Abstract
Background:
Bladder tumors are identified and treated using a surgical procedure called as transurethral resection of bladder tumors (TUR-BT). During TUR-BT resection, stimulation of the obturator nerve may cause violent adductor muscle spasms. The “obturator reflex,” as this disorder is known, generally causes the legs to move inadvertently (leg jerking). Since this condition can cause several complications, it is preferable to avoid it.
Objective:
In this study, we investigated the effectiveness of spinal anesthesia combined with obturator nerve block or general anesthetic without muscle relaxant in preventing adductor muscle spasm during TUR-BT procedures.
Methods:
Forty consecutive patients were enrolled in a prospective observational evaluation and divided into two groups. Patients in Group I underwent spinal anesthesia along with an obturator nerve block, while those in Group II underwent general anesthesia without a neuromuscular relaxant. The following details were recorded: time for obturator block performance, the severity of the motor blockade, the length of the procedure in both groups because a probable adductor spasm might make it more difficult. The level of the surgeon’s pleasure was noted throughout the surgery. Additionally, the patient’s satisfaction and any issues that may have arisen were documented (the incidence of vascular puncture, hematoma, nerve damage, and visceral injury was noted).
Results:
Block performance time in Group I was 4.8±0.5 minutes, whereas it was 5.0±0.3 minutes in Group II. The ease of access for the two groups was the same. Group I demonstrated increased patient and surgeon satisfaction with a general anesthesia without neuromuscular relaxants and an obturatorius nerve block. Mean surgical time did not differ between the groups.There were no complications in either group.
Conclusion:
During such operations, routine use of ONB in combination with spinal anaesthetic or general anesthetic without a neuromuscular blocker can enhance oncological outcomes for patients, reduce complication rates, and extend the period of time spent living without disease.
Keywords: obturator nerve block, transurethral resection of bladder tumor, spinal anesthesia, general anesthesia
1. BACKGROUND
Bladder tumors are identified and treated using a surgical procedure called as transurethral resection of bladder tumors (TUR-BT). The diagnostic goal of TUR-primary BT is to gather histological information on the kind of tumor and the course of the disease. The complete eradication of all invasive, microscopic malignancies is the main goal of treatment (1).
The obturator nerve is placed near to the inferolateral bladder wall and the bladder neck in the pelvis. During transurethral resections of tumors in these localizations, electrical current travelling via the resectoscope activates the obturator nerve. With spinal anesthesia, the motor branch of the nerve can be inhibited, but the sensory branch might not. Adductor muscle contractions can be fierce as a result of this stimulation. The “obturator reflex,” as this disorder is known, generally causes the legs to move inadvertently (leg jerking). A few of the worst negative effects that could result from an unintended leg movement are incomplete resection, bladder perforation, vascular injury, extravesical dissemination of cancer cells, uncontrollable bladder hemorrhage, and obturator muscle hematomas (2). Obturator nerve stimulation is a regular occurrence, although little is known about how to avoid it. To eliminate adductor muscle spasm, a number of alternative procedures have been tested, including resection while under general anesthesia, partial bladder retention during resection, reducing the intensity of the electrocautery, and switching the polarity of the electrical current (2, 3). However, not all of these techniques have been shown to be as effective at lessening obturator nerve stimulation (3).
The obturator nerve block (ONB) technique, which was first introduced by Prentiss et al. in 1965 (4), is a straightforward treatment with a low risk of complications. Obturator block is clinically necessary, albeit it might not be effective if the nerve is severely compressed (3). The adductor muscle contracts and related effects occur when the ONB fails during TUR-BT because the obturator nerve is stimulated (5, 6). Research has been conducted so far to evaluate the effectiveness of a variety of ONB techniques that have been described (3, 7). According to past studies in the literature, ONB can prevent adductor spasms and the complications they may cause (1, 5). On the other hand, in some situations ONB alone is insufficient, and additional effective anesthetic techniques are currently being studied (1, 8). TUR-B operations are short-term activities. This type of technique, which is unique to anesthetic management, is routinely performed on elderly patients with comorbidities. In terms of anesthetic applications, spinal anesthesia or laryngeal mask anesthesia (LMA) without the use of muscle relaxants are usually preferable.
In this evaluation for the first time in our center ONB was performed. We sought to determine if general anesthesia without muscle relaxant combined with ONB or spinal anesthesia combined with ONB is effective to avoid adductor muscle spasm in TUR-BT surgeries.
2. OBJECTIVE
In this study, we investigated the effectiveness of spinal anesthesia combined with obturator nerve block or general anesthetic without muscle relaxant in preventing adductor muscle spasm during TUR-BT procedures.
3. MATERIAL AND METHODS
With the approval of the hospital’s Ethics Committee and the patients’ signed informed consent, a prospective observational research was developed. Retrospective analysis of 200 patients with primary bladder cancer who underwent TUR-BT under general or spinal anesthesia without the use of a neuromuscular relaxant was done in accordance with the principles of the Helsinki Declaration. The preoperative computer tomography or ultrasound results of 40 of these patients were chosen for the evaluation because it showed that their tumor was on the lateral bladder wall. An abnormal coagulation profile, damage to the obturator nerve, neurological conditions that affect the central nervous system, a history of allergies to local anesthetic agents, prior hip or inguinal surgery, inguinal lymphadenopathy, a perineal infection or hematoma at the site of the needle insertion and the presence of conditions that preclude the use of regional anesthesia were among the exclusion criteria. All patients had definite physical status of the American Association of Anesthesiologist.
When regional anesthesia was neither appropriate nor preferred, general anesthesia was administered with the help of an LMA without the use of neuromuscular relaxant. These individuals were assigned to Group I. Group II categorized patients under spinal anesthesia. The study consisted of 40 patients, 20 in each group.
Using a 20 G intravenous cannula, preoperative prophylactic antibiotics and premedication (0.05 mg/kg midazolam) were administered to every patient. They received 500 ml of intravenous 0.9% normal saline as preloading as well. The operating hours of each group were noted. All patients underwent routine anesthesia monitoring in the operating room, which included continuous electrocardiography (ECG), heart rate, and non-invasive blood pressure readings. The same urology team operated on both groups, as did the same anesthetic team for ONB. Comparisons were made between the groups in terms of adductor muscle contraction and bladder perforation.
Method of general anesthesia
Patients in Group I underwent induction in anesthesia with 1-2 mcg/kg fentanyl and 2 mcg/kg propofol. Patients having LMA were anesthetized using 4-5% desflurane. LMA was used in this group without neuromuscular block.
Method of spinal anesthesia
Spinal anesthesia was carried out while the patient was seated. A 26 G Quincke spinal needle was used to administer 10–15 mg of 0.5% hyperbaric bupivacaine to the patients in Group II, entering from the L3-4 or L4-5 intervertebral regions. After receiving the medication, the patients were positioned in the supine position.
Obturator nerve block technique
Following general anesthesia with LMA or spinal anesthesia ONB was performed. Depending on where the tumor was localized, ONB was done on the right or left side. Prior to ONB, the inguinal regions of the patients were cleansed with iodopovidone while they were supine with their legs slightly (30°) abducted. A peripheral nerve stimulator (Stimuplex®, B. Braun, Melsungen, Germany) and a 50 mm Teflon-insulated needle (22 G Stimuplex® A, B. Braun, Melsungen, Germany) were used. High-frequency linear VF 12-4 ultrasound (Siemens Acuson NX3 )and the interadductor approach were used to implement the obturator block. The linear probe was positioned across the inguinal ligament, 2 cm caudal and 2 cm medial to the femoral artery. The in-plane method was used to implant the needle. The adductor longus and adductor brevis muscles’ fasciae were crossed by the needle as it was advanced. There, the obturator nerve’s anterior branch is attained. The Stimuplex® simultaneously detected fasciculations in the knee. At first, a 2 mA current and a 2 Hz frequency were set. To get the intrinsic twitch response, the current was lowered to 0.5 mA at a frequency of 2 Hz and 0.1 ms. Then 15 ml of 0,5 % of Bupivacain was administered. On ultrasound imaging, the distribution of local anesthetic was seen between the two fasciae. The same operation was carried out between the fascias of the adductor brevis and adductor magnus muscles. The posterior branch of the obturator nerve was also occluded in this location.
The following details were noted throughout the procedure: The time it took from the commencement of ultrasonography till the needle was taken out at the end of the block, and how simple the procedure was The following categories are utilized depending on how many needle redirections are required to complete the block: Number of successful, unsuccessful, and easy needle passes. 2, >2, and >10 needle passes were made.
The surgeon entered the operating room without being aware of the group assignment to start the TURBT and rate the motor obstruction as follows: Adductor spasm score: 0; reduced adductor spasm score: 1; no adductor spasm score: 2. Due to the possibility of an adductor spasm, both groups additionally evaluated the length of the surgery. The level of surgeon satisfaction (excellent, good, moderate, and bad) was assessed for the two different groups during the procedure and was also documented. The patient’s satisfaction was noted, and any complications, if any, were noted (the incidence of vascular puncture, hematoma, nerve damage, and visceral injury was noted).
Statistical analysis
Using the Shapiro-Wilk test, continuous variables’ normality was assessed. The Mann-Whitney U test was used to compare nonparametric variables between the two groups, whereas an independent sample ttest was employed to compare parametric variables between the two groups. IBM SPSS Statistics 21 was used to perform the statistical analysis (IBM Corp., Armonk, NY). Statistical significance was defined as a p-value less than 0.05. Demografoc and clinical data were recorded as well. Descriptive data were expressed as mean and standard deviation.
4. RESULTS
Between February 2022 and October 2022, 40 individuals (aged 45 to 89) were enrolled in the study. In Table 1, demographic data are displayed.
Table 1. Demographic data Group I: General anesthesia + obturator nerve block. Group II: spinal anesthesia + obturator nerve block. ASA, American Society of Anesthesiologists physical status.
| Group I | Group II | p value | |
|---|---|---|---|
| Age (mean±SD) | 74±9 | 78±7 | 0.10 |
| Gender | 0.40 | ||
| Female (n, %) | 1 (5%) | 3 (15%) | |
| Male (n, %) | 19 (95%) | 17 (85%) | |
| ASA | 0.36 | ||
| I (n, %) | 4 (20%) | 1 (20%) | |
| II (n, %) | 12 (60%) | 11 (60%) | |
| III (n, %) | 4 (20%) | 8 (35%) |
Block performance time in Group I was 4.8±0.5 min, while in Group II it was 5.0±0.3 min. There were no differences in the two groups’ ease of approach. With a combination of general anesthesia without neuromuscular relaxants and an obturatorius nerve block, Group I showed improved patient and surgeon satisfaction. Both groups did not have any complications. Table 2 illustrates the block performance time, ease of approach, surgeon and patient satisfaction scores for the two groups, the grade of the motor block, and complications.
Table 2. Opturatorius nerve block characteristics.
| Group I (n=20) | Group II (n=20) | P value | |
|---|---|---|---|
| Block performance time (min) mean±SD | 4.8±0.5 | 5.0±0.3 | 0.29 |
| Ease of approach to perform block (n, %) Easy <2 Difficult 2-10 Failed >10 |
15 (75%) 5 (25%) / |
17 (85%) 3 (15%) / |
0.79 |
| Grade of the motor block (n, %) Adductor spasm Reduced spasm No adductor spasm |
/ 1 (5%) 19 (95%) |
/ 2 (10%) 18 (90%) |
0.19 |
| Surgeon satisfaction (n, %) Bad Moderate Good Excellent |
/ / 4 (20%) 16 (80%) |
/ / 5 (25%) 15 (75%) |
0.14 |
| Patient satisfaction (n, %) Bad Moderate Good Excellent |
/ / 1 19 |
/ / 2 18 |
0.19 |
| Complications | / | / | / |
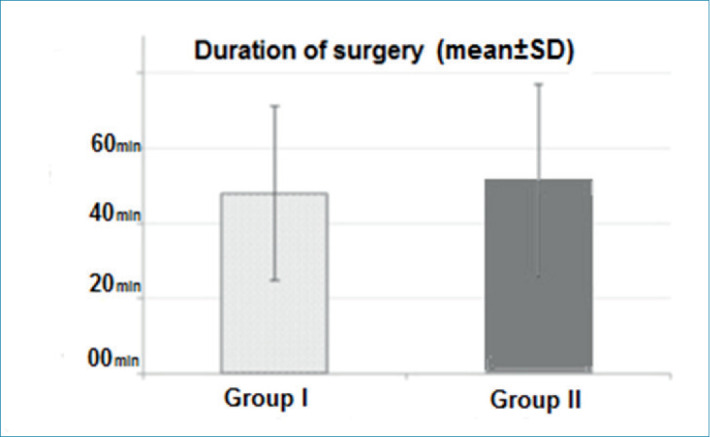
Mean surgical time did not differ between the groups (Figures 1).
Figure 1. Mean surgical operation time.
5. DISCUSSION
Although TUR-BT is frequently used to treat superficial and well-differentiated transitional cell bladder cancers, most urologists are concerned about the potential consequences of this procedure’s ability to trigger the obturator reflex (9). Obturator reflex is a prevalent issue in urology practice because 46.8% of all superficial bladder cancers are situated on the lateral wall (10). The negative outcomes of TUR-BT include bladder perforation, difficult-to-control bleeding, and occasionally insufficient tumor removal (11). Strong adductor muscle contractions may also have other important implications, such as a full bladder perforation and the dissemination of extravesical tumor cells (12,13). The most common strategy to prevent these serious issues is ONB (13).
At this study, we used ONB for the first time in our center and compared its effectiveness to spinal anesthesia for general anesthesia without the use of muscle relaxants. We showed that in cases where using muscle relaxants is not desirable or in which patients are unable to receive spinal anesthesia due to technological difficulties, surgeries can be planned with the addition of ONB to general anesthetic without neuromuscular block. Direct stimulation of the motor branch of the obturator nerve activates adduction. Some methods, such as partial bladder retention while under general anesthesia, electrical current power reduction, and electrical polarity adjustment, have been tested to prevent adductor muscle spasm during TUR-BT. However, none of these strategies have been effective enough to stop the obturator. However, none of these techniques has been effective in halting obturator nerve activation. In 1965, Prentiss et al. proposed ONB as a way to prevent adductor spasms during TUR-BT (4). ONB was suggested in addition to spinal and general anesthesia. Additional documented uses for ONB include the treatment of severe hip joint diseases and the easing of pain brought on by adductor muscle spasm linked to obturator neuralgia, multiple sclerosis, and paraplegia (14). As a result, ONB became more well-known in the years that followed. Atanassoff and associates evaluated ONB with three-in-one block to prevent adductor spasm during TUR-BT (5). Adductor spasms during TUR-BT were shown to happen more frequently (55%) when spinal anesthetic was used alone. According to Tatlsen and colleagues, adductor spasm incidence was reported to be 3% when ONB was given to spinal anesthesia (2). During our inquiry, we found that the adductor spasm incidence was 10% lower and absent in the spinal anesthesia with ONB group. In a study by Patel et al., it was discovered that doing ONB in conjunction with spinal anesthetic prior to TUR-BT totally eliminated adductor spasm in 96% of instances. However, when ONB was not combined with spinal anesthesia in the control group, the surgeon’s satisfaction was not consistently maintained throughout the treatment. Two patients in the control group developed bladder perforation as a result of substantial adductor spasm, needing an urgent laparotomy for one of them (7). So and colleagues saw an adductor muscle spasm in a patient who received spinal anesthesia for TUR-BT, which forced them to stop the procedure. When they attempted to complete the treatment while also using bilateral ONB and general anesthesia, they were successful (15). In contrast to patients receiving ONB in addition to spinal anesthesia (6.6%), those receiving spinal anesthesia alone had a higher rate of obturator reflexes (83.3%). The combined group’s adductor reaction was barely noticeable (16). According to reports, the classic ONB method has a 50-91% success rate. Obese patients struggle to feel the pubis tubercle, which is the main problem (15). The inguinal approach of the ONB has reportedly less success with obese patients since it is difficult to locate or palpate surface markers due to the presence of dense adipose tissue (16). Furthermore, it requires a bigger needle, has technical problems, and is a disruptive process. The likelihood of problems could therefore increase as a result (3). As a result, the inguinal approach of ONB was praised as a novel, surface-level, and generally easier treatment with fewer complication rates (17). The major flaw in this approach is that it is unable to access the obturator nerve branches that originate in the hip joint fossa. The inguinal procedure, however, was reported in multiple studies to have higher success rates than the conventional approach (97.1% vs. 71.4%) due to less jerking of the limbs (3, 7, 18). A speedier block onset time was noted for the inguinal route by Aghamohammadi et al. (4). However, Moningi et al. (3) did not discover any statistically significant differences between the success rates of the two modalities. In our analysis, we had no failed blocks. We employed an LMA without a neuromuscular block on patients who had received general anesthesia. Although earlier studies (3), (15), and (19) advised the use of succinylcholine and tubocurarine to reduce adductor spasms while undergoing general anesthesia, subsequent studies produced inconsistent results and determined that these anesthetic medications were useless (2, 7, 14, 15). In TUR-BT procedures, spinal anesthesia has frequently been preferred over general anesthesia because most TUR-BT patients are older and have more comorbidities (20). In order to minimize intraoperative and postoperative complications, spinal anesthesia is preferred to general anaesthetic. Spinal anesthesia cannot be used to inhibit adductor spasms and the obturator reflex on its own (1). An unsatisfactory reaction to an obturator block administered during spinal anesthesia or general anesthesia with muscle relaxants may be caused by the presence of an auxiliary obturator nerve branch or the invasiveness of the tumor. In our study, ONB was carried out using a neural stimulator and Labat’s traditional method, and 95% of the patients in the general anesthesia group and 90% in the spinal anesthesia group had a satisfactory nerve block. Despite the fact that this strategy is the most common, prior studies have demonstrated that ONB success rates were equivalent when other approaches, such as intravesical, inguinal, or interadductor approaches, were used (3, 21). The intravesical approach has not been widely employed because it only had a 60% claimed success rate (21). Wassef et al. acknowledged the interadductor method as a more effective tactic (22). They claim that the traditional method had low patient satisfaction ratings, although we had no unfavorable experiences related to this during or after the traditional way. In our investigation, individuals did not suffer adductor muscular spasms, but the spinal anesthetic group showed reduced spasm with modest reactions. Our success rates with the combination method under both general anesthesia and spinal anesthesia were in line with previous research. Although predicting the incidence of adductor muscle spasm during TUR-BT is difficult due to anesthesia technique, surgical technique, and tumor localization, especially in cases of tumors localized in the inferolateral bladder wall, the higher rates of obturator reflex have been documented thus far (3). In this study, we looked at the efficacy of ONB given to TUR-BT patients before spinal or general anesthesia. Although there were no significant differences in adductor muscle spasm or surgeon satisfaction, the patients’ adductor responses were more severe in the combination spinal anesthetic group when adductor spasm occurred.
6. CONCLUSION
This study shows that, regardless of the size or number of tumors, full resection is made possible by spinal anesthesia combined with ONB or ONB with general anesthesia without a neuromuscular relaxant, which lowers the recurrence rate by preventing the obturator reflex during TUR-BT. Regular use of ONB combined with spinal anesthesia or general anesthesia without a neuromuscular blocker during such surgeries can improve oncological outcomes for patients, lower complication rates, and lengthen the time spent living without disease.
Author’s contribution:
All authors were involved in all steps of preparation this article. Final proofreading was made by the first author.
Conflict of interest:
None declared.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Mydlo JH, Weinstein R, Shah S, Solliday M, Macchia RJ. Longterm consequences from bladder perforation and/or violation in the presence of transitional cell carcinoma: results of a small series and a review of the literature. J Urol. 1999;161:1128e32. [PubMed] [Google Scholar]
- 2.Tatlisen A, Sofikerim M. Obturator nerve block and transurethral surgery for bladder cancer. Minerva Urol Nefrol. 2007;59:137–141. [PubMed] [Google Scholar]
- 3.Moningi S, Durga P, Ramachandran G, Murthy PV, Chilumala RR. Comparison of inguinal versus classic approach for obturator nerve block in patients undergoing transurethral resection of bladder tumors under spinal anesthesia. J Anaesthesiol Clin Pharmacol. 2014;30:41–45. doi: 10.4103/0970-9185.125702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prentiss RJ, Harvey GW, Bethard WF, Boatwright DE, Pennington RD. Massive adductor muscle contraction in transurethral surgery: cause and prevention; development of new electrical circuitry. Trans Am Assoc Genitourin Surg. 1965;56:64–72. [PubMed] [Google Scholar]
- 5.Atanassoff PG, Weiss BM, Brull SJ, Horst A, Kulling D, Stein R, Theiler I. Electromyographic comparison of obturator nerve block to three-in-one block. Anesth Analg. 1995;81:529–533. doi: 10.1097/00000539-199509000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Chen WM, Cheng CL, Yang CR, Chung V. Surgical tip to prevent bladder perforation during transurethral resection of bladder tumors. Urology. 2008;72:667–668. doi: 10.1016/j.urology.2008.04.042. [DOI] [PubMed] [Google Scholar]
- 7.Patel D, Shah B, Patel BM. Contribution of the obturator nerve block in the trans-urethral resection of bladder tumours. Indian J Anaesth. 2004;48:47–49. [Google Scholar]
- 8.Erbay G, Akyol F, Karabakan M, Celebi B, Keskin E, Hirik E. Effect of obturator nerve block during transurethral resection of lateral bladder wall tumors on the presence of detrusor muscle in tumor specimens and recurrence of the disease. Kaohsiung J Med Sci. 2017;33:86–90. doi: 10.1016/j.kjms.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Babjuk M, Oosterlinck W, Sylvester R, Kaasinen E, Bo¨hle A, Palou-Redorta J, et al. EAU guidelines on non-muscle invasive urothelial carcinoma of the bladder e the 2011 update. Eur Urol. 2011;59:997e1008. doi: 10.1016/j.eururo.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 10.Tekgu¨l ZT, Divrik RT, Turan M, Konyalio_glu E, S. ims.ek E, Go¨nu¨llu¨ M. Impact of obturator nerve block on the short-term recurrence of superficial bladder tumors on the lateral wall. Urol J. 2014;11:1248e52. [PubMed] [Google Scholar]
- 11.Thallaj A, Rabah D. Efficacy of ultrasound guided obturator nerve block in transurethral surgery. Saudi J Anaesth. 2011;5:42e4. doi: 10.4103/1658-354X.76507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen WM, Cheng CL, Yang CR, Chung V. Surgical tip to prevent bladder perforation during transurethral resection of bladder tumors. Urology. 2008;72:667e8. doi: 10.1016/j.urology.2008.04.042. [DOI] [PubMed] [Google Scholar]
- 13.Garci´La Rodri´Lguez J, Jalo´Monzo´n A, Gonza´lez Alvarez RC, Ardura Laso C, Ferna´Lndez Gomez JM, Rodri´Lguez Martinez JJ, et al. An alternative technique to prevent of obturator nerve stimulation during lateral bladder tumors transurethral resection. Actas Urol Esp. 2005;29:445e7. doi: 10.1016/s0210-4806(05)73273-3. [DOI] [PubMed] [Google Scholar]
- 14.Heywang-Kobrunner SH, Amaya B, Okoniewski M, Pickuth D, Spielmann RP. CT-guided obturator nerve block for diagnosis and treatment of painful conditions of the hip. Eur Radiol. 2001;11:1047–153. doi: 10.1007/s003300000682. [DOI] [PubMed] [Google Scholar]
- 15.So PC: Two case reports of obturator nerve block for transurethral resection of bladder tumour. Hong Kong Med J. 2004;10:57–59. [PubMed] [Google Scholar]
- 16.Darc.n K, Bengisun ZK, Ekmekci P, Hali.lo.lu AH, Suer AH. Obturator nerve block using levobupivacaine for the prevention of adductor spasm in transurethral bladder tumor resection. Turkiye Klinikleri J Med Sci. 2013;33:49–53. doi: 10.5336/medsci.2012-28161. [DOI] [Google Scholar]
- 17.Choquet O, Capdevila X, Bennourine K, Feugeas JL, Bringuier- Branchereau S, Manelli JC. A new inguinal approach for the obturator nerve block: anatomical and randomized clinical studies. Anesthesiology. 2005;103:1238–1245. doi: 10.1097/00000542-200512000-00020. [DOI] [PubMed] [Google Scholar]
- 18.Aghamohammadi D, Gargari RM, Fakhari S, Bilehjani E, Poorsadegh S. Classic versus inguinal approach for obturator nerve block in transurethral resection of bladder cancer under spinal anesthesia: a randomized controlled trial. Iran J Med Sci. 2018;43:75–80. [PMC free article] [PubMed] [Google Scholar]
- 19.Cesur M, Erdem AF, Alici HA, Yapanoglu T, Yuksek MS, Aksoy Y. The role of succinylcholine in the prevention of the obturator nerve reflex during transurethral resection of bladder tumors. Saudi Med J. 2008;29:668–671. [PubMed] [Google Scholar]
- 20.Fanelli G, Casati A, Garancini P, Torri G. Nerve stimulator and multiple injection technique for upper and lower limb blockade: failure rate, patient acceptance, and neurologic complications. Study Group on Regional Anesthesia. Anesth Analg. 1999;88:847–852. doi: 10.1097/00000539-199904000-00031. [DOI] [PubMed] [Google Scholar]
- 21.Khorrami MH, Javid A, Saryazdi H, Javid M. Transvesical blockade of the obturator nerve to prevent adductor contraction in transurethral bladder surgery. J Endourol. 2010;24:1651–1654. doi: 10.1089/end.2009.0659. [DOI] [PubMed] [Google Scholar]
- 22.Wassef MR. Interadductor approach to obturator nerve blockade for spastic conditions of adductor thigh muscles. Reg Anesth. 1993;18:13–17. [PubMed] [Google Scholar]


