Abstract
OBJECTIVE:
To identify potential differential changes in youth suicide deaths associated with the coronavirus disease (COVID-19) pandemic to better inform suicide prevention strategies.
METHODS:
This cross-sectional study analyzed national suicide data for US youth aged 5 to 24 years from 2015 to 2020. Annual and monthly numbers of suicides were extracted overall and by sex, age, race and ethnicity, and method. Expected suicides were modeled from the trend in monthly deaths before COVID-19 (January 1, 2015–February 29, 2020), by using interrupted time-series analyses with quasi-Poisson regression. Rate ratios (RR) and corresponding 95% confidence intervals (CI) were used to compare expected and observed suicides during the first 10 months of COVID-19 (March 1, 2020–December 31, 2020).
RESULTS:
Among 5568 identified youth suicides during the 2020 pandemic, 4408 (79.2%) were male, 1009 (18.1%) Hispanic, 170 (3.3%) non-Hispanic American Indian/Alaska Native, 262 (4.7%) Asian/Pacific Islander, 801 (14.4%) Black, and 3321 (59.6%) white. There was a significant increase in overall observed versus expected youth suicides during the COVID-19 pandemic (RR = 1.04, 95% CI = 1.01–1.07), equivalent to an estimated 212 excess deaths. Demographic subgroups including males (RR = 1.05, 95% CI = 1.02–1.08), youth aged 5 to 12 years (RR = 1.20, 95% CI = 1.03–1.41) and 18 to 24 years (RR = 1.05, 95% CI = 1.02–1.08), non-Hispanic AI/AN youth (RR = 1.20, 95% CI = 1.03–1.39), Black youth (RR = 1.20, 95% CI = 1.12–1.29), and youth who died by firearms (RR = 1.14, 95% CI = 1.10–1.19) experienced significantly more suicides than expected.
CONCLUSIONS:
Suicide deaths among US youth increased during COVID-19, with substantial variation by sex, age, race and ethnicity, and suicide method. Suicide prevention strategies must be tailored to better address disparities in youth suicide risk.
Youth suicide is a significant global public health problem and the second leading cause of death among 5- to 24-year-olds in the United States.1 Depression, anxiety, isolation, and decreased social support associated with the coronavirus disease 2019 (COVID-19) pandemic and related lockdowns have likely contributed to increased suicide risk in youth.2–5 Preliminary international data from 2020 suggest that suicide rates across the lifespan remained stable or may have slightly decreased early in the pandemic;6 however, a study comparing pre- and peri-pandemic monthly suicide rates in Japan later in the pandemic found rates to be rising in October and November of 2020, with the most significant increase among young adults.7
Importantly, the observed associations between the pandemic and suicide deaths may vary by race and ethnicity. A study comparing prepandemic and early pandemic suicide mortality in the state of Maryland found suicide deaths to be decreasing for white youth while doubling for Blacks,8 which is consistent with results of a Connecticut study that reported similar increases in the suicide rates among non-white individuals early in the pandemic.9 Although racial and ethnic differences in suicide rates have been consistently reported prepandemic,10–12 observed increases in suicide among non-white populations peri-pandemic appear to be disproportionate relative to expectations. To our knowledge, no national study has evaluated trends in youth suicide associated with COVID-19 using full-year and final 2020 mortality numbers, the most recent year for which data are available. The purpose of this study is to compare the overall observed suicide deaths in 5- to 24-year-old US youths during the first 10 months of COVID-19 (March 1, 2020–December 31, 2020) with expected numbers of suicide deaths before COVID-19 (January 1, 2015–February 29, 2020), and by demographic subgroup and suicide method.
METHODS
Data with suicide listed as the underlying cause of death among persons aged 5 to 24 years from 2015 to 2020 were obtained from the Web-based Wide-Ranging Online Data for Epidemiologic Research (WONDER) of the Centers for Disease Control and Prevention.13 Annual and monthly numbers of suicides were extracted overall and by sex, age, race and ethnicity, and suicide method. Suicide counts <10 are suppressed in WONDER for confidentiality reasons and excluded from analyses. Race and ethnicity was categorized on the basis of the Office of Management and Budget Standards for the Classification of Federal Data on Race and Ethnicity.14 Observed suicide deaths between March 1, 2020 to December 31, 2020 were compared to expected suicides from these same months both overall and by demographic subgroups.
Expected suicide deaths represent the number of monthly suicide deaths had the COVID-19 pandemic not occurred and were modeled from the trend in monthly youth suicide deaths before COVID-19 (January 1, 2015–February 29, 2020) by using interrupted time-series analyses with quasi-Poisson regression to account for overdispersion. March was treated as the start of COVID-19 because the World Health Organization declared COVID-19 a pandemic on March 11, 2020.15 Time was modeled as a quadratic predictor because it provided a better fit to the data than time modeled as a linear predictor; seasonal variation was modeled using harmonic functions of time. Rate ratios (RR) and 95% confidence intervals (CI) were used to compare expected and observed suicides during the COVID-19 period. This cross-sectional study was not considered human subjects research by the Nationwide Children’s Hospital institutional review board. Analyses were performed using Stata/IC Statistical Software, version 16.1(StataCorp).
RESULTS
Among 5568 American youth aged 5 to 24 years who died by suicide during the COVID-19 period in 2020, 4408 (79.2%) were male, 1009 (18.1%) Hispanic, 170 (3.1%) non-Hispanic American Indian/Alaska Native (AI/AN), 262 (4.7%) non-Hispanic Asian/Pacific Islander (A/PI), 801 (14.4%) non-Hispanic Black, and 3321 (59.6%) non-Hispanic white. The most common method of suicide was by firearm, 2843 (51.1%). During the COVID-19 period under study, there was a significant overall increase in observed versus expected youth suicide deaths (RR = 1.04, 95% CI = 1.01–1.07) (Fig 1); in absolute numbers, we estimated 212 (95% CI = 183–241) excess youth suicide deaths in association with the pandemic in 2020. The association between COVID-19 and youth suicide was not uniform across demographic subpopulations. Groups experiencing more suicide deaths than expected in the first 10 months of COVID-19 included males (RR = 1.05, 95% CI = 1.02–1.08), youth aged 5 to 12 years (preteens) (RR = 1.20, 95% CI = 1.03–1.41) and 18 to 24 years (young adults) (RR = 1.05, 95% CI = 1.02–1.08), non-Hispanic AI/AN youth (RR = 1.20, 95% CI = 1.03–1.39), and non-Hispanic Black youth (RR = 1.20, 95% CI = 1.12–1.29).
FIGURE 1.
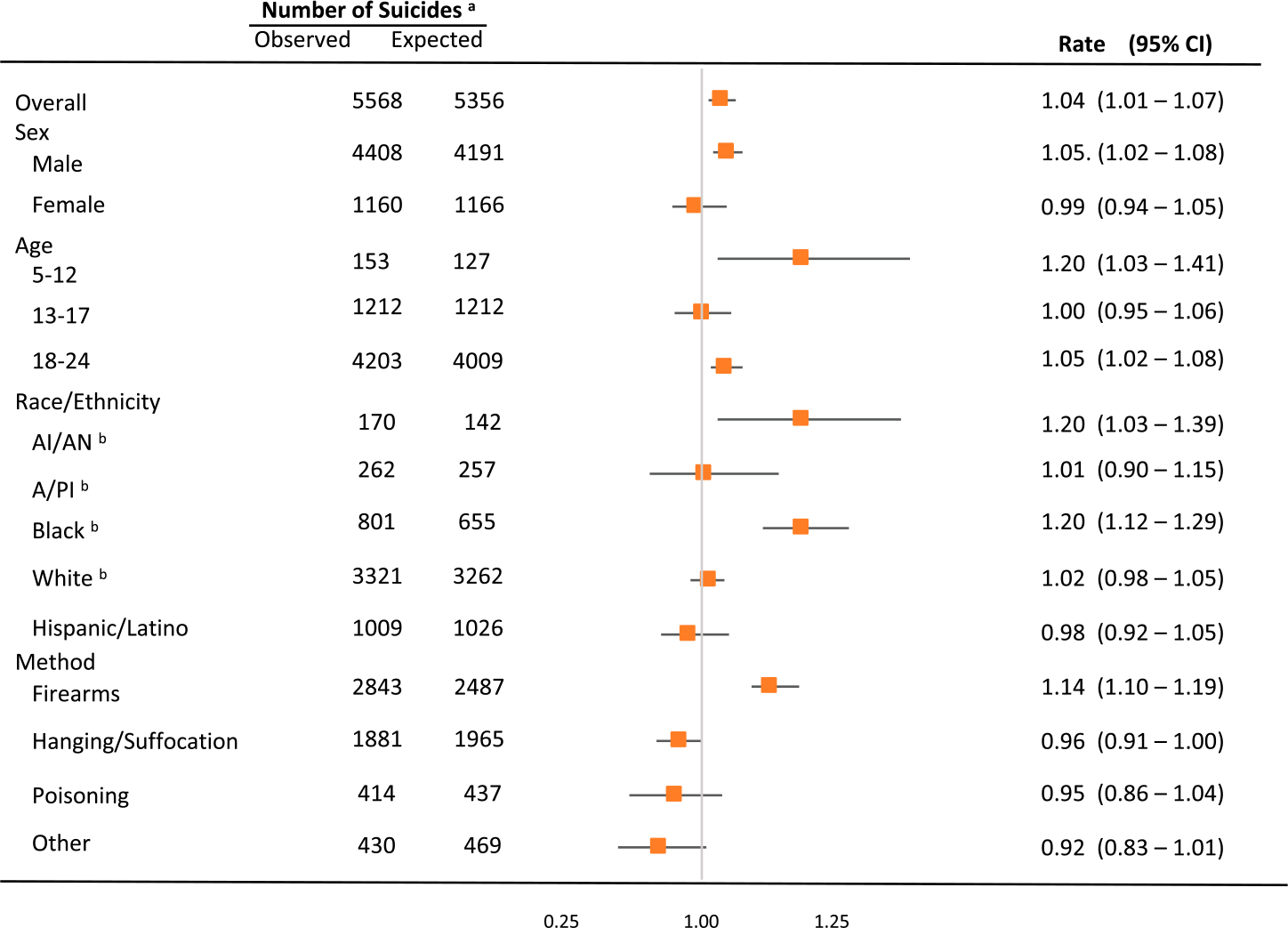
Observed and expected suicide deaths for the COVID-19 period from March 1, 2020 to December 31, 2020. aObserved and expected rates are reported for the COVID-19 period; however, expected rates were modeled from the trend in monthly suicide deaths before COVID-19 (January 1, 2015–February 29, 2002). bNon-Hispanic.
Suicide deaths by firearm were also higher than expected (RR = 1.14, 95% CI = 1.10–1.19). These findings were consistent for both females (RR = 1.21, 95% CI = 1.08–1.34) and males (RR = 1.14, 95% CI = 1.09–1.18), and in youth aged 5 to 12 (RR = 2.13, 95% CI = 1.61–2.80) and 18 to 24 years (RR = 1.17, 95% CI = 1.13–1.22) (Supplemental Table 2). Observed suicide deaths by firearm were also higher than expected among every racial and ethnic group except A/PI youth.
In stratified analyses (Table 1), excess suicide deaths were detected in non-Hispanic AI/AN males of all ages and 18- to 24-year-olds, non-Hispanic Black males of all ages and those aged 18 to 24 years, and non-Hispanic white 5- to 12-year-olds. Although there was no significant increase in suicide deaths noted for non-Hispanic A/PI youth in general, the largest increase in observed-to-expected suicides was found in non-Hispanic A/PI females (RR = 1.39, 95% CI = 1.12–1.73).
TABLE 1.
Observed and Expected Rates During the COVID-19 Period in the United States From March 1, 2020 to December 31, 2020 by Race and Ethnicity
| Observeda | Expecteda | Rate Ratio | 95% CI | |
|---|---|---|---|---|
|
| ||||
| American Indian or Alaska Nativeb | ||||
| Female | 43 | 43 | 1.00 | 0.74–1.35 |
| Male | 127 | 99 | 1.28 | 1.08–1.53 |
| 5–12c | — | — | — | — |
| 13–17 | 49 | 52 | 0.94 | 0.71–1.25 |
| 18–24 | 119 | 93 | 1.28 | 1.07–1.53 |
| Asian or Pacific Islanderb | ||||
| Female | 82 | 59 | 1.39 | 1.12–1.73 |
| Male | 180 | 201 | 0.90 | 0.77–1.04 |
| 5–12c | — | — | — | — |
| 13–17 | 58 | 60 | 0.97 | 0.75–1.25 |
| 18–24 | 199 | 183 | 1.09 | 0.95–1.25 |
| Blackb | ||||
| Female | 161 | 144 | 1.12 | 0.96–1.30 |
| Male | 640 | 521 | 1.23 | 1.14–1.33 |
| 5–12 | 34 | 27 | 1.26 | 0.90–1.76 |
| 13–17 | 133 | 136 | 0.98 | 0.83–1.16 |
| 18–24 | 634 | 501 | 1.27 | 1.17–1.37 |
| Whiteb | ||||
| Female | 647 | 691 | 0.94 | 0.87–1.01 |
| Male | 2674 | 2573 | 1.03 | 1.00–1.08 |
| 5–12 | 80 | 61 | 1.31 | 1.05–1.63 |
| 13–17 | 730 | 749 | 0.97 | 0.91 –1.05 |
| 18–24 | 2511 | 2453 | 1.02 | 0.98–1.06 |
| Hispanic | ||||
| Female | 226 | 231 | 0.98 | 0.86–1.11 |
| Male | 783 | 795 | 0.98 | 0.92–1.06 |
| 5–12 | 32 | 30 | 1.07 | 0.75–1.51 |
| 13–17 | 242 | 218 | 1.11 | 0.98–1.26 |
| 18–24 | 735 | 781 | 0.94 | 0.88–1.01 |
Observed and expected rates are reported for the COVID-19 period; however, expected rates were modeled from the trend in monthly suicide deaths before COVID-19 (January 1, 2015-February 29, 2020).
Non-Hispanic.
Data not reported given small or zero values.
—, not reported because there were 9 or fewer observed deaths.
Monthly observed versus expected number of suicides during the COVID-19 period for 2020 are shown in Figure 2 and Supplemental Tables 3 to 5. The overall number of observed suicide deaths was higher than expected in July (RR = 1.10, 95% CI = 1.02–1.20), August (RR = 1.09, 95% CI = 1.01–1.19), September (RR = 1.15, 95% CI = 1.07–1.25), and October (RR = 1.16, 95% CI = 1.07–1.25). This pattern of higher-than-expected monthly suicide deaths during mid- to late-2020 was observed in several subgroups, including males, youth aged 18 to 24 years, and youth who died by firearms. Among non-Hispanic Black youth, the observed versus expected suicide deaths were higher beginning in June and persisted through October. Lower-than-expected monthly suicide deaths were observed in the early pandemic for all females in May (RR = 0.75, 95% CI = 0.61–0.92) and December (RR = 0.79, 95% CI = 0.64–0.97), and among all 13- to 17-year-olds in March (RR = 0.76, 95% CI = 0.61–0.92), April (RR = 0.79, 95% CI = 0.65–0.95), and May (RR = 0.79, 95% CI = 0.65–0.97). When examining monthly deaths by method, observed deaths were higher than expected for firearms beginning in June (RR = 1.14, 95% CI = 1.01–1.28) through December (RR = 1.17, (1.04–1.32), except for the month of November. Monthly suicide deaths by hanging or suffocation were lower than expected in May (RR = 0.84, 95% CI = 0.73–0.98) and December (RR = 0.85, 95% CI = 0.72–0.98).
FIGURE 2.
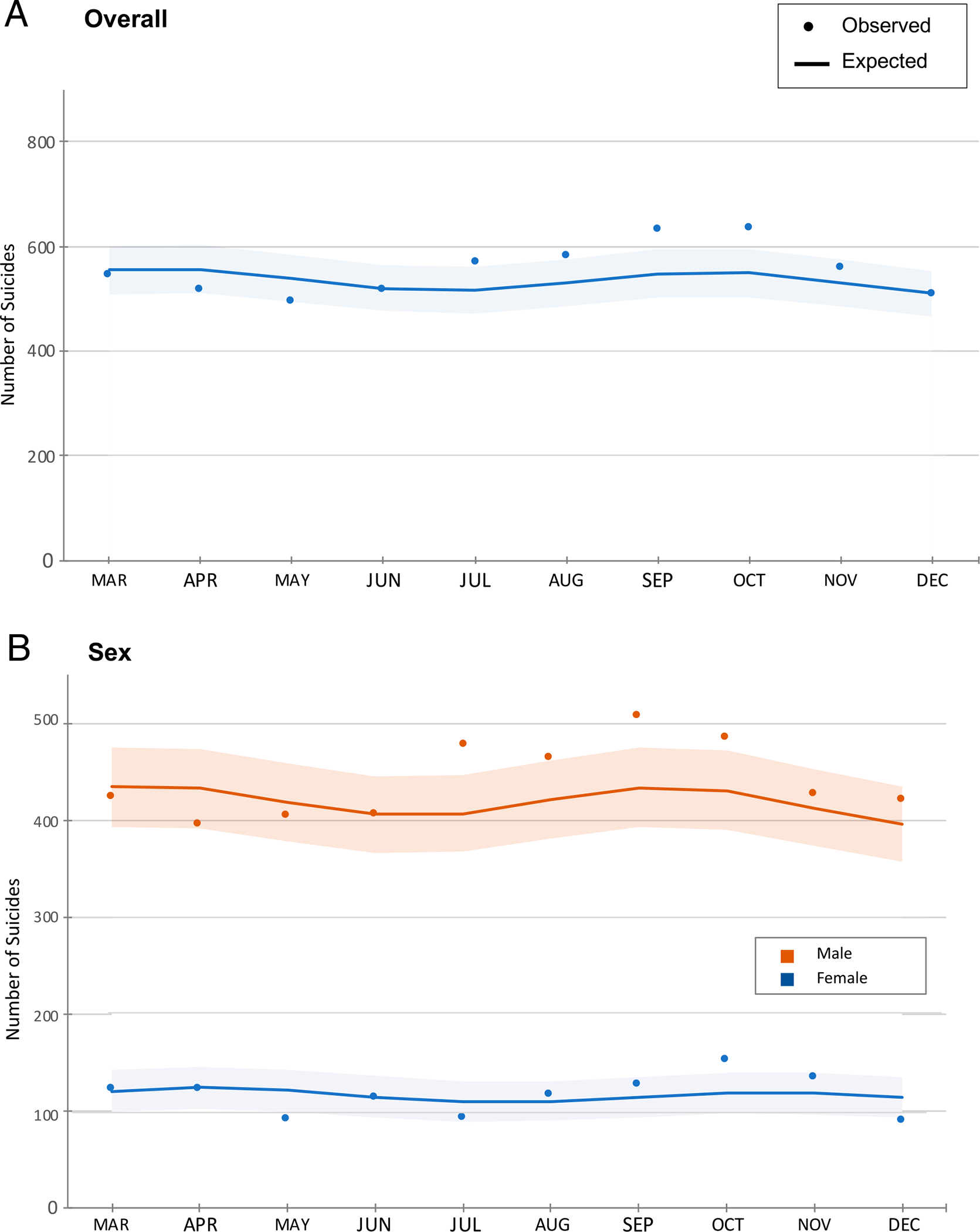
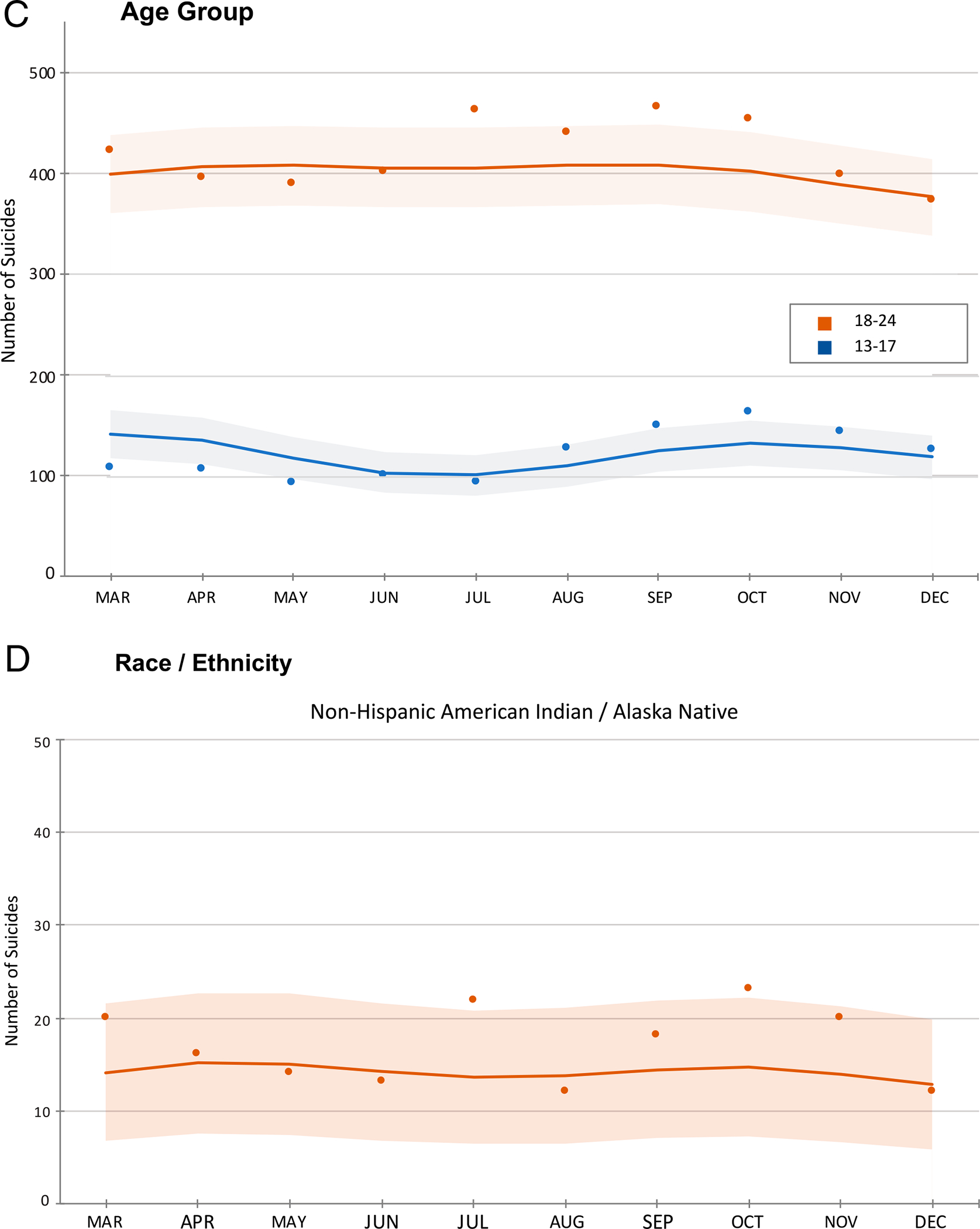
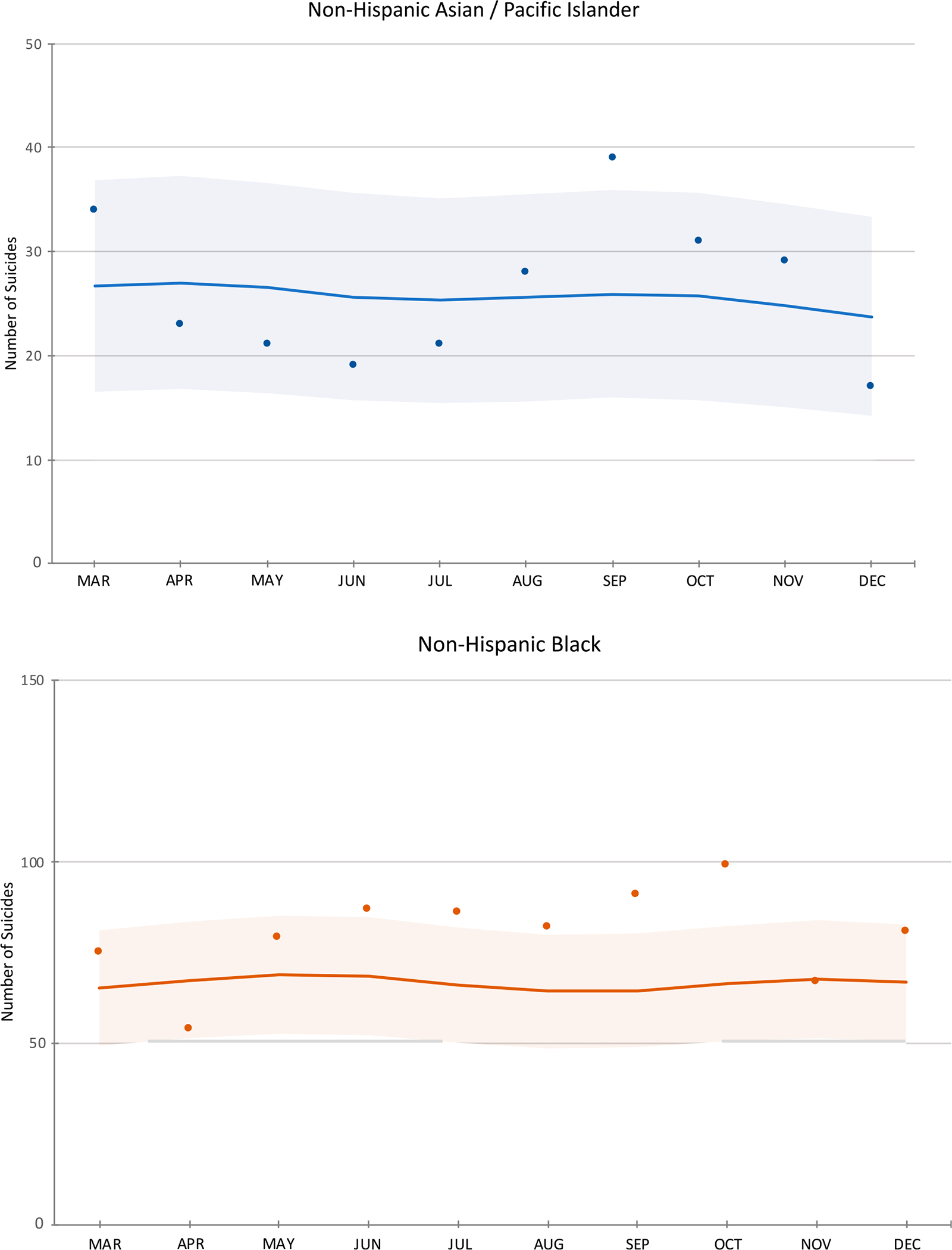
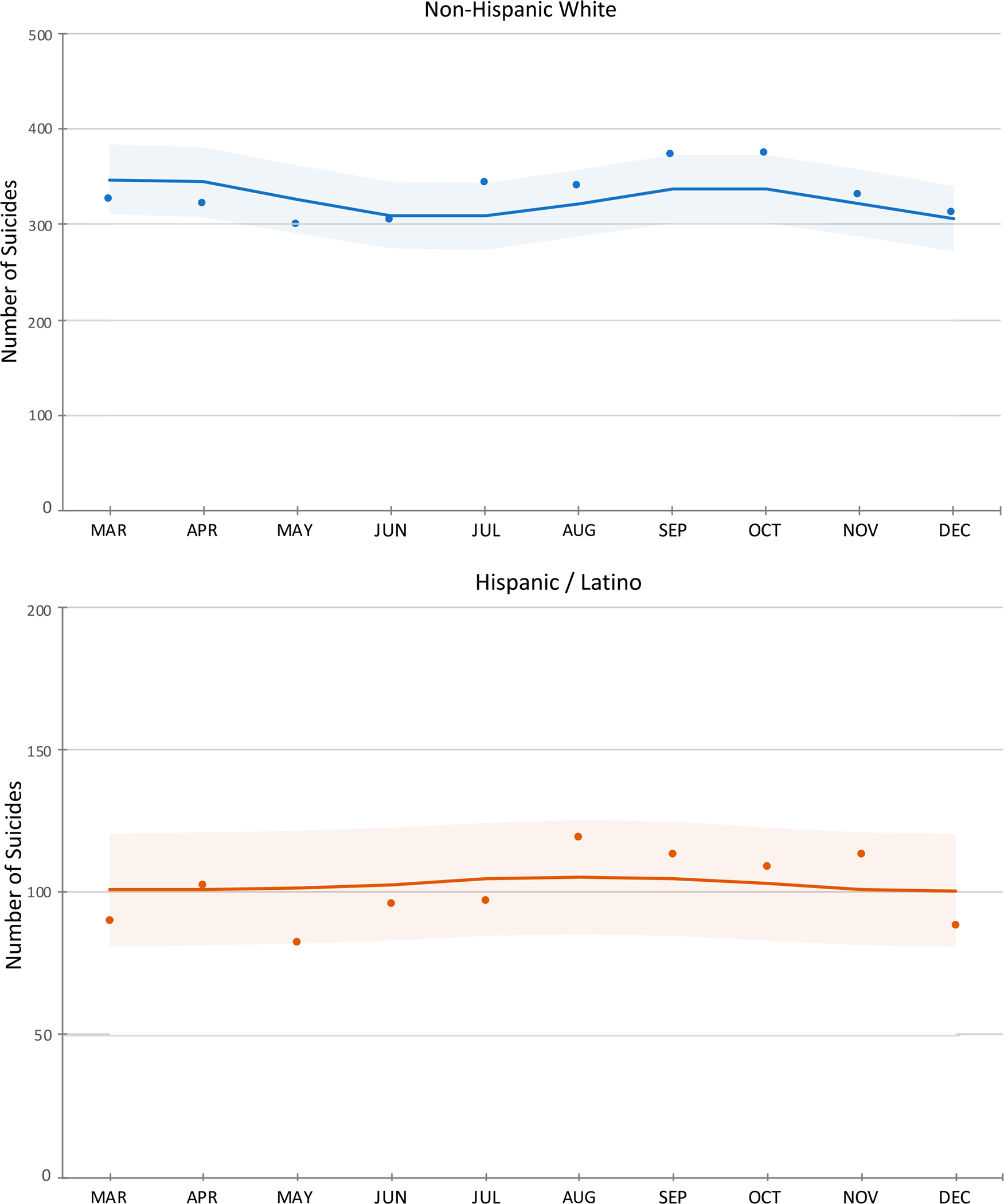
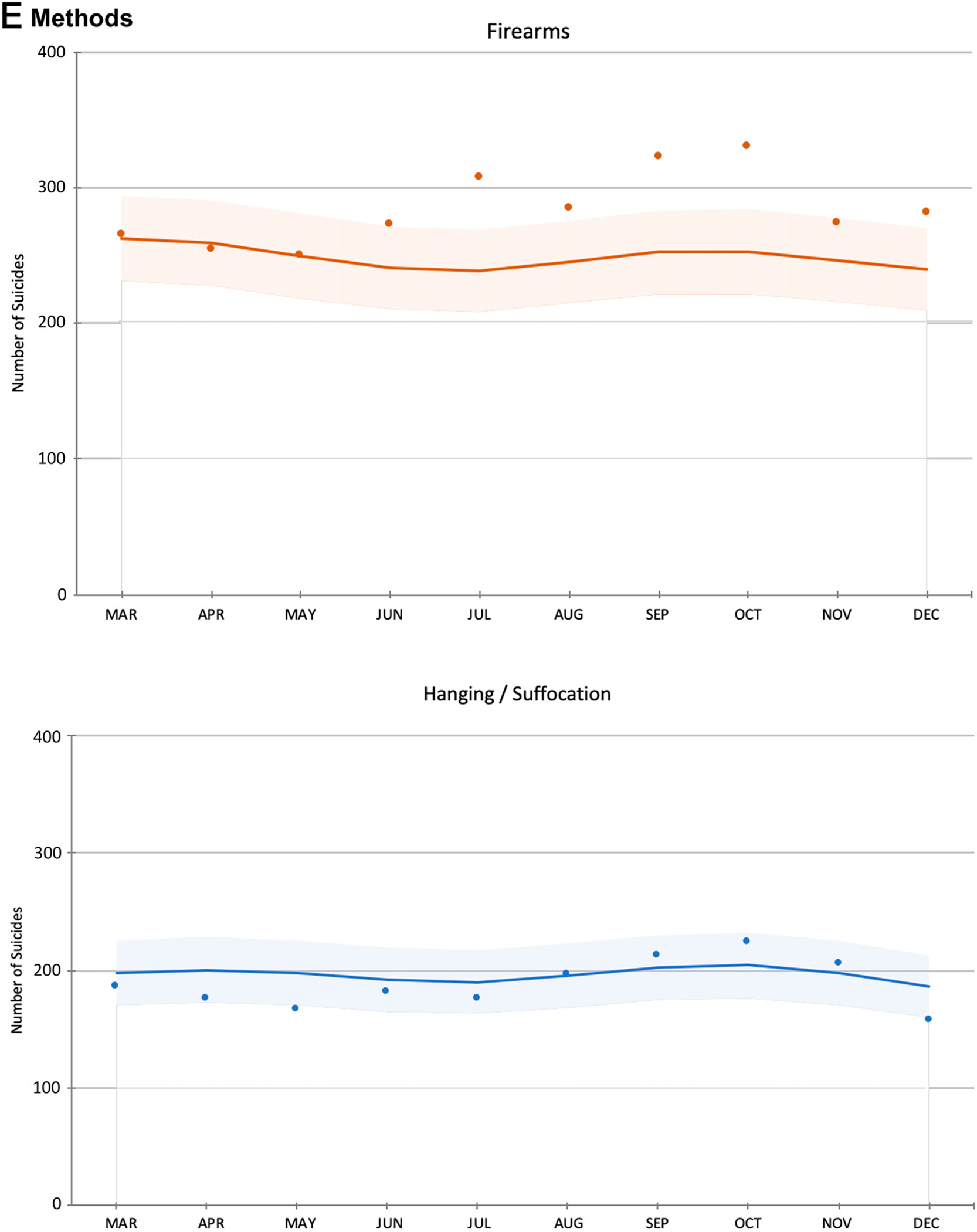
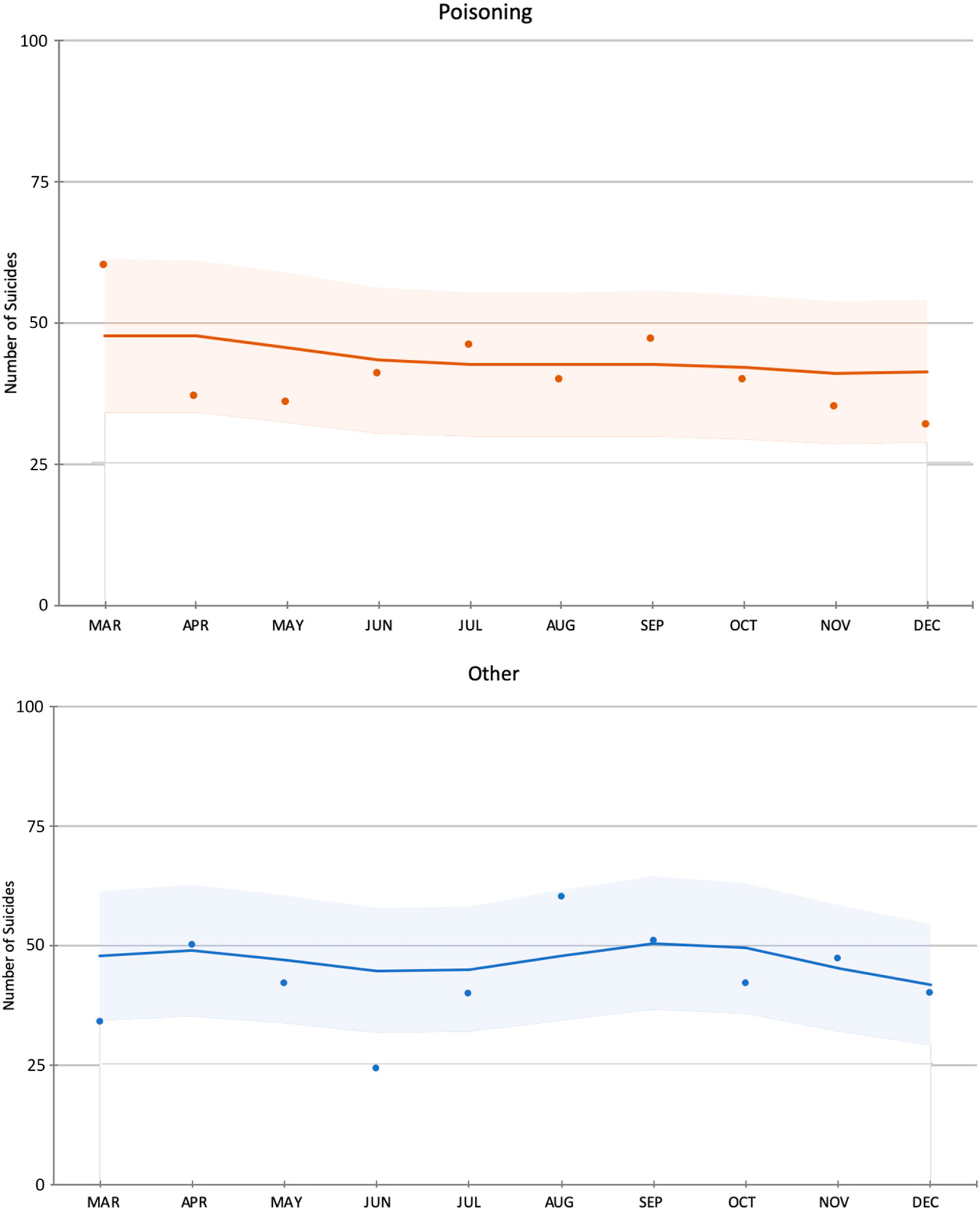
Observed and expected monthly suicide rates during the COVID-19 Period in the United States from March 1, 2020 to December 31, 2020. aObserved and expected rates are reported for the COVID-19 period; however, expected rates were modeled from the trend in monthly suicide deaths before COVID-19 (January 1, 2015–February 29, 2002). bShaded areas represent 95% confidence intervals for expected rates.
DISCUSSION
Findings from this national study suggest an overall increase in youth suicide deaths across the first 10 months of the COVID-19 pandemic. The association between the pandemic and increases in youth suicides varied significantly by sex, age, race or ethnicity, and suicide method. Variation across racial and ethnic groups was particularly striking, with non-Hispanic AI/AN and non-Hispanic Black youth experiencing significantly more suicide deaths than predicted. Sex and age differences were also significant but appeared to be largely driven by disparities within specific racial and ethnic subgroups. These findings provide further evidence of significant racial and ethnic disparities in suicide trends in association with the pandemic. Observed suicide eaths by firearm were also higher than expected. Analyses by month revealed a clear pattern of higher-than-expected overall suicide deaths beginning in July 2020, with no excess youth suicide deaths observed from March through May 2020.
Non-Hispanic AI/AN youth, a group with the highest suicide rate in the United States before COVID-19,16 experienced excess suicide mortality overall in males and 18 to 24-year-olds during the pandemic. Disproportionately high rates of COVID-19 observed in AI/AN communities have been associated with negative social (eg, community gatherings postponed), cultural (eg, inability to gather for ceremonies), and economic (eg, loss of tribal revenue to fund local services) consequences,17,18 with potential to increase AI/AN youth suicide rates during the study period. Lack of clinician cultural responsiveness, stigma, underresourced mental health care, and structural barriers to accessing services present significant and ongoing challenges to addressing mental health inequities in AI/AN communities.19 Avenues to address these persistent challenges include approaching mental health holistically (eg, using tribal values and traditional healing),20 prioritizing community-driven and culturally-tailored programs,20 increasing mental health workforce development within tribes and urban AI/AN populations,19,20 and promoting AI/AN health and well-being under federally guaranteed health care services for AI/AN communities.20
The largest observed-to-expected ratio of suicides during the COVID-19 period was detected among A/PI females. Suicide among A/PI youths has emerged as a significant public health issue. Since 2017, suicide has become the leading cause of death among Asian American youth aged 10 to 24 years,1 and the impact of COVID-19-related discrimination on mental health may underlie higher than expected suicide deaths among A/PI females. Discrimination including physical assaults against A/PI increased by 145% in 2020, with 8 of 10 A/PI youth reporting being bullied and 8% reporting physical attacks.21 A/PI female youths were particularly vulnerable being 2.5 times more likely to report hate incidents than A/PI youth males.21 Perceived COVID-19-related discrimination was also significantly associated with elevated posttraumatic stress disorder symptoms among Asian American young adults.22 A/PI women at high risk for suicide are vulnerable to suffering alone and underreporting symptoms of suicide, complicating identification and intervention efforts.23,24 A/PI women reported that a mismatch between cultural needs and available mental health services were primary reasons for not seeking mental health services.24
Among non-Hispanic Black youth, excess suicide mortality during the COVID-19 period was observed overall in males and 18- to 24-year-olds. Month-to-month analyses revealed higher-than-expected mortality beginning in June 2020 and extending through October. Although the increase in suicides may be influenced by factors specific to the pandemic, the potential impact of societal unrest because of the murder of George Floyd, an unarmed Black man on May 25, 2020, by a white police officer while in custody, must also be considered a potential contributor. The video of Mr Floyd’s death and subsequent public protests were widely shared around the world through multiple media outlets, and police-involved deaths of unarmed Black Americans are associated with adverse effects on mental health among other Black Americans in the United States.25 In a recent national survey, large increases in depression and anxiety in the week after Mr. Floyd’s murder compared to the 5 weeks before were seen in Black respondents, and the increases were significantly larger for Black Americans than for white Americans.26 Finally, Black youth, are less likely to seek help for depression, suicidal ideation, or suicide attempts than white youth, leading to a higher likelihood of undetected and untreated symptoms.27,28
A statistically significant increase in suicide was observed in non-Hispanic white 5 to 12-year-olds, with a 31% increase in suicide deaths over the number of expected suicide deaths during the COVID-19 period. Suicide rates in US preteens increased 135% between 2010 to 2019.1 Recognizing child suicide as an emerging public health problem,29 the National Institute of Mental Health convened a research roundtable series in 2021 to identify potential ways to mitigate child suicide risk by addressing key knowledge and research gaps.30
When examining suicide deaths by method, firearm deaths were significantly higher than expected across every demographic subgroup. Although the underpinnings of this striking finding are unclear, spending more time in the home rather than at school or interacting with peers may increase the relative likelihood of exposure to unsecured firearms. This observed increase in firearm-related youth suicide calls attention to the importance of securing firearms in homes and lethal means restriction in general. Our finding that females experienced greater than expected suicide deaths by firearms is consistent with previous research showing a shift among female youth to more lethal means.31,32 Given the existing gender paradox of suicidal behavior with females exhibiting higher rates of suicidal ideation or attempts, but being less likely to die by suicide,33 a sustained shift of female youth toward a highly lethal method such as firearms could have grave public health implications. Results further show that preteens experienced a twofold increase in observed versus expected suicide deaths by firearm. Finally, aligned with overall increased suicide deaths in AI/AN youth during the COVID-19 pandemic, the largest observed-to-expected ratio of suicide deaths by firearms was also identified in this racial group.
Consistent with previous international research,6,7 monthly suicide deaths remained stable or declined during the early pandemic months (March–May 2020), followed by increases from mid- to late-2020. Our analyses expand knowledge on suicide deaths during this COVID-19 period by using full-year final data on national suicide mortality in 2020. It will be important to continue to monitor trends in both youth suicide mortality and morbidity, such as pediatric emergency department presentations for mental health and suicidal behavior-related concerns.
Several clinical implications emerge from these findings. Screening for youth suicide risk as a public health prevention strategy for detection should be implemented and adopted more broadly, including in medical settings, schools, and other community-based settings that serve young people. Relatedly, clinicians should be trained in cultural literacy to better understand the cultural and socio-political contexts affecting their young patients, including broader assessment of cultural risk and protective processes that may impact a young person’s well-being such as intergenerational facilitators or barriers34 and individual experiences of discrimination and racism.35 Prioritizing community-based youth suicide prevention efforts like those supported by the Garrett Lee Smith Memorial Act are also critical.36,37
The pandemic has further highlighted racial and ethnic health disparities38 that may put already vulnerable youth at higher risk for suicidal behavior, emphasizing the need to address equity in health care access for disadvantaged communities. A shift to telehealth during the pandemic has been effective for a variety of outpatient services27,28 and may be a more permanent approach for increasing access to mental health care in underserved populations. Expanding telehealth technologies including broadband internet access and telehealth hardware are necessary to remedy the “digital divide” observed in the United States39 and has strong potential to reduce barriers to needed care for underserved youth.40 Additional online and digital interventions provide further strategies for improving health care access, and the full potential of these options should be explored as potential treatment solutions.41,42 Culturally adapted mental health services have proven efficacy43 and should be incorporated into suicide prevention strategies. Preventative interventions such as the American Indian Life Skills curriculum, Asian Women’s Action for Resilience and Empowerment, and the Adapted-Coping With Stress program for Black adolescents that are responsive to local contexts and cultural implications, while also engaging community members in the intervention approach, show promising results.44–47
School settings can play an important role in suicide prevention by providing age-appropriate programs that reach a large and diverse number of youth. Although the impact of school closures on youth suicide risk during the COVID-19 pandemic is unclear, racial and ethnic disparities in access to in-person instruction have been documented during the pandemic, and the lack of live instruction has been associated with impaired academic progress, decreased physical activity, lower levels of social and emotional support, and greater emotional distress and exposure to in-home conflict.48 Strong evidence exists for the effectiveness of school-based suicide prevention programs to increase mental health literacy, enhance awareness about suicide risk, and to decrease the incidence of suicide attempts and suicidal ideation.49–51 Opportunities exist to continue adapting these programs to broaden their reach with on-line modes of instruction and delivery.
Family-based interventions are also shown to be impactful in reducing youth suicide risk.52,53 One program, the Family Intervention for Suicide Prevention/Safety-Acute, is a cognitive-behavioral intervention for youth and parents or caregivers designed to decrease the risk of youth suicidal ideation and behavior.53 The Family-Based Crisis Intervention54 is an additional empirically supported family therapy model focused on improving interpersonal family relations associated with depression and the risk for suicide. Lastly, our finding that suicide deaths by firearms were significantly higher than expected during the pandemic underscores the importance of lethal means restriction interventions including educational programs,55 youth-focused firearm laws,56 and safe firearm storage public awareness campaigns.57 Additional research is needed to identify the specific COVID-19-related factors that have contributed to observed disparities in youth suicide during this period, namely the role of social distancing and isolation, school closures, interpersonal loss, lack of exercise, changes in use of social media or internet access, and interactional effects of poverty and trauma. A recent US Surgeon General’s Advisory provides further research recommendations to effectively respond to the pandemic’s impact on the mental health of the nation’s youth.58 A Justice, Equity, Diversity, and Inclusion–informed framework applied to the study and prevention of youth suicide also offers a promising approach to achieving health equity and reducing suicide risk for all youth.59,60 Examining geographic variations in youth suicide during the COVID-19 pandemic is another important opportunity for future research, and a comparative analysis across subgroups may also shed perspective on this study’s findings.
This study has several limitations. First, as discussed above, there may have been other events or unmeasured factors that occurred during the COVID-19 period that increased risk for suicide in US youth. Second, the study cannot identify causes or mechanisms underlying the observed increases in youth suicides during the pandemic. Third, the COVID-19 observation period was limited to 10 months in 2020, and final national mortality data for 2021 will not be available until late 2022. Ongoing surveillance is needed to monitor longer-term trends. Fourth, observed suicide deaths in this study are likely an underestimate among youth because of racial and ethnic misclassification that limits accuracy in suicide mortality data.61 Further, these data are not disaggregated to address racial and ethnic within-group variations or multiracial and mixed heritage youth, potentially limiting our knowledge of specific suicide trends to inform local prevention efforts. Finally, information on certain subcategories were excluded given small cell counts that are suppressed in WONDER.
CONCLUSIONS
Suicide deaths among US youth increased overall during the COVID-19 pandemic, with substantial variation in demographic subgroups. Significant racial or ethnic disparities continue to be uncovered among marginalized and understudied youth populations. An increase in suicide by firearms also draws attention to the continuing need to promote safe gun storage practices. Findings highlight the need to identify potential mechanisms underlying differential increases in youth suicide deaths associated with the pandemic and to develop broadened and more effective suicide preventive interventions tailored to better address racial and ethnic disparities in youth at highest risk for suicide. Additionally, preteen rates of suicide are increasing warranting further research and clinical attention for this understudied subpopulation at risk. Future research is needed to understand the impact of racial and ethnic disparities62 on emotional and mental health of young people, and to monitor longer-term trends of COVID-19-related suicide morbidity and mortality.
Supplementary Material
WHAT’S KNOWN ON THIS SUBJECT:
Suicide is a leading cause of death among youth in the United States. Evidence suggests the coronavirus disease (COVID-19) pandemic may have exacerbated the problem of youth suicide, particularly in demographic subgroups.
WHAT THIS STUDY ADDS:
This study estimates national trends in youth suicide associated with COVID-19 by using full-year 2020 mortality numbers. Findings highlight the need for prevention strategies that address developmental and racial and ethnic disparities in youth at elevated risk for suicide.
ABBREVIATIONS
- AI/AN
American Indian/Alaska Native
- A/PI
Asian/Pacific Islander
- CI
confidence interval
- COVID-19
coronavirus disease 2019
- WONDER
Web-based Wide-Ranging Online Data for Epidemiologic Research
- RR
rate ratio
Footnotes
CONFLICT OF INTEREST DISCLOSURES: Drs Bridge, Ruch, Sheftall, Fontanella, Brock, and Campo receive funding from the National Institute of Mental Health (NIMH), National Institutes of Health. Dr Bridge also receives research grant funding from the Patient-Centered Outcomes Research Institute (PCORI) and the Centers for Disease Control and Prevention (CDC); he is also a member of the Scientific Advisory Board of Clarigent Health. Dr O’Keefe was supported by grant 1K01MH122702 from the National Institute of Mental Health (NIMH), National Institutes of Health. Dr Sheftall also receives research grant funding from the American Foundation for Suicide Prevention (AFSP). No financial disclosures were reported by the other authors of this paper.
REFERENCES
- 1.Centers for Disease Control and Prevention. WISQARS Leading Causes of Death Reports, National and Regional, 2019. Data Source: National Center for Health Statistics (NCHS), National Vital Statistics System. Accessed January 13, 2022. [Google Scholar]
- 2.Hawes MT, Szenczy AK, Olino TM, Nelson BD, Klein DN. Trajectories of depression, anxiety and pandemic experiences; A longitudinal study of youth in New York during the Spring-Summer of 2020. Psychiatry Res. 2021;298:113778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175(11):1142–1150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ridout KK, Alavi M, Ridout SJ, et al. Emergency department encounters among youth with suicidal thoughts or behaviors during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(12):1319–1328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021;147(3):e2020029280. [DOI] [PubMed] [Google Scholar]
- 6.Pirkis J, John A, Shin S, et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8(7):579–588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sakamoto H, Ishikane M, Ghaznavi C, Ueda P. Assessment of suicide in Japan during the COVID-19 pandemic vs previous years. JAMA Netw Open. 2021;4(2):e2037378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bray MJC, Daneshvari NO, Radhakrishnan I, et al. Racial differences in statewide suicide mortality trends in Maryland during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Psychiatry. 2021;78(4):444–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell TO, Li L. State-level data on suicide mortality during COVID-19 quarantine: early evidence of a disproportionate impact on racial minorities. Psychiatry Res. 2021;295:113629. [DOI] [PubMed] [Google Scholar]
- 10.Xiao Y, Cerel J, Mann JJ. Temporal trends in suicidal ideation and attempts among US adolescents by sex and race/ethnicity, 1991–2019. JAMA Netw Open. 2021;4(6):e2113513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindsey MA, Sheftall AH, Xiao Y, Joe S. Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics. 2019;144(5):e20191187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bridge JA, Horowitz LM, Fontanella CA, et al. Age-related racial disparity in suicide rates among US youths from 2001 through 2015. JAMA Pediatr. 2018;172(7):697–699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC WONDER. Annual and Monthly Underlying Cause of Death data produced by the Mortality Statistics Branch, Division of Vital Statistics, National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention (CDC), United States Department of Health and Human Services (US DHHS); 2015–2020. Published 2021. Accessed January 2-11, 2022 [Google Scholar]
- 14.Office of Management and Budget. Revisions to the standards for the classification of federal data on race and ethnicity. Fed Regist. 1997;62:58781–58790 [Google Scholar]
- 15.World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 - March 11, 2020; Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19–11-march-2020. Published March 11, 2020. Accessed January 13, 2021
- 16.Cha CB, Franz PJ, M Guzmán E, Glenn CR, Kleiman EM, Nock MK. Annual Research Review: Suicide among youth - epidemiology, (potential) etiology, and treatment. J Child Psychol Psychiatry. 2018;59(4):460–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.John Hopkins University. New data shows COVID-19’s disproportionate impact on American Indian, Alaska Native tribes. Available at: https://hub.jhu.edu/2021/10/11/map-covid-19-impact-american-indian-population/. Accessed January 24, 2022 [Google Scholar]
- 18.Owen MJ, Sundberg MA, Dionne J, Kosobuski AW. The impact of COVID-19 on American Indian and Alaska Native communities: a call for better relational models. Am J Public Health. 2021;111(5):801–803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Keefe VM, Cwik MF, Haroz EE, Barlow A. Increasing culturally responsive care and mental health equity with indigenous community mental health workers. Psychol Serv. 2021;18(1):84–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Substance Abuse and Mental Health Services Administration (SAMHSA). The National Tribal Behavioral Health Agenda. Available at: https://store.samhsa.gov/product/The-National-Tribal-Behavioral-Health-Agenda/PEP16-NTBH-AGENDA. Accessed February 1, 2022
- 21.Center for the Study of Hate & Extremism. FACT SHEET: Anti-Asian prejudice March 2021: anti-Asian hate crime reported to police in America’s largest cities: 2019 & 2020. Available at: https://www.csusb.edu/sites/default/files/FACT%20SHEET-%20Anti-Asian%20Hate%202020%20rev%203.21.21.pdf. Accessed February 2, 2022
- 22.Hahm HC, Ha Y, Scott JC, Wongchai V, Chen JA, Liu CH. Perceived COVID-19-related anti-Asian discrimination predicts post traumatic stress disorder symptoms among Asian and Asian American young adults. Psychiatry Res. 2021;303:114084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.NYU School of Medicine. Center for the Study of Asian American Health. Asian Americans in the U.S. Available at: https://med.nyu.edu/asian-health/about-us/asian-americans-us. Accessed February 3, 2022 [Google Scholar]
- 24.Augsberger A, Yeung A, Dougher M, Hahm HC. Factors influencing the underutilization of mental health services among Asian American women with a history of depression and suicide. BMC Health Serv Res. 2015;15:542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bor J, Venkataramani AS, Williams DR, Tsai AC. Police killings and their spillover effects on the mental health of black Americans: a population-based, quasi-experimental study. Lancet. 2018;392(10144):302–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eichstaedt JC, Sherman GT, Giorgi S, et al. The emotional and mental health impact of the murder of George Floyd on the US population. Proc Natl Acad Sci USA. 2021;118(39):e2109139118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freedenthal S Racial disparities in mental health service use by adolescents who thought about or attempted suicide. Suicide Life Threat Behav. 2007;37(1):22–34 [DOI] [PubMed] [Google Scholar]
- 28.Aseltine RH Jr, DeMartino R. An outcome evaluation of the SOS Suicide Prevention Program. Am J Public Health. 2004;94(3):446–451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ayer L, Colpe L, Pearson J, Rooney M, Murphy E. Advancing research in child suicide: a call to action. J Am Acad Child Adolesc Psychiatry. 2020;59(9):1028–1035 [DOI] [PubMed] [Google Scholar]
- 30.National Institute of Mental Health. Understanding suicide risk among children and pre-teens: a synthesis workshop. Available at: https://www.nimh.nih.gov/news/events/2021/understanding-suicide-risk-among-children-and-pre-teens-a-synthesis-workshop. Accessed February 5, 2022
- 31.Bridge JA, Greenhouse JB, Sheftall AH, Fabio A, Campo JV, Kelleher KJ. Changes in suicide rates by hanging and/or suffocation and firearms among young persons aged 10–24 years in the United States: 1992–2006. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2010;46(5):503–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ruch DA, Sheftall AH, Schlagbaum P, Rausch J, Campo JV, Bridge JA. Trends in suicide among youth aged 10 to 19 years in the United States, 1975 to 2016. JAMA Netw Open. 2019;2(5):e193886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schrijvers DL, Bollen J, Sabbe BG. The gender paradox in suicidal behavior and its impact on the suicidal process. J Affect Disord. 2012;138(1–2):19–26 [DOI] [PubMed] [Google Scholar]
- 34.Wyatt LC, Ung T, Park R, Kwon SC, Trinh-Shevrin C. Risk factors of suicide and depression among Asian American, Native Hawaiian, and Pacific Islander youth: a systematic literature review. J Health Care Poor Underserved. 2015;26(2 Suppl):191–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meza JI, Bath E. One size does not fit all: making suicide prevention and interventions equitable for our increasingly diverse communities. J Am Acad Child Adolesc Psychiatry. 2021;60(2):209–212 [DOI] [PubMed] [Google Scholar]
- 36.Godoy Garraza L, Kuiper N, Goldston D, McKeon R, Walrath C. Long-term impact of the Garrett Lee Smith Youth Suicide Prevention Program on youth suicide mortality, 2006–2015. J Child Psychol Psychiatry. 2019;60(10):1142–1147 [DOI] [PubMed] [Google Scholar]
- 37.Godoy Garraza L, Walrath C, Goldston DB, Reid H, McKeon R. Effect of the Garrett Lee Smith Memorial Suicide Prevention Program on suicide attempts among youths. JAMA Psychiatry. 2015;72(11):1143–1149 [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. COVID-19 death data and resources. National Center for Health Statistics. Available at: https://www.cdc.gov/nchs/nvss/covid-19.htm. Accessed January 15, 2022 [Google Scholar]
- 39.Pew Research Center. The Internet and the pandemic. Available at: https://www.pewresearch.org/internet/2021/09/01/the-internet-and-the-pandemic/. Accessed February 3, 2022
- 40.National Congress of American Indians. U.S. Commission on Civil Rights Hearing on COVID-19 in Indian Country: The impact of federal broken promises on Native Americans, written testimony of President Fawn Sharp National Congress of American Indians, July 17, 2020. Available at: https://www.ncai.org/attachments/Testimonial_DZsioKxiANtlqzyGvRcGDaWpLsbZjlzhnmJpREpHubPVEyMOlYO_NCAI-Written-Testimony-USCCR%207_17_20-Hearing.pdf. Accessed February 3, 2022
- 41.Schleider JL, Mullarkey MC, Fox KR, et al. A randomized trial of online single-session interventions for adolescent depression during COVID-19. Nat Hum Behav. 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Torous J, J€an Myrick K, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment Health. 2020;7(3):e18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Soto A, Smith TB, Griner D, Domenech Rodríguez M, Bernal G. Cultural adaptations and therapist multicultural competence: Two meta-analytic reviews. J Clin Psychol. 2018;74(11):1907–1923 [DOI] [PubMed] [Google Scholar]
- 44.Hahm HC, Liu CH, Tompson MC. Cultural and developmental principles for Asian American women’s mental health: lessons from AWARE on college campuses. Psychiatr Serv. 2020;71(11):1199–1202 [DOI] [PubMed] [Google Scholar]
- 45.Hahm HC, Zhou L, Lee C, Maru M, Petersen JM, Kolaczyk ED. Feasibility, preliminary efficacy, and safety of a randomized clinical trial for Asian Women’s Action for Resilience and Empowerment (AWARE) intervention. Am J Orthopsychiatry. 2019;89(4):462–474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Robinson WL, Case MH, Whipple CR, et al. Culturally grounded stress reduction and suicide prevention for African American adolescents. Pract Innov (Wash D C) 2016;1(2):117–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.LaFromboise TD, Malik SS. A culturally informed approach to American Indian/Alaska Native youth suicide prevention. In: Zane NW, Bernal G, Leong FT, eds. Evidence-Based Psychological Practice With Ethnic Minorities: Culturally Informed Research and Clinical Strategies. American Psychological Association; 2016 [Google Scholar]
- 48.Parolin Z, Lee EK. Large socio-economic, geographic and demographic disparities exist in exposure to school closures. Nat Hum Behav. 2021;5(4):522–528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robinson J, Cox G, Malone A, et al. A systematic review of school-based interventions aimed at preventing, treating, and responding to suicide- related behavior in young people. Crisis. 2013;34(3):164–182 [DOI] [PubMed] [Google Scholar]
- 50.Wasserman D, Hoven CW, Wasserman C, et al. School-based suicide prevention programmes: the SEYLE cluster-randomised, controlled trial. Lancet. 2015;385(9977):1536–1544 [DOI] [PubMed] [Google Scholar]
- 51.Katz C, Bolton SL, Katz LY, Isaak C, Tilston-Jones T, Sareen J; Swampy Cree Suicide Prevention Team. A systematic review of school-based suicide prevention programs. Depress Anxiety. 2013;30(10):1030–1045 [DOI] [PubMed] [Google Scholar]
- 52.Reider EE, Sims BE. Family-based preventive interventions: can the onset of suicidal ideation and behavior be prevented? Suicide Life Threat Behav. 2016;46(Suppl 1 Suppl 1):S3–S7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Asarnow JR, Baraff LJ, Berk M, et al. An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatr Serv. 2011;62(11):1303–1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wharff EA, Ginnis KB, Ross AM, White EM, White MT, Forbes PW. Family-based crisis intervention with suicidal adolescents: a randomized clinical trial. Pediatr Emerg Care. 2019;35(3):170–175 [DOI] [PubMed] [Google Scholar]
- 55.Suicide Prevention Resource Center (SPRS). CALM: Counseling on access to lethal means. Available at: https://www.sprc.org/resources-programs/calm-counseling-access-lethal-means. Accessed October 5, 2022
- 56.Webster DW, Vernick JS, Zeoli AM, Manganello JA. Association between youth-focused firearm laws and youth suicides. JAMA. 2004;292(5):594–601 [DOI] [PubMed] [Google Scholar]
- 57.The Advertising Council Inc. Safety: gun safety - the end family fire campaign. Available at: https://www.adcouncil.org/campaign/gun-safety. Accessed October 5, 2022
- 58.US Department of Health and Human Services. U.S. Surgeon General issues advisory on youth mental health crisis further exposed by COVID-19 pandemic. Available at: https://www.hhs.gov/about/news/2021/12/07/us-surgeon-general-issues-advisory-on-youth-mental-health-crisis-further-exposed-by-covid-19-pandemic.html. Accessed February 5, 2022
- 59.Bath E, Njoroge WFM. Coloring outside the lines: making Black and Brown lives matter in the prevention of youth suicide. J Am Acad Child Adolesc Psychiatry. 2021;60(1):17–21 [DOI] [PubMed] [Google Scholar]
- 60.Marraccini ME, Lindsay CA, Griffin D, Greene MJ, Simmons KT, Ingram KM. A Trauma-and Justice, Equity, Diversity, and Inclusion (JEDI)-informed approach to suicide prevention in school: Black boys’ lives matter. School Psych Rev. 2021;25(Nov):1–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Herne MA, Bartholomew ML, Weahkee RL. Suicide mortality among American Indians and Alaska Natives, 1999–2009. Am J Public Health. 2014;104(Suppl 3 Suppl 3):S336–S342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee S, Waters SF. Asians and Asian Americans’ experiences of racial discrimination during the COVID-19 pandemic: impacts on health outcomes and the buffering role of social support. Stigma Health. 2021;6(1):70–78 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


