Abstract
Introduction:
Central cancer registries are responsible for managing appropriate research contacts and record releases. Do not contact (DNC) flags are used by some registries to indicate patients who should not be contacted or included in research. Longitudinal changes in DNC coding practices and definitions may result in a lack of code standardization and inaccurately include or exclude individuals from research.
Purpose:
We performed a comprehensive manual review of DNC cases in the Utah Cancer Registry to inform updates to standardization of DNC code definitions, and use of DNC codes for exclusion/inclusion in research.
Methods:
We identified 858 cases with a current or prior DNC flag in the SEER Data Management System (SEER*DMS) or a research database, with cancers diagnosed from 1957-2021. We reviewed scanned images of correspondence with cases and physicians, incident forms, and comments in SEER*DMS and research databases. We evaluated whether there was evidence to support the current DNC code, a different DNC code, or insufficient evidence for any code.
Results:
Of the 755 cases that had a current DNC flag and reason code in SEER*DMS, the distribution was as follows: 58%, Patient requested no contact; 20%, Physician denied; 13%, Patient is not aware they have cancer; 4%, Patient is mentally disabled [sic]; 4%, Other; and 1%, Unknown. In 5% of these cases, we found evidence supporting a different DNC reason code. Among cases included because of a prior DNC flag in SEER*DMS (n = 10) or a DNC flag in a research database (ie, cases with no current DNC flag or reason code in SEER*DMS, n = 93), we found evidence supporting the addition of a SEER*DMS DNC flag and reason code in 50% and 40% of cases, respectively. We identified DNC reason codes with outdated terminology (Patient is mentally disabled) and codes that may not accurately reflect patient research preferences (Physician denied without asking the patient). To address this, we identified new reason codes, retired old reason codes, and updated current reason code definitions and research handlings.
Conclusion:
The time and resource investment in manual review allowed us to identify and, in most cases, resolve discordance in DNC flags and reason codes, adding reason codes when they were missing. This process was valuable because it informed recommended changes to DNC code definitions and research handlings that will ensure more appropriate inclusion and exclusion of cancer cases in research.
Keywords: cancer registries, cancer research, do not contact record releases, research contacts, Surveillance, Epidemiology, End Results (SEER) Program
Introduction
Central cancer registries are the foundational source of information for cancer surveillance and control in the United States1,2 and are widely used for population-based research.3,4 Central registries participating in the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) Program or the Centers for Disease Control and Prevention's National Program of Cancer Registries (NPCR) are required to maintain a population-based reporting system with annual follow-up that meets specific quality standards.1,2,5,6 These practices allow for more accurate data reporting and timely dissemination of information for cancer surveillance and control.3,7,8 Cancer is a reportable disease, and individuals diagnosed with cancer cannot opt out of state-legislated public health surveillance reporting.9 However, many registries are also engaged in contacting and recruiting representative samples of individuals with cancer or survivors for research, which requires careful tracking and documentation of individuals’ preferences for being contacted and having their records released to ensure patient privacy.1
The handling of research contacts and record releases differs across registries, including whether physician permission is required before contacting a patient and whether the registry or the researchers make the first contact with the patient.10 Additionally, some registries are "opt in," meaning a patient must agree to research contacts or record releases, while other registries are "opt out." Many cancer registries have developed tools for managing and documenting patient contacts and record releases. For example, in the SEER Data Management System (SEER*DMS), a patient record can be flagged as Do not contact (DNC), and a reason code explaining the flag can be provided.11 Because of different processes for handling research contacts and recorded releases, the use and interpretation of the DNC flag and reason code are not standardized across registries. Additionally, coding practices and code definitions can change over time within a registry. Although this flexibility allows registries to use the DNC features to meet their current operational needs, changes in code definitions over time may inaccurately exclude individuals from opportunities to participate in studies requiring contact or research linkages.
The Utah Cancer Registry is a SEER and NPCR registry that receives reports for approximately 14,000 new cancer diagnoses every year.12 Cancer was first designated as a reportable disease in Utah in 1948. However, systematic cancer surveillance was not conducted in the state until 1966. The Utah Cancer Registry was designated as a SEER site in 1973 and joined NPCR in 2017. The Utah Cancer Registry routinely contacts cancer patients or survivors for research, conducts linkages for research studies, and generates research data sets for investigators. The Utah Cancer Registry uses the DNC flag in SEER*DMS to indicate individuals who should not be contacted and whose records potentially should be excluded from research linkages. DNC reason codes provide the rationale for a flag and can be assigned at either the tumor or patient level. Tumor-level flags should exclude individuals from research contacts for that diagnosis only (eg, if the person is not aware of the cancer diagnosis), while patient-level flags exclude individuals from research contacts for all diagnoses and specific database linkages. Contact events with individuals or health care providers can result in a DNC flag. DNC reason codes correspond to situations arising from common patient responses during a contact event, such as, "I do not want to be contacted" or "I do not have cancer." Additionally, research databases for specific projects have a separate DNC data field used by research staff. Research databases do not automatically transfer DNC codes to SEER*DMS, and manual transfers from these databases may have missed, incorrectly assigned, or even erased codes. Additionally, while the Utah Cancer Registry DNC flag is now used only for research contacts and linkages, it was historically used for operational practices such as contact events for follow-up. Concern that these longitudinal changes may have resulted in a lack of code standardization and the realization that contemporizing current code definitions and practices were necessary prompted a manual review of records in the Utah Cancer Registry. We reviewed records with a current or prior DNC flag in SEER*DMS or a DNC code in our research database for evidence supporting the flag and reason code. This manual review informed efforts to appropriately update and standardize codes and processes for coding DNCs and handling research contacts within the Utah Cancer Registry.
Methods
Identification of Cancer Cases with a DNC Flag
We sought to perform a comprehensive review of all cancer cases in the Utah Cancer Registry that were flagged as DNC either in SEER*DMS or in Utah Cancer Registry research databases. Of 401,382 cases in the Utah Cancer Registry diagnosed between 1948 and 2020, we identified 765 with a current (n = 755) or prior (n = 10) DNC flag in SEER*DMS. In order to identify cases that may have been miscoded in SEER*DMS or for which the SEER*DMS code was erased, we also searched Utah Cancer Registry research databases to identify cases that did not have a DNC flag in SEER*DMS, but did have a flag indicating DNC in the research database. Using this method, we identified another 93 cases, for a total of 858 cases with a DNC flag. These cases were diagnosed between 1957 and 2020.
Manual Review of Documentation of DNC Flags and Reason Codes
For all 858 cases, we reviewed all available documentation for evidence related to a current DNC flag or reason code. Documentation included scanned images of correspondence with individuals and physicians, including incident forms, comments in SEER*DMS, and codes and comments in linked research databases. Some sources were from historic practices that have been discontinued, including patient responses to annual contact letters previously used for follow-up and permission request forms sent to physicians. We evaluated whether there was evidence to support the current DNC code, evidence to support a different DNC code, or insufficient evidence for any code. We recorded the evidence type, location, date, description, and the recommended code based on the evidence found. If a record had evidence to support the historic Physician denied reason code, the reason for denial was recorded. For cases with evidence supporting multiple codes, the evidence for all codes was recorded, but a single patient-level code with the highest levels of restrictions for case contact and record release was recommended. A trained research assistant completed the manual review and recorded results in a REDCap database. Training included an introduction to SEER*DMS and research databases as well as a pilot review of 20 cases led by Utah Cancer Registry managers. Throughout the manual review, the reviewer met with the Utah Cancer Registry managers to provide updates on the results of the manual review and discuss coding recommendations, conflicting evidence, and any other questions. We defined discordant cases as those with an absence of evidence for any code or evidence that did not support the current DNC flag or reason code.
Results
All reviewed flags and codes were at the patient, not tumor, level. Of the 858 reviewed cases, most (88%) had a current DNC flag in SEER*DMS, though 1% had a prior DNC flag in SEER*DMS, and another 11% had a DNC flag in a research database but no DNC flag in SEER*DMS (Table 1). Among the 755 cases with a current SEER*DMS DNC flag, the distribution of the current accompanying DNC reason codes was as follows: Patient requested no contact (n = 440; 58%); Physician denied (n = 150; 20%); Patient is not aware they have cancer (n = 100; 13%); Patient is mentally disabled [sic] (n = 27; 4%); Other (n = 27; 4%); and Unknown (n = 11; 1%) (Table 1).
Table 1.
Distribution of Cases Included in the Manual Review
| Source of cases included in the manual review | n | % |
|---|---|---|
| Current SEER*DMS DNC flag | 755 | 88 |
| DNC in research database | 93 | 11 |
| Prior DNC in SEER*DMS | 10 | 1 |
| Total | 858 | 100 |
| Distribution of reason codes among cases with a current DNC flag in SEER*DMS | n | % |
|---|---|---|
| Patient requested no contact (includes requests to have records removed from registry) | 440 | 58 |
| Physician denied | 150 | 20 |
| Patient is not aware they have cancer | 100 | 13 |
| Patient is mentally disabled [sic] | 27 | 4 |
| Other | 27 | 4 |
| Unknown | 11 | 1 |
| Total | 755 | 100 |
DMS, Data Management System; DNC, do not contact.
Cases were identified through 3 sources: those with a current DNC flag in SEER*DMS; those with a prior DNC flag in SEER*DMS; and those with a DNC flag in a research database. Only cases with a current DNC flag in SEER*DMS had a corresponding reason code.
Among the 755 cases with a current SEER*DMS DNC flag, we found evidence supporting the current SEER*DMS code status (ie, supporting the presence of a flag and specific reason code) for 402 cases (53%), evidence supporting a different DNC reason code in 38 cases (5%), and no evidence to support either a flag or a code in 315 cases (42%). Of the 402 cases with evidence supporting the current SEER*DMS code status, 32 (8%) had evidence supporting a different code in addition to the current code. All cases identified in this category had evidence supporting a combination of 2 of the following reason codes: Patient requested their data be removed from registry, Patient requested no contact, or Patient is not aware they have cancer. Of the 315 with no evidence to support either a flag or a code, 150 currently have a DNC flag and historic reason code of Physician denied. This code was based on a historic form sent to physicians that asked them for permission to "locate" the patient for follow-up, not for permission to contact the patient for research purposes. We therefore did not consider responses to this physician contact form to be evidence. The other 165 cases with no evidence to support either a flag or a code had no documentation of any type in SEER*DMS.
Among cases with no current DNC flag or reason code in SEER*DMS that were included because of a prior DNC flag in SEER*DMS (n=10) or a DNC flag in a research database (n=93), we found evidence supporting the addition of a SEER*DMS DNC flag and reason code for 5 (50%) and 37 (40%) cases, respectively. For the remaining 5 (50%) and 56 (60%) cases in each group, respectively, we found no evidence to support either a flag or a code.
For 29 of the total 858 cases reviewed (3%), we found evidence that the patient wanted their records removed from the registry; 23 were currently coded as Patient requested no contact, and 6 were identified from research databases.
Recommendations for DNC Codes and Research Handling in the Utah Cancer Registry
Common reasons for discordance included lack of evidence to support the current DNC flag and reason code, changes in code definitions over time (ie, historic changes), and ambiguity in a physician contact form. These findings informed recommendations for updates to the DNC reason codes to resolve discordance and ensure more appropriate inclusion and exclusion of cancer cases in research.
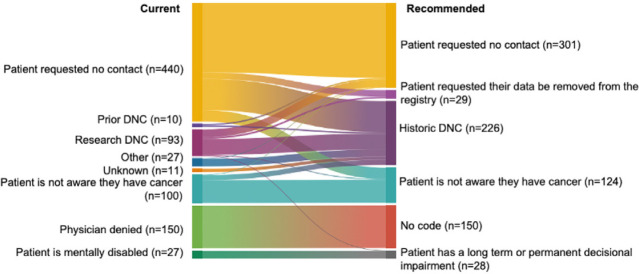
Recommended changes to the Utah Cancer Registry DNC coding include the addition of 2 new reason codes (Patient requested their data be removed from registry and Historic DNC) and the retiring of the Physician denied code. The Patient requested their data be removed from the registry code would be applied to the 29 cases (6 of which were from research databases) with supporting evidence found during the manual review (Figure 1). While cancer is a reportable disease and surveillance is mandated (meaning that records cannot be removed from the Utah Cancer Registry), from a research perspective, we sought to distinguish these cases to exclude their records from all research database linkages as well as research contacts. The Historic DNC code would be applied to the 226 cases with a current or prior DNC code in SEER*DMS or a research database, but no evidence found to support any DNC code during the manual review (Figure 1). Our recommendation is that these cases would be included in research linkages but excluded from research contacts. For all 150 cases currently coded as Physician denied, we recommend removing the DNC flag and including these records in research linkages and research contacts. Additionally, we will contemporize the code definition for Patient is mentally disabled to Patient has a long-term or permanent decisional impairment. For cases included because of a prior DNC flag in SEER*DMS or a current DNC flag in a research database (but with no reason code), we recommend the addition of a SEER*DMS DNC flag and reason code based on the evidence found. This recommendation included adding the Patient requested no contact code to 5 prior DNC cases and 27 research DNC cases; adding the Patient is not aware they have cancer for 3 research DNC cases; and adding the Patient has a long-term or permanent decisional impairment for 1 research DNC case. For cases with a current SEER*DMS DNC flag and reason code, if we found no evidence supporting the current DNC reason code, but did find evidence supporting a different code, we recommend updating to the code with supporting evidence. For cases with evidence found supporting the current reason code and also a different code, we recommended using the code with the highest contact and research restriction. The priority for code recommendation in order of decreasing priority was as follows: (1) Patient requested their data be removed from registry, (2) Patient requested no contact, and (3) Patient is not aware they have cancer. The change in distribution of DNC reason codes following these recommended changes can be found in Figure 2. We propose to use the comprehensive REDCap form that was developed for manual review for future DNC incidents to allow for more informative tracking of future cases.
Figure 1.
Change in the Distribution of Cases and DNC Reason Codes Between the Current Classification and the Recommended Classification Following Manual Review
Figure 2.
Changes in the Proportions of Cases Assigned to DNC Reason Codes Following Manual Review
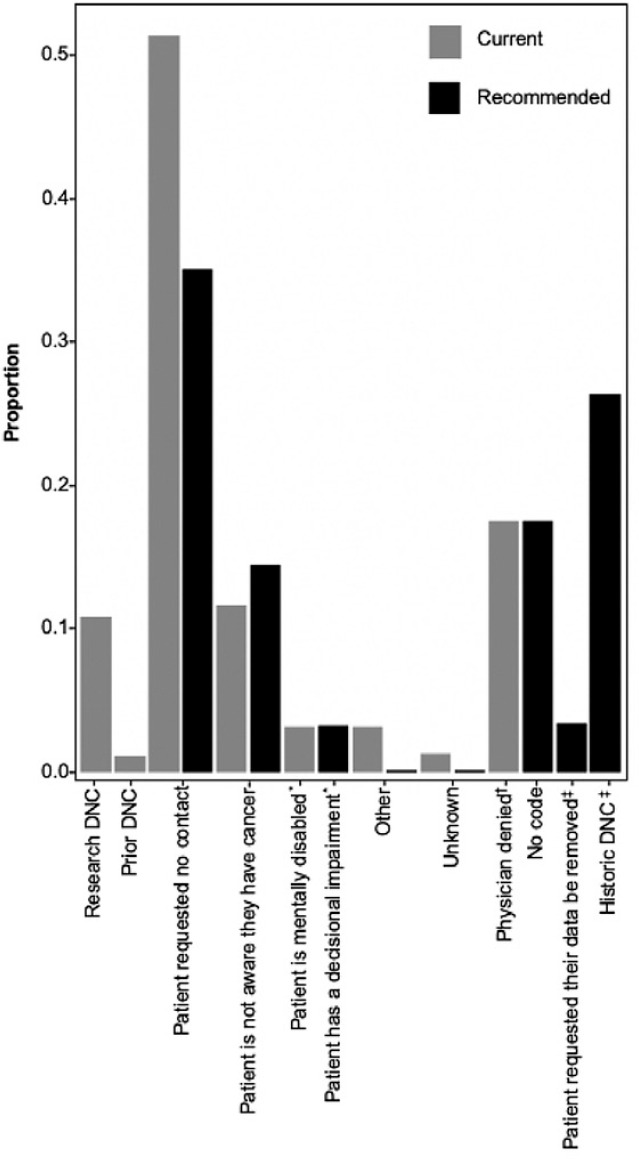
DMS, Data Management System; DNC, do not contact. The proportions of cases classified by current DNC reason codes in SEER*DMS are shown in grey, and the proportions classified by recommended DNC codes are shown in black (n = 858). Cases included because of a prior DNC flag in SEER*DMS or a DNC flag in a research database do not have a current DNC reason code and are included in the "Prior DNC" and "Research DNC" categories, respectively. All individuals in these two categories were re-classified into recommended codes.
*Recommended updated definition DNC codes: Patient has a decisional impairment.
+Recommended retired DNC codes: Physician denied (all of the cases in this category were changed to having no code).
DMS, Data Management System; DNC, do not contact.
Cases included because of a prior DNC flag in SEER*DMS or a DNC flag in a research database do not have a current DNC reason code and are included in the "Prior DNC" and "Research DNC" categories, respectively. The alluvial flow from left to right shows the change in distribution of the cases and DNC reason codes based on the evidence found during manual review.
New NAACCR Standard No Patient Contact Flag
Starting with diagnosis year 2023, the North American Association of Central Cancer Registries (NAACCR) will introduce a new standard data item, No Patient Contact Flag,13 which registries can use to identify cases in which the patient should not be contacted for research purposes. The Utah Cancer Registry will set this new field to, "1 -Patient may NOT be contacted" if a case has any Utah Cancer Registry-defined DNC reason code. In addition to these standardized fields, registries will continue to have autonomy over the use and interpretation of DNC flags and reason codes in SEER*DMS to maintain the reason for DNC.
Discussion
Cancer registries have become increasingly responsible for managing appropriate research contacts and record releases. Through a manual review of case records in SEER*DMS, we identified opportunities to improve DNC flag and reason code assignments and research handling in the Utah Cancer Registry. These findings informed the addition of 2 new reason codes, the retiring of an older reason code, and the contemporizing of code definitions. Results from our study suggest that changes in historical practices and code definitions over time may erroneously include or exclude cases from research contacts and research linkages.
While the Utah Cancer Registry now performs passive follow-up through multiple database linkages, including the National Death Index, we historically performed active follow-up by contacting patients and their providers by letter. Notably, the physician letter used during follow-up asked physicians for permission to "locate" rather than "contact" the patient. During this period of active follow-up, the DNC flag was used to indicate patients who either responded to the letter and asked not to be contacted or providers who marked the "do not locate" box. Consequently, discordant cases were identified during manual review that were currently coded as "physician denied" but had no other evidence to support any DNC code besides the checked box on the physician form. The DNC flag and reason codes are now only used for research and are no longer used for any operational processes. Additionally, while other registries require physician permission prior to research contacts, the Utah Cancer Registry discontinued this practice more than 10 years ago. Thus, we recommend retiring the Physician denied code.
In addition to changes in the use of DNC codes, the Utah Cancer Registry's practices for recording DNC codes, including incident forms and data management systems, have changed over time. During the manual review, we found a subset of discordant cases currently coded as DNC that had no evidence to support any DNC code. Many of these discordant cases likely resulted from a data transfer between data management systems that accidentally removed supporting documentation for any DNC reason code. We recommended recoding these cases with a new DNC reason code, Historic DNC. We also found cases currently coded as DNC in research databases missing a DNC flag and reason code in SEER*DMS. This finding confirmed the suspicion that some DNC codes may have been missed during the manual transfer from research databases to SEER*DMS.
The manual review allowed us to identify reasons for discordance that would have been missed without a review of scanned images, comment boxes, and research databases. The manual review also allowed us to distinguish patients who wanted their records removed from those who did not want to be contacted, and resolve all cases currently coded as Unknown reason. While cancer is a reportable disease and these records will be retained by Utah Cancer Registry for surveillance data sets, distinguishing cases with patients who want their records removed is important for excluding their records from research linkages. These findings informed the addition of a Historic DNC code, and a Patient requested their data be removed from the registry code. Cases with the Historic DNC code will be included in research database linkages but excluded from research contacts, while cases with the Patient requested their data be removed from the registry code will be excluded both from research database linkages and research contacts. We will discuss our recommendations for updated research handling of each DNC reason code with a panel of experts in the ethical conduct of human subjects research, including representatives from our institutional review board, before proceeding with any changes.
Limitations of our manual review include that, for the reason code Patient is not aware they have cancer, we did not distinguish evidence for the tumor- versus patient-level code. A tumor-level code would exclude the patient from research contacts for that diagnosis only while a patientlevel code would exclude the patient from any research contacts. While it would have been possible to distinguish whether the evidence supported the tumor- or patient-level code for some cases, for other cases, this code resulted from a research contact, and it was unclear from the documentation which diagnosis was being referenced. No changes were made to the Patient is not aware they have cancer code, and all cases coded at the patient level will continue to be excluded from research contacts. Updated research patient contact procedures define how to set this reason code at the tumor or patient level going forward.
With increasing concerns about data use and privacy,14 it is important to critically review existing processes for documenting research contacts and record linkages, particularly when potential study participants request not to be contacted. Our manual review of 858 case records in the Utah Cancer Registry took approximately 150 hours (an average of 10 minutes per record) and 25 hours were required for training and meetings with the Utah Cancer Registry managers. Findings from our manual review highlight the need to contemporize codes and coding practices and the value of manual review to inform this process. A manual review of the DNC flags and reason codes in the Utah Cancer Registry informed updates to the Utah Cancer Registry SEER*DMS reason code definitions and practices that will improve the precision of DNC codes in the Utah Cancer Registry. These policy and procedural updates will ensure that our practices are true to the intended code meaning and respect patient wishes while balancing the need for accurate and complete research data.
Footnotes
The Utah Cancer Registry is funded by the National Cancer Institute's SEER Program, Contract No. HHSN261201800016I, and the US Centers for Disease Control and Prevention's National Program of Cancer Registries, Cooperative Agreement No. NU58DP007131, with additional support from the University of Utah and Huntsman Cancer Foundation. The research reported in this publication was also supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.White MC, Babcock F, Hayes NS, et al. The history and use of cancer registry data by public health cancer control programs in the United States. Cancer. 2017;123(suppl 24):4969–4976. doi: 10.1002/cncr.30905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Overview of the SEER program. National Cancer Institute's Surveillance, Epidemiology, and End Results Program website. Accessed September 1, 2022. https://seer.cancer.gov/about/overview.html [Google Scholar]
- 3.Tucker TC, Durbin EB, McDowell JK, Huang B. Unlocking the potential of population-based cancer registries. Cancer. 2019;125(21):3729–3737. doi: 10.1002/cncr.32355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gallicchio L, Elena JW, Fagan S, et al. Utilizing SEER cancer registries for population-based cancer survivor epidemiologic studies: a feasibility study. Cancer Epidemiol Biomarkers Prev. 2020;29(9):1699–1709. doi: 10.1158/1055-9965.EPI-20-0153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NPCR standards. Centers for Disease Control and Prevention website. Published August 29, 2022. Accessed September 14, 2022. https://www.cdc.gov/cancer/npcr/standards.htm [Google Scholar]
- 6.SEER 2022 Submission Requirements and Guidelines. The Surveillance, Epidemiology, and End Results (SEER) Program; 2022. https://seer.cancer.gov/tools/seer.nov22.instructions.pdf [Google Scholar]
- 7.Osborne JD, Wyatt M, Westfall AO, Willig J, Bethard S, Gordon G. Efficient identification of nationally mandated reportable cancer cases using natural language processing and machine learning. J Am Med Inform Assoc. 2016;23(6):1077–1084. doi: 10.1093/jamia/ocw006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xie F, Lee J, Munoz-Plaza CE, Hahn EE, Chen W. Application of text information extraction system for real-time cancer case identification in an integrated healthcare organization. J Pathol Inform. 2017;8:48. doi: 10.4103/jpi.jpi_55_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cancer Reporting Rule, R384-100. Utah Office of Administrative Rules; 2010. https://uofuhealth.utah.edu/documents/cancer-reporting-rule-july-2021 [Google Scholar]
- 10.Beskow LM, Sandler RS, Weinberger M. Research recruitment through US central cancer registries: balancing privacy and scientific issues. Am J Public Health. 2006;96(11):1920–1926. doi: 10.2105/AJPH.2004.061556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thornton ML, ed. Standards for Cancer Registries Volume II: Data Standards and Data Dictionary, Record Layout Version 18. North American Association of Central Cancer Registries; 2018. [Google Scholar]
- 12.Millar M, Herget K, Sweeney C. Cancer in Utah: Incidence and Mortality Statistics through 2017. The Utah Cancer Registry; 2020. https://uofuhealth.utah.edu/documents/cancer-utah-2017 [Google Scholar]
- 13.Item 1854, No Patient Contact Flag. In: Thornton ML, ed. Standards for Cancer Registries Volume II: Data Standards and Data Dictionary. Version 23, 24th ed. North American Association of Central Cancer Registries; 2022. [Google Scholar]
- 14.McGraw D, Mandl KD. Privacy protections to encourage use of health-relevant digital data in a learning health system. NPJ Digit Med. 2021;4(1):1–11. doi: 10.1038/s41746-020-00362-8 [DOI] [PMC free article] [PubMed] [Google Scholar]