Abstract
Introduction
The Food and Drug Administration (FDA) has issued proposed product standards banning menthol as a characterising flavour in cigarettes and cigars. The public health benefits of these product standards may be attenuated by the role of plausible substitutes in the marketplace. Therefore, the present study examined the addiction potential of plausible combustible menthol alternatives compared with usual brand menthol cigarettes (UBMC).
Methods
Ninety-eight adult menthol cigarette smokers completed four visits, smoking their UBMC at the first session and three menthol cigarette alternatives in random order at the subsequent visits: (1) a preassembled menthol roll-your-own (mRYO) cigarette using menthol pipe tobacco and mentholated cigarette tube, (2) a menthol filtered little cigar (mFLC) and (3) a non-menthol cigarette (NMC). Measures of smoking topography, exhaled carbon monoxide (CO), craving and withdrawal, subjective effects and behavioural economic demand indices were assessed.
Results
Compared with UBMC, menthol cigarette alternatives resulted in different puffing topography and CO exposure (except mRYO), and lower levels of positive subjective experience and behavioural economic demand indices. Among the alternative products, participants reported the highest level of positive subjective experience and higher demand for mRYO, compared with mFLC and NMC. Similarly, participants were significantly more likely to want to try again, purchase and use the mRYO product regularly compared with mFLC and NMC.
Conclusions and relevance
mRYO cigarettes were the most highly rated cigarette alternative among study products, suggesting their potential appeal as a menthol cigarette substitute and needed inclusion of menthol pipe tobacco and cigarette tubes in FDA’s proposed ban.
Keywords: Addiction, Smoking topography, Public policy, Hand-rolled/RYO tobacco
WHAT IS ALREADY KNOWN ON THIS TOPIC
Menthol cigarettes are associated with increased smoking initiation, higher nicotine dependence and decreased adult cessation, particularly among vulnerable populations. To address this public health issue, the Food and Drug Administration announced in April 2021 its intention to issue product standards banning menthol as a characterising flavour in both cigarettes and cigars within a year. However, the public health benefits of these product standards may be attenuated by the role of plausible substitutes available in the marketplace.
WHAT THIS STUDY ADDS
In this randomised cross-over design study that included 98 adult menthol cigarette smokers, each of the alternative products demonstrated the ability to significantly reduce nicotine craving and withdrawal symptoms, but the combination of mentholated pipe tobacco and tubes in a menthol roll-your-own cigarette resulted in the highest behavioural economic demand and positive subjective experience.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
To maximise the benefits of a menthol cigarette ban, restrictions should extend to plausible substitutes, particularly menthol pipe tobacco and cigarette tubes.
Introduction
The decreasing prevalence of cigarette smoking in the USA1 has been driven by decreases in non-menthol cigarette (NMC) use.2 3 In contrast, menthol cigarette consumption has remained largely stable since 2000, resulting in a more than 10% increase in menthol cigarette market share over the past two decades2 and reaching 37% market share in 2020.4 Menthol cigarettes are associated with increased smoking initiation and progression to regular use,5 6 higher nicotine dependence and decreased adult cessation.7–9 People who smoke menthol cigarettes are also more likely to be of low socioeconomic status, female, black or Hispanic, and identify as lesbian, gay, bisexual and transgender compared with non-menthol smokers.10 11 Menthol cigarette smoking is estimated to have caused 10.1 million extra smokers, 3 million life years lost and 378 000 premature deaths between 1980 and 2018.12
The 2009 Family Smoking Prevention and Tobacco Control Act granted the US Food and Drug Administration (FDA) broad authority to regulate tobacco products, leading to bans of flavoured cigarettes, excluding menthol, and some flavoured e-cigarette devices. In May 2022, the FDA issued proposed rules for product standards banning menthol as a characterising flavour in both cigarettes and cigars.13 14 While evidence from systematic reviews,7 15–17 evaluations of Ontario’s menthol cigarette ban18–20 and simulation studies strongly support the likely positive public health impact of a menthol ban on cigarette and cigars,21–23 experimental evidence is also needed to bolster these findings to withstand tobacco industry lawsuits.
Even with regulation, tobacco companies frequently exploit regulatory loopholes to maintain sales of their products.24 25 Djarum, for example, launched clove filtered cigars in the USA in anticipation of the 2009 ban on flavoured cigarettes, and sales of clove filtered cigars increased by more than 1400% between 2009 and 2012.26 Similarly, following the 2009 Children’s Health Insurance Programme Reauthorization Act, which levied large increases in federal excise tax rates on cigarettes, cigars and roll-your-own (RYO) tobacco, tobacco companies repackaged and labelled RYO tobacco as pipe tobacco to avoid these policies.27 As a result, while the market share of pipe tobacco declined from 30.4% in 2002 to 13.6% in 2008, it increased significantly to 89.6% in 2012.27 This reflects an increase of approximately 25.49 million pounds of loose tobacco (ie, RYO and pipe tobacco) sold per year from 2002 to 2012.27 These examples highlight how the potential public health benefits of regulation, such as a product standard, can be attenuated and suggest that estimating the impact of a potential ban on menthol in cigarettes requires accounting for likely substitutes in the marketplace that may also need to be restricted to effectively protect public health.
Current tobacco products, including menthol filtered little cigars (mFLCs), menthol pipe tobacco and cigarette tubes for menthol roll-your-own (mRYO) cigarettes, and NMC, are relevant targets as potential menthol cigarette substitutes.28 Neither mRYO nor NMC will be affected by the proposed FDA ban on menthol cigarettes and cigars. NMC, mFLC and mRYO are all comparable to menthol cigarettes with respect to shape, size and filters,25 29 and both mFLCs and mRYO are increasing in use.30–32 While no single study has compared all of these products, findings are mixed in terms of differences in user puffing topography, nicotine delivery and toxicant exposure.31–35 The limited research does suggest that each of these products are capable of delivering significant levels of nicotine and harmful tobacco-related toxicants. With important FDA menthol regulation under way, it is critical to assess their potential as substitutes to help guide effective FDA regulation, closing any pertinent loopholes (eg, mentholated pipe tobacco and cigarette tubes), and to provide support for further regulation of NMCs (eg, reducing nicotine to non-addictive levels).
With the ultimate goal of informing FDA menthol regulations by identifying potential market substitutes that may attenuate the positive public health effects of the proposed regulation, the purpose of this study was to assess the addiction potential of other plausible combustible menthol cigarette alternatives in adults who smoke menthol cigarettes by examining the impact of these alternatives on subjective effects, behavioural economic demand indices, smoking topography and resultant toxicant exposure compared with the participants’ usual brand menthol cigarette (UBMC). We hypothesised that, compared with UBMC, alternatives would result in similar smoking topography and carbon monoxide (CO) exposure, but fewer positive subjective effects and lower demand.
Methods
Setting and participants
Menthol cigarette smokers from the Columbus, Ohio metropolitan area, were recruited via internet advertisements, flyers and word-of-mouth advertising from January 2020 to August 2021. Potential participants were screened for eligibility via an online questionnaire and then over the telephone. Eligibility criteria included (1) current menthol cigarette smoker (>90% menthol cigarette use, ≥5 cigarettes per day) for at least the past 6 months; (2) between 21 and 50 years old; (3) willing to abstain from tobacco, nicotine and marijuana use for at least 12 hours prior to each of the study visits; (4) access to a smartphone or email, and (5) ability to read and speak in English. Exclusionary criteria included (1) self-reported diagnosis of lung disease; (2) cardiac event or distress within the past 3 months; (3) pregnancy, breast feeding or planning to become pregnant; (4) use of other tobacco products (eg, e-cigarette, cigar, etc) >5 days in the past month; (5) currently using one of the study products; (6) any reported use of illicit drugs (other than marijuana) during the last 30 days; and (7) currently engaging in smoking cessation treatment.
Procedure
Using an in-laboratory and outpatient mixed design, participants completed a three-phase study lasting approximately 3 weeks. In phase I, the participants completed four smoking session visits, smoking their UBMC or one of the three menthol cigarette alternatives at each visit. Each visit was separated by a 48-hour washout period. This phase used multiple methods of assessing addiction potential in a lab-based setting, including measurements of drug self-administration, suppression of craving and withdrawal, measures of drug liking and behavioural economic measures.36 In phase II, the participants were instructed to completely substitute their preferred product from phase I for their UBMC for 1 week and to complete daily assessments of their use behaviour. In phase III, the participants completed a final in-lab visit to assess the substitutability of their preferred product, under simulated ban conditions using a progressive ratio task. We report the results of phase I further.
All participants completed sociodemographic measures and provided their tobacco use history including their years of smoking, usual cigarette brand, smoking frequency and quantity, number and recency of previous quit attempts, and their level of cigarette dependence (Fagerstrom Test for Nicotine Dependence).37 Then, over four visits, the participants completed standardised smoking sessions, smoking a different product each session. During each session, a research assistant with a stopwatch instructed the participants to take a puff every 30 s, resulting in 10 puffs during the first 5 min. Participants sampled their UBMC during the first session; the order of subsequent products was randomised at the time of enrolment from a prespecified block randomisation table with blocks of size 6. Products included a preassembled (by study staff), machine-injected RYO cigarette using a mentholated cigarette tube and mentholated pipe tobacco (mRYO; OHM menthol pipe tobacco, hot rod tubes, menthol king size), an mFLC (Cheyenne 100’s menthol) and a NMC (Newport Non-Menthol Red). For mRYO assembly, the Powermatic III was used to insert 1 g of tobacco into the rod to fill. See online supplemental table 1 and figure 1 for additional product characteristics. When machine-smoked, NMC had the greatest nicotine emissions (mg/rod) (M=2.51, SD=0.13), followed by mRYO (M=2.11, SD=0.08) and then mFLC (M=0.99, SD=0.11); mFLC had the highest menthol emissions (mg/rod) (M=3.04, SD=0.30), followed by mRYO (M=2.25, SD=0.16) and NMC with the least (M=0.003, SD=0.000); and mFLC had the highest resistance to draw (mm H2O) (M=193.0, SD=13.0), followed by NMC (M=123.0, SD=6.9) and mRYO with the least (M=103.0, SD=8.3). All products were provided in plain boxes without brand or identifying information. Brand name was present, however, on the NMC filter wrapper. The participants were instructed to abstain from smoking (biochemically confirmed with exhaled CO ≤10 ppm),38 39 as well as from nicotine and marijuana for 12 hours before the sessions (abstinence from nicotine and marijuana was not confirmed).
tc-2022-057421supp001.pdf (2.3MB, pdf)
During the smoking session, participant puffing topography was collected using the eTop (American University of Beirut), which includes mouthpiece adaptors to accommodate cigarettes of different diameters and provides valid measurements at puff flow rates as low as 3 mL/s.40 41 Puffing topography measures collected included average flow rate, interpuff interval, puff volume, puff duration, maximum puff volume and total inhaled volume. Measures of cigarette craving (Tiffany-Drobes Questionnaire of Smoking Urges (QSU): Brief Form42 and withdrawal (Minnesota Nicotine Withdrawal Scale (MNWS)43) were also administered immediately before (0) and after the smoking session (5 min), and at 15, 30, 60 and 90 min. The QSU is a 10-item self-report measure with items rated from 1 (strongly disagree) to 7 (strongly agree). Items are summed and have been shown to load on two factors—‘desire to smoke’ and ‘anticipated relief from withdrawal’. For the MNWS, participants completed the 15-item version, but for analysis, we used the nine-item version assessing the Diagnostic and Statistical Manual of Mental Disorders symptoms for Tobacco Withdrawal and the ‘craving to smoke’ item; items were rated on a 5-point scale from 0 (none) to 4 (severe) and summed. We did not include sleep problems in our analysis since this item was not expected to change during the smoking sessions. Exhaled breath carbon monoxide level (eCO), a biomarker of smoke exposure, was assessed using a handheld monitor (Smokerlyzer Micro, Bedfont Scientific) at time 0 and 5 min to determine eCO boost (eCO at time 5 min minus eCO at time 0).
After each smoking session, measures of subjective effects were completed. The 11-item modified Cigarette Evaluation Questionnaire (mCEQ)44 45 includes five subscales: Smoking Satisfaction, Psychological Reward, Aversion, Enjoyment of Respiratory Tract Sensations and Craving Reduction, with items rated from 1 (not at all) to 7 (extremely likely). Five visual analogue scale items ranging from 0 (‘not at all’) to 100 (‘extremely’) assessed wanting to smoke the product again, liking the product, enjoying the product, and finding the product pleasurable and satisfying.46 47 Behavioural intentions to use the menthol cigarette alternatives were also collected. Participants reported how likely they were to ‘try this product again’, ‘purchase this product for personal use’ and ‘use this product regularly’ if menthol cigarettes were no longer available to be purchased; responses were rated on a 5-point scale (1, extremely unlikely; 2, unlikely; 3, neutral; 4, likely; 5, extremely likely). For analysis, answers were collapsed into ‘unlikely’ for users who responded ‘extremely unlikely’ or unlikely, ‘neutral’ for those who answered neutral, and ‘likely’ for those who answered extremely likely or likely. Participants also completed the Cigarette Purchase Task,48 49 a behavioural economic task that assesses hypothetical tobacco product consumption across varying prices. Demand indices include demand intensity (Q 0; the number of products consumed per day when free), essential value (EV, a measure of reinforcing efficacy that measures the rate of change in demand elasticity across the range of prices), Pmax (the price associated with the maximal expenditure, ie, the highest price before the curve changes from inelastic to elastic) and breakpoint (the last price in which consumption is greater than 0), with higher scores indicating greater abuse liability. Finally, following the completion all of smoking sessions, the participants selected their most preferred menthol alternative product to completely substitute for their UBMC for 1 week.
Data analytical plan
The study was powered based on a laboratory study examining the abuse liability of cigarettes containing different doses of nicotine,50 such that with 80 participants, there was over 80% power to detect decreases in product satisfaction of up to 50% as compared with UBMC and decreases of 68%–72% in the cigarette purchase task indices of maximum expenditure, maximum price and price sensitivity.
Topography measures were winsorised at the 1st and 99th percentiles and analysed using repeated measures analysis of variance (ANOVA) with Tukey’s adjustment for all pairwise comparisons between products. Subjective smoking experiences were similarly analysed using repeated measures ANOVA models with Tukey’s adjustment, while the categorical behavioural intentions data were modelled with mixed effects multinomial logistic regression. For QSU, which was measured repeatedly within each visit, linear mixed effects models with Holm’s procedure to adjust for post hoc comparisons were used to assess differences between products. Further, logistic regression was employed to assess the association of demographic and tobacco use characteristics with selection of mRYO as the preferred product. For all models, log transformations were employed as necessary to satisfy assumptions. All analyses were conducted in SAS V.9.4.
Demand data were fit to the normalised zero-bound model of demand using the freely available GraphPad Prism template provided by the Institute for Behaviour Resources (https://ibrinc.org/behavioral-economics-tools/). To assess normality for all demand indices, we conducted the D’Agostino-Pearson omnibus normality test using GraphPad Prism V.9. Results indicated the distributions for all demand indices deviated from a Gaussian distribution; therefore, we used the non-parametric Friedman test with Dunn’s correction for multiple comparisons for all analyses (see online supplemental appendix for detailed methods).
Results
Participant demographics and smoking history
A total of 98 participants enrolled in the study and were included in the analysed sample. The participants had a mean age of 37.0 years (SD=7.4) were predominantly female (74.5%), white (69.4%) and non-Hispanic or Latino (93.9%, table 1). The participants reported smoking an average of 11.9 cigarettes per day (SD=5.5) and smoking at this frequency for the last 15.9 years (SD=9.8), with a mean FTND (Fagerstrom Test for Nicotine Dependence) score of 3.44 (SD=2.16), indicating a moderate level of dependence. The participants reported minimal past 30-day use of other tobacco products (table 1).
Table 1.
Demographics and tobacco use history (n=98)
| Analysed sample (n=98) |
||
| Demographics | ||
| Age (years), mean (SD) | 37.04 | 7.43 |
| What term below best describes your ethnicity? n (%) | ||
| Hispanic or Latino | 6 | 6.12 |
| Not Hispanic or Latino | 92 | 93.88 |
| What term(s) below best describe your race? n (%) | ||
| Black or African–American | 19 | 19.39 |
| White or Caucasian | 68 | 69.39 |
| Biracial or multiracial | 11 | 11.22 |
| Below is a list of terms that people often use to describe their sexuality or sexual orientation. Please check the term that best applies to you. n (%) | ||
| Gay | 3 | 3.06 |
| Bisexual | 17 | 17.35 |
| Straight/eterosexual | 77 | 78.57 |
| Queer | 1 | 1.02 |
| What sex were you assigned at birth (what the doctor put on your birth certificate)? n (%) | ||
| Male | 25 | 25.51 |
| Female | 73 | 74.49 |
| What is the highest level of school you have completed? n (%) | ||
| 12th grade, no diploma | 3 | 3.06 |
| High school graduate/GED | 17 | 17.35 |
| Some college, no degree /associates degree | 53 | 54.08 |
| Bachelor’s degree/master’s degree | 25 | 25.51 |
| Which of the following categories best describes your total household income in the past 12 months? n (%) | ||
| Less than $35 000 | 42 | 42.86 |
| $35 000–$149 999 | 56 | 57.14 |
| On average, about how many cigarettes do you currently smoke each day? (one pack usually equals 20 cigarettes) (mean, SD) | 11.90 | 5.49 |
| Years smoked at this frequency (mean, SD) | 15.85 | 9.83 |
| Usual brand of store-bought cigarettes, n (%) | ||
| Marlboro | 23 | 23.47 |
| Newport | 28 | 28.57 |
| Camel | 23 | 23.47 |
| Maverick | 8 | 8.16 |
| American Spirit | 4 | 4.08 |
| Other | 12 | 12.24 |
| Years smoked this brand of cigarettes (mean, SD) | 10.16 | 8.02 |
| Fagerstrom Test for Nicotine Dependence Score (mean, SD) | 3.44 | 2.16 |
| Other tobacco product use in past 30 days (n, %) | ||
| Any | 21 | 21.43 |
| Pipe (with tobacco, not including hookah) | 2 | 2.04 |
| Cigars (like Cohiba or Romeo y Julieta) | 4 | 4.08 |
| Cigarillos | 4 | 4.08 |
| Little cigars or filtered cigars | 2 | 2.04 |
| e-cigarette or vaping device (like JUUL, blu, Vuse, MarkTen or Suorin) | 17 | 17.35 |
| Smokeless tobacco (like chewing tobacco, snuff or dip) | 2 | 2.04 |
| Snus (like Camel Snus) | 0 | 0.00 |
| Hookah/shisha/waterpipe/hookah tobacco | 2 | 2.04 |
Smoking topography and eCO boost
Table 2 compares all four products on topography and exposure measures. Compared with smoking UBMC, the participants demonstrated greater puff duration and eCO boost when smoking mFLC, as well as a lower flow rate, average puff volume, total inhaled volume and maximum puff volume. When smoking NMC, the participants had smaller average puff volume and total inhaled volume than any of three mentholated products. No significant differences in topography were seen between UBMC and mRYO.
Table 2.
Smoking topography for UBMCs and menthol cigarette alternatives (n=98)
| UBMC | mRYO cigarette | mFLC | NMC | |
| M (SD) | M (SD) | M (SD) | M (SD) | |
| Average puff duration* (s) | 1.99 (0.56)† | 2.06 (0.64)†‡ | 2.65 (0.90)§¶‡ | 1.87 (0.60)¶† |
| Average flow rate (ml/s) | 23.77 (6.98)† | 24.89 (7.53)†‡ | 16.97 (5.42)§¶‡ | 22.07 (7.22)¶† |
| Average interpuff interval (s) | 27.54 (1.71)† | 27.54 (1.22)† | 26.35 (2.64)§¶‡ | 27.77 (1.58)† |
| Average puff volume (mL) | 45.74 (13.49)†‡ | 48.19 (12.40)†‡ | 42.53 (12.77)§¶‡ | 38.96 (12.10)§¶† |
| Maximum puff volume (mL) | 63.16 (18.81)†‡ | 63.94 (15.23)†‡ | 56.59 (18.71)§¶ | 55.92 (16.16)§¶ |
| Total inhaled volume (mL) | 462.56 (138.46)†‡ | 484.78 (124.38)†‡ | 434.66 (127.95)§¶‡ | 389.33 (122.21)‡§† |
| CO boost (ppm) | 8.10 (3.92)† | 7.36 (2.98)† | 9.30 (4.35)§¶‡ | 7.71 (2.91)† |
Mean (M) and SDs for topography measures. P values estimated from repeated measures analysis of variance with Tukey adjustment for all pairwise comparisons. All measures were winsorised at the 1st and 99th percentiles. Superscripts denote differences in pairwise comparisons between study products at the p<0.05 level.
*Variable log transformed for analysis. See online supplemental table 2 for specific p values.
†Differs from mFLC.
‡Differs from NMC.
§Differs from UBMC.
¶Differs from mRYO.
mFLC, menthol filtered little cigar; mRYO, menthol roll-your-own; NMC, non-menthol cigarette; UBMC, usual brand menthol cigarette.
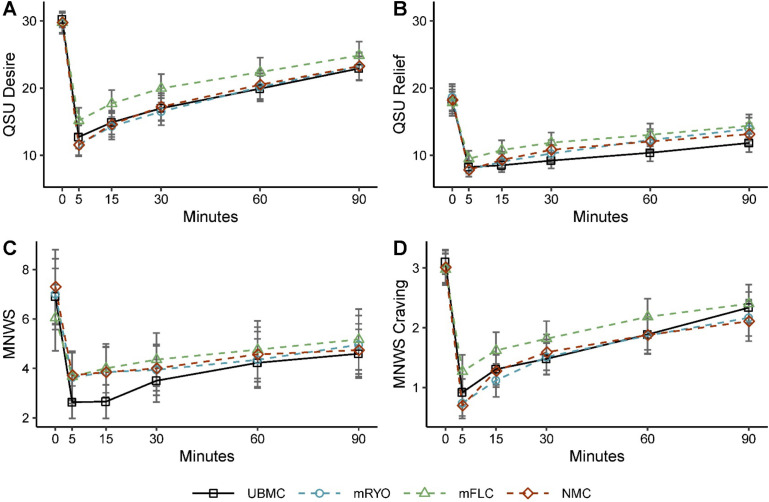
Cigarette craving and withdrawal
Mean values for QSU–brief desire and relief factors for all four products over time are depicted in figure 1A,B, respectively. Significant within-participant reduction was observed in both subscales for all products following the initial directed puffing segment, supporting the ability of each of the four products to reduce craving. Significant differences comparing UBMC to the study products were not observed for desire or anticipated relief (see online supplemental table 3A,B for p values). Similarly, significant within-participant reduction was observed in withdrawal symptoms for all products following the initial directed puffing segment, but no significant differences were observed between any of the products (figure 1C,D; see online supplemental table 3online supplemental appendix 1 for p values).
Figure 1.
Measures of cigarette craving (Tiffany-Drobes QSU) and withdrawal (MNWS) for each product (n=98). (A) QSU–Desire, (B) QSU–Relief, (C) MNWS withdrawal symptoms and (D) MNWS craving. Mean and 95% CI estimated immediately before (0) and after the smoking session (5 min), and at 15, 30, 60 and 90 min; QSU–Relief and MNWS were log transformed for analysis. mFLC, menthol filtered little cigar; MNWS, Minnesota Nicotine Withdrawal Scale; mRYO, menthol roll-your-own; NMC, non-menthol cigarette; QSU, Questionnaire of Smoking Urges; UBMC, usual brand menthol cigarette.
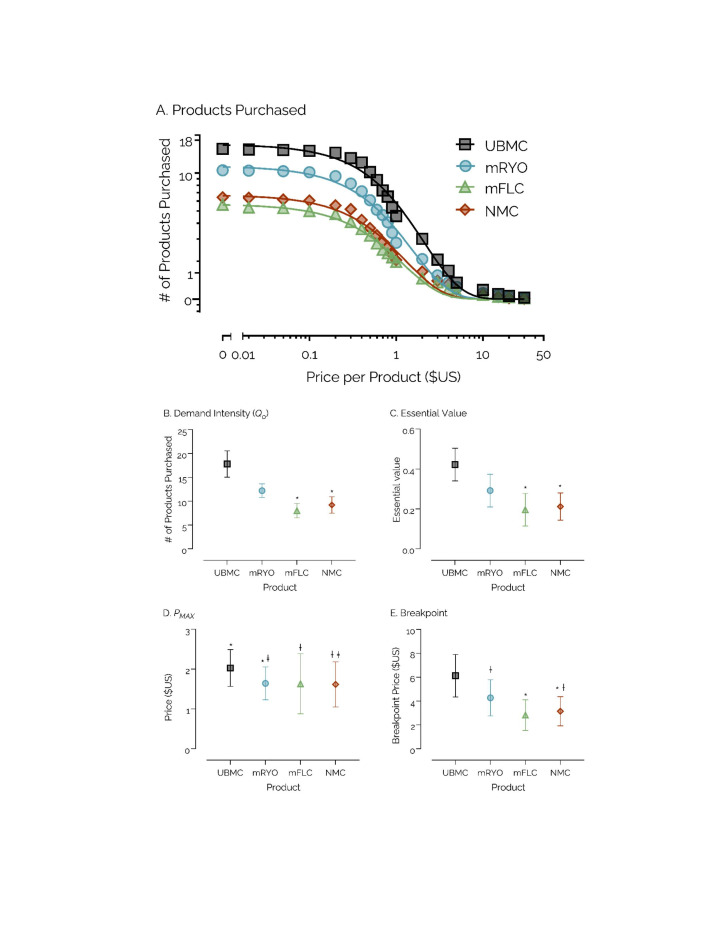
Product demand indices
Demand curves for four participants (5%) were determined to be non-systematic and were removed from analyses. Post hoc analyses for multiple comparisons indicated significantly greater addiction potential of UBMC when compared with all three alternative products for measures of demand intensity, EV and breakpoint (p<0.05; figure 2). Among alternative products, mRYO indicated the greatest addiction potential, with significantly higher intensity and EV than both mFLC and NMC, significantly higher Pmax than NMC, and significantly higher breakpoint than mFLC (p<0.05). There were no significant differences between NMC and mFLC.
Figure 2.
Behavioural economic measures of addiction potential by study product (n=76). (A) Overall demand across all four products. Data points indicate estimated daily consumption (y-axis) across varying price points per cigarette ranging from $0 (free) to $30 (x-axis) for all participants. (B–E) Demand indices across all four products. Data points represent mean scores across participants with 95% CIs. Along the x-axis is product type, and along the y-axis are the respective scores or price (in US$). For all indices, a higher score or price indicates greater abuse liability. Data points that do not share a symbol differ significantly (p <0.05). Note: four participants were removed from analyses due to non-systematic data. mFLC, menthol filtered little cigar; mRYO, menthol roll-your-own; NMC, non-menthol cigarette; UBMC, usual brand menthol cigarette.
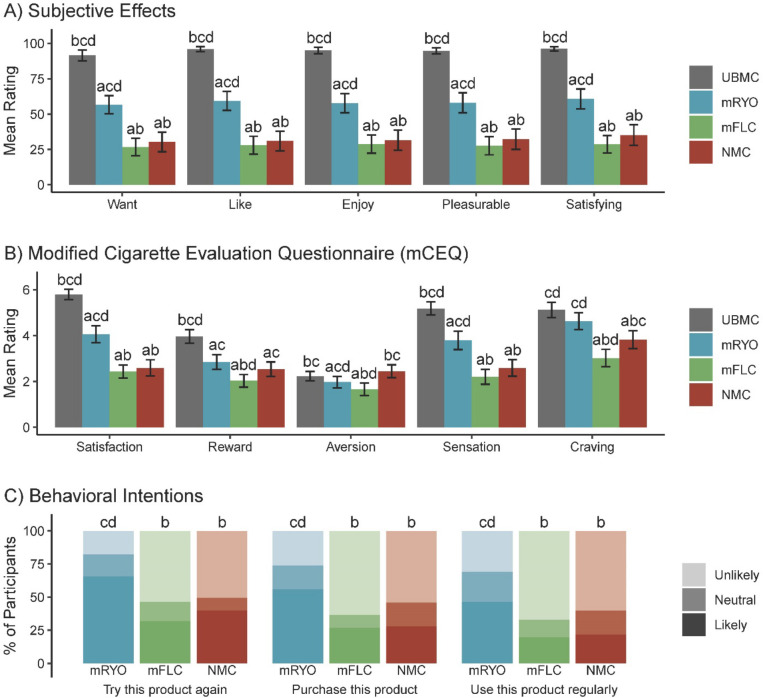
Subjective smoking experience, behavioural intentions and product selection
Figure 3 depicts mean ratings for all subjective smoking experience items, and online supplemental table 4 provides p values for all comparisons. Compared with UBMC, the participants reported significantly lower levels of wanting to smoke the product again, liking, enjoyment, pleasure and satisfaction for each of the alternative products (p<0.001, figure 3A). Among the alternative products, the participants reported the most favourable subjective experience when smoking mRYO (p<0.001) compared with mFLC and NMC, with no significant differences between mFLC and NMC (figure 3A). Similarly, on the mCEQ, UBMCs were rated as more satisfying, rewarding and had more enjoyable sensations in the throat and chest than the alternative products (p<0.05, figure 3B). However, UBMC had similar levels of aversion to NMC and higher levels compared with mRYO and mFLC (p<0.05, figure 3B). Similarly, UBMC had similar levels of craving reduction to mRYO but higher levels compared with mFLC and NMC (p<0.05, figure 3B). The participants were also significantly more likely to want to try again (p<0.001), purchase (p<0.001) and use the mRYO product regularly (p<0.001) compared with mFLC and NMC, with no significant differences between mFLC and NMC (figure 3C). Consistent with these findings, 65.0% (n=52) of the participants chose mRYO as their preferred menthol alternative to use during phase II; 22.5% (n=18) chose NMC; and 12.5% chose mFLC (n=10). In a supplementary analysis to examine potential predictors of mRYO as the preferred menthol alternative, neither UBMC, ever use of other tobacco products, sexual orientation nor race was significantly associated with mRYO preference (see online supplemental appendix 1).
Figure 3.
Subjective effects, mCEQ and behavioural intentions by study product (n=98). P values estimated from mixed effects models accounting for repeated measures, mCEQ-Aversion was log transformed for analysis; superscripts denote differences in pairwise comparisons between study products at p<0.05. a, differs from UBMC; b, differs from mRYO; c, differs from mFLC; d, differs from NMC. mCEQ, modified Cigarette Evaluation Questionnaire; mFLC, enthol filtered little cigar; mRYO, menthol roll-your-own; NMC, non-menthol cigarette; UBMC, usual brand menthol cigarette.
Discussion
Using a large within-subjects study of adults who smoke menthol cigarettes and multiple methods of assessing addiction potential, our study expands prior cross-over studies of menthol and NMCs33–35 to include other potential menthol cigarette substitutes, specifically mFLCs and the combination of mentholated pipe tobacco and tubes in a mRYO. The variability in the physical attributes and mainstream emissions of the mRYO cigarette was similar to the other study products, indicating the by-hand preparation of this product was carried out with a reproducibility similar to that obtained by commercial machines. All products suppressed craving and withdrawal, with few differences over time across the four study products. Findings on subjective effects of each product were similar to other studies,33 34 with participants reporting the most favourable subjective effects for their UBMC, with mRYO cigarettes rated next highest and outperforming the other two menthol cigarette alternatives. In line with behavioural intention data on likelihood of trying, purchasing and using the product regularly, prefilled mRYO cigarettes were the products chosen by most participants to be used in a subsequent 1-week trial at home and the most highly rated cigarette alternative, suggesting their potential appeal as a menthol cigarette substitute. These findings are of particular importance, given the components of this product: pipe tobacco, which now comprises most of the loose tobacco market,27 and cigarette tubes, which have been authorised by the FDA in prior substantial equivalence applications. While the FDA used its enforcement authority in 2013 to call out misbranding of RYO cigarette tobacco as pipe tobacco,51 retailer education in 2021 embraced slippage between the product categories and encouraged convenience store owners and operators to promote both to their clients.52 Given the 2020 court order vacating the FDA’s health warning requirement for pipe tobacco,53 continued ambiguity in differentiating pipe from RYO tobacco, and anticipated FDA action on menthol cigarettes and cigars, our findings suggest that components of mRYO products, including menthol rolling papers, cigarette tubes and pipe tobacco, be considered for inclusion under a menthol cigarette ban.
Beyond measures of the subjective experiences of smoking, topography data provide useful information about how the product is likely to be used in the natural environment and can significantly influence uptake of nicotine in the body, both critical for the addiction potential and toxicity of menthol cigarette alternatives.36 Findings showed that UBMC and mRYO cigarettes were used similarly. There were several topography measures that differed, however, between UBMCs and the other two study products, which may be related to the more negative subjective ratings of these products. Consistent with other studies,34 35 participants had shorter puff duration, lower average puff volume and lower total inhaled smoke volume when using NMC compared with any of the mentholated products. The higher smoke volume seen for our three menthol products may result in higher exposure to nicotine, tobacco-specific nitrosamines and ultrafine particulates.35 Novel findings supported that compared with all other products, mFLC had a higher puff duration, lower average flow rate and higher CO boost. This finding likely reflects both the greater density of tobacco in the filtered cigar product and the much higher resistance to draw.54 Increased puff duration may also be related to the mFLC’s lower nicotine delivery, which was at most half that of the other two study products. The higher exhaled CO for mFLC is likely related to the incomplete combustion that comes from the narrower, longer and more densely packed column of tobacco and the lower flow rate of air through the burning end of the cigarette. The puffing behaviour data suggest that mFLCs, used as cigarettes,30 may induce greater smoke exposure in their users.
Strengths of our study include use of a within-subjects design, multiple methods of estimating the addiction potential of menthol cigarette alternatives and a large clinical laboratory sample of adults who currently smoke menthol cigarettes. The fact that our sample had a high proportion of people who identified as white and female and of lower socioeconomic status is both a strength and a limitation of our study. Even though the prevalence of menthol cigarette use is highest among black adults who smoke,3 11 there remains a larger absolute number of white adults who smoke menthol cigarettes in the USA. Our sample reflects the midwestern city in which it was recruited but is likely generalisable to a broader population of menthol cigarette smokers in the USA, including women and people of lower socioeconomic status who have a higher prevalence of menthol cigarette use.3 11 While our study design is consistent with recommended methods to determine the comparative abuse liability of tobacco products,36 the use of a longer ad libitum use period, in addition to a standardised puffing session, may have further elucidated differences in puffing topography and drug self-administration. Our study’s use of a limited number of products to evaluate menthol cigarette alternatives does not reflect the range of alternative products that could be substituted for menthol cigarettes under a potential ban, but recent research using an online experimental tobacco marketplace to simulate product choice following a menthol cigarette ban supports menthol little cigars, NMCs, menthol cigarillos and menthol vapes as potential substitutes.55 Expanding our multimethod design to a broader range of products, including menthol e-cigarettes and other mentholated smokeless tobacco products, may identify the most likely menthol cigarette alternative.
Our current findings suggest that menthol pipe tobacco and tubes should be a target for research and regulation. The FDA’s current proposal to restrict the use of menthol in both cigarettes and cigars has the potential to significantly improve public health with a reduction in new smokers as well as increased cessation among current mentholated cigarette and cigar smokers. Recent announcements regarding a product standard for reduced nicotine content in cigarettes may also reduce the harms of NMCs,56 studied in this trial. However, the present findings suggest that components of mRYO products, including menthol rolling papers, cigarette tubes and pipe tobacco, should also be included in the menthol cigarette and flavoured cigar product standards. Their absence from this restriction will result in a critical loophole that is already being exploited by the tobacco industry and has the potential to attenuate the potential public health benefits of the proposed menthol ban.
Footnotes
Twitter: @TheodoreWagener
Contributors: TLW and ACV conceived of and designed the study and wrote the manuscript. TM managed the study and was overseen by TLW and ACV. AH, JAS and TGE conducted and are responsible for the data analysis. MCB and CW conducted tobacco product characterisation, including emissions testing. TM, AH, JAS, TGE, MCB, CW, and JT reviewed, edited and approved the final version. TLW, ACV and AH had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. TLW is responsible for the overall content as guarantor.
Funding: Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health (under award number R21DA046333; MPI: TLW and ACV). JS, JT and TE were supported by the National Institute on Drug Abuse of the National Institutes of Health (under award number U54DA036114). MCB, TLW and CW also received salary support from UC2FD007229. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the US Food and Drug Administration. The funder had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The corresponding author will make deidentified participant data and the data dictionary available following publication. Institutions and individuals wishing to access any resources or data must contact the corresponding author (theodore.wagener@osumc.edu). Data will only be made available to those whose proposed use of the data has been approved by the corresponding author. Data will be made available for the sole purpose of replicating the analyses reported in the manuscript. The recipient must agree to not transfer the data to other users and that the data are only to be used for research purposes. The private investigators will require requestors of data to sign a data sharing agreement that will ensure (1) use of the data is only for research purposes, (2) data security using appropriate technology/firewalls, (3) destruction of data after data analysis and (4) proper citation in publications or other written materials. A record of transfer of data and a copy of the dataset that was distributed will be kept by The Ohio State University.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the institutional review board (IRB) of Ohio State University (IRB protocol number 2019C0107). All participants provided written informed consent before taking part in the study.
References
- 1. Cornelius ME, Wang TW, Jamal A, et al. Tobacco Product Use Among Adults - United States, 2019. MMWR Morb Mortal Wkly Rep 2020;69:1736–42. 10.15585/mmwr.mm6946a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Delnevo CD, Giovenco DP, Villanti AC. Assessment of menthol and Nonmenthol cigarette consumption in the US, 2000 to 2018. JAMA Netw Open 2020;3:e2013601. 10.1001/jamanetworkopen.2020.13601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Villanti AC, Mowery PD, Delnevo CD, et al. Changes in the prevalence and correlates of menthol cigarette use in the USA, 2004-2014. Tob Control 2016;25:ii14–20. 10.1136/tobaccocontrol-2016-053329 [DOI] [PubMed] [Google Scholar]
- 4. Federal Trade Commission . Federal Trade Commission cigarette report for 2020, 2021. Available: https://www.ftc.gov/reports/federal-trade-commission-cigarette-report-2020-smokeless-tobacco-report-2020 [Accessed 03 Nov 2021].
- 5. Villanti AC, Johnson AL, Glasser AM, et al. Association of flavored tobacco use with tobacco initiation and subsequent use among US youth and adults, 2013-2015. JAMA Netw Open 2019;2:e1913804. 10.1001/jamanetworkopen.2019.13804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Villanti AC, Johnson AL, Halenar MJ, et al. Menthol and MINT cigarettes and Cigars: initiation and progression in youth, young adults and adults in waves 1-4 of the path study, 2013-2017. Nicotine Tob Res 2021;23:1318–26. 10.1093/ntr/ntaa224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Villanti AC, Collins LK, Niaura RS, et al. Menthol cigarettes and the public health standard: a systematic review. BMC Public Health 2017;17:983. 10.1186/s12889-017-4987-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Delnevo CD, Gundersen DA, Hrywna M, et al. Smoking-cessation prevalence among U.S. smokers of menthol versus non-menthol cigarettes. Am J Prev Med 2011;41:357–65. 10.1016/j.amepre.2011.06.039 [DOI] [PubMed] [Google Scholar]
- 9. Smith PH, Assefa B, Kainth S, et al. Use of Mentholated cigarettes and likelihood of smoking cessation in the United States: a meta-analysis. Nicotine Tob Res 2020;22:307–16. 10.1093/ntr/ntz067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rath JM, Villanti AC, Williams VF, et al. Correlates of current menthol cigarette and flavored other tobacco product use among U.S. young adults. Addict Behav 2016;62:35–41. 10.1016/j.addbeh.2016.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Delnevo CD, Ganz O, Goodwin RD. Banning menthol cigarettes: a social justice issue long overdue. Nicotine Tob Res 2020;22:1673–5. 10.1093/ntr/ntaa152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Le TT, Mendez D. An estimation of the harm of menthol cigarettes in the United States from 1980 to 2018. Tob Control 2021. doi: 10.1136/tobaccocontrol-2020-056256. [Epub ahead of print: 25 Feb 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. U.S. Food and Drug Administration . Tobacco product standard for characterizing flavors in Cigars, 2022. Available: https://www.federalregister.gov/documents/2022/05/04/2022-08993/tobacco-product-standard-for-characterizing-flavors-in-cigars
- 14. U.S. Food and Drug Administration . Tobacco product standard for menthol in cigarettes, 2022. Available: https://www.federalregister.gov/documents/2022/05/04/2022-08994/tobacco-product-standard-for-menthol-in-cigarettes
- 15. Tobacco Products Scientific Advisory Committee . Menthol cigarettes and public health: review of the scientific evidence and recommendations. Rockville, MD: Center for Tobacco Products, Food and Drug Administration, 2011. [Google Scholar]
- 16. U.S. Food and Drug Administration . Preliminary scientific evaluation of the possible public health effects of menthol versus Nonmenthol cigarettes. Silver Spring, MD: Center for Tobacco Products, Food and Drug Administration, 2013. [Google Scholar]
- 17. U.S. Food and Drug Administration . Reference addendum: preliminary scientific evaluation of the possible public health effects of menthol versus Nonmenthol cigarettes. Silver Spring, MD: Center for Tobacco Products, Food and Drug Administration, 2013. [Google Scholar]
- 18. Chaiton M, Schwartz R, Cohen JE, et al. Association of Ontario's ban on menthol cigarettes with smoking behavior 1 month after implementation. JAMA Intern Med 2018;178:710–1. 10.1001/jamainternmed.2017.8650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chaiton M, Schwartz R, Shuldiner J, et al. Evaluating a real world ban on menthol cigarettes: an interrupted time-series analysis of sales. Nicotine Tob Res 2020;22:576–9. 10.1093/ntr/ntz041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chaiton MO, Nicolau I, Schwartz R, et al. Ban on menthol-flavoured tobacco products predicts cigarette cessation at 1 year: a population cohort study. Tob Control 2020;29:341–7. 10.1136/tobaccocontrol-2018-054841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Levy DT, Meza R, Yuan Z, et al. Public health impact of a US ban on Menthol in cigarettes and cigars: a simulation study. Tob Control 2023;32:e37–44. 10.1136/tobaccocontrol-2021-056604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Li Y, Sisti J, Flórez KR, et al. Assessing the health and economic impact of a potential menthol cigarette ban in New York City: a modeling study. J Urban Health 2021;98:742–51. 10.1007/s11524-021-00581-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Levy DT, Pearson JL, Villanti AC, et al. Modeling the future effects of a menthol ban on smoking prevalence and smoking-attributable deaths in the United States. Am J Public Health 2011;101:1236–40. 10.2105/AJPH.2011.300179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Delnevo CD, Giovenco DP, Miller Lo EJ. Changes in the Mass-merchandise cigar market since the tobacco control act. Tob Regul Sci 2017;3:8–16. 10.18001/TRS.3.2(Suppl1).2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Delnevo CD, Hrywna M, Giovenco DP, et al. Close, but no cigar: certain cigars are pseudo-cigarettes designed to evade regulation. Tob Control 2017;26:349–54. 10.1136/tobaccocontrol-2016-052935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Delnevo CD, Hrywna M. Clove cigar sales following the US flavoured cigarette ban. Tob Control 2015;24:e246–50. 10.1136/tobaccocontrol-2013-051415 [DOI] [PubMed] [Google Scholar]
- 27. Agaku IT, Alpert HR. Trends in annual sales and current use of cigarettes, cigars, roll-your-own tobacco, pipes, and smokeless tobacco among US adults, 2002-2012. Tob Control 2016;25:451–7. 10.1136/tobaccocontrol-2014-052125 [DOI] [PubMed] [Google Scholar]
- 28. MENTHOL . What works and what don't?: Roll Your Own Resource, 2015. Available: http://www.rollyourownresource.com/forums/viewtopic.php?t=707 [Accessed 12 Sep 2017].
- 29. Byron MJ, Strasser AA, Delnevo CD. Little and filtered cigars meet the legal definition of cigarettes and should be included in nicotine reduction regulation. Tob Control 2019;28:350–1. 10.1136/tobaccocontrol-2018-054410 [DOI] [PubMed] [Google Scholar]
- 30. Delnevo CD, Hrywna M. "A whole 'nother smoke" or a cigarette in disguise: how RJ Reynolds reframed the image of little cigars. Am J Public Health 2007;97:1368–75. 10.2105/AJPH.2006.101063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Koszowski B, Rosenberry ZR, Strasser AA, et al. Experimentally switching from factory made to Self-Made cigarettes: a preliminary study of perceptions, toxicant exposure and smoking behavior. J Addict Res Ther 2014;5:179. 10.4172/2155-6105.1000179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hamad SH, Johnson NM, Tefft ME, et al. Little Cigars vs 3R4F cigarette: physical properties and HPHC yields. Tob Regul Sci 2017;3:459–78. 10.18001/TRS.3.4.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Strasser AA, Ashare RL, Kaufman M, et al. The effect of menthol on cigarette smoking behaviors, biomarkers and subjective responses. Cancer Epidemiol Biomarkers Prev 2013;22:382–9. 10.1158/1055-9965.EPI-12-1097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Watson CV, Richter P, de Castro BR, et al. Smoking behavior and exposure: results of a menthol cigarette cross-over study. Am J Health Behav 2017;41:309–19. 10.5993/AJHB.41.3.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Brinkman MC, Chuang JC, Gordon SM, et al. Exposure to and deposition of fine and ultrafine particles in smokers of menthol and nonmenthol cigarettes. Inhal Toxicol 2012;24:255–69. 10.3109/08958378.2012.667218 [DOI] [PubMed] [Google Scholar]
- 36. Carter LP, Stitzer ML, Henningfield JE, et al. Abuse liability assessment of tobacco products including potential reduced exposure products. Cancer Epidemiol Biomarkers Prev 2009;18:3241–62. 10.1158/1055-9965.EPI-09-0948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Heatherton TF, Kozlowski LT, Frecker RC, et al. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br J Addict 1991;86:1119–27. 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- 38. SRNT Subcommittee on Biochemical Verification . Biochemical verification of tobacco use and cessation. Nicotine Tob Res 2002;4:149–59. 10.1080/14622200210123581 [DOI] [PubMed] [Google Scholar]
- 39. Brose LS, Tombor I, Shahab L, et al. The effect of reducing the threshold for carbon monoxide validation of smoking abstinence-evidence from the English Stop Smoking Services. Addict Behav 2013;38:2529–31. 10.1016/j.addbeh.2013.04.006 [DOI] [PubMed] [Google Scholar]
- 40. Felicione NJ, Karaoghlanian N, Shihadeh A, et al. Comparison of measurement methods for electronic cigarette puff topography. Tob Regul Sci 2020;6:318–30. 10.18001/TRS.6.5.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shihadeh A, Antonios C, Azar S. A portable, low-resistance puff topography instrument for pulsating, high-flow smoking devices. Behav Res Methods 2005;37:186–91. 10.3758/BF03206414 [DOI] [PubMed] [Google Scholar]
- 42. Cox LS, Tiffany ST, Christen AG. Evaluation of the brief questionnaire of smoking urges (QSU-brief) in laboratory and clinical settings. Nicotine Tob Res 2001;3:7–16. 10.1080/14622200020032051 [DOI] [PubMed] [Google Scholar]
- 43. Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry 1986;43:289–94. 10.1001/archpsyc.1986.01800030107013 [DOI] [PubMed] [Google Scholar]
- 44. Cappelleri JC, Bushmakin AG, Baker CL, et al. Confirmatory factor analyses and reliability of the modified cigarette evaluation questionnaire. Addict Behav 2007;32:912–23. 10.1016/j.addbeh.2006.06.028 [DOI] [PubMed] [Google Scholar]
- 45. Westman E, Levin E, Rose J. Smoking while wearing the nicotine patch-is smoking satisfying or harmful. Clinical Research 1992;40:A871–A71. [Google Scholar]
- 46. Leavens EL, Driskill LM, Molina N, et al. Comparison of a preferred versus non-preferred waterpipe tobacco flavour: subjective experience, smoking behaviour and toxicant exposure. Tob Control 2018;27:319–24. 10.1136/tobaccocontrol-2016-053344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wagener TL, Leavens ELS, Mehta T, et al. Impact of flavors and Humectants on Waterpipe tobacco smoking topography, subjective effects, Toxicant exposure and intentions for continued use. Tob Control 2021;30:366–72. 10.1136/tobaccocontrol-2019-055509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jacobs EA, Bickel WK. Modeling drug consumption in the clinic using simulation procedures: demand for heroin and cigarettes in opioid-dependent outpatients. Exp Clin Psychopharmacol 1999;7:412–26. 10.1037/1064-1297.7.4.412 [DOI] [PubMed] [Google Scholar]
- 49. MacKillop J, Murphy JG, Ray LA, et al. Further validation of a cigarette purchase task for assessing the relative reinforcing efficacy of nicotine in college smokers. Exp Clin Psychopharmacol 2008;16:57–65. 10.1037/1064-1297.16.1.57 [DOI] [PubMed] [Google Scholar]
- 50. Higgins ST, Heil SH, Sigmon SC, et al. Addiction potential of cigarettes with reduced nicotine content in populations with psychiatric disorders and other vulnerabilities to tobacco addiction. JAMA Psychiatry 2017;74:1056–64. 10.1001/jamapsychiatry.2017.2355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Campaign for Tobacco-Free Kids . Fda acts to stop Misbranding of Roll-Your-Own cigarette tobacco as pipe tobacco, 2013. Available: https://www.tobaccofreekids.org/press-releases/2013_08_12_fda_ryo [Accessed 31 Jan 2021].
- 52. Ericksen AB. What is the difference between RYO and pipe tobacco?: CStore decisions, 2021. Available: https://cstoredecisions.com/2021/04/19/what-is-the-difference-between-ryo-and-pipe-tobacco/ [Accessed 31 Jan 2022].
- 53. U.S. Food and Drug Administration . Compliance policy for certain labeling and warning statement requirements for Cigars and pipe tobacco, 2020. Available: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/compliance-policy-certain-labeling-and-warning-statement-requirements-cigars-and-pipe-tobacco [Accessed 31 Jan 2022].
- 54. Reilly SM, Goel R, Bitzer Z, et al. Little Cigars, filtered Cigars, and their carbonyl delivery relative to cigarettes. Nicotine Tob Res 2018;20:S99–106. 10.1093/ntr/ntx274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Denlinger-Apte RL, Cassidy RN, Carey KB, et al. The impact of menthol flavoring in combusted tobacco on alternative product purchasing: a pilot study using the experimental tobacco marketplace. Drug Alcohol Depend 2021;218:108390. 10.1016/j.drugalcdep.2020.108390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. U.S. Food and Drug Administration . Fda Announces plans for proposed rule to reduce Addictiveness of cigarettes and other combusted tobacco products, 2022. Available: https://www.fda.gov/news-events/press-announcements/fda-announces-plans-proposed-rule-reduce-addictiveness-cigarettes-and-other-combusted-tobacco [Accessed 09 Jun 2022].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tc-2022-057421supp001.pdf (2.3MB, pdf)
Data Availability Statement
Data are available upon reasonable request. The corresponding author will make deidentified participant data and the data dictionary available following publication. Institutions and individuals wishing to access any resources or data must contact the corresponding author (theodore.wagener@osumc.edu). Data will only be made available to those whose proposed use of the data has been approved by the corresponding author. Data will be made available for the sole purpose of replicating the analyses reported in the manuscript. The recipient must agree to not transfer the data to other users and that the data are only to be used for research purposes. The private investigators will require requestors of data to sign a data sharing agreement that will ensure (1) use of the data is only for research purposes, (2) data security using appropriate technology/firewalls, (3) destruction of data after data analysis and (4) proper citation in publications or other written materials. A record of transfer of data and a copy of the dataset that was distributed will be kept by The Ohio State University.