ABSTRACT
Introduction
The Impact Stratification Score (ISS) is a measure of the impact of chronic low back pain (LBP) consisting of nine Patient-Reported Outcomes Measurement Information System (PROMIS-29) items, but no studies have examined the ISS or its association with psychological symptoms in military samples. This study examines longitudinal associations between psychological symptoms and the ISS among military service members.
Material and Methods
The study involved secondary data analysis of a sample of active duty U.S. military service members aged 18-50 years with LBP (n = 733). Participants completed the PROMIS-29 at three time points during treatment: baseline (time 1, T1), week 6 of treatment (time 2, T2), and week 12 of treatment (time 3, T3). The impact of LBP was quantified using the ISS (ranging from 8 = least impact to 50 = greatest impact). Psychological symptoms were assessed as PROMIS-29 anxiety and depression scores. Separate autoregressive cross-lagged models examined reciprocal associations of ISSs with anxiety, depression, and emotional distress scores from T1 to T3.
Results
Within each time point, the ISS was significantly and positively correlated with anxiety and depression. In autoregressive cross-lagged models, anxiety and depression predicted the ISS at the next time point and associations were similar in magnitude (e.g., anxiety T2 to ISS T3: β = 0.12, P < .001; depression T2 to ISS T3: β = 0.12, P <.001). The ISS did not predict future depression or emotional distress scores at any time point, but the ISS at T2 was significantly, positively associated with anxiety scores at T3 (β = 0.07, P = .04).
Conclusion
Psychological symptoms consistently and prospectively predict the impact of LBP as measured by the ISS among service members undergoing pain treatment. The ISS may also be associated with future anxiety but not depression. PROMIS-29 anxiety and depression items may be useful adjunctive measures to consider when using the ISS to support LBP treatment planning and monitoring with service members.
INTRODUCTION
As in the general population,1,2 low back pain (LBP) is both prevalent and debilitating among U.S. military service members.3–5 In addition to its economic costs and impact on individuals’ functioning and well-being,6 LBP among service members also has implications for factors such as deployment readiness and ability of service members to meet the demands of military service. For example, in previous studies of military samples, LBP has been shown to correlate with higher utilization of medical services, more lost workdays, absenteeism, and presenteeism.3,4,7 A recent study of health-related occupational impairment among U.S. active duty service members found that LBP was the most commonly endorsed physical health condition (reported by 23% of respondents) and was associated with a greater proportion of lost workdays than all other physical or mental health conditions examined.7 Evidence also suggests that LBP may persist after service: for example, LBP is among the most common reasons for presenting for medical treatment among veterans.8,9 This underscores the importance of efforts to improve the detection and treatment of LBP for military service members.
The NIH Pain Consortium proposed the Impact Stratification Score (ISS) to measure the impact of chronic LBP using a nine-item subset of the PROMIS-29, a psychometrically sound and widely used instrument for assessing pain and other health domains.10,11 The ISS proposed by the NIH Pain Consortium represents physical function, pain interference with activities, and pain intensity. The PROMIS-29 items that comprise the ISS have been used and tested extensively with a wide range of adults.12 However, few studies have evaluated the ISS, especially in treatment settings with military service members. This is a key gap that has implications for understanding the properties and clinical utility of tools such as the ISS in military samples. In a recent study, Hays et al. examined psychometric properties of the ISS in a sample of active duty service members in treatment for LBP and found strong support for reliability and construct validity.13 However, additional studies are needed to understand the application and clinical utility of the ISS in military samples.
Another key gap in the evidence base on the ISS is the extent to which it is associated with other constructs known to correlate with the impact of LBP, such as psychological distress.14 The ISS items largely represent physical health (i.e., physical function, pain interference with activities, and pain intensity scores). However, the psychological components of pain are well established, and psychiatric conditions are highly comorbid with chronic pain.15–17 Some prior work also indicates that anxiety or depression symptoms may show bidirectional associations with pain over time17,18 and can be conceptualized as antecedents and consequences of pain. Moreover, depression and/or anxiety symptoms have been shown to correlate with pain treatment outcomes (e.g., reductions in pain over time among those in treatment19; recurrence of future episodes of LBP20) and psychological interventions (e.g., cognitive behavioral therapy; mindfulness-based stress reduction) may improve treatment outcomes for LBP, particularly among those with comorbid psychiatric symptoms.21–23 The importance of psychological factors in LBP management is reflected in guidelines developed by the U.S. DVA and the U.S. DoD, which recommend “performing a mental health screening as part of the low back pain evaluation and taking results into consideration during selection of treatment” among service members and veterans presenting with LBP.24 This underscores the importance of considering reciprocal associations between the ISS and psychological factors for individuals in treatment for LBP.
Although symptoms of depression and anxiety are highly correlated25 and are often combined in measures of general psychological distress,26,27 there is some evidence for potential differences in the relative contribution of anxiety or depression to pain and the impact of LBP. For example, pain with comorbid anxiety alone may be less prevalent than pain with comorbid depression,28 and the combination of both anxiety and depression has been associated with greater pain and poorer treatment outcomes than either depression or anxiety alone.28 In addition, anxiety symptoms may have interactive or additive effects on pain distinct from depression, such that individuals with greater anxiety may also experience greater pain and greater disability.29 Studies have also found that individuals who reported greater pain interference may show poorer responses to anxiety treatment.30,31 Furthermore, patients with comorbid anxiety and LBP may be more likely to endorse pain interference with activities due to avoidance-related coping and worry of exacerbating pain.32 This underscores the importance of considering potentially distinct roles of depression and anxiety symptoms in the impact of LBP and has important ramifications for assessment, diagnosis, and treatment planning for individuals presenting with LBP.23,32
Few studies have attempted to disentangle the relative roles of anxiety and depression symptoms in pain and response to treatment for LBP. This has important implications for considering whether depression and/or anxiety assessments may be useful adjuncts to pain impact measures such as the ISS in research and clinical practice. Examining the interplay between the ISS and anxiety/depression also has relevant practical implications. For example, if the full PROMIS-29 profile is administered in LBP treatment settings, clinicians and researchers will have information on both anxiety and depression symptoms in addition to the ISS. However, no studies to date have examined whether and how PROMIS-29 anxiety and depression scores are reciprocally associated with total ISSs over time for individuals receiving treatment for LBP. The current study aims to address these gaps by examining the interplay between depression and anxiety symptoms and ISSs over 12 weeks among military service members receiving treatment for LBP. To this end, we use autoregressive cross-lagged (ARCL) models to examine reciprocal associations between anxiety and depression symptoms—separately and combined with an emotional distress (ED) composite score—and the ISS across three time points over the course of LBP treatment.
MATERIALS AND METHODS
Dataset
The current study involves secondary analysis of data collected as part of a larger, completed multisite pragmatic parallel-group comparative effectiveness clinical trial that examined the addition of chiropractic care to usual medical care (UMC+CC) compared to usual care alone (UMC) on pain relief and pain-related functioning. Details of the larger trial (ClinicalTrials.gov Identifier: NCT01692275) are described elsewhere.33 The trial was conducted between 2012 and 2016, and study procedures for the trial were reviewed and approved by the RAND Human Subject Protections Committee (Institutional Review Board). Briefly, participants in the clinical trial were active duty U.S. military service members aged 18-50 years with musculoskeletal LBP recruited from three military treatment facilities. Individuals were assigned to condition balancing groups on the following factors: age, gender, duration of LBP, and pain intensity. UMC+CC participants received a 6-week chiropractic care intervention consisting of spinal manipulative therapy and other procedures (e.g., rehabilitation exercise and cryotherapy); UMC participants received usual care. Repeated questionnaire measures assessing the ISS, mental health symptoms, and other variables were administered at three time points: baseline (time 1, T1), week 6 of treatment (time 2, T2), and week 12 of treatment (time 3, T3). The final analytic sample included 733 patients (365 UMC and 368 UMC+CC).
Measures
Pain Impact Stratification Scores
ISSs were generated from the following nine items in the PROMIS-29.10,11 “Physical function (four items)”—Participants provided ratings on their capacity to engage in the following tasks related to physical functioning: “Are you able to… do chores such as vacuuming or yard work? Go up and down stairs at a normal pace? Go for a walk of at least 15 minutes? Run errands and shop? (response options: without any difficulty, with a little difficulty, with some difficulty, with much, difficulty, unable to do).” “Pain interference with usual activities (four items)”—In the past seven days, “How much did pain interfere …” With your day-to-day activities? With work around the home? With your ability to participate in social activities? With your household chores? (1 = not at all to 5 = very much). “Pain intensity (1 item)”—Participants provided numeric ratings of average LBP intensity in the past week (0 = no pain to 10 = worst imaginable pain). Items were summed to create a total ISS ranging from 8 (least impact) to 50 (greatest impact).
Anxiety
Individuals reported on the frequency of experiencing anxiety symptoms in the past week (e.g., “In the past seven days …” I felt fearful, I found it hard to focus on anything other than my anxiety, my worries overwhelmed me, I felt uneasy; response options: 1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always) using the four PROMIS Adult Anxiety items from the PROMIS-29 questionnaire.12 Items were summed to create raw scores ranging from 4 to 20.
Depression
Participants rated how often in the past week they experienced the following symptoms of depression using four items in the PROMIS-29 (e.g., “In the past seven days I felt…” worthless; helpless; depressed; hopeless; response options: 1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always).12 Items were summed to create raw scores ranging from 4 to 20.
Emotional distress composite
As an indicator of overall distress (without focusing on depression or anxiety in isolation), we also calculated ED composite scores26 based on PROMIS-29 anxiety and depression items. Scores were computed as the mean of anxiety and depression raw scores.
Demographic characteristics
Participants reported on age, gender (male and female), race (Black, White, Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, multi-racial, or unspecified), and ethnicity (Hispanic/Latino and not Hispanic/Latino).
Data Analysis
We first conducted univariate analyses on variables of interest to the current study. We then conducted simple bivariate correlations (Pearson r) to examine how ISSs and anxiety, and depression symptoms are correlated at each time point. Finally, we used ARCL models to examine reciprocal associations of total ISSs with PROMIS-29 anxiety, depression, and ED scores from T1 to T3 in separate models. In total, we estimated three ARCL models and evaluated fit using conventional model fit criteria such as root mean square error of approximation (RMSEA ≤ 0.08),34 Comparative Fit Index (CFI ≥ 0.95), and standardized root mean residual (SRMR ≤ 0.08).35 Note χ2 is not included as a model fit index given that it is extremely sensitive to sample size and in large samples, as the one used here, even trivial differences are significant, thus rendering this fit index uninformative. Preliminary analyses showed similar longitudinal patterns of ISS, anxiety, or depression by treatment group; as such, UMC and UMC+CC groups were combined for the analysis. All models controlled for demographic characteristics (age, gender, race, and ethnicity) and treatment condition (UMC; UMC+CC) and were estimated in Mplus v8.1.36
RESULTS
The sample was 76% male, 16% Hispanic/Latino, 57% White, 20% Black, 7% Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, multi-racial, or unspecified, and averaged 30.9 years old (SD = 8.7).
Table I shows mean scores for depression, anxiety, and overall ED and mean ISSs at each time point. Across all time points, bivariate tests showed that the ISS was significantly and positively correlated with anxiety, depression, and ED scores. At T1, the ISS correlated with anxiety (r = 0.40) and depression (r = 0.34). The correlation increased between the ISS and anxiety (r = 0.51) and depression (r = 0.40) at T2. Lastly, at T3, correlations with the ISS increased for both anxiety (r = 0.52) and depression (r = 0.43). A similar pattern of correlations was observed between the ED composite and the ISS across time points: T1 (r = 0.40), T2 (r = 0.48), and T3 (r = 0.50).
TABLE I.
Mean Scores for Anxiety, Depression, and Emotional Distress and Mean ISSs Across Time Points
| Time 1 (baseline) M (SD) |
Time 2 (6 weeks) M (SD) |
Time 3 (12 weeks) M (SD) |
|
|---|---|---|---|
| Mental health | |||
| Anxiety | 6.2 (3.0) | 5.5 (2.8) | 5.4 (2.6) |
| Depression | 5.2 (2.4) | 5.1 (2.5) | 5.0 (2.3) |
| Emotional distress composite | 5.7 (2.5) | 5.3 (2.5) | 5.2 (2.3) |
| Impact of LBP | |||
| Total ISS | 24.2 (8.4) | 19.1 (8.8) | 17.9 (9.1) |
Abbreviations: ISS = Impact Stratification Score, LBP = low back pain.
Emotional distress composite score is calculated as the average of anxiety and depression scores. The range for anxiety, depression, and emotional distress scores is from 4 to 20. The range for ISSs is from 8 to 50.
Autoregressive Cross-lagged Model Results
ISS and anxiety
The ARCL model for the ISS and anxiety fit the data well (RMSEA = 0.056, CFI = 0.96, SRMR = 0.054). Figure 1 shows model-based effect estimates for statistically significant (at P < .05) associations between the ISS and anxiety (within-time point correlations and paths from T1 to T2 and T2 to T3). Anxiety at T1 significantly predicted the ISS at T2 (P =.04). Similarly, anxiety at T2 significantly predicted the ISS at T3 (P < .001). With regard to the effects of ISSs on subsequent anxiety, the ISS at T1 did not predict anxiety at T2 (P =.87), but the ISS at T2 significantly predicted anxiety at T3 (P =.04). Further, within time points, anxiety and ISSs were significantly and positively correlated (r’s:T1 = 0.40; T2 = 0.50, T3 = 0.37).
FIGURE 1.
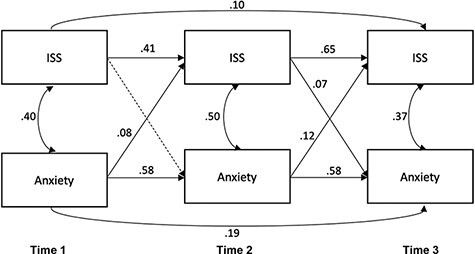
Autoregressive cross-lagged model of anxiety and Impact Stratification Scores (ISSs) across time points (standardized betas and correlations).
ISS and depression
The ARCL model for the ISS and depression also fit the data well (RMSEA = 0.055, CFI = 0.96, SRMR = 0.054). Statistically significant (P < .05) effect estimates are shown in Figure 2. Similar to results for the anxiety model, depression at T1 significantly predicted the ISS at T2 (P = .03). Similarly, depression at T2 significantly predicted the ISS at T3 (P < .001). However, the ISS at T1 did not significantly predict depression at T2 (P = .79), nor did the ISS at T2 predict depression at T3 (P = .11). Within time points, depression and ISSs were significantly and positively correlated (r’s: T1 = 0.34; T2 = 0.38, T3 = 0.30).
FIGURE 2.
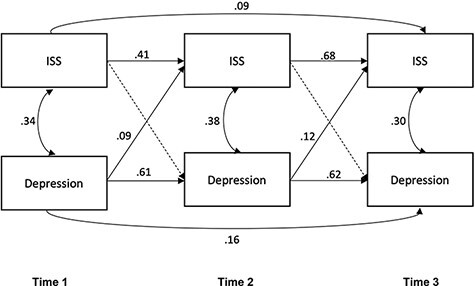
Autoregressive cross-lagged model of depression and Impact Stratification Scores (ISSs) across time points (standardized betas and correlations).
ISS and emotional distress
The ARCL model for the ISS and ED fit the data well (RMSEA = 0.056, CFI = 0.96, SRMR = 0.054). Statistically significant (P < .05) effect estimates are shown in Figure 3. Prospective effects of the ED composite on ISSs mirrored those observed in the anxiety and depression models: ED at T1 predicted the ISS at T2 (P = .02), and ED at T2 significantly predicted the ISS at T3 (P < .001). Similar to the depression model, the ISS at T1 did not significantly predict ED at T2 (P = .45) nor did the ISS at T2 significantly predict ED at T3 (P = .21). Within time points, overall ED and ISS were significantly and positively correlated (r’s: T1 = 0.41; T2 = 0.48, T3 = 0.37).
FIGURE 3.
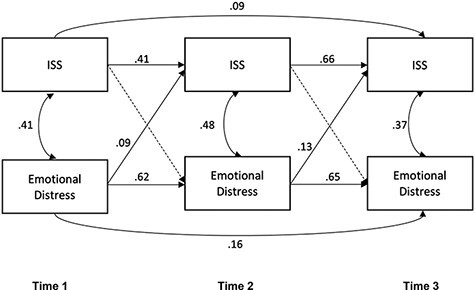
Autoregressive cross-lagged model of emotional distress and Impact Stratification Scores (ISSs) across time points (standardized betas and correlations).
DISCUSSION
Prior work has not examined reciprocal associations between PROMIS-29 anxiety and depression symptoms and ISSs over time among individuals in treatment for LBP. In this sample of military service members, both anxiety and depression were positively correlated with the ISS at each time point, corresponding to baseline, 6 weeks, and 12 weeks after initiating pain treatment, with slightly more robust associations at the final time point compared to baseline. In addition, in ARCL models, anxiety and depression symptoms—individually and combined—were prospectively associated with the ISS across time points.
We found that higher anxiety and depression symptoms are prospectively, positively associated with a more negative impact of LBP on physical health—as measured by the ISS—during the course of treatment, consistent with previous work.19,37 This may suggest that assessing and addressing anxiety and depression symptoms early in treatment might be beneficial for improving response to LBP treatment. We observed largely similar patterns for anxiety and depression models and for the ED composite score, with respect to prospective associations with subsequent ISS. This was anticipated because, although depression and anxiety represent distinct symptom clusters, they are highly correlated. In addition, measures of anxiety and depression perform very similarly in many populations, and they are often combined in summary measures of general psychological or ED.26,27 Indeed, in the analyses examined here, the magnitude of associations between anxiety and subsequent ISS and depression and subsequent ISS (e.g., anxiety T2 → ISS T3: beta = 0.12; depression T2 → ISS T3: beta = 0.12) were nearly identical and similar to that observed for the ED total score (e.g., ED T2 → ISS T3: beta = 0.13). However, longitudinal associations with the ISS were unidirectional for depression and ED total scores predicting subsequent ISS; that is, we did not observe reciprocal associations between the ISS and subsequent depression or ED. This unidirectional pattern is consistent with findings from a prior study examining reciprocal, longitudinal associations between a latent anxiety and depression symptom factor and pain and pain-related disability among individuals in treatment for chronic pain.37 However, findings contrast with other studies that have shown reciprocal associations between depression symptoms and pain over time. For example, Kroenke et al. reported reciprocal associations between changes in pain severity and changes in depression severity across four time points (spanning 12 months) for individuals in primary care with persistent back, hip, or knee pain.18 In addition, a separate study examining cross-lagged associations between physical health (physical function, role limitations due to physical health, and pain) and mental health (emotional well-being; role limitations due to emotional problems) over 4-year scores among primary care patients with chronic conditions showed that physical health factor scores prospectively predicted mental health scores but not vice versa.38 These divergent findings may be attributable to myriad factors, including differences in sample composition, time period, and measurement. For example, in contrast to the aforementioned studies, the current investigation focused on active duty service members in treatment for LBP for a comparatively short time period. It is possible that longitudinal associations between symptoms of depression and the impact of pain may differ depending upon treatment context, medical and treatment history, and duration/chronic nature of pain, as suggested by others.37
In contrast to depression and ED models, we observed reciprocal associations for the ISS and anxiety, such that the ISS at 6 weeks (mid-point) was also positively, prospectively associated with anxiety at 12 weeks. In the context of LBP, depression and anxiety may differentially contribute to experiences of pain and its impact on functioning over the course of the treatment.15,28,29 Furthermore, patients with comorbid anxiety and LBP may be more likely to endorse pain interference with activities due to avoidance-related coping and worry of exacerbating pain.32 This underscores the importance of routinely assessing anxiety—in addition to depression—in clinical settings to understand potentially different contributions of these sets of symptoms on pain over the course of treatment and inform treatment planning. Among military personnel, LBP is a substantial contributor to occupational impairment3,4,7 and may interfere with the rigorous mental and physical demands of military service. For active duty service members undergoing treatment for LBP, experiencing a more severe impact of LBP mid-way through treatment may lead to greater frustration, worry, or catastrophizing based on expectations about capacity to perform work duties. Moreover, military culture emphasizing toughness and self-reliance39 may contribute to or exacerbate anxiety associated with a greater and/or persistent pain for some individuals as treatment progresses. Although perhaps not unique to service members, such factors may account for the slightly divergent patterns observed for associations between anxiety and depression symptoms in this sample. Efforts to manage treatment expectations and address potentially maladaptive coping strategies (e.g., avoidance-related coping)32 for pain and anxiety symptoms throughout treatment may be beneficial in reducing both the impact of LBP and distress over the course of treatment.
Collectively, these findings support the potential utility of the PROMIS-29 as part of the routine assessment for service members undergoing treatment for LBP. As noted above, the ISS items capture constructs that pertain primarily to the physical impact of pain (i.e., physical function, pain interference with activities, and pain intensity scores). However, the psychological impact of pain is well accepted, and other measures explicitly incorporate psychological factors in quantifying the impact of pain on overall functioning (e.g., Keele STarT Back Screening Tool40). Although it was beyond the scope of the current investigation, future work may benefit from examining whether and how incorporating anxiety and depression items from the PROMIS-29 into a revised ISS impact measure may be useful as a more comprehensive physical and mental health impact scoring system for use in persons with chronic pain.
Findings should be interpreted in the context of study limitations. First, this study involved secondary analysis on data from an existing randomized clinical trial, which included individuals undergoing usual care as well as those undergoing usual care plus chiropractic intervention. The goal of the current study was to assess longitudinal associations between the ISS and anxiety/depression symptoms among individuals undergoing pain treatment rather than identify differences in patterns by the type of pain treatment. Thus, treatment groups were combined for analysis. Although preliminary analyses showed similar longitudinal patterns of the ISS or anxiety/depression symptoms by treatment group and all models controlled for the treatment group, it is possible that longitudinal associations between the ISS and psychological symptoms may differ in relation to specific types of pain treatment. Additionally, due to limitations in the source dataset, we were unable to assess differences in relation to the use of medications for pain (e.g., prescription or over the counter) or for anxiety/depression or other conditions. Future studies would benefit from examining differences in longitudinal associations between the ISS and mental health in relation to different types of treatment programs, including medications. In addition, data were limited to three time points spanning 12 weeks during active treatment. It is unclear whether or how findings may generalize to longer treatment/assessment periods. Moreover, we were unable to examine the clinical diagnosis of specific conditions (e.g., generalized anxiety disorder or major depressive disorder) in relation to changes in the impact of LBP over time. Although it was beyond the scope for the current study, future studies with large, diverse, longitudinal samples should assess whether and how mental health symptoms and specific conditions may contribute to changes in the ISS over the course of treatment. In addition, the current study only examined the ISS; however, other measures, such as the Defense and Veterans Pain Rating Scale v2.0 with supplemental items (DVPRS 2.0), have been developed and tested for use specifically with military populations41; although it includes a supplemental item assessing the impact of pain on “stress,” the DVPRS 2.0 does not include assessments of anxiety or depression symptoms. Finally, this study involved active duty service members. As such, findings may not generalize to other samples such as veterans or civilians.
Findings from this study indicate that PROMIS-29 anxiety and depression scores are positively correlated with and prospectively predict the ISS pain impact scores over time for service members undergoing pain treatment for LBP. This indicates that anxiety and depression screens may be important adjunctive measures to consider for service members in treatment for LBP24 (e.g., to inform treatment planning) and supports the potential utility of using the PROMIS-29 profile as part of routine clinical assessment for this group.
Contributor Information
Michael S Dunbar, RAND Corporation, Pittsburgh, PA 15213, USA.
Anthony Rodriguez, RAND Corporation, Boston, MA 02116, USA.
Maria O Edelen, RAND Corporation, Boston, MA 02116, USA; Department of Surgery, Patient-Reported Outcomes, Value & Experience (PROVE) Center, Brigham and Women’s Hospital, Boston, MA 02120, USA.
Ron D Hays, RAND Corporation, Santa Monica, CA 90401, USA; Department of Medicine, University of California, Los Angeles, CA 90024, USA.
Ian D Coulter, RAND Corporation, Santa Monica, CA 90401, USA.
Daniel Siconolfi, RAND Corporation, Pittsburgh, PA 15213, USA.
Patricia M Herman, RAND Corporation, Santa Monica, CA 90401, USA.
FUNDING
This work was funded by the National Center for Complementary and Integrative Health at the NIH (R01AT010402, Principal Investigators (PI): Herman and Hays).
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts to disclose.
REFERENCES
- 1. Freburger JK, Holmes GM, Agans RP, et al. : The rising prevalence of chronic low back pain. Arch Intern Med 2009; 169(3): 251–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hoy D, Bain C, Williams G, et al. : A systematic review of the global prevalence of low back pain. Arthritis Rheum 2012; 64(6): 2028–37. [DOI] [PubMed] [Google Scholar]
- 3. Berkowitz SM: Occupational back disability in U.S. Army personnel. Mil Med 1999; 164(6): 412–8. [PubMed] [Google Scholar]
- 4. Feuerstein M, Berkowitz SM, Peck CA: Musculoskeletal-related disability in U.S. Army personnel: prevalence, gender, and military occupational specialties. J Occup Environ Med 1997; 39(1): 68–78. [DOI] [PubMed] [Google Scholar]
- 5. Knox J, Orchowski J, Scher DL, Owens BD, Burks R, Belmont PJ: The incidence of low back pain in active duty United States military service members. Spine 2011; 36(18): 1492–500. [DOI] [PubMed] [Google Scholar]
- 6. Hoy D, March L, Brooks P, et al. : Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol 2010; 24(2): 155–65. [DOI] [PubMed] [Google Scholar]
- 7. Dunbar MS, Schuler M, Meadows SO, Engel CC: Associations between mental and physical health conditions and occupational impairments in the U.S. Military. Mil Med 2021; usab021.doi: 10.1093/milmed/usab021(in press). [DOI] [PubMed] [Google Scholar]
- 8. Childs JD, Wu SS, Teyhen DS, Robinson ME, George SZ: Prevention of low back pain in the military cluster randomized trial: effects of brief psychosocial education on total and low back pain-related health care costs. Spine J 2014; 14(4): 571–93. [DOI] [PubMed] [Google Scholar]
- 9. Gironda RJ, Clark ME, Massengale JP, Walker RL: Pain among veterans of Operations Enduring Freedom and Iraqi Freedom. Pain Med 2006; 7(4): 339–43. [DOI] [PubMed] [Google Scholar]
- 10. Deyo RA, Dworkin SF, Amtmann D, et al. : Report of the NIH Task Force on research standards for chronic low back pain. Pain Med 2014; 18(8): 1249–67. [DOI] [PubMed] [Google Scholar]
- 11. Deyo RA, Ramsey K, Buckley DI, et al. : Performance of a Patient Reported Outcomes Measurement Information System (PROMIS) short form in older adults with chronic musculoskeletal pain. Pain Med 2016; 17(2): 314–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cella D, Choi SW, Condon DM, et al. : PROMIS® adult health profiles: efficient short-form measures of seven health domains. Value Health 2019; 22(5): 537–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hays RD, Edelen MO, Rodriquez A, Herman P: Support for the Reliability and Validity of the National Institutes of Health Impact Stratification Score in a sample of active duty U.S. military personnel with low back pain. Pain Med 2021; pnab175.doi: 10.1093/pm/pnab175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pincus T, Burton AK, Vogel S, Field AP: A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 2002; 27(5): E109–20. [DOI] [PubMed] [Google Scholar]
- 15. Bair MJ, Robinson R, Katon W, Kroenke K: Depression and pain comorbidity: a literature review. Arch Intern Med 2003; 163(20): 2433–45. [DOI] [PubMed] [Google Scholar]
- 16. McWilliams LA, Cox BJ, Enns MW: Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain 2003; 106(1–2): 127–33. [DOI] [PubMed] [Google Scholar]
- 17. Means-Christensen AJ, Roy-Byrne PP, Sherbourne CD, Craske MG, Stein MB: Relationships among pain, anxiety, and depression in primary care. Depress Anxiety 2008; 25(7): 593–600. [DOI] [PubMed] [Google Scholar]
- 18. Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W: Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain 2011; 12(9): 964–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Oliveira DS, Vélia Ferreira Mendonça L, Sofia Monteiro Sampaio R, Manuel Pereira Dias de Castro-lopes J, Ribeiro de Azevedo LF: The impact of anxiety and depression on the outcomes of chronic low back pain multidisciplinary pain management-a multicenter prospective cohort study in pain clinics with one-year follow-up. Pain Med 2019; 20(4): 736–46. [DOI] [PubMed] [Google Scholar]
- 20. Pinheiro MB, Ferreira ML, Refshauge K, et al. : Symptoms of depression and risk of new episodes of low back pain: a systematic review and meta-analysis. Arthritis Care Res 2015; 67(11): 1591–15603. [DOI] [PubMed] [Google Scholar]
- 21. Boersma K, Södermark M, Hesser H, Flink IK, Gerdle B, Linton SJ: Efficacy of a transdiagnostic emotion-focused exposure treatment for chronic pain patients with comorbid anxiety and depression: a randomized controlled trial. Pain 2019; 160(8): 1708–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hoffman BM, Papas RK, Chatkoff DK, Kerns RD: Meta-analysis of psychological interventions for chronic low back pain. Health Psychol 2007; 26(1): 1–9. [DOI] [PubMed] [Google Scholar]
- 23. Janzen K, Peters-Watral B: Treating co-occurring chronic low back pain & generalized anxiety disorder. Nurse Pract 2016; 41(1): 12–8. [DOI] [PubMed] [Google Scholar]
- 24. The Diagnosis and Treatment of Low Back Pain Work Group : VA/DoD Clinical Practice Guidelines for Diagnosis and Treatment of Low Back Pain Version 2.0. US Department of Defense, US Department of Veterans Affairs; 2017. [Google Scholar]
- 25. Jacobson NC, Newman MG: Anxiety and depression as bidirectional risk factors for one another: a meta-analysis of longitudinal studies. Psychopharmacol Bull 2017; 143(11): 1155–200. [DOI] [PubMed] [Google Scholar]
- 26. Hays RD, Spritzer KL, Schalet BD, Cella D: PROMIS®-29 v2.0 profile physical and mental health summary scores. Qual Life Res 2018; 27(7): 1885–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kessler RC, Andrews G, Colpe LJ, et al. : Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psycho Med 2002; 32(6): 959–76. [DOI] [PubMed] [Google Scholar]
- 28. Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K: Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med 2008; 70(8): 890–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Asmundson GJKJ: Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depress Anxiety 2009; 26(10): 888–901. [DOI] [PubMed] [Google Scholar]
- 30. Morone NE, Belnap BH, He F, Mazumdar S, Weiner DK, Rollman BL: Pain adversely affects outcomes to a collaborative care intervention for anxiety in primary care. J Gen Intern Med 2013; 28(1): 58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Teh CF, Morone NE, Karp JF, et al. : Pain interference impacts response to treatment for anxiety disorders. Depress Anxiety 2009; 26(3): 222–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jordan KD, Okifuji A: Anxiety disorders: differential diagnosis and their relationship to chronic pain. J Pain Palliat Care Pharmacother 2011; 25(3): 231–45. [DOI] [PubMed] [Google Scholar]
- 33. Goertz CM, Long CR, Vining RD, et al. : Assessment of chiropractic treatment for active duty, U.S. military personnel with low back pain: study protocol for a randomized controlled trial. Trials 2016; 17; 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. MacCallum RC, Brown MW, Sugawara HM: Power analysis and determination of sample size for covariance structure modeling. Psychol Methods 1996; 1(2): 130–49. [Google Scholar]
- 35. Hu LT, Bentler PM: Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999; 6(1): 1–55. [Google Scholar]
- 36. Muthén LK, Muthén B: Mplus User's Guide. Muthén & Muthén 2012–18. [Google Scholar]
- 37. Lerman SF, Rudich Z, Brill S, Shalev H, Shahar G: Longitudinal associations between depression, anxiety, pain, and pain-related disability in chronic pain patients. Psychosom Med 2015; 77(3): 333–41. [DOI] [PubMed] [Google Scholar]
- 38. Hays RD, Marshall GN, Wang EY, Sherbourne CD: Four-year cross-lagged associations between physical and mental health in the Medical Outcomes Study. J Consult Clin Psychol 1994; 62(3): 441–9. [DOI] [PubMed] [Google Scholar]
- 39. Langston V, Gould M, Greenberg N: Culture: what is its effect on stress in the military? Mil Med 2007; 172(9): 931–5. [DOI] [PubMed] [Google Scholar]
- 40. Hill JC, Dunn KM, Lewis M, et al. : A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum 2008; 59(5): 632–41. [DOI] [PubMed] [Google Scholar]
- 41. Polomano RC, Galloway KT, Kent ML, et al. : Psychometric testing of the Defense and Veterans Pain Rating Scale (DVPRS): a new pain scale for military population. Pain Med 2016; 17(8): 1505–19. [DOI] [PubMed] [Google Scholar]


