ABSTRACT
When patient with coronavirus disease 2019 (COVID-19) are hospitalized, the limited space for activity, disease itself causes fever, muscle aches, fatigue, respiratory failure with mechanical ventilation, or medications such as steroids or neuromuscular blocking can cause muscle dysfunction. Pulmonary rehabilitation (PR) should be arranged for these patients with COVID-19. However, the literature on early PR within 1 week of admission on patients with COVID-19 are limited. This review focuses on early PR in COVID-19 patients admitted to isolation wards or intensive care units. The essential components of early PR programs include education, breathing exercise, airway clearance, and physical activity training. Breathing exercises, including diaphragmatic and pursed-lip breathing, are known to improve lung function in chronic obstructive pulmonary disease and are also recommended for COVID-19 patients. Poor airway clearance can further aggravate pneumonia. Airway clearance techniques help patients to clear sputum and prevent the aggravation of pneumonia. Early physical activity training allows patients to maintain limb muscle function during hospitalization. It is recommended to design appropriate indoor exercise training for patients with frequency 1–2 times a day, and intensity should not be too high (dyspnea Borg Scale ≤3) in the acute stage. In order to achieve safe training, criteria for selecting stable patients and training termination are important. Early PR may help reduce the length of hospital stay, maintain functional status, improve symptoms of dyspnea, relieve anxiety, and maintain health-related quality of life in these patients after discharge.
KEYWORDS: Coronavirus disease 2019, Hospitalization, Pulmonary rehabilitation
INTRODUCTION OF CORONAVIRUS DISEASE 2019
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. It was found in 2019 and has caused a great impact on global public health due to the lack of effective treatment [1]. COVID-19 has spread globally with 540,535,654 confirmed cases and 6,321,976 deaths (June 22, 2022). Disease severity levels are defined as asymptomatic, mild, moderate, severe, and critical [2]. Patients with asymptomatic infection are the patients who test positive for SARS-CoV-2 but without COVID-19-related symptoms. Patients with mild illness are those with COVID-19-related manifestations such as cough, fever, headache, malaise, sore throat, muscle pain, and nausea but without breathlessness, oxygen desaturation, or abnormal chest imaging. Patients with moderate illness are those with rapid or difficulty in breathing, chest tightness or pain, evidence of lower respiratory disease, and oxygen saturation (SpO2) is ≥94% on room air. Patients with severe illness are those with SpO2 <94% on room air, a ratio of arterial partial pressure of oxygen (PaO2) to the fraction of inspired oxygen (FiO2) <300 mm Hg, a RR >30 breaths/min, or lung infiltrates >50%. Patients with a critical illness are those with have septic shock, respiratory failure, or multiple organ dysfunction [2]. Patients with moderate severity are often admitted to the isolation ward. Severe and critical cases of COVID-19 have a high mortality rate with a mortality rate of 35%–85% and they are often admitted to intensive care units (ICUs) [1].
IMPACT OF REDUCTION IN ACTIVITY DURING HOSPITALIZATION
Hospitalization and ICUs care are often required for these patients. During the isolation period in a narrow-range room, fever, muscle aches, anxiety, depression, and fatigue result into reducing daily activity [2,3]. If pneumonia and myocarditis occur, exercise intolerance will be more obvious, resulting in even bed rest [4]. This may result in decreased sputum expectoration and aggravates pneumonia [5]. Prolonged bed rest increases the risk of deep-vein thrombosis and even pulmonary embolism [6]. Therefore, early pulmonary rehabilitation (PR) should be applied to these patients. We systematically searched MEDLINE, EMBASE, CABI, AMED, PUBMED, and CENTRAL for randomized controlled trials (RCTs) of PR in patients of COVID-19 in wards and ICUs. However, there are no RCTs of early PR for patients in the wards or ICUs. Therefore, much of this review is based on observational studies or guidance on PR in patients with COVID-19.
DEFINITION OF PULMONARY REHABILITATION
The European Respiratory Society and American Thoracic Society (ATS/ERS) defined PR as “a comprehensive intervention based on a thorough patient assessment, followed by patient-tailored therapies that include, but are not limited to, exercise training, education, and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence to health-enhancing behaviors” [7,8]. The committee emphasized that the success of PR depends on the essential components provided. The goals of PR include improved exercise capacity, health-related quality of life, and reduced admissions [8]. The “early” PR in patients with COVID-19 was defined as the initiation of PR within 7 days of admission [9]. For the early PR of patients with COVID-19, intervention is still based on the above principles to improve dyspnea, relieve anxiety, reduce complications, maintain function, and improve the health-related quality of life [10]. Although there are some literature on PR in patients with COVID-19, they often focused on patients with COVID-19 who are in recovering stage. There are limited literature on early PR in COVID-19 patients at the acute stage during admission. This review focuses on the early PR in patients with COVID-19 during admission to an isolation ward or ICU. The ATS/ERS Committee discussed the PR of hospitalized patients with COVID-19 and more than 95% of experts agreed that PR should be arranged for patients during hospitalization [11]. We summarize the principle of PR for patients during hospitalization is “at the appropriate time, for the appropriate patients and provide appropriate PR training.” In view of the risk of infection in the hospital during care, as well as the risk of disease progression, the early PR of COVID-19 patients should still be carefully evaluated [12]. If direct supervision is required for PR, medical staff must have complete protective equipment, including gloves, masks, gowns, and facial masks or goggles to reduce the risk of infection [13]. One study showed that no physiotherapists were infected and no subject adverse effects were found in the patients [9]. Early PR in COVID-19 is suggested to be safe for patients and health-care workers [9].
SELECTION OF APPROPRIATE PATIENTS WITH CORONAVIRUS DISEASE 2019 FOR PULMONARY REHABILITATION
The safety should be considered when starting PR in the acute stage. The evaluation items are [14]: (1) Assessment of whether the patient has high-risk factors of disease progression such as advanced age, obesity, diabetes, chronic obstructive pulmonary disease, and heart disease is important before performing PR. (2) Duration of disease onset: 3%–5% of patients may progress to critical conditions within 7–14 days after infection. (3) Symptoms of fever and dyspnea to confirm whether the condition is stable. (4) Vital signs are important [14].
The patients at high risk for PR are listed in Figure 1 [13]. PR training should be excluded when they met these criteria.
Figure 1.
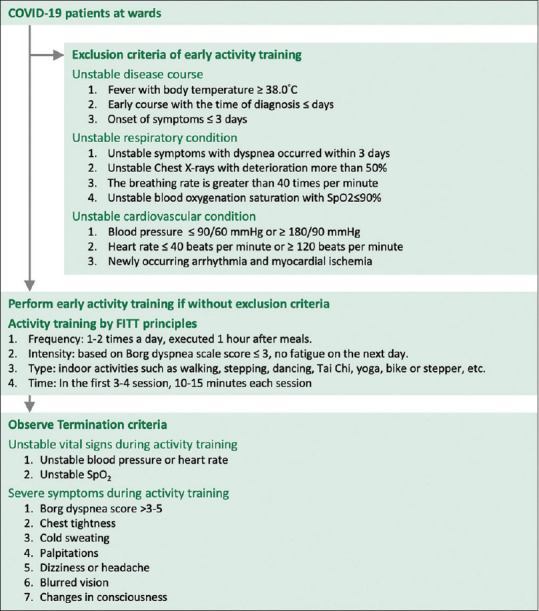
Physical activity training at the isolation ward
PULMONARY REHABILITATION FOR PATIENTS WITH MILD-TO-MODERATE CORONAVIRUS DISEASE 2019 DURING HOSPITALIZATION IN ISOLATION WARDS
Education
Patients should be instructed on wearing masks, expectoration hygiene, and hand hygiene [13]. Education should also be provided on important topics such as the course of COVID-19, nutrition, weight control, activity training, and smoking cessation [12].
Airway clearance techniques
Respiratory secretions can be increased due to COVID-19 infection. The treatment of patients with COVID-19 using airway clearance techniques (ACTs) can help patients to avoid sputum accumulation. However, there are no RCTs that focus on the effect of ACTs in patients with COVID-19. Rather, this advice is derived from the treatment experience of other lung diseases, such as bronchiectasis or COPD [15-17].
Several ACTs can be used to treat patients, including active cycle of breathing techniques (ACBT), forced expiration technique (FET), autogenic drainage (AD), manual techniques (MT), postural drainage (PD), positive expiratory pressure (PEP), oscillating PEP (OPEP), and high-frequency chest wall oscillation (HFCWO) [15-17]. Previous studies on bronchiectasis have shown that ACTs can effectively increase the volume of sputum expectoration [17], and patients have good acceptance and tolerance using ACTs without serious adverse reactions [15]. For patients with COVID-19, ACTs were also included in the PR programs [9,10].
Breathing exercise
Patients can be taught to perform diaphragmatic breathing (DB) and pursed lip breathing (PLB). The recommended frequency is 2–3 times a day, with the duration of the first 3–4 sessions being 10–15 min, with the duration gradually increasing every 2–3 sessions [13]. The goal is to reach a total duration of 30–60 min per day [13]. Past experience in COPD is that a combination of DB and PLB can effectively improve the patient’s lung function and exercise capacity [18]. The combination of DB and PLB is a simple and low-cost physical therapy measure, which should be used as a daily treatment for many respiratory diseases [18]. Thus, we suggest that DB and PLB should be applied in patients with COVID-19.
Physical activity training
Physical activity training is a core component of PR. It is recommended to design exercise training for patients to perform during isolation [10]:
Frequency: One to two times a day, executed 1 h after meals
Intensity should not be too high in the acute stage of COVID-19. The target intensity is based on the dyspnea Borg Scale of ≤3 during activity training. In addition, there should be no feeling of fatigue the next day. After every three to four training sessions, the intensity can be gradually increased to the dyspnea Borg scale of 4–5. However, there should still be no feeling of fatigue when the training intensity is increased
Type: There is no specific type of training. Because patients are isolated in the ward, indoor sports must be designed. If infection control issues are considered, try to focus on training that does not require equipment such as walking, stepping, dancing, Tai Chi, or yoga. If necessary, exercises with equipment such as exercise bikes or steppers can still be used
In the first three to four sessions, 10–15 min each session is suggested. After that, the training duration can be gradually increased as the patient’s tolerance. The goal of the training duration should be 15–45 min for each session, with a training duration of 30–60 min per day
Educate patients to use DB and PLB to make exercise more efficient.
Criteria for training termination
Training must be terminated if they meet the criteria of termination listed in Figure 1 [10].
PULMONARY REHABILITATION OF CRITICALLY ILL PATIENTS WITH CORONAVIRUS DISEASE 2019 IN INTENSIVE CARE UNITS
Situation faced by critically ill patients with coronavirus disease 2019 in intensive care units
Critically ill patients with COVID-19 admitted to an ICU are often under mechanical ventilation, high doses of sedation, and neuromuscular blockers, which cause obvious muscle weakness and physical dysfunction [19].
Due to this muscle weakness and physical dysfunction, they may take months or years to recover. Early PR is recommended to restore physical function as soon as possible.
Although early PR in ICUs is important, it requires careful consideration and should not be at the expense of the safety of medical staff [20].
AIRWAY CLEARANCE TECHNIQUES
ICU-acquired neuromuscular weakness, loss of consciousness, or respiratory muscle weakness may reduce the patient’s ability to clear respiratory secretions. Therefore, ACTs are important. For patients who have not yet been intubated, all the ACTs, including ACBT, FET, PD, MT, AD, PEP, OPEP, and HCWO [15-17]. However, if the patient has been intubated with a mechanical ventilator, the most common method for these patients is chest percussion combined with PD or HFCWO. Li et al. evaluated 13 patients with COVID-19 that were breathing on high-flow nasal oxygenation or nasal cannula in an ICU [21]. They performed ACTs and found that ACTs were safe and associated with improved respiratory and physical function [21].
PHYSICAL ACTIVITY AND EXERCISE TRAINING
Critically ill patients in ICUs are sometimes unstable, and the safety of performing PR must be evaluated carefully [Figure 2] [10].
Figure 2.
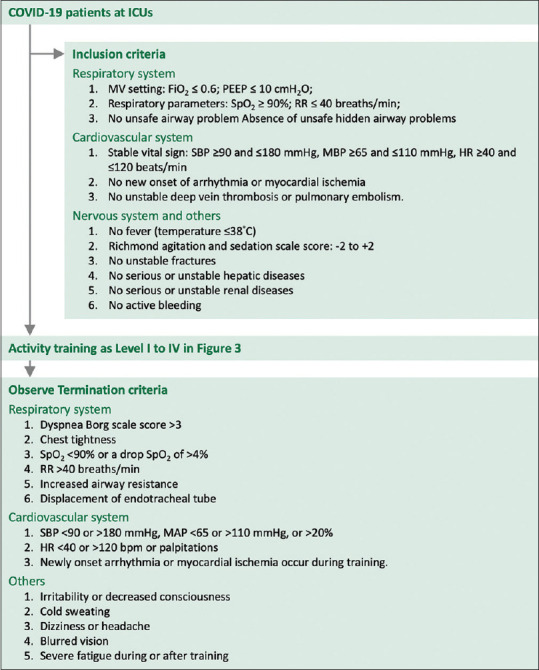
Inclusion and termination criteria for activity training for critically ill patients in intensive care units
Four training levels (Level I to IV) can be designed for critically ill patients [Figure 3] [22]. Level I is for unconscious patients. The caregivers only perform passive range of motion (PROM) on all upper and lower limb joints. Five repetitive PROMs for each joint, three times a day, are recommended.
Figure 3.
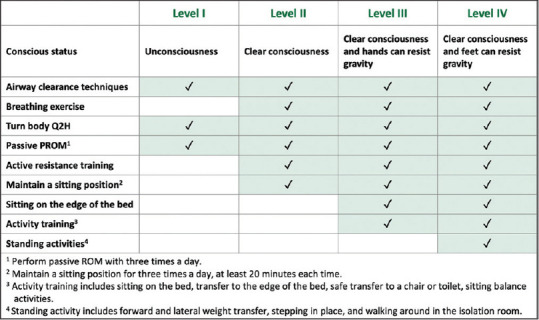
Airway clearance techniques, breathing exercise and physical activity training in intensive care units. *Adapted from “Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med 2008; 36: 2238-43”
Levels II-IV are for conscious patients. Patients must correctly respond to nurses’ or therapist’s commands before being considered for activity training. If the patient’s level of consciousness and the physical condition improves, they can increase their participation. Active activity training can be provided, and the training level can be gradually increased to level III to IV. Training activities are increasingly focused on functional activities, such as transferring to the edge of the bed, safely transferring to a chair or toilet, and seated balance activities. Activity training can progress to standing activities and walking around in the isolation room. It is important to carefully monitor whether patients meet the criteria for terminating training [Figure 2] [10,13]. In addition to activity training, breathing exercises can also be performed if the patient can respond to the order.
CLINICAL STUDIES OF EARLY PULMONARY REHABILITATION IN PATIENTS WITH CORONAVIRUS DISEASE 2019
Clinical studies on the early PR of patients with COVID-19 in isolation wards or ICUs are limited. There is an observational study from a large England hospital, Queen Elizabeth Hospital Birmingham [23]. They included 177 critically ill patients in the ICU. All adults with confirmed COVID-19 and mechanical ventilation used for more than 24 h. Of these 177 critically ill patients, 110 patients survived and they were included in the analysis. The duration of mechanical ventilation was 19 ± 10 days. Most patients (90%) received neuromuscular blocking agents. There were 67% of patients performed at least one prone position. All these patients were assessed by physical therapists within 24 h of admission to the ICU for initiation and progress of PR. The care team assisted patients in repositioning, including prone position, and provided chest physical therapy and activity training. At ICU discharge, 50% of patients were able to stand and step around to a chair. They further analyzed the factors affecting the effects of activity training and revealed that those with high body mass index, elderly patients, and patients with more comorbidities were more likely to require further rehabilitation after discharge [23].
There is an observational study from the National Taiwan University Hospital and College Medicine, Taiwan [24]. Chuang et al. shared the experience of multi-disciplinary PR in critically ill patients [24]. There were four critically ill patients with COVID-19 who used high-flow oxygen nasal cannula, noninvasive positive pressure ventilation, or intubation using mechanical ventilator. The number of days in the ICU was 12—39 days. All patients received physical therapy, occupational therapy, and speech therapy. The duration of patients who received PR was 11—44 days. The score of the Barthel Index at admission was 17.5 (0—40), and the score at discharge was 63.8 (40—65). They also suggested that PR should be performed early during admission [24].
Qi et al., recruited 80 critically ill COVID-19 patients in Chongqing, China, who received PR or usual care within 72 h of ICU admission [25]. They found no significant differences between the PR and usual care groups in terms of mortality rates, and lengths of stay in the ICU and hospital. However, early PR enhanced the duration of ventilator-free days. Total lung capacity, diffusing capacity, Barthel index, health-related quality of life by St. George’s Respiratory Questionnaire, and functional independence at hospital discharge and 1 month after discharge were better in the PR group than those in the usual care group [25].
Recently, there was a retrospective observational study of early PR in patients with COVID-19 [9]. The PR programs included limbs training, respiratory muscle training, and ACTs (PEP and AD). A total of 159 patients were included and PR was performed on 108 patients, 32 patients with early PR and 76 patients with nonearly PR. The mean length of hospital stay was 19 days for the early PR group and 34 days for the nonearly PR group. Obesity, invasive mechanical ventilation, and nonearly PR were identified as independent factors associated with the prolonged hospital stay. They suggested that early PR is safe and could reduce the length of hospital stay. However, the outcomes of dyspnea, walking capacity, quality of life, and lung infiltrates by chest X-ray did not differ between early and nonearly PR groups. In addition, both groups showed a decrease in oxygen therapy and corticosteroid requirements at 2 months [9].
Table 1 summarizes the patient’s character, duration, types, and outcomes of PR in these studies.
Table 1.
Summary of studies on early pulmonary rehabilitation in patients with coronavirus disease 2019
| Study | Patient’s character | Initiation of PR | Duration of PR | Type of PR | Outcomes |
|---|---|---|---|---|---|
| McWilliams et al., 2021 [23] | 110 COVID-19 patients with respiratory failure using IMV | Assessment within 24 h of ICU admission | Not mentioned | Repositioning Chest physiotherapy Mobilization | 50% of patients able to stand and step at ICU discharge |
| Chuang et al., 2022 [24] | Four critically ill patients of COVID-19 Two use HFNC One use HFNC+BIPAP One with IMV | At ICU | 11-44 days | Physical therapy (motor strengthening, balance training, aerobic training and ambulation training) Occupational therapy Speech therapy Breathing exercises | The score of Barthel Index at admission was 17.5 (0-40), and the score at discharge was 63.8 (40-65) |
| Qi, et al., 2020 [25] | 80 critically ill COVID-19 patients 43 patients with PR 37 patients with UC | Within 72 h of ICU admission | Not mentioned | Position management Early mobilization Respiratory muscle training Percussion and vibrations Stretching Physical exercises | No significant differences between the two groups: Mortality rates, lengths of stay in ICU and hospital Ventilator-free days: 5 (3-6) days in PR group, 4 (2–5) in UC group TLC, DLCO, Barthel index, SGRQ and functional independence at hospital discharge and one month after discharge: Better in PR group than those in UC group |
| Bordas-Martínez et al., 2022 [9] | 159 critically ill COVID-19 patients 51 patients without PR 32 patients with early PR 76 patients with nonearly PR | Within 1 week of admission | Not mentioned | Limbs muscle training Respiratory muscle training Airway clearance techniques | The mean length of hospital stay was 19 days for early PR group and 34 days for nonearly PR group The outcomes of dyspnea, walking capacity, quality of life, lung infiltrates, decrease in oxygen therapy and corticosteroids requirements at 2 months did not differ between early and nonearly PR groups |
BiPAP: Bi-phase positive airway pressure, COVID-19: Coronavirus disease 2019, DLCO: Diffusing capacity for carbon monoxide, HFNC: High-flow nasal cannula, ICU: Intensive care unit, IMV: Invasive mechanical ventilation, PR: Pulmonary rehabilitation, SGRQ: St. George’s respiratory questionnaire, TLC: Total lung capacity, UC: Usual care, 6MWD: 6-min walking distance, FEV1 (%): First second of forced expiration % predicted, FVC (%): Forced vital capacity % predicted, HAD questionnaire: Hospital Anxiety and Depression questionnaire, PCLS: Posttraumatic stress disorder checklist scale, PImax: Maximal inspiratory pressures
CONCLUSIONS
Appropriate PR should be provided for carefully selected patients with COVID-19 during hospitalization in isolated wards or ICUs. Early PR including education, airway clearance, and physical activity training may help maintain functional status, improve symptoms of dyspnea, relieve anxiety, and maintain health-related quality of life for these patients after discharge. Proper PR programs, criteria for inclusion, and termination for early activity training are important. This review provides these important issues for early PR in patients with COVID-19 during admission.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zhang J, Huang X, Ding D, Zhang J, Xu L, Hu Z, et al. Comparative study of acute lung injury in COVID-19 and non-COVID-19 patients. Front Med (Lausanne) 2021;8:666629. doi: 10.3389/fmed.2021.666629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maier HE, Kuan G, Saborio S, Bustos Carrillo FA, Plazaola M, Barilla C, et al. Clinical spectrum of SARS-CoV-2 infection and protection from symptomatic re-infection. Clin Infect Dis. 2022;75:e257–66. doi: 10.1093/cid/ciab717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dong L, Bouey J. Public mental health crisis during COVID-19 pandemic, China. Emerg Infect Dis. 2020;26:1616–8. doi: 10.3201/eid2607.200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woods JA, Hutchinson NT, Powers SK, Roberts WO, Gomez-Cabrera MC, Radak Z, et al. The COVID-19 pandemic and physical activity. Sports Med Health Sci. 2020;2:55–64. doi: 10.1016/j.smhs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li B, Li Z, Cheng W, Zhang B, Zhu W, Lin Z. Application of sputum suction by fiberoptic bronchoscope in patients with severe pneumonia and its effect on inflammatory factors. Am J Transl Res. 2021;13:8409–14. [PMC free article] [PubMed] [Google Scholar]
- 6.Kaptein FH, Stals MA, Huisman MV, Klok FA. Prophylaxis and treatment of COVID-19 related venous thromboembolism. Postgrad Med. 2021;133:27–35. doi: 10.1080/00325481.2021.1891788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American thoracic society/European respiratory society statement:Key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:e13–64. doi: 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 8.Holland AE, Cox NS, Houchen-Wolloff L, Rochester CL, Garvey C, ZuWallack R, et al. Defining modern pulmonary rehabilitation. An official American thoracic society workshop report. Ann Am Thorac Soc. 2021;18:e12–29. doi: 10.1513/AnnalsATS.202102-146ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bordas-Martínez J, Luzardo-González A, Arencibia A, Tormo F, Matéu L, Vicens-Zygmunt V, et al. Effects of early physical therapy and follow-up in acute severe coronavirus disease 2019 pneumonia:A retrospective observational study. Front Med (Lausanne) 2022;9:866055. doi: 10.3389/fmed.2022.866055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhao HM, Xie YX, Chen Wang C. Recommendations for respiratory rehabilitation of coronavirus disease 2019 in adult. Chin Med J. 2020;43:308–14. [Google Scholar]
- 11.Spruit MA, Holland AE, Singh SJ, Tonia T, Wilson KC, Troosters T. COVID-19:Interim guidance on rehabilitation in the hospital and post-hospital phase from a European respiratory society and american thoracic society-coordinated international task force. Eur Respir J. 2020;56:2002197. doi: 10.1183/13993003.02197-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak –An update on the status. Mil Med Res. 2020;7:11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang TJ, Chau B, Lui M, Lam GT, Lin N, Humbert S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am J Phys Med Rehabil. 2020;99:769–74. doi: 10.1097/PHM.0000000000001505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aly MH, Rahman SS, Ahmed WA, Alghamedi MH, Al Shehri AA, Alkalkami AM, et al. Indicators of critical illness and predictors of mortality in COVID-19 patients. Infect Drug Resist. 2020;13:1995–2000. doi: 10.2147/IDR.S261159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eaton T, Young P, Zeng I, Kolbe J. A randomized evaluation of the acute efficacy, acceptability and tolerability of flutter and active cycle of breathing with and without postural drainage in non-cystic fibrosis bronchiectasis. Chron Respir Dis. 2007;4:23–30. doi: 10.1177/1479972306074481. [DOI] [PubMed] [Google Scholar]
- 16.Phillips J, Lee A, Pope R, Hing W. Effect of airway clearance techniques in patients experiencing an acute exacerbation of bronchiectasis:A systematic review. Physiother Theory Pract. 2020;36:1300–15. doi: 10.1080/09593985.2019.1579286. [DOI] [PubMed] [Google Scholar]
- 17.Snijders D, Fernandez Dominguez B, Calgaro S, Bertozzi I, Escribano Montaner A, Perilongo G, et al. Mucociliary clearance techniques for treating non-cystic fibrosis bronchiectasis:Is there evidence? Int J Immunopathol Pharmacol. 2015;28:150–9. doi: 10.1177/0394632015584724. [DOI] [PubMed] [Google Scholar]
- 18.Yang Y, Wei L, Wang S, Ke L, Zhao H, Mao J, et al. The effects of pursed lip breathing combined with diaphragmatic breathing on pulmonary function and exercise capacity in patients with COPD:A systematic review and meta-analysis. Physiother Theory Pract. 2022;38:847–57. doi: 10.1080/09593985.2020.1805834. [DOI] [PubMed] [Google Scholar]
- 19.Van Aerde N, Van den Berghe G, Wilmer A, Gosselink R, Hermans G COVID-19 Consortium. Intensive care unit acquired muscle weakness in COVID-19 patients. Intensive Care Med. 2020;46:2083–5. doi: 10.1007/s00134-020-06244-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67:568–76. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li L, Yu P, Yang M, Xie W, Huang L, He C, et al. Physical therapist management of COVID-19 in the intensive care unit:The West China hospital experience. Phys Ther. 2021;101:pzaa198. doi: 10.1093/ptj/pzaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36:2238–43. doi: 10.1097/CCM.0b013e318180b90e. [DOI] [PubMed] [Google Scholar]
- 23.McWilliams D, Weblin J, Hodson J, Veenith T, Whitehouse T, Snelson C. Rehabilitation levels in patients with COVID-19 admitted to intensive care requiring invasive ventilation. An observational study. Ann Am Thorac Soc. 2021;18:122–9. doi: 10.1513/AnnalsATS.202005-560OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chuang HJ, Hsiao MY, Wang TG, Liang HW. A multi-disciplinary rehabilitation approach for people surviving severe COVID-19-a case series and literature review. J Formos Med Assoc. 2022 doi: 10.1016/j.jfma.2022.02.002. S0929-6646:00064-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qi D, Xiang J, Peng J, Yu Q, Tang X, Tong J, et al. Effects of early physical and pulmonary rehabilitation for severely and critically ill covid-19 patients:A retrospective, cohort, and multicenter study. Res Sq. 2020:1–17. [Google Scholar]


