LEARNING OBJECTIVES
Know the history of Lean, Six Sigma, and DMAIC
Describe the applicability of DMAIC methodology to healthcare
Describe the steps and process tools used in DMAIC
HISTORY OF LEAN, SIX SIGMA, AND DMAIC METHODOLOGY
The term DMAIC, which stands for “define, measure, analyze, improve, and control,” represents a method for process analysis used in Lean Six Sigma. To understand DMAIC methodology, one must first know the history of Lean and Six Sigma. “Lean” production originates from the Toyota Production System introduced in Japan by engineer Taiichi Ohno in the 1950s through 1980s. Lean principles (aspects of which are shaped by Japanese culture and Japanese Zen Buddhism) are designed to permeate every aspect of an organization from company culture and philosophy down to leadership, technology, teamwork, and task standardization.[1] Ultimately, the goal of Lean is to improve efficiency of a process and deliver the best product by eliminating waste.[1] Six Sigma is a Western concept that originated from statistical modeling of manufacturing processes themselves. In the 1920s, Walter Shewhart created the basis for statistical process control with the concept that observed variation in a manufacturing process leads to deviation which results in an unideal product.[2] Furthermore, changing a manufacturing process without proper analysis can worsen variation and result in more defects. Shewhart went on to work with physicist Edwards Deming to develop the “Plan Do Study Act” (PDSA) cycle in the 1930s.[3] These concepts were applied by engineer Bill Smith in the 1980s to reduce process variation at Motorola and were coined, “Six Sigma.” [2] “Lean Six Sigma” combines the principles of both Lean and Six Sigma with the overarching goal to reduce both waste and variation within a system using data and continuous quality improvement. To reduce variation in a process, Six Sigma utilizes statistical analysis through a 5-step approach called the DMAIC method.
APPLICATION OF SIX SIGMA AND DMAIC IN HEALTHCARE
Six Sigma and the DMAIC method originated in the manufacturing industry; however, by the late 1990s several healthcare organizations had adopted these concepts to improve patient safety and healthcare delivery.[4] Challenges exist when implementing DMAIC methodology into a dynamic multifaceted health system. Unlike the production line in a factory, a health system is not delivering a singular standardized product and patients are not the only consumers. Healthcare professionals may bristle at the notion of standardization, believing it will limit their autonomy to make decisions.[5] Gold-standards and medical recommendations may exist, but often with variation in strength of evidence; these are meant not as hard rules but rather as a guide in conjunction with clinical judgment. These qualities of patient care make removal of variation difficult; however, ample opportunities appropriate for standardization still exist. Lean Six Sigma concepts have been applied successfully to improve these various aspects of patient care. In a recent systematic review from 2020, Ninerola and colleagues identified 196 manuscripts outlining Six Sigma use in the healthcare sector.[6] Most of these originated from the United States and were published case studies. Multiple specialties and services have used these methods to standardize and improve one or more processes. For example, Six Sigma methodologies using DMAIC have been used to reduce wait times for radiology results, improve the safe administration of medications, and decrease unnecessary antibiotic use.[7–9]
STEPS OF DMAIC
Figure 1 is adapted from recent publications discussing the use of DMAIC in healthcare and outlines the steps and process tools involved.[9,10] One advantage to DMAIC methodology compared to PDSA cycles (also known as the Deming or Shewhart cycle) is that a more robust preparation of measurement and analysis occurs before any change or improvements are proposed. Change is not proposed until step 4 of 5 (as opposed to step 2 of the PDSA cycle). Additionally, process control is required as a built-in final step, which may help impart lasting change regardless of whether the cycle is repeated.
Figure 1.
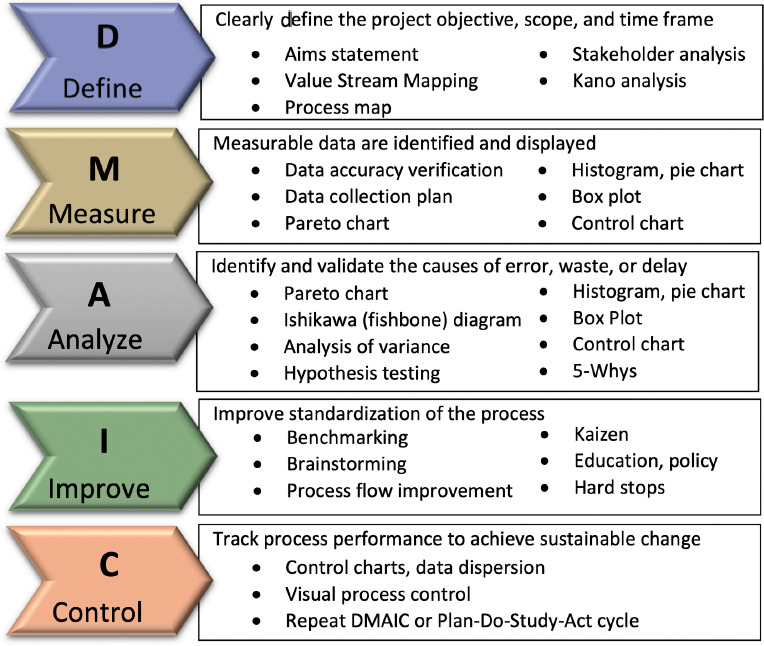
Define, measure, analyze, improve, control (DMAIC) methodology and process tools[9,10]
Step 1: Define
In the define phase, stakeholders must clearly define the project objective, scope, and if possible, the time frame. Stakeholders must agree on what the target of the project is, as well as its duration. This may include a process map or other analysis (Financial, Stakeholder, or Kano analysis), to develop an aims statement.
Step 2: Measure
Measurable data to serve as quality or safety indicators are identified. This may require conducting data collection to establish baseline metrics. Data extracted from aggregate databases should be analyzed for accuracy. Data should be able to be displayed visually for subsequent analysis. Box plots, pareto charts, control charts, or histograms may be used which will subsequently be used in further steps. An exemption from the institutional review board can usually be obtained for data being used for quality improvement.
Step 3: Analyze
This step merges what is known about the process as well as the baseline data to identify and validate the causes of errors, deviation, delays, waste, or other etiologies of defects in the process. Analysis may include pareto diagrams, histograms, pie charts, Ishikawa (fishbone) diagrams, a 5-whys analysis, or other tools to explore cause and effect.
Step 4: Improve
In this phase, the team works to address the root cause and make changes to eliminate the issues leading to variability and waste in the process. Communication with team members and team involvement and commitment is parament. Stakeholders should be comfortable brainstorming and using clear and regular communication about potential solutions. Various stakeholders may disagree about who or what needs to change to reach the targeted goal. National benchmarking and discussion of established best practices may be needed. Keep in mind that interventions relying on human memory (education, pocket cards, policy changes, email reminders) may be appropriate, but will be weaker than those that are tied directly to process flow (hard stops in ordering, electronic alerts). The concept of Kaizen (a Japanese term meaning, “change for the better”) can help ground the group in the idea that improved operations should involve all employees and are continuous and methodical process.[11]
Step 5: Control
The control phase is crucial to achieving sustainable change and requires tracking process performance. A process control plan usually builds on the new ideal process map indicating who is responsible for each aspect of the new process. The team must be aware of new potential problems that could arise because of work arounds, design flaws, or resistance to process change. Ongoing control charts can monitor variation. Team members must be aware of the metrics on a regular basis so that “out of control” performance can be corrected, and the control plan can be updated. How often team members are updated (daily, weekly, annually, etcetera) is dependent on the metric being tracked and the amount of time required to gather and/or verify the data.
CONCLUSION
DMAIC can serve as a roadmap to apply the Lean Six Sigma philosophy and improve a process even in a complex field such as healthcare. Involving the relevant stakeholders and building in long-term plans for process control are crucial to its applicability and sustainability.
Funding Statement
Source of support: None.
Footnotes
Conflict of interest: None.
References
- 1.Chiarini A, Baccarani C, Vittorio M. Lean production, Toyota Production System and Kaizen philosophy: A conceptual analysis from the perspective of Zen Buddhism. TQM J . 2018;30:425–438. [Google Scholar]
- 2.Dahlgaard JJ, Dahlgaard-Park SM. Lean production, Six sigma quality, TQM and company culture. The TQM Magazine . 2006;18:263–281. [Google Scholar]
- 3.Harolds J. Quality and safety in health care, part I: Five pioneers in quality. Clin Nucl Med . 2015;40:660–662. doi: 10.1097/RLU.0000000000000877. [DOI] [PubMed] [Google Scholar]
- 4.Chassin MR. Is health care ready for Six Sigma quality. Milbank Q . 1998;76(4) doi: 10.1111/1468-0009.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Llody R. Does standardization mean the end of autonomy? Why it matters standardization for health care improvement does not mean practicing “cookbook medicine.”. Institute for Healthcare Improvement Nov 8, 2018 Accessed Mar 20, 2022. www.ihi.org/communities/blogs/does-standardization-mean-the-end-of-autonomy .
- 6.Niñerola A, Sánchez-Rebull MV, Hernández-Lara AB. Quality improvement in healthcare: six sigma systematic review. Health Policy . 2020;124:438–445. doi: 10.1016/j.healthpol.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Cavagna E, Berletti R, Schiavon F, Scarsi B, Barbato G. Optimized delivery radiological reports: applying Six Sigma methodology to a radiology department. Radiol Med (Torino) . 2003;105:205–214. [PubMed] [Google Scholar]
- 8.Castle L, Franzblau-Isaac E, Paulsen J. Using six sigma to reduce medication errors in a home-delivery pharmacy service. Jt Comm J Qual Patient Saf . 2005;31:319–324. doi: 10.1016/s1553-7250(05)31041-5. [DOI] [PubMed] [Google Scholar]
- 9.Monday LM, Yazdanpaneh O, Sokolowski C, et al. A physician-driven quality improvement stewardship intervention using lean six sigma improves patient care for community-acquired pneumonia. Glob J Qual Saf Healthc . 2021;4:109–116. doi: 10.36401/JQSH-21-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed S. Integrating DMAIC approach of lean six sigma and theory of constraints toward quality improvement in healthcare. Rev Environ Health . 2019;34:427–434. doi: 10.1515/reveh-2019-0003. [DOI] [PubMed] [Google Scholar]
- 11.Yamada S. Are you ready for kaizen in your clinical practice. Circ J . 2020;84:546–548. doi: 10.1253/circj.CJ-20-0087. [DOI] [PubMed] [Google Scholar]


