Abstract
Background:
Psychotherapy is the gold standard treatment for posttraumatic stress disorder (PTSD), yet psychotherapy utilization and retention among veterans is low. Little is known about the barriers to care and factors associated with women veterans’ PTSD psychotherapy utilization and retention.
Objectives:
Using a nationally-representative sample of 986 women Veterans Health Administration (VHA) Primary Care users with PTSD and a perceived need for mental health care, we examined (1) the proportion of women who utilized psychotherapy; (2) retention in psychotherapy among women who used any psychotherapy; and (3) individual factors related to psychotherapy utilization and retention.
Methods:
Women completed a survey on their mental health care experiences. Outpatient mental health care utilization in the year prior to survey was obtained from VHA administrative data.
Results:
Most women (79.1%) utilized psychotherapy, and 41.7% of those women had a minimal therapeutic dose of psychotherapy (≥ 8 visits). Mental health diagnostic comorbidity and being African American/Black or identifying as neither African American/Black nor White were significantly associated with higher psychotherapy utilization. Mental health diagnostic comorbidity, exposure to military sexual trauma, and receiving treatment aligned with gender-related and group-related preferences were associated with higher psychotherapy retention. Being a parent was associated with lower retention.
Conclusion:
Although a significant proportion of women veterans with PTSD are utilizing psychotherapy, retention is enhanced when women are able to obtain treatment aligned with their preferences. Thus, efforts to promote patient-centered, shared decisions regarding mental health treatment options could increase the efficacy and efficiency of treatment for PTSD among women.
Keywords: women, veterans, PTSD, psychotherapy, patient preferences
Posttraumatic stress disorder (PTSD) is a prevalent and debilitating condition that can significantly lower quality of life (Gates et al., 2012; Schnurr, Lunney, Bovin, & Marx, 2009). An estimated 14–23% of Veteran’s Health Administration (VHA) users suffer from PTSD (Fulton et al., 2015; Gates et al., 2012). In 2017, the Department of Veterans Affairs (VA)/Department of Defense (DoD) clinical practice guidelines revised recommendations for PTSD treatment, with trauma-focused psychotherapy alone as the gold standard treatment. Psychotherapy is more efficacious in reducing PTSD symptoms and a more cost-effective treatment option compared to pharmacotherapy (Le, Doctor, Zoellner, & Feeny, 2014; Pull & Pull, 2014).
Despite recommendations for veterans with PTSD to utilize psychotherapy, many do not, even when provided a referral (DeViva, 2014; Kehle-Forbes, Meis, Spoont, & Polusny, 2016). Among those that do, the rate of retention in psychotherapy for PTSD, long enough to achieve clinical benefit, is low (Doran, Pietrzak, Hoff, & Harpaz-Rotem, 2017; Rosen et al., 2011; Valenstein-Mah et al., 2019). There is evidence that over one third of veterans drop out prematurely from PTSD psychotherapy treatment (Kehle-Forbes et al., 2016; Goetter et al., 2015). Extant literature has pointed to several factors that may predict PTSD psychotherapy utilization and retention among veterans, including age, sex, employment, marital status, race/ethnicity, military service era, and diagnostic comorbidity (DeViva et al., 2015; Doran et al., 2017; Nobles et al., 2017; Valenstein-Mah et al., 2019). These factors, however, explain only a portion of the difference between veterans who use psychotherapy and stay in treatment and others who do not. Many questions remain unanswered, such as what additional factors predict psychotherapy utilization and retention and how these factors differ across specific veteran populations, including women. To better promote psychotherapy use in VA and identify potential areas of intervention, it is necessary to have a more comprehensive understanding of the barriers to care and factors associated with PTSD psychotherapy utilization and retention.
Existing information regarding psychotherapy utilization and retention among veterans with PTSD is limited. Most studies focus on newly-diagnosed veterans and psychotherapy use shortly after diagnosis (Doran et al., 2017; Spoont, Murdoch, Hodges, & Nugent, 2010), but we know little about psychotherapy use for non-newly diagnosed veterans. Repeated attempts at psychotherapy engagement are common among veterans seeking PTSD treatment (Buchholz et al., 2017; Oliva, Bowe, Harris, & Trafton, 2013), signifying that non-newly diagnosed veterans might reengage in treatment long after PTSD diagnosis.
Additionally, many studies fail to consider whether individuals even want care and the type of care they prefer (e.g., Doran et al., 2017; Spoont et al., 2010). Not all individuals who meet criteria for PTSD may perceive a need for mental health care, especially in the context of competing treatment needs associated with comorbid conditions (Durai et al., 2011). Among those individuals who perceive a need for treatment, some may prefer pharmacotherapy over psychotherapy (Simiola, Neilson, Thompson, & Cook, 2015). Low utilization of psychotherapy among individuals with a satisfactory response to pharmacotherapy may be a function of patient preferences rather than limited psychotherapy reach. Thus, studies accounting for non-newly diagnosed veterans, veterans with a perceived need for mental health services, and pharmacotherapy use will provide more complete estimates of PTSD psychotherapy utilization and retention by capturing those who want psychotherapy and may reengage with care at time points after diagnosis.
The current literature provides an even more limited depiction of the psychotherapy utilization and retention among women veterans with PTSD as most studies focus on largely male samples and any effects particular to women are obscured (e.g., DeViva et al., 2015; Doran et al., 2017). Women are an underrepresented minority in VA (Frayne et al., 2018) and have the potential to be under-served as a result of discomfort in predominantly male VA mental health care settings (Kehle-Forbes et al., 2017; Kimerling et al., 2015b). As such, treatment preferences may be an important factor in women veterans’ PTSD psychotherapy utilization and retention, where women who receive care in accordance with strongly held preferences are more likely to stay in care compared to those who do not receive preference concordant care. Indeed, gender-related treatment preferences have been documented among women veterans. Preferences for gender-specialized services, such as women’s clinics, female providers, or gender tailored treatments, are especially strong with respect to PTSD-related services, as compared to care for other conditions, with the majority of women rating these preferences as highly important (Kimerling et al., 2015a). When these preferences are met, women are significantly more likely to report that their mental health services met their needs, while women who do not receive gender-specialized services as often as they desired reported greater unmet needs for care (Kimerling et al., 2015b). If gender-related preferences and other treatment preferences, such as a preference for group treatment, play a role in psychotherapy retention, then efforts to promote patient-centered, shared decisions regarding mental health treatment options could result in greater proportions of women retained in care, thereby enhancing the efficacy and efficiency of treatment for PTSD.
Other factors distinct to women may be associated with utilization and retention of psychotherapy for PTSD and in turn help inform strategies for promoting treatment. For example, compared to veteran men, women veterans are more likely to identify as a racial/ethnic minority (Frayne et al., 2018). In FY 2015, approximately half of women using VHA between 18–45 years old identified as a racial/ethnic minority (Frayne et al., 2018). Studies indicate that certain racial groups have disparate rates of VHA mental health utilization (Koo, Madden, & Maguen, 2015). This suggests that race may play a larger role in women veterans’ PTSD psychotherapy utilization and retention compared to men. If so, greater efforts may be necessary in tailoring mental health services to accommodate diverse women and help them stay in treatment.
Women veterans, compared to men, also have unique parenting and trauma experiences. Women in the military are more likely to be single parents than are men in the military (Clever & Segal, 2013). Thus, parenting may be a more significant barrier for women in attending PTSD treatment given childcare and household responsibilities. Similarly, women in the military report a greater number of adverse childhood experiences than their male counterparts (Katon et al., 2015). Gaska and Kimerling (2018) identified five distinct patterns of childhood and military adversity among women in VHA primary care. They found that women who experienced adversity during both childhood and military service or only during military service had increased likelihood of having PTSD compared to women with low probabilities of experiencing adversity during childhood and military service or with adverse experiences during childhood only. Those same women along with women who had adverse experiences during childhood only were more likely to have comorbid mental health conditions than the low adversity women. This may suggest that women with particular trauma experiences utilize PTSD psychotherapy treatment at different rates given potential differences in need to address mental health concerns.
The current population-based study provides a unique opportunity to examine the aforementioned factors that are distinct to women and may influence their PTSD psychotherapy retention and utilization. Most population-based studies rely on administrative data and are unable to examine such information. Using a sample of women veterans diagnosed with PTSD who reported a perceived need for mental health care in the past year, we examined (1) the proportions of women who utilized psychotherapy, pharmacotherapy, or both; (2) retention in psychotherapy among women who used any psychotherapy services; and (3) individual factors (i.e., gender-related and group-related treatment preferences, demographic variables, and veteran characteristics such as parenting status and trauma exposure) related to psychotherapy utilization and retention.
Method
Study Design
This study utilized data from the Women’s Overall Mental Health Assessment of Needs (WOMAN) Survey, a cross-sectional telephone survey of a population-based stratified random sample of 6,287 women veterans (84.3% participation rate) who used VHA primary care. The WOMAN Survey consists of 145 items designed to determine the need for and access to VHA mental health care services. Sampling was stratified based on age and race/ethnicity and included an over-sample of nonwhite women and women aged 18–44. Data were collected between June 12, 2012 and September 30, 2012 and then linked to administrative data for VHA utilization in the year prior to the survey using the VHA National Patient Care Database (NPCD) outpatient encounter files (VA Information Resource Center, 2011). All study procedures were approved by the Stanford University Institutional Review Board.
Participants
Inclusion criteria for this study were: (1) an ICD-9 diagnosis of PTSD (309.81) present for at least one outpatient encounter in the year prior to the survey (Abrams, Vaughan-Sarrazin, Keane, & Richardson, 2015) and (2) self-reported perceived need for mental health care in the past year. Perceived need for mental health care was defined according to prior research (Kimerling, & Baumrind, 2005), with an item that asked, in the past year, “Did you ever want (or need) help with personal, family, or emotional problems from a doctor or mental health professional, such as a psychologist, psychiatrist, counselor, or therapist?”
Of the 6,287 women who participated in the survey, 17.1% (N = 1,073) had a current PTSD diagnosis. Of these 1,073 women, 91.9% (n = 986) reported a perceived need for mental health care within the last year. Thus, the final sample was comprised of 986 women VHA primary care users with PTSD and a perceived need for mental health care.
Measures
Demographics.
Demographic characteristics including age, race, parent/guardian status, and Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) service were assessed using the survey. A variable from the Planning Systems Support Group Enrollee File (Phibbs, Cowgill, & Fan, 2013), a file of geographic information on VHA patients, was matched to the survey to classify a veteran’s geographic residence as urban, rural, or highly rural. Regarding race, women were asked to select from White, African American/Black, Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, and other. Only a small number of women identified as Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, or other, so we recoded these into an “other” category.
Utilization of mental health services.
Mental health visits, using criteria consistent with VHA Mental Health Operations performance monitoring criteria (Trafton et al., 2013) and VHA guidelines for mental health workload capture, were obtained for the year prior to the survey from NPCD outpatient treatment files (VA Information Resource Center, 2011). Psychotherapy visits were identified from outpatient mental health encounters using Current Procedural Terminology codes and further divided as group versus individual psychotherapy for additional analyses. We examined psychotherapy utilization (i.e., having at least one psychotherapy visit) and psychotherapy retention (i.e., total number of psychotherapy visits); to better describe the amount of psychotherapy utilization, we calculated the proportions of women with numbers of visits indicating minimal psychotherapy engagement (3 or more psychotherapy visits) (Doran et al., 2017) and a minimally adequate therapeutic dose (8 or more visits, as has been established in prior research) (Cook et al., 2014; DeViva et al., 2015).
Past-year use of pharmacotherapy for PTSD was abstracted from the Pharmacy Benefits Management (PBM) database (VA Information Resource Center, 2008) and determined based on medication fills consistent with PTSD treatment, including amitriptyline, citalopram, desipramine, imipramine, mirtazapine, nefazodone, nortriptyline, paroxetine, phenezine, prazosin, sertraline, desvenlafaxine, venlafaxine, fluoxetine, fluvoxamine, duloxetine, escitalopram, and trazodone. Use of non-VHA outpatient mental health care services was based on survey self-report of outpatient mental health treatment.
Medical and psychiatric diagnoses.
Chronic physical health conditions were quantified by grouping ICD-9 diagnoses into non-overlapping categories, using a comorbidity measure designed for use with large administrative datasets (Centers for Medicare & Medicaid Services, 2015). A dichotomous variable was created to reflect whether the patient had either zero or one or more comorbid chronic physical health conditions.
Mental health conditions were categorized from ICD-9 codes according to the Agency for Healthcare Research and Quality Clinical Classifications Software framework (Agency for Health Care Research and Quality, 2012). Each patient was coded for the presence or absence of comorbid adjustment disorder, anxiety disorders, depressive disorders, bipolar disorder, psychotic spectrum disorders, and substance use disorders. Women were classified as having zero, one, or two or more mental health comorbidities based on the number of diagnoses present from the list above.
Trauma exposure variables.
Types of traumatic experiences were assessed in the survey. Childhood physical or sexual abuse (age of <18) was assessed using the physical abuse item from the Adverse Childhood Experiences scale (Felitti et al., 1998) and the sexual assault item from the Life Stressors Checklist (Wolfe, J. W., Kimerling, Brown, Chrestman, & Levin, 1996). Military sexual trauma was assessed using the sexual harassment subscale of the Deployment Risk and Resiliency Inventory (DRRI) (King, King, & Vogt, 2003). Combat exposure was endorsed when participants indicated that they had served in a peacekeeping operation or a combat or conflict zone and had witnessed death or wounding of others, discharged a weapon, or felt in danger of being hurt or killed (Department of Defense, 2008). Post-military interpersonal violence included sexual assault after military discharge as measured by the sexual assault item from the Life Stressors Checklist (Wolfe et al., 1996) and past-year intimate partner violence as measured by the HARK screen (Sohal, Eldridge, & Feder, 2007).
Treatment preferences.
Treatment preferences were assessed via survey. Gender-related treatment preferences were assessed for VHA mental health services. Preferences included seeing a female mental health provider as often as wished, receiving care in a specialized women’s setting as often as wished, and participating in women-only group treatments as often as wished. These items were rated on a 5-point Likert scale ranging from “never” to “always” or “no preference” if the item was not applicable because the participant did not have strong preferences in that area. Items were dichotomized to indicate that preferences were met (‘always’ or ‘most of the time’) or not met, or not applicable. For the women-only groups item, the majority of women who responded ‘no preference’ specified that it was due to preferences for individual vs. group treatment, rather than gender-related preferences. We re-coded this item post-hoc to indicate preferences for group treatment, with all responses for women-only groups coded as ‘acceptable’ for group treatment.
Data Analysis
All analyses were conducted using STATA version 12 (StataCorp, 2011). Data were weighted in analysis for design characteristics of the survey and to adjust for survey nonresponse. Logistic regressions were used to model the odds of any psychotherapy utilization. Negative binomial regressions were used to model the number of psychotherapy visits in the year prior to the survey among women with at least one outpatient psychotherapy visit. Generalized estimating equations were used to adjust variance estimation and standard errors for clustering within facilities.
Results
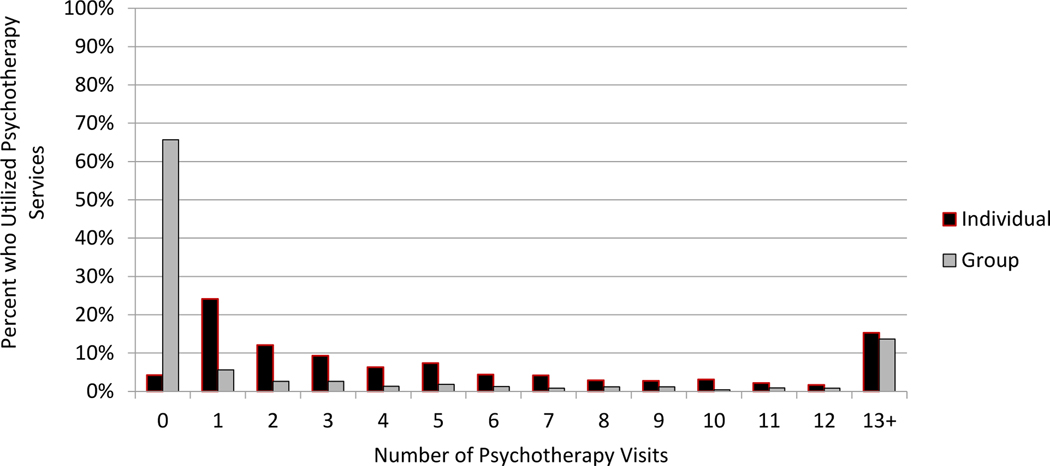
The majority of women in the sample (79.1%) utilized psychotherapy services, and a similar majority (73.8%) utilized pharmacotherapy. Only 3.4% of the sample received neither intervention, and 58.0% utilized both pharmacotherapy and psychotherapy. Among women who received any psychotherapy, 69.1% had ≥ 3 visits, and 41.7% had a minimal therapeutic dose of ≥ 8 visits (60.3% of minimally engaged women). Among women who received any psychotherapy, the median number of psychotherapy visits was 6 with an interquartile range (IQR) of 2–14. The median number of individual psychotherapy visits was 4 (IQR = 1–9), and the median number of group psychotherapy visits was 0 (IQR = 0–3). Figure 1 displays the number of individual and group psychotherapy visits among women who used any psychotherapy services.
Figure 1.
Number of individual and group psychotherapy visits among women veterans with psychotherapy utilization (n = 729).
Table 1 shows descriptive statistics as well as the associations of veteran characteristics with psychotherapy utilization and retention. African American/Black women, women who identified as neither African American/Black nor White women, and women with two or more mental health comorbidities had increased odds of using psychotherapy. Parenting women demonstrated lower psychotherapy retention. Women with one or more mental health comorbidities had higher psychotherapy retention. Table 2 demonstrates descriptive statistics as well as the association between trauma exposure characteristics and psychotherapy utilization and retention. Women with a history of MST demonstrated higher psychotherapy retention.
Table 1.
Demographic and Clinical Characteristics Associated with VHA Psychotherapy Utilization and Retention among Women Veterans Diagnosed with PTSD
| Any Utilization (N=986) | Retention (n=729) | |||
|---|---|---|---|---|
| Variable | n | % | AOR [95% CI] | IRR [95% CI] |
|
| ||||
| Age, years | ||||
| 65+ (ref) | 61 | 6.2% | ||
| 45–64 | 510 | 51.7% | 1.03 [0.47, 2.29] | 1.41 [0.88, 2.26] |
| 18–44 | 415 | 42.1% | 2.02 [0.82, 4.95] | 1.21 [0.79, 1.87] |
| Race | ||||
| White (ref) | 642 | 65.9% | ||
| African American/Black | 211 | 21.7% | 1.67* [1.13, 2.46] | 0.79 [0.61, 1.02] |
| Other | 121 | 12.4% | 1.96* [1.09, 3.54] | 0.80 [0.60, 1.07] |
| Parent/guardian | ||||
| No (ref) | 677 | 68.7% | ||
| Yes | 309 | 31.3% | 0.79 [0.55, 1.15] | 0.77* [0.60, .98] |
| Geographic residence | ||||
| Urban (ref) | 597 | 60.6% | ||
| Rural/highly rural | 388 | 39.4% | 0.99 [0.72, 1.38] | 0.92 [0.86, 1.36] |
| OEF/OIF | ||||
| No (ref) | 709 | 71.9% | ||
| Yes | 277 | 28.1% | 0.88 [0.59, 1.32] | 0.79 [0.74, 1.16] |
| Comorbid psychiatric diagnosis | ||||
| None (ref) | 126 | 12.8% | ||
| 1 condition | 418 | 42.1% | 1.43 [0.79, 2.58] | 1.47* [1.01, 2.12] |
| 2+ conditions | 442 | 45.1% | 2.51** [1.49, 4.23] | 2.35** [1.57, 3.52] |
| Comorbid chronic medical conditions | ||||
| None (ref) | 441 | 44.7% | ||
| 1+ conditions | 545 | 55.3% | 1.10 [0.74, 1.65] | 1.11 [0.88, 1.41] |
Note. OEF/OIF = Operation Enduring Freedom/Operation Iraqi Freedom; ref = reference group; AOR = adjusted odds ratio; IIR = incidence rate ratio; CI = confidence interval; odds ratios and incidence rate ratios adjusted for all other demographic and clinical characteristics; missing values possible on each variable.
p < .05
p < .01.
Table 2.
Trauma Exposure Characteristics Associated with VHA Psychotherapy Utilization and Retention among Women Veterans Diagnosed with PTSD
| Any Utilization N=986 | Retention n=729 | |||
|---|---|---|---|---|
| Variable | n | % | AOR [95% CI] | IRR [95% CI] |
|
| ||||
| Trauma Exposure | ||||
| Child physical/sexual abuse | 691 | 73.3% | 1.17 [0.80, 1.70] | 0.91 [0.71, 1.17] |
| Military sexual trauma | 776 | 80.4% | 1.08 [0.71, 1.63] | 1.36* [1.03, 1.82] |
| Combat exposure | 399 | 40.5% | 0.97 [0.71, 1.31] | 0.99 [0.79, 1.25] |
| Post-military interpersonal violence | 428 | 46.5% | 1.32 [0.91, 1.91] | 0.93 [0.72, 1.20] |
Note. AOR = adjusted odds ratio; IIR = incidence rate ratio; CI = confidence interval. Odds ratios and incidence rate ratios adjusted for race, parenting status, and comorbid psychiatric diagnoses, and all other trauma exposure categories; missing values possible on each variable.
p < .05
p < .01.
Table 3 shows descriptive statistics as well as the associations of treatment characteristics and preferences with utilization and retention. Our analytical models examining treatment preferences indicated that gender-related preferences and group-related preferences were significantly associated with psychotherapy retention. Specifically, women veterans who had any gender-related preference met (access to female providers OR access to women-only clinics) or both gender-related preferences met (access to female providers AND access to women-only clinics) had higher retention compared to women veterans who had none of their gender-related preferences met. The effect size for having both gender-related preferences met was significantly greater at p < .05 compared to the effect size for having any gender-related preference met. Additionally, women who had access to group treatment and found it an acceptable form of treatment demonstrated higher retention than women who did not prefer group treatment. Our analytical models examining treatment characteristics (i.e., non-VHA outpatient mental health care utilization; pharmacotherapy use for PTSD) had no significant effects.
Table 3.
Treatment Characteristics and Treatment Preferences and their Associations with VHA Psychotherapy Utilization and Retention among Women Veterans Diagnosed with PTSD
| Any Utilization N=986 | Retention n=729 | |||
|---|---|---|---|---|
| Variable | n | % | AOR [95% CI] | IRR [95% CI] |
|
| ||||
| Outpatient MH care outside VHA |
||||
| No (ref) | 853 | 86.5% | ||
| Yes | 133 | 13.5% | 1.42 [0.90, 2.26] | 0.95 [0.75, 1.20] |
| Pharmacotherapy for PTSD | ||||
| No (ref) | 260 | 26.4% | ||
| Yes | 726 | 73.6% | 0.95 [0.57, 1.60] | 1.06 [0.74, 1.52] |
| Gender-related preferences* | ||||
| None met (ref) | 247 | 33.1% | ||
| Any preference met | 396 | 42.0% | 1.03 [0.61, 1.72] | 1.69** [1.36, 2.12] |
| Both provider and setting preferences met | 240 | 25.4% | 0.80 [0.49, 1.31] | 2.18** [1.66, 2.86] |
| Group-related preferences | ||||
| Do not prefer groups (ref) | 211 | 29.0% | ||
| Groups acceptable | 516 | 71.0% | 1.06 [0.74, 1.53] | 2.22** [1.85, 2.67] |
Note. *Excludes 44 women with neither preference; PTSD = Posttraumatic Stress Disorder; MH = mental health; VHA = Veterans Health Administration; ref = reference group; AOR = adjusted odds ratio; IIR = incidence rate ratio; CI = confidence interval; Odds ratios and rate ratios are adjusted for race, parenting status, comorbid psychiatric diagnoses, and military sexual trauma; odds ratios and incidence rate ratios for non-VA MH care and pharmacotherapy are each adjusted for the other; odds ratios and incidence rate ratios for gender-related preferences and group-related preferences are also each adjusted for the other; missing values possible on each variable.
p < .05
p < .01
Discussion
This study provides insight on the psychotherapy utilization and retention of women veterans with PTSD. The majority of women utilized psychotherapy and engaged with care beyond the initial 3 visits, when drop-out most frequently occurs (Olfson et al., 2009; Oliva et al., 2013). Substantial proportions of women who initiated psychotherapy (41%) received 8 or more psychotherapy visits, which is considered the minimally adequate dose for clinical benefit (DeViva, 2015). This proportion is comparable to the findings of other studies (Doran et al., 2017), suggesting that despite women’s greater likelihood of initiating and completing psychotherapy, more efforts are needed to assure that the majority of individuals who initiate psychotherapy for PTSD receive a clinically meaningful dose.
Most notably, our findings document the importance of care delivered according to patient needs and preferences. Women who received care consistent with their preferences demonstrated greater psychotherapy retention than women whose care was not consistent with their treatment preferences. Perceptions that both gender-related and group-related preferences were met were each independently associated with better retention. Furthermore, results for gender-related preferences suggest that each gender-related preference met conferred significantly greater effects. Taken together, these results suggest that any degree to which we can identify preferences and tailor care may significantly increase retention in psychotherapy. Previous research with this sample found that women with access to their preferred gender-related services are two times more likely to report that these services met their mental health needs compared to women without access to their preferred gender-related services (Kimerling et al., 2015a). Taken together, the current study adds corroborating evidence regarding the importance of providing patient-centered, preference concordant mental health care to women.
While the availability of gender-specialized settings or individual psychotherapy may vary, especially in smaller facilities or community-based clinics, failure to address preferences may effectively restrict access to effective levels of treatment. Patient-provider dialogue regarding patient preferences in PTSD treatment can open the door for shared decisions around options such as telemental health, alternative waiting room arrangements, or other strategies to structure care that will enhance treatment retention. A greater emphasis on patient-centered care that aligns with treatment preferences may be an important part of efforts to promote utilization of evidence-based treatments throughout the system. Since collection of our data, a broad range of VHA policies for mental health care, including services for PTSD and MST, have highlighted the importance of patient-centered care including preferences regarding provider gender, same-gender groups, and other aspects of gender-sensitive care. Further efforts to promote patient centered care, such as decision aids (Watts et al., 2015) show promise.
Several other gender-related factors were also associated with psychotherapy use. Parenting women demonstrated lower psychotherapy retention as compared to other women. Logistical barriers related to attending psychotherapy as a parent (e.g., lack of time or childcare) may prevent parenting women from engaging in psychotherapy, especially given women veterans’ increased likelihood of being a single parent. Alternatively, women veterans who are parents may view psychotherapy or other mental health services as low on the list of many competing priorities for their time. Though non-VA mental health care use was not associated with VHA psychotherapy utilization, parenting women veterans may have better access to non-VHA mental health care either because they have access to health coverage through a partner or co-parent, or because it is more efficient to receive care in the same location that provides care for their family. A more sensitive measure of non-VA psychotherapy utilization may have detected such effects. This finding bears further investigation.
Possibly owing to a greater need for care, women who experienced MST and women with multiple mental health comorbidities showed increased psychotherapy utilization. For all other trauma exposures, women veterans with PTSD received psychotherapy at similar rates. For example, women who experienced post-military interpersonal violence were as likely to receive and engage with care, as were the substantial proportion of women who experienced combat exposure.
Additionally, findings of this study shed light on the association between psychotherapy use and race. Consistent with prior research (Bosworth et al., 2000), we found that African American/Black women and women who identified as neither African American/Black nor White were more likely to utilize psychotherapy than White women, though, no significant differences emerged when examining psychotherapy retention. These findings suggest that, perhaps, African American/Black women and women who identify as neither African American/Black nor White are more likely to utilize psychotherapy due to a greater need for care compared to White women, as has been found in prior studies (Bosworth et al., 2000), but additional efforts may be necessary to keep these women in treatment.
Limitations and Future Directions
Several limitations should be considered in the interpretation of these results. First, although study findings cannot be generalized to women outside VHA, they do highlight important information about psychotherapy among women VHA users that past studies have not reported because women make up only a small proportion of study samples. Second, because psychotherapy utilization was calculated only for the year prior to the survey, this study may not have fully captured psychotherapy utilization intensity by not accounting for psychotherapy utilization that could have occurred prior to the observation period. Methodological work to define and describe episodes of PTSD care could help inform designs for studies of intensity and quality of care. Our study capitalized on the ability to incorporate survey data from a large representative sample, and because surveys were administered subsequent to utilization, we were able to obtain women’s subjective appraisals of their care experiences.
We also note the heterogeneity in definitions and justification for what constitutes a ‘minimally adequate dose’ of psychotherapy in studies of VHA psychotherapy utilization. Most investigations have used eight or nine visits as a cutoff with time frames for visits ranging from 15 weeks (DeViva, 2015) up to 12 months (Maguen et al., 2014). Although the definition used in this study is consistent with several past studies, other research suggests that the therapeutic dose of psychotherapy also depends on session frequency (Reese, Toland, & Hopkins, 2011) and individual patient characteristics (Owen et al., 2015). However, another study which accounted for session frequency as well as number of visits found similar rates of women veterans with PTSD receiving minimally adequate doses of treatment (41% in this study versus 48.3% in that study) (Hebenstreit et al., 2015). This suggests that accounting for session frequency may lead to only slight differences in psychotherapy use.
Finally, we highlight that the present study focused on psychotherapy utilization, but these psychotherapy visits may not have represented one of the evidenced-based treatments (EBTs) recommended for PTSD. To date, there is ongoing progress both in enhancing methods to reliably ascertain evidence-based trauma-focused psychotherapy from administrative data (Maguen et al., 2019), as well as efforts to identify a broader range of psychotherapies that may effectively treat PTSD (Belsher et al., 2019; Gutner et al., 2016). Assuring access to an effective dose of psychotherapy remains essential as this research evolves.
Implications for Practice and/or Policy
Women veterans with PTSD have treatment needs and preferences that may influence their ability to access or obtain clinically beneficial doses of psychotherapy. It is evident that the majority of women veterans with PTSD are receiving some psychotherapy, but many of the factors that influence retention can guide efforts to increase the proportions that receive a clinically meaningful dose. When women are able to obtain treatment aligned with their preferences, retention in mental health treatment is enhanced. These data should inform not only initiatives aimed at enhancing services for women veterans, but also implementation of VHA policies that emphasize respect for patient preferences, shared-decision making, and patient-centered care for all PTSD populations.
Acknowledgements:
This study was funded by the VA HSR&D SDR 12-196. This study is also supported in part by the VA Office of Academic Affiliations and Health Services Research and Development Service Research funds. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
References
- Abrams TE, Vaughan-Sarrazin M, Keane TM, & Richardson K. (2015). Validating administrative records in post-traumatic stress disorder. International Journal of Methods in Psychiatric Research. doi: 10.1002/mpr.1470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agency for Health Care Research and Quality. (2012). Clinical Classifications Software (CCS) for ICD-9-CM’, Agency for Health Care Research and Quality. Retrieved from http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp>2011 [Google Scholar]
- Belsher BE, Beech E, Evatt D, Smolenski DJ, Shea MT, Otto JL, Rosen CS, & Schnurr PP (2019). Present-centered therapy (PCT) for post-traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews. 10.1002/14651858.CD012898.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosworth HB, Parsey KS, Butterfield MI, McIntyre LM, Oddone EZ, Stechuchak KM, & Bastian LA (2000). Racial variation in wanting and obtaining mental health services among women veterans in a primary care clinic. Journal of the National Medical Association, 92(5), 231–236. [PMC free article] [PubMed] [Google Scholar]
- Buchholz KR, Bohnert KM, Pfeiffer PN, Valenstein M, Ganoczy D, Anderson RE, & Sripada RK (2017). Reengagement in PTSD psychotherapy: A case-control study. General Hospital Psychiatry, 48, 20–24. 10.1016/j.genhosppsych.2017.06.009 [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2015). The CMS Chronic Conditions Data Warehouse. Retrieved from http://www.ccwdata.org/chronic-conditions/index.htm
- Clever M, & Segal DR (2013). The demographics of military children and families. Future of Children, 23(2), 13–39. 10.1353/foc.2013.0018 [DOI] [PubMed] [Google Scholar]
- Cook BL, Zuvekas SH, Carson N, Wayne GF, Vesper A, & McGuire TG (2014). Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health Services Research, 49(1), 206–229. 10.1111/1475-6773.12095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Defense. (2008). Enhanced Post-Deployment Health Assessment (PDHA) Process (DD Form 2796). [Google Scholar]
- Department of Veterans Affairs/Department of Defense. (2017). VA/DOD clinical practice guideline for the management of posttraumtic stress disorder and acute stress disorder. https://www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal012418.pdf
- DeViva JC (2014). Treatment utilization among OEF/OIF veterans referred for psychotherapy for PTSD. Psychological Services, 11(2), 179–184. doi: 10.1037/a0035077 [DOI] [PubMed] [Google Scholar]
- Doran JM, Pietrzak RH, Hoff R, & Harpaz-Rotem I. (2017). Psychotherapy Utilization and Retention in a National Sample of Veterans With PTSD. J Clin Psychol. doi: 10.1002/jclp.22445 [DOI] [PubMed] [Google Scholar]
- Durai UNB, Chopra MP, Coakley E, Llorente MD, Kirchner JE, Cook JM, & Levkoff SE (2011). Exposure to trauma and posttraumatic stress disorder symptoms in older veterans attending primary care: Comorbid conditions and self-rated health status. Journal of the American Geriatrics Society, 59(6), 1087–1092. doi: 10.1111/j.1532-5415.2011.03407.x [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, … Beckham JC (2015). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: A meta-analysis. Journal of Anxiety Disorders, 31, 98–107. doi: 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Gaska KA, & Kimerling R. (2018). Patterns of Adverse Experiences and Health Outcomes Among Women Veterans. American Journal of Preventive Medicine, 55(6), 803–811. 10.1016/j.amepre.2018.06.029 [DOI] [PubMed] [Google Scholar]
- Gates MA, Holowka DW, Vasterling JJ, Keane TM, Marx BP, & Rosen RC (2012). Posttraumatic stress disorder in veterans and military personnel: Epidemiology, screening, and case recognition. Psychological Services, 9(4), 361–382. doi: 10.1037/a0027649 [DOI] [PubMed] [Google Scholar]
- Goetter EM, Bui E, Ojserkis RA, Zakarian RJ, Brendel RW, & Simon NM (2015). A systematic review of dropout from psychotherapy for posttraumatic stress disorder among iraq and afghanistan combat veterans. Journal of Traumatic Stress, 28(5), 401–409. doi: 10.1002/jts.22038 [DOI] [PubMed] [Google Scholar]
- Gutner CA, Galovski T, Bovin MJ, & Schnurr PP (2016). Emergence of Transdiagnostic Treatments for PTSD and Posttraumatic Distress. Current Psychiatry Reports, 18(10), 95. 10.1007/s11920-016-0734-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehle-Forbes SM, Harwood EM, Spoont MR, Sayer NA, Gerould H, & Murdoch M. (2017). Experiences with VHA care: a qualitative study of U.S. women veterans with self-reported trauma histories. BMC Women’s Health, 17(1), 38. doi: 10.1186/s12905-017-0395-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frayne SM, Phibbs CS, Saechao F, Friedman SA, Shaw JG, Romodan Y, … Haskell S. (2018). Sourcebook: Women Veterans in the Veterans Health Administration, Volume 4, Longitudinal Trends in Sociodemographics, Utilization, Health Profile, and Geographic Distribution (p. 144). Washington, D.C.: Women’s Health Evaluation Initiative, Women’s Health Services, Veterans Health Administration, Department of Veterans Affairs. [Google Scholar]
- Hebenstreit CL, Madden E, Koo KH, & Maguen S. (2015). Minimally adequate mental health care and latent classes of PTSD symptoms in female Iraq and Afghanistan veterans. Psychiatry Research, 230(1), 90–95. 10.1016/j.psychres.2015.08.028 [DOI] [PubMed] [Google Scholar]
- Katon JG, Lehavot K, Simpson TL, Williams EC, Barnett SB, Grossbard JR, … Reiber GE (2015). Adverse childhood experiences, military service, and adult health. American Journal of Preventive Medicine, 49(4), 573–582. doi: 10.1016/j.amepre.2015.03.020 [DOI] [PubMed] [Google Scholar]
- Kehle-Forbes SM, Meis LA, Spoont MR, & Polusny MA (2016). Treatment Initiation and Dropout from Prolonged Exposure and Cognitive Processing Therapy in a VA Outpatient Clinic. Psychological Trauma: Theory, Research, Practice, and Policy, 8(1), 107–114. 10.1037/tra0000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimerling R, Bastian LA, Bean-Mayberry BA, Bucossi MM, Carney DV, Goldstein KM, … Frayne SM (2015a). Patient-centered mental health care for female veterans. Psychiatr Serv, 66(2), 155–162. doi: 10.1176/appi.ps.201300551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimerling R, & Baumrind N. (2005). Access to specialty mental health services among women in California. Psychiatr Serv, 56(6), 729–734. doi: 10.1176/appi.ps.56.6.729 [DOI] [PubMed] [Google Scholar]
- Kimerling R, Pavao J, Greene L, Karpenko J, Rodriguez A, Saweikis M, & Washington DL (2015b). Access to mental health care among women Veterans: is VA meeting women’s needs? Med Care, 53(4 Suppl 1), S97–S104. doi: 10.1097/MLR.0000000000000272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DW, King LA, & Vogt DS (2003). Manual for the Deployment Risk and Resilience Inventory (DRRI): A Collection of Measures for Studying Deployment-Related Experienced of Military Veterans. Boston, MA: National Center for PTSD. [Google Scholar]
- Koo KH, Madden E, & Maguen S. (2015). Race-Ethnicity and Gender Differences in VA Health Care Service Utilization Among U.S. Veterans of Recent Conflicts. Psychiatric Services, 66(5), 507–513. 10.1176/appi.ps.201300498 [DOI] [PubMed] [Google Scholar]
- Le QA, Doctor JN, Zoellner LA, & Feeny NC (2014). Cost-effectiveness of prolonged exposure therapy versus pharmacotherapy and treatment choice in posttraumatic stress disorder (the optimizing ptsd treatment trial): A doubly randomized preference trial. Journal of Clinical Psychiatry, 75(3), 222–230. doi: 10.4088/JCP.13mO8719 [DOI] [PubMed] [Google Scholar]
- Maguen S, Li Y, Madden E, Seal KH, Neylan TC, Patterson OV, … Shiner B. (2019). Factors associated with completing evidence-based psychotherapy for PTSD among veterans in a national healthcare system. Psychiatry Research, 274, 112–128. 10.1016/j.psychres.2019.02.027 [DOI] [PubMed] [Google Scholar]
- Maguen S, Madden E, Neylan TC, Cohen BE, Bertenthal D, & Seal KH (2014). Timing of mental health treatment and PTSD Symptom improvement among Iraq and Afghanistan veterans. Psychiatr Serv, 65(12), 1414–1419. doi: 10.1176/appi.ps.201300453 [DOI] [PubMed] [Google Scholar]
- Nobles CJ, Valentine SE, Zapeda ED, Ahles EM, Shtasel DL, & Marque L, (2017). Usual course of treatment and predictors of treatment utilization for patients with posttraumatic stress disorder. Journal of Clinical Psychiatry, 78(5), e559–e566. 10.4088/JCP.16m10904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Mojtabai R, Sampson NA, Hwang I, Druss B, Wang PS, … Kessler RC (2009). Dropout from outpatient mental health care in the United States. Psychiatr Serv, 60(7), 898–907. doi: 10.1176/appi.ps.60.7.898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliva EM, Bowe T, Harris AH, & Trafton JA (2013). Datapoints: false starts in psychotherapy for substance use disorders and PTSD in the VHA. Psychiatr Serv, 64(8), 722. doi: 10.1176/appi.ps.201300145 [DOI] [PubMed] [Google Scholar]
- Owen J, Adelson J, Budge S, Wampold B, Kopta M, Minami T, & Miller S. (2015). Trajectories of Change in Psychotherapy. J Clin Psychol, 71(9), 817–827. doi: 10.1002/jclp.22191 [DOI] [PubMed] [Google Scholar]
- Phibbs CS, Cowgill EH, & Fan AY (2013). Guide to the PSSG Enrollee FileGuidebook. Menlo Park, CA: VA Palo Alto, Health Economics Resource Center. Retrieved from http://www.herc.research.va.gov/files/BOOK_739.pdf [Google Scholar]
- Pull CN, & Pull CB (2014). Current status of treatment for posttraumatic stress disorder: Focus on treatments combining pharmacotherapy and cognitive- behavioral therapy. International Journal of Cognitive Therapy, 7(2), 149–161. doi: 10.1521/ijct.2014.7.2.149 [DOI] [Google Scholar]
- Reese RJ, Toland MD, & Hopkins NB (2011). Replicating and extending the good-enough level model of change: considering session frequency. Psychother Res, 21(5), 608–619. doi: 10.1080/10503307.2011.598580 [DOI] [PubMed] [Google Scholar]
- Rosen CS, Greenbaum MA, Fitt JE, Laffaye C, Norris VA, & Kimerling R. (2011). Stigma, help-seeking attitudes, and use of psychotherapy in veterans with diagnoses of posttraumatic stress disorder. Journal of Nervous and Mental Disease, 199(11), 879–885. 10.1097/NMD.0b013e3182349ea5 [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Bovin MJ, & Marx BP (2009). Posttraumatic stress disorder and quality of life: Extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical Psychology Review, 29(8), 727–735. 10.1016/j.cpr.2009.08.006 [DOI] [PubMed] [Google Scholar]
- Simiola V, Neilson EC, Thompson R, & Cook JM (2015). Preferences for trauma treatment: A systematic review of the empirical literature. Psychological Trauma: Theory, Research, Practice and Policy, 7(6), 516–524. doi: 10.1037/tra0000038 [DOI] [PubMed] [Google Scholar]
- Sohal H, Eldridge S, & Feder G. (2007). The sensitivity and specificity of four questions (HARK) to identify intimate partner violence: a diagnostic accuracy study in general practice. BMC Family Practice, 8, 49. doi: 10.1186/1471-2296-8-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoont MR, Murdoch M, Hodges J, & Nugent S. (2010). Treatment receipt by veterans after a PTSD diagnosis in PTSD, mental health, or general medical clinics. Psychiatr Serv, 61(1), 58–63. doi: 10.1176/appi.ps.61.1.58 [DOI] [PubMed] [Google Scholar]
- StataCorp. (2011). Stata Statistical Software: Release 12. College Station, TX: StataCorp LP. [Google Scholar]
- Trafton JA, Greenberg G, Harris AHS, Tavakoli S, Kearney L, McCarthy J, … Schohn M. (2013). VHA mental health information system: Applying health information technology to monitor and facilitate implementation of VHA uniform mental health services handbook requirements. Medical Care, 51(3 SUPPL. 1), S29–S36. doi: 10.1097/MLR.0b013e31827da836 [DOI] [PubMed] [Google Scholar]
- VA Information Resource Center. (2011). VHA Medical SAS® Outpatient Datasets and Inpatient Encounters Dataset FY2009: VIReC Research User Guide. http://www.virec.research.va.gov/DataSourcesName/Medical-SAS-Datasets/MedSAS-Outpt-RUG/MedSAS-RUG-Outpt.htm. Retrieved from: http://vaww.virec.research.va.gov/RUGs/MedSAS/RUG-MedSAS-OP-FY09-RA.pdf
- VA Information Resource Center. (2008). VIReC Research User Guide: VHA Pharmacy Prescription Data, 2nd Edition. Hines, IL: Department of Veterans Affairs. [Google Scholar]
- VA. Programs for veterans with post-traumatic stress disorder (PTSD). Washington, DC: Veterans Health Administration; 2019. (VHA Directive 1160.03(1)). [Google Scholar]
- Valenstein-Mah H, Kehle-Forbes S, Nelson D, Danan ER, Vogt D, & Spoont M. (2019). Gender Differences in Rates and Predictors of Individual Psychotherapy Initiation and Completion Among Veterans Health Administration Users Recently Diagnosed With PTSD. Psychological Trauma: Theory, Research, Practice, and Policy. 10.1037/tra0000428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts BV, Schnurr PP, Zayed M, Young-Xu Y, Stender P, & Llewellyn-Thomas H. (2015). A Randomized Controlled Clinical Trial of a Patient Decision Aid for Posttraumatic Stress Disorder. Psychiatric Services, 66(2), 149–154. 10.1176/appi.ps.201400062 [DOI] [PubMed] [Google Scholar]
- Wolfe JW, Kimerling R. Brown PJ, Chrestman KR, & Levin K. (1996). Psychometric review of The Life Stressor Checklist-Revised. In Stamm BH (Ed.), Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press. [Google Scholar]