Abstract
Objectives
COVID-19–related policies introduced extraordinary social disruption in nursing homes. In response, nursing facilities implemented strategies to alleviate their residents’ loneliness. This study sought to describe interventions nursing homes used, document the perceived effectiveness of efforts, and determine barriers to implementing strategies to mitigate social isolation and loneliness.
Design
National survey of nursing homes sampled in strata defined by facility size (beds: 30-99, 100+) and quality ratings (1, 2-4, 5).
Settings and Participants
US Nursing Home Directors of Nursing/Administrators (n = 1676).
Methods
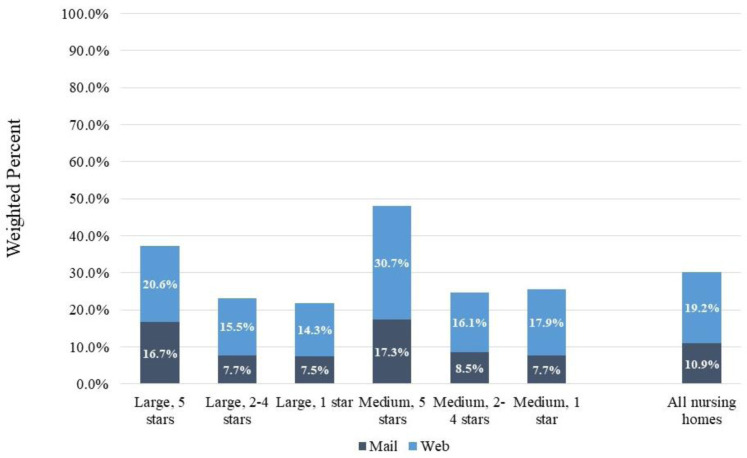
The survey was conducted between February and May 2022 (response rate: 30%; n = 504, weighted n = 14,506). Weighted analyses provided nationally representative results.
Results
One-third were extremely concerned about their home's ability to meet residents' medical and social needs during COVID-19 before vaccines were available and 13% after vaccines. Nearly all reported trying to mitigate residents' social isolation during the pandemic. Efforts tried, and perceived as most useful, included using technology (tablets, phones, emails), assigning staff as a family contact, and more staff time with residents. Most frequently cited barriers to implementation were related to staffing issues.
Conclusions and Implications
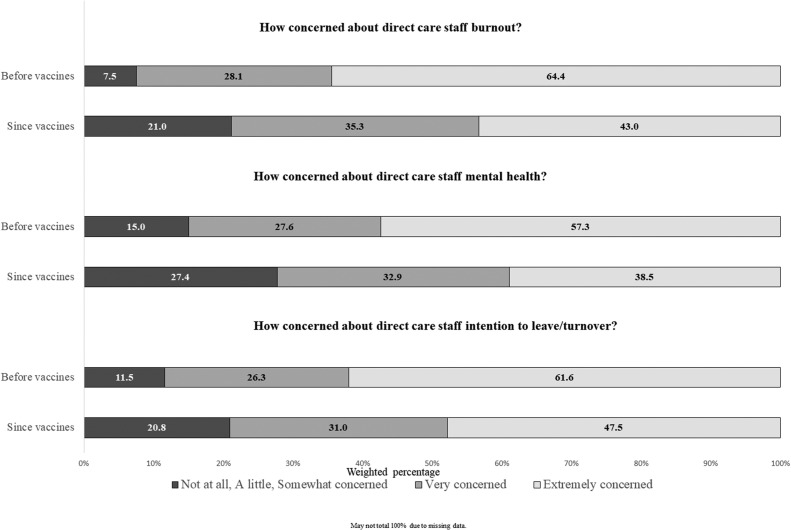
Despite multiple challenges, nearly all nursing homes tried to implement many different approaches to address residents’ social needs, with some (eg, having an assigned family contact, use of tablets and phones) perceived as more useful than others. Staffing issues presented barriers for addressing the social needs of nursing home residents. Many strategies for addressing social isolation placed more demands on a workforce already stretched to the limit. While concerns about resident social isolation reduced after vaccine availability, administrators remained extremely concerned about staff burnout and mental health.
Keywords: Loneliness, social isolation, activities, COVID-19, staff burnout
Nursing homes have been disproportionately affected by the COVID-19 pandemic, accounting for up to a third of COVID-19 deaths at various times since March 2020.1 COVID-19–related policies, although necessary, introduced unprecedented social disruption in nursing homes.1 , 2 Before the pandemic, loneliness was prevalent in nursing homes.3, 4, 5 The negative health impacts of loneliness and lack of social connectedness in nursing homes specifically are known. The toll the COVID-19 pandemic has taken on residents’ mental health has also been noted.6, 7, 8 Despite the multitude of challenges faced by nursing homes including serving a population most adversely affected by COVID-19 and dealing with a virus easily transmitted within congregate living settings, nursing homes received harsh media attention,9 , 10 although hospital workers were often described as heroes.11 This was demoralizing to nursing home staff.12
Nursing homes employed new approaches and strategies to alleviate loneliness in residents during the COVID-19 pandemic.13 , 14 To our knowledge, no nationally representative studies in the United States have documented such attempts. We surveyed directors of nursing and administrators at US nursing homes to document how nursing homes rose to the occasion to address residents' social needs during COVID-19. We also sought information about the context in which they provided care to address the social needs of their residents. In a nationally representative sample of nursing homes, we aimed to describe nursing home leadership perceptions and concerns about resident loneliness and social isolation, describe specific interventions nursing homes used to mitigate residents' social isolation, document the perceived effectiveness of efforts, and describe the barriers to implementation strategies. To better understand the barriers to implementing strategies to address the social needs of residents, we also described the nursing home leadership perceptions of direct care staff work stressors and staffing issues (eg, burnout, mental health, and turnover) likely to impact ability to address residents’ social isolation.
Methods
The XXXX Institutional Review Boards approved this study.
Design and Survey Development
We used a cross-sectional descriptive study design with nursing home as the unit of analysis. The survey was intended to be completed by nursing home leadership working at the nursing home during the COVID-19 pandemic. The current study offers a quantitative analysis of the nationally representative survey data collected in February to May 2022.
We designed an eight-page survey (web/paper) to assess nursing home leadership's (ie, Director of Nursing (DoN) or Administrator) perceptions of nursing home residents' experiences during the COVID-19 pandemic. The survey included a screening question asking, “Have you worked for your nursing home since the Spring of 2020?” If the respondent said “no”, instructions directed them to give the survey to another administrator with knowledge of resident care during the pandemic. Cognitive interviews with four DoNs were conducted and results were used to refine the survey.
Sampling Frame, survey Process, and Sample
From a publicly available list of all nursing homes rated by the Centers for Medicare & Medicaid Services, we selected a sample of 1676 nursing homes from a sampling frame of 14,613 nursing homes with ≥30 beds (Supplementary Table 2). We excluded homes with fewer than 30 beds because the resources available to these homes were quite different than larger homes. To ensure representation of nursing homes that received poor ratings (1 star) or high ratings (5 stars), we selected 283 nursing homes from six groups (2 size strata and 3 quality rating strata). Twenty-two nursing homes in the selected samples were found to be closed from phone calls to the nursing homes or web searches. We calculated adjusted population sizes in each strata based on the rates of ineligibility.
On February 14, 2022, we sent email invitations to 185 DoNs for whom we had a name and email address, explaining the study, providing a hyperlink to the online survey, and promising $45 upon survey completion. Reminder emails were sent two days later to nonrespondents. A letter with a link to the web survey and a $5 incentive was sent to those sampled DoNs without an email address (n = 1491) and to email non-responders (an additional $40 would be sent after survey completion). Two weeks after the prenotification letter was mailed, all non-responders were sent a survey packet. Three weeks later, a second packet was sent to non-responders. Research staff then called nursing homes encouraging DoNs to complete the survey. The final disposition for each of the 1676 nursing homes sampled is included on Supplementary Table 3. The response rate was 30.1% (Supplementary Figure 1).
Supplementary Fig. 1.
Survey response rates by nursing home size and quality rating.
Measures
Supplementary Table 3 shows the wording of the survey questions used in this analysis. Respondent sociodemographic and work-related questions included gender, age (<30 years, 30-50 years, ≥ 51 years), race/ethnicity, job title, and length of time working for their nursing home. Perceptions of and concern about resident social isolation and loneliness were determined before vaccines were widely available and after. For these two time periods, DoNs were also asked about their concerns about the effectiveness of their nursing home to meet residents’ medical needs and their social needs. Questions about specific interventions to mitigate social isolation were used (eg, use of technology such as tablets, outdoor visits). Questions about the perceived effectiveness of each strategy were included. Fourteen questions probed about specific barriers to implementing strategies to mitigate social isolation and loneliness.
We included questions to provide further context regarding the toll the pandemic had on nursing home workers and to describe the stressors at work the direct care staff experienced. DoNs were asked separate questions about their level of concern about direct care staff mental health, burnout, and staffing turnover. These questions were asked separately for the periods before and after vaccines were widely available. Eighteen questions were asked regarding specific stressors at work for direct care staff.
Analysis
Because the probabilities of selection varied among strata, we developed survey design weights to estimate survey results for all medium and large nursing homes in the United States. All analyses were weighted to consider the stratified sampling design and non-response (Supplementary Table 4). Survey statistical procedures in SAS version 9.4 (Cary, North Carolina) accounted for the sampling design and non-response to ensure that the proportions and standard errors were correctly calculated.
Results
Among US nursing home leadership, 87.4% were DoNs, 88.3% identified as a woman, and 37.6% were aged ≥ 51 years. With respect to race/ethnicity, the majority reported being non-Hispanic White (79.2%). Nearly one quarter (22.7%) had worked for the nursing home for ≥ 15 years, 33.8% between 5 and 14 years, and 43.2% < 4 years.
Toll on residents and Ability to Meet Needs during COVID-19 before and after Vaccines
Most homes restricted indoor visits before vaccines were available (98.5%) and 9.6% restricted them since vaccines became available. Before vaccines became available in their nursing home, 44.7% of DoNs rated loneliness and 46.8% rated social isolation as much worse compared to before the pandemic. DoNs reported concern about their nursing home being able to meet the residents’ social needs (extremely: 34.4%, very: 39.0%, somewhat concerned: 18.3%) and medical needs (extremely: 33.4%, very: 25.4%, somewhat concerned: 25.1%) before vaccines were available.
Since the vaccines, 6.0% stated that resident loneliness and 5.4% rated social isolation as much worse than before the pandemic. Since vaccines became available, DoNs reported much less concern regarding their home's ability to meet the residents' social needs (extremely: 13.7%, very: 17.5%, somewhat concerned: 30.4%) or medical needs (extremely: 13.0%, very: 19.9%, somewhat concerned: 32.5%). About one in ten DoNs remained extremely concerned about resident loneliness (11.6%) and social isolation (10.6%) since vaccines became available.
Efforts to Mitigate Social Isolation and Loneliness during COVID-19 and Perceived Effectiveness of efforts
Nearly all nursing homes attempted to mitigate resident social isolation and loneliness and most DoN's felt that their nursing homes were at least moderately successful in their efforts (very: 10.8%, moderately: 52.9%). Table 1 shows that most homes used tablets/emails/phones, and over 90% of homes tried alternatives to in-person visits, physically distanced games/crafts, or addressed social isolation in care plans. Of the most common strategies, use of tables/emails/phones was reported to be very useful by 44.8%. Among the more than 70% of homes that tried having staff spend more time with residents and/or virtual religious services, 39.5% and 31.1% found these strategies very useful. Among the 40.8% of homes having a staff member assigned as a family contact, 44.1% viewed it as very useful.
Table 1.
Efforts to Mitigate Social Isolation in nursing Homes During the COVID-19 Pandemic (n = 504, weighted n = 14,506)
| Approach | Among all (n = 504) |
Among nursing Homes that tried∗ |
||
|---|---|---|---|---|
| Weighted Percentage | ||||
| Tried | Very Useful | Somewhat Useful | Not at all Useful | |
| Tablets, emails, phone | 99.0 | 44.8 | 50.8 | 3.6 |
| Alternative to in-person visits | 98.8 | 29.0 | 67.1 | 3.1 |
| Physically distanced games/crafts | 95.8 | 26.2 | 68.3 | 5.3 |
| Addressed social isolation in care plan | 91.1 | 15.2 | 66.4 | 18.1 |
| Staff spend more time with residents | 72.9 | 39.5 | 59.8 | 0.2 |
| Virtual religious activities | 70.0 | 31.1 | 65.2 | 1.9 |
| Include grief counseling in care plans | 44.5 | 20.4 | 71.5 | 7.6 |
| Staff member assigned as family contact | 40.8 | 44.1 | 50.6 | 4.7 |
| Use face masks with clear plastic | 15.5 | 19.5 | 49.8 | 29.3 |
May not add up to 100% due to missing data.
Barriers to Implementation
When asked how big a problem staffing issues were when implementing strategies to mitigate resident loneliness, most respondents reported: short staffing: 82.0%, turnover: 67.4%, low morale: 59.7%, staff fear of COVID-19: 57.7%, and use of temporary staff: 52.1%. Resident factors that were barriers to implementation of social isolation mitigation strategies included resident's inability to dine socially (70.5%) or be with each other (66.6%), changes in resident routines (57.9%), cohorting to unfamiliar rooms (44.5%), and increases in resident behavioral problems (28.3%). Many indicated that frequent changes in COVID-19 guidance (80.0%) and staff usage of masks interfering with communication (57.6%) were problems.
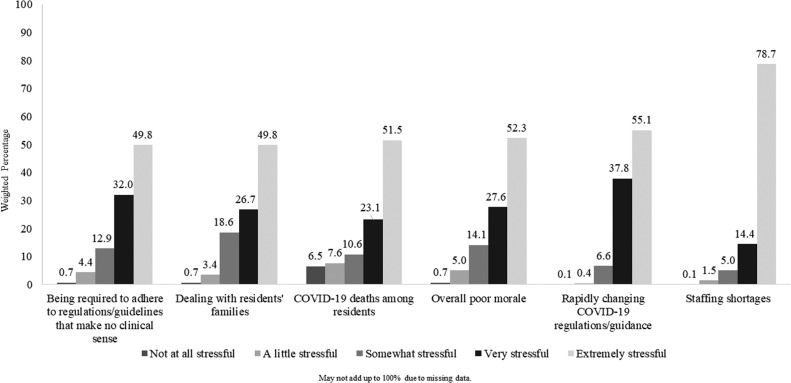
Stressors at Work during the Pandemic for Direct Care staff
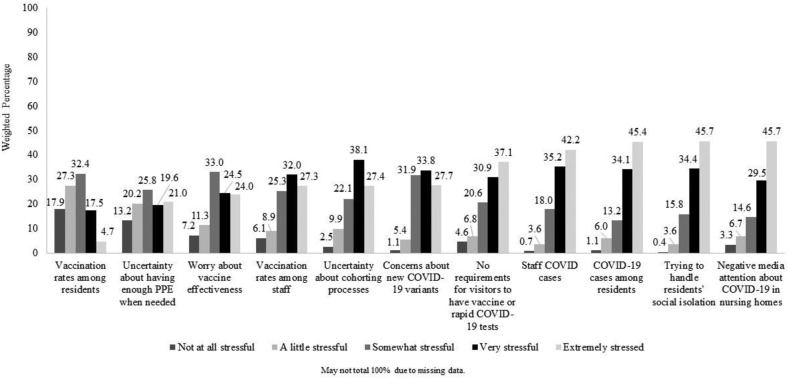
Figure 1 shows three of four DoNs noted that staffing shortages were “extremely stressful” for direct care staff, while about half of DoN's reported that rapidly changing COVID-19 regulations/guidance, overall poor staff morale, COVID-19 deaths among residents, dealing with residents' families, and being required to adhere to regulations/guidelines that make no clinical sense were extremely stressful. Supplementary Figure 2 shows the additional stressors which included negative media attention (45.7%), trying to handle residents' social isolation (45.7%), and COVID-19 cases among residents (45.4%) were considered extremely stressful for direct care staff. Few DoNs (4.7%) reported that resident vaccination rates were extremely stressful.
Fig. 1.
Shows the major stressors at work during the pandemic for direct care nursing home staff (n = 504, weighted n = 14,506).
Supplementary Fig. 2.
Additional stressors at work during the pandemic for direct care nursing home staff (n = 504, weighted n = 14,506).
Reflecting on the time during COVID-19 before vaccines were available, 64.4% were extremely concerned about direct care staff burnout (Figure 2 ). Since vaccines became available, 43.0% noted they were extremely concerned about burnout. DoNs were extremely concerned about mental health among direct care staff before and after vaccines were available (before: 57.3%, after: 38.5%) and staff turnover (before: 61.6%, after: 47.5%).
Fig. 2.
Shows the nursing home Director of Nursing concerns about direct care staff before and since vaccines (n = 504, weighted n = 14,506).
Discussion
The COVID-19 pandemic had widespread impacts on nursing home residents. This nationally representative survey documents that nearly half of DoNs rated resident loneliness and social isolation as much worse compared to before the pandemic. The majority were extremely or very concerned about their nursing home being able to meet the residents' social needs before vaccines were widely available. One in ten DoNs remained extremely concerned about resident loneliness and social isolation after vaccines were available, but were less likely to be very or extremely concerned about their home's ability to meet the residents' social needs. Nursing homes attempted a variety of approaches to address the social needs of their residents, with some more effective than others. Barriers to implementing strategies to mitigate social isolation were mostly related to staffing issues. While several staff-related barriers and stressors diminished after vaccines for COVID-19 became available, others remained at high levels.
Early in the COVID-19 pandemic, the Centers for Medicare and Medicaid Services advised all nursing homes in the United States to 1) restrict visitation of all visitors except for compassionate care; 2) cancel communal dining and all group activities; and 3) remind residents to practice social distancing.15 When COVID-19 was found in a facility, the Centers for Disease Control advised that all residents be confined to their rooms and health care workers don personal protective equipment.16 Our study documented the concerns of nursing home leadership regarding the negative impact of COVID-19 on the social isolation and loneliness of residents. This was consistent with research documenting COVID-19–related impacts on residents’ mental health.6 , 7
Most nursing homes in our study employed new approaches and strategies to address residents' social needs. Use of technology such as tablets and emails were commonly employed and thought to be effective, consistent with previous research.17 , 18 Yet, technological difficulties in the use of these approaches in nursing homes has been reported.19 Our study found that increased staff time spent with residents was useful, however, staffing challenges were noted in our study and by others.20 , 21 Approaches reported to be used in our study included increased staff-resident contact time. The increased staff-resident contact time may have exacted an additional toll on an already overworked workforce.22 In our study, four in ten homes had a staff member assigned as a family contact and this approach was considered very effective. Others have reported that this approach is useful23 and reduced essential family caregivers’ trauma from prolonged separation from loved ones.24 This effective means of communication could continue well past the COVID-19 pandemic. Barriers to implementing social interventions during the COVID-19 pandemic included changes in processes such as cohorting residents to unfamiliar rooms and the disruption to resident routines. Staff-resident communication was hampered by wearing masks. Even clear plastic masks when used, were not considered effective in addressing social isolation by many DoNs.
The context in which direct care nursing home staff were attempting to address their residents’ social needs must be considered when interpreting the findings about the effectiveness of implementation of strategies to address resident loneliness. As others have reported,25 the COVID-19 pandemic made even worse the precarious working conditions in nursing homes (ie, lack of social, economic, and professional recognition compared to colleagues working in other healthcare sectors).26 Consistent with what has been documented for decades,27 our study found that staffing shortages were identified as extremely stressful for direct care staff. During the pandemic, DoNs reported that direct care staff found rapidly changing COVID-19 regulations and guidance that often made no clinical sense extremely stressful. This is aligned with previous research in which nursing home direct care staff reported that having non-healthcare professionals (ie, surveyors) tell them how to do their jobs was a source of stress.28 More than half of DoNs reported that dealing with resident death was very stressful. Despite the stress of COVID-19 deaths among residents during an unprecedented pandemic, nursing home direct care staff continued to address social isolation among their residents and communicate with family members. During the pandemic, nursing homes struggled with significant staff shortages.29
Strengths and Limitations
This is the first nationally representative study of medium and large sized nursing homes to describe the efforts nursing homes undertook to address the social needs of their residents during the COVID-19 pandemic. The survey differentiated between the periods before and after vaccines were available in each nursing home. Our findings represent the DoN's perceptions of how well strategies to mitigate loneliness and social isolation worked. Residents and/or family members may have offered different perspectives. We had hoped to achieve a higher response rate given our rigorous survey process and appropriate incentives, but the desired survey participants likely remained overworked with little time for study participation. Nevertheless, our analysis weighted the data to account for non-response. Lastly, our survey did not ask about the extent to which the physical layout of the nursing homes posed challenges to implementing innovative social interventions (eg, narrow hallways, limited shared space).15
Conclusions and Implications
Despite stressful working environments and staffing shortages, most nursing homes asked more of their direct care staff as they attempted to mitigate the harmful effects of social isolation during the COVID-19 pandemic. The extent to which various approaches were implemented varied. Insights the DoNs provided about the perceived usefulness of approaches to address social isolation revealed promising strategies, and things that simply did not work. Concerns about resident loneliness and social isolation reduced after vaccines were available. Lessons learned during the worst of times may help nursing homes employ more effective approaches to better address their residents’ social needs in the future.
To understand more about potential staffing related issues that may have impacted the nursing homes' ability to implement strategies to address residents' social isolation, we described nursing home leadership's perceptions of direct care staff and mental health. Despite the widespread availability of vaccines, our study showed that DoNs remain extremely concerned about direct care staff burnout and mental health. Our findings are consistent with a growing body of research documenting the burden of COVID-19 on nursing home direct care staff.30 , 31 A recent scoping review focused on long term care26 identified unique challenges of nursing home direct care providers (including nurses aids, nurses, social workers, and physicians). How best to sustain nursing home healthcare professionals who may have been traumatized by working under such extreme circumstances requires attention.
Acknowledgments
This work was supported by a grant to Dr. Lapane from the National Institutes of Health (R01AG071692). We thank Carol Bova, Laurie Toohey, and Natalia Neilson for their efforts contributing to this work. We also thank the nursing home administrators and directors of nursing who voluntarily completed our survey.
Footnotes
The authors declare no conflicts of interest.
Funding: The work was supported by a grant to K.L.L. from the National Institutes of Health (R01AG071692).
Supplementary Data
Summary of Contents
Additional materials are provided here to complement the manuscript. Below is a summary of the materials assembled.
| Item | Description | Page # |
|---|---|---|
| Supplementary Table 1. Nursing Home Population Characteristics by Size and Quality Rating | Counts of nursing homes within strata defined by size category and quality ratings, and adjusted population counts based on rates of ineligibility identified in calls to the selected sample | 2 |
| Supplementary Table 2. Survey final disposition by sampling group | Provides non-response, refusals, and counts of how responded (mail or online) by sampling strata (size and quality ratings) | 3 |
| Supplementary Figure 1. Survey response rates by nursing home size and quality rating | Also shows differences in response rates by online and paper | 4 |
| Supplementary Table 3. Relevant survey questions | Provide exact wording of survey questions and response sets | 5-11 |
| Supplementary Table 4. Survey weights to account for Design (Sample Strata) and Survey Non-response | Creation of survey weights | 12 |
| Supplementary Figure 2. Additional stressors at work during the pandemic for direct care nursing home staff | Additional stressors not shown on Figure 1 | 13 |
Supplementary Table 1.
Nursing Home Population Characteristics by Facility Size and Quality Rating
| Characteristics | Population | Rate of Ineligibility∗ | Adjusted Population† |
|---|---|---|---|
| Medium: 30-99 beds | |||
| 1 star | 955 | 0.0318 | 925 |
| 2-4 stars | 4632 | 0.0071 | 4599 |
| 5 stars | 1308 | 0.0212 | 1280 |
| Large: ≥100 beds | |||
| 1 star | 1170 | 0.0106 | 1158 |
| 2-4 stars | 5920 | 0.0000 | 5920 |
| 5 stars | 628 | 0.0071 | 624 |
| Total | 14,613 | 14,506 |
Twenty-two nursing homes in the selected samples were found to be closed from phone calls to the nursing homes or web searches.
Using the rates of ineligibility, we inferred that the population of nursing homes in 2022 might have these same rates. For example, there were 955 medium (30-99-bed) 1-star NHs. We assume that 3.18% of them might be ineligible. So, we would estimate 925 small 1-star NHs, or 955 –(955 × .03180).
Supplementary Table 2.
Survey Final Disposition by Sampling Group
| Characteristics | Nonresponse | Bad Address | Refusal | Response by |
Total | ||
|---|---|---|---|---|---|---|---|
| Web | All | ||||||
| Medium: 30-99 beds | |||||||
| 1 star | 194 | 2 | 8 | 21 | 49 | 70 | 274 |
| 2-4 stars | 207 | 1 | 3 | 24 | 45 | 69 | 280 |
| 5 stars | 138 | 2 | 4 | 48 | 85 | 133 | 277 |
| Large: ≥100 beds | |||||||
| 1 star | 208 | 2 | 9 | 21 | 40 | 61 | 280 |
| 2-4 stars | 215 | 0 | 3 | 22 | 44 | 66 | 284 |
| 5 stars | 174 | 0 | 2 | 47 | 58 | 105 | 281 |
| Total | 1136 | 7 | 29 | 183 | 321 | 504 | 1676 |
Supplementary Table 3.
Relevant Survey Questions and Response Sets
| Survey question | Response Set |
|---|---|
| About how long have you worked for your nursing home? | Less than 1 year 1 to 4 years 5 to 9 years 10 to 14 years 15 or more years |
| Limiting indoor visits | |
| During the COVID-19 pandemic before vaccines were widely available to residents and staff in your nursing home, did your nursing home limit most indoor visitors? | Yes/No |
| During the COVID-19 pandemic since vaccines were widely available to residents and staff in your nursing home, does your nursing home limit most visits inside the nursing home? | Yes/No |
| Perceptions and concern about resident loneliness and social isolation | |
| During the pandemic before vaccines were widely available, how would you rate the degree of loneliness among your residents as compared to before the pandemic began? | 0 – same as before the pandemic though 10 – much worse than before the pandemic |
| During the pandemic before vaccines were widely available, how would you rate the degree of social isolation among your residents as compared to before the pandemic began? | 0 – same as before the pandemic though 10 – much worse than before the pandemic |
| During the COVID-19 pandemic before vaccines were widely available to residents and staff in your nursing home, how concerned were you about the degree of loneliness among your residents? | Not at all concerned A little concerned Somewhat concerned Very concerned Extremely concerned |
| During the COVID-19 pandemic before vaccines were widely available to residents and staff in your nursing home, how concerned were you about the degree of social isolation among your residents? | Not at all concerned A little concerned Somewhat concerned Very concerned Extremely concerned |
| During the pandemic since vaccines were widely available, how would you rate the degree of loneliness among your residents as compared to before the pandemic began? | 0 – same as before the pandemic though 10 – much worse than before the pandemic |
| During the pandemic since vaccines were widely available, how would you rate the degree of social isolation among your residents as compared to before the pandemic began? | 0 – same as before the pandemic though 10 – much worse than before the pandemic |
| During the COVID-19 pandemic since vaccines were widely available to residents and staff in your nursing home, how concerned were you about the degree of loneliness among your residents? | Not at all concerned A little concerned Somewhat concerned Very concerned Extremely concerned |
| During the COVID-19 pandemic since vaccines were widely available to residents and staff in your nursing home, how concerned were you about the degree of social isolation among your residents? | Not at all concerned A little concerned Somewhat concerned Very concerned Extremely concerned |
| Concerns about ability to meet residents' needs | |
| During the COVID-19 pandemic before vaccines were widely available to residents and staff in your nursing home, how concerned were you about the effectiveness of your nursing home in meeting residents' medical needs? | Not at all concerned A little concerned Somewhat concerned Very concerned Extremely concerned |
| During the COVID-19 pandemic before vaccines were widely available to residents and staff in your nursing home, how concerned were you about the effectiveness of your nursing home in meeting residents' social needs? | Not at all concerned A little concerned Somewhat concerned Very concerned Extremely concerned |
| During the COVID-19 pandemic since vaccines were widely available to residents and staff in your nursing home, how concerned were you about the effectiveness of your nursing home in meeting residents' medical needs? | Not at all concerned A little concerned Somewhat concerned Very concerned Extremely concerned |
| During the COVID-19 pandemic since vaccines were widely available to residents and staff in your nursing home, how concerned were you about the effectiveness of your nursing home in meeting residents' social needs? | Not at all concerned A little concerned Somewhat concerned Very concerned Extremely concerned |
| Efforts to mitigate social isolation and loneliness | |
| During the pandemic, did your nursing home do anything to mitigate social isolation and loneliness? | Yes/No |
| During the pandemic, did your nursing home use tablets, laptops, phones, email? | Yes/No |
| How useful was using technology in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home use alternative in-person visits with family or friends, such as visits outdoors, through glass doors or windows? | Yes/No |
| How useful were the alternative in-person visits in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home use physically distanced crafts or games? | Yes/No |
| How useful were physically distanced activities in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home address social isolation in individual resident care plans? | Yes/No |
| How useful was addressing social isolation in individual resident care plans in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home have staff spend more time sitting and talking to residents? | Yes/No |
| How useful was having staff spending more time sitting and talking to residents in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home have virtual religious activities, such as video services, or calls from chaplains, rabbis, etc.? | Yes/No |
| How useful were virtual religious activities in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home include grief counseling as part of individual resident care plans? | Yes/No |
| How useful was including grief counseling as part of individual resident care plans in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did family members have a staff member assigned as a primary contact? | Yes/No |
| How useful was having a staff member assigned as a primary contact for each family in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home use face masks with clear plastic in front of the mouth? | Yes/No |
| How useful was using face masks with clear plastic in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| Other than what was already asked in this survey, did your nursing home do anything else to mitigate social isolation and loneliness? | Yes/No |
| What did your nursing home do? | Open-ended |
| Overall, how successful was your nursing home in mitigating the social isolation and loneliness of your residents during the pandemic? | Not at all successful A little successful Moderately Very successful |
| Stressors at work during the pandemic for direct care staff | |
| Efforts to mitigate social isolation and loneliness | |
| During the pandemic, did your nursing home do anything to mitigate social isolation and loneliness? | Yes/No |
| During the pandemic, did your nursing home use tablets, laptops, phones, email? | Yes/No |
| How useful was using technology in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home use alternative in-person visits with family or friends, such as visits outdoors, through glass doors or windows? | Yes/No |
| How useful were the alternative in-person visits in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home use physically distanced crafts or games? | Yes/No |
| How useful were physically distanced activities in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home address social isolation in individual resident care plans? | Yes/No |
| How useful was addressing social isolation in individual resident care plans in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home have staff spend more time sitting and talking to residents? | Yes/No |
| How useful was having staff spending more time sitting and talking to residents in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home have virtual religious activities, such as video services, or calls from chaplains, rabbis, etc.? | Yes/No |
| How useful were virtual religious activities in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home include grief counseling as part of individual resident care plans? | Yes/No |
| How useful was including grief counseling as part of individual resident care plans in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did family members have a staff member assigned as a primary contact? | Yes/No |
| How useful was having a staff member assigned as a primary contact for each family in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| During the pandemic, did your nursing home use face masks with clear plastic in front of the mouth? | Yes/No |
| How useful was using face masks with clear plastic in mitigating social isolation and loneliness? | Not at all useful Somewhat useful Very useful |
| Other than what was already asked in this survey, did your nursing home do anything else to mitigate social isolation and loneliness? | Yes/No |
| What did your nursing home do? | Open-ended |
| Overall, how successful was your nursing home in mitigating the social isolation and loneliness of your residents during the pandemic? | Not at all successful A little successful Moderately Very successful |
| Barriers to implementation of strategies to mitigate social isolation | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was short staffing? | No problem A small problem A big problem |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was staff turnover? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was low morale? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was staff's fear of COVID-19? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was use of temporary staff who lack familiarity with residents? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was insufficient COVID-19 education among staff? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was residents unable to dine socially? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was resident's inability to be with other residents? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was changes in resident's routines such as dining and activities? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was cohorting to different unfamiliar rooms or units? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was increase in resident behavioral problems due to anxiety or fear? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was frequent changes in COVID-19 guidance? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was staff wearing masks interfering with resident's ability to respond to non-verbal communication? | |
| Thinking about when your nursing home tried to implement strategies to mitigate social isolation during the pandemic, how much of a problem was shortages of PPE? | |
| Concerns about staff | |
| During the COVID-19 pandemic before vaccines were widely available to residents and staff in your nursing home, how concerned were you about direct care staff burnout? | Not at all concerned A little concerned Somewhat concerned Very concerned Extremely concerned |
| During the COVID-19 pandemic before vaccines were widely available to residents and staff in your nursing home, how concerned were you about direct care staff mental health? | |
| During the COVID-19 pandemic before vaccines were widely available to residents and staff in your nursing home, how concerned were you about direct care staff turnover? | |
| During the COVID-19 pandemic since vaccines were widely available to residents and staff in your nursing home, how concerned were you about direct care staff burnout? | |
| During the COVID-19 pandemic since vaccines were widely available to residents and staff in your nursing home, how concerned were you about direct care staff mental health? | |
| During the COVID-19 pandemic since vaccines were widely available to residents and staff in your nursing home, how concerned were you about direct care staff turnover? | |
| Stressors at work during the pandemic for direct care staff | |
| Since the COVID-19 pandemic began, how stressful were staffing shortages for your direct care staff? | Not at all stressful A little stressful Somewhat stressful Very stressful Extremely stressful |
| Since the COVID-19 pandemic began, how stressful were rapidly changing COVID-19 related regulations for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were overall poor staff morale for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were COVID-19 deaths among residents for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were dealing with residents' families for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were being required to adhere to regulations or guidelines that do not make clinical sense for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were negative media attention about COVID-19 in nursing homes for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were trying to handle residents' social isolation for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were COVID-19 cases among residents for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were vaccination rates among residents for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were uncertainty about cohorting processes for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were no requirements for visitors to have vaccination proof or rapid COVID-19 tests for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were vaccination rates among residents for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were vaccination rates among staff for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were uncertainty of having enough PPE when needed for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were COVID-19 cases among staff for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were worry about vaccine effectiveness for your direct care staff? | |
| Since the COVID-19 pandemic began, how stressful were concerns about new COVID-19 variants for your direct care staff? | |
Supplementary Table 4.
Survey Final Disposition by Sampling Group
| Characteristics | Population∗ | Sample∗ | Respondents | Probability of Selection |
Weight for Design and Response | |
|---|---|---|---|---|---|---|
| Design | Response | |||||
| Medium: 30-99 beds | ||||||
| 1 star | 925 | 274 | 70 | 0.296 | 0.255 | 13.214 |
| 2-4 stars | 4599 | 280 | 69 | 0.061 | 0.246 | 66.652 |
| 5 stars | 1280 | 277 | 133 | 0.216 | 0.480 | 9.624 |
| Large: ≥100 beds | ||||||
| 1 star | 1158 | 280 | 61 | 0.242 | 0.218 | 18.984 |
| 2-4 stars | 5920 | 284 | 66 | 0.048 | 0.232 | 89.697 |
| 5 stars | 624 | 281 | 105 | 0.450† | 0.374 | 5.943 |
†The probability of selection was 281/624 or 0.450. To create the design weight, we calculated the inverse of the probability of selection (1/0.450 or 2.221). This means that every response in this stratum represents about 2 nursing homes. The nonresponse weight is equal to the inverse of the probability of responding to the survey or 105/281, which results in a nonresponse weight of (1/0.374 or 2.676). To account for differential probabilities of selection and survey nonresponse, we combined these 2 weights. In other words, the final weight for the nursing homes in this stratum is equal to the design weight multiplied by the nonresponse weight. The calculation for this weight is as follows: [1/(281/624)] × [1/(105/281)] or 5.943.
Population size and sample size for each stratum adjusted for estimated ineligible nursing homes based on calls to nursing homes and web searches. Twenty-two nursing homes were found to have closed via phone calls and web searches. Note: Total population size is 14,505. Estimates add to 14,506 because of rounding.
References
- 1.Koszalinski R.S., Olmos B. Communication challenges in social isolation, subjective cognitive decline, and mental health status in older adults: a scoping review (2019-2021) Perspect Psychiatr Care. 2022;58:2741–2755. doi: 10.1111/ppc.13115. [DOI] [PubMed] [Google Scholar]
- 2.Staempfli S., Havaei F., Phinney A., MacPhee M. Unintended consequences of pandemic management strategies on residents and family in one long-term care home in British Columbia: a patient-supported qualitative study. Innov Aging. 2022;6 doi: 10.1093/geroni/igac036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Theurer K., Mortenson W.B., Stone R., Suto M., Timonen V., Rozanova J. The need for a social revolution in residential care. J Aging Stud. 2015;35:201–210. doi: 10.1016/j.jaging.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Trybusińska D., Saracen A. Loneliness in the context of quality of life of nursing home residents. Open Med. 2019;14:354–361. doi: 10.1515/med-2019-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen-Mansfield J.M., Dakheel-Ali M., Marx M.S., Thein K., Regier N.G. Which unmet needs contribute to behavior problems in persons with advanced dementia? Psychiatry Res. 2015;228:59–64. doi: 10.1016/j.psychres.2015.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.LeVasseur A.L. Effects of social isolation on a long-term care resident with dementia and depression during the COVID-19 pandemic. Geriatr Nurs. 2021;42:780–781. doi: 10.1016/j.gerinurse.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bethell J., Aelick K., Babineau J., et al. Social connection in long-term care homes: a scoping review of published research on the mental health impacts and potential strategies during COVID-19. J Am Med Dir Assoc. 2021;22:228–237.e25. doi: 10.1016/j.jamda.2020.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saad A., Magwood O., Benjamen J., et al. Health equity implications of the COVID-19 lockdown and visitation strategies in long-term care homes in Ontario: a mixed method study. Int J Environ Res Public Health. 2022;19:4275. doi: 10.3390/ijerph19074275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.https://www.nytimes.com/2020/04/17/us/coronavirus-nursing-homes.html
- 10.Miller E.A., Simpson E., Nadash P., Gusmano M. Thrust Into the spotlight: COVID-19 focuses media attention on nursing homes. J Gerontol: Series B. 2021;76:e213–e218. doi: 10.1093/geronb/gbaa103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.https://www.nytimes.com/article/they-get-brave.html
- 12.White E.M., Wetle T.F., Reddy A., Baier R.R. Front-line nursing home staff experiences during the COVID-19 pandemic. J Am Med Dir Assoc. 2021;22:199–203. doi: 10.1016/j.jamda.2020.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ickert C., Rozak H., Masek J., Eigner K., Schaefer S. Maintaining resident social connections during COVID-19: considerations for long-term care. Gerontol Geriatr Med. 2020;6 doi: 10.1177/2333721420962669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferdous F. Social distancing vs social interaction for older adults at long-term care facilities in the midst of the COVID-19 pandemic: a rapid review and synthesis of action plans. Inquiry. 2021;58 doi: 10.1177/00469580211044287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Director, Quality, Safety & Oversight Group, CMS Memo: guidance for infection control and prevention of coronavirus disease 2019 (COVID-19) in nursing homes. https://www.cms.gov/files/document/3-13-2020-nursing-home-guidance-covid-19.pdf
- 16.CDC Key strategies to prepare for COVID-19 in long-term care facilities (LTCFs) https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care-strategies.html
- 17.Monin J.K., Ali T., Syed S., et al. Family communication in long-term care during a pandemic: lessons for enhancing emotional experiences. Am J Geriatr Psychiatry. 2020;28:1299–1307. doi: 10.1016/j.jagp.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schuster A.M., Cotten S.R. COVID-19's influence on information and communication technologies in long-term care: results from a web-based survey with long-term care administrators. JMIR Aging. 2022;5 doi: 10.2196/32442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chu C.H., Ronquillo C., Khan S., Hung L., Boscart V. Technology recommendations to support person-centered care in long-term care homes during the covid-19 pandemic and beyond. J Aging Soc Policy. 2021;33:539–554. doi: 10.1080/08959420.2021.1927620. [DOI] [PubMed] [Google Scholar]
- 20.Gadbois E.A., Brazier J.F., Meehan A., et al. Perspectives of nursing home administrators across the United States during the COVID-19 pandemic [published online ahead of print, 2022 Nov 23] Health Serv Res. 2022;10:1111. doi: 10.1111/1475-6773.14104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Franzosa E., Mak W., R Burack O., et al. Perspectives of certified nursing assistants and administrators on staffing the nursing home frontline during the COVID-19 pandemic. Health Serv Res. 2022;57:905–913. doi: 10.1111/1475-6773.13954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lavoie-Tremblay M., Gélinas C., Aubé T., et al. Influence of caring for COVID-19 patients on nurse's turnover, work satisfaction and quality of care. J Nurs Manag. 2022;30:33–43. doi: 10.1111/jonm.13462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGilton K.S., Krassikova A., Boscart V., et al. Nurse practitioners rising to the challenge during the coronavirus disease 2019 pandemic in long-term care homes. Gerontol. 2021;61:615–623. doi: 10.1093/geront/gnab030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chu C.H., Yee A.V., Stamatopoulos V. “It's the worst thing I've ever been put through in my life”: the trauma experienced by essential family caregivers of loved ones in long-term care during the COVID-19 pandemic in Canada. Int J Qual Stud Health Well-Being. 2022;17 doi: 10.1080/17482631.2022.2075532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schuster A.M., Cotten S.R. COVID-19's influence on information and communication technologies in long-term care: results from a web-based survey with long-term care administrators. JMIR Aging. 2022;5 doi: 10.2196/32442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boamah S.A., Weldrick R., Havaei F., Irshad A., Hutchinson A. Experiences of healthcare workers in long-term care during covid-19: a scoping review. J Appl Gerontol. 2022:1118–1136. doi: 10.1177/07334648221146252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.French R., Aiken L.H., Fitzpatrick Rosenbaum K.E., Lasater K.B. Conditions of nursing practice in hospitals and nursing homes before COVID-19: implications for policy action. J Nurs Regul. 2022;13:45–53. doi: 10.1016/S2155-8256(22)00033-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lapane K.L., Hughes C.M. Considering the employee point of view: perceptions of job satisfaction and stress among nursing staff in nursing homes. J Am Med Dir Assoc. 2007;8:8–13. doi: 10.1016/j.jamda.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 29.Abbasi J. “abandoned” nursing homes continue to face critical supply and staff shortages as COVID-19 toll has mounted. JAMA. 2020;324:123–125. doi: 10.1001/jama.2020.10419. [DOI] [PubMed] [Google Scholar]
- 30.Franzosa E., Mak W., R Burack O., et al. Perspectives of certified nursing assistants and administrators on staffing the nursing home frontline during the COVID-19 pandemic. Health Serv Res. 2022;57:905–913. doi: 10.1111/1475-6773.13954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Havaei F., Ma A., Staempfli S., MacPhee M. nurses' workplace conditions impacting their mental health during COVID-19: a cross-sectional survey study. Healthcare (Basel) 2021;9:84. doi: 10.3390/healthcare9010084. [DOI] [PMC free article] [PubMed] [Google Scholar]