Introduction:
Orthopaedic surgery is recognized as one of the most popular but least diverse medical subspecialties. Although significant efforts have been made in recent years to improve gender diversity, orthopaedic surgery continues to lag behind other surgical subspecialties. A recent study predicted that it would take 217 years for orthopaedic surgery to reach gender parity matching the 36.3% of practicing female physicians in the United States. The purpose of our study was to evaluate the annual percentages of female medical student applicants in orthopaedic surgery over the past 15 years and to determine when this gender parity percentage may be reached among residency applicants.
Methods:
The Electronic Residency Application Service was queried for orthopaedic residency applicant data from 2007 to 2022. The annual percentage of female applicants as well as the annual change in percentage of female applicants was recorded. A best-fit trendline was calculated and extrapolated to predict future rates of female applicants.
Results:
The percent of female applicants has increased from 11.8% in 2007 to 23.0% in 2022. Between 2007 and 2022, there were 9 years with annual increases in percentage of females applying into orthopaedic surgery with a statistically significant increase in 4 of those years (2008, 2014, 2019, and 2022). There were 6 years with annual decreases in percentage of females applying to orthopaedic surgery, none of which were statistically significant. The best-fit curve is exponential with a correlation coefficient of 0.8 (p < 0.001). This predicts reaching the predetermined gender parity percentage of 36.3% in 16 years.
Conclusion:
In the past 15 years, there has been a near-doubling in the percentage of female medical students applying to orthopaedic surgery residency. Although orthopaedic surgery remains the least gender-diverse field of medicine, these trends are encouraging and support the initiatives currently in place including early education and increased mentorship to help close the gender gap in orthopaedic surgery.
Introduction
Over the past century, the medical field has made great strides regarding gender equality. In 2019, 50.5% of medical students were female, and for the first time, women comprised over half of currently enrolled medical students in the United States1. Although women compose 50.8% of the US population, the overall proportion of women in medicine is 36.3%2,3. Based on the Association of American Medical College's physician specialty report, although 38% of practicing physicians in nonsurgical specialties are female, there remains a paucity of women pursuing careers in surgical specialties (29%), especially orthopaedic surgery4,5. For decades, orthopaedic surgery has reported the lowest percentage of women, whereas other surgical specialties are approaching more equal gender representation6-9. One recent report found that only 18.3% of current orthopaedic surgery residents are women compared with 46% of general surgery residents and 40.3% of otolaryngology residents10.
It has been shown that a more diverse, gender-balanced workforce may improve patient care11,12. Specifically, gender equity leads to improved patient satisfaction and patient-centered communication in addition to enriching the collective aptitude and performance of healthcare teams13-15. Despite these crucial benefits, gender inequality remains a major challenge in medicine, particularly within orthopaedic surgery. Several studies have investigated possible solutions to gender disparity in orthopaedic surgery in addition to ongoing research assessing our annual progress16-24. Acuna et al. evaluated the time it would take for the representation of women orthopaedic surgeons to match the proportion of all women physicians and found that it would take 217 years (or by 2,236) to reach gender parity with the overall medical profession, assuming a constant national growth rate of 2% per year from 201925.
A recent study investigating match rates of traditionally underrepresented groups in orthopaedic surgery, including females, found that female applicants applying to orthopaedic surgeries successfully match at a rate reflective of their application rates26. This thereby suggests that an increasing number of female applicants will likely lead to a predictable increase in female orthopaedic surgery residents and ultimately practicing physicians.
Therefore, the purpose of this study was to evaluate the annual percentages of female medical student applicants in orthopaedic surgery over the past 15 years and to determine when the gender parity percentage of 36.3% may be reached among residency applicants.
Methods
The Electronic Residency Application Service (ERAS) was queried in December 2022 for all publicly available data on orthopaedic residency applications from 2007 to 2022. ERAS is a service associated with the Association of American Medical Colleges (AAMC), which medical students use to submit their applications to residency programs in various specialties. Annually, the AAMC releases a data set with the total number of applicants, applications per program, as well as applicants by medical school type, self-identified gender, self-identified race, and alpha omega alpha status. These data are also stratified based on specialties. No individual level data are made available.
Using these data sets, we identified the total number of applicants and number of female applicants for the given years. The proportion of females per given year were calculated as a percentage of total applicants. The change in annual percentages was compared using z-scores. Regression was used to calculate the best fit trendline and extrapolated using Microsoft Excel. Statistical significance was defined as p < 0.05.
Results
The total number of applicants, female applicants, percent of female applicants, and annual percentage change are found in Table I. The percentage of female applicants increased from 11.8% in 2007 to 23.0% in 2022 demonstrating a 11.2% percent increase over the past 15 years. Between 2007 and 2022, there were 9 years (2008, 2010, 2011,2014, 2015, 2017, 2019, 2020, and 2022) with annual increases in percentage of females applying into orthopaedic surgery with a statistically significant increase in 4 of those years (2008, 2014, 2019, and 2022). There were 6 years (2009, 2012, 2013, 2016, 2018, and 2021) with annual decreases in percentage of females applying to orthopaedic surgery, none of which were statistically significant. The data demonstrate an exponential increase in the number of female applicants over the study period (r2 = 0.8, p < 0.001, Fig. 1). It is estimated that there will be greater than 36.3% female applicants by 2038 if current trends continue.
Fig. 1.
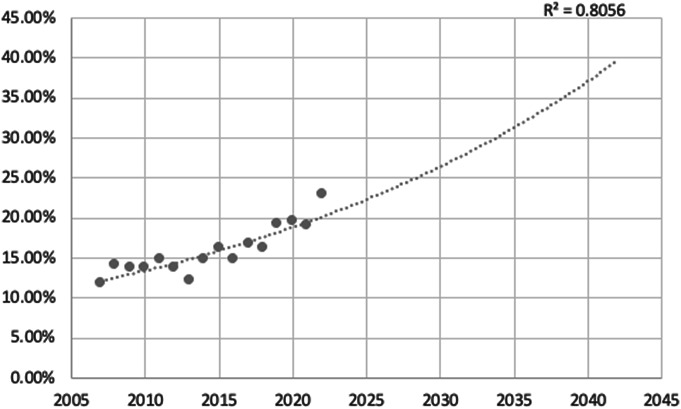
The annual percentage of female applicants to orthopaedic surgery by the Electronic Residency Application Service (ERAS) from 2007 to 2022. The best-fit curve demonstrates an exponential increase in the number of female applicants over the study period (r2 = 0.8, p < 0.001) and predicts reaching the predetermined gender parity percentage of 36.3% in 16 years.
Table I.
Annual breakdown of residency applications in orthopaedic surgery including the total number of applicants, number of females, percent female applicants, and the annual change in percentage of female applicants from 2007-2022*
| Year | Total | Female | % Female | Change | Z score | p |
|---|---|---|---|---|---|---|
| 2007 | 1,420 | 168 | 11.83% | |||
| 2008 | 1,360 | 193 | 14.19% | 2.36% | 1.85 | 0.03 |
| 2009 | 1,368 | 188 | 13.74% | −0.45% | 0.34 | 0.36 |
| 2010 | 1,539 | 213 | 13.84% | 0.10% | 0.076 | 0.47 |
| 2011 | 1,520 | 226 | 14.87% | 1.03% | 0.81 | 0.21 |
| 2012 | 1,370 | 189 | 13.80% | −1.07% | 0.82 | 0.21 |
| 2013 | 1,312 | 160 | 12.20% | −1.60% | 1.23 | 0.11 |
| 2014 | 1,582 | 234 | 14.79% | 2.59% | 2.03 | 0.021 |
| 2015 | 1,324 | 216 | 16.31% | 1.52% | 1.13 | 0.13 |
| 2016 | 1,309 | 193 | 14.74% | −1.57% | 1.11 | 0.13 |
| 2017 | 1,474 | 247 | 16.76% | 2.02% | 1.45 | 0.073 |
| 2018 | 1,387 | 226 | 16.29% | −0.47% | 0.33 | 0.37 |
| 2019 | 1,577 | 304 | 19.28% | 2.99% | 2.11 | 0.017 |
| 2020 | 1,699 | 334 | 19.66% | 0.38% | 0.28 | 0.39 |
| 2021 | 1,766 | 337 | 19.08% | −0.58% | 0.43 | 0.33 |
| 2022 | 1,739 | 400 | 23.00% | 3.92% | 2.85 | 0.0022 |
Bold indicates p < 0.05.
2020 is the first year of combined DO/MD match.
Discussion
The present work sought to determine how the percentage of women applying to orthopaedic surgery residency programs has changed over the past 15 years using data from the AAMC ERAS database from 2007 to 2022. We found that female application rates in orthopaedic surgery have nearly doubled from 11.8% in 2007 to 23.0% in 2022. We estimate that if the current trends continue, it will take approximately 16 years to reach the percentage of female applicants needed to achieve the previously described gender parity percentage of 36.3% in orthopaedic surgery residency applicants. To the best of our knowledge, our study is the first to use this simple and direct approach to measure our progress toward gender parity in orthopaedic surgery residency applicants.
The American Orthopaedic Association and the American Academy of Orthopaedic Surgeons (AAOS) recognized the significant deficits in diversity in the field of orthopaedic surgery in the late 1990s27. With the goal of increasing gender diversity, several initiatives and programs have been developed including the Ruth Jackson Orthopaedic Society (RJOS), Nth Dimensions as well as the Perry Outreach Program (POP) and Medical Student Outreach Program (MSOP), the latter 2 which are both components of the Perry Initiative. Close partnership with the leadership of such organizations has remained central to the AAOS Strategic Plan for closing the gender gap in orthopaedics.
RJOS was founded in 1983 as a support and networking group for women orthopaedic surgeons that has grown from 42 women to more than 1,000 members. The women at the first meeting felt that they shared many challenges which could best be solved by pooling resources, ranging from issues in orthopaedic practice/residency to surviving motherhood. Since then, the RJOS has promoted women in orthopaedics for over 40 years through numerous professional development opportunities and resources such as their Mentoring Ambassador Program as well as annual scholarship, grant, and fellowship opportunities for medical students, residents, and fellows. Their efforts can be highlighted by the fact that 65 (80%) of the 81 female RJOS scholarship winners are currently practicing orthopaedic surgeons or are in orthopaedic surgery residency19.
The Perry Initiative is a nonprofit organization that was founded in 2009 with a mission to provide young women with increased exposure to orthopaedic surgery and engineering9. The POP and the MSOP have been successful in their commitment to inspiring women in high school and medical school, 2 critical points on the path to a career in orthopaedic surgery28. The MSOP has been ongoing at medical centers nationwide and has provided orthopaedic-specific exposure and mentoring opportunities to first and second year female medical students since 2012. A recent study found that the orthopaedic surgery match rate for program participants was 31% in their first graduating class in 2015 and 28% in their second class in 2016. In addition, the match rate for program alumnae was twice the percentage of females in current orthopaedic residency classes28.
In addition to the 2 above initiatives, Nth Dimensions as well have many subspecialties including the Arthroscopy Association of North America, the Orthopaedic Trauma Association (OTA), the American Orthopaedic Foot and Ankle Society (AOFAS), and American Association of Hip and Knee Surgeons (AAHKS) have put forth major efforts to improve gender diversity in orthopaedics through the creation of gender and diversity task forces, initiatives, and committees.
This study predicts that it will take approximately 16 years for female medical student application rates in orthopaedic surgery to achieve a previously defined rate of gender parity in orthopaedic surgery. Although this study does not directly address match rates, a recent study suggests that female applicants match into orthopaedics concordant with their application rates26. Further studies are needed to validate these findings. A prior study estimated that it would take 217 years to achieve gender parity among practicing physicians25. The difference in time lag between these studies is attributable to several factors. It takes several years for current applicants to become practicing orthopaedic surgeons. Thus, recent increases in female applicants are not yet reflected in the numbers of practicing female orthopaedic surgeons. In addition, the number of graduating residents each year is only a small percentage of the number of practicing orthopaedic surgeons in the United States. Thus, the annual increases observed here will only result in small annual changes in the gender breakdown of practicing surgeons. Although it will take substantially longer for the national body of practicing orthopaedic surgeons to achieve this percentage of gender parity, it is encouraging that the percentage of female applicants applying in orthopaedic surgery has been increasing exponentially. This trend suggests that the organizations and initiatives that have been implemented are not only effective at fostering interest but are also successfully helping women to match in orthopaedic surgery.
There are several limitations to this study. First, the combined allopathic and osteopathic match beginning in 2020 increased both the total number of applicants and number of female applicants. To help mitigate this, we used the annual percentage of women applying to orthopaedic surgery in this study vs. the absolute number of female applicants. Second, the percentage goal for gender parity was based on a prior study, which used the percentage of women physicians in the United States in 2019. Future studies should consider analyzing gender parity using an updated percentage that is reflective of the proportion of women physicians today, as this is expected to increase as medical school graduates are now greater than 50% female.
Conclusion
We found that the proportion of females applying into orthopaedic surgery will take approximately 16 years (by 2038) to achieve a previously defined gender parity percentage of 36.3%, assuming current trends continue. These findings highlight how the current state of medical education is constantly evolving, as well as the impact of the many initiatives to improve gender disparity in orthopaedics29. Diversity in medicine provides inclusive patient care, as well as improved learning environments for training physicians. Although orthopaedic surgery currently remains the least gender diverse surgical specialty and female representation in the field is still far less than males, our findings suggest that we are moving in the right direction. Continued efforts can fortify existing programs and initiatives, as well as discover new strategies that will maintain the current trend of more women applying and matching into orthopaedic surgery.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, New York
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A516).
Contributor Information
Camille Pinpin, Email: cpinpin@northwell.edu.
Peter B. White, Email: pwhite11@northwell.edu.
Kate W. Nellans, Email: knellans@northwell.edu.
Adam D. Bitterman, Email: abitterman@northwell.edu.
Mary K. Mulcahey, Email: mary.mulcahey.md@gmail.com.
References
- 1.The Association of American Medical Colleges. The Majority of U.S. Medical Students Are Women, New Data Show; 2010. Available at: https://www.aamc.org/news-insights/press-releases/majority-us-medical-students-are-women-new-data-show. Accessed December 19, 2022. [Google Scholar]
- 2.Department of Commerce, US. U.S. Census Bureau QuickFacts: United States. Census Bureau QuickFacts; 2021. Available at: https://www.census.gov/quickfacts/fact/table/US/LFE046219. Accessed July 4, 2021. [Google Scholar]
- 3.Active Physicians by Sex and Specialty. AAMC: Physician Specialty Data Report; 2019. Available at: https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-sex-and-specialty-2019. Accessed July 4, 2021. [Google Scholar]
- 4.The Association of American Medical Colleges. Current Trends in Medical Education; 2016. Available at: https://www.aamcdiversityfactsandfigures2016.org/report-section/section-3/#figure-16. Accessed December 19, 2022. [Google Scholar]
- 5.AAMC. Active physicians by sex and specialty, 2021. Available at: https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-sex-specialty-2021. Accessed February 16, 2023. [Google Scholar]
- 6.Haffner MR, Van BW, Wick JB, Le HV. What is the trend in representation of women and under-represented minorities in orthopedic surgery residency? Clin Orthop Relat Res. 2021;479(12):2610-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties: a comparative study. J Bone Joint Surg Am. 2010;92:2328-35. [DOI] [PubMed] [Google Scholar]
- 8.Poon S, Kiridly D, Mutawakkil M, Wendolowski S, Gecelter R, Kline M, Lane LB. Current trends in sex, race, and ethnic diversity in orthopaedic surgery residency. J Am Acad Orthop Surg. 2019;27:e725-e733. [DOI] [PubMed] [Google Scholar]
- 9.Harbold D, Dearolf L, Buckley J, Lattanza L. The Perry initiative's impact on gender diversity within orthopedic education. Curr Rev Musculoskelet Med. 2021;14(6):429-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Association of American Medical Colleges. Report on Residents: 2021-22 Active Residents; 2022. Available at: https://www.aamc.org/data-reports/students-residents/interactive-data/report-residents/2022/table-b3-number-active-residents-type-medical-school-gme-specialty-and-gender. Accessed December 20, 2022. [Google Scholar]
- 11.Abtahi AM, Presson AP, Zhang C, Saltzman CL, Tyser AR. Association between orthopaedic outpatient satisfaction and non-modifiable patient factors. J Bone Joint Surg Am. 2015;97:1041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmid Mast M, Hall JA, Roter DL. Disentangling physician sex and physician communication style: their effects on patient satisfaction in a virtual medical visit. Patient Educ Couns. 2007;68:16-22. [DOI] [PubMed] [Google Scholar]
- 13.Dineen HA, Patterson JMM, Eskildsen SM, Gan ZS, Li Q, Patterson BC, Draeger RW. Gender preferences of patients when selecting orthopaedic providers. Iowa Orthop J. 2019;39:203-10. [PMC free article] [PubMed] [Google Scholar]
- 14.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288:756-64. [DOI] [PubMed] [Google Scholar]
- 15.Woolley AW, Chabris CF, Pentland A, Hashmi N, Malone TW. Evidence for a collective intelligence factor in the performance of human groups. Science. 2010;330:686-8. [DOI] [PubMed] [Google Scholar]
- 16.Miller EK, LaPorte DM. Barriers to women entering the field of orthopedic surgery. Orthopedics. 2015;38(9):530-3. [DOI] [PubMed] [Google Scholar]
- 17.Lillemoe KD, Ahrendt GM, Yeo CJ, Herlong HF, Cameron JL. Surgery: still an “old boys' club.” Surgery. 1994;116(2):255-9. [PubMed] [Google Scholar]
- 18.Summers MA, Matar RN, Denning JR, Dixon TL, Ramalingam WG, Asghar FA, Grawe BM. Closing the gender gap: barriers to success for recruitment and retention of the female orthopaedic surgery applicant. JBJS Rev. 2020;8(5):e0211. [DOI] [PubMed] [Google Scholar]
- 19.Vajapey S, Cannada LK, Samora JB. What proportion of women who received funding to attend a Ruth Jackson Orthopaedic Society meeting pursued a career in orthopaedics? Clin Orthop Relat Res. 2019;477(7):1722-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mulcahey MK, Nemeth C, Trojan JD, O'Connor MI. The perception of pregnancy and parenthood among female orthopaedic surgery residents. J Am Acad Orthop Surg. 2019;27:527-32. [DOI] [PubMed] [Google Scholar]
- 21.Bohl DD, Iantorno SE, Kogan M. Inappropriate questions asked of female orthopaedic surgery applicants from 1971 to 2015: a cross-sectional study. J Am Acad Orthop Surg. 2019;27:519-26. [DOI] [PubMed] [Google Scholar]
- 22.Chambers CC, Ihnow SB, Monroe EJ, Suleiman LI. Women in orthopaedic surgery: population trends in trainees and practicing surgeons. J Bone Joint Surg Am. 2018;100:e116. [DOI] [PubMed] [Google Scholar]
- 23.Ghert M, Krell ES, Potter JS, Ranpura A, Beebe KS. How well represented are women orthopaedic surgeons and residents on major orthopaedic editorial boards and publications? Clin Orthop Relat Res. 2020;478:1569-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poon SC, Nellans K, Gorroochurn P, Chahine NO. Race, but not gender, is associated with admissions into orthopaedic residency programs. Clin Orthop Relat Res. 2022;480(8):1441-9. Erratum in: Clin Orthop Relat Res. 2022 Aug 1;480(8):1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Acuña AJ, Sato EH, Jella TK, Samuel LT, Jeong SH, Chen AF, Kamath AF. How long will it take to reach gender parity in orthopaedic surgery in the United States? An analysis of the national provider identifier registry. Clin Orthop Relat Res. 2021;479:2759-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.White PB, Chen MM, Bitterman AD, Oni JK, Zacchilli MA, Poon SC, Cohn RM. Residency match rates in orthopedic surgery based on gender, under-represented in medicine status and degree type. JB JS Open Access. 2023;8(1):e22.00143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Onuoha AC, Meadows AM, Faraj MT, Skinner MM, Day C, Ravi K. Comparative analysis of racial and gender diversity in orthopedic surgery applicants and residents from 2007 and 2019. J Orthopaedic Experience Innovation. 2022. [Google Scholar]
- 28.Lattanza LL, Meszaros-Dearolf L, O'Connor MI, Ladd A, Bucha A, Trauth-Nare A, Buckley JM. The Perry initiative's medical student Outreach program recruits women into orthopaedic residency. Clin Orthop Relat Res. 2016;474(9):1962-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Myers TG, Marsh JL, Nicandri G, Gorczyca J, Pellegrini VD, Jr. Contemporary issues in the acquisition of orthopaedic surgical skills during residency: competency-based medical education and simulation. J Bone Joint Surg Am. 2022;104(1):79-91. doi. [DOI] [PubMed] [Google Scholar]


