic bone quality - a finite element assisted study
Ferenc Bereczki 1,2 , Máté Turbucz 1,2 , Ágoston Jakab Pokorni 1,2 , Marton Ronai 3 , Aron Lazary 1,4 , and Peter Eltes 1,4
1 National Center for Spinal Disorders, Buda Health Center, In Silico Biomechanics Laboratory, Budapest, Hungary
2 School of PhD Studies
3 Department of Spine Surgery, National Center for Spinal Disorders, Buda Health Center, Budapest, Hungary
4 Department of Spine Surgery, Department of Orthopaedics, Semmelweis University, Budapest, Hungary
Introduction: Oblique lumbar interbody fusion (OLIF) is becoming more accepted, and popular with spinal surgeons as a minimally invasive surgical technique. Due to its minimal invasiveness, it can be ideal for older population, with numerous comorbidities and decreased bone quality. After cage insertion, stabilisation can be achieved with bilateral pedicle screws (BPS), which requires additional incisions and longer operative time, or self-anchoring stand-alone lateral plate systems (SSA) can be used where no additional incision is required. The primary stability of these constructs plays an important role in the long-term success of the surgery. In the aforementioned older population PMMA augmentation is often used to reinforce screws inside osteoporotic bone. The aim of this study was to investigate the effect of screw augmentation on the primary stability of different implants used in oblique lumbar interbody fusion with normal and osteoporotic bone quality using finite element analysis. Material and Methods: Based on a CT scan of a 24-year-old healthy male an L2-L4 bi-segmental finite element model was created and validated with different bone material properties. Geometries based on the OLIF implants were created, and inserted inside the L3-L4 motion-segment with increasing volumes of PMMA augmentation. The following simulation setup was used: For the first step, 400 N follower load was applied on the instrumented models, then 10 Nm torque was used on the L2 vertebra in flexion/extension, left/right bending, and rotation. The same setup was used in normal, and osteoporotic bony conditions. Results: In the case of global segmental L3-L4 ROM (range of motion) BPS system had smaller values compared to SSA system. Due to osteoporosis all ROM values, and the difference between the two constructs were increased. With increasing amount of PMMA volume/screw augmentation the difference between the constructs decreased. At 3 cm3 injected PMMA/screw, the difference between augmented SSA, and standard BPS were comparable in osteoporotic bone. In the case of osteoporosis, the caudal displacement of the inserted cage was increased in both constructs (BPS had in general 24% less displacement). After 3 cm3 PMMA/screw augmentation the difference between the constructs decreased by 30%. The average screw tip displacement was also increased in porotic bone during the 6 general movements (BPS: 40%, SSA: 61%). PMMA augmentation decreased these values by 34% on average, showing a stabilizing effect on the screws inside the osteoporotic vertebra. Conclusion: Based on the results, the BPS system provides more primal segmental stability compared to SSA system, and the presence of osteoporosis further increases these differences. Screw augmentation in TLIF surgeries are commonly used, however in OLIF lateral plate systems are a fairly new concept. OLIF screw augmentation has the possibility to reduce the observed differences in primary stability between the two investigated constructs, and this effect seems to correlate with the amount of PMMA injected. However, further in silico, and possibly in vitro testing is required to thoroughly understand the investigated biomechanical aspects.
847
A237: The change in lordosis from the standing to lateral position: implications for lateral interbody fusion
Emily Mills 1 , Jennifer Wang 1 , Brian Chung 1 , Lucas Mayer 1 , Mary Richardson 1 , Andy Ton 1 , Raymond Hah 1 , and Nathanael Heckmann 1
1 Orthopaedic Surgery, Keck School of Medicine of USC, Los Angeles, United States
Introduction: Lateral interbody fusion (LLIF) is increasing in popularity. However, the change in lordosis between standing radiographs and lateral positioning has not been established. Here, we sought to establish the correlation between lumbar lordosis (LL) in the standing and lateral decubitus positions. Material and Methods: Fifty subjects, 25 male and 25 female, without prior hip or spine disease were prospectively recruited to participate in this study. Three lateral radiographs were obtained: standing, relaxed seated, and lateral decubitus. Radiographic variables measured included lumbar lordosis (LL) and motion at each lumbar level (L1-L2, L2-L3, L3-L4, L4-L5, L5-S1). The motion through each lumbar segment was calculated as the change in angle between a standing position and the lateral and sitting positions. Each segment’s contribution to overall lumbar motion was calculated as the ratio of the individual segment to the overall lumbar lordosis. The correlation between standing and sitting compared to lateral lordosis was calculated. Additionally, the correlation between the change in lumbar lordosis (ΔLL) when going from standing to seated and ΔLL when going from standing to lateral was calculated. Finally, the correlation between standing pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS) and the ΔLL when going from standing to lateral was calculated. A p-value of < 0.05 was considered significant. Results: Subjects had an average age of 25.70 ± 2.34 years and body mass index (BMI) of 24.10 ± 3.02 kg/m2. On average, 11.86 ± 8.22° (range -7-29°) of lumbar lordosis was lost when transitioning from a standing to the lateral decubitus position. Standing lumbar lordosis had a higher correlation with lateral decubitus lumbar lordosis than seated lumbar lordosis (standing R = 0.725, p < 0.001; relaxed seated R = 0.434, p < 0.001). The segment with the maximal change in LL when transitioning from a standing to the lateral decubitus position was most often at the segment of maximal lordosis when standing (25/50, 50%), although there was significant variability. There was no correlation between the ΔLL when going from standing to sitting and ΔLL when going from standing to lateral (R = 0.08, p > 0.05). There was no correlation between standing PT, SS, or PI and ΔLL when going from a standing to lateral position (all p > 0.05). Conclusion: Standing lordosis was strongly correlated to lateral lordosis, although subjects lost an average of 11.86° from the standing to the lateral decubitus position. This has important implications for fusion in the lateral position.
836
A238: Decreased hip motion is associated with inferior spine outcomes
Emily Mills 1 , Jennifer Wang 1 , Joshua Sanchez 1 , Gabriel Bouz 1 , Andy Ton 1 , Annabel Kim 1 , Jeffrey C. Wang 1 , Ram Alluri 1 , Nathanael Heckmann 1 , and Raymond Hah 1
1 Orthopaedic Surgery, Keck School of Medicine of USC, Los Angeles, United States
Introduction: Decreased motion through the lumbar spine leads to significantly higher rates of prosthetic dislocation following total hip arthroplasty (THA). However, data on the relationship between decreased hip motion and spine outcomes is not well understood. This study aims to determine if decreased hip motion is associated with patient reported outcomes in patients presenting for evaluation of their lumbar spine. Material and Methods: A prospectively-collected database of consecutive patients presenting to spine clinic for evaluation of their lumbar spine at a single institution was retrospectively reviewed. Both patients who had undergone previous fusion and those presenting for initial evaluation of their lumbar spine were included. Standing and sitting lateral radiographs were measured for pelvic femoral angle (PFA). The change in this parameter (ΔPFA) is commonly used as a measure of hip motion. Oswestry Disability Index (ODI) was recorded for each patient. Patients in the lowest 20th percent of motion for ΔPFA were compared to the remaining patients. Multivariate analysis was performed controlling for age, gender, body mass index (BMI), and history of lumbar surgery. Results: Ninety-nine patients were included with an average age of 59.7 ± 16.3 years and BMI of 28.4 ± 5.38 kg/m2. The average ΔPFA for the cohort was 59.0 ± 16.6°. The lowest 20th percentile for ΔPFA (mean ΔPFA 33.4° ± 10.7°) had an average ODI of 51.5 ± 23.9, which was significantly greater than the remaining patients (mean ODI 33.6 ± 19.6) (p < 0.001). After controlling for confounders, patients who fell into the bottom 20th percentile of ΔPFA were 3.97 times more likely to have an ODI above the median (95% CI 1.22-12.93, p = 0.022). Conclusion: Decreased hip motion is correlated with inferior patient reported outcomes in patients presenting for evaluation of their lumbar spine.
913
A239: Dynamics of C1-C2 rotation related to age, sex and smoking- a population study of 308 patients
Jan Lodin 1 , Petr Vachata 1 , Martin Sameš 1 , and Jan Terč 2
1 Neurosurgical Department
2 Radiological Department, Masaryk Hospital Krajská Zdravotní a.s., Ústí nad Labem-Severní Terasa, Czech Republic
Introduction: Posterior C1/2 fixation is a popular and stable means of achieving C1/2 stability for traumatic and degenerative diseases of the cervicocranial junction. The main drawback of this technique is major limitation of cervical spine rotation, however the degree of this limitation has not been quantified based on demographic parameters including sex and age. Material and Methods: A total of 308 patients undergoing head and neck CT performed maximal tolerable right and left head rotation. The degree of C0-C1, C1-C2 and total cervical spine rotation were measured. C1-C2 rotation, total cervical spine rotation and the percentage of C1-C2 rotation were compared between three age groups (< 50, 50-70 and > 70 years of age). Furthermore, all three variables were compared between males and females, smokers and non-smokers. Nineteen patients underwent these measurements twice to determine result repeatability. Results: Statistically significant differences in C1-C2 rotation and total cervical spine rotation were discovered between all three age groups. C1-C2 rotation progressively decreased from a mean value of 64.4° to 50.2° and total cervical spine rotation decreased from a mean value of 131.2° to 103.2°. The percentage of C1-C1 from total cervical spine rotation did not significantly differ between age groups and was stable at 49-51%. Significant differences in the dynamic of C1-C2 and total cervical spine rotation for both sexes. In the age interval 27-68 years C1-C2 rotation decreases at a lower rate in women compared to men. Smoking did not significantly affect C1-C2 rotation. Nineteen patients underwent measurements C1-C2 rotations twice with a mean difference of 2.4° between two measurements. Conclusion: The price of posterior C1/2 junction fixation is a major decrease in total cervical spine rotation. However, the degree of this decrease as well as its dynamics throughout the population have not yet been quantified. Results of this study have allowed us to quantify the degree of C1-C2 rotation at various ages for both sexes and thus allow us to improve our decision making for cases requiring C1/2 fixation. Contrary to many opinions, C1-C2 rotation remains quite significant in the elderly patient group.
865
A240: Percutaneous juxtapedicular cement salvage of failed pedicle screws: a cadaveric biomechanical study
David Kurland 1 , Matin Lendhey 2 , Nader Delavari 1 , Jalen Winfield 3 , Jonathan Mahoney 2 , Brandon Bucklen 2 , and Anthony Frempong-Boadu 1
1 NYU Langone Health, Neurosurgery
2 Globus Medical Inc.
3 Drexel University, School of Biomedical Engineering, Science, and Health Systems, Philadelphia, United States
Introduction: Posterior spinal fixation with pedicle screw-based constructs is the gold standard for stabilizing the thoracolumbar spine; however, these constructs sometimes fail due to fatigue loading, necessitating revision surgery. Hardware revision strategies involve open surgery for screw upsizing, with or without cement augmentation, and extension of fusion. Others have described good clinical outcomes following percutaneous juxtapedicular cement salvage of failing pedicle screws. The relative biomechanical properties of these various approaches have not been evaluated. The objective of this study is investigate the biomechanical strength of juxtapedicular cement salvage of failed thoracic and lumbar pedicle screws, and to compare it to three other common revision techniques. Material and Methods: Thirty-two fresh, un-embalmed vertebrae from four cadaveric thoracolumbar spines were used for the study. The study was conducted in two phases. The first phase involved primary pedicle screw insertions and pullout strength testing to simulate critical pedicle screw failure. The second phase involved revision of the simulated failed pedicle screws followed by pullout testing. The four revision cohorts were: 1) Screw Upsizing: Failed primary screw was removed and a new larger diameter screw was implanted in preexisting screw canal; 2) Vertebroplasty: Failed primary screw was removed, bone cement was injected in the preexisting screw canal and a same diameter new screw was implanted; 3) Fenestrated Screws: Failed primary screw was removed and a same diameter fenestrated screw was inserted and augmented with cement; 4) Juxtapedicular Cement Salvage: Failed primary screw remained engaged in the vertebral body which was augmented with cement using a novel juxtapedicular cementing technique. Results: There was no statistically significant difference in primary fixation strength between the cohorts. The Screw Upsizing cohort exhibited inferior pullout strength compared to the other groups which involved cement augmentation. There was no significant difference in pullout strength between Vertebroplasty, Fenestrated Screws, or Juxtapedicular Cement Salvage cohorts. Conclusion: Cement augmentation confers superior pullout strength compared to screw upsizing only. The key finding of this study is that the technique of percutaneous juxtapedicular cement salvage is biomechanically non-inferior to other revision strategies that require an open procedure to perform.
1547
A241: Biomechanical and minimum one year clinical results of a novel 3-D expandable cage for lumbar interbody fusion
Richard Fessler 1
1 Neurosurgery, Rush University Medical Center, Chicago, United States
Background/Context: Transforaminal lumbar interbody fusion (TLIF) is the most frequently lumbar fusion operation. However, due to anatomical constraints the size of the cage which can be inserted into the disc space is limited. The consequence of this is minimal endplate surface interface with the cage. Attempts have been made to compensate for this but no cage has successfully accomplished expansion in both the sagittal and axial plane. To accomplish greater endplate surface interface, anterior lumbar interbody fusion (ALIF) has been a frequently chosen surgical alternative. Purpose: Examine both the biomechanical characteristics and clinical outcome of a novel lumbar cage which expands in both the sagittal and axial planes. Study Design/Setting and Patient Series: Twelve cadaveric spine specimens (L1-L5) were tested intact and after implantation of both control and open experimental devices in two (L2-L3 and L3-L4) segments of each specimen, alternating assignment levels. Moments were applied to the specimens in flexion-extension (FE), lateral bending (LB) and axial rotation (AR). The effect of physiologic preload on construct stability was evaluated in FE. Segmental motions were measured using an optoelectronic motion measurement system. This patient series consisted of 47 consecutive patients with one year follow up. 55 % received a non-lordotic expandable cage and 45 % received a lordotic expandable cage. 53 % were male and 47 % were female. Mean age was 61 years old. Variables measured at pre-op and one year were: segmental lordosis (SL), lumbar lordosis (LL), disc height (DH), back pain VAS (BP), leg pain VAS (LP), and Oswestry Disability Index (ODI). Results: FE motion was significantly reduced by the TLIF cage compared to the intact condition (p < 0.05). Segmental motions in LB and AR were also significantly reduced with both devices (p < 0.05). Under no pre-load, the expandable TLIF cage resulted in significantly smaller FE motion compared to the control cage (p < 0.01). Under all other test-modes, the postoperative motions of the constructs did not differ statistically. Lordosis was maintained between pre-op and post-op both segmentally and globally for both the lordotic and non-lordotic cages (p > 0.05). DH increased significantly for both groups (p < 0.001). BP and LP improved significantly for both groups (BP Lordotic p < 0.001; BP Non-lordotic p < 0.008; LP Lordotic p < 0.004; LP Non-lordotic p < 0.002). ODI also improved for both groups (Lordotic p < 0.001; Non-lordotic p < 0.07). Conclusions: The ability of the expandable interbody cage in reducing segmental motion was equivalent to the control cage. Lordosis was maintained using either a lordotic or non-lordotic cage. Clinical results excellent relief of BP and LP as well as ODI at one year. The larger footprint of the expandable TLIF cage combined with the preservation of the anterior soft-tissue tension band may provide a better biomechanical fusion environment, combining the advantages of the traditional ALIF and TLIF approaches.
596
A242: Open-pore titanium grid cage versus standard full titanium cage for interbody fusion: an experimental study using an instrumented model in sheep regarding radiographic, biomechanical and histological outcomes
Tuna Pehlivanoglu 1 , Bahadir Gokcen 1 , Kursat Kara 1 , O. Nuri Eroglu 1 , Ufuk Aydinli 1 , and Cagatay Ozturk 1
1 Liv Hospital Ulus, Dept. of Orthopaedic Surgery, Liv Spine Center certified by AOSpine, Dept. of Orthopaedic Surgery, Liv Spine Center certified by AOSpine, Istanbul, Turkey
Introduction: New generation porous coated cages with improved osteoconductivity and stability were shown to provide great success in terms of interbody fusion. The aim of the present animal study as to compare two designs of TLIF cages (Structural Titanium (open-pore titanium grid structure) vs. Standard Full titanium) by means of osseointegration, overall bone formation around the implants and bone-implant contact lines by conducting radiographic, biomechanical and histologic analysis. Materials and Methods: Twenty-four merino sheep underwent lumbar interbody fusion at the levels of L3-4 and L4-5 with one level placed with new generation structural, open-pore titanium grid cage (ST-cage) and the other level with standard full titanium cage (FT-cage) combined with 3-levels of pedicle screw placement. In half of the sheep, ST-cages were placed at L3-4 and FT-cages were placed at L4-5. In the other half of the animals, vice versa. One third of animals (8) were euthanatized at 4th week, 1/3 (8) at 8th week and the rest (8) at 12th week. Lumbar spines were removed en-bloc followed by X-ray, CT scan aimed to evaluate the quantitative amount of radiographic fusion by measuring bone volume fraction (in all 8), biomechanical pull-out tests aimed to evaluate mechanical stability by measuring micromotion (in 5 of 8) and histological analysis aimed to evaluate osseointegration and overall bone formation in a subsequent order by assessing bony ingrowth (in remaining 3 of 8). Results: CT analysis, at the end of 4th, 8th and 12th week revealed a fusion rate of 87.5% - 100% (p < 0.001) - 100% (p > 0.05) for ST-group and 50%-75% (p < 0.001)-75% (p = 0.27) for FT-group, indicating the significant improvements of fusion from 1st to 2nd month, while rates of fusion remained constant from 2nd to 3rd month. Significant superiority (p < 0.001 for all weeks) of fusion in ST-group in terms of fusion was noted. Biomechanical tests revealed, that the mean pull-out strength of ST and FT groups significantly increased from 4th week to 8th week (p = 0.003) and significantly dropped from 8th week to 12th week (p < 0.001). At all times of biomechanical testing, ST-group was detected to have significantly superior maximum pull-out strength as compared to FT-group (p < 0.001 for all weeks). Histological examination revealed significant improvements of bony ingrowth at all weeks in both groups, while ST-cages provided a significantly faster bony ingrowth with higher quality and significantly less fibrous-connective tissue adjacent to implants at the 8th and 12th weeks with high statistical significance (p < 0.001 for both) and at the 4th week with low statistical significance (p = 0.032). Conclusions: Both ST and FT groups at the end of 12 weeks showed significant improvements regarding bony fusion, pull-out strengths and bony ingrowth. ST cages characterized with open pore titanium grid structure, were able to provide superior rates of fusion, superior maximum pull-out strength indicating superior stability accompanied with faster osseointegration and less fibrous tissue around the implants indicating less micromotion and better stability, underlining their possible advantages when used in TLIF surgery.
1863
A243: The possible accelerating effect of cranial endplate damaging screws in severe adjacent disc degeneration - a finite element assisted study
Ágoston Jakab Pokorni 1,2 , Ferenc Bereczki 1,2 , Máté Turbucz 1,2 , Zoltan Hoffer 3 , Peter Eltes 1,4 , and Aron Lazary 3,4
1 National Center for Spinal Disorders, Buda Health Center, In Silico Biomechanics Laboratory, Budapest, Hungary
2 School of PhD Studies
3 National Center for Spinal Disorders, Buda Health Center, Budapest, Hungary
4 Department of Spine Surgery, Department of Orthopaedics, Semmelweis University, Budapest, Hungary
Introduction: In spinal fusion surgeries, cranial fusion extension is used to treat adjacent segment degeneration where the pathology greatly impairs the patient’s quality of life. This study aimed to evaluate whether cranial endplate damaging screws can facilitate disc degeneration in the adjacent cranial segment in the lumbar spine based on a patient cohort and finite element modeling. Material and Methods: We investigated the cranial fusion-extension surgeries at the National Center for Spinal Disorders, Budapest, Hungary, between 2012 and 2020, where the index fusion surgery occurred on the lumbar spine (L1-S1 and ileum, n = 471). After the exclusion criteria, n = 199 cases remained in the cohort. The cohort was divided into two groups based on postoperative lateral x-ray scans taken after the index surgery. The cases where the most cranial pedicle screws bordered or penetrated the cranial endplate were placed in Group 1 (Cranial Screw Position (CNS), n = 28), while the other cases were placed in Group 2 (Parallel Screw Position (PSP), n = 171). The time between the index and the cranial fusion-extension surgery was assessed. Finite Element Models (FEMs) of the lumbar spine with different levels of posterior fixation (L2-L3, L2-L4, L2-L5) and positions of pedicle screws (CSP, PSP) in the L2 vertebra were constructed using a validated FEM of the intact lumbar spine. The models were compared at the same displacement using the range of motion (ROM) of the two-level fixation models (L2-L4) against a 400 N follower load and a 7.5 Nm bending moment in flexion, lateral bending, and axial rotation. A region of interest (ROI) for stress distribution was defined as the central part of the L2 vertebra’s cranial endplate. The distributions and maximums of von Mises stress in the ROI were investigated for every model. Results: The minimum, the maximum, and the median of the time between the index and the cranial fusion-extension surgery were 75, 397, and 1840 days in Group 1 and 49, 974, and 4045 in Group 2, respectively. The non-parametric Mann-Whitney U test showed a statistically significant difference (p < 0.005, Z = -5.055) between Group 1 and Group 2 in the median of the days between the two surgeries. The CSP resulted in larger high-stressed areas and higher stress peaks in the ROI for any load case and level of fixation than the PSP. The CSP created 163.1, 178.9, and 165.3 % higher maximum stresses in flexion, 153.6, 151.7, and 165.8 % higher maximum stresses in lateral bending, and 178.0, 193.6, and 174.6 % higher maximum stress in axial rotation at one, two and three levels of fixation, respectively. Conclusion: Based on the investigated cohort, the CSP required reoperation earlier than the PSP, suggesting that the screw position accelerates adjacent disc degeneration. Furthermore, finite element results showed that both the level of fixation and the screw position deeply impacts the stress distributions in the central part of the bony endplate, the CSP providing substantially higher stress peaks.
OP28: Current Management of Metastatic Spinal Disease
1492
A244: Patients with radicular pain improve more than those with axial pain alone following treatment for metastatic spine disease
Arthur Bartolozzi 1 , Ori Barzilai 2 , Dean Chou 2 , Ilya Laufer 2 , Jorrit-Jan Verlaan 2 , Arjun Sahgal 2 , Laurence Rhines 2 , Daniel Sciubba 2 , Aron Lazary 2 , Michael Weber 2 , James Schuster 2 , Stefano Boriani 2 , Chetan Bettegowda 2 , Paul Arnold 2 , Michelle Clarke 2 , Michael Fehlings 2 , Jeremy Reynolds 2 , Ziya Gokaslan 2 , Charles Fisher 1,2 , and Nicolas Dea 1,2
1 University of British Columbia, Vancouver Spine Surgery Institute, Vancouver, Canada
2 AO Spine Knowledge Forum Tumor
Introduction: Pain is an important presenting symptom in patients with metastatic spine disease. Pain can be either axial or radicular, both of which are further defined by etiology as either mechanical (increases with movement and weight bearing) or biological (unrelated to movement). Pain improvement is the most significant driver of quality-of-life scores in this population. It is generally accepted that mechanical axial pain improves with surgical and radiation-based interventions. We sought to delineate how radicular pain specifically responds to cancer treatment. Methods: Patients treated with surgery and/or radiotherapy for spine metastases were identified from the Epidemiology, Process, and Outcomes of Spine Oncology (EPOSO) international multicentre prospective observational study. Two groups were identified: those who reported radicular pain and those who reported axial pain only. Demographic, diagnostic, treatment, and HRQOL measures were collected. The primary outcome was patient pain measured by numeric pain rating scale (NRS) at 3 months post-treatment, referring to an overall pain magnitude rather than to a specific location or type. Patients were excluded if they had no pre-treatment pain or no pain follow-up data available. Standard tests were used for demographic differences and change of pain score over follow-up was analyzed using mixed models for repeated measures. Results: Of 284 patients who met inclusion criteria, 129 (45%) had radicular pain with or without axial pain and 155 (55%) had axial pain alone. Groups did not differ based on age, comorbidities, primary cancer, epidural compression, tumor location, SINS score, and treatment regimen (p > 0.05 for all). 202 (71%) patients had surgery ± radiotherapy and 82 (29%) had radiotherapy alone. Of patients with radicular pain, 93 (72%) had a mechanical component to their pain. Patients with radicular pain reported higher preoperative NRS than patients with axial pain only (p = 0.028). Radicular pain patients’ mean NRS score was 6.7 (95% CI: 6.2; 7.1) at baseline and improved 3.2 points (95% CI: 2.5; 4.0) at 3 months follow-up (p < 0.001). Patients with isolated axial pain had a preoperative mean 5.8 (95% CI: 5.5; 6.2) which improved a mean 2.2 points (95% CI: 1.5; 2.9) over the same interval (p < 0.001). The magnitude of improvement was significantly higher for patients with radicular pain than those with only axial pain (p = 0.041). However, pain at 3 months was similar for both groups (p = 0.97). Patients with radicular pain undergoing surgery ± radiotherapy (n = 95) had higher pretreatment pain (NRS mean 7.0, 95% CI: 6.5; 7.5) than radiotherapy alone (n = 34, NRS mean 5.6, 95% CI: 4.8; 6.5, p = 0.027). Surgical patients with radicular pain experienced a larger improvement (mean improvement 3.8, 95% CI: 2.9; 4.7) than those treated with radiotherapy alone (1.8, 95% CI: 0.3; 3.2, p = 0.015). Patients with isolated biological radicular pain showed similar pain improvement as those with isolated mechanical radicular pain (p = 0.993). Conclusion: The magnitude of improvement for patients with a component of radicular pain following surgery and radiotherapy for metastatic spine disease is higher than patients presenting with axial pain alone. Surgery is associated with a larger improvement in pain scores than radiotherapy alone. No differences were identified based on mechanical or biological pain etiology.
1102
A245: Transpedicular approach is a safe and effective route to achieve separation surgery and circumferential decompression in spinal metastases. Analysis of a multicenter experience
Fabio Cofano 1,2 , giuseppe di perna 1,3 , Salvatore Petrone 2 , Marco Ajello 4 , Nicola Marengo 4 , Marco Bozzaro 2 , francesco zenga 4 , Fulvio Tartara 5 , and Diego Garbossa 1
1 Neuroscience, University of Turin, Italy
2 Spine Surgery Unit, Humanitas Gradenigo Hospital, Italy
3 Spine Surgery Unit, Casa di Cura Città di Bra, Italy
4 Neurosurgery, Città della Salute e della Scienza, Italy
5 Neurosurgery, Istituto Clinico Città Studi, Milan, Italy
Background and Objective: Surgery for spinal metastases has undergone multiple transformations in terms of surgical technique. The need for a more aggressive surgical strategy for local control of the disease, given the advances in radiosurgery and targeted therapies, has met the incorporation of many different technological adjuncts. Separation surgery has become one of the main targets to achieve in the treatment of spinal metastases. Transpedicular approach represents a safe and valuable approach to reach the ventral aspect of the dural sac and achieve circumferential decompression and corpectomy with reduced risks compared to constotransversectomy or anterior lumbar approaches. A case series is described with clinical and radiological outcomes. Methods: Adult patients with a diagnosis of single-level thoracic or lumbar metastases requiring surgery for epidural compression were included. Data recorded for each case concerned patient demographics, surgical technique, clinical, radiological and surgical data, intra- and postoperative complications, follow-up. NSE score was the main reference used in the multidisciplinary management. Results: A total number of seventy-nine patients were treated from January 2018 to April 2022 with a pure transpedicular approach at authors Institutions (73% thoracic, 27% lumbar). A circumferential decompression was achieved in all cases, as well as a proper separation between the tumor and the spinal cord as confirmed by post-operative imaging. Axial pain always improved after the procedure as well as neurological functions, when compromised before surgery, with statistical significance (p < 0.05). Mean hospital stay was 4 days after surgery with early mobilization. Mean follow-up was 19.2 months. Only 3,9% of patients experienced neurological worsening during follow-up. The rate of complications included a post-operative hematoma, 2 wound infections, 2 wound dehiscence and a single case of hardware failure. In 12 cases the procedure was assisted by 3D-endoscope, in 3 cases with the exoscope. Conclusion: Transpedicular approach for separation surgery and corpectomy appeared to be a safe and effective technique to achieve proper circumferential decompression, decreasing then the need for costotransversectomy and its burden in thoracic locations and for anterior approaches to the lumbar spine when body replacement is not mandatory.
420
A246: Factors contributing to delayed surgery in multiple myeloma vertebral column lesions and proposal for a prospective registry
Vanessa Hubertus 1 , Charlotte Buhre 1 , Nitzan Nissimov 1 , Martin Stangenberg 2 , Lennart Viezens 2 , Hanno S. Meyer 3 , Caroline von Bassenheim 1 , Sebastian Schulz 2 , Theresa Keller 4 , David Kaul 5 , Piet Habbel 6 , Igor-Wolfgang Blau 6 , Ulrich Keller 6 , Bernhard Meyer 3 , Marc Dreimann 2 , Peter Vajkoczy 1 , and Julia Onken 1
1 Neurosurgery
2 Division of Spine Surgery, Department of Trauma and Orthopedic Surgery, University Medical Center Hamburg-Eppendorf, Germany
3 Neurosurgery,Technical University, Munich, Germany
4 Biometry and Clinical Epidemiology
5 Radiation Oncology and Radiotherapy
6 Hematology, Oncology, and Tumor Immunology, Charité Universitätsmedizin Berlin and Berlin Institute of Health, Berlin, Germany
Introduction: In advanced stage, more than 50% of Multiple Myeloma (MM) patients suffer from vertebral column lesions. Indications for surgery are made with restraint and often delayed because of an allegedly high complication rate, even in symptomatic and (potentially) instable lesions. The aim of this study is to evaluate potential factors leading to a treatment cross-over from non-surgical to delayed surgical therapy of vertebral column lesions in a large multicentric cohort of MM patients. Material and Methods: Patients with MM vertebral column lesions were enrolled at three academic oncological centers between 2005-2020. Data sets were retrospectively assessed regarding epidemiological, clinical, oncological, treatment and outcome data. Univariate and multivariate logistic regression analyses identifying factors at risk for a cross-over from non-surgical to delayed surgical therapy were performed. Where sufficient imaging follow-up was available (>2 images, >3 months), changes in the sagittal Cobb-angle of index lesions were assessed longitudinally in a group of patients treated with delayed surgery and a matched-pair group of non-surgical patients. Ethical approval (EA4/063/20) was granted. Results: 450 patients were enrolled in this study. Of 308 patients treated surgically, 75 (24%) crossed over from intended non-surgical to delayed surgical treatment at a median of 36 (12-300) months. Univariate and multivariate analyses identified a lower grade in the MM International Staging System (ISS 1 and 2) as significant risk factor for a cross-over to delayed surgery (p = 0.007). Age, clinical status, other oncological factors, and SINS were not statistically significant. Longitudinal changes of >10% in the sagittal Cobb-angle revealed increasing deformity from start to preoperative imaging in more patients in the delayed surgery group (13/24, 55%) than from start to follow-up in the non-surgical group (5/20, 25%, p = 0.0685). Conclusion: With this study, we report on a large multicentric cohort of 450 MM patients of which 24% were treated in a delayed fashion. Uni- and multivariate analyses identified a lower ISS (grade 1 and 2) as risk factor for a cross-over from non-surgical to delayed surgical therapy. An increase of the sagittal Cobb-angle occurred from start to preoperative imaging in more patients in the delayed surgery group than in the matched non-surgical control-group. However, adequate longitudinal imaging follow-up was available only in a subset of patients. Future prospective cohort studies should consider a structured imaging protocol to examine the role of progressive spinal deformity in the surgical management of MM vertebral column lesions.
556
A247: Comparison of different therapies including surgery, stereotactic body radiotherapy, conventional radiotherapy for advanced cancer with spinal metastases: a systematic review and meta-analysis
Yen-Ting Lai 1 , Po-Lung Cheng 2 , Ping-Hsiu Wu 3 , Ching-Yu Lee 4 , Tsung-Jen Huang 4 , Jeng-Fong Chiou 3 , Chih-Sheng Hsu 5 , Hsin-Lun Lee 3 , and Meng-Huang Wu 4
1 School of Medicine, College of Medicine
2 Department of Medical Education
3 Department of Radiation Oncology
4 Department of Orthopedics
5 International PhD Program in Biotech and Healthcare Management, College of Management, Taipei Medical University, Taipei, Taiwan
Introduction: The incidence of spinal metastasis has increased because patients with primary cancer have prolonged survival time due to improved treatments or early diagnosis tools. When there are multiple treatment options available, patients usually choose treatments with a higher survival rate or better quality of life. Thus, in this systematic review and meta-analysis, we aimed to compare common treatments for spinal metastasis: surgery (including open surgery and vertebroplasty), conventional radiotherapy (CRT), and stereotactic body radiotherapy (SBRT). Material and Methods: PubMed and Embase databases were searched to identify potentially eligible studies in the English language. The hazard ratios (HRs) with 95% confidence intervals (CIs) were extracted from included studies and pooled with a random- or fixed-effect model. Results: Forty-three studies (patient number = 5,123) were included and analyzed finally after screening 21,725 studies. The overall analysis showed that CRT was superior to other treatments in 6-month local control rate. SBRT was associated with lower incidence of skeletal-related events and higher pain response rate, 1-year local control rate, 1-year overall survival rate. Surgical therapy showed significantly better performance in regaining ambulatory status and pain score reduction. In subgroup analysis, minimal invasive spinal surgery (MISS) reported the highest 1-year overall survival rate. In addition, patients received additional RT and/or chemotherapy post-intervention had significantly better 1-year overall survival compared with patients received pre-intervention. The most frequent complication reported was cement leakage in the surgical group. Conclusion: SBRT and CRT had better performance in 1-year overall survival rate compared to surgical therapy, while MISS had the highest 1-year OS rate. All therapy showed similar post-intervention ambulatory rate, while surgical group and CRT had significantly higher regaining ambulation rate compared to SBRT. Surgery showed better performance in regaining ambulatory status and reducing pain, provided emergent treatment for neurological deficits and mechanical instability. MISS following by addition RT and/or chemotherapy seems to be a reasonable choice for advanced cancer with spinal metastasis to improve quality of life.
1270
A248: Performance of the SORG machine learning algorithm for patients with spinal metastasis in the presence of missing data
Chi-Ching Huang 1 , Kuang-Ping Peng 1 , Hsiang-Chieh Hsieh 1 , Olivier Groot 1 , Hung-Kuan Yen 1 , Cheng-Chen Tsai 1 1 , Aditya Karhade 2 , Yen-Po Lin 1 , Yin-Tien Kao 1 , Jiun-Jen Yang 1 , Shih-Hsiang Dai 1 , Chuan-Ching Huang 1 , Chih-Wei Chen 1 , Mao-Hsu Yen 1 , Fu-Ren Xiao 1 , Wei-Hsin Lin 1 , Jorrit-Jan Verlaan 3 , Joseph Schwab 2 , Feng-Ming Hsu 1 , Tze Hong Wong 1 , Rong-Sen Yang 1 , Shu-Hua Yang 1 , and Ming-Hsiao Hu 1
1 National Taiwan University Hospital, Taipei, Taiwan
2 Massachusetts General Hospital, Boston, United States
3 University Medical Center, Utrecht, Thw Netherlands
Introduction: The Skeletal Oncology Research Group machine learning algorithm (SORG-MLA) was developed to predict survival of patients with spinal metastasis. The algorithm was successfully tested in five international institutions, using 1,101 patients from different continents. The incorporation of 18 prognostic factors strengthened its predictive ability, but limit its clinical utility since some prognostic factors might not be clinically available in time. Therefore, we aimed at developing a web-application to impute the possible missing data and evaluate the SORG-MLA’s performance in the presence of missing data. Material and Methods: Seven factors, serum albumin and alkaline phosphatase level, international normalized ratio, lymphocyte and neutrophil count, and the presence of visceral or brain metastasis were considered possible missing items based on the reports of previous validation studies and clinical experience. A total of 2,768 patients were included in this study. The data of 617 patients were intentionally erased and the data of the other 2,151 patients were used to impute the artificially missing data with the MissForest imputation technique. Discrimination, calibration, overall performance, and decision curve analysis were applied to evaluate the SORG-MLA’s performance. Results: In general, the SORG-MLA demonstrate good discriminatory ability and overall performance in the presence of 1-3 missing items. However, it tended to underestimate the patients’ s survival. As the number of missing items increased, its discriminatory ability decreased gradually and the gap of underestimation became more significant. The decision curves tangled around when 1-3 items were missed, which might indicate the consistent predictions by the SORG-MLA. Of notice, the algorithm demonstrated suboptimal predictions when albumin and lymphocyte count were missed. Conclusion: The SORG-MLA performed well when the missing items presented, and a web-application was developed (https://sorg-spine-mets-missing-data-imputation.azurewebsites.net/) accordingly. The results suggested the algorithm could be helpful when the radiological survey, due to the lengthy waiting time, could not be performed in time, especially in situations that an early operation could be beneficial. It could help orthopedic surgeons to decide whether to intervene palliatively or extensively although the surgical indication is clear. We recommend future clinicians and researchers to develop prediction models that also allow missing data or provide imputation application as input data is not always available in the real world.
1130
A249: Same-day stereotactic body radiotherapy and pedicle screw fixation for patients with unstable spinal metastases: the BLEND RCT - study protocol for a randomized controlled trial following the trials within cohorts design
Eline Huele 1 , Joanne van der Velden 2 , Nicolien Kasperts 2 , Wietse Eppinga 2 , Joost Verhoeff 2 , Saskia Teunissen 3 , Jorrit-Jan Verlaan 4 , Lenny Verkooijen 1,2 , and Roxanne Gal 1
1 Division of Imaging and Oncology
2 Department of Radiotherapy
3 Julius Center for Health Sciences and Primary Care
4 Department of Orthopedic Surgery, UMC Utrecht, The Netherlands
Introduction: Spinal metastases can lead to unremitting pain and neurological deficits which substantially impair daily functioning and quality of life (QoL). Patients with unstable spinal metastases currently receive surgical stabilization, followed by palliative radiotherapy as soon as wound healing allows. The time between surgery and radiotherapy delays radiotherapy-induced pain relief, local tumor control, and restart of systemic therapy. Implementation of curative radiotherapy techniques for palliative treatments, e.g. stereotactic body radiotherapy (SBRT), enables delivery of high-dose ablative radiotherapy while sparing organs/tissues at risk. SBRT allows for delivery of preoperative radiotherapy while actively avoiding irradiation of the surgical field, and can be followed directly by stabilizing surgery (i.e. the BLEND procedure). This combined same-day procedure provides an extremely short treatment interval of only hours with potentially earlier pain relief, earlier improvement of mobility and faster continuation of systemic therapy. In the BLEND RCT, we evaluate the effectiveness of SBRT followed by surgery within 24 hours for the treatment of symptomatic, unstable spinal metastases. Material and Methods: BLEND is a phase III randomized controlled trial embedded within the PRospective Evaluation of interventional StudiEs on boNe meTastases (PRESENT) cohort. In PRESENT, all patients with bone metastases referred to radiation therapy in university medical center Utrecht are enrolled. Patients with symptomatic, unstable spinal metastases requiring surgery and radiotherapy will be randomized (1:1). The intervention group (n = 50) will be offered same-day SBRT and surgery, which they can either accept or refuse. According to the Trial within Cohorts (TwiCs) design, the control group (n = 50) will not be informed and receive standard treatment (surgery followed by conventional radiotherapy after 1-2 weeks when the wound is healed sufficiently). Baseline characteristics and outcome measures are captured in the context of the PRESENT cohort study. The primary outcome is physical functioning (measured with the EORTC-QLQ-C15-PAL) four weeks after start of treatment. Secondary endpoints include pain response, time until return to systemic therapy, QoL (EORTC-QLQ-BM22, Brief pain inventory, EuroQol EQ-5D-3L), local control and adverse events following up to three months after treatment. Data will be analyzed according to intention-to-treat. In case of high refusal in the intervention arm, per protocol analysis including patients who completed treatment as allocated will be conducted. In addition, a cost-effectiveness analysis will be performed to assess whether the BLEND procedure is cost-effective compared to the standard of care. Results and Conclusion: The BLEND RCT is designed to evaluate the effect of SBRT, with active dose-sparing of the surgical site, followed by surgical stabilization with or without decompression within 24 hours for the treatment of unstable spinal metastases compared with standard of care. The innovative TwiCs design enables efficient recruitment within the context of an ongoing cohort study, as well as prevention of disappointment bias and drop-out, as control patients will not be informed about the trial.
730
A250: The role of mini-invasive surgery (MIS) in symptomatic spinal metastases
Stefano Telera 1 , Laura Raus 1 , Francesco Crispo 1 , Catia Pompea Delfinis 1 , Fabrizio Rasile 1 , Mario Lecce 1 , Laura Marucci 2 , Alessia Farneti 2 , and Roberto Gazzeri 3
1 Neurosurgery
2 Radiotherapy, IRCCS National Cancer Institute Regina Elena, Rome, Italy
3 Pain Therapy, Azienda Ospedaliera San Giovanni Addolorata, Rome, Italy
Background: The combination of surgery and radiotherapy/radiosurgery has been demonstrated to be effective in achieving pain relief, maintaining or restoring ambulatory function and improving overall quality of life in patients with symptomatic spinal metastases. In the last fifteen years significant advancements in radiotherapy and radiosurgery as well as improvements in surgical mini-invasive surgery (MIS) techniques have led to a shift in treatment paradigm for spinal metastases toward less invasive surgical approach and ablative radiation treatments. Methods: A consecutive series of patients affected by symptomatic spinal metastases due to solid and hematological tumors, operated between January 2020 and January 2022 with MIS has been analyzed. Results: During this time frame 35 patients have been operated through MIS approaches involving spinal decompression, open kyphoplasty, augmentation techniques, short percutaneous fixation. Median age was 64 years; 19 females and 17 males. Median Tokuhashi score was 10; median SINS score 13. In 23 cases the level of compression was lumbar, in 12 cased it was dorsal. There was one perioperative death, due to medical issues, in one case there were two durotomy during surgery. Only one patient presented a deterioration of his neurologic conditions, all patients significantly improve their spine pain according to VAS and Dennis Pain Scale. 32 were able to be treated with radiotherapy/radiosurgery within three weeks. No patients presented wound problems. Median LOS was 9 days. Median follow-up was 11 months. Conclusions: The combination of different MIS spinal techniques seem to be very effective to deal with patients with compression and pain in the setting of metastatic spine disease.
1227
A251: Local microstructural properties in the bone tissue surrounding vertebral metastases
Giulia Cavazzoni 1,2 , Silvia Casadei 1 , Luca Cristofolini 1 , Giovanni Barbanti Bròdano 3 , Enrico Dall'Ara 2 , and Marco Palanca 1,2
1 Department of Industrial Engineering, University of Bologna, Bologna, Italy
2 Department of Oncology and Metabolism, University of Sheffield, Sheffield, United Kingdom
3 Department of Spine Surgery, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Load-bearing capacity of the spine is ensured by the optimized architecture of vertebral bone tissue. However, bone metastases alter the local bone mineral density (lower in case of lytic metastases and higher for blastic metastases) and the bone microstructure [1]. The resulting change in local material properties affects the distribution of stresses within the structure and the share of load on the different regions. Consequently, also the mechanical stimuli that drive the bone remodelling process are altered [2]. Nevertheless, little is known about to what extent the tissue surrounding metastatic lesions is affected. This study aims to evaluate the effects of focalized metastases (lytic, blastic or mixed) on the tissue microstructure in regions close and far from the metastatic lesion. Materials and Methods: Healthy vertebrae (n = 9) and vertebrae with lytic (5), blastic (2) and mixed (4) metastases were obtained from an ethically approved donation program. Each specimen was scanned with a micro-Computed Tomography (CT) scanner (VivaCT80, Scanco, isotropic voxel size of 39µm). The volumes of the lytic and the blastic lesions were manually segmented (VOI_0). A series of volumes of interest was then created as concentric enlargement of 100 voxels (3.9 mm) of VOI_0, within the volume of the vertebra. The microCT images were analysed (CTAn, Bruker SkyScan) to compute the following 3D microstructural parameters: Bone Volume Fraction (BV/TV), Trabecular Thickness (Tb.Th.), Trabecular Spacing (Tb.Sp.) and Trabecular Number (Tb.N.) in each VOI. Results: Median values for entire healthy vertebrae were: BV/TV (9 ± 2%), Tb.Th. (159 ± 7 µm), Tb.Sp. (1039 ± 134 µm) and Tb.N. (0.54 ± 0.2 1/mm). In correspondence of the lytic lesion in both vertebrae with lytic and mixed metastases, the lowest values for BV/TV (1 ± 0.04%), Tb.Th. (128 ± 13 µm) and Tb.N. (0.17 ± 0.2 1/mm) and the highest Tb.Sp. (1987 ± 452 µm) were found. The highest values for BV/TV (58 ± %), Tb.Th. (267 ± 18 µm) and Tb.N. (2.18 ± 0.45 1/mm) and lowest values for Tb.Sp. (262 ± 80 µm) were found in correspondence of the blastic lesions. Significant differences were found in BV/TV, Tb.Th. and Tb.N. between metastatic and control vertebrae (p < 0.05). No significant differences were found between the microstructural parameters in the regions close and far from the lesion, for both lytic and blastic cases. Conclusions: Despite the overall changes in the microstructure in the metastatic vertebrae with respect to healthy ones, the regions close to the metastases showed microstructural properties similar to those observed in the regions far from the metastases and in healthy vertebrae [3,4] highlighting the localized impact of the metastases.
Ackowledgments
The study was partially funded by AOSpine (AOSDIA_2019_063), Marie Skłodowska-Curie (MSCA-IF-EF-ST, 832430/2018) and EPSRC Multisim Grant (EP/K03877X/1 and EP/S032940/1).
References
1. Burke et al. Journal of the mechanical behavior of biomedical materials 2017.
2. Selvaggi et al. Elsevier Oncology/Hematology 2005.
3. Nägele et al. Calcified Tissue International 2004.
4. Sone et al. Bone 2004.
1084
A252: Micro-finite element modelling can predict the mechanical behaviour of vertebrae with metastases
Marco Palanca 1,2 , Giulia Cavazzoni 1,2 , and Enrico Dall'Ara 2
1 Dept of Industrial Engineering, Alma Mater Studiorum - University of Bologna, Bologna, Italy
2 Dept of Oncology and Metabolism, The University of Sheffield and INSIGNEO Institute for in silico medicine, Sheffield, United Kingdom
Introduction: Evaluation of the risk of fracture in vertebrae with metastases is a multifactorial problem that experimental studies and retrospective studies have not completely addressed [1]. The main reason is that the heterogeneity of the bone and lesion microstructure is not considered. Finite Element models based on high resolution images (micro-FE) can help researchers understanding the influence of microstructural parameters and lesion’s properties (e.g. size and location) on the vertebral strength and local deformation [2]. However, before considering reliable a computational model, its validation is mandatory. The aim of this study is to validate the ability of micro-FE models in predicting displacement field of human vertebrae with and without metastases under realistic loading conditions. Materials and Methods: Six spine segments, consisting of a vertebra with lytic (4) or blastic (2) metastases and the adjacent healthy (6) vertebra as a control, were mechanically tested. Each spine segment was scanned twice in a micro-computed tomography (Scanco VivaCT80, isotropic voxel size = 39 micrometers): first in unloaded condition and then under a physiological axial load. A global Digital Volume Correlation (DVC) approach [3] was used to measure the displacement field inside the vertebral body with a measurement spatial resolution of 1.95 mm. Linear elastic micro-FE models of the metastatic and control vertebrae were generated from the unloaded scans [4] (element size: 39 micrometers; elastic modulus: 12GPa; Poisson’s ratio: 0.3; regardless the tissue type). The same loading conditions of the experiments were applied to the metastatic and control vertebrae. The predicted local displacements (ANSYS, APDL) within the vertebral bodies were compared to the experimental DVC measurements (linear correlation). Results: The displacements measured by DVC ranged from 15 to 550 micrometers. In particular, the displacements measured in the metastatic vertebrae were larger that the those in the control vertebrae, due to their lower stiffness. Fair-to-excellent agreement was found between the predicted and measured displacements both for metastatic (vertebrae with lytic lesions: 0.64 < R2 < 0.88, vertebrae with blastic lesions: 0.82 < R2 < 0.95) and control (0.44 < R2 < 0.91) vertebrae. Conclusions: For the first time this study confirmed that linear micro-FE models predict accurately the local deformation of human vertebrae with blastic and lytic lesions. These validated models can now be used to evaluate the effect of bone microstructure and lesion’s properties on the mechanical properties of the vertebral body.
Acknowledgments
The study was partially funded by AOSpine (AOSDIA_2019_063), Marie Skłodowska-Curie (MSCA-IF-EF-ST, 832430/2018) and EPSRC Multisim Grant (EP/K03877X/1 and EP/S032940/1).
References
1. Confavreux et al. Cancers 2021; 13: 5711.
2. Costa et al. Bone Rep 2020.
3. Dall’Ara et al. Front.Mater 2017; 4: 31.
4. Palanca et al. J Mech Behav Biomed Mater 2022; 125: 104872.
OP29: Minimally Invasive Spine Surgery
637
A253: The incidence of complications in split tubular, endoscopic and robot-assisted endoscopic TLIF: there is a difference
Michael Gerling 1 , Melissa Baker 1 , Eloise Stanton 2 , Evan Chaladoff 1 , and Zorica Buser 1
1 Gerling Institute, Brooklyn, United States
2 Keck School of Medicine, Los Angeles, United States
Introduction: With the advancements in the field of spinal surgery, fusion procedures have substantially increased and have led to the improvement of minimally invasive Transforaminal Lumbar Interbody Fusions (TLIFs) and its application in outpatient care centers. The aim of the current study was to compare the incidence of post-operative complications between tubular, endoscopic and Robot-assisted TLIF. Material and Methods: Patients who underwent single or multi-level TLIF between 2020 and 2022. Demographic and intra-operative variables (type of TLIF, levels, surgery time, blood loss, length of stay) were recorded. Data on post-operative complications was collected at 2 weeks, up to 3 months, 6 months and 1 year. ODI and CAT domains at different time points were collected. One way ANOVA with Bartlett’s equal-variance test was used to compare demographics and intra-op variables among three approaches. Complication rates between three procedures were compared using Pearson chi-squared test. Results: The current study included 137 patients undergoing TLIF. 57% were tubular, 28% were endoscopic, and 15% were Robot-assisted. The average age of the patients who underwent tubular was 50.73 ± 10.93 years, endoscopic 43.03 ± 10.33 years, and Robot-assisted was 46.68 ± 10.63 years. 67.15% of the patients were male, with 33.58% tubular, 20.44% endoscopic, and 13.14% Robot-assisted. 78.8% of the patients underwent single level TLIF (55.56 % tubular, 31.48% endoscopic, 12.96% Robot-assisted). 19.71% underwent 2 level TLIF (16.67% tubular, 14.81% endoscopic, 18.52% Robot-assisted). 1.46% of patients underwent 3 level TLIF (100% Robot-assisted). At 2 weeks post-operatively tubular TLIF had the lowest incidence of any complication (28.8%%) compared to Endo TLIF (54.5%) or Robot-assisted (47.6%, p = 0.032). The most common complication for tubular, endoscopic, and Robot-assisted TLIF was new neurological complication (radiculitis or numbness/tingling). All complications in Endo and Robot-assisted TLIFs were new neurological complication. In the tubular TLIF, 63% were new neurological complication, 21% wound and 10% (2 patients) other. Up to 3 months post-op the complication rates were not significantly different among groups 15% (tubular), 8.6% (Endo) and 5.5% (Robot-assisted, p = 0.419). All were the new onset of radiculitis or numbness/tingling. Up to 6 months there were 2 complications in the tubular and three complications in the Endo group. Although Robot-assisted TLIFs had higher revision rates they were not significant (2.6% (tubular) vs. 2.6% (Endo) vs. 4.8% (Robot-assisted), p = 0.862). There were no significant differences in ODI or CAT domains at different time points. When tubular TLIF was compared to all Endo approaches significant differences in complication rates at 2 weeks were observed (28.8% vs. 51.9%, p = 0.010). ODI and CAT domains (pain interference, function and pain intensity) were similar across the groups. Conclusion: The current study demonstrated that the tubular TLIF had lower complication rates than both Endo and Robot-assisted TLIF procedures at early time points. There were significantly less neurological complications in the tubular group compared to both Endo TLIF procedures. Robot-assisted cases had higher revision rates, however not significant. Patient reported outcomes were similar between the groups. Some of the limitations included learning curve, lack of randomization and use of BMP2.
901
A254: Preliminary results of self-expansing rod in neuromuscular scoliosis. An international retrospective cohort study
Mareille Post 1 , Mathilde Gaume 2 , Agnita Stadhouder 1 , Moyo Kruyt 3 , Jeroen Renkens 4 , Jean-Paul Kaleeta Maalu 5 , B.J. Van Royen 1 , and Lotfi Miladi 2
1 Orthopedics, Amsterdam UMC, Amsterdam, The Netherlands
2 Orthopedics, Necker-Enfants Malades Hospital, Paris, France
3 Orthopedics, Universitair Medisch Centrum Utrecht, Utrecht, The Netherlands
4 Orthopedics, Erasmus MC, Rotterdam, The Netherlands
5 Orthopedics, Queen Fabiola Children's University Hospital, Brussels, Belgium
Introduction: Fusionless surgical techniques are increasingly used for the treatment of patients diagnosed with neuromuscular scoliosis (NMS). These systems provide correction and stabilization of the scoliotic curves, while allowing patients to continue their natural growth. The aim of this study to evaluate clinical and radiological outcomes 2 years after surgery with the one-way self-expanding rod (OWSER) system in patients with NMS. We hypothesized that this technique provides a stable deformity correction while allowing continuous spinal growth. Methodology: 37 NMS patients who underwent surgical scoliosis correction using the minimally invasive bipolar OWSER system in four different European centers were retrospectively included in the study. The minimum follow-up of all included patients is 2 years. The surgical technique consists of a bilateral OWSER system from the level of upper fixation to the pelvis by ilio-sacral screws using a minimally invasive approach. Changes in Cobb angle, pelvic obliquity, thoracic kyphosis, lumbar lordosis, T1 -S1 and T1-T12 length were assessed. Results: In total 37 patients were included (13 male, 24 female). Mean age at surgery was 9.9 years. The diagnoses were cerebral palsy (n = 12), spinal muscular atrophy (n = 10), muscular dystrophy (n = 1), and others neuromuscular disorders (n = 14). Mean pelvic obliquity improved from 14.6° (0° to 43°) to 4.1° (0° to 10°) at 2 years follow-up. Mean Cobb angle improved from 72.1° (13.8° to 107°) to 31.7° (4.4° to 91°) at 2 years follow-up. Mean preoperative kyphosis was reduced from 44.4° (3° to 84.7°) to 31.8° (13° to 60°) at last follow-up. Mean preoperative lordosis was 35.4° and 34.1° at last follow-up. Mean growth in two years of the T1-T12 segment was 42 mm (p < 0.001) and 6.3 mm (p < 0.001) for T1-S1. Radiologically, 3 patients had sagittal imbalance of who 1 patient required revision surgery. 21 complications occurred in 11 patients (6 surgical site infections, 2 PJK, 1 DJK, 3 disfunction of connector, 2 failing of distraction, 2 failing of diabolo, 1 proximal anchor migration, 1 malposition of ilio-sacral screw, 1 mal placement of the nut and 4 rod fracture). These complications resulted in 16 unplanned surgeries. Three patients needed a conversion to spinal arthrodesis before the end of spinal growth. Three patients needed new rods since they had reached the maximum growing capacity of the rods. Conclusion: The minimally invasive fusionless surgical technique associated to the OWSER provides a stable correction of pelvic obliquity and Cobb angle after 2 years follow-up, while allowing patients to continue their natural growth. This technique may be considered as a reliable alternative to the existing fusionless options in multiple disabled and vulnerable early onset neuromuscular scoliosis patients.
855
A255: MISS technique of unilateral lumbar interbody fusion (UNILIF), a clinical and radiological study at more than 5 years of follow up
Quentin Hamel 1 , Prebet Rémi 2 , Lucas Olivier 2 , Hayek Ghassan 2 , Audrey Angelliaume 2 , and Parent Henry 2
1 Ortopedic Surgery, CHU Angers, Angers, France
2 Centre du Rachis, Clinique Saint Léonard, Trélazé, France
Introduction: Unilateral pedicle screw constructs (UNILIF) have been shown to be effective for 10 years in degenerative lumbar disease. This method has obvious advantages because of its unilateral nature, its causes less destruction of posterior element thus less destabilization of the spine. There are only few studies in literature and studies have short follow-up. The aim of this study was to report clinic, functional and radiographic results with a minimum of 5 years of follow-up after UNILIF. We hypothesized that clinic, functional and radiographic results after UNILIF remain stable over time. Material and Methods: We conduct a monocentric study, all patients operated on with an UNILIF between January 2012 and December 2016 were included. A minimum of 5 years of follow-up was necessary for inclusion. Demographic and surgical were obtained in medical record. A clinical examination, a functional evaluation and an x-ray were performed 2 years postoperatively and at the last follow-up. Results: A total of 169 patients were included. There were 88 women and 81 men, mean age at surgery was 60 years-old and the mean follow-up was 7,5 ans. The level operated was L4L5 in 58%, L5S1 in 36% and L3L4 in 6%. Functional scores were significantly improved between the preoperative and the postoperative. The ODI was 44 preoperatively and 12 at the last follow-up (p < 0.05); the SF 12 was 31.5 preoperatively and 43.4 at the last follow-up (PCS); and 38.7 and 47.1 (MCS) (p < 0.05). Functional score were significantly improved between preoperative and 2-years postoperative and between 2-years postoperative and the last follow-up. Radiographic correction was stable in time. We reported 5 complications in the first 2 years of follow-up that necessitate a reintervention: 3 misplacement of screw and 2 patients not fused. Conclusion: UNILIF method reported satisfying clinical, functional and radiological results, these results remain stable over 5 years of follow-up.
1730
A256: Epidural fibrosis prevention post endoscopic decompression in Lumbar spinal stenosis
Andre Calderaro 1
1 Full Endoscopic Surgery, Centro Ortopedico Valqueire, Rio de Janeiro, Brazil
Purpose: To compare the role of Gelfoam in the prevention of postoperative epidural fibrosis (EF) after lumbar spine stenosis treated by full endoscopic decompression. Background: The application of antifibrotic materials can alleviate epidural fibrosis by restricting excessive fibroblast proliferation and mitigating scar tissue formation. EF is a possible sequelae of lumbar surgery, mainly in laminectomy during spinal stenosis decompression, accepted that its incidence ranges between 10% and 40% after lumbar laminectomy with or without fusion. Although the etiology of EF is not completely understood, it is possibly multifactorial, and the causative factors may be categorized into preoperative, operative, and postoperative factors. Different treatments and surgical strategies have been attempted to prevent postoperative fibrosis without providing consistent long-term results. Methods: The study was conducted on 64 adult patients who underwent full endoscopic decompression for treatment of lumbar spinal stenosis (LSS). The patients were allocated into two groups of 32 patients each: group A, standard group (without gelfoam) and group B, Gelfoam group. A piece of gelfoam was placed over the surgical site after laminectomy covering the exposed neural structures. The postoperative follow-up was conducted at intervals of 4 weeks, 3 month and 6 months. Both groups were evaluated clinically (Oswestry Low Back Pain Disability Questionnaire [ODI], Visual Analog Scale [VAS], and radiologically (using Ross grading by contrast magnetic resonance imaging [MRI]) for development of radicular pain and hence EF. Results: Based on the analysis, improvement in mean values of ODI score, VAS score, were found to be statistically significant postoperatively at intervals of 4weeks, 3 months, 6 months when compared individually in both groups. However, improvement was greater in the Gelfoam group. Based on contrast-enhanced MRI, the number of patients who developed EF was smaller in the Gelfoam group. Conclusions: In the present study, on clinical and radiological assessment, we conclude that gelfoam post full endoscopic surgery for LSS, prevent radicular pain and postoperative EF.
1043
A257: Trans-pars microscopic assissted nucleotomy for extraforaminal-foraminal lumbar disc herniations
Hamdan Abdelrahman 1,2 , Ahmed Shawky Abdelgawaad 1,2 , Seyed Emadaldin Sadat 1 , Metin Akkoyunlu 1 , and Ali Ezzati 1
1 Spine Surgery, Helios-Hospitals Erfurt, Erfurt, Germany
2 Orthopedics and Trauma, Asiut Universty Hospital, Asiut, Egypt
Introduction: Foraminal and extraforaminal lumbar disc herniations are uncommon and they present 10% of all lumbar disc prolapses. The main presentation is radicular pain related to the exiting nerve root at the affected level. Different approaches for surgical intervention have been described. This study aimed to evaluate clinical outcomes, complications, recurrence, and reoperation rate of the trans-pars microscopic-assisted percutaneous nucleotomy (TP-MAPN) in cases of extraforaminal and foraminal-extraforminal (EF&F-EF) lumbar disc herniations (LDH). Methods: A prospective cohort study in a high-flow spine center. Between January 2017 and January 2020, 46 consecutive patients with EF and F-EF LDH were operated upon. The following were the outcome measures: (1) self-report measures: Visual Analogue Scale (VAS) for leg pain and back pain; (2) physiological measures: standing plain X-rays (anter-posterior, lateral, and dynamic views); and (3) functional measures: Oswestry Disability Index (ODI) (validated German version) and Odom’s criteria. All patients were operated upon with (TP-MAPN). This is a minimally invasive trans-tubular microscopic-assisted procedure. the bony docking site is the pars interaticularis. The sequestrated fragment is approached through the lateral border of the pars of the cranial lamina after removal of few millimeters of the lateral border of pars are removed with the high-speed burr. Perioperative radiographic and clinical evaluations were reported. The mean follow-up period was 25 months. Results: The mean age was 67 years. L2/3 was the commonest affected level (26 patients). The mean preoperative VAS for leg pain was 7 (±2.06), improved to 1 (±0.59) postoperatively. The average operative time was 50 minutes. There were no intraoperative complications. Two patients had temporary dysthesia postoperatively. Improved neurological function was reported in 23/25 Patients (complete neurological improvement rate of 92%) at the final follow up. There was a significant improvement in the mean ODI values, from 54 ± 3.82 preoperatively to 9.184 ± 1.92 postoperatively (p < 0.001). Forty four out of 46 patients (95.7%) showed an excellent or good functional outcome according to Macnab’s criteria. Two patients were reoperated as fusion surgery, one because of large recurrent herniation and the other one because of instability. Conclusion: The trans-pars approach is a viable minimal invasive technique for EF und F-EF LDH. The preservation of the flavum ligament and Facet joint as well as the intertransverse ligament is one of the main advantages of this technique. The main aim is to avoid extensive manipulation and exposure of the nerve root ganglion to avoid postoperative sensory affection of the roots. It is an effective, safe, and reproducible minimally invasive surgical alternative in treatment of such LDHs.
1680
A258: Clinical and radiological outcomes of transforaminal lumbar interbody fusion using unilateral biportal endoscopic technique and double cages
Jwo-Luen Pao 1
1 Orthopaedic Department, Far Eastern Memorial Hospital, New Taipei, Taiwan
Introduction: This study is aimed to report the surgical techniques, clinical, and radiological outcomes of the biportal endoscopic transforaminal lumbar interbody fusion (BETLIF) using two cages. Material and Methods: This study included 90 patients who received 120 segments of BETLIF from July 2019 to May 2019. They were 17 males and 73 females with an average age of 64.8 (range 35 ∼ 85). 1-segment fusion was done in 72 patients, 2-segment in 22 patients, and 3-segment in 2 patients. The diagnoses were spondylolisthesis in 85 patients and degenerative disc disease in 5 patients. Bilateral decompression was accomplished via the unilateral approach. One PEEK cage and one composite PEEK cage with outer Titanium plates along with laminectomy bone chips and demineralized bone matrix were impacted into the disc space. Clinical data including ODI, JOA scores, VAS score, and complications were retrieved from the chart records. Computed tomography (CT) of the lumbar spine was arranged 1 year post-operatively to evaluate the fusion status. Results: The average follow-up period was 15.5 months (range 12 ∼ 31 months). The average hospital stay was 5.7 ± 1.1 days (range 3 ∼ 7 days). At final follow-up, the ODI was improved from 46.7 ± 17.0 to 12.7 ± 16.1. The JOA score was improved from 15.6 ± 6.3 to 26.4 ± 3.2. The VAS were improved from 5.2 ± 3.1 to 1.7 ± 2.1 for low back pain; and from 6.3 ± 2.5 to 1.7 ± 2.0 for leg pain. All these improvements were statistically significant with a p-value < 0.005. CT scan was available in 44 patients. Solid interbody fusion was achieved in 43 patients (fusion rate 97.7%), and cage subsidence was noted in 9 patients (20.9%). Complications included 1 dural tear (1.1%), 2 pedicle screw malposition (2.2%), and 2 epidural hematoma (2.2%). No patient required blood transfusion. Re-operation was required in 2 patients for evacuating the epidural hematoma and adjusting the pedicle screw. Conclusion: Using the UBE technique, adequate neural decompression, radical discectomy, and endplate preparation could be done perfectly done in a crystal clear and magnified surgical field with almost no bleeding. The treatment outcomes were excellent with a very high fusion rate and great improvement in ODI, JOA scores, and VAS. BETLIF is a safe, effective, and revolutionary minimally invasive technique for the spinal fusion.
1318
A259: Circumferential minimally-invasive adult spinal deformity surgery provides incremental benefit for increasingly frail patients
Peter Passias 1 , Peter Tretiakov 1 , Jamshaid Mir 1 , Pierce Nunley 1 , Paul Park 1 , Robert Eastlack 1 , Adam Kanter 1 , David Okonkwo 1 , Gregory Mundis 1 , Dean Chou 1 , Juan Uribe 1 , Neel Anand 1 , Khoi Than 1 , Gregory Brusko 1 , Kai-Ming Fu 1 , Jay Turner 1 , Breton Line 1 , Christopher Ames 1 , Justin Smith 1 , Christopher Shaffrey 1 , Douglas Burton 1 , Virginie Lafage 1 , Frank Schwab 1 , Shay Bess 1 , and Praveen Mummaneni 1
1 NYU Langone Orthopedic Hospital, Department of Orthopaedic Surgery, New York, United States
Introduction: Circumferential minimally-invasive surgery (cMIS) techniques in ASD surgery provides greater incrementally benefit to patients with increasing frailty states, though may be limited with increasing deformity status. Purpose: Circumferential minimally-invasive surgery (cMIS) may provide incremental benefit for patients with increasing frailty status by decreasing peri- and post-op complications versus open technique. Methods: Operative ASD patients ≥ 18yrs with baseline and 2-year postoperative data were assessed. Propensity score matching was used to match the circumferential minimally invasive surgery (CMIS) group with a similar open surgery group (Open) groups based on baseline body mass index, C7-S1 sagittal vertebral axis, pelvic incidence to lumbar lordosis mismatch, and S1 pelvic tilt. Frailty categorization was calculated per the Passias modified adult spinal deformity frailty index (mASD-FI) and stratified as Not Frail (NF), Frail (F), and Severely Frail (SF). Baseline and post-operative factors were assessed using two-way ANCOVA and MANCOVA analysis while controlling for baseline age, Charlson Comorbidity Index (CCI), and levels fused. Results: 174 ASD patients (62.71 ± 13.93 years, 75.7% female, 29.23 ± 6.64 kg/m2) were included after propensity score matching, split evenly between cMIS and Open groups. Surgically, Open patients had greater posterior levels fused (p = .021) and were more likely to undergo three column osteotomies (p > .05). Peri-operatively, cMIS patients had lower intraoperative blood loss and decreased use of cell saver across frailty groups (when adjusting for baseline age, CCI, and levels fused), as well as less peri-operative complications (p < .001). Adjusted analysis also revealed that increasingly frail MIS patients were also more likely to demonstrate larger improvement in one year and two year postoperative ODI, SRS-36 (Total), EQ5D, and SF-36 metrics compared to Open patients (all p < .05). By post-operative complications, increasingly frail cMIS patients were noted to experience significantly less complications overall (p = .037), less major intra-operative complications (p = .039), and were less likely to need reoperation than their Open counterparts (p = .043). Conclusion: Circumferential minimally invasive technique may offer acceptable outcomes with diminishment of peri-operative complications and mitigation of catastrophic outcomes in increasingly frail patients who may not be candidates for traditional open techniques. However, further study should investigate the long-term impact of less optimal alignment in this population.
151
A260: Feasibility and outcomes of mini open correction and fusion for adolescent idiopathic scoliosis (AIS): 2-5 years follow-up
Matthew Geck 1 , Devender Singh 1 , Ashley Duncan 1 , John Stokes 1 , and Eeric Truumees 2
1 Spine, Ascension Texas Spine and Scoliosis, Austin, United States
Introduction: Minimally invasive surgery (MIS)offers an innovative treatment option for the correction of scoliosis. A few studies in the literature describe MIS multi-level fusion to address complex spinal deformity. Aim: This study reports 2 years follow-up surgical outcome scores on patients undergoing MIS for adolescent idiopathic scoliosis (AIS) and to provide ongoing evidence of the feasibility and outcomes of this innovative treatment. Materials and Methods: Medical records on 61 patients with MIS correction of AIS were reviewed. Age, operative time, estimated blood loss (EBL), length of hospital stays (LOS), Lenke curve, preoperative (pre-op) and postoperative (post-op) Cobb angles, Scoliosis Research Society-22r (SRS-22r), Oswestry Disability Index (ODI) and Visual Analogue Scale (VAS) were evaluated. Surgical technique was uniform in all patients using two or three midline incisions. Matched pair t-tests were conducted for statistical significance (α = 0.05). Results: Mean patient age was 16.5 years (11-47 yrs.). Mean body mass index (BMI) was 18.6 (±2.1). Curves were classified as: 36 Lenke 1A, 13 Lenke 1B, 3 Lenke 1C; 9 Lenke 5C. Mean flexibility index of the main curve was 54.6% (±8.4%). Post-op follow-up landmarks of our cohort were 49 patients with 2 years and 12 with 5 years follow ups. Mean pre-op, 2- and 5-years follow-up Cobb angles were 54.2° (±3.5°), 12.8º (±3.1°), and 11.1° (±2.3°), respectively. Mean corrections at 2 and 5 years were 76% (±7.6%) and 82% (±7.4%), respectively. This difference was statistically significant (p < 0.001). Mean loss of correction on follow-ups was less than 5º. Mean operative time was 321 minutes with mean EBL of 147 mls (±67.7 mls). Mean LOS was 3.2 days (±1.2 days). Pre-op mean VAS and ODI scores were 22 and 17.4, respectively; 11.6 and 8.0 at 2 years and 9.4 and 6.6 at 5 years post-op, which were statistically significantly improved (p < 0.001). The mean SRS-22r score at 2 and 5 years were 4.58 (±0.5) and 4.65(±0.6), respectively. The radiographic evaluation showed solid fusion rates in all patients at 2 years. At 5 years, 2 patients underwent revisions for L3-L4 non-unions. No other complications or revisions were observed in our cohort. Conclusions: Based on our cohort’s 2-5 years follow-up data we conclude that MIS provides an effective treatment option for AIS reconstruction. Our study indicates that MIS can achieve adequate deformity correction and positive clinical outcomes over long run as indicated by cobb angle, VAS, ODI and SRS-22r scores during follow-ups. If the goals of AIS surgery can be achieved, consideration should be given to less invasive techniques.
153
A261: Learning curve of mini-open correction and fusion for adolescent idiopathic scoliosis (AIS) correction: a single surgeon's 12 years' experience
Matthew Geck 1 , Devender Singh 1 , John Stokes 1 , Ashley Duncan 1 , and Eeric Truumees 1
1 Spine, Ascension Texas Spine and Scoliosis, Austin, United States
Introduction: Although minimally invasive surgery (MIS) offers a potentially less morbid treatment option for patients requiring stabilization of adolescent idiopathic scoliosis (AIS), the learning curve of the procedure has not been sufficiently established. Aim: Report a single surgeon’s learning curve of MIS technique over the course of 12 years for the treatment of AIS corrections. Materials and Methods: 68 consecutive patients undergoing MIS correction of AIS from 2008 to 2020 performed by a single surgeon at one institution were studied. Our cohort were equally divided into three groups: group I (first 22 cases); group II (23-45 cases) and group III (46-68 cases). Age, gender, operative time (OR), estimated blood loss (EBL), length of hospital stays (LOS), number of spinal levels treated, radiologic outcomes, complications, Oswestry Disability Index (ODI), Visual Analogue Scale (VAS) and Scoliosis Research Society-22r (SRS-22r) were evaluated. Surgical technique was uniform in all patients using two or three midline incisions. OR, EBL and LOS were normalized per spinal levels treated for analysis. Results: Demographics of the groups were similar. ANOVA showed no significant difference in mean normalized EBL between the groups (p = 0.321). Mean normalized OR differed significantly between the groups. These were mainly due to the significant differences between groups I vs. III (p = 0.004) and groups II vs. III (p = 0.023). Percent change in mean normalized OR between groups I vs. III and II vs. III were 24.3% and 15.3%, respectively. ANOVA showed significant differences in overall mean normalized LOS between the three groups (p = 0.014). Post-hoc analysis showed significant differences in mean normalized LOS between groups I vs. II (p = 0.004) and groups I vs. III (p = 0.03). Percent change in mean normalized LOS between groups I vs. II and I vs. III were 32.7 % and 35.3%, respectively. At the final follow-up, there were no significant differences in VAS, ODI and SRS-22r scores between the two groups. Mean loss of correction at the final follow-ups between the two groups was less than 5º. The radiographic evaluation showed similar solid fusion rates in both groups. In group I, there were two L3-L4 non-unions at 5 years post-operative follow ups. In group II, there was one reoperation for a medial pedicle screw at L2 giving a radiculopathy which resolved with removal. Conclusions: Our cohort analysis elucidate technical proficiency in MIS for the treatment of AIS corrections. There were significant differences in operative time and length of hospital stay for patients treated in the later part.
OP30: Adolescent Deformity
1888
A262: Early sagittal spinal shape predicts development of scoliosis: a prospective cohort study
Steven de Reuver 1 , Jelle Homans 1 , Michiel Houben 1 , Tom Schlosser 1 , Keita Ito 1 , Moyo Kruyt 1 , and René Castelein 1
1 Orthopedic Surgery, University Medical Center Utrecht, Utrecht, The Netherlands
Introduction: Idiopathic scoliosis is a deformation of the spine and trunk with a prevalence of 2-4%, mostly affecting otherwise healthy girls in early adolescence. Scoliosis can be progressive and in some cases necessitates spinal fusion surgery. This condition is a classic orthopedic disorder, its etiology is still to a large extent a mystery. It has been suggested that posteriorly inclined segments of the spine, unique for humans, are rotationally unstable and the initiators of scoliosis. We were able, for the first time in a prospective study, to analyze the predictive value of this segment, before the onset of the disorder by following a pediatric sub-population with a much higher likelihood (50%) of developing scoliosis that closely resembles idiopathic scoliosis, i.e. children with 22q11.2 deletion syndrome (22q11.2DS). Material and Methods: We prospectively followed a cohort of children with confirmed 22q11.2DS by biplanar spinal radiographs at two-year intervals, in an IRB approved institutional registry. Included children had a straight spine, were skeletally immature, and were followed until skeletal maturity. On standardized lateral radiographs, the size of the ‘posteriorly inclined triangle’ (PIT) area was measured (defined as the right-angled triangle between the centroid of the most upper and lower posteriorly inclined vertebral bodies), a previously described parameter reflecting the functional anatomy of the posteriorly inclined part of the thoracic and lumbar spine in the sagittal plane. Results: Of 50 included children (54% boys, mean age 10.7 ± 1.7, mean follow-up 4.8 ± 1.6 years), 24 (48%) developed scoliosis. The area of the PIT in participants that would later develop a scoliosis was 73 ± 25 cm2, over 1.5 times greater than the 47 ± 20 cm2 in no scoliosis. Having an above average PIT-area of 60 cm2 or higher at inclusion was associated with a relative risk of 2.55 (95%CI:1.22-5.34) for developing scoliosis. Comparing PIT-area subgroups, scoliosis developed in 20% in the lowest group (PIT-area 0-30 cm2) and in 100% in the highest group (PIT-area > 90 cm2; p < 0.001). In addition, the shape of the PIT dictates the type of scoliosis. A more slender, and more vertical PIT precedes thoracic curves and a broader and more horizontal PIT predicts (thoraco)lumbar scoliosis (15 ± 4° in thoracic versus 20 ± 5° in (thoraco)lumbar scoliosis; p = 0.048). Conclusion: Increased posterior inclination of the pre-adolescent spine precedes scoliosis development during adolescence, and the shape of this segment determines the scoliosis location. This substantiates the important biomechanical component of its etiology and might offer possibilities for early detection, treatment, and most importantly: scoliosis prevention.
944
A263: Thoracic kyphosis increases, but cervical and lumbar lordosis does not change through unfused segments after surgical correction of Lenke 5 and 6 curves
Josephine Coury 1 , Zeeshan Sardar 1 , Yong Shen 1 , Mark Ren 1 , Michael Vitale 1 , and Lawrence Lenke 1
1 Columbia University Medical Center, Och Spine Hospital, New York, United States
Introduction: Lenke Type 5 and 6 adolescent idiopathic scoliosis (AIS) patients who undergo surgical deformity correction typically have fusion levels spanning the thoracolumbar and lumbar regions. The lower lumbar levels and upper to mid thoracic levels are typically not fused and can undergo reciprocal changes in their alignment after surgery. No previous studies have researched the changes in these unfused segments overtime. In this study, we investigated the sagittal balance compensatory changes in the unfused vertebral levels proximal and distal to the instrumentation and fusion. Material and Methods: A retrospective review of prospectively collected multicenter data was performed. 193 patients were identified, 191 with 2-year and 93 with 5-year follow up were included in the final analysis. Cervical lordosis, thoracic kyphosis proximal to the upper instrumented vertebra (UIV) and lumbar lordosis distal to the lower instrumented vertebra (LIV) were measured preoperatively and at 1, 2, and 5 years postoperatively. All analyses were performed with SAS and alpha was set at p < 0.05 to declare significance. Results: Lenke type 5CN (n = 147) was the most common curve type. T10 to L4 were the most frequently fused levels (n = 54) followed by T11 to L3 (n = 38) and T9 to L3 (n = 34). Patients underwent an average 5-level fusion (range 3-9). No significant changes in cervical lordosis from preop to postop year 5 occurred. On average, from preop to 1 year postop there was 0.6° loss of cervical lordosis. From postop year 1 to 2 cervical lordosis increased an average 3° and from year 2 to 5 decreased 1.4°. Thoracic kyphosis proximal to UIV increased significantly from preop 29.1° to 32.7° at 5 years postop. Kyphosis increased an average of 2° from preop to postop year 1, 1° from postop year 1 to 2, and 1° from year 2 to 5. Lordosis distal to LIV had no significant changes; 1° of lordosis was lost from preop to postop year 1, with no change in lordosis from postop year 1 to 2, or 2 to 5. Conclusion: Thoracic kyphosis proximal to the UIV in Lenke type 5 and 6 curves increases significantly postoperatively by a mean of 3.6°, with the largest change occurring during the first year, and a slower rate of progression thereafter. No significant compensatory changes occurred in cervical lordosis or in the unfused distal lumbar lordosis secondary to curve correction.
1082
A264: What matter most? The effect of olisthesis reduction and lordosis restoration in surgery for high dysplasia developmental spondylolisthesis
Giovanni Andrea La Maida 1 , Enrico Gallazzi 1 , Marcello Ferraro 1 , Donata Rita Peroni 1 , Andrea Della Valle 1 , Davide Cecconi 1 , Luca La Verde 2 , and Bernardo Misaggi 1
1 UOC Patologia Vertebrale e Scoliosi,ASST Centro Specialistico Ortopedico Traumatologico G. Pini - CTO, Milano, Italy
2 Dipartimento di Scienze Biomediche per la Salute, Università degli Sudi di Milano, Milano, Italy
Introduction: The need to achieve reduction as well as the extension of the instrumentation area of High Dysplasia Developmental Spondylolisthesis (HDDS) are still controversial. Many studies have emphasized the effect of reduction on sagittal balance after surgery. On the other hand, it is still unclear what postoperative parameters are predictive of surgical failure: especially, whether is the olisthesis reduction or the lordosis restoration that prevent failures. Therefore, the purpose of this study is to evaluate the relationship between reduction and change of spinopelvic parameters in HDDS postoperatively. Methods: This is a single-center retrospective study of patients treated surgically by instrumented posterior vertebral fusion of (L4)L5-S1 with cage in L5-S1, with a diagnosis of HDDS and a minimum of 1 year of follow-up. Pre, postoperative and at 1-year follow-up X-RAYs were evaluated for all patients included in the study, on which global spinopelvic parameters (pelvic incidence, PI; sacral slope, SS; pelvic tilt, PT, L5-S1 segmental lordosis and global lordosis) and Meyerding grade (MD) were measured. Surgical failures, defined as the need for reoperation due to deformity progression or implant loosening, were also recorded. Results: After searching the Institutional database, 28 patients were included. The mean age was 30.67 years. 4 patients underwent revision surgery: 2 for fixation failure and 2 for secondary spondylolisthesis of L4. 6 patients were initially treated with L4-S1 arthrodesis, the remaining with L5-S1 arthrodesis. The mean preoperative MD was 2.88, while in the postoperative was 0.75. Preoperative spinopelvic parameters were as follows: Mean PI 75.47 (±11.71°), SS of 47.94° (±12.32°), and PT of 23.82° (±13.99°), As for lordosis, there was a mean of 59.56° (±17.17°), for total and a mean of 9.93° (±14.97°), for segmental. Postoperatively, spino-pelvic balance was essentially unchanged with an average SS of 47.64° (±8.50°), and an average PT of 24.75° (±12.20°) Postoperative total lumbar lordosis was 58.95° (±13.57°), and Segmental Lordosis was 20.25° (±10.33°, p < 0.01 compared to preop). Four patients (13.8%) underwent revision surgery for progression of the deformity, with proximal extension of the implant, or implant failure with need for revision surgery. Of these patients, three had initially been treated with L5-S1 fusion and one with L4-S1 fusion; in these patients, the mean postoperative MD grade was 1(p < 0.01 compared to preop, p = ns compared to the non reoperated group), while segmental lordosis was lower than in non reoperated patients (4.98° vs 22.03°, p < 0.001). Conclusions: In the surgical treatment of HDDS, the main predictive parameter of surgical success is the proper restoration of segmental lordosis compared with the degree of reduction of olisthesis itself. Despite limited by the low sample size, the results of this study highlight how the adoption of a surgical strategy that achieves the restoration of segmental lordosis is essential in the planning for HDDS surgery, while both global lordosis and the degree of reduction are found to be less significant.
804
A265: Dual modality of vertebral body tethering: anterior scoliosis correction versus growth modulation with mean 5 year follow up
Jason Bernard 1 , Timothy Bishop 1 , Jan Herzog 1 , Shahnawaz Haleem 1 , Emily Tsang 1 , Bisola Ajayi 1 , and Darren Lui 1
1 Trauma & Orthopaedics, St. George's University Hospital, London, United Kingdom
Introduction: Vertebral body tethering (VBT) is a non-fusion technique to correct scoliosis. It allows correction of scoliosis through Growth Modulation (GM) by tethering the convex side to allow concave unrestricted growth similar to the hemi-epiphysiodesis concept. The other modality is Anterior Scoliosis Correction (ASC) where the tether is able to perform most of the correction immediately where limited growth is expected. Methods: Retrospective analysis of clinical and radiographic data of 20 patients between 2014 and 2016 with a mean 5 year follow (range 4-7). Results: There were 10 patients in each group with a total of 23 curves operated on. VBT-GM mean age was 12.5y with mean Risser 0.63 and VBT-ASC was14.9y with a Risser of 3.66. Mean preop VBT-GM Cobb was 46°with a Fulcrum unbend of 13.6° compared to VBT-ASC 56.9° with 32.2° unbend. Postop VBT-GM was 21°and VBT-ASC Cobb was 10.8°. The early postop Correction Rate was 54.3% vs 81% whereas FBCI was77.1% vs 186.6%. The last XR at mean 5y was 19.4° (VBT-GM) and 16.5° (VBT-ASC). Open TRC group had 3 over corrections. 1 patient alone had overcorrection, a second stage tether release and final conversion to fusion. 95% of patients avoided fusion with VBT. Discussion and Conclusion: We show a high success rate (95%) in helping children avoid fusion. Vertebral body tethering is a safe technique for correction of scoliosis in the skeletally immature patient. This is the first report at 5 years that shows two modalities of VBT can be employed depending on the skeletal maturity of the patient: Growth Modulation and Anterior Scoliosis Correction.
1646
A266: Cardiopulmonary function is compromised more in patients with early-onset scoliosis from high altitude area
Zihao Ding 1 , Yong Hai 1 , and Lijin Zhou 1
1 Department of Orthopedic Surgery, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Background: Early onset scoliosis (EOS) adversely affects patients’ cardiopulmonary function. We aimed to compare the differences in cardiopulmonary function between patients with EOS in high-altitude and plain areas and determine the relationship between spinal imaging parameters and cardiopulmonary function. Study design: A retrospective cohort study was conducted including 104 EOS patients, aged 5-11 years, with thoracic curvature in a single research center between June 2013 and June 2021. Based on the inclusion and exclusion criteria, 38 and 66 EOS patients were enrolled in the high-altitude and plain area groups, respectively. The high-altitude group comprised 20 boys and 18 girls, with a mean age of 8.42 years (range, 6-10 years). The plain area group comprised 26 boys and 40 girls, with a mean age of 8.77 years (range, 4-11 years). Cobb angle, kyphosis angle (TK), and main thoracic curvature (MT) were measured. Doppler echocardiographic data, pulmonary function indices, and blood gas analysis results of EOS patients were collected. The correlations between the upper thoracic curve (UT), main curve, KT, and cardiopulmonary function were analyzed. Results: Pulmonary artery internal dimension, left ventricular end-diastolic diameter, and interventricular septum thickness was significantly lower in the high-altitude group (p < 0.05). Vital capacity (VC), maximal voluntary ventilation (MVV), and forced expiratory volume in 1 s (FEV1) were lower in the high-altitude group (p < 0.05). In the high-altitude group, MT was significantly correlated with the indices of the left ventricular end-systolic dimension, interventricular septum extent, right ventricle basal diameter, left atrium left-right diameter, partial pressure of oxygen, and blood oxygen saturation (rho1 = -0.399, rho2 = 0.565, rho3 = -0.358, rho4 = -0.371, rho5 = -0.400, rho6 = -0.406). UT correlated with VC, MVV, forced vital capacity, and FEV1. Conclusion: EOS patients in high-altitude areas had poorer cardiac and pulmonary functions than those who live in plain areas. Cardiopulmonary function and the degree of scoliosis interact with each other. We should pay more attention to preoperative evaluation and postoperative rehabilitation for EOS patients living in high-altitude areas.
557
A267: Cumulative radiation exposure in patients treated for adolescent idiopathic scoliosis
J. Cool1,2, G.J. Streekstra2,3, J. Van Schuppen2,4, J.C. Van den Noort5, Agnita Stadhouder1,2, and B.J. Van Royen1,2,6
1 Orthopedic Surgery and Sports Medicine
2 Amsterdam Movement Sciences, Amsterdam, The Netherlands
3 Department of Biomedical Engineering & Physics
4 Department of Radiology and Nuclear Medicine
5 Department of Radiology and Nuclear Medicine, Medical Imaging Quantification Center, Amsterdam UMC, Amsterdam, The Netherlands
6 Amsterdam UMC, Emma Children’s Hospital, Amsterdam, The Netherlands
Purpose: Adolescent idiopathic scoliosis (AIS) is a progressive spinal deformity, most often seen in female patients around the age of puberty. The severity of the spinal deformity, over-time progression, and treatment follow-up of the deformity is assessed by radiological evaluation of the full spine regularly. This often results in a high whole number of full spine radiographs over many years. As a result, concerns are present regarding the cumulative amount of radiation received by patients treated for AIS. This study aimed to determine the average cumulative radiation exposure in patients with AIS treated by brace treatment or surgical treatment during their entire treatment period at our institution. In addition, the potential increased radiation exposure of recently introduced preoperative low-dose CT planning for 3D printed patient-specific screw guides in surgical treatment was assessed in comparison to standard intraoperative 2D fluoroscopy. Methods: A single-center retrospective medical chart review of AIS patients treated by surgery and/or brace treatment was conducted. Patients were included when the end of treatment took place over the last 5 years (2016-2021). An average radiological work-up for AIS was quantified for all treatment groups and the mean total number of imaging procedures was calculated for all patients. Radiation exposure of plain radiographs and CT imaging was measured in dose area product (DAP) (mGy-cm) or dose length product (DLP) (mGy-cm2) and converted to effective dose (mSv). The average cumulative radiation dose in AIS patients treated by brace treatment or surgical treatment was subsequently determined by effective dose (mSv). Results: A total of 73 patients were included, with 28 patients treated with a brace, and 45 with posterior spinal fusion surgery. Patients treated with a brace received an average of 9.11 (range 4-16) full spine radiographs, resulting in a cumulative effective dose of 0.488 mSv during a median whole treatment period of 2.76 (range 1.07-11.24) years. Patients treated with surgery received an average of 14.26 (range 9-27) full spine radiographs during a median treatment period of 3.23 years (range 1.24-8.74). Resulting in a cumulative effective dose of 0.820 mSv for patients treated using intraoperative 2D fluoroscopy, and 1.710 mSv when 3D printed screw guides were used. Conclusion: The cumulative radiation exposure of AIS patients during their entire treatment period over years in this study was very low, considering the earth's annual background radiation dose. However, every exposure to ionizing radiation due to medical imaging should be limited, and caution, therefore, remains desirable. The use of intraoperative 3D printed screw guides doubled the cumulative effective dose in surgical treated AIS patients, compared to 2D fluoroscopy, however, remains still very low.
880
A268: Validation of a new classification to differentiate curve types of adolescent idiopathic scoliosis - A benefit/risk approach to non-fusion surgery
Per Trobisch 1 , Domenico Compagnone 2 , Christof Birkenmaier 3 , Filippo Migliorini 4 , Teresa Bas 5 , Pedro Berjano 2 , Samuel Cho 6 , Aurelien Courvoisier 7 , Sajan Hegde 8 , Ilkka Helenius 9 , Darren Lui 10 , Elias Papadopoulos 11 , and Alice Baroncini 1
1 Department of Spine Surgery, Eifelklinik St. Brigida, Simmerath, Germany
2 GSpine4, IRCCS Istituto Galeazzi - Sant'Ambrogio, Milan, Italy
3 Department of Spine Surgery, Kliniken München Süd, München, Germany
4 Department of Orthopaedic Surgery, RWTH Aachen University Clinic, Aachen, Germany
5 Hospital Universitario y Politécnico La Fe 1, Valencia, Spain
6 Icahn Mount Sinai School of Medicine, New York, United States
7 Grenoble Alps University Hospital, Grenoble, France
8 Apollo Hospitals, Tamil Nadu, India
9 Department of Paediatric Orthopaedics and Traumatology, University of Helsinki and Helsinki University Hospital, Helsinki, Finland
10 St. George's University Hospital, London, United Kingdom
11 Kapodistrian University, Athens, Greece
Introduction: Vertebral body tethering (VBT) may represent a paradigm shift in the management of adolescent idiopathic scoliosis (AIS). However, the ideal candidates, who may profit the most from this technique, have not yet been identified. We evaluated patients based on their curve type and on the potential benefits of VBT over fusion and developed a new classification to guide decision making for VBT, evaluating 5 different curve types (lumbar, double, long thoracic, short thoracic, presence of high thoracic curve). This study analyzed the inter- and intrarater variability of this new classification. Material and Methods: 11 spinal deformity surgeons contributed to the validation. Four radiographs (p. a., lateral, right and left p. a. side bending) were prepared for 27 patients. Two sets of the patients’ images were sent to each participant, with identical radiographs but in different order. Each participant was given instructions on how to employ the classification and was asked to apply it to the radiographs. The inter- and intra-observer reliability was assessed evaluating the kappa coefficient (k). Results: The overall inter-observer reliability was k = 0.84 (confidence interval: 0.76 to 0.91). The overall intra-observer reliability was k = 0.88 (confidence interval 95%: 0.68 to 1.00). All k values were statistically significant and indicated an excellent inter- and intra-observer reliability of the classification. Conclusion: The newly developed classification for VBT planning showed an excellent reliability.
2002
A269: Determination of selecting the distal fusion level using 'touched vertebra' in thoracic curves of adolescent idiopathic scoliosis: suggestion of “modified Suk classification”
Jin-Hyok Kim 1 , Dong-Gune Chang 2 , Jong-Beom Park 3 , Hong Jin Kim 2 , Se-Il Suk 2 , Jae Hyuk Yang 4 , Seung Woo Suh 5 , Yunjin Nam 5 , and Sung Cheol Park 4
1 Orthopedic Surgery, Hanil General Hospital, Seoul, South Korea
2 Orthopedic Surgery, Inje University Sanggye Paik Hospital, Seoul, South Korea
3 Orthopedic Surgery, College of Medicine, the Catholic University of Korea, Gyeonggi-do, South Korea
4 Orthopedic Surgery, Korea University Anam Hospital, Seoul, South Korea
5 Orthopedic Surgery, Korea University Guro Hospital, Seoul, South Korea
Introduction: Optimal determination of distal fusion level in adolescent idiopathic scoliosis (AIS) is utmost important to avoid adding-on phenomenon, coronal, or sagittal decompensation. Although severe recommendations for lowest instrumented vertebra (LIV) selection have been introduced, there is no universally acceptable guidelines yet. Recently, Lenke et al. described touched vertebra (TV) modifier as universal reference point for LIV selection, which is easy to understand and utilize. Therefore, the selecting the TV as LIV need to be studied by comparing the determination through Suk classification. Material and Methods: A total of 129 patients with thoracic curves of AIS by Suk classification were retrospectively analyzed after deformity correction for 3-year follow-up. All included patients were divided three groups according to whether the LIV matched with TV: matched TV (n = 62), cephalad TV (n = 21), and caudad TV (n = 46) groups. Radiological variables were assessed by central sacral vertical line (CSVL) – LIV difference, end vertebra rotation, coronal, and sagittal parameters. Complications were included in distal junctional kyphosis (a change of ≥ 10° between the superior endplate of the LIV and the inferior end plate of the vertebra below it), unsatisfactory results (adding-on, LIV tilt of >10 degrees, or coronal balance > 15mm), and coronal decompensation (the absolute value of coronal balance greater than 20mm) in this study. Results: Selecting the distal fusion level by Suk classification showed that 48.1% (62/129) of LIV was matched with touched vertebra. The CSVL-LIV difference was significantly improved in matched TV group (7.6 mm) compared to cephalad TV (14.5 mm) and caudad TV groups (9.4 mm) for 3-year follow-up (p = 0.001). End vertebra rotation was no significantly differences between three groups (p = 0.174). Regarding the complications, distal junctional kyphosis (4.8% vs 7.5%), unsatisfactory results (21.0% vs 25.3%), and coronal decompensation (3.3% vs 13.4%) were lower in the matched TV group than unmatched TV group. Among the three complications, only coronal decompensation showed a statistical significance between three groups (p = 0.038). The 3-year follow-up CSVL-LIV difference showed significant weak correlation of change in disc angulation (r = 0.204, p = 0.020) and 3-year follow-up LIV tilt angle (r = 0.243, p = 0.005). Conclusion: Selecting the TV as distal fusion level in thoracic curve of AIS is better choice in terms of LIV translation, LIV tilt angle, distal unctional angle and reducing the complications (especially, coronal decompensation). Furthermore, DVR was not impact on determination of LIV using TV at 3-year follow-up. Therefore, our study support that TV is important landmark for determination in distal fusion level in the view of Suk classification.
599
A270: Traditional growing rod versus magnetically controlled grwowing rod finalized with posterior spinal fusion for patients with early onset scoliosis: a comparison of radiographic, clinical and functional outcomes of 38 patients with at least 3 years of follow-up
Tuna Pehlivanoglu 1 , Bahadir Gokcen 2 , Kursat Kara 1 , O. Nuri Eroglu 1 , Tugay Yagci 1 , and Cagatay Ozturk 1
1 Dept. of Orthopaedic Surgery, Liv Hospital Ulus, Liv Spine Center certified by AOSpine, Istanbul, Turkey
2 Dept. of Orthopaedic Surgery, Liv Hospital Vadi, Liv Spine Center certified by AOSpine, Istanbul, Turkey
Introduction: Early onset scoliosis (EOS) was reported to be successfully treated with tradition growing rod (TGR) by applying invasive lengthening and magnetically controlled growing rod (MCGR) by applying non-invasive lengthening, while both methods were frequently finalized with posterior spinal fusion (PSF). The aim of the present study was to compare the radiographic and clinical outcomes of TGR and MCGR to question, if one method was able to provide any superiority. Patients and Methods: Selection of both groups was based on the following inclusion criteria: an age <10 at index procedure, a major curve magnitude > 30°, no previous spine surgery and a minimum follow-up period of 3 years, having dual rod constructs. A total number of 17 patients with MCGR (mean age: 7.4 year, mean follow-up duration: 38.2 months) and 21 gender-age-pre-op major curve magnitude matched patients with TGR (mean age: 8.2 year, mean follow-up duration: 44.7 months) were detected to meet the inclusion criteria and they were enrolled. Results: MCGR-TGR groups had a mean pre-operative major curve magnitude of 48.2°-51.4°, a mean major curve magnitude with growing rod before fusion surgery of 33.1°-30.8° (Improvements p < 0.001 for both. Comparison p = 0.32), a mean major curve magnitude after fusion surgery at the latest follow-up visit of 16.4°-13.1° (Improvements p < 0.001 for both. Comparison p = 0.27). Mean T1-S1 distance of MCGR and TGR groups improved from 274-281 mm pre-operatively, to 342-357 mm at the latest follow-up (Improvements p < 0.003 for both. Comparison p = 0.40). MCGR patients were detected to have 47 non-invasive lengthenings with 2 unplanned revision (all in syndromic cases: 1 rod breakage, 1 loss of distraction) procedures, while TGR group was detected to have 58 non-invasive lengthenings with 4 unplanned revision procedures (3 in syndromic cases, 1 in neuromuscular case: 3 loss of initial distraction, 1 pull-out of 1 screw). MCGR and TGR group had a mean sagittal and coronal balances of 21.3-22.9 mm and 14.1-13.8 mm pre-operatively and 16.4-17.1 mm and 11.2-10.7 mm at the latest follow-up visit (Improvements p < 0.001 for both. Comparison p = 0.17). MCGR and TGR groups had a mean pre-operative total SRS-22 score of 3.1-2.9, improved to 4.6-4.2 at the latest follow-up visit (Improvements p < 0.001 for both. Comparison p = 0.23). Conclusions: The present study concluded, that EOS could be successfully managed with both of the methods comprising MCGR and TGR, while both systems were detected to provide similar major curve corrections, T1-S1 length improvements, requirements of the number of lengthenings, improvements in coronal-sagittal profiles, rates of complications and revisions, underlining the safety and efficacy of both of the methods. However, more complications and rates of revision were noted in syndromic patients with either of the methods. The present study also concluded, that both of the methods were able to yield similar clinical and functional improvements with high patient satisfaction, although TGR group needed open surgeries for lengthening.
OP31: Surgical Complications 2
1900
A271: Has covid affected the outcomes in patients undergoing spinal surgeries: a retrospective analysis
Akshaya Gadekar 1 and Rajdeep Singh Bagga 1
1 Department of Orthopaedics & Emergency Medicine, SAIMS, Indore, Indore, India
Introduction: Covid-19 pandemic has impacted the entire world due to mortalities caused and the morbidities that followed covid infection which in term burdened the entire medical system and impacted human lives financially and morally. Covid-19 infectivity has been critically associated with significant attenuation of patient’s immunity that has lead to increased incidence of post operative complications, mobidity & mortality. With continuous propogation of covid-19 it mutated over a period of time and presented itself in association with new complications like different types of fungal infections, post operative complications etc. We aimed to look for the impact of covid-19 in patients undergoing lumbar spine surgeries at our institute. Material and Methods: We conducted a retrospective analysis & data of patients undergoing lumbar spine surgeries between 2017 and 2022 was collected. Patients undergoing Lumbar spine surgery with or without instrumentation above the age of 18yrs were included. Patients who had lumbar infections e.g. potts spine etc. were excluded from our study. On applying inclusion criteria we had 224 patients in our study of which 103 patients belonged to pre-covid era group (2017-19) & 121 patients belonged to post-covid era group (2020-22). Patients were evaluated Preoperatively as patient’s age, gender, ASA Grading, additionally RTPCR &HRCT was done in post covid era group. Intraoperative evaluation of intraop-blood loss, duration of surgery & dural tears were recorded. Post operative evaluation of Superficial & deep infection as per CDC Criteria, length of ICU stay, duration of hospital stay, medical complications were addressed and recorded. The data collected was then subjected to SPSS software for further analysis. Functional & radiological outcomes were also evaluated. Results: Both groups (Pre&Post-Covid) were comparable in terms of Age and Sex distribution (p value >0.05) Avg Age - 34.3yrs & M:F ratio - 1.4:1. Avg ASA Grade in Pre-Covid Group was 1.2 & in Post-Covid Group was 1.1 & thus were comparable (p value > 0.05). Intraop. Blood loss & duration between the two groups was comparable (p value >0.05). Dural Tear incidence in Pre-Covid group was 3.2% whereas in Post-Covid group was 3.8% & thus was comparable. According to CDC Criteria the incidence of Superficial infection in Pre-Covid group was 3.1% whereas in Post-Covid group it had increased to 9.6%; the incidence of Deep infection in Pre-Covid group was 1.1% whereas in Post-Covid group it had increased to 6.8% (p value 0.03). Incidental cardiac arrest on post operative day 3 was noted in 4 patients belonging to post covid group, no such cases were reported in pre-covid group. The avg duration of Hospital stay was also increased from 15 days precovid to 23 days in post covid era. Conclusion: Covid-19 has reduced general and local immunity that lead to increased number complications like superficial and deep infections associated with lumbar spine surgeries. Which has increased the cost of treatment, thus increasing the financial burden on society and has prolonged the duration of hospital stay of the patients increasing the rehabilitation time as well.
815
A272: Incidence and risk factors of venous thromboembolism after spine surgery - a single center experience
André Santos Moreira 1 , João Carvalho Pereira 1 , Ana Catarina Águas 2 , Joana Araújo de Azevedo 1 , Nuno Oliveira 3 , Pedro Varanda 1 , and Bruno Direito Santos 1
1 Orthopaedics Department, Hospital de Braga, E. P. E, Braga, Portugal
2 School of Medicine, University of Minho, Braga, Portugal
Introduction: Venous thromboembolism (VTE) is a well-documented complication after spine surgery. However, the incidence of VTE and the need for thromboprophylaxis remain insufficiently studied. Therefore, we aim to evaluate the prevalence and study the risk factors regarding VTE occurrence after spine surgery. Additionally, we aim to estimate the impact of thromboprophylaxis on VTE development. Material and Methods: We retrospectively analyzed all patients who underwent spine surgery at a secondary-care center between 2015 and 2019 with at least twelve-month follow-up. Results: A total of 1247 patients were included. Seventeen patients (1.4%) developed a venous thromboembolic event in the follow-up period. Median time to event was 28 days, with 50% of VTEs occurring in the first month. Ten patients (58%) underwent lumbar spine surgery, and eight cases (47%) were associated with minimally invasive spine (MIS) surgery. Mean age at surgery was fifty-seven years old. Oncological related spine surgery (n = 2; 11.8%) and procedures that involved both an anterior and posterior approach (n = 5; 29.4%) revealed statistically significant higher rates of VTE (p < 0.05). Among thromboembolic events, eight (47.1%) patients used at least one method of thromboprophylaxis. Per protocol VTE chemoprophylaxis was not associated with lower VTE occurrence (p = 0.184) and tranexamic acid intravenous use was not found to be a risk factor for VTE (p = 0.176). Conclusion: The incidence of VTE after spine surgery is low. Thromboprophylaxis was not a significant independent predictor of thromboembolic events in our study. Age, sex, anatomic region, MIS surgery and tranexamic acid intravenous use did not influence VTE incidence. Further studies with a larger number of patients are needed to address the risk-benefit relationship of thromboprophylaxis.
261
A273: Predictive models for length of stay and discharge disposition in elective spine surgery: development, validation, and comparison to the ACS NSQIP calculator
Ayush Arora 1 , Dmytro Lituiev 2 , Deeptee Jain 3 , Dexter Hadley 4 , Atul Butte 2 , Sigurd Berven 1 , and Thomas Peterson 1
1 Department of Orthopaedic Surgery
2 Bakar Computational Health Sciences Institute, University of California, San Francisco, United States
3 Department of Orthopaedic Surgery, Washington University in St. Louis, St. Louis, United States
4 Department of Pathology, University of Central Florida, Orlando, United States
Introduction: Complications and delayed recovery following elective spine surgery can greatly impact patient quality of life and perception of improvement. Both extended length of stay (LOS) and discharge to rehabilitation care may reflect a combination of worsening patient morbidity, cost, and postoperative outcome. Accurate preoperative identification of patients at risk for extended LOS and discharge to rehabilitation can provide substantial benefit, including cost savings and preemptive administrative action. The purpose of this study is to utilize machine learning to predict hospital length of stay (LOS) and discharge disposition following adult elective spine surgery, and to compare performance metrics of machine learning models to the American College of Surgeon’s National Surgical Quality Improvement Program’s (ACS NSQIP) calculator. Material and Methods: Data were acquired on 3,678 adult patients undergoing elective spine surgery between 2014 and 2019 from the Electronic Health Record (EHR) at a single academic institution. Patients were divided into 3 stratified cohorts: cervical degenerative, lumbar degenerative, and adult spinal deformity groups (ASD). Predictive variables included demographics, BMI, diagnosis group, surgical region, surgical invasiveness index, surgical approach, and comorbidities. Regression, classification trees, and Least Absolute Shrinkage and Selection Operator (LASSO) were used to build predictive models. Validation of the models was conducted on 16% of patients (N=587), using area under the receiver operator curve (AUROC), sensitivity, specificity, and correlation. Patient data were manually entered into the ACS NSQIP online risk calculator to compare performance. Outcome variables were discharge disposition (home vs rehabilitation) and LOS (days). Results: Of 3,678 patients analyzed, 51.4% were male (n = 1,890) and 48.6% were female (n = 1,788). The average LOS was 3.66 days. 78% were discharged home and 22% discharged to rehabilitation. Compared to NSQIP (Pearson R2 = 0.16), the predictions of poisson regression (R2 = 0.29) and LASSO (R2 = 0.29) models were significantly more correlated with observed LOS (p = 0.025 and p = 0.004, respectively). Of the models generated to predict discharge location, logistic regression yielded an AUROC of 0.79, which was statistically equivalent to the AUROC of 0.75 for NSQIP (p = 0.135). Conclusion: The predictive models developed in this study can enable accurate preoperative estimation of LOS and risk of rehabilitation discharge for adult patients undergoing elective spine surgery. The demonstrated models exhibited better performance than NSQIP for prediction of LOS and equivalent performance to NSQIP for prediction of discharge location.
1811
A274: Complications in spine surgery: prospective 13-year follow-up of unplanned revision spinal surgeries
Petr Nesnídal 1,2,3 , Jan Štulík 2 , and Michal Barna 2
1 Neurosurgical Department Hospital, České Budějovice, Czech Republic
2 Department of Spinal Surgery, 1 st Medical Faculty, Charles University and Teaching Hospital Motol, Prague, Czech Republic
3 Institute of Hygiene and Epidemiology, 1 st Faculty of Medicine, Charles University, Prague, Czech Republic
The purpose of the study is to carry out a prospective evaluation of the most serious complications requiring unplanned revision spinal surgeries in the course of 13 years at a single department. Material and Methods: In the period 2006 - 2018, a total of 16872 patients underwent a surgery at our department. During this period, in 556 patients an unplanned revision spinal surgery was performed. The patients were categorised by cause for revision: 1/impaired wound suprafascial (superficial) healing - superficial infection, 2/impaired wound subfascial (deep) healing-deep infection, 3/surgical wound hematoma, 4/deterioration or occurrence of new neurological symptoms, 5/cerebrospinal fluid leak (liquorrhoea) and 6/ others. Demographic effects, tobacco smoking and comorbidities were followed up in the cohort, together with the effects of surgery, diagnosis, surgical approach and physician. Results: Of the total number of 16872 operated patients, a group of 521 (3.09%) patients undergoing a revision surgery for complications was analysed in detail. Impaired wound healing - infection (SSI) was found in 199 (1.18%) patients, of whom superficial infection in 124 cases (0.73%) and deep infection in 75 cases (0.44%). Hematoma in a surgical site was detected in 149 (0.88%) patients. In 63 (0.37%) cases, deterioration of the existing neurological finding or occurrence of a new neurological finding were observed, in 68 (0.40%) cases cerebrospinal fluid leak was reported and in 40 (0.24%) cases other complications were identified. The prevalence of smokers in the group with complications (N = 521) was 34.7%. The control group (N = 3650) included 30.1% of smokers (p < 0.05). The mean BMI in the group with complications was (N = 521) 27.3. In this case the significance (p > 0.05) was not confirmed. The complications prevailed strongly in posterior surgical approach, namely in 483 patients (92.7%). As concerns the surgically treated segment, lumber spine dominates with 320 (61.4%) cases. The group of patients with complications (N = 521) showed a much higher average length of hospital stay of 12.8 days compared to the average of 4.6 days. Discussion: In our cohort, the complication rate was 3.09%, of which infections constituted 1.18%, which is in agreement with similarly focused papers. As regards the patient-related factors, in our study the results reported by literature were confirmed with respect to the age, smoking and comorbidities. Moreover, the posterior surgical procedure, lumber spine surgery and presence of a medical resident are essential (p < 0.05). No major age difference was observed between women and men (p > 0.05). Obesity is one of the key risk factors, especially in infectious complications. In our cohort, a higher BMI did not increase the risk of complications in general (p > 0.05). Conclusions: In correlation with current literature, our cohort confirmed a significantly higher risk of complications leading to revision spinal surgery associated with age, smoking, posterior surgical procedure in thoracic or lumber spine, and presence of a medical resident as a surgical assistant. The average length of hospital stay was demonstrably longer in complicated patients, it almost tripled compared to the whole cohort. Contrary to literature, the effect of obesity on the occurrence of complications was not confirmed.
1682
A275: The effect of the difference in C2-7 angle on occurrance of dysphagia after anterior cervical discectomy and fusion with the Zero-P implant system
Chengyi Huang 1 and Hao Liu 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Introduction: We noticed that after the ACDF with Zero-P, the changes of lordosis in some patients are obvious, especially the C2-7 angle, and these could cause changes in the anatomical relationship between the cervical spine and the anterior esophagus, which may cause dysphagia. However, there have been few reports describing the effect of difference between postoperative and preoperative C2-7 angle (dC2-7A) on postoperative dysphagia after ACDF with Zero-P. Thus, the purpose of this retrospective study was to investigate the effect of the difference in C2-7 angle on dysphagia after anterior cervical discectomy and fusion (ACDF) with the Zero-P Implant System. Material and Methods: A retrospective analysis of 181 patients who underwent ACDF with the Zero-P Implant System and had at least one year of follow-up was performed from January 2011 to November 2018. All patients were divided into a non-dysphagia group and a dysphagia group to explore the effect of difference between postoperative and preoperative C2-7 angle (dC2-7A) on postoperative dysphagia. At the same time, other possible related factors including the difference between postoperative and preoperative O-C2 angle (dO-C2A), sex, age, body mass index (BMI), intraoperative time, estimated blood loss, diabetes mellitus, hypertension, smoking, alcohol consumption, prevertebral soft-tissue swelling (PSTS), the highest segment involved in the surgery and the levels of surgery segments were analyzed. Results: There were 139 patients in the non-dysphagia group and 42 patients in the dysphagia group. The single-factor analysis showed smoking, PSTS and dC2-7A was significantly different between two groups (p < 0.05). Spearman’s correlation coefficient showed no significant correlation between degree of dysphagia and dC2-7A (p > 0.05). The results of multiple-factor analysis with an ordinal logistic regression model showed that smoking, PSTS and dC2-7A were significantly associated with the incidence of dysphagia (p < 0.05). Conclusion: The postoperative C2-7 angle has an important effect on the occurrence of dysphagia in patients undergoing Zero-P implant system interbody fusion surgery.
Keywords: Dysphagia, Zero-P, Cervical vertebrae, Related factors
1413
A276: Assessment of coronal balance in scoliotic patients with lumbar distal junctional pathology: a retrospective analysis
Sara Montanari 1 , Giulia Delbue 1 , Cristiana Griffoni 2 , Luca Cristofolini 1 , Alessandro Gasbarrini 2 , and Giovanni Barbanti Bròdano 2
1 Department of Industrial Engineering, Alma Mater Studiorium - University of Bologna, Bologna, Italy
2 Spine Surgery Unit, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Posterior fixation aims to recover the physiological coronal balance and alignment of the spine in patients where less invasive treatments are unsuccessful. One of the main complications of lumbar posterior fixation is the distal junctional pathology. The impact of coronal imbalance on junctional pathology onset is less investigated in the literature than the effect of the sagittal alignment [1] and the correlation between radiological data and clinical outcomes is an open challenge. So, the aim of this study was to investigate if the spinopelvic parameters in the coronal plane affect the probability of distal fixation failure. Material and Methods: All posterior screws-based surgical corrections of scoliosis performed at Rizzoli Institute in 2017-2018 were retrospectively analysed, after ethical committee approval. A total of 31 cases which required a revision surgery due to distal lumbar junctional pathology were included in the fixation failure group (FAIL). The inclusion criteria were that distal fixation failure was caused by: i) pedicle screws pullout and/or ii) breakage of rods or screws and/or iii) vertebral fracture and/or iv) disc degeneration in the most caudal instrumented level, or immediately below. All the 66 surgeries which to date have not shown complications were identified as a control group (CONTR). Demographic and clinical data were collected. Pelvic obliquity (PO), Clavicle angle (CA), Sacral obliquity (SO), T1 tilt, Coronal balance distance (CBD) and the Cobb angle in the main, second and third curve were measured with the software Surgimap (Nemaris) from pre-operative (pre-op) and post-operative (post-op) standing frontal X-rays both for FAIL and CONTR, and before the revision (pre rev) for FAIL. Results: Junctional pathology in the distal region was caused by the breakage of rods in the 50% of cases. Failure onset was observed within a mean period of 27 months (64.5% of cases). Both the mean age and BMI differed significantly between the two groups (age: FAIL = 31, CONTR = 60; BMI: FAIL = 25.8, CONTR = 20.4; p < 0.0001, unpaired t-test, both). PO, CA, SO and T1 tilt did not show statistically significant differences. CBD was out of the range of coronal balance (CBD < 30 mm[2]) in FAIL before the primary surgery, and statistically significant differences were observed between pre-op and post-op (p = 0.0064, Anova). All the Cobb angles differed significantly between FAIL and CONTR pre-operatively (p < 0.001 unpaired t-test); larger Cobb angles were observed in CONTR. Statistically significant differences were also observed between pre-op and post-op both in FAIL and CONTR Cobb angles (p < 0.001, paired t-test, all cases). Conclusion: These results show that some coronal parameters are correlated with distal lumbar junctional pathology. Specifically, PO, CA, SO and T1 tilt did not seem to impact fixation failure. Conversely, CBD values out the recommended ranges of coronal balance before fixation seemed to be predictors of failure. Moreover, the Cobb angles appeared to be strongly linked with the CBD: low values of the deformity associated with a spine imbalance had a high correlation with the lumbar distal junctional pathology.
References
1. Daubs et al, Spine, 2013
2. Bao et al, Bone Joint J, 2016
650
A277: Determining the effect of intraoperative TXA on postoperative blood loss in ACDF
Anthony Steinle 1 , Jessa Fogel 1 , Jeffrey Chen 1 , Hani Chanbour 2 , Andrew Croft 1 , Wilson Vaughan 1 , Ayub Karwandyar 1 , Judy Mcdonough 1 , Philip Chandler 1 , Raymond Gardocki 1 , Scott Lawrence Zuckerman 1,2 , Amir Abtahi 1,2,3 , and Byron Stephens 1,2,3
1 Department of Orthopaedic Surgery
2 Department of Neurological Surgery
3 Center for Musculoskeletal Research, Vanderbilt University Medical Center, Nashville, TN, United States
Introduction: Fibrinolysis is a highly regulated enzymatic process that can transiently increase during medical procedures and cause increased blood loss. TXA is often administered during procedures to reduce postoperative blood loss and surgical duration without increasing risk of complications or thrombotic events. The primary aim of our study was to examine the impact of intraoperative TXA in ACDF on postoperative bleeding. Material and Methods: A tertiary medical center’s prospectively collected registry was queried for patients who underwent elective ACDF and received a drain postoperatively. Patients with coagulopathy, perioperative anticoagulant use, liver/renal failure, severe cardiac disease, cancer, or traumatic indication for ACDF were excluded. Patients were separated into two groups; those who received intraoperative TXA and those who did not. Baseline variables included age, gender, BMI, number of levels fused, and spine pathology. The primary outcome was postoperative blood loss, measured by 24-hour drain output. Secondary outcomes included total drain output, intraoperative EBL, surgery duration, drain duration (total time drain remained in place), changes in preoperative to postoperative Hb and Hct levels, and rate of transfusions, complications (including hematomas and thromboembolic events), and reoperations within 3 months. Multiple statistical tests were used to compare groups. Results: Our sample had 190 TXA patients and 96 non-TXA patients. There were no differences between groups for any baseline variables or number of levels fused. On bivariate analysis, the non-TXA group had a greater decrease in Hb (1.50 ± 1.41 vs 1.00 ± 1.26, p = 0.006) and Hct (4.93 ± 4.56 vs 3.15 ± 3.81, p = 0.003) between preoperative and postoperative labs compared to the TXA group. There were no differences in 24-hour drain output, total drain output, drain duration, or complication rates between groups. On univariate analysis, intraoperative TXA was associated with a decrease in 24-hour drain output (β = -9.65, 95% CI: -17.5 to -1.79, p = 0.016), total drain output (β = -11.6, 95% CI: -21.2 to -1.97, p = 0.018), and a reduction in change in Hb (β = -0.5, 95% CI: -0.87 to -0.13, p = 0.008) and Hct (β = -1.78, 95% CI: -2.96 to -0.61, p = 0.003) between preoperative and postoperative labs. There was no association between TXA and drain duration, intraoperative EBL, surgery duration, or rate of transfusions, complications, or reoperations. Controlling for baseline variables, multivariate analysis showed intraoperative TXA was associated with shorter drain duration (β = -5.74, 95% CI: -10.9 to -0.53, p = 0.031) and reduction in 24-hour drain output (β = -12.2, 95% CI: -19.4 to -4.89, p = 0.001) and total drain output (β = -14.0, 95% CI: -22.9 to -5.05, p = 0.002). Additionally, intraoperative TXA was associated with smaller decreases between preoperative and postoperative Hb (β=-0.49, 95% CI: -0.86 to -0.12, p=0.011) and Hct (β = -1.76, 95% CI: -2.95 to -0.58, p = 0.004). TXA had no impact on intraoperative EBL, surgery duration, or rate of transfusions, complications, or reoperations. Conclusion: Our results suggest intraoperative TXA use in ACDF procedures leads to a decrease in perioperative blood loss and faster drain removal. Additionally, TXA administration did not increase the risk of thromboembolic complications. We conclude that intraoperative TXA is a safe and effective agent for reducing perioperative blood loss in ACDF surgery.
1135
A278: The impact of prolonged operative duration on postoperative venous thromboembolic events following thoracolumbar spine surgery
Khoa Tran 1 , Yunsoo Lee 1 , Mark Lambrechts 1 , Tariq Issa 1 , Cannon Hiranaka 1 , Skylar Nahi 1 , Andrew To karski 1 , Dominic Lambo 1 , Blaire Adler 1 , Jose Canseco 1 , Alan Hilibrand 1 , Christopher Kepler 1 , Alexander Vaccaro 1 , and Gregory Schroeder 1
1 Rothman Orthopedic Institute at Thomas Jefferson University, Philadelphia, United States
Introduction: VTE risk stratification and proper prophylaxis protocols are particularly important in spine surgery due to the risk of potentially catastrophic bleeding events such as epidural hematomas, which can lead to irreversible neurologic deficits. The relationship between operative duration and its effect on postoperative venous thromboembolism (VTE), however, remains unclear in spine surgery. Therefore, the aim of this study was to determine the effect of operative duration on 90-day postoperative VTE rates in patients undergoing thoracolumbar spinal procedures and to determine whether an optimal cutoff exists that marks significant increases in VTE risk. Material and Methods: A retrospective cohort study was conducted on patients who received surgery at an urban, academic medical center and affiliated sites. A structured query language (SQL) search was used to identify patients over 18 years of age who underwent thoracolumbar fusion between 2007 and 2021. Patients were excluded from the study if they lacked recorded operative durations or received surgical intervention for any malignant tumors, infections, trauma, or revision. Operative duration was defined as time from first skin incision to skin closure. A receiver operating characteristic (ROC) curve using Youden’s index was created to determine a “cutoff” time for predicting increased likelihood of a VTE event based on surgical duration. Results: After controlling for patient demographics, a 2:1 propensity match was constructed resulting in a final cohort of 81 patients with VTE and 161 without. There were no differences in any matched patient or surgical characteristics. Patients with a thromboembolic event had higher operative duration (defined as cut-to-close time) (341 vs. 261 minutes, p = 0.001), longer total hospital length of stay (LOS) (6.15 vs. 4.50 days, p < 0.001), and were more likely to experience a 90-day readmission (21.0% vs 4.25%, p < 0.001). Operative duration (OR: 1.004, 95% CI: 1.002 – 1.006, p < 0.001) was a predictor of VTE risk. Moreover, for each per-hour increase in operative duration, there was a 24% increase in VTE event risk. Total hospital LOS (OR: 1.14, 95% CI: 1.05-1.24, p = 0.003), and discharge to acute inpatient rehab (reference: home, OR: 2.29, 95% CI: 1.13-4.62, p = 0.021) were also predictors of increased postoperative VTE rates on unadjusted bivariate logistic regression analysis. On multivariate logistic regression, operative duration was an independent predictor of VTE risk (OR: 1.004, 95% CI: 1.001 – 1.006, p = 0.002). When evaluating the ROC, a cutoff time of 218.00 mins was identified (AUC [95% CI] = 0.631 [0.555 – 0.706]) as an optimal predictor of increased risk for a VTE event. The sensitivity of this predictor was 77.8% while specificity was 43.5%. Conclusion: Our study demonstrated that operative duration, defined as time from skin incision to skin closure, significantly predicted venous thromboembolic events, especially after surgical time cutoff of 218 minutes. Each additional hour of operative duration was found to increase VTE risk by 24%. Identifying these high-risk patients can be important to optimizing discharge pathways and streamlining postoperative care for such patients to help prevent VTE events and their potentially catastrophic sequelae.
740
A279: Surgical outcomes and opioid consumption after lumbar decompression in patients with preoperative marijuana use
Delano Trenchfield 1 , Yunsoo Lee 1 , Mark Lambrechts 1 , Parker Brush 1 , Alex Christianson 1 , Azra Deez 1 , Bright Wiafe 1 , Tariq Issa 1 , Jeremy Heard 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alexander Vaccaro 1 , Chris Kepler 1 , and Gregory Schroeder 1
1 Division of Spine Surgery, Rothman Orthopaedic Institute, Philadelphia, United States
Introduction: Studies have shown that cannabinoids, the active components of marijuana, are effective pain modulators. Providers have begun to explore marijuana as an alternative for pain, particularly with the well-known consequences of opioids and increased legislation limiting its use. However, there is insufficient literature available investigating the effects of marijuana use on patient outcomes and opioid use after spine surgery. Our study aims to analyze this in patients who have undergone lumbar decompression without fusion. Materials and Methods: All patients >18 years of age who underwent lumbar decompression from 2017-2022 with preoperative marijuana at our academic institution were retrospectively identified. A 3:1 propensity match incorporating demographics, procedure type, and levels decompressed was performed to compare preoperative marijuana users and non-users. Patient demographics, clinical outcomes including readmissions, revisions, and complications, and 1-year preoperative and postoperative opioid consumption in milligram of morphine equivalents were compared between groups. A multivariate regression model was performed to measure the effect of marijuana use on the likelihood of a spine reoperation. Statistical significance was set at p < 0.05. Results: Of the 312 included patients, 78 used marijuana preoperatively. There were no significant differences in complications, 90-day readmissions, revision rates, preoperative opioid consumption, or postoperative opioid consumption (p > 0.05). Multivariate logistic regression analysis demonstrated that marijuana use trended towards being a predictor for all-spine reoperations (OR = 1.96, p = .063). Conclusions: There were no differences after lumbar decompression in surgical outcomes or opioid consumption between patients who did and did not use marijuana. This is in stark contrast to preoperative narcotic use. Furthermore, while we found no significant association between marijuana use and reoperation rate, a trend toward it being a predictive factor was noted, indicating a need for further research on the effects of marijuana after spine surgery.
OP32: Complex Cervical Surgery
84
A280: The role of disc degeneration in planning fusion at the cervicothoracic junction: a kinematic MRI study of 93 individuals
Michael Kim 1 , Zachary Gilbert 1,2 , Zabiullah Bajouri 2 , Sagar Telang 1 , Zoe Fresquez 1 , Trevor Pickering 3 , Seung Min Son 4 , Ram Alluri 1 , Jeffrey C. Wang 1 , and Zorica Buser 1,5,6
1 Orthopaedic Surgery
2 Neurological Surgery
3 Southern California Clinical and Translational Science Institute, Keck School of Medicine of USC, Los Angeles, United States
4 Pusan National University Yangsan Hospital, Orthopedic Surgery, Yangsan-si , South Korea
5 NYU Grossman School of Medicine, Orthopedic Surgery, New York, United States
6 Gerling Institute, Center for Musculoskeletal and Neurological Care, New York, United States
Introduction: Cervical spine fusion can increase biomechanical stress on unfused levels, increasing the risk of adjacent segment degeneration (ASD). Fusion terminating at C7 increases risk of ASD due to the unique biomechanics of the cervicothoracic junction (CTJ). Fixation across the CTJ may reduce risk of re-operation due to ASD. However, multi-level fusion increases operative time, complexity, and risk of complication. Furthermore, recent studies reporting contradicting results. While many studies have examined the impact of cervical fusion on CTJ DD, no study has investigated biomechanics or risk factors that may contribute to surgical planning. Planned distal and adjacent levels should be assessed for disc degeneration (DD), which increases risk of ASD. This study assessed whether DD at the CTJ was associated with DD, disc height, translational motion, or angular motion in the adjacent superior (C6/C7) or inferior (T1/T2) levels. Material and Methods: Initially, 100 patients without previous spine surgery were randomly selected from a database of kinematic MRI studies. DD was assessed using Pfirrmann classification. Disc height was measured at the mid-disc in neutral and extension. Translational motion and angular motion were calculated by assessing translational or angular motion segment integrity respectively in flexion and extension. All variables were examined for univariate and bivariate distributions. The association between disc degeneration at the CTJ and all other variables was assessed using scatterplots and nonparametric Kendall’s Tau correlation coefficient. A value of α = 0.05 was used for all statistical tests. Results: This study included 93 patients (48 males, 45 females) with a mean age of 47 ± 17 years (range 20 - 99 years). Seven patients were excluded due to insufficient image quality. Lordosis, disc degeneration, and disc height were found to be normally distributed, while translational motion, angular motion, and Modic changes were right-skewed. No missingness was appreciated in any variable. DD at the CTJ was positively associated with DD at C6/C7 (tau = 0.53, p < 0.01) and T1/T2 (tau = 0.58, p < 0.01), with greater disc height in neutral position at T1/T2 (tau = 0.22, p < 0.01), and with greater disc height in extended position at C7/T1 (tau = 0.17, p = 0.04) and at T1/T2 (tau = 0.21, p < 0.01). DD at C7/T1 was negatively associated with angular motion at C6/C7 (tau = -0.23, p < 0.01). No association was appreciated between DD at C7/T1 and translational motion. Conclusion: This study demonstrates that DD at the CTJ is associated with DD and greater disc height at adjacent levels. Previous studies have demonstrated DD at levels adjacent to the terminal fusion level increase risk of ASD. This emphasizes the necessity for careful selection of the distal level in multilevel fusion in the cervical spine, particularly at the CTJ where the biomechanics of the level itself increase risk of ASD. Further studies are required to provide clinical correlation. However, surgeons should consider DD and disc height at levels adjacent to the CTJ when considering where to terminate multi-level cervical spine fusion.
262
A281: The utility of RAPT score to identify risk of extended length of stay and non-home discharge following surgery for cervical degenerative pathology: a multivariate analysis
Ayush Arora 1 , Alekos Theologis 1 , Matt Callahan 1 , Thomas Peterson 1 , and Sigurd Berven 1
1 Department of Orthopaedic Surgery, University of California, San Francisco, San Francisco, United States
Introduction: Cases of high-cost outliers in spine surgery for cervical degenerative pathology are strongly implicated with patients who require extended length of stay (eLOS) and post-operative rehabilitative services. There is thus a need to identify risk factors that are pre-operatively associated with eLOS and non-home discharges for patients with cervical degenerative pathology. So far, few studies utilize social support in cervical spine surgery risk assessment. One such measure known as the Risk Assessment and Prediction Tool (RAPT) score holds significant potential by capturing presence of patient community support, extent of home care, gait aid, and preoperative functional ability. The purpose of this study is to identify independent risk factors, including the RAPT score, associated with eLOS and discharge to rehabilitation following elective operations for cervical degenerative pathology. Material and Methods: Records were obtained from the Electronic Health Record (EHR) for adult patients with a pre-operative RAPT score, who underwent surgical intervention for cervical degenerative pathology at a single academic institution (2016-2021). Predictor variables included demographics, comorbidities, operative information, and social support (RAPT score). Outcomes were eLOS ( days) and discharge location (home vs rehabilitation). Fisher’s exact test was used for univariate analysis, and significant variables were considered for multivariate binary logistic regression, with generation of 95% percent confidence intervals (CI), odds ratios (OR), and p-values. Results: Four hundred twelve patients met inclusion and were analyzed. Post-operatively, 14.1% (n = 58) had eLOS and 15% (n = 62) were discharged to acute rehabilitation. Variables significant for both outcomes(eLOS and rehabilitation discharge) were lower RAPT scores and a diagnosis of depression or anxiety. Risk factors only associated with eLOS were surgical procedure (posterior fusion 1-3 levels, circumferential fusions) and chronic obstructive pulmonary disease (COPD), while the risk factor only associated with discharge to rehabilitation was eLOS. Conclusion: Preoperative identification of patients at risk for eLOS and non-home discharges after elective degenerative cervical spine surgery ideally will assist in shared decision making, management of patient expectations, a priori discharge planning, and minimization of financial risk to payor and hospital. Given the RAPT score’s high degree of association with eLOS and rehabilitation discharge, preoperative optimization of the RAPT’s individual components may prove fruitful for decreasing LOS and modifying discharge disposition.
1675
A282: Bibliometric and visualized analysis of the top 100 most cited articles on anterior cervical surgery
Junbo He 1 , Tingkui Wu 1 , Beiyu Wang 1 , and Hao Liu 1
1 Orthopedic Surgery, West China Hospital, Sichuan University, China
Introduction: Anterior cervical surgery (ACS) owes its development to various pioneering individuals whose revolutionary works form key advances and guide current medical decisions. This bibliometric aimed to identify, analyze and visualize the main features of the most-cited papers in ACS. Material and Methods: A literature search was performed on the Web of Science Core Collection database using pre-defined search terms. The results were ranked according to the citation count and selected to create a single database. Title, authorship, year of publication, country and institution of publication, number of citations, citations per year, topic, and surgical types were recorded for analysis. VOSviewer software was used to create graphical bibliometric maps. Results: A total of 18,556 eligible papers were retrieved. Citations for the top 100 most-cited articles ranged from 148 to 1,197, and citations per year ranged from 3.1 to 89.8. Most top 100 articles represented Level III evidence, followed by Levels IV, II, I, and Ⅴ. The articles were published from 1958 to 2016, with the 2000s being the most active decade. The majority of the articles were from the United States, followed by Japan and Germany. The leading journals of publication were Spine with the highest number of citations and the Journal of Bone and Joint Surgery American Volume with the highest number of mean citations. The two main focus areas were “fusion” and “complications”. About 80% of the top 100 articles were related to anterior cervical discectomy with fusion (ACDF), followed by anterior cervical corpectomy with fusion (ACCF, 28%), cervical disc arthroplasty (CDA, 15%), and anterior cervical discectomy (ACD, 7%). Conclusion: This bibliometric study provides detailed information on the top 100 most-cited articles in ACS. Generally, the United States, as the birthplace of ACS, has the most in-depth and influential articles and the most prominent contribution. Although ACDF is the most mentioned, CDA is of gradual greater impact. These insights into the priorities and trends of the research could help future academic pursuits.
1129
A283: Is disc height loss at one year predictive of pseudarthrosis and revision surgery following anterior cervical discectomy and fusion
Jeremy Heard 1 , Yunsoo Lee 1 , Nicholas D'Antonio 1 , Mark Lambrechts 1 , Goutham Yalla 1 , Hannah Levy 1 , Garrett Breyer 2 , Tariq Issa 1 , Delano Trenchfield 1 , Parker Brush 1 , John Bodnar 2 , Jose Canseco 1 , Christopher Kepler 1 , Alan Hilibrand 1 , Alexander Vaccaro 1 , and Gregory Schroeder 1
1 Orthopedic Surgery, The Rothman Orthopedic Institute at Thomas Jefferson University Hospital, Philadelphia, United States
2 Thomas Jefferson University, Philadelphia, United States
Introduction: Structural allograft is a commonly used option for recreating disc height during anterior cervical discectomy and fusion (ACDF) due to the morbidity associated with of iliac crest autograft harvesting. As it can behave as a scaffold for bone remodeling before its incorporation into the fusion mass, structural allograft is an attractive and cost-effective option. However, it can also lead to resorption and subsidence, which causes a loss of disc height. There are few studies characterizing whether disc height loss affects the likelihood of successful fusion or if it has any effect on patient-reported outcome measures (PROMs). To determine the effect of disc height loss on surgical and clinical outcomes, we aimed to study the following objectives: (1) investigate if disc height loss is associated with a greater risk of pseudarthrosis following ACDF and (2) determine the effect of disc height loss on one-year postoperative patient-reported outcomes measures (PROMs). Methods: Upon approval, all patients greater than 18 years of age who underwent primary one- to three-level ACDF with structural allograft interbody spacers at our urban, academic medical center from 2016 to 2019 were retrospectively identified. Only patients with one-year postoperative lateral and flexion-extension cervical spine radiographs were included. Patients were excluded if the ACDF was performed as a revision procedure, part of a combined anterior/posterior approach, included a concomitant cervical corpectomy, or was indicated in the setting of trauma, infection, or neoplasm. PROMs extracted included the VAS Neck and VAS Arm, the NDI, and the Mental and Physical Component Scores of the Short-Form 12 (SF-12) Health Survey (MCS-12 and PCS-12, respectively). Radiographic fusion was defined as <1 mm of interspinous motion between each instrumented level and >4 mm of motion at any adjacent unfused level in accordance with the guidelines published by the Cervical Spine Research Society (CSRS) Special Project Committee, while >1 mm of interspinous motion at any instrumented level was defined as a pseudarthrosis. Logistic regression models and receiver operating characteristic (ROC) curves were used for analysis. Alpha was set at p < 0.05. Results: Of the 466 included patients, 221 (47.4%) had <2 mm of anterior or posterior disc height loss, while 245 patients (52.6%) had >2 mm of anterior or posterior disc height loss. Patients in the >2 mm group were more likely to develop pseudarthrosis (p = 0.021), but not undergo revision surgery due to pseudarthrosis (p = 0.459). Those patients had significantly less improvement (D) in NDI (p = 0.002), VAS Arm (p = 0.018), and VAS Neck (p = 0.011) at one year following surgery. Multivariable analysis identified male sex (OR = 1.66, p = 0.013), the number of levels fused (OR = 2.09, p < 0.001), and fusion at C6-C7 (OR = 1.52, p = 0.043) as predictors of disc height loss. Disc height loss (OR = 1.29, p = 0.232) was not identified as a significant predictor of pseudarthrosis. Conclusions: Disc height loss following ACDF is not predictive of pseudarthrosis development or revision surgery for pseudarthrosis. Additionally, loss in disc height was significantly associated with worsened PROMs.
1579
A284: Malposition rates of subaxial cervical pedicle screws placed using intraoperative CT (O-arm) based 3D navigation
Jonathan N. Sembrano 1 , Jason Haselhuhn 1 , Kenneth Holton 1 , Michael Brush 1 , Christopher Martin 1 , Matthew Hunt 2 , Ann M. Parr 1 , Kristen Jones 1 , David Polly 1 , and Robert Morgan 3
1 University of Minnesota, Minneapolis, United States
2 M Health Fairview Spine and Brain Clinic, Edina, United States
3 St. Louis Minimally Invasive Spine Center, St. Louis, United States
Introduction: Cervical pedicle screws (CPS) are biomechanically superior to other spinal fixation anchors; however, placement is technically demanding, and screw malposition could have catastrophic consequences. Computer navigation has been shown to improve accuracy rates in thoracolumbar pedicle screw placement. However, there are limited studies on use of navigation for placing CPS. We report accuracy rates of computer navigated (CN) CPS placement in a single institution. Materials and Methods: Between January 2014 and March 2020, we identified 100 patients who underwent CN CPS placement (C3-C7) and with either postoperative computed tomography (CT) or intraoperative O-arm 3D scan for screw evaluation. Screw position was evaluated in axial, coronal and sagittal planes, and graded as follows (figure 1): 0 – fully in bone; I –minor breach deemed inconsequential (< 25% of screw width); II – breach that is considered not ideal, but acceptable (25-50% of screw width); III – breach that is considered either dangerous or compromising strength of fixation. Screws that were >50% outside the pedicle in any direction were considered grade III. Results: 413 CN CPS screws (C3-C7) were placed in 100 patients (54M:46F), with a mean age of 56 years (range 10-81). Number of fusion levels ranged from 1 to 12. 44 patients had previous cervical spine fusion (29 anterior; 15 posterior). 12 patients underwent proximal extension of previous thoracolumbar fusion. Rates of serious screw malpositions: Gr III = 15/413 (3.6%), combined Gr II/III = 42/413 (10.2%). A breakdown of Gr III screws per level: C3 = 1/33 (3.0%), C4 = 3/63 (4.8%), C5 = 3/72 (4.2%), C6 = 5/85 (5.9%), C7 = 3/160 (1.9%). Breaking down the combined Gr II/III screws per level: C3 = 8/33 (24.2%), C4 = 9/63 (14.3%), C5 = 8/72 (11.1%), C6 = 10/85 (11.8%), C7 = 7/160 (4.4%). Mean screw grade per level: C3 = 0.88; C4 = 0.67; C5 = 0.51; C6 = 0.46; C7 = 0.26. Using non-parametric ranksum tests with Bonferroni correction, significant differences were noted between the following: C3 vs each of the two most caudal levels (C6 and C7; p = 0.029 and <0.001 respectively); and C7 vs each of the upper 2 levels (C3 and C4; p = 0.029 and <0.001, respectively). Conclusion: Our study shows a 3.6% rate of dangerous/unacceptable (Gr III) screw placement, and 10.2% non-optimal (combined Gr II and III) using intraoperative 3D imaging and computer navigation. Mean screw grade incrementally decreased in a cephalad to caudad direction (C3 to C7), indicating that pedicle breach is more likely at the upper subaxial cervical levels. This also confirms that C7 is the safest level for CPS placement. Our results add to only few other studies that have reported on this technique. To our knowledge this is the biggest study on a uniform technique of navigated pedicle screw placement that included only subaxial levels C3-C7.
649
A285: Are all cervical cages created equal? An analysis of decade of adverse event reports in the United States
Victor Ungurean 1 , Amit Piple 1 , Oluwatodimu Raji 1,2 , Andrea Rowland 2 , Adam Schlauch 2 , Dimitriy Kondrashov 1,2 , Ken hsu 2 , and James Zucherman 2
1 The Taylor Collaboration, San Francisco, United States
2 Orthopaedic Surgery, St. Mary's Medical Center, San Francisco, United States
Introduction: Although The Food and Drug Administration (FDA) aims to ensure safety and efficacy of cervical interbody cages post-implantation, these implants may experience transient loading conditions during implantation which may be overlooked. Despite its importance for preoperative planning before cervical spine fusion, there is a paucity of data in the literature characterizing perioperative failure rates among the commercially available implants in the U.S. Therefore, the goal of this study is to characterize perioperative failure patterns of cervical interbody cages on the basis of their manufacturer and production material. Methods: The FDA’s Manufacturer and User Facility Device Experience (MAUDE) database was queried for all reports of cervical interbody cage device failures from 2012 to 2021. Each report was manually analyzed and categorized on the basis of failure type (i.e. cage breakage, cage migration, screw failure, instrumentation failure, and assembly failure). The implants were then categorized by their core and surface material. Two market analyses were performed. First, “failure-to-market share indices” were generated by dividing the number of failures per year for each implant material subtype by its yearly U.S. market share in cervical spine fusion. Second, “failure-to-revenue indices” were calculated by dividing the total number of failures per year for each manufacturer by their approximate yearly revenue from spinal implants in the U.S. Outlier analysis was performed to generate a threshold value above which failure rates exceeded the normal index. Results: Overall, 807 entries were and 716 met inclusion criteria. Of these, 303 (42.3%) were breakages, 48 (6.7%) were migrations, 152 (21.2%) were instrumentation-related failures, 151 (21.1%) were assembly failures, and 72 (10.1%) were screw failures. Of the breakages, 287 had a core composed of PEEK (94.7%) whereas 6 (2.0%) had a core composed of titanium. Of the migrations, 22 (45.8%) had a surface composed of PEEK, 23 (47.9%) were composed of titanium, and 2 (4.2%) were composed of silicon-nitride. PEEK implants had a higher failure-to market-share index for both migration and breakage compared to titanium. A yearly decrease in failure-to-market share indices were observed for both failure subtypes. Upon manufacturer analysis, Zimmer-Biomet, K2M, and LDR Medical had failure-to-revenue indices exceeding the calculated threshold (3.92 failures/100 million). Discussion: Cervical cages manufactured using PEEK were more likely to fail by breakage than migration whereas titanium cages were more likely to fail by migration than breakage. However, PEEK implants had a higher failure-to-market share index for both failure types compared to titanium. A year-over-year reduction in failure-to-market share indices was observed for both PEEK and titanium. Market analysis of manufacturers demonstrated that Zimmer-Biomet implants exceeded the failure-to-revenue index threshold in the most recent years. Importantly, many of these implant failures occurred intraoperatively during instrumentation, which underscores the need for FDA evaluation of these implants under these loading conditions prior to commercial approval. Further studies regarding the influence of patient and operative factors on cervical interbody failures are warranted as the MAUDE database does not contain clinical data.
1984
A286: Comparative complications associated with BMP use in patients undergoing ACDF for degenerative spinal conditions: systematic review and meta-analysis
Christopher Martin 1 , Kenneth Holton 1 , Samuel Broida 2 , Anne-Katrin Hickmann 3 , Caitlin Bakker 1 , Paul Lender 1 , Kota Watanabe 4 , Meisel Hans-Jorg 5 , Zorica Buser 6 , Steven Presciutti 7 , and Timothy S. Yoon 7
1 University of Minnesota, Minneapolis, United States
2 Mayo Clinic, Rochester, United States
3 Kantonsspital St. Gallen, St. Gallen, Switzerland
4 Keio University, Tokyo, Japan
5 Berufsgenossenschaftliche Clinic, Halle, Germany
6 Gerling Institute, New York, United States
7 Emory University, Atlanta, United States
Introduction: Anterior cervical discectomy and fusion (ACDF) is amongst the most commonly performed surgical interventions in spine surgery with generally reported excellent outcomes. However, concerns over nonunion persist in certain patient populations, so recombinant human bone morphogenic protein-2 (BMP2) has been used as a strategy to combat nonunion in these patients. In 2008 the FDA issued a warning recommending against BMP2 use in anterior cervical applications due to reports of significantly increased incidence of anterior swelling and dysphagia with use of BMP2. Despite this warning, BMP2 continues to be used off label in the anterior cervical spine, with various strategies reported as successfully reducing morbidity risk. Thus, the overall morbidity profile of BMP2 use in anterior cervical surgery remains unclear. The purpose of this study was to perform a systematic review and meta-analysis of studies that reported on BMP2 use in ACDF surgeries. Materials and Methods: A comprehensive systematic search of nine online databases was conducted using PRISMA guidelines. Inclusion criteria included English language studies with a minimum of 10 adult patients undergoing instrumented ACDF surgery for a degenerative spinal condition in which BMP2 was used in one of the treatment arms. Studies with patients undergoing circumferential fusions, with non-degenerative indications, or which did not report post-operative complication data were excluded. Patients with and without BMP2 were compared in terms of the incidence of dysphagia/dysphonia, any anterior soft tissue complication (hematoma, seroma, infection, dysphagia/dysphonia), nonunion, any medically related complication, and any new neurologic deficit. Results: Of 1,832 preliminary search results, 27 manuscripts were included in the review. In the resultant meta-analysis, the incidence of dysphagia or dysphonia (weighted mean of 18.6% v. 4.2%, p < 0.05) and anterior soft tissue complications (weighted mean 13.8% v. 4.3%, p < 0.05) were significantly higher in the BMP2 cohort. There was a significant decrease in the incidence of nonunion in the BMP2 cohort (weighted mean 0.9% v. 5.5%, p < 0.05). There was no difference in the incidence of general medical complications, or in the incidence of new neurologic deficits. Conclusions: This meta-analysis identified a high rate of arthrodesis when BMP2 was used in anterior cervical fusions, but confirmed the previously widely reported concerns regarding increased rates of dysphagia and anterior soft tissue complications. Surgeons who choose to use BMP2 may wish to reserve implementation for cases with a high risk of non-union, and should be aware of the risk of airway compromise.
1979
A287: A systematic review of current terminology for conditions preceding degenerative cervical myelopathy: evidence to inform an AO Spine expert opinion statement
Vinisha Agrawal 1 , Froher Yasin 1 , Aria Nouri 2 , Benjamin Davies 3 , Ratko Yurac 4 , Vishal Kumar 5 , Rory Murphy 6 , Enrico Tessitore 2 , Granit Molliqaj 2 , Joost Dejaegher 7 , Guy Wynne-Joes 8 , Juan José Zamorano 9 , and Oliver Mowforth 10
1 School of Clinical Medicine
2 Division of Neurosurgery, University of Geneva, Geneva, Switzerland
3 Division of Neurosurgery
4 Department of Orthopaedic Surgery, Universidad del Desarrollo, Santiago, Chile
5 Department of Orthopaedic Surgery, PIGMER, Chandigarh, India
6 Division of Neurosurgery, Barrow Neurological Institute, Phoenix, United States
7 Division of Neurosurgery, Faculty of Medicine KU Leuven, Leuven, Belgium
8 Division of Neurosurgery, The Newcastle Upon Tyne Hospitals NHS Foundation Trust, Newcastle, United Kingdom
9 Department of Orthopaedic Surgery, Clinica Alemania de Santiago, Santiago, Chile
10 Department of Clinical Neurosciences, University of Cambridge, Cambridge, United Kingdom
Introduction: Degenerative Cervical Myelopathy (DCM) is a disease of ageing spines, which results in symptomatic spinal cord compression. It is an umbrella term introduced by Nouri et al 2015 that encompasses various degenerative spinal cord diseases such as cervical spondylotic myelopathy (CSM), degenerative disk disease (DDD), ossification of the posterior longitudinal ligament (OPLL) and ossification of ligamentum flavum (OLF). More recently, work has been done to understand the asymptomatic stage of DCM, where degenerative changes can be detected with imaging but patients are do not present with symptoms. Unfortunately, literature on the asymptomatic DCM contains various inconsistencies in their use of terminology to describe it. We believe that better characterisation of this stage will lead to more efficient stratification of patients and it will be easier for clinicians to find the appropriate management for their patients. Our aim is to produce standardised definitions of certain terminology to inform an AO Spine statement. Materials and Methods: We created a search strategy and used the Medline and Embase databases to find all articles on asymptomatic DCM. Two authors independently screened the title and abstract of 1937 articles using the pre-set inclusion and exclusion criteria. The selected 118 articles moved on for data extraction where the two authors independently extracted information on the different terminology used for asymptomatic stages of DCM and their definitions. With clinical studies, further patient demographic information was extracted. Additionally, both authors assessed the quality and bias of these papers using various JBI checklists. Finally, from the data collected, the frequency of different terminology in the literature was calculated and the different definitions for specific terms was analysed. Results: Overall, we found many synonyms of ‘asymptomatic’ used in the literature for example, ‘pre-symptomatic’, ‘non-myelopathic’, ‘sub-clinical DCM’ and ‘silent CSM.’ We have found that the largest inconsistencies have been with the terms “asymptomatic” and “myelopathy.” Regarding the term “asymptomatic” some papers define this as the stage where patients have radiological signs of degeneration but no clinical signs, whereas others use the term synonymously with ‘healthy controls.’ This became especially ambiguous in clinical studies where symptomatic patients were compared to pre-symptomatic and healthy volunteers. The other major discrepancy in the literature was whether the term “myelopathy” is just spinal cord compression or specifically symptomatic spinal cord compression. Conclusions: To conclude, there is substantial inconsistency in the terms used to describe degenerative states preceding DCM in the literature. We propose that ‘myelopathy’ is used specifically for symptomatic spinal cord compression as this is seen in the majority of papers and that the term ‘asymptomatic’ or ‘pre-symptomatic’ is used for patients with radiological signs but no clinical symptoms of DCM. We also propose the cessation in use of the term ‘non-myelopathic DCM’ to improve the consistency in the literature.
1604
A288: Are variable screw angle change and screw-to-vertebral body ratio associated with radiographic subsidence following anterior cervical discectomy and fusion?
Philip Louie 1 , Spencer Raub 1,2 , Caroline Drolet 1 , Jesse Shen 1,3 , Nicole Vivelo 1 , Michelle Gilbert 1 , Kellen Nold 1 , Jean Christophe Leveque 1 , and Venu Nemani 1
1 Neurosurgery, Virginia Mason Franciscan Health, Seattle, United States
2 School of Medicine, University of Washington, Seattle, United States
3 Université de Montréal, Canada
Introduction: Graft subsidence has been described as an inherent process in graft placement and healing following anterior cervical discectomy and fusion. However, excessive subsidence can lead to worsening neck pain, additional stenosis, and thus, a potential re-operation. Various factors have been identified as risk factors for subsidence including graft type, graft location, sagittal alignment change, number of levels, and bone mineral density. However, two other important variables: screw length and changes in variable screw angle over time, have not been evaluated in relation to subsidence. Longer screws are correlated with increased pull-out strength and reduction in pseudarthrosis rates. No studies have examined the impact of the change in angle of variable screw placement over time. Thus, the purpose of this study was to evaluate the impact of the screw-to-vertebral body ratio and change in angle of variable screws placed at the cephalad and caudal aspects of the construct on subsidence rates, based on interscrew distance and intradiscal heights (anterior/middle/posterior). Material and Methods: A retrospective cohort analysis was performed on consecutive patients who underwent a 1-3 level ACDF (allograft or PEEK cage) for degenerative pathology between January 2018 and June 2021 with 6 months follow-up by 3 spine-fellowship trained surgeons with similar techniques at a single center. Pre- and 6-month post-operative radiographic assessment included intradiscal height (ant/mid/post), intervertebral screw distance, and screw-vertebral body ratio of the cephalad and caudal screws. Demographic information, complications, and re-operation data was obtained. All analyses predict subsidence change scores (ant/mid/post intradiscal height, interscrew distance) from screw angle change (cephalad or caudal depending on top or bottom), postop screw angle, screw-to-vertebral body ratio, ACDF vs ACCF, postop subsidence measurement and demographic variables (age, sex, BMI, CCI). Screw angle change was included as an intermediate variable and was predicted by postop screw angle, screw to vertebral body ratio, and demographic variables. Results: In total, 65 patients undergoing a 1-3 level ACDF met inclusion criteria with 6 months follow-up. Graft type and number of levels fused consistently have no significant effect on any of the subsidence outcomes. Aside from females experiencing greater subsidence than males based on interscrew distance at both the top (p = 0.02) and bottom levels (p = 0.01), demographic variables are not associated with amount of subsidence. Greater screw-to-vertebral body ratio is associated with less subsidence (p < 0.05). The amount of variable screw angle change at the cephalad and caudal aspect of the construct do not impact the amount of subsidence observed. No patients reported neck pain in the setting subsidence greater than 3mm in any of the 4 measurements. Overall, no re-operations were performed for subsidence-related pathology. Conclusion: At a single center with similar surgical techniques, the change in angle of variable screws placed at the cephalad and caudal aspect are not associated with radiographic subsidence following anterior cervical discectomy and fusion for degenerative pathology 6 months following surgery. Greater screw-to-vertebral body ratio may be protective against some regions of radiographic subsidence. The clinical impact of these subsidence differences is an area of ongoing investigation.
OP33: Surgical Complications 3
1752
A289: Pharyngoesophageal perforations after anterior cervical surgery; literature review and illustrative case treatment algorithm
Brox Felix 1 , Darrel Brodke 1 , Nicholas Spina 1 , Ryan Spiker 1 , and Brandon Lawrence 1
1 Orthopedic Surgery, University of Utah Health, Salt Lake City, United States
Introduction: Pharyngoesophageal perforations (PEP) are extremely rare, yet very dangerous, complications that may follow anterior cervical spine surgery (ACSS). Among current literature, the incidence rate of PEP has been reported between 0.02% to 1.49%, while the mortality rate ranges from 20-50%.2 There is no consensus on the best treatment strategy. The literature reports differing techniques such as, no removal of ACSS hardware,3,11 removal of previous anterior hardware with insertion of new hardware at adjacent levels,10,12 insertion of autograft with and without plate fixation,11,13 and removal of hardware without direct repair of the defect.9 Not removing hardware has been found to be a primary factor in recurring perforations, chronic infections, and flap failure,3,6,10,17,20 all of which can lead to revision procedures with drastically higher levels of complexity. As recurrent perforations and stubborn infections are two of the largest possible risks after a PEP operation, proper care should be taken to avoid them without compromising the structural integrity of the cervical spine. We propose that 1) removing all anterior hardware, 2) performing a posterior cervical instrumented fusion, 3) closing the esophageal perforation through primary repair, and 4) reinforcing the site with a pedicled flap results in the best outcome. Material and Methods: We present a literature review of the current PEP treatment techniques and retrospectively discuss 10 cases of PEP at our facility. We examine how different treatment techniques had various levels of success in resolution of the PEP compared to the literature and propose a treatment algorithm. Results: We found that total removal of the anterior hardware, including any cages present (PEEK, titanium, allograft, etc.) in addition to reinforcement of the wall with a muscle flap resulted in the highest rate of success. One patient had several attempted surgeries without hardware removal but developed recurrent perforations/infections which were not resolved until her hardware was removed completely. The remainder of our patients had no problems with spinal stability/alignment despite a posterior-only reconstruction after their operations. Each showed surprising levels of bony re-incorporation of the anterior defects left by the removed hardware after repair and flap coverage which allowed for improved vascular inflow. This was achieved without any biologics or bone graft. These case illustrations highlight the importance of obtaining a hardware-free anterior cervical field for healing of the esophageal wall and reducing the risk of complex revision cases, especially in the setting of flap coverage. Conclusion: While the group of patients was small, we believe many things can still be learned from the outcomes of these patients after this rare complication. In the treatment of PEP after ACSS operations, we advocate for complete removal of all anterior hardware, reconstructing the structural integrity of the spine with posterior fixation, and allowing for vascular ingrowth of the perforation by the placement of muscle flaps. In our experience, this technique achieves the most optimal outcome of achieving spinal stability while allowing the esophagus to heal, drastically decreasing the risk of reoperation due to flap failure or infection.
1661
A290: Comparison of patients-reported postoperative dysphagia in patients undergoing one-level versus two-level anterior cervical discectomy and fusion with the Zero-P implant system
Chengyi Huang 1 and Hao Liu 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Introduction: We hypothesize that a greater number of surgical levels may result in a higher incidence of dysphagia due to more dissection of soft tissue, although whether the incidence of postoperative dysphagia differs between these procedures in anterior cervical discectomy and fusion (ACDF) with the Zero Profile (Zero-P) Implant System is unknown. Thus, the purpose of this retrospective study was (1) to investigate whether the incidence of postoperative dysphagia differs between one-level and two-level ACDF with the Zero-P and (2) to examine patient characteristics that may be associated with the occurrence of dysphagia after ACDF with the Zero-P. Material and Methods: A retrospective analysis of 208 patients who underwent ACDF with the Zero-P Implant System and had at least one year of follow-up was performed from January 2013 to December 2018. The patients were divided into two groups based on the number of operated levels (one-level group, N=86; two-level group, N = 122). Dysphagia was assessed based on the Bazaz grading system. The incidence of dysphagia and the severity of dysphagia at each follow-up were compared between the two groups. The patients were divided into two groups (nondysphagia group, N = 160; dysphagia group, N = 48), and covariates were obtained for multivariate analysis, including demographic parameters, surgical parameters, and radiographic parameters. Results: The results showed that the incidence and severity of postoperative dysphagia in the two-level group were significantly greater at 1 week, 1 month and 3 months postoperatively than those in the one-level group. The results of ordinal logistic regression showed that older age, two-level surgery, greater prevertebral soft tissue swelling (PSTS) and the difference between the postoperative and preoperative C2-7 angle (dC2-7A) were significantly associated with a higher incidence of dysphagia after ACDF with the Zero-P. Conclusion: Two-level ACDF with the Zero-P can result in a significantly greater incidence and severity of transient postoperative dysphagia. Older age, greater PSTS and the dC2-7A were also associated with postoperative dysphagia after ACDF with the Zero-P.
Keywords: ACDF, Zero-P, Cervical degenerative disc disease, Dysphagia
1450
A291: The effect of positional graft placement on pseudoarthrosis rates in anterior cervical discectomy and fusion
Soroush Shabani 1 , Ethan Faye 1 , Emily Mills 1 , Brandon Yoshida 1 , Andy Ton 1 , Jeffrey C. Wang 1 , Raymond Hah 1 , and Ram Alluri 1
1 Department of Orthopaedic Surgery, Keck School of Medicine of USC, Los Angeles, United States
Introduction: Anterior cervical discectomy and fusion (ACDF) is a common surgical treatment for cervical radiculopathy and degeneration. The procedure involves placement of an interbody graft, which may be paired with anterior plate fixation. Fusion degradation is a common outcome for ACDF, ultimately resulting in pseudarthrosis through loosening and subsequent intersegmental motion of hardware. The current study aims to determine an association between location of graft placement along the vertebral body and pseudarthrosis occurrence. Material and Methods: This was a retrospective analysis of 79 patients with single- (43) and multi-level ACDF (36) with a total of 128 individual analyzed levels. A dynamic mobility criteria was used to determine pseudarthrosis status by utilizing >= 4 mm superjacent interspinous motion to validate functional cervical mobility and >= 1 mm interspinous movement to indicate pseudarthrosis. Graft length and vertebral body length were measured at 175% magnification on the most recent radiograph after time of surgery. These measurements were calibrated to the flexion and extension radiographs. Flexion and extension spinous movements were measured at 150% magnification on the radiograph closest to the 2 year post operative mark, and at least 9 months after surgery and less than 2 years post-surgery. T1 slope, cervical lordosis angle, and sagittal vertical axis length were also measured in neutral position on the flexion and extension radiographs. All measurements were determined by a single independent investigator. Both univariate and multivariate logistic regression were used to analyze the data. The multivariate analysis controlled for age, gender, and smoking status. Results: Of the 128 levels, 78 were fused and 50 were consistent with radiographic criteria for pseudarthrosis. Increases in unoccupied space posterior to the graft decreases the likelihood of pseudarthrosis (p < 0.05) on both univariate and multivariate logistic regression. Similarly, the percentage of unoccupied space posterior to the graft was also associated with decreased pseudarthrosis on univariate analysis (p < 0.05). Notably, the anterior length between graft and anterior edge of the vertebral body was not associated with pseudarthrosis (p > 0.05). The mean posterior graft distance overall for successful fusions was 3.98 mm and 2.97 mm for pseudarthrosis (p < 0.05). Conclusion: The results of this study indicate that increasingly, posterior placement of the graft increases likelihood of pseudarthrosis. Therefore, our results support positioning of grafts more anteriorly along the vertebral body to decrease the risk of pseudarthrosis following ACDF.
1649
A292: Building clinically actionable models for predicting mechanical complicaitons in postoperatively well-aligned adult spinal edformity patients using XGBoost algorithm
Baris Balaban 1 , Caglar Yilgor 2 , Altug Yucekul 2 , Tais Zulemyan 3 , Ugur Sezerman 1 , Javier Pizones 4 , Ibrahim Obeid 5 , Frank Kleinstuck 6 , Francisco J. Sanchez Perez-Grueso 4 , Ferran Pellisé 7 , Ahmet Alanay 2 , and European Spine Study Group ESSG 8
1 Acibadem Mehmet Ali Aydinlar University School of Medicine, Istanbul, Turkey
2 Department of Orthopaedics and Traumatology, Acibadem Mehmet Ali Aydinlar University School of Medicine, Istanbul, Turkey
3 Comprehensive Spine Center, Acibadem Mehmet Ali Aydinlar University Maslak Hospital, Istanbul, Turkey
4 Spine Surgery Unit, Hospital Universitario Laz Paz, Madrid, Spain
5 Department of Spinal Surgery Unit 1, Bordeaux University Hospital, C.H.U Tripode Pellegrin, Bordeaux, France
6 Spine Surgery Unit, Schulthess Klinik, Zurich, Switzerland
7 Spine Surgery Unit, Hospital Vall d'Hebron, Barcelona, Spain
8 Vall d'Hebron Institute of Research, Barcelona, Spain
Introduction: Spinal disorders causing pain in the lower back lead to more global disability than any other medical condition. Surgical correction of spinal deformity can relieve pain and reduce disability, however, more than 45% of operated patients are unfortunately foreseen to suffer mechanical complications. Nowadays, progress in health care comes from data-driven approaches. In an ideal world, clinicians should work closely with data scientists to derive clinical outcomes. The aim of this collaborative clinical and data engineering study was to build clinically actionable models for predicting mechanical complications in postoperatively well-aligned adult spinal deformity patients using the XGBoost algorithm. Materials and Methods: Adult spinal deformity surgery clinical data was collected prospectively in a study group database. Preoperative, operative and postoperative patient characteristics, radiographic measurements, technical details as well as patient-reported outcome measures were retrieved and analyzed. Several feature engineering strategies were applied, so that the splits in the resulting trees can be informative and combined effects of several features can be tested. Variable selection process included correlation analysis. The XGBoost model was built using default parameters where the objective function was “binary logistic”, and the booster was “gbtree”. The model hyperparameters were optimized with 9-times 3-fold repeated cross-validation in three grid search rounds. An expert-guided model was built upon the initial model to make it clinically sensible, explainable, and actionable, where a methodical expert interference was carried out regardless of the gain scores of the features. The means (and standard deviation) of the area under the receiving operating curve (AUC), sensitivity, specificity, area under the precision-recall curve (AUPRC), precision, recall, and F score was calculated for cross-validation analysis. The importance matrix was built to stratify the important factors and influential nodes were evaluated. Results: Two separate models (unguided and expert-guided) were built using 244 patients (200F, 44M, 44 ± 19 years) with a mean follow-up of 41 (24-101) months. Forty-two (17%) patients experienced a mechanical complication. The unguided model had 5 trees and 23 leaves and used 14 features. Unguided model achieved 77% accuracy, 80% sensitivity, 76% specificity and 95% negative predictive value while the precision was 40% and the F score was 0.53. On the other hand, the expert-guided model had 4 trees and 16 leaves and used 7 features. Expert-guided model achieved comparable results with 74% accuracy, 80% sensitivity, 73% specificity, and 95% negative predictive value while the precision was 36% and the F score was 0.50. Conclusions: Within a post-operatively well-aligned group of patients (i.e. GAP Score of 0, 1 and 2), the most effective features for predicting mechanical complications were LIV location, estimated blood loss, pre-operative ODI walking score, age, BMI, the combined effect of the number of levels fused and the construct location, and the follow-up duration after surgery. The authors believe this methodical expert-guided model will be beneficial not only to alert surgeons to possible mechanical complications following adult spinal deformity surgery but also aid the planning phase of the surgeries as well as patient selection and counselling.
362
A293: Neurologic outcomes of adult spinal deformity patients with baseline preoperative lower extremity weakness: will they improve following surgery?
Fthimnir Hassan 1 , Lawrence Lenke 1 , Douglas Burton 2 , Alan Daniels 3 , Munish Gupta 4 , Richard Hostin 5 , Khaled Kebaish 6 , Michael Kelly 4 , Han Jo Kim 7 , Eric Klineberg 8 , Stephen Lewis 9 , Peter Passias 10 , Themistocles Protopsaltis 10 , Frank Schwab 11 , Christopher Shaffrey 12 , Justin Smith 13 , Renaud Lafage 14 , Virginie Lafage 14 , Shay Bess 15 , and International Spine Study Group (ISSG) 16
1 Department of Orthopaedic Surgery, Columbia University Medical Center, The Och Spine Hospital at New York-Presbyterian, New York, United States
2 Department of Orthopaedic Surgery, University of Kansas Medical Center, Kansas City, United States
3 Department of Orthopaedic Surgery, University Orthopedics - Providence, Providence, United States
4 Department of Orthopaedic Surgery, Washington University – SOM, St. LouisUnited States
5 Department of Orthopaedic Surgery, Southwest Scoliosis Institute, Plano, United States
6 Department of Orthopaedic Surgery, Johns Hopkins Medical Institute, Baltimora, United States
7 Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, United States
8 Department of Orthopaedic Surgery, University of California, Davis, United States
9 Department of Surgery and Spine Program, University of Toronto, Toronto, Canada
10 Department of Orthopaedic Surgery, NYU Hospital for Joint Diseases - Langone Medical Center, New York, United States
11 Department of Orthopaedic Surgery, Lenox Hill Hospital, New York, United States
12 Department of Neurosurgery, University of Virginia Medical Center, Charlottesville, United States
13 Department of Orthopaedic Surgery, University of Virginia Medical Center, Charlottesville, United States
14 Department of Orthopaedic Surgery, Northwell Health, New York, United States
15 Department of Orthopaedic Surgery, Denver International Spine Center/Presbyterian St. Luke's Medical Center, Denver, United States
16 International Spine Study Group
Introduction: Adult spinal deformity (ASD) patients undergoing surgery risk neurological decline following surgery. However, surgery may be the key in improving outcomes in pts starting with lower extremity motor deficits at baseline (BL). We aim to analyze the improvement in neurological outcomes of ASD patients undergoing spinal reconstruction with BL and 6-week Postop LEMS. Methods: ASD patients ages ≥18 were prospectively studied from 2018-2021. All patients underwent an instrumented PSF with a few also having an ASF of the lumbar spine. Patients were dichotomized based on baseline (BL) LEMS (NML = 50, ABML <50). The ABNML group was then dichotomized based on whether LEMS improved overall from BL or experienced no change or declined by 1st postop (PO) and various factors were analyzed and compared using standard statistical tests. Results: Of the 205 patients evaluated, 134 (65.4%) were NML and 71 were ABNML (34.3%) at BL. Among the 71 patients with ABML LEMS at BL, 49% (N = 35) improved to NML levels, 21% (N = 15) improved from BL levels but not to NML, 20% (N = 14) remained the same, and 10% (N = 7) declined further at 6 wk PO. Compared to ABNML patients with no change or a decline in LEMS at 1st PO, patients who improved overall (70%; N = 50) had significantly more decompressions performed (86% vs 57%; p = 0.0092), and had more PCOs performed intraoperatively (90% vs 62%, p = 0.0074). There were no statistical differences between the groups in age, BL LEMS, BMI, total instrumented vertebrae (TIV), EBL, and OR time. Overall, the number of patients with NML LEMS at 6 wks PO increased by 7.5% (65.4% to 70.2%; p < .0001). Conclusion: 70% of patients with ABML LEMS at BL improved their motor strength by the 1st PO visit, while 30% stayed the same or declined. ABNML Patients who improved from BL had significantly more decompressions performed and, surprisingly, more PCOs performed. Interestingly, patient factors between the two groups demonstrated no statistical differences further highlighting that improvement may be influenced by the differences in surgical techniques.
1937
A294: Comparison of implant failure rates in three versus four rod constructs in adult idiopathic scoliosis surgery
Kevin Kwan 1 , Fthimnir Hassan 1 , Evan Joiner 2 , Carolyna Quiles-Luna 3 , Joseph Lombardi 1 , Zeeshan Sardar 1 , Ronald A. Lehman 1 , and Lawrence Lenke 1
1 Medical Center, The Och Spine Hospital at New York-Presbyterian, Department of Orthopaedic Surgery
2 Medical Center, Department of Neurosurgery
3 Roy and Diana Vagelos College of Physicians and Surgeons, Columbia University, New York, United States
Introduction: Given the significant clinical morbidity and economic burden associated with surgery following symptomatic implant failure for adult idiopathic scoliosis (AdIS), there is an unmet need to identify ways of reducing rates of implant failure/pseudarthrosis and the need for revision surgery. This is the first study to compare rates of implant failure and revision surgery for pseudarthrosis between AdIS patients with three rod (3R) and four rod (4R) constructs. Methods: AdIS pts treated with PSF to the Sacrum/Pelvis with bilateral S2AI screws and operated on by a single surgeon with at least 2 yr follow up (FU) were retrospectively evaluated from 2012 to 2019. Pts were dichotomized based on Thoracolumbar (TL)-Lumbosacralpelvic (LSP) rod constructs (3R vs 4R). The primary outcome was implant failure defined as radiographic implant fracture(s). Secondary outcomes included differences in revision rates for implant failure with pseudarthrosis, pt reported outcomes (ODI and SRS), and postop radiographic parameters (sagittal vertical axis (SVA), coronal vertical axis (CVA), TL cobb measurements). Results: 35 pts were included: 3R = 17; 4R = 18, with F/U between 2-6 yrs. All constructs were 6.0 mm cobalt -chrome hybrid rods with a transition to 5.5 mm at the UIV with bilateral pelvic fixation distally. Mean age was 55 ± 7.9 years. 97% of pts were women. Mean preop SVA was 42 ± 38.8 mm, CVA 23 ± 17.3 mm, PT curve 17° ± 12.8, MT curve 46° ± 20.1, TL/L curve 44° ± 19.1, and total instrumented vertebrae (TIV) 16 ± 3.2. There were no statistical differences between 3R and 4R pts in terms of age, sex, preop CVA, SVA, TL curves, or TIV. 3R pts had fewer TLIF levels (3R: 1.2 ± 0.6 vs 4R: 2 ± 0.6, p = 0.0014). 3R pts experienced a greater rate of implant failure at the 2yr FU when compared to 4R pts (41.2% vs 11%, p = 0.043). No 4R pts had any rod failures, but 2 pts had pelvic fixation failure. Rev. rates for pseudarthrosis were 3R: 5/17 (29.4%) vs 4R: 1/18 (5.6%) p = 0.06. There was no difference in 2-year ODI (p = 0.5) or SRS (p = 0.85) between groups. Conclusion: This is the first single-surgeon study with min. 2yr FU to show a statistically significant decrease in implant failure rates with 4R vs. 3R long constructs for AdIS pts treated to the Sacrum/Pelvis. Notably, no rod failures were seen in the 4R group, but 2 pelvic fixation failures were seen (1 revised) suggesting a need for refinement in the pelvic fixation for AdIS long constructs.
1279
A295: Evaluating dysphagia duration and severity after ACDF in patients with underlying dysphagia - A prospective, multicenter study
Aditya Mazmudar 1 , Khoa Tran 1 , Taylor Paziuk 1 , Samuel Oh 1 , Daniel Habbal 1 , Goutham Yalla 1 , Brandon Sherrod 2 , Erica Bisson 2 , Darrel Brodke 3 , Jose Canseco 1 , Christopher Kepler 1 , Gregory Schroeder 1 , Alexander Vaccaro 1 , Alan Hilibrand 1 , and Jeffrey Rihn 1
1 Rothman Orthopedic Institute at Thomas Jefferson University, Philadelphia, United States
2 Department of Neurosurgery, Clinical Neurosciences Center at University of Utah, Salt Lake City, United States
3 Department of Orthopaedic Surgery, University Orthopaedic Center at University of Utah, Salt Lake City, United States
Introduction: Risk factors of postoperative dysphagia after undergoing anterior cervical discectomy and fusion (ACDF) have yet to be fully elucidated in the literature as numerous studies disagree on patient specific risk factors or surgical interventions that could mitigate the incidence of postoperative dysphagia. In particular, the effect of anterior cervical surgery on the worsening and prolongation of symptoms in patients with underlying dysphagia also remains unclear. Therefore, the purpose of this study was to prospectively evaluate differences in postoperative incidence and severity of dysphagia and determine which factors, if any, are associated with increased postoperative dysphagia. Material and Methods: Patients over 18 years of age who underwent an elective ACDF for a degenerative condition were prospectively enrolled at two academic centers. Patients were excluded from the study if they received surgical intervention for tumors, infections, trauma, or revision. Informed consent for study participation was obtained, and patients were asked to complete a preoperative demographic and medical history questionnaire. Patients also completed dysphagia surveys (Bazaz, Dysphagia Short Questionnaire, 10-item Eating Assessment Tool) during their preoperative visit, and these dysphagia surveys were repeated at 2, 6, 12, and 24 weeks postoperatively during regularly scheduled follow-up appointments. Additionally, in-hospital course events were recorded including diet alteration, unplanned postoperative steroid usage, consults from speech pathologists and otolaryngology (ENT), adjunct cervical spine MRI, nasogastric tube usage, reintubation. Results: A total of 168 patients (23 with preoperative dysphagia, 145 without preoperative dysphagia) met study criteria and were enrolled in the study. Patients with preoperative dysphagia had less frequent alcohol consumption (23.8% vs 53.7%, p = 0.021) and had a nonsignificant increase in surgery length (120 ± 57.3 vs 98.9 ± 56.8 mins, p = 0.085). Total rates of dysphagia increased to 43.2% at 2-week follow-up but eventually decreased to 18.1% at 24-weeks. Patients with preoperative dysphagia had higher rates of dysphagia at 2-weeks (77.8% vs 38.7%, p = 0.004) and 24-weeks (43.8% vs 14.8%, p = 0.010) postoperatively. These patients also had higher severity scores for dysphagia on the Bazaz (p = 0.001), DSQ (p = 0.012), EAT-10 (p = 0.022) questionnaires at the 2-week follow-up period, higher DSQ scores (p = 0.036) at the 6-week follow-up period, higher EAT-10 scores (p = 0.009) at the 12-week follow-up period, and higher Bazaz (p = 0.001), DSQ (p = 0.002), and EAT-10 (p = 0.005) scores at the 24-week follow-up period. There were no differences in groups when comparing rates of diet alteration (p = 0.688), unplanned postoperative steroid usage (p = 0.620), speech and swallow assessment (p = 0.309), adjunct cervical spine MRI (p = 0.265), and nasogastric tubing (p = 1.000). There were no patients who had postoperative ENT consultation or experienced reintubation. Additionally, there were no differences in 90-day hospital readmissions (p = 0.588) or ED visits (p = 1.000). Conclusion: Patients undergoing ACDF who had preoperative dysphagia have prolonged postoperative dysphagia, greater dysphagia severity, and a nonsignificant increase in surgery lengths. There were no differences in demographic, medical history, surgical variables, rates of ENT consultation, length of stay, or other in-hospital events between groups. Surgeons should be aware of the risk of prolonged dysphagia severity that may persist past 24 weeks after surgery when discussing clinical decisions with patients.
364
A296: GAP score potential in predicting post-operative spinal mechanical complications: a systematic review of the literature
Emanuele Quarto 1 , Andrea Zanirato 1 , Marco Pellegrini 1 , Sergio Vaggi 1 , Federico Vitali 1 , Stephane Bourret 2 , Jean Charles Le Huec 2 , and Matteo Formica 1
1 IRCCS Policlinico San Martino, Clinica Ortopedica - DISC, Italy
2 Polycliclinique Bordeaux Nord Aquitaine, Vertebra, France
Purpose: In 2017, the GAP score was proposed as a tool to reduce mechanical complications (MC) in adult spinal deformity (ASD) surgery: the reported MC rate for the GAP proportioned category was only 6%, which is clearly lower to the MC rate reported in the literature. The aim of this study is to analyse if the most recent literature confirms the promising results of the original article. Material and Methods: Using the PRISMA flowchart we reviewed the literature to analyse GAP score capacity in predicting MC occurrence. We included articles clearly reporting ASD surgery MC stratified by GAP categories and the score’s overall capacity to predict MC using the area under the curve (AUC). The quality of the included studies was evaluated using GRADE and MINORS systems. Results: Eleven retrospective articles (1,517 patients in total) were included. The MC distribution per GAP category was as follows: GAP-P, 32.8%; GAP-MD, 42.3%; GAP-SD, 55.4%. No statistically significant difference was observed between the different categories using the Kruskal-Wallis test (p = 0.08) and the two-by-two Pearson-Chi square test (P Vs MD, p = 0.300; P Vs SD, p = 0.275; MD Vs SD, p = 0.137). The global AUC was 0.68 ± 0.2 (moderate accuracy). The included studies were of poor quality according to the GRADE system and had a high risk of bias based on the MINORS criteria. Conclusion: The actual literature does not corroborate the excellent results reported by the original GAP score article. Further prospective studies, possibly stratified by type of MC and type of surgery, are necessary to validate this score.
884
A297: Does surgical timing affect the occurrence of postoperative complications in spinal trauma patients?
Charlotte Adegeest 1 , Cas Hilke 1 , Godard de Ruiter 2 , Mark Arts 2 , Wilco Peul 1 , and Valerie ter Wengel 2
1 Neurosurgery, Leiden University Medical Center, Leiden, The Netherlands
2 Neurosurgery, Haaglanden Medical Center Westeinde, Den Haag, The Netherlands
Introduction: Traumatic spinal fractures are an important cause of disability in the adult population and sometimes require surgical intervention. The incidence of traumatic spinal fractures is increasing in time, especially in the elderly population. The timing of surgical stabilization has been a point of debate. While some question the safety of early surgery, in particular in multi-trauma patients, other question whether prolonged bedrest leads to unnecessary risk in spinal trauma patients. In recent years, studies investigating surgical timing in spinal trauma patients mostly focused on neurological and functional outcomes. The safety of early surgery has been an underexposed, but important subject. We therefore examined the relation of surgical timing and postoperative complications in spinal trauma patients. Material and Methods: We performed a retrospective cohort study in consecutive spinal trauma patients who underwent surgery between January 2010 and April 2020 in two Level-I trauma centers in the Netherlands. Patients were excluded when they had concomitant traumatic brain injury (EMV < 12) or other preoperative life-threatening injuries which hindered the possibility of early surgical management. Patients were divided into an early (<24 h) and late (≥24 h) surgical cohort, in concordance with surgical timing in guidelines in long bone fractures and SCI studies. We further stratified the patients into spinal fractures without spinal cord injury (non-SCI) and with spinal cord injury (SCI), since the occurrence of SCI can influence postoperative complications. For non-SCI we also analyzed the <72 h and ≥72 h in concordance with other studies in non-SCI spinal trauma patients. The primary outcome was the occurrence of 30-day postoperative complications in relation to surgical timing. Trauma and patient specific factors associated with the occurrence of complications were also analyzed. Results: A total of 407 patients met the inclusion criteria, of whom 162 received early (<24 h) and 245 received late surgical fixation and/or decompression. Patients in the early cohort were significantly younger (median (IQR) 58.5 (36.0, 69.0) vs 63.0 (45.0, 74.0), p = 0.012), more often male, AO-type C injuries and had SCI. In non-SCI patients, surgical timing (<24 h vs ≥24 h and <72 h vs ≥72 h) was not related to the occurrence of complications. The overall length of stay (LOS) was significantly higher in patients who underwent late surgery (≥24 h), while the overall postoperative LOS was not different between the early and late cohorts. In patients with SCI who underwent early surgery (<24 h), 40.0% experienced a complication in comparison to 60.0% in the late surgical group, however this difference was non-significant. Factors associated with the occurrence of a postoperative complication were age, COPD, AO-type C injuries, ASA 3 and 4 and the presence of SCI. Conclusion: Early surgery (<24 h) does not appear to influence the occurrence of 30-day postoperative complications in patients with spinal fractures. The presence of SCI is associated with an increased risk of postoperative complications. While SCI patients who underwent early surgery appeared to experience less complications, this difference was non-significant.
OP 34: Early Onset Scoliosis and Non Fusion Techniques
1625
A298: Efficacy of night-time brace and scoliosis-specific exercise for the treatment of adolescent idiopathic scoliosis: results of a mulicenter randomized controlled trial
Anastasios Charalampidis 1 , Elias Diarbakerli 1 , Marlene Dufvenberg 2 , Kourosh Jalalpour 3 , Acke Ohlin 4 , Anna Aspberg Ahl 5 , Hans Möller 1 , Allan Abbott 2 , and Paul Gerdhem 1,6
1 Department of Clinical Science, Intervention and Technology, Karolinska Institutet, Huddinge, Stockholm, Sweden
2 Department of Health, Medicine and Caring Sciences, Unit of Physiotherapy, Linköping University, Linköping, Sweden
3 Department of Reconstructive Orthopaedics, Karolinska University Hospital, Stockholm, Sweden
4 Section of Spinal Surgery, Department of Orthopedic Surgery, Skåne University Hospital, Malmö, Sweden
5 Department of Orthopaedics, Ryhov County Hospital, Jönköping, Sweden
6 Uppsala University Hospital, Dep of Orthopaedics and Hand surgery, Uppsala, Sweden
Introduction: The efficacy of night-time bracing and exercise treatment in patients with adolescent idiopathic scoliosis is controversial. Material and Methods: We conducted a multicenter trial and included untreated girls and boys with idiopathic scoliosis, 9 to 17 years of age with at least one year of remaining growth and a curve Cobb angle of 25-40 degrees. 135 patients were randomly assigned to night-time brace, scoliosis-specific exercise or self-mediated physical activity (control group). The primary outcome was curve progression of more than 6 degrees seen on two consecutive posteroanterior standing radiographs compared to the inclusion radiograph (treatment failure), or skeletal maturity without curve progression (treatment success). Results: In the intention-to-treat analysis, night-time brace resulted in significantly higher success rate as compared to only self-mediated physical activity (75.6% vs 53.3%; p = 0.027). The average time in the study was 22.8 (12.9) months in the night-time brace group and 16.2(10.5) in the self-mediated physical activity group (p = 0.012). There was no significant difference in the success rate in the scoliosis-specific exercise group as compared to self-mediated physical activity group (57.8% vs 53.3%; p ≥ 0.67). In the per-protocol analysis, which included 122 patients, there was a higher success rate in the night-time brace group as compared to self-mediated physical activity group (73.8% vs 48.8%; p = 0.0192). Conclusion: Night-time brace demonstrated higher success rate compared to only self-mediated physical activity on the prevention of progress in patients with adolescent idiopathic scoliosis. Scoliosis-specific exercise did not show any significant clinical benefit when compared to self-mediated physical activity.
97
A299: Vertebral body tethering in adolescent idiopathic scoliosis with more than two years of follow-up, systematic review and meta-analysis
Elie Najjar 1 and Mohamed Hassanin 1
1 Spinal Surgery, Nottingham University Hospital, Nottingham, United Kingdom
Introduction: Whilst spinal fusion remains the gold standard in the treatment of Adolescent Idiopathic Scoliosis (AIS), anterior vertebral body tethering (AVBT) is gaining momentum with relatively few studies on its efficacy thus far. We aimed to conduct a systematic review reporting on the early results of AVBT for patients undergoing surgery for AIS. We aimed to systematically evaluate the relevant literature pertaining to the efficacy of AVBT with respect to degree of correction of the major curve Cobb angle, complications and revision rates. Methods: A systematic review of the literature on AVBT was performed for studies published between Jan 1999-March 2021 applying the PRISMA guidelines. Isolated case reports were excluded. Of a total of 259 articles, 9 studies met the inclusion criteria and were analysed. Overall, 196 patients of (mean age 12.08 years) underwent an AVBT procedure for correction of AIS with a mean follow-up of 34 months. Degree of Cobb angle correction, complications and revision rates were used as outcome measures. Results: Overall, 196 patients of (mean age 12.08 years) underwent an AVBT procedure for correction of AIS with a mean follow-up of 34 months. There was a significant correction of the main thoracic curve of scoliosis (mean preoperative Cobb angle 48.5°, post-operative Cobb angle at final follow up of 20.1°, p = 0.01). Overcorrection and mechanical complications were seen in 14.3% and 27.5% of cases respectively. Pulmonary complications including atelectasis and pleural effusion were seen in 9.7% of patients. Tether revision was performed in 7.85%, and revision to a spinal fusion in 7.88%. Conclusion: This systematic review incorporated 9 studies of AVBT and 196 patients with AIS. The complication and revision to spinal fusion rates were 27.5% and 7.88% respectively. The current literature on AVBT is restricted largely to retrospective studies with non-randomized data. We would recommend a prospective, multi-centre trial of AVBT with strict inclusion criteria and standardised outcome measures.
202
A300: Guided posterior vertebral modulation (GPVM): a new fusionless technique for correction of adolescent idiopathic scoliosis
Jesús Burgos 1 , Gonzalo Mariscal 2 , Luis Miguel Antón-Rodrigálvarez 3 , Ignacio Sampera 4 , Eduardo Hevia 5 , Vicente García 6 , and Carlos Barrios 2
1 Spine Unit, Clínica Fuensanta, Madrid, Spain
2 School of Doctorate, Valencia Catholic University, Valencia, Spain
3 Pediatric Orthopedics, Ramon y Cajal University Hospital, Madrid, Spain
4 Pediatric Orthopedics, Hospital Son Espases, Palma de Mallorca, Spain
5 Spine Unit, Hopsital La Fraternidad-Muprespa, Madrid, Spain
6 Sección de Cirugía de Columna, Hospital Universitario Araba, Vitoria, Spain
Introduction: Current techniques of anterior vertebral growth modulation by vertebral body stapling or tethering provide an incomplete and unpredictable correction of the deformity in addition to the disadvantages of the required thoracotomy. Recently, experimental evidence of growth modulation of the vertebral epiphyseal plates utilizing a posterior approach using pedicle screws was confirmed. The aim of this study was to report the corrective ability of a vertebral modulation technique with a posterior approach without fusion in AIS patients. Materials and Methods: This is a retrospective analysis of prospectively collected data. A series of 36 AIS patients (Risser 3 or less) underwent surgical correction of their deformities by posterior pedicle screws without fusion. Instrumentation was removed once the maturity stage was advanced with almost completed fusion of the iliac apophysis. Most of the cases had main thoracic Lenke-1 curves. Coronal and sagittal curve correction was assessed by conventional standing X-rays pre- and postoperatively, before instrumentation removal, immediately after removal, and at the 2-year follow-up after the removal surgery. A coronal wedging ratio (WR) was also calculated between the height of the apex vertebra at the concave and convex sides of the main curve (MC). Results: The mean preoperative coronal Cobb angle of the MC curves was 53.7° ± 7.5° (95% CI: 50.7-56.6°) and was corrected to 5.5° ± 7.5° (89.7%) immediately postoperatively. Before removal of the instrumentation, there was a loss of correction of 3.4° and another additional 2.8° just after removal. In the 2-year check-up after removal of the implants, the mean MC was 13.1°, which is a 75.4% correction of the initial curve. T5-T12 kyphosis showed a significant improvement from a mean angle of 19.0° (95% CI: 13.3-24.8) to 27.1° (95% CI: 20.1-26.1) 2 years after implant removal (29.9% increase) (p < 0.05). Before surgery, the WR was 0.71 ± 0.06, and 2 years after removal, the WR was 0.98 ± 0.08 (p < 0.001), indicating that the wedging at the apex vertebra was almost completely corrected. At the end of follow-up, the mean sagittal ROM of the T12-S1 segment was 51.2 ± 21.0°. The SRS-22 scores improved from 3.31 ± 0.25 preoperatively to 3.68 ± 0.25 at the final assessment (p < 0.001). Conclusion: Vertebral growth modulation through a fusionless posterior approach using pedicle screws satisfactorily corrects scoliotic main curves in AIS patients with Risser 3 skeletal maturity or less. After removal of the instrumentation, more than two years after surgery, there was a small and nonsignificant loss of correction without subsequent progression during the next two years of follow-up. This technique permits conservation of an acceptable ROM of the lower instrumented segments and a final accurate correction of the spine deformity.
1173
A301: Are we looking at a paradigm shift in the management of adolescent idiopathic scoliosis? A comprehensive retrospective analysis of 75 patients treated with non-fusion anterior scoliosis correction (NFASC) with 2 years follow up - A single centre experience
Umesh P. Kanade 1 , Sharan Achar T 1 , Harith Reddy 1 , Sasidharan M D S 1 , keyur Akbari 1 , Vignesh Badikillaya 1 , Appaji Krishnan 2 , and Sajan Hegde 1
1 Orthopedics, Apollo Hospitals, Chennai, India
2 Orthopaedics, SIMS Hospitals, Chennai, India
Introduction: The gold standard for surgical management Adolescent idiopathic scoliosis (AIS) patients remains spinal fusion, but recently non-fusion anterior scoliosis correction (NFASC) has gained interest. Non-fusion anterior scoliosis correction is a new, fusionless revolutionary motion preserving treatment method for surgical management of Adolescent idiopathic scoliosis, but the technique is novel and there is a visible dearth in clinical data related to the procedure. NFASC differs from traditional vertebral body tethering in that it relies more on intra-operative translational and derotational maneuvers instead of merely tensioning the band during correction. The present study evaluates the radiological and clinical outcomes non-fusion anterior scoliosis correction surgery in patients with Adolescent idiopathic scoliosis. Material and Methods: A study of 75 patients who underwent the NFASC with a mean follow up of 26 ± 12.2 months (12-60 months), managed for structural major curve, cobbs 40°- 80°, having >50% flexibility on dynamic x rays. Pertinent clinical and radiological data collected regarding skeletal maturity, curve type, cobb angle, surgery details and SRS-22r questionnaire. A Post hoc analysis following repeated measures ANOVA test was used to examine statistically significant trends. Results: 75 patients (70 Female, 5 Male) enrolled, with a mean age of 14.96 ± 2.69 years. The mean Risser and Sanders’s score was 4.22 ± 0.7 and 7.15 ± 0.74 respectively. The mean main thoracic (MT) Cobb angle at first follow-up (17.2 ± 5.36) and at latest follow-up (16.92 ± 5.06) were significantly lower than the preoperative mean MT cobb angle (52.11 ± 7.74) by post-hoc analysis (p < 0.05). Similarly, the mean Thoracolumbar/Lumbar ((TL/L) Cobb angle at first follow-up (13.48 ± 5.11) and last follow-up (14.24 ± 4.85) were also significantly lower than the preoperative mean TL/L Cobb angle (51.45 ± 11.26) (p < 0.05). The mean correction in MT cobb angle was 66.88 ± 0.09 % at first follow-up, while it was 67.93 ± 0.08% at latest follow-up. The mean TL/L cobb angle correction was 73.6 ± 0.08% at first follow-up while it was 72.57 ± 0.1% at the latest follow-up. Mean preoperative and postoperative SRS-22 scores were 78.0 ± 3.2 and 92.5 ± 3.1 respectively (p value < .01). None of the patient had any complications till the recent follow up. Conclusion: Non-fusion anterior scoliosis correction surgery offers promising curve correction and stabilization of curve progression in cases with Adolescent idiopathic scoliosis with a low risk of complications particularly with regard to the long-term impact of unfused segments, with preservation of spinal mobility and decreased risk of adjacent level disc disease and proves to be a favorable alternative to fusion modality. Further study with long term follow up will elucidate potential risks and benefits of this novel technique.
1187
A302: Retrospective matched comparison study on non-fusion anterior scoliosis correction (NFASC) versus posterior spinal fusion (PSF) for Lenke 5 adolescent idiopathic scoliosis (AIS) curves in skeletally mature children: clinico-radiological outcomes with 2 years follow up
Umesh P. Kanade 1 , Sharan Achar T 1 , Harith Reddy 1 , Sasidharan M D S 1 , keyur Akbari 1 , Vignesh Badikillaya 1 , and Dr Sajan Hegde 1
1 Orthopedics, Apollo Hospitals, Chennai, India
Introduction: Posterior spinal fusion (PSF) or anterior spinal fusion (ASF) is the standard treatment options for AIS correction. Non-fusion anterior scoliosis correction (NFASC) is a motion sparing alternative to fusion surgery for Lenke 5 Adolescent idiopathic scoliosis (AIS). There is a dearth of literature comparing between the two techniques for Lenke 5 AIS. The current study aims to compare the clinic-radiological outcomes between the two procedures at 2 years follow up. Methods: 38 consecutive Lenke 5 AIS patients treated by a single surgeon with NFASC (group A) or PSF (group B) were matched by age, Cobb’s angle, and skeletal maturity. Intra operative blood loss, operative time, LOS, coronal Cobbs and SRS22 scores at 2 years were compared. Continuous variables were compared using student t-tests and categorical variables were compared using chi-square. Results: The cohort included 19 patients each in group A and B The mean follow-up of patients in group A and B were 24.5 ± 1.8 months and 27.4 ± 2.1 months respectively. Mean pre op thoraco- lumbar/lumbar (TL/L) cobbs for group A and group B were 55° ± 7° and 57.5° ± 8° respectively. At two years follow up, the cobbs for group A and B were 18.2° ± 3.6° and 17.6° ± 3.5° respectively (p = 0.09). The average operating time for group A and B were 169 ± 14.2 mins and 219 ± 20.5 mins respectively (p < 0.05). Conclusion: Our study shows no significant difference in PSF and NFASC in terms of Cobbs correction and SRS scores, but NFASC group had significantly reduced blood loss, operative time and fewer instrumented levels while preserving flexibility.
2012
A303: Predictive factors of quality of life in children with early-onset scoliosis according to CHQPF 50 and EOSQ24
Rodrigo Goes 1 , Alberto Gotfryd 1 , Murilo Alexandre 1 , William Zarza Santos 1 , Olavo Biraghi Letaif 2 , Raphael Marcon 2 , Alexandre Fogaça Cristante 2 , Patricia Fucs 1 , and Robert Meves 1
1 Department of Orthopedics and Traumatology, Santa Casa de Misericórdia de São Paulo, São Paulo, Brazil
2 Department of Orthopedics and Traumatology, Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brazil
Introduction: The most common causes of early-onset scoliosis (IPE) are: idiopathic, congenital, neuromuscular or syndromic. Currently, psychological factors have become the focus of treatment, being considered the specific instrument for assessing the quality of life of patients with IPE, Early -Onset Scoliosis-24 Questionnaire (EOSQ-24), developed by Corona et al, in the United States, in 2011 and applied to caregivers of children; and already cross-culturally validated for our language by internationally established standards (De Mendonça et al, 2021). The Child Health Questionnaire (CHQ), Machado et al. (2001) is considered a generic health instrument designed to capture both physical and psychosocial well-being, understanding the underlying disease as irrelevant. The aim of the study was to apply and correlate the specific early-onset scoliosis questionnaire 24 Items EOSQ-24 with the generic CHQ-50-PF and analyze whether there are predictive factors that impact quality of life. Materials & Methods: Cross-sectional study with the study population formed by caregivers of patients with early-onset scoliosis. The sample consisted of 72 patients, with variables defined by: gender, age, diagnosis, walking ability and curve magnitude. There was prior multicenter approval from the ethics and research committee. The following inclusion criteria were considered: caregivers of patients with early-onset scoliosis, necessarily performing outpatient follow-up of their condition and in accordance with the Free and Informed Consent Term. Exclusion criteria: those who did not agree with the free and informed consent form, patients diagnosed with scoliosis after 10 years of age and patients with spinal deformities resulting from trauma or tumor. The Portuguese version of the EOSQ-24 and CHQ-50 PF questionnaires both scored (0-100) was administered in three deformity treatment centers by two separate research assistants. Results: Seventy-two (72) cases of scoliosis were studied, of which 41 (56.9%) were female, with a mean age of 11.9 + 4.2 years, with a minimum and maximum age between 3 and 24 years. The origin of the most common scoliosis was neuromuscular disease, 23 (32%) followed by congenital, 19 (26.4%). The CHQPF 50 questionnaire showed that family-related items had high scores, >75 points. The subcategory that was most affected was physical function, 45.5 and the one that was better was mental health, 90.8. In the EOSQ24 questionnaire, it was observed that the most affected category was daily life and physical function, 45.1 and 47.8, respectively, and the least affected were the transfer and pulmonary function categories, 70.83 and 68.92, respectively. In the correlation analysis between the two questionnaires, a correlation of 0.652 (p < 0.0001) was observed between the overall mean score of the questionnaires. Two subcategories showed the strongest correlation, the general health subcategories, 0.749 (p < 0.001) and physical function, 0.645 (p < 0.001). Conclusions: There is a significant correlation between the EOSQ-24 questionnaire and the CHQPF 50. Two subcategories showed the strongest correlation, general health (r = 0.749, p < 0.001) and physical function (r = 0.645, p < 0.00). Syndromic scoliosis was a predictor of worse quality of life according to the CHQ-50 PF questionnaire. The significant coefficient in the linear regression for the EOS questionnaire was -5.935 (95%CI -19.59 to 7.72).
1285
A304: 5-year follow-up study evaluating the medium-term efficacy of the Active Apex Correction (APC) technique in early onset scoliosis (EOS)
Alaa Azmi Ahmad 1,2 , Daksh Jayaswal 2 , Mohammad Emar 1 , Farah Shahin 1 , Ayat Aljuba 1 , Asala Hasani 1 , Mohammad Awad 1 , Siraj Abdelnabi 1 , and Aakash Agarwal 2
1 Palestine Polytechnic University, Hebron, Palestine
2 University of Toledo, Toledo, United States
Introduction: The Active Apex Correction (APC) technique is designed to actively control the apex through vertebral remodulation via posterior tethering while providing guided growth to manage EOS patients clinically. Previous studies have focused on understanding the clinical efficacy of the APC technique when compared to traditional growing rods (TGR) over a 2-year follow-up period. As the technique matures, it is critical to evaluate and study the mid to long-term effects to get a complete picture. The current study reports the medium-term clinical outcomes in a patient cohort treated using APC as a primary and secondary interventional surgery, with an average follow-up of 5 years. Material and Methods: The study patient cohort comprised 27 patients (20 females and 7 males). In 13 patients, the initial surgery was either TGR or the vertical expandable prosthetic titanium rib (VEPTR), later changed to APC. In the remaining patients, the APC was the index surgery performed. The recorded outcomes included the Cobb angle, Apical Vertebral Translation (AVT) and spinal height, besides number of surgeries, complications etc. Statistical comparisons (p ≤ 0.05) within the group were computed using paired ANOVA, with the Shapiro-Wilk test used to assess normality. Results: Output data showed a significant reduction in the AVT and Cobb angle when the post-operative data was compared to the pre-operative data. At the last follow-up, the data showed maintenance of both these parameters with no significant difference when compared to the post-op data. Similarly, the T1-L5 height significantly increased at post-op and last follow-up, when compared to the pre-op data. There were 26 complications recorded, which led to 14 unplanned surgeries. Conclusion: The data from this study show excellent management of the EOS deformity while allowing for significant spinal growth using the APC over a medium-term follow-up timeline. Most complications (73%) and unplanned surgeries (93%) were seen in the patient-group where the APC used as a secondary technique. Therefore, the study strongly indicates effective management of the apex using the APC technique; an inexpensive, easy-to-use, and adaptable alternate to the current mainstays (TGR and SHILLA) in EOS intervention.
1814
A305: The application of finite element analysis to determine the optimal UIV of growing-rod treatment in early-onset scoliosis
Aixing Pan 1 and Yong Hai 1
1 Orthopedic ,Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: To analyze the stress distribution in the proximal vertebral body and soft tissue of dual growing-rod (GR) with different upper instrumented vertebra (UIV) to determine the optimal UIV. Material and Methods: A ten-year-old male EOS case treated with GR was selected. Based on spiral computed tomography (CT) scanning performed in 0.6 mm thick slices, a finite element model (FEM) of the preoperative state (M0, the original spine state) of the patient was created. Subsequently, four models with different UIV fixations were numerically analyzed by FEM, including M1 (UIV = T1, i.e., the upper-end vertebrae (UEV) of the upper thoracic curve), M2 (UIV = T2), M3 (UIV = T3) and M4 (UIV = T4, i.e., the lower end vertebrae (LEV) of the upper thoracic curve). Displacement and maximum stress in the proximal vertebral body and soft tissue were measured and compared among the five models. Results: The spine model was fixed with the sacrum, and the gravity conditions were imposed on each vertebral body according to the research of Clin and Pearsall. The results are as follows: M4 model has the largest overall displacement, while M1 has the least displacement among the four models. Except M2, the maximum normalized stress of UIV increases with the downward movement of UIV. M1 has the lowerest annulus fibrosus stress and highest joint capsule stress, which is characterized by the vertebrae backward leaning, while M4 is the opposite. The supraspinous ligament stress of M3 and M4 is significantly higher than that of M1 and M2. This suggests that UIV downshift increases the tendency of the proximal vertebral bodies to bend forward, thereby increasing the tension of the posterior ligaments (PL). Conclusion: The UIV of the GR is recommended to be close to the UEV of the upper thoracic curve, which can reduce the stress of the proximal PL, thereby reducing the occurrence of proximal junctional kyphosis (PJK).
551
A306: Comparison of radiographic outcomes between spontaneous fusion and final fusion surgery after growing rod insertion in early onset scoliosis
Yunjin Nam 1 , Sangmin Lee 1 , Young Ha Kim 1 , Jungwook Lim 1 , Seong Chul Park 2 , Hong Jin Kim 3 , Dong-Gune Chang 3 , Jae Hyuk Yang 2 , and Seung Woo Suh 1
1 Department of Orthopaedics, Korea University Guro Hospital, Seoul, South Korea
2 Department of Orthopaedics, Korea University Anam Hospital, Seoul, South Korea
3 Department of Orthopaedics, Inje University Sanggye Paik Hospital, Seoul, South Korea
Introduction: In patients with early onset scoliosis, early spinal fusion is effective in deformity correction, but it causes trunk growth inhibition. For this reason, in early-onset scoliosis, growing rod insertion and lengthening surgery is often performed for trunk growth. In most cases, the final fusion surgery is performed after the screw is inserted at the point when growth is slowed or completed. It is also reported that there is no significant difference in the correction of the main curvature compared to spontaneous fusion. However, growing rod insertion and lengthening surgery may be disadvantageous for sagittal correction such as thoracic kyphosis or lumbar lordosis because the compression-distraction method is mainly used for deformation correction, and there are few existing studies on this. Material and Methods: From 2015 to 2019, patients underwent surgery for early onset scoliosis were included. Nine patients underwent final fusion were classified as 'final fusion group’, and 10 patients had passed more than 12 months after growing rod lengthening were classified as 'graduated group'. Sex, age at initial and last surgery, follow-up period, number of lengthening, interval from initial to last surgery, diagnosis name, type of curve, and Risser stage were compared between two groups. In addition, Cobb's angle, correction rate, coronal balance, clavicular angle, thoracic kyphosis, lumbar lordosis, and sagittal vertical axis were compared before surgery and at the final follow-up. Results: There was no statistical difference between two groups in demographic data and all preoperative radiologic measures. Postoperative cobb’s angle of major curve (p = 0.002), coronal balance (p = 0.004), and correction rate (p = 0.001) were showed a larger correction in the 'final fusion group'. Postoperative shoulder height (p = 0.434), thoracic kyphosis (p = 0.352), lumbar lordosis (p = 0.186), and vertical sagittal axis (p = 0.604) were showed better outcomes in the 'final fusion group’, but there was no statistical difference. Conclusion: In early onset scoliosis, the case of final fusion showed satisfactory radiological outcomes compared to the case of not performing final fusion. It showed better outcomes in the magnitude of the main curvature, correction rate, and the coronal balance.
OP35: Cervical SCI: Improving Patient Care
477
A307: Length of cervical stenosis, admission ASIA motor score, and BASIC scores are predictors of recovery rate following central cord syndrome
ChangMeng Zhang 1 , Victor Lee 1 , Jeremy Yu 2 , Jason Cheung 1 , Paul Koljonen 1 , and Graham Shea 1
1 Department of Orthopaedics and Traumatology, The University of Hong Kong, Hong Kong
2 Department of Radiology, Queen Mary Hospital, Hong Kong
Introduction: Controversy remains in whether central cord injury syndrome (CCS) should be managed conservatively or by early surgical decompression. It is essential to understand how clinical and radiological parameters correlate with neurological deficits and how they predict recovery trajectories. This retrospective cohort study aims to determine whether quantitative magnetic resonance imaging (MRI) parameters and radiological scoring systems could be used as a reliable assessment tool for predicting neurological recovery trajectory following acute traumatic CCS. Methods: We identified patients with CCS admitted between 2011 and 2018 with a minimum of 1-year follow-up. Cervical MRIs were analysed for cord/canal dimensions, Brain and Spinal Injury Center (BASIC) scores and sagittal grading as ordinal scales of intraparenchymal cord injury. Japanese Orthopaedic Association (JOA) recovery rates (> 50% as good, <50% as poor) were analysed against these variables by logistic regression and receiver operator characteristic (ROC) curves. Additionally, we evaluated American Spinal Injury Association motor scale (AMS) scores/recovery rates. Results: Sixty patients were included, of which 30 were managed conservatively and 30 via surgical decompression. The average follow-up duration for the entire cohort was (51.1 ± 25.7) months. Upon admission, sagittal grading correlated with AMS and JOA scores (p < 0.01, b 1⁄4 0.48). Volume of the C2 to C7 canal and axial cord area over the site of maximal compression correlated with AMS and JOA scores respectively (P1⁄40.04, b1⁄40.26; P1⁄40.01, b1⁄40.28). We determined admission AMS more than 61 to be a clinical cut-offs for good recovery (area under the receiver operating curve [AUC]1⁄40.74, 95% confidence interval [CI]: 0.61-0.85, sensitivity 80.9%, specificity 69.2%, p < 0.01). Radiological cut-offs to identify patients with poor recovery rates were length of cervical spinal stenosis more than 3.9 cm (AUC1⁄40.76, 95% CI: 0.63-0.87, specificity 91.7%, sensitivity 52.2%, p < 0.01), BASIC score of more than 1 (AUC1⁄40.69, 95% CI: 0.56-0.81, specificity 80.5%, sensitivity 51.1%, P1⁄40.02). Surgical decompression performed as a salvage procedure upon plateau of recovery did not improve neurological outcomes. Conclusion: Clinical and radiological parameters upon presentation were prognosticative of neurological recovery rates in CCS. Surgery performed beyond the acute post-injury period failed to improve outcomes.
Keywords: central cord syndrome, prognostic factors, spinal cord injury, surgical decompression, trauma.
991
A308: Mechanism of injury and neurological outcomes of cervical acute traumatic spinal cord injury: a pooled analysis of four clinical trials and registries
Alex Bak 1 , Ali Moghaddamjou 2 , Anahita Malvea 2 , and Michael Fehlings 2
1 University of Toronto
2 Neurosurgery, University of Toronto, Canada
Introduction: Mechanism is an understudied descriptor of acute traumatic spinal cord injury (tSCI). Previous studies have been limited in sample size and long-term follow-up to control for potential confounders and clearly establish a relationship between mechanism of injury and neurological outcomes. The aim of the study was to compare the impact of high-energy (HEMI) and low-energy (LEMI) mechanisms of injury on neurological outcomes of cervical sensorimotor complete tSCI. Material and Methods: Patients with tSCI were identified in four prospective, multicenter clinical trials and registries. American Spinal Injury Association Impairment Scale (AIS) grade was assessed ≤ 72 hours post-injury and followed up between 12 and 52 weeks. Patients were included if they had a cervical and sensorimotor complete (AIS–A) injury at baseline. Study outcomes were change in AIS grade and lower extremity motor, upper extremity motor, and total motor scores. Propensity-score matching between high-energy mechanisms of injury (HEMI; e.g. motor vehicle collisions) and low-energy mechanisms of injury (LEMI; e.g. falls) groups was performed. Adjusted groups were compared with paired t-tests and McNemar’s test. Results: A total of 2452 acute traumatic SCI patients were identified in the combined dataset of four high-quality prospective, multicenter SCI databases. After 1785 patients were removed following the exclusion criteria, 667 patients were divided into two groups: HEMI (n = 523, 78.4%) and LEMI (n = 144, 21.6%). Prior to propensity score matching, HEMI patients were generally younger (32.8 ± 13.5 years v. 47.9 ± 17.9 years, p < 0.001) and had a greater proportion of patients with associated fractures, subluxations, and dislocations with their tSCI compared to LEMI patients (91.6% v. 75.0%, p < 0.001). After admission, a greater proportion of LEMI patients received early surgical decompression ≤ 24 hours of initial injury (47.2% v. 34.0%, p = 0.005). The HEMI and LEMI groups were balanced in a match that resulted in 118 pairs. In paired analysis, HEMI patients had a significantly worse motor recovery from baseline to follow-up based on their smaller change in upper extremity motor scores with a mean difference of 3.7 (12.0 ± 12.3 v. 8.3 ± 12.0, p = 0.010). Change in total motor scores (17.8 ± 19.6 v. 11.9 ± 17.5, p = 0.011) was significantly diminished in HEMI patients compared to LEMI patients with a mean difference of 5.9 (Table 2). We detected no significant differences between HEMI and LEMI patients on AIS grade conversion (LEMI: 41.5% v. HEMI: 45.8%, p = 0.609) or change in LEMS (LEMI: 5.9 ± 12.6 v. HEMI: 3.7 ± 9.6, p = 0.119). Conclusion: Cervical sensorimotor complete tSCIs from HEMI were associated with significantly lower motor recovery compared to LEMI patients. Our findings suggest that mechanism of injury should be considered in modelling prognosis and in understanding the heterogeneity of outcomes after acute tSCI.
973
A309: An opportunity to enhance spinal cord injury trial design and execution: predicting who is lost to follow-up
Ali Moghaddamjou 1 , Alex Bak 1 , Vishu Karthikeyan 1 , Jefferson Wilson 1 , and Michael Fehlings 1
1 University of Toronto, Canada
Introduction: Despite advancements in research and promising pre-clinical findings we have yet to isolate any new practice-changing interventions for the treatment of spinal cord injury (SCI) in clinical trials. This raises concerns about the methodology and design of clinical trials in SCI. One of the concerns in SCI trials is with high rates of missing data. Combined with difficulty in recruiting patients and the cost associated with clinical trials in SCI strategies need to be implemented to reduce the rates of loss to follow-up (LTFU) in trials. Material and Methods: Multicenter, prospective data from the STASCIS study and the NACTN registry database were analyzed for this study. All adult patients with SCI from the STASCIS and NACTN registries were selected. LTFU was defined to be in patients who did not come to follow up at 12 months and previously did not come to follow up at least 3 months after baseline ASIA Impairment Scale assessment (≤ 72 hours post-injury). Missing data were imputed with multiple imputations. Univariate analysis was performed for each independent variable, and predictors with p < 0.2 were included in the final multivariate model for backward stepwise logistic regression based on AIC values. Odds ratios with 95% confidence intervals were calculated with a significance level set as p < 0.05. Results: A total of 885 patients (46.5 ± 17.6, 45.5% female) were eligible for inclusion. On univariate analysis, 23 variables were significant and included for feature selection. In the final model, patients were less likely to miss follow-up if they had higher baseline lower extremity motor scores (OR: 0.99[0.98-0.99], p = 0.021), received early surgery (OR: 0.49[0.35-0.69], p < 0.001), of Asian (OR: 0.31[0.18-0.54], p < 0.001) or Black race (OR: 0.63[95% CI 0.45-0.88], p = 0.006) compared to White Caucasian, or had a systemic infection complication (OR: 0.35[0.17-0.70], p = 0.003). Independent predictors of LTFU were post-operative DVT (OR: 3.28[1.64-6.55], p = 0.001) and hematological complications (OR: 1.67[1.07-2.60], p = 0.025), and a history of malignancy (OR: 3.65[1.01-13.15], p = 0.048) and smoking (OR: 1.55[1.15-2.08], p = 0.004). Higher baseline GCS was associated with making follow-up (OR: 0.94[0.88-1.00], p = 0.053) and diabetic history with LTFU (OR: 1.56[0.97-2.52], p = 0.068), but were not statistically significant in the final model. Conclusion: Patients that had a greater motor disability, late surgery, and associated co-morbidities (such as the history of malignancy, smoking, DVT, and hematological complications), are at greater risk for LTFU and may require concerted patient engagement approaches to ensure comprehensive spinal care and track recovery trajectory.
1001
A310: Hospital transfer and neurological recovery after acute traumatic spinal cord injury: is it time for a code spine?
Alex Bak 1 , Ali Moghaddamjou 2 , and Michael Fehlings 2
1 University of Toronto
2 Neurosurgery, University of Toronto, Canada
Introduction: Interhospital transfer from community hospitals to centers specialized in the management of traumatically injured individuals can strain patients, healthcare systems, and delay appropriate care. However, the impact of transfer on patient outcomes after acute traumatic spinal cord injury, wherein time to surgery is critical, remain unclear. We aimed to compare long-term neurological outcomes in transferred or directly admitted patients with traumatic spinal cord injury. Material and Methods: We conducted an ambispective cohort study with prospectively accrued data from eleven specialized trauma centres across USA and Canada enrolled in the Surgical Timing in Acute Spinal Cord Injury Study clinical trial and the North American Clinical Trials Network Spinal Cord Injury registry between 2005 and 2017. Two comparison cohorts were created based on whether they were directly admitted or transferred from an intermediate hospital. The main outcomes were change in American Spinal Injury Association Impairment Scale grade and its components: upper extremity motor, lower extremity motor, pin prick, and light touch scores from baseline (assessed ≤ 72 hours post-injury) to follow-up (between 12 and 52 weeks). Nearest-neighbour 1:1 propensity-score matching between the transferred and directly admitted cohorts was performed using a caliper width of 0.2 with 17 baseline variables as covariates. Paired analysis using McNemar’s test and paired Student’s t-test was used to determine the extent of the difference in neurological outcomes. Results: A total of 1090 patients (42.8% female, 54.0 ± 19.3 years) with traumatic spinal cord injury were directly admitted to a specialized trauma centre (N = 532, 48.8%) or transferred from an intermediate hospital (N = 558, 51.2%). After propensity-score matching, 321 pairs were matched. Compared to a matched cohort of transferred patients, American Spinal Injury Association Impairment Scale grade improved significantly more in directly admitted patients (50.2% v. 41.7%, p = 0.044), as did upper extremity motor score (12.5 ± 12.3 v. 10.4 ± 11.5, p = 0.018) and light touch score (21.3 ± 30.0 v. 15.3 ± 24.6, p = 0.007). Conclusion: Direct admission of traumatic spinal cord injury patients to a specialized trauma centre is associated with greater neurological recovery compared to patients that are transferred from an intermediate hospital. Feasibility of direct admission to a center specialized in the management of acute SCI through implementation of standardized code programs or surgery at a community site must be investigated.
1430
A311: Management of traumatic cervical cord contusions at a tertiary healthcare centre in India - Outcomes and analysis
Srikrishnaditya Manne 1
1 Neurosurgery, Sunrise Hospital, Nizamabad, India
Introduction: The management of a patient with spinal cord contusion has been a point of great debate over the years between conservative and surgical management. In this study, we compared the neurological outcomes in patients who underwent surgery and those who were managed conservatively for spinal cord contusions to tailor a better management principle depending on the clinical status of patient. Material & Methods: A non-randomised prospective study was conducted on all patients admitted at a tertiary center with a diagnosis of Cord Contusion from January 2018 to December 2019. 147 patients were admitted with spinal cord contusions during this duration. Out of which 95 patients, were managed surgically and the rest 52 patients were managed conservatively. The outcomes were analysed on the basis of ASIA scores and the Functional Independence measure (FIM) scores at the time of admission and up to 6 months. ASIA score at the end of 6 months was considered the best attainable score. Statistical analysis was done based on Chi Square test and Fisher exact test of significance. Results: In this study, 78 patients were below 50 years of age, whereas 69 patients were above or equal to 50 years. 85.72 % of all patients in this study were male. 67 patients (70.5%) in surgical group (95 patients) had a good outcome while only 15 patients (28.8%) had good outcome in conservative group (52 patients). The difference of 41.7% in the two groups was statistically highly significant (p-value-0.001). Out of the 95 patients who underwent surgery only 31 patients were operated within 24 hours of injury and 30 of them had good outcome. p value is 0.001 for early (< 24 hours) v/s delayed surgery (> 24 hours). Spinal cord contusion sustained in a road traffic accident (RTA) (57 patients-38.77%) had poorer outcome in comparison to simple falls (79 patients-53.74%) (p-value-0.02). Conclusion: In this study, we concluded that Surgery is a better mode of management for cervical cord contusions and if it is done in early (< 24 hours) period, outcome will be better. Spinal cord contusion sustained in a RTA had poorer outcome in comparison to simple falls.
Keywords: spinal cord contusions, ASIA score, Functional Independence measure (FIM) score
229
A312: Perioperative complications and medical costs associated with epidemic preventive management after spinal cord injury surgery during COVID-19 pandemic
Hiroki Ushirozako 1,2 , Kota Suda 1 , Satoko Matsumoto Harmon 1 , Miki Komatsu 1 , Masahiro Ota 1 , Tomoaki Shimizu 1 , Akio Minami 1 , and Yukihiro Matsuyama 2
1 Department of Orthopaedic Surgery, Hokkaido Spinal Cord Injury Center, Bibai, Japan
2 Department of Orthopaedic Surgery, Hamamatsu University School of Medicine, Hamamatsu, Japan
Introduction: Coronavirus disease 2019 (COVID-19) epidemic preventive management have led to delays in active rehabilitation, which may negatively impact the outcomes of patients with traumatic spinal cord injury (SCI). In our institution, we continued to perform prompt surgical intervention for patients with SCI during the pandemic; however, we could not continue active rehabilitation due to COVID-19 preventive management from May 2020. Therefore, this study aimed to clarify the influence of the COVID-19 pandemic on perioperative complications and medical costs after SCI surgery. Material and Methods: This single-centered retrospective study examined 248 patients with SCI who underwent posterior fusion surgery between 2017 and 2021 (mean age 65.0 years; follow-up period ≥1 year). Demographic and surgical data were analyzed. Following the preliminary study, we established a 1:1 matched model using propensity scores to adjust for age, sex, American Spinal Injury Association impairment scale score at admission, and risk factors for perioperative complications, as reported previously. Perioperative complication rates were compared between patients before (BCP group) and during (DCP group) the COVID-19 pandemic (DCP group). Results: Preliminary analysis of 248 unmatched patients (66 and 182 in the DCP and BCP group, respectively) revealed significant differences in hypertension (50.0% vs. 34.6%; p = 0.028), history of cerebral stroke (9.1% vs. 2.7%; p = 0.042), hemoglobin level (13.1 g/dL vs. 12.6 g/dL; p = 0.026), D-dimer level (13.4 µg/mL vs. 23.7 µg/mL; p = 0.019), and intraoperative estimated blood loss (161 mL vs. 228 mL; p = 0.018) between the groups. There were significant differences in cardiopulmonary dysfunction (29% vs. 16%; p = 0.024) and delirium (26% vs. 10%; p = 0.002) between the DCP and BCP groups. Using a 1:1 propensity score-matched analysis, 50 patient pairs from the DCP and BCP groups were selected. There were no significant differences in baseline and surgical data between the groups. The C-statistic was 0.837 in the propensity score model. Score-matched analysis showed significant differences in cardiopulmonary dysfunction (30% vs. 10%; p = 0.012) and medical costs in the second postoperative month (777 USD vs. 716 USD; p = 0.045) between the DCP and BCP groups. Conclusion: nEpidemic preventive management negatively affected the timing of active rehabilitation intervention, perioperative complication rates, and medical costs after SCI surgery. Early surgical and active rehabilitation interventions were important in reducing perioperative complication rates and medical costs. As ethical considerations are important in clinical research, the results of this study would not have been clarified without the COVID-19 pandemic.
769
A313: Early surgical decompression in traumatic cervical ASIA A spinal cord injury patients
Michael Fehlings 1 , Ali Moghaddamjou 1 , Alex Bak 2 , and Jefferson Wilson 1
1 Neurosurgery, University of Toronto, Canada
2 University of Toronto, Canada
Introduction: While there is increasing evidence for the efficacy of early surgical decompression for traumatic cervical spinal cord injury (tSCI), the impact of early surgery on motor and sensory complete (ASIA A) patients is still the subject of debate. To date, there have been no studies focusing specifically on ASIA A cervical tSCI patients. We aim to study the impact of early surgical decompression (<24 hrs) on neurological recovery of ASIA A cervical tSCI patients. Material and Methods: Patients with cervical ASIA A injury were identified from 4 prospective, multi-center datasets (NACTN, STASCIS, NASCIS 3, and SYGEN). Patients who had a GCS < 15 at baseline or were younger than 18 or older than 80 were excluded. We tabulated the number of functional motor levels gained below the neurological level of injury. A functional motor level was defined as a myotome with at least grade 3 power on the MRC scale. We defined a gain of greater than 2 functional motor levels at 1 year as a significant improvement. A-priori we isolated age, mechanism of injury, and use of steroids for multivariate analysis. Logistic regression models were used to calculate the Odds Ratio for significant improvement. Results: We identified 365 cervical ASIA A tSCI patients with an average age of 33 yrs and an average time to surgery of 168 hrs. Of those patients who had early surgery, 39.40% had a significant improvement in functional motor levels vs. 28.80% of those who did not have early surgery (p = 0.049). In Multi-variate analyses, early surgery was the only significant covariate associate with significant impact on functional recovery (Odds Ratio of 1.65; p = 0.048). Conclusion: For the first time, we have shown a clear therapeutic benefit of early surgical decompression within 24 hrs in ASIA A tCSCI patients. These data further support the principle of early surgical intervention for all types of SCI, even those with clinically complete lesions at baseline.
Patients with a traumatic cervical ASIA A injury would benefit from early aggressive surgical treatment.
558
A314: Comparison of age and modified Frailty Index-5 as predictors of in-hospital mortality for patients with complete traumatic spinal cord injury
Husain Shakil 1,2,3 , Blessing Jaja 2 , Peng Zhang 2 , Rachel Jaffe 2,3 , Armaan Malhotra 1,2,3 , Jefferson Wilson 1,2,3 , and Christopher Witiw 1,2,3
1 Division of Neurosurgery, Department of Surgery
2 Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, Canada
3 Institute of Health Policy Management and Evaluation, University of Toronto, Toronto, Canada
Introduction: Complete traumatic spinal cord injury (ctSCI) confers significant in-hospital mortality risk to patients, which has been estimated to be up to 17%. Increased clinical frailty, as measured by the mFI-5 and older age have been found to be associated with increased mortality in the setting of ctSCI. However, a comparative analysis of the predictive power of each measure has not been completed. In this study, we aim to address this knowledge gap and discern how each patient factor contributes to a patient mortality predication model. Material and Methods: Using the American College of Surgeons (ACS) Trauma Quality Improvement Program (TQIP) database for 2011 to 2018, we formed a cohort of adult (≥ 16 years) patients who sustained complete traumatic cervical SCI using Abbreviated Injury Scale (AIS) codes. We developed a predictive model of in-hospital mortality using age and mFI-5 in conjunction with a base model of clinical, treatment, and hospital covariates. We conducted Receiver Operating Characteristic (ROC) analysis and decision curve analysis using STATA and R statistical software to compare the contribution of age and mFI-5 to decision making. Results: We identified 4,814 adult patients from the 2011-2018 TQIP database with complete traumatic spinal cord injury. Mean age was 49, with 63% of patients having an mFI of 0, 22% mFI of 1, and 14% mFI ≥ 2. Using ROC analysis, we found the area under the ROC curve (AUROC) for age (0.81 AUROC) to be superior to mFI-5 (0.75 AUROC) in our predictive model for in-hospital mortality. Decision curve analysis determined that age has more clinical utility in decision making than mFI-5 in our cohort of patients. Conclusion: Amongst our identified cohort of patients with adult ctSCI, age appears superior to mfI-5 for decision making in a predictive model for in-hospital mortality.
1831
A315: The association of race with outcomes and procedural administration in cervical spine trauma
Sanket Mehta 1 , Venkat Boddapati 1 , Nicholas Danford 1 , Joseph Lombardi 1 , Zeeshan Sardar 1 , Lawrence Lenke 1 , Ronald A. Lehman 1 , and K. Daniel Riew 1
1 Department of Orthopedic Surgery, Columbia University Medical Center, New York, United States
Introduction: Non-white patients often experience greater delays in orthopedic care, undergo fewer procedures, and have greater postoperative complication rates when compared to white patients. However, the manifestation of such disparities in the acute trauma setting pertaining to the cervical spine is poorly understood and remains an issue of debate. This study investigates the association of nonwhite race with clinical outcomes and the probability of diagnostic and therapeutic procedure administration in patients undergoing cervical spine trauma. Materials and Methods: We performed a retrospective cohort study involving cervical spine trauma patients aged 18 to 64 years registered in the National Trauma Data Bank (NTDB) 2011-2019. Patients who were missing race information, dead on arrival, or had an injury severity score (ISS) less than 9 were excluded. Baseline patient characteristics were compared using bivariate analysis. Multivariate logistic analysis was employed to investigate the association of nonwhite race with in-hospital mortality, complications, and select diagnostic and therapeutic procedure administration, adjusting for age, sex, insurance status, ethnicity, ISS, presence of shock, mechanism of injury, intent of injury, Glasgow Coma Scale motor score, significantly different comorbidities, and year of admission. Results: A total of 118,306 patients with acute cervical spine trauma met the inclusion criteria. Overall, 87,421 patients were white and 30,885 patients were non-white. Non-white patients had a higher rate of chronic renal failure and a lower rate of alcoholism, bleeding disorder, current smoking status, functionally dependent health status, history of myocardial infarction, hypertension, respiratory disease, and cirrhosis (p < 0.001 for all). Non-white patients were younger (37 vs. 44 years) and more likely to present in shock (6.9% vs. 5.8%; p < 0.001 for all). In-hospital mortality rate was greater in non-white patients compared to their white counterparts (7.7% vs. 6.8%; p < 0.001). Multivariable logistic regression analyses demonstrated an association of non-white race with increased likelihood of any complication (odds ratio [OR] = 1.15; p < 0.001), cardiac arrest (OR=1.35; p < 0.001), pulmonary embolism (OR = 1.19; p = 0.02), severe sepsis (OR = 1.24; p = 0.004), catheter related bloodstream infection (OR = 1.54; p = 0.001), organ/space surgical site infection (OR=1.37; p = 0.02), acute kidney injury (OR = 1.41; p < 0.001), acute respiratory distress syndrome (OR = 1.13; p = 0.01), urinary tract infection (OR = 1.19; p < 0.001), and pressure ulcer (OR = 1.13; p = 0.01) compared to white race. There was no association between non-white race and in-hospital mortality (OR = 0.96, p = 0.18). In a multivariable analysis of select diagnostic and therapeutic procedure administration, non-white race was associated with an increased likelihood of receiving plain radiography (OR = 1.08; p = 0.02), computerized tomography (CT) of the spine (OR = 1.05; p = 0.003), magnetic resonance imaging (MRI) of the spine (OR = 1.13; p < 0.001), packed red blood cell (PRBC) transfusion within 4 hours (OR = 1.07; p = 0.03), operative spinal fixation (OR = 1.19; p < 0.001) and decreased likelihood of withdrawal of care (OR = 0.75; p < 0.001) compared to white patients. Conclusion: In summary, non-white race was independently associated with increased in-hospital complications in acute cervical spine trauma even after controlling for insurance status, ethnicity, injury severity, and comorbidities. Despite controlling for many of the medical factors that can influence outcomes, our data suggest that being non-white with cervical trauma portends a poorer prognosis.
OP36: Novel Technologies and Robotics
1045
A316: Assessment of accuracy of free hand pedicle screw placement by experienced surgeon vs navigated pedicle screw placement by beginner - a cadaveric study
Varun Agarwal 1
1 Orthopedics, Rohilkhand Medical College and Hospital, Bareilly, India
Introduction: Various techniques are being used for pedicle screw placement in spine. The conventional freehand technique uses anatomic landmarks and tactile palpation for pedicle screw placement. New techniques like navigation assisted, 3D pedicle guide surgeries are being done recently which use pre procedure computed tomography scan. This study was done to assess the accuracy of pedicle screw placement by freehand technique done by a spine surgeon compared to pedicle screws placed by a beginner using navigation assisted technique in thoracolumbar spine of cadavers. This study also evaluated whether the new technology bridges the learning curve of pedicle screw placement and whether it gives advantage to a beginner or an untrained surgeon. Material and Methods: Four cadavers were exposed by posterior midline approach. K-wires were placed from T1 to L5 vertebrae by freehand and navigation assisted technique on either side by spine surgeon and orthopaedic resident respectively. Post procedure CT evaluation was done to see the accuracy of K-wire placement. K-wires having cortex violation of the pedicles of more than 2 mm, were considered significant. Results: A total of 136 K-wires were inserted. The spine surgeon and the resident placed 68 K-wires each. The spine surgeon had a rate of 18% (12 out of 68) medial breach, 13% (9 out of 68) lateral breach by freehand technique while the resident had a rate of 7% (5 out of 68) medial breach, 12% (8 out of 68) lateral breach by navigation assisted technique on CT evaluation. Conclusion: Navigation assisted technique does give advantage in pedicle screw placement to a beginner with advantage of less doses of radiation compared to the conventional freehand technique but is expensive.
1820
A317: Prospective 3D imaging study of screw position using two different spinal surgery techniques
Fedan Avrumova 1 , William Zelenty 1 , Samuel Goldman 1 , Frederik Abel 2 , and Darren Lebl 1
1 Spine
2 Radiology, Hospital for Special Surgery, New York, United States
Introduction: Robotic-navigated assisted (RNA) surgery with integrated navigation continues to expand its applications across orthopaedic surgery – particularly in pedicle screw insertion during spinal surgery. Despite the assistance of the robotic arm-guide and navigated instruments, there is still potential for screw deviation from planned trajectories. First generation anti-skive instruments include an anti-skive cannula (ASC), which is a spiked second cannula attached to bone through the drill guide involving four total components. In this study we examined a new workflow utilizing a navigated, high-speed drill (HSD) to create a pilot-hole to streamline the RNA workflow and further prevent instrument skive. Material and Methods: A single-center, prospectively collected data series of patients were evaluated as surgeries with RNA were completed between 2019 and 2022. Demographic data as well as positioning, registration, and screw insertion times were recorded. Planned screw trajectory from software based preoperative CT was compared with final intraoperative 3D fluoroscopic images to grade screw position in sagittal and axial planes. Results: A total of 602 instrumented pedicles were planned robotically between each group (311 ASC, 291 HSD). 277 (98.5%) of the HSD screws were inserted robotically; 13 screws were converted to freehand (4.5%) and 1 screw was planned freehand. No screws were inserted over a k-wire. In the ASC group, 259 (83.3%) of the screws were inserted robotically; 8 (2.6%) were converted to freehand, 10 (3.2%) were converted to freehand over a k-wire, and 34 (10.9%) were planned freehand. 100% of the robotically inserted HSD screws were Liebermann Grade A versus 94.2% of the ASC screws (remainder were Grade B). 4 skive events (3 superior, 1 inferior skives) were recorded using the HSD workflow versus 15 (11 superior, 4 inferior skives) in the ASC workflow (p < 0.05). Comparison of the intraoperative 3D fluoroscopic images versus the preoperative plan for the HSD workflow in the axial plane showed mean lateral deviation of 0.5 ± 0.6 mm (SD), medial deviation of 0.7 ± 0.6 mm, and 4 accurate screws without deviation; in the sagittal plane, mean deviation was 0.7 ± 0.7 mm and 0.6 ± 0.5 mm with cranial and caudal directionality, respectively. Two screws were accurate. For the ASC workflow in the axial plane, mean lateral deviation was 1.0 ± 1.1 mm, medial deviation 1.2 ± 1.1 mm, and 18 were determined to be accurate; in the sagittal plane mean cranial deviation was 0.7 ± 0.7 mm and caudal 1 ± 0.6 mm, and 12 accurate. Average time per screw (TPS) was significantly lower in the HSD group versus ASC (2.0 ± 1.1 mins vs 3.4 ± 2.2 mins, (p < 0.001)). Lastly, screws placed using the HSD workflow were closer to preoperative planned trajectory in all directions except cranial deviation where no significant difference was found (p > 0.05). No adverse clinical sequelae occurred from the implantation of any screw. Conclusion: The implementation of the HSD workflow has significantly reduced both the rate of instrumentation skive (likewise overall screw accuracy) and TPS. The HSD workflow shows an improvement in rate of skive and screw accuracy because the side-cutting tip ignores variable contact with the surface anatomy and allows some redirection within the length of the pedicle.
1003
A318: Accuracy of posterior spinal instrumentation using computer-assisted spine navigation: a pooled analysis of 16,040 screws
John-Peter Bonello 1 , Robert Koucheki 1,2 , Johnathan Lex 2,3 , Aazad Abbas 1 , Nicholas Nucci 4 , Jeremie Larouche 3,5 , Henry Ahn 3 , Joel Finkelstein 3,5 , Stephen Lewis 3,6 , and Jay Toor 3
1 Temerty Faculty of Medicine
2 Institute of Biomedical Engineering
3 Division of Orthopaedic Surgery, University of Toronto, Toronto, Canada
4 Division of Orthopaedic Surgery, University of Ottawa, Ottawa, Canada
5 Department of Orthopaedic Surgery, Sunnybrook Health Sciences Centre, Toronto, Canada
6 Department of Orthopaedic Surgery, Toronto Western Hospital, Toronto, Canada
Introduction: Multiple navigation technologies have been developed to aid in the instrumentation of spinal hardware. This meta-analysis attempts to evaluate all available published literature on computer-assisted spine navigation (CAN) to compare the prominent manufacturers of these technologies, using conventional techniques (free-hand or fluoroscopy) as a common control. Material and Methods: Literature searches were performed using major databases. Studies must have utilized computed tomography (CT) confirmation to compare CAN with conventional screw placement. Participants included adult patients undergoing spinal instrumentation surgery at any spinal level. The objective of this study was to compare screw placement accuracy, neurologic complications (NC), operative time (OT), and blood loss (BL) sub-grouped by various CAN manufacturers. Results: Among the 28 included studies, 2959 patients underwent spinal instrumentation surgery, of which 1471 patients were in the CAN group and 1488 patients in the conventional group. Average age of patients in the CAN and conventional groups were 59.1 and 57.8 years old, respectively. 16,040 screws were included of which 7957 screws were placed using CAN technologies and 8083 screws were placed using conventional methods. CAN manufactures included in the pooled analysis were Medtronic (15 studies, screws = 9421), BrainLab (8 studies, screws = 4778), Stryker (4 studies, screws = 1684), and SeaSpine (7D Surgical) (1 study, screws = 157). At all spinal levels, there was a significantly lower risk of major breach in the CAN group compared to the conventional group (OR 0.42, 95% CI 0.27 to 0.63, p < 0.0001, I2 = 56%, random effect model). No significant difference in risk of major breach was found between CAN manufacturers (p = 0.27). At the thoracolumbar levels, there was also a significantly lower risk of major breach in the CAN group compared to the conventional group (OR 0.32, 95% CI 0.17 to 0.60, p = 0.0004, I2 = 34%, random effect model), with Stryker demonstrating the highest screw accuracy among manufacturers (OR 0.05, 95% CI 0.01 to 0.39, p = 0.004). There was no significant difference in rates of NC, OT, and BL between CAN and conventional groups. However, when comparing CAN manufacturers, BrainLab demonstrated significantly faster OT compared to Medtronic by about 30 minutes (95% CI -63.27 to -2.47, p = 0.03, I2 = 74%). Conclusion: Our results indicate that use of CAN platforms in spine surgery leads to an approximately 60% reduction in rates of major breach at all spinal levels compared to conventional methods. Furthermore, we demonstrated that this increased accuracy is without a change in NC, OT, or BL, with Stryker demonstrating the highest accuracy among the manufacturers. These findings have implications as an aid in guiding the choice of navigation platforms by surgeons and institutions.
1048
A319: Accuracy of placement and revision rates for cervical pedicle screws inserted using spinal navigation compared with screws inserted without navigation: a systematic review and meta-analysis
Bas Bindels 1 , Bastian Dronkers 1 , Maarten Smits 1 , and Jorrit-Jan Verlaan 1
1 Orthopedic Surgery, University Medical Center Utrecht, Utrecht, The Netherlands
Introduction: Inserting cervical pedicle screws is technically challenging due to the complex anatomy of the cervical spine. Spinal navigation systems have been developed to give surgeons more control during insertion of pedicle screws and improve pedicle screw accuracy of placement (AoP). However, acquiring navigational equipment is expensive. Given the low incidence of malpositioned cervical pedicle screws causing neurovascular symptoms (0-6%), a significant improvement in AoP or postoperative screw revision rates is needed to justify the costs associated with using navigation for the cervical spine. This systematic review and meta-analysis compared the AoP and screw revision rates for cervical pedicle screws inserted with and without navigation. Methods: A Cochrane, Embase, and PubMed literature search was conducted. Eligible studies reported cervical pedicle screw AoP, measured AoP on cone-beam CT or regular CT, and defined accurately placed pedicle screws as screws breaching the pedicle wall less than 2 mm or with less than 50% of the screw diameter in any direction. Data on cervical pedicle screw AoP, screw revision rates, and use of navigation for screw insertion were extracted from the included studies and summarized for analysis. A random-effects model was applied to calculate the pooled estimates for AoP and revision rates. We compared pooled estimates by fitting them into a fixed-effects meta-regression model. The Methodological Index for Non-Randomized Studies (MINORS) criteria were used to assess the methodological quality of included studies. Results: After screening 4902 articles, 50 studies were included. All studies were non-randomized observational studies. Overall, 31 studies assessed 4185 navigated screws reporting AoP rates of 79-100%, and 25 studies assessed 5490 non-navigated screws reporting AoP rates of 67-100%. When including all 50 studies, the pooled AoP for navigated screws was 97% [95%-99%] and did not differ from the pooled AoP for non-navigated screws of 95% [93%-97%] (p = 0.154). Also, when only including the 20 higher-quality studies, the pooled AoP for navigated screws (96% [92%-98%]) did not differ from the pooled AoP for non-navigated screws (94% [90%-96%]) (p = 0.301). The pooled intraoperative revision rate for navigated screws was 2% [1%-4%] (reported in 14/31 studies), which was higher than the revision rates for non-navigated screws (0% [0%-1%]) (p = 0.007) (reported in 7/25 studies). Pooled postoperative screw revision rates did not differ between the guidance methods: 0% [0%-0%] for navigated screws (27 studies) and 0% [0%-1%] for non-navigated screws (23 studies) (p = 0.327). Conclusion: This systematic review and meta-analysis found no difference in AoP between cervical pedicle screws inserted with navigation and screws inserted without navigation. Intraoperative screw revision rates increased if surgeons used navigation, but postoperative revision rates did not decrease. However, the included studies were prone to selection and publication bias, and comparative studies are warranted. Before the high costs for navigation in the cervical spine are justified, future studies should explore other elements; including the possibility of minimally invasive surgery and the treatment of more anatomically complex cases, even for less experienced surgeons.
875
A320: C-arm based navigated pedicle screw placement in the cervical spine is highly accurate: An experimental study on identical spine models
Justine Wolf 1,2 , Eric Mandelka 1 , Jula Gierse 1 , Felix Zimmermann 1 , Paul Alfred Grützner 1 , Jochen Franke 1 , and Vetter Sven 1
1 Department of Trauma Surgery and Orthopedics, BG Klinik Ludwigshafen, Ludwigshafen, Germany
2 Medical Faculty Heidelberg, University of Heidelberg, Heidelberg, Germany
Introduction: Compared to other techniques, pedicle screws provide biomechanically superior fixation of the subaxial cervical spine, yet, screw placement is technically demanding due to the proximity of neurovascular structures and the variation in pedicle size and angulation in different cervical levels. In recent years, navigated screw placement has been increasingly reported on as a safe and accurate technique, however, studies have mainly focused on O-arm Cone Beam Computed Tomography (CBCT) based StealthStation navigation (Medtronic, Dublin, Ireland). The aim of this study was to analyse the accuracy of cervical pedicle screw (CPS) placement using a novel platform for 3D C-arm CBCT based navigation in an experimental spine model setting. Material and Methods: For 8 artificial spine models (Synbone, Zizers, Switzerland) with identical spinal anatomy (pedicle width between 2.5 mm for C4 and 7.9 mm for T1), 3D scans were acquired using a latest generation flat-panel mobile 3D C-arm CBCT (Cios Spine, Siemens, Erlangen, Germany). Subsequently, two different surgeons performed navigated CPS placement using Pulse navigation platform (Nuvasive, San Diego, California, United States) on levels C2 to T1. After automatic drilling using a navigated drill guide, polyaxial screws (VuePoint, DePuy Synthes) with a diameter of 3.5 mm were inserted with a navigated screwdriver. A second 3D scan was then acquired to allow for screw assessment by two independent observers (Obs1 and Obs2). CPS accuracy was assessed according to the Neo classification with grades 0 (no perforation) and 1 (breach < 2 mm) deemed acceptable and pedicle breaches of ≥2 mm deemed inacceptable. Interrater agreement was calculated using kappa (κ). In order to account for close matches of the two assessments, Kappa was weighted (κw). Consequently, a rating of 0 by Obs1 and 1 by Obs2 is weighted higher than a rating of 0 by Obs1 and 2 by Obs2. Interpretation of kappa was made according to Landis and Koch. Fisher’s exact test was used to compare accuracy between the two surgeons. Results: In total, 112 screws were placed. 32 (28.6%; Obs1) and 43 (38.4%; Obs2) of the screws were graded as 0 and 79 (70.5%; Obs1) and 69 (61.6%; Obs2) as grade 1. Accordingly, Obs1 assessed 1 screw (0.9%) as grade 2 (medial perforation on C7) while Obs2 did not find a perforation ≥2 mm. Overall, the CPS accuracy was 99.1% for Obs1 and 100.0% for Obs2. Interrater agreement was moderate (κ = 0.569, 95% confidence interval 0.413-0.725; κw = 0.572) with 80.4% agreement on the exact grade and 99.1% on screws being acceptable or not. Independent of the observer, there were no significant differences between the two surgeons regarding CPS accuracy (p > 0.999 and p = 0.835, respectively). Average pedicle width was significantly higher for screws with no pedicle perforation (p < 0.0001 for Obs1 and Obs2). Conclusion: In our experimental setup, CPS placement in the cervical spine using 3D C-arm CBCT based navigation proved to be highly accurate, especially when considering the screw diameter to pedicle width ratio of up to 140%. Further studies should investigate the clinical safety and feasibility of CPS placement with the navigation platform used in the present study.
1255
A321: Radiation free navigation for spine surgery an in vitro study
Josh Schroeder 1 , Leon Kaplan 1 , and Tushar Patel 2
1 Orthopedic Surgery, Hebrew University Hadassah Medical Center, Jerusalem, Israel
2 Washington University, Seattle, United States
Introduction: Surgery and spine surgery specifically are using increasing amounts of ionizing radiation in order to allow tracking and navigation during surgery. This increase in harmful radiation increases the risk of cancer for both the patients and the surgical staff. In addition, in cases in which the spine is mobile, the vertebras move during the case causing decreased accuracy as the case progress. In light of these issues, research into optical imaging and navigation has been conducted to allow a radiation-free solution. Materials and Methods: Using a specialized high definition 3D camera, augmented technology for optical imaging and AI software allowing radiation free matching of the preoperative imaging to the real anatomy of a patient, pedicle screws were planned and executed in thoracolumbar in 7 cadavers (both female and male). Real time tracing and imaging was tested in all cases. Screw accuracy was tested by postoperative computed tomography (CT) imaging. Results: 80 pedicle screws were inserted by five surgeons using optical navigation between T2 and L5 vertebrae, using the real-time tracking software. In order to assess real time tracking, during the procedure the cadavers were moved, in addition extensive dissection and osteotomies of spine were performed in order to allow spine motion during procedures. Real time tracking and imaging was tested and successful throughout the cases. Accuracy rate using system guidance was 100% throughout surgery as well as in postoperative CT verification in all cadavers. Summary: Optical navigation is an emerging new technology that provides a safe solution for a radiation free spine surgery. As this technology continues to evolve allowing sub-millimeter accuracy and real time imaging, it shall be able to decrease the need of intraoperative CT scans for patients. Live patient testing is needed to translate this promising technology from the bench to the operating room table.
1533
A322: Robotic-navigated assistance in spine surgery: a single institution evaluation of 1001 pedicle screws
Frederik Abel 1 , Fedan Avrumova 2 , Samuel Goldman 2 , Celeste Abjornson 2 , and Darren Lebl 2
1 Radiology
2 Spine, Hospital for Special Surgery, New York, United States
Introduction: To study pedicle screw placement, complication rate, radiation exposure, and potential technology failure in adult patients undergoing robotic-navigated spinal surgery for degenerative thoracic and lumbar disorders. Material and Methods: A single-center, prospectively collected data series of patients referred for spinal surgery with robot-navigated assistance (RNA) between 2019 and 2022. Post-instrumentation, intraoperative 3D fluoroscopy scans were performed in all patients and screw positioning was compared to the preoperative plan to assess reliability, accuracy, and risk factors for malposition. Clinical and intraoperative data, radiation time, and radiation exposure were recorded. Results: A total of 1129 pedicle screws were implanted in 196 adult patients over the 3-year study period. Screws were placed robotically in 1001 (89%), converted from robotic placement to k-wire or freehand technique in 68 (6%), and planned and inserted freehand in 60 (5%) patients. Of the robotically placed screws, 94.1% were determined to be GRS Grade A with median deviation from preoperative planning templates of 1.1 ± 1.2 mm (IQR). Breaches (≥ 2 mm exceeding pedicle cortex) were registered in 19 (5.1%) of screws. Skive events were noted in 20 screws (1.8%) due to hypoplastic pedicles, unfavorable morphology of screw starting point, and soft-tissue pressure on the robotic cannula. The most common skive level was L5 (11 screws). Complete robot abandonment was recorded in three patients (1.5%). In cases with suboptimal screw position noted on intraoperative 3D scans, implants were repositioned in all cases uneventfully. Mean fluoroscopic time per screw was 5.2 ± 4.4s (SD). There were no durotomies, neurological deficits, or returns to the operating room related to implant positioning in any patient. Conclusion: RNA allows for high accuracy and reliability of screw placement in the thoracic and lumbar spine with a low rate of complications. Identification of patient anatomical features that may make suboptimal screw position more likely will aid in future implementation of robotic surgical techniques.
675
A323: Augmented reality head mounted display operating room cost are equivalent to robotic spine operative navigation cost
Miguel Ruiz Cardozo 1 , Michael Olufawo 1 , Som Singh 1 , Samuel Brehm 1 , Gabriel Trevino Verastegui 1 , Abby Carey-Ewend 1 , Matthew De la Paz 1 , Ahmed Hanafy 1 , Priscilla Stecher 1 , Michael Kann 1 , Karma Barot 1 , Raj Lavadi 1 , Alexander Yahanda 1 , Alexander Perdomo-Pantoja 1 , Magalie Cadieux 1 , Julio Jauregui 2 , and Camilo Molina 1
1 Neurosurgery
2 Orthopaedic Surgery, Washington University in St. Louis, St. Louis, United States
Introduction: Systems using augmented reality head-mounted displays (AR-HMDs) have the ability to aid the instrumentation of the spine effectively, safely, and accurately. According to previous data from clinical research, the accuracy of AR-HMD guided pedicle screw insertion ranges from 98% to 100%, which is superior to free-hand instrumentation approaches and on par with the accuracy of robotic technology. There is little information available regarding the expense of integrating this technology into operating rooms, especially when compared to concurrently developing novel supporting technologies like robotic-assisted computer navigation. This study was done to compare the operating room cost of using robotic-assisted platforms versus AR-HMD-assisted for spine surgery. Methods: We recruited a retrospective cohort of 212 patients from Washington University in St. Louis who underwent navigated pedicle screw placement by either Augmented Reality Head Mounted Displays (AR-HMD) (n = 42), Robotic Navigation (RN) (n = 54), or user-operated imaged-guided (IG) navigation (n = 118) from January 1, 2021, to January 30, 2022, in a single institution. All Hospital Costs (HC) incurred for 18 functional areas were obtained from Hospital billing for each patient’s surgical admission. We performed comparisons of ancillary costs (AC) and operating costs (OC) across different navigation groups. We used tableau desktop and R Studio for data visualization and statistical analyses. Cost distributions were compared using the non-paired samples Wilcoxon rank sum test. Results: The HC for AR-HMD ranged from $16,888 to $291,000, while the HC for IG navigation and Robotic Navigation ranged from $11,556 to $300,467, and $20,121 to $186,222, respectively. The median OC for AR-HMD, Robotic, and IG Navigation were $43,396, $36,313, and $39,063 respectively. We found no statistically significant differences between HC AR-HMD and Robotic Navigation (p = 0.3798). We found a significant difference between median OR Costs for AR-HMD and IG Navigation p < .05 (0.01305). OCs were not significantly different between IG and Robotic Navigation in our cohort p = 0.1381. The median AC for AR-HMD, Robotic Navigation, and IG Navigation was 27,898, 19,251, and 11,523, respectively. We found no statistically significant difference between Augmented Reality and IG Navigation median AC (p = 0.05493). Ancillary costs were significantly different between Augmented Reality and IG Navigation p < 0.001 (0.0004694) and between IG Navigation and Robotic Navigation p < 0.01 (p = 0.007068). Conclusion: This study suggests that the cost of enabling AR-HMD technology in a tertiary health center is similar to robotic technologies. To further clarify the economic differences between enabling technologies and the cost-effectiveness of AR-HMD-assisted surgeries in comparison to robotic-assisted surgery, a distributional cost-utility analysis is required in the future. The only commercially available AR-HMD system has an initial acquisition cost of $165,000. In contrast, robotic platform acquisition costs range from $1.0 to $1.5 million. As a result of the lower acquisition costs, AR-HMD has the potential to lower the expenses related to instrumenting the spine for similar health benefits.
644
A324: Comprehensive accuracy analysis of robotic models in spine surgery: a pooled analysis of 14,462 screws
Robert Koucheki 1,2 , John-Peter Bonello 1 , Aazad Abbas 1 , Johnathan Lex 2,3 , Nicholas Nucci 4 , Albert Yee 3,5 , Joel Finkelstein 3,5 , Jeremie Larouche 3,5 , Stephen Lewis 3,6 , and Jay Toor 3
1 Temerty Faculty of Medicine
2 Biomedical Engineering
3 Division of Orthopaedic Surgery, University of Toronto, Toronto, Canada
4 Orthopedic Surgery, University of Ottawa, Toronto, Canada
5 Division of Orthopaedic Surgery, Sunnybrook Health Sciences Centre, Toronto, Canada
6 Division of Orthopaedic Surgery, University Health Network, Toronto, Canada
Introduction: This meta-analysis attempts to evaluate the literature surrounding robot-assisted spine surgery to compare prominent robotic models, using conventional techniques (free-hand or fluoroscopy) and non-robotic navigation as common controls. Material and Methods: Literature searches were performed using four major databases. All level 3 or higher studies comparing robot-assisted surgery with freehand/fluoroscopic screw placement, or non-robotic navigation were included. Participants were adult patients undergoing spinal instrumentation surgery at any spinal level. The primary objective of this study was to compare screw placement accuracy and incidence of breaches by various robot models. Included studies must have had computed tomography (CT) confirmation of screw trajectory. The secondary objective of this study was to compare these platforms in neurologic complication (NC) rate and blood loss (BL). Results: 27 studies were included, of which 20/27 studies compared robotic surgery to conventional (freehand/fluoroscopy) and 8/27 studies compared robotic surgery to non-robotic navigation (1 common study). 3404 patients underwent spinal instrumentation surgery of which 1279 patients had robotic surgery, 1573 patients were treated with conventional techniques, and 552 patients with non-robotic navigation. There were significantly less overall breaches in the robotic group compared to the conventional group (OR 0.54, 95% CI 0.39 to 0.76, p = 0.0004, I2 = 81%, random effect model (REM)). When using conventional techniques as common control, the TiRobot (TINAVI) and Renaissance (Mazor) had the best overall accuracy. Also compared to conventional techniques, the robotic group had significantly lower NC (OR 0.3, 95% CI 0.11 to 0.81, p = 0.02, I2 = 0%), however, there was no significant difference between each robot model (p = 0.97). Additionally, there was significantly less BL in the robotic group (MD: -112.74 mL, 95% CI -173.04 to -52.43, p = 0.002, I2 = 88%). When interpreting these findings, it should also be noted that 60% of TiRobot (TINAVI) studies and 30% of SpineAssist (Mazor) studies, had potential conflicts of interest and source bias from industry/governmental sponsors with a financial interest in the product, while none of the Renaissance (Mazor) studies had any stated sources of financial bias. Furthermore, compared to non-robotic navigation, robotic surgery had significantly lower rates of major breaches (OR 0.39, 95% CI 0.16 to 0.98, p = 0.04, I2 = 62%, REM). When using non-robotic navigation as a common control, no significant differences existed between rates of overall breach between MazorX (OR 0.28) vs. TiRobot (OR 0.41) (p = 0.26) or rates of major breach between MazorX (OR 0.05) vs. TiRobot (OR 0.36) (p = 0.22). Conclusion: Our results indicate that in adults undergoing spinal instrumentation surgery, use of robot-assisted navigation platforms leads to almost significant reduction in rates of overall breach compared to conventional (freehand or fluoroscopy) and non-robotic navigation techniques. MazorX (Mazor), TiRobot (TINAVI), and Renaissance (Mazor) emerge as the current leaders in robotic spine surgery. However, further RCTs with international collaborations using fundings from sources without financial interest in the products are required.
OP37: MIS complications and Challenges
579
A325: The anatomical positioning of retroperitoneal organs in single-position prone lateral lumbar surgery
Yusuke Dodo 1,2 , Ichiro Okano 2 , Neil Kelly 3 , Haffer Henryk 1 , Maximilian Muellner 1 , Erika Chiapparelli 1 , Jennifer Shue 1 , Darren Lebl 1 , Frank Cammisa 1 , Federico Girardi 1 , Alexander Hughes 1 , Gbolabo Sokunbi 1 , and Andrew Sama 1
1 Hospital for Special Surgery, Spine Care Institute, New York, United States
2 Department of Orthopaedic Surgery, Showa University Hospital, Shinagawa, Japan
3 Weill Cornell Medicine, New York, United States
Introduction: There are reports that performing lateral lumbar interbody fusion (LLIF) in a prone, single position with posterior fixation may result in a shorter operative time by eliminating patient repositioning. It is also hypothesized that the LLIF procedure can be done safely in the prone position because the retroperitoneal organs reflect anteriorly with gravity. However, no study has investigated the safety of this single-position prone LLIF (single-prone LLIF) procedure and retroperitoneal organ positioning in the prone position. Our study aim to investigate the positioning of retroperitoneal organs in the prone position and evaluate the safety of single-position prone lateral lumbar interbody fusion surgery. Material and Methods: A total of 94 patients undergoing posterior lumbar fusion surgery were retrospectively reviewed. The anatomical positioning of the retroperitoneal organs was evaluated by CT in the preoperative supine and intraoperative prone position. The distances from the center line of the intervertebral body to the organs including aorta, inferior vena cava, ascending and descending colons, and bilateral kidneys were measured for the lumbar spine. An “at risk” zone was defined as distance less than 10 mm anterior from the center line of the intervertebral body. Results: Compared to supine preoperative CTs, bilateral kidneys at the L2/3 level as well as the bilateral colons at the L3/4 level had statistically significant ventral shift with prone positioning. The proportion of retroperitoneal organs within the at risk zone ranged from 29.6% to 88.6% in the prone position. Females had significantly smaller distances for most measurements compared to males. Conclusion: The retroperitoneal organs shifted ventrally with prone positioning. However, the amount of shift was not large enough to avoid risk for organ injuries and substantial proportion of patients had organs within the cage insertion corridor. Careful preoperative planning is warranted when considering single-prone LLIF.
869
A326: The coronal anatomic location of the lumbar plexus: implications for lateral lumbar interbody fusion
Luiz Pimenta 1 , Emily Mills 2 , Tara Shelby 2 , Andy Ton 2 , Jeffrey C. Wang 2 , Raymond Hah 2 , and Ram Alluri 2
1 Instituto de Patalogia da Coluna, Sao Paulo, Brazil
2 Orthopaedic Surgery, Keck School of Medicine of USC, Los Angeles, United States
Introduction: Lateral lumbar interbody fusion (LLIF) has gained in popularity in recent years. However, the anatomy of the lumbar plexus in the coronal plane has not been well studied. Therefore, the purpose of this study was to determine the coronal anatomy of the lumbar plexus as it relates to commonly accessed disc spaces in LLIF. Material and Methods: Four fresh frozen cadavers were studied. Radiopaque dye was injected into the lumbar plexus and fluoroscopic images were obtained. The coronal distance from the L3-L4 and the L4-L5 disc spaces to the lateral aspect of the lumbar plexus was measured by two independent authors. The average distance of the lumbar plexus from each disc space, L3-L4 and L4-L5, was calculated. A Mann-Whitney U test was used to assess for a significant difference between the two disc spaces. A p-value of less than 0.05 was considered significant. Results: A total of eight disc spaces were measured. The lumbar plexus was an average of 1.25 ± 0.76 mm lateral to the L3-L4 disc space and an average of 5.17 ± 3.49 mm lateral to the L4-L5 disc space in the coronal plane, which was significantly different (p = 0.0117). Conclusion: The lumbar plexus becomes increasingly lateral in the coronal plane as it moves caudally within the psoas. This has important implications in terms of surgical anatomy and safety when retracting and dissecting within the psoas muscle during LLIF.
1145
A327: The utility of intraoperative transabdominal muscle action potentials (TMAP) during lateral lumbar interbody fusion: can we predict postoperative neuropraxia?
Michael Rogers 1 , Ashish Patel 1 , Jahangir Asghar 2 , and Alfredo Guiroy 2
1 Spine Surgery, Duly Health and Care, Naperville, United States
2 Spine Surgery, Elite Spine Health and Wellness, Plantation, United States
Introduction: There are substantial limitations in current neuromonitoring modalities for predicting postoperative neuropraxia during lateral lumbar interbody fusion (LLIF). Electromyography (EMG), saphenous nerve somatosensory-evoked potentials (SSEP) monitoring, and surgical time in the psoas are methods used to predict postoperative neuropraxia. TMAP has potential superiority over other modalities due to its ability to monitor the function of individual myotomes, specifically, quadriceps function during LLIF. Our study seeks to investigate the strengths and weaknesses of utilizing TMAP as a neuromonitoring modality. Material and Methods: This is a retrospective study of 41 patients who underwent a prone lateral interbody fusion from August 2020 to June 2022. All patients underwent intraoperative TMAP neuromonitoring. All increases in stimulation needed to obtain a similar compound muscle action potential compared to a baseline stimulation were analyzed and compared to post-operative quadriceps strength. Results: 41 patients underwent prone LLIF, including 31 levels at L4-L5. There were two cases of patients who underwent fusion at the L4-L5 level and presented with 3/5 quadriceps muscle weakness on the ipsilateral surgical side. One patient improved by the 5-week mark, but the other remained at 4/5 quadriceps muscle strength at one year. The average retractor time was 24 minutes (12 to 51 min). 40% (n = 155) of all myotomes at the L4-L5 level met or exceed the current standard alarm criteria of 150mA or more. At the current alarm criteria, TMAP showed a sensitivity of 100%, specificity of 37.93%, and a false positive rate of 62.07%. When the alarm criteria was increased to 400 mA or more, sensitivity remained at 100%, specificity increased to 83.33%, and the false positive rate decreased to 16.67%. There were no false negatives recorded at the L4-L5 level. Conclusion: TMAP is a reliable intraoperative neuromonitoring modality used to assess lower extremity motor function during LLIF. Ventral migration of the plexus within the psoas may lead patients more likely to have a quadriceps injury at L4-L5. The researchers believe that TMAP has the potential to intraoperatively predict postoperative neuropraxia. There is an extremely encouraging 0% false negative rate. Further work is underway to delineate the appropriate threshold to optimize specificity and decrease the false positive rate while maintaining high sensitivity.
113
A328: Incindental dura tears in endoscopic spine surgery - results of an international multicenter study
Stefan Hellinger 1 and Lewandrowski Kai Uwe 2
1 OOCCM MVZ, Munich, Germany
2 Spine Surgery, Orthopaedic Spine Surgeon Center for Advanced Spine Care of Southern Arizona and Surgical Institute of Tucson, Tucson, United States
Background: Incidental dural tears during lumbar endoscopy can be challenging to manage. Unfortunately, there is limited information on their appropriate management, risk factors, and the clinical consequences of this typically uncommon complication. Materials and Methods: To improve the statistical power of studying durotomy with lumbar endoscopy, we performed a retrospective survey study among endoscopic spine surgeons worldwide by email and chat groups on social media networks. Descriptive and correlative statistics were done on the surgeons’ recorded responses to multiple-choice questions. In addition, surgeons were asked about their clinical experience with spinal endoscopy, training background, the types of lumbar endoscopic decompression they perform by approach, the decompression instruments they use, and incidental durotomy incidence and handling routine lumbar endoscopy. Results: There were 689 dural tears in 64,470 lumbar endoscopies, resulting in an incidental durotomy incidence of 1.07%. Endoscopic stenosis decompression (54.8%; p = .0001), rather than endoscopic discectomy (44.1%; 41/93), was significantly more associated with durotomy. Medium-sized dural tears (1-10 mm) were the most common (52.2%; 48/93). Small pinhole durotomies (less than 1 mm) were the second most common type (46.7%; 43/93). Rootlet herniations were seen by 46.2% (43/93) of responding surgeons. Over half of surgeons did not attempt any repair or closure (52.2%; 47/90). Forty percent (36/90) used sealants. Only 7.8% (7/ 90) of surgeons attempted an endoscopic repair or sutures. Nearly half of the patients (48.3%; 43/89) were treated with 24-48 hours of bed rest. The majority of participating surgeons (64%; 57/89) reported that the long-term outcome was unaffected. Only 18% of surgeons reported having seen the development of a postoperative cerebrospinal fluid (CSF)-fistula (18%;16/89). However, the absolute incidence of CSF fistula was only 0.025% (16/64470). Severe radiculopathy with dysesthesia, sensory loss, and motor weakness in association with an incidental durotomy was reported by 12.4% (11/89), 3.4% (3/89), and 2.2% (2/89) of surgeons, respectively. Discussion: The incidence of dural tears with lumbar endoscopy is about 1%. The incidence of durotomy is higher with the use of power drills and the interlaminar approach. Stenosis decompression that typically requires the more aggressive use of these power instruments has a slightly higher incidence of dural tears than does endoscopic decompression for a herniated disc. Most dural tears are small and can be successfully managed with mechanical compression with Gelfoam and sealants. Two-thirds of patients with incidental dural tears had an entirely uneventful postoperative course. The remaining one-third of patients may develop a persistent CSF leak, radiculopathy with dysesthesia, sensory loss, or motor function loss. Therefore, patients should be educated preoperatively and reassured.
631
A329: Association of nerve retraction time during lumbar endoscopic discectomy with the onset of post-operative radiculitis
Michael Gerling 1 , Melissa Baker 1 , Evan Chaladoff 1 , Eloise Stanton 2 , and Zorica Buser 1
1 Gerling Institute, Brooklyn, United States
2 Keck School of Medicine, Los Angeles, United States
Introduction: Lumbar disc herniations are one of the most common spinal pathologies leading to low back pain and radiculopathy. The open lumbar discectomy was considered a gold standard, however, it involves general anesthesia, a large skin incision and substantial muscle retraction. Recent advancements in discectomy procedures include the use of full endoscopic techniques using the inter laminar and extraforaminal approaches. While endoscopy reduces tissue retraction and incision size, the procedures require scope placement within the foramen and lateral recess and substantial nerve root retraction. Nerve root retraction time has shown to correlate with neurologic complications in other lumbar surgical techniques. The aim of the current study was to evaluate the relationship between nerve root retraction time and post-operative radiculitis and other patient reported outcomes. Material and Methods: The current study included patients who underwent single or multi-level lumbar discectomy between 2020 and 2022 for lumbar disc herniations. Demographic and intra-operative variables were recorded. Data on post-operative complications, pre- and post-operative PROs (VAS, ODI and CAT) were collected at various time points up to one year. Paired sample two-tailed t-test and multivariate regression with p < 0.05 being significant were utilized. Results: The current study included 157 patients who underwent single or multi-level endoscopic lumbar discectomy between 2020 and 2022. 112 (71.3%) of the discectomies were single-level procedures, 44 (28.0%) were two-level, and one (0.7%) was three-level. 43 (27.4%) were performed via an interlaminar approach, 5 (3.2%) were performed via a sublaminar approach, and 107 (68.2%) were performed via an extraforaminal approach. Average surgical time was 29.4 minutes and average estimated blood loss was 7.05 mL. Average patient age was 44 years of age, and 64% were male patients. Nerve retraction time was between 4 and 15 minutes. Twenty-four patients (18%) reported a new neurological deficit - radiculitis at 2-weeks post-operatively. In patients with radiculitis 86% reported significantly worse VAS leg at 2 weeks post-op (4.2 vs 8.3, p < 0.001) compared to 14% who had improved VAS leg (9.3 vs 7, p = 0.1181). Patients with radiculitis and worse VAS scores had substantially longer nerve retraction time (13.8 ± 7.5 min) than patients with improved VAS leg (6.7 ± 1.2 min). In radiculitis patients with longer nerve retraction time VAS leg remained higher than the pre-operative values at later time points. At 6 months in patients with longer nerve retraction time there was no significant improvement in the ODI score (0.52 vs 0.46, p = 0.306). Similar trends were observed for CAT domains for Pain interference, Pain intensity and Physical function. Conclusion: This is the largest study to our knowledge that has looked at the nerve root retraction time as a risk factor for radiculitis and diminished patient outcomes in the endoscopic discectomy literature. The initial findings show that patients with new onset radiculitis who had longer nerve retraction time have worse VAS leg outcomes at early and later time points, and minimal improvement in ODI and CAT scores.
48
A330: The impact of Body Mass Index on outcomes following the minimally invasive antepsoas (MIS-ATP) approach for lumbar arthrodesis
Chadi Tannoury 1 , Rahul Bhale 1 , Christopher Maatouk 1 , and Tony Tannoury 1
1 Orthopedic Surgery, Boston University Medical Campus, Boston, United States
Introduction: Obesity is a well-known contributing factor to developing cardiovascular diseases, intervertebral disc disorders, and low back pain. The primary objective of this investigation is to study the relationship between body mass index (BMI) and complications, as well as length of stay (LOS), following the minimally invasive antepsoas (MIS-ATP) lumbar fusion. Methods: This is a retrospective chart review of 509 consecutive patients who underwent MIS-ATP fusions with posterior percutaneous fixation addressing one-to-six level pathologies. Patient characteristics including age, sex, smoking status, length of stay, and body mass index were extracted from patient records, along with relevant short- and long-term complications. Complications studied included medical (deep vein thrombosis, pulmonary embolism, urinary tract infection, pneumonia, ileus, and anemia requiring transfusion), mechanical (hardware failure, adjacent segment disease, and pseudarthrosis), neurological (weakness, and leg paresthesia), and subsequent surgical site infections (superficial and deep infections). Logistic regression was used to report the strength of association between patients’ BMI and complications. Linear regression was performed to evaluate the correlation between BMI and the LOS following surgery. Results: Consecutive 509 patients were included in this retrospective study (average age 55.5 years, 56.4% females, 48.9% smokers, average length of stay 3.61 days, average BMI 30.8). There were 54 reported complications, with 49 patients (9.6%) experiencing at least one. Upon performing logistic regression, increased BMI was not a statistically significant risk factor for any of these complications. Corresponding odds ratio and p-values were: deep vein thrombosis (O.R. = 1.09, p = 0.32), pulmonary embolism (O.R. = 1.09, p = 0.51), urinary tract infection (O.R. = 0.89, p = 0.54), pneumonia (O.R. = 0.95, p = 0.70), ileus (O.R. = 1.02, p = 0.77), anemia requiring transfusion (O.R. = 0.99, p = 0.71), adjacent segment disease (O.R. = 1.02, p = 0.82), hardware failure (O.R. = 0.93, p = 0.31), pseudarthrosis (O.R. = 1.10, p = 0.47), chronic leg paresthesia (O.R. = 1.02, p = 0.77), superficial wound infection (O.R. = 1.02, p = 0.85), and deep infection (O.R. = 1.00, p = 0.98). Linear regression yielded an unlikely correlation between BMI and LOS following surgery (R-squared 0.0004). Conclusion: Increased BMI was not statistically associated with increased complications or LOS in patients who underwent MIS-ATP lumbar fusion supplemented with posterior percutaneous fixation. While our findings are corroborated by other publications, increased BMI is still considered a risk factor affecting the outcomes of lumbar fusion by others.
60
A331: Prospective Randomized Cohort Evaluation Of Ambulatory Uniportal And Biportal Endoscopic Spinal Decompression For Lumbar Spinal Stenosis Surgery
Pang Hung Wu 1
1 Ng Teng Feng General Hospital, Orthopaedic Surgery , SINGAPORE, Singapore
Prospective Randomized Cohort Evaluation Of Ambulatory Uniportal And Biportal Endoscopic Spinal Decompression For Lumbar Spinal Stenosis Surgery
Background: Endoscopic spine surgery has been established as a practical, minimally invasive technique for decompression in patients with lumbar spinal stenosis. However, there remains a paucity of studies comparing uniportal lumbar endoscopic unilateral laminotomy with bilateral decompression (LE-ULBD) and unilateral biportal endoscopic unilateral laminotomy with bilateral decompression (UBE) with open spinal decompression– both viable techniques with satisfactory clinical outcomes in the treatment of lumbar spinal stenosis. Objective/Aim: To compare the efficacy of LE-ULBD and UBE for patients with lumbar spinal stenosis. Methods: Patients with lumbar spinal stenosis and neurogenic claudication were randomized to either uniportal or biportal endoscopic decompression. Total enrolment period was 12 months. Baseline characteristics, initial clinical presentation, and operative details including complications were recorded for all included patients. Clinical outcomes, such as visual analogue scale (VAS) and Oswestry Disability Index (ODI), were recorded at preoperative, immediate postoperative, 2 weeks, 3, 6, and 12-month follow-up periods. Results: A total of 62 patients underwent endoscopic decompression surgery for lumbar spinal stenosis (29 LE-ULBD, 33 UBE). No significant baseline differences were found between uniportal and biportal decompression, when comparing operative duration (130 vs 140 mins; p = 0.30), intraoperative blood loss (5.4 vs 6 mLs; p = 0.05), and length of hospital stay (23.6 vs 20.3 hours; p = 0.35). Two patients (7%) who underwent uniportal endoscopic decompression required conversion to open surgery due to inadequate decompression. There was significantly higher intraoperative complication (13.4% vs 0%, p < 0.05). VAS score (leg & back) and ODI improved significantly (p < 0.001) in both endoscopic decompression groups across all follow-up time points, with no appreciable statistical differences between both groups. Conclusion: LE-ULBD has the same efficacy as UBE in the treatment of lumbar spinal stenosis. While LE-ULBD surgery enjoys added aesthetic benefits of only one wound, UBE had potentially lower risks of intraoperative complication, inadequate decompression and conversion to open surgery during early period of learning curve.
332
A332: Endoscopic spine solutions in spondylodiscitis
Ayush Sharma 1
1 Department of Orthopedic and Spine, Dr B R Ambedkar Memorial Hospital, Mumbai, India
Introduction: Diagnosis of infectious spondylodiscitis is difficult considering traditional biopsy methods. Isolation of causative organism by culture using Fluroscopy or CT guided biopsy material have yield of only 30% to 38%. We present our case series of 18 patients for obtaining endoscopy biopsy for spondylodiscitis. Materials & Methods: Patients presenting with features of spondylodiscitis such as back pain, fever, signs of neurological compression were included in the study. Pre-operative Xray, CT scan and MRI were evaluated for confirmation of radiological diagnosis. Patients included in the study were neurologically intact and no signs of spinal instability were present- as absence of this would warrant decompression and instrumentation. Biopsy material was sent for culture and histopathology. Pre-Op and Post-Op VAS, ODI scores, ESR, CRP were recorded. Patients were followed up for minimum of one year or until complete resolution of infection. Results: 18 patients were included in study- 10 were males and 8 females. Mean age of presentation was 44.78 years (Range 25 to 67). PreOp VAS score 7.77 ± 0.97 and PostOp VAS was 3.78 ± 1.22. This difference is statistically significant (p = 0.0002). Clinical diagnosis for microbial identification was established in 88.89% patients (16 out of 18). 62.5% had Mycobacterium tuberculosis infection. Among the rest Staphylococcus aureus was most common. ODI scores improved statistically at 6 month and 1 year follow up. ESR and CRP values normalized with institution of appropriate drug therapy. Conclusion: Use of Endoscopy for biopsy in Spondylodiscitis is far efficient than traditional methods. It has a targeted approach to the site of pathology. Debulking and wash of the abscess gives immediate pain relief to patient. This procedure can be done under local anaesthesia. This turned out to be especially helpful for post-covid patients with poor lung functions and impaired immunity by steroids causing spondylodiscitis.
497
A333: Minimally invasive versus open posterior cervical fusion techniques: fusion rates and perioperative parameters
Gabriel Tender 1
1 Neurosurgery, Louisiana State University, New Orleans, United States
Introduction: Posterior cervical fusions for degenerative spinal pathologies typically imply extensive muscle dissection and high postoperative morbidity. A relatively new, minimally invasive technique, involving facet decortication and placement of interfacet spacers, has shown promise in terms of safety and patient satisfaction improvement. However, it is unclear how the actual bony fusion rates compare between this new technique and the gold standard, open posterior cervical fusion with lateral mass screws and rods. Material and Methods: Between 01.01.2014 and 02.28.2022, we retrospectively reviewed all the patients who underwent either an interfacet fusion (Group 1) or a traditional, open posterior cervical fusion (Group 2), at 3 levels or less, between C2 and T1 (i.e., subaxial cervical spine), for degenerative pathology. Group 1 surgical indications included pseudarthrosis after anterior cervical discectomy and fusion (19 patients), augmenting multilevel ACDF in smokers (6 patients), cervical radiculopathy (4 patients), and juxtafusional disease (3 patients). Group 2 surgical indication was myelopathy due to cervical stenosis. The primary outcome measure was the presence of fusion versus pseudarthrosis on follow-up imaging. Secondary outcome measures included perioperative parameters (operative room time, estimated blood loss, length of hospital stay) and postoperative complications. Results: Group 1 had 32 patients undergoing interfacet decortication and spacer placement at 62 levels. Group 2 had 26 patients undergoing open posterior cervical fusion at 64 levels. Four patients in Group 1 and 5 patients in Group 2 were lost for follow-up after the 2-month visit. In Group 1, 27 of 28 patients had confirmed fusion on postoperative imaging, whereas one patient treated for juxtafusional disease with a hypermobile segment experienced symptomatic pseudarthrosis and had to undergo subsequent revision surgery (anterior discectomy and fusion at the respective level). In Group 2, 14 of 21 patients had confirmed fusion on imaging, whereas 7 patients exhibited lucency around at least one of the lateral mass screws, suggestive of pseudarthrosis; however, none of these patients required revision surgery during the study period. The perioperative parameters favored the minimally invasive technique. There were 3 deep wound infections requiring washout and one postoperative aspiration pneumonia in Group 2. Conclusion: The minimally invasive, interfacet posterior cervical technique results in high fusion and low pseudarthrosis rates, compared to the open, traditional technique. The minimally invasive technique should be employed, when indicated.
OP38: Adult Deformity 3
1808
A334: Coronal alignment classification for severe idiopathic scoliosis based on the relationship between the apical vertebras and CSVL: a treatment-oriented guideline
Aixing Pan 1 Yong Hai 1
1 Orthopedic, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: To establish a classification of coronal alignment for severe idiopathic scoliosis (IS) based on the positional relationship between apical vertebras and central sacral vertical line (CSVL) and to propose a treatment algorithm to avoid post-operative coronal malalignment (CM). Material and Methods: Patients are classified on the basis of the coronal balance distance (CBD) between the C7 plumb line (C7PL) and the CSVL, and the positional relationships between the centers of the apical vertebras (CoAVs) and CSVL. Four types of CM patterns were defined: Type 1: CBD ≤ 2 cm, CoAVs on the same side of the CSVL. Type 2: CBD ≤ 2 cm, CoAVs on either side of the CSVL. Type 3: CBD > 2 cm, CoAVs on either side of the CSVL. Type 4: CBD > 2 cm, CoAVs on the same side of the CSVL. Results: A total of 80 patients with IS who underwent posterior spinal fusion (PSF) were enrolled. At post-operation and follow-up, CM occurred in 23 (50%) and 13 (28.26%) of type 1 patients, 7 (70%) and 4 (40%) of type 2 patients, 6 (60%) of all type 3 patients, 9 (64.29%) and 10 (71.43%) of type 4 patients. To avoid postoperative CM, correction rate of the main curve (CRMV) should match the compensatory curve for types 1 and 2; the CRMV should be greater than the compensatory curve for type 3; and the CRMV should be less than the compensatory curve for type 4, and the angle of inclination of the LIV needs to be reduced. Conclusion: The coronal alignment classification of IS proposed in this study has good consistency. Type 1 and type 2 patients have good compensatory ability in the event of postoperative CM. Type 3 and type 4 patients have limited compensatory ability. The proposed surgical algorithm facilitates the handling of each type of coronal alignment.
2010
A335: Multiple asymmetric ponte osteotomy (MAPO) in adult severe rigid congenital or idiopathic kyphoscoliosis: the modified masterpiece of alberto ponte with minimum 2-year clinical and radiological outcomes
Nicholas Van Halm-Lutterodt 1,2,3 , Ziyang Ye 3,4 , Yangpu Zhang 2 , Aixin Pan 2 , Lijin Zhou 2 , Tie Liu 2 , Yuzeng Liu 2 , Jincai Yang 2 , Sunny Kim 3 , and Yong Hai 2
1 School of Professional Studies, Brown University, Providence, United States
2 Department of Orthopedics Surgery, Beijing Chaoyang Hospital Affiliated Capital Medical University, Beijing, China
3 Department of Orthopedic and Neurosurgery, Inspired Spine Health, Burnsville, United States
4 Department of Analytics and Data Science, University of Chicago, Chicago, United States
Background: Alberto Ponte initially innovated ‘Ponte osteotomy’, a posterior-only osteotomy for the management of hyperkyphotic conditions such as Scheuermann’s disease or ankylosing spondylitis from the late 1960s, and its wide application has evolved with the advancement of technology. Ponte osteotomy was recently classified by Schwab and colleagues as grade-II posterior column osteotomy (PCO), which is less aggressive than pedicle subtraction osteotomy (PSO), but more aggressive that Smith-Petersen’s osteotomy (SPO, ie., grade-I) since the Ponte osteotomy involves total facetectomies and often, laminectomies in addition to other posterior elements. The clinical and radiographic outcomes of MAPOs (Schwab-grade-II) in adults with severe rigid scoliosis and kyphoscoliosis would be an interesting facet of discussion for global spine experts. Methods: Following approval by the institutional review board (IRB) of Beijing Chaoyang Hospital-Affiliated Capital Medical University in Beijing, a pool of 14 adult (≥18 years) severe rigid scoliosis or kyphoscoliosis patients (curves ≥ 80o) who had Schwab-grade-II PCO as a primary corrective surgical technique from 2009 to 2014 were retrospectively evaluated. The primary outcomes included the perioperative clinical, radiographic patient-reported outcomes were evaluated at minimum 2-year, final follow-up (FFU) period. Secondary outcomes included preoperative and final follow-up ODI and SRS-22 scores. Statistical analyses were carried out by Student t-test, Mann-Whitney test, and Pearson’s Chi-squared test (Fisher’s Exact Test), through Python statistical software package. Statistical significance was set at (p < 0.05). Results: A total of 14 Schwab-grade-II treated patients were observed. The average age was 22.4 years with a female incidence of 50.0%. The etiologies were approximately 35.7% idiopathic and 64.3% congenital patients. The average body mass index (BMI) was 19.4 kg/m2. The average fusion length was 13.7 and the surgical duration was 303.6 minutes with a median blood loss volume of 950 ml. The average follow-up time was 2.6 years. The preoperative major curve Cobb angle of 105.2o was corrected to 47.1o at immediate postoperative and 45.5o at FFU, (p < 0.001). The preoperative compensatory curve Cobb angle of 57.6o was corrected to 29.6o at immediately postoperative and 30.5o at FFU, (p < 0.001). The average preoperative apical vertebral translation (AVT) of 9.7-cm was corrected to 3.4-cm at FFU, (p < 0.001). The averages of preoperative thoracic kyphotic (TK) and lumbar lordotic (LL) angles of 66.0o and 68.0o were corrected to 40.0o and 52.4o at FFU, respectively, (p < 0.001). The average vertical axes of coronal (CVA) and sagittal (SVA) outcomes demonstrated that normal alignment was achieved in these patients. Major curve corrective rate was 56.4% at FFU. The ODI and SRS-22 scores significantly improved from baseline at FFU, (p < 0.01). Conclusion: The findings from this study indicate MAPO remains a potent osteotomy for severe rigid kyphoscoliosis and can achieve major curve correction of over 55% in spinal rigid deformity patients while correcting both coronal and sagittal alignments. As a posterior-column-only approach, we can attest that this approach is also safe and can be widely utilized for the effective management of severe rigid congenital or idiopathic deformity phenotypes.
1489
A336: The cranial sagittal vertical axis to the hip (CrSVA-H) is the best sagittal alignment predictor of patient reported outcomes at 2 years postoperative in adult spinal deformity surgery
Christopher Lai 1 , Sarthak Mohanty 2 , Fthimnir Hassan 1 , Caroline Taber 1 , Jaques Williams 1 , Nathan Lee 1 , Zeeshan Sardar 1 , Ronald A. Lehman 1 , and Lawrence Lenke 1
1 Department of Orthopaedic Surgery, Columbia-New York Presbyterian Hospital, New York, United States
2 Department of Orthopaedic Surgery, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, United States
Introduction: Sagittal alignment measurements including C7SVA and PI-LL are established drivers of outcomes in adult spinal deformity (ASD). Increasing consideration has now been given to the role of total body sagittal alignment. Recent evidence suggests that cranial sagittal vertical axis (CrSVA), may be a better predictor of preoperative PROs. This study thus sought to evaluate CrSVA as a predictor of PROs at 2-years postoperative. Material and Methods: A single-center database was queried for ASD patients undergoing ≥ 6 level fusions from 2015-2020. CrSVA to the sacrum(S), hip(H), knee(K), and ankle(A) were measured as the horizontal distance to the vertical plumbline from the nasion-inion midpoint, with positive values indicating cranial center of mass anterior to the reference point. Standard sagittal alignment parameters (pelvic incidence[PI], lumbar lordosis[LL], PI-LL, C2-sacrum/hip/knee/ankle, and C7SVA) were also collected. Total SRS score at 2-year postop was the dependent variable. Two conceptual, multivariable linear regression models were built after adjusting for impact of preop SRS scores on 2-year outcomes. Model 1 assessed pre/postoperative alignment only relative to C2/C7 while Model 2 assessed alignment relative to C2/C7 as well as the cranium. Significance was defined as p-value < 0.05, with post-hoc Bonferroni corrections for multiple comparisons. Results: There was a total of 161 patients with 2-year follow-up, with 72.6% female and average age of 50.49(SEM = 1.38), BMI 18.67 (SEM = 1.01), and TIL of 13.5 (SEM = 0.32) levels. A stepwise univariate linear regression discerned predictors of lower, or worse, SRS scores at 2-year postoperatively, where negative β indicates worse scores. Among patient characteristics, older age [per year increase] (β = -0.19, p = 0.02), greater preoperative morbidity [per unit increase in ASA score] (β = -8.05, p = 0.001), and lower baseline total SRS [per point increase] (β = 0.56, p < 0.0001) were significantly associated with worse 2-year SRS scores. Sagittal alignment, both pre- and postoperatively, was also robustly associated with 2-year PROs. Greater PI-LL mismatch (β[preop] = -0.12, p = 0.047; β[postop] = -0.21, p = 0.033) and greater anterior translation of the cranium relative to the hip (CrSVA-H) (β[preop] = -1.43, p < 0.0001; β[postop] = -0.58, p = 0.029), sacrum(CrSVA-S) (β[preop] = -0.61, p = 0.006; β[postop] = -0.61,P = 0.006), and ankle (CrSVA-A) (β[preop] = -1.79, p < 0.0001); β[postop] = -0.79, p = 0.022) were associated with significantly worse PROs. Consistently, anterior translation of C2 relative to sacrum (C2-S), hip (C2-H), and ankle (C2-A) as well as C7SVA (β[preop] = -1.23, P = 0.002); β[postop] = -0.67, p = 0.004) were associated with worse PROs. Interestingly, in multivariable regression analysis, after adjusting for the impact of baseline SRS scores (β = 0.53, p < 0.0001), greater preop C7SVA was found to be the only independent predictor of 2-year SRS score (β = 1.62, p = 0.0201) when considered with preop and postop alignment only relative to C2. However, in a subsequent model including CrSVA-H, C7 SVA no longer remained an independent predictor (β[preop] = 1.16, p = 0.12; β[postop] = −0.69, p = 0.35). Instead, more anterior postop CrSVA-H (β = −2.08, 0.0044) alignment independently drove worse SRS scores postoperatively when both sagittal alignment relative to the cranium, C2, and C7 were considered together. Conclusion: Multivariable regression analysis found that C7SVA is supplanted by CrSVA-H alignment as a significant, independent driver of two-year SRS scores in patients with ASD and should be considered the new gold standard of postoperative sagittal alignment target goal.
1042
A337: Beware of positive SPECT/CT findings when investigating pain generators in patients with scoliosis with scoliosis: hospital cohort of cancer patients show high prevalence of high uptake degenerative changes
Atharv Patankar 1 , Angelo Fragkakis 2 , Nikolaos Papadakos 2 , Bisola Ajayi 2 , Nigel Beharry 2 , Cristina Lupu 2 , Jason Bernard 3 , Timothy Bishop 3 , and Darren Lui 3
1 Student
2 Spine Research Team
3 Orthopaedics, St. George's Hospital, London, London, United Kingdom
Introduction: Scoliosis can affect the general population at all ages via a wide range of configurations and presentations. Degenerative de novo scoliosis develops as an adult rather than during adolescence. Although not always painful, the unevenly distributed biomechanical axial overload could contribute to pain and accelerate degenerative spondylosis (DS). SPECT/CT is typically used as a second line of investigation for defining the features of a metabolic abnormality particularly in screening for metastatic cancer. It can also provide the exact location and nature of a pain generator in spondylosis. By examining a hospital cohort of oncological patients with or without back pain being screened for metastases, we estimated the prevalence of high uptake osteoblastic SPECT/CT activity in spinal spondylosis with scoliosis. This study analysed the prevalence of scoliosis, DS, and associated pain, in oncologic patients undergoing SPECT/CT for possible metastases and analysis of pain generators. Material and Methods: 1182 SPECT/CT reports of oncology patients between 2015-2019 were analysed. Exclusion criteria: inflammatory disorders, metastases, trauma, infection, age > 80 (n = 274), non-cancer (n = 312). Inclusion criteria: scoliosis, DS, spinal pain. Results: 596 made the inclusion criteria and their reports were analysed with patient’s mean age of 65 years (4-80). The 6.2% (n = 37) of presented with scoliosis, of which 46% (n = 17) had spinal pain, usually lumbalgia and 97% (n = 36) had DS.
Prevalence of Scoliosis with/without pain by age groups
Scoliosis was not noted in age groups under 40.
4% of patients aged 41-50 (n = 46) had scoliosis of which all presented with pain.
7.5% of patients aged 51-60 (n = 108) had scoliosis. 5.5% of the patients had painful scoliosis.
7% of patients aged 61-70 (n = 201) had scoliosis. 2.5% of patients had painful scoliosis.
6% of patients aged 71-80 (n = 223) had scoliosis. 2% of patients had painful scoliosis.
Distribution of DS in Scoliosis Patients in Each Age Group
In the 41-50 age group with scoliosis (n = 2), 100% of patients had DS in the thoracic region and 50% in the cervical region.
51-60 group (n = 8); 50% had DS in thoracic, 12.5% lumbo-sacral, 50% whole spine.
61-70 group (n = 13); 8% had DS in cervical, 46% thoracic, 69% lumbo-sacral, 8% sacroiliac, 31% whole spine.
71-80 group (n = 13); 8% had DS in cervical, 54% thoracic, 69% lumbo-sacral, 8% sacroiliac, 23% whole spine.
Conclusion: Prevalence of scoliosis in our cohort coincided with the general population. Our data shows for the first time that almost 70% of 70-year-olds have degenerative spondylosis with high uptake on SPECT/CT in at least one region in patients with scoliosis. DS affected almost all scoliosis patients, with a 1:1 ratio between painful vs non-painful cases. This is in line with the general asymptomatic population, ranging from 50-96% in ages 40-80 years. Although CT and MRI can satisfactorily investigate pain generators, SPECT/CT can highlight triggering factors in complex cases requiring higher accuracy. Nevertheless, it is not used for routine investigation due to the cost and radiation exposure. Further analysis is required to ascertain sensitivity and specificity of pain and positive SPECT/CT findings.
1854
A338: Variations of sagittal alignments in two sitting positions under different Roussouly spinal curves
Fang Xie 1 , Xueyu Hu 1 , Zhe Wang 1 , and Zhuojing Luo 1
1 Orthopaedics, The First Affiliated Hospital of Air Force Medical University, Xi´an, China
Introduction: To investigate the changes of spinal alignments in erect and working sitting positions based on different spinal Roussouly curves. Material and Methods: A total of 320 asymptomatic volunteers were enrolled. All were taken standing full-length lateral X-ray films of spine. Sagittal parameters including PT, PI, SS, LL, LDI, PI-LL, TL, TK, T9SPi, T1S, TPA, T1SPi, CL, T1-CL, C2S, TPA, cSVA, SVA and C7SFD were measured. Spinal curve types were categorized in standing position according to Roussouly classifications. In erect sitting position, the cadets sat on a wooden stool and look forward with trunk upright. Flexions of hips and knees were 90 °. Their arms naturally extended with hands placed on the knee joints. The working sitting position were obtained with trunk forward 20 ° based on erect sitting position. Changes of spinal alignments in the two positions were analyzed and compared with those in standing position. Results: In erect sitting position, SS, LL and TK decreased significantly compared with standing position, PT, CL, T1S and cSVA increased significantly. LL in type 1/3/4 were higher than that in type 2. In working sitting position, TK decreased, while PT and SS approached those in standing position. T1SPi, T1S, CL and cSVA increased significantly. LL in type 1/2 were lower than those in type 3/4. In both sitting positions, changes of LL showed no differences in type 2 and 3, while the value was higher than type 1 and lower than type 4. Conclusion: When changed from standing position to erect sitting position, candidates relied on flattening of sacrum, pelvic rotation and compensation of thoracic spine to achieve spinal balance; when changed to flying sitting position, they mainly relied on adaptive compensation of thoracic spine to obtain balance.
1736
A339: Lumbar vacuum disc presence and size are related to spinopelvic balance
Matthew Follett 1 , Tanmaya Sambare 2 , Jayme Koltsov 1 , Ivan Cheng 3 , Todd Alamin 1 , Kirkham Wood 1 , John Kleimeyer 1 , and Serena Hu 1
1 Department of Orthopaedic Surgery, Stanford University, Redwood City, United States
2 Department of Orthopaedic Surgery, University of California Los Angeles, Torrance, United States
3 Spine Surgery, Austin Spine, Austin, United States
Introduction: Vacuum discs, the collection of gas within the intervertebral disc space, are believed to represent end-stage disc degeneration. The relationship between vacuum discs and the presence of adult spinal deformity is not well described, and there is little with regard to relevance in clinical characteristics. This study aims to characterize radiographic findings in vacuum disc patients and identify associated relevant clinical features. Material and Methods: All adult patients with lumbar scoliosis evaluated in our facility between 2010 and 2019 were included if they had upright scoliosis radiographs and lumbar spine CT. Patients were excluded if they had a prior history of surgical lumbar fusion or poor quality imaging. From the radiographs, spinopelvic balance parameters were determined, including lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), PI-LL mismatch, sagittal vertical axis (SVA), coronal balance, and coronal curve cobb angles. On CT imaging, the presence and size (less than 50% of the disc space, versus greater than 50%) of vacuum discs were determined at each disc space from T12 to S1. Univariate and repeated measures analyses were performed in SAS v. 9.4 with a two-sided level of significance of α = 0.05. Results: Sixty-six patients with a mean age of 71 ± 9 years were included. Sixty-two percent were female. Diagnoses included idiopathic, degenerative, and acquired thoracolumbar / lumbar scoliosis, flat back syndrome, thoracolumbar kyphosis. Ninety-eight percent of patients had a vacuum disc (VD) between T12 and S1, most commonly occurring at the L3-4 (75.8%) and L2-3 levels (68.2%). The number of VD did not significantly correlate with spinopelvic balance parameters, but patients with a vacuum disc occupying > 50% of the disc space had lower lumbar lordosis (LL) [18.8 (95%CI: 14.1, 23.6) deg vs. 30.2 (18.4, 42.0) deg, p = 0.042] and better coronal balance [5.5 (-7.7, 18.6) mm vs. -29.3 (-70.7, 12.1) mm, p = 0.040] compared to those occupying < 50% of the disc space. The presence of a VD at L2-3 was significantly associated with negative sagittal balance [-34.6 (-61.4, -7.5) mm, p = 0.016], and at L4-5 with a positive sagittal balance [39.3 (8.9, 69.8) mm, p = 0.021]. There was no clear association between VD presence or number and scoliosis cobb angles. Conclusion: VD are common in the symptomatic adult scoliosis patient population, with three most common levels being L3-4, L2-3, and L4-5. When the VD occupy greater than 50% of the disc space, patients were found to have lower LL, possibly related to disc collapse causing loss of normal LL. Additionally, the presence of a VD at L2-3 portended negative sagittal balance, while those at L4-5 that portended positive sagittal balance. To the authors’ knowledge, this is the first study to examine the relationship between vacuum discs and spinopelvic balance parameters.
1353
A340: Morbidity and mortality rates in patients with ankylosing spinal disorders based on the number of spine injuries
Celeste Tavolaro 1 , Jonathan Yamaguchi 1 , Eli Bunzel 1 , Mathew Vincent 1 , Mark Hsiao 1 , Richard Bransford 1 , and Carlo Bellabarba 1
1 Orthopaedics and Sport Medicine, Harborview Medical Center - University of Washington, Seattle, United States
Introduction: Patients with ankylosing spine disorders (ASD), such as ankylosing spondylitis (AS) and diffuse idiopathic skeletal hyperostosis (DISH), have a fourfold fracture risk during their lifetime as compared with the general population. (Finkelstein, 1999) Patients with spine fractures and ASD are at high risk for complications and death (Caron, 2010). The most frequently injured region is the lower cervical spine and the cervical-thoracic region (Sapkas, 2009, Westerveld LA, 2009), followed by the thoracolumbar function (Whang 2000. Westerveld, 2009, Olerud, 1996, Yau 1974). To the author’s knowledge, fracture development involving unstable pelvic fracture patterns has not been addressed in the literature. In addition, morbidity and mortality rates associated with a single-level spine fracture, multiple-level spine fractures, or the combination of spine and pelvis fracture have not been reported. Material and Methods: After IRB approval was obtained, we conducted a retrospective cohort review of a large consecutive series of adult patients with ASD from 2005 to 2020 at a level 1 trauma center.Demographic data, procedural data, hospital data, and 90-days postoperative data were obtained. Statistical analyses compared single-level, multi-level, and spinopelvic injuries groups using Fisher’s Exact test and analysis of variance to compare categorical and continuous variables, respectively. Results: A total of 383 cases of ASD (155 Ankylosing Spondylitis and 228 diffuse idiopathic skeletal hyperostosis) were identified from 2005 to 2020. There were 323 patients with a single-level injury, 45 with multi-level injury, and 15 with spine and pelvic injuries. There were 96 (25.1%) patients with complications. The most common complications were wound infection 52 (13.6%), pulmonary complications 38 (9.9%), and hardware related 7 (1.9%). There were 57 deaths within 90-days (14.9%), 42 (10.9%) occurring during the inpatient period. Complication rates in these three groups were significantly different for infection (11.5%, 26.7 and 20%, respectively, p = 0.015). Significantly difference among the groups were identified for ASD type, surgical invasiveness index, energy of mechanism, injury location, instrumented levels, estimated blood loss, and discharge disposition (p < 0.05). Conclusion: The overall complication rate in the treatment of ankylosing spine disorder patients is 25.1%. The complication rate is significantly higher in patients with multilevel injury and in patients with a combination of spine and pelvic fractures. The overall 90-days mortality rate was 14.9%, not significantly different between the groups.
57
A341: Spinopelvic parameters in fragility fractures of the pelvis
Moritz Lodde 1 , Thies Fischer 2 , Oliver Riesenbeck 1 , Steffen Roßlenbroich 1 , Christoph Katthagen 1 , Dennis Günes 2 , Justinus Kösters 2 , Sebastian Schmeil 2 , Philipp Salmen 2 , Marc Schneider 2 , Michael Raschke 1 , and Ulf Liljenqvist 2
1 Department of Trauma-, Hand- and Reconstructive Surgery, University Hospital Münster, Münster, Germany
2 St. Franziskus-Hospital Münster GmbH, Münster, Germany
Introduction: The incidence, the awareness and surgical treatment of fragility fractures of the pelvis (FFP) have increased substantially during the last decades [1-3]. FFP are associated with osteoporosis and occur in the absence of trauma or after low energy trauma as a ground level fall [4-6]. According to the FFP classification FFP types II-IV present an injury of the lumbosacral junction. To the best of our knowledge there are no studies analyzing the interaction between the pelvis and the sagittal alignment of the spine in patients with FFP. An inter-relationship between the spinopelvic parameters and occurrence of FFP may be an interesting factor in the diagnosis and treatment of patients with FFP. The aim of this study was to investigate the association of spinopelvic parameters LL, PI, PT and SS in patients with FFP. Material and Methods: All patients treated for FFP in a center of maximal care of the German Spine Society (DWG) between 2017-2021 were included. Inclusion criteria of this retrospective study were FFP, age > 60 years, low energy trauma, radiography of the lumbar spine and femoral heads and a CT or MRI scan. The spinopelvic parameters were determined: lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS) and lumbar lordosis index (LLI). Results: The examined population (n = 57) consisted of 49 female patients and 8 male patients. Mean age of the present study group was 81.0 years (interquartile range [IQR] 77.1-84.8 years]. Most of the patients had a FFP type II (n = 44, 77.2%). FFP type I occurred in 8 patients (14.0%), FFP type III in 1 patient (1.8%) and FFP type IV in 4 patients (7.0%). The median LL (49.1°) and the median PI (61.6°) are significantly different (p < 0.001). The median difference of LL and PI is 12.5°. The median PT is 28.7° and the median SS is 33.3°. The LLI is 0.74. The measured median LL, PI, PT and SS are significantly (p < 0.05) different from the previous published values of asymptomatic patients of Schwab, LeHuec and Barrey-Roussouly [8-10]. Conclusion: It could be demonstrated that LL and LLI are substantially reduced in patients with FFP compared to asymptomatic patients. PT and PI are significantly increased in patients with FFP. An increased PI correlates with isthmic spondylolisthesis [11] and leads to a concentration of stress at the L5-S1 junction [12]. A reduced LL is a risk factor for subchondral insufficiency fractures of the femoral head [13]. The results of the present study show that an increased PI and a reduced LL might be a risk factor for occurrence of FFP. The spinopelvic parameters are substantially different in patients with FFP compared to asymptomatic patients.
References
1. Rommens doi:10.4103/ortho.IJOrtho_631_17.
2. Sullivan doi:10.3928/01477447-20140225-50.
3. Lodde doi:10.1007/s00113-020-00893-5
4. Rommens doi:10.1007/s00068-012-0224-8.
5. Morris doi:10.1136/pmj.76.900.646.
6. Koval doi:10.1097/00005131-199701000-00003.
7. Rommens doi:10.1016/j.injury.2013.06.023.
8. Schwab doi:10.1097/01.brs.0000248126.96737.0f.
9. Le Huec doi:10.1007/s00586-016-4485-5.
10. Barrey doi:10.1007/s00586-006-0294-6.
11. Labelle doi:10.1097/01.brs.0000138279.53439.cc.
12. Sevrain doi:10.1186/1748-7161-7-2.
13. Jo doi:10.3346/jkms.2016.31.10.1650.
1666
A342: Long vs. short sacroiliac screw in osteoporotic sacrum fractures - a biomechanical comparison
Raffael Cintean 1 , Cornelius Fritzsche 1 , Alexander Eickhoff 1 , Alexander Boehringer 1 , Florian Gebhard 1 , and Konrad Schütze 1
1 Orthopaedic Trauma Surgery, University Hospital of Ulm, Ulm, Germany
Introduction: Pelvic fractures were often associated with high-energy trauma in young patients, but data show a significant increase in osteoporotic pelvic fractures in old age due the progressive demographic change4. In order to treat these fractures adequately, appropriate therapy algorithms are required. There is an ongoing discussion about the best fixation techniques, which are ranging from lumbopelvic fixation to sacral bars or long transiliac-transsacral (TITS) screws. This study analyzes one of the most commonly used minimally invasive osteosynthesis procedures, transiliac-transacral screw osteosynthesis and sacroiliac screw osteosynthesis (SI), according to biomechanical criteria of fracture stability in osteoporotic human pelvic cadaver’s ex vivo. Material and Methods: Ten osteoporotic cadaver pelvises were randomized into two groups of 5 pelvises each. The average t-score of the pelvises was -2.35. An FFP-IIc fracture was initially placed unilaterally. The fracture was surgically treated with a navigated SI or a TITS screw. The fractured side was measured in a test setup according to Bergmann et al. with increasing physiological load up to 100N. The examinations were performed under radiological as well as 3D visual control. After testing, the fractured site was fixed with 3 SI screws for testing the contralateral side. The recorded data was evaluated every 1000 cycles. Due to variable implant failure only the first 18.000 cycles were included in the statistical analysis of anterior (total) and posterior displacement (total, vertical, gap angle, flexion). Results: At the posterior pelvic ring, the TITS screw was more stable in all measured factors. The gap angle (p < 0.0001) showed the highest difference between 6000-10000 cycles with 1.6°. The flexion (p < 0.0001) as well as the vertical dislocation (p < 0.0001) showed highest difference between 6000-1000 cycles. For total dislocation, the largest difference was found between 11000-15000 cycles (p < 0.0001). Regarding anterior dislocation, the TITS screw showed significantly better results. The highest difference in dislocation was found within 11000-15000 cycles (p < 0.0001). Conclusion: In this study, we demonstrated that the long transiliac-transsacral screws in FFP IIc type osteoporotic pelvic fractures showed higher stability under physiological loading in the biomechanical examination. In particular, the posterior pelvic ring, which is important for mobilization, was significantly more stable in all factors examined. For clinical practice, the osteosynthetic treatment of osteoporotic pelvic ring fractures should prefer the TITS screw to the short SI screw. A comparison of the TITS screw with cement-augmented SI screw may provide further important data on the best possible treatment of osteoporotic pelvic ring fractures.
OP39: Complications and Outcome in Spine Tumor Patients
1543
A343: The Prognostic Nutritional Index (PNI) is independently associated with 90-day and 12-month mortality after metastatic spinal tumor surgery
Rafael De la Garza Ramos 1 , Jessica Ryvlin 1 , Mousa Hamad 1 , Yaroslav Gelfand 1 , Saikiran Murthy 1 , and Reza Yassari 1
1 Neurosurgery, Montefiore Einstein, New York, United States
Introduction: Prognostication of postoperative survival is important in the decision-making process for patients with spinal metastases. Nutritional status has been associated with poor outcome and limited survival in the general cancer population. The objective of this study is to evaluate the prognostic capability of the prognostic nutritional index (PNI) for postoperative survival after metastatic spinal tumor surgery. Material and Methods: A total of 139 patients who underwent oncological surgery for metastatic spine disease between April 2012 and August 2022 and had a minimum follow-up of 90 days were included in this study. The median age of the population was 63 years (interquartile range: 54 - 70) and 60% were male (82 of 139). The median ECOG performance status was 2 (IQR 1 – 2) and the three most common unique primary cancers were hematological (22%), prostate (17%), and lung (16%). The PNI was calculated using the preoperative serum albumin level and total lymphocyte counts; the mean PNI for the group was 43 (standard deviation: 7.7). The primary endpoint was 90-day mortality, and the secondary endpoint was 12-month mortality. Multivariate logistic regression analyses were performed. Results: The 90-day mortality rate was 27% (37 of 139). After controlling for factors such as age, ECOG performance status, psoas muscle cross sectional area, and primary cancer type, the PNI was independently associated with 90-day mortality (odds ratio 0.95 [95% confidence interval 0.79 to 0.94]; p = 0.001). The 12-month mortality rate 56% (51 of 91). After controlling for variables such as ECOG performance status, ASA class, psoas muscle cross sectional area, and primary cancer type, the PNI was independently associated with 12-month mortality (OR 0.90 [95% CI 0.82 to 0.99]; p = 0.039). Conclusion: The PNI was found to be independently associated with 90-day and 12-month mortality after metastatic spinal tumor surgery in this study, independent of performance status, psoas muscle size, and primary cancer type. External validation of this metric as a prognostic factor is needed.
1531
A344: The placement of intraoperative epidural catheters reduces inpatient postoperative pain after complex oncologic spine surgery
Shalin Patel 1 , Douglas Fletcher 1 , Yun Qing 2 , Liang Li 2 , Christopher Alvarez-Breckenridge 3 , Rob North 3 , Claudio Tatsui 3 , Laurence Rhines 3 , Hart Donahue 4 , Keyuri Popat 4 , and Justin Bird 1
1 Orthopaedic Oncology
2 Biostatistics
3 Neurosurgery
4 Anesthesiology and Perioperative Medicine, The University of Texas MD Anderson Cancer Center, Houston, United States
Introduction: Complex oncologic spine surgery is associated with significant morbidity, including longer operative times, increased blood loss, and higher complication rates. Postoperative pain from these operations can be difficult to manage and affects the ability of patients to mobilize, safely discharge from the inpatient setting, and can affect their long-term utilization of opioids postoperatively. However, traditional preoperative placement of epidural catheters for intra- and postoperative pain control is not routinely performed in these cases due to anatomical considerations and the large, complex nature of the operations. Therefore, we sought to determine if the use of epidural catheters placed intraoperatively in complex oncologic spine surgeries would reduce immediate postoperative pain scores. Materials and Methods: A retrospective cohort analysis included patients undergoing oncologic spine surgery, with or without intraoperative epidural catheter placement, between 2016-2022 at a single tertiary-care cancer center. Postoperative day 0, 1, and 2 pain scores using the visual analogue scale were obtained by chart review. Patients were stratified by the spine surgery invasiveness index as described by Mirza et al [1]. One-way ANOVA testing was performed to assess for differences in postoperative pain scores based on surgery invasiveness. Two-sample t-tests were calculated to determine if intraoperative epidural catheter placement affected postoperative pain control. Results: A total of 305 patients were included in this study, with 103 undergoing placement of an intraoperative epidural catheter. Postoperative day 1 and 2 pain scores were similar across all groups of patients when stratified by spine surgery invasiveness index. Postoperative day 2 pain scores were significantly lower in patients who received an intraoperative epidural catheter compared to those who did not (p = 0.028), and this effect trended towards significance on postoperative day 1 (p = 0.061). Conclusions: The use of intraoperatively placed epidural catheters in oncologic spine surgery significantly reduced postoperative day 2 pain scores in our cohort and we hypothesize that this effect would also be seen on postoperative day 1 with a larger sample size. The relative invasiveness of the surgeries did not affect pain scores in our cohort. Taken together, our findings suggest that placement of epidural catheters intraoperatively reduces immediate postoperative pain during the initial hospitalization. Further studies assessing how this relates to postoperative mobilization, earlier safe discharge, and total opioid utilization in this patient population remains to be investigated.
References
1. Mirza SK, et al. Development of an index to characterize the “invasiveness” of spine surgery: Validation by comparison to blood loss and operative time. Spine 2008; 33: 2651-2661.
462
A345: Factors associated with neurological deterioration after radiotherapy for severe spinal cord compression in patients with multiple myeloma
Hester Zijlstra 1,2,3,4 , Brandon Striano 1 , Alexander Crawford 1 , Nienke Wolterbeek 2 , Diyar Delawi 2 , Diederik Kempen 3 , Jorrit-Jan Verlaan 4 , and Joseph Schwab 1
1 Department of Orthopedic Surgery, Massachusetts General Hospital/Harvard Medical School, Boston, United States
2 Department of Orthopedic Surgery, St. Antonius Hospital, Utrecht, The Netherlands
3 Department of Orthopedic Surgery, OLVG Amsterdam, Amsterdam, The Netherlands
4 Department of Orthopedic Surgery, UMC Utrecht, Utrecht, The Netherlands,
Introduction: Multiple myeloma (MM) is a malignant plasma cell dyscrasia and is the second most diagnosed hematological malignancy in the western world. Bone disease is the most frequent disease-defining clinical feature of MM, caused by diffuse, monoclonal proliferations of plasma cells in the bone marrow. These bone lesions lead to an increased risk of skeletal related events (SREs) like back pain, pathological fractures, and neurologic compromise such as epidural spinal cord compression (ESCC). SREs significantly increase the burden of MM in terms of mortality and quality of life. Up to 30% of MM patients will be affected by ESCC during the course of their disease. ESCC is a medical emergency that needs rapid diagnosis and treatment to prevent permanent paralysis. Radiotherapy has been proven to be highly effective in pain relief. However, a critical knowledge gap remains in predicting the extent of neurologic recovery in patients with deficits due to myeloma related severe ESCC (grade 2 or 3). This study focuses on neurologic outcomes after radiotherapy for severe ESCC in MM patients. Material and Methods: This retrospective cohort study was approved by our institutional review board. The following inclusion criteria were applied: patients with MM, spinal myeloma lesions, received radiotherapy for the spinal tumor between 2010 and 2021 in one of the Mass General Brigham hospitals, and exhibited an ESCC grade 2 or 3 on a cross-sectional T2-weighted MRI made within 6 weeks before radiation. Baseline characteristics were manually extracted from the patient’s records. The primary outcome was the patient’s end-stage ASIA score. To determine factors associated with worse neurological outcomes after radiation treatment, uni- and multivariate analyses were performed. To predict neurologic outcome after radiotherapy, three different algorithms were developed and validated using a 75:25 train/test split. Recursive feature elimination with cross-validation (RFECV) was used to select the best combination of variables to use in the development of the predictive models. The performance of these models was compared with respect to the area under the receiver operating curve (AUROC), recall and accuracy. Results: 162 consecutive patients with severe ESCC were included in this study. After radiotherapy, 60 patients (37.0%) did not achieve full neurologic function or deteriorated neurologically. Thirty-six patients needed further treatment after radiotherapy, either surgery or re-irradiation. The best variable set for prediction, filtered by RFECV, included the baseline ASIA score, age, BMI, time from MM diagnosis to radiotherapy, number of levels affected by ESCC, duration of neurologic symptoms, the total radiation dose, ECOG score, ISS disease stage, presence of motor symptoms, radiation of lumbar spine, degree of disease spread, and whether the patient had an improvement of symptoms after a steroid booster. The Random Forest algorithm demonstrated best accuracy (90.6%), recall (81.8%) and AUROC (89.2%) on the hold-out testing set. Conclusion: The risk factors described here can guide new avenues of research and provide specific, personalized risk assessment for a patient facing radiotherapy for spinal myeloma lesions. Our RF model, based solely on clinical parameters, proved to be a powerful predictor of neurological deterioration after radiotherapy.
1653
A346: Gender differences in clinical outcomes and survival after treatment for spinal metastases
C. Rory Goodwin 1 , Meghan Price 1 , Andrea Goodwin 2 , Tara Dalton 1 , Anne Versteeg 3 , Arjun Sahgal 4 , Laurence Rhines 5 , Michael Weber 6 , Aron Lazary 7 , Stefano Boriani 8 , Chetan Bettegowda 9 , Michael Fehlings 10 , Niccole Germscheid 11 , Nicolas Dea 12 , Raphaële Charest-Morin 12 , James Schuster 13 , Paul Arnold 14 , John Shin 15 , Ilya Laufer 16 , Ziya Gokaslan 17 , Dean Chou 18 , Michelle Clarke 19 , Charles Fisher 12 , and Daniel Sciubba 20
1 Neurosurgery, Duke University, Durham, United States
2 Sociology, Carolina Population Center, University of North Carolina at Chapel Hill, United States
3 University of Toronto, Canada
4 Sunnybrook Odette Cancer Centre and University of Toronto, Canada
5 The University of Texas, MD Anderson Cancer Center, Houston, USA
6 McGill University and Montreal General Hospital, Canada
7 National Center for Spinal Disorders and Buda Health Center, Budapest, Hungary
8 IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
9 Johns Hopkins University School of Medicine, Baltimora, United States
10 University of Toronto and Toronto Western Hospital, Toronto, Canada
11 AO Spine, AO Network Clinical Research, AO Foundation
12 University of British Columbia and Vancouver General Hospital, Canada
13 University of Pennsylvania, Philadelphia, United States
14 Carle Foundation Hospital, Urbana, United States
15 Massachusetts General Hospital and Harvard Medical School, Boston, United States
16 NYU Langone Health, New York, United States
17 The Warren Alpert Medical School of Brown University and Rhode Island Hospital and The Miriam Hospital, Providence, United States
18 University of California, San Francisco, United States
19 Mayo Clinic, Rochester, United States
20 Zucker School of Medicine at Hofstra, Long Island Jewish Medical Center and North Shore University Hospital, Northwell Health, New York, United States
Introduction: Metastatic spine disease (MSD) can be associated with significant adverse symptoms, poor prognosis, and increased risk for low health-related quality of life (HRQoL). Gender differences in health-related outcomes are demonstrated in numerous studies, with women experiencing worse outcomes and receiving lower standards of care than men, however, the influence that gender has on HRQoL and clinical outcomes after spine surgery remains unclear. The aim of this study is to describe the effect of gender on HRQoL, clinical outcomes and survival for patients with spinal metastases treated with either surgery and/or radiation. Materials and Methods: Patient demographic data, overall survival, treatment details, perioperative complications, and HRQoL measures including EQ-5D, pain NRS, the short form 36 version 2 (SF-36v2) and the Spine Oncology Study Group Outcomes Questionnaire (SOSGOQ2.0) were extracted from a prospective, multicenter and international cohort study. Patients were stratified by sex, and a separate sensitivity analysis that excluded gender-specific cancers (i.e., breast, prostate, etc.) was performed. Results: The study cohort included 207 female and 183 male patients, with age (mean ± standard deviation [SD] 57.4 ± 10.2 years vs. 60.8 ± 9.8 years, p = 0.001), smoking status (3.6% female smokers vs. 14.9% male smokers; p < 0.001), and site of primary cancer (p < 0.001) being significantly different between the two cohorts (higher representation of gender-specific cancers in females, and kidney cancers in males). After excluding gender-specific cancers (sensitivity analysis), significant differences were found in smoking status (p = 0.022) and site of primary cancer (p = 0.046), with a higher representation of lung cancer in females (36.5%) and kidney cancers in males (30.6%). Both males and females experienced significantly improved SOSGOQ2.0, EQ-5D, and pain NRS scores at all study time points from baseline (p < 0.001). Upon sensitivity analysis, in which patients with gender-specific cancers were removed from the analysis, the significant improvement in SOSGOQ physical, mental, and social subdomains and on SF-36 domains disappeared for females. After sensitivity analysis, males experienced higher rates of postoperative complications (45.1%) as compared to females (36.8%). Kaplan-Meier survival analysis of both the overall cohort and the cohort after sensitivity analysis showed a survival benefit in females after treatment (p = 0.001 and 0.043, respectively). Conclusion: Both males and females experienced significantly improved HRQoL scores after treatment. Female patients showed a survival benefit after treatment and a lower rate of postoperative complication. This study suggests that gender may be a prognostic factor in survival and clinical outcomes for patients undergoing treatment for spine metastases and should be taken into consideration when counseling patients accordingly.
1035
A347: Preoperative Bilsky grade is a predictor of outcomes and ambulation following transpedicular decompression and fusion for metastatic epidural spinal cord compression
Rohit Mauria 1 , Manish Kasliwal 1 , Eric Herring 1 , Adel Azghadi 1 , Mohit Patel 1 , Collin Labak 1 , and Pranav Kumar 2
1 Department of Neurosurgery, University Hospitals Cleveland Medical Center, Cleveland, United States
2 Case Western University School of Medicine, Cleveland, United States
Introduction: Metastatic epidural spinal cord compression (MESCC) occurs in up to 10% of all cancer patients (PMID: 16112300). Many of these patients require large surgeries that carry high morbidity in a population with median survival around 6 months (PMID:7607970, 2311062). The Bilsky score, also referred to as Epidural Spinal Cord Compression (ESCC) score, has been widely used as part of the NOMS framework to guide decision-making for surgical intervention. The purpose of the study is to elucidate postoperative outcomes and ambulation for patients who have undergone transpedicular decompression and fusion to guide patient discussion and surgical decision-making. Methods: A retrospective chart review was conducted of patients from 2014-2022 who underwent decompression and fusion for MESCC. Baseline health and demographic information were collected. Characteristics such as SINS score, pre-and post-operative Bilsky score, and primary tumor type were elucidated. Levels of compression involving the thoracic spine down to the conus were included. Patients who only had laminectomy only, laminectomy and fusion without transpedicular decompression, involvement of cervical spine, and prior spine surgery were excluded. Effect of the variables were each analyzed by univariate analyses using simple logistic regression for dichotomous outcomes or linear regression for continuous outcomes. Effect sizes were summarized by odds ratio (dichotomous outcomes) or beta coefficients (continuous outcomes) and associated 95% confidence intervals (95% confidence interval). Bilsky scores were converted into categories of low grade (0, 1a, 1b, and 1c), moderate grade (2) and high grade (3). Primary outcomes were evaluated according to the following variables: 180- day mortality, non-home disposition, reoperation within 90 days and ECOG performance status at last follow up. Mortality within the first 180 days was the selected outcome due to the 6 month prognostic requirement designated preoperatively in order to be a surgical candidate. Results:A total of 113 patients (ages 19-85) were included in this study. The predominant primary tumors were prostate, lung, breast, colon, and blood dyscrasias. ECOG performance status was recorded at the last documented follow up, with a median interval of 4.54 months. Approximately 8% of the included patients were classified at low grade, 30% were classified as moderate grade, and 62% as high grade. Univariate analysis demonstrated that increasing Bilsky grade was a predictor for non-home disposition (OR 2.55, 95% CI 1.32 - 4.92, p < 0.01), worse ECOG performance status at follow up (beta coefficient 0.54, 95% CI 0.04 - 1.04, p < 0.05), and mortality within the first 180 days following surgery (OR 2.69, 95% CI 1.19 - 6.06, p < 0.05). Non-home disposition (p = 0.001) and 180-day mortality (p < 0.05) remained predictors on multivariate analysis adjusting for age, sex, and BMI. Conclusion: These findings suggest that Bilsky grading, which is used consistently in the treatment of MESCC, is a reliable predictor of discharge to non-home location, 180-day mortality and post-operative ambulation.
923
A348: Perceptions of frailty in spinal metastatic disease: results of an AO spine international survey
Mark Maclean 1 , Miltiadis Georgiopoulos 2 , Raphaële Charest-Morin 3 , C. Rory Goodwin 4 , Niccole Germscheid 5 , and Michael Weber 2
1 Department of Surgery, Dalhousie University, Division of Neurosurgery, Halifax, Canada
2 Spine Surgery Program, McGill University, Department of Surgery, Montreal, Canada
3 Department of Surgery, Spine Surgery Institute, Vancouver General Hospital, Vancouver, Canada
4 Spine Division, Department of Neurosurgery, Duke Unviersity, Durham, United States
5 AO Spine International, Davos, Switzerland
Introduction: Frailty is increasingly recognized among the surgical spine literature for an association with adverse events, mortality, and hospital discharge disposition. Despite this, frailty has not been clearly defined in the context of spinal metastatic disease (SMD). The purpose of this study was to better understand how spinal surgeons conceptualize, define, and assess frailty in the context of SMD. Materials and Methods: The AO Spine Knowledge Forum Tumor conducted an international, self-administered, cross-sectional survey of the AO Spine community. The 33-question survey was developed using a modified Delphi technique. The survey was designed to elucidate preoperative surrogate markers of frailty and relevant postoperative clinical outcomes in the context of SMD, respectively. Responses were ranked using weighted averages. Consensus was defined as ≥ 70% agreement among respondents. A subgroup analysis was performed, stratifying responses based on respondents’ subjective perceived level of knowledge regarding frailty in SMD. Results: Results were analyzed for 312 respondents. Most respondents were orthopedic (61.2%) or neurosurgical spine surgeons (35.6%). Study participants represented 71 countries and 6 geographic regions. Most respondents reported they informally assess frailty and cognition in patients with SMD by forming a general perception based on clinical condition and patient history. Consensus was attained among respondents regarding the association between 14 preoperative clinical variables and frailty. Severe comorbidities, extensive systemic disease burden, and poor performance status were most associated with frailty. Severe comorbidities associated with frailty included high-risk cardio-pulmonary disease, renal failure, liver failure, and malnutrition. The most clinically relevant outcomes were major complications, neurological recovery, and change in performance status. Conclusion: This international study represents an important first step toward defining the multi-dimensional nature of frailty in SMD. Surgeons recognized frailty is important but most commonly evaluate it based on general clinical impression rather than using existing frailty tools. We identified numerous preoperative surrogate markers of frailty and postoperative clinical outcomes that spine surgeons perceived as most relevant in this population. These results may guide the future development of an objective, clinimetrically robust tool for assessing frailty in patients with SMD.
1576
A349: The association between pre-operative nutritional status and survival in patients requiring treatment for spinal metastases
Anne Versteeg 1 , Raphaële Charest-Morin 2 , Ilya Laufer 3 , William Teixeira 4 , Ori Barzilai 5 , Alessandro Gasbarrini 6 , Michael Fehlings 7 , Dean Chou 8 , Michael Johnson 9 , Ziya Gokaslan 10 , Jorrit-Jan Verlaan 11 , Tony Goldschlager 12 , John Shin 13 , John O'Toole 14 , Daniel Sciubba 15 , Chetan Bettegowda 16 , Michelle Clarke 17 , Michael Weber 18 , Addisu Mesfin 19 , Norio Kawahara 20 , C. Rory Goodwin 21 , Alexander Disch 22 , Nicolas Dea 2 , Arjun Sahgal 23 , Laurence Rhines 24 , and Charles Fisher 2
1 Department of Orthopaedics, University of Toronto, Canada
2 Vancouver General Hospital / University of British Columbia, Canada
3 Neurosurgery, New York University Langone Health, United States
4 Spine Surgery Program, Instituto do Câncer do Estado de São Paulo, Brazil
5 Neurosurgery, Memorial Sloan Kettering Cancer Center, United States
6 Orthopaedics, Istituto Ortopedico Rizzoli, Bologna, Italy
7 Neurosurgery, University of Toronto, Canada
8 Department of Neurosurgery, Columbia University, Vancouver, Canada
9 Department of Orthopaedics, University of Mannitoba, Winnipeg, Canada
10 Neurosurgery, Warren Alpert Medical School of Brown University, Providence, United States
11 Department of Orthopaedics, University Medical Center Utrecht, The Netherlands
12 Neurosurgery, Monash Health, Melbourne, Australia
13 Neurosurgery, Massachusetts General Hospital, Harvard University, Boston, United States
14 Neurosurgery, Rush University, Chicago, United States
15 Neurosurgery, Zucker School of Medicine at Hofstra, Long Island Jewish Medical Center and North Shore University Hospital, New York, United States
16 Neurosurgery, John Hopkins University School of Medicine, Baltimora, United States
17 Neurosurgery, Mayo Clinic, Rochester, United States
18 Spine Surgery Program, Montreal General Hospital, McGill University Health Center, Canada
19 Orthopaedics, University of Rochester Medical Center, United States
20 Orthopaedics, Kanazawa Medical University, Uchinada, Japan
21 Neurosurgery, Duke University, Durham, United States
22 University Hospital Carl Gustav Carus at the TU Dresden, Germany
23 Radiation Oncology, University of Toronto, Sunnybrook Health Sciences Centre, Canada
24 Neurosurgery, The University of Texas, MD Anderson Cancer Centre, Houston, United States
Introduction: Malnutrition is common among cancer patients, and has been associated with profound consequences such as increased morbidity, mortality, risk of complications, length of stay and decreased patient reported treatment outcomes. The Patient Generated Subjective Global Assessment (PG-SGA) is a standardized tool for assessing malnutrition in patients with cancer. The aim of this study was to assess the impact of preoperative nutritional status as measured by PG-SGA on survival for patients requiring surgical intervention and/or radiotherapy for spinal metastases. Material and Methods: Patients with spinal metastases who underwent surgery and/or radiation therapy for symptomatic spinal metastatic disease were enrolled in the AO Spine Metastatic Tumor Research and Outcomes Network (MTRON), a prospective international multicenter research registry, between September 2017 and August 2022. The PG-SGA consists of a patient reported section that includes an assessment on weight, weight change, nutritional intake, nutritional symptoms and performance status. The sum of the different assessments results in a numeric score where 0-3 is considered well nourished, 4-8 malnourished, and ≥ 9 severely malnourished. In addition, nutritional status is classified by the physician into three categories: A – well nourished, B – moderately malnourished, and C-severely malnourished. Data regarding demographics, diagnosis, treatment, neurological function, and HRQOL was also evaluated. Results: Of the 1825 patient enrolled in MTRON, 569 patients met the inclusion criteria; 453 underwent surgery ± radiation therapy and 116 were treated with radiotherapy alone. Of these, 348 (61%, PG-SGA score A) were classified by their physician as well-nourished, 155 were moderately malnourished (27%, PG-SGA score B), and 66 were severely malnourished (12%, PG-SGA score C). Based on the numeric score; 237 (42%) were classified as well-nourished, 175 (31%) as malnourished, and 157 (27%) as severely malnourished. Malnourishment based on the pre-treatment PG-SGA numeric and category scores was significantly associated with impaired post-treatment survival (p < 0.01). The median survival for patients in category A was 475 days, 321 days in category B, and 110 days in category C post-treatment. The median survival of patients with a PG-SGA score of 0-3 was 562 days, 318 days for a patient with a score between 4-8, and 238 for a score ≥ 9 post-treatment. Patients who required surgical intervention and were malnourished (PG-SGA C) had a significantly increased risk of mortality (Hazard Ratio 2.7, p < 0.01) as compared to those who were well nourished (PG-SGA A). Conclusion: The prevalence of malnutrition among surgically treated patients with spinal metastases is high. Malnutrition as measured by the PG-SGA demonstrated to be significantly and independently associated with postoperative survival. The PG-SGA is a simple tool to identify spinal metastases patients at risk for early postoperative mortality and it is recommended to be included in the preoperative evaluation of these patients.
990
A350: Medium term follow-up outcomes in palliative posterior transpedicular corpectomy with cement based anterior vertebral reconstruction performed for patients with spinal metastasis
Zhi Wang 1 , Maroun Rizkallah 1 , Sung-Joo Yuh 2 , Daniel Shedid 2 , Jesse Shen 1 , Fidaa Al-Shakfa 3 , Celine Belguendouz 4 , Rayane Kafi 4 , and Ghassan Boubez 1
1 Orthopedic Surgery
2 Neurosurgery Department
3 Centre de Recherche, Centre Hospitalier de l'Universite de Montreal, Montreal, Canada
4 Universite de Montreal, Ecole de Medecine, Montreal, Canada
Introduction: Multiple reconstruction techniques provide anterior column support following posterior transpedicular corpectomy in patients with spine metastasis. Cage reconstruction is known as the gold standard for anterior reconstruction, however cement based mechanical stabilization would offer good structure with reduced cost in these patients with a relatively shorter life expectancy. This is the first paper to assess the medium term outcomes related to cement-based anterior reconstruction after posterior corpectomy in spinal metastasis. Material and Methods: This is a retrospective monocentric study in which consecutive adult patients who underwent posterior spine decompression and fusion with transpedicular corpectomy and cement based anterior reconstruction, with a minimum 6 months follow-up, were included. Ambulatory status and pain analog score were evaluated in all patients at every check-point. Pre-operative and post-operative A/P and lateral spine x-rays were routinely performed and repeated on every follow-up. Local sagittal angle was defined as the sagittal Cobb angle between the lower end-plate of the under-lying vertebra and the upper end-plate of the over-lying vertebra, adjacent to the targeted metastatic level. Results: In total, 142 patients (mean age 62.8 ± 10 years; 49% females) were included, with a mean follow-up of 11.06 months [6-60]. One hundred and fifteen patients (81%) deceased during their follow-up with a mean survival reaching 13.2 months. Sixty-four patients (45%) were ambulatory pre-operatively, whereas 39 patients (27%) were ambulating with assistive device and 39 other patients (27%) were non-ambulant. At the last follow-up, 70 patients (49%) were ambulatory, 52 patients (37%) were ambulating with assistive device and 13 patients (9%) were non-ambulating; p = 0.02. Pain analog scores were reduced from a mean of 8.2 pre-operatively to 4.3 at the latest follow-up; p = 0.003). Mean local sagittal angle went from 19.63⁰ ± 13 post-operatively to 18.86⁰ ± 12.5 at the latest follow-up; p = 0.86. At the last follow-up subsidence of the cement into the adjacent end-plates was observed in 17 patients (12%) whereas 125 patients (88%) maintained their cement in its initial position. No mechanical complications occurred except for a proximal adjacent vertebral fracture that happened in 2 patients (1.4%). No surgical revisions were recorded in this series. Conclusion: This study suggests that the mechanical stability offered by the cement based anterior reconstruction is maintained during the lifespan of patients operated for the spinal metastasis. Satisfying functional and radiological outcomes observed at the last follow-up show this cost sparing, relatively simple reconstruction technique, as a valid alternative for the costly and more complicated cage based reconstruction.
977
A351: 3D printed novel titanium spine rods with lower flexural modulus & stiffness profile with optimised imaging compatibility
Naresh Kumar 1 , Sridharan Alathur Ramakrishnan 1 , Jerry Fuh 2 , Balamurugan Vellayappan 3 , James Hallinan 4 , and Senthil Kumar 2
1 Orthopaedic Surgery
2 Mechanical Engineering
3 Radiation Oncology
4 DDI, National University Health System, Singapore, Singapore
Introduction: Many of the cancer patients (∼10%) develop metastatic spine disease (MSD) at some point of their lifetime. Titanium (Ti6Al4V) is currently the ‘gold standard’ material for spine implants. However, titanium is still not the optimal implant material for use in metastatic spine tumour surgery (MSTS) due to various considerations. Standard solid titanium rods (SSR) have high flexural modulus (110GPa)/stiffness that can lead to stress-shielding and eventually result in delayed implant loosening/construct failure at implant-bone interface. Titanium implants, even though have improved compatibility with CT/MR imaging compared to stainless steel, still generates artefacts, hindering early detection of tumour recurrence and postoperative complications. Artefacts generated by SSR interfere with RT planning/tissue segmentation and dose delivery. New/emerging implant material such as polyether-ether-ketone (PEEK) and carbon-fiber reinforced-PEEK (CFR-PEEK) have been explored for use in MSTS due to their lower modulus of elasticity (∼17GPa). These implants exhibit improved imaging and RT-compatibility. However, rods manufactured using PEEK-based materials are not intraoperatively contourable and are manufactured with pre-determined curvatures and lengths, limiting their operative applications. We aimed to manufacture and test novel design titanium spine rods with lower flexural modulus/stiffness vs SSR using 3D printing technology. Additionally, we also aimed to reduce generation of artefacts during CT and MR imaging observed in SSR. Materials and Methods: Novel spine rod designs with/without internal cellular structures were created using nTopology software (nTopology, Inc. USA). Dimensions of rods included diameter-5.5 mm, shell thickness-0.5 mm and length-100 mm. Rods were designed based finite element analysis (FEA) results. The rods were then 3D printed using selective laser melting method. Three-point bending test was performed to assess mechanical performance of 3D printed rods, while a French bender was used to assess intraoperative rod contourability and haptic feedback was documented. Furthermore, 3D printed spine rods were tested for compatibility and artefact generation (qualitatively assessment) utilising CT & MR imaging. Results: Different spine rod designs generated includes shell, voronoi, gyroid, diamond, weaire-phelan, kelvin, and star. Three-point bending tests showed 3D printed rods had lower flexural modulus with reduction ranging from 2-25% compared to SSR. Shell rods exhibited the highest reduction in flexural modulus of 25% (∼77.4GPa) and star rod exhibited lowest reduction in flexural modulus of 2% (100.8GPa). Gyroid rod exhibited an increase in flexural modulus by 8% (∼111.8GPa). 3D printed rod showed reduction in stiffness ranging from 40-59%. Shell rod displayed highest reduction in stiffness of 59% (179.9N/mm) and gyroid had least reduction in stiffness of 40% (∼259.2N/mm). Haptic feedback rod bending test showed that shell, voronoi, and diamond rods demonstrated lesser difficulty in bending compared to other rods, however, gyroid exhibited bending difficulty similar to SSR. All 3D printed rods demonstrated improved CT and MR imaging compatibility with reduced artefacts vs SSR. Conclusion: By utilising novel design approach, we successfully generated a spine rod design portfolio with lower flexural modulus/stiffness profile and better CT/MR imaging compatibility for potential use in MSTS/other conditions such as osteoporosis. Thus, exploration of new rod designs in surgical application could enhance treatment outcome and improve quality of life for patients.
OP40: Novel Surgical Technologies
79
A352: Mazor X stealth versus O-arm navigation for pedicle screw insertion: preliminary results of the RGNV trial on the first 100 patients
Marc Prod'homme 1 , Grasset Didier 1 , Alain Akiki 2 , Gilles Dietrich 3 , Jonas Müller 2 , and Duccio Boscherini 1
1 Neuro Orthopedic Center, Clinic La Source, Lausanne, Switzerland
2 Orthopedic Surgery, Riviera-Chablais Hospital, Rennaz, Switzerland
3 Orthopedic Surgery, University Hospital of Lausanne, Lausanne, Switzerland
Introduction: Computerized navigation is currently widespreading around the world in spine surgery, aiming to allow more accurate and safe procedures. Since the end of the 20th century, navigation appeared to be superior to traditional free-hand technique to insert pedicle screws. Thus its use is becoming a gold standard in many facilities. Robotic guidance aims to stabilize a robotic arm after surgical planning of screw trajectory. The Mazor X Stealth is a recent device which combines robotic guidance and navigation. The aim of the study was to compare operative and radiologic results and also radiation exposure between the Mazor X Stealth and the O-arm navigation for pedicle screw insertion. Material and Methods: All patients who required pedicle screw insertion for posterior lumbar fusion were prospectively included and divided into two groups: RG when operated with the Mazor X Stealth, and NV when operated with the O-arm and navigation as a control group. Age, operative data such as number of levels operated, number of screws inserted, operative time in minutes (min), estimated blood loss (EBL in milliliters, ml), time to insert screws (in min). Satisfaction of screw positioning was assessed with the Gertzbein-Robbins classification. Dosimetric data of the imaging devices were collected for calculation of the effective dose E (in millisievert, mSv) for the whole procedure according to the International Commission on Radiological Protection using conversion factors. The absolute risk of cancer (AR, in %) equivalent to a whole-body acquisition was also calculated. Intraoperative and postoperative complications were recorded. Results: 100 patients were included, 50 in each group. Mean age was similar: 72 versus 69 in groups RG and NV respectively, p = 0.21. 227 vertebrae were operated: 106 in group RG and 121 in group NV. A total of 438 screws were inserted, 205 in group RG and 233 in group NV. Operative time was similar between the groups, with 161 versus 151 minutes in RG and NV respectively (p = 0.37), as well as EBL (350 versus 454 ml, p = 0.13). Mean time to insert screws was significantly lower in group RG, with 13 minutes versus 18 minutes in group NV, p = 0.03; but time per screw was similar: 3.4 versus 3.8 respectively, p = 0.11. 96.6% screws were satisfactory in group RG versus 98.7% in group NV. Overall E was significantly higher in group RG, with 7.24 and 5.77 mSv in group NV, p < 0.01, as well as AR, with 3.6x10-4% in RG and 2.9x10-4% in NV groups (p < 0.01). Overall complication rate was 26% in the RG group and 36% in the NV group. Conclusion: The Mazor X Stealth showed promising results especially in accuracy of pedicle screw insertion, operative parameters and also complications, but was inferior to the O-arm navigation in terms of radiation exposure.
1025
A353: Micro-ct analysis of Titanium-nanocoated PEEK cages: biomimetic surface topography leads to higher osseointegration in lumbar interbody fusions
Karel Willems 1
1 Orthopedie, AZ Delta Roeselare, Roeselare, Belgium
Introduction: Posterior interbody fusion is frequently used to treat degenerative low back pain. Titanium and PEEK are two of the most popular materials for fusion cages. PEEK is an excellent material, but leads to limited osseointegration. There is a strong correlation between the grade of bony fusion and the clinical results. The observation of faster and more intense bone at the bone-implant interface is a crucial area to achieve definite fusion. Coating PEEK cages with Ti therefore seems to be a good strategy to improve clinical outcome. The standard plasma-spray coating technique leads to a large variation in coating thickness, and makes the combination 30% stiffer than PEEK and less radiolucent. Furthermore, the level of debris due to mechanical wear raises questions on the long-term stability. Not only the type of coating, but also the surface topography plays a crucial role. This research study uses Ti-nanocoated PEEK cages (Orthobion, GmbH). The Ti-nanocoated cages have a specific topography on the macro-, micro- and nanoscale which mimics the bioenvironment (biomimetic surface topography). Macroscopically, the cage surface is 360° nanocoated, including the graft window, effectively enlarging the coated surface area. A specific microtopography is applied for increased bone cell anchorage and adhesion. Additionally, a nanotopography is provided. In this study, we analyze the biomimetic surface topography with the latest µCT-technology and correlate the findings with the radiological results of a clinical trial of the Ti-nanocoated cages. Material and Methods: To analyze the biomimetic surface topography, we use the state-of-the-art Tescan UniTOM HR, which is the only µCT-system to provide submicron spatial resolution and high temporal resolution dynamic CT in a single system. For the blinded randomized radiological study, 81 patients between 18 and 75 years with chronic mechanical low back pain were included: 44 with Ti-nanocoated and 37 with uncoated PEEK cages. Primary radiological outcome parameters were implant stability and fusion status, evaluated by an independent radiologist. Results: The µCT-images clearly demonstrate the existence of microgrooves, allowing the anchorage and adhesion of the bone cells participating in the osseointegration. A detailed image analysis shows that the surface area increases with a factor of 3.71 only thanks to the microtopography. The nano-roughness is also clearly visualized. This increases the surface area for proteins in the osseointegration process. Clinically, 65.6% of patients with uncoated PEEK cages achieved definite fusion one year after the surgery. Significantly more patients with a Ti-nanocoated PEEK cage with biomimetic surface achieved definite fusion: 93.9% (p = 0.0034). Conclusion: The Ti-nanocoated cages with an optimized biomimetic surface topography lead to a higher number of patients with definite fusion. The visualization of the surface enlargement created by the cage design and the Ti-nanocoating explains the better bone-implant interdigitation. A higher osseointegration is indeed a significant predictor of a positive long-term clinical outcome and improved implant longevity.
1040
A354: Microscope assistated minimally invasive anterior submandibular retropharyngeal key-hole approach for C1-C2 pathologies - a new technic
Árpád Viola 1,2 and Dávid Süvegh 1
1 Department of Neurotraumatology, Semmelweis University, Budapest, Hungary
2 Department of Neurosurgery and Neurotraumatology, Dr Manninger Jenő Trauma Center, Budapest, Hungary
Background: Odontoidectomy serves as the resolution of ventral compression of the upper cervical medulla. It can be performed via traditional transoral, endoscopic endonasal, anterior transcervical retropharyngeal, or with a lateral approach. Objectives: Our objective is to introduce a new surgical method that we have used for C1-C2 ventral decompression, the microscope assisted minimally invasive anterior submandibular retropharyngeal key-hole approach (MIS ASR), which – similarly to the traditional anterior retropharyngeal surgery – preserves the hard and soft palates, yet can be performed through a 25 mm wide incision with the use of only one retractor. Materials and Methods: All 12 patients were supine, stabilized in Mayfield headrest. During the MIS ASR approach, we began with a 25 mm wide ventral and submandibular incision, 30-40 mm below the mental protuberance, beginning from the right side and extending 5 mm left towards the midline. The platysma muscle was incised crosswise with a 25 mm wide incision, then access to the spine was achieved by blunt dissection of the mylohyoid muscle, corresponding to its fibers, while retracting the anterior belly of the right digastric muscle laterally. We mobilized the upper portion of the oropharynx cranio-medially to reach the corpus of the C2 vertebra and odontoid process as well as the C1 anterior tubercle and arch. In order to elevate the upper part of the oropharynx, we used one 15 mm wide - 80 mm long carbon retractor. According to the different stages of the surgery, the suction, bipolar diathermy, micro drill and Kerrison Rongeur were positioned in the surgeon’s left and right hand in order to provide adequate retraction of the lateral and medial soft tissue. Results: The most common complications associated with transoral and transnasal odontoidectomy are CSF leakage, velopharyngeal insufficiency, wound dehiscence, pulmonary issues, meningitis and death. The minimally invasive anterior submandibular retropharyngeal key-hole approach we used is a novel method for the decompression of C1, C2 ventral pathologies. From the four presented cases, we cannot come to long term conclusions, but we can state that during the MIS ASR - with the preservation of the hard and soft palates - the risk of velopharyngeal insufficiency associated with the transoral method can be eliminated, as well as the risk of liquor-leakage. The blood-loss is minimal, the patients do not need tracheostomy, and can be started on oral diet within 24 hours after surgery. Conclusions: The novel, microscope assisted minimally invasive anterior submandibular retropharyngeal key-hole approach was feasible for C1-C2 pathologies in our twelve cases: 4 trauma, 3 tumor and 3 rheumatoid arthritis cases.
1452
A355: Implementation of a robotic-assisted system - a prospective comparative evaluation of learning curve and surgery times
Jana Ulrich 1 , Philipp Schenk 2 , Denis Rappert 3 , Götz Achim 3 , Streikus Jonas 3 , Zolotoverkh Oleksandr 3 , Rohde Dirk 3 , and Klaus Schnake 3
1 Trauma and Orthopedic Surgery, Klinikum Nürnberg Süd, Nürnberg, Germany
2 Department of Science and Research, BG Klinikum Bergmannstrost Halle, Halle, Germany
3 Spine Surgery, Waldkrankenhaus Erlangen, Erlangen, Germany
Introduction: Robotic assisted surgery is continuously getting more common in spinal surgery. Many studies have already shown an improvement in the accuracy of pedicle screw placement and a decrease of surgical revisions. Up to now only a few studies exist regarding the learning curve and the time needed for robotic assisted spinal fusions. This prospective and comparative study focussed on the learning curve compared to the standard surgical procedure. Material and Methods: Single-center prospective data collection of all performed spinal fusions, whether standard open (SO) or robotic assisted (RAS, Mazor X Stealth Station, Medtronic), over a period of 10 months. Evaluation of time needed for robotic registration and pedicle screw placement, amount of blood loss, x-ray dose, and complications. Learning curve for the time needed per screw over the performed surgeries was calculated using linear regression in SPSS. Results: 142 non-randomized patients were included of whom 80 (age 63±14 years) underwent RAS surgery and 62 (age 58 ± 21 years, p = 0.131) underwent standard (SO). The average number of implanted screws for SO was 6 ± 4, and for RAS 7 ± 3 (p = 0.470). No differences in blood loss per screw SO 82 ± 60 ml, RAS 97 ± 68 ml could be found (p = 0.174). X-ray dose (cGYm2) per screw was for SO with 168 ± 137 higher as for RAS 108 ± 130 (p = 0.010). There was no sig. difference for time for pedicle screw placement per screw (SO 8.0 ± 4.7 min, RAS 7.5 ± 3.8 min, p = 0.541). Specific complications for robotic surgery were all technical difficulties and occurred in 16% (n = 13). The linear regression showed a significant decrease for time needed for screw placement over time (r = -0.376, p = 0.001). The time per screw in the 1st quarter of surgeries was with 9.0 ± 2.9 min nearly twice as much compared to the time needed in the last quarter (5.5 ± 2.7 min, p = 0.001). In addition, the time for RAS screw placement of the last quarter was significant lower, compared to SO (p = 0.004). Discussion: During the 10-month period using RAS, the learning curve showed reduction for both, time needed for robotic registration and X-ray dose. The blood loss seems comparable. The time for screw placement decreased significantly and finally the screw placement via RAS became faster than for SO. Nevertheless, the time required for patient positioning is still an add-on in the RAS and therefore the incision-suture time is still comparable to the standard open procedure. The higher the number of inserted screws the more advantageous the robotic assisted procedure gets. During the learning period substantial time deviations as well as technical complications must be expected.
1989
A356: Interlaminar fusion stabilization versus pedicle screw instrumentation, a retrospective study of lumbar circumferential fusion
Philip Paschal 1 , Daniel Alicea 1 , Kevin Tang 1 , Celeste Abjornson 1 , and Frank Cammisa 1
1 Spine, Hospital for Special Surgery, New York, United States
Lumbar spinal fusion procedures are commonly performed with an anterior column support utilizing an interbody device and posterior supplemental fixation with pedicle screw instrumentation (PSI) and bone grafting. Although PSI techniques have advanced, there are reports of significant morbidities, decreased lordosis, and limit options if revision surgery is required. Interlaminar fusion devices (ILFD) have been shown to provide similar support to PSI with less morbidity. An ILFD differs from an interspinous device with regards to placement and load transfer. ILFD is a U-shaped device that is fixed to the adjacent spinous processes, with the stabilizing portion lying between the laminae. The implant is designed for one to two level lumbar fusion for patients with degenerative disc disease without significant spondylolisthesis.
The purpose of this study is to compare the clinical outcomes of patients undergoing 1 or 2 level circumferential lumbar fusion supplemented by either ILFD or PSI.
After IRB approval, a single center, retrospective, matched consecutive series study was performed using data from the electronic medical record. Operative reports were utilized to identify patients who underwent a single-level lateral lumbar interbody fusion (LLIF) supplemented with posterior stabilization with ILFD (Cofix®: Surgalign, San Diego, CA) or PSI. 153 patients were categorized into two groups: ILFD (n = 80) or PSI (n = 73). Perioperative outcomes included surgical time and estimated blood loss (EBL). Radiographic assessment of fusion status by disc height, global lordosis, and segmental lordosis occurred postoperatively. Clinical outcomes included patient reported outcomes, narcotic usage, length of stay (LOS), and reoperations. Fusion was assessed as less than 2° of motion. Statistical comparison was performed to confirm pair match population. Statistical regression was performed on all outcome measures.
The patient populations were found to be statistically similar. The average age of ILFD and PSI groups was 56.4 ± 8.4 years and 58.8 ± 11.4 years, respectively. Compared to the ILFD group, the PSI group had more patients who received two-level surgery (57.5% in PSI versus 35% in ILFD). Those who received ILFD had significantly less mean EBL (ILFD: 209.3 ± 122.2 cc, PSI: 329.5 ± 244.6 cc; p < 0.001) and mean procedure time (ILFD: 195.8 ± 84.6 minutes, PSI: 256.6 ± 96.6 minutes; p < 0.001). There were no statistical differences in fusion rate at 6- and 12 months (or ILFD: 90.5% and 92.2%; PSI: 84.1% and 88.9%). Segmental and global lordosis were statistically similar between groups. Kaplan Meier Survivability curve based on reoperation rates favored ILFD to PSI. 2 participants (2.5%) in the ILFD group required a reoperation, compared to 18 (24.7%) in the PSI group. Those who received ILFD were less likely than those who received PSI to use narcotics at 6 months (ILFD: 21.1%, PSI: 50.7%; p < 0.001) and 12 months (ILFD: 9.2%, PSI: 31%; p < 0.001).
ILFD is a minimally invasive option for circumferential fusion that is safe and durable. Compared to PSI, it provides similar restoration of lordosis and fusion stability, and offers greater options for revision and less narcotic use.
1546
A357: Expandable vs. static transforaminal lumbar interbody fusion grafts: a comparison of 1-yyear radiographic parameters and clinical outcomes
Richard Fessler 1
1 Neurosurgery, Rush University Medical Center, Chicago, United States
Background: In response to the increasing incidence of degenerative pathology and growing number of operative candidates, minimally invasive surgical (MIS) approaches to the lumbar spine continue to evolve. In opposition to conventional static thoracolumbar intervertebral fusion (TLIF) cages, expandable cages have gained popularity as they offer an increased axial fusion footprint without compromised rates of osseous fusion through a comparable operative corridor. Objective: To evaluate and compare the radiographic and clinical outcomes between a novel expandable vs. static MIS TLIF cage for the treatment of degenerative disc disease. Study Design: A single center retrospective review of 120 consecutive adult patients undergoing 1 or 2-level MIS TLIF with a novel expandable (Luna 3D, Benvenue Medical Inc., Santa Clara, CA, n = 60) vs. static (UniLIF, Stryker Kalamazoo, MI) was performed. Preoperative and 1-year postoperative radiographic and clinical outcomes were assessed by serial confidential surveys and upright flexion/extension radiographs. Results: A 120 patient (mean 63.3 years, 60.0 % female) who underwent 1 or 2-level MIS TLIF were included. A baseline difference in female participants favored the static vs. expandable cohort (68.3% vs. 51.6%), moreover a difference in segmental lordosis (SL) and lumbar lordosis (LL) were observed (p < 0.05). At 1-year post surgery these radiographic differences were not maintained as the expandable cohort showed relatively unchanged SL and slightly improved LL and the static cohort showed reduced SL and LL (p < 0.05). At 1-year post surgery, significant reduction of spondylolisthesis, restoration of anterior/posterior disc height and foraminal height were observed in the expandable cohort (all p < 0.05). Comparable rates of fusion, 93% and 91% in the expandable vs. static cohort were noted at 1-year. Moreover, significant reduction in NRS back and ODI were observed in both cohorts but more pronounced in the expandable (5.9 ± 2.4 to 2.2 ± 1.9 and 37.3 ± 16.2 to 17.1 ± 15.2) vs. static (6.2 ± 2.8 to 3.2 ± 2.5 and 41.8 ± 16.1 to 24.3 ± 17.5) cohort (p < 0.05). One instance of cage migration requiring reoperation occurred in the expandable cohort. Conclusions: Significant improvement in anterior and posterior disc height, foraminal height, reduction of spondylolisthesis and lumbar lordosis favored the expandable cage cohort. Improved PROs that were observed, which failed to reach statistical significance were likely attributable to limited patient number. Ultimately, these radiographic and clinical outcomes suggest an expandable cage placed through an MIS corridor represents a safe and efficacious alternative to a conventional static cage in those with lumbar degenerative disc disease.
2027
A358: How low can we go? A propensity score matched study on high versus low dose bone morphogenetic protein (BMP) in transforaminal lumbar interbody fusion (TLIF) procedures
Ramkumar Mohan 1 , Andrew Wu Guan Ru 2 , and Reuben Soh 1
1 Orthopaedic Surgery Department, Singapore General Hospital, Singapore
2 National University of Singapore, Singapore
Introduction: We present a study on a direct comparison between low dose (2.1 mg) and high dose (4.2 mg) Bone Morphogenetic Protein (BMP) usage in Transforaminal Lumbar Interbody Fusion (TLIF) cases. Recombinant Human BMP-2was initially found to have strong osteogenic or osteoproliferative signaling properties in initial preclinical studies. Eventually, such benefits were noted in early clinical trials and rhBMP2 was subsequently approved for the use in anterior lumbar fusion cases. From then, its use has grown widely in an ‘off-label’ fashion to various spinal arthrodesis procedures. However, subsequent studies documenting increased adverse effect with the use of BMP has led to discussion on use of low dose BMP and adequate dosing regimen. Our study therefore aims to show that low dose (2.1 mg) BMP usage has similar rates of fusion and recovery with possible improved adverse effect profile. Material and Methods: 216 patients that underwent TLIF procedures from January 2011 to September 2018 in our institution were included into the study. From the years 2011 to 2013 4.2 mg of BMP was used in TLIF procedures in this institution, subsequently, from 2014, 2.1 mg of BMP was used. Demographic, perioperative, follow up and adverse effect data was collected retrospectively for all patients. 172 patients received BMP dose of 4.2 mg while 44 patients received BMP dose of 2.1 mg. Patients were subsequently propensity score matched at a 1:1 ratio (n = 43) and reevaluated. Results: Epidemiological data of all 216 patients were included in total, mean age at surgery was 58.9 years (SD: 11.1). 16 (7.4%) of patients were noted to be osteoporotic and 7 (3.2%) had previous spinal operations. Overall at 6 month mark 158 (74.9%) of patients had fusion noted. In terms of adverse effects there were 9 recorded overall, of which there were 4 cases of subsidence noted, 3 cases of heterotropic ossification and 2 cases of post-operative back or leg pain. When cohorts of high and low dose BMP were directly compared, there were no significant differences noted in terms of fusion at 6 month mark (127 (73.8%) vs 31 (70.5%) p = 0.387) or at the 12 month mark (124 (72.1%) vs 35 (79.5%) p = 0.668). No statistical differences were noted in terms of adverse effects between the 2 cohorts, however trends toward lower adverse effect in low dose cohort was noted with a combined total of 8 out of 9 adverse effects occurring in the high dose cohort. After matching similarly, there were no significant findings in terms of post-operative outcomes or adverse effects noted. Conclusion: Our study suggests that lower dosage of BMP for TLIF procedures provide similar post-operative outcomes of surgery. Though no significant findings were found in terms of adverse effects, based on observed trends, it is possible that with larger cohort data with overall increased number of adverse effects, significant differences may be observed. Follow up studies prospective studies or larger studies are suggested to further corroborate suggested findings.
1967
A359: Poly-ether-ketone-ketone versus titanium interbody cages in patients undergoing anterior cervical discectomy and fusion, a prospective evaluation
Philip Paschal 1 , Celeste Abjornson 1 , Gregory Paschal 1 , Fedan Avrumova 1 , Darren Lebl 1 , and Frank Cammisa 1
1 Spine, Hospital for Special Surgery, New York, United States
Introduction: Titanium implants have been of growing interest in anterior cervical discectomy and fusion (ACDF) procedures. Titanium can be three-dimensionally (3D) printed allowing optimization of surfaces to promote hydrophilicity and bony apposition. However, titanium poses disadvantages, most notably its high elastic modulus, which can cause stress shielding and higher rates of subsidence. PEEK, poly-ether-ether-ketone, has been widely utilized primarily to mitigate this disadvantage with an elastic modulus similar to bone. However, PEEK is hydrophobic, elicits the formation of a biofilm layer and does not allow for bone apposition. A novel material, PEKK, poly-ether-ketone-ketone, can be 3D printed for highly designed surfaces, an elastic modulus similar to bone, and provides a hydrophilic environment for bony on-growth. PEKK aims to merge the advantages of materials such as titanium and PEEK. Aims/Objectives: The purpose of the study is to evaluate the clinical outcomes of a PEKK cage in ACDF procedures compared to a previously used titanium cage. Methods: A prospective, consecutive cohort of 60 patients undergoing primary ACDF surgery with a PEKK interbody cage compared to a matched retrospective cohort of primary ACDF patients with a titanium interbody cage at a single center. All patients met the inclusion/exclusion criteria which included between the ages of 18 and 80 and had not previously undergone cervical surgery. Patient demographic data was collected. Radiographic data was collected pre-operative, immediately post-operative, and at 1 year follow-up. The primary outcomes are rates of fusion and subsidence. Fusion was defined as bridging bone with less than 2° of flexion-extension motion. Subsidence defined as a decrease in disc height of 3 mm from discharge. Additional outcomes that were assessed included pain levels pre- and post-operatively, secondary surgical intervention, and post-op opioid usage. This study was approved by our institutional review board and ethics review panel. Results: The average age was 57.7 ± 10 years in the titanium group and 56.6 ± 11 years in the PEKK group. Among patients who have received PEKK cages, there was an average 28.1% decrease in Visual Analog Scale (VAS)neck scores, and a 31.7% average decrease in VAS arm scores at the 6-month post-operative mark from baseline. There was also a 10.5% decrease in Neck Disability Index (NDI) scores. In the PEKK group, 1-, 2-, and 3-level cases were distributed in 36%, 42%, and 21% of patients, respectively. In the titanium group, 1- 2-, and 3- level cases were distributed in 26%, 42%, and 32% of patients, respectively. Subsidence was more prevalent in the titanium group than the PEKK group. Fusion rates were greater than 90% in both groups and was similar at 6 months and 1 year. No differences were found in secondary interventions or opioid usage. Conclusion: Our preliminary results indicate PEKK cages as a viable alternative to titanium implants in ACDF procedures.With a more similar elastic modulus to bone, PEKK cages exhibited less subsidence than titanium cages.
976
A360: Augmented reality-assisted percutaneous pedicle screw insertion in the cervical vertebrae: a cadaveric proof-of concept study
Miguel Ruiz Cardozo 1 , Som Singh 1 , Karma Barot 1 , Abby Carey-Ewend 1 , Samuel Brehm 1 , Gabriel Trevino Verastegui 1 , Matthew De la Paz 1 , Ahmed Hanafy 1 , Michael Olufawo 1 , Alexander Yahanda 1 , Alexander Perdomo-Pantoja 1 , Julio Jauregui 1 , Magalie Cadieux 1 , Ripul Panchal 2 , Kornelis Poelstra 3 , Timothy F. Witham 4 , and Camilo Molina 1
1 Neurosurgery, Washington University in St. Louis, St. Louis, United States
2 Neurosurgery, American Neurospine Institute, Plano, United States
3 Orthopaedic Surgery, The Robotic Spine Institute of Las Vegas, Las Vegas, United States
4 Neurosurgery, Johns Hopkins University, Baltimore, United States
Introduction: A unique minimally invasive technique called augmented reality-mediated spine surgery (ARMSS) has the potential to improve the effectiveness, precision, and safety of traditional percutaneous pedicle screw insertion techniques. This method eliminates the need for the operator to alter their field of vision or their focus to a distant display by immediately projecting visual 3D spinal anatomy and 2D navigation pictures onto their retina and superimposing them over the surgical field. Previous data from cadaveric studies and in real patients showed the clinical utility of AR for guiding instrumentation of the thoracolumbar spine, however, the technical feasibility of utilizing this technology for the cervical spine is unknown. The objective of this cadaveric study was to assess the accuracy and precision of percutaneous pedicle implant insertion guided by ARMSS. Material and Methods: Instrumentation was placed in 5 cadaveric torsos via ARMSS platform at levels ranging from C3 to C7. Postprocedural CT scans were graded by two independent neuroradiologists using the Gertzbein-Robbins scale (grades A–E) for clinical accuracy. Technical precision was calculated using superimposition analysis employing the Medical Image Interaction Toolkit to yield angular trajectory (°) and linear screw tip (mm) deviation from the virtual pedicle screw position compared with the actual pedicle screw position on postprocedural CT imaging. The positional error was calculated as the difference in the actual screw tip position, derived from the post-op scan and its virtual tip, as recorded by the ARMSS platform. The trajectory error was calculated as the difference in the screw orientation and its recorded virtual trajectory. Results: In total, forty-one (41) cervical screws (C3-C7, Pedicle Screws and Lateral Mass) were positioned in at the 5 cadavers. Each surgeon navigated at least seven (7) screws. Clinical accuracy (Gertzbein-Robbins Scale Grades 0 + Grades1) was found to be 100%. The mean values of tip and trajectory errors were found statistically significantly lower than 3 mm and 30 respectively (p < 0.05). None of the instrumented cervical screws had cortex violation over 2 mm. The 99% upper bound limit for the tip and trajectory error was 2.42 mm and 2.940, respectively. Conclusion: These accuracy results are similar to literature reported accuracy results for cervical screws instrumentation using image-guided navigation systems were inaccuracy was defined as cortical breach, i.e., pedicle violation larger than 2 mm (Grade 2 and above). This demonstrates that pedicle implant insertion via ARMSS is technically feasible, accurate, and highly precise. The performance of the ARMSS in accurate percutaneous placement of screws in C3-C7 cervical vertebrae is comparable to the accuracy results that were reported for the instrumentation of the thoracic and sacro-lumbar vertebrae.


