Abstract
Assisted living provides housing and long-term care services to more than 811,000 older adults in the United States daily, and is regulated by the states. This study describes changes in the specificity of state regulations governing the staffing in assisted living settings (that is, requirements for sufficient staffing or staffing ratios or levels) between 2007 and 2018 and the association between these changes and rates of hospitalization among a national sample of assisted living residents, including a subgroup with dementia. We found that increased regulatory specificity for direct care workers (for example, a change from requiring “sufficient” direct care worker staffing to requiring a specific staffing ratio or level) is associated with a 4 percent reduction in the monthly risk for hospitalization among residents in our sample and a 6 percent reduction among the subgroup with dementia. However, an increase in regulatory specificity for licensed practical nurses is associated with a 2.5 percent increase in the monthly risk for hospitalization and a 5 percent increase among the subgroup with dementia. Given that no federal requirements for the number of staff members or composition of staff in assisted living exist, these findings can inform states’ policy decisions about staffing requirements for assisted living settings.
Keywords: Assisted Living, Long-term Care, Staffing, State Policy
Assisted living provides housing and long-term care services to more than 811,000 older adults in the US each day. Residents in assisted living settings receive assistance in activities of daily living (for example, 64 percent needed assistance with bathing and 48 percent with dressing in 2015–16), and many have complex health service needs (for example, 42 percent had dementia in 2015–16).1 However, unlike nursing homes, assisted living communities are regulated by states, which vary in their regulatory approach, including their staffing requirements.2-5
Previous research suggests that staffing levels and skill mix in assisted living vary considerably, from communities without any presence of licensed nurses to those in which licensed nurses deliver a significant amount of care.6 This variability is believed to be a function of services offered,6 resident case-mix,7 and state regulations.8,9 It has also been documented that licensed nurse staffing levels are higher among assisted living communities with dementia units than among those without.10 Staffing levels, training, and skill mix are posited to have implications for quality of life and safety, particularly among persons living with dementia in assisted living.11
Research in the nursing home setting has consistently correlated higher staffing levels with better quality of care12-14 and changes in staffing requirements with improvements in nursing home residents’ outcomes.15 However, there is limited evidence to understand the staffing–outcomes relationship in assisted living, particularly as it relates to hospitalization—a patient-centered outcome that is publicly reported in other long-term settings as an important marker of quality. The studies that have examined the relationship between assisted living staffing and hospitalization, although valuable, are limited in their generalizability and interpretation because they focus on specific geographies or employ a cross-sectional study design.7,16,17
In an effort to build the evidence base around the impact of staffing regulations on assisted living residents’ outcomes, we use an established methodology to identify a national cohort of Medicare beneficiaries residing in assisted living settings with twenty-five or more beds.18,19 We also use a data set of the substantive changes made to state regulations that governed assisted living communities from 2007 to 2018.4 These regulations are documented at the license level. This is important because staffing requirements can vary within a state by license and certification (hereafter, license types). In Florida, for example, an assisted living facility can be certified to provide both limited nursing services and limited mental health—two separate certifications that have different staffing requirements.20
We draw on neo-institutional theory to understand the relationship between changes to assisted living staffing regulations and residents’ outcomes.21 From this perspective, regulations affect assisted living providers’ behaviors (for example, staffing decisions) through the apparent means of mandatory legal compliance, but also through shifts in expectations from customers and other service providers, financial pressures from market changes, and normative pressures from competitors.22 Although we cannot capture and dissociate these pathways, our study describes the association between changes in the specificity of assisted living staffing-related regulations with the rates of hospitalization among assisted living residents, including a subgroup of residents living with dementia. We hypothesize that in response to more prescriptive, or “specific,” staffing requirements, providers change their behaviors (for example, increase staff presence) in ways that affect residents’ outcomes—namely, hospitalization.
Study Data And Methods
Overview
In this retrospective cohort study, we combined administrative data from the Centers for Medicare and Medicaid Services (CMS) with historical data on state regulations pertaining to assisted living staffing. We examined the association between increased specificity in the regulations (for example, including more detailed requirements such as staffing levels) and the hospitalization of assisted living residents.
Data
The Medicare Master Beneficiary Summary File was used to obtain each beneficiary’s age, race, sex, and dual Medicare and Medicaid enrollment. The Chronic Conditions Warehouse segment of the Master Beneficiary Summary File was used to identify beneficiaries’ chronic conditions. The Master Beneficiary Summary File was linked to a ZIP code history file to obtain beneficiaries’ residential ZIP codes over time.19 The Medicare Provider Analysis and Review file was used to identify any acute care hospitalization.
Data on staffing policies came from prior work recording the specificity of assisted living regulations for each type of licensed assisted living setting (n = 350 license types across the fifty states and Washington, D.C., in 2018), sourced using the LexisNexis legal database.4 The resulting data set consisted of binary variables indicating the presence or absence of provisions specific to staffing in the rules applicable to each type of licensed setting on December 31 of each study year.
Variables
Our outcome variable of interest was acute care hospitalization. We specified whether or not a beneficiary residing in assisted living at the start of each month had an acute care hospitalization while in assisted living (that is, before transfer to a nursing home) in each of the 144 study months.
Our exposure of interest was the specificity of state regulations pertaining to staffing. As a component of stringency, which additionally encompasses the breadth of regulations, oversight processes, and penalties associated with noncompliance, specificity referred to the level of details in the regulations, such as the minimum number of required licensed practical nurses on site. Our reasons for focusing on specificity versus stringency were both theoretical and practical. First, we posited that changes in organizations’ behaviors are spurred by more than enforcement alone, consistent with neo-institutional theory. Second, our analysis was based on a single topic—staffing—to isolate specific regulatory provisions that policy makers can address and that are likely to be associated with the outcome of interest, hospitalization. Finally, there are no national, standardized data on enforcement practices for assisted living.
To construct an exposure variable representing the specificity of staffing regulation, we assigned a specificity score to each license type and year for three types of staff members who care for residents: direct care workers or certified nursing assistants (heretofore, direct care workers), licensed practical nurses, and registered nurses. The specificity score ranged from 0 to 3 for each type of staff, with a score of 3 indicating the most specific regulatory requirements, such as a minimum staffing ratio (see online appendix exhibits 1 and 2).23 We also created an overall specificity score by summing the scores for each staff type, which could range from 0 to 9. Each resident was assigned a regulatory specificity score based on the license type of the assisted living community in which the person lived at the beginning of the index month.
To adjust for any changes over time in residents’ characteristics that could be correlated with hospitalization risk, we included time-varying resident-level covariates that reflected residents’ sociodemographic characteristics (that is, age, sex, race, dual enrollment in Medicare and Medicaid) and health status (that is, indicators for the presence and cumulative number of thirteen chronic conditions such as cancer, depression, and heart failure). See the appendix for the full list of chronic conditions.23
Sample
To identify Medicare beneficiaries residing in assisted living communities, we used a previously published methodology relying on beneficiaries’ nine-digit ZIP codes reported in the Master Beneficiary Summary File.18,19 Because a larger assisted living community (one with twenty-five or more beds) is likely to have its own nine-digit ZIP code, if not multiple nine-digit ZIP codes, we created a yearly finder file of nine-digit ZIP codes that correspond to continuously operating and licensed larger (twenty-five or more beds) assisted living communities. Although larger assisted living communities (twenty-five or more beds) make up approximately 39 percent of these settings, they include 84 percent of all licensed beds nationally.1 Using this finder file, we searched beneficiaries’ residential ZIP codes to identify fee-for-service Medicare beneficiaries with a nine-digit ZIP code corresponding to an assisted living community on the first of each month, excluding settings where we identified fewer than ten beneficiaries. Our final analytic sample included 1,414,792 Medicare beneficiaries residing in 10,664 assisted living communities with twenty-five or more beds at any point during the study period. We also identified a subsample of residents with a diagnosis of dementia, using the Chronic Conditions Warehouse flag reported in the Master Beneficiary Summary File during this period (n = 634,464).
Analyses
We first described changes over time (2007–18) in the staffing regulatory specificity scores at the assisted living community and resident levels. To evaluate the association between changes in staffing regulations and residents’ hospitalizations, we estimated a linear probability model controlling for resident characteristics, assisted living fixed effects, and year fixed effects. We estimated five separate models. Model 1 included the individual specificity scores for each type of staff. Models 2–5 included each specificity score separately. Statistical analyses were conducted using STATA, version 16.0, and SAS, version 9.4. Additional details about the construction of the cohorts, variables, and statistical analyses are provided in the appendix.23
Limitations
Our methodology to identify Medicare beneficiaries residing in assisted living communities relied on postal delivery routes (nine-digit ZIP codes), which introduced some limitations to our study. First, we only included assisted living communities that have twenty-five or more beds because smaller settings are likely to include non-assisted-living addresses in the same ZIP code. Our sample may have included people residing in independent living on the same campus that shared a ZIP code with an assisted living setting, thereby potentially attenuating the effect of changing regulations.
Another important limitation was that we excluded residents enrolled in a Medicare Advantage plan. Given the increase in Medicare Advantage enrollment24 and the care coordination that is a hallmark of the Medicare Advantage program,25 additional research is needed to understand whether Medicare Advantage beneficiaries’ outcomes are similarly shaped by state regulations. We also did not examine nurse practice laws, which vary by state and may influence care practices,8,26 or other policies that may interact with the influence of changing staffing levels (for example, admission policies that affect the case mix of assisted living residents). Year fixed effects control for national changes in rates of hospitalization, but state-specific changes in policy or medical care associated with hospitalization might bias our estimates.
Also, this study did not examine enforcement or the other factors that—according to neo-institutional theory—influence providers’ behaviors.21 Finally, given data availability, we could not observe the actual staffing levels or more proximal health outcomes that have been linked to changes in nursing home staffing (for example, pressure sores).12 However, our logic model posited that increased regulatory staffing specificity leads to more personnel, which in turn reduces the rates of complications that necessitate hospitalization.
Study Results
Changes In The Specificity Of Staffing Regulations
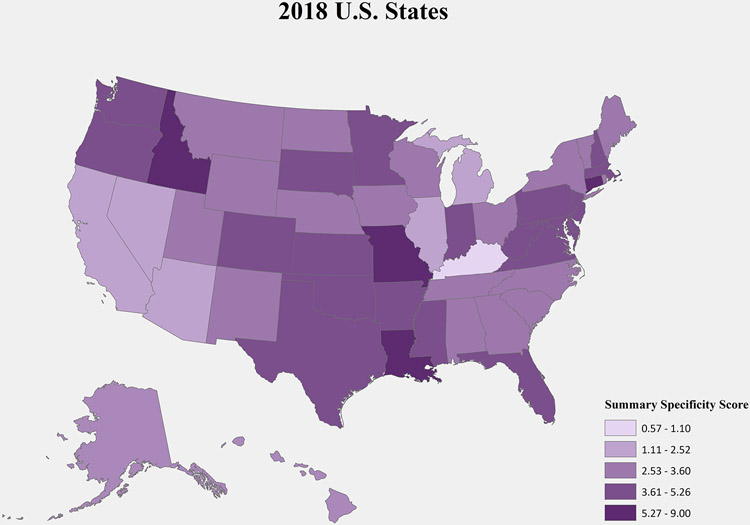
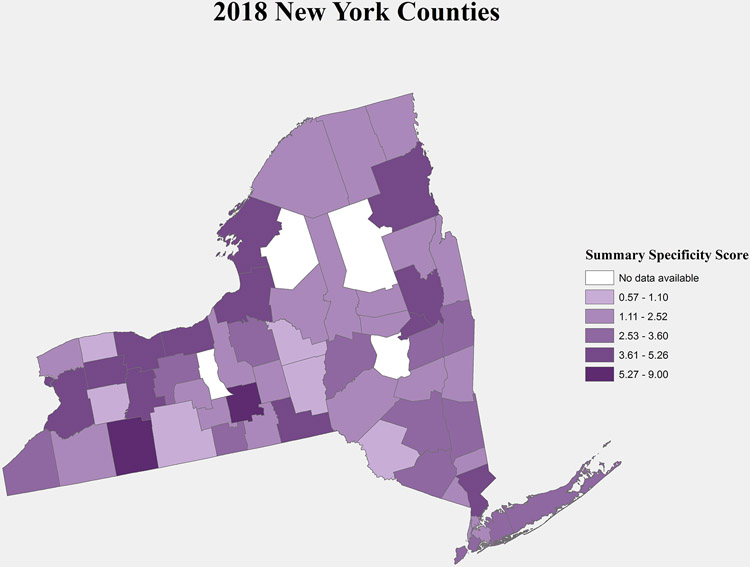
The 2018 mean summary staffing specificity score for each state is displayed in exhibit 1. Thirteen states had increases in their assisted living mean summary staffing specificity score between 2007 and 2018, as shown in appendix exhibit 3.23 As we see in the New York example in exhibit 2 and appendix exhibit 3, changes in regulations could increase the specificity within a state in some areas more than others, depending on the geographic distribution of assisted living license types within the state.23 In appendix exhibit 4, we present the distribution of our sample, by staffing specificity score, in 2007 and 2018.23
Exhibit 1.
Map of mean summary specificity score, US states, 2018
Source/Notes: SOURCE Authors’ analysis of regulations pertaining to staffing in assisted living and states’ assisted living licensure information in 2018. NOTES Mean specificity score among assisted living communities operating in 2018 (n = 8,620).
Exhibit 2.
Map of mean summary specificity score, New York counties, 2018
Source/Note: SOURCE Authors’ analysis of regulations pertaining to staffing in assisted living and states’ assisted living licensure information in 2018. NOTE Mean specificity score among assisted living communities operating in New York in 2018.
During the study period, the average total staffing specificity score increased slightly (going from 3.48 in 2007 to 3.67 in 2018; see appendix exhibit 1).23 That overall difference was a result of regulatory changes that affected 1,328 (12.5 percent) assisted living communities in thirteen states and 145,643 residents (10.3 percent) in our sample of Medicare beneficiaries residing in these settings (data not shown). Among the staffing types, the mean registered nurse staffing specificity score had the greatest absolute increase, going from 0.83 (standard deviation = 0.8) to 0.96 (SD = 0.9), with the percentage of assisted living settings without registered nurse staffing requirements decreasing from 39.5 percent in 2007 to 33.8 percent in 2018—a 14 percent relative decrease from 2007. Licensed practical nurse mean staffing specificity score increased from 0.45 (SD = 0.7) in 2007 to 0.49 (SD = 0.8) in 2018, with nineteen states in 2018 having some regulatory language about licensed practical nurse staffing requirements, up from fifteen states in 2007. The mean direct care worker staffing score increased slightly from 2.20 (SD = 0.6) to 2.23 (SD = 0.5), with 450 (4.22 percent) assisted living communities in six states having to comply with increased regulatory specificity in direct care worker staffing requirements.
Sample Characteristics
Exhibit 3 displays the characteristics of our sample of Medicare beneficiaries residing in assisted living. We observed significant increases in the percentage of residents who were non-White or Hispanic and an increase in residents dually enrolled in Medicare and Medicaid over time. In addition, there were increases in the percentage of residents who had any of twelve of the thirteen chronic conditions (dementia diagnoses decreased), as well as increases in the number of comorbid chronic conditions. However, the changes in the rates of hospitalization during the study period varied for the two samples: the mean monthly risk of hospital admission decreased by 0.006, going from 0.046 per resident in 2007 to 0.040 per resident in 2018, whereas it increased among residents with dementia (0.051 in 2007 versus 0.057 in 2018).
Exhibit 3:
Characteristics of a national sample of Medicare beneficiaries residing in assisted living communities with twenty-five or more beds (2007 and 2018)
| 2007 | 2018 | |||
|---|---|---|---|---|
| Total sample of assisted living residents (n = 329,092) |
Assisted living residents with a dementia diagnosis (n = 169,835) |
Total sample of assisted living residents (n = 340,532) |
Assisted living residents with a dementia diagnosis (n = 145,594) |
|
| Age group (years), % | ||||
| <65 | 7.2 | 4.2 | 8.0 | 5.1 |
| 65–74 | 10.8 | 7.5 | 16.6 | 10.8 |
| 75–84 | 31.1 | 31.8 | 25.2 | 24.0 |
| 85+ | 50.9 | 56.5 | 50.2 | 60.0 |
| Sex, % | ||||
| Male | 30.9 | 28.0 | 34.8 | 32.1 |
| Female | 69.1 | 72.0 | 65.2 | 67.9 |
| Race, % | ||||
| White | 93.1 | 93.3 | 90.1 | 89.7 |
| Black | 3.3 | 3.4 | 4.7 | 5.4 |
| Hispanic | 1.8 | 1.9 | 2.4 | 2.8 |
| Other | 1.9 | 1.5 | 2.8 | 2.2 |
| Dually enrolled in Medicare and Medicaid, % | 19.8 | 21.3 | 24.1 | 30.4 |
| Chronic conditions, % | ||||
| Anemia | 66.9 | 73.1 | 74.5 | 86.7 |
| Atrial fibrillation | 23.6 | 24.8 | 27.0 | 32.0 |
| Cancer | 18.9 | 19.2 | 20.6 | 22.1 |
| Chronic kidney disease | 22.2 | 23.5 | 48.1 | 58.4 |
| Chronic obstructive pulmonary disease | 33.4 | 35.4 | 37.0 | 45.4 |
| Depression | 43.9 | 53.5 | 55.9 | 72.4 |
| Diabetes | 31.9 | 33.4 | 41.8 | 48.9 |
| Heart failure | 43.7 | 47.4 | 43.0 | 54.8 |
| Hyperlipidemia | 67.9 | 69.7 | 84.4 | 90.2 |
| Hypertension | 85.2 | 89.0 | 87.7 | 95.2 |
| Ischemic heart disease | 59.2 | 63.7 | 60.9 | 72.2 |
| Stroke | 25.8 | 31.9 | 27.5 | 38.0 |
| <2 chronic conditionsa | 8.0 | 4.2 | 6.9 | 1.1 |
| 2–3 chronic conditionsa | 18.2 | 15.7 | 11.8 | 5.9 |
| 4–5 chronic conditionsa | 27.3 | 27.5 | 20.7 | 16.7 |
| 6+ chronic conditionsa | 46.5 | 52.6 | 60.6 | 76.3 |
| Monthly hospital admission rate, mean (SD) | 0.046 (0.210) | 0.051 (0.221) | 0.040 (0.195) | 0.057 (0.231) |
SOURCE Authors’ analysis of the Medicare Master Beneficiary Summary File and Medicare Provider Analysis and Review data for a cohort of Medicare beneficiaries residing in nine-digit ZIP code corresponding to an assisted living with twenty-five or more beds in 2007 and 2018. NOTES Denominator is the number of assisted living residents who contributed at least one month of data to the study in each year. SD is standard deviation.
Condition counts were created from the conditions listed.
Association Between Increases In Specificity Of Staffing Regulations And Resident Hospitalization
In exhibit 4, we report the effect of a one-unit increase in regulatory specificity, adjusting for resident characteristics and year and license-type fixed effects. We estimated that a one-unit increase in the specificity of regulations for direct care workers was associated with a 0.00179 decrease in a resident’s probability of hospital admission in a month (p = 0.006), representing a 4 percent relative decrease from the 2007 average of 0.046 hospitalizations per month (see Exhibit 3). An increase in specificity regarding licensed practical nurses was associated with an increase in per month hospital admission of 0.00115 (p = 0.043), which is a 2.5 percent relative increase from the 2007 average. Among residents with a dementia diagnosis, increases in specificity for direct care workers and licensed practical nurses were associated with a −0.00238 decrease (p < 0.001) and 0.00195 increase (p = 0.018) in risk for hospital admission, representing a 6 percent relative decrease and 5 percent relative increase from the 2007 average, respectively. We did not find a statistically significant effect of changes in registered nurse regulation or of changes in the overall summary score, either in the full sample or among residents with dementia.
Exhibit 4:
Results from linear probability models examining relationships among staffing specificity scores and hospitalization of assisted living residents
| Summary specificity score |
DCW specificity score |
LPN specificity score |
RN specificity score |
|
|---|---|---|---|---|
| Full sample of beneficiaries residing in assisted living | ||||
| Model 1 (main model) | —a | −0.0018*** | 0.0011** | 0 |
| Models using individual specificity score | ||||
| Model 2 | −0.0001 | —a | —a | —a |
| Model 3 | —a | −0.0017*** | —a | —a |
| Model 4 | —a | —a | 0.001* | —a |
| Model 5 | —a | —a | —a | 0 |
| Subsample of beneficiaries with a dementia diagnosis residing in assisted living | ||||
| Model 1 (main model) | —a | −0.0024*** | 0.002** | 0.0001 |
| Models using individual specificity score | ||||
| Model 2 | 0 | —a | —a | —a |
| Model 3 | —a | −0.0023*** | —a | —a |
| Model 4 | —a | —a | 0.0019** | —a |
| Model 5 | —a | —a | —a | 0.0003 |
SOURCE Authors’ analysis of regulations pertaining to staffing in assisted living, states’ assisted living licensure information, the Medicare Master Beneficiary Summary File, and Medicare Provider Analysis and Review data for a cohort of Medicare beneficiaries residing in a nine-digit ZIP code corresponding to an assisted living with twenty-five or more beds in 2007 and 2018. NOTES Data include Medicare beneficiaries residing in assisted living settings with twenty-five or more beds who contributed one or more months of data between 2007 and 2018. Total sample is 38,586,949 person-months among 1,414,792 people residing in 10,664 assisted living communities. Each reported effect represents the coefficient on staffing specificity score in a separate model that includes individual-level health and demographic covariates (see exhibit 3), year fixed effects, and assisted living community fixed effects. Robust standard errors (not shown) are estimated with clustering at the assisted living community level. DCW is direct care worker. LPN is licensed practical nurse. RN is registered nurse.
The model did not include the indicated specificity score.
p < 0.1
p < 0.05
p < 0.01
Discussion
This is the first study to examine the changes in assisted living staffing regulations over time, as well as the relationship between staffing regulations and resident outcomes. Controlling for the health and demographic characteristics of residents, we found that increases in the specificity of regulations for direct care workers were associated with decreases in the monthly risk for hospital admission for assisted living residents, whereas more specific regulations for licensed practical nurse staffing were associated with increased risk for hospitalization.
In overall magnitude, the results have striking implications for policy, practice, and research in assisted living. The 4 percent relative decrease in monthly hospital admission risk that was associated with an increase in the specificity of direct care worker staffing regulation amounted to 30 percent of the total change in mean hospitalization risk from 2007 to 2018 (see exhibit 3). Among residents with dementia, increased staffing specificity was also associated with decreases in hospitalization, even in the presence of secular increases in hospitalizations among residents with dementia. Importantly, these reductions occurred in the context of a general decreasing trend in hospitalizations among Medicare beneficiaries (17 percent decrease between 2010 and 2016) attributable to the Medicare Recovery Audit Contractor Program and the Hospital Readmissions Reduction Program, implemented in 2010 and 2012, respectively.27 Given that implementation of these two sweeping legislative actions to reduce hospitalization occurred during our study period, the finding that increases in direct care worker regulatory specificity is associated with further reductions in rates of hospitalization among our sample of assisted living residents, including those living with dementia, is noteworthy.
Direct care workers perform essential activities for assisted living residents, such as assistance with activities of daily living.28 Assisted living residents have high levels of functional need (for example, 57 percent need assistance with walking or locomotion).1 Given the time necessary to provide adequate activities of daily living care to assisted living residents, particularly those living with dementia,28 more specific regulations as they relate to minimum staff, and therefore potential increases in direct care worker staffing in assisted living, could prevent resident falls, functional decline, and exacerbation of other conditions that lead to hospitalization.29
We found that increasing specificity for licensed practical nurse staffing is associated with increases in assisted living resident hospitalization, including for the subgroup with dementia. This somewhat counterintuitive finding has been witnessed in the nursing home literature as well.30,31 Our finding may reflect a substitution of staff, where requirements for more expensive licensed practical nurse labor reduces staffing in other areas. An alternative explanation is that more specific staffing requirements, particularly for staff members with higher wages, that are not accompanied by subsidies to fund those increases may result in cost-cutting measures in other areas that adversely affect the quality of care that residents receive. This behavior is especially likely if prices are fixed or assisted living operators’ ability to negotiate higher per diem rates is limited, particularly for contracts with Medicaid managed care organizations.32
Florida, a state that greatly increased staffing requirements in nursing homes, financially supported those increases with higher Medicaid payment rates. The resulting increase in nursing staff was credited with raising the quality of nursing home care in that state.14 Despite increases in Medicaid waivers and state plans that cover services in assisted living,33,34 the majority of care provided in assisted living, nationally, is not state subsidized. Thus, there are few mechanisms to increase financial support to help assisted living communities meet increased staffing requirements (that is, unfunded mandates), potentially leaving providers to cut costs at the margins or pass on the additional costs to residents.
In addition, our findings may reflect a “dampening effect” in which increased regulatory specificity raises the staffing levels among facilities with the lowest staffing levels, but may cause other providers to “staff down” if they view minimum staffing requirements as the “maximum” staff needed.35 Therefore, careful consideration must be given to the unintended consequences of increased specificity in assisted living staffing regulations, particularly for higher-paid staff members.
It could also be the case that increased licensed practical nurse presence in assisted living heightened the recognition of signs and symptoms of declining health that could result in hospitalization. Licensed practical nurses may not have the training or scope of practice needed to care for sick residents safely in the assisted living environment, requiring sufficient backup by registered nurses to prevent hospitalization.30,36 Increases in regulatory specificity pertaining to licensed practical nurse staffing may also reflect policy makers’ responses to consumer preferences and changes in the resident composition within these settings. Although we did attempt to account for the observed increase in acuity during this period by adjusting for residents’ chronic conditions and secular time trends, there may be other important factors (for example, functional impairment, frailty) that we are unable to measure. Future work is needed to better understand the impetus for changes in staffing requirements and how they may relate to hospitalization of assisted living residents.
According to neo-institutional theory, greater specificity in regulations may influence providers through multiple mechanisms (for example, mandatory legal compliance, shifts in expectations/norms) to increase staffing, thereby reducing hospitalization rates. Because we could not directly observe staffing levels or the multiple mechanisms that could have influenced providers’ responses (for example, enforcement), additional research is needed to confirm the relationship between regulatory specificity and actual staffing levels.
Conclusion
Our study is among the first to examine the influence of changing staffing regulations on assisted living residents’ outcomes. The data, analytic approach, and framework underpinning this study provide a foundation for future analyses to understand what internal and external forces influence staffing decisions in assisted living to ensure safe, person-centered, and high-quality care. Given the increase in the population and vulnerability of assisted living residents, additional research is needed to guide states as they seek the most effective ways to ensure optimal outcomes for older adults and people with disabilities in these settings.
Supplementary Material
Acknowledgment
This research was presented at the 2021 AcademyHealth Virtual Annual Research Meeting. This research was supported by a grant to Kali Thomas from the National Institute on Aging (Grant No. R01AG057746). The authors acknowledge Joan Brazier, MS, for her excellent project management and Jaclyn Winfree, MA, for her contributions sourcing the policy information. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the National Institutes of Health, the Department of Veterans Affairs, or the United States government.
Biographies
Kali S. Thomas (kali_thomas@brown.edu) is an associate professor in the Department of Health Services, Policy and Practice in the Brown University School of Public Health, and a research health scientist in the Center of Innovation in Long-Term Services and Supports at the Providence Veterans Affairs (VA) Medical Center, all in Providence, Rhode Island.
Portia Y. Cornell is a health science specialist in the Center of Innovation for Long-Term Services and Supports, Providence VA Medical Center, and an investigator in the Center for Gerontology and Healthcare Research, Brown University School of Public Health.
Wenhan Zhang is an analyst in the Center for Gerontology and Health Care Research, Brown University School of Public Health.
Lindsey Smith is a PhD student in the Institute on Aging, Portland State University, in Portland, Oregon.
Cassandra Hua is an investigator in the Center for Gerontology and Healthcare Research, Brown University School of Public Health.
Brian Kaskie is an associate professor in the Department of Health Management and Policy, Iowa State University, in Iowa City, Iowa.
Paula Carder is a professor in the Institute on Aging, Portland State University.
Contributor Information
Kali S. Thomas, School of Public Health, Brown University, Center of Innovation in Long-Term Services and Supports, Providence VA Medical Center.
Portia Cornell, School of Public Health, Brown University, Center of Innovation in Long-Term Services and Supports, Providence VA Medical Center.
Wenhan Zhang, School of Public Health, Brown University.
Lindsey Smith, Oregon Health & Science University - Portland State University School of Public Health, Portland State University Institute on Aging, Portland, OR, USA.
Cassandra L. Hua, School of Public Health, Brown University.
Brian Kasie, University of Iowa College of Public Health.
Paula Carder, Oregon Health & Science University - Portland State University School of Public Health, Portland State University Institute on Aging, Portland, OR, USA.
Notes
- 1.Harris-Kojetin L, Sengupta M, Lendon JP, Rome V, Valverde R, Caffrey C. Long-term care providers and services users in the United States, 2015–2016 [Internet]. Hyattsville (MD): National Center for Health Statistics, Vital Health Statistics; 2019. Feb; [cited 2021 Jul 13]. Available from: https://www.cdc.gov/nchs/data/series/sr_03/sr03_43-508.pdf [PubMed] [Google Scholar]
- 2.Carder PC. State regulatory approaches for dementia care in residential care and assisted living. Gerontologist. 2017;57(4):776–86 [DOI] [PubMed] [Google Scholar]
- 3.Trinkoff AM, Yoon JM, Storr CL, Lerner NB, Yang BK, Han K. Comparing residential long-term care regulations between nursing homes and assisted living facilities. Nurs Outlook. 2020;68(1):114–22 [DOI] [PubMed] [Google Scholar]
- 4.Smith L, Carder P, Bucy T, Winfree J, Brazier JF, Kaskie B, et al. Connecting policy to licensed assisted living communities, introducing health services regulatory analysis. Health Serv Res. 2021;56(3):540–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Temkin-Greener H, Mao Y, Ladwig S, Cai X, Zimmerman S, Li Y. Variability and potential determinants of assisted living state regulatory stringency. J Am Med Dir Assoc. 2020. Nov 13. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beeber AS, Zimmerman S, Reed D, Mitchell CM, Sloane PD, Harris-Wallace B, et al. Licensed nurse staffing and health service availability in residential care and assisted living. J Am Geriatr Soc. 2014;62(5):805–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stearns SC, Park J, Zimmerman S, Gruber-Baldini AL, Konrad TR, Sloane PD. Determinants and effects of nurse staffing intensity and skill mix in residential care/assisted living settings. Gerontologist. 2007;47(5):662–71 [DOI] [PubMed] [Google Scholar]
- 8.Beeber AS, Zimmerman S, Madeline Mitchell C, Reed D. Staffing and service availability in assisted living: the importance of nurse delegation policies. J Am Geriatr Soc. 2018;66(11):2158–66 [DOI] [PubMed] [Google Scholar]
- 9.Rome V, Harris-Kojetin L, Carder P. Variation in licensed nurse staffing characteristics by state requirements in residential care. Res Gerontol Nurs. 2019;12(1):27–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zimmerman S, Sloane PD, Reed D. Dementia prevalence and care in assisted living. Health Aff (Millwood). 2014;33(4):658–66 [DOI] [PubMed] [Google Scholar]
- 11.Tilly J, Reed P, editors. Dementia care practice recommendations for assisted living residences and nursing homes [Internet]. Chicago (IL): Alzheimer’s Association, Campaign for Quality Residential Care; 2006. Sep [cited 2021 Jul 13]. Available from: https://www.alz.org/media/documents/dementia-care-practice-recommend-assist-living-1-2-b.pdf [Google Scholar]
- 12.Dellefield ME, Castle NG, McGilton KS, Spilsbury K. The relationship between registered nurses and nursing home quality: an integrative review (2008–2014). Nurs Econ. 2015;33(2):95–108 [PubMed] [Google Scholar]
- 13.Thomas KS, Rahman M, Mor V, Intrator O. Influence of hospital and nursing home quality on hospital readmissions. Am J Manag Care. 2014;20(11):e523–31 [PMC free article] [PubMed] [Google Scholar]
- 14.Hyer K, Thomas KS, Branch LG, Harman JS, Johnson CE, Weech-Maldonado R. The influence of nurse staffing levels on quality of care in nursing homes. Gerontologist. 2011;51(5):610–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin H. Revisiting the relationship between nurse staffing and quality of care in nursing homes: an instrumental variables approach. J Health Econ. 2014;37:13–24 [DOI] [PubMed] [Google Scholar]
- 16.Zimmerman S, Sloane PD, Eckert JK, Gruber-Baldini AL, Morgan LA, Hebel JR, et al. How good is assisted living? Findings and implications from an outcomes study. J Gerontol B Psychol Sci Soc Sci. 2005;60(4):S195–204 [DOI] [PubMed] [Google Scholar]
- 17.Caffrey C, Harris-Kojetin L, Rome V, Schwartz L. Relationships between residential care community characteristics and overnight hospital stays and readmissions: results from the National Study of Long-Term Care Providers. Seniors Hous Care J. 2018;26(1):38–49 [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas KS, Dosa D, Gozalo PL, Grabowski DC, Nazareno J, Makineni R, et al. A methodology to identify a cohort of medicare beneficiaries residing in large assisted living facilities using administrative data. Med Care. 2018;56(2):e10–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomas KS, Zhang W, Cornell PY, Smith L, Kaskie B, Carder PC. State variability in the prevalence and healthcare utilization of assisted living residents with dementia. J Am Geriatr Soc. 2020;68(7):1504–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chapter 58A–5, assisted living facilities. Florida Administrative Code, 2018. [Google Scholar]
- 21.Powell WW, Di Maggio PJ, editors. The new institutionalism in organizational analysis. Chicago (IL): Chicago University Press; 1991 [Google Scholar]
- 22.Aragòn-Correa JA, Marcus AA, Vogel D. The effects of mandatory and voluntary regulatory pressures on firms' environmental strategies: a review and recommendations for future research. Acad Management Ann. 2020;14(1):339–65. [Google Scholar]
- 23.To access the appendix, click on the Details tab of the article online.
- 24.Freed M, Damico A, Neuman T. A dozen facts about Medicare Advantage in 2020 [Internet]. San Francisco (CA): Henry J. Kaiser Family Foundation; 2021. Jan 13 [cited 2021 Jul 13]. Available from: https://www.kff.org/medicare/issue-brief/a-dozen-facts-about-medicare-advantage-in-2020/ [Google Scholar]
- 25.Broussard BD, Shrank WH. Medicare Advantage and the future of value-based care. Health Affairs Blog [blog on the Internet]. 2019. Jul 3 [cited 2021 Jul 13]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20190627.482360/full/ [Google Scholar]
- 26.Mitty E, Resnick B, Allen J, Bakerjian D, Hertz J, Gardner W, et al. Nursing delegation and medication administration in assisted living. Nurs Adm Q. 2010;34(2):162–71 [DOI] [PubMed] [Google Scholar]
- 27.Medicare Payment Advisory Commission. Chapter 1: Mandated report: the effects of the Hospital Readmissions Reduction Program [Internet]. Washington (DC): MedPAC; 2018. Jun [last updated 2019 Nov 27; cited 2021 Jul 13]. Available from: http://www.medpac.gov/docs/default-source/reports/jun18_ch1_medpacreport_rev_nov2019_v2_note_sec.pdf?sfvrsn=0 [Google Scholar]
- 28.Simmons SF, Coelho CS, Sandler A, Shah AS, Schnelle JF. Managing person-centered dementia care in an assisted living facility: staffing and time considerations. Gerontologist. 2018;58(4):e251–9 [DOI] [PubMed] [Google Scholar]
- 29.Leland NE, Gozalo P, Teno J, Mor V. Falls in newly admitted nursing home residents: a national study. J Am Geriatr Soc. 2012;60(5):939–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mukamel DB, Weimer DL, Harrington C, Spector WD, Ladd H, Li Y. The effect of state regulatory stringency on nursing home quality. Health Serv Res. 2012;47(5):1791–813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang BK, Carter MW, Trinkoff AM, Nelson HW. Nurse staffing and skill mix patterns in relation to resident care outcomes in US nursing homes. J Am Med Dir Assoc. 2021;22(5):1081–7. [DOI] [PubMed] [Google Scholar]
- 32.Sudo C. Medicaid could help unlock middle-market senior living—but policies, MCOs may not favor providers. Senior Housing News [serial on the Internet]. 2021. Mar 10 [cited 2021 Jul 13]. Available from: https://seniorhousingnews.com/2021/03/10/medicaid-could-help-unlock-middle-market-senior-living-but-policies-mcos-may-not-favor-providers/ [Google Scholar]
- 33.Government Accountability Office. Medicaid assisted living services: improved federal oversight of beneficiary health and welfare is needed [Internet]. Washington (DC): 2018. Jan [cited 2021 Jul 13]. Available from: https://www.gao.gov/assets/gao-18-179.pdf [Google Scholar]
- 34.Fabius CD, Cornell PY, Zhang W, Thomas KS. State Medicaid financing and access to large assisted living settings for Medicare-Medicaid dual-eligibles. Med Care Res Rev. 2021. Jan 19. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mueller C, Arling G, Kane R, Bershadsky J, Holland D, Joy A. Nursing home staffing standards: their relationship to nurse staffing levels. Gerontologist. 2006;46(1):74–80 [DOI] [PubMed] [Google Scholar]
- 36.Corazzini KN, Anderson RA, Mueller C, Thorpe JM, McConnell ES. Licensed practical nurse scope of practice and quality of nursing home care. Nurs Res. 2013;62(5):315–24 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.