ABSTRACT
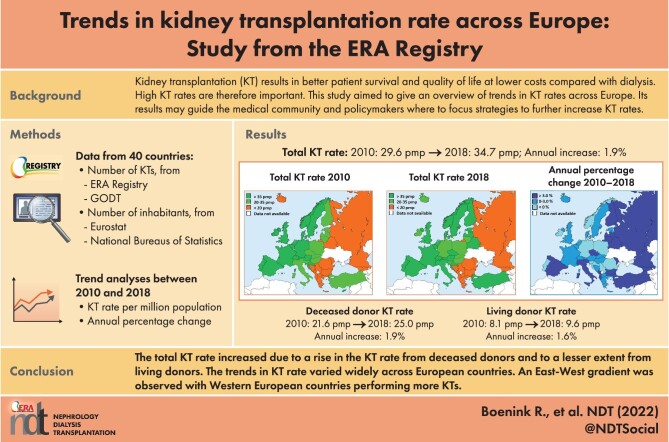
Background
The aim of this study was to identify trends in total, deceased donor (DD) and living donor (LD) kidney transplantation (KT) rates in European countries.
Methods
The European Renal Association (ERA) Registry and the Global Observatory on Donation and Transplantation (GODT) databases were used to obtain the number of KTs in individual European countries between 2010 and 2018. General population counts were obtained from Eurostat or the national bureaus of statistics. The KT rate per million population (p.m.p.) and the average annual percentage change (APC) were calculated.
Results
The total KT rate in the 40 participating countries increased with 1.9% annually [95% confidence interval (CI) 1.5, 2.2] from 29.6 p.m.p. in 2010 to 34.7 p.m.p. in 2018, reflecting an increase of 3.4 p.m.p. in the DD-KT rate (from 21.6 p.m.p. to 25.0 p.m.p.; APC 1.9%; 95% CI 1.3, 2.4) and of 1.5 p.m.p. in the LD-KT rate (from 8.1 p.m.p. to 9.6 p.m.p.; APC 1.6%; 95% CI 1.0, 2.3). The trends in KT rate varied widely across European countries. An East–West gradient was observed for DD-KT rate, with Western European countries performing more KTs. In addition, most countries performed fewer LD-KTs. In 2018, Spain had the highest DD-KT rate (64.6 p.m.p.) and Turkey the highest LD-KT rate (37.0 p.m.p.).
Conclusions
The total KT rate increased due to a rise in the KT rate from DDs and to a lesser extent from LDs, with large differences between individual European countries.
Keywords: Europe, kidney transplantation, trends
Graphical Abstract
Graphical Abstract.
KEY LEARNING POINTS.
What is already known about this subject?
Renal registries around the world have published data on kidney transplantation (KT) counts and rates, showing large international differences for both deceased (DD) and living donor (LD) transplants.
A recent international overview of time trends in KT rate for most European countries is lacking.
What this study adds?
The total KT rate in the 40 participating European countries increased with 1.9% annually from 29.6 per million population (p.m.p.) in 2010 to 34.7 p.m.p. in 2018, reflecting an increase of 3.4 p.m.p. in the DD-KT rate (from 21.6 p.m.p. to 25.0 p.m.p.; APC 1.9%) and of 1.5 p.m.p. in the LD-KT rate (from 8.1 p.m.p. to 9.6 p.m.p.; APC 1.6%).
The trends in KT rate varied widely across European countries, with most countries performing fewer LD-KTs than DD-KTs.
An East–West gradient was observed for the DD-KT rate with Western European countries performing more KTs.
What impact this may have on practice or policy?
These trends in KT rate in individual European countries combined with information on potentially successful measures as well as perceived barriers from previously published papers may guide the medical community and policymakers in determining where and how to target strategies to increase KT rate.
INTRODUCTION
Kidney transplant recipients have a longer life expectancy and a better quality of life than patients receiving dialysis [1, 2]. Unfortunately, not all patients with end-stage kidney disease (ESKD) who are suitable for transplantation receive a donor kidney. The large number of kidney transplantation (KT) candidates on the waiting list shows that the organ shortage is one of the major challenges in organ transplantation [3, 4].
Over the past decades, most countries have taken initiatives aiming to increase the number of KTs from deceased (DDs) and/or living donors (LDs). For example, earlier referral of potential DDs to the transplantation coordination team, taking measures to minimize inappropriate discard of DD organs [5], home-based education about living donation and a nationwide collaboration regarding paired exchange of LD kidneys [6]. On the other hand, countries may have faced barriers limiting the number of KTs, such as legislative issues, financial barriers, lack of donors, and patients’ or nephrologists’ attitudes or beliefs [7–9]. Such initiatives and barriers may have affected KT rates.
Renal registries around the world have published data on KT counts and rates [10–13], showing large international differences for both DD and LD transplants. However, a recent international overview of time trends in KT rate for most European countries is lacking.
Therefore, the aim of this study was to give a comprehensive overview of time trends in KT rate in European countries between 2010 and 2018, in total and separately for DD- and LD-KT. The results of this study are put into the perspective of the literature on initiatives to increase KT rates and the related barriers.
MATERIALS AND METHODS
Data sources
Patient data
The European Renal Association (ERA) Registry [14] and the Global Observatory on Donation and Transplantation (GODT) [15] databases were used to obtain the number of performed KTs in individual European countries between 2010 and 2018. The ERA Registry annually collects individual and aggregated data on patients with ESKD receiving kidney replacement therapy via the national and regional renal registries in Europe and countries bordering the Mediterranean Sea [14]. The GODT collects data on organ transplantation worldwide on an annual basis [15].
The choice of data source was based on the following criteria: (i) where possible one data source was used for a country and (ii) data from the ERA Registry database was preferred except where data for the complete study period from 2010 until 2018 were not available in the ERA Registry database or when the geographical coverage of the country was higher in the GODT database. When the number of KTs performed was missing for 1 or 2 years, the national or regional renal registry was asked to provide the missing data if possible. In case we were unable to use one data source (ERA Registry or GODT), we used both databases. For 19 countries data were obtained from the ERA Registry database, for 18 countries the GODT database was used, and for 3 countries both the ERA Registry and the GODT database were used (Supplementary data, Fig. S1).
General population data
For countries providing individual patient data to the ERA Registry and countries for which the data was obtained via the GODT database, the midyear general population counts were used from Eurostat [16]. For countries that had provided aggregated data to the ERA Registry, and for Austria, Bosnia and Herzegovina, and the UK, midyear general population counts from their national bureaus of statistics were used. For the Russian Federation we used the general population data in 2014 from the United Nations Population Fund [17].
Definition of variables
The KT rates were expressed per million population (p.m.p.) and were calculated by dividing the number of KTs in a year by the general population counts in the same year, multiplied by 1 million. The KT rate was calculated for all KTs performed in a country (total) and separately for DD and LD kidneys.
Statistical analyses
Time trends in KT rates were analyzed using Joinpoint regression [18]. The average annual percentage change (APC) with 95% confidence interval (95% CI) was computed using Poisson regression provided by the Joinpoint regression program [18]. Details of this method have been previously described [19]. Joinpoint identifies points in time (e.g. years) at which the trend of, in this case KT rates, changes statistically significantly [20, 21]. For the analyses the year of KT was added to the model as the independent variable and the KT rate (total, DD or LD) as the dependent variable.
Corresponding to the availability of nine data points (i.e. years in our study period) a maximum of one joinpoint (two trends) was used [20]. In addition, analyses were performed using zero joinpoints to obtain a single trend for the entire study period. The analyses were performed to obtain an overall trend for all participating countries together and for each country separately. If the number of KTs was zero in a country for a particular year, the transplantation rate was set on 0.1 p.m.p. to be able to calculate the APC. All analyses were performed using Joinpoint 4.2.0.2 (2015; National Cancer Institute, Calverton, MD, USA) [18].
RESULTS
Total kidney transplantation
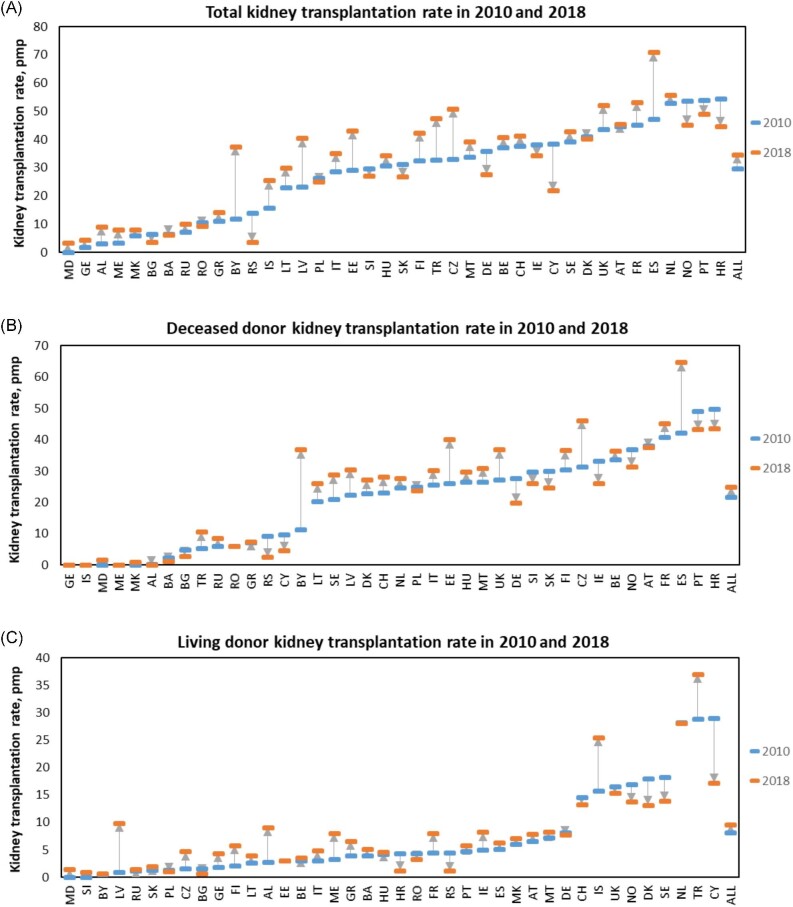
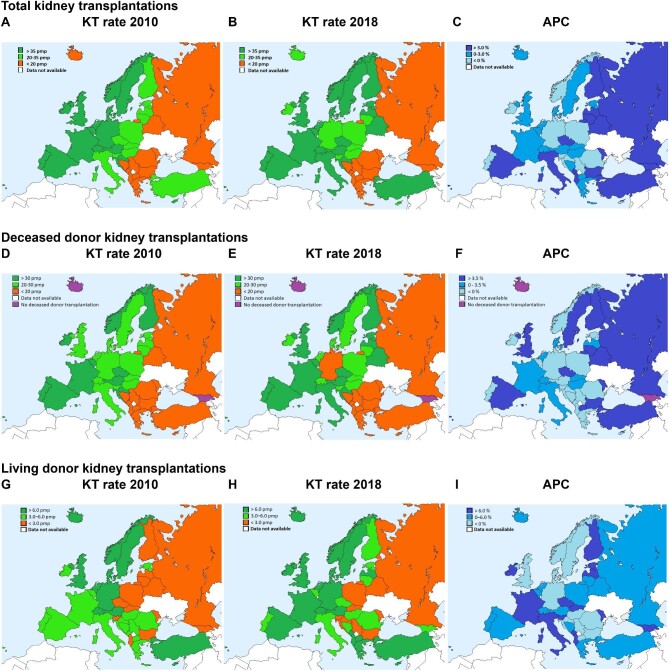
Table 1 shows the KT rate p.m.p. and APC for the period 2010 to 2018 for all 40 participating European countries combined and each country separately. The KT counts are presented in Supplementary data, Table S1. The combined KT rate increased from 29.6 p.m.p. in 2010 to 34.7 p.m.p. in 2018, corresponding to an average annual increase of 1.9% (APC 1.9; 95% CI 1.5, 2.2) (Table 1). Figures 1A, and 2A, B show the KT rate by country in 2010 and 2018. In addition, Fig. 1A presents the absolute change in KT rate, while Fig. 2C displays the relative change as APC with zero joinpoints (one trend) by country. The KT rate as well as the APC between 2010 and 2018 varied widely across Europe. Overall, the KT rate in 2010 was higher in Western European countries than in Eastern European countries (Fig. 2A). This disparity persisted in 2018 (Fig. 2B), although several Eastern European countries showed a higher APC for the KT rate than some Western European countries between 2010 and 2018 (Fig. 2C).
Table 1:
Time trends in total KT rate.
| Total KT rate by year, p.m.p. | Trend between 2010 and 2018 with zero joinpoints | Trend when allowing one joinpoint | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | APC (95% CI) | Period 1 | APC (95% CI) | Period 2 | APC (95% CI) | |||
| All | 29.6 | 30.9 | 30.8 | 31.0 | 31.6 | 32.2 | 33.3 | 33.9 | 34.7 | ↑ | 1.9 (1.5, 2.2) | ||||||
| Albania | 3.2 | 3.9 | 2.1 | 2.8 | 8.6 | 9.3 | 5.9 | 8.7 | 9.1 | ↑ | 17.9 (4.6, 33.0) | ||||||
| Austria | 44.7 | 44.6 | 47.3 | 45.9 | 46.8 | 43.8 | 46.7 | 45.4 | 45.5 | − | 0.1 (−0.7, 0.9) | ||||||
| Belarus | 12.0 | 18.2 | 21.2 | 33.0 | 30.8 | 35.1 | 40.4 | 38.1 | 37.5 | ↑ | 14.5 (7.7, 21.7) | 2010–2013 | ↑ | 37.2 (14.8, 63.9) | 2013–18 | − | 4.6 (−3.4, 13.3) |
| Belgium | 37.1 | 41.8 | 42.2 | 40.0 | 37.2 | 40.5 | 39.5 | 40.3 | 40.7 | − | 0.2 (−1.2, 1.7) | ||||||
| Bosnia and Herzegovina | 6.6 | 6.3 | 7.1 | 6.8 | 8.0 | 9.9 | 6.8 | 6.8 | 6.2 | − | 0.5 (−4.1, 5.4) | 2010–2015 | ↑ | 7.0 (1.9, 12.3) | 2015–18 | − | –11.3 (−20.4, −1.1) |
| Bulgaria | 6.5 | 2.3 | 1.8 | 3.9 | 7.8 | 6.7 | 5.2 | 5.7 | 3.6 | − | 5.1 (−10.3, 23.1) | ||||||
| Croatia | 54.5 | 53.7 | 54.3 | 60.1 | 48.4 | 46.7 | 48.5 | 51.2 | 44.7 | ↓ | –2.3 (−4.4, −0.2) | ||||||
| Cyprus | 38.6 | 36.4 | 33.6 | 36.0 | 36.4 | 23.6 | 22.3 | 22.1 | 21.8 | ↓ | –8.0 (−11.3, −4.6) | ||||||
| Czech Republic | 32.9 | 31.9 | 41.5 | 44.7 | 49.6 | 44.0 | 44.6 | 47.3 | 50.9 | ↑ | 5.2 (2.1, 8.4) | ||||||
| Denmark | 41.0 | 41.4 | 38.4 | 37.7 | 43.9 | 47.0 | 45.3 | 43.8 | 40.3 | − | 1.1 (−1.1, 3.4) | ||||||
| Estonia | 29.1 | 32.8 | 44.6 | 35.7 | 24.3 | 28.9 | 31.9 | 29.6 | 43.1 | − | 0.6 (−5.6, 7.3) | ||||||
| Finland | 32.4 | 32.7 | 35.8 | 34.4 | 43.9 | 44.7 | 47.5 | 43.2 | 42.4 | ↑ | 4.7 (1.9, 7.5) | ||||||
| France | 45.3 | 46.3 | 46.7 | 46.8 | 48.8 | 52.4 | 54.1 | 56.6 | 53.3 | ↑ | 2.8 (1.8, 3.8) | ||||||
| Georgia | 1.9 | 4.0 | 3.5 | 7.4 | 6.3 | 12.5 | 4.8 | 5.4 | 4.4 | − | 9.4 (−5.9, 27.2) | 2010–2015 | ↑ | 33.9 (7.1, 67.4) | 2015–18 | − | –27.0 (−55.7, 20.4) |
| Germany | 35.9 | 35.5 | 32.2 | 28.2 | 26.3 | 26.9 | 25.4 | 23.2 | 27.6 | ↓ | –4.6 (−7.0, −2.2) | ||||||
| Greece | 11.1 | 17.8 | 16.9 | 14.7 | 12.6 | 10.5 | 13.1 | 16.9 | 14.1 | − | –0.0 (−6.0, 6.3) | ||||||
| Hungary | 30.7 | 25.2 | 27.8 | 29.4 | 39.2 | 34.8 | 34.8 | 30.3 | 34.3 | − | 2.7 (−1.0, 6.6) | ||||||
| Iceland | 15.7 | 34.5 | 18.7 | 24.7 | 24.4 | 21.2 | 14.9 | 23.3 | 25.5 | − | 0.3 (−7.9, 9.2) | ||||||
| Ireland | 38.2 | 41.9 | 35.4 | 40.0 | 32.6 | 32.5 | 36.2 | 39.9 | 34.3 | − | –1.2 (−4.0, 1.6) | ||||||
| Italy | 28.6 | 29.5 | 30.0 | 28.5 | 30.3 | 31.0 | 34.2 | 37.1 | 35.2 | ↑ | 3.2 (1.7, 4.7) | ||||||
| Latvia | 23.3 | 36.1 | 32.0 | 36.2 | 30.8 | 40.7 | 34.0 | 31.0 | 40.4 | − | 3.4 (−1.4, 8.3) | ||||||
| Lithuania | 22.9 | 24.8 | 29.5 | 28.7 | 24.6 | 39.6 | 38.7 | 26.9 | 30.0 | − | 3.7 (−1.7, 9.4) | ||||||
| Malta | 33.8 | 43.2 | 21.4 | 30.5 | 46.0 | 18.0 | 43.9 | 44.9 | 39.2 | − | 2.7 (−7.9, 14.6) | ||||||
| Montenegro | 3.2 | 3.2 | 9.6 | 16.1 | 14.5 | 9.6 | 3.2 | 9.6 | 8.0 | − | 7.3 (−12.3, 31.2) | ||||||
| Norway | 53.8 | 61.0 | 59.6 | 53.0 | 53.3 | 49.0 | 45.8 | 52.1 | 45.2 | ↓ | –2.9 (−4.9, −0.9) | ||||||
| Poland | 26.3 | 28.2 | 30.1 | 30.5 | 30.2 | 27.6 | 29.2 | 28.7 | 24.9 | − | –0.5 (−2.7, 1.7) | 2010–2013 | ↑ | 5.4 (−4.6, 16.3) | 2013–18 | − | –3.4 (−7.6, 1.0) |
| Portugal | 53.9 | 50.2 | 40.6 | 42.7 | 43.0 | 46.7 | 49.5 | 47.8 | 49.0 | − | –0.1 (−3.0, 2.9) | 2010–2012 | ↓ | –13.1 (−24.1, −0.5) | 2012–18 | ↑ | 3.1 (0.8, 5.5) |
| Republic of Moldova | 0.0 | 0.3 | 1.1 | 1.7 | 2.9 | 2.4 | 5.4 | 4.6 | 3.3 | ↑ | 53.4 (24.6, 89.0) | 2010–2012 | ↑ | 179.4 (53.5, 408.5) | 2012–18 | − | 13.7 (−13.0, 48.6) |
| Republic of North Macedonia | 6.0 | 2.9 | 13.3 | 18.1 | 19.5 | 5.7 | 2.9 | 8.1 | 8.1 | − | 0.2 (−20.5, 26.2) | ||||||
| Romania | 10.5 | 10.9 | 8.8 | 14.7 | 15.6 | 12.4 | 13.5 | 7.6 | 9.4 | − | –1.4 (−8.8, 6.6) | ||||||
| Russian Federation | 7.3 | 6.8 | 6.6 | 6.5 | 7.2 | 6.5 | 7.5 | 8.2 | 10.0 | ↑ | 3.5 (0.1, 7.0) | 2010–2015 | − | –1.4 (−5.9, 3.3) | 2015–18 | ↑ | 14.0 (2.7, 26.6) |
| Serbia | 13.9 | 15.6 | 12.5 | 15.6 | 9.7 | 8.5 | 10.6 | 12.4 | 3.7 | ↓ | –10.8 (−19.5, −1.2) | ||||||
| Slovakia | 31.3 | 23.9 | 24.6 | 22.0 | 23.1 | 33.9 | 26.3 | 28.1 | 26.8 | − | 0.7 (−3.8, 5.5) | ||||||
| Slovenia | 29.8 | 22.4 | 30.1 | 29.1 | 26.7 | 31.0 | 22.3 | 23.2 | 27.0 | − | –1.4 (−5.4, 2.8) | ||||||
| Spain | 47.3 | 52.9 | 54.0 | 54.2 | 57.3 | 62.3 | 64.4 | 70.2 | 70.9 | ↑ | 5.1 (4.2, 5.9) | ||||||
| Sweden | 39.3 | 45.2 | 41.0 | 43.2 | 45.3 | 42.7 | 42.6 | 46.1 | 42.8 | − | 0.8 (−0.7, 2.3) | ||||||
| Switzerland | 37.6 | 35.6 | 31.4 | 34.4 | 36.8 | 38.9 | 36.4 | 42.6 | 41.3 | − | 2.3 (−0.1, 4.6) | 2010–2012 | − | –7.1 (−22.9, 12.1) | 2012–18 | ↑ | 4.5 (1.2, 7.8) |
| The Netherlands | 52.8 | 51.6 | 57.1 | 56.4 | 59.2 | 57.9 | 58.8 | 54.6 | 55.8 | − | 0.8 (−0.6, 2.2) | 2010–2014 | − | 3.3 (−1.0, 7.8) | 2014–18 | − | –1.6 (−5.7, 2.7) |
| Turkey | 32.8 | 39.6 | 38.6 | 38.7 | 38.0 | 41.0 | 43.2 | 41.6 | 47.6 | ↑ | 3.2 (1.5, 5.0) | ||||||
| UK | 43.6 | 43.7 | 44.5 | 48.3 | 46.6 | 46.5 | 48.3 | 50.5 | 52.3 | ↑ | 2.2 (1.4, 2.9) | ||||||
The total KT rate p.m.p. between 2010 and 2018 with the corresponding average APC for 40 European countries, combined and by country. Only for countries where the Joinpoint model detected a change in the trend of the KT rate the separate APCs are presented. Arrows indicate statistically significant trends.
Figure 1:
KT rate in 2010 and 2018 p.m.p. for the 40 European countries combined (ALL) and by country. Total KT rate (A), DD-KT rate (B) and LD-KT rate (C). Discrepancy may exist between the APC trends (increasing or decreasing transplantation rate) in Tables 1–3 and the trends (up or down arrow) in this figure since this figure only displays the difference in transplantation rate between the year 2010 and 2018 and not the average annual change over the entire study period. Country abbreviations are shown in Supplementary data, Fig. S1.
Figure 2:
KT rate p.m.p. in 2010 and 2018 and the average APC per donor type. (A) Total KT rate in 2010 p.m.p. (B) Total KT rate in 2018 p.m.p. (C) The APC between 2010 and 2018 with zero joinpoints (i.e. one trend for the entire study period) for the total KT rate. (D) DD-KT rate in 2010 p.m.p. (E) DD-KT rate in 2018 p.m.p. (F) The APC between 2010 and 2018 with zero joinpoints (i.e. one trend for the entire study period) for the DD-KT rate. (G) LD-KT rate in 2010 p.m.p. (H) LD-KT rate in 2018 p.m.p. (I) The APC between 2010 and 2018 with zero joinpoints (i.e. one trend for the entire study period) for the LD-KT rate.
In 16 countries the KT rate rose during (a part of) the study period (Table 1), with the largest increase in the Republic of Moldova (APC 2010–12 179.4%; 95% CI 53.5, 408.5), Belarus (APC 2010–13 37.2%; 95% CI 14.8, 63.9) and Georgia (APC 2010–15 33.9%; 95% CI 7.1, 67.4) (Table 1). Nevertheless, the Republic of Moldova and Georgia still had a relatively low KT rate at the end of the study, as the absolute increase was small (Table 1 and Fig. 1A). In six countries the KT rate decreased during (a part of) the study period, with the largest decrease in Portugal (APC 2010–12 −13.1%; 95% CI −24.1, −0.5), Serbia (APC 2010–18 −10.8%; 95% CI −19.5, −1.2) and Cyprus (APC 2010–18 −8.0%; 95% CI −11.3, −4.6). Although Norway and Croatia had a decreasing trend in the KT rate over time, in 2018 the KT rate was still relatively high (Table 1 and Fig. 1A). Spain already had one of the highest KT rates in Europe in 2010, and due to a relatively high increase in the KT rate (APC 2010–18 5.1%; 95% CI 4.2, 5.9), it had the highest KT rate in 2018 (70.9 p.m.p.).
Deceased donor kidney transplantation
Across the entire study period around 72% of the KTs were performed using DD grafts for all countries together. The DD-KT rate was stable at around 22.0 p.m.p. between 2010 and 2013 (APC 0.3%; 95% CI −1.3, 2.0), but increased thereafter by an average of 2.7% per year to 25.0 p.m.p. in 2018 (APC 2.7%; 95% CI 1.9, 3.4; Table 2 and Supplementary data, Table S2). The DD-KT rate and the APC varied widely across Europe (Table 2, and Figs 1B and 2D–F). Georgia and Iceland did not perform any DD-KTs during the study period. In 2010, an East–West gradient existed for the DD-KT rate, with Western European countries performing more DD transplantations (Fig. 2D). This inequality remained in 2018 (Fig. 2E), even though some Eastern European countries had a higher APC between 2010 and 2018 (Fig. 2F).
Table 2:
Time trends in DD-KT rate.
| DD-KT rate by year, p.m.p. | Trend between 2010 and 2018 with zero joinpoints | Trend when allowing one joinpoint | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | APC (95% CI) | Period 1 | APC (95% CI) | Period 2 | APC (95% CI) | |||
| All | 21.6 | 22.0 | 22.0 | 22.0 | 22.5 | 23.0 | 24.0 | 24.6 | 25.0 | ↑ | 1.9 (1.3, 2.4) | 2010–2013 | − | 0.3 (−1.3, 2.0) | 2013–18 | ↑ | 2.7 (1.9, 3.4) |
| Albania | 0.4 | 0.0 | 0.4 | 0.0 | 1.0 | 2.1 | 0.7 | 0.0 | 0.0 | − | –1.1 (−32.4, 44.6) | ||||||
| Austria | 38.1 | 39.2 | 39.9 | 38.2 | 39.6 | 36.9 | 39.5 | 38.4 | 37.5 | − | –0.3 (−1.1, 0.5) | ||||||
| Belarus | 11.5 | 17.6 | 18.3 | 30.4 | 28.3 | 32.7 | 38.5 | 37.2 | 36.8 | ↑ | 15.2 (8.9, 21.8) | 2010–2013 | ↑ | 34.4 (8.7, 66.1) | 2013–18 | − | 6.6 (−3.0, 17.2) |
| Belgium | 33.8 | 38.3 | 39.3 | 36.0 | 33.7 | 36.6 | 35.6 | 35.6 | 36.4 | − | –0.2 (−1.8, 1.5) | ||||||
| Bosnia and Herzegovina | 2.3 | 1.7 | 3.4 | 1.4 | 2.0 | 2.8 | 3.1 | 1.1 | 1.1 | − | –5.7 (−16.9, 6.9) | ||||||
| Bulgaria | 4.9 | 1.1 | 0.5 | 2.3 | 6.1 | 5.3 | 3.6 | 4.5 | 2.8 | − | 11.9 (−12.3, 42.6) | ||||||
| Croatia | 49.8 | 43.6 | 50.4 | 57.2 | 46.4 | 45.2 | 46.6 | 49.8 | 43.5 | − | –0.9 (−3.5, 1.8) | ||||||
| Cyprus | 9.6 | 14.1 | 5.8 | 10.4 | 10.6 | 1.2 | 4.7 | 11.6 | 4.6 | − | –9.7 (−28.5, 13.9) | ||||||
| Czech Republic | 31.3 | 28.1 | 34.7 | 36.6 | 43.4 | 38.9 | 40.1 | 42.1 | 46.2 | ↑ | 5.3 (2.8, 7.9) | ||||||
| Denmark | 22.8 | 23.1 | 24.8 | 19.0 | 24.6 | 26.8 | 26.8 | 28.3 | 27.2 | ↑ | 3.1 (0.1, 6.1) | ||||||
| Estonia | 26.1 | 30.6 | 43.8 | 34.9 | 23.6 | 26.6 | 28.9 | 20.5 | 40.1 | − | –1.0 (−8.6, 7.3) | ||||||
| Finland | 30.4 | 30.3 | 33.6 | 32.2 | 41.2 | 41.8 | 43.5 | 37.4 | 36.6 | ↑ | 3.7 (0.4, 7.0) | 2010–2016 | ↑ | 6.8 (2.0, 11.9) | 2016–18 | − | –9.3 (−31.1, 19.3) |
| France | 40.8 | 41.6 | 41.1 | 40.7 | 41.0 | 44.1 | 45.5 | 47.4 | 45.2 | ↑ | 1.8 (0.8, 2.8) | ||||||
| Georgia | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | NA | |||||||
| Germany | 27.8 | 25.6 | 22.6 | 19.2 | 18.6 | 19.0 | 18.2 | 16.5 | 19.9 | ↓ | –5.0 (−8.0, −2.0) | 2010–2014 | ↓ | –10.3 (−18.0, −1.8) | 2014–18 | − | 0.6 (−8.1, 10.0) |
| Greece | 7.2 | 13.2 | 12.6 | 10.1 | 8.4 | 7.0 | 8.2 | 10.7 | 7.5 | − | –2.8 (−9.8, 4.7) | ||||||
| Hungary | 26.5 | 20.5 | 22.5 | 25.4 | 34.6 | 30.8 | 31.4 | 26.3 | 29.7 | − | 3.5 (−1.1, 8.3) | ||||||
| Iceland | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | NA | |||||||
| Ireland | 33.1 | 36.0 | 28.5 | 31.8 | 24.0 | 25.5 | 25.7 | 29.3 | 26.1 | ↓ | –3.3 (−6.4, −0.0) | ||||||
| Italy | 25.5 | 25.9 | 26.8 | 24.9 | 26.1 | 26.0 | 29.6 | 31.9 | 30.3 | ↑ | 2.6 (0.9, 4.4) | ||||||
| Latvia | 22.4 | 34.4 | 29.1 | 33.1 | 27.1 | 33.7 | 28.2 | 23.3 | 30.5 | − | 0.0 (−4.9, 5.2) | ||||||
| Lithuania | 20.3 | 23.8 | 25.4 | 26.4 | 20.1 | 36.5 | 36.6 | 24.7 | 26.1 | − | 3.7 (−2.6, 10.3) | ||||||
| Malta | 26.5 | 28.8 | 19.0 | 23.5 | 34.5 | 18.0 | 32.9 | 34.2 | 31.0 | − | 3.3 (−4.1, 11.3) | ||||||
| Montenegro | 0.0 | 3.2 | 1.6 | 1.6 | 1.6 | 0.0 | 0.0 | 0.0 | 0.0 | − | –26.8 (−52.4, 12.4) | ||||||
| Norway | 36.8 | 46.2 | 43.4 | 39.8 | 40.1 | 36.8 | 36.9 | 37.3 | 31.4 | ↓ | –2.8 (−5.3, −0.2) | ||||||
| Poland | 24.9 | 27.2 | 28.7 | 29.0 | 28.8 | 26.0 | 27.9 | 27.3 | 23.9 | − | –0.6 (−2.7, 1.6) | 2010–2012 | − | 8.7 (−11.2, 33.1) | 2012–18 | − | –2.5 (−5.8, 0.8) |
| Portugal | 49.1 | 45.7 | 36.2 | 37.9 | 37.8 | 40.8 | 43.3 | 40.3 | 43.3 | − | –0.8 (−3.8, 2.4) | 2010–2012 | ↓ | –14.4 (−26.4, −0.4) | 2012–18 | ↑ | 2.6 (0.0, 5.2) |
| Republic of Moldova | 0.0 | 0.0 | 0.0 | 0.0 | 2.3 | 1.5 | 3.4 | 4.1 | 1.8 | ↑ | 71.5 (29.7 126.8) | ||||||
| Republic of North Macedonia | 0.0 | 0.0 | 0.0 | 0.0 | 5.7 | 1.4 | 0.0 | 0.0 | 1.0 | − | 21.5 (−24.9, 96.3) | ||||||
| Romania | 6.1 | 7.1 | 6.2 | 12.0 | 13.7 | 10.0 | 11.4 | 5.0 | 6.1 | − | –0.1 (−11.3, 12.6) | 2010–2014 | − | 24.4 (−12.6, 76.8) | 2014–18 | − | –19.7 (−43.5, 14.2) |
| Russian Federation | 6.1 | 5.6 | 5.3 | 5.2 | 5.9 | 5.2 | 5.9 | 6.8 | 8.5 | − | 3.7 (−0.4, 8.0) | 2010–2015 | − | –2.2 (−7.8, 3.7) | 2015–18 | ↑ | 16.7 (2.3, 33.1) |
| Serbia | 9.33 | 9.51 | 7.08 | 11.17 | 5.75 | 3.66 | 6.18 | 8.81 | 2.56 | − | –10.7 (−20.9, 0.9) | ||||||
| Slovakia | 30.0 | 21.5 | 24.0 | 20.1 | 20.3 | 30.4 | 22.8 | 26.1 | 24.8 | − | 0.2 (−4.7, 5.3) | ||||||
| Slovenia | 29.8 | 22.4 | 30.1 | 29.1 | 26.7 | 31.0 | 21.3 | 22.3 | 26.0 | − | –2.0 (−6.2, 2.5) | ||||||
| Spain | 42.2 | 46.3 | 46.3 | 46.0 | 48.2 | 54.0 | 57.0 | 63.1 | 64.6 | ↑ | 5.5 (4.1, 6.9) | ||||||
| Sweden | 21.1 | 25.7 | 24.8 | 27.5 | 29.6 | 29.3 | 29.1 | 33.7 | 28.8 | ↑ | 4.1 (1.7, 6.6) | ||||||
| Switzerland | 23.0 | 22.9 | 19.4 | 20.9 | 22.1 | 26.8 | 22.1 | 27.4 | 28.1 | − | 3.1 (−0.1, 6.5) | ||||||
| The Netherlands | 24.6 | 24.9 | 28.1 | 25.5 | 27.5 | 27.4 | 25.4 | 24.0 | 27.7 | − | 0.4 (−1.5, 2.3) | ||||||
| Turkey | 5.4 | 7.0 | 7.0 | 7.7 | 8.2 | 8.6 | 9.9 | 8.6 | 10.6 | ↑ | 7.1 (4.5, 9.7) | ||||||
| UK | 27.2 | 27.3 | 29.4 | 32.3 | 31.2 | 31.5 | 33.9 | 35.9 | 36.9 | ↑ | 3.9 (2.9, 4.9) | ||||||
The DD-KT rate p.m.p. between 2010 and 2018 with the corresponding average APC for 40 European countries, combined and by country. Only for countries where the Joinpoint model detected a change in the trend of the KT rate the separate APCs are presented. Arrows indicate statistically significant trends. NA, not applicable.
In 13 countries the DD-KT rate rose during (a part of) the study period, with the largest increase in the Republic of Moldova (APC 2010–18 71.5%; 95% CI 29.7, 126.8), Belarus (APC 2010–13 34.4%; 95% CI 8.7, 66.1) and the Russian Federation (APC 2015–18 16.7%; 95% CI 2.3, 33.1) (Table 2). In 4 countries the DD-KT rate decreased during (a part of) the study period, with the largest decrease in Portugal (APC 2010–12 −14.4%; 95% CI −26.4, −0.4) and Germany (APC 2010–14 −10.3%; 95% CI −18.0, −1.8). Interestingly, Portugal experienced an increase from 2012 onwards (APC 2.6%; 95% CI 0.0, 5.2). Although Spain already had a high DD-KT rate in 2010 (42.2 p.m.p.), the DD-KT rate continued to increase throughout the study period (APC 5.5%; 95% CI 4.1, 6.9), resulting in Spain being the leading European country for the DD-KT rate (64.6 p.m.p.) in 2018 (Fig. 1B).
Living donor kidney transplantation
Overall, the LD-KT rate increased by an average of 1.6% per year (APC 1.6; 95% CI 1.0, 2.3), from 8.1 p.m.p. in 2010 to 9.6 p.m.p. in 2018 (Table 3 and Supplementary data, Table S3). Substantial differences were observed in the country-specific results for the LD-KT rate as well as the APC (Table 3, and Figs 1C and 2G–I). Other than for DD-KT, there was no clear East–West gradient for the LD-KT rate in either 2010 or 2018 (Fig. 2G and H).
Table 3:
Time trends in LD-KT rate.
| LD-KT rate by year, p.m.p. | Trend between 2010 and 2018 with zero joinpoints | Trend when allowing one joinpoint | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | APC (95% CI) | Period 1 | APC (95% CI) | Period 2 | APC (95% CI) | |||
| All | 8.1 | 8.8 | 8.8 | 9.0 | 9.0 | 9.2 | 9.2 | 9.3 | 9.6 | ↑ | 1.6 (1.0, 2.3) | ||||||
| Albania | 2.8 | 3.9 | 1.8 | 2.8 | 7.6 | 7.3 | 5.2 | 8.7 | 9.1 | ↑ | 18.6 (5.5, 33.3) | ||||||
| Austria | 6.6 | 5.5 | 7.3 | 7.7 | 7.2 | 6.9 | 7.1 | 7.0 | 7.9 | − | 2.2 (−0.8, 5.3) | ||||||
| Belarus | 0.5 | 0.6 | 2.8 | 2.6 | 2.5 | 2.3 | 1.9 | 0.9 | 0.6 | − | 1.8 (−18.9, 27.9) | 2010–2013 | ↑ | 97.0 (4.1, 272.8) | 2013–18 | ↓ | –26.8 (−45.0, −2.6) |
| Belgium | 3.0 | 3.3 | 2.9 | 3.3 | 3.6 | 3.9 | 4.0 | 4.4 | 3.5 | ↑ | 3.8 (1.0, 6.8) | ||||||
| Bosnia and Herzegovina | 4.0 | 4.6 | 3.4 | 5.4 | 6.0 | 7.1 | 3.7 | 5.7 | 5.1 | − | 3.5 (−3.8, 11.3) | ||||||
| Bulgaria | 1.6 | 1.2 | 1.2 | 1.5 | 1.7 | 1.4 | 1.5 | 1.1 | 0.7 | − | –5.1 (−11.7, 1.9) | 2010–2016 | − | 1.8 (−7.7, 12.3) | 2016–18 | − | –30.8 (−61.3, 23.8) |
| Croatia | 4.3 | 7.5 | 1.9 | 1.5 | 2.0 | 1.5 | 1.9 | 1.3 | 1.2 | ↓ | –15.6 (−25.5, −4.3) | ||||||
| Cyprus | 28.9 | 22.3 | 27.8 | 25.5 | 25.8 | 22.4 | 17.6 | 10.5 | 17.2 | ↓ | –8.6 (−14.5, −2.2) | ||||||
| Czech Republic | 1.6 | 3.8 | 6.8 | 8.1 | 6.2 | 5.1 | 4.5 | 5.1 | 4.7 | − | 6.7 (−7.2, 22.6) | 2010–2012 | ↑ | 110.2 (24.2, 255.8) | 2012–18 | − | –8.4 (−16.2, 0.1) |
| Denmark | 18.0 | 15.8 | 13.6 | 18.7 | 19.3 | 20.2 | 18.5 | 15.5 | 13.2 | − | –1.1 (−5.9, 4.0) | ||||||
| Estonia | 3.0 | 2.2 | 0.8 | 0.8 | 0.8 | 2.3 | 3.0 | 9.1 | 3.0 | − | 14.5 (−10.5, 46.4) | 2010–2013 | − | –38.6 (−81.7, 106.3) | 2013–18 | − | 56.3 (−9.1, 168.8) |
| Finland | 2.1 | 2.4 | 1.8 | 2.2 | 2.7 | 2.7 | 4.0 | 5.1 | 5.8 | ↑ | 14.6 (8.5, 20.9) | 2010–2013 | − | –0.7 (−21.9, 26.2) | 2013–18 | ↑ | 23.1 (10.5, 37.0) |
| France | 4.5 | 4.7 | 5.5 | 6.1 | 7.8 | 8.2 | 8.6 | 9.1 | 8.1 | ↑ | 9.7 (6.2, 13.4) | 2010–2016 | ↑ | 13.4 (9.6, 17.2) | 2016–18 | − | –5.0 (−22.0, 15.7) |
| Georgia | 1.9 | 4.0 | 3.5 | 7.4 | 6.3 | 12.5 | 4.8 | 5.4 | 4.4 | − | 9.4 (−5.9, 27.2) | 2010–2015 | ↑ | 33.9 (7.1, 67.4) | 2015–18 | − | –27.0 (−55.7, 20.4) |
| Germany | 8.1 | 9.9 | 9.5 | 9.0 | 7.7 | 7.9 | 7.2 | 6.7 | 7.7 | ↓ | –3.4 (−6.0, −0.6) | ||||||
| Greece | 3.9 | 4.6 | 4.2 | 4.6 | 4.1 | 3.5 | 4.9 | 6.2 | 6.6 | ↑ | 5.3 (0.1, 10.7) | 2010–2015 | − | –1.6 (−8.1, 5.3) | 2015–18 | ↑ | 20.5 (3.5, 40.2) |
| Hungary | 4.2 | 4.7 | 5.3 | 4.0 | 4.7 | 4.1 | 3.5 | 4.1 | 4.6 | − | –1.5 (−5.2, 2.3) | ||||||
| Iceland | 15.7 | 34.5 | 18.7 | 24.7 | 24.4 | 21.2 | 14.9 | 23.3 | 25.5 | − | 0.3 (−7.9, 9.2) | ||||||
| Ireland | 5.0 | 5.9 | 7.0 | 8.2 | 8.6 | 7.0 | 10.5 | 10.6 | 8.2 | ↑ | 7.6 (2.6, 12.8) | ||||||
| Italy | 3.1 | 3.6 | 3.2 | 3.6 | 4.1 | 5.0 | 4.6 | 5.2 | 4.8 | ↑ | 6.9 (4.3, 9.5) | ||||||
| Latvia | 0.9 | 1.7 | 2.9 | 3.1 | 3.8 | 7.0 | 5.8 | 7.8 | 9.9 | ↑ | 31.2 (22.4, 40.7) | ||||||
| Lithuania | 2.6 | 1.0 | 4.0 | 2.4 | 4.4 | 3.1 | 2.1 | 2.1 | 3.9 | − | 5.0 (−9.1, 21.3) | ||||||
| Malta | 7.2 | 14.4 | 2.4 | 7.0 | 11.5 | 0.0 | 11.0 | 10.7 | 8.3 | − | –2.6 (−41.3, 61.8) | ||||||
| Montenegro | 3.2 | 0.0 | 8.0 | 14.5 | 12.9 | 9.6 | 3.2 | 9.6 | 8.0 | − | 28.6 (−18.0, 101.7) | ||||||
| Norway | 17.0 | 14.7 | 16.1 | 13.2 | 13.2 | 12.1 | 9.0 | 14.8 | 13.7 | − | –3.4 (−8.4, 1.8) | ||||||
| Poland | 1.3 | 1.1 | 1.3 | 1.5 | 1.4 | 1.6 | 1.3 | 1.5 | 1.1 | − | 0.2 (−4.5, 5.2) | ||||||
| Portugal | 4.8 | 4.4 | 4.4 | 4.9 | 5.2 | 6.0 | 6.3 | 7.5 | 5.7 | ↑ | 5.4 (2.1, 8.8) | ||||||
| Republic of Moldova | 0.0 | 0.3 | 1.1 | 1.7 | 0.6 | 1.0 | 2.0 | 0.5 | 1.5 | − | 24.0 (−3.5, 59.4) | 2010–2012 | − | 239.0 (−73.9, 4299.6) | 2012–18 | − | –1.0 (−35.8, 52.6) |
| Republic of North Macedonia | 6.0 | 2.9 | 13.3 | 18.1 | 13.8 | 4.3 | 2.9 | 8.1 | 7.1 | − | –1.2 (−20.7, 23.2) | ||||||
| Romania | 4.3 | 3.7 | 2.6 | 2.7 | 1.9 | 2.3 | 2.1 | 2.6 | 3.3 | − | –4.6 (−11.8, 3.2) | 2010–2014 | ↓ | –18.7 (−30.0, −5.6) | 2014–18 | − | 12.0 (−3.5, 30.1) |
| Russian Federation | 1.2 | 1.3 | 1.4 | 1.3 | 1.3 | 1.3 | 1.6 | 1.4 | 1.5 | ↑ | 2.7 (0.8, 4.5) | ||||||
| Serbia | 4.5 | 6.1 | 5.4 | 4.5 | 3.9 | 4.7 | 4.4 | 3.6 | 1.1 | ↓ | –11.7 (−21.2, −1.1) | 2010–2016 | − | –1.4 (−10.9, 9.0) | 2016–18 | ↓ | –46.0 (−70.2, −2.0) |
| Slovakia | 1.3 | 2.4 | 0.6 | 1.8 | 2.8 | 3.5 | 3.5 | 2.0 | 2.0 | − | 9.7 (−7.2, 29.7) | ||||||
| Slovenia | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 1.0 | 1.0 | 1.0 | ↑ | 40.5 (13.8, 73.6) | ||||||
| Spain | 5.1 | 6.6 | 7.6 | 8.1 | 9.0 | 8.3 | 7.4 | 7.1 | 6.3 | − | 1.7 (−3.7, 7.3) | 2010–2014 | ↑ | 14.0 (6.5, 22.0) | 2014–18 | ↓ | –9.3 (−15.3, −2.9) |
| Sweden | 18.2 | 19.5 | 16.2 | 15.7 | 15.7 | 13.4 | 13.5 | 12.4 | 14.0 | ↓ | –4.8 (−6.8, −2.7) | ||||||
| Switzerland | 14.6 | 12.8 | 12.0 | 13.5 | 14.7 | 12.1 | 14.3 | 15.1 | 13.3 | − | 0.6 (−2.1, 3.4) | ||||||
| The Netherlands | 28.2 | 26.7 | 28.9 | 30.6 | 31.2 | 30.4 | 33.5 | 30.6 | 28.1 | − | 1.1 (−0.8, 3.1) | 2010–2016 | ↑ | 3.1 (0.5, 5.8) | 2016–18 | − | –7.2 (−20.3, 8.0) |
| Turkey | 28.8 | 32.6 | 31.7 | 31.0 | 29.8 | 32.4 | 33.3 | 33.0 | 37.0 | ↑ | 2.0 (0.4, 3.6) | ||||||
| UK | 16.5 | 16.3 | 15.1 | 15.8 | 15.0 | 14.1 | 13.9 | 13.9 | 15.3 | ↓ | –1.8 (−3.2, −0.3) | 2010–2016 | ↓ | –3.1 (−4.9, −1.2) | 2016–18 | − | 4.4 (−6.9, 17.0) |
The LD-KT rate p.m.p. between 2010 and 2018 with the corresponding average APC for 40 European countries, combined and by country. Only for countries where the Joinpoint model detected a change in the trend of the KT rate the separate APCs are presented. Arrows indicate statistically significant trends.
Across the entire study period most countries performed fewer LD-KTs than DD-KTs except for Albania, Bosnia and Herzegovina, Cyprus, Georgia, Iceland, Montenegro, Republic of North Macedonia, the Netherlands and Turkey (Tables 2 and 3). In 17 countries the LD-KT rate rose during (a part of) the study period, with the largest increase in the Czech Republic (APC 2010–12 110.2%; 95% CI 24.2, 255.8), Belarus (APC 2010–13 97.0%; 95% CI 4.1, 272.8) and Slovenia (APC 2010–18 40.5%; 95% CI 13.8, 73.6) (Table 3). However, these countries with the highest APC still had a relatively low LD-KT rate in 2018 (Table 3 and Fig. 1C). On the other hand, in 9 countries the LD-KT rate decreased during (a part of) the study period, with the largest decrease in Serbia (APC 2016–18 −46.0%; 95% CI −70.2, −2.0), Belarus (APC 2013–18 −26.8%; 95% CI −45.0, −2.6) and Romania (APC 2010–14 −18.7%; 95% CI −30.0, −5.6). Interestingly, Belarus and Spain had an increasing trend for the LD-KT rate at the beginning of the study period and a decreasing trend thereafter. Turkey already had one of the highest LD-KT rates (28.8 p.m.p.) in 2010 and a further increase in the rate (APC 2.0%; 95% CI 0.4, 3.6) placed the country in the lead in Europe with respect to LD-KT rate in 2018 (37.0 p.m.p.).
DISCUSSION
This study identified time trends in KT rate in 40 European countries. The total KT rate increased by an average of 1.9% per year from 29.6 p.m.p. in 2010 to 34.7 p.m.p. in 2018, reflecting an increase of 3.4 p.m.p. in the DD-KT rate (from 21.6 p.m.p. to 25.0 p.m.p.; APC 1.9%) and of 1.5 p.m.p. in the LD-KT rate (from 8.1 p.m.p. to 9.6 p.m.p.; APC 1.6%).
The country-specific results showed that the KT rate and accompanying APC varied widely across Europe. An East–West gradient was observed for DD-KT rate with Western European countries performing more KTs. At the end of the study period, Spain had the highest KT rate for kidneys from DDs and Turkey the highest rate for kidneys from LDs.
Worldwide perspective
In line with our results, large international differences have been observed for the trends in KT rate worldwide [11, 12]. The US Renal Data System examined the average annual change in KT by country or region between 2009 and 2018, including some European countries. The largest average annual increase in KT was observed in Israel (2.9 p.m.p.), Kuwait (2.4 p.m.p.) and Jalisco, Mexico (2.2 p.m.p.) [11]. On the other hand, the KT rate decreased in this period in Greece, Malaysia, Hong Kong, Portugal, Norway and Iceland. In 2018, the KT rate was highest in the Aguascalientes state of Mexico, at 128 p.m.p., followed by Kazakhstan (82 p.m.p.) and the USA (68 p.m.p.). Aguascalientes is a chronic kidney disease hotspot with a high incidence of kidney replacement therapy between ages 20 and 40 years [22].
Substantial differences existed in the proportion of DD- versus LD-KTs between countries. The increasing trend in total KT rate in the USA was mainly explained by an increase in DD-KT rate [23], while in Japan this was mainly caused by a rise in LD-KT rate [24]. In 2018, all kidney transplants originated from LDs in Albania, Bangladesh and Iceland, whereas in Italy, Uruguay and the Czech Republic, more than 90% of donors were deceased [11]. Moreover, in Greece, Taiwan and Singapore among other countries, a similar proportion of both donor types was used [11].
European perspective
Total kidney transplantation
In many Eastern European countries the total KT rate was substantially lower than in Western European countries, although the prevalence of chronic kidney disease may be higher in Eastern European countries [25]. We have performed a Kidney Transplantation Rate Survey among transplantation experts in European countries to investigate which factors may explain the observed trends in KT rate [26]. Countries were divided in low, middle and high KT rate countries (corresponding to, respectively, orange, light green and dark green countries in Fig. 2A). This study showed that for 2010 experts of more than 60% of the middle and high KT rate countries indicated to have already sufficient staff, equipment and facilities available to perform KTs, whereas these percentages were lower for low KT rate countries. As a result, in Eastern European countries in particular there might be room for improvement with respect to optimizing staff, equipment and facilities [25, 26]. In addition, experts from countries with lower KT rates reported to perceive more barriers, especially lack of knowledge about KT for recipients and their relatives, and distrust in the healthcare system. To overcome these barriers and increase KT, more and better information provision to the general population and ESKD patients in particular about KT is warranted [26, 27].
Deceased donor kidney transplantation
The results of this study show that in general Western European countries performed more DD-KTs than Eastern European countries. Transplantation experts in more than 80% of countries with middle and high KT rate reported that several measures to increase the DD-KT rate were successful, such as the use of expanded criteria donors, standard protocols for screening of potential DDs and the presence of transplantation coordinators [26]. In low KT rate countries these measures were reported to be taken less often. Once a measure was taken, no differences across the low, middle and high KT rate countries were observed for the success of the measure to increase KT rate [26].
In some of the countries with the highest KT rates the government has been actively involved in strategies to increase the KT rate. For example, Croatia had the highest DD-KT rate about a decade ago after implementing the Croatian model of organ donation and transplantation which included the appointment of hospital and national transplantation coordinators, donor hospital reimbursement, a public awareness campaign, international cooperation, adoption of new legislation and implementation of a donor quality assurance program [28]. In addition, the Ministry of Health of Belarus implemented measures regarding legislation, transplantation programs and training of professionals between 2008 and 2013 [29], leading to a large increase in their DD-KT rate. During the current study, Spain became the leading European country for DD-KT rate which is likely the result of efforts to promote earlier referral of potential donors to the intensive care unit, using expanded criteria and non-standard risk donors and stimulating donation after circulatory death [5]. Germany was among the countries with the largest decline in DD-KT rate. Around 2012 Germany faced a transplantation scandal which may have led to the decreasing trend due to distrust in the healthcare system [30].
Living donor kidney transplantation
In the majority of countries fewer KTs were performed with LDs than with DDs. Although LD-KT is associated with better graft and recipient survival compared with DD-KT [13], some nephrologists might be reluctant towards KT with LDs since the long-term effects of kidney donation, especially at a young age, still remains uncertain [31].
Turkey and the Netherlands had the highest LD-KT rate during the study period. Between 2008 and 2010 there have been some major changes in the Turkish transplant regulations, for example the Turkish Ministry of Health increased the financial incentives for KT, gave permission to private hospitals to perform KT, and promoted education on organ donation both for medical providers and the public [32]. Measures taken in the Netherlands included a national LD kidney exchange program for incompatible donors (from 2004 onwards), home-based education about living donation, and financial compensation for additional health care costs and loss of income for the LD [6]. Albania and Latvia were among the countries with the largest increase in LD-KT rate. Transplantation experts from Albania indicated that several measures implemented to increase their LD-KT rate were extremely successful such as the use of standard protocols for the definition of suitable donors, public campaigns to raise LD organ donation awareness and financial compensation for the LD [26]. For Latvia, experts reported that some of the measures taken were successful, e.g. providing information to ESKD patients on the possibility of LD-KT and the use of expanded criteria regarding the age of the recipient [26]. Nevertheless, the Latvian experts also perceived barriers for transplantation, especially lack of knowledge by both the donor and recipient as well as distrust in the healthcare system [26]. Other countries had a decreasing trend in LD-KT rate. Experts from Croatia indicated that most measures were taken to enhance DD-KT rate and only few for LD-KT rate, probably leading to a decrease in LD-KT rate [26]. Finally, in Cyprus experts indicated that they perceived many barriers for LD-KT rate, primarily lack of knowledge about transplantation among potential LDs [26].
Strength and limitations
A main strength of this study is that we present the trends in total, DD, and LD KT rates from nearly all European countries for almost a decade.
This study also has limitations. First, both the ERA Registry and GODT databases were used to obtain the number of KTs, and the data in these two databases did not always fully match due to for example differences in geographical coverage of the country. For most countries the same database was used for the entire study period to minimize bias in time trends. Second, the Joinpoint analyses do not detect an increase or decrease over a period of only 1 or 2 years. Finally, we can only speculate on measures that might have been successful in increasing KT rate but cannot prove causation.
CONCLUSION
In Europe, the total KT rate increased due to an increase in the DD-KT rate (3.4 p.m.p.) and to a lesser extent by an increase in the LD-KT rate (1.5 p.m.p.). The trends in KT rate varied widely from country to country. KT rates were higher in Western than in Eastern European countries, especially for total and DD transplants. In most countries, KTs with grafts from DDs were performed more often than those with grafts from LDs. These variations represent differences in, amongst other things, policies, laws, resources and attitudes. These trends in KT rate in individual countries combined with information on potentially successful initiatives as well as perceived barriers from previously published papers may guide the medical community and policymakers in determining where and how to target strategies to increase KT rate.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank the patients and the staff of the dialysis and transplant units for contributing the data via their national and regional renal registries to the ERA Registry and the GODT. Furthermore, we gratefully acknowledge the following registries and persons for their contribution of the data: Albanian Renal Registry (M. Rroji and E. Likaj); Austrian Dialysis and Transplant Registry (OEDTR) (F. Engler, R. Kramar, G. Mayer, and the Austrian Society of Nephrology); Belarus Renal Registry (K.S. Komissarov and K.S. Kamisarau); Dutch-speaking Belgian Society of Nephrology (NBVN) (M. Couttenye and F. Schroven); French-speaking Belgian Society of Nephrology (GNFB) (J.M. des Grottes and F. Collart); Renal Registry Bosnia and Herzegovina; Cyprus Renal Registry (A. Pastelli and L Yioukas); Czech Republic: Registry of Dialysis Patients (RDP) (F. Lopot, I. Rychlík and J. Potucek); Danish Nephrology Registry (DNS); Estonian Society of Nephrology (Ü. Pechter and K. Lilienthal); Finnish Registry for Kidney Diseases (P. Finne and H. Niemelä); France: The Epidemiology and Information Network in Nephrology (REIN) (M. Lassalle and C. Couchoud); Hellenic Renal Registry (G. Moustakas); Icelandic End-Stage Renal Disease Registry; Montenegro Renal Registry (M. Ratkovic, D. Radunović and F. Tomović); Italian Registry of Dialysis and Transplantation (RIDT) (A. Limido and M. Postorino); Latvian Renal Registry (V. Kuzema, A. Popovam and A. Pētersons); Lithuanian Renal Registry (V. Vainauskas and I. Nedzelskiene); North Macedonian Renal Registry (O. Stojceva and R.I. Bushljetik); Norwegian Renal Registry (A.V. Reisæter); Portuguese Renal Registry (A. Ferreira); Romanian Renal Registry (RRR) (G. Mircescu, and E. Podgoreanu); Russian Renal Registry (A. Andrusev and N. Tomilina); Renal Registry in Serbia (M. Lausevic, all of the Serbian renal units, and the Serbian Society of Nephrology); Slovakian Renal Registry (I. Lajdová, V. Spustová and M.J. Rosenberger); Spain Renal Registry (B. Mahillo Durán and M.O. Valentín Muñoz); Swedish Renal Registry (SRR) (K.G. Prütz, M. Stendahl, M. Evans, S. Schön and H. Rydell); Swiss Dialysis Registry (P. Ambühl and R. Guidotti); Dutch Renal Registry (RENINE) (L. Heuveling, S. Vogelaar and M. ten Dam); Registry of the Nephrology, Dialysis and Transplantation in Turkey (TSNNR) (K. Ateş and G. Süleymanlar); UK Renal Registry (all the staff of the UK Renal Registry and of the renal units submitting data); Scottish Renal Registry (SRR) (All of the Scottish renal units); and the other ERA Registry committee members not mentioned above for their advice in the analysis and the drafting of this paper: C. Wanner, P. Ambühl, P.M. Ferraro, S.A. Bakkaloglu, J. Helve, J.E. Sánchez-Alvarez, S.S. Sørensen and E. Vidal. The ERA Registry is funded by the European Renal Association (ERA). This article was written by Rianne Boenink et al. on behalf of the ERA Registry which is an official body of the ERA.
Contributor Information
Rianne Boenink, ERA Registry, Amsterdam UMC location University of Amsterdam, Department of Medical Informatics, Amsterdam, The Netherlands; Amsterdam Public Health, Quality of Care and Ageing & Later Life, Amsterdam, The Netherlands.
Anneke Kramer, ERA Registry, Amsterdam UMC location University of Amsterdam, Department of Medical Informatics, Amsterdam, The Netherlands; Amsterdam Public Health, Quality of Care and Ageing & Later Life, Amsterdam, The Netherlands.
Rosalie E Tuinhout, ERA Registry, Amsterdam UMC location University of Amsterdam, Department of Medical Informatics, Amsterdam, The Netherlands.
Emilie Savoye, Direction Prélèvement Greffe Organes-Tissus, Agence de la biomédecine, Saint-Denis La Plaine, France.
Anders Åsberg, The Norwegian Renal Registry, Department of Transplantation, Oslo University Hospital – Rikshospitalet, Oslo, Norway; Department of Pharmacy, University of Oslo, Oslo, Norway.
Alma Idrizi, Service of Nephrology, UHC “Mother Teresa”, Tirana, Albania.
Julia Kerschbaum, Austrian Dialysis and Transplant Registry, Department of Internal Medicine IV – Nephrology and Hypertension, Medical University Innsbruck, Innsbruck, Austria.
Ieva Ziedina, Pauls Stradins Clinical University Hospital, Riga, Latvia.
Edita Ziginskiene, Lithuanian Nephrology, Dialysis and Transplantation Association, Lithuania; Nephrology Department, Medical Academy, Lithuanian University of Health Sciences, Lithuania.
Emanuel Farrugia, Division of Nephrology, Mater Dei Hospital, Msida, Malta.
Liliana Garneata, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania; Department of Internal Medicine and Nephrology, Dr Carol Davila Teaching Hospital of Nephrology, Bucharest, Romania.
Elena V Zakharova, Nephrology and Hemodialysis, Russian Medical Academy of Continuing Professional Education, Moscow, Russian Federation.
Samira Bell, Scottish Renal Registry, Public Health Scotland, Meridian Court, Glasgow, UK; Division of Population Health & Genomics, University of Dundee, Ninewells Hospital, Dundee, UK.
Miha Arnol, Department of Nephrology, University Medical Centre Ljubljana, Ljubljana, Slovenia; Medical Faculty, University of Ljubljana, Ljubljana, Slovenia.
Mårten Segelmark, Department of Clinical Sciences in Lund, Lund University and Skane University Hospital, Lund, Sweden.
Kyriakos Ioannou, Cyprus Renal Association, Nicosia, Cyprus.
Kristine Hommel, Department of Cardiology, Endocrinology and Nephrology, Holbaek Hospital, Holbaek, Denmark.
Mai Rosenberg-Ots, Department of Internal Medicine, Tartu University and Tartu University Hospital, Tartu, Estonia.
Evgueniy Vazelov, Dialysis Center “El Masri”, Burgas, Bulgaria.
Jaakko Helve, Finnish Registry for Kidney Diseases, Helsinki, Finland; Nephrology, Abdominal Center, University of Helsinki, Helsinki University Hospital, Helsinki, Finland.
Sándor Mihály, Hungarian National Blood Transfusion Service, Budapest, Hungary.
Runólfur Pálsson, Division of Nephrology, Landspitali–The National University Hospital of Iceland, Reykjavik, Iceland; Faculty of Medicine, School of Health Sciences, University of Iceland, Reykjavik, Iceland.
Maurizio Nordio, Division of Nephrology, AULSS2, Treviso, Italy.
Nikola Gjorgjievski, University Hospital of Nephrology, Skopje, North Macedonia; Faculty of Medicine, University Ss Cyril and Methodius, Skopje, North Macedonia.
Aiko P J de Vries, Department of Medicine, Division of Nephrology, Leiden Transplant Center, Leiden University Medical Center, Leiden, The Netherlands.
Nurhan Seyahi, Department of Nephrology, Istanbul University-Cerrahpasa, Cerrahpasa Medical Faculty, Istanbul, Turkey.
Winnie A Magadi, UK Kidney Association, Bristol, UK.
Halima Resić, Society of Nephrology And Dialysis of Bosnia and Herzegovina, Sarajevo, Bosnia and Herzegovina.
Aleh Kalachyk, Minsk Scientific and Practical Center for Surgery, Transplantation and Hematology, State Institution, Minsk, Republic of Belarus.
Axel O Rahmel, Deutsche Stiftung Organtransplantation, Frankfurt am Main, Germany.
Ana A Galvão, Portuguese Society of Nephrology, Coimbra, Portugal.
Radomir Naumovic, Zvezdara University Clinical Hospital, Belgrade, Serbia; High Medical School, University of Belgrade, Belgrade, Serbia.
Torbjörn Lundgren, Division of Transplantation Surgery, CLINTEC, Karolinska Institute, Stockholm, Sweden.
Mustafa Arici, Department of Nephrology, Faculty of Medicine, Hacettepe University, Ankara, Turkey.
Johan M de Meester, Department of Nephrology, Dialysis and Hypertension, Dutch-speaking Belgian Renal Registry (NBVN), VITAZ, Sint-Niklaas, Belgium.
Alberto Ortiz, Fundación Jiménez Díaz, Universidad Autónoma de Madrid, Fundación Renal Iñigo Alvarez de Toledo, Madrid, Spain.
Kitty J Jager, ERA Registry, Amsterdam UMC location University of Amsterdam, Department of Medical Informatics, Amsterdam, The Netherlands; Amsterdam Public Health, Quality of Care and Ageing & Later Life, Amsterdam, The Netherlands.
Vianda S Stel, ERA Registry, Amsterdam UMC location University of Amsterdam, Department of Medical Informatics, Amsterdam, The Netherlands; Amsterdam Public Health, Quality of Care and Ageing & Later Life, Amsterdam, The Netherlands.
FUNDING
K.J.J. and V.S.S. report grants from the European Renal Association.
DATA AVAILABILITY STATEMENT
The data underlying this article are available in the article and in its online supplementary material.
CONFLICT OF INTEREST STATEMENT
No conflicts of interest were declared.
REFERENCES
- 1. Tonelli M, Wiebe N, Knoll Get al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 2011;11:2093–109. [DOI] [PubMed] [Google Scholar]
- 2. Hellemans R, Kramer A, De Meester Jet al. Does kidney transplantation with a standard or expanded criteria donor improve patient survival? Results from a Belgian cohort. Nephrol Dial Transplant 2021;36:918–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eurotransplant. Annual Report 2019. Leiden, The Netherlands: CIP-Gegevens Koninklijke Bibliotheek, Den Haag, 2020. [Google Scholar]
- 4. Scandiatransplant. Available at: http://www.scandiatransplant.org/data/sctp_figures_2021_2Q.pdf (23 August 2021, date last accessed). [Google Scholar]
- 5. Matesanz R, Domínguez-Gil B, Coll Eet al. How Spain reached 40 deceased organ donors per million population. Am J Transplant 2017;17:1447–54. [DOI] [PubMed] [Google Scholar]
- 6. Working Group on Living Donation under the European Union . Toolbox Living Kidney Donation. Action Plan on organ donation and transplantation (2009–2015): Strengthened Cooperation between Member States. 2016. Available at: https://ec.europa.eu/health/sites/health/files/blood_tissues_organs/docs/eutoolbox_living_kidney_donation_en.pdf (2 June 2022, date last accessed). [Google Scholar]
- 7. Domínguez-Gil B, Haase-Kromwijk B, Van Leiden Het al. Current situation of donation after circulatory death in European countries. Transpl Int 2011;24:676–86. [DOI] [PubMed] [Google Scholar]
- 8. Lennerling A, Lovén C, Dor FJet al. Living organ donation practices in Europe - results from an online survey. Transpl Int 2013;26:145–53. [DOI] [PubMed] [Google Scholar]
- 9. Tushla L, Rudow DL, Milton Jet al. Living-donor kidney transplantation: reducing financial barriers to live kidney donation—recommendations from a consensus conference. Clin J Am Soc Nephrol 2015;10:1696–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. UK Renal Registry (2020) UK Renal Registry 22nd Annual Report – data to 31/12/2018, Bristol, UK. Available from: renal.org/audit-research/annual-report. [Google Scholar]
- 11. United States Renal Data System . 2020 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. ANZDATA Registry. 42nd Report, Chapter 7: Kidney Transplantation. Adelaide, Australia:Australia and New Zealand Dialysis and Transplant Registry, 2019. Available at: http://www.anzdata.org.au. [Google Scholar]
- 13. ERA Registry: ERA Registry Annual Report 2019. Amsterdam, The Netherlands: Amsterdam UMC, location AMC, Department of Medical Informatics, 2021. [Google Scholar]
- 14. ERA-EDTA Registry: ERA-EDTA Registry Annual Report 2018. Amsterdam, The Netherlands: Amsterdam UMC, location AMC, Department of Medical Informatics, 2020. [Google Scholar]
- 15. GODT . Methodology. http://www.transplant-observatory.org/methodology/ (5 November 2020, date last accessed). [Google Scholar]
- 16. Eurostat . Population change - Demographic balance and crude rates at national level. https://ec.europa.eu/eurostat/web/products-datasets/-/demo_gind (5 November 2020, date last accessed). [Google Scholar]
- 17. The United Nations Population Fund. Available at: https://www.unfpa.org/data/world-population-dashboard (5 November 2020, date last accessed). [Google Scholar]
- 18. Joinpoint Regression Program, Version 4.2.0.2. June 2015; Statistical Research and Applications Branch, National Cancer Institute. [Google Scholar]
- 19. Kramer A, Stel V, Zoccali Cet al. An update on renal replacement therapy in Europe: ERA-EDTA Registry data from 1997 to 2006. Nephrol Dial Transplant 2009;24:3557–66. [DOI] [PubMed] [Google Scholar]
- 20. National Cancer Institute . Joinpoint Help Manual 4.7.0.0. Bethesda, MD: Division of Cancer Control and Population Sciences, 2019. [Google Scholar]
- 21. Kim HJ, Fay MP, Feuer EJet al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000;19:335–51. [DOI] [PubMed] [Google Scholar]
- 22. Gutierrez-Peña M, Zuñiga-Macias L, Marin-Garcia Ret al. High prevalence of end-stage renal disease of unknown origin in Aguascalientes Mexico: role of the registry of chronic kidney disease and renal biopsy in its approach and future directions. Clin Kidney J 2021;14:1197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wang JH, Hart A.. global perspective on kidney transplantation: United States. Kidney360 2021;2:1836–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yagisawa T, Mieno M, Ichimaru Net al. Trends of kidney transplantation in Japan in 2018: data from the kidney transplant registry. Ren Replace Ther 2019;5:3. [Google Scholar]
- 25. Sever M, Jager KJ, Vanholder Ret al. A roadmap for optimizing chronic kidney disease patient care and patient-oriented research in the Eastern European nephrology community. Clin Kidney J 2021;14:23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Boenink R, Kramer A, Vanholder RCet al. Factors influencing kidney transplantation rates: study from the ERA Registry. Nephrol Dial Transplant 2023;gfad001. 10.1093/ndt/gfad001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. European Kidney Health Alliance . Joint Statement. Thematic Network on Improving Organ Donation and Transplantation in the EU 2019. 2019. http://ekha.eu/wp-content/uploads/FINAL_Joint-Statement-of-the-Thematic-Network-on-Organ-Donation-and-Transplantation.pdf(10 May 2022, date last accessed). [Google Scholar]
- 28. Živčić-Ćosić S, Bušić M, Župan Žet al. Development of the Croatian model of organ donation and transplantation. Croat Med J 2013;54:65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liashchuk SP. Organ donation in the Republic of Belarus: 10 years of experience, ethical problems and the prospects for development. Available at: https://rm.coe.int/liashchuk-10-ten/16808d71d1 (10 May 2022, date last accessed). [Google Scholar]
- 30. Spiegel Online . Organ transplant scandal shocks Germany. http://www.spiegel.de/international/germany/organ-transplant-scandal-shocks-germany-a-848016.html (20 August 2021, date last accessed). [Google Scholar]
- 31. Claisse G, Gaillard F, Mariat C.. Living kidney donor evaluation. Transplantation 2020;104:2487–96. [DOI] [PubMed] [Google Scholar]
- 32. Andacoglu O, Aki FT.. Global perspective on kidney transplantation: Turkey. Kidney360 2021;2:1160–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.