Abstract
Background
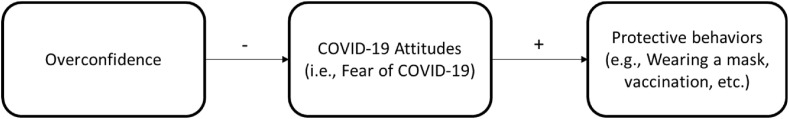
Health education campaigns often aim to create awareness by increasing objective knowledge about pathogens, such as COVID-19. However, the present paper proposes that confidence in one's knowledge more than knowledge is a significant factor that leads to a laxer attitude toward COVID-19 and hence lower support for protective measures and reduced intention to comply with preemptive behaviors.
Methods
We tested two hypotheses in three studies conducted between 2020 and 2022. In Study 1, we assessed participants’ level of knowledge and confidence, as well as attitudes toward COVID-19. In Study 2, we tested the relation between fear of COVID-19 and protective behaviors. In Study 3, we used an experimental approach to show the causal effect of overconfidence on fear of COVID-19. In addition to manipulating overconfidence and measuring fear of COVID-19, we also measured prophylactic behaviors.
Results
In Study 1, more overconfident participants had a laxer attitude toward COVID-19. While knowledge had an increasing effect on worry, confidence in said knowledge significantly decreased worry about COVID-19. In Study 2, participants who were more worried about COVID-19 were more likely to engage in protective behaviors (e.g., wearing masks). In Study 3, we show that when overconfidence was experimentally diminished, fear of COVID-19 increased. The results support our claim that the effect of overconfidence on attitudes toward COVID-19 is causal in nature. Moreover, the results show that people with higher fear of COVID-19 are more likely to wear masks, use hand sanitizers, avoid crowded places or social gatherings, and get vaccinated.
Conclusions
Managing adherence to public health measures is critical when it comes to highly infectious diseases. Our findings suggest that efficient information campaigns to increase adherence to public health measures should focus on calibrating people's confidence in their knowledge about COVID-19 to prevent the spread of the virus.
Keywords: Overconfidence, COVID-19, Health education campaigns, Preventive behaviors, Fear of COVID-19, Health knowledge, Health behavior, Coronavirus
1. Introduction
Official responses to highly transmittable viral outbreaks often involve some form of public health education. Recent examples of such information campaigns include responses to Ebola (Levy et al., 2017), Zika (Wilson and Nguyen, 2017), and COVID-19 (Ahorsu et al., 2020; Bagcchi, 2021; Bonell et al., 2020) outbreaks. These programs aim to increase objective knowledge about a pathogen to change attitudes, and, ultimately, behaviors (Weiss and Tschirhart, 1994). While well-designed information campaigns can be effective in improving public health (Breitbart et al., 2006; Thompson and Harutyunyan, 2006), studies in social psychology (Koriat and Bjork, 2005; Oskamp, 1965), sports (Hall et al., 2007), climate science (Trémolière and Djeriouat, 2021), among several other fields, have shown that confidence in one's knowledge increases faster than knowledge itself, essentially creating an illusion of knowledge. Such unjustified confidence has been shown to significantly influence attitudes and behaviors, sometimes outperforming any positive impacts of objective knowledge (Parker and Stone, 2014). Yet the different impacts of confidence, knowledge, and associated overconfidence (i.e., the excess between confidence and knowledge) on attitudes toward infectious diseases are critically understudied. For instance, are those who objectively know more about, say COVID-19, more fearful than those who think they know more about the virus? How would such fear of the virus affect protective behaviors (e.g., wearing a mask or getting a vaccine) meant to reduce the spread of the disease?
In the context of COVID-19, several studies have investigated the predictors of attitudes toward the virus. For example, older women have been found to have higher fear of COVID-19 than older men (Caycho-Rodríguez et al., 2022). Also, younger Spanish people reported higher levels of fear of the virus than older people (Martínez-Lorca et al., 2020). Notably, previous studies have shown ambivalent effects of COVID-19 knowledge and scientific literacy on attitude (e.g., Lee et al., 2021; Motoki et al., 2021; Zhong et al., 2020). However, while most of the studies are correlational in nature and focus on specific aspects of knowledge (e.g., COVID-19 specific or vaccines), previous research has neglected to consider the role that confidence in that knowledge might play. In this paper, we propose that confidence, more than knowledge, predicts people’ attitudes toward COVID-19.
Previous literature in the health domain provides only partial evidence of a potential relation between overconfidence and attitudes. For example, some studies have explored aspects of overconfidence, such as overestimation and overplacement, in the health context (see Dunning et al., 2004 for a review). Also, there is some evidence that the misperception of one's knowledge of a health threat (e.g., cardiac arrest) is related to lower levels of worry (Radcliffe and Klein, 2002). Moreover, other forms of overconfidence (e.g., being unrealistically optimistic about future outcomes) have been associated with COVID-19-related attitudes and behaviors (Park et al., 2021). However, in addition to a lack of evidence on the impact of confidence and knowledge, these studies did not specifically measure overconfidence. Thus, there is currently no evidence on whether overconfidence in one's knowledge causes overly lax attitudes and failure to carry out preventative behaviors and whether such effects are driven by objective knowledge or confidence in one's knowledge.
The present paper proposes that a false sense of security arising from overconfidence may lead to being less afraid of COVID-19, which, in turn, can inhibit protective health behaviors. A lack of correspondence between performance and confidence judgments, commonly referred to as miscalibration, has a flawed metaknowledge at its core – a false perception about the boundaries of one's knowledge (Piehlmaier, 2022; Russo and Schoemaker, 1992). In the case of overconfidence, this reflects a false sense of superiority, based on subjective feelings of competence (Larrick et al., 2007). The overestimation of knowledge can make individuals feel that their knowledge is sufficient to enable them to navigate a situation safely. However, these perceptions would be necessarily flawed due to the inherent uncertainty of a public health crisis. Information about COVID-19 should be taken with caution as conclusions and results regarding a developing situation, such as the pandemic, are often preliminary and come with a margin of error (Lippi et al., 2020). Therefore, the rational approach should be to appreciate the inherent uncertainty of scientific evidence, especially when distributed through third-party channels, such as media outlets. Yet despite all this, people might still believe they have all the necessary information and relax their attitudes, thinking that they should not care and protect themselves. Furthermore, motivational processes may maintain and exacerbate such overconfidence to reduce worries, enabling more uninhibited behaviors. Thus, we hypothesize that:
H1
Individuals who exhibit overconfidence in their knowledge will demonstrate a laxer attitude toward COVID-19 than individuals who do not exhibit overconfidence in their knowledge.
Throughout the COVID-19 pandemic, news outlets reported on large-scale non-adherence. Illegal “quarantine raves” drawing thousands of attendees were reported all over the world from Greater Manchester (BBC, 2020) to New York (Lipsky, 2021). Non-adherence also extends to top-level policymakers, as indicated by several parties in Downing Street during national lockdowns. However, less sensational disobedience at the individual level (for instance, failing to wear face masks on public transportation) is arguably much more common and problematic from a public health standpoint. Moreover, even in the presence of highly effective vaccines, the World Health Organization (WHO) reiterated that using preventive measures, such as wearing facial masks and social distancing, remain critically important tools to control the current and future outbreaks (WHO, n.d.). Thus, understanding what drives adherence behavior in general, and, more specifically in the case of the COVID-19 pandemic, becomes crucial both for individuals and society at large.
Previous research has documented several drivers of people's compliance behaviors with COVID-19 regulations such as age (Daoust, 2020; Nivette et al., 2021), gender (Galasso et al., 2020), national levels of human development index (Lin et al., 2021), and temporal perception (Sobol et al., 2020). Only a few studies have been focusing on the attitude toward COVID-19 as a key construct to understanding compliance behavior. In particular, fear of Covid has been proposed as one of the key psychological drivers to fight the pandemic (Ahorsu et al., 2020). According to the Protection Motivation Theory (Rogers, 1975), people would seek protection when they experience a potential threat. Moreover, feeling personally at risk of infection has been associated with a greater propensity of engaging in hand washing and social distancing behaviors in the early stages of the pandemic (Wise et al., 2020). Such results are in line with the Health Belief Model (Rosenstock, 1966) and health and risk information-seeking models, such as the Planned Risk Information Seeking Model (Kahlor, 2010), which posit that the perception of personal risk and affective risk responses (e.g., worry and anxiety) are prerequisites of protective and information-seeking behaviors. However, current studies provide only partial evidence of the predictive power of fear of Covid to explain people's likelihood to engage in prophylactic behaviors. For example, previous research shows that individuals with higher fear of COVID-19 were more likely to change their behaviors to protect themselves (Harper et al., 2021). Besides, the study is correlational in nature and provides limited insights into the predictive role of fear of COVID-19 while controlling for other demographic drivers (e.g., gender or age). Thus, we propose that fear of COVID-19 can act as a statistically significant and clinically meaningful predictor of the likelihood of engaging in preventive behaviors such that when people are afraid of COVID-19, they are more likely to engage in protective behaviors. Thus, we hypothesize that:
H2
Individuals with a more negative attitude (i.e., higher fear) toward COVID-19 have a greater likelihood of engaging in protective behaviors.
A summary of our theoretical model is illustrated in Fig. 1 below.
Fig. 1.
Conceptual model.
2. Method
We conducted three studies to test the effect of overconfidence on attitude toward COVID-19 and preventive behaviors. We conducted the first two studies between August 2020 and October 2021 using Amazon's Mechanical Turk (MTurk), an online participant pool commonly employed for data collection in experimental and cross-sectional research (Goodman and Paolacci, 2017), including on vaccinations (e.g., Acar-Burkay and Cristian, 2022) and COVID-19 research (Latkin et al., 2021). The sample of Study 1 was composed of mostly U.S. residents. Instead, the sample from Study 2 was composed of only U.S. residents. We conducted the third study with U.S. residents in September 2022 on Prolific, an alternative pool that research has shown to produce high-quality data on different measures, including attention, honesty, comprehension, and reliability (Peer et al., 2022; Srichan et al., 2020). The combined usage of MTurk and Prolific entails higher demographic diversity and a greater degree of external validity, compared to other online-based convenience samples (Moss et al., 2020). All respondents were paid $1 in exchange for their participation in our short (∼5 min) surveys. The three studies were preregistered and received ethical approval from the University of Sussex Business School before data collection. All participants in the studies were 18 years or older. All instruments, data, statistical code, and output logs are publicly available as part of the preregistration (OSF link).
To determine our target sample size, we conducted an a priori power analysis using G*Power (version 3.1.9.4). Due to the lack of previous research explicitly using our measure of attitude in Study 1, we define our effect size by what other papers have been showing with similar dependent variables. For example, according to Srichan et al. (2020), one could infer a medium effect size. Thus, we set a conservative type I and II error rate both to 0.50, and aimed to detect f2 = 0.15, with 8 predictors, concluding a target sample size of N ≥ 160. In Study 2 and 3, following existing literature (e.g., Clark et al., 2020; Mertens et al., 2020; Nivette et al., 2021), we set an effect size respectively of f2 = 0.12 and 0.07, concluding a target sample size of N ≥ 198 and 333.
3. Study 1: General overconfidence and COVID-19 attitudes
The aim of study 1 was to explore if overconfidence in one's general knowledge is connected to a laxer attitude toward COVID-19 during the first wave of the virus.
3.1. Participants
In August 2020, we recruited 260 participants on MTurk with the following characteristics: 40% female, mean age 34.74 (SD = 9.96, range = 18–67), 80% held at least a bachelor's degree, 61% married, 81% full-time employed, 22% working in the healthcare sector, and 34% living with a healthcare worker. Given the nature of MTurk samples, there were no missing observations.
3.2. Measures
Our key dependent variable was COVID-19 attitudes, measured on a 5-point Likert scale, ranging from strongly disagree (1) to strongly agree (5). At the time of data collection, there was no established scale to measure attitude toward COVID-19. Consequently, we measured attitude with 12 items based on previous literature (Cowling et al., 2020; Srichan et al., 2020; Zhong et al., 2020). Higher scores in the aggregated variable, ranging from 22 to 60 (M = 42.1, SD = 7.57), can be interpreted as higher concern toward COVID-19. Some examples of items are: “I worry about COVID-19”, or “I should avoid taking public transportation because of COVID-19”. Fifty percent of the items were reverse-coded. The reliability score of the scale was good (α = 0.8). All instruments and raw data can be found in the preregistration (OSF link).
To measure overconfidence (M = 9.36, SD = 22.12, min = −41.29, max = 66.42), we computed a differential score between average confidence and average accuracy. Accuracy was measured by the percentage of correct answers to 24 questions in three alternatives forced choice format (Ronay et al., 2017a, 2017b). Confidence was measured by 24 sliders, ranging from not at all confident (0) to completely confident (100). Finally, we measured mental age, biological age, gender, ethnicity, education, household income, marital status, occupational status, and country of residence.
3.3. Procedure
After the information sheet and the consent form, participants answered 24 general knowledge questions (e.g., Q: “What is inflamed when one has gingivitis?“, A: “Gum tissue, toe tissue, eye tissue”). Under each question, participants were also asked to indicate the level of confidence they had in their answer being correct, ranging from 0 (displayed as “not confident at all”) to 100 (displayed as “completely confident”). After completing the questionnaire, participants answered the aforementioned battery of questions about their attitude toward COVID-19. Finally, participants reported their demographic information.
3.4. Analyses
The primary analyses rely on hierarchical ordinary least squares (OLS) estimates with heteroskedasticity-robust standard errors to assess the impact of overconfidence on COVID-19 concerns. A robustness check was carried out, separating subjective and objective knowledge to assess whether unwarranted confidence or general knowledge drives any detectable association. Changes in effect sizes between the nested baseline model, using only demographics as predictors, and the full models that includes overconfidence or confidence and knowledge, separately, were tested using Wald tests (Chou and Bentler, 1990).
3.5. Results
The results (column (1) in Table 1 ) show a negative relation between overconfidence and COVID-19 concerns (p < 0.001). This suggests that people who are excessively confident in their knowledge have a laxer attitude toward COVID-19. Apart from the primary variable of interest (i.e., overconfidence), participants with higher educational attainment (p < 0.05) and those living with a healthcare worker in their household (p < 0.001) seem less concerned about COVID-19.
Table 1.
Study 1 hierarchical OLS regressions on the association between attitude toward COVID-19 (C19) and overconfidence in One's general knowledge.
| (1) |
(2) |
|
|---|---|---|
| C19 Attitude w/Overconfidence | C19 Attitude Robustness Check | |
| General overconfidence | −0.08*** (0.02) | |
| Confidence | −0.06* (0.03) | |
| General knowledge | 0.11*** (0.03) | |
| Age | 0.08 (0.04) | 0.07 (0.04) |
| Female | 1.48 (0.87) | 1.43 (0.87) |
| Full-time employed | 1.65 (1.28) | 1.71 (1.28) |
| University degree | −2.87* (1.34) | −2.98* (1.34) |
| Married | −1.29 (1.09) | −1.37 (1.09) |
| Living alone | −0.20 (1.20) | −0.11 (1.20) |
| Living w/healthcare worker | −5.02*** (1.10) | −4.97*** (1.11) |
| Healthcare worker | 0.68 (1.10) | 0.54 (1.11) |
| Ethnic/racial minority | −0.16 (0.86) | −0.36 (0.86) |
| Constant | 42.96*** (2.07) | 40.54*** (2.87) |
| Observations | 260 | 260 |
| R-squared | 0.28 | 0.28 |
| ΔR-squared | 0.05*** | 0.05*** |
Note: Columns (1) and (2) are hierarchical models. Changes in R-squared are in comparison to the nested model (i.e., block 1, only including demographics) in Supplementary Table 2 in the Web Appendix. P-values of these changes are based on Wald tests. Negative coefficients indicate a laxer attitude toward C19 in August 2020. Overconfidence in column (1) was defined as the difference between confidence (in %) and accuracy (in %) in 24 general knowledge questions and 24 associated confidence sliders. The robustness check is based on Parker and Stone (2014) and assesses confidence and knowledge separately. Robust standard errors in parentheses. ***p < 0.001, **p < 0.01, *p < 0.05.
A moderately strong effect size of 0.28 indicates that the model may hold practical implications. Furthermore, a statistically significant 5% increase in effect size from the nested to the full model suggests that overconfidence substantially improves the goodness of fit. A post hoc power analysis performed using G*Power (version 3.1.9.4), with the observed effect size, α = 0.05, and N = 260 shows that our study was sufficiently powered to detect the predicted effect (power = 1.00).
However, the results could be challenged. For instance, one may argue that knowledge and confidence in said knowledge are two fundamentally different constructs. In this case, creating a single indicator (i.e., overconfidence), combining the two, may lead to inaccurate associations. The following subsection checks the robustness of the presented results by disentangling confidence and knowledge.
3.6. Robustness check
To assess the individual association between confidence, general knowledge, and attitude toward COVID-19, a second hierarchical OLS regression was fitted. Following Parker and Stone (2014), the robustness check sheds light on what their paper calls unjustifiable confidence. That is, a statistically significant confidence coefficient after controlling for knowledge. Column (2) in Table 1 shows that while higher general knowledge is affiliated with greater concern over COVID-19, the opposite effect can be observed for confidence in one's general knowledge. All other coefficients remain virtually unchanged. The robustness check illustrates an almost identical effect size and changes in R2, compared to the previous model. In summary, study 1 provides preliminary evidence in favor of our hypothesis that individuals who exhibit overconfidence in their knowledge demonstrate a laxer attitude toward COVID-19 (H1). This effect seems to be driven by confidence in one's knowledge because explicit knowledge leads to the opposite effect on COVID-19 attitudes. In the following study, we assess whether a laxer attitude translates into less stringent prophylactic behaviors.
4. Study 2: Fear of COVID-19 and prophylactic behaviors
The aim of study 2 was to assess whether a laxer attitude toward COVID-19, specifically fear of COVID-19, is connected to less stringent preventive behaviors, in particular mask wearing and propensity to get vaccinated.
4.1. Participants
In October 2021, we recruited 199 U.S. participants on MTurk with the following characteristics: 41% female, mean age 38.21 (SD = 10.87, range = 19–73), 68.39% held at least a bachelor's degree, 63.21% married, median household income $50,000–$59,999, and 27.89% working in the healthcare sector. Three participants preferred not to say whether they were healthcare workers, and one person did not reveal their vaccination status.
4.2. Measures
Our key dependent variables were the likelihood of wearing masks, measured on a 5-point Likert scale, ranging from extremely unlikely (1) to extremely likely (5), and a binary indicator for a participant's COVID-19 vaccination status.
Our key independent variable was attitude toward COVID-19, measured on an established 5-point Likert scale, ranging from strongly disagree (1) to strongly agree (5). The scale was first proposed by Ahorsu et al. (2020) and contains items such as “It makes me uncomfortable to think about COVID-19”, and “I cannot sleep because I'm worrying about getting COVID-19.” The reliability score for the scale was good (α = 0.94). The scale has been used numerous times in previous literature and it has been validated across multiple countries (Martínez-Lorca et al., 2020; Reznik et al., 2021). Scales in Studies 1 and 2 share similar items such as “I worry about COVID-19”. However, the scale used in Study 2 specifically focused on fear of COVID-19.
4.3. Procedure
After the information sheet and the consent form, participants answered a series of COVID-19-related questions. Participants then reported their likelihood of wearing masks and their COVID-19 vaccination status. Finally, participants answered common demographic questions. Following previous literature (e.g., Ali et al., 2021; Hall et al., 2022), we included also income as a potential predictor of fear of COVID-19 due to socioeconomic implications of lockdown and social distancing measures. All materials can be found in the preregistration (OSF link).
4.4. Analyses
In accordance with study 1, we performed a hierarchical OLS regression for mask wearing and a hierarchical generalized linear model, using a logit link and odds ratios, for vaccination status. All models were fitted with heteroskedasticity-robust standard errors.
4.5. Results
The results show that fear of COVID-19 is a significant predictor of the likelihood of wearing a mask (p < 0.01, column (1) in Table 2 ). Moreover, greater fear of the virus is associated with a more than 50% higher likelihood of having been vaccinated against COVID-19 per one unit increase in fear in October 2021 (column (3)). Apart from the main independent variable, only higher educational attainment and marital status show significant main effects. Namely, those who held at least a bachelor's degree had triple the odds of having been vaccinated against the virus (p < 0.01) and married participants were significantly less likely to wear masks (p < 0.05). A modest effect size in model (1) indicates limited goodness of fit. That said, a 7% increase in R2 from the nested to the full model suggests that fear of COVID-19 substantially increases the predictive power of the model. In contrast, the generalized linear model predicting vaccination status exhibits a moderately strong effect size with a statistically significant but comparably small increase of 3% from the nested to the full model.
Table 2.
Study 2 hierarchical regressions for the relation between fear of COVID-19 and prophylactic behaviors.
| (1) |
(2) |
|
|---|---|---|
| Mask Wearing | Vaccination | |
| Fear of COVID-19 | 0.32** (0.10) | 1.69* (1.08–2.65) |
| Age | −0.01 (0.01) | 1.03 (0.99–1.07) |
| Female | −0.13 (0.17) | 0.52 (0.23–1.18) |
| Household income | 0.05 (0.03) | 1.11 (0.95–1.29) |
| Bachelor or higher | 0.04 (0.19) | 3.10** (1.36–7.08) |
| Married | −0.45* (0.21) | 0.78 (0.31–1.97) |
| Ethnic/racial minority | −0.28 (0.21) | 0.50 (0.18–1.40) |
| Healthcare worker | −0.31 (0.17) | 4.59 (0.89–23.69) |
| Constant | 3.71*** (0.53) | 0.17 (0.02–1.57) |
| Observations | 196 | 195 |
| R-squared | 0.11 | 0.21 |
| ΔR-squared | 0.07** | 0.03* |
Note: Model (1) is a hieratical OLS regression with robust standard errors in parentheses and (2) is a hierarchical logistic regression with odds ratios, robust standard errors, and 95% confidence intervals in parentheses. Changes in R-squared are in comparison to the nested models (i.e., block 1, only including demographics) in Supplementary Table 4 in the Web Appendix. P-values of these changes are based on Wald tests. R-squared and its changes in (2) refer to Nagelkerke's (1991) pseudo R-squared. Fear of COVID-19 is based on Ahorsu et al. (2020). ***p < 0.001, **p < 0.01, *p < 0.05.
Two post hoc power analyses performed using G*Power (version 3.1.9.4), with the observed effect sizes, α = 0.05, and N = 196 confirmed that our study was sufficiently powered to detect the predicted effects (powermask_wearing = 0.94; powervaccine = 0.99).
In Study 2, we show that fear of COVID-19 is a consistent and statistically significant predictor for preventive behaviors which have the potential to reduce the spread of the virus (e.g., wearing masks and getting vaccinated). The variable consistently improves the predictability of the models. While studies 1 and 2 show correlational evidence of the relation between overconfidence, attitudes (e.g., fear of COVID-19), and downstream behaviors of a laxer attitude toward the virus, Study 3 aims to shed light on the causal link between these variables.
5. Study 3: Within-subjects experimental design
Study 3 served three purposes. First, we explored whether overconfidence in COVID-19-related knowledge differs in effect and significance from overconfidence in one's general knowledge (study 1). Second, we aimed to test for the causal relation between overconfidence and fear of COVID-19. Third, we included additional items for protective behaviors to examine the role of fear of COVID-19 as a predictor in different domains of public health.
5.1. Participants
In September 2022, we recruited 408 U.S. participants on Prolific with the following characteristics: 47% female, 76% fully vaccinated, mean age 40.32 (SD = 14.91, range = 18–85), 81% held at least a bachelor's degree, median household income $50,000–$59,999, 36% married, 28% self-identified as non-white/not Caucasian, and 8% working in the healthcare sector. Five participants did not provide consent and had to be removed.
5.2. Measures
Mirroring study 2, we measured fear of Covid on a 5-point Likert scale (Ahorsu et al., 2020). The reliability score was good (α = 0.91). Moreover, in line with study 2, to measure protective behaviors against COVID-19, participants reported the likelihood of wearing masks in crowded indoor spaces and their binary COVID-19 vaccination status. In addition, participants also reported the likelihood of using hand sanitizer while outdoors, avoiding crowded places, and attending social gatherings (Takahashi et al., 2022) on a 5-point Likert scale, ranging from extremely unlikely (1) to extremely likely (5). The addition of the other measures aims at generalizing the effect of fear of COVID-19 on other protective behaviors that are relevant for reducing the spread of the virus (Catching et al., 2021).
To manipulate overconfidence, participants were randomly assigned to two different within-subjects experimental groups. In the first group, participants (n = 201) answered 10 general knowledge questions that were unrelated to COVID-19 (e.g., “If it's noon in Boston, what time is it New York?“) and indicated their level of confidence in the accuracy of their answers on sliders, ranging from not at all confident (0) to completely confident (100), essentially replicating the main element of study 1. In the second group, participants (n = 202) answered 10 questions about COVID-19 (e.g., “How many vaccine doses of COVID-19 have been administered around the world so far?“) and indicated their level of confidence in the correctness of their answers on sliders identical to those in the first group. The second arm aimed to test for causality. In both arms, participants were informed that one in ten will be selected to be rewarded with a bonus payment based on the number of correct answers to all quiz questions in this survey to ensure incentive-conform behavior. All quiz questions were in a forced-choice format.
After completing the task, all participants wrote a reflection piece on their experience in answering the survey (Q: “How would you describe your user experience with this survey?“) in one or two sentences (minimum 80 characters). This allowed participants in the second arm with COVID-19 questions to reflect on their virus-specific knowledge. Previous research suggests that the task can calibrate participants' confidence through an increase in metaknowledge (Piehlmaier, 2022). No such effect was expected from the general knowledge questions in the first group since they were unrelated to the subsequent block. All participants then replied to a series of 10 COVID-19 questions (e.g., Q: “When was the Covid pandemic officially declared?“, A: “February 27, 2020, March 11, 2020, April 13, 2020”) and 10 associated confidence sliders. Following previous literature on the domain-specific effect on confidence (Muthukrishna et al., 2014), we expect that participants’ overconfidence would be affected only in the group that answered the questions about COVID-19 both times (before and after). Instead, the group that answered general knowledge questions first and COVID-19 questions afterward would have no reason to reassess their confidence as the two blocks were unrelated. Finally, we measured age, gender, ethnicity, education, household income, marital status, and occupation (healthcare worker or not).
5.3. Procedure
After the information sheet and the consent form, participants were randomly assigned to one of the two within-subjects arms. Once participants completed the 10 questions with their 10 confidence sliders, they wrote a reflection piece on their experience with the survey and answered another set of questions related to COVID-19. Then, participants reported their fear of COVID-19 and their likelihood of engaging in preventive behaviors. Finally, participants provided common demographics. All instruments, raw data, statistical code, and output logs can be found in the preregistration (OSF link).
5.4. Analyses
All participants passed the attention checks. Eight participants were overrecruited, five of whom did not consent to participate and had to be removed. Consequently, we conducted our analysis with a sample of 403 people. Of those, four preferred not to say whether they were healthcare workers, 11 did not provide information on their vaccination status, and five participants selected a gender other than female or male. Following study 1, we computed overconfidence as the difference between average confidence and average knowledge. That is, the number of correct answers to the quiz questions per block and arm. There was no statistically significant difference in post-manipulation overconfidence between the arms (p = 0.42). Therefore, we focused on the COVID-19 questions arm to test for causal selection. First, we conducted a manipulation check by running a two-tailed paired t-test (i.e., within-subjects design) for the difference in confidence between pre- and post-manipulation (i.e., before and after the written reflection task). Mirroring the statistical approach taken in studies 1 and 2, the primary analyses rely on hierarchical (generalized) linear regressions with heteroskedasticity-robust standard errors to assess the impact of overconfidence on fear of COVID-19. We run the models both for the pre-post-difference in overconfidence as well as confidence and knowledge, separately. Moreover, we conducted an additional analysis using the same procedure to investigate the effect of fear of COVID-19 on prophylactic behaviors across all participants.
5.5. Results
5.5.1. Overconfidence and fear of COVID-19
To demonstrate that our manipulation was effective, we expected a significant difference in confidence, but not in knowledge, before and after the writing task, such that the writing task would calibrate participants' confidence in their knowledge of COVID-19. Indeed, a paired t-test shows that participants were more confident before the writing task (M = 0.82, SD = 0.11) than after (M = 0.71, SD = 0.13). The decrease in confidence (M diff = - 0.11, 95% CI [0.09, 0.12]) was highly statistically significant (t = 17.19, df = 201, p < 0.001). Actual knowledge scores, on the other hand, did not statistically differ between the two experimental groups (i.e., those who were tested on COVID-19 specific questions vs. those who were tested on random questions). Using a two-parameter item response theory (IRT) model to ensure that the level of difficulty of the two quizzes or similarity between items does not bias the results (Nguyen et al., 2014), we are able to show that participants’ latent knowledge remains virtually unchanged throughout the experiment (difference: M = 0.00, SD = 1.05, t = 0.00, df = 201, p > 0.99).
To test the causal effect of overconfidence on fear of COVID-19, we continued our analysis by regressing pre- and post-manipulation overconfidence on fear of COVID-19 (Table 3 ). The results show that a higher level of overconfidence led to lower fear of COVID-19 (p < 0.05) before participants reflected on their experience answering COVID-19-related questions (column (1) in Table 3). However, after the reflection had decreased participants’ confidence in their COVID-19 knowledge, there was no longer a statistically significant effect (p = 0.85) on fear of COVID-19 (column (2)). Apart from these causal effects, ethnic or racial minorities can be associated with greater fear of the virus (p < 0.05). As expected, the effect sizes pre- and post-manipulation are small. More importantly, overconfidence only significantly increases predictability of the model pre-manipulation (1) but is statistically no different to the nested model after participants were calibrated by the reflection task (2).
Table 3.
Study 3 hierarchical OLS regressions to estimate the causal effect of overconfidence on fear of COVID-19.
| (1) |
(2) |
(3) |
|
|---|---|---|---|
| Pre-Treatment Fear | Post-Treatment Fear | Robustness Check | |
| Overconfidence | −0.98* (0.49) | −0.08 (0.39) | |
| Confidence | −0.01† (0.01) | ||
| Knowledge | 0.86† (0.52) | ||
| Age | −0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) |
| Female | 0.15 (0.14) | 0.23 (0.13) | 0.14 (0.14) |
| Household income | −0.02 (0.02) | −0.01 (0.02) | −0.02 (0.02) |
| Bachelor or higher | −0.06 (0.13) | −0.07 (0.13) | −0.05 (0.13) |
| Married | 0.04 (0.15) | 0.02 (0.15) | 0.06 (0.15) |
| Ethnic/racial minority | 0.34* (0.17) | 0.33* (0.17) | 0.34* (0.16) |
| Healthcare Worker | −0.07 (0.22) | −0.14 (0.22) | −0.06 (0.22) |
| Constant | 2.15*** (0.26) | 2.08*** (0.27) | 2.49*** (0.57) |
| Observations | 199 | 199 | 199 |
| R-squared | 0.07 | 0.05 | 0.07 |
| ΔR-squared | 0.02* | 0.00 | 0.02 |
Note: All models use fear of COVID-19 as the dependent variable. Model (1) is based on overconfidence in 10 COVID-19 quiz questions before any experimental manipulation (i.e., reflection task). Model (2) is based on another set of 10 COVID-19 quiz questions after the reflection task. Model (3) is based on pre-reflection knowledge and confidence about 10 COVID-19 quiz questions. Changes in R-squared are in comparison to the nested model (i.e., block 1, only including demographics) in Supplementary Table 6 in the Web Appendix. P-values of these changes are based on Wald tests. Robust standard errors in parentheses. ***p < 0.001, **p < 0.01, *p < 0.05, †p < 0.10.
Similarly, the robustness check using confidence and knowledge as the main independent variables shows that while confidence in one's COVID-19 knowledge reduces fear of COVID-19, knowledge seems to have the opposite effect (column (3)). While fully in line with the robustness check in study 1, the main results in column (3) do not reach the traditional 5% critical value (p = 0.069 for confidence and p = 0.097 for knowledge). Taken together, the results reject the notion of causal selection that would drive the results. Instead, it shows that overconfidence leads to a laxer attitude toward COVID-19, not the other way around.
5.5.2. Fear of COVID-19 and prophylactic behaviors
Fear of COVID-19 is a highly significant predictor of all the preventive behaviors we tested for in this study (Table 4 ). People with greater fear of COVID-19 were more likely to wear a mask (column (2), b = 0.66, p < 0.001), use hand sanitizer (column (3), b = 0.43, p < 0.001), and avoid crowded places (column (4), b = 0.56, p < 0.001). Moreover, people with greater fear of COVID-19 are significantly less likely to attend social gatherings (column (5), b = 0.45, p < 0.001). Apart from the results of these four hierarchical regressions, a hierarchical logistic regression using robust standard errors and odds ratios (column (1)) shows that fear of COVID-19 significantly increases the odds of getting fully vaccinated by 1.74 for every one-point increase in fear (p < 0.01).
Table 4.
Study 3 hierarchical regressions for the relation between fear of COVID-19 and various preventive behaviors.
| (1) |
(2) |
(3) |
(4) |
(5) |
|
|---|---|---|---|---|---|
| COVID-19 Vaccine | Mask Wearing | Use Hand Sanitizer | Avoid Crowded Places | Avoid Social Gatherings | |
| Fear of COVID-19 | 1.74** (1.23–2.46) |
0.66*** (0.07) |
0.43*** (0.07) |
0.56*** (0.07) |
0.45*** (0.08) |
| Age | 1.00 (0.99–1.02) |
0.02*** (0.00) |
−0.01 (0.00) |
0.02*** (0.00) |
0.02** (0.00) |
| Female | 0.84 (0.51–1.40) |
0.34* (0.13) |
0.27* (0.13) |
0.13 (0.12) |
0.02 (0.13) |
| Household income | 1.10* (1.02–1.19) |
−0.03 (0.02) |
−0.01 (0.02) |
−0.04* (0.02) |
−0.06** (0.02) |
| Bachelor or higher | 1.43 (0.87–2.35) |
0.09 (0.14) |
−0.10 (0.14) |
−0.02 (0.13) |
−0.23 (0.13) |
| Married | 1.08 (0.63–1.86) |
−0.14 (0.14) |
0.13 (0.14) |
−0.19 (0.14) |
−0.29* (0.14) |
| Ethnic/racial minority | 1.58 (0.86–2.89) |
0.41** (0.14) |
0.39** (0.14) |
0.18 (0.14) |
0.07 (0.15) |
| Healthcare Worker | 1.95 (0.63–6.08) |
0.37 (0.23) |
0.24 (0.25) |
−0.04 (0.24) |
−0.45* (0.22) |
| Constant | 0.37 (0.12–1.17) |
1.16*** (0.29) |
2.84*** (0.29) |
1.90*** (0.28) |
1.83*** (0.30) |
| Observations | 386 | 394 | 394 | 394 | 394 |
| R-squared | 0.06 | 0.23 | 0.13 | 0.20 | 0.17 |
| ΔR-squared | 0.03** | 0.15*** | 0.08*** | 0.14*** | 0.08*** |
Note: Model (1) is a hierarchical logistic regression with odds ratios, robust standard errors, and 95% confidence intervals in parentheses. Models (2)–(5) are hierarchical OLS regressions with robust standard errors in parentheses. Changes in R-squared are in comparison to the nested models (i.e., block 1, only including demographics) in Supplementary Table 7 in the Web Appendix. P-values of these changes are based on Wald tests. R-squared and its changes in (1) refer to Nagelkerke's (1991) pseudo R-squared. Both within-subjects groups were used. ***p < 0.001, **p < 0.01, *p < 0.05.
The results further suggest that older people are more likely to adopt preventive behaviors than their younger peers. However, this excludes hand sanitizer usage and COVID-19 vaccination. Contrasting study 2, there was no significant difference among people working for the healthcare services nor among people with different education levels in terms of their likelihood of adopting prophylactic behaviors. Moreover, people with higher income were more likely to be vaccinated, but less likely to avoid crowded places and social gatherings. Finally, ethnic or racial minorities and female participants exhibited a greater tendency to wear masks and use hand sanitizer.
Effect sizes for all models illustrate a significant increase, compared to the nested models. In fact, the moderately strong effect sizes in models (2) and (4) increase by 15% and 14%, respectively, once fear of COVID-19 is included in the regressions. Post hoc power analyses performed G*Power (version 3.1.9.4), with the observed effect sizes, α = 0.05, and N = 386/394 (depending on the model) confirmed that our study was sufficiently powered to detect the predicted effects (powervaccine = 0.94; powermask_wearing = 1.00; powerhand_sanitizer = 1.00; poweravoiding_crowds = 1.00; powersocial_gatherings = 1.00).
In summary, study 3 shows that overconfidence causally decreases fear of COVID-19 which, in turn, decreases prophylactic behaviors, such as mask wearing, hand sanitizing, and the odds of getting fully vaccinated. The within-subjects experiment also suggests that the underlying questions that were used to measure overconfidence (i.e., general knowledge or COVID-19-related) do not change the reported effect on laxer COVID-19 attitudes.
6. Discussion
The current paper aimed to investigate whether overconfidence in one's knowledge is related to a laxer attitude toward COVID-19, and how such attitudes ultimately affect protective behaviors. To test our hypotheses, we conducted three studies. In study 1, the findings show that a higher level of overconfidence in general is associated with a laxer attitude toward COVID-19. These findings are in line with previous studies suggesting that other forms of overconfidence (for instance optimism bias) are related to lower levels of concern toward COVID-19 (Park et al., 2021) and other health issues (Radcliffe and Klein, 2002). In study 2, we show that attitude toward COVID-19 is linked to a higher likelihood of engaging in protective behaviors, such as wearing a mask and getting vaccinated. Finally, in experimental Study 3, we show that the effect of overconfidence on fear of Covid is causal. Indeed, the findings show that participants were less likely to fear COVID-19 before they have been asked to reflect on their knowledge of the virus. After the reflection, the effect of overconfidence on fear of the virus becomes insignificant. The robustness checks show that the effect is driven by a decrease in confidence rather than any changes in objective knowledge. Moreover, in the study, we show that a less fearful attitude toward COVID-19 leads to less engagement in protective behaviors, from wearing masks to attending social gatherings and getting vaccinated.
Across our studies, we also show a number of main effects of demographic distributions on the likelihood of engaging in protective behaviors. For example, replicating findings from previous literature (Stoler et al., 2022), in study 2, we show that people with higher education were more likely to get vaccinated in the early stages of the vaccination campaign. Moreover, in study 3, the findings extend previous literature (Bearth et al., 2021) by suggesting that older people are more likely to engage in protective behaviors than their younger peers.
Overall, the study provides important implications for both theory and practice. From a theoretical perspective, the current paper extends existing findings showing that attitude toward COVID-19 is an important driver of adherence behavior (e.g., Ahorsu et al., 2020; Harper et al., 2021). Although excessive fear of Covid can negatively impact one's wellbeing (Satici et al., 2022), previous studies have shown that appropriate situational fear can encourage people to avoid threats and adopt self-preservatory behaviors (Rogers, 1975). We show that fear of Covid is a strong predictor in different stages of the pandemic (i.e., between 2020 and 2022) of several protective behaviors which range from wearing masks to getting vaccinated.
Moreover, given the importance of attitude as a predictor of protective behaviors, the study also contributes to a better understanding of what can influence people's attitude toward COVID-19. While previous studies have focused on objective knowledge with inconclusive findings (e.g., Lee et al., 2021; Srichan et al., 2020), we show that confidence in knowledge is a key predictor when it comes to attitude toward COVID-19. Importantly, confidence and objective knowledge have conflicting effects on attitude. That is, while higher knowledge leads to higher fear of Covid, higher confidence in one's knowledge leads to a laxer attitude.
The paper offers also important insights for policymakers and public health officials who design health education campaigns to encourage citizens to adopt protective behaviors. Since the beginning of the pandemic, governments across the world have implemented a wide range of interventions to promote adherence to protective behaviors (e.g., wearing masks or keeping social distance) or incentivize vaccination (WHO, n.d.). Many of these campaigns (see HHS, 2022 for a recent example) have included educational elements devoted to improving citizens' knowledge of the contagiousness of the virus. Our studies show that while such campaigns might increase objective knowledge, they may also come with an unintended increase in confidence which, in turn, leads to laxer attitude toward COVID-19. Thus, based on our findings, more effective campaigns to reduce the spread of COVID-19 should be based on messages which challenge the confidence in one's knowledge more than knowledge itself. For instance, health education programs can challenge people's preconceptions of the virus rather than simply pointing out facts. Moreover, by creating campaigns around calibrated confidence, policymakers and public health officials can ultimately affect people's fear of Covid to induce more responsible behaviors in order to control the spread of the virus.
6.1. Limitations
While methodological issues have been raised within each study, some more general limitations ought to be acknowledged. First, a limitation of our findings is related to the lack of behavioral measures in the operationalization of the main protective indicators. Indeed, in all three studies, we measure self-reported attitudes and intentions. Future studies might address this aspect by using national electronic health records instead of comparably small survey samples. Second, it is worth acknowledging that while crowdsourcing platforms, such as MTurk and Prolific, are heavily used in social science research (Hauser et al., 2022), they remain convenience samples with limited representativeness. Future studies could replicate aspects of the presented studies using nationally representative samples across various populations. Moreover, future studies may also want to investigate the role of overestimating one's knowledge in preventing everyday health issues. Indeed, overconfidence may lead to a false sense of security and increase the likelihood of taking risks with potential negative consequences in diseases, such as heart attacks, diabetes, or sexually transmitted infections. Furthermore, pilot information campaigns aimed at calibrating people's confidence in their knowledge should be tested for a host of infectious diseases, including HIV and Ebola. Finally, exploring the root causes of overconfidence in one's health knowledge are beyond the scope of this paper. Prior studies suggested that, among other possible explanations, a lack of metaknowledge or correlation neglect may drive such overconfident believes (Ortoleva and Snowberg, 2015; Piehlmaier, 2022). Future studies could use these explanations as a starting point to explore the origin of health-related overconfidence.
7. Conclusion
This paper is the first to causally investigate overconfidence in knowledge and attitude toward the virus. It illustrates how excessive confidence in one's knowledge leads to a laxer attitude toward COVID-19 which negatively influences tendencies to protect oneself and others from COVID-19. We hope that our study of overestimating one's knowledge might lay the foundation for future research in this area.
Acknowledgements
Piehlmaier acknowledges funding from the British Academy (SRG2021\211013). The authors would like to thank Daniela-Carmen Cristian for her helpful comments on an earlier version of this paper.
Handling Editor: M Hagger
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2023.116000.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
The data are freely available as indicated in the manuscript.
References
- Acar-Burkay S., Cristian D.-C. Cognitive underpinnings of COVID-19 vaccine hesitancy. Soc. Sci. Med. 2022;301 doi: 10.1016/j.socscimed.2022.114911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addiction. 2020 doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali M., Uddin Z., Banik P.C., Hegazy F.A., Zaman S., Ambia A.S.M., Siddique MdK.B., Islam R., Khanam F., Bahalul S.M., Sharker M.A., Hossain Fma, Ahsan G.U. Knowledge, attitude, practice, and fear of COVID-19: an online-based cross-cultural study. Int. J. Ment. Health Addiction. 2021 doi: 10.1007/s11469-021-00638-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagcchi S. The world's largest COVID-19 vaccination campaign. Lancet Infect. Dis. 2021;21:323. doi: 10.1016/S1473-3099(21)00081-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC . BBC News; 2020. Greater Manchester Illegal Raves: “Almost Impossible” to Stop. [Google Scholar]
- Bearth A., Luchsinger L., Siegrist M. Reactions of older Swiss adults to the COVID-19 pandemic: a longitudinal survey on the acceptance of and adherence to public health measures. Soc. Sci. Med. 2021;280 doi: 10.1016/j.socscimed.2021.114039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonell C., Michie S., Reicher S., West R., Bear L., Yardley L., Curtis V., Amlôt R., Rubin G.J. Harnessing behavioural science in public health campaigns to maintain ‘social distancing’ in response to the COVID-19 pandemic: key principles. J. Epidemiol. Community Health. 2020;74:617–619. doi: 10.1136/jech-2020-214290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitbart E.W., Greinert R., Volkmer B. vol. 92. International Commission on Non-ionizing Radiation Protection; Munich, Germany: 2006. Effectiveness of information campaigns. Progress in Biophysics and Molecular Biology, UV exposure guidance: a balanced approach between health risks and health benefits of UV and Vitamin D; pp. 167–172. (Proceedings of an International Workshop). 17-18 October, 2005. [DOI] [PubMed] [Google Scholar]
- Catching A., Capponi S., Yeh M.T., Bianco S., Andino R. Examining the interplay between face mask usage, asymptomatic transmission, and social distancing on the spread of COVID-19. Sci. Rep. 2021;11 doi: 10.1038/s41598-021-94960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caycho-Rodríguez T., Tomás J.M., Barboza-Palomino M., Ventura-León J., Gallegos M., Reyes-Bossio M., Vilca L.W. Assessment of fear of COVID-19 in older adults: validation of the fear of COVID-19 scale. Int. J. Ment. Health Addiction. 2022;20:1231–1245. doi: 10.1007/s11469-020-00438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou C.-P., Bentler P.M. Model modification in covariance structure modeling: a comparison among likelihood ratio, Lagrange multiplier, and Wald tests. Multivariate Behav. Res. 1990;25:115–136. doi: 10.1207/s15327906mbr2501_13. [DOI] [PubMed] [Google Scholar]
- Clark C., Davila A., Regis M., Kraus S. Predictors of COVID-19 voluntary compliance behaviors: an international investigation. Global Transitions. 2020;2:76–82. doi: 10.1016/j.glt.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling B.J., Ali S.T., Ng T.W., Tsang T.K., Li J.C., Fong M.W., Liao Q., Kwan M.Y., Lee S.L., Chiu S.S. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daoust J.-F. Elderly people and responses to COVID-19 in 27 Countries. PLoS One. 2020;15 doi: 10.1371/journal.pone.0235590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunning D., Heath C., Suls J.M. Flawed self-assessment: implications for health, education, and the workplace. Psychol. Sci. Publ. Interest. 2004;5:69–106. doi: 10.1111/j.1529-1006.2004.00018.x. [DOI] [PubMed] [Google Scholar]
- Galasso V., Pons V., Profeta P., Becher M., Brouard S., Foucault M. Gender differences in COVID-19 attitudes and behavior: panel evidence from eight countries. Proc. Natl. Acad. Sci. USA. 2020;117:27285–27291. doi: 10.1073/pnas.2012520117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman J.K., Paolacci G. Crowdsourcing consumer research. J. Consum. Res. 2017;44:196–210. [Google Scholar]
- Hall C.C., Ariss L., Todorov A. The illusion of knowledge: when more information reduces accuracy and increases confidence. Organ. Behav. Hum. Decis. Process. 2007;103:277–290. doi: 10.1016/j.obhdp.2007.01.003. [DOI] [Google Scholar]
- Hall L.R., Sanchez K., da Graca B., Bennett M.M., Powers M., Warren A.M. Income differences and COVID-19: impact on daily life and mental health. Popul. Health Manag. 2022;25:384–391. doi: 10.1089/pop.2021.0214. [DOI] [PubMed] [Google Scholar]
- Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addiction. 2021;19:1875–1888. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser D.J., Moss A.J., Rosenzweig C., Jaffe S.N., Robinson J., Litman L. Evaluating CloudResearch’s Approved Group as a solution for problematic data quality on MTurk. Behavior Research Methods. 2022. pp. 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HHS . 2022. Facts about COVID-19 and the Vaccines.https://wecandothis.hhs.gov/resource/facts-about-covid-19-and-the-vaccines [WWW Document]. WECANDOTHIS.HHS.GOV. URL. [Google Scholar]
- Kahlor L. PRISM: a planned risk information seeking model. Health Commun. 2010;25:345–356. doi: 10.1080/10410231003775172. [DOI] [PubMed] [Google Scholar]
- Koriat A., Bjork R.A. Illusions of competence in monitoring one's knowledge during study. J. Exp. Psychol. Learn. Mem. Cognit. 2005;31:187–194. doi: 10.1037/0278-7393.31.2.187. [DOI] [PubMed] [Google Scholar]
- Larrick R.P., Burson K.A., Soll J.B. Social comparison and confidence: when thinking you’re better than average predicts overconfidence (and when it does not) Organ. Behav. Hum. Decis. Process. 2007;102:76–94. [Google Scholar]
- Latkin C.A., Dayton L., Yi G., Konstantopoulos A., Boodram B. Trust in a COVID-19 vaccine in the US: a social-ecological perspective. Soc. Sci. Med. 2021;270(1982) doi: 10.1016/j.socscimed.2021.113684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M., Kang B.-A., You M. Knowledge, attitudes, and practices (KAP) toward COVID-19: a cross-sectional study in South Korea. BMC Publ. Health. 2021;21:295. doi: 10.1186/s12889-021-10285-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B., Edholm C., Gaoue O., Kaondera-Shava R., Kgosimore M., Lenhart S., Lephodisa B., Lungu E., Marijani T., Nyabadza F. Modeling the role of public health education in Ebola virus disease outbreaks in Sudan. Infectious Disease Modelling. 2017;2:323–340. doi: 10.1016/j.idm.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin T., Harris E.A., Heemskerk A., Van Bavel J.J., Ebner N.C. A multi-national test on self-reported compliance with COVID-19 public health measures: the role of individual age and gender demographics and countries' developmental status. Soc. Sci. Med. 2021;286 doi: 10.1016/j.socscimed.2021.114335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi G., Simundic A.-M., Plebani M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID-19) Clin. Chem. Lab. Med. 2020;58:1070–1076. doi: 10.1515/cclm-2020-0285. [DOI] [PubMed] [Google Scholar]
- Lipsky J. 2021. How the Illegal Rave Scene Thrives during the Pandemic - the New York Times.https://www.nytimes.com/2021/03/19/nyregion/illegal-dance-parties-covid-nyc.html [WWW Document]. URL. [Google Scholar]
- Martínez-Lorca M., Martínez-Lorca A., Criado-Álvarez J.J., Armesilla M.D.C., Latorre J.M. The fear of COVID-19 scale: validation in Spanish university students. Psychiatr. Res. 2020;293 doi: 10.1016/j.psychres.2020.113350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens G., Gerritsen L., Duijndam S., Salemink E., Engelhard I.M. Fear of the coronavirus (COVID-19): predictors in an online study conducted in March 2020. J. Anxiety Disord. 2020;74 doi: 10.1016/j.janxdis.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss A.J., Rosenzweig C., Robinson J., Litman L. Demographic stability on Mechanical Turk despite COVID-19. Trends Cognit. Sci. 2020;24:678–680. doi: 10.1016/j.tics.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motoki K., Saito T., Takano Y. 2021. Scientific Literacy Linked to Attitudes toward COVID-19 Vaccinations: A Pre-registered Study. [Google Scholar]
- Muthukrishna M., Heine S.J., Toyakawa W., Hamamura T., Kameda T., Henrich J. Manuscript submitted for publication; 2014. Overconfidence Is Universal? Depends what You Mean. [Google Scholar]
- Nagelkerke N.J.D. A note on a general definition of the coefficient of determination. Biometrika. 1991;78:691–692. doi: 10.2307/2337038. [DOI] [Google Scholar]
- Nguyen T.H., Han H.-R., Kim M.T., Chan K.S. An introduction to item response theory for patient-reported outcome measurement. Patient. 2014;7:23–35. doi: 10.1007/s40271-013-0041-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nivette A., Ribeaud D., Murray A., Steinhoff A., Bechtiger L., Hepp U., Shanahan L., Eisner M. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: insights from a longitudinal cohort study. Soc. Sci. Med. 2021;268 doi: 10.1016/j.socscimed.2020.113370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortoleva P., Snowberg E. Overconfidence in political behavior. Am. Econ. Rev. 2015;105:504–535. doi: 10.1257/aer.20130921. [DOI] [Google Scholar]
- Oskamp S. Overconfidence in case-study judgments. J. Consult. Psychol. 1965;29:261–265. doi: 10.1037/h0022125. [DOI] [PubMed] [Google Scholar]
- Park T., Ju I., Ohs J.E., Hinsley A. Optimistic bias and preventive behavioral engagement in the context of COVID-19. Res. Soc. Adm. Pharm. 2021;17:1859–1866. doi: 10.1016/j.sapharm.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker A.M., Stone E.R. Identifying the effects of unjustified confidence versus overconfidence: lessons learned from two analytic methods. J. Behav. Decis. Making. 2014;27:134–145. doi: 10.1002/bdm.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peer E., Rothschild D., Gordon A., Evernden Z., Damer E. Data quality of platforms and panels for online behavioral research. Behav. Res. Methods. 2022;54:1643–1662. doi: 10.3758/s13428-021-01694-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piehlmaier D.M. The one-man show: the effect of joint decision-making on investor overconfidence. Journal of Consumer Research ucac054. 2022 doi: 10.1093/jcr/ucac054. [DOI] [Google Scholar]
- Radcliffe N.M., Klein W.M. Dispositional, unrealistic, and comparative optimism: differential relations with the knowledge and processing of risk information and beliefs about personal risk. Pers. Soc. Psychol. Bull. 2002;28:836–846. [Google Scholar]
- Reznik A., Gritsenko V., Konstantinov V., Khamenka N., Isralowitz R. COVID-19 fear in eastern europe: validation of the fear of COVID-19 scale. Int. J. Ment. Health Addiction. 2021;19:1903–1908. doi: 10.1007/s11469-020-00283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers R.W. A protection motivation theory of fear appeals and attitude change. J. Psychol. 1975;91:93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Ronay R., Oostrom J.K., Lehmann-Willenbrock N., Van Vugt M. Pride before the fall:(Over) confidence predicts escalation of public commitment. J. Exp. Soc. Psychol. 2017;69:13–22. [Google Scholar]
- Ronay R., Tybur J.M., van Huijstee D., Morssinkhof M. Embodied power, testosterone, and overconfidence as a causal pathway to risk-taking. Comprehensive Results in Social Psychology. 2017;2:28–43. [Google Scholar]
- Rosenstock I.M. Why people use health services. Milbank Mem. Fund. Q. 1966;44:94–127. [PubMed] [Google Scholar]
- Russo J.E., Schoemaker P.J. Managing overconfidence. Sloan Manag. Rev. 1992;33:7–17. [Google Scholar]
- Satici B., Saricali M., Satici S.A., Griffiths M.D. Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Int. J. Ment. Health Addiction. 2022;20:2731–2742. doi: 10.1007/s11469-020-00305-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobol M., Blachnio A., Przepiorka A. Time of pandemic: temporal perspectives related to compliance with public health regulations concerning the COVID-19 pandemic. Soc. Sci. Med. 2020;265 doi: 10.1016/j.socscimed.2020.113408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srichan P., Apidechkul T., Tamornpark R., Yeemard F., Khunthason S., Kitchanapaiboon S., Wongnuch P., Wongphaet A., Upala P. Knowledge, attitudes and preparedness to respond to COVID-19 among the border population of northern Thailand in the early period of the pandemic: a crosssectional study. WHO South-East Asia journal of public health. 2020;9:118–125. doi: 10.4103/2224-3151.294305. [DOI] [PubMed] [Google Scholar]
- Stoler J., Klofstad C.A., Enders A.M., Uscinski J.E. Sociopolitical and psychological correlates of COVID-19 vaccine hesitancy in the United States during summer 2021. Soc. Sci. Med. 2022;306 doi: 10.1016/j.socscimed.2022.115112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi S., Yamada S., Sasaki S., Takahashi N., Nohara M., Kawachi I. A high level of vaccine knowledge increases people's behavioral risks for contracting COVID-19 in Japan. Soc. Sci. Med. 2022;310 doi: 10.1016/j.socscimed.2022.115256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson M.E., Harutyunyan T.L. Contraceptive practices in Armenia: panel evaluation of an information-education-communication campaign. Soc. Sci. Med. 2006;63:2770–2783. doi: 10.1016/j.socscimed.2006.07.026. [DOI] [PubMed] [Google Scholar]
- Trémolière B., Djeriouat H. Exploring the roles of analytic cognitive style, climate science literacy, illusion of knowledge, and political orientation in climate change skepticism. J. Environ. Psychol. 2021;74 doi: 10.1016/j.jenvp.2021.101561. [DOI] [Google Scholar]
- Weiss J.A., Tschirhart M. Public information campaigns as policy instruments. J. Pol. Anal. Manag. 1994;13:82–119. doi: 10.2307/3325092. [DOI] [Google Scholar]
- Who n.d. Strengthening the health system response to. https://www.who.int/europe/tools-and-toolkits/strengthening-the-health-system-response-to-covid-19 COVID-19 [WWW Document]. URL.
- Wilson A., Nguyen T. The Zika virus epidemic: public health roles for nurses. Online J. Issues Nurs. 2017;22 doi: 10.3912/OJIN.Vol22No01Man04. [DOI] [PubMed] [Google Scholar]
- Wise T., Zbozinek T.D., Michelini G., Hagan C.C., Mobbs D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. Royal Society open science. 2020;7(9):200742. doi: 10.1098/rsos.200742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong B.-L., Luo W., Li H.-M., Zhang Q.-Q., Liu X.-G., Li W.-T., Li Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int. J. Biol. Sci. 2020;16:1745. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are freely available as indicated in the manuscript.