Abstract
Caregivers of older adults with cognitive impairment experience significant caregiver burden, stress, anxiety, and depression. Mindfulness Therapy, a non-pharmacological behavioral intervention, may support caregiver mental health given its preliminary evidence base for the management of stress and anxiety among caregivers. We examined the feasibility, acceptability, and preliminary efficacy of Mindfulness Coach, an mHealth Mindfulness Therapy intervention. We recruited 58 informal caregivers of older adults with cognitive impairment for this pilot feasibility trial. Participants completed measures of caregiver burden, stress, anxiety, and depression at baseline, 2 weeks, 4 weeks, and 8 weeks as well as acceptability and usability data at 8-weeks. The mobile app collected in-app use data including minutes spent using the app and number of unique visits to the app. Users found the app acceptable to use and were satisfied with its design and usability. Over the course of the study period, depression, anxiety, caregiver burden and perceived stress improved. These outcome variables also improved more as caregivers spent more time using the Mindfulness Therapy mHealth intervention. Our results suggest that mHealth mindfulness therapy with caregivers of older adults with cognitive impairment is both feasible and acceptable to users, and that it successfully reduces psychological symptoms. Future work should focus on determining the appropriate doses of the mHealth therapy for particular outcomes and strategies to integrate it into routine care. Mindfulness Therapy delivered in an mHealth format may increase access to psychological treatment for caregivers.
Keywords: caregiving, mHealth interventions, mindfulness therapy, dementia caregiving
Introduction
Nearly 8 million older adults in the United States rely on informal caregivers (neighbours, friends) for assistance with health needs,(Spillman et al., 2014) and informal caregivers provide 75–80% of total care hours to community-dwelling older adults (Freedman & Spillman, 2014). Decades of research have documented the profound, negative effects of caregiving on unpaid caregivers (Pinquart & Sörensen, 2003; “Predicting Caregiver Burden and Depression in Alzheimer’s disease,” 2000; Vilchinsky et al., 2015). For example, compared to non-caregivers, caregivers are more likely to suffer from high levels of stress (Capistrant, 2016; National Academies of Sciences Engingeering and Medicine, 2012) and anxiety (Berglund et al., 2015; Vilchinsky et al., 2015).
Informal caregivers of older adults with cognitive impairment are especially at risk for adverse outcomes and face additional challenges (Alzheimer’s Association., 2019; Alzheimer’s Association, 2016). For example, caregivers of older adults with cognitive impairment provide more care hours compared to caregivers of individuals with other illnesses (Riffin et al., 2017) and endure additional stressors, such as making proxy health care decisions, acting as the patient’s advocate, and managing the older adult’s safety (National Alliance for Caregiving and the Alzheimer’s Association, 2017). As a result, additional methods of psychological support are needed to ensure the wellbeing of this unique group of caregivers (Gitlin et al., 2003; Vaingankar et al., 2016).
Mindfulness Therapy (MT) is a behavioral intervention with preliminary evidence for managing stress and anxiety in caregivers of older adults with cognitive impairment (Corporation et al., 2014; Epstein-Lubow et al., 2011; Paller et al., n.d.). MT utilizes psychoeducation, guided meditation, and other targeted mindfulness exercises to help individuals cultivate non-judgmental awareness of present moment experiences. While the evidence base for MT in caregiving is growing, elements of traditional MT (8+ hours of face-to-face treatment with trained providers (Hofmann et al., 2010) create barriers for caregivers, given the limited availability of providers trained in MT, uneven and arbitrary provider reimbursement, and caregiver time constraints (Kozlov et al., 2017). Therefore, an innovative delivery model for MT is required to meet the unique needs of caregivers of older adults with cognitive impairment.
MHealth strategies can be effective to deliver behavioral interventions, as they overcome barriers of traditional psychotherapy such as provider availability, scheduling conflicts, and cost (Price et al., 2014). Multiple studies have demonstrated that mHealth interventions are feasible and efficacious in treating adults and older adults with depression or anxiety (Crabb et al., 2012; Firth et al., 2017; Jones et al., 2015; Olthuis Janine et al., 2016; Tara et al., 2013). There is also preliminary evidence that MT, specifically, can be feasibly and effectively delivered using mHealth. For example, Chittaro and Vianello, (2014), found that a mindfulness-based mobile application effectively taught naïve meditators how to utilize a mindfulness technique to reduce their distress. Another study found that depression scores were significantly decreased after the use of a smartphone delivered mindfulness-based content in a sample of middle-aged females (Howells et al., 2016). Mani and colleagues (2015) found that mindfulness app interventions has the potential to complement and support face-to-face interventions, but future work should focus on determining app efficacy. Despite this preliiminary evidence, no studies have evaluated if mHealth MT is feasible, acceptable, and effective among informal caregivers of older adults with cognitive impairment. Because these caregivers face unique challenges, it is unknown if mHealth-delivered MT will be acceptable, feasible, and preliminarily effective in this population.
In response to a call to increase research for smartphone-based interventions for caregivers of individuals with cognitive impairment (Brown et al., 2019), the purpose of this pilot study was to determine the feasibility, acceptability, and preliminary efficacy of Mindfulness Coach, an mHealth-delivered MT developed by the Veterans Affairs National Center for PTSD Research. We hypothesized that Mindfulness Coach, combined with a caregiver-specific orientation to the mobile app, would be feasible and acceptable (defined as 70% of caregivers would rate the app as acceptable on the ease of use and satisfaction scale, and 70% of caregivers would use the app at least one additional time outside of the orientation session) to caregivers of older adults with cognitive impairment. We also hypothesized that Mindfulness Coach would be preliminarily effective at reducing symptoms of anxiety, depression, stress, and caregiver burden.
Method
Study Design
This pilot feasibility study employed a single-group, repeated measures design with assessments at baseline, 2-, 4- and 8-week intervals. The protocol was approved by the Rutgers University Internal Review Board.
Recruitment and Participants
Recruitment occurred between November 2019 and December 2020. Participants were recruited from three geriatric primary care settings via physician referral and warm hand-off to a research assistant stationed in the waiting room between November 2019 and March 14th, 2020. In March 2020, the COVID-19 pandemic necessitated a change in recruitment strategy, as in-person recruitment was no longer feasible. As a result, participants were recruited remotely via community agencies, physician telehealth visit referrals, and online caregiver support communities.
Participants were family caregivers for an older adult with cognitive impairment. Eligibility criteria included age over 21; English-speaking; ownership of a smartphone or tablet; self-identification as a person who provides care to an older adult with a diagnosis of mild cognitive impairment or dementia because of a personal connection, not for financial compensation. Written or virtual informed consent was collected from all participants.
Intervention
Mindfulness Coach is an iOS- and Android-based app designed to deliver 14 sequential levels, a practice now area with evidence-based mindfulness audio exercises, assessments using the Five Factor Mindfulness Questionnaire Short Form, and education about mindfulness. To progress to the next level, users must interact with every element. The training plan levels include psychoeducation and exercises (guided meditations and seated practices), which increase in duration as users progress. The mindfulness training course is centered on Veterans Affairs (VA) protocols. To use the research version, participants enter an invitation code. The app then transmits de-identified usage data to a secure GovCloud server hosted on AWS and approved under the VA’s Technical Reference Model. The research app captures key information including number of visits to the app and amount of time spent per visit. Mindfulness Coach is HIPAA compliant, does not collect data for third parties, and does not have in-app purchases or advertisements, thus making it distinct from other mindfulness apps on the market.
The app was developed by the VA’s National Center for PTSD to support a broad range of psychological needs across patient populations. To address this lack of specificity, we developed and included an orientation to the app that was specific to caregivers of older adults with dementia and focused on anxiety, stress, and coping with caregiving. The orientation session was based on protocols developed by the Center for Research and Education on Aging and Technology Enhancement (CREATE) (Czaja et al., 2015, 2018). The orientation consisted of the following components: (1) education about the app, its developers, MT, and how MT can be helpful to caregivers (to establish credibility and buy-in); (2) discussion of goals of the app; (3) procedural information about how to launch and navigate the app; and (4) assessment of participant’s ability to use the app. Participants were required to be able to open, launch, navigate, and use the app independently to complete the orientation. During orientation, study personnel also asked whether participants would be willing to set a daily mindfulness practice goal. If the participant was amenable, study personnel helped participants set reminders (i.e., push notifications) within Mindfulness Coach to facilitate daily practice. Participants were encouraged to set mindfulness practice goals (e.g., daily practice, weekly practice, etc.) tailored to their unique needs. Participants were also given a laminated instructional card explaining how to access and use Mindfulness Coach. Between November 2019 and March 2020, this orientation was administered in-person. Between April 2020 and December 2020, the orientation was delivered via telephone to enrolled participants.
The orientation and study assessments were conducted by a Master’s level research assistant who had been trained by the PI. A checklist was developed to ensure uniformity of protocol and procedures. Training consisted of several role plays to ensure fidelity in administering the orientation. The PI also observed the research assistant during the first session with a participant and regularly conducted quality control checks on the data as it was collected. The study RA scheduled a 1-week booster phone call with participants to troubleshoot potential issues with app use. At this session, participants were asked if they had used the app in their first week. If they had not, the RA provided additional troubleshooting and encouragement. Interviews were conducted at baseline, 2-weeks, 4-weeks, and 8-weeks. Baselines were conducted in person between November 2019 and March 2020 and were switched to phone-based interviews between April 2020 and December 2020. All 2-, 4-, and 8-week follow up interviews were conducted via telephone.
Measures
Anxiety and depression were measured with the Hospital Anxiety and Depression Scale anxiety subscale (HADS-A) and depression subscale (HADS-D). Each subscale has 7 items rated on a scale from 0 to 3. Sub-scale total scores range from 0–21, with higher values indicating more severe anxiety or depression symptomatology (Bjelland et al., 2002; Mykletun et al., 2001; Zigmond & Snaith, 1983). The HADS-A and HADS-D have validity and internal consistency to measure anxiety and depression symptom severity caregivers of individuals with serious illness (Gough & Hudson, 2009) and older adults (Bjelland et al., 2002).
Stress was measured with the Perceived Stress Scale (Cohen et al., 1983), a 10-item self-report inventory with validity and reliability to measure an individual’s perceived level of stress. Participants rate each item on a scale of 0 (never) to 5 (very often). Scores range from 0–40, with higher scores indicating worse perceived stress. The PSS has acceptable internal consistency among caregivers of persons with dementia and convergent validity with inventories measuring similar constructs (Deeken et al., 2018; Lee, 2012).
Caregiver burden was assessed with the Bakas Caregiving Outcomes Scale (Bakas et al., 2006a), a 15-item measure that examines caregivers’ beliefs about how caregiving responsibilities have affected their lives. Participants rate each item on 7-point response scale; thus, scores range from 15–105, with lower scores indicating that more negative life changes because of caregiving. This scale has been p validated with caregivers of adults with memory impairment (Bakas et al., 2006a). The Bakas Caregiving Outcomes Scale has strong internal consistency in family caregivers of patients with stroke and heart failure (Bakas et al., 2006b).
Satisfaction with the app was measured by a modified ease-of-use scale (Davis, 1989) that included items about accessibility of the app and caregiver experiences using the app. Satisfaction items were added to this scale to further assess caregivers’ interest in continued app use and willingness to recommend the app to other caregivers. The scale consisted of 21 items rated on a Likert scale from 1 (strongly disagree) and 5 (strongly agree). The original ease-of-use scale has high validity and strong internal consistency in general populations (Gao et al., 2018).
The app passively collected data that were used to examine feasibility, including number of unique visits to the app, total time spent using the app (in minutes), and level of mindfulness coach (1–14) reached in the app. To progress from one level to the next, a user must interact with (click) all elements of the modules including psychoeducation, a practice exercise, and a seated mindfulness meditation. Based on our prior research using Mindfulness Coach (Elissa Kozlov et al., n.d.) we defined visits as clusters of usage events (clicks within the app) that occurred less than 30 minutes apart.
To account for the impact of the COVID-19 pandemic on participants, we added a variable to indicate if data was collected pre or post the start of the COVID-19 pandemic. Data collected on or prior to March 15th, 2020 was labeled “pre- pandemic data,” and data collected after March 15th was labeled “post- pandemic data.”
Analyses
The SAS 9.4 (SAS Institute Inc., Cary, NC) software performed all data management and analyses. Prior to running the analyses, we rescaled all outcome measures (anxiety, depression, perceived stress, and caregiver burden) to 0–100, and converted total number of app minutes to hours. Caregiver outcomes were inversely scored to provide consistency with the other psychological measures (higher scores indicate more distress). The SAS Mixed procedure applied a separate polynomial (linear and quadratic) repeated-measures regression analysis for each outcome of interest (anxiety, depression, perceived stress, and caregiver burden) and predictor (study weeks and time spent in the app). All models included a time-level variable for COVID-19 timeframe (before or after March 15, 2020) and its interaction with each predictor. We entered the predictors and interactions sequentially for hypothesis testing, but simultaneously for drawing graphs. Because multicollinearity was high, we ran a separate model for each predictor. Fully anonymous and encrypted event sequences were stored using the javascript object notation (JSON) format on a remote AWS GovCloud server.
We conducted descriptive statistical analyses to characterize the demographic data as well as the feasibility and acceptability data.
Results
Participants
Prior to March 15th, 2020, participants (n = 20) were recruited using in-person strategies to participate in the study. Following March 15th, 2020, participants (n = 41) were recruited through virtual strategies. Of the 61 participants, 58 completed all interviews. One participant dropped out due to technical issues and time constraints, and 2 participants were lost to follow up at the 4-week interview. An additional 38 individuals responded to study advertisements and expressed initial interest in the study but were never consented or enrolled for the following reasons: ineligible (n = 3), unable to contact after 3 attempts (n = 22) or changed their mind about participation (n = 13). See Table 1 for demographic and recruitment data.
Table 1.
Participant baseline demographic and recruitment data (N = 60) and acceptability and usability data from 8 week (n = 58).
| Characteristic | Participants N(%)/Mean(SD) |
|---|---|
| Female | 57 (95.0%) |
| Caregiving for partner | 54 (90.0%) |
| Hours of care per week | 73.56 (67.47) |
| Age (years) | 61.78 (11.44) |
| Cohabitates with patient | 40 (66.7%) |
| Race | |
| Non-Hispanic white | 39 (65.0%) |
| African American | 8 (13.3%) |
| Multiracial | 1 (1.67%) |
| Hispanic | 9 (15.0%) |
| Asian/Pac. Islander | 3 (5.0%) |
| Recruitment period | |
| Participants recruited pre-COVID-19 | 20 (33.33%) |
| Participants recruited post-COVID-19 | 40 (66.67%) |
| Recruitment Site | |
| Community agencies | 29 (48.33%) |
| Physician in-person & telehealth visit referrals | 23 (38.33%) |
| Online caregiver support communities | 8 (13.33%) |
| 8-week Acceptability and Usability Scale | |
| I plan to use Mindfulness Coach in the next month | 50 (86.2%) |
| I will recommend Mindfulness Coach to a friend | 49 (84.5%) |
| I was satisfied with Mindfulness Coach | 49 (84.5%) |
| I found the Mindfulness Coach to be helpful to me | 49 (84.5%) |
| I think caregivers would benefit from Mindfulness Coach | 48 (82.8%) |
| Learning to use Mindfulness Coach was easy | 47 (81.1%) |
| Using Mindfulness Coach was clear and understandable | 45 (77.5%) |
| It was easy to become skillful at using Mindfulness Coach | 42 (72.4%) |
Satisfaction with the app and skill transfer
In general, participants reported that Mindfulness Coach was easy to use, and that the app helped them feel calmer, learn new skills, and reduce their stress. Nearly all participants (96.5%, n = 56) agreed that “most caregivers would benefit from using Mindfulness Coach,” and 84.5% (n = 49) reported that they were “satisfied with the app.” See Table 1 for ease and satisfaction with use data. In week 8, 96.7% reported practicing mindfulness without the app in the past two weeks for an average of 81.43 min (SD=164.1)
Feasibility
On average, participants spent a mean of 3.48 hours using the app (Median = 2.64 hours, SD = 2.78 hours). The mean and median level mindfulness coach level reached was 6.36 (SD = 4.62). However, 19% of participants completed all 14 levels, and 20.1% of participants only reached level 1, representing a bimodal distribution. The app was visited a mean of 29.47 times (Median = 21.5, SD = 23.37). In week eight, 80% of participants self-reported using Mindfulness Coach in the prior two weeks for an average of 45.5 min (SD = 37.24).
Anxiety
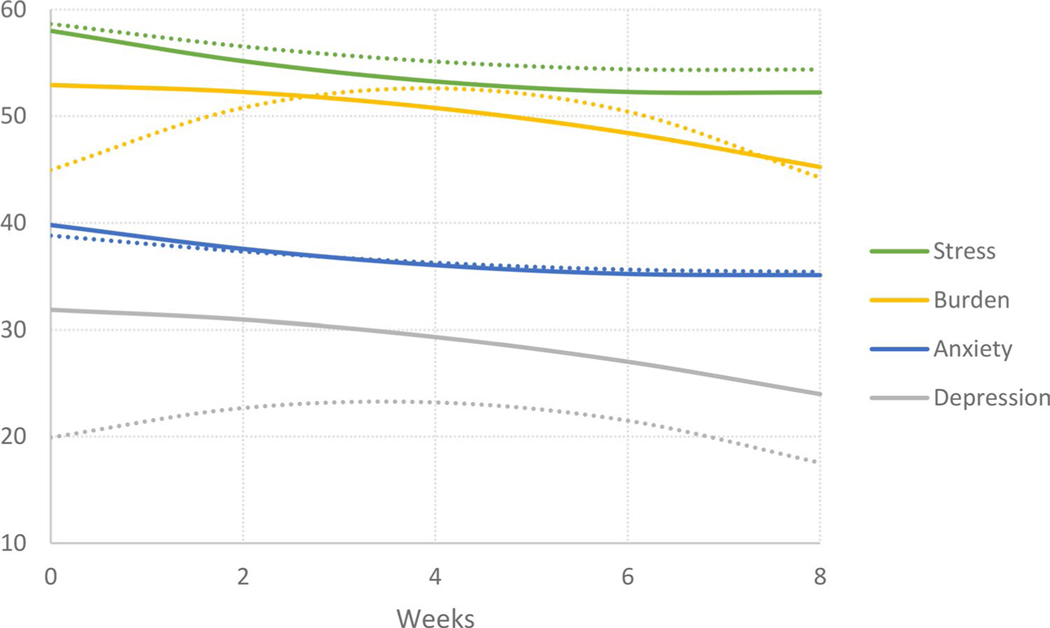
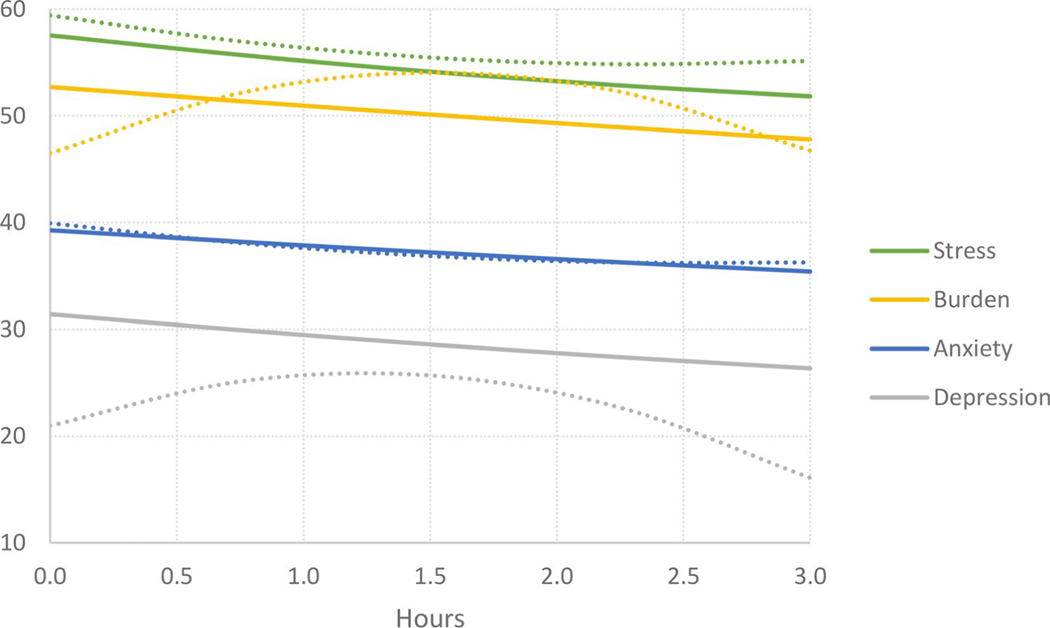
There was a significant linear effect of study weeks on HADS-A scores. See Table 2 and Figure 1. Anxiety symptoms significantly decreased as study weeks increased for both pre-COVID-19 and post-COVID-19 timeframes. There was also a significant linear effect of time spent using the app on HADS-A scores, such that more time spent using the app was associated with decreases in symptoms of anxiety. See Table 3 and Figure 2. The same significant linear trend held for app level reached and number of total app visits (see supplemental data).
Table 2.
Effect of study weeks on psychological outcomes, (n = 58).
| Outcome | Effect | B3 | B1 | P | f2 | R2 |
|---|---|---|---|---|---|---|
| Anxiety | Intercept | 38.81 | 0.05 | |||
| COVID | 1.00 | −1.82 | .47 | 0.00 | 0.05 | |
| Linear | −0.85 | −0.48 | .01 | 0.05 | 0.05 | |
| COVID x L | −0.45 | −0.07 | .88 | 0.00 | 0.05 | |
| Quadratic | 0.05 | 0.08 | .22 | 0.01 | 0.05 | |
| COVID x Q | 0.04 | 0.04 | .83 | 0.00 | 0.05 | |
|
| ||||||
| Stress | Intercept | 58.65 | 0.15 | |||
| COVID | −0.65 | −3.44 | .03 | 0.01 | 0.15 | |
| Linear | −1.23 | −0.58 | .0000 | 0.13 | 0.15 | |
| COVID x L | −0.42 | −0.07 | .84 | 0.00 | 0.15 | |
| Quadratic | 0.09 | 0.11 | .01 | 0.04 | 0.15 | |
| COVID x Q | 0.03 | 0.03 | .79 | 0.00 | 0.15 | |
|
| ||||||
| Depression | Intercept | 19.91 | 0.15 | |||
| COVID | 11.95 | 6.43 | .02 | 0.02 | 0.15 | |
| Linear | 1.94 | −0.94 | .0000 | 0.12 | 0.15 | |
| COVID x L | −2.22 | −0.74 | .18 | 0.01 | 0.15 | |
| Quadratic | −0.28 | −0.13 | .09 | 0.02 | 0.15 | |
| COVID x Q | 0.19 | 0.19 | .31 | 0.00 | 0.15 | |
|
| ||||||
| Burden | Intercept | 44.96 | 0.16 | |||
| COVID | 7.95 | 0.64 | .84 | 0.00 | 0.16 | |
| Linear | 3.91 | −0.88 | .0001 | 0.11 | 0.16 | |
| COVID x L | −4.03 | −1.00 | .08 | 0.01 | 0.16 | |
| Quadratic | −0.50 | −0.18 | .02 | 0.04 | 0.16 | |
| COVID x Q | 0.39 | 0.39 | .04 | 0.02 | 0.16 | |
Figure 1.
Effect of study weeks on psychological outcomes
Dotted lines = pre-COVID-19 assessment. Solid lines = post-COVID-19 assessment.
Table 3.
Effect of time spent using Mindfulness Coach on psychological outcomes, (n = 58).
| Outcome | Effect | B3 | B1 | P | f2 | R2 |
|---|---|---|---|---|---|---|
| Anxiety | Intercept | 39.93 | 0.05 | |||
| COVID | −0.66 | −1.82 | .47 | 0.00 | 0.05 | |
| Linear | −2.87 | −1.04 | .003 | 0.06 | 0.05 | |
| COVID x L | 1.40 | 0.25 | .83 | 0.00 | 0.05 | |
| Quadratic | 0.55 | 0.06 | .50 | 0.00 | 0.05 | |
| COVID x Q | −0.49 | −0.49 | .64 | 0.00 | 0.05 | |
|
| ||||||
| Stress | Intercept | 59.41 | 0.18 | |||
| COVID | −1.87 | −3.44 | .03 | 0.01 | 0.18 | |
| Linear | −3.84 | −0.84 | .0004 | 0.10 | 0.18 | |
| COVID x L | 1.21 | 0.68 | .40 | 0.00 | 0.18 | |
| Quadratic | 0.81 | 0.25 | .0001 | 0.10 | 0.18 | |
| COVID x Q | −0.56 | −0.56 | .41 | 0.00 | 0.18 | |
|
| ||||||
| Depression | Intercept | 20.98 | 0.11 | |||
| COVID | 10.43 | 6.43 | .02 | 0.02 | 0.11 | |
| Linear | 7.90 | −1.13 | .006 | 0.04 | 0.11 | |
| COVID x L | −9.97 | 0.22 | .88 | 0.00 | 0.11 | |
| Quadratic | −3.18 | 0.10 | .38 | 0.00 | 0.11 | |
| COVID x Q | 3.31 | 3.31 | .007 | 0.06 | 0.11 | |
|
| ||||||
| Burden | Intercept | 46.49 | 0.11 | |||
| COVID | 6.20 | 0.64 | .84 | 0.00 | 0.11 | |
| Linear | 9.98 | −1.24 | .002 | 0.06 | 0.11 | |
| COVID x L | −11.78 | −1.75 | .23 | 0.00 | 0.11 | |
| Quadratic | −3.30 | 0.02 | .82 | 0.00 | 0.11 | |
| COVID x Q | 3.35 | 3.35 | .006 | 0.06 | 0.11 | |
Figure 2.
Effect of hours spent using Mindfulness Coach on psychological outcomes
Dotted lines = pre-COVID-19 assessment. Solid lines = post-COVID-19 assessment.
Perceived Stress
There were significant linear and quadratic effects of study weeks and time spent using the app on Perceived Stress scores. See Tables 2 and 3 and Figures 1 and 2. The linear results indicated that as study weeks increased, perceived stress decreased; the same pattern held true for amount of time spent using the app. The quadratic results revealed that the effects of study weeks and of hours spent using the app on perceived stress were smaller over time, such that perceived stress decreased at a faster rate in early weeks of the study. Lastly, there was a significant main effect of COVID-19 timeframe on participant ratings of stress such that ratings of stress were significantly higher overall in the pre-COVID-19 time period compared to the post-COVID-19 time period.
Depression
There were significant linear effects of study weeks and time spent using the app on HADS-D scores, indicating that depressive symptoms improved as study weeks progressed and as amount of time spent using the app increased. See Tables 2 and 3 and Figures 1 and 2. There was also a significant quadratic interaction between COVID-19 time frame and time spent using the app: a quadratic (nonlinear) trend is present only in the post-COVID-19 timeframe. There was also a significant main effect of COVID-19 timeframe on participant ratings of depression: ratings of depression were significantly higher in the post-COVID-19 period compared to the pre-COVID-19 period.
Caregiver Burden
There was a significant linear effect of study weeks on caregiver burden scores: as study weeks increased, ratings of caregiver burden decreased. See Tables 2 and 3 and Figures 1 and 2. Results also indicated a significant quadratic effect of study weeks and an interaction with COVID-19 timeframe. The improvement in caregiver burden in the post-COVID-19 period was nearly linear, whereas a nonlinear trend was apparent pre-COVID-19. The linear effect of total time spent using the app on caregiver burden was also significant, signaling that caregiver burden decreased as time spent using the app increased. The same quadratic interaction effect COVID-19 timeframe held for time spent using the app.
Discussion
This study demonstrated that mHealth-delivered Mindfulness Therapy is feasible, acceptable, and preliminarily effective in alleviating symptoms of anxiety, stress, depression, and caregiver burden in informal caregivers of older adults with cognitive impairment. More than 70% of participants in our study rated the app as acceptable and used the app throughout the 8-week study. Importantly, we found significant associations between metrics of app use and improvements in psychological symptoms, suggesting that more overall app use confers greater benefit. These results indicate that mHealth strategies to mitigate the negative psychological effects of caregiving for older adults with cognitive impairment are an important area for further research and development.
Caregivers of older adults with cognitive impairment were amenable to Mindfulness Coach. Participants not only reported that the app was helpful and easy to use, but their user data also indicated that they used it for significant amounts of time across the study period. This finding is consistent with previous research about the feasibility, acceptability, and efficacy of mHealth mindfulness interventions for caregivers. For example, Kubo and colleagues studied an mHealth mindfulness intervention in informal cancer caregivers and found that most caregivers found the mHealth app feasible, acceptable and preliminarily effective to reduce depression and improve quality of life (Kubo et al., 2019). Other prior studies also found mHealth mindfulness to improve psychological outcomes in general adult populations, and that participants were highly satisfied with the app and used it several times per week or daily (Bostock et al., 2019, Van Emmerik, Berings & Lancee, 2018). However, because previous work has not specifically evaluated the utility of these interventions in caregivers of older adults with cognitive impairment, the current study expands our understanding of the range of interventions acceptable to this specific caregiver population. Though caregivers have unique demands on their time, their satisfaction ratings and frequency of use are similar to studies of the general adult population. Utilizing mHealth strategies may make access to treatment options more equitable for caregivers with common barriers to psychological treatment (e.g., time limitations, transportation, finances).
Our results also suggest that symptoms of anxiety, stress, depression, and caregiver burden decreased over the study period and with increased app use. Given the nature of neurodegenerative diseases such as Alzheimer’s Disease, providers might expect caregiver mental health to decline over an 8-week study period, as care recipients’ condition tends to worsen over time (van den Kieboom et al., 2020) which can impact the mental health of the caregiver. In fact, our study indicated this was not the case, implying a potential protective effect of mHealth mindfulness approaches to maintaining or improving psychological symptoms. Given the 2018 review of inter-net based interventions to support family caregivers of people with dementia which revealed generally positive effects in 40 mostly low-quality studies (Hopwood et al., 2018), this study adds to the growing evidence that caregivers of adults with dementia may benefit from accessible web or mobile health based interventions. Notably, in the case of depressive symptoms and caregiver burden, there were differential effects of app use on symptoms between periods of interest (pre-pandemic and post-pandemic), such that symptoms improved at a faster rate during the post-pandemic period. This finding suggests that an mHealth intervention, like Mindfulness Coach, may confer different benefits for populations under different amounts of life stress. The pandemic caused additional stress and burden for caregivers, which may have made the need for an mHealth based intervention more urgent and impactful, especially given the diminishing opportunity to utilize alternative resources for both patients and caregivers such as home health aides, adult day programs, support groups and in-person counselling. Future work should consider participants’ ratings of severity of other external life stressors to elucidate the potential differential impact of mHealth MT based on individual circumstances.
The findings of this study raise additional questions about the dose of Mindfulness Coach that is required to produce meaningful change in psychological symptoms and skill transfer (Carmody & Baer, 2009). Our study revealed that most participants spent substantial amounts of time meditating without using the app, indicating that the app taught participants how to practice mindfulness independently. Because we only assessed time spent meditating away from the app in week 8, we do not know when participants learned enough skills from the app to practice mindfulness independently. Our results also found a significant quadratic main effect of stress, suggesting that rate of change in improvement in stress may plateau after a certain amount of time spent using the app, thus additional use may not confer additional benefits. Alternatively, it may be that individuals with greater stress are more likely to use the app more regularly. Further investigation expanding this preliminary work is needed to elucidate the dose-response relationship of Mindfulness Coach.
Limitations
This study was constrained by several limitations. First, we are unable to calculate the response rate to this study due to the shift in our recruitment methodology: it was not possible to track how many individuals received our email advertisement or social media postings for the study. Second, our findings are possibly shaped by selection and response bias, as virtual recruitment was inherently more accessible to technology-savvy caregivers. Future work should prioritize recruitment strategies to maximize generalizability. Additionally, our sample was primarily female, thus results may vary with non-female users. Notably, women step into caregiving roles more often than men (61% of caregivers are women while 39% of caregivers are men, respectively) (AARP, 2020), so our sampling is reflective of the gender breakdown in caregiving. Additionally, our sample skewed white and older, thus raising additional limitations on the generalizability of this study. Future research is needed on participants from diverse racial and ethnic backgrounds as well as from different age groups to ensure generalizability of findings.
Implications
The shortage of mental health care professionals (Butryn et al., 2017) in the United States underscores the need for scalable mHealth psychological interventions. Our promising findings suggest that Mindfulness Coach may be one feasible way to address caregiver mental health needs. Moreover, given that caregivers of persons with cognitive impairment are at increased risk of social isolation (Kovaleva et al., 2018)—especially considering social-distancing guidelines associated with the COVID-19 pandemic (Savla et al., 2021)—mHealth interventions that are accessible at any time are essential: they offer opportunities for caregivers to address mental health needs without interference from structural and personal barriers that might reduce help-seeking behaviour. From an equitability standpoint, mHealth apps remove the financial burden of psychological treatment: there are scant mental health providers who accept insurance, and many caregivers remain under or uninsured. Evidence-based mHealth approaches for caregiver mental health can make treatment widely accessible. Future research should focus on determining strategies to integrate accessible mental health care for caregivers, such as mHealth strategies, into routine care for older adults with cognitive impairment.
Caregiver mental health is an insidious public health issue. Our preliminary results suggest that an mHealth approach to managing psychological distress in caregivers of older adults with cognitive impairment may be a scalable, and acceptable way to address rampant caregiver distress. Given the magnitude of caregiver distress and its associated negative outcomes, interventions like Mindfulness Coach that have preliminary efficacy in addressing these symptoms should be prioritized in further investigation.
Supplementary Material
Acknowledgments
We would like to acknowledge Jessica Israel, MD, Ibiyonu Lawrence, MD and Fred Kobylarz, MD, for their support with recruitment.
Source of Funding
This work was supported by Elissa Kozlov’s KL2 award from the Rutgers Clinical and Translational Science Center, funded by the National Institutes of Health: KL2TR003018.
Footnotes
Conflicts of Interest
There is no conflict of interest.
References
- AARP and National Alliance for Caregiving. (2020). Caregiving in the United States 2020. Washington, DC: AARP. 10.26419/ppi.00103.001 [DOI] [Google Scholar]
- Alzheimer’s Association. (2019). Alzheimer’s Disease Facts and Figure. https://www.alz.org/media/Documents/alzheimers-facts-and-figures-2019-r.pdf [Google Scholar]
- Alzheimer’s Association. (2016). 2016 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia : The Journal of the Alzheimer’s Association, 12(4), 459–509. http://www.ncbi.nlm.nih.gov/pubmed/27570871 [DOI] [PubMed] [Google Scholar]
- Bakas T, Champion V, Perkins SM, Farran CJ, & Williams LS (2006a). Psychometric testing of the revised 15-item bakas caregiving outcomes scale. Nursing Research. 10.1097/00006199-200609000-00007 [DOI] [PubMed] [Google Scholar]
- Bakas T, Champion V, Perkins SM, Farran CJ, & Williams LS (2006b). Psychometric testing of the revised 15-item bakas caregiving outcomes scale. Nursing Research. 10.1097/00006199-200609000-00007 [DOI] [PubMed] [Google Scholar]
- Berglund E, Lytsy P, & Westerling R. (2015). Health and wellbeing in informal caregivers and non-caregivers: A comparative cross-sectional study of the Swedish a general population. Health and Quality of Life Outcomes. 10.1186/s12955-015-0309-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, & Neckelmann D. (2002). The validity of the Hospital Anxiety and Depression Scale. Journal of Psychosomatic Research, 52, 69–77. 10.1016/S0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- Brown EL, Ruggiano N, Li J, Clarke PJ, Kay ES, & Hristidis V. (2019). Smartphone-Based Health Technologies for Dementia Care: Opportunities, Challenges, and Current Practices. Journal of Applied Gerontology, 38(1), 73–91. 10.1177/0733464817723088 [DOI] [PubMed] [Google Scholar]
- Butryn, Bryant L, Marchionni C, & Sholevar F. (2017). The shortage of psychiatrists and other mental health providers: Causes, current state, and potential solutions. International Journal of Academic Medicine, 3(1), 5. 10.4103/IJAM.IJAM_49_17 [DOI] [Google Scholar]
- Capistrant BD (2016). Caregiving for Older Adults and the Caregivers’ Health: an Epidemiologic Review. Current Epidemiology Reports. 10.1007/s40471-016-0064-x [DOI] [Google Scholar]
- Carmody J, & Baer RA (2009). How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology, 65(6), 627–638. 10.1002/jclp.20555 [DOI] [PubMed] [Google Scholar]
- Chittaro L, & Vianello A. (2014). Computer-supported mindfulness: Evaluation of a mobile thought distancing application on naive meditators. International Journal of Human-Computer Studies, 72(3), 337–348. 10.1016/J.IJHCS.2013.11.001 [DOI] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior. [PubMed] [Google Scholar]
- Corporation UB, Street B, Bohlmeijer E, Prenger R, Taal E, Cuijpers P, Meyers FJ, Linder J, Beckett L, Christensen S, Blais J, Gandara DR, Palmer JL, Ph D, Zhang TAO, Bruera E, Costantini A, Kalus C, Werth JL, … Lo C. (2014). Place of death: hospital-based advanced home care versus conventional care. A prospective study in palliative cancer care. Palliative Medicine, 18(6), 563–569. 10.1191/0269216304pm924oa [DOI] [PubMed] [Google Scholar]
- Crabb RM, Cavanagh K, Proudfoot J, Learmonth D, Rafie S, & Weingardt KR (2012). Is computerized cognitive-behavioural therapy a treatment option for depression in late-life? A systematic review. In British Journal of Clinical Psychology (Vol. 51, Issue 4, pp. 459–464). Wiley-Blackwell. 10.1111/j.2044-8260.2012.02038.x [DOI] [PubMed] [Google Scholar]
- Czaja SJ, Boot WR, Charness N, A Rogers W, Sharit J, Fisk AD, Lee CC, Nair SN, A Rogers W, Sharit J, Fisk AD, Lee CC, & Nair SN (2015). The personalized reminder information and social management system (PRISM) trial: Rationale, methods and baseline characteristics. Contemporary Clinical Trials, 40, 35–46. 10.1016/j.cct.2014.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czaja SJ, Boot WR, Charness N, Rogers WA, & Sharit J. (2018). Improving Social Support for Older Adults Through Technology: Findings From the PRISM Randomized Controlled Trial. Gerontologist, 58(3), 467–477. 10.1093/geront/gnw249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis FD (1989). Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly: Management Information Systems. 10.2307/249008 [DOI] [Google Scholar]
- Deeken F, Häusler A, Nordheim J, Rapp M, Knoll N, & Rieckmann N. (2018). Psychometric properties of the Perceived Stress Scale in a sample of German dementia patients and their caregivers. International Psychogeriatrics, 30(1), 39–47. 10.1017/S1041610217001387 [DOI] [PubMed] [Google Scholar]
- Epstein-Lubow G, McBee L, Darling E, Armey M, & Miller IW (2011). A Pilot Investigation of Mindfulness-Based Stress Reduction for Caregivers of Frail Elderly. Mindfulness, 2(2), 95–102. 10.1007/s12671-011-0047-4 [DOI] [Google Scholar]
- Firth J, Torous J, Nicholas J, Carney R, Rosenbaum S, & Sarris J. (2017). Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. Journal of Affective Disorders, 218, 15–22. 10.1016/J.JAD.2017.04.046 [DOI] [PubMed] [Google Scholar]
- Freedman VA, & SPILLMAN BC (2014). Disability and care needs among older americans. Milbank Quarterly, 92(3), 509–541. 10.1111/1468-0009.12076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao M, Kortum P, & Oswald F. (2018). Psychometric Evaluation of the USE (Usefulness, Satisfaction, and Ease of use) Questionnaire for Reliability and Validity. 10.1177/1541931218621322 [DOI]
- Gitlin LN, Belle SH, Burgio LD, Czaja SJ, Mahoney D, Gallagher-Thompson D, Burns R, Hauck WW, Zhang S, Schulz R, & Ory MG (2003). Effect of multicomponent interventions on caregiver burden and depression: The REACH multisite initiative at 6-month follow-up. Psychology and Aging. 10.1037/0882-7974.18.3.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gough K, & Hudson P. (2009). Psychometric Properties of the Hospital Anxiety and Depression Scale in Family Caregivers of Palliative Care Patients. Journal of Pain and Symptom Management, 37(5), 797–806. 10.1016/j.jpainsymman.2008.04.012 [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, & Oh D. (2010). The Effect of Mindfulness-Based Therapy on Anxiety and Depression: A Meta-Analytic Review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood J, Walker N, McDonagh L, Rait G, Walters K, Iliffe S, Ross J , & Davies N. (2018). Internet-Based Interventions Aimed at Supporting Family Caregivers of People With Dementia: Systematic Review. Journal of medical Internet research, 20(6), e216. 10.2196/jmir.9548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howells A, Ivtzan I, & Eiroa-Orosa FJ (2016). Putting the ‘app” in Happiness: A Randomised Controlled Trial of a Smartphone-Based Mindfulness Intervention to Enhance Wellbeing.’ Journal of Happiness Studies, 17(1), 163–185. 10.1007/s10902-014-9589-1 [DOI] [Google Scholar]
- Jones SL, Hadjistavropoulos HD, & Soucy JN (2015). A randomized controlled trial of guided internet-delivered cognitive behaviour therapy for older adults with generalized anxiety. Journal of Anxiety Disorders, 37, 1–9. 10.1016/j.janxdis.2015.10.006 [DOI] [PubMed] [Google Scholar]
- Kovaleva M, Spangler S, Clevenger C, & Hepburn K. (2018). Chronic stress, social isolation, and perceived loneliness in dementia caregivers. Journal of Psychosocial Nursing and Mental Health Services, 56(10), 36–43. 10.3928/02793695-20180329-04 [DOI] [PubMed] [Google Scholar]
- Kozlov E, Eghan C, Moran S, Herr K, & Reid MC (2017). Palliative Care Providers’ Practices Surrounding Psychological Distress Screening and Treatment: A National Survey. American Journal of Hospice and Palliative Medicine. 10.1177/1049909117743960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozlov Elissa, Bantum E, Pagano I, Walser R, Ramsey K, Taylor K, Jaworski B. & Owen J. (n.d.). Assessing the reach, use and impact of a free mHealth Mindfulness app in the general population. Journal of Medical Internet Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubo A, Kurtovich E, McGinnis MA, Aghaee S, Altschuler A, Quesenberry C, Kolevska T, & Avins AL (2019). A Randomized Controlled Trial of mHealth Mindfulness Intervention for Cancer Patients and Informal Cancer Caregivers: A Feasibility Study Within an Integrated Health Care Delivery System. Integrative Cancer Therapies. 10.1177/1534735419850634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EH (2012). Review of the psychometric evidence of the perceived stress scale. In Asian Nursing Research (Vol. 6, Issue 4, pp. 121–127). Elsevier. 10.1016/j.anr.2012.08.004 [DOI] [PubMed] [Google Scholar]
- Mani M, Kavanagh DJ, Hides L, & Stoyanov SR (2015). Review and Evaluation of Mindfulness-Based iPhone Apps. JMIR MHealth and UHealth, 3(3), e82. 10.2196/mhealth.4328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mykletun A, Stordal E, & Dahl AA (2001). Hospital Anxiety and Depression (HAD) scale: factor structure, item analyses and internal consistency in a large population. The British Journal of Psychiatry : The Journal of Mental Science, 179, 540–544. 10.1192/bjp.179.6.540 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences Engingeering and Medicine. (2012). Families Caring for an Aging America : Health and Medicine Division. The National Academies Press. http://www.nationalacademies.org/hmd/Reports/2016/families-caring-for-an-aging-america. aspx [PubMed] [Google Scholar]
- National Alliance for Caregiving and the Alzheimer’s Association. (2017). Dementia Caregiving in the U.S. http://www.caregiving.org/wp-content/uploads/2017/02/DementiaCaregivingFINAL_WEB.pdf
- Olthuis Janine V, Watt Margo C, Bailey K, Hayden Jill A, & Stewart Sherry H. (2016). Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database of Systematic Reviews, 3. 10.1002/14651858.CD011565.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paller KA, Creery JD, Florczak SM, Weintraub S, Mesulam M-M, Reber PJ, Kiragu J, Rooks J, Safron A, Morhardt D, Gigler KL, Molony JM, & Maslar M. (n.d.). Benefits of Mindfulness Training for Patients With Progressive Cognitive Decline and Their Caregivers. 10.1177/1533317514545377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, & Sörensen S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychology and Aging. [DOI] [PubMed] [Google Scholar]
- Predicting caregiver burden and depression in Alzheimer’sdisease. (2000). The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 55(1), S2−−13. 10.1093/geronb/55.1.S2 [DOI] [PubMed] [Google Scholar]
- Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, & Ruggiero KJ (2014). mHealth: A mechanism to deliver more accessible, more effective mental health care. Clinical Psychology and Psychotherapy, 21(5), 427–436. 10.1002/cpp.1855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riffin C, Van Ness PH, Wolff JL, & Fried T. (2017). Family and Other Unpaid Caregivers and Older Adults with and without Dementia and Disability. Journal of the American Geriatrics Society. 10.1111/jgs.14910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savla J, Roberto KA, Blieszner R, McCann BR, Hoyt E, & Knight AL (2021). Dementia Caregiving During the “Stay-at-Home” Phase of COVID-19 Pandemic. The Journals of Gerontology: Series B, 76(4), e241–e245. 10.1093/geronb/gbaa129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillman B, Wolff J, Freedman V, & Kasper J. (2014). Informal Caregiving for Older Americans: An Analysis of the 2011 National Survey of Caregivgining. Report to the Assistant Secretary for Planning and Evaluation, Office of Disability, Aging and Long-Term Care Policy. 10.1093/geronb/gbu004 [DOI] [Google Scholar]
- Tara D, Katherine P, Judy P, Janine C, Rose BM, Helen C, Donker T, Petrie K, Proudfoot J, Clarke J, Birch M-R, & Christensen H. (2013). Smartphones for Smarter Delivery of Mental Health Programs: A Systematic Review. Journal of Medical Internet Research, 15(11), e247. 10.2196/jmir.2791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaingankar JA, Chong SA, Abdin E, Picco L, Jeyagurunathan A, Zhang YJ, Sambasivam R, Chua BY, Ng LL, Prince M, & Subramaniam M. (2016). Care participation and burden among informal caregivers of older adults with care needs and associations with dementia. International Psychogeriatrics. 10.1017/S104161021500160X [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Kieboom R, Snaphaan L, Mark R , & Bongers I. (2020). The Trajectory of Caregiver Burden and Risk Factors in Dementia Progression: A Systematic Review. Journal of Alzheimer’s disease : JAD, 77(3), 1107–1115. 10.3233/JAD-200647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilchinsky N, Dekel R, Revenson TA, Liberman G, & Mosseri M. (2015). Caregivers’ burden and depressive symptoms: The moderational role of attachment orientations. Health Psychology. 10.1037/hea0000121 [DOI] [PubMed] [Google Scholar]
- Zigmond AS, & Snaith RP (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.