Abstract
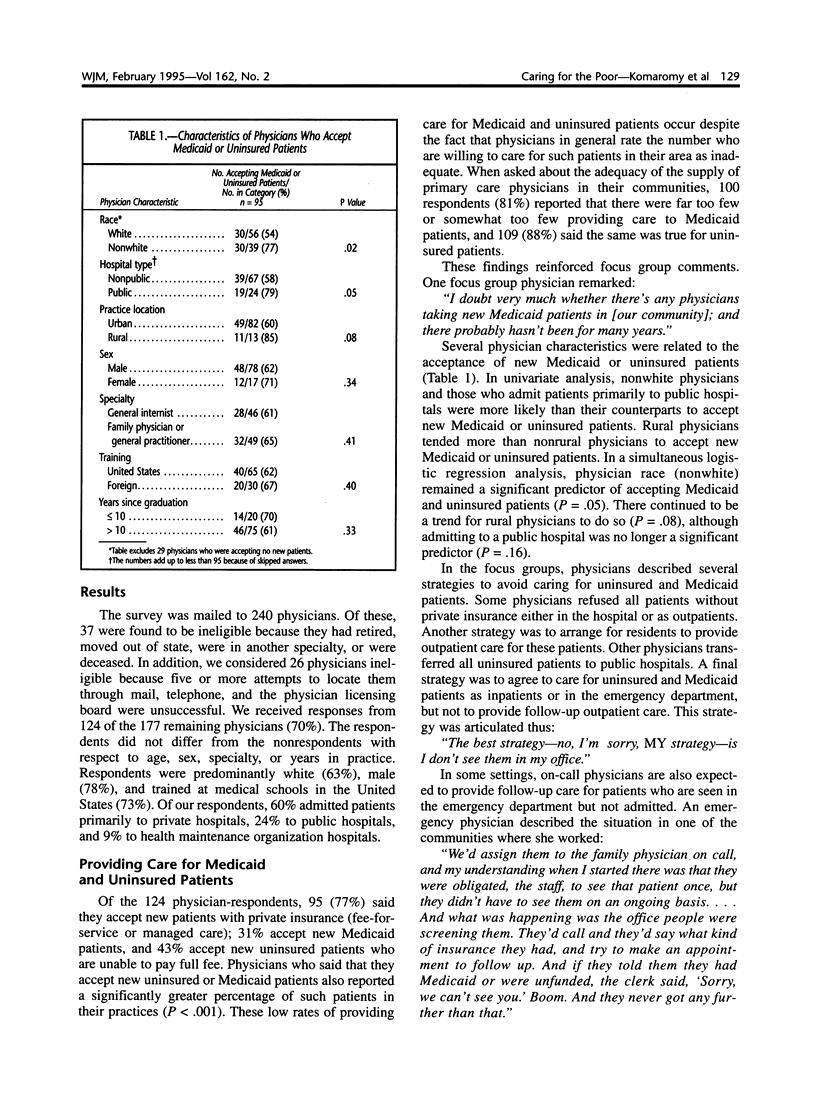
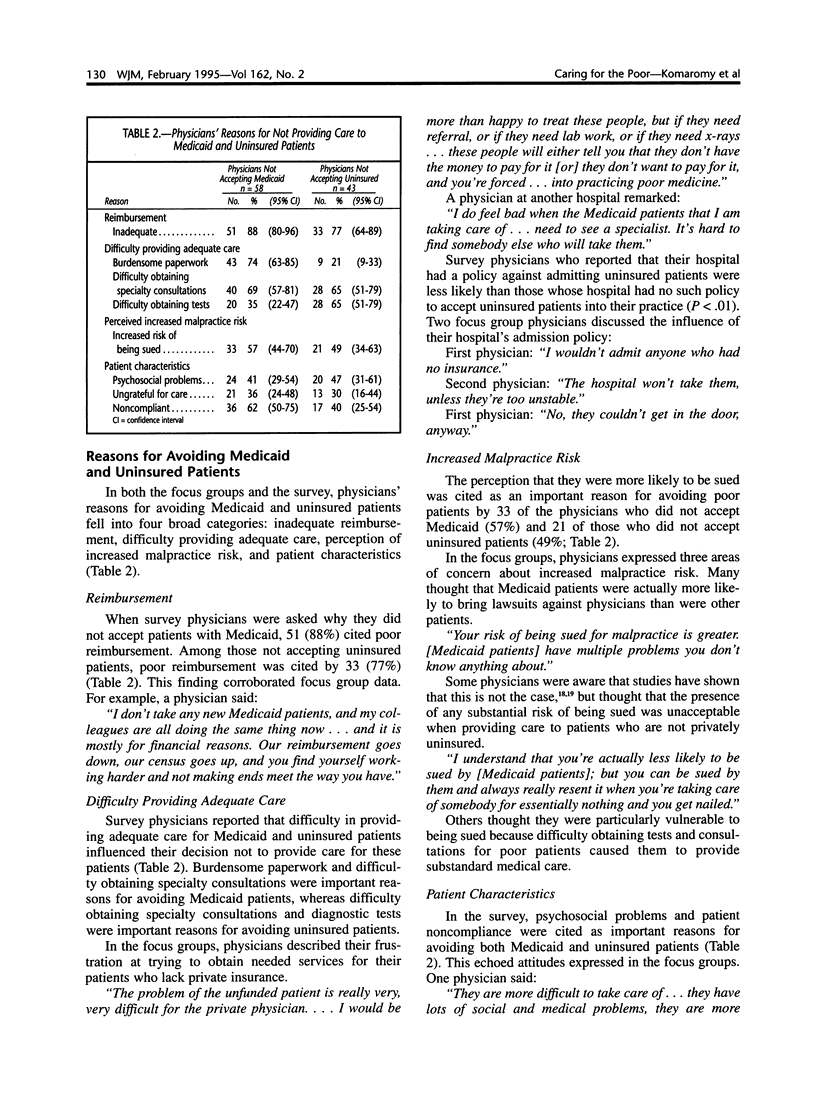
Although generalist physicians appear to be more likely than specialists to provide care for poor adult patients, they may still perceive financial and nonfinancial barriers to caring for these patients. We studied generalist physicians' attitudes toward caring for poor patients using focus groups and used the results to design a survey that tested the generalizability of the focus group findings. The focus groups included a total of 24 physicians in 4 California communities; the survey was administered to a random sample of 177 California general internists, family physicians, and general practitioners. The response rate was 70%. Of respondents, 77% accepted new patients with private insurance; 31% accepted new Medicaid patients, and 43% accepted new uninsured patients. Nonwhite physicians were more likely to care for uninsured and Medicaid patients than were white physicians. In addition to reimbursement, nonfinancial factors played an important role in physicians' decisions not to care for Medicaid or uninsured patients. The perception of an increased risk of being sued was cited by 57% of physicians as important in the decision not to care for Medicaid patients and by 49% for uninsured patients. Patient characteristics such as psychosocial problems, being ungrateful for care, and noncompliance were also important. Poor reimbursement was cited by 88% of physicians as an important reason not to care for Medicaid patients and by 77% for uninsured patients. Policy changes such as universal health insurance coverage and increasing the supply of generalist physicians may not adequately improve access to care unless accompanied by changes that address generalist physicians' financial and nonfinancial concerns about providing care for poor patients.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adkins R. J., Anderson G. R., Cullen T. J., Myers W. W., Newman F. S., Schwarz M. R. Geographic and specialty distributions of WAMI Program participants and nonparticipants. J Med Educ. 1987 Oct;62(10):810–817. doi: 10.1097/00001888-198710000-00004. [DOI] [PubMed] [Google Scholar]
- Baldwin L. M., Greer T., Wu R., Hart G., Lloyd M., Rosenblatt R. A. Differences in the obstetric malpractice claims filed by Medicaid and non-Medicaid patients. J Am Board Fam Pract. 1992 Nov-Dec;5(6):623–627. [PubMed] [Google Scholar]
- Basch C. E. Focus group interview: an underutilized research technique for improving theory and practice in health education. Health Educ Q. 1987 Winter;14(4):411–448. doi: 10.1177/109019818701400404. [DOI] [PubMed] [Google Scholar]
- Bashshur R. L., Homan R. K., Smith D. G. Beyond the uninsured: problems in access to care. Med Care. 1994 May;32(5):409–419. doi: 10.1097/00005650-199405000-00001. [DOI] [PubMed] [Google Scholar]
- Burstin H. R., Johnson W. G., Lipsitz S. R., Brennan T. A. Do the poor sue more? A case-control study of malpractice claims and socioeconomic status. JAMA. 1993 Oct 13;270(14):1697–1701. doi: 10.1001/jama.270.14.1697. [DOI] [PubMed] [Google Scholar]
- Burstin H. R., Lipsitz S. R., Brennan T. A. Socioeconomic status and risk for substandard medical care. JAMA. 1992 Nov 4;268(17):2383–2387. [PubMed] [Google Scholar]
- Crandall S. J., Volk R. J., Loemker V. Medical students' attitudes toward providing care for the underserved. Are we training socially responsible physicians? JAMA. 1993 May 19;269(19):2519–2523. [PubMed] [Google Scholar]
- Ginzberg E., Ostow M. Beyond universal health insurance to effective health care. JAMA. 1991 May 15;265(19):2559–2562. [PubMed] [Google Scholar]
- Haas J. S., Udvarhelyi I. S., Morris C. N., Epstein A. M. The effect of providing health coverage to poor uninsured pregnant women in Massachusetts. JAMA. 1993 Jan 6;269(1):87–91. [PubMed] [Google Scholar]
- Kindig D. A., Movassaghi H. The adequacy of physician supply in small rural counties. Health Aff (Millwood) 1989 Summer;8(2):63–76. doi: 10.1377/hlthaff.8.2.63. [DOI] [PubMed] [Google Scholar]
- Kletke P. R., Davidson S. M., Perloff J. D., Schiff D. W., Connelly J. P. The extent of physician participation in Medicaid: a comparison of physician estimates and aggregated patient records. Health Serv Res. 1985 Dec;20(5):503–523. [PMC free article] [PubMed] [Google Scholar]
- Krieger J. W., Connell F. A., LoGerfo J. P. Medicaid prenatal care: a comparison of use and outcomes in fee-for-service and managed care. Am J Public Health. 1992 Feb;82(2):185–190. doi: 10.2105/ajph.82.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell J. B. Physician participation in Medicaid revisited. Med Care. 1991 Jul;29(7):645–653. doi: 10.1097/00005650-199107000-00004. [DOI] [PubMed] [Google Scholar]
- Nesbitt T. S., Tanji J. L., Scherger J. E., Kahn N. B. Obstetric care, Medicaid, and family physicians. How policy changes affect physicians' attitudes. West J Med. 1991 Dec;155(6):653–657. [PMC free article] [PubMed] [Google Scholar]
- Perloff J. D., Neckerman K., Kletke P. R. Pediatrician participation in Medicaid--findings of a five-year-follow-up study in California and elsewhere. West J Med. 1986 Oct;145(4):546–550. [PMC free article] [PubMed] [Google Scholar]
- Piper J. M., Ray W. A., Griffin M. R. Effects of Medicaid eligibility expansion on prenatal care and pregnancy outcome in Tennessee. JAMA. 1990 Nov 7;264(17):2219–2223. [PubMed] [Google Scholar]
- Politzer R. M., Harris D. L., Gaston M. H., Mullan F. Primary care physician supply and the medically underserved. A status report and recommendations. JAMA. 1991 Jul 3;266(1):104–109. [PubMed] [Google Scholar]
- Rabinowitz H. K. Evaluation of a selective medical school admissions policy to increase the number of family physicians in rural and underserved areas. N Engl J Med. 1988 Aug 25;319(8):480–486. doi: 10.1056/NEJM198808253190805. [DOI] [PubMed] [Google Scholar]
- Rivo M. L., Satcher D. Improving access to health care through physician workforce reform. Directions for the 21st century. JAMA. 1993 Sep 1;270(9):1074–1078. [PubMed] [Google Scholar]
- Tambor E. S., Chase G. A., Faden R. R., Geller G., Hofman K. J., Holtzman N. A. Improving response rates through incentive and follow-up: the effect on a survey of physicians' knowledge of genetics. Am J Public Health. 1993 Nov;83(11):1599–1603. doi: 10.2105/ajph.83.11.1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verby J. E., Newell J. P., Andresen S. A., Swentko W. M. Changing the medical school curriculum to improve patient access to primary care. JAMA. 1991 Jul 3;266(1):110–113. [PubMed] [Google Scholar]


