Abstract
Introduction:
A higher prevalence of osteoporosis and osteopenia, as well as an increased risk of fracture is seen in patients with HIV infection. Anti-retroviral therapy (ART) is the one of the factors associated with pathological fractures in those patients. We present one case with multiple pathological fractures secondary to severe osteoporosis in a known case of HIV on Tenofovir-based ART. The patient was managed with a combined surgical and conservative approach with a satisfactory outcome at 1-year follow-up.
Case Report:
We analyzed a 35-year-old female patient with HIV infection on ART for 5 years. She was diagnosed with right-sided subtrochanteric femur and bilateral forearm fracture and stress fracture in the left lower limb. Tenofovir was substituted with Zidovudine before surgery. Subtrochanteric femur fracture and right forearm fracture were managed surgically, whereas the other fractures were managed conservatively. The patient was followed up till 1 year and assessed with serial X-rays, blood investigations, Harris Hip Score, and Upper Extremity Functional Index. Functional outcome in all four limbs was found to be satisfactory.
Conclusion:
The patient taking ART based on Tenofovir should be monitored for pathological fractures. ART-induced fractures can be managed surgically and conservatively like any other pathological fracture. Tenofovir-containing regimens may be gradually replaced with alternative regimens for the treatment of HIV infection, especially in those at a higher risk for fragility fractures.
Keywords: HIV, tenofovir, antiretroviral therapy, pathological fracture, osteopenia, osteoporosis
Learning Point of the Article:
One should have a high index of suspicion for pathological fracture in patients taking Tenofovir-based ART. These fractures can be managed surgically or conservatively, and the treatment can be changed to a non-Tenofovir-containing regimen.
Introduction
There is approximately 37.7 million people across the globe are living with HIV infection. Of these, 36 million were adults and 1.7 million were children aged 0–14 years, more than half were women and girls. Dual-energy X-ray absorptiometry (DEXA) is globally accepted as a standard technique for measuring bone mineral density (BMD). Osteoporosis and osteopenia predispose to fractures, thereby causing morbidity and increasing the risk for mortality. Regardless of beneficial increase in survival, the use of anti-retroviral therapy (ART) in people living with HIV (PLWHIV) is associated with low BMD [1]. Up to 50% of HIV-infected patients on highly active ART have osteopenia or osteoporosis and 21% of these patients have severe osteoporosis as determined by DEXA [2]. Apart from ART, factors such as a lack of physical activity, low body mass index, female sex, older age, deficiencies of calcium and vitamin D, depression, contraception use, smoking, and alcohol use are also believed to contribute to high prevalence of low BMD among PLWHIV. We present one case of multiple pathological fractures secondary to severe osteoporosis in a known case of HIV on a Tenofovir-based ART.
Figure 1.

X-ray Pelvis with both hip showing right sided subtrochanteric femur fracture.
Figure 2.

X-ray right sided femur lateral view showing subtrochanteric femur fracture.
Figure 3.

X-ray Right forearm anteroposterior view showing radius and ulna shaft fracture.
Case Report
A 38-year-old female presented with complaints of pain in both upper limbs and right hip and the inability to walk for 1-month duration without any history of trauma. She was a known case of retroviral disease detected 5 years ago, for which she took ART-containing Tenofovir, Lamivudine, and Efavirenz since past 5 years. Among this tenofovir, has a known side effect of osteoporosis. Clinical findings were consistent with fractures in both forearm and right proximal femur. X-ray showed right-sided subtrochanteric femur fracture, right-sided radius and ulna shaft fracture, and left-sided ulna shaft fracture and generalized osteopenia.
Skeletal survey detected stress fractures in left subtrochanteric femur and distal fibula shaft.
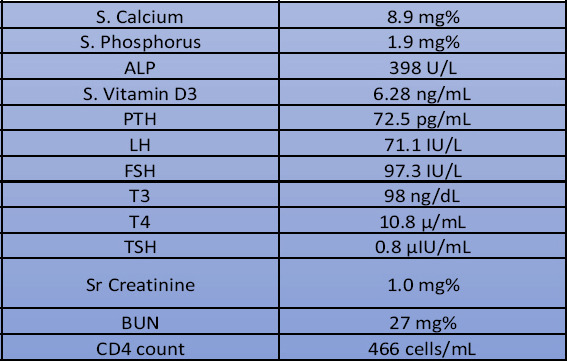
She also had hypercalciuria, hypophosphatemia, and metabolic acidosis with lower Vitamin D3 and elevated ALP levels. USG neck showed normal thyroid and parathyroid glands. Blood investigations are shown in Table 1.
Table 1.
Initial blood investigations.
These investigations pointed diagnosis toward ART-induced Fanconi syndrome [3] and pathological fractures. The patient had pain in both upper limbs initially. One week later, she developed hip pain. Upper limb fractures occurred first, followed by a right subtrochanteric femur fracture. We started her on oral calcium and Vitamin D supplementation. In ART Regimen, tenofovir was stopped and Zidovudine added after consulting infectious disease department. Right sided subtrochanteric femur fracture operated with proximal femur nail and right upper limb fractures with titanium elastic nail. Left-sided ulna shaft fracture conservatively managed with closed reduction and cast. Left lower limb fracture is also managed conservatively. The patient was followed up with serial X-rays and blood investigations at 3, 6, 9, and 12 months and assessed with Harris Hip Score (HHS) [4] and Upper Extremity Functional Index (UEFI) [5].
Figure 4.

X-ray both forearms lateral view.
Figure 5.

Skeletal survey detected unicortical fracture in right subtrochanteric femur and distal fibula shaft old fracture.
Figure 6.

X-ray showing healed right sided subtrochanteric femur fracture at 1 year post surgery.
Figure 7.

X-ray showing healed right sided subtrochanteric femur fracture at 1 year post surgery.
Figure 8.

X-ray showing healed right sided radius and ulna shaft fracture at 1 year post surgery.
Figure 9.

X-ray showing healed left sided ulna shaft fracture managed conservatively with cast.
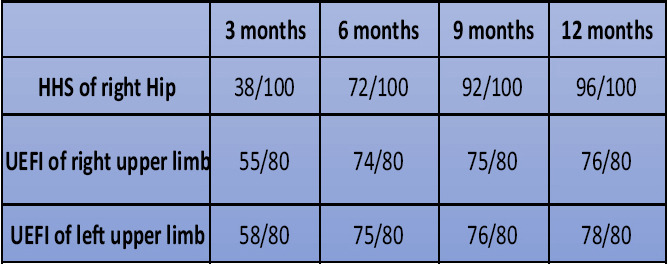
The patient was started on full weight-bearing walking at 6-week post-surgery. At 3-month post–surgery, functional assessment of both upper limb and lower limbs showed the patient having slight difficulty in household activities and mobilization was limited within the home. Blood parameters were also showed normal values by the end of 3 months. Follow-up blood investigation showed satisfactory levels of CD4 cells count. At 9-month postoperative, the patient had slight occasional pain in the right hip but walked without limp and support. Currently, she uses public transport and is able to squat and sit crossed legged without any difficulty. She is able to walk and climb stairs without any discomfort. Active flexion of right hip is 0–120°, abduction of 0–40, adduction of 0–40, internal rotation of 0–30, and external rotation of 0–40° at 12-month post-surgery. Implant removal is planned once bone quality is improved. Lower limb implant is planned to remove only if the patient has pain or implant loosening.
Discussion
HIV-infected patients show the high prevalence of osteopenia and osteoporosis. The pathogenesis of these bone metabolism disorders in HIV infection is still a question. Some studies shows HIV infection itself affect bone density by activation of T-lymphocytes directly or indirectly [6]. Osteopenia is attributed to highly active ART, also especially tenofovir and retroviral protease inhibitor. Initiation of ART, irrespective of regimen has been associated with increase in bone loss in PLWHIV [7]. It has been found that there is a decrease of about 2–6% in BMD in the first 2 years after initiation of ART regardless of the regimen [8]. Although Tenofovir-based regimens are associated with more bone loss than other regimens [9], this could be suggestive of an independent effect of tenofovir on bone demineralization regardless of host, viral, and immunological factors. The WHO recommends tenofovir-containing ART as the first-line treatment regimens in developing countries [10]. Rebolledo et al. [11] described pathological femur neck fracture on the right and intertrochanteric femur fracture on the left side, in a 54-year-old patient with HIV infection on ART. Both the fractures were surgically treated and they united uneventfully. Marco et al. [12] described bilateral femur neck fracture and distal end radius fracture in a 14-year-old female on ART. Hip fractures were operated, and wrist fractures were managed with closed reduction and cast. They concluded that HIV and ART can lead to unrecognized stress fractures. In a 51-year-old male who was on ART including Adefovir and Tenofovir, Brim et al. [13] described a case of left femur neck fracture and right intertrochanteric femur fracture. They highlighted the importance of monitoring not only for renal impairment but also for bone disease in patients receiving tenofovir. A bilateral subtrochanteric femur pathological fracture is reported by Rajnish et al. [14] in their study, in which a 45-year-old female on antiretroviral drugs for HIV. The patient was managed with the cessation of tenofovir and surgical fixation of fracture. He concluded that patients receiving tenofovir should be regularly investigated for their renal impairment and bone health. Similarly, a 45–year-old male who developed right hip fragility fracture was reported by Suh et al. [15]. They described a case of a Hepatitis B virus positive patient with preexisting bone disease who developed tenofovir-induced Fanconi syndrome and subsequently sustained pathologic fracture. Tenofovir treatment was discontinued and internal fixation was done, satisfactory outcome was achieved. They concluded that one needs to regularly monitor bone metabolism in patients on tenofovir-based ART for early diagnosis before its progression to pathologic fractures. Our patient presented with the involvement of all four limbs while in literature no cases have been reported with all four limb involvement.
Table 2.
Functional assessment scores.
Conclusion
HIV infection and ART based on tenofovir should be considered independent risk factors for osteopenia and osteoporosis. Tenofovir will cause proximal renal tubule dysfunction and Fanconi syndrome and associated pathological fractures. It is important to stop tenofovir and switch to alternative safer drugs to prevent systemic complications. Such fractures need prompt diagnosis, metabolic corrections, fracture fixation, and early mobilization for optimal outcomes.
Clinical Message.
We should have high index of suspicion for pathological fractures in patients on ART based on tenofovir. Proper investigation and metabolic correction with switch to alternative ART regimen is necessary in such cases.
Biography



Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Liu AY, Vittinghoff E, Sellmeyer DE, Irvin R, Mulligan K, Mayer K, et al. Bone mineral density in HIV-negative men participating in a tenofovir pre-exposure prophylaxis randomized clinical trial in San Francisco. PLoS One. 2011;6:e23688. doi: 10.1371/journal.pone.0023688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tebas P, Powderly WG, Claxton S, Marin D, Tantisiriwat W, Teitelbaum SL, et al. Accelerated bone mineral loss in HIV-infected patients receiving potent antiretroviral therapy. AIDS. 2000;14:F63–7. doi: 10.1097/00002030-200003100-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kashoor I, Batlle D. Proximal renal tubular acidosis with and without Fanconi syndrome. Kidney Res Clin Pract. 2019;38:267–81. doi: 10.23876/j.krcp.19.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris Hip Score 156-158. The Harris hip score is a multidimensional observational assessment based on eight items that address pain, walking function, daily activity, and range of motion. In:Kelley and Firestein's Textbook of Rheumatol. Netherlands: Elsevier; 2017. [Google Scholar]
- 5.Stratford PW, Binkley JM, Stratford DM. Development and initial validation of the upper extremity functional index. Phys Can. 2001;53:259–67. [Google Scholar]
- 6.McGowan I, Cheng A, Coleman S, Johnson A, Genant H. Chicago IL, editor. Assessment of Bone Mineral Density (BMD) in HIV-Infected Antiretroviral-Therapy Naive Patients. In:8th Conference on Retroviruses and Opportunistic Infections. USA. 2001. [Last accessed on 2004 Aug 14]]. Available from: https://www.retroconference.org2001/abstracts/abstracts/abstracts/628.htm .
- 7.Yin MT, Overton ET. Increasing clarity on bone loss associated with antiretroviral initiation. J Infect Dis. 2011;203:1705–7. doi: 10.1093/infdis/jir184. [DOI] [PubMed] [Google Scholar]
- 8.Duvivier C, Kolta S, Assoumou L, Ghosn J, Rozenberg S, Murphy RL, et al. Greater decrease in bone mineral density with protease inhibitor regimens compared with nonnucleoside reverse transcriptase inhibitor regimens in HIV-1 infected naive patients. AIDS. 2009;23:817–24. doi: 10.1097/QAD.0b013e328328f789. [DOI] [PubMed] [Google Scholar]
- 9.Grant PM, Cotter AG. Tenofovir and bone health. Curr Opin HIV AIDS. 2016;11:326–32. doi: 10.1097/COH.0000000000000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection. In:Guidelines. Switzerland: World Health Organization; 2013. pp. 1–269. [Google Scholar]
- 11.Rebolledo BJ, Unnanuntana A, Lane JM. Bilateral pathologic hip fractures associated with antiretroviral therapy:A case report. J Bone Joint Surg Am. 2011;93:e78. doi: 10.2106/JBJS.J.00885. [DOI] [PubMed] [Google Scholar]
- 12.Marco P, Cristian A, Isabel GM, Veronica V, Juan H. Bilateral hip fracture in adolescents with antiretroviral treatment. J Am Acad Orthop Surg Glob Res Rev. 2017;1:e005. doi: 10.5435/JAAOSGlobal-D-17-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brim NM, Cu-Uvin S, Hu SL, O'Bell JW. Bone disease and pathologic fractures in a patient with tenofovir-induced Fanconi syndrome. AIDS Read. 2007;17:322–8. C3. [PubMed] [Google Scholar]
- 14.Rajnish RK, Rathod PM, Aggarwal S, Agarwal S, Kumar P. Bilateral sub-trochanteric femur fragility fractures in a patient on antiretroviral therapy:A case based discussion and review of literature. Int J Burns Trauma. 2020;10:121–6. [PMC free article] [PubMed] [Google Scholar]
- 15.Suh YS, Chun DI, Choi SW, Lee HW, Nho JH, Kwon SH, et al. Pathologic femoral fracture due to tenofovir-induced Fanconi syndrome in patient with chronic hepatitis B:A case report. Medicine (Baltimore) 2017;96:e8760. doi: 10.1097/MD.0000000000008760. [DOI] [PMC free article] [PubMed] [Google Scholar]


