Learning Objectives
Understand the importance of patient safety in medical care
Explain the role of proactive risk management methods in patient safety
Know the applications, process, and types of failure mode and effects analysis (FMEA) as a risk management tool
Understand the Importance of Patient Safety in Medical Care
Patient safety has become a strategic pillar in healthcare organizations, requiring significant resources to avoid accidents during the hospital stay. Patient care processes are documented precisely in detailed policy and procedure manuals. The expectation has been that competent healthcare providers, acting per defined policies and procedures, will create a safe environment for patients.[1] This expectation, although laudable, has proven to be unrealistic. Safety studies in healthcare and other socio-technological industries have repeatedly demonstrated that human error is the cause of many accidents in complex systems.[1] Because the error is inherent to human nature, its consequences must be minimized. Healthcare may create risks, and patient safety is the most important care quality objective.[2]
The importance of patient safety, or protecting patients from harm incurred in medical care, is a topic of much discussion, which has been demonstrated in various international and national publications since the late 1990s.[3,4] Most reporting systems concentrate on analyzing adverse events; this means that injury has already occurred.[3] More progressive systems also concentrate on analyzing close calls, which facilitates learning from an event that did not result in injury or harm to a patient. Systems also permit proactive evaluation of vulnerabilities before close calls occur.[3,5]
Proactive Risk Management Methods in Patient Safety
Risk management is a process-oriented method that provides a structured framework for identifying, assessing, and reducing risk within an organization. In the medical industry, risk management tools can assist organizations in improving the effectiveness of care delivery and protect healthcare providers.[6,7] Examples of risk management tools include failure mode and effect analysis (FMEA), root cause analysis (RCA), bow-tie model, and hazard and operability analysis (HAZOP).[8–12] These tools can positively impact patient safety and quality of care rather than simply addressing potential losses due to litigation.[7,13]
In general, proactive risk management methods are system-based approaches that are broadly and successfully utilized in other safety-critical industries, including chemical and aerospace industries.[7] Healthcare can potentially be improved by learning from the experiences and methods used in other safety-critical industries to proactively identify a comprehensive list of risks. Because the nature of health systems is dynamic and complex, a proactive system-based approach is crucial to optimize patient safety and quality of care.[14]
Much of what needs to be done to improve patient safety is already being done in other industries. When the United States Joint Commission on Accreditation of Healthcare Organizations (JCAHO) considered standardizing changes to encourage a proactive approach to risk reduction, they researched various safety improvement techniques used in other high-risk industries to find one that would be adaptable to healthcare services.[1]
Application of Failure Mode and Effects Analysis (FMEA)
Although more than a hundred system-based approaches are used in a range of safety-critical industries, most methods have not been applied in the healthcare field.[9] From such methods, FMEA has gotten greater recognition in healthcare since the 1990s, and it is currently one of the most widely known and practiced proactive risk assessment tools.[15]
FMEA is an analytical method that has been used for decades in engineering to identify and reduce hazards. This process examines the individual components of a system to determine the variety of ways each component could fail and the effect of a particular failure on the stability of the entire system. FMEA focuses on manufacturing processes and involves calculating a risk priority number through a three-variable equation where each variable is scored from 1 to 10. Medical device manufacturers use this process when evaluating their equipment.[3]
There are two types of FMEA methods: design FMEA and process FMEA. It is common to find both methods used in manufacturing, aviation, computer software design, and other industries to evaluate system safety.[1] Modified FMEA methods have been developed; these include failure mode effects and criticality analysis (FMECA) (3) and healthcare failure mode and effect analysis (HFMEA).[16] HFMEA was developed by the United States Department of Veterans Affairs' National Center for Patient Safety (NCPS) in 2002 by combining concepts, components, and definitions from FMEA, hazard analysis and critical control point (HACCP), and root cause analysis.[3] This method was designed to enable healthcare organizations to evaluate and improve healthcare processes before actual incidents occur.[16]
The application of FMEA in the healthcare sector has been slow despite its strong implementation in the industrial arena.[2] FMEA has been adopted to assess risks and identify areas that need improvement in the healthcare system.[17] The United Kingdom National Patient Safety Agency recommends applying FMEA to assess new policies and procedures before implementing them.[18] The JCAHO has asked its accredited institutes to carry out an annual proactive risk assessment study such as FMEA.[17,18] Results of the FMEA process aid in establishing priority actions for improvement and failure-prevention countermeasures (Figure 1).[2,19]
Figure 1.
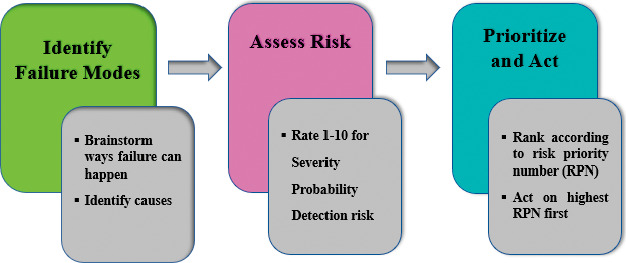
Failure mode and effects analysis (FMEA) process.
An example of how FMEA has been used to prevent medical errors or reduce risk is reported by Anjalee et al.[17] The study consisted of two independent teams of pharmacists at a teaching hospital in Sri Lanka who conducted the FMEA over a 2-month period. Each team had five meetings of 2 hours each, where the dispensing process and sub-processes were mapped, and possible failure modes, their effects, and their causes were identified. A score for potential severity (S), frequency (F), and detectability (D) was assigned for each failure mode. Both teams identified 90 failure modes and prioritized 66 of them for corrective action using the scores. They identified overcrowded dispensing counters as a cause for 57 failure modes. Redesigning of dispensing tables, dispensing labels, the dispensing and medication re-packing processes, and establishing a patient counseling unit were the major suggestions for correction.[17]
Summary
The FMEA technique is easy to use and an efficient tool for identifying potential failures to increase the reliability and safety of complex systems. Also, this technique is useful for gathering data for decision-making and proactive risk control. In a healthcare setting, FMEA can aid in avoiding or reducing the medical errors that cause patient harm.
Funding Statement
Source of support: None.
Footnotes
Conflicts of interest: None.
References
- 1.Spath PL. Using failure mode and effects analysis to improve patient safety. AORN J . 2003 Jul;78:14–16. doi: 10.1016/s0001-2092(06)61343-4. [DOI] [PubMed] [Google Scholar]
- 2.Vázquez-Valencia A, Sáez AS, Perea Pérez B, et al. Usefulness of failure mode and effects analysis for improving mobilization safety in critically ill patients. Colomb J Anesthesiol . 2018;46(1 SE-Original):3–10. [Google Scholar]
- 3.DeRosier J, Stalhandske E, Bagian JP, Nudell T. Using health care failure mode and effect analysis: the VA National Center for Patient Safety's prospective risk analysis system. Jt Comm J Qual Improv . 2002;28:248–267. doi: 10.1016/s1070-3241(02)28025-6. 209. [DOI] [PubMed] [Google Scholar]
- 4.Merino P, Álvarez J, Cruz Martín M, et al. Adverse events in Spanish intensive care units: the SYREC study. Int J Qual Heal Care . 2012;24:105–113. doi: 10.1093/intqhc/mzr083. [DOI] [PubMed] [Google Scholar]
- 5.Thornton E, Brook O, Mendiratta-Lala M, et al. Application of failure mode and effect analysis in a radiology department. Radiographics . 2010;31:281–293. doi: 10.1148/rg.311105018. [DOI] [PubMed] [Google Scholar]
- 6.Ferdosi M, Rezayatmand R, Molavi Taleghani Y. Risk management in executive levels of healthcare organizations: insights from a scoping review (2018) Risk Manag Healthc Policy . 2020;13:215–243. doi: 10.2147/RMHP.S231712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGowan J, Wojahn A, Nicolini JR. Risk Management Event Evaluation and Responsibilities . StatPearls; 2022. [PubMed] [Google Scholar]
- 8.Rezaei F, Yarmohammadian MH, Haghshenas A, et al. Revised risk priority number in failure mode and effects analysis model from the perspective of healthcare system. Int J Prev Med . 2018;9:7. doi: 10.4103/2008-7802.224046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trucco P, Cavallin M. A quantitative approach to clinical risk assessment: The CREA method. Saf Sci . 2006;44:491–513. [Google Scholar]
- 10.Abdi Z, Ravaghi H, Abbasi M, et al. Application of Bow-tie methodology to improve patient safety. Int J Health Care Qual Assur . 2016;29:425–440. doi: 10.1108/IJHCQA-10-2015-0121. [DOI] [PubMed] [Google Scholar]
- 11.Taleghani YM, Rezaei F, Sheikhbardsiri H. Risk assessment of the emergency processes: healthcare failure mode and effect analysis. World J Emerg Med . 2016;7:97–105. doi: 10.5847/wjem.j.1920-8642.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prijatelj V, Rajkovič V, Šušteršič O. A model for risk assessment in health care using a health care failure method and effect analysis. Slov J Public Heal . 2013;52:316–331. [Google Scholar]
- 13.Simsekler MCE, Kaya GK, Ward JR, Clarkson PJ. Evaluating inputs of failure modes and effects analysis in identifying patient safety risks. Int J Health Care Qual Assur . 2019;32:191–207. doi: 10.1108/IJHCQA-12-2017-0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, et al. Human factors systems approach to healthcare quality and patient safety. Appl Ergon . 2014;45:14–25. doi: 10.1016/j.apergo.2013.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ward J, Clarkson J, Buckle P, et al. Prospective hazard analysis: tailoring prospective methods to a healthcare context. University of Cambridge repository. 2010. [DOI]
- 16.Habraken MMP, Van der Schaaf TW, Leistikow IP, Reijnders-Thijssen PMJ. Prospective risk analysis of health care processes: a systematic evaluation of the use of HFMEA in Dutch health care. Ergonomics . 2009;52:809–819. doi: 10.1080/00140130802578563. [DOI] [PubMed] [Google Scholar]
- 17.Anjalee JAL, Rutter V, Samaranayake NR. Application of failure mode and effects analysis (FMEA) to improve medication safety in the dispensing process – a study at a teaching hospital, Sri Lanka. BMC Public Health . 2021;21:1430. doi: 10.1186/s12889-021-11369-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shebl NA, Franklin BD, Barber N. Is failure mode and effect analysis reliable. J Patient Saf . 2009;5:86–94. doi: 10.1097/PTS.0b013e3181a6f040. [DOI] [PubMed] [Google Scholar]
- 19.Juan JM, Godfrey AB, Hoogstoel RE, Schilling EG. Juran's Quality Handbook 5th ed . McGraw-Hill; 1999. [Google Scholar]


