Abstract
Aim:
Comorbid anxiety disorder is related to greater illness severity among individuals at clinical high risk (CHR) for psychosis, but its potential role in moderating response to Family Focused Therapy (FFT) for CHR is unexamined. We investigated whether comorbid anxiety disorder in CHR individuals is associated with less constructive communication during family problem-solving interactions, whether their communication skills differentially improve after FFT, and whether FFT is effective in reducing anxiety in this population.
Methods:
Individuals recruited into the second phase of the 8-site North American Prodrome Longitudinal Study (NAPLS2) participated (N = 129). They were randomly assigned to 18-sessions of FFT-CHR or three-sessions of Enhanced Care (EC). Participants completed a diagnostic interview at pre-treatment, a family interaction task at pre-treatment and 6-months, and a self-report anxiety measure at pretreatment, 6 and 12-months.
Results:
Individuals at CHR with comorbid anxiety engaged in more negative and fewer positive behaviours during family problem-solving interactions at pre-treatment than did those without comorbid anxiety. There was a significant interaction between anxiety diagnosis and time on interactional behaviour scores, such that individuals at CHR with an anxiety diagnosis showed a greater decrease in negative behaviours and increase in positive behaviours from baseline to 6-months than those without anxiety disorder(s) regardless of treatment condition. However, individuals’ self-reported anxiety symptoms decreased more in FFT-CHR than in EC from pre-treatment to 12-month follow-up, regardless of anxiety diagnoses.
Conclusions:
Individuals at CHR with symptoms of anxiety benefit from family interventions in showing reductions in anxiety and improvements in family communication.
Keywords: anxiety, clinical high risk for psychosis, enhanced care, family focused treatment, family problem-solving interaction task
1 |. INTRODUCTION
Psychoses are among the most severe psychiatric disorders (Armando et al., 2015; Gore et al., 2011). Adolescents and young adults at clinical high-risk (CHR) for psychosis—with subthreshold levels of unusual thought content, perceptual abnormalities, or thought disorder combined with functional deterioration - are at risk for transitioning to psychosis in 2–5 years (Addington et al., 2020). Anxiety is a primary complaint among individuals at CHR (Häfner et al., 1995; Yung & McGorry, 1996), and tends to presage the onset of psychosis (Fusar-Poli et al., 2014). Efforts to prevent and/or attenuate the course of psychosis may be facilitated through treatments that focus on reducing anxiety in individuals at CHR. Targeting anxiety in this population may have the secondary benefit of improving global functioning, given that comorbid disorders persist even among individuals at CHR who do not develop a psychotic disorder (Lin et al., 2015; Rutigliano et al., 2016).
Since individuals at CHR for psychosis tend to be adolescents and young adults living with their families, it will be informative to study day-to-day experiences of stress and anxiety within the family environment. Despite the high level of anxiety disorders within the CHR population (McAusland et al., 2017), there has been little research on family interactions in this subgroup. Daily interactions build upon each other and attune youths to parents’ emotion regulation and influence their own emotional responses to events (Leerkes et al., 2020; Perlman et al., 2022). According to dyadic synchrony theories, the moment-to-moment coordination of behavioural, neural, and physiological processes between parents and youths enable the transmission of adaptive or maladaptive strategies for coping with challenges (Perlman et al., 2022).
Prior work examining family problem-solving interactions has found that the intensity of conflictual behaviour varies by youth symptom presentation. For example, families with a youth at CHR for psychosis display more conflictual behaviour than families with a youth at risk for bipolar illness (Salinger et al., 2018). Nonetheless, there is variability in the intensity of conflict among families with CHR youths, which may predict future functioning. Individuals at CHR who engage in angry criticism, withdrawal, and off-task behaviour during family problem-solving interactions are more likely to experience an increase in positive symptoms of psychosis over 6 months (O’Brien et al., 2009). Conversely, CHR youths’ positive behaviours during family interactions predict improvement in symptoms and social functioning (O’Brien, 2006).
Research on families of youth with an anxiety disorder have found that these youth are more likely to disengage, complain, engage in off-task behaviour (Schrock & Woodruff-Borden, 2010), and provide less positive feedback than do youth without an anxiety disorder during family interaction tasks (Hummel & Gross, 2001). Also, parents of children with anxiety disorders have been found to be more inattentive and to use less positive feedback during a family interaction task than parents of non-anxious children (Hummel & Gross, 2001; Williams et al., 2012). Family environments with high rates of negative communication (criticism, rejection) and a lack of parental warmth and acceptance may contribute to the development of anxiety in children (Bögels & Brechman-Toussaint, 2006; Crawford & Manassis, 2001; Rapee, 1997; Siqueland et al., 1996). Negative family interactions are hypothesized to lead to anxiety in children through the development of negative self-perceptions and expectations of a hostile interpersonal environment (Bögels & Brechman-Toussaint, 2006). Additionally, children raised in these environments may learn inappropriate conflict and problem-solving strategies through modelling and reinforcement (Crawford & Manassis, 2001). Conversely, parental warmth may help to decrease the child’s reactivity to potentially threatening social interactions. For example, following 16-weeks of individual CBT for anxiety, adolescents who rated their mothers as high in warmth exhibited less neural activation while listening to tapes of their mothers’ criticism 2 years later and reported lower levels of anxiety (Butterfield et al., 2021).
Family interventions that focus on communication may be well-suited for families of youth at CHR with a comorbid anxiety disorder. For youth at CHR for psychosis, family-focused treatment (FFT), which includes psychoeducation, communication, and problem-solving training, reduced negative communication and increased positive communication more effectively than brief family psychoeducation (O’Brien et al., 2014). Family-focused interventions are also efficacious in reducing symptoms of anxiety in youths without CHR symptoms (Peris et al., 2021). For example, family-based CBT that teaches family communication skills was more effective in reducing anxiety than a family-based education control (Kendall et al., 2008). Additional studies indicate that enhancing parenting behaviours that convey warmth and strengthen communication is related to decreased anxiety at long-term follow-up (Barrett et al., 1996; Cobham et al., 2010).
Family interventions such as FFT that include ample opportunities for family members to practice communication and problem-solving skills may facilitate maintenance of treatment gains through family members’ modelling and reinforcement of skills after treatment has ended, and a related reduction in the emotional contagion of distress. Furthermore, enhanced problem-solving and communication skills may enable family members to approach rather than avoid challenges (Butterfield et al., 2021), an important process in the reduction of anxiety.
1.1 |. Primary aims and hypotheses
The present study utilized data from a randomized clinical trial (Miklowitz et al., 2014) to examine the relationship of anxiety disorders to family problem-solving behaviours and the efficacy of FFT for CHR (FFT-CHR) compared to brief family psychoeducation (‘enhanced care’) in modifying these behaviours among individuals at risk for psychosis. Additionally, the efficacy of FFT for reducing self-reported anxiety symptoms was evaluated. We hypothesized that: (1) individuals at CHR for psychosis with one or more anxiety disorders would be more likely to exhibit negative behaviours (e.g., criticism) and less likely to exhibit positive behaviours (e.g., listening) during 10-minute family problem-solving interactions than individuals at CHR without an anxiety disorder; (2) the presence of at least one anxiety disorder would predict more favourable responses to FFT-CHR (versus enhanced care) in terms of decreases in individuals’ negative behaviours and increases in positive behaviours during family interactions; and (3) FFT-CHR would be associated with greater decreases in self-reported symptoms of anxiety than brief psychoeducation.
2 |. METHODS
2.1 |. Participants
Participants were recruited into the second phase of the North American Prodrome Longitudinal Study (NAPLS2; Addington et al., 2012), conducted through a consortium of eight research centres (N = 129). In NAPLS2, individuals between the ages of 12 and 35 years who are primarily English speaking and met criteria for one of three psychosis-risk syndromes assessed by the Structured Interview for Psychosis-Risk Syndromes (SIPS: McGlashan et al., 2010) were considered for inclusion. Exclusion criteria included any current or past DSM–IV psychotic disorder, intellectual disability, current drug or alcohol dependence, and the presence of a neurological disorder. Over half of the participants (n = 67) met DSM-IV criteria for one or more anxiety disorders based on the SCID-IV (First et al., 2002). See Table 2.
TABLE 2.
Sample characteristicsa
| Variable | Total population (n = 129) | No anxiety diagnosis (n = 62) | Anxiety diagnosis (n = 67) | Statistical test and sig. |
|---|---|---|---|---|
| Age, y (Mean, SD) | 17.4 (4.1) | 17.6 (4.4) | 17.1 (3.7) | t = 0.84, p = 0.40 |
| Sex | X2 = 0.70, p = .40 | |||
| Female, n | 38 | 17 | 21 | |
| Male, n | 58 | 31 | 27 | |
| Medication, n | 26 | 16 | 10 | X2 = 2.37, p = .12 |
| Race, n | X2 = 4.46, p = .72 | |||
| Asian | 5 | 1 | 4 | |
| Black | 9 | 6 | 3 | |
| Latinx | 16 | 7 | 9 | |
| Middle Eastern | 1 | 1 | 0 | |
| Multiracial | 5 | 2 | 3 | |
| Native American | 2 | 1 | 1 | |
| N/A | 42 | 19 | 23 | |
| White | 49 | 25 | 24 | |
| Education, y (Mean, SD) | 10.3 (2.7) | 10.3 (2.7) | 10.2 (2.7) | t = 0.17, p = 0.87 |
| Comorbid Diagnoses, n | ||||
| Mood disorder | 45 | 22 | 23 | X2 = 0.05, p = .83 |
| Bipolar disorder | 6 | 3 | 3 | X2 = 0.01, p = .93 |
| Substance use disorder | 8 | 6 | 2 | X2 = 2.81, p = .42 |
| Obsessive compulsive disorder | 9 | - | 9 | |
| Post-traumatic stress disorder | 3 | - | 3 | |
| Panic disorder | 12 | - | 12 | |
| Agoraphobia | 1 | - | 1 | |
| Social anxiety | 12 | - | 12 | |
| Specific anxiety | 16 | - | 16 | |
| General anxiety | 30 | - | 30 | |
| Somatoform disorder | 5 | - | 5 | |
| Treatment, n | X2 = .65, p = .42 | |||
| Family focused treatment group | 66 | 34 | 32 | |
| Enhanced care treatment group | 63 | 28 | 35 |
Anxiety and no anxiety groups did not differ by descriptives.
2.2 |. Measures
2.2.1 |. Zung Self-rating Anxiety Scale
At pre-treatment, 6 months, and 12 months, individuals completed this 20-item self-report measure of anxiety symptoms as experienced during the previous week (Zung, 1971). Participants rated items, such as ‘I feel more nervous and anxious than usual’ and ‘I feel calm and can sit still easily’, on a 4-point scale, ranging from 1 (None or a little of the time) to 4 (Most or all of the time). A total score of 36 or above suggests the need for an assessment of generalized anxiety disorder (Zung, 1971). The Zung Scale has acceptable construct validity and is widely used (Jegede, 1977).
2.2.2 |. Family interaction task
To evaluate family communication, all families engaged in 10-minute problem-solving interactions (O’Brien et al., 2014). Families were asked to rate how much tension each of 19 topics created in their family on a scale from 1 (low) to 5 (high). Then, therapists asked the individuals at CHR to select a topic that was rated highly and that they would be willing to discuss in the lab. The family was asked to discuss the topic for 10 min and try to reach a resolution. The family interactions were video recorded, later transcribed, and independently coded for negative and positive behaviours by at least two observers.
The percentage of total positive behaviour was calculated by dividing the total number of speaking opportunities during which an individual demonstrated positive behaviours by the total number of times they spoke during the 10-min interaction. Similarly, the percentage of total negative behaviour was calculated by dividing the total number of speaking opportunities during which an individual demonstrated negative behaviours by the total number of times they spoke during the 10-min interaction. Acceptable levels of inter-rater agreement were achieved (with ICCs ranging from 0.61 to 0.86; Shrout & Fleiss, 1979). For a list of behaviour codes and their respective percentages, see Table 1. Additionally, a two-tailed independent samples t-test indicated that there was no difference in the number of speaking opportunities (floor switches; t = −0.361, p = .72) between the CHR youths with (M = 40.54; SD = 21.55) and without anxiety disorders (M = 39; SD = 19.99).
TABLE 1.
Coding categories for the 10-min family problem solving interaction
| Codes | Definition | Example | Mean percentages baseline | Differ by anxiety group? |
|---|---|---|---|---|
| Positive behaviours | ||||
| 1. Affection | Displays of affection; caring, touching | Smiling and patting someone gently on the arm; ‘We are all in this together’. | 0.02 | NS |
| 2. Compliments | Supportive remarks; expressing positive feelings about others' behaviour or attributes | ‘You just provided a really good example’. | 0.01 | NS |
| 3. Mild listening | Minor indication of listening | Saying ‘mm-hm’; nodding head | 0.06 | NS |
| 4. Active listening | Listening empathically, eliciting another's point of view, summarizing, asking follow-up questions | ‘That sounds tough’; ‘Tell me more about that’; ‘Are you mad at Mike all the time or just when he borrows your stuff?’ | .07 | NS |
| 5. Calm speaking | Expressing oneself clearly and concisely in a neutral or positive tone of voice | ‘I think it is reasonable to expect someone your age to be doing their own laundry’. | 0.54 | Anxiety < No Anxiety (p = .04*) |
| Negative behaviours | ||||
| 1. Irritability | Using an irritated tone of voice; withdrawing | ‘Whatever’ | 0.25 | Anxiety > No Anxiety (p = .04*) |
| 2. Anger | Using a markedly angry tone of voice | ‘I said I DON'T want to talk to you anymore!’ | 0.01 | NS |
| 3. Complaints | Complaints, overgeneralizations, demanding or intrusive statements, monologues | ‘Every time I go to sit down at the kitchen table what do I find but your dirty dishes’; ‘You never help’. | 0.05 | NS |
| 4. Criticism | Criticisms | ‘You are so lazy’ | 0.00 | NS |
| 5. Off-task comments | One person goes off on a tangent during the conversation | ‘Hey, they have crayons here’. | 0.09 | NS |
Positive and negative behaviour codes during 10-min family problem solving interaction, along with baseline rates and differences by anxiety group.
2.3 |. Procedure
NAPLS2 participants who expressed interest in a randomized clinical trial of family therapy were recruited between January 2009 and February 2012. Individuals at CHR and their parent(s) or significant others signed informed consent documents and were randomly assigned to an 18-session Family Focused Therapy (FFT-CHR) or to a three-session Enhanced Care protocol (EC) using a modification of Efron’s biased coin-toss procedure. Randomizations were stratified by study site and individuals at CHR’s use of antipsychotic medication. This study was reviewed and approved by the Institutional Review Board at each participating university. For details and a consort flow diagram, see O’Brien et al. (2014) or Miklowitz et al. (2014). Participants were administered a SCID interview at pre-treatment and completed the Zung scale at pre-treatment, 6-month follow-up, and 12-month follow-up. The Family Interaction Task was completed at pre-treatment and 6-month follow-up.
2.3.1 |. Family-focused treatment and enhanced care
Treatment sessions were approximately 50 min in both conditions, and were conducted with each family individually. Therapists who delivered the intervention were primarily doctoral level, with some master’s level therapists. As part of FFT-CHR, approximately six sessions focused on psychoeducation during which the therapist facilitated discussions of the identified patients’ symptoms, daily stressors, and youth and family coping strategies; and developed prevention action plans. These same topics were addressed in an abbreviated manner during the three-session enhanced care (EC) brief psychoeducational treatment. As part of FFT-CHR only, approximately five sessions were dedicated to communication enhancement, with the therapist introducing and modelling a new skill each week, practicing that skill with family members, organizing opportunities for family members to practice the skill with each other in session, providing feedback and coaching to participants, and assigning tasks that required family members to practice the skills between sessions. The following communication skills were introduced routinely: expressing positive feelings, listening actively, making positive requests for change, expressing negative feelings, and communicating clearly. Six additional sessions were devoted to problem-solving training and integration of communication and problem-solving skills. Family members were taught a structured approach that included defining problems, breaking complex problems into a series of smaller problems, brainstorming solutions, analysing pros and cons of possible solutions, and selecting and implementing action plans. (For more information regarding FFT-CHR and EC, see Schlosser et al., 2012). Those with anxiety disorder diagnoses (M = 2.96; SD = 0.21) and without anxiety disorder diagnoses (M = 2.90; SD = 0.44) completed most of the EC treatment (3 sessions) as planned. Similarly, those with anxiety disorder diagnoses (M = 12.96; SD = 5.57) and without anxiety disorder diagnoses (M = 14.38; SD = 4.73) completed the majority of the FFT-CHR treatment (18 sessions).
2.4 |. Statistical analysis
Two-tailed independent samples t-tests were conducted to compare individuals’ behaviours (positive and negative) during family problem-solving interactions across participants with and without anxiety disorders. Follow-up two-tailed independent samples t-tests were conducted to understand the specific interactional behaviours that differed across groups. In a prior report using mixed effects analysis of variance to examine change in problem-solving behaviour as a function of treatment group, O’Brien et al. (2014) found a significant interaction between time and treatment on negative and positive behaviours pre-treatment to 6-month follow-up. In the present report, the presence of a comorbid anxiety disorder at baseline was added into these models. Another mixed effects analysis of variance was conducted to examine changes in self-reported anxiety as a function of treatment group (FFT-CHR vs. EC).
3 |. RESULTS
As displayed in Table 2, there were no significant differences in sociodemographic factors by anxiety disorder status.
Hypothesis 1:
A two-tailed independent samples t-test indicated that participants at CHR for psychosis with comorbid anxiety disorder(s) engaged in negative behaviours at a higher rate during pre-treatment family problem-solving interactions (M = 0.65; SD = 0.48) than did participants at CHR without comorbid anxiety disorder(s) (M = 0.46; SD = 0.42; t = −2.07, p = .04; η2 = 0.041). Additionally, participants at CHR with comorbid anxiety disorder(s) engaged in positive behaviours at a lower rate (M = 0.63; SD = 0.34) than participants at CHR without anxiety disorder(s) (M = 0.77; SD = 0.30; t = 2.15, p = .03; η2 = 0.043). Follow-up two-tailed independent samples t-tests found that irritability and clear speaking were contributing most to the significant results (see Table 1).
Hypothesis 2:
There was a significant interaction between anxiety diagnosis and time on improvement in interactional behaviour, such that those with an anxiety diagnosis showed greater decreases in negative interactional behaviours from baseline to 6-month follow-up (baseline M = 0.61, SE = 0.08; 6-months, M = 0.33, SE = 0.07) than those without an anxiety disorder (baseline M = 0.46, SE = 0.08; 6-months, M = 0.44, SE = 0.07; F[1, 62] = 5.22, p = .03; η2 = 0.077). Those with an anxiety diagnosis also showed greater increases in positive interactional behaviours from baseline to 6-month follow-up (baseline M = 0.68; SE = 0.05; 6-months, M = 0.86; SE = 0.05) than those without an anxiety diagnosis (baseline M = 0.82, SE = 0.05; 6-months, M = 0.83, SE = 0.05; F[1, 62] = 5.04, p = .02; η2 = 0.075). There was not a significant interaction between anxiety diagnosis and treatment group in relation to changes in negative behaviour (F [1, 62] = 1.02, p = .31; η2 = 0.016) or positive behaviour (F[1, 62] = 1.64, p = .20; η2 = 0.025) from pre- to post-treatment. See Figures 1 and 2. For the analysis of change in interaction of behaviour as a function of anxiety disorder and treatment group, we had adequate power (80%) to detect a moderately large effect (Cohen’s f = 0.355, η2 = 0.112).
FIGURE 1.
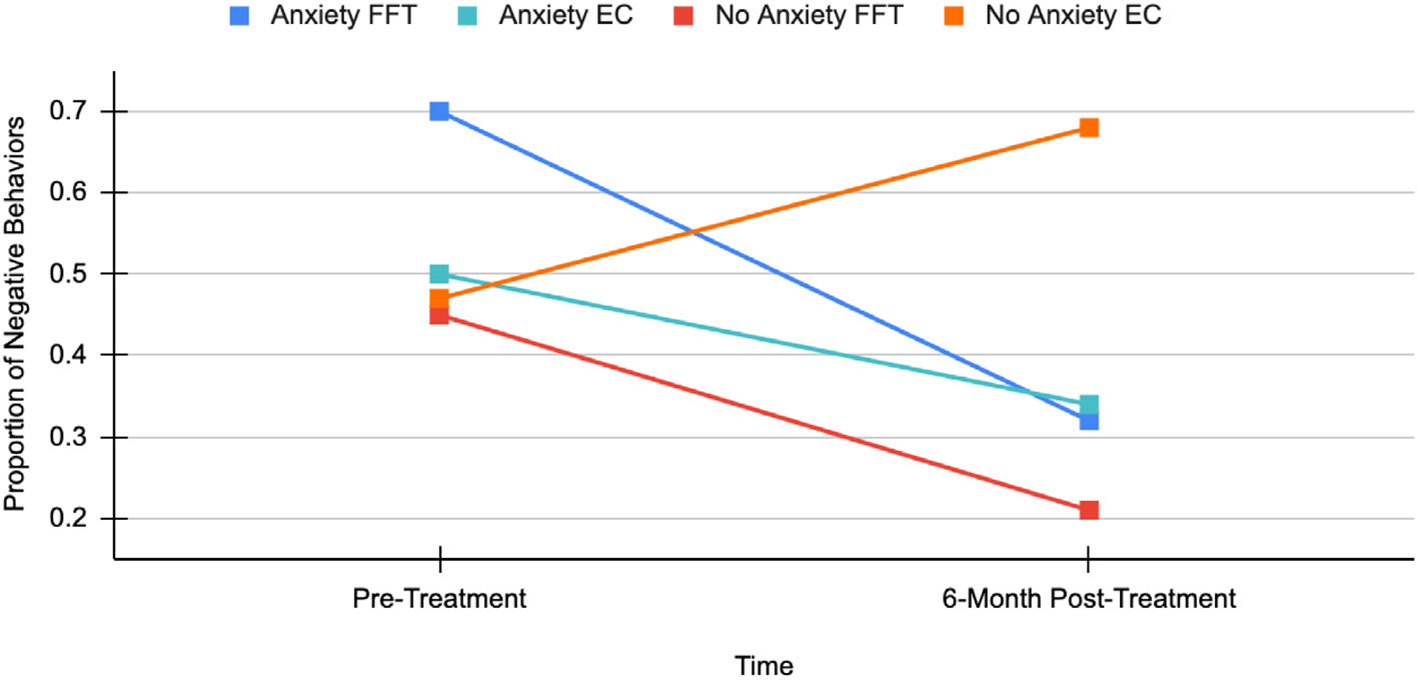
Anxiety disorder by treatment group by time for negative behaviours
FIGURE 2.
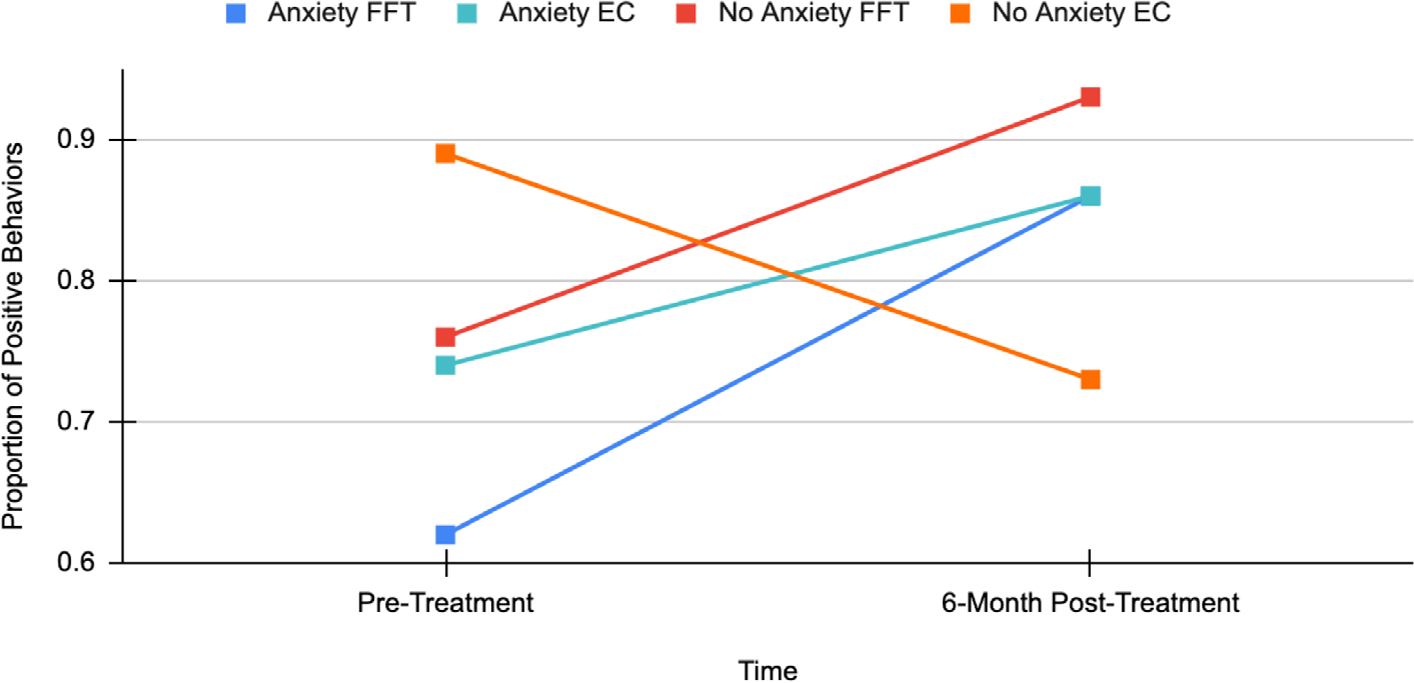
Anxiety disorder by treatment group by time for positive behaviours
Hypothesis 3:
In a mixed effects analysis of variance model with self-reported anxiety as the dependent variable, there was a significant interaction between time (measures at baseline, 6-months and 12-months) and treatment, such that participants’ self-reported anxiety symptoms decreased more in FFT than in EC from pre-treatment to 12-months (F[2, 64] = 4.20, p = .02; η2 = 0.116). There were no significant differences between treatment groups at the 6-month mark. However, at 12-months, those who received EC reported an increase in anxiety symptoms while those who received FFT reported a further reduction of anxiety, compared to the 6-month time point (Figure 3).
FIGURE 3.
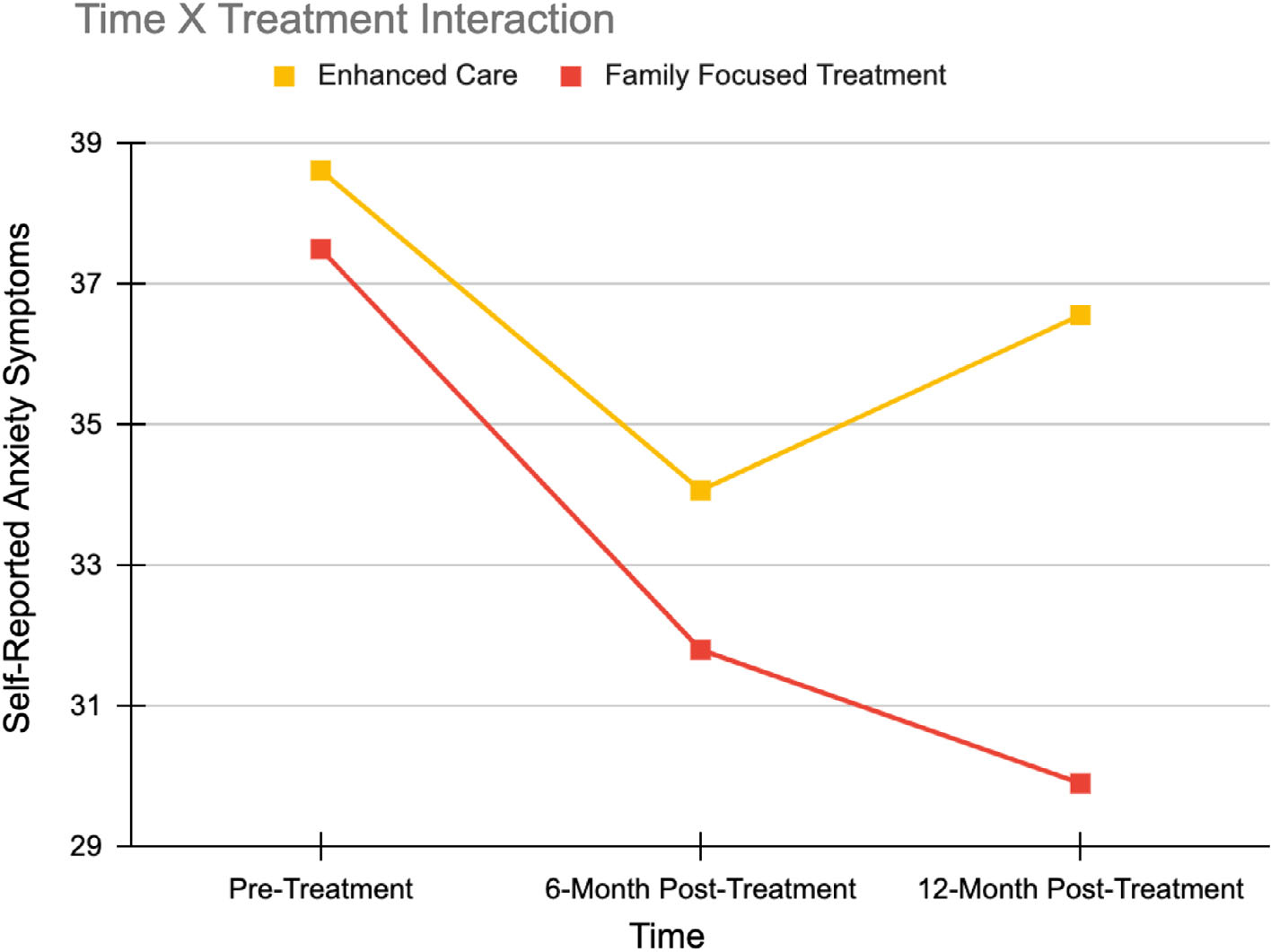
Self-report anxiety symptoms by treatment group from baseline to 12-month follow up
4 |. DISCUSSION
This study is the first to examine family communication behaviours and the efficacy of FFT-CHR for individuals at CHR for psychosis with comorbid anxiety. As predicted, those at CHR for psychosis with a comorbid anxiety disorder engaged in more negative behaviours and less positive behaviours during family problem-solving interactions, as rated by observers at pretreatment, than did those without a comorbid anxiety disorder. Speaking clearly and calmly appeared to be especially difficult for those with a comorbid anxiety diagnosis. Nonetheless, those with anxiety disorders demonstrated greater improvement in their behaviours during family problem-solving interactions at 6-month follow-up than did those without a comorbid anxiety disorder, regardless of treatment. The hypothesis that those with anxiety disorder(s) would be particularly responsive to FFT was not confirmed.
It may be that, for those with anxiety, even a minimal family intervention (family psychoeducation) helped to improve their behaviours, perhaps due to greater family understanding and support facilitated during treatment. Prior research with this CHR sample found that perceived maternal criticism decreased from pre- to post-treatment for both treatment groups (FFT-CHR and EC), lending support to the idea that participation in structured family treatment is associated with improvement in youths’ perceptions of the family environment (O’Brien et al., 2015). Given the higher level of negative communication at pre-treatment among individuals with anxiety disorders, it is also possible that the differential change in these behaviours among this subgroup represents spontaneous recovery or a statistical artefact (regression to the mean) rather than the influences of a treatment programme.
Confirming our hypothesis, self-reported anxiety decreased more in FFT than in EC from pre-treatment to 12-month follow-up. This finding appears to represent a treatment-related effect given that the two treatment groups did not differ in self-reported anxiety at baseline, and the differential improvement among those in the FFT condition grew stronger with time. These findings are similar to a prior study comparing FFT to individual treatment in a bipolar population that found that relapse rates did not differ immediately after 9 months of treatment but were significantly lower for the FFT group in the post-treatment year (Rea et al., 2003). These findings speak to the importance of longer-term follow-up.
The present findings and those from an earlier analysis of this trial, which found that families who were randomized to FFT-CHR demonstrated greater improvement in communication than families who participated in EC (O’Brien et al., 2014), are consistent with theories regarding the family’s ability to maintain youths’ treatment gains due to enhanced family functioning. It is possible that the skill building components of FFT (training in communication skills and problem-solving) lead to more robust improvement in youths’ self-reported anxiety even after active treatment has ended. Of course, it is also possible that the greater length and number of sessions of FFT-CHR treatment rather than the communication and problem-solving components per se could have contributed to the greater improvement in self-reported anxiety within the FFT-CHR group.
Based on self-report, rates of anxiety in this population are high and are responsive to FFT. This intervention which focuses on reducing family stress and enhancing family communication appears to have a secondary benefit of reducing self-reported anxiety despite the primary focus on reducing subthreshold symptoms of psychosis.
These findings must be understood within the context of the limitations of the larger randomized trial. A greater number of sessions provided in FFT than in EC may have given participants a greater degree of exposure to non-specific aspects of therapy, such as social support, hopefulness, and encouragement. Another limitation is that the current sample is not diverse enough to specifically test whether FFT is effective in reducing anxiety across racial and ethnic groups that may be embedded in social contexts with varying levels of stress. Additionally, family interaction was assessed only at pre-treatment and 6-month follow-up. There was a trend towards those with anxiety disorders improving more on constructive communication in FFT than in EC at 6-month assessment (p = .20), but as we see with Hypothesis 3, evaluation at 12-months may have elucidated the potential benefits of FFT-CHR, which teaches skills that strengthen with rehearsal over time. Also, we did not examine whether the behavioural changes demonstrated within the family environment generalize to peer and other significant relationships.
These findings suggest that while a focus on reducing the transition to psychosis is extremely important, given the high base rates of anxiety within this population, reducing these additional facets of suffering also merits further investigation. Additionally, future work could examine whether decreasing anxiety enhances social functioning and strengthens interpersonal supports that may protect against psychotic symptoms.
ACKNOWLEDGEMENTS
This study was supported by a (Challenge Grant RC1 MH088546) to Tyrone Cannon and by a gift to the UCLA Foundation from the International Mental Health Research Organization (IMHRO). Development of the treatment manuals was supported by gifts from the Rinaldi, Lindner and Staglin families. The authors would like to thank the families who participated in this randomized trial; therapists on the project: Ayesha Delany Brumsey, Kristin Candan, Sandra De Silva, Isabel Domingues, Michelle Friedman-Yakoobian, Erin Jones, Stephanie Lord, Nora MacQuarrie, Catherine Marshall, Sarah Marvin, Shauna McManus, Silvia Saade, Danielle Schlosser, Shana Smith, Kathernie Tsai, Miguel Villodas, Barbara Walsh, Kanchana Wijesekera, Kristen Woodberry, and Jamie Zinberg; transcribers and coders: Elizabeth Cabana, Anna Chen, Kelsey Hwang, Zia Kanani, Lynn Leveille, Amber Kincaid, Ashley Kusuma, Grace Lee, Phuong Nguyen, Stefan Nguyen, Christine Sayegh, and Alex Wonnaparhown; and project coordinators: Angie Andaya, Elisa Rodriguez and Serine Uguryan.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Addington J, Farris M, Devoe D, & Metzak P (2020). Progression from being at-risk to psychosis: Next steps. NPJ Schizophrenia, 6(1), 1–7. 10.1038/s41537-020-00117-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Cadenhead KS, Cornblatt BA, Mathalon DH, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Addington JA, & Cannon TD (2012). North American prodrome longitudinal study (NAPLS 2): overview and recruitment. Schizophrenia research, 142(1–3), 77–82. 10.1016/j.schres.2012.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armando M, Pontillo M, De Crescenzo F, Mazzone L, Monducci E, Cascio NL, & Schultze-Lutter F (2015). Twelve-month psychosis-predictive value of the ultra-high risk criteria in children and adolescents. Schizophrenia Research, 169(1–3), 186–192. 10.1016/j.schres.2015.10.033 [DOI] [PubMed] [Google Scholar]
- Barrett PM, Dadds MR, & Rapee RM (1996). Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology, 64(2), 333–342. 10.1037/0022-006X.64.2.333 [DOI] [PubMed] [Google Scholar]
- Bögels SM, & Brechman-Toussaint ML (2006). Family issues in child anxiety: Attachment, family functioning, parental rearing and beliefs. Clinical Psychology Review, 26(7), 834–856. 10.1016/j.cpr.2005.08.001 [DOI] [PubMed] [Google Scholar]
- Butterfield RD, Silk JS, Lee KH, Siegle GS, Dahl RE, Forbes EE, Ryan ND, Hooley JM, & Ladouceur CD (2021). Parents still matter! Parental warmth predicts adolescent brain function and anxiety and depressive symptoms 2 years later. Develoment and Psychopathology, 33, 226–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobham VE, Dadds MR, Spence SH, & McDermott B (2010). Parental anxiety in the treatment of childhood anxiety: A different story three years later. Journal of Clinical Child & Adolescent Psychology, 39(3), 410–420. 10.1080/15374411003691719 [DOI] [PubMed] [Google Scholar]
- Crawford AM, & Manassis K (2001). Familial predictors of treatment outcome in childhood anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 40(10), 1182–1189. 10.1097/00004583-200110000-00012 [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (2002). Structured clinical interview for DSM–IV–TR Axis I disorders: Research version, patient edition (SCID-I/P). New York State Psychiatric Institute. [Google Scholar]
- Fusar-Poli P, Nelson B, Valmaggia L, Yung AR, & McGuire PK (2014). Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: Impact on psychopathology and transition to psychosis. Schizophrenia Bulletin, 40(1), 120–131. 10.1093/schbul/sbs136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, Sawyer SM, & Mathers CD (2011). Global burden of disease in young people aged 10–24 years: A systematic analysis. Lancet, 377(9783), 2093–2102. 10.1016/S0140-6736(11)60512-6 [DOI] [PubMed] [Google Scholar]
- Häfner H, Maurer K, Löffler W, Bustamante S, Van der Heiden W, Riecher-Rössler A, & Nowotny B (1995). Onset and early course of schizophrenia. In Häfner H, & Gattaz WF (Eds.), Search for the causes of schizophrenia (pp. 43–66). Springer. 10.1007/978-3-642-79429-2_3 [DOI] [Google Scholar]
- Hummel RM, & Gross AM (2001). Socially anxious children: An observational study of parent-child interaction. Child & family behavior therapy, 23(3), 19–40. 10.1300/J019v23n03_02 [DOI] [Google Scholar]
- Jegede RO (1977). Psychometric attributes of the self-rating anxiety scale. Psychological Reports, 40(1), 303–306. 10.2466/pr0.1977.40.1.303 [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, & Suveg C (2008). Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology, 76(2), 282–297. 10.1037/0022-006X.76.2.282 [DOI] [PubMed] [Google Scholar]
- Leerkes EM, Bailes LG, & Augustine ME (2020). The intergenerational transmission of emotion socialization. Developmental Psychology, 56(3), 390–402. 10.1037/dev0000753 [DOI] [PubMed] [Google Scholar]
- Lin A, Wood SJ, Nelson B, Beavan A, McGorry P, & Yung AR (2015). Outcomes of nontransitioned cases in a sample at ultra-high risk for psychosis. The American Journal of Psychiatry, 172, 249–258. 10.1176/appi.ajp.2014.13030418 [DOI] [PubMed] [Google Scholar]
- McAusland L, Buchy L, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, & Addington J (2017). Anxiety in youth at clinical high risk for psychosis. Early Intervention in Psychiatry, 11(6), 480–487. 10.1111/eip.12274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlashan T, Walsh B, & Woods S (2010). The psychosis-risk syndrome: Handbook for diagnosis and follow-up. Oxford University Press. [Google Scholar]
- Miklowitz DJ, O’Brien MP, Schlosser DA, Addington J, Candan KA, Marshall C, & Cannon TD (2014). Family-focused treatment for adolescents and young adults at high risk for psychosis: Results of a randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(8), 848–858. 10.1016/j.jaac.2014.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MP, Miklowitz DJ, Candan KA, Marshall C, Domingues I, Walsh BC, & Cannon TD (2014). A randomized trial of family focused therapy with populations at clinical high risk for psychosis: Effects on interactional behavior. Journal of Consulting and Clinical Psychology, 82(1), 90–101. 10.1037/a0034667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MP, Miklowitz DJ, & Cannon TD (2015). Decreases in perceived maternal criticism predict improvement in subthreshold psychotic symptoms in a randomized trial of family-focused therapy for individuals at clinical high risk for psychosis. Journal of Family Psychology, 29(6), 945–951. 10.1037/fam0000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MP, Gordon JL, Bearden CE, Lopez SR, Kopelowicz A, & Cannon TD (2006). Positive family environment predicts improvement in symptoms and social functioning among adolescents at imminent risk for onset of psychosis. Schizophrenia research, 81(2–3), 269–275. 10.1016/j.schres.2005.10.005 [DOI] [PubMed] [Google Scholar]
- O’Brien MP, Zinberg JL, Ho L, Rudd A, Kopelowicz A, Daley M, & Cannon TD (2009). Family problem-solving interactions and 6-month symptomatic and functional outcomes in youth at ultra-high risk for psychosis and with recent onset psychotic symptoms: A longitudinal study. Schizophrenia Research, 107(2–3), 198–205. 10.1016/j.schres.2008.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Thamrin H, & Rozenman MS (2021). Family intervention for child and adolescent anxiety: A meta-analytic review of therapy targets, techniques, and outcomes. Journal of Affective Disorders, 286, 282–295. 10.1016/j.jad.2021.02.053 [DOI] [PubMed] [Google Scholar]
- Perlman SB, Lunkenheimer E, Panlilio C, & Perez-Edgar K (2022). Parent-to-child anxiety transmission through dyadic social dynamics: A dynamic developmental model. Clinical Child and Family Psychology Review, 25, 110–129. 10.1007/s10567-022-00391-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM (1997). Potential role of childrearing practices in the development of anxiety and depression. Clinical Psychology Review, 17(1), 47–67. 10.1016/S0272-7358(96)00040-2 [DOI] [PubMed] [Google Scholar]
- Rea MM, Tompson MC, Miklowitz DJ, Goldstein MJ, Hwang S, & Mintz J (2003). Family-focused treatment versus individual treatment for bipolar disorder: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 71(3), 482–492. 10.1037/0022-006X.71.3.482 [DOI] [PubMed] [Google Scholar]
- Rutigliano G, Valmaggia L, Landi P, Frascarelli M, Cappucciati M, Sear V, & Fusar-Poli P (2016). Persistence or recurrence of non-psychotic comorbid mental disorders associated with 6-year poor functional outcomes in patients at ultra high risk for psychosis. Journal of Affective Disorders, 203, 101–110. 10.1016/j.jad.2016.05.053 [DOI] [PubMed] [Google Scholar]
- Salinger JM, O’Brien MP, Miklowitz DJ, Marvin SE, & Cannon TD (2018). Family communication with teens at clinical high-risk for psychosis or bipolar disorder. Journal of Family Psychology, 32(4), 507–516. 10.1037/fam0000393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlosser DA, Miklowitz DJ, O’Brien MP, De Silva SD, Zinberg JL, & Cannon TD (2012). A randomized trial of family focused treatment for adolescents and young adults at risk for psychosis: Study rationale, design and methods. Early Intervention in Psychiatry, 6(3), 283–291. 10.1111/j.1751-7893.2011.00317.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrock M, & Woodruff-Borden J (2010). Parent-child interactions in anxious families. Child & Family Behavior Therapy, 32(4), 291–310. 10.1080/07317107.2010.515523 [DOI] [Google Scholar]
- Shrout PE, & Fleiss JL (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86, 420–428. 10.1037/0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- Siqueland L, Kendall PC, & Steinberg L (1996). Anxiety in children: Perceived family environments and observed family interaction. Journal of Clinical Child Psychology, 25(2), 225–237. 10.1207/s15374424jccp2502_12 [DOI] [Google Scholar]
- Williams SR, Kertz SJ, Schrock MD, & Woodruff-Borden J (2012). A sequential analysis of parent–child interactions in anxious and nonanxious families. Journal of Clinical Child & Adolescent Psychology, 41(1), 64–74. 10.1080/15374416.2012.632347 [DOI] [PubMed] [Google Scholar]
- Yung AR, & McGorry PD (1996). The prodromal phase of first-episode psychosis: Past and current conceptualizations. Schizophrenia Bulletin, 22(2), 353–370. 10.1093/schbul/22.2.353 [DOI] [PubMed] [Google Scholar]
- Zung WW (1971). A rating instrument for anxiety disorders. Psychosomatics: Journal of Consultation and Liaison Psychiatry, 12, 371–379. 10.1016/S0033-3182(71)71479-0 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


