Abstract
Nasogastric tube syndrome (NGTS) induced by a nasointestinal ileus tube is an uncommon but potentially life-threatening complication. NGTS often becomes serious and progresses to acute upper airway obstruction caused by bilateral vocal cord paralysis or laryngeal infection. Early detection and proper treatment of NGTS are necessary. We describe the case of a 78-year-old patient with this syndrome induced by a nasointestinal ileus tube. At administration, ileus was suspected based on physical examination and thoracoabdominal X-ray findings. A nasointestinal ileus tube was placed through the left nasal cavity. Three days after tube placement, hoarseness and wheezing were found during nutrition support team rounds. Upper airway obstruction was suspected and evaluated immediately with flexible laryngoscopy by an otolaryngologist. The nasointestinal ileus tube was removed. The symptoms decreased with prompt proper management. Immediate removal of the tube and early recognition of symptoms are the first steps in the treatment for this syndrome, in addition to the initiation of steroid, proton pump inhibitor, and antibiotic therapy. The cause of NGTS is thought to be continuous pressure on the hypopharynx and cervical esophagus. NGTS should be considered in patients with either nasogastric or nasointestinal ileus tubes. Early diagnosis and proper management of NGTS are important.
Keywords: Upper airway obstruction, Nasogastric tube syndrome, Nasointestinal ileus tube, Laryngoscope, Vocal cord paralysis
Introduction
Recently, nasogastric tube syndrome (NGTS), a serious complication induced by nasogastric tubes, has been often reported [1, 2, 3]. Early detection and proper treatment for NGTS are necessary because NGTS often becomes serious and progresses to acute upper airway obstruction caused by bilateral vocal cord paralysis or laryngeal infection. The main noticeable physical symptoms consist of throat pain, wheezing, and hoarseness due to vocal cord dysfunction [2]. Immunocompromised states such as malnutrition have been suggested as risk factors for NGTS [2]. There is little correlation between the duration of nasogastric tube placement and the onset of NGTS [1].
Like nasogastric tubes, nasointestinal ileus tubes are also inserted through the nasal cavity. They are located in the upper airway and gastrointestinal tract. NGTS induced by nasointestinal ileus tubes has been also reported, in addition to NGTS induced by nasogastric tubes [4, 5]. We hypothesized that both early observation and adequate treatment of patients with a nasointestinal ileus tube have an effect on timely management of NGTS.
Case Report/Case Presentation
The patient was a 78-year-old man admitted to Sanin Rosai Hospital for treatment of aspiration pneumonia. His medical condition at admission included mild malnutrition. His height was 151 cm, and his body weight was 39.2 kg (body mass index, 17.2 kg/m2). Laboratory tests showed white blood cell count of 10,900/μL, lymphocyte cell count of 1,060/μL, and albumin level of 2.3 g/dL. The patient was bedridden due to spinal disease. At admission, ileus was also suspected based on physical examination and thoracoabdominal X-ray findings.
A nasointestinal ileus tube (18 Fr, 5.3 mm in diameter) was placed through the left nasal cavity for bowel decompression (Fig. 1). Two days after admission, symptoms of ileus decreased. The nasointestinal ileus tube was kept in place to administer medications. Three days after administration, hoarseness and wheezing were found during nutrition support team (NST) rounds. The NST consisted of physicians, including an otorhinolaryngologist, a nutritionist, a pharmacist, a speech therapist, and a nurse. Upper airway obstruction was suspected and evaluated immediately with flexible laryngoscopy by an otorhinolaryngologist. Left arytenoid edema and erythema with pooling of saliva in the hypopharynx were found in the larynx. The left vocal cord was paralyzed and completely fixed. The right vocal cord was partly paralyzed (Fig. 2). Oxygen saturation remained at 96% on room air. The nasointestinal ileus tube was removed immediately due to the risk of suffocation. Intravenous steroids were administered for 2 days. A proton pump inhibitor and an antibiotic were given for a week. Six hours after removal, arytenoid edema decreased markedly (Fig. 3). Three days after removal, the risk of upper airway obstruction was decreasing. Tracheostomy was avoided because vocal cord mobility and the glottic opening were normal based on flexible laryngoscopy and wheezing had resolved (Fig. 4). By 7 days after removal, the symptom of hoarseness decreased significantly. Oral intake was restarted based on the swallowing function examination results. By 8 days after removal, bilateral vocal cord paralysis and arytenoid edema had resolved (Fig. 5). Eleven days after removal, the treatment for aspiration pneumonia was completed. The patient was discharged without any sequelae.
Fig. 1.
Nasointestinal ileus tube positioning. A nasointestinal ileus tube (18 Fr, 5.3 mm in diameter) was placed through the left nasal cavity.
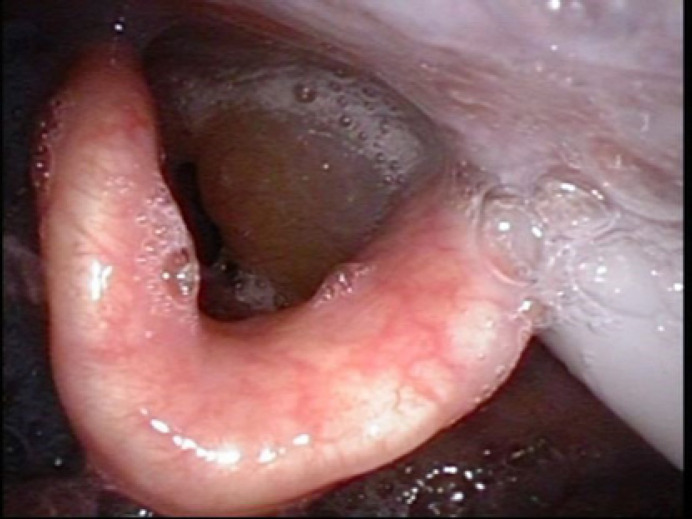
Fig. 2.
Laryngoscopic findings. There was left arytenoid edema and erythema in the larynx. The nasointestinal ileus tube was placed through the left hypopharynx.
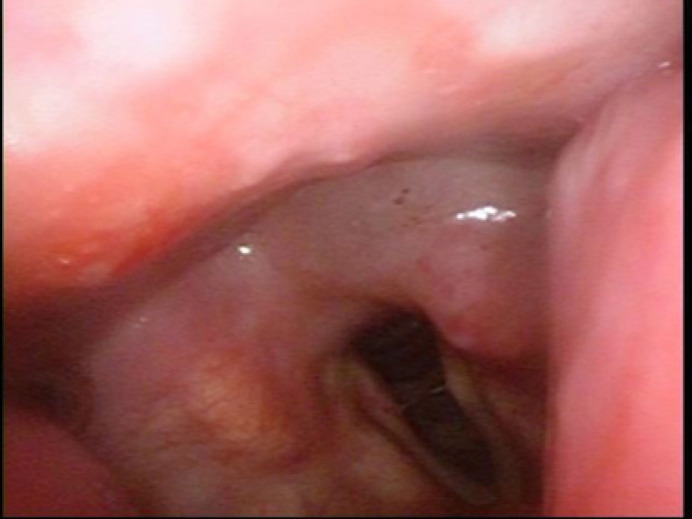
Fig. 3.
Laryngoscopic findings immediately after removal of nasointestinal ileus tube. Left arytenoid edema and erythema had clearly decreased.
Fig. 4.
Laryngoscopic findings 3 days after removal and treatment. Patency of the upper airway was confirmed.
Fig. 5.
Laryngoscopic findings 8 days after removal and treatment. Left arytenoid edema and erythema had decreased significantly.
Discussion/Conclusion
Though cases of NGTS attributed to nasogastric tubes have been reported, only two reports have shown NGTS induced by nasointestinal ileus tubes, not including this case [1, 2, 3, 4, 5, 6, 7, 8]. The proposed mechanism is tissue injury caused by continuous pressure on the region of physiologic narrowing between the hypopharynx and the cervical esophagus [2, 9, 10]. Another possible mechanism is a relationship between NGTS and gastroesophageal reflux due to being in the supine position [1, 11].
Appropriate therapy for NGTS consists of immediate removal of the nasointestinal ileus tube to prevent the pressure it induces [5, 6, 12]. In our study, early-stage medical treatment was important because arytenoid edema could be caused by infection from the injured posterior cricoarytenoid muscle [1, 9, 10]. In addition, we speculated that vocal cord dysfunction was caused by temporary paralysis induced by reversible injury of the posterior cricoarytenoid muscle because we identified early laryngeal symptoms. The clinical course, which consisted of the development of NGTS symptoms during intubation and decrease of NGTS symptoms after extubation, suggested that this case resulted from a nasogastric tube complication. There are several reports of NGTS in which the tube diameter was 18 Fr, as in this case [1, 2]. This finding suggests that a narrow tube diameter is preferable, considering the mechanism [5].
In this case, NGTS developed 3 days after tube placement, which is shorter than in other reports; the syndrome has been reported 5 days or more after tube placement [1, 3, 6, 10, 13]. However, one report described symptom onset within 12 h after tube placement [12]. Therefore, the thoracic symptoms of hoarseness and wheezing in patients with a nasogastric tube in place warrant attention due to the risk of rapid acute deterioration. Of note, immunocompromised states have been reported to be risk factors for NGTS [2, 3, 13, 14]. In general, the nutritional status of patients with nasogastric tubes or nasointestinal ileus tubes deteriorates due to the lack of oral intake. In our patient, immunocompromised status was assumed because the physical findings and laboratory tests indicated malnutrition. In our patient, early detection and immediate treatment for NGTS were performed without any sequelae. However, the symptoms of NGTS could potentially become severe, as in cases of tracheotomy or death due to upper airway obstruction [12]. Thus, the condition of the vocal cords and larynx should be examined carefully. Vocal cord paralysis associated with NGTS is a common observation confirmed by laryngoscopy [12]. Immediately after NGTS is suspected due to symptoms such as hoarseness and wheezing in patients with a nasointestinal ileus tube, laryngoscopy is mandatory [12].
A nasointestinal ileus tube is usually used by gastroenterologists who are not used to making medical assessments of the larynx and pharynx. In addition, there are few reports about NGTS associated with nasointestinal ileus tubes. Thus, NGTS associated with nasointestinal ileus tubes is not well known.
Patients with nasointestinal ileus tubes might not display the symptoms of NGTS immediately and accurately due to low ability to perform activities of daily living or poor general condition, as in our patient. Early recognition of NGTS symptoms is important. In our patient, early recognition of hoarseness during NST rounds might have averted life-threatening NGTS. Nasointestinal ileus tube placement is an effective treatment for ileus [15]. Ideally, a narrower tube diameter should be chosen to reduce the pressure against the organization [1]. However, a nasointestinal ileus tube of a larger diameter sometimes has to be used to treat ileus more effectively [16, 17]. Consequently, when a nasointestinal ileus tube is used, systems for early diagnosis and proper management should be put into place, in addition to more widespread knowledge of NGTS.
In conclusion, NGTS should be considered in patients with nasogastric tubes and nasointestinal ileus tubes. Early diagnosis and proper management of NGTS are important to prevent mortality.
Statement of Ethics
This retrospective review of patient data did not require ethics approval in accordance with local and national guidelines. Written informed consent was obtained from the patient for publication of the details of their medical case and any accompanying images.
Conflict of Interest Statement
The authors declare that they have no conflicts of interest to disclose.
Funding Sources
This case report was not supported by relevant funds.
Author Contributions
Kenkichiro Taira: drafting of the manuscript; clinical work-up and therapy; design of the report; and revision of the language and grammar of the manuscript. Satoshi Koyama, Tsuyoshi Morisaki, Takahiro Fukuhara, and Ryouhei Donishi: critical revision of the manuscript. Kazunori Fujiwara: critical revision of the manuscript, design of the report, and revision of the language and grammar of the manuscript.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Funding Statement
This case report was not supported by relevant funds.
References
- 1.Nehru VIN, Al Shammari HJ, Jaffer AM. Nasogastric tube syndrome the unilateral variant. Med Princ Pract. 2003 Jan-Mar;12((1)):44–46. doi: 10.1159/000068162. [DOI] [PubMed] [Google Scholar]
- 2.Sofferman RA, Haisch CE, Kirchner JA, Hardin NJ. The nasogastric tube syndrome. Laryngoscope. 1990 Sep;100((9)):962–968. doi: 10.1288/00005537-199009000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Apostolakis LW, Funk GF, Urdaneta LF, McCulloch TM, Jeyapalan MM. The nasogastric tube syndrome two case reports and review of the literature. Head Neck. 2001 Jan;23((1)):59–63. doi: 10.1002/1097-0347(200101)23:1<59::aid-hed9>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 4.Sanaka M, Kishida S, Yoritaka A, Sasamura Y, Yamamoto T, Kuyama Y. Acute upper airway obstruction induced by an indwelling long intestinal tube attention to the nasogastric tube syndrome. J Clin Gastroenterol. 2004 Nov-Dec;38((10)):913. doi: 10.1097/00004836-200411000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Sano N, Yamamoto M, Nagai K, Yamada K, Ohkohchi N. Nasogastric tube syndrome induced by an indwelling long intestinal tube. World J Gastroenterol. 2016 Apr 21;22((15)):4057–4061. doi: 10.3748/wjg.v22.i15.4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcus EL, Caine Y, Hamdan K, Gross M. Nasogastric tube syndrome a life-threatening laryngeal obstruction in a 72-year-old patient. Age Ageing. 2006 Sep;35((5)):538–539. doi: 10.1093/ageing/afl042. [DOI] [PubMed] [Google Scholar]
- 7.Vielva del Campo B, Moráis Pérez D, Saldaña Garrido D. Nasogastric tube syndrome a case report. Acta Otorrinolaringol Esp. 2010 Jan-Feb;61((1)):85–86. doi: 10.1016/j.otorri.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Harmon J, Balakrishnan K, de Alarcon A, Hart CK. The nasogastric tube syndrome in infants. Int J Pediatr Otorhinolaryngol. 2014 May;78((5)):882–884. doi: 10.1016/j.ijporl.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 9.Friedman M, Baim H, Shelton V, Stobnicki M, Chilis T, Ferrara T, et al. Laryngeal injuries secondary to nasogastric tubes. Ann Otol Rhinol Laryngol. 1981 Sep-Oct;90((5 Pt 1)):469–474. doi: 10.1177/000348948109000511. [DOI] [PubMed] [Google Scholar]
- 10.Isozaki E, Tobisawa S, Naito R, Mizutani T, Hayashi H. A variant form of nasogastric tube syndrome. Intern Med. 2005 Dec;44((12)):1286–1290. doi: 10.2169/internalmedicine.44.1286. [DOI] [PubMed] [Google Scholar]
- 11.Dotson RG, Robinson RG, Pingleton SK. Gastroesophageal reflux with nasogastric tubes. Effect of nasogastric tube size. Am J Respir Crit Care Med. 1994 Jun;149((6)):1659–1662. doi: 10.1164/ajrccm.149.6.8004326. [DOI] [PubMed] [Google Scholar]
- 12.Brousseau VJ, Kost KM. A rare but serious entity nasogastric tube syndrome. Otolaryngol Head Neck Surg. 2006 Nov;135((5)):677–679. doi: 10.1016/j.otohns.2006.02.039. [DOI] [PubMed] [Google Scholar]
- 13.Sofferman RA, Hubbell RN. Laryngeal complications of nasogastric tubes. Ann Otol Rhinol Laryngol. 1981 Sep-Oct;90((5 Pt 1)):465–468. doi: 10.1177/000348948109000510. [DOI] [PubMed] [Google Scholar]
- 14.Wolff AP, Kessler S. Iatrogenic injury to the hypopharynx and cervical esophagus an autopsy study. Ann Otol Rhinol Laryngol. 1973 Nov-Dec;82((6)):778–783. doi: 10.1177/000348947308200605. [DOI] [PubMed] [Google Scholar]
- 15.Shi Y, Zhang XP, Qin H, Yu YJ. Naso-intestinal tube is more effective in treating postoperative ileus than naso-gastric tube in elderly colorectal cancer patients. Int J Colorectal Dis. 2017 Jul;32((7)):1047–1050. doi: 10.1007/s00384-017-2760-5. [DOI] [PubMed] [Google Scholar]
- 16.Li L, Xue B, Zhao Q, Xie HQ, Luan XR, Cui Q. Observation on the curative effect of long intestinal tube in the treatment of phytobezoar intestinal obstruction. Medicine. 2019 Mar;98((11)):e14861. doi: 10.1097/MD.0000000000014861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li RH, Li DC, Lv XP, Quan B. Radiophotographically controlled nasointestinal intubation to treat recurrent postoperative adhesive ileus. Cell Biochem Biophys. 2015 Jun;72((2)):509–514. doi: 10.1007/s12013-014-0496-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.