Abstract
Advances in data science and timely access to health informatics provide a pathway to integrate patient-reported outcome measures (PROMs) into clinical workflows and optimize rehabilitation service delivery. With the shift toward value-based care in the US healthcare system, as highlighted by the recent Centers for Medicare and Medicaid Services incentive and penalty programs, it is critical for rehabilitation providers to systematically collect and effectively use PROMs to facilitate evaluation of quality and outcomes within and across health systems.
This editorial discusses the potential PROMs have to transform clinical practice, provides examples of health systems using PROMs to guide care, and identifies barriers to aggregating data from PROMs to conduct health services research. The paper proposes two priority areas to help advance rehabilitation health services research: 1) standardize collecting PROMs data in electronic health records to facilitate comparing health system performance and quality, and 2) increased partnerships between rehabilitation providers, researchers, and payors to accelerate health system learning. As healthcare reform continues to emphasize value-based payment strategies, it is essential for the field of physical medicine and rehabilitation to be at the forefront of demonstrating its value in the care continuum.
Keywords: patient-reported outcomes, rehabilitation, care delivery, value-based care
Introduction
Traditionally, rehabilitation services are provided using a dynamic and cyclical process of collaborative goal setting, therapeutic interventions, and progress assessment that occurs directly between a clinician and a patient. Although it is established that rehabilitation efforts result in improved function and return to valued activities, there is still frustratingly little empirical evidence quantifying these gains and their impact on health outcomes. In fact, analyses of nationally representative data are unable to fully quantify the causal relationship between interventions and functional improvement in acute and post-acute rehabilitation settings.1–7 Perhaps, more tellingly, they raise concerns regarding value of rehabilitation and its impact on health outcomes.
Payors are increasingly moving toward adopting value-based payment models, such as alternative payment models (APMs), that use patient-centered outcomes to drive reimbursement and improve the value of care.8–10 Therefore, it is imperative that the field of rehabilitation leverages recent advances in data science, health informatics, and availability of standardized outcome measures to identify ways in which data can be used to improve care delivery and evaluate the effectiveness of rehabilitative care.
The Centers for Medicare and Medicaid Services (CMS) have implemented numerous valued-based APMs, such as the Bundled Payments for Care Improvement (BPCI) and the Comprehensive Care for Joint Replacement Model (CJR). Some APMs, such as the CJR, incentivize collecting patient-reported outcome measures (PROMs)11 by giving providers who do collect them additional reimbursement. Early evaluations of CJR and BPCI have focused on initial cost savings and differences in mortality and complications. These investigations found that CJR and BPCI models improved care coordination and resulted in 3% reduced spending, largely attributed to a 5% decrease in post-acute care (PAC) utilization.12–14 While initial decreases in PAC utilization have produced savings, information is lacking about the cost-effectiveness of high and low-value rehabilitation care15 on patient-centered outcomes, such as change in function, pain, symptom burden, and quality of life. These represent potential indicators of high-value care in rehabilitation, yet are typically not systematically collected or evaluated.
Tying reimbursement to patient-centered outcomes is becoming a reality. Thus, we propose that systematically collecting PROMs data across acute and post-acute rehabilitation settings is not only a necessity—but an essential step toward demonstrating the value of rehabilitation and ensuring adequate reimbursement. To achieve this goal, the field of physical medicine and rehabiliation (PM&R) needs to use those PROMs developed in recent years to quantify patients’ experiences. Some measures span various patient populations, such as the PROMIS® system, Neuro-QoL™, NIH Toolbox®,16 while others capture the unique needs and experiences of specific populations, such as the SCI-FI system17 and PEDI-CAT.18
This editorial aims to discuss the potential for PROMs to improve clinical practice, provide examples of health systems using PROMs to guide patient care, and identify barriers and potential solutions to aggregating PROMs data to conduct effective health services research in physical medicine and rehabilitation. We conclude with summary recommendations for rehabilitation clinicians and researchers to advance this rapidly evolving field and support a sustainable and central role for our field.
Potential of PROMs to Improve Rehabilitation Care
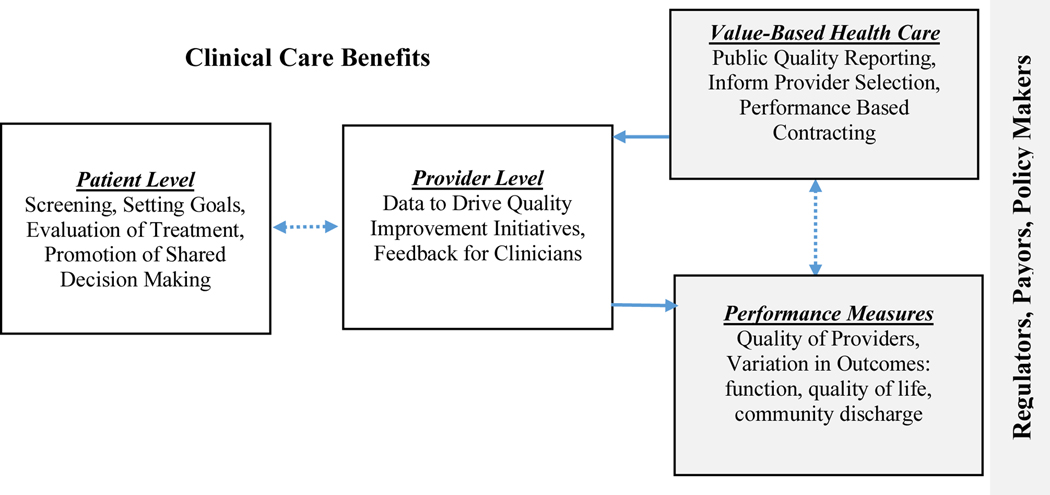
Standardized PROM collection has the potential to improve rehabilitation care delivery and outcomes in a variety of ways. Olde Rikkert et al. provide a useful framework to conceptualize the multi-faceted benefits of standardized collection of PROMs in clinical practice, which we adapt to reflect the flow of how PROM data is generated and collected in the U.S. healthcare system (Figure 1).19 In clinician-patient interactions, PROMs can facilitate identifying rehabilitation needs and baseline function and provide a starting point for targeted evaluation and goal setting. Data from serially collected PROMs can allow clinicians to detect patient improvement during therapy and deliver more tailored intervention. Routinely collected PROMs can then be aggregated at the provider or facility level and provide a powerful tool to improve care delivery and patient-centered outcomes.
Figure 1.
Adapted from: Olde Rikkert MGM, van der Wees PJ, Schoon Y, Westert GP. Using Patient Reported Outcomes Measures to Promote Integrated Care. Int J Integr Care. 2018;18(2):8.
Payors, regulators, policy makers, and professional organizations strongly influence collection of PROMs. As described in the introduction, CMS value-based reimbursement incentives are being used to motivate providers to use PROMs to demonstrate improved performance, patient satisfaction, and engagement. Collecting PROM data at the provider level allows regulators and payors to identify variations in outcomes and rate providers against national benchmark data. This, in turn, provides support for value-based payment systems, whereby provider reimbursement is determined, in part, by patient outcomes.
This is not all in the future. These data are currently being used to create online dashboards with the goal of assisting patients/caregivers with decision-making when choosing providers. Currently, CMS uses Quality Reporting Program (QRP) data and, when available, patient experience information to create dashboards that compare facility quality and outcomes for hospitals, nursing homes, inpatient rehabilitation facilities, and home health providers.20 However, quality ratings for some settings such as nursing homes and inpatient rehabilitation facilities are incomplete as they do not include any PROM data.
Health System Implementation of PROMs to Guide Patient Care
Although many health systems are implementing and utilizing PROMs to improve patient care and efficiency, little has been published in the peer-reviewed literature. Nevertheless, several useful examples exist that illustrate how health systems have integrated PROMs into their clinical workflow and how they are being used to improve efficiency and quality of care.
PROMs in Pediatric Care
The Cincinnati Children’s Hospital Medical Center undertook a system-wide effort to collect PROMs across various clinical settings and patient populations. Gerhardt et al outlined the steps taken to implement PROMs, including engaging stakeholders, establishing a process to select measures, specifying scores to trigger alerts for care needs, and monitoring PROM collection and use.21 Champion-led clinician work groups facilitated high (75%) patient completion rates across clinics. PROMs scores alert clinicians when targeted interventions are needed that may have gone unnoticed. For example, improved quality of life was noted for patients seen in a food allergy clinic when PROM scores triggered referral to a dietician, and multidimensional PROM scores improved care planning discussions during endocrine clinic visits by alerting clinicians to patient concerns about self-management and treatment options.21 Similarly, Shriners Hospitals implemented PROMIS® pediatric instruments across 10 locations using iPads to facilitate completion by patients and/or their parent or guardian. Participating hospitals reported completion rates of up to 93% and used those scores to trigger additional interventions and consults (e.g. physical therapy).22 Providers also reported improved care conversations with patients, stating that some patients appeared more comfortable reporting symptoms and other issues ahead of time rather than bringing them up during face to face interactions.22
PROMs in Orthopedic Care
As described in the introduction, the CMS CJR model uses increased reimbursement to motivate providers to submit PROM data during the pre- and post-operative phases of joint replacement.11 As a result, many orthopedic providers have implemented PROMs in their clinical practice and expanded their use to procedures and diagnoses beyond total hip and knee arthroplasty. For example, the Department of Orthopedic Surgery at Cleveland Clinic uses a collection of PROMs to track longitudinal progress of outcomes across the continuum of orthopedic care. For patients undergoing surgery for a variety of orthopedic conditions, PROMs have been collected to quantify pain, function, and quality of life prior to and after surgery.23
Patient-level PROM data is aggregated into the OrthoMiDaS Episode of Care tool,24 which is designed to promote shared decision making between providers and patients about the potential value of surgical interventions.23 A similar program, called Partners Care Decisions, was instituted across orthopedic providers at Partners Healthcare in Boston.25 In this program, providers use PROM data alongside a decision support tool in patient discussions about the potential risks and benefits of operative treatment for knee arthritis and spinal stenosis. Partners Care Decisions also uses data from PROMs to assist patients with benchmarking their individual progress in pain and functioning following surgery. In addition, many institutions have partnered to create orthopedic care and outcomes registries that include PROMs, such as the Function and Outcomes Research for Comparative Effectiveness in Total Joint Replacement (FORCE-TJR),26 and the American Academy of Orthopaedic Surgeons Registry Program.27
PROMs in Oncologic Care
Notably, oncology researchers report success integrating electronic PROMs to monitor and manage symptom burden, quality of life, and function for their patients. Although little evidence is available to guide score interpreting scores and managing patients,28 their findings suggest that assessing PROMs longitudinally may improve quality of life,29 decrease healthcare utilization,29, 30 and lessen mortality during cancer treatment.31 Additionally, PROM-based monitoring combined with telerehabilitation decreased acute and post-acute care utilization among patients with advanced stage cancer.32 In 2021, the Oncology Care First model—a value-based payment model for Medicare beneficiaries undergoing cancer treatment—is anticipated to require that participating practices collect PROM data.33, 34 Although further research is needed to fully understand how to successfully implement and use PROMs in oncologic care, payors have demonstrated their interest in using PROMs to benchmark the value of care.
Barriers and Potential Solutions: Collecting PROMs for Effective Health Services Research in Rehabilitation
Institutional Barriers
Meaningfully implementing PROMs routinely at the point of rehabilitation care is limited by barriers that include a lack of financial incentives to collect PROMs35 and difficulty navigating the realities of large, complex health systems.36 As PROMs are not directly tied to reimbursement, busy providers prioritize other aspects of documentation they believe are important or are directly tied to payment. Furthermore, determining which measure is most appropriate for a patient population is often unclear, as an instrument may be validated in one patient population and setting, yet not in others. Additionally, PROMs need to be collected so as to avoid increasing clinician burden—particularly in busy and, perhaps, under-resourced environments. PROMs can be delivered via computerized adaptive tests (CATs) to facilitate quick administration of item banks and delivers precise estimates of a desired trait (e.g. function, quality of life, etc.).37 In fact, many PROMs have already been developed to measure rehabilitation focused constructs using CATs to decrease administrative burden on already overtasked staff, especially when entered directly into the patient’s electronic health record (EHR).38–41
Regardless of institutional-level barriers to collecting and aggregating of PROMs for health services research, recent work has identified key components to facilitate successful implementation. Thoughtful and supportive leadership by the health system is vital to successfully implement PROMs.36 Institutional governance is essential to fostering a culture that supports collecting PROMs and to provide oversight for selecting and integrating appropriate measures into technical platforms for PROM delivery.36 It is critical that rehabilitation clinicians be included and have a voice in these governance committees at their institution.
At the departmental level, leadership should work with frontline staff to align PROM collection with clinical needs and workflows.35, 36 Leadership and staff should collaboratively identify workgroups and clinical champions who will monitor quality and consistency of collecting data. Engaging staff in the process is vital to successfully collect PROMs data and ensure sustained implementation over time. Recent research within a large health system found that clinician and administrative engagement and presence of a clinical champion were associated with an increased rate of standardized PROM use across a variety of clinical settings.42,43
Barriers in Health Information Technology
Barriers also exist in health information technology, as many existing EHRs are not designed to meaningfully present PROM data.35 Even when EHR systems are able to display PROM data, they often lack an intuitive and ‘user friendly’ interface that allows clinicians to interpret and use scores to inform care decisions.35, 36 The ability to track patient-centered outcomes across the continuum of care from inpatient to outpatient settings also remains limited. Despite the increased sharing of EHR access between inpatient and outpatient clinical settings, PROM data is not consistently collected across settings, even with increased availability of standardized methods to collect data (e.g. smart phones, tablets, etc.) and their ability to integrate with the EHR systems.44 Longitudinal assessment is further impeded by a lack of established metrics for sensitivity and responsiveness to change for measures across care settings, thereby limiting their use throughout recovery.
As above, institutional buy-in and governance is key to facilitating PROM integration in technical platforms within health systems. It is also beneficial to have key rehabilitation staff undergo technical training to become skilled in navigating the structure of the institution’s EHR system. This fluency in information technology is important for understanding the flow of information throughout the institution and can be used to identify strategies to collect and display PROM data. Staff with advanced training in EHR platforms can collaborate with rehabilitation staff and leadership to develop ways to meaningfully use PROM data to inform clinical practice.45
Barriers to Measurement Across Rehabilitation Settings
Overall, the inconsistency and variability of collecting PROMs across rehabilitation settings create an array of methodological challenges to quantifying the relationship between rehabilitation and outcomes. We currently lack the data needed to examine how rehabilitation services impact functional recovery, quality of life, and participation at the population level. This challenge is compounded for patient populations with condition-specific physical and cognitive limitations, such as persons with amputations and moderate/severe traumatic brain injury. Although national-level administrative claims data provide clinician-rated functional assessments collected in post-acute care settings, such measures are not present in acute care or outpatient data submissions. The lack of a common clinical usage of a standardized set of validated, psychometrically-sound PROMs either limits the potential of cross-institution research or poses the risk of spurious findings and measurement error in cross-institutional research.
During an episode of care, patients often receive rehabilitation across numerous care settings, starting at the point of hospitalization and transitioning to intensive inpatient rehabilitation or skilled nursing facilities, followed by outpatient or home health care. Thus, standardizing PROM collection across all rehabilitation settings will be crucial. With the implementation of the Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act of 2014), the CMS began to collect standardized assessments of patients’ medical, functional, cognitive, and social support status across all post-acute settings, using the Continuity Assessment Record and Evaluation (CARE) tool. However, most assessments in the CARE tool are clinician-rated.
Tackling the complex issues that impede PROM measurement across rehabilitation settings will require a methodical and concerted effort. Functional recovery, for example, can be measured broadly for many patient populations using various components of the PROMIS® system, AM-PAC CAT or the FAM-CAT. For patients with neurologic injuries, the Neuro-QoL or SCI-FI system may be more appropriate. The PEDI-CAT has been developed and validated for children with disability. To fully elucidate trajectories of recovery, further work is needed to quantify the sensitivity and responsiveness of each PROM over time and across settings. It is also important to collect PROMs to quantify other aspects of the patient experience impacted by rehabilitation, such as quality of life and symptom burden. This is particularly important for patients who may not experience functional improvement but who benefit from rehabilitation interventions to optimize or maintain function (e.g. neurodegenerative disorders, complex chronic illness) and participation in valued life roles in the face of serious illness.
While a ‘one-size-fits all’ approach will not be feasible or appropriate for all populations, collecting a core set of PROMs to capture the patient experience across the continuum of care is vital. Rehabilitation researchers and clinicians should collaborate to develop protocols to collect PROMs in a standardized manner and design methodologically rigorous evaluation of implementation and outcomes. These efforts should occur simultaneously within and across settings, starting at the level of the health system and expanding nationally.
Future Directions
An increasing focus on comparing the quality of rehabilitation services across care settings accentuates how PROMs data can be used to quantify important patient outcomes such as pain, function, participation, and quality of life. It is likely that collecting PROMs data will soon be standardized in rehabilitation settings similar to what has occurred in other CMS value-based payment models. We urge the field of rehabilitation to advocate for CMS innovation models to support these activities as a way to facilitate a culture ready to implement these changes across rehabilitation settings. As policy drives practice, more efforts are needed to link PROMs with value-based initiatives and outcomes. Participating in novel payment and service delivery models would provide the resources needed to invest in health technology and staffing needed to ensure consistent reporting.
PROMs provide an opportunity to improve rehabilitation delivered in clinical settings while promoting health services research. We propose two priority areas in rehabilitation to ensure comparisons between rehabilitation providers and settings are fair and appropriate—1) improve standardized collecting of PROMs data in EHRs to allow comparing performance and quality in and across hospital systems, and 2) increase partnerships between rehabilitation clinicians and researchers to generate rehabilitation focused health services research to yield health policy and patient care benefits. Barriers to address these priorities exist, but to advance the evidence base of rehabilitation science and ensure equitable reimbursement, we must act to overcome these challenges and implement at least a basic set of common PROMs in practice settings. Strategies outlined to overcome barriers to meaningful PROM use include: 1) strong administrative leadership and support, 2) implementing and integrating CAT-based PROMs into existing EHR to decrease clinician burden, 3) collaborating with partners in health information technology, and 4) engaging front line staff. We contend that standardizing and collecting PROM data across rehabilitation settings hold the promise of benefiting all constituencies from patients, providers, researchers, policy makers, and payors. PROMs can play a crucial role in individualizing the rehabilitation experience and improving care delivery. Yet to achieve the core goals of rehabilitation—remediating impairments, restoring function, and facilitating return to the community—PROMs should become a central part of the rehabilitation process.
Funding Sources:
This study was funded in part by an Agency for Healthcare Research and Quality National Research Service Award T32 (Grant #5T32 HS000011-33), and a Center on Health Services Training and Research fellowship funded by the Foundation for Physical Therapy Research.
Abbreviations:
- APM
Alternative payment models
- CMS
Centers for Medicare and Medicaid Services
- BPCI
Bundled Payments for Care Improvement
- CJR
Comprehensive Care for Joint Replacement Model
- PROM
Patient-reported outcome measures
- PAC
Post-acute care
- PM&R
Physical Medicine and Rehabilitation
- Neuro-QoL™
Quality of Life in Neurological Disorders
- PROMIS®
Patient-Reported Outcomes Measurement Information System
- SCI-FI
Spinal Cord Injury-Functional Index
- PEDI-CAT
Pediatric Evaluation of Disability Inventory-Computer Adaptive Test
- QRP
Quality Reporting Program
- CAT
Computerized adaptive tests
- EHR
Electronic health record
- CARE tool
Continuity Assessment Record and Evaluation
- AM-PAC CAT
Activity Measure for Post-Acute Care Computer Adaptive Test
- FAM-CAT
Functional Assessment in Acute Care Multidimensional Computer Adaptive Test
Footnotes
Conflicts of Interest: The authors have no conflicts to disclose.
References
- 1.Freburger JK, Holmes GM, Ku LJ. Postacute rehabilitation care for hip fracture: who gets the most care? J Am Geriatr Soc. Oct 2012;60(10):1929–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freburger JK, Li D, Johnson AM, Fraher EP. Physical and Occupational Therapy From the Acute to Community Setting After Stroke: Predictors of Use, Continuity of Care, and Timeliness of Care. Arch Phys Med Rehabil. Jun 2018;99(6):1077–1089 e7. [DOI] [PubMed] [Google Scholar]
- 3.Graham JE, Prvu Bettger J, Middleton A, Spratt H, Sharma G, Ottenbacher KJ. Effects of Acute-Postacute Continuity on Community Discharge and 30-Day Rehospitalization Following Inpatient Rehabilitation. Health Serv Res. Oct 2017;52(5):1631–1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar A, Adhikari D, Karmarkar A, et al. Variation in Hospital-Based Rehabilitation Services Among Patients With Ischemic Stroke in the United States. Phys Ther. May 1 2019;99(5):494–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar A, Rahman M, Trivedi AN, Resnik L, Gozalo P, Mor V. Comparing post-acute rehabilitation use, length of stay, and outcomes experienced by Medicare fee-for-service and Medicare Advantage beneficiaries with hip fracture in the United States: A secondary analysis of administrative data. PLoS Med. Jun 2018;15(6):e1002592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Middleton A, Graham JE, Prvu Bettger J, Haas A, Ottenbacher KJ. Facility and Geographic Variation in Rates of Successful Community Discharge After Inpatient Rehabilitation Among Medicare Fee-for-Service Beneficiaries. JAMA Netw Open. Nov 2 2018;1(7):e184332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reistetter TA, Karmarkar AM, Graham JE, et al. Regional variation in stroke rehabilitation outcomes. Arch Phys Med Rehabil. Jan 2014;95(1):29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Medicare and Medicaid Services (CMS). Bundled Payments for Care Improvement (BPCI) Initiative: General Information. 2020; https://innovation.cms.gov/innovation-models/bundled-payments. Updated June 19, 2020. Accessed June 25, 2020.
- 9.. Patient Driven Payment Model. 2020; https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/PDPM. Updated March 31, 2020. Accessed June 11, 2020.
- 10.Center for Medicare Advocacy. Site Neutral Payment for Rehab Care. 2020; https://medicareadvocacy.org/site-neutral-payment/#:~:text=Site%20Neutral%20Payment%20is%20the,rehabilitation%20hospital%20or%20nursing%20home. Accessed June 11, 2020.
- 11.Centers for Medicare and Medicaid Services (CMS). Overview of CJR Quality Measures, Composite Quality Score, and Pay-for-Performance Methodology. 2020; https://innovation.cms.gov/files/x/cjr-qualsup.pdf. Accessed June 11, 2020.
- 12.Barnett ML, Wilcock A, McWilliams JM, et al. Two-Year Evaluation of Mandatory Bundled Payments for Joint Replacement. N Engl J Med. Jan 17 2019;380(3):252–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haas DA, Zhang X, Kaplan RS, Song Z. Evaluation of Economic and Clinical Outcomes Under Centers for Medicare & Medicaid Services Mandatory Bundled Payments for Joint Replacements. JAMA Intern Med. Jul 1 2019;179(7):924–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu JM, Patel V, Shea JA, Neuman MD, Werner RM. Hospitals Using Bundled Payment Report Reducing Skilled Nursing Facility Use And Improving Care Integration. Health affairs (Project Hope). 2018;37(8):1282–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnett ML, Mehrotra A, Grabowski DC. Postacute Care - The Piggy Bank for Savings in Alternative Payment Models? N Engl J Med. Jul 25 2019;381(4):302–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Health Measures. Transforming How Health is Measured. 2020; https://www.healthmeasures.net/explore-measurement-systems/promis. Accessed October 30, 2020.
- 17.Fyffe D, Kalpakjian CZ, Slavin M, et al. Clinical interpretation of the Spinal Cord Injury Functional Index (SCI-FI). J Spinal Cord Med. Sep 2016;39(5):527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haley SM, Coster WJ, Dumas HM, et al. Accuracy and precision of the Pediatric Evaluation of Disability Inventory computer-adaptive tests (PEDI-CAT). Dev Med Child Neurol. Dec 2011;53(12):1100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olde Rikkert MGM, van der Wees PJ, Schoon Y, Westert GP. Using Patient Reported Outcomes Measures to Promote Integrated Care. Int J Integr Care. Apr 19 2018;18(2):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Verma S. Making it Easier to Compare Providers and Care Settings on Medicare.gov. 2020; https://www.cms.gov/blog/making-it-easier-compare-providers-and-care-settings-medicaregov. Accessed June 11, 2020.
- 21.Gerhardt WE, Mara CA, Kudel I, et al. Systemwide Implementation of Patient-Reported Outcomes in Routine Clinical Care at a Children’s Hospital. Jt Comm J Qual Patient Saf. Aug 2018;44(8):441–453. [DOI] [PubMed] [Google Scholar]
- 22.Health Measures. In Clinical Practice: Clinical Case Studies. 2020; https://www.healthmeasures.net/applications-of-healthmeasures/overview/in-clinical-practice/clinical-case-studies. Accessed June 17, 2020.
- 23.Spindler K. Transforming Healthcare to Value: The Orthopaedic Solution. 2017; https://consultqd.clevelandclinic.org/transforming-healthcare-value-orthopaedic-solution/. Accessed June 17, 2020.
- 24.Cleveland O, Piuzzi NS, Strnad G, et al. Implementing a Scientifically Valid, Cost-Effective, and Scalable Data Collection System at Point of Care: The Cleveland Clinic OME Cohort. J Bone Joint Surg Am. Mar 6 2019;101(5):458–464. [DOI] [PubMed] [Google Scholar]
- 25.Healthcare Partners. About Partners Care Decisions. 2020; http://caredecisions.partners.org/partners-care-decisions/. Accessed June 17, 2020.
- 26.Lavallee DC, Chenok KE, Love RM, et al. Incorporating Patient-Reported Outcomes Into Health Care To Engage Patients And Enhance Care. Health Aff (Millwood). Apr 2016;35(4):575–82. [DOI] [PubMed] [Google Scholar]
- 27.American Academy of Orthopaedic Surgeons (AAOS). About the AAOS Registry Program. 2020; https://www.aaos.org/registries/registry-program/about-the-aaos-registry-program/. Accessed June 17, 2020.
- 28.Anatchkova M, Donelson SM, Skalicky AM, McHorney CA, Jagun D, Whiteley J. Exploring the implementation of patient-reported outcome measures in cancer care: need for more real-world evidence results in the peer reviewed literature. J Patient Rep Outcomes. Dec 27 2018;2(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basch E, Deal AM, Kris MG, et al. Symptom Monitoring With Patient-Reported Outcomes During Routine Cancer Treatment: A Randomized Controlled Trial. J Clin Oncol. Feb 20 2016;34(6):557–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barbera L, Sutradhar R, Seow H, et al. Impact of Standardized Edmonton Symptom Assessment System Use on Emergency Department Visits and Hospitalization: Results of a Population-Based Retrospective Matched Cohort Analysis. JCO Oncol Pract. May 28 2020:JOP1900660. [DOI] [PubMed]
- 31.Basch E, Deal AM, Dueck AC, et al. Overall Survival Results of a Trial Assessing Patient-Reported Outcomes for Symptom Monitoring During Routine Cancer Treatment. JAMA. Jul 11 2017;318(2):197–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheville AL, Moynihan T, Herrin J, Loprinzi C, Kroenke K. Effect of Collaborative Telerehabilitation on Functional Impairment and Pain Among Patients With Advanced-Stage Cancer: A Randomized Clinical Trial. JAMA Oncol. May 1 2019;5(5):644–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Basch E, Wilfong L, Schrag D. Adding Patient-Reported Outcomes to Medicare’s Oncology Value-Based Payment Model. JAMA. Jan 2 2020. [DOI] [PubMed]
- 34.Young G, Schleicher SM, Dickson NR, Lyss AJ. Insights From the Oncology Care First Proposal-Where We’ve Been and Where We’re Going in Value-Based Care. JCO Oncol Pract. Apr 2020;16(4):151–153. [DOI] [PubMed] [Google Scholar]
- 35.Hsiao CJ, Dymek C, Kim B, Russell B. Advancing the use of patient-reported outcomes in practice: understanding challenges, opportunities, and the potential of health information technology. Qual Life Res. Jun 2019;28(6):1575–1583. [DOI] [PubMed] [Google Scholar]
- 36.Austin E, LeRouge C, Hartzler AL, Chung AE, Segal C, Lavallee DC. Opportunities and challenges to advance the use of electronic patient-reported outcomes in clinical care: a report from AMIA workshop proceedings. JAMIA Open. Dec 2019;2(4):407–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bass M, Morris S, Neapolitan R. Utilizing Multidimensional Computer Adaptive Testing to Mitigate Burden With Patient Reported Outcomes. AMIA Annu Symp Proc. 2015;2015:320–8. [PMC free article] [PubMed] [Google Scholar]
- 38.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. Nov 2010;63(11):1179–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haley SM, Siebens H, Coster WJ, et al. Computerized adaptive testing for follow-up after discharge from inpatient rehabilitation: I. Activity outcomes. Arch Phys Med Rehabil. Aug 2006;87(8):1033–42. [DOI] [PubMed] [Google Scholar]
- 40.Jette AM, Haley SM, Ni P, Olarsch S, Moed R. Creating a computer adaptive test version of the late-life function and disability instrument. J Gerontol A Biol Sci Med Sci. Nov 2008;63(11):1246–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tulsky DS, Jette AM, Kisala PA, et al. Spinal cord injury-functional index: item banks to measure physical functioning in individuals with spinal cord injury. Arch Phys Med Rehabil. Oct 2012;93(10):1722–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sisodia RC, Dankers C, Orav J, et al. Factors Associated With Increased Collection of Patient-Reported Outcomes Within a Large Health Care System. JAMA Netw Open. Apr 1 2020;3(4):e202764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heinemann AW, Nitsch KP, Gracz K, Engel E, Wilson M, Zale C. Lessons Learned while Implementing Patient-Reported Outcome Measures in Inpatient Rehabilitation. Archives of Physical Medicine and Rehabilitation. Under Review as part of this supplement [DOI] [PubMed]
- 44.Austin E, LeRouge C, Hartzler AL, Segal C, Lavallee DC. Capturing the patient voice: implementing patient-reported outcomes across the health system. Qual Life Res. Feb 2020;29(2):347–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Daley KN. Adding Power to Systems Science in Rehabilitation. Phys Ther. Aug 1 2018;98(8):725–726. [DOI] [PubMed] [Google Scholar]