Abstract
Objective:
There is support for the use of mindfulness-based approaches with trauma-exposed adults. However, limited data are available on feasibility and acceptability of group-based mindfulness interventions in urban medical clinics serving primarily Black adults with low socioeconomic resources, where rates of trauma exposure are high. The present randomized pilot study evaluated the feasibility and acceptability of an 8-week adapted mindfulness-based cognitive therapy (MBCT) group for trauma-exposed Black adults who screened positive for posttraumatic stress disorder (PTSD) and depression in an urban primary care clinic setting.
Methods:
Participants were randomized to waitlist control (WLC) or MBCT. Feasibility and acceptability were assessed through examination of retention rates, measures of group satisfaction and treatment barriers, and qualitative interview. Forty-two Black adults (85% women) were consented; of those, 34 (81%) completed pre-assessment and randomization.
Results:
Feasibility of study design was shown, with >75% (n=26) of randomized participants completing the study through post-assessment. Twenty-four individuals (70.5%) completed through 1-month follow-up. Results showed high levels of group acceptability across quantitative and qualitative measures. Perceived barriers to psychological treatment were high, with an average of >6 barriers present.
Conclusions:
The findings indicate feasibility and acceptability of MBCT group interventions in urban primary care settings with trauma-exposed patients with significant psychopathology. However, substantial barriers to treatment engagement were endorsed and to improve numbers for successful engagement in the intervention, continued efforts to reduce treatment barriers and increase access to mindfulness-based interventions in under-resourced communities are needed.
Keywords: trauma, posttraumatic stress disorder, depression, mindfulness, urban settings
Black adults in urban areas experience high levels of chronic trauma exposure, which increases their risk for posttraumatic stress disorder (PTSD) and major depressive disorder (MDD) (Gluck et al., 2021). Rates as high as 50% for these disorders are observed among low-income, urban-dwelling Black adults, and up to half of these individuals meet criteria for both disorders (Golin et al., 2016). Heightened exposure to trauma in these communities occurs in the context of racial stress and marginalization (Sibrava et al., 2019). Because chronic trauma exposure increases the risk of PTSD and MDD, it is critical to intervene with underserved populations to mitigate the risk for these and other psychiatric disorders.
Individuals exposed to chronic trauma may be less likely than those with a discrete trauma exposure to benefit from standard trauma-focused treatment for PTSD (Cloitre et al., 2016). There are also limitations to first line cognitive behavioral therapies, such as Prolonged Exposure and Cognitive Processing Therapy, including low tolerability for patients with chronic trauma exposure, high rates of dropout, and persistence of PTSD symptoms (Orsillo & Batten, 2005; Resick et al., 2002). In addition, comorbid MDD increases risk of dropout from trauma-focused treatment (Flory & Yehuda, 2015). Since MDD and PTSD have a bidirectional influence in the context of chronic trauma exposure and co-occur at high rates (Horesh et al., 2017), it is necessary to focus on treatments that target both disorders. Considering the limitations of trauma-focused treatments, finding alternative and enhancing approaches that address transdiagnostic factors in the context of trauma is critical to increasing treatment access and effectiveness in low-income Black urban communities.
One contender is mindfulness-based cognitive therapy (MBCT). Originally designed to reduce depression relapse (Kuyken et al., 2016), MBCT is also effective for current depressive symptoms across diverse populations (see Goldberg et al., 2019). Although results are mixed when comparing mindfulness to other PTSD treatments (Davis et al., 2019; Heffner et al., 2016), mindfulness-based approaches are effective in reducing PTSD symptoms (see Hopwood & Schutte, 2017). Taken together, MBCT may be useful for treating comorbid PTSD and MDD.
Mindfulness-based interventions (MBIs) show promise for addressing the long-term health effects of chronic stress and trauma in urban-dwelling Black adults (Watson-Singleton, Hill, et al., 2019), yet access to both trauma and culturally informed MBIs in Black communities is limited. Research supports the use of MBIs in trauma-exposed Black women (Burnett-Zeigler, et al., 2019; Zhang & Emory, 2015). However, to our knowledge, no studies have examined the feasibility and acceptability of primary care-based MBCT for trauma-exposed Black adults with comorbid PTSD and MDD. In addition, with few exceptions, prior work has not prioritized cultural modifications for MBIs, even though cultural modifications can help reduce barriers to engagement due to concerns of incongruence of MBI practices with cultural beliefs/coping and may promote relevance to unique needs of people of color often ignored in non-adapted MBIs (DeLuca et al., 2018; Watson-Singleton, Black, et al., 2019).
Given barriers to behavioral healthcare among chronically trauma-exposed Black adults living in low-income communities in the United States (Alegría et al., 2016), integrating MBIs into primary care locations may both reduce stigma (Rowan et al., 2021) and increase access, since primary care clinics in safety net hospitals often serve as the only option for regular healthcare for individuals with limited socioeconomic resources and may enable buy in for mental health services (Farber et al., 2017; Nath et al., 2016). Evidence supports the value of MBIs in primary care settings, including with individuals with symptoms of both PTSD and MDD (Possemato et al., 2016). However, prior studies do not focus on the target population.
To address gaps in treatment research, this pilot study examined feasibility and acceptability of an 8-week adapted MBCT protocol in an urban primary care setting for Black adults screening positive for PTSD and MDD. Adaptations ensured the intervention was trauma-informed and culturally responsive. Based on completion rates in previous studies (Burnett-Zeigler et al., 2016; Dutton et al., 2013; King et al., 2013), we predicted a retention rate of 75%. Acceptability of the intervention, including satisfaction, perceived benefits, and potential barriers to engagement, was assessed through a quantitative and qualitative approach, and thus, no predictions were made.
Method
Participants
Thirty-four adults (84.8% women) who were randomized into the study were included in analyses. From September 2018 to March 2020, participants were recruited from primary care clinics within a large public hospital in the southeastern United States. Although sample size was originally set at N=80, due to COVID-19, the in-person intervention was halted1. Inclusion criteria included positive PTSD screen (Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) ≥ 3), positive depression screen (Patient Health Questionnaire (PHQ-9) ≥ 10), chronic trauma exposure (Traumatic Events Inventory (TEI) ≥ 3 criterion A traumas)2, self-identification as Black or African American, and age 18–653. Exclusion criteria included active mania, psychosis, cognitive impairment, or past-month alcohol or substance use disorder (based on alcohol and substance use screeners). See Table 1 for sample characteristics and descriptive details of measures and Supplemental Table 1 for randomized participants’ concomitant treatments.
Table 1.
Sample characteristics
| Variables | Overall Sample | WLC | MBCT |
|---|---|---|---|
|
| |||
| n (%) | n (%) | n (%) | |
|
| |||
| Gender | |||
| Female | 28 (84.8%) | 14 (87.5%) | 14 (82.4%) |
| Male | 5 (14.7%) | 2 (12.5%) | 3 (17.6%) |
| Race | |||
| Black/African American | 34 (100%) | 16 (100%) | 18 (100%) |
| Marital status | |||
| Single, never married | 12 (36.4%) | 8 (50%) | 4 (12.5%) |
| Married | 7 (21.2%) | 0 | 7 (41.2%) |
| Divorced or separated | 7 (21.3%) | 6 (37.5%) | 1 (5.9%) |
| Widowed | 6 (18.2%) | 2 (12.5%) | 4 (23.5%) |
| Domestic partner | 1 (3%) | 0 | 1 (5.9%) |
| Employed | 9 (27.3%) | 6 (37.5%) | 3 (17.6%) |
| Supported by disability | 12 (35.3%) | 4 (25%) | 8 (47.1%) |
| Income | |||
| Less than $2,000 per month | 25 (78.1%) | 14 (87.5%) | 11 (68.8%) |
|
| |||
| Mean (SD), Range | Mean (SD), Range | Mean (SD), Range | |
|
| |||
| Age | 45.4 (11.9) | 44.3 (11.8) | 46.5 (12.3) |
| Trauma exposure | |||
| Number of types of trauma exposure | 8.81 (3.35), 2–16 | 10.07 (3.33), 6–16 | 7.63 (3.01), 2–15 |
| Frequency of trauma exposure | 61.38 (22.7), 13–119 | 69.22 (17.44) 39–99 | 55.31 (43.87), 27–109.64 |
| PC-PTSD-5 | 4.4 (0.71), 3–5 | 4.5 (0.63), 3–5 | 4.4 (0.79), 3–5 |
| PHQ-9 | 17.6 (4.7), 10–25 | 18.5 (4.4), 10–23 | 16.8 (4.9), 10–25 |
| FFMQ* | 96.00 (19.69), 70–154 | 91.5 (15.75), 74–136 | 99.3 (22.1), 70–154 |
|
| |||
| n (%) | n (%) | n (%) | |
|
| |||
| Current PTSD | 19 (61.3%) | 8 (53.3%) | 11 (68.8%) |
| Current MDD | 18 (58.1%) | 10 (66.7%) | 8 (50%) |
| Comorbid PTSD + MDD | 13 (41.9%) | 6 (37.5%) | 7 (41.2%) |
| Past PTSD (not including current) | 11 (35.3%) | 6 (40%) | 5 (31.3%) |
| Past MDD (not including current) | 8 (25.8%) | 3 (20%) | 5 (31.3%) |
N=34;
N=28
Procedure
Informed consent for the screening assessment and randomized controlled trial (RCT; NCT03922581) was approved by the Emory Institutional Review Board and the Grady Research Oversight Committee and completed in accord with the provisions of the Declaration of Helsinki.
Screening assessment.
Individuals were recruited through provider referrals or waiting rooms of medical clinics in a large, publicly funded hospital in the southeastern United States as part of a larger project on PTSD (see Gillespie et al., 2009). Screening assessments were conducted verbally by trained research assistants in private areas of waiting rooms or the laboratory. The assessments included questionnaires related to psychological and trauma history. Participants were compensated $15. If eligible and interested, after completing the screening, participants were referred to the RCT.
RCT.
Participants in the RCT completed a baseline diagnostic assessment focused on presence of PTSD, mood, substance use, and psychotic symptoms and diagnoses. Interviewers conducting assessments were graduate-level practicum students or postdoctoral residents trained and supervised by a licensed psychologist. Participants were compensated $60. Randomization occurred at the end of the baseline assessment if all inclusion criteria were met and no exclusion criteria emerged (e.g., psychotic symptoms). See Supplemental Methods for additional detail on randomization approach. Participants were randomized to 8-week MBCT group or waitlist control (WLC) with the option to participate in the MBCT group after study completion. MBCT group members were compensated $20 per session to aid with potential barriers to attending (e.g., cost of transportation or parking, childcare). Patients in the MBCT group were reminded of group each week. WLC participants were contacted at five weeks into 8-week waitlist and then again at eight weeks for the post-assessment. No additional efforts were made to retain contact.
Post-assessment.
After MBCT or WLC completion, a post-assessment was completed; pre- and post-assessments were completed by separate interviewers blinded to study randomization. All participants were compensated $20 for post- and 1-month follow-up.
Measures
Traumatic Events Inventory (TEI; Gillespie et al., 2009).
The TEI assesses lifetime exposure to traumatic events. Eighteen types of traumas are assessed, and for each traumatic event reported, participants indicated frequency on a scale of 0 (1 time) to 8 (greater than 20 times). The TEI has shown construct validity in similar populations (Mekawi et al., 2021). The TEI was obtained during the screening assessment.
Primary Care PTSD Screen for DSM-5 (PC-PTSD-5; Prins et al., 2016).
The 5-item PC-PTSD-5 screening measure is used to identify probable PTSD symptoms within the past 30 days and has been validated across multiple samples (Hawn et al., 2020; Van Dam et al., 2010). Total scores range from 0 to 5; three is the suggested cut-off for probable PTSD. The PC-PTSD-5 was obtained during the screening assessment, post-assessment, and 1-month follow-up assessment.
Patient Health Questionnaire (PHQ-9; Arroll et al., 2010).
The 9-item PHQ-9 is a self-report screener that identifies presence and severity of depressive symptoms. It has been validated in racially and ethnically diverse samples (Huang et al., 2006). Each item is scored from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 27; a cut-off score of 10 or above indicates moderate severity of depression symptoms. Internal consistency in this sample was adequate (α = .73). The PHQ-9 was obtained during the screening assessment, post-assessment, and 1-month follow-up assessment.
Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2013).
The CAPS-5 is an interviewer-administered psychometrically valid and standardized diagnostic instrument (Weathers et al., 2018; Weathers et al., 2001). All interviewers for this study underwent training on the CAPS, including in-person observations, weekly supervision, and tape review with a licensed psychologist. Previously examined interrater reliability (IRR) has been high for the diagnosis of PTSD (κ = 0.83; Powers et al., 2017). The CAPS-5 was conducted at the pre- and post-assessment by different interviewers who were blinded to study randomization.
MINI International Neuropsychiatric Interviewer (MINI; Sheehan et al., 1998).
The MINI is a reliable and validated diagnostic interview that assesses mood, substance use, and psychotic disorders. Interviewers underwent the same training as described for CAPS. The MINI was conducted at the pre-assessment. The MINI current depression module was re-assessed in the post-assessment by a separate interviewer blinded to study randomization.
Five Factor Mindfulness Questionnaire (FFMQ; Baer et al., 2006).
The 39-item FFMQ is a self-report measure that assesses five facets of trait mindfulness: 1) observing, 2) describing, 3) acting with awareness, 4) nonjudgment, and 5) nonreacting (Pang & Ruch, 2019). Participants responded to statements on a Likert-type scale from 1 (never or very rarely true) to 5 (very often or always true). FFMQ total score and subscale scores were calculated based on summation of scores; higher scores suggest higher levels of mindfulness. The FFMQ has been validated in a demographically similar clinical sample of Black women (Watson-Singleton et al., 2018). Internal consistency of the FFMQ total scale in this sample was high (α = .93). FFMQ was obtained at pre- and post-assessment and 1-month follow-up.
Client Satisfaction Questionnaire (CSQ-8; Attkisson & Greenfield, 1999).
The CSQ-8 is a self-report measure that assesses level of satisfaction with care. Each item is scored on a Likert scale from 1 (low satisfaction) to 4 (high satisfaction), and sum to a total score between 8 and 32, with higher scores indicating greater satisfaction. The CSQ-8 was given at post-assessment.
Perceived Barriers to Psychological Treatments (PBPT; Mohr et al., 2006).
The 27-item PBPT is a self-report measure of barriers to participating in psychological interventions. Individual items correspond with eight subscales: stigma, lack of motivation, emotional concerns, negative evaluations of therapy, misfit of therapy to needs, time constraints, participation restriction, and availability of services. For each item, participants “rate the degree to which different kinds of problems might get in the way of seeking therapy or counseling.” Items are scored on a Likert scale from 1 (not difficult at all) to 5 (impossible). To be considered a significant barrier, an individual item must have been rated as moderately difficult (3), extremely difficult (4), or impossible (5). The PBPT was given at post-assessment.
Post-group Follow-up Questionnaire.
The post-group follow up questionnaire was given only to MBCT group members during the post-assessment. It is a qualitative, 12-item assessment created internally assessing participants’ feelings about MBCT group, components they did/did not like, aspects they would change, group size, barriers to implementing skills, whether their needs were met, and what emotional or behavioral changes they noticed in themselves due to participation. These questions aimed to assess acceptability and identify areas for improvement.
Group Leader Manual Adherence and Competence Rating Form (GLMACRF; Weisman et al., 1998).
The 15-item GLMACRF was patterned after the Behavioral Family Management Therapist Competency/Adherence Scale (BFM-TCAS) and uses a 5-point scale to rate therapists’ manual adherence and competence (empathy, co-leader rapport, rapport with participants, active listening, and validation). It was adapted for the current MBCT protocol but was not specifically designed for MBCT. Manual adherence in the present study was 99.6% based on a randomized review of 20 sessions (36%, out of 56 sessions) by an independent rater who was trained in the MBCT protocol but not a clinician for any of the sessions reviewed.
MBCT Group Intervention
Participants randomized to MBCT attended weekly in-person group sessions conducted in a conference room within the primary care clinic. The MBCT intervention was patterned after the MBCT for depression intervention (Segal et al., 2018) but adapted to be trauma-informed and culturally responsive. Briefly, trauma-informed adaptations included 1) inclusion of psychoeducation geared toward trauma, stress physiology, and PTSD symptoms; 2) frequent and repeated directions related to autonomy for all exercises and the ability to adjust as needed (e.g., not requiring closed eyes); 3) grounding exercises at the beginning of every session; and 4) a maximum time for sitting meditations lasting only 10 minutes each. Cultural adaptations included 1) collaboration between PI and expert Black clinicians on protocol formulation, training, and intervention administration, 2) delivery of intervention in primary care clinic location, 3) weekly supervision with focus on cultural humility, 4) less emphasis on written homework to avoid challenges that may arise for participants with literacy difficulties; and 5) inclusion of group leaders who self-identify as Black whenever possible (see Supplemental Materials for full details of adaptations). The MBCT group consisted of eight, weekly 90-minute sessions that were conducted with rolling admission. Two therapists and between 1–6 group members attended each MBCT group. Sessions involved 1) skills training and in-class practice in mindfulness techniques, 2) psychoeducation, and 3) feedback and supportive group discussion of exercises (see Supplemental Figure 1 for session outline). All participants were given a handout about trauma effects in their first session. The manualized intervention was delivered by trained and closely supervised therapists who were overseen by a board-certified psychologist with training and expertise in MBCT in trauma-exposed Black adult populations (more detail provided in Supplemental Materials).
Data Analysis
Descriptive details of the adapted MBCT program and descriptive statistics on the study sample are provided. Enrollment, study completion, and MBCT group participation rates were used to evaluate feasibility. Acceptability was assessed using quantitative and qualitative data at the post-assessment interview to capture MBCT participants’ satisfaction with the intervention, perceived benefits, and engagement barriers. To identify themes related to acceptability, participants were asked to explain how the intervention changed specific aspects of their functioning, including how they handle stressful situations, physical health, and interpersonal functioning through 12 open-ended questions. Qualitative responses were collected verbatim by research interviewers. Response transcripts were compiled, and common themes were discussed and chosen by two authors [HDD and AP], who then independently categorized responses into those themes. Sample size calculations suggested at least 71 participants would need to be enrolled to detect mean differences in matched pairs of a medium effect size (0.30) at 80% power; therefore, treatment effects on symptoms or trait mindfulness were not analyzed (see Supplemental Table 2 for pre-, post-, and 1-month follow-up descriptive data).
Results
Feasibility
Enrollment
As shown in Figure 1, of the 191 individuals screened for eligibility between September 2018 and March 2020, 104 were excluded due to inability to contact, ineligibility, or lack of interest. Of those who did not wish to participate in the eligibility screen, four reported lack of interest, one reported transportation issues, and four reported scheduling issues. Of the 87 who met inclusion criteria, 42 were enrolled; 80.9% of those (n = 34) were randomized (18 to MBCT, 16 to WLC). Some eligible participants did not proceed to enrollment due to schedule conflicts or lack of interest. Some enrolled participants were not randomized because they were unable to be contacted, moved out of town, reported changes in availability post-enrollment, or developed new health conditions that prohibited participation.
Figure 1.
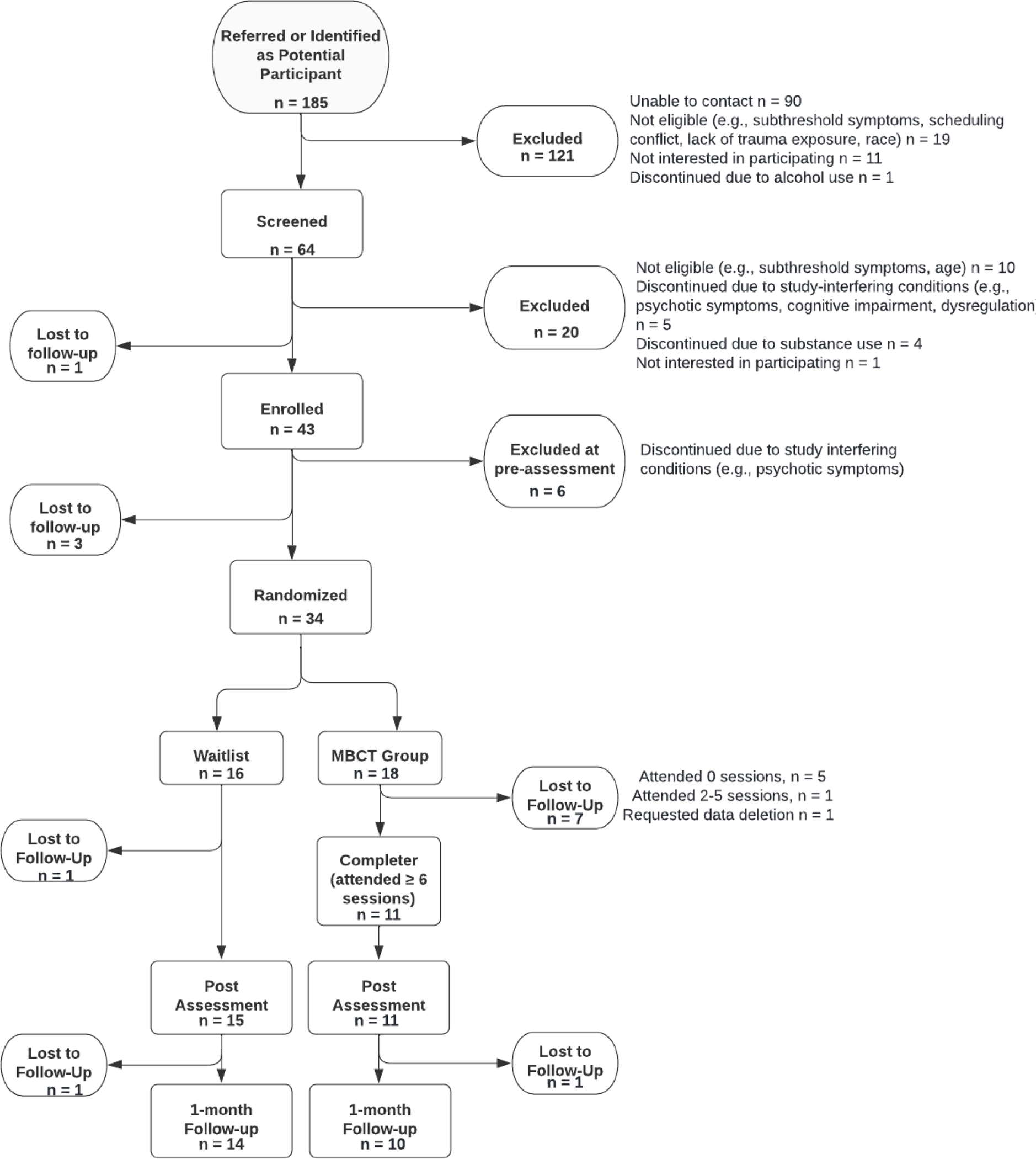
Recruitment flowchart for study
Study Completion
Study completion reflected engagement in all components of the MBCT group (including attending six or more sessions) or WLC through the post-assessment (see Figure 1). Twenty-six (76.5%) participants were study completers (61.1% of MBCT, 93.7% of WLC). Additionally, twenty-four (70.5%) completed through 1-month follow up (55.5% of MBCT, 87.5% of WLC).
MBCT Group Participation
Thirteen out of 18 (72.2%) participants randomized to MBCT group attended at least one session. Of those who attended at least one session, 11 (84.6%) attended all eight sessions.
Acceptability
Satisfaction
The mean CSQ-8 score among MBCT group completers (n = 11) was 31.6 (SD = .67) on a scale of 8–32; high scores correspond with high satisfaction. The quality of the MBCT group was rated as “excellent” by 100% of participants; 90.9% indicated they “definitely” got the kind of service they needed, and one responded they “generally” got the service they needed. All participants said they would “definitely” recommend this group to a friend and agreed that they deal with their problems more effectively because of the group. Regarding overall satisfaction with the group, 100% endorsed “very satisfied.”
MBCT participants also completed a qualitative assessment that assessed group satisfaction, acceptability of intervention format, and perceived helpfulness of the intervention. When asked about the MBCT group experience and what they liked about the intervention, participants noted that it was helpful (n = 7) and/or educational (n = 5). Most also stated it provided a new way of looking at things and specific tools (see Supplemental Materials).
Acceptability of Intervention Format
Regarding acceptability of intervention format, when asked what could have enhanced their experience, seven participants indicated there was nothing they would change about the intervention. Three participants mentioned missing their peers after group ended, wanting more time together, or desiring to extend the length of the intervention. One person did not like the space, another suggested the inclusion of snacks, and one person had to ask facilitators to speak up due to a hearing impairment.
Perceived Benefits of MBCT Group Participation
When asked about MBCT group participation gains, several themes emerged from narrative analysis, including greater awareness (n = 7) and attention (n = 4), improvements in emotion regulation (n = 5), skills to cope with stress or depression (n = 9), and feeling more in control (n = 4) (see Supplemental Materials for direct interview quotes). When asked if they noticed any changes to how they experience emotions or handle stress, all MBCT participants indicated a positive change and noted the use of mindfulness skills when distressed. When asked if they noticed any changes in how they feel physically, participants commented on having more energy (n = 4) and more positive affect (n = 2), feeling more relaxed or calmer (n = 2), and experiencing less physical pain (n = 2). Additionally, when asked about changes in how they relate to themselves or others, MBCT group members noted improvements in self-awareness and cognitions about themselves (n = 8), fewer interpersonal conflicts (n = 7), and benefits of peer support (n = 7).
Barriers to General and MBCT-Specific Treatment Engagement
Participants (n = 25) from MBCT and WLC completed the PBPT. Participants indicated an average of >6 significant barriers to receiving psychological services, more generally (M = 6.54, SD = 5.97, range 0–21). The most frequently reported barrier subscale was participation restrictions (64%; i.e., physical and transportation problems associated with attendance), followed by stigma, lack of motivation, availability of services, emotional concerns, misfit of therapy to needs, time constraints, and negative evaluation (see Supplemental Table 3). Cost of treatment is not included in any subscale but does contribute to the overall PBPT score. Fifty-six percent (n = 14) of respondents indicated that cost of treatment was a significant barrier.
MBCT group members were also asked about specific barriers that interfered with participating in MBCT group or practicing skills outside of group during their post-assessment interview. In the qualitative interview (n = 11), seven people denied barriers, one reported hearing impairment, two described trouble with concentration/motivation, and two reported initial worries about exposing their thoughts and feelings in front of others. Despite concerns regarding opening up in front of others, when asked about preference regarding individual versus group, all participants indicated that they preferred the group format.
Discussion
This study examined feasibility and acceptability of an adapted MBCT group intervention for Black adults who screened positive for PTSD and MDD in an urban primary care clinic setting. Results demonstrated feasibility for the incorporation of this intervention into the clinic setting, as evidenced by >75% of randomized participants completing the study through post-assessment and the majority of MCBT participants attending six or more sessions. Acceptability was demonstrated by high levels of satisfaction and several perceived benefits reported by MCBT group completers. Offering trauma-informed MBIs in primary care clinics within communities with limited access to behavioral health services could be a valuable step toward improving health outcomes and reducing health inequities that disadvantage Black adults.
As hypothesized, retention rates through post-assessment were >75%, supporting the feasibility of the protocol and general retention. Feasibility dropped slightly at 1-month follow-up, suggesting challenges maintaining contact with patients after intervention completion. Additionally, feasibility rates were lower in MBCT (<75%) than WLC, emphasizing that barriers exist to engagement in treatment and need to be addressed to improve outcomes. Of note, among individuals that attended at least one session, retention was high (>80%), highlighting feasibility among those who do show up and the need to better support those who do not.
Across all measured components of intervention acceptability, response was positive. Satisfaction was high among group members across quantitative and qualitative measures. It is important to note, however, that satisfaction data were gathered at post-assessment; participants who did not attend all eight sessions could not be contacted for post-assessment, so their satisfaction levels are not represented. Acceptability of the intervention format was also high, and most participants had no recommended changes to the intervention. The main suggestion for change was extending the group duration, an easily addressable change that could be tested.
Regarding perceived benefits of MBCT group identified from narrative data, several themes emerged related to improvements in self-awareness, emotion regulation, attention and control, and skills to manage stress and mood. Greater flexibility in cognitions and physical improvement regarding energy, pain level, and overall reductions in stress were also described. Previous findings have demonstrated that MBIs increase attentional control and cognitive flexibility, enhance awareness and regulation of emotional experience, and provide a space for experiential exposure to internal emotional responses through nonjudgment and acceptance (Bhatnagar et al., 2013; Gu et al., 2015; Krygier et al., 2013). Further, MBIs have been found to have positive health effects and reduce stress more generally (Grossman et al., 2004). These proposed mechanisms and observed outcomes of MBIs are consistent with the described benefits reported by MBCT group members in this study, although this study was not designed to investigate outcomes.
The value of peer support in this intervention also was identified by numerous group members. MBCT is traditionally delivered in a group setting to promote connection and exposure to others’ experiences. The benefits of peer and social support in promoting resilience among trauma-exposed adults is well documented (e.g., Pickover et al., 2021). Awareness of cultural context is crucial when working with individuals from communities of color and those who hold other marginalized identities (Bryant-Davis, 2019), and enabling connection within the MBCT group may have promoted positive change among the group members.
Cultural considerations were a part of the implementation and delivery of this intervention, given that culturally responsive modifications for MBIs within Black communities are vital in promoting intervention success (Watson-Singleton, Black, et al., 2019). However, we did not directly assess perceptions of cultural responsiveness or ask MBCT group members if the inclusion of only self-identifying Black members was helpful. In future studies with communities of color, reflections about group members’ race as well as whether the identity of group leaders had any effect on trust or group cohesion should be assessed.
Consistent with prior research in ethnoracial minority samples (Anderson et al., 2006; Mohr et al., 2006), participants reported a high level of perceived barriers to engagement in psychological services. Stigma and shame are common barriers that impede treatment engagement in trauma-exposed adults (Kantor et al., 2017), and stigma is particularly prominent in Black communities (Watson-Singleton, Black, et al., 2019). In our sample, almost half of the sample endorsed stigma-related barriers, such as stigma around friends or family members finding out or judgment by others or seen being emotional. While it is possible that offering the group in the clinic where patients receive medical care reduced stigma-related barriers, additional research on stigma and the location of psychological service delivery is needed. Importantly, participation barriers, such as physical limitations due to illness and limited ability to travel to appointments, were the most commonly identified group of barriers in our sample. Modifications to help address physical and transportation-related limitations in primary care populations might include virtual delivery of services, which have been shown to be promising in previous research (Segal et al., 2020; Shallcross et al., 2021). Studies on barriers to treatment engagement in low-income Black urban communities remain limited, and continued examination of barriers is needed. Efforts should include active engagement with community members in the planning and implementation of interventions to ensure important cultural considerations are not overlooked.
Despite the strengths of the study, there are limitations to consider. Generalizability is limited due to the specificity of the sample. However, the goal of the study was to address treatment research gaps for low-income Black adults in urban environments. Because this sample was predominantly Black women, additional research is necessary to evaluate feasibility and acceptability in samples with larger representation of Black men or gender non-binary individuals. It would have been beneficial to gather data on how the intervention fit with cultural values to ensure cultural adaptations were appropriate and if setting was helpful in reducing MBCT-specific barriers or if other sites are more desirable; future studies should explore patient perceptions of adaptations and preferences for implementation. Given the lower rate of retention among MBCT participants as compared to WLC participants, understanding barriers to retaining those in the MBCT group will be key for future implementation. Perhaps, current participants were more inclined to attend MBCT sessions given noted barriers to treatment and low socioeconomic resources. The trauma-informed and cultural adaptations have not been tested for efficacy, and thus it is critical that outcomes be tested for this protocol moving forward. At times, group sessions included only one participant and that could have impacted the experience of this group model. Additionally, the manual adherence and competency form we used was not specifically designed for MBCT. Finally, this pilot study was not powered to evaluate efficacy of the intervention in reducing PTSD and MDD symptoms, so further examination of the efficacy of MBCT in this population is necessary.
Given high rates of trauma, PTSD, and MDD among low resourced Black adults seeking primary care services, there is a need for universal trauma screening in primary care settings and access to trauma-informed and culturally responsive behavioral health interventions that can benefit patients with a range of psychological and physical health effects from chronic trauma exposure. Our findings demonstrate the potential for MBCT groups as a useful service in primary care settings and highlight the value of incorporating MBIs into broader trauma-informed service planning for urban hospitals serving trauma-exposed Black adults.
Supplementary Material
Clinical Impact Statement.
This study shows that providing a mindfulness-based cognitive therapy group to trauma-exposed Black adult patients with low socioeconomic resources and comorbid posttraumatic stress disorder and depression symptoms in a primary care clinic setting is feasible and acceptable. However, many barriers must be addressed to improve behavioral health care engagement and access in marginalized communities.
Funding.
This work was supported by the National Center for Complementary & Integrative Health (K23AT009713 for Powers).
Footnotes
Financial and Non-financial Interests. The authors have no relevant financial or non-financial interests to disclose.
Declarations
Ethics Approval and Consent. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Emory University Institutional Review Board and the Grady Research Oversight Committee.
Consent to Participate. Informed consent was obtained from all individual participants included in the study.
Clinical Trials Registration Information. NCT03922581, April 22, 2019.
In-person activities for the study halted as a result of the COVID-19 pandemic shut down and were transitioned to an all-virtual model on March 16 with full IRB-approval. Three participants randomized to group and one person randomized to control were still enrolled at this time and all completed through 1-month follow-up. Two participants were actively enrolled in the group at this time and completed their last group sessions (four for one participant and two for the other participant) via HIPAA-compliant Zoom.
Presence of 3 or more traumas was used as an inclusion criterion to ensure the presence of chronic trauma exposure.
Age cutoff of 65 was already required for the screening study used to enroll participants so was included for this study also.
References
- Alegría M, Alvarez K, Ishikawa RZ, DiMarzio K, & McPeck S (2016). Removing obstacles to eliminating racial and ethnic disparities in behavioral health care. Health Affairs, 35(6), 991–999. 10.1377/hlthaff.2016.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson CM, Robins CS, Greeno CG, Cahalane H, Copeland VC, & Andrews RM (2006). Why lower income mothers do not engage with the formal mental health care system: Perceived barriers to care. Qualitative Health Research, 16(7), 926–943. 10.1177/1049732306289224 [DOI] [PubMed] [Google Scholar]
- Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, Falloon K, & Hatcher S (2010). Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. The Annals of Family Medicine, 8(4), 348–353. 10.1370/afm.1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attkisson CC, & Greenfield TK (1999). The UCSF Client Satisfaction Scales: I. The Client Satisfaction Questionnaire-8. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. 10.1177/1073191105283504 [DOI] [PubMed] [Google Scholar]
- Bhatnagar R, Phelps L, Rietz K, Juergens T, Russell D, Miller N, & Ahearn E (2013). The effects of mindfulness training on post-traumatic stress disorder symptoms and heart rate variability in combat veterans. The Journal of Alternative and Complementary Medicine, 19(11), 860–861. 10.1089/acm.2012.0602 [DOI] [PubMed] [Google Scholar]
- Bryant-Davis T (2019). The cultural context of trauma recovery: Considering the posttraumatic stress disorder practice guideline and intersectionality. Psychotherapy, 56(3), 400. 10.1037/pst0000241 [DOI] [PubMed] [Google Scholar]
- Burnett-Zeigler I, Hong S, Waldron EM, Maletich C, Yang A, & Moskowitz J (2019). A mindfulness-based intervention for low-income African American women with depressive symptoms delivered by an experienced instructor versus a novice instructor. The Journal of Alternative and Complementary Medicine, 25(7), 699–708. 10.1089/acm.2018.0393 [DOI] [PubMed] [Google Scholar]
- Burnett-Zeigler IE, Satyshur MD, Hong S, Yang A, Moskowitz JT, & Wisner KL (2016). Mindfulness based stress reduction adapted for depressed disadvantaged women in an urban Federally Qualified Health Center. Complementary Therapies in Clinical Practice, 25, 59–67. 10.1016/j.ctcp.2016.08.007 [DOI] [PubMed] [Google Scholar]
- Cloitre M, Petkova E, Su Z, & Weiss B (2016). Patient characteristics as a moderator of post-traumatic stress disorder treatment outcome: combining symptom burden and strengths. British Journal of Psychiatry Open, 2(2), 101–106. 10.1192/bjpo.bp.115.000745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis LL, Whetsell C, Hamner MB, Carmody J, Rothbaum BO, Allen RS, & Bremner JD (2019). A multisite randomized controlled trial of mindfulness-based stress reduction in the treatment of posttraumatic stress disorder. Psychiatric Research and Clinical Practice, 1(2), 39–48. 10.1176/appi.prcp.20180002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLuca SM, Kelman AR & Waelde LC (2018). A systematic review of ethnoracial representation and cultural adaptation of mindfulness- and meditation-based interventions. Psychological Studies, 63, 117–129. 10.1007/s12646-018-0452-z [DOI] [Google Scholar]
- Dutton MA, Bermudez D, Matas A, Majid H, & Myers NL (2013). Mindfulness-based stress reduction for low-income, predominantly African American women with PTSD and a history of intimate partner violence. Cognitive and Behavioral Practice, 20(1), 23–32. 10.1016/j.cbpra.2011.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farber EW, Ali MK, Van Sickle KS, & Kaslow NJ (2017). Psychology in patient-centered medical homes: Reducing health disparities and promoting health equity. American Psychologist, 72(1), 28. 10.1037/a0040358 [DOI] [PubMed] [Google Scholar]
- Flory JD, & Yehuda R (2015). Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialogues in Clinical Neuroscience, 17(2), 141. 10.31887/DCNS.2015.17.2/jflory [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs CH, Haradhvala N, Evans DR, Nash JM, Weisberg RB, & Uebelacker LA (2016). Implementation of an acceptance- and mindfulness-based group for depression and anxiety in primary care: Initial outcomes. Families, Systems, & Health, 34(4), 386–395. 10.1037/fsh0000237 [DOI] [PubMed] [Google Scholar]
- Gillespie C, Bradley B, Mercer K, Smith A, Conneely K, Gapen M, & Ressler K (2009). Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry, 31, 505–514. 10.1016/j.genhosppsych.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluck R, Hartzell G, Dixon HD, Michopoulos V, Powers A, Stevens J, Fani N, Carter S, Schwartz A, Jovanovic T, Ressler K, Bradley B, & Gillespie CF (2021). Trauma exposure and stress-related disorders in a large, urban, predominantly African American female sample. Archives of Women’s Mental Health. 10.1007/s00737-021-01141-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Kearney DJ, & Simpson TL (2019). Mindfulness-based cognitive therapy for the treatment of current depressive symptoms: a meta-analysis. Cognitive Behaviour Therapy, 48(6), 445–462. 10.1080/16506073.2018.1556330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golin CE, Haley DF, Wang J, Hughes JP, Kuo I, Justman J, Adimora AA, Soto-Torres L, O’Leary A, & Hodder S (2016). Post-traumatic stress disorder symptoms and mental health over time among low-income women at increased risk of HIV in the US. Journal of Health Care for the Poor and Underserved, 27(2), 891. 10.1353/hpu.2016.0093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, & Walach H (2004). Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research, 57(1), 35–43. 10.1016/S0022-3999(03)00573-7 [DOI] [PubMed] [Google Scholar]
- Gu J, Strauss C, Bond R, & Cavanagh K (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12. 10.1016/j.cpr.2015.01.006 [DOI] [PubMed] [Google Scholar]
- Hawn SE, Cusack SE, George B, Sheerin CM, Group S.f.S.W., Dick D, & Amstadter AB. (2020). Diagnostic validity of the PC-PTSD screen in college students. Journal of American College Health, 1–11. 10.1080/07448481.2020.1841768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heffner KL, Crean HF, & Kemp JE (2016). Meditation programs for veterans with posttraumatic stress disorder: Aggregate findings from a multi-site evaluation. Psychological Trauma: Theory, Research, Practice, and Policy, 8(3), 365. 10.1037/tra0000106 [DOI] [PubMed] [Google Scholar]
- Hopwood TL, & Schutte NS (2017). A meta-analytic investigation of the impact of mindfulness-based interventions on post traumatic stress. Clinical Psychology Review, 57, 12–20. 10.1016/j.cpr.2017.08.002 [DOI] [PubMed] [Google Scholar]
- Horesh D, Lowe SR, Galea S, Aiello AE, Uddin M, & Koenen KC (2017). An in-depth look into PTSD-depression comorbidity: A longitudinal study of chronically-exposed Detroit residents. J Affect Disord, 208, 653–661. 10.1016/j.jad.2016.08.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang FY, Chung H, Kroenke K, Delucchi KL, & Spitzer RL (2006). Using the patient health questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. Journal of General Internal Medicine, 21(6), 547–552. 10.1111/j.1525-1497.2006.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantor V, Knefel M, & Lueger-Schuster B (2017). Perceived barriers and facilitators of mental health service utilization in adult trauma survivors: A systematic review. Clinical Psychology Review, 52, 52–68. 10.1016/j.cpr.2016.12.001 [DOI] [PubMed] [Google Scholar]
- King AP, Erickson TM, Giardino ND, Favorite T, Rauch SA, Robinson E, Kulkarni M, & Liberzon I (2013). A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD). Depress Anxiety, 30(7), 638–645. 10.1002/da.22104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krygier JR, Heathers JA, Shahrestani S, Abbott M, Gross JJ, & Kemp AH (2013). Mindfulness meditation, well-being, and heart rate variability: a preliminary investigation into the impact of intensive Vipassana meditation. International Journal of Psychophysiology, 89(3), 305–313. 10.1016/j.ijpsycho.2013.06.017 [DOI] [PubMed] [Google Scholar]
- Kuyken W, Warren FC, Taylor RS, Whalley B, Crane C, Bondolfi G, Hayes R, Huijbers M, Ma H, & Schweizer S (2016). Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: an individual patient data meta-analysis from randomized trials. JAMA Psychiatry, 73(6), 565–574. 10.1001/jamapsychiatry.2016.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Hart SL, Howard I, Julian L, Vella L, Catledge C, & Feldman MD (2006). Barriers to psychotherapy among depressed and nondepressed primary care patients. Annals of Behavioral Medicine, 32(3), 254–258. 10.1207/s15324796abm3203_12 [DOI] [PubMed] [Google Scholar]
- Nath JB, Costigan S, & Hsia RY (2016). Changes in demographics of patients seen at federally qualified health centers, 2005–2014. JAMA Internal Medicine, 176(5), 712–714. 10.1001/jamainternmed.2016.0705 [DOI] [PubMed] [Google Scholar]
- Orsillo SM, & Batten SV (2005). Acceptance and commitment therapy in the treatment of posttraumatic stress disorder. Behavior Modification, 29(1), 95–129. 10.1177/0145445504270876 [DOI] [PubMed] [Google Scholar]
- Pang D, & Ruch W (2019). Scrutinizing the components of mindfulness: insights from current, past, and non-meditators. Mindfulness, 10(3), 492–505. 10.1007/s12671-018-0990-4 [DOI] [Google Scholar]
- Pickover AM, Bhimji J, Sun S, Evans A, Allbaugh LJ, Dunn SE, & Kaslow NJ (2021). Neighborhood disorder, social support, and outcomes among violence-exposed African American women. Journal of Interpersonal Violence, 36(7–8), NP3716–NP3737. 10.1177/0886260518779599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Possemato K, Bergen-Cico D, Treatman S, Allen C, Wade M, & Pigeon W (2016). A Randomized Clinical Trial of Primary Care Brief Mindfulness Training for Veterans With PTSD. Journal of Clinical Psychology, 72(3), 179–193. 10.1002/jclp.22241 [DOI] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, Kaloupek DG, Schnurr PP, Kaiser AP, & Leyva YE (2016). The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 31(10), 1206–1211. 10.1007/s11606-016-3703-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, & Feuer CA (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70(4), 867. 10.1037/0022-006X.70.4.867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowan AB, Grove J, Solfelt L, & Magnante A (2021). Reducing the impacts of mental health stigma through integrated primary care: an examination of the evidence. Journal of Clinical Psychology in Medical Settings, 28(4), 679–693. 10.1007/s10880-020-09742-4 [DOI] [PubMed] [Google Scholar]
- Santorelli S, & Meleo-Meyer F (n.d.). Mindfulness Based Stress Reduction from the Center for Mindfulness in Medicine, Health, and Society. [Google Scholar]
- Segal ZV, Dimidjian S, Beck A, Boggs JM, Vanderkruik R, Metcalf CA, Gallop R, Felder JN, & Levy J (2020). Outcomes of online mindfulness-based cognitive therapy for patients with residual depressive symptoms: a randomized clinical trial. JAMA Psychiatry, 77(6), 563–573. 10.1001/jamapsychiatry.2019.4693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams M, & Teasdale J (2018). Mindfulness-based Cognitive Therapy for Depression. Guilford Publications. [Google Scholar]
- Shallcross AJ, Duberstein ZT, Sperber SH, Visvanathan PD, Lutfeali S, Lu N, Carmody J, & Spruill TM (2021). An Open Trial of Telephone-Delivered Mindfulness-Based Cognitive Therapy: Feasibility, Acceptability, and Preliminary Efficacy for Reducing Depressive Symptoms. Cognitive and Behavioral Practice. 10.1016/j.cbpra.2020.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, & Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. [PubMed] [Google Scholar]
- Sibrava NJ, Bjornsson AS, Pérez Benítez ACI, Moitra E, Weisberg RB, & Keller MB (2019). Posttraumatic stress disorder in African American and Latinx adults: Clinical course and the role of racial and ethnic discrimination. American Psychologist, 74(1), 101. 10.1037/amp0000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dam D, Ehring T, Vedel E, & Emmelkamp PM (2010). Validation of the Primary Care Posttraumatic Stress Disorder screening questionnaire (PC-PTSD) in civilian substance use disorder patients. Journal of Substance Abuse Treatment, 39(2), 105–113. 10.1016/j.jsat.2010.05.005 [DOI] [PubMed] [Google Scholar]
- Watson-Singleton NN, Black AR, & Spivey BN (2019). Recommendations for a culturally-responsive mindfulness-based intervention for African Americans. Complementary Therapies in Clinical Practice, 34, 132–138. 10.1016/j.ctcp.2018.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson-Singleton NN, Hill LK, & Case AD (2019). Past Discrimination, Race-Related Vigilance, and Depressive Symptoms: the Moderating Role of Mindfulness. Mindfulness, 10(9), 1768–1778. 10.1007/s12671-019-01143-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson-Singleton NN, Walker JH, LoParo D, Mack SA, & Kaslow NJ (2018). Psychometric evaluation of the five facet mindfulness questionnaire in a clinical sample of African Americans. Mindfulness, 9(1), 312–324. 10.1007/s12671-017-0776-0 [DOI] [Google Scholar]
- Weathers F, Blake D, Schnurr P, Kaloupek D, Marx B, & Keane T (2013). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5)[Measurement Instrument]. [Google Scholar]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, Keane TM, & Marx BP (2018). The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383. 10.1037/t71324-000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, & Davidson JR (2001). Clinician-Administered PTSD Scale: A review of the first ten years of research. Depress Anxiety, 13(3), 132–156. 10.1002/da.1029 [DOI] [PubMed] [Google Scholar]
- Weisman AG, Okazaki S, Gregory J, Goldstien MJ, Tompson MC, Rea M, & Miklowitz DJ (1998). Evaluating therapist competency and adherence to behavioral family management with bilpor patients. Family Profess, 37(1), 107–121. 10.1111/j.1545-5300.1998.00107.x [DOI] [PubMed] [Google Scholar]
- Zhang H, & Emory EK (2015). A mindfulness-based intervention for pregnant African-American women. Mindfulness, 6(3), 663–674. 10.1007/s12671-014-0304-4 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


