Abstract
Self-injurious behavior (SIB) by individuals with intellectual and developmental disabilities including autism (I/DD) is among the most clinically disturbing, socially costly, and scientifically challenging behavior disorders. Forty years of clinical research has produced a knowledge base supporting idiographic behavioral assessment and treatment approaches. Despite the treatment progress, from a public health and population perspective, we argue it is less clear that we have reduced the disorder’s burden. The developmental course of the disorder is mostly unknown and empirically informed population-level models of risk are absent. In this review, we systematically examined the published scientific literature specific to risk for SIB in the I/DD population. We reviewed study methodology in detail intentionally informed by an epidemiological perspective with a set of questions intended to test the quality of the inferences about risk. Results are discussed in terms of conceptual, methodological, and translational issues with respect to what needs to be done to create credible and useful clinical models for SIB risk in the I/DD population.
Keywords: Self-injurious behavior, Longitudinal studies, Prospective cohort, Intellectual/developmental disabilities
1. Introduction
Self-injurious behavior (SIB) is among the most severe behavior disorders for individuals living with intellectual disability and associated developmental disabilities and disorders including autism (I/DD). Lifetime prevalence estimates vary from 5 to 20% of the population with I/DD and higher in autism spectrum disorders (ASD) in some studies, ranging from 30%–50% (Baghdadli, Pascal, Grisi, & Aussilloux, 2003; Soke et al., 2016). The forms or topographies are as varied as the different ways in which one could physically inflict damage to oneself including but not limited to head-hitting, head-banging, self-biting, self-scratching, skin picking, and eye gouging with varying degrees of tissue damage and trauma. Severe SIB permanently scars, detaches retinas, and, in extreme cases, causes death (Nissen & Haveman, 1997). Self-injury can be highly treatment-resistant and the cost of care is considerable. Over three decades ago, an NIH Consensus panel estimated expenditures associated with SIB and other forms of associated destructive behavior to be $3 billion nationally (National Institutes of Health, 1991). There is little reason to think the prevalence estimates have changed but assuredly the costs of care have. Quality of life is significantly reduced for individuals who chronically self-injure as well as for their families (Rojahn, Schroeder, & Hoch, 2008). The myriad issues associated with SIB collectively considered attest to its public health significance.
1.1. SIB risk factors: conventional wisdom from conventional approaches
In terms of identified SIB risk factors (i.e., a factor that directly increases the probability of SIB emerging and is part of a causal chain) and risk markers for SIB (i.e., an attribute that is associated with increased probability of SIB, but is not necessarily causal; Burt, 2001), there are disparate findings and data primarily specific to the latter. It is apparent, though, that within the neurodevelopmental disability literature the terms ‘risk factor’ and ‘risk marker’ tend to be used interchangeably. The tendency to use the terms as if they mean the same thing is problematic because each requires different types of evidence from data generated by different methodological approaches. The available findings on risk markers and factors for SIB are described and summarized succinctly below for both adults and children with or at risk for I/DD.
Previous risk markers found to be associated with SIB in adults with I/DD in a meta-analysis include deficits in intellectual and adaptive skills, expressive and receptive communication deficits, and a diagnosis of autism spectrum disorder (ASD) (McClintock, Hall, & Oliver, 2003). Other risk markers for SIB in adult I/DD populations include stereotypy (Bodfish, Crawford, Powell, Parker, et al., 1995; Gal, Dyck, & Passmore, 2009), and primary sensory impairments (Jan, Good, Freeman, & Espezel, 1994). Among other cross-sectional samples of individuals with ASD, SIB was associated with higher levels of hyperactivity, impulsivity, lower intellectual functioning, negative affect, and impulsive speech (Richards, Oliver, Nelson, & Moss, 2012). Similarly, in child and adolescent samples, high frequency repetitive or ritualistic behavior was associated with a 16 times greater risk of severe self-injury among a similar cross-sectional sample of 4–18 year olds with severe intellectual disabilities (Oliver, Petty, Ruddick, & Bacarese-Hamilton, 2012). In most cases, however, the risk markers identified were based on relatively heterogeneous older or adult samples primarily with established SIB and were not necessarily specific to the development or emergence of SIB.
In contrast, the research to date on risk markers for SIB onset among children with developmental disabilities and children at risk is more limited. Kurtz et al. (2003), and Richman and Lindauer (2005) reported that both SIB and proto-SIB (i.e., engaging in topographies similar to SIB but without causing tissue damage) can emerge before or by 25 months of age. When conventional-wisdom risk markers identified in adult I/DD populations are examined for young children with or at risk for I/DD (< age 5), it is not clear that they are reliably associated with SIB. For example, MacLean, Tervo, Hoch, Tervo, and Symons (2010) conducted a retrospective chart review of a clinical sample of 196 children with or at risk for a developmental disability. Children with and without SIB did not differ on developmental level, language level, mobility status, sensory functioning, or in rates of cerebral palsy, seizure disorders, or autism indicating that these variables were not associated with SIB. These findings were replicated by the same group (Hoch, Spofford, Dimian, Tervo, & Symons, 2015) but independent replication of these findings are needed. The MacLean et al. and Hoch et al. findings seem to suggest that SIB early in development may be qualitatively different than SIB observed later among adults with I/DD. There are severity and intensity differences, but the phenomenon itself may be different (if for no other reason than measurement artefact – a parent-endorsed SIB item for a 3 -year old and a group-home staff endorsed SIB item for a 28 year old may not necessarily reflect the same ‘thing’ – a conceptual and measurement point we will revisit in the Discussion).
Overall, the majority of studies from which the field has relied on to make claims about risk use cross-sectional designs oriented toward prevalence (not incidence) estimates and shed little light on developmental pathways or mechanisms for the early development of SIB and the factors conferring risk. The dominant research strategies tend to reflect a variable-oriented approach – which can be important to understanding what is expected at a group level. Such approaches may be considered ‘first-generation’ in that they are establishing important relations among variables in samples representative of populations of interest. Informed, at least in part, from variable-oriented approaches, but in contrast, would be pathway-oriented approaches investigating the different ‘routes’ by which the outcome of interest occurred while trying to accommodate individual differences. The focus of this review, however, is on the longitudinal work that has been conducted within I/DD to evaluate our understanding of risk pathways to SIB.
1.2. SIB state of the science: where are we and where do we need to be?
In the past 4 decades, advances in our understanding of SIB among individuals with I/DD have resulted in robust behavioral assessment technology and a set of evidence-based intervention practices (Rojahn et al., 2008). Functional analysis technology, based on the conceptual work of Carr (1977) and the pioneering work of Iwata et al. (1982/1994), lead to efficacious direct behavioral interventions because they target the operant mechanism maintaining SIB. Notably, however, for a significant minority of individuals learned reinforcement mechanisms appear to be absent (or, at least, difficult to document) making it much more difficult to design targeted behavioral interventions. Pharmacologically, despite theoretically plausible predictions, and evidence for responders during trials, we still do not have any proven tailoring variables to guide medication selection (Symons, Thompson, & Rodriguez, 2004).
There is little epidemiological evidence that the burden of the condition has been reduced (i.e., no reduction in incidence). As noted above, the majority of the prevalence findings have been cross-sectional, descriptive, and specific to adults although there are increasingly studies based on children. The state of the scientific knowledge about risk for the development of SIB in I/DD is limited, but longitudinal investigations have been accumulating (Symons & Devine, 2013). Psychosocial, developmental, and biological correlates of SIB are documented, but there is little corresponding knowledge concerning causal mechanisms and the pathophysiological pathways to developing the disorder. The term ‘risk’ and ‘risk factor’ appear to have been used descriptively in SIB research with respect to correlational patterns, but rarely applied in an epidemiological sense of understanding mechanisms conferring relative risk for the disorder.
Theoretically, the bulk of the SIB research has proceeded with little attention directed toward models of vulnerability and individual differences. From a broader epidemiological perspective, SIB research appears stuck in the risk factor stage because it appears so few studies use designs that are able to document causality or, at least, approximate it. In some cases, we know what statistically predicts SIB, but not how or why. Considering the enormous costs associated with chronic SIB, in Terrie Moffitt’s words “the cost of getting causation wrong is not trivial” (Moffitt, 2005; writing about developmental psychopathology and antisocial behavior). So, how do we get causation for SIB in I/DD right? One missing puzzle piece concerns population-based approaches to model risk that would, if designed correctly, provide empirical estimates of incidence and clarify the causal status of the putative risk factors. This issue –modeling and estimating risk for SIB in I/DD, particularly how to do so - forms the basis for the systematic literature review described in this paper.
1.3. Measuring and modeling early development of SIB – A framework for building epidemiologically credible evidence
Despite 4 decades of assessment and treatment research, the focus on the early development of SIB is relatively recent. The rationale is clear and compelling. Identifying the causal agents and contributing risk factors for SIB development would help researchers and clinicians create comprehensive models for SIB risk across the lifespan. Such models would have implications for early intervention and prevention. A prevention approach to SIB could be cost-effective and ultimately help ameliorate the extreme limiting effects SIB has on quality of life for affected individuals and their families. Prevention programming targeting SIB development, however, requires data on risk. The specific goal of the current review was to examine critically the longitudinal literature on risk factors for SIB among people with I/DD conducted through an epidemiological framework.
In general, the field of epidemiology is concerned primarily with the distribution and frequency of disease in a given population (Aschengrau & Seage, 2014). Risk is the probability of the occurrence of a disease or a condition over a period of time. At a population level, there are three core issues to consider in terms of a condition’s base rate. The first is the number of people affected by the condition. The second is the size of the population from which the cases of condition arise. The third is the length of time that the population is followed. Impact of the condition can be mischaracterized if one of the above issues is not properly delineated, defined, and subsequently measured (Aschengrau & Seage, 2014). How a condition is characterized and quantified in terms of burden is important for evaluating the effects of interventions and prevention trials.
Prevalence and incidence provide estimates of a condition’s frequency to determine how common a condition is in a given population. Prevalence is an estimate of the number of existing cases of the condition. Incidence is the occurrence of new cases of the condition that develop in a population over a specified time period (e.g., new cases of SIB over a specified period of time) (Aschengrau & Seage, 2014). New cases of the condition are measured within a population of people who are at risk for the condition (e.g., in the population of children with developmental delays). Incidence takes into account the specific amount of time that the members of the population are followed until they develop the condition. The amount of time is important for making inferences about possible risk factors that lead to the development of the condition (Aschengrau & Seage, 2014). There is a close connection between prevalence and incidence in that prevalence depends on the rate of new cases and the duration of time individuals have the condition (i.e., persist engaging in SIB; P═I × D). The duration ends when the person dies, is cured, or in remission (or, for SIB, the individual no longer self-injures).
Incidence is most useful for evaluating the effectiveness of programs that try to prevent conditions from occurring in the first place. Prevalence tends to complicate the identification of causal relationships because it combines incidence and survival rates/duration (i.e., new cases and people cured). Temporal relationships are discernable from incidence, but not from prevalence estimates. Prevalence is useful for estimating the needs of tertiary treatment facilities (like hospitals) and for allocating resources for treating people. Cumulative incidence proportions (relative risk) and incidence rate proportions (i.e., taking into account follow along time until a person develops the condition) help identify potential risk factors where the incidence of disease is compared between exposed and unexposed groups (exposure to the putative risk variable). Relative risk (RR) is often used within epidemiology to distinguish the strength of the relationship between an exposure/risk factor and a condition/outcome (Aschengrau & Seage, 2014). Put another way, RR tells us how many times more likely an outcome (e.g., SIB) occurs among individuals with the exposure to the potential risk factor (Viera, 2008). The aforementioned concepts and terms will be used throughout the remainder of the review to frame the relevant SIB work in an epidemiological perspective.
1.4. Review goal: what do the retrospective/prospective SIB risk studies show?
As stated, our overall goal is to revisit and review the concept of SIB risk by applying an epidemiological framework to identify as clearly as possible the variables that have or have not been established as risk markers or factors for SIB in I/DD. Additionally, we aimed to synthesize the wide range studies on SIB risk factors and their findings. Our approach was as follows. First, identify the retrospective and prospective studies specific to SIB in I/DD samples or samples at risk for I/DD. Then, review each using a framework informed by general observational study design approaches that support deriving risk estimates. Finally, address a set of questions about the scientific rigor and quality of the risk evidence in relation to the nature of the design used. The specific purpose was to answer the following questions by synthesizing studies on SIB risk with a cohort or longitudinal design: (1) of the prospective and retrospective cohort studies in the literature, what are the potential risk markers or factors identified for SIB, (2) among the prospective SIB cohort studies, were incidence and RR estimates reported, and (3) what are the common risk factors identified in the literature to date?
2. Method
We searched three literature databases (PsychINFO, PubMed, & Academic Search Premier) using the following terms: self-injurious behavior or self-injury (self-injur*, self-injurious behav*, self-injurious behavior, self-harm*, self- destructive behave*) in combination with intellectual disability, IDD, Autism spectrum disorder/ autis*, ASD, Asperger, Pervasive developmental disorder not otherwise specified, PDD-NOS, developmental delay, DD, genetic linked intellectual diabili*, Fragile X, developmental disability, risk factors, risk markers, or risk*, correlates, and prospective, retrospective and or longitudinal (e.g., self-injurious behavior AND developmental disabilities AND risk). The first author also conducted ancestral searches with the publications that met the selection criteria in the following section.
2.1. Selection criteria and analysis
The inclusion/exclusion criteria applied to identified articles were as follows: (a) study conducted between January 1970 and January 2022, (b) study was empirically based and peer-reviewed, (c) the study design included a prospective cohort, retrospective cohort, or longitudinal design with at least 2 months of follow up and two time points, (d) the study included a measure of SIB and (e) the participants were at risk for or were diagnosed with an intellectual or developmental disability (e.g., autism, developmental delay). Treatment only studies were excluded as were studies with participants labeled with psychiatric diagnosis only without including information about intellectual and developmental level/function.
Fig. 1 displays the search process for identifying the included articles. The initial electronic search using the search terms yielded 185 results. The first author reviewed the initial search results (title, abstracts, headings) for studies explicitly focusing on SIB among individuals with or at risk for I/DD. Ancestral searches of the articles were conducted. Sixty-four articles potentially met the criteria for inclusion and were subjected to further detailed review and coding. Of these, 28 articles met the full inclusion criteria. Inter-rater agreement (IRA) checks were conducted for the initial 54 studies reviewed based on the electronic literature search and ancestral search. Two independent coders reviewed the abstracts for the selection criteria stated above. IRA (number of agreements divided by number of agreements plus disagreements and multiplying by 100) was 93%.
Fig. 1.
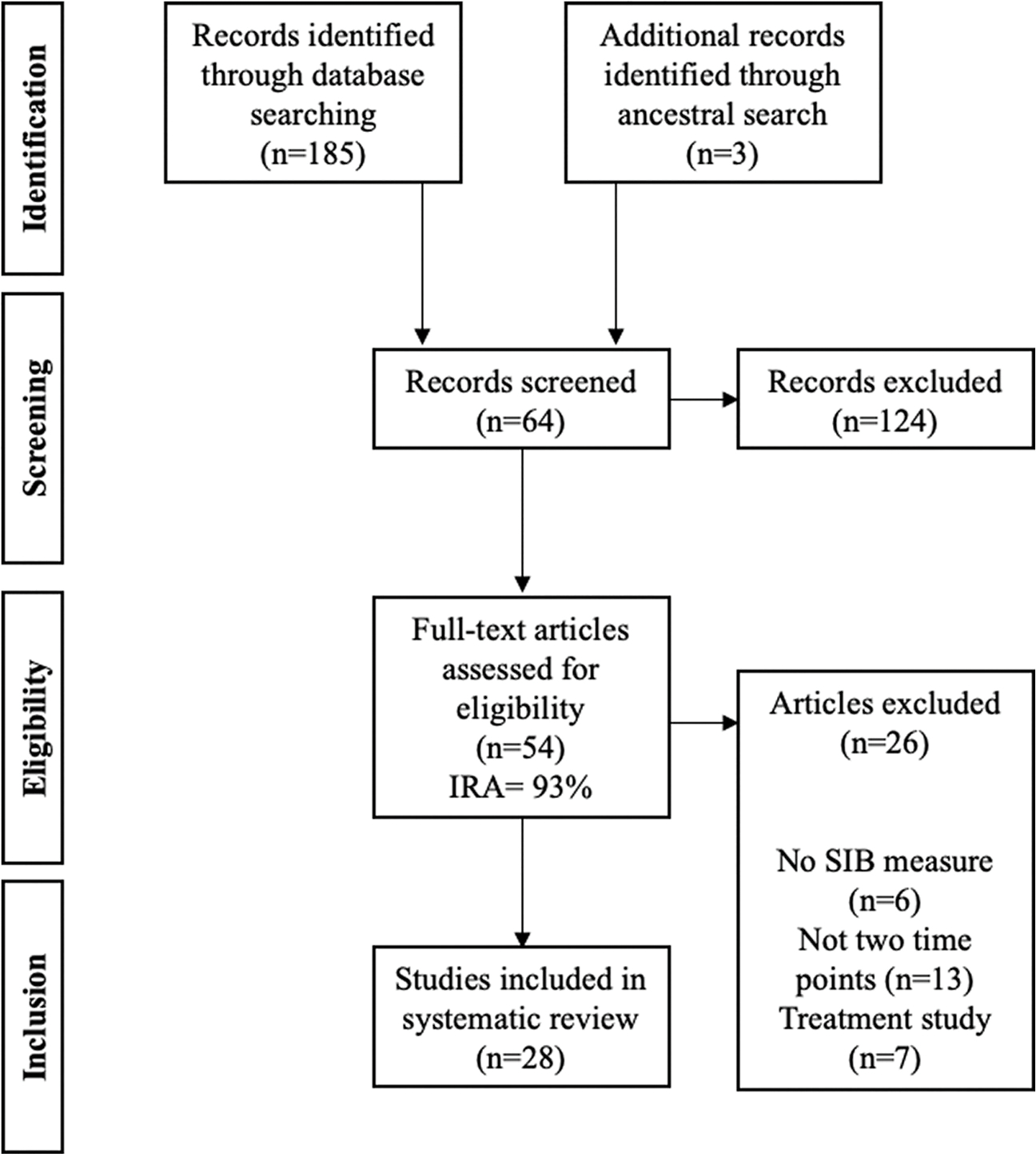
PRISMA Flow diagram illustrating the process of identifying eligible studies.
The systematic evaluation of each article included age and target population, SIB measurement, data analysis methodology and results regarding potential risk markers and factors including incidence, prevalence, relative risk and odds ratio estimates. For each article, we also ascertained whether incidence was reported and if it could be estimated post-hoc.
2.2. Incidence calculations
Cumulative incidence was either calculated or reported based on data at Time 1 (T1) on participants without SIB (i.e., at risk) and at Time 2 (T2) on participants with reported SIB onset. Cumulative incidence, or absolute risk, was calculated by counting new cases of SIB at T2 and dividing by the number of participants at risk at T1 for developing SIB (i.e., cases with no SIB at T1).
3. Results
The aims, age ranges, target populations, and measures of SIB varied considerably across studies. Table 1 displays the information used to examine each article. The following sections highlight the common patterns among the identified articles in terms of themes, age groups and target populations studied, SIB measurement approaches, data analysis techniques, and outcomes.
Table 1.
Literature review results.
| Article | Follow-up | n | Population | Age | Measure of SIB | Main Findings |
|---|---|---|---|---|---|---|
|
| ||||||
| Schroeder et al., 1978 | 3 yrs. (1973,1975, 1976) |
208 | Individuals with intellectual disabilities institutionalized | 5–85 yrs. (M = 22) | Survey completed by social workers and health care professionals | Cross-sectional analyses showed that individuals with SIB had more impairments in vision, receptive language, expressive language, and more prevalent among the younger, and the severely impaired who had been institutionalized longer. |
| Kiernan & Alborz, 1996 | 5 yrs. (1988–1993) |
34 | Adults with learning disabilities living at home with caregivers | 25–37 yrs | Caregiver report (semistructured interview) | At both time points, SIB was correlated with poorer expressive and receptive language and at T2 with poorer mobility and self-help skills. |
| Murphy et al., 1999 | 4–24 mos (M = 16.88 mo. in 3–6 mo intervals) | 27 | Children with severe intellectual disabilities | 2.6–10.11 yrs. (M = 5.27) |
Teacher concern scale, and direct observation | Matched comparison group used with no potential SIB at T1. Developmental age and mobility were correlated with percentage duration of SIB and regression analyses indicated that increases in SIB were associated with degree of teacher concern at T1. |
| Emerson et al., 2001a | 7 yrs. (1988–1995) |
95 | Individuals with Intellectual disabilities with severe SIB at T1 | 12–65 yrs. (M = 34.7) | Individual Schedule of the Challenging Behavior Survey (Alborz et al., 1994) completed by staff members | SIB to head, stability of SIB at T1, and younger age predicted SIB at T2 in a logistic regression analysis (stepwise). Relative risk between predictors and SIB persistence at follow up were also calculated. |
| Emerson et al., 2001b | 7 yrs. (1988–1995) |
679 T1 (1988) & 245 T2 (1995) | Individuals with Intellectual disabilities | 5–85 yrs | Same as above | Logistic regression analyses (stepwise) conducted at each time point indicated that poorer communication skills, more stereotyped behavior and, restricted mobility were associated with SIB at T1 and less self-care skills were associated with SIB at T2. |
| Nøttestad & Linaker, 2001 | 8 yrs. (1987–1995) |
68 | Adults with Intellectual disabilities without SIB who developed SIB after deinstitutionalization | 25–75 yrs. (M = 48.6) | Caregiver report | Severe ID, epilepsy, mobility impairment, hearing impairment, personal care skills, and less communication associated with SIB. |
| Berkson et al., 2001 | 1–3 yrs | 39 | Children with developmental disabilities | 3–40 mos | Video sampling, clinical and parent report | Incidence estimates reported for SIB = 1.3%; proto-injurious =2.2%, transient SIB = 2.6% |
| Berkson, 2002 | 1–3 yrs | 39 | Children with developmental disabilities | 3–40 mos | Same as above | Descriptive analysis of age trends |
| Hall, Oliver, & Murphy, 2001 | 12–24 mos (M = 17.67 mos) | 16 | Children with severe intellectual disabilities | 2.6–10.11 yrs. (M = 5.27) |
Direct observations | An association with SIB and low levels of social contact over time for the 4 children whose SIB increased. |
| Baghdadli et al., 2003 | Retrospective | 222 | Children with autistic disorders | 2–7 yrs. (M = 5) | Questionnaire completed by care staff members | Logistic regression analysis indicated that children who had a higher severity of autism, daily living skills delay, a perinatal condition and a lower age were more likely to have SIB. |
| Oliver, Hall, & Murphy, 2005 | 2- yrs | 16 | Children with severe intellectual disabilities; 6 with genetic disorders (Fragile X, Sturge- Weber, Cornelia de Lange, Seckel syndrome, Trisomy Q) | 2.6–10.11 yrs. (M = 5.27) |
Direct observations | Linear growth models indicated that increases in SIB were correlated with social contact |
| Richman & Lindauer, 2005 | 2–23 months (M = 12 mos) | 12 | Children with Developmental delay; 11 with genetic disorders (Lissenchaphaly, Trisomy 13, Cerebral palsy, Angelman, Cri du Chat, Smith-Magenis, Williams) | 14–32 mos | Repetitive Behavior Scale (Bodfish, Symons, & Lewis, 1999); Functional Analysis |
Topography and functional analysis pattern remained the same, but some forms eventually caused tissue damage for 5 participants; protoinjurious behavior a possible risk factor. |
| Chadwick et al., 2005 | 4.05–6.10 yrs. (M = 5.04 yrs) (1997–2002) |
82 | Adolescents with Severe intellectual disabilities | 11–17 yrs. at T2 (M = 13.06) |
Disability Assessment Schedule (Holmes et al., 1982; Wing, 1989) |
48% of the sample persisted in engaging in SIB at T1 and T2. |
| Chadwick et al., 2008 | Same as above | 82 | Adolescents with severe intellectual disabilities | Same as above | Same as above | Logistic regression found significant associations between adaptive behavior, communication ability, daily living skills, limited language use, expressed parental criticism and SIB. |
| Baghdadli et al., 2008 | 3 yrs. | 185 | Children with PDD-NOS | 5–10 yrs. at T2 (M = 8) |
Adapted International Classification of Individual Handicaps scoring system (Badley, 1993) Schedule of the Challenging Behavior |
Logistic regression (stepwise) indicated that autism severity and lower speech level predicted SIB at T2. |
| Totsika et al., 2008 | 11 yrs. (1992–2003) |
58 | Adults with severe intellectual disabilities | 23–83 yrs. (M = 45) | Survey (Alborz et al.,1994) | Younger age and less social skills were associated with persistent SIB. |
| Cooper et al., 2009 | 2 yrs. (2002–2004; 2004–2006) |
651 at follow up |
Adults with intellectual disabilities | 16 yrs. & older | Diagnostic Criteria for Psychiatric Disorders (DC-LD) | Logistic regression (stepwise) indicated that comorbid ADHD, visual impairment, lower functioning, not having down syndrome, and living in a residential facility were strongly associated with SIB at T1. |
| Taylor et al., 2011 | 18 yrs | 49 | Adults with severe intellectual disabilities | 24–82 yrs | Caregiver report | Persistence estimates indicated that 84% of the sample continued to engage in SIB at T2. SIB topographies reported as well |
| Medeiros et al., 2013 | 12 mos | 160 | Children with or at risk for-developmental delays | 4–44 mos at T1 | Behavior Problems Inventory (BPI-0; Rojahn et al., 2001) | Structural equation modeling results suggested that the frequency of SIB was a strong indicator of later SIB frequency and severity. |
| Schroeder et al., 2014 | T2: 6 mos; T3: 12 mos | 180 | Young children at risk for intellectual and developmental disabilities; 5 with genetic conditions (Joubert, West, Moebius, Russell Silver) | 4–48 mos | Behavior Problems Inventory (BPI-0; Rojahn et al., 2001) | General linear mixed model results indicated that SIB had a significant time effect, (significant mean differences between T1 and T3). |
| Rojahn et al., 2015 | Same as above | 160 | Same as above | 4–44 mos at T1 | Behavior Problems Inventory (BPI-0; Rojahn et al., 2001) | Latent growth modeling indicated the best fitting model consisted of stereotypy predicting SIB. |
| Rattaz, Michelon, & Baghdadli, 2015 | T2: 3 yrs.; T3: 10 yrs | 152 | Children with autism spectrum disorder | 5–15 yrs | Aberrant Behavior Checklist (Aman et al., 1985) | Logistic regressions indicated severity of autism at T1 significantly increased the risk of SIB at T3. |
| Davies & Oliver, 2016 | T2: 15–18 mos | 417 | Children with severe intellectual disability | 2–12 (M = 7.33) yrs. at T1, 4–14 (M = 8.56) yrs. at T2 | Self-injury, aggression and destruction screening questionnaire (SAD-SQ; Davies & Oliver, 2016) | Relative risk estimates indicated that presence of repetitive and restricted behaviors and interests at T1 significantly predicted the presence of SIB at follow up. |
| Richards et al., 2016 | T2: 3 yrs | 67 | Individuals with autism spectrum disorder | Mdn age = 13.5 yrs. (10–17 yrs) | Challenging Behavior Questionnaire (CBQ; Hyman, Oliver, & Hall, 2002) | 77.8% persisted with SIB at T2. Impulsivity and deficits in social interaction at T1 were associated with persistence of SIB over 3 years. |
| Dimian et al., 2017 | 12 mos | 235 | Young children at familial risk for autism spectrum disorder | 12–24 mos | Repetitive Behavior Scale Revised (Bodfish, Symons, & Lewis, 1999) | Logistic regression analysis indicated that children who had SIB and lower intellectual functioning at 12 months were more likely to have SIB at 24 mos. |
| Gulsrud et al., 2018 | Retrospective | 144 | Individuals with autism spectrum disorder | 2.5–60.1 yrs | Autism Diagnostic Interview- Revised (Rutter et al., 2003) | One way ANOVA indicated that age at crawling and age at bladder and bowel control milestones were associated with SIB presence. |
| Crawford et al., 2019 | T2: 3–4 yrs.T3: 5–6 yrs | 79 | Individuals with Fragile X | 6–54 yrs. | Challenging Behavior Questionnaire (Hyman et al., 2002) | Binary logistic regression indicated that restricted, repetitive, stereotyped behavior predicted persistent SIB. |
| Laverty et al., 2020 | T2: 3 yrs.T3: 7 yrs | 67 | Individuals with autism spectrum disorder | M = 23.9 yrs. at T3 | Challenging Behavior Questionnaire (Hyman et al., 2002) | LASSO analysis results showed that impulsivity, interest/pleasure, stereotypy, social communication and adaptive functioning predicted SIB 10 years later. |
3.1. Focus/approaches: onset, persistence
Two foci were evident among the studies investigating risk for SIB included in the review and were used to organize the findings. The first was the early development of SIB among young children. Early SIB development was the primary focus of 13 studies. A majority of the aims statements were specific to early SIB, potential SIB, or proto-SIB (i.e., topographically/form similar behavior (e.g., head hit) that does not produce tissue damage but that may be part of the early SIB developmental pathway) among children with or at risk for I/DD as the primary study purpose.
The second focus was documenting the prevalence and persistence of SIB among adolescents and adults with I/DD. Eleven of the thirteen studies in this category explicitly stated that the aim of their study was to investigate the persistence and or prevalence of SIB. Nøttestad and Linaker (2001) was the only study that investigated the incidence of SIB - among an adult population that had been recently deinstitutionalized (i.e., new cases of SIB at follow up).
3.2. Age groups and target populations
A quarter of the studies included children under the age of 2 years with only five including school-aged children. The remaining articles assessed adolescents and/or adults with I/DD. Individuals with I/DD was the target population of this review, however, approximately 40% of the studies included children with or at risk for I/DD, developmental delay, or autism. Only four studies included information about participants with genetic linked syndromes.
3.3. SIB measurement approaches
SIB measurement included direct and indirect data collection methods and are also listed in Table 1. Half the studies used the same measurement tool. Caregiver reports and surveys or interviews were the most common. Only five studies reported using direct observation data collection methods for measuring SIB. Eighteen of the studies reported SIB as an aggregate among the sample analyzed.
3.4. Incidence of SIB
Cumulative incidence estimates (i.e., new cases) were reported in 7 of the 28 articles (see Table 2). The range of estimates for children 3 months to 17 years of age was 1.3% to 22% over 12 to 36 months of follow up (Baghdadli et al., 2008; Berkson, Tupa, & Sherman, 2001; Davies & Oliver, 2016; Dimian et al., 2017). The highest cumulative incidence estimates reported were among a sample of children at familial risk for ASD ages 12 to 24 months with a cumulative incidence of 22% over 12 months of follow up (Dimian et al., 2017). For studies with adolescents and adults, the estimates ranged from 0% to 22%. Murphy, Hall, Oliver, and Kissi-Debra (1999) reported the highest cumulative incidence estimate for the initial recruitment of their study and indicated an incidence of SIB of 3% over 12 months of follow up (n = 614).
Table 2.
Cumulative incidence estimates.
| Article | n | Cumulative Incidence Estimate | Follow up |
|---|---|---|---|
|
| |||
| Children with I/DD | |||
| Berkson et al., 2001 | 39 | SIB = 1.3%; proto-injurious =2.2%, transient SIB = 2.6% |
1–3 yrs |
| Dimian et al., 2017 | 235 | 22% | 12 mos |
| Richman & Lindauer, 2005 | 12 | 16.7%* | 2–23 mos |
| Murphy et al., 1999 | 614 | 3% | 12 mos |
| Davies & Oliver, 2016 | 417 | 4.7% | 12 mos |
| Baghdadli et al., 2008 | 185 | 15.1%* | 3 yrs |
| Richards et al., 2016 | 67 | 17.5% | 36 mos |
| Adolescents and adults with I/DD | |||
| Cooper et al., 2009 | 651 | 0.6% | 2 yrs |
| Kiernan & Alborz, 1996 | 34 | 0% | 5 yrs |
| Nøttestad & Linaker, 2001 | 68 | 22%* | 8 yrs |
| Totsika et al., 2008 | 58 | 16.3%* | 11 yrs |
| Laverty et al., 2020 | 67 | T1-T3: 10.8%* T2-T3: 6.9%* | 10 yrs |
Notes:
indicates that the incidence estimate was not reported in the article, the first author calculated the estimate base on the data reported.
In the studies for which cumulative incidence estimates of SIB were not reported but the data necessary to do so was included, we derived post-hoc estimates of cumulative incidence (i.e., number of people without SIB at T1 and number of people who were new cases of SIB at T2). Five studies reported the relevant data required to calculate cumulative incidence (Baghdadli et al., 2008; Laverty, Oliver, Moss, Nelson, & Richards, 2020; Nøttestad & Linaker, 2001; Richman & Lindauer, 2005; Totsika, Toogood, Hastings, & Lewis, 2008). The cumulative incidence of SIB from these five studies ranged from 6.9% over 10 years to 22% over 8 years.
3.5. Prevalence and persistence of SIB
Point prevalence and persistence estimates of SIB are graphically displayed in Fig. 2. Twenty of the reviewed studies reported point prevalence estimates of individuals in their sample that engaged in SIB. Overall, point prevalence estimates at T1 ranged from 4.9% (Cooper et al., 2009) to 100% (Emerson et al., 2001a). In contrast, point prevalence estimates at T2 ranged from 4.6% (Berkson et al., 2001) to 71% (Emerson et al., 2001a). For studies with adolescents and adults with I/DD, five of the eight studies with point prevalence estimates at both time points the estimates increased or stayed the same (Chadwick, Kusel, Cuddy, & Taylor, 2005; Crawford, Karakatsani, Singla, & Oliver, 2019; Nøttestad & Linaker, 2001; Richards, Moss, Nelson, & Oliver, 2016; Taylor, Oliver, & Murphy, 2011). For those studies in which persistence estimates were included, persistence rates reported ranged from 19% (Dimian et al., 2017) to 95% (Nøttestad & Linaker, 2001). Persistence appeared to vary by age group, with higher persistence rates reported among adults.
Fig. 2.
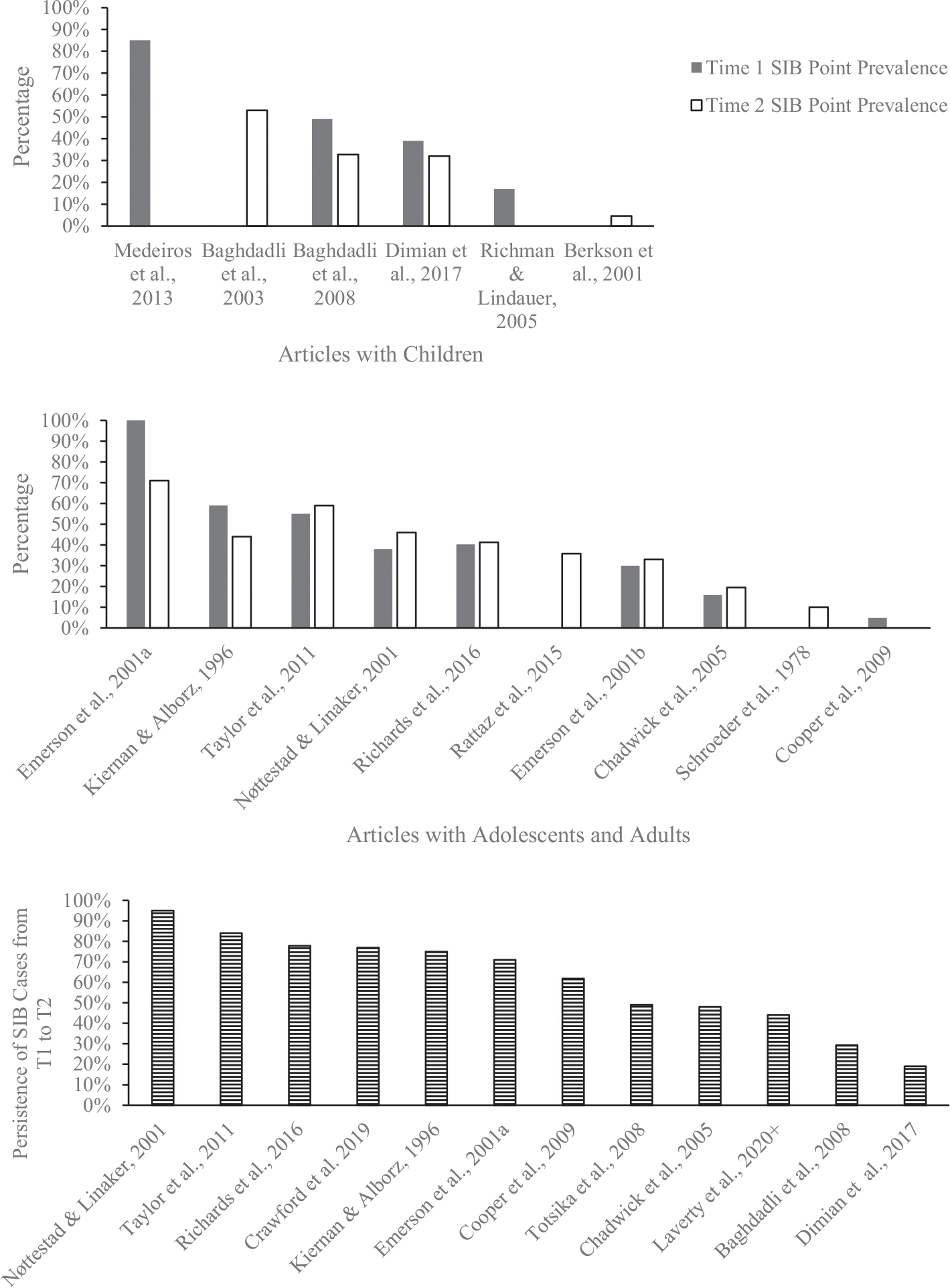
Point prevalence estimates and persistence estimates of SIB by age group and time point. Bars with no fill indicate estimates from T1 and no fill bars are from T2. Stripped bars are persistence estimates. The top panel are estimates from articles with children, the middle panel are estimates from articles with adolescents and adults, and the bottom panel are persistence estimates reported.
3.6. Data analyses utilized
3.6.1. Descriptive analyses
Some of the studies primarily assessed change in SIB over time by tracking the changes in form, age trends, and environmental influences of SIB. Berkson et al. (2001), Berkson (2002), and Dimian et al. (2017) for instance reported specific forms of stereotyped, proto-injurious (i.e., SIB did not cause tissue damage), and SIB over time (i.e., whether they were increasing or changing forms across time). Overall takeaways from the work analyzed descriptively were that SIB topographies and frequency appear to change over time for some but not all individuals. SIB persistence and stability rates were high for adult samples with I/DD.
3.6.2. Correlational analyses
Four studies primarily utilized correlations to analyze the data collected at each time point within the prospective cohort studies examined (Kiernan & Alborz, 1996; Nøttestad & Linaker, 2001; Schroeder, Schroeder, Smith, & Dalldorf, 1978; Totsika et al., 2008). For example, Schroeder et al. (1978) reported statistically significant associations between SIB and visual impairments, receptive and expressive language, and younger chronological age.
3.6.3. Regression models
Nine of the studies utilized logistic regression analyses (i.e., SIB was the dependent variable and was coded as binary (yes or no) to identify possible risk factors for SIB. For instance, among the logistic regression results, Emerson et al. (2001a) examined the persistence of SIB among individuals with ID and severe SIB (ages 12–65). The results of their analysis indicated 3 variables predicted SIB persistence (i.e., SIB still occurring at follow up) including SIB topography (head-directed SIB), SIB stability (at T1), and younger age (Emerson et al., 2001a). At follow up (7-years), only fewer self-care skills were associated with SIB (Emerson et al., 2001b). Other approaches employed included structural equation modeling (Medeiros, Curby, Bernstein, Rojahn, & Schroeder, 2013), general linear mixed modeling (e.g., Schroeder et al., 2014), growth modeling (Rojahn, Barnard-Brak, Medeiros, & Schroeder, 2015), and a least absolute shrinkage and selection operator (LASSO) analysis (i.e., a penalized form of regression analysis) using T1 variables to predict SIB at T3 (Laverty et al., 2020).
3.7. Risk marker estimates for SIB
Based on the analyses conducted, there were several common risk markers reported. The risk markers identified across the studies and across individuals with I/DD for the persistence (i.e., not emergence) of SIB are listed in Table 4. The top three risk markers for the persistence of SIB among children were autism severity or being at risk for an autism diagnosis, proto-injurious, frequency or severity of SIB, and lower levels of social interaction over time or social deficits. Across the studies with adolescents and adults with I/DD lower receptive or expressive language, lower adaptive behavior skills, and intellectual impairment (severe) or cognitive ability were the three most common risk markers reported. There was some overlap in risk markers reported between the two main age groups examined, however, replication of many of the findings with similar sample characteristics appears to be warranted; or, put another way – the risk markers were not uniformly replicated across the existing studies particularly when moving across age groups.
Table 4.
Relative risk and odds ratio estimates reported.
| Article | Follow-up | n | Age | Relative Risk Estimates | Odds Ratio Estimates |
|---|---|---|---|---|---|
|
| |||||
| Emerson et al., 2001a | 7 yrs | 95 | 12–65 yrs. (M = 34.7 yrs) | Persistence of SIB at T2*: SIB to head = 2.7 SIB sometimes to head = 2.3 Stability of SIB at T1 = 2.4 Poor expressive communication = 2.2 |
|
| Totsika et al., 2008 | 11 yrs | 58 | 23–83 yrs. (M = 45 yrs) | Persistence of SIB at T2: Severe challenging behavior at T1 = 0.93 (95% CI 0.55, 1.58) |
|
| Richards et al., 2016 | 3 yrs | 67 | 10–17 yrs | Persistence of SIB at T2: Ability = 2.4 (95% CI 1.5–3.8) Speech = 2.8 (95% CI 2.0–3.9) |
|
| Davies & Oliver, 2016 | 15–18 mos | 417 | 2–12 yrs | SIB at T1: Repetitive and restrictive behavior = 4.87 (95% CI 2.31, 10.3) Overactivity/impulsivity = 3.51 (95% CI 1.64, 7.54) SIB at T2: Repetitive and restrictive behavior = 3.29 (95% CI 1.46, 7.41) |
Logistic regression analysis: Repetitive restrictive behavior = 3.44 |
| Dimian et al., 2017 | 12 mos | 235 | 12–24 mos | SIB at T2: ASD diagnosis =1.85 |
Logistic regression analysis: Developmental ability = 0.97 (95% CI 0.94, 0.99) SIB = 1.92 (95% CI 1.45, 2.54) |
| Baghdadli et al., 2003 | Retrospective | 222 | 2–7 yrs. (M = 5 yrs) | Logistic regression analysis: Age = 0.69 (95% CI 0.5, 0.9) Daily living skills = 0.98 (95% CI 0.96, 1.02) CARS total score = 1.1 (95% CI 1.02, 1.13) Perinatal condition = 5.5 (95% CI 1.04, 28.7) |
|
| Chadwick et al., 2008 | 4.05–6.10 yrs. (M = 5.04 yrs) | 82 | 11–17 yrs. at T2 (M = 13.06 yrs) | Logistic regression analysis: Vineland overall score = 0.93 Communication score = 0.95 Daily living skills = 0.94 Limited language use = 1.96 Expressed parental criticism = 10.63 |
|
| Baghdadli et al., 2008 | 3 yrs | 185 | 5–10 yrs. at T2 (M = 8 yrs) |
Logistic regression (stepwise): Autism severity = 1.1 (95% CI 1.0, 1.2) Lower speech level = 3.5 (95% CI 1.1, 13.4) |
|
| Cooper et al., 2009 | 2 yrs | 651 | 16 yrs. + | Logistic regression (stepwise): Lower ability level = 7.19 (95% CI 3.27, 15.82) Not living at home = 2.41 (95% CI 1.12, 5.19) ADHD = 10.95 (95% CI 3.50, 34.19) Not having Down syndrome = 0.24 (95% CI 0.06, 0.99) Visual impairment = 1.94 (95% CI 1.01, 3.72) |
|
| Rattaz et al., 2015 | 10 yrs | 152 | 5–15 yrs. at T3 | Logistic regression (polytomic): Childhood autism rating scale total score at T1 = 2.4 (95% CI 1.0, 5.5) for high SIB group Object- related cognition functioning at T1 = 0.6 (95% CI 0.3, 1.0) for high SIB group |
|
| Crawford et al., 2019 | 8 yrs | 79 | 6–54 yrs | Logistic regression: Increased restricted, repetitive, and stereotyped behavior at T1 = 1.57 |
|
Notes:
indicates that the top four significant findings were reported from the article.
3.8. Relative risk and odds ratios for SIB development and persistence
Table 4 displays the statistically significant RR and OR estimates reported in the reviewed articles. Only 5 of the 28 articles reviewed calculated RR (Davies & Oliver, 2016; Dimian et al., 2017; Emerson et al. (2001a); Totsika et al., 2008; Richards et al., 2016). Laverty et al. (2020) reported that they calculated RRs but did not include the estimates, therefore we did not include this study in this part of the analysis. Each of those five studies reported RR of predictors at T1 for the persistence of SIB at T2.
In general, the analysis approaches relying on logistic regression used them to evaluate potential risk markers and SIB with OR estimates. Eight studies reported OR estimates produced by the logistic regression models. Of the studies that did report ORs, associated perinatal condition (OR = 5.5, CI = 1.04, 28.7; Baghdadli et al., 2003), expressed parental criticism (OR = 10.63; Chadwick, Kusel, & Cuddy, 2008), lower speech level (OR = 3.5, CI = 1.1,13.4; Baghdadli et al., 2008), and a diagnosis of Attention Deficit Hyperactivity Disorder (OR = 10.95, CI = 3.5, 34.19) were among the highest OR estimates reported across the studies reviewed. There are advantages and disadvantages to using RR and OR estimates as well as conditions in which the OR approximates the RR estimate are reviewed further in the Discussion section.
4. Discussion
It is not clear that we have a sufficient understanding of risk factors necessary to build a robust risk model of SIB in I/DD to inform a next generation effort targeting risk reduction and therefore reducing SIB incidence and ultimately public health burden of the behavioral disorder. In addition to specific assessment and treatment reports, researchers in the field of neurodevelopmental disabilities have produced a relatively small series of observational studies over the last 40-years focusing on the prevalence and persistence of SIB. Among the research conducted to date, there does appear to be increasing attention devoted to identifying and understanding specific causal risk factors for the development and persistence of SIB. Unfortunately, the conventional wisdom about risk factors for SIB is plagued by terminological imprecision and historically tends to be based on cross-sectional methodology.
The focus of the current review was specific to the findings from longitudinal/ prospective and retrospective cohort studies investigating SIB and its correlates in relation to risk. The literature reviewed was characterized by incongruent findings, making it difficult to start creating a cohesive model of risk to inform early intervention and prevention programming. The Discussion will focus on the validity evidence supporting the inferences and findings on potential risk factors for SIB. Modest recommendations for improvement are suggested. A general summary of the systematic review results is presented followed by more detailed discussion of conceptual, methodological, and translational issues.
4.1. Systematic review results summarized
The results from the 28 articles reflect a relatively recent ‘up tick’ of SIB specific studies centering on multiple possible psychosocial variables that increase the risk (i.e., putative risk factors) of SIB among individuals at risk for or with I/DD. A variety of age groups, populations, and putative risk markers (i.e., associated variables) were studied. Less clear is whether the variables authors advanced as ‘risk factors’ are causally related to the primary outcomes of interest (SIB onset, SIB persistence).
As stated earlier, from an epidemiological perspective, the advantage of the prospective cohort design is the ability to derive incidence and RR estimates (i.e., the gold standard for quantifying risk) over a follow-up time period. Unfortunately, only a few studies (4) reported the incidence of SIB among the sample followed (see Table 2), and in only 2 studies were RR estimates derived (e.g., the likelihood of developing SIB given a certain variable/exposure; see Table 3; Laverty et al. calculated but did not report the specific RRs). The conclusions about putative risk factors that legitimately can be made based on the data analysis strategies employed by a majority of the studies is therefore limited. Recall the distinction between the terms/concepts of ‘risk markers’ and ‘risk factors’ in regard to causality (factors increase the probability of a condition and are part of the causal chain; markers are associated with an increased probability of a condition but are not necessarily causal). The studies that aimed to examine the persistence of early SIB and the studies that focused on persistence of SIB among adolescents and adults are summarized next to better understand the extant literature with respect to the identification of putative risk factors for SIB.
Table 3.
Risk markers for the persistence of SIB reported for individuals with intellectual and developmental disabilities.
4.1.1. Persistence of early SIB
Almost half of the studies reviewed investigated early SIB among children at risk for or identified with I/DD. The studies that focused on the persistence of early SIB also employed a variety of different measurement tools and data analyses. Half of the studies relied on indirect assessments of SIB (i.e., questionnaires) and the other half used direct observation or a combination of measures (i.e., counting instances of SIB in situ over a course of observations). Data analyses and aims varied with most of the studies assessing how SIB changed over time (i.e., across observational time points) with respect to sample characteristics, such as age, form or topography, and relative to the distribution of social contact in a classroom setting. All samples included participants with SIB at T1; thus data analyses were conducted with the aggregate of both SIB and ‘non-SIB’ cases, precluding the ability to investigate the emergence of early SIB.
Among the different age groups and populations, the top 3 common risk markers identified across the articles among children with or at risk for I/DD included autism severity or being at risk for an autism diagnosis, social contact/deficits, and proto-injurious behavior/frequency or severity of SIB (see Table 3). The point prevalence estimates among the early SIB studies ranged from approximately 5% to 85%. Only Baghdadli et al. (2008) and Dimian et al. (2017) calculated a persistence estimate for SIB reported at both T1 and T2 (29% and 19%, respectively). Cumulative incidence for SIB among children ranged from 1.3% to 22% (see Table 2).
Taken together, the collective knowledge of what constitutes a risk factor for the emergence or persistence of early SIB is still unclear at least as it relates to specific causal knowledge readily translatable into an action strategy to reduce risk. The studies presented and reviewed indicate that there are some common risk markers across a few studies, but that the evidence is primarily correlational and descriptive. The areas in which research could be expanded as well as rectified with respect to conceptual and methodological issues is discussed below following a summary of findings on the persistence of SIB among adolescents and adults.
4.1.2. Persistence of SIB among adolescents and adults
The remaining studies reviewed centered on the persistence of SIB among adolescent and older individuals with I/DD. Compared to the early SIB studies, the ages ranged more widely with some studies including individuals from 2 to 85 years old (Gulsrud, Lin, Park, Hellemann, & McCracken, 2018; Schroeder et al., 1978). It is promising that the empirical work to date includes a wide range of age groups, however, the measurement of SIB is incongruent across the studies. The studies that examined the persistence of SIB among adolescents and adults all reported using indirect assessments, primarily caregiver report and questionnaires to assess SIB. It is unclear if SIB was quantified in the same way (i.e., in terms of severity, topographies, and frequency dimensions) across the studies, limiting the generalizability of the inferences and sample estimates reported.
The most common data analysis strategy employed by researchers was logistic regression analyses to evaluate the relation between explanatory variables (i.e., potential risk factors) and SIB occurrence at follow up. Nøttestad and Linaker (2001) were the only study to investigate SIB emergence by utilizing a sample of individuals with no SIB at T1. The sample included people with intellectual disabilities that were living in a residential facility (T1) and then were deinstitutionalized (T2). The causal inferences that could be made were strengthened due to the recruitment and sampling strategy (i.e., only including participants not engaging in SIB but vulnerable (at risk group) and following them over time).
Among the studies reviewed involving adolescents and adults with I/DD, shared risk markers were identified and included lower receptive or expressive language, lower adaptive behavior skills, and severe intellectual impairment (see Table 3). The point prevalence estimates reported in the studies ranged from 4.9% to 100%. Persistence estimates on the other hand varied from 48% up to 95% (Nøttestad & Linaker, 2001). Cooper et al. (2009) and Kiernan and Alborz (1996) were the only two studies for adults that reported CIs. Estimates ranged from 0% to 0.6% over 2–5 years of follow up, respectively. RR estimates, however, were reported in only 5 of the 28 studies. Replication is needed to assess if the results are generalizable (i.e., have strong external validity evidence) among other populations adults with I/DD.
There were some similar findings and risk markers overall among the prospective work focusing on the persistence of SIB in older individuals. However, as with the early SIB persistence studies, the evidence is equivocal about risk factors for SIB emergence and persistence among individuals with I/DD. In the sections that follow, we identify and discuss several conceptual models and methodological issues. The intent is to highlight a more precise and informed path forward for research into putative risk factors for SIB.
4.2. Conceptual issues relevant for expanding models
For research purposes, SIB tends to be conceptualized as a homogenous phenomenon in the sense that it is either ‘present’ or ‘absent’. But, as reviewed, SIB is characterized by considerable heterogeneity with respect to forms, function, severity, and correlates. It is likely that risks considered specific to etiology and developmental pathways are also characterized by heterogeneity. From the perspective of developmental psychopathology (Beauchaine, Klein, Crowell, Derbidge, & Gatzke-Kopp, 2009; Cicchetti & Blender, 2006), the concepts of ‘equifinality’ and ‘multifinality’ informed by complex systems theory may be useful for addressing etiological heterogeneity and SIB. Equifinality refers to the tendency of open systems to have properties in which a given end state can be reached by many potential means. In such systems, there is a convergence of mechanisms so a common denominator may well underlie the actions of various surface pro-vulnerability factors.
Equifinality with respect to SIB and I/DD may occur at the most general level in the sense that there are many different genetic or environmental factors that confer biological risk to the developing brain, and if the brain is damaged, lead to some form of I/DD with subsequent increased risk for the emergence of SIB. For example, despite the likely differences in causative factors in autism, the core characteristics of social impairment, lack of communication, and restricted/stereotyped interests and behaviors are the common outcome, and the best predictor for the etiology of SIB in young children with autism appears to be the overall severity of these core features (Dominick, Davis, Lainhart, Tager-Flusberg, & Folstein, 2007).
Conversely, multifinality refers to a common starting point leading to many different end states. Multifinality with respect to SIB as an endpoint is exemplified in Fragile X syndrome (FXS). The common starting point is a genotype characterized by a CGG tri-nucleotide repeat but different end states with respect to variability in the behavioral phenotype, specific to SIB, in which approximately 50% of males with FXS self-injure (Arron, Oliver, Moss, Berg, & Burbidge, 2011). Thus, some but not all males with FXS self-injure, in spite of a common starting point (tri-nucleotide repeat). One issue, here, however, is that despite shared diagnosis (FXS), not all males with FXS – even with full mutations - are ‘starting’ from the ‘same’ place. Individuals with full FXS mutations frequently have only partial methylation or mosaic forms – each of which allows for partial expression of FMRP. Individuals with higher levels of FMR1 expression have higher functioning levels, and so it might seem reasonable to suspect a direct relationship between degree of methylation (lower functioning) and amount of SIB. The evidence, to date, however has not found a clear linear relationship between degree of CpG methylation and propensity to self-injure (Symons, Sutton, Walker, & Bodfish, 2003).
Such results suggest that main effects are not always to be expected with respect to gene (or any biological variable) and behavior relations, but the key findings may be in the interactions. In a first of its kind study, Hessl et al. (2008) found that additional genetic background can significantly contribute to the behavioral outcome for males with FXS. Males with FXS who carry the long 5-HTTLPR L/L genotype had more aggressive and destructive behaviors than did individuals homozygous for the short genotype (S/S). Individuals with L/L genotype also had the most stereotypic behavior. Given these observations, it would be reasonable to postulate that individuals with FXS who carry the L/L genotype might be more vulnerable for developing SIB if exposed to the right potentiating environment, but to our knowledge this potential association has not been investigated in FXS or more generally the logic of gene X environment interaction tested directly in I/DD populations in relation to modeling risk for SIB.
Neurobiological mechanistic frameworks.
Given the above discussion, it is fair to say that the biological basis for SIB is not well understood and our scientific knowledge of developmental pathways incorporating biological variables specific to SIB in IDD is limited. It is also important to point out that there has been a body of biologically-oriented empirical work in animal models (rodent, monkey; See Breese et al., 2005; Devine, 2012; Novak, Crockett, & Sackett, 2002) as well as relevant work specific to non-suicidal self-injury (NSSI) occurring among individuals with psychiatric diagnoses (Nock, 2009) with relevance to consider SIB risk in I/DD populations. There has also been a line of work specific to pain and sensory function and SIB in I/DD germane to considering risk (Symons, 2011). In the remainder of the section below; we focus a selective review of such work specific to IDD samples and draw from broader observations as needed to support the argument for including biological variables in SIB risk models for I/DD that also help to address important conceptual issues not always acknowledged in I/DD SIB risk research (multifinality/equifinality as mentioned; heterotypic/homotypic continuity as will be discussed).
Another useful conceptual perspective is the notion of considering carefully individual differences while acknowledging a diversity of processes and diversity of outcomes (Cicchetti & Rogosch, 1996; Rovine & Lawrence, 2017). In the original description of what became the ‘gold-standard’ experimental technology for the assessment of SIB in I/DD (i.e., ‘functional analysis’), Iwata et al. stated that the purpose of a functional analysis was not to address the issue of environmental versus physiological determinants of self-injury in regard to etiology or maintenance (Iwata et al., 1982/1994). Herein lies an additional important point – the problem of ‘either/or’ thinking with respect to SIB in I/DD - either it is ‘behavioral’ or it is ‘biological’. Behavior is the property of a biological system, arbitrarily dichotomizing SIB as ‘behavioral’ or ‘biological’ makes no more sense than outdated arguments about nature versus nurture. Contemporary accounts of developmental science turn on nature and nurture and so must our thinking on self-injury, particularly with regard to risk and development. Dichotomizing does not readily reflect underlying individual differences while acknowledge process and outcome diversity. There are numerous systems with high relevance for SIB risk when individual differences and biologically-meaningful subgroups are considered.
Pain, stress/arousal, and endocrine systems.
Among the various theoretical biological perspectives, the opioid model of SIB has been heavily investigated and is complementary, perhaps, to more general theoretical perspectives related to stress/arousal and neuroendocrine mechanisms involving the hypothalamic pituitary-adrenal system (HPA axis) which may be dysregulated among at least some SIB subgroups. Specifically, the proopiomelanocortin (POMC) molecule has been implicated in SIB (Sandman, Spence, & Smith, 1999). POMC is a precursor to several active peptides, including adrenocorticotropin (ACTH – a stress mediator), β-endorphin (a pain/analgesia mediator), and melanotrophin (A, B and Y-MSH), mainly expressed in both the anterior and intermediate pituitary gland in the hypothalamus, amygdala and other regions of the CNS.
There are two general versions of the opioid model in SIB and I/DD. One perspective holds that individuals with SIB have an increased pain tolerance because of elevated opioid (i.e., β-endorphin) levels and do not ‘feel’ pain and therefore there is no natural ‘brake’ on self-injury. The other theory presents the possibility of an addiction-like model of SIB, such that SIB is, in a sense, an addictive behavior maintained by dependence on endogenous opioid release and receptor binding. Within the addiction model, it is assumed that stress or pain associated with SIB induces the release of opioids (Sandman et al., 1999). In both models, the risk for SIB may be increased because of an irregularity in the POMC gene, or a different related opioid gene/molecule. There have been no empirical tests of such a risk model, however, with respect to the POMC gene and possible mutations. It is worth noting that subgroups of individuals exhibiting SIB have been found to respond to opioid antagonists (Symons et al., 2004). But, there has been little to no work toward biologically stratifying patients prior to a trial to increase the predictive validity evidence to understand/differentiate responders from non-responders.
Pain and sensory function.
In a related but different line of biologically-oriented research investigating peripheral physiology and self-injury, there have been a series of observations specific to nociceptive (i.e., pain) and sensory afferents (epidermal nerve fiber innervation) in the skin that may be relevant to the notion of individual difference variables or sub-clinical markers for biological vulnerability and SIB risk (Symons, 2011). A SIB subtype or subgroup associated with a specific pattern of peripheral biomarkers has been characterized in adults with IDD by differences in the density of small-diameter unmyelinated sensory nerve fibers and concentrations of substance P (SP), a neuropeptide relevant to nociceptive (i.e., ‘pain’) signaling (Symons et al., 2003). Initial observations in adult samples with I/DD and chronic SIB described intra-epidermal nerve density differences (Symons et al., 2008) relative to non-disability controls which were subsequently replicated with a larger sample of adult SIB cases relative to matched developmental disability controls. (Symons, Wendelschafer-Crabb, Kennedy, Heeth, & Bodfish, 2009). Increased SP-positive fiber counts in some, but not all, samples along with extensive mast cell degranulation (consistent with immune mediated inflammatory response) was documented. It was also found that individuals with SIB and altered peripheral markers were more (not less) responsive during a modified quantitative sensory testing protocol compared to matched controls without SIB (Symons, Shinde, Clary, Harper, & Bodfish, 2010).
To the degree that there may be individual differences in peripheral innervation and epidermal nerve fiber density, there are a number of interesting but highly speculative issues that are not typically considered with regard to the problem of SIB and risk among I/DD. Initial risk may be related to variation in the underlying early tactile and nociceptive circuitry and the nature of early experience. Basic neuroscience work on peripheral nociception has found that prolonged neuroinflammation in the dorsal horn of the spinal cord can produce a switch between normally inhibitory to excitatory spinal pathways resulting in hyperalgesic phenotypes (exaggerated pain sensitivity/responsivity) such that non-noxious touch evokes pain (allodynia) (Pitcher, Nieto, & Cervero, 2013). It appears that the circuitry dedicated to nociception is ‘co-opted’; spinal nociceptive neurons are able to be activated by low-threshold mechanoreceptors (touch) because of inflammation-enhanced Na(+)-K(+)-Cl(−) cotransporter 1 (NKCC1) activity. Whether this is an issue for children with I/DD and increased ENF densities is completely unknown, but the finding is relevant in so far as it promotes inquiry into the nature of tactile and noxious experience and the consequences of pathology in ‘pain pathways’ (in this case, early neuroinflammation) as possible risk factors for SIB.
Mood & affect regulation.
Co-morbid affect dysregulation may be a risk factor conferring SIB vulnerability. Expression of SIB is particularly prevalent in diagnoses where ongoing distress and pathological irritability are prominent features (Sovner & Fogelman, 1996), and negative affect has been linked with self-injury across multiple diagnostic categories (Anderson & Ernst, 1994; Lindauer, DeLeon, & Fisher, 1999; Tsiouris & Brown, 2004; Tsiouris, Cohen, Patti, & Korosh, 2003; Verhoeven et al., 1999). Consistent with these observations, are biological findings that abnormal basal activity and responsiveness of the limbic-hypothalamic-pituitary-adrenal (LHPA) axis appear to be a common characteristic among some children with I/DD and SIB (Kemp et al., 2008; Sandman, Touchette, Lenjavi, Marion, & Chicz-DeMet, 2003; Sandman, Touchette, Marion, & Chicz-DeMet, 2008; Verhoeven et al., 1999). The data as generated do not conclusively point to affect dysregulation as a causal factor in etiology of SIB, but the strong association between emotional hyper-responsiveness and prevalence of SIB should be further investigated in I/DD. This is underscored by observations that upward to approximately 50% of children with autism exhibit clinically significant levels of anxiety (Kim, Szatmari, Bryson, Streiner, & Wilson, 2000; Muris, Steerneman, Merckelbach, Holdrinet, & Meesters, 1998; Sukhodolsky et al., 2008; Weisbrot, Gadow, DeVincent, & Pomeroy, 2005), but to our knowledge no study has identified whether anxiety and SIB reliably co-occur in pediatric I/DD/ASD samples.
Overall, across the different bio-behavioral investigations and conceptual issues and models reviewed briefly above, there has been no real attempt to incorporate then intentionally within an epidemiological framework as we adopted for this systematic literature review. It is clear that the empirical literature on risk factors for SIB in clinical samples/populations and their approaches and analyses is for all intents and purposes exclusively psycho-social-environmental. We think it is imperative to incorporate biological systems relevant to risk and individual differences. One of the critical goals for research on SIB must be to elucidate innate and environmental factors to inform us about vulnerability for self-injury within at-risk-for-SIB populations (e.g. autism, severe intellectual disability). Studies of prevalence rates for co-morbid features in clinical samples and manipulations in animals with pre-existing SIB do not directly address this important etiological issue. In the section below, we offer some considerations and recommendations for ‘next steps’ based on our synthesis of the past four decades of longitudinal/cohort literature on SIB risk to move the field forward that would include integrating bio-behavioral mechanisms as well as more informative design strategies.
4.3. Translational issues – a path forward to risk reduction and prevention
Currently, assumptions are being made based on mostly correlational data from single time points from which the field collectively considers ‘conventional wisdom’ regarding risk factors for SIB. Because of all the issues identified (sample size variability/heterogeneity, operationalization of SIB, and methodologies used), it is difficult to come to an overall consensus regarding risk factors for SIB based on the literature as analyzed and synthesized in our review. The amount of observational work is impressive, but there are many limitations to the approaches and external validity of the findings. As discussed so far, importing research strategies or at least adapting research strategies from the field of developmental psychopathology, epidemiology and prevention sciences may be one way to move our understanding of risk factors and SIB forward.
4.3.1. Recruitment
To restate, with a prospective cohort study, the emergence or persistence of SIB is measured over time. Temporal and possible causal relations could be assessed. Attrition is always a limitation of this type of methodology, but if a population-based sample were obtained and followed from ‘cradle to grave’ (i.e., a lifespan approach), putative risk factors associated with the emergence and persistence of SIB could be identified. For example, in autistic research, investigators are recruiting families that are expecting a child and already have an autistic child. The purpose of these studies are to investigate the early signs and risk factors associated with a diagnosis of ASD. A similar strategy could target families with children with developmental delays to evaluate SIB risk and development or study SIB development using the ‘baby siblings’ approach to at least get estimates of SIB risk within ASD samples. In many of the studies reviewed in this paper, convenience samples were utilized. Schroeder and colleagues recruitment of Peruvian families at risk for disabilities is the closest our field has come to studying a population at risk for SIB to develop. A way to take this one step further would be to exclude young children already engaging in SIB if the research question of interest is specific to risk factors for the development or emergence of SIB. Nøttestad and Linaker (2001) were the only study to utilize a sample of individuals with incident SIB after deinstitutionalization. This is a start at addressing the emergence of SIB among adults with I/DD but a similar recruitment logic needs to be replicated in younger-aged samples as well.
Case-control design is a methodology that could be used more often to model and address risk factors. A case-control design can help to articulate the developmental trajectory of SIB with the use of a control group. Three studies included in this review did have a matched no-SIB group and attempted to compare differences in terms of characteristics that might contribute to SIB (i.e., Murphy et al., 1999; Nøttestad & Linaker, 2001; Schroeder et al., 1978). One way to extend the studies mentioned would be to use a normative/typically developing control group to help elucidate any developmental patterns associated with age and onset of SIB (e.g., Hoch et al., 2015).
4.3.2. Measurement
Although there are decades of behavioral research on SIB, it may be time to reconsider how SIB is defined and measured to clarify a taxonomy of SIB (e.g., Rojahn, 1994), in which topographies of repetitive behavior are examined over time. Most studies used different measures of SIB relying on indirect and direct data collection approaches and so results across studies are challenging to compare. Researchers also need to start expanding the scope of potential risk factors for SIB and investigate bio-markers, neuro-correlates, environmental, and developmental factors in relation to SIB, to name a few. For example, proto-injurious behaviors could be a risk factor predicting the emergence of SIB early on, but there have been limited empirical studies targeting protoinjurious behaviors, or objective measures to assess this type of repetitive behavior in a way that is comparable to current measurement approaches for stereotypy or SIB. Finally, particularly for the persistence of SIB, functional subtyping (i.e., functional analysis characterizing/identify whether SIB is sensitive to social reinforcement contingencies) may help facilitate identification of potential risk factors for certain functional groups of SIB.
In terms of broad types of measurement, assessment of SIB across the studies primarily utilized indirect measures. Proxy reporters ranged from caregivers to staff and teachers either interviewed or asked to complete a survey comprised of a rating scale. The variety of indirect assessments used make replicating and generalizing the findings across studies in terms of topographies, frequency, severity, and intensity of SIB, impractical if not impossible. For instance, in some scales, a definition or SIB topography is provided and the rater is required to report the frequency and severity of the behavior within a specific time period (e.g., BPI-01, DAS, RBS-R). Other assessments use clinical judgment of SIB that is then classified into categories (i.e., mild, moderate, etc.) based on severity, frequency, duration, and intensity (e.g., the Adapted International Classification of Handicaps scoring) or into a multi-axial structure (e.g., DC-LD). With only 6 out of the 28 studies using direct observations of SIB (i.e., observing and counting instances of SIB in situ), there is risk of information bias or misclassification associated with relying solely on informant report and indirect measures. For a comprehensive review of the psychometric properties of some of the standardized measures employed by the studies reviewed see the assessment chapter by Rojahn et al. (2008) which although dated remains highly relevant.
4.3.3. Epidemiology
To better understand the distribution of SIB within the population of individuals with I/DD and their families, an epidemiological strategy or something approaching it is needed. Cohort studies are ideal because they follow a group of people over a certain time period and could help ascertain whether the incidence of SIB is related to a suspected risk factor exposure (Szklo & Nieto, 2014). We recognize the ‘needle in the haystack’ problem, but RR and incidence calculations offer a way of looking across time and risk factors to examine how they may contribute to the emergence and persistence of SIB (Viera, 2008). Among the studies reviewed, very few studies reported the types of analysis to quantify risk. Future research should include them. Rojahn et al. (2008) conducted a review on the epidemiology of SIB up until that point and came to a similar conclusion. Rojahn et al. ended up focusing their chapter simply on a summary review of prior prevalence estimates of SIB because there were an insufficient number of datasets to confidently derive risk estimates. Incidence and RR estimates are the sine qua non for cohort studies but these estimates can only be derived from a prospective design. Incidence estimates are needed to help inform if prevention efforts are working and so relevant data from well-designed cohort studies are needed before early intervention or prevention trials are conducted. Selecting specific ‘exposures’ (i.e., risk factors) based on the literature would help refine the precision of previous work conducted.
A number of different considerations would then be faced by investigators adopting prospective approaches beginning with careful (re) considering of the initial question being asked – e.g., ‘how much SIB is there in this sample’ compared with ‘does variable X function as a prognostic vs a predictive factor?’ To answer/test the latter question is a very different proposition than the former. As an editorial-like comment we have, as a field, likely spent too much time on prognostic factors and confused them with predictive factors; in oncology approaches predictive biomarkers provide information about the effect of a therapeutic intervention whereas prognostic biomarkers provide information about overall outcomes. It is in considering prediction tied to treatment outcomes that much more careful consideration needs to be given to individual differences in stress reactivity, sensory/nociceptive mechanisms, and impulsivity/self-regulatory mechanisms as they relate to subgroups and underlying biological vulnerability (including genomic variables and specific genetic syndromes).
To shift to credible risk estimates, more consideration would then need to be given to biases that can undermine epidemiological risk studies (e.g., immortal time bias considerations in which time blocks are erroneously ‘immortalized’ and positive outcome estimates are inflated would need to be considered carefully for prospective designs in which very young children with delays are screened into a prospective protocol and the various assignments to group status (risk/no risk exposure) are made. Statistical approaches that help control for error associated with varying follow up lengths and confounding variables should be used. The amount of follow up time should be taken under consideration in future studies as well so critical time periods could possibly be identified.
4.3.4. Prevention
An organizing framework to move forward may be to start conceptualizing risk factors within a model of prevention. Prevention science uses information about risk factors and protective factors to create programming using a multi-tiered system across universal (population of children with global developmental delay without regard for individual risk factors), selective (for subgroups of children with elevated risk), and indicated (for individual children showing clear signs of SIB) levels (O’Connell, Boat, & Warner, 2009; not unlike ‘response to intervention’ [RTI] initiatives within regular and special education). Currently, there are no empirical prevention studies regarding the prevention of SIB among individuals at risk or with I/DD. Effective evidence-based prevention programs in the area of children’s mental health addressing externalizing behavior may help inform how to address risk factors for SIB in young children at risk. For example, the Incredible Years is a prevention program that targets social-emotional development and uses curricula at various levels to prevent and address conduct disorder and anti-social behavior among at-risk children (Webster-Stratton & Taylor, 2001). Similar approaches could be tried among samples of children with I/DD considered to be at-risk for SIB.
A prevention science model could help inform the direction of future research by providing a framework for the development of ‘SIB-risk’ screening tools. If nothing else, logic models are useful for creating screening and prevention programs in which a theory of change is depicted to reduce incidence of a condition (e.g., inputs, outputs, outcomes, assumptions, and external factors are specified) but this model also relies on risk factor identification. All prevention programming or screening is therefore predicated on first identifying risk factors for SIB. The idea of screening for risk factors is distinctive from screening for SIB (O’Connell et al., 2009). For example, newborn screening for phenylketonuria (PKU) requires immediate treatment whereas screening for risk factors may indicate a propensity for developing a condition. The aforementioned points taken together suggest, at least to us, that risk factor research is critical and will be needed if effective prevention programming is to be developed.
In conclusion, our purpose was to critically review studies specific to SIB among individuals with or at risk for I/DD and evaluate our current scientific understanding of putative risk factors for the development and persistence of SIB. More specifically, we evaluated the evidence supporting conventional wisdom claims regarding SIB risk factors as reported in studies that utilized retrospective or prospective cohort designs. Overall, we think it is safe to say that our conventional wisdom specific to risk factors in the field of SIB and I/DD research lacks solid empirical evidence. SIB is a multivariate problem, with multiple risk ‘pathways’. Current evidence is limited in support of any particular variable let alone confirming a particular pathway. Future lines of research are needed to address the problem using more precision in terms of how SIB is measured and leveraging the strength of prospective designs to isolate temporal causal relations. To increase long- term positive outcomes, researchers must consider their approach to the problem. It may be that the past is not necessarily the guide to the future when it comes to prior work and study designs. Ours was a review of approach and methods which is necessarily ‘looking backward’, but we acknowledge any conversation about modeling risk would also necessarily be built on theory. We were critiquing methods, but it may also be that there needs to be attention given to the different conceptual models of SIB that would inform ‘where to look’ as much as the ‘how to look’. Given the scope of the problem and severity of the burden, it is imperative we consider new approaches with a goal of early intervention or prevention.
Acknowledgements
This work was supported, in part, by the Eunice Kennedy Shriver NICHD/NIH – Grant HD 44763 and the Birkmaier Chair and Distinguished McKnight Professorship for FS.
Funding
This work was supported, in part, by grants from the National Institutes of Health under award no HD 44763.
Footnotes
Declaration of Competing Interest
None.
References
- Anderson LT, & Ernst M (1994). Self-injury in Lesch-Nyhan disease. Journal of Autism and Developmental Disorders, 24(1), 67–81. [DOI] [PubMed] [Google Scholar]
- Arron K, Oliver C, Moss J, Berg K, & Burbidge C (2011). The prevalence and phenomenology of self-injurious and aggressive behaviour in genetic syndromes. Journal of Intellectual Disability Research, 55(2), 109–120. [DOI] [PubMed] [Google Scholar]
- Aschengrau A, & Seage GR (2014). Essentials of epidemiology in public health. Burlington, MA: Jones & Bartlett Publishers. [Google Scholar]
- Baghdadli A, Pascal C, Grisi S, & Aussilloux C (2003). Risk factors for self-injurious behaviours among 222 young children with autistic disorders. Journal of Intellectual Disability Research, 47, 622–627. [DOI] [PubMed] [Google Scholar]
- Baghdadli A, Picot MC, Pry R, Michelon C, Burzstejn C, Lazartigues A, & Aussilloux C (2008). What factors are related to a negative outcome of self-injurious behavior during childhood in pervasive developmental disorders? Journal of Applied Research in Intellectual Disabilities, 21, 142–149. [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, & Gatzke-Kopp L (2009). Multifinality in the development of personality disorders: A biology× sex× environment interaction model of antisocial and borderline traits. Development and Psychopathology, 21(3), 735–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkson G (2002). Early development of stereotyped and self-injurious behaviors: II. Age trends. American Journal on Mental Retardation, 107, 468–477. [DOI] [PubMed] [Google Scholar]
- Berkson G, Tupa M, & Sherman L (2001). Early development of stereotyped and self injurious behaviors: I. incidence. American Journal on Mental Retardation, 106, 539–547. [DOI] [PubMed] [Google Scholar]
- Bodfish JW, Crawford TW, Powell S, Parker DE, et al. (1995). Compulsions in adults with mental retardation: Prevalence, phenomenology, and comorbidity with stereotypy and self-injury. American Journal on Mental Retardation, 100(2), 183–192. [PubMed] [Google Scholar]
- Breese GR, Knapp DJ, Criswell HE, Moy SS, Papadeas ST, & Blake BL (2005). The neonate-6-hydroxydopamine-lesioned rat: a model for clinical neuroscience and neurobiological principles. Brain Res.Brain Res.Rev, 48, 57–73. [DOI] [PubMed] [Google Scholar]
- Burt BA (2001). Definitions of risk. Journal of Dental Education, 65(10), 1007–1008. [PubMed] [Google Scholar]
- Carr EG (1977). The motivation of self-injurious behavior: A review of some hypotheses. Psychological Bulletin, 84, 800–816. [PubMed] [Google Scholar]
- Chadwick O, Kusel Y, & Cuddy M (2008). Factors associated with the risk of behaviour problems in adolescents with severe intellectual disabilities. Journal of Intellectual Disability Research, 52(10), 864–876. [DOI] [PubMed] [Google Scholar]
- Chadwick O, Kusel Y, Cuddy M, & Taylor E (2005). Psychiatric diagnoses and behaviour problems from childhood to early adolescence in young people with severe intellectual disabilities. Psychological Medicine, 35, 751–760. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Blender JA (2006). A multiple-levels-of-analysis perspective on resilience: Implications for the developing brain, neural plasticity, and preventive interventions. Annals of the New York Academy of Sciences, 1094(1), 248–258. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Rogosch FA (1996). Equifinality and multifinality in developmental psychopathology. Development and Psychopathology, 8(4), 597–600. [Google Scholar]
- Cooper SA, Smiley E, Allan LM, Jackson A, Finlayson J, Mantry D, et al. (2009). Adults with intellectual disabilities: Prevalence, incidence and remission of self-injurious behaviour, and related factors. Journal of Intellectual Disability Research, 53, 200–216. [DOI] [PubMed] [Google Scholar]
- Crawford H, Karakatsani E, Singla G, & Oliver C (2019). The persistence of self-injurious and aggressive behavior in males with fragile X syndrome over 8 years: A longitudinal study of prevalence and predictive risk markers. Journal of Autism and Developmental Disorders, 49(7), 2913–2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies LE, & Oliver C (2016). Self-injury, aggression and destruction in children with severe intellectual disability: Incidence, persistence and novel, predictive behavioural risk markers. Research in Developmental Disabilities, 49, 291–301. [DOI] [PubMed] [Google Scholar]
- Devine DP (2012). Animal models of self-injurious behaviour: an overview. Psychiatric disorders, 65–84. [DOI] [PubMed] [Google Scholar]
- Dimian AF, Botteron KN, Dager SR, Elison JT, Estes AM, Pruett JR, & Network I (2017). Potential risk factors for the development of self-injurious behavior among infants at risk for autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(5), 1403–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H, & Folstein S (2007). Atypical behaviors in children with autism and children with a history of language impairment. Research in Developmental Disabilities, 28(2), 145–162. [DOI] [PubMed] [Google Scholar]
- Emerson E, Kiernan C, Alborz A, Reeves D, Mason H, Swarbrick R, … Hatton C (2001a). Predicting the persistence of severe self-injurious behavior. Research in Developmental Disabilities, 22, 67–75. [DOI] [PubMed] [Google Scholar]
- Emerson E, Kiernan C, Alborz A, Reeves D, Mason H, Swarbrick R, … Hatton C (2001b). The prevalence of challenging behaviors: A total population study. Research in Developmental Disabilities, 22, 77–93. [DOI] [PubMed] [Google Scholar]
- Gal E, Dyck MJ, & Passmore A (2009). The relationship between stereotyped movements and self-injurious behavior in children with developmental or sensory disabilities. Research in Developmental Disabilities, 30, 342–352. [DOI] [PubMed] [Google Scholar]
- Gulsrud A, Lin CE, Park MN, Hellemann G, & McCracken J (2018). Self-injurious behaviours in children and adults with autism spectrum disorder (ASD). Journal of Intellectual Disability Research, 62(12), 1030–1042. [DOI] [PubMed] [Google Scholar]
- Hall S, Oliver C, & Murphy G (2001). Early development of self-injurious behavior: An empirical study. American Journal on Mental Retardation, 106(2), 189–199. [DOI] [PubMed] [Google Scholar]
- Hessl D, Tassone F, Cordeiro L, Koldewyn K, McCormick C, Green C, & Hagerman RJ (2008). Brief report: Aggression and stereotypic behavior in males with fragile X syndrome—Moderating secondary genes in a “single gene” disorder. Journal of Autism and Developmental Disorders, 38(1), 184–189. [DOI] [PubMed] [Google Scholar]
- Hoch J, Spofford L, Dimian A, Tervo R, MacLean WE, & Symons FJ (2015). A direct comparison of self-injurious behavior between preschool-aged children with and without developmental delays. Journal of Pediatric Psychology, 41(5), 566–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata BA, Dorsey MF, Slifer KJ, Bauman KE, & Richman GS (1982/1994). Toward a functional analysis of self-injury. Analysis and Intervention in Developmental Disabilities, 2, 3–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jan JE, Good WV, Freeman RD, & Espezel H (1994). Eye-poking. Developmental Medicine and Child Neurology, 36, 321–325. [DOI] [PubMed] [Google Scholar]
- Kemp AS, Fillmore PT, Lenjavi MR, Lyon M, Chicz-DeMet A, Touchette PE, & Sandman CA (2008). Temporal patterns of self-injurious behavior correlate with stress hormone levels in the developmentally disabled. Psychiatry Research, 157 (1–3), 181–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiernan C, & Alborz A (1996). Persistence and change in challenging behaviour and problem behaviours of young adults with intellectual disability living in the family home. Journal of Applied Research in Intellectual Disabilities, 9, 181–193. [Google Scholar]
- Kim JA, Szatmari P, Bryson SE, Streiner DL, & Wilson FJ (2000). The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism, 4(2), 117–132. [Google Scholar]
- Kurtz PF, Chin MD, Huete JM, Tarbox RSF, O’Connor JT, Paclawskyj TR, & Rush KS (2003). Functional analysis and treatment of self-injurious behavior in young children: A summary of 30 cases. Journal of Applied Behavior Analysis, 36, 205–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laverty C, Oliver C, Moss J, Nelson L, & Richards C (2020). Persistence and predictors of self injurious behaviour in autism: A ten-year prospective cohort study. Molecular Autism, 11(1), 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindauer SE, DeLeon IG, & Fisher WW (1999). Decreasing signs of negative affect and correlated self-injury in an individual with mental retardation and mood disturbances. Journal of Applied Behavior Analysis, 32(1), 103–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLean WE, Tervo RC, Hoch J, Tervo M, & Symons FJ (2010). Self-injury among a community cohort of young children at risk for intellectual and developmental disabilities. Journal of Pediatrics, 157, 979–983. [DOI] [PubMed] [Google Scholar]
- McClintock K, Hall S, & Oliver C (2003). Risk markers associated with challenging behaviours in people with intellectual disabilities: A meta-analytic study. Journal of Intellectual Disability Research, 47, 405–416. [DOI] [PubMed] [Google Scholar]
- Medeiros K, Curby TW, Bernstein A, Rojahn J, & Schroeder SR (2013). The progression of severe behavior disorder in young children with intellectual and developmental disabilities. Research in Developmental Disabilities, 34(11), 3639–3647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt T (2005). The new look of behavioral genetics in developmental psychopathology: Gene-environment interplay in antisocial behaviors. Psychological Bulletin, 131(4), 533–554. [DOI] [PubMed] [Google Scholar]
- Muris P, Steerneman P, Merckelbach H, Holdrinet I, & Meesters C (1998). Comorbid anxiety symptoms in children with pervasive developmental disorders. Journal of Anxiety Disorders, 12(4), 387–393. [DOI] [PubMed] [Google Scholar]
- Murphy G, Hall S, Oliver C, & Kissi-Debra R (1999). Identification of early self-injurious behaviour in young children with intellectual disabilities. Journal of Intellectual Disability Research, 43, 149–163. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health. In. Treatment of destructive behaviors in persons with developmental disabilities. (NIH Publication No. 91–2410), (1991). [Google Scholar]
- Nissen JMJF, & Haveman MJ (1997). Mortality and avoidable death in people with severe self-injurious behaviour: Results of a Dutch study. Journal of Intellectual Disability Research, 41(3), 252–257. [PubMed] [Google Scholar]
- Nock MK (2009). Understanding nonsuicidal self-injury: Origins, assessment, and treatment. Washington, DC: American Psychological Association. [Google Scholar]
- Nøttestad JA, & Linaker OM (2001). Self-injurious behaviour before and after deinstitutionalization. Journal of Intellectual Disability Research, 45(2), 121–129. [DOI] [PubMed] [Google Scholar]
- Novak MA, Crockett CM, & Sackett GP (2002). Self-injurious behavior in captive macaque monkeys. In Schroeder SR, Oster-Granite ML, & Thompson T (Eds.), Self injurious behavior: Gene-brain-behavior relationships (pp. 151–161). Washington D.C: American Psychological Association. [Google Scholar]
- O’Connell ME, Boat T, & Warner KE (2009). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Washington, D.C.: National Academy of Sciences. [PubMed] [Google Scholar]
- Oliver C, Hall S, & Murphy GH (2005). The early development of self-injurious behaviour: Evaluating the role of social reinforcement. Journal of Intellectual Disability Research, 49, 591–599. [DOI] [PubMed] [Google Scholar]
- Oliver C, Petty J, Ruddick L, & Bacarese-Hamilton M (2012). The association between repetitive, self-injurious and aggressive behavior in children with severe intellectual disability. Journal of Autism and Developmental Disorders, 42(6), 910–919. [DOI] [PubMed] [Google Scholar]
- Pitcher MH, Nieto FR, & Cervero F (2013). Stimulation of cutaneous low threshold mechanoreceptors in mice after intracolonic capsaicin increases spinal c-Fos labeling in an NKCC1-dependent fashion. Journal of Pain, 14(1), 57–65. [DOI] [PubMed] [Google Scholar]
- Rattaz C, Michelon C, & Baghdadli A (2015). Symptom severity as a risk factor for self injurious behaviours in adolescents with autism spectrum disorders. Journal of Intellectual Disability Research, 59(8), 730–741. [DOI] [PubMed] [Google Scholar]
- Richards C, Moss J, Nelson L, & Oliver C (2016). Persistence of self-injurious behaviour in autism spectrum disorder over 3 years: A prospective cohort study of risk markers. Journal of Neurodevelopmental Disorders, 8(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards C, Oliver C, Nelson L, & Moss J (2012). Self-injurious behaviour in individuals with autism spectrum disorder and intellectual disability. Journal of Intellectual Disability Research, 56(5), 476–489. [DOI] [PubMed] [Google Scholar]
- Richman DM, & Lindauer SE (2005). Longitudinal assessment of stereotypic, protoinjurious, and self-injurious behavior exhibited by young children with developmental delays. American Journal on Mental Retardation, 110, 439–450. [DOI] [PubMed] [Google Scholar]
- Rojahn J (1994). Epidemiology and topographic taxonomy of self-injurious behavior. In Thompson T, & Gray DB (Eds.), Destructive behavior in developmental disabilities: Diagnosis and treatment (pp. 49–67). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Rojahn J, Barnard-Brak L, Medeiros K, & Schroeder SR (2015). Stereotyped behaviours as precursors of self-injurious behaviours: A longitudinal study with infants and toddlers at risk for developmental delay. Journal of Intellectual Disability Research, 1–11. [DOI] [PubMed] [Google Scholar]
- Rojahn J, Schroeder SR, & Hoch TA (2008). Self-injurious behavior in intellectual disabilities. Amsterdam, The Netherlands: Elsevier. [Google Scholar]
- Rovine MJ, & Lawrence LL (2017). Person-specific individual difference approaches in developmental research. In Card NA (Ed.), Monographs of the Society for Research in Child Development. Serial No. 325: vol. 82. Developmental Methodology (pp. 84–104). No. 2. [DOI] [PubMed] [Google Scholar]
- Sandman CA, Spence MA, & Smith M (1999). Pro-opiomelanocortin (POMC) dysregulation and response to opiate blockers. Mental Retardation and Developmental Disability Research Reviews, 5, 314–321. [Google Scholar]
- Sandman CA, Touchette P, Lenjavi M, Marion S, & Chicz-DeMet A (2003). β-Endorphin and ACTH are dissociated after self-injury in adults with developmental disabilities. American Journal on Mental Retardation, 108(6), 414–424. [DOI] [PubMed] [Google Scholar]
- Sandman CA, Touchette PE, Marion SD, & Chicz-DeMet A (2008). The role of proopiomelanocortin (POMC) in sequentially dependent self-injurious behavior. Developmental Psychobiology: The Journal of the International Society for Developmental Psychobiology, 50(7), 680–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder SR, Marquis JG, Reese RM, Richman DM, Mayo-Ortega R, & Lawrence L (2014). Risk factors for self-injury, aggression, and stereotyped behavior among young children at risk for intellectual and developmental disabilities. American Journal of Intellectual and Developmental Disabilities, 119(4), 351–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder SR, Schroeder CS, Smith B, & Dalldorf J (1978). Prevalence of self injurious behaviors in a large state facility for the retarded: A three-year follow-up study. Journal of Autism and Childhood Schizophrenia, 8, 261–269. [DOI] [PubMed] [Google Scholar]
- Soke GN, Rosenberg SA, Hamman RF, Fingerlin T, Robinson C, Carpenter L, & DiGuiseppi C (2016). Brief report: Prevalence of self-injurious behaviors among children with autism spectrum disorder—A population-based study. Journal of Autism and Developmental Disorders, 46(11), 3607–3614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sovner R, & Fogelman S (1996). Irritability and Mental Retardation. Seminars in Clinical Neuropsychiatry, 1(2), 105–114. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky DG, Scahill L, Gadow KD, Arnold LE, Aman MG, McDougle CJ, & Vitiello B (2008). Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology, 36(1), 117–128. [DOI] [PubMed] [Google Scholar]
- Symons FJ (2011). Self-injurious behavior in neurodevelopmental disorders: Relevance of nociception and immune mechanisms. Neuroscience and Biobehavioral Reviews, 35(5), 1266–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symons FJ, & Devine DD (2013). Biological risk and early development of self-injury in intellectual disability. In Hastings R, & Rojahn J (Eds.), Vol 44. International review of research in intellectual and developmental disabilities (pp. 37–67). [Google Scholar]
- Symons FJ, Shinde S, Clary J, Harper V, & Bodfish JW (2010). A sham-controlled sensory testing protocol for nonverbal individuals with intellectual and developmental disabilities: Self-injury and gender effects. Journal of Pain, 11, 773–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symons FJ, Sutton KA, Walker C, & Bodfish JW (2003). Altered diurnal pattern of salivary substance P in adults with developmental disabilities and chronic self injury. American Journal on Mental Retardation, 108(1), 13–18. [DOI] [PubMed] [Google Scholar]
- Symons FJ, Thompson A, & Rodriguez MR (2004). Self-injurious behavior and the efficacy of naltrexone treatment: A quantitative review. Mental Retardation and Developmental Disabilities Research Reviews, 10, 193–200. [DOI] [PubMed] [Google Scholar]
- Symons FJ, Wendelschafer-Crabb G, Kennedy W, Hardrict R, Dahl N, & Bodfish JW (2008). Evidence of altered epidermal nerve fiber morphology in adults with self injurious behavior and neurodevelopmental disorders. Pain, 134 (1–2), 232–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symons FJ, Wendelschafer-Crabb G, Kennedy W, Heeth W, & Bodfish JW (2009). Degranulated mast cells in the skin of adults with self-injurious behavior and neurodevelopmental disorders. Brain, Behavior, and Immunity, 23(3), 365–370. [DOI] [PubMed] [Google Scholar]
- Szklo M, & Nieto FJ (2014). Epidemiology beyond the basics (3rd ed.). Burlington, MA: Jones & Bartlett Learning. [Google Scholar]
- Taylor L, Oliver C, & Murphy G (2011). The chronicity of self-injurious behaviour: A long term follow-up of a total population study. Journal of Applied Research in Intellectual Disability, 25, 107–117. [Google Scholar]
- Totsika V, Toogood S, Hastings RP, & Lewis S (2008). Persistence of challenging behaviours in adults with intellectual disability over a period of 11 years. Journal of Intellectual Disability Research, 52, 446–457. [DOI] [PubMed] [Google Scholar]
- Tsiouris JA, & Brown WT (2004). Neuropsychiatric symptoms of fragile X syndrome. CNS Drugs, 18(11), 687–703. [DOI] [PubMed] [Google Scholar]
- Tsiouris JA, Cohen IL, Patti PJ, & Korosh WM (2003). Treatment of previously undiagnosed psychiatric disorders in persons with developmental disabilities decreased or eliminated self-injurious behavior. The Journal of Clinical Psychiatry, 64 (9), 1081–1090. [DOI] [PubMed] [Google Scholar]
- Verhoeven WMA, Tuinier S, Van den Berg YWMM, Coppus AMW, Fekkes D, Pepplinkhuizen L, & Thijssen JHH (1999). Stress and self-injurious behavior; hormonal and serotonergic parameters in mentally retarded subjects. Pharmacopsychiatry, 32(01), 13–20. [DOI] [PubMed] [Google Scholar]
- Viera AJ (2008). Odds ratios and risk ratios: What’s the difference and why does it matter? Southern Medical Journal, 101(7), 730–734. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, & Taylor T (2001). Nipping early risk factors in the bud: Preventing substance abuse, delinquency, and violence in adolescence through interventions targeted at young children (0–8 years). Prevention Science, 2, 165–190. [DOI] [PubMed] [Google Scholar]
- Weisbrot DM, Gadow KD, DeVincent CJ, & Pomeroy J (2005). The presentation of anxiety in children with pervasive developmental disorders. Journal of Child & Adolescent Psychopharmacology, 15(3), 477–496. [DOI] [PubMed] [Google Scholar]
Further readings
- Murphy GH, Beadle-Brown J, Wing L, Gould J, Shah A, & Holmes N (2005). Chronicity of challenging behaviours in people with severe intellectual disabilities and/or autism: A total population sample. Journal of Autism and Developmental Disorders, 35(4), 405–418. [DOI] [PubMed] [Google Scholar]
- Richman DM, Barnard-Brak L, Bosch S, Thompson S, Grubb L, & Abby L (2012). Predictors of self-injurious behaviour exhibited by individuals with autism spectrum disorder. Journal of Intellectual Disability Research, 1–11. [DOI] [PubMed] [Google Scholar]
- Rojahn JL (1984). Self-injurious behavior in institutionalized, severely/profoundly retarded adults: Prevalence data and staff agreement. Journal of Behavioral Assessment, 6, 13–27. [Google Scholar]


