ABSTRACT
Background
Large international differences exist in kidney transplantation (KT) rates. We aimed to investigate which factors may explain the total, deceased donor and living donor KT rates over the last decade.
Methods
KT experts from 39 European countries completed the Kidney Transplantation Rate Survey on measures and barriers and their potential effect on the KT rate in their country. In the analyses, countries were divided into low, middle and high KT rate countries based on the KT rate at the start of study period in 2010.
Results
Experts from low KT rate countries reported more frequently that they had taken measures regarding staff, equipment and facilities to increase the total KT rate compared with middle and high KT rate countries. For donor type–specific KT, the largest international differences in measures taken were reported for deceased donor KT, with middle and high KT rate countries taking more measures, such as the use of expanded criteria donor kidneys, the presence of transplantation coordinators and (inter)national exchange of donor kidneys. Once a measure was taken, experts’ opinion on its success was similar across the low, middle and high KT rate countries. Experts from low KT rate countries more often reported potential barriers, such as patients’ lack of knowledge and distrust in the healthcare system.
Conclusions
Particularly in low KT rate countries, the KT rate might be stimulated by optimizing staff, equipment and facilities. In addition, all countries may benefit from measures specific to deceased and living donors.
Keywords: barrier, Europe, kidney transplantation, measure
Graphical Abstract
Graphical Abstract.
KEY LEARNING POINTS.
What is already known about this subject?
Many countries have been taking measures aimed at increasing their kidney transplantation (KT) rate.
The observed international differences in KT rates among European countries suggest that there is still room for improvement.
What this study adds?
We found that experts in the field of KT from low KT rate countries reported perceiving barriers more frequently and had taken measures regarding staff, equipment and facilities to increase the total KT rate.
For donor type–specific KT, the largest international differences in measures taken were reported for deceased donor KT, with middle and high KT rate countries taking more measures, such as the use of expanded criteria donor kidneys, the presence of transplantation coordinators and (inter)national exchange of donor kidneys.
Once a measure was taken, experts’ opinion on its success was similar across the low, middle and high KT rate countries.
What impact this may have on practice or policy?
The present study may assist countries in learning from each other's experiences on what measures may or may not work in attempts to increase KT rates.
INTRODUCTION
Among patients with end-stage kidney disease (ESKD), recipients of a kidney transplant have a longer life expectancy, better quality of life and lower societal costs compared with patients receiving dialysis [1–5]. However, there is a considerable shortage of donor kidneys and the large international differences in kidney transplantation (KT) rates among European countries [6] suggest that in many countries there is still room for improvement [7].
In recent decades, the European Commission and the European nephrology and transplantation communities have made considerable efforts in this regard, e.g. by defining key areas along with specific measures to stimulate transplantation activity in countries and institutions [7–9]. In addition, many countries have put measures into force aimed at increasing their KT rates. In some of them, such as Spain and Croatia, measures have mainly been aimed at increasing the deceased donor KT rate, such as early referral of potential donors to the intensive care unit (ICU) transplantation teams and increasing the acceptance of expanded criteria and non-standard-risk donor organs [10]. Other countries, like the Netherlands and the UK, have made efforts to increase their living donor KT rate, e.g. by using crossover and chain donation for incompatible donors [11–13]. During these processes, countries may face barriers in the access to KT, such as legislation [14] and distrust in the healthcare system [15].
The aim of this study was to investigate which factors may explain the trends in the total, deceased donor and living donor KT rates across European countries over the last decade that are described in an accompanying article [16]. The present study may assist countries in learning from each other's experiences on what measures may or may not work in attempts to increase KT rates.
MATERIALS AND METHODS
Development of the Kidney Transplantation Rate Survey
The Kidney Transplantation Rate Survey (Supplementary Material A) was designed in English using LimeSurvey [17]. A draft survey was developed based on the World Health Organization Global Observatory on Donation and Transplantation (WHO-GODT) Human Organ Donation and Transplantation Survey [18], information from previous studies on measures and barriers in KT [19, 20] and expert opinion. Questions were divided into donation, allocation and transplantation levels and related to total, deceased donor and living donor KT. A pilot survey was completed by five experts in the field of KT from different European countries. These experts provided feedback on the content, structure and feasibility and the survey was modified accordingly. Experts who participated in the pilot study remained eligible as participants for the main study.
Expert selection and invitation
The network of the European Renal Association (ERA) Registry was used to find experts in the field of KT (e.g. representatives of transplantation organizations, transplantation surgeons and nephrologists). For each country for which the KT rate was available in the ERA Registry database or in the GODT database for the period 2010–2018 [21, 22], experts were selected from different regions and transplantation centres. Up to three KT experts from each country were invited by e-mail to complete the survey. The experts received the KT rates of their country over the study period and the link to the online survey. The survey was accessible for 8 weeks (6 July–31 August 2021). The introductory text of the survey informed participants about study aims, instructions on how to complete the survey and about data storage and processing. Participation in the survey was voluntary and participants could indicate whether their name should be included in the acknowledgements of the resulting article. Experts were able to review and change their answers until submission of the survey.
Content of survey
Experts were asked about measures for KT in force in 2010 (explaining the baseline KT rate in a specific country in the first year of the study period), measures in force in 2010 or put into force after 2010 aiming to increase the KT rate between 2010 and 2018 and their opinion on how successful they were and potential barriers for increasing the KT rate in their country and their opinion on the negative effects of those barriers.
Statistical analysis
Country-specific results
Experts could indicate whether or not a particular measure was already in force at the start of the study period in 2010. For the country-specific results (Supplementary Material C), measures were presented as in force (+), not in force (−) or as disagreement between the experts (+/−).
To indicate how successful measures in force in 2010 or put into force thereafter were in increasing the KT rate between 2010 and 2018, experts could choose between the answers ‘measure not put into force (0)’, ‘measure put into force recently and therefore success unknown (0)’, ‘not at all successful (−)’, ‘moderately successful (+)’ and ‘extremely successful (++)’. If there was disagreement between experts within one country, responses were averaged (for more details on recoding, see Supplementary Tables SC1 and SC2).
With regard to potential barriers that could have negatively affected the KT rate between 2010 and 2018, experts were asked to indicate whether this potential barrier had ‘no effect (−)’, ‘a moderate effect (+)’ or ‘a large effect (++)’. Again, if there was disagreement between experts within one country, responses were averaged (for recoding, see Supplementary Table SC3).
Low, middle and high KT rate countries
Using tertiles based on the KT rate in 2010, participating countries were divided into low, middle and high KT rate countries (Supplementary Figure SB1). The country composition of these groups was different for total, deceased donor and living donor KT rates. To ensure that each country was weighted equally, each survey received a weighting factor depending on the number of surveys completed in that country. Across the low, middle and high KT rate countries, the percentage of countries in which a measure or barrier existed was calculated by dividing the sum of surveys with a certain answer category by the total sum of surveys and multiplied by 100. Pearson's chi-squared test was used to test for statistically significant differences across the KT rate country groups.
Ethics
The Medical Ethics Review Committee of the Amsterdam University Medical Center, location Academic Medical Center, Amsterdam, The Netherlands, provided a waiver for ethical approval of this study (W21_290 #21.317).
RESULTS
The KT rate for the period 2010–2018 was available for all European countries except for Andorra, Liechtenstein, Luxembourg, Monaco, Republic of Kosovo, San Marino, Ukraine and Vatican City [16]. For the Republic of Moldova, no expert was found, leaving 39 countries (Table 1 and Supplementary Figure SB1). In total, 110 surveys were distributed, of which 89 surveys (81%) were completed and used for the analyses. In 17 countries (44%) the survey was completed by three experts, in 16 countries (41%) by two experts and in 6 countries (15%) by one expert (Table 1). All country-specific results are presented in Supplementary Material C (Supplementary Tables SC4–SC11).
Table 1:
Number of completed surveys and the KT rate per million population at the start of the study period (in 2010) by country.
| Country | Total | Deceased donor | Living donor | Surveys, n |
|---|---|---|---|---|
| Albania | 3.2 | 0.4 | 2.8 | 2 |
| Austria | 44.7 | 38.1 | 6.6 | 3 |
| Belarus | 12.0 | 11.5 | 0.5 | 2 |
| Belgium | 37.1 | 33.8 | 3.0 | 2 |
| Bosnia-Herzegovina | 6.6 | 2.3 | 4.0 | 3 |
| Bulgaria | 6.5 | 4.9 | 1.6 | 2 |
| Croatia | 54.5 | 49.8 | 4.3 | 3 |
| Cyprus | 38.6 | 9.6 | 28.9 | 3 |
| Czech Republic | 32.9 | 31.3 | 1.6 | 3 |
| Denmark | 41.0 | 22.8 | 18.0 | 3 |
| Estonia | 29.1 | 26.1 | 3.0 | 2 |
| Finland | 32.4 | 30.4 | 2.1 | 2 |
| France | 45.3 | 40.8 | 4.5 | 3 |
| Georgia | 1.9 | 0.0 | 1.9 | 1 |
| Germany | 35.9 | 27.8 | 8.1 | 1 |
| Greece | 11.1 | 7.2 | 3.9 | 1 |
| Hungary | 30.7 | 26.5 | 4.2 | 1 |
| Iceland | 15.7 | 0.0 | 15.7 | 1 |
| Ireland | 38.2 | 33.1 | 5.0 | 3 |
| Italy | 28.6 | 25.5 | 3.1 | 2 |
| Latvia | 23.3 | 22.4 | 0.9 | 2 |
| Lithuania | 22.9 | 20.3 | 2.6 | 2 |
| Malta | 33.8 | 26.5 | 7.2 | 2 |
| Montenegro | 3.2 | 0.0 | 3.2 | 3 |
| Norway | 53.8 | 36.8 | 17.0 | 3 |
| Poland | 26.3 | 24.9 | 1.3 | 3 |
| Portugal | 53.9 | 49.1 | 4.8 | 3 |
| Republic of North Macedonia | 6.0 | 0.0 | 6.0 | 3 |
| Romania | 10.5 | 6.1 | 4.3 | 3 |
| Russia | 7.3 | 6.1 | 1.2 | 2 |
| Serbia | 13.9 | 9.3 | 4.5 | 2 |
| Slovakia | 31.3 | 30.0 | 1.3 | 3 |
| Slovenia | 29.8 | 29.8 | 0.0 | 2 |
| Spain | 47.3 | 42.2 | 5.1 | 2 |
| Sweden | 39.3 | 21.1 | 18.2 | 2 |
| Switzerland | 37.6 | 23.0 | 14.6 | 1 |
| The Netherlands | 52.8 | 24.6 | 28.2 | 3 |
| Turkey | 32.8 | 5.4 | 28.8 | 3 |
| UK | 43.6 | 27.2 | 16.5 | 2 |
Total KT
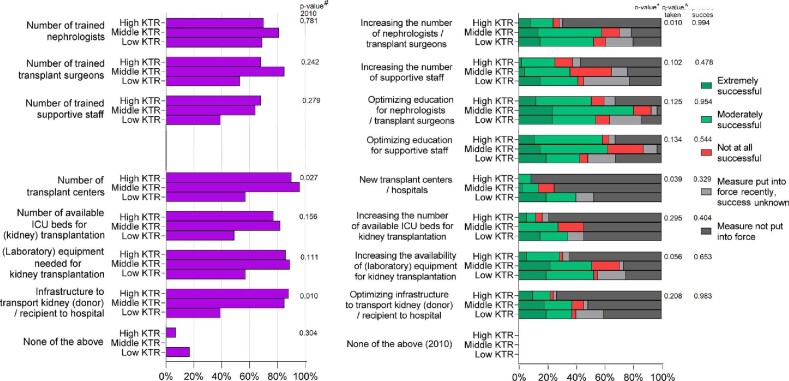
More than 60% of the middle and high KT rate countries indicated that staff, equipment and facilities were already sufficiently available in 2010, with lower percentages in low KT rate countries (Fig. 1 and Supplementary Table SB1). Compared with the middle and high KT rate countries, in the low KT rate countries, fewer experts indicated that the number of transplant centres (P = .027) and the infrastructure to transport kidneys (donors) or recipients to the hospital were sufficiently available in 2010 (P = .010).
Figure 1:
Resources sufficiently available in 2010 (left panel) and measures put into force (right panel) to increase total KT rates between 2010 and 2018, by KT rate group. The Pearson's chi-squared test was used to test for differences between KT rate groups in the percentage of countries for which a measure was in force in 2010 (#P-value 2010), a measure was put into force after 2010 (*P-value taken) and a measure in force was rated as successful (^P-value success). KTR: Kidney Transplantation Rate.
Measures put into force after 2010 that were reported as most successful included optimizing education for nephrologists, transplantation surgeons and supportive staff (Fig. 1 and Supplementary Table SB2). Low KT rate countries more often reported having increased the number of nephrologists, transplant surgeons (P = .010) and the number of transplant centres (P = .039) after 2010. Once a measure was taken, there was no statistically significant difference in the degree of success across low, middle and high KT rate countries.
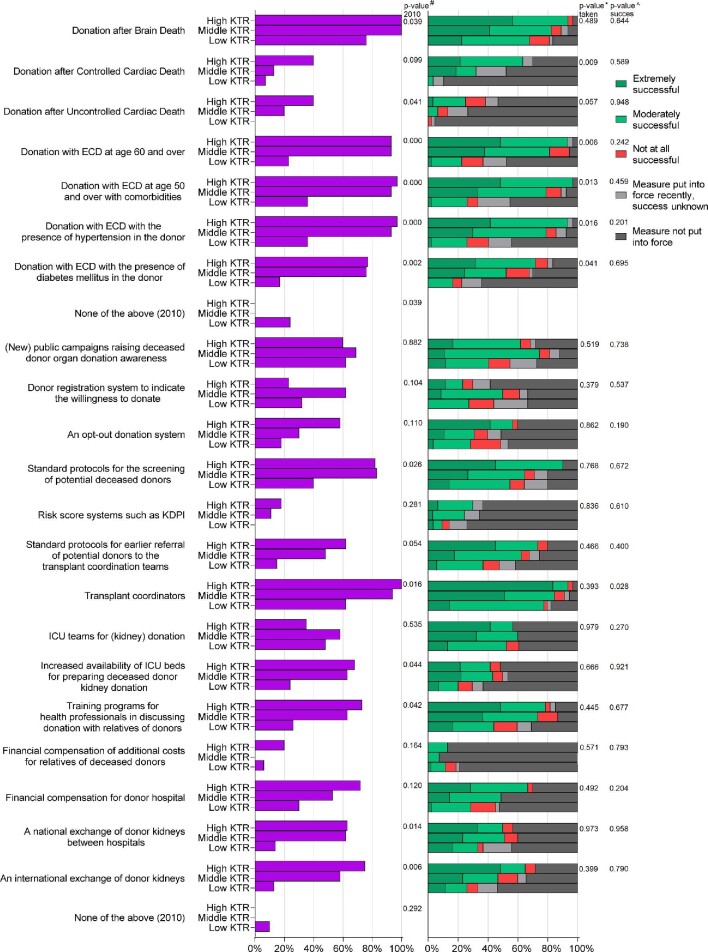
Deceased donor KT
In 2010, 8% of participating countries did not perform deceased donor KTs (Supplementary Table SC6). In the same year, all middle and high KT rate countries did perform deceased donor KTs with kidneys from brain dead donors (DBDs), compared with 76% of low KT rate countries (P = .039; Fig. 2 and Supplementary Table SB3). Compared with middle and high KT rate countries, a lower percentage of low KT rate countries had measures in force in 2010, including donation with expanded criteria donor (ECD) kidneys (P < .01), standard protocols for screening of potential deceased donors (P = .026), the presence of transplant coordinators (P = .016), national (P = .014) and international (P = .006) exchange of donor kidneys and old-for-old programs (P = .025) (Figs. 2 and 3 and Supplementary Table SB3).
Figure 2:
Measures in force in 2010 (left panel) and measures put into force (right panel) on the donation level to increase the deceased donor KT rate between 2010 and 2018, by KT rate group. The Pearson's chi-squared test was used to test for differences between KT rate groups in the percentage of countries for which a measure was in force in 2010 (#P-value 2010), a measure was taken during the study period (*P-value taken) and a measure in force was rated as successful (^P-value success). KDPI: Kidney Donor Profile Index, KTR: Kidney Transplantation Rate.
Figure 3:
Measures in force in 2010 (left panel) and measures put into force (right panel) on the allocation and transplantation level to increase the deceased donor KT rate between 2010 and 2018, by KT rate group. The Pearson's chi-squared test was used to test for differences between KT rate groups in the percentage of countries for which a measure was in force in 2010 (#P-value 2010), a measure was taken during the study period (*P-value taken) and a measure in force was rated as successful (^P-value success).
In >80% of the middle and high KT rate countries the following measures taken were considered successful to increase the deceased donor KT rate during the study period: DBD, donation with ECD kidneys, standard protocols for screening of potential deceased donors, the presence of transplantation coordinators and provision of sufficient information on the possibility of deceased donor KT to ESKD patients (Figs. 2 and 3 and Supplementary Tables SB3 and SB4). During the study period, in low KT rate countries a larger proportion of measures were recently put into place. For some measures, the percentage of low KT rate countries taking the measure remained lower compared with middle and high KT rate countries: donation after controlled cardiac death (P = .009), donation with ECD kidneys (P < .05) and human leucocyte antigen (HLA)-incompatible allocation (P = .009). Once a measure was taken, there was no difference in success across the KT rate countries, except for the presence of transplant coordinators, which was considered moderately successful in low KT rate countries and extremely successful in high KT rate countries (P = .028).
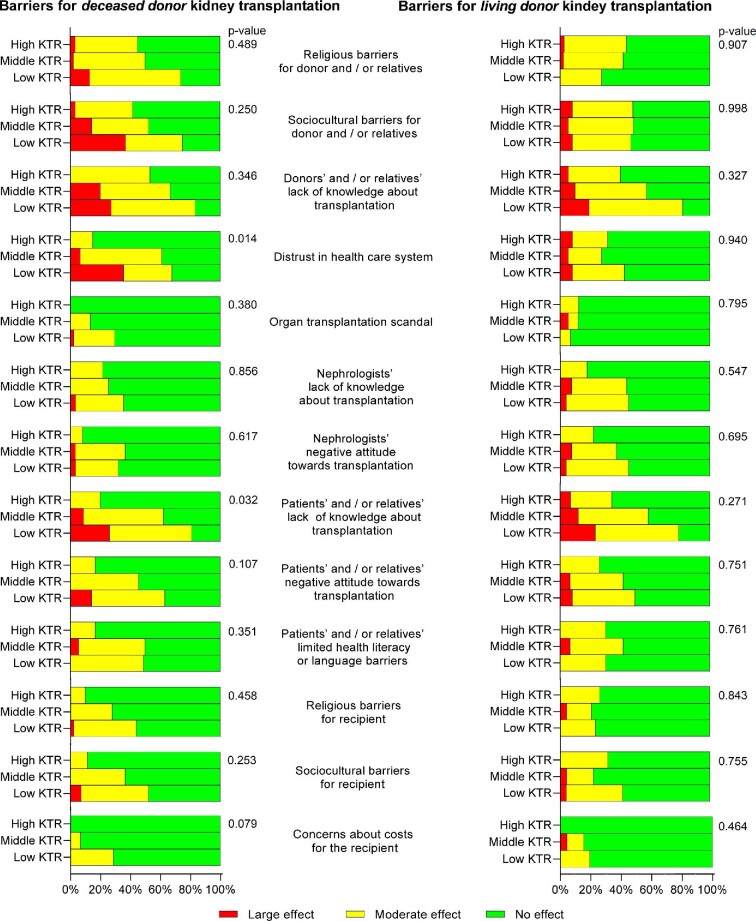
Experts from low KT rate countries more often experienced barriers compared with middle and high KT rate countries (Fig. 4 and Supplementary Table SB5), especially donor- and patient-related factors such as lack of knowledge about transplantation for the recipient and their relatives (P = .032) and distrust in the healthcare system (P = .014).
Figure 4:
Potential barriers for deceased donor (left panel) and living donor (right panel) KT between 2010 and 2018, by KT rate group. The Pearson's chi-squared test was used to test for differences between KT rate groups in the percentage of countries experiencing a barrier for KT.
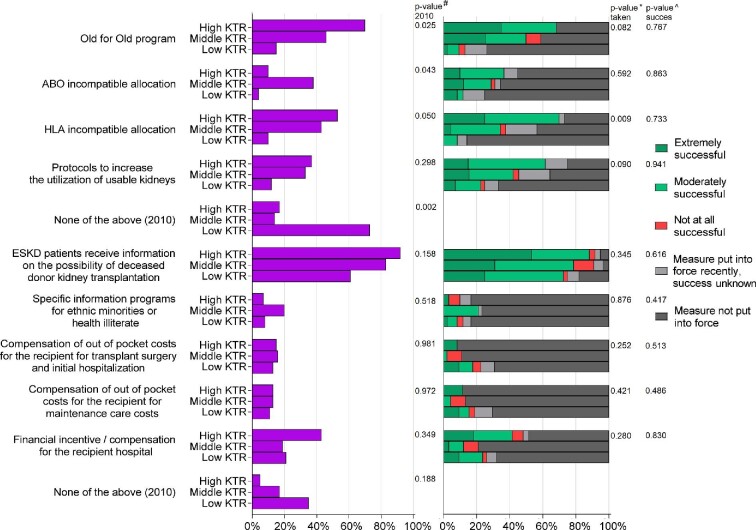
Living donor KT
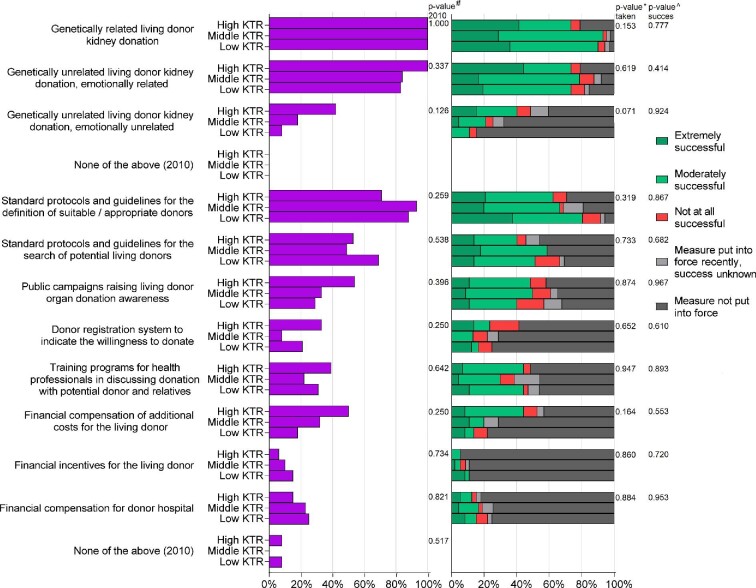
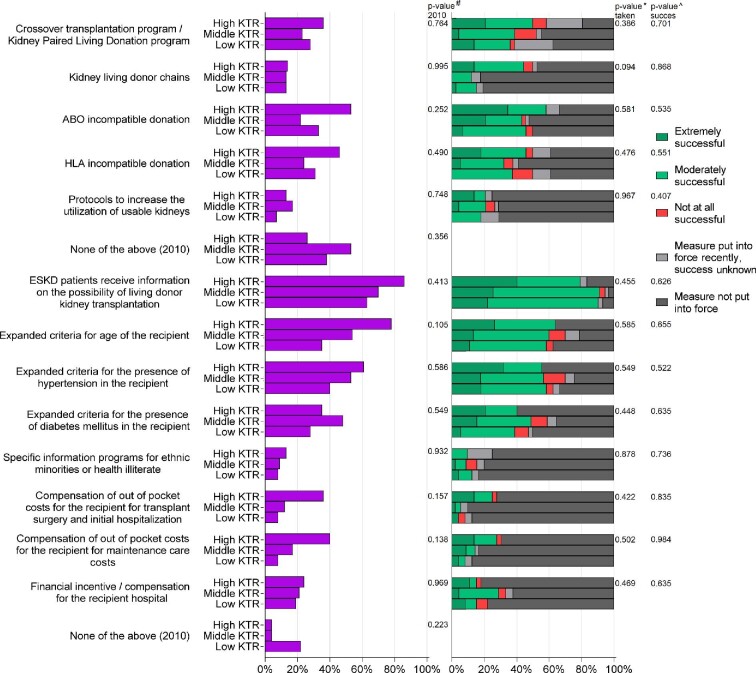
In 2010, all countries performed KTs with kidneys from genetically related living donors (Supplementary Table SC9). Measures put into force and reported as at least moderately successful by >50% of all countries included donation with a genetically or emotionally related living donor, standard protocols and guidelines for the definition of suitable donors, providing sufficient information to ESKD patients on the possibility of living donor KT and expanded criteria for age or hypertension of recipients (Figs. 5 and 6 and Supplementary Table SB7). There were no differences across low, middle and high KT rate countries in measures taken and their success rates (Figs. 5 and 6 and Supplementary Tables SB6 and SB7). Nevertheless, some measures were taken >30% less in low KT rate countries compared with high KT rate countries, such as donation of genetically and emotionally unrelated living donor kidneys, financial compensation for additional costs for the living donor and the use of kidney living donor chains.
Figure 5:
Measures in force in 2010 (left panel) and measures put into force (right panel) on the donation level to increase the living donor KT rate between 2010 and 2018, by KT rate group. The Pearson's chi-squared test was used to test for differences between KT rate groups in the percentage of countries for which a measure was in force in 2010 (#P-value 2010), a measure was taken during the study period (*P-value taken) and a measure in force was rated as successful (^P-value success).
Figure 6:
Measures in force in 2010 (left panel) and measures put into force (right panel) on the allocation and transplantation level to increase the living donor KT rate between 2010 and 2018, by KT rate group. The Pearson's chi-squared test was used to test for differences between KT rate groups in the percentage of countries for which a measure was in force in 2010 (#P-value 2010), a measure was taken during the study period (*P-value taken) and a measure in force was rated as successful (^P-value success).
Although not statistically significant, experts from low KT rate countries more often reported a lack of knowledge about living donor KT in donors, recipients and relatives as a potential barrier (Fig. 4 and Supplementary Table SB8).
DISCUSSION
This study includes a comprehensive overview of measures taken to improve the KT rate and experts’ opinion on the potential effect in 39 European countries with low, middle and high KT rates. It also outlines the barriers that may affect KT. In general, greater international differences existed in measures taken for deceased donor KT than for living donor KT, with middle and high KT rate countries taking more measures. Once a measure was taken, experts’ opinion was similar on the degree of success of the measure across the low, middle and high KT rate countries.
The measure that was considered most successful to increase the total KT rate was optimized education of nephrologists, transplantation surgeons and supportive staff. For deceased donor KT, suggested successful measures according to experts’ opinion included DBD, donation with ECD kidneys, use of standard protocols for the screening of potential donors, the presence of transplantation coordinators and providing information to patients on the possibility of KT. For living donor KT, the most reported successful measures were donation with a genetically or emotionally related living donor, standard protocols and guidelines for the definition of suitable donors, providing information to patients on the possibility of KT and expanded criteria for age or hypertension in the recipient. Regarding perceived barriers for KT, experts from low KT rate countries more often reported donor- and patient-related factors, such as a lack of knowledge and distrust in the healthcare system, compared with middle and high KT rate countries.
Total KT
In middle and high KT rate countries, experts reported that most resources were already sufficiently available in 2010. Thus most middle and high KT rate countries would benefit more from donor type–specific measures. In contrast, in most low KT rate countries, improvement of staff, equipment and facilities is needed to increase the KT rate. A number of these measures have been taken only recently in some countries, so their effect is still unknown. Further in-depth national research is necessary to find which measures are most likely to increase the KT rate.
Also, after our study period, large differences in the total KT rate between European countries remained, ranging from 3 per million population (pmp) in Serbia to 73 pmp in Spain [23, 24]. The KT rate is even higher in the USA (75 pmp) [23], suggesting that in many European countries there is still room for improvement. As a follow-up on the initial European Union Action Plan on organ donation and transplantation [8], in 2019 the European Kidney Health Alliance (EKHA) presented a roadmap with 12 key areas that measures could focus upon to improve the KT rate [25, 26]. These include measures optimizing the transplantation process and improving infrastructure, collaborations, education, equality and research [25]. The (timing of) implementation of specific measures as well as their effectiveness might differ by country depending on, among other things, the ethical and legislative framework [14], sociocultural background [27] and the proportion of KTs performed with living or deceased donors [24].
Measures to increase deceased donor KT
In Europe, ≈70% of KTs are performed with kidneys from deceased donors [24]. In 2010, the largest differences in measures taken between low and high KT rate countries were observed in the use of ECD kidneys, international exchange of donor kidneys, and old for old programs. In countries affiliated with Eurotransplant—an organization that has been implementing all these measures for quite some time—the median age of a deceased donor increased from 53 years in 2010 to 55 years in 2019 [28]. Our results are in line with the EKHA joint statement [25], in that donation of ECD kidneys, standard protocols for screening of potential donors, the presence of transplantation coordinators and providing information to patients are important measures to increase the deceased donor KT rate. Interestingly, no differences were observed between low, middle and high KT rate countries in the financial compensation and incentive measures.
Measures to increase living donor KT
International differences in measures taken and their effect were smaller for living donor KT compared with deceased donor KT. Although transplantation with living donor kidneys is associated with better patient and graft survival [24], nephrologists might be more careful in suggesting living donor kidney donation since the long-term effects for the donor, especially at a young age, still remain uncertain [29]. On the other hand, the results of a previous survey among European nephrologists showed that 71% of the respondents indicated that the uptake of living donor KT should be increased [30]. In the EKHA joint statement, experts also suggest improving the living donor KT rate by expanding the donor and recipient pool (less restrictive eligibility criteria), using financial compensation for the donor and performing donation with a spouse and unrelated donors, which is in line with our study [25].
Barriers
Experts from low KT rate countries more frequently reported donor- and patient-related factors as potential barriers, especially a lack of knowledge about transplantation and distrust in the healthcare system. The results of our study also indicate that providing information about KT to patients helped to increase both living and deceased donor KT. In addition, other studies have indicated that information should be provided to patients earlier, before the start of kidney replacement therapy, to aid in choosing suitable (transplantation) treatment options for the patient [30, 31]. Furthermore, increasing the awareness of KT in the general population and home visits to inform patients and their families may further increase the KT rate [26, 32].
In line with previous studies, our results suggest that nephrologists’ lack of knowledge or negative attitude towards KT might also have a negative effect on the KT rate—be it only limited [30]. Our results also suggest that optimized education of nephrologists, transplantation surgeons and supportive staff might increase the KT rate. For example, training is needed to improve the communication skills of critical care professionals to discuss the possibility for kidney donation with relatives of potential deceased donors [33, 34].
Finally, a previous study showed that the gross domestic product of a country is correlated to the KT rate [35]. For countries with a lower gross domestic product, it may be more challenging to implement measures to increase the KT rate.
Strengths and limitations
A main strength of this study is that experts from almost all Eastern and Western European countries participated in this study on measures and barriers influencing total, deceased donor and living donor KT.
This study has some limitations. First, the surveyed measures and barriers were predetermined, therefore important measures and barriers may have been missed. However, no further major factors were stated in the free text boxes, allowing participants to point out missing elements. Second, experts may have had difficulty remembering the measures in force in 2010, possibly leading to recall bias as well as to some disagreement in responses between experts from the same country. Third, the effect of a measure or barrier was based on expert opinion and not on objective outcomes such as a measured change in KT rate. In addition, the experts’ personal attitude and beliefs towards KT may have influenced our results [30]. To limit this effect, in most countries surveys were completed by two or three experts. Finally, given the limited number of experts surveyed, it is possible that regional clinical practice has affected our results. However, we included experts from different regions in most countries and asked them to base their response on the national situation. Moreover, the grouping of countries based on KT rate may have diluted the effect of random variation between experts from the same country.
CONCLUSION
The results of our survey among kidney transplantation experts from almost all European countries suggest that, compared with low KT rate countries, middle and high KT rate countries had more measures in force to increase the KT rate, especially for deceased donor KT, and perceived fewer barriers. Once a measure was taken, experts’ opinion with regard to its success to increase the KT rate was similar across low, middle and high KT rate countries.
Experts’ opinions suggest that particularly in low KT rate countries, optimization of staff, equipment and facilities is needed to increase the KT rate. All countries may increase their KT rate by taking deceased and living donor–specific measures.
The results on the current status of measures to increase the KT rate reported in this article may help medical communities and policymakers in their decision process on how and where to focus strategies to (further) increase KT rates.
Supplementary Material
ACKNOWLEDGEMENTS
The authors wish to thank all the nephrologists and kidney transplantation surgeons who pretested the survey or filled out the Kidney Transplantation Rate Survey. This article was written on behalf of the ERA Registry, which is an official body of the European Renal Association.
APPENDIX: SURVEY COLLABORATORS
Albania (M. Barbullushi, A. Idrizi), Austria (B. Watschinger, H. Neuwirt, K. Eller), Belarus (O. Kalachik, S. Leschuk, O. Petkevich), Belgium (D. Abramowicz, R. Hellemans, K.M. Wissing, L. Colenbie), Bosnia-Herzegovina (S. Trnacevic, D. Rebic, H. Resic), Bulgaria (J. Filipov, P. Megerov), Croatia (M. Bušić, R. Žunec, D. Markić), Cyprus (A. Soloukides, I. Savva, E. Toumasi), Czech Republic (O. Viklicky, T. Reischig, K. Krejčí), Denmark (S.S. Sørensen, C. Bistrup, K. Skov), Estonia (K. Lilienthal, M. Ots-Rosenberg), Finland (I. Helanterä, A. Koivusalo), France (M. Hourmant, M. Essig, L. Frimat), Georgia (G. Tomadze), Germany (B. Banas), Greece (I. Boletis), Hungary (M. Sándor), Iceland (R. Pálsson), Ireland (W. Plant, P. Conlon, A. Cooney), Italy (L. Biancone, M. Cardillo), Latvia (I. Ziedina, J. Jusinskis), Lithuania (R. Vaiciuniene, E. Dalinkeviciene), Malta (L. Delicata, E. Farrugia), Montenegro (D. Radunović, V. Prelević, F. Tomović), The Netherlands (L. Hilbrands, F.J. Bemelman, B. Schaefer), Norway (A.V. Resisæter, B. Lien, M. Skauby), Poland (A. Dębska-Ślizień, M. Durlik, A. Wiecek), Portugal (S. Sampaio, C. Romãozinho, C. Jorge), Republic of North Macedonia (I. Rambabova-Bushljetikj, I.G. Nikolov, L. Trajceska), Romania (D. Tacu, A. Elec, A. Covic), Russia (E. Zakharova), Serbia (R. Naumovic, M. Lausevic), Slovakia (T. Baltesová, Z. Žilinská, I. Dedinská), Slovenia (J. Buturović Ponikvar, M. Arnol), Spain (M.O. Valentín, B. Domínguez-Gil, M. Crespo, A. Mazuecos), Sweden (C. Wallquist, T. Lundgren), Switzerland (M. Dickenmann), Turkey (H. Toz, T. Aki, K. Keven) and the UK (R. Ravanan, C. Geddes).
Contributor Information
Rianne Boenink, ERA Registry, Department of Medical Informatics, Amsterdam UMC location AMC, University of Amsterdam, Amsterdam, The Netherlands; Amsterdam Public Health, Quality of Care, Amsterdam, The Netherlands.
Anneke Kramer, ERA Registry, Department of Medical Informatics, Amsterdam UMC location AMC, University of Amsterdam, Amsterdam, The Netherlands; Amsterdam Public Health, Quality of Care, Amsterdam, The Netherlands.
Raymond C Vanholder, Nephrology Section, Department of Internal Medicine and Pediatrics, Ghent University Hospital, Ghent, Belgium; European Kidney Health Alliance, Brussels, Belgium.
Beatriz Mahillo, Organización Nacional de Trasplantes, Madrid, Spain.
Ziad A Massy, Paris-Saclay University, UVSQ, Inserm, CESP, Team 5, Clinical Epidemiology, Villejuif, France; Paris-Saclay University, AP-HP, Ambroise Paré Hospital, Nephrology Department, Boulogne-Billancourt, France.
Mirela Bušić, Ministry of Health, Zagreb, Croatia.
Alberto Ortiz, Fundación Jiménez Díaz, Universidad Autónoma de Madrid, Madrid, Spain.
Vianda S Stel, ERA Registry, Department of Medical Informatics, Amsterdam UMC location AMC, University of Amsterdam, Amsterdam, The Netherlands; Amsterdam Public Health, Quality of Care, Amsterdam, The Netherlands.
Kitty J Jager, ERA Registry, Department of Medical Informatics, Amsterdam UMC location AMC, University of Amsterdam, Amsterdam, The Netherlands; Amsterdam Public Health, Quality of Care, Amsterdam, The Netherlands.
Survey Collaborators:
M Barbullushi, A Idrizi, B Watschinger, H Neuwirt, K Eller, O Kalachik, S Leschuk, O Petkevich, D Abramowicz, R Hellemans, K M Wissing, L Colenbie, S Trnacevic, D Rebic, H Resic, J Filipov, P Megerov, M Bušić, R Žunec, D Markić, A Soloukides, I Savva, E Toumasi, O Viklicky, T Reischig, K Krejčí, S S Sørensen, C Bistrup, K Skov, K Lilienthal, M Ots-Rosenberg, I Helanterä, A Koivusalo, M Hourmant, M Essig, L Frimat, G Tomadze, B Banas, I Boletis, M Sándor, R Pálsson, W Plant, P Conlon, A Cooney, L Biancone, M Cardillo, I Ziedina, J Jusinskis, R Vaiciuniene, E Dalinkeviciene, L Delicata, E Farrugia, D Radunović, V Prelević, F Tomović, L Hilbrands, F J Bemelman, B Schaefer, A V Resisæter, B Lien, M Skauby, A Dębska-Ślizień, M Durlik, A Wiecek, S Sampaio, C Romãozinho, C Jorge, I Rambabova-Bushljetikj, I G Nikolov, L Trajceska, D Tacu, A Elec, A Covic, E Zakharova, R Naumovic, M Lausevic, T Baltesová, Z Žilinská, I Dedinská, J Buturović Ponikvar, M Arnol, M O Valentín, B Domínguez-Gil, M Crespo, A Mazuecos, C Wallquist, T Lundgren, M Dickenmann, H Toz, T Aki, K Keven, R Ravanan, and C Geddes
FUNDING
K.J.J. and V.S.S. report grants from the European Renal Association.
AUTHORS’ CONTRIBUTIONS
R.B., A.K., V.S. and K.J. designed the study and survey. R.V., B.M., Z.M., M.B. and A.O. tested and improved the content of the survey. R.B. performed the data collection, and R.B. and A.K. the analyses. R.B., A.K., V.S. and K.J. interpreted the results and drafted the manuscript. All authors reviewed and approved the manuscript before submission.
DATA AVAILABILITY STATEMENT
The data underlying this article are available in the article and in its online supplementary material.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Tonelli M, Wiebe N, Knoll Get al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 2011;11:2093–109. [DOI] [PubMed] [Google Scholar]
- 2. Rose C, Gill J, Gill JS. Association of kidney transplantation with survival in patients with long dialysis exposure. Clin J Am Soc Nephrol 2017;12:2024–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang Y, Hemmelder MH, Bos WJWet al. Mapping health-related quality of life after kidney transplantation by group comparisons: a systematic review. Nephrol Dial Transplant 2021;36:2327–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wallisch C, Strohmaier S, Kammer Met al. Survival benefit of kidney transplantation compared to long-term dialysis across ages: a retrospective cohort study using target trial emulation. Available at SSRN: https://ssrn.com/abstract=3991625 or 10.2139/ssrn.3991625. [DOI] [PMC free article] [PubMed]
- 5. Mohnen SM, van Oosten MJM, Los Jet al. Healthcare costs of patients on different renal replacement modalities - Analysis of Dutch health insurance claims data. PLoS One 2019;14:e0220800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kramer A, Boenink R, Stel VSet al. The ERA-EDTA Registry Annual Report 2018: a summary. Clin Kidney J 2021;14:107–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vanholder R, Stel VS, Jager KJet al. How to increase kidney transplant activity throughout Europe—an advocacy review by the European Kidney Health Alliance. Nephrol Dial Transplant 2019;34:1254–61. [DOI] [PubMed] [Google Scholar]
- 8. European Commission . Action plan on organ donation and transplantation (2009–2015): strengthened cooperation between member states. https://ec.europa.eu/health/ph_threats/human_substance/oc_organs/docs/organs_action_en.pdf (accessed 19 July 2021).
- 9. Van der Spiegel S, Schröder-Bäck P, Brand H. Organ transplantation and the European Union, 2009–2015 developments. Transpl Int 2020;33:603–11. [DOI] [PubMed] [Google Scholar]
- 10. Matesanz R, Domínguez-Gil B, Coll Eet al. How Spain reached 40 deceased organ donors per million population. Am J Transplant 2017;17:1447–54. [DOI] [PubMed] [Google Scholar]
- 11. de Klerk M, Keizer KM, Claas FHet al. The Dutch national living donor kidney exchange program. Am J Transplant 2005;5:2302–5. [DOI] [PubMed] [Google Scholar]
- 12. Johnson RJ, Allen JE, Fuggle SVet al. Early experience of paired living kidney donation in the United Kingdom. Transplantation 2008;86:1672–7. [DOI] [PubMed] [Google Scholar]
- 13. Lee LY, Pham TA, Melcher ML.. Living kidney donation: strategies to increase the donor pool. Surg Clin North Am 2019;99:37–47. [DOI] [PubMed] [Google Scholar]
- 14. Lomero M, Gardiner D, Coll Eet al. Donation after circulatory death today: an updated overview of the European landscape. Transpl Int 2020;33:76–88. [DOI] [PubMed] [Google Scholar]
- 15. Spiegel Online . Organ transplant scandal shocks Germany. http://www.spiegel.de/international/germany/organ-transplant-scandal-shocks-germany-a-848016.html (accessed on 20 August 2021).
- 16. Boenink R, Kramer A, Tuinhout REet al. Trends in kidney transplantation rate across Europe: study from the ERA Registry. Nephrol Dial Transplant 2022;doi: 10.1093/ndt/gfac333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. LimeSurvey . LimeSurvey: an open source survey tool. http://www.limesurvey.org. [Google Scholar]
- 18. World Health Organization Global Observatory on Donation and Transplant . Human Organ Donation and Transplantation Survey. http://www.transplant-observatory.org/questionnaire-pdf/. [Google Scholar]
- 19. Domínguez-Gil B, Haase-Kromwijk B, Van Leiden Het al. Current situation of donation after circulatory death in European countries. Transpl Int 2011;24:676–86. [DOI] [PubMed] [Google Scholar]
- 20. Lennerling A, Lovén C, Dor FJet al. Living organ donation practices in Europe – results from an online survey. Transpl Int 2013;26:145–53. [DOI] [PubMed] [Google Scholar]
- 21. ERA-EDTA Registry . ERA-EDTA Registry Annual Report 2018. Amsterdam: Amsterdam UMC, location AMC, Department of Medical Informatics, 2020. [Google Scholar]
- 22. World Health Organization Global Observatory on Donation and Transplant . Methodology. http://www.transplant-observatory.org/methodology/.
- 23. US Renal Data System . 2021 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2021:chap. 11. [Google Scholar]
- 24. ERA Registry . ERA Registry Annual Report 2019. Amsterdam: Amsterdam UMC, location AMC, Department of Medical Informatics, 2021. [Google Scholar]
- 25. European Kidney Health Alliance. Joint Statement. Thematic Network on Improving Organ Donation and Transplantation in the EU 2019. http://ekha.eu/wp-content/uploads/FINAL_Joint-Statement-of-the-Thematic-Network-on-Organ-Donation-and-Transplantation.pdf.
- 26. Vanholder R, Domínguez-Gil B, Busic Met al. Organ donation and transplantation: a multi-stakeholder call to action. Nat Rev Nephrol 2021;17:554–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. de Jong RW, Stel VS, Heaf JGet al. Non-medical barriers reported by nephrologists when providing renal replacement therapy or comprehensive conservative management to end-stage kidney disease patients: a systematic review. Nephrol Dial Transplant 2021;36:848–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Eurotransplant . Annual Report 2019. Leiden, the Netherlands: CIP-Gegevens Koninklijke Bibliotheek; 2020. [Google Scholar]
- 29. Claisse G, Gaillard F, Mariat C.. Living kidney donor evaluation. Transplantation 2020;104:2487–96. [DOI] [PubMed] [Google Scholar]
- 30. de Jong RW, Jager KJ, Vanholder RCet al. Results of the European EDITH nephrologist survey on factors influencing treatment modality choice for end-stage kidney disease. Nephrol Dial Transplant 2021;37:126–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. de Jong RW, Stel VS, Rahmel Aet al. Patient-reported factors influencing the choice of their kidney replacement treatment modality. Nephrol Dial Transplant 2022;37:477–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Working Group on Living Donation under the European Union . Toolbox Living Kidney Donation. Action plan on organ donation and transplantation (2009–2015): strengthened cooperation between member states. https://ec.europa.eu/health/sites/health/files/blood_tissues_organs/docs/eutoolbox_living_kidney_donation_en.pdf (accessed 2 June 2022).
- 33. Domínguez-Gil B, Murphy P, Procaccio F.. Ten changes that could improve organ donation in the intensive care unit. Intensive Care Med 2016;42:264–7. [DOI] [PubMed] [Google Scholar]
- 34. Miller C, Breakwell R.. What factors influence a family's decision to agree to organ donation? A critical literature review. London J Prim Care (Abingdon) 2018;10:103–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mudiayi D, Shojai S, Okpechi Iet al. Global estimates of capacity for kidney transplantation in world countries and regions. Transplantation 2022;106:1113–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.