Abstract
Introduction:
Our research assessed associations between stigma-related variables and medical care ratings among clients with HIV in HIV Prevention Trials Network (HPTN) 078 who were men who have sex with men (MSM).
Methods:
Logistic regression explored care ratings, stigma, socio-demographics (N = 637). Qualitative thematic coding and themes explored stigmatizing experiences in different settings (N = 111).
Results:
Whites were twice as likely as African-Americans to report high care ratings (P < .05). Clients who reported familial exclusion due to having sex with men were 40% less likely to report high medical care ratings (P < .05). Clients who agreed healthcare providers think people with HIV “sleep around” were half as likely to report high care ratings (P < .08). Stigmatization included “treating me like they’ll catch HIV from my hand,” and care avoidance so others didn’t “know I was having sex with men”.
Conclusions:
Providers can promote African American MSM client retention with more affirming healthcare provision, namely minimizing assumptions and addressing identities and client needs beyond just HIV care.
Keywords: LGBT health, health disparities, healthcare utilization, HIV/AIDS, African Americans, men who have sex with men
African Americans comprise half of all new HIV diagnoses but 12% of the United States (US) population.1-3 HIV prevalence rates among African Americans are higher than all other races, and this inequity is particularly striking among men who have sex with men (MSM). Socioeconomic marginalization among African Americans with HIV is higher than other racial/ethnic groups, resulting in insurance inequities,4,5 lower access to healthcare,6,7 and higher HIV complication rates.8,9 The “Ending the HIV Epidemic” Plan set forth by the US Department of Health and Human Services calls for sustained viral suppression of 90% of clients with HIV by 2030. 10 Achieving this goal requires greater understanding of the needs of African American MSM, given that only half achieve sustained viral suppression after being engaged in care.11,12
Beyond access to care inequities due to socioeconomic factors,4-7 African American MSM may also experience lower quality of care in living with HIV or being MSM, and/or provider/healthcare-level stigmatization of African American race, HIV seropositivity, and/or sexual identity. All of these forms of stigma, including the experience of multiple forms of stigma, are associated with poorer care satisfaction.12-16 Previous research shows similar associations between sexuality disclosure, medical mistrust, and care satisfaction, whereby societal stigmatization of African American MSM may increase avoidance of HIV preventive healthcare prior to HIV diagnosis, and is associated with delays in care partially due to internalized HIV stigma after diagnosis. 17
While research has called for multilevel stigma reduction, existing interventions often only address HIV stigma and tend to track individual client-level outcomes like viral non-suppression. Neglecting the contribution of multiple stigmatized identities reduces the likelihood of intervention effectiveness among the individuals who are most in need of these efforts.8,12,14-16,18-21 HIV stigma reduction interventions often do not engage healthcare staff like front desk workers, who may unknowingly stigmatize clients even before clinical encounters.8,12,14-16,18-21 Although some healthcare providers are trained to provide affirming HIV care for clients identifying as MSM, research suggests most healthcare centers lack standardized protocols for clients living with HIV and/or MSM clients,22-25 which could include procedures for (a) how to handle discrepancies between identification cards and name/physical presentation of clients who are transgender; (b) documentation of preferred pronouns and emergency contacts who are not next of kin; and/or (c) minimum required referrals and affirming language for provision of social service needs other than HIV such as housing assistance, and/or sliding scale mental health resources. These are needs that are often great needs in this population and impacts their ability to remain in care. This is particularly problematic when, as mentioned, stigmatization can occur anytime during the care experience (ie, with the process of registration and enrollment, the physical care environment, and/or in interactions with providers including having needs other than HIV minimized) yet most interventions do not address all of these components and do not adequately assess how this deterred clients from care.19-24,26 Best practices for stigma reduction in healthcare settings are still urgently needed, as African American MSM living with HIV face poorer quality care, lower healthcare satisfaction, and higher rates of viral non-suppression even when insured and enrolled in care.21-26
Methods
The present research utilized qualitative and quantitative data from HIV Prevention Trials Network (HPTN) 078, entitled: “Enhancing Recruitment, Linkage to Care and Treatment for HIV-Infected MSM in the United States” and ran from 2014 to 2019.27,28 HPTN 078 assessed the ability of: (a) deep-chain respondent-driven sampling to reach HIV-infected MSM who are not virally non-suppressed; and (b) a case management-focused intervention to promote viral suppression compared to standard of care.27,28 Study site locations corresponded to regions of high HIV prevalence among African American MSM: Baltimore, Boston, Atlanta, and Birmingham.27,28 All individuals were consented for screening procedures, which include the provision of written consent, contact information, completion of several questionnaires including the baseline survey, and samples collected for laboratory assessments. Participants then completed written consent for study enrollment which included randomization to a study treatment arm, and participation in exit interviews at the completion of the study. Quantitative data were from baseline surveys completed by all screened participants, who were virally non-suppressed at enrollment. Qualitative data were from exit interviews with participants who completed the study. Therefore, qualitative participants are a subset of the larger baseline sample. All study activities were fully approved by the Protection of Human Subjects Committee, which is FHI 360’s Institutional Review Board.
Purpose
We explored stigma and medical care ratings among HIV Prevention Trials Network (HPTN) 078 participants, an enhanced linkage-to-care management intervention among MSM in 4 US sites. 27 Aims were to: (a) examine HIV stigma- and sociodemographic-related factors as correlates of medical care ratings; and (b) describe lived experiences of multiple stigmatized identities (e.g., multilevel stigma).
Measures
Quantitative survey
Dependent variable
The outcome was, “What number would you use to rate the medical care you received for your HIV in the past 12 months?” (where 0 = “Low/Worst” and 10 = “High/Best.”) Since 54% of responses reported 10 out of 10, all other responses were dichotomized as less than high/best (0 = “Lower 0 to 9”vs 1 = “High 10 out of 10.”). Beyond dichotomizing data at the median which is a data-driven approach, the decision to distinguish care as 10/10 compared to anything else is theoretically driven. African Americans, not only those living with HIV, should be equally as likely as White Americans to access and receive healthcare they would rate this highly, yet they are not.12-16,18 Therefore, we theorized anything less than this ideal (10/10) as an unfavorable outcome.
Independent variables
Variables consisted of socio-demographic factors and multilevel stigma.
Socio-demographics
Participants were asked to identify race where 0 = African American/Black, 1 = White, and 2 = Other. Education was assessed where 0 = Up to high school education; 1 = Some college/vocational/trade/tech school; and 2 = Associate degree or higher. Sexual orientation was asked via “Do you identify as?” where 0 = Gay/homosexual, 1 = Bisexual, 2 = Other. Employment status was coded as 0 = Unemployment, 1 = Part-time, and 2 = Full-time. Marital status was categorized as 0 = Single/divorced/widowed, 1 = Married/civil union/legal partnership/having a main partner.
Multilevel stigma
Variables were: (a) Interpersonal/social stigma: “People blame me for having HIV,” “I have been excluded from family gatherings because I have HIV (yes/no),” and “I have been verbally harassed because I have sex with men (yes/no)” (b) Individual-level internalized HIV stigma: “People treat me as less than human now that I have HIV”; and (c) Provider/healthcare-level stigma: “Medical providers assume people with HIV sleep around.” Response categories for all variables were Likert responses and were collapsed where 0 = Strongly disagree/Disagree, 1 = Neither agree nor disagree, and 2 = Agree/Strongly agree. Items were adapted from Herek et al. 29
Qualitative Exit Interviews Guide
Between March 2018 and January 2019, 1-h phone interviews were conducted with HPTN 078 participants who enrolled in the study (N = 111 of 144) after completion of their 12-month study visit. While these individuals also completed the quantitative baseline surveys for screening, this study sample consists only of individuals who enrolled in and completed the study. Interviews explored experiences with: (a) linkage to care; (b) HIV medication attitudes and adherence; (c) HIV care clinic staff interactions including experiences of stigma; and (d) self-identified health status. Due to preliminary study data suggesting that HIV and syphilis co-infection rates were high among study participants, questions about seeking treatment for sexually transmitted infections was added to the latter half of interviews.
Data Analyses
Quantitative analyses
Descriptive frequencies were generated on the total sample using the baseline survey (N = 657 screened at baseline who were MSM and living with HIV). 30 Variables marginally significant (P < .08) at the bivariate (unadjusted) level were entered into a multiple logistic regression model; sensitivity analyses were conducted to assess models with a dichotomous outcome versus a categorical outcome. Variables included in the final model are the only ones shown in Table 2. Robust standard errors were used to account for non-heterogenous data dispersion. 28 Education, employment status, age, and marital status were retained as control variables in the final model since they are all known confounders. Acceptable model fit was assessed via goodness-of-fit tests for all models (P > .05) 31 Marginal effects were then calculated to show predicted probabilities of high medical care ratings as related to stigma-related variables, by averaging over the other variables based on their distribution in the data. 32 Analyses were run in STATA Version 13.0. 33
Table 2.
Correlates of Having Rated Health Care 10 Out of 10 (high) Among Men Who Have Sex With Men (MSM) in HIV Prevention Trials Network (HPTN 078; N = 538).
| Unadjusted adjusted | ||||
|---|---|---|---|---|
| UOR a | CI | AOR b | CI c | |
| Sociodemographics | 1.01 ǂ | (1.00, 1.03) | 1.00 | (0.99, 1.02) |
| Age (continuous) | ||||
| Race | ||||
| White | 1.31 | (0.84, 2.05) | 1.83 * | (1.07, 3.16) |
| Other | 1.65 | (0.86, 3.14) | 1.78 | |
| Ref: African American | 1.00 | 1.00 | (0.85, 3.75) | |
| Education | ||||
| Tech/Some college/Associate’s | 0.84 | (0.59, 1.21) | 0.80 | (0.52, 1.21) |
| Bachelor’s degree or more | 0.95 | (0.63, 1.42) | 0.84 | (0.52, 1.37) |
| Ref: <8th grade/Some HS | 1.00 | 1.00 | ||
| Sexual orientation | ||||
| Bisexual | 1.21 | (0.84, 1.75) | 1.22 | (0.77, 1.95) |
| Ref: Homosexual | 1.00 | 1.00 | ||
| Employment status | ||||
| Part-time employment | 1.40 | (0.70, 1.65) | 1.05 | (0.56, 2.00) |
| Full-time employment | 1.08 | (0.79, 2.50) | 0.78 | (0.46, 1.31) |
| Ref: Unemployment | 1.00 | 1.00 | ||
| Marital status | ||||
| Have a main partner/Married | 1.26 | (0.83, 1.91) | 1.00 | (0.63, 1.58) |
| Ref: Single/divorced/Widowed | 1.00 | 1.00 | ||
| Interpersonal/social stigma | ||||
| Harassed in public due to sex with men | ||||
| Yes | 0.62 ** | (0.45, 0.84) | 0.67 * | (0.45, 0.98) |
| Ref: No | 1.00 | 1.00 | ||
| Excluded by family due to sex with men | ||||
| Yes | 0.54 *** | (0.37, 0.78) | 0.60 * | (0.39, 0.93) |
| Ref: No | 1.00 | 1.00 | ||
| Individual-level internalized stigma | ||||
| People blame me for having HIV | ||||
| Neither agree nor disagree | 0.62 * | (0.41, 0.94) | 0.83 | (0.50, 1.36) |
| Agree/strongly agree | 0.57 ** | (0.38, 0.85) | 0.72 | (0.43, 1.19) |
| Ref: Strongly disagree/disagree | 1.00 | 1.00 | ||
| People think less of me due to HIV | ||||
| Neither agree nor disagree | 0.60* | (0.40, 0.90) | 1.04 | (0.61, 1.77) |
| Strongly agree/agree | 0.84 | (0.54, 1.29) | 1.68 ǂ | (0.94, 3.00) |
| Ref: Strongly disagree/disagree | 1.00 | 1.00 | ||
| Provider/healthcare-level stigma | ||||
| Medical prof think those w/ HIV “sleep around” | ||||
| Neither agree nor disagree | 0.66 * | (0.45, 0.97) | 0.77 | (0.50, 1.21) |
| Agree/strongly agree | 0.43 *** | (0.29, 0.64) | 0.47 ** | (0.29, 0.75) |
| Ref: Strongly disagree/disagree | 1.00 | 1.00 | ||
UOR = Unadjusted Odds Ratio.
AOR = Adjusted Odds Ratio.
CI = 95% Confidence Interval.
ǂP <.08, *P < .05, **P < .01, ***P < .001 in unadjusted and/or adjusted models.
Qualitative analyses
Five team members independently coded transcripts, using: (a) structural coding to group responses by interview question; and (b) thematic coding to understand lived experiences of HIV and linkage to care; the main coder is the principal investigator of this research who was deeply familiar with the qualitative data and able to conceptually match its themes to the survey data for data triangulation purposes. 34 A preliminary codebook was built from structural coding and iteratively refined once preliminary thematic coding was completed. Coders met throughout both phases to ensure coding consistency, revise coding, and apply additional sub-codes to transcripts. 34 In primary analyses, coding reports were generated, and analytic memos explored and described barriers and facilitators of care and viral suppression by study arm. The present analyses did not evaluate these factors; instead, a coding report was generated for transcripts coded with “Stigma,” to describe the lived experiences of participants based on MSM or HIV-positive identity. Most instances were double-coded with codes: HIV History, HIV Stigma, Other Stigma, HIV Care Adherence (Barriers), and Current Clinic Support. Multiple memos were created to track considerations like the setting of stigmatizing experiences. After review of the raw data to verify themes, quotes were extracted. Analyses were conducted in NVivo Version 12.0. 35
Results
A total of 657 MSM were screened at baseline; as shown in Table 1, participants were mostly African American (77.6%), identified as gay (75.2%), single (82.5%), and employed full-time (69.6%; N = 538). Mean age was 44 years (SD: 11.7).
Table 1.
Demographic Characteristics of Baseline Survey Participants in HPTN 078 (N = 657).
| Characteristic | N (%) or mean (SD) |
|---|---|
| Race | |
| African American or Black | 510 (77.6) |
| White | 99 (15.1) |
| Other | 48 (7.3) |
| Education | |
| Eighth grade or less/Some high school/High school graduate | 286 (43.5) |
| Some college/Vocational/Trade/Tech school | 218 (33.2) |
| Associates or other 2-year degree/Bachelors/Masters | 153 (23.3) |
| Self-identified sexual orientation | |
| Gay/Homosexual | 494 (75.2) |
| Bisexual | 163 (24.8) |
| Employment status | |
| Not employed | 110 (16.7) |
| Part-time employment | 90 (13.7) |
| Full-time employment | 457 (69.6) |
| Marital status | |
| Single/Divorced/Widowed | 537 (82.5) |
| Married/Civil union/Legal partnership/Have primary or main partner | 114 (17.5) |
| Verbal harassment due to having sex with men | |
| No | 372 (56.6) |
| Yes | 285 (43.4) |
| Excluded from family gatherings due to having sex with men | |
| No | 431 (73.2) |
| Yes | 158 (26.8) |
| People blame me for having HIV | |
| Strongly disagree/Disagree | 349 (55.2) |
| Neither agree nor disagree | 133 (21.0) |
| Agree/Strongly agree | 150 (23.7) |
| Medical providers assume people with HIV sleep around | |
| Strongly disagree/Disagree | 265 (41.6) |
| Neither agree nor disagree | 194 (30.5) |
| Agree/Strongly agree | 170 (27.9) |
| People treat me as less than human now that I have HIV | |
| Strongly disagree/Disagree | 397 (62.4) |
| Neither agree nor disagree | 129 (20.3) |
| Agree/Strongly agree | 110 (17.3) |
| Health care satisfaction rating | |
| Poor to Good (0-9 out of 10) | 275 (43.3) |
| Best possible (10 out of 10) | 360 (56.7) |
| Age (in years) | 44 (11.7) |
Quantitative Results
Regression results
White clients were nearly twice as likely as African American clients to report high medical care ratings (Adjusted Odds Ratio (AOR) = 1.83; 95% Confidence Interval (95% CI) = 1.07, 3.16; P < .05) (Table 2). Interpersonal-level social HIV and sexual stigma were both associated with less likelihood of high medical care ratings. Similarly, clients who were harassed in public had 33% lower odds of reporting high medical care ratings as those who did not report this (AOR = 0.67; 95% CI = 0.45, 0.98; P < .05). Clients who reported being excluded at family gatherings had a 40% lower odds of reporting high medical care ratings as those who had not (AOR = 0.60; 95% CI = 0.39, 0.93; P < .05). Regarding provider/healthcare-level HIV stigma, individuals who agreed that medical professionals think those with HIV “sleep around” were less than half as likely to report high medical care ratings as those who disagreed (AOR = 0.47; 95% CI = 0.29, 0.75; P < .01). While marginally significant, compared to clients who agreed that people think less of them due to HIV, those who disagreed were nearly twice as likely to report high medical care ratings (AOR = 1.68; 95% CI = 0.94, 3.00; P < .08).
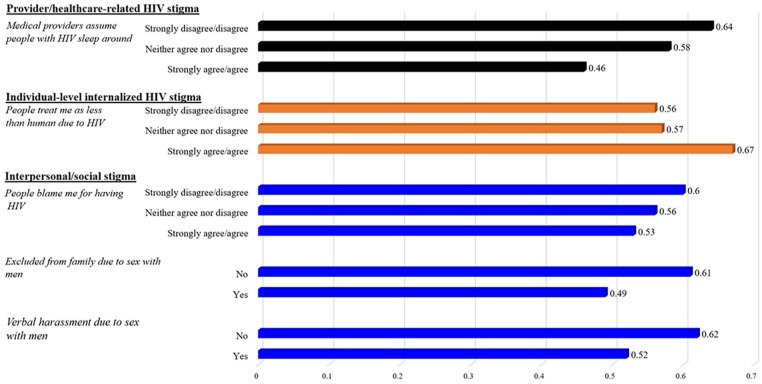
Marginal effects
Figure 1 reports predicted probabilities (rather than odds ratios) of high medical care ratings related to multilevel stigma, holding all other variables at their means. Provider/healthcare-level stigma was shown to reduce probability of high medical care ratings, comparing those who agreed versus disagreed that medical providers think people living with HIV “sleep around” (.46 vs .64, respectively; P < .05). Interpersonal/social HIV stigma showed a similar association, if individuals agreed versus disagreed that people treat them as “less than human due to their HIV” (0.56 vs 0.67, respectively; P < .05).
Figure 1.
Predicted probability of high healthcare ratings related to multilevel stigma among screened participants in HPTN 078.
Qualitative Results
Because the qualitative exit interview study sample derived from the larger quantitative baseline sample, interview participants were also mostly African American, self-identified as clients, and of lower socioeconomic status (N = 111). Experience of stigma described by participants were mostly related to provider/healthcare-level stigma, and interpersonal/social stigma. Within each of those levels, participants described experencies of stigma due to living with HIV, and due to their sexual identity (Table 3).
Table 3.
Experiences of Stigma Among Exit Interview Participants in HPTN 078.
| Discussion of stigma | Example quotes |
|---|---|
| Provider/healthcare-level stigma |
HIV stigma.
[My clinic has made me uncomfortable by the way
they]. . .um, like treating somebody with HIV like they
can catch it by just touching them on the hand or
something. . .[but rather than complain,] I’m just
thinking about changing my clinic. . . I’m very
observant so, just how they’re, I’ve observed their body
language while treating the patients. –
(Male/Pansexual/African American/23 years old/6 years in
HIV care)
It just embarrassed me [seeking care for HIV]. Like you know no one wants to really go sit in a room full of people that’s coming to get checked or are newly diagnosed, or they’re coming to see – or they’re coming for an STD check so to me even to this day, it’s kind of embarrassing but like I said, it’s part of me. It’s part of who I am now so I have to deal with it, and whoever I see in there, whatever. – (Male/Gay/African American/33 years old/2 years in HIV care) What makes it hard? Um, well for one, my clinic it’s very annoying, the community, with the kind of clinic it is, so they put the stigma of this in the community. . .when I first started going, that was the hardest thing about going to the appointment there because it was the stigma of the community, because everybody knew what the building was for. So. – (Male/Bisexual/African American/39 years old/11 years in HIV care) Sexual stigma. “There was this one uh nurse, I think she was a nurse. . .and I’m not sure if um, you know if she’s in harmony with, you know with the disease itself or, you know, my sexuality, that type of thing. Like I said uh previously, you know some people they just work to work and make a living, but I’m not sure if they are always comfortable or you know, with the mission basically. You know, and ideally when people, different sexualities, you know, being a gay person or bi-sexual person, that type of thing. . .I did have some misgivings about her presence. I don’t know, it might be my own personal imagining, but I just felt a certain vibe from this person and you know, I wasn’t too comfortable with it. I was actually going to introduce that but, I don’t know. . . – (Male/Gay/African American/58 years old/25 years in HIV care) Um, and I didn’t – I didn’t – I didn’t know what it was [my symptoms I was having due to having HIV], and I was so afraid to go to the doctor’s office about it because I didn’t want anyone to know I was having sex with men at the time. . .And so, it took me years to even go get that treated. . .I mean, almost, like, seven or 8 years [before I sought medical care and got my HIV diagnosis]. – (Male/Gay/African American/36 years old/4 years in HIV care) |
| Interpersonal/social-level stigma |
HIV stigma
. . . .I got my first master’s [and my HIV
status was] found out by [my school and they] put a
whole billboard and sent it to every student and faculty
member, “[name] is in the hospital dying of
AIDS.”. . .how do y’all know? [so I’ll] spend the rest
of my life getting people together for running their
mouth. . .But then, when you come to me [about my HIV
illness], I won’t know if you’re here to help or hurt, I
really don’t. – (Male/Gay/African American/33 years
old/6 years in HIV care) Um, but it’s so fearful to have to tell other people that you have it who don’t, because of how you think they’re going to look at you, or if they’re going to want to deal with you or anything like that.. . .when I found out I had it, me and my ex were together, so, of course, I’m not going to – you know, he’s already – he has it, I have it, there’s no care in the world. But when we separated, I was in fear for the rest of my life. . . – (Male/Gay/African American/52 years old/13 years in care) [I had a friend with HIV and]. . .he didn’t take any medication. He knew he had HIV, but he was one of those people who made fun of people for HIV, for having HIV. Like. . .he was with a group of friends who swore for now that they were HIV negative. So, they’re, “Oh, yeah. I’m HIV negative, you know,” and they’re all saying, “You know, I’m not sick. You know, I’m protected and people who are HIV positive are hoes and sluts,” and everything in the book. And that’s what their perception was and he knew he had it. – (Male/Gay/African American/35 years old/5 years in HIV care) Sexual stigma. . . .Like right now the shelter where I’m at I’m having problems with discrimination. There’s a Jamaican guy that’s always calling me all these things and telling me all these things. [My case manager]. . .told me. . .what this guy is doing is called a hate crime. . .[so] I feel safe coming to see this guy [for HIV care]. You know, besides being a case manager, he’s about to graduate from law school. And he knows exactly what he’s doing [and it helps me manage this]. – (Male/Gay/ White/Hispanic/53 years old) . . .[A] lot of people won’t face that spectrum [of being LGBT+ and at higher risk of HIV]. Sometimes it’s [a] shame, some things are better unknown or unsaid, I guess [about sexuality and HIV]. . .a lot of young men of color, you know there may be a so-called “down low” and they’re not getting tested, and that’s the thing. It’s you get tested, and get a diagnosis, and you get on meds right away, therefore your numbers are a lot better, you know. . . – (Male/Gay/African American/58 years old/25 years in HIV care) |
Provider/healthcare-level stigma
Participants largely described experiences of provider/healthcare-related stigma related to their medical appointments for managing their HIV care needs, however some clients felt stigmatized by the act of seeking care while others felt stigmatized being seen seeking care.
HIV stigma in healthcare
Clients described feelings of shame, judgment, and embarrassment due to their HIV status during healthcare visits (Table 3). Multiple dimensions of provider/healthcare-level HIV stigma were described, including feeling stigmatized by healthcare providers and by the healthcare environment itself. Several discussed discomfort with healthcare providers who seemed hesitant to physically touch them for fear of “catching” HIV:
My clinic has made me uncomfortable. . .um, like treating somebody with HIV like they can catch it by just touching them on the hand or something. . .rather than complain, I’m just thinking about changing my clinic. . . I’m very observant so, just how they’re, I’ve observed their body language while treating the patients. – (Male/Pansexual/African American/23 years old/6 years in HIV care)
Others described feeling stigmatized from the act of seeking HIV care. This was described as embarrassment by “being seen” seeking care by others regardless of their HIV status. One client described this as a process he worked through when he was first diagnosed and that now he felt “HIV is a part of me, so whatever.” He stated that, although he still feels embarrassment, this does not prevent him from seeking healthcare.
It just embarrassed me seeking care for HIV. Like you know no one wants to really go sit in a room full of people that’s coming to get checked or are newly diagnosed, or they’re coming to see. . .It’s part of who I am now so I have to deal with it, and whoever I see in there, whatever. – (Male/Gay/African American/33 years old/2 years in HIV care)
Sexual stigma in healthcare
Provider/healthcare-level sexual stigma was often described in concert with living with HIV. Feeling alienated while seeking healthcare was described, including not wanting to seek HIV care because of “not wanting anyone to know I was having sex with men.” Others described discomfort but not being sure if it was due to “the HIV disease itself” or “my sexuality.” One individual stated that his provider was “working just for a living” rather than really caring for clients:
“There was this one, uh, nurse. . .you know some people they just work to work and make a living, but. . . ideally when people, different sexualities, you know, being a gay person or bi-sexual person, that type of thing. . .I did have some misgivings about her presence. I don’t know, it might be my own personal imagining, but I just felt a certain vibe from this person and you know, I wasn’t too comfortable with it. . . – (Male/Gay/African American/58 years old/25 years in HIV care)
Another stated that many African American MSM are on the “down low” in order to avoid being labeled, which includes avoiding healthcare which increased their risk of being diagnosed with HIV.
. . .A lot of people won’t face that spectrum of being LGBT+ and at higher risk of HIV. . . .some things are better unknown or unsaid, I guess. . .a lot of young men of color, you know there may be a so-called ‘down low’ and they’re not getting tested, and that’s the thing. . .you get tested, and get a diagnosis, and you get on meds right away, therefore your numbers are a lot better. . . – (Male/Gay/African American/58 years old/25 years in HIV care)
Interpersonal/social HIV stigma
Outside of provider/healthcare-level stigma, a few individuals described experiences of interpersonal/social HIV stigma in the form of fear of disclosing HIV status. One individual explained he was more concerned with disclosing now that he was single as compared to when he was first diagnosed and in a relationship with an HIV-positive partner:
. . . it’s so fearful to have to tell other people that you have it who don’t, because of how you think they’re going to look at you. . .when I found out I had it, me and my ex were. . .he has it. . . But when we separated, I was in fear for the rest of my life. . . – (Male/Gay/African American/52 years old/13 years in care)
Other individuals mentioned people in their social networks who were “in denial” and did not disclose having HIV to individuals who they thought were HIV-negative. One man mentioned a friend who actively denied his status around his friends and even engaged in “HIV-shaming”:
I had a friend with HIV and. . .he didn’t take any medication. He knew he had HIV, but . . .he was with a group of friends who swore for now that they were HIV-negative. So, they’re, “Oh, yeah. I’m HIV-negative, you know,” and they’re all saying, “You know, I’m not sick. You know, I’m protected and people who are HIV-positive are hoes and sluts,. . .” and he knew he had it. – (Male/Gay/African American/35 years old/5 years in HIV care)
Interpersonal/social sexual stigma
Interpersonal/social sexual stigma experiences also included being verbally harassed at a housing shelter and discussing it with a case manager “who told me that it was a hate crime.” Because the case manager was knowledgeable about this issue, the client mentioned feeling more comfortable talking about the harassment, and dealing with it in his daily live outside of the care seeking context.
Discussion
The present research explored experiences of stigma and its relation to healthcare ratings among screened and enrolled participants in HPTN 078. Findings suggest that stigma due to multiple stigmatized identities was associated with reduced healthcare satisfaction ratings among a sample of clients who predominantly identified as African American and MSM. While 60% of clients rated their healthcare as optimal (10/10), stigma was prevalent in both qualitative and quantitative findings, and this is far less than the ideal whereby 100% would have identifed their care as optimal. These and other findings are in keeping with existing literature focused on understanding stigma in populations of color living with HIV.12,14-16,18-21
African American clients were nearly twice as likely as other groups to report suboptimal medical care ratings. This reinforces decades of literature highlighting poorer engagement in care, and adverse HIV outcomes in this population.12-16,19,20,23,26 Dissatisfaction with care was described, often in the context of provider/healthcare-level stigma. Stigma associated with sexual identity and HIV seropositive status were each independently associated with reporting lower medical care ratings. It is noteworthy that these experiences included examples of multi-level intersectional stigma both within and outside of the healthcare settings. This included individual-level internalized HIV stigma and interpersonal/social stigma such as being alienated from family due to being MSM.
Stigmatization of both HIV status and sexual identity were described interpersonally and at the provider/healthcare levels. Also, while marginally significant, higher endorsement of experiences related to individual-level stigma was associated with higher healthcare ratings. These findings represent the multidirectional, transactional relationship between social stigma and stigma within healthcare settings experienced by this population.21-26,36-40 Given that existing stigma interventions generally lack intersectional and/or multi-level components,13,14,16 simultaneously addressing racial, sexual, and HIV stigma in healthcare settings for African American and other clients who identify as sexual minorities and are living with HIV is needed. These needs, notably, are currently being explored in studies such as HPTN 096 which is evaluating the impact of a status neutral population-based multilevel intervention to promote HIV prevention outcomes among MSM clients in the South.
Limitations
HPTN 078’s primary objectives were not focused on examining multiple stigmatized identities or medical care ratings; similarly, dichotomizing our dependent variable as 10 versus all other ratings may have lowered variability to detect differences by individual rating level though this was theoretically sound as described earlier. As with all research which includes elements of self-report data, our findings may be subject to social desirability bias. Results are not generalizable to clients who are newly diagnosed, virally suppressed, or other racial groups and regions. Analyses did not use validated intersectional stigma measures in their entirety though the items used were from previous research. 29 Still, they should be interpreted with caution, because the focus of HPTN 078 was to evaluate the effects of an enhanced case management intervention on HIV viral suppression among clients with non-suppressed HIV viral load. Similarly, analyses are limited in their ability to discuss racism in the context of the healthcare setting as this was not an explicit study focus. Survey analyses included all screened clients who identified as HIV-positive, while interviews were only conducted with participants who were actually enrolled in the intervention. Experiences may have differed among those screened versus enrolled in relevant dimensions like consistent access to HIV care, experiences of stigma, and/or barriers to care like limited financial resources though directionality of these differences obviously cannot be posited. Nonetheless, the qualitative sample represents roughly one-third of participants in the quantitative models, and findings are in keeping with literature related to intersectional stigma.
Conclusions
Previous literature has documented the relationship between stigmatization, race, healthcare access, and retention among clients who are African American, MSM and living with HIV; reasons for these consistent inequities include structural racism which propagate medical mistrust, lack of training in LGBTQ health care and diversity among providers, greater burden of barriers to care like housing insecurity, food insecurity, mental health challenges, and/or less financial resources to remain in care and virally suppressed.16,18,22,38,41,42 Multi-level assessments of stigma should be prioritized to design and implement effective stigma reduction in healthcare settings for African American MSM clients43-45 who have the highest rates of HIV and related negative health outcomes in the US. These poor outcomes are due to these multi-level challenges which impact their care outcomes at the individual level but require changes at the structural level. At a modicum, clinics should routinely standardized protocols for HIV positive and/or clients as mentioned earlier,22-25 for example, how to handle discrepancies between identification cards and name/physical presentation of clients who are transgender; minimum required referrals and affirming language for provision of social service needs other than HIV. Future research in clinic-based settings should critically evaluate ways in which stigma impact client care engagement, care satisfaction, and HIV viral suppression. Recent findings by Babel et al 41 document similar need as in our study, specifically that: (1) Perceived health care discrimination was negatively associated with PrEP awareness; and (2) among young MSM of color, intersectional stigma compounded the social structural barriers to PrEP adherence. Doing so requires understanding of how societal power structures including racism, homophobia, and serophobia may be perpetuated through healthcare systems and structures and how they impact engagement in care more broadly than just HIV care seeking. Gunn et al 42 also note that stigma needs to be assessed consistently pre-post as well. Along with structural changes to challenge these processes, stigma reduction in healthcare settings that is cognizant of the multilayered, intersectional identities of African American clients who are sexual minorities and also MSM living with HIV can ensure equitable care receipt not just in HIV-specific areas, but can also progress national efforts to “end the HIV epidemic.”26,43-46
Acknowledgments
The authors thank the participants and study staff at the HPTN 078 clinic. Participating sites were Alabama Vaccine Research Center (Birmingham, AL); Fenway Health (Boston, MA); Johns Hopkins HIV Prevention Trials Network Unit (Baltimore, MD); and the Ponce de Leon Center (Atlanta, GA). Finally, the authors would like to thank the HTPN Scholars Program: Sten Vermund, Darrell Wheeler, Quarraisha Abdool-Karim, David Serwadda, Sherri Johnson, Tanette Headen, and Gabriela Salinas-Jimenez.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The HIV Prevention Trials Network (HPTN) is funded by the National Institute of Allergy and Infectious Diseases (UM1AI068619, UM1AI068613, UM1AI1068617), with co-funding from the National Institute of Mental Health, and the National Institute on Drug Abuse, all components of the U.S. National Institutes of Health.
Clinical Trial Number: NCT02663219
ORCID iD: D. Scott Batey  https://orcid.org/0000-0002-2422-5787
https://orcid.org/0000-0002-2422-5787
References
- 1.Krueger A, Dietz P, Van Handel M, Belcher L, Johnson AS. Estimates of CDC-funded and national HIV diagnoses: a comparison by demographic and HIV-related factors. AIDS Behav. 2016;20(12):2961-2965. [DOI] [PubMed] [Google Scholar]
- 2.Crepaz N, Hess KL, Purcell DW, Hall HI. Estimating national rates of HIV infection among MSM, persons who inject drugs, and heterosexuals in the United States. AIDS. 2019;33(4):701-708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Serovich JM, Laschober TC, Brown MJ, Kimberly JA. Evaluation of HIV disclosure behavior following a randomized controlled disclosure intervention for men who have sex with men living with HIV. Arch Sex Behav. 2018;47(7):2051-2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauermeister JA, Eaton L, Andrzejewski J, Loveluck J, VanHemert W, Pingel ES. Where you live matters: structural correlates of HIV risk behavior among young men who have sex with men in Metro Detroit. AIDS Behav. 2015;19(12): 2358-2369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanner AE, Mann L, Song E, et al. WeCARE: a social media-based intervention designed to increase HIV care linkage, retention, and health outcomes for racially and ethnically diverse young MSM. AIDS Educ Prev. 2016;28(3):216-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerr J, Northington T, Sockdjou T, Maticka-Tyndale E. Perceived neighborhood quality and HIV-related stigma among African diasporic youth; results from the African, Caribbean, and Black Youth (ACBY) study. J Health Care Poor Underserved. 2018;29(2):651-663. [DOI] [PubMed] [Google Scholar]
- 7.Mays VM, Cochran SD, Zamudio A. HIV prevention research: Are we meeting the needs of African American men who have sex with men? J Black Psychol. 2004;30(1):78-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van de Laar MJ. HIV/AIDS and other STI in men who have sex with men–a continuous challenge for public health. Eurosurveillance. 2009;14(47):19423. [DOI] [PubMed] [Google Scholar]
- 9.Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: social disadvantage and the US HIV epidemic. Am Psychol. 2013;68(4):197-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. Jama. 2019;321(9):844-845. [DOI] [PubMed] [Google Scholar]
- 11.Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267-1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turan JM, Elafros MA, Logie CH, Banik S, Bulent T, et al. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med. 2019;17(7):1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nyblade L, Stockton MA, Giger K, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. 2019;17(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deacon H, Boulle A. Commentary: factors affecting HIV/AIDS-related stigma and discrimination by medical professionals. Int J Epidemiol. 2007;36(1):185-186. [DOI] [PubMed] [Google Scholar]
- 15.Quinn K, Bowleg L, Dickson-Gomez J. The fear of being black plus the fear of being gay”: the effects of intersectional stigma on PrEP use among young black gay, bisexual, and other men who have sex with men. Soc Sci Med. 2019;232(C):86-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varas-Díaz N, Rivera-Segarra E, Neilands TB, et al. HIV/AIDS and intersectional stigmas: Examining stigma related behaviours among medical students during service delivery. Glob Public Health. 2019;14:1598-1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Griffin M, Cahill S, Kapadia F, Halkitis PN. Healthcare usage and satisfaction among young adult gay men in New York city. J Gay Lesbian Soc Serv. 2020;32(4):531-551. [Google Scholar]
- 18.Earnshaw VA, Reed NM, Watson RJ, Maksut JL, Allen AM, Eaton LA. Intersectional internalized stigma among black gay and bisexual men: a longitudinal analysis spanning HIV/sexually transmitted infection diagnosis. J Health Psychol. 2019;26(3):465-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arnold EA, Rebchook GM, Kegeles SM. Triply cursed’: racism, homophobia and HIV-related stigma are barriers to regular HIV testing, treatment adherence and disclosure among young Black gay men. Cult Health Sex. 2014;16(6):710-722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferguson L, Gruskin S, Bolshakova M, et al. Frameworks and measures for HIV-related internalized stigma, stigma and discrimination in healthcare and in laws and policies: a systematic review. J Int AIDS Soc. 2022;25 Suppl1:e25915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kerr J, Lelutiu-Weinberger C, Nelson LE, et al. Addressing intersectional stigma in programs focused on ending the HIV epidemic. Am J Public Health. 2022;112(S4):S362-S366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stringer KL, Turan B, McCormick L, et al. HIV-related stigma among healthcare providers in the deep south. AIDS Behav. 2016;20(1):115-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brinsdon A, Abel G, Desrosiers J. I’m taking control”: how people living with HIV/AIDS manage stigma in health interactions. AIDS Care. 2017;29(2):185-188. [DOI] [PubMed] [Google Scholar]
- 24.Wagner AC, Girard T, McShane KE, Margolese S, Hart TA. HIV-related stigma and overlapping stigmas towards people living with HIV among health care trainees in Canada. AIDS Educ Prev. 2017;29(4):364-376. [DOI] [PubMed] [Google Scholar]
- 25.Batey DS, Whitfield S, Mulla M, et al. Adaptation and implementation of an intervention to reduce HIV-related stigma among healthcare workers in the United States: piloting of the FRESH workshop. AIDS Patient Care STDS. 2016;30(11): 519-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maragh-Bass AC. ‘The Ask’ is ‘The Answer:’ implementing routine documentation of sexual orientation and gender identity in health care. Am J Public Health. 2019;109:1071-1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gamble T, Wang Z, Gaydos CA, Batey S, Mayer K, del Rio C, et al. Finding MSM who may be potential amplified HIV transmitters: results from HPTN 078. AIDS Res Hum Retroviruses. 2018;34:178.29037050 [Google Scholar]
- 28.Mitchell KM, Hoots B, Dimitrov D, German D, Flynn C, Farley JE, et al. Improvements in the HIV care continuum needed to meaningfully reduce HIV incidence among men who have sex with men in Baltimore, US: a modelling study for HPTN 078. J Int AIDS Soc. 2019;22(3):e25246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herek GM, Cogan JC, Gillis J, Glunt E. Correlates of internalized homophobia in a community sample of lesbians and gay men. J Gay Lesbian Med Assoc. 1997;2:17-25. [Google Scholar]
- 30.Long JS. Regression Models for Categorical and Limited Dependent Variables. SAGE Publishing; 1997. [Google Scholar]
- 31.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed.John Wiley & Sons, Inc; 2000. [Google Scholar]
- 32.Gordon RA. Applied Statistics for the Social and Health Sciences. Routledge; 2012. [Google Scholar]
- 33.Bennett DA. How can I deal with missing data in my study? Aust N Z J Public Health. 2001;23(5):464-469. [PubMed] [Google Scholar]
- 34.Plano Clark VL, Creswell JW. The Mixed Methods Reader Mixed Methodology Combining Qualitative and Quantitative Approaches. 11th ed.SAGE Publications; 2008. [Google Scholar]
- 35.QSR International Pty Ltd. NVivo (released in March 2020). 2020. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- 36.Sayles JN, Ryan GW, Silver JS, Sarkisian CA, Cunningham WE. Experiences of social stigma and implications for healthcare among a diverse population of HIV positive adults. J Urban Health. 2007;84(6):814-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67-S79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. 2017;21(1):283-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Friedland BA, Sprague L, Nyblade L, et al. Measuring intersecting stigma among key populations living with HIV: implementing the people living with HIV Stigma Index 2.0. J Int AIDS Soc. 2018;21(Suppl Suppl 5):e25131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pachankis JE, Hatzenbuehler ML, Hickson F, et al. Hidden from health: structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM Internet Survey. AIDS. 2015;29(10):1239-1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Babel RA, Wang P, Alessi EJ, Raymond HF, Wei C. Stigma, HIV risk, and access to HIV prevention and treatment services among men who have sex with men (MSM) in the United States: a scoping review. AIDS Behav. 2021;25:3574-3604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gunn JKL, Rooks-Peck C, Wichser ME, et al. Effectiveness of HIV stigma interventions for men who have sex with men (MSM) with and without HIV in the United States: a systematic review and meta-analyses. AIDS Behav. 2022; 26:51-89. [DOI] [PubMed] [Google Scholar]
- 43.Ramos MC, Smith-Lovin L, Young B. Intersectional identities and stigma recovery. Identities Everyday Life. 2019;26:167. [Google Scholar]
- 44.Birbeck GL, Bond V, Earnshaw V, El-Nasoor ML. Advancing health equity through cross-cutting approaches to health-related stigma. BMC Med. 2019;17:40-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dale SK, Ayala G, Logie CH, Bowleg L. Addressing HIV-related intersectional stigma and discrimination to improve public health outcomes: an AJPH supplement. Am J Public Health. 2022;112(S4):S335-S337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karver TS, Atkins K, Fonner VA, et al. HIV-related intersectional stigma and discrimination measurement: state of the science. Am J Public Health. 2022;112(S4):S420-S432. [DOI] [PMC free article] [PubMed] [Google Scholar]