Abstract
Introduction
Clostridioides difficile infection (CDI) is increasingly recognized as a public health threat at the community level in addition to being one of the most common causes of healthcare-associated infections. In Germany, the epidemiology of CDI is primarily informed by national hospital-based CDI surveillance. We used health claims data from Germany to obtain valuable insights on population-level disease burden and risk factors for CDI.
Methods
This was a retrospective cohort study using a representative sample from the InGef research database. Overall and age- and sex-stratified CDI incidence rates were estimated for German adults from 2013 to 2017 using different case definitions (i.e., main, broad, strict), and further stratified by setting (inpatient versus outpatient). Risk factors for CDI were assessed for the 2013–2016 period.
Results
The CDI incidence rate was high but declined by 15.3% from 2013 [141 (95% confidence interval, CI 137–145) cases/100,000 person-years] to 2017 [120 (95% CI 116–123)]. Annual CDI incidence rates were higher in female patients and the elderly. The most important risk factors for CDI were chronic inflammatory bowel disease [odds ratio (OR) 4.7, 95% CI 4.0–5.5], chemotherapy (OR 4.7, 95% CI 4.1–5.2), chronic kidney disease (OR 2.9, 95% CI 2.6–3.3), and ciprofloxacin receipt (OR 2.6, 95% CI 2.4–2.8).
Conclusions
Despite prevention strategies leading to declining incidence, CDI remains an important public health threat in Germany, with a high burden in the hospital setting and an outpatient epidemiology that is poorly understood. These findings, which are relevant both regionally and globally, can be used as a basis for further research on the full burden of CDI in Germany.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40121-023-00800-6.
Keywords: Administrative claims, healthcare; Clostridioides difficile; Cohort studies; Epidemiology; Incidence; Infection; Retrospective studies; Risk factors; Secondary data
Key Summary Points
| Why carry out this study? | |
| Similar to other geographies globally, Clostridioides difficile infection (CDI) is an important threat to public health in Germany in both healthcare settings and increasingly, in the community. | |
| Population-level evidence of CDI from hospital-based studies or administrative health claims data is scarce in Germany. | |
| This study used a representative sample from a large health claims database to estimate CDI incidence in Germany between 2013 and 2017, assess the distribution of CDI diagnosis by inpatient or outpatient setting, and evaluate the risk factors for CDI. | |
| What was learned from the study? | |
| While CDI incidence rates in Germany declined by 15.3% between 2013 [141 cases/100,000 person years (95% confidence interval, CI 137–145)] and 2017 [120 cases/100,000 person years (95% CI 116–123)], high CDI incidence was observed in female and older adult patients across all study years. | |
| This knowledge is important to inform healthcare professionals regarding the urgent threat of CDI and can help to further leverage the implementation of existing and innovative treatment and prevention to lower the CDI burden. | |
| Our study provides valuable population-level insights on CDI in the hospital setting in Germany and highlights the need for targeted research in the outpatient setting to estimate the full burden of CDI in Germany. |
Introduction
Clostridioides difficile (C. difficile) remains one of the most common causes of healthcare-associated infections and is increasingly recognized as a public health threat at the community level, despite widespread preventive efforts [1, 2]. Advanced age, antimicrobial exposure, hospitalization, chronic disease comorbidities, and immunosuppression have been identified as risk factors for C. difficile infection (CDI) [3]. CDI is associated with an increased risk of hospitalization, the need for skilled nursing care, placement in a nursing home or other long-term care facility, high healthcare costs including extended hospital stay, and excess mortality in cases of severe CDI [4–10].
Globally, the burden of CDI is reported as high [11]; however, considerable heterogeneity is observed owing to differences in diagnostic testing policies, laboratory methods, and data reporting between countries [12]. Compared with other geographies, the USA, which is also represented disproportionately in studies assessed for systematic literature reviews, has a very high incidence of CDI [11]. In a systematic literature review by Finn and colleagues, Germany had the highest CDI incidence rates among the EU5 countries, which include France, Italy, Spain, and the United Kingdom. CDI recurrence is also very common, with median CDI recurrence rates ranging from 5.4% (range 3.8–18.4%) in Japan to 23.7% (range 10.4–36.1%) in Canada. Globally, there are no clear trends in CDI incidence over time; CDI incidence was stable in many countries, decreased in Canada, and increased in the USA between 2009 and 2012 [11] before decreasing from 2012 onward, mainly driven by decreases in healthcare-associated CDI cases [2].
Recent population-level evidence of CDI burden in Germany is scarce [8]. National-level CDI surveillance, including routine population- or hospital-based surveillance, is conducted by different entities. The Robert Koch Institute (RKI) reports the annual incidence of severe CDI (e.g., 1595 severe CDI cases in 2020) [13]. The CDAD–KISS (Clostridium difficile assoziierten Diarrhö–Krankenhaus Infektions Surveillance Systems, Nationales Referenzzentrum für Nosokomiale Infektionen) module of the voluntary hospital-based surveillance system for nosocomial infections reports all CDI hospitalizations (e.g., 22,426 reported CDI hospitalizations across 525 hospitals in 2020) [14] but only covers approximately one-fourth of all German hospitals [15]. The Federal Health Monitoring Information System (Gesundheitsberichterstattung des Bundes or GBE–BUND) reports discharge diagnoses on the basis of the International Classification of Diseases, 10th Revision, German Modification codes (ICD-10-GM) for all hospitals in Germany, and identified 16,877 hospitalized cases in 2020 with a primary diagnosis for CDI [16]. There is no public surveillance of CDI in Germany outside of hospitals, and data on outpatient CDI are therefore very limited at a national level, as is the understanding of patient characteristics and distribution of CDI risk factors.
This study intended to supplement public statistics and population- or hospital-based CDI surveillance from Germany through the retrospective analysis of a large, nationally representative, health claims database to estimate CDI incidence and assess associated risk factors in German adults. The inclusion of outpatient claims data and patient demographic and clinical characteristics helps address current gaps in evidence on the epidemiology of CDI in Germany.
Methods
We used a health claims database to conduct a retrospective cohort study of the incidence, risk factors, economic, and clinical burden of CDI in Germany. In this article, we report on the annual population-based CDI incidence rates in German adults, CDI diagnosis by setting, and CDI risk factors. Additionally, we describe how different case definitions can impact CDI incidence estimates as part of a sensitivity analysis on the potential misclassification of cases.
Health Insurance in Germany
Health coverage in Germany is universal and compulsory under the country’s healthcare system. Health insurance is provided under the statutory health insurance (SHI) scheme that covers approximately 87% of the population and substitutive private health insurance for approximately 11% of the population on the basis of income above a certain level; coverage is also provided under special programs (e.g., soldiers) [17]. Irrespective of individual contributions, everyone has equal access to healthcare in Germany. SHI is provided by 105 sickness funds [17]; while all insurances offer common services, differences arise on the basis of additional services covered, such as travel vaccines, homeopathy, etc.
Data Source
This study was based on anonymized health claims data from the InGef (Institute for Applied Health Research Berlin GmbH) research database comprising data from more than 8 million insured persons across all federal states of Germany covered under approximately 60 SHI programs [18]. The InGef database, which contains patient sociodemographic information; hospitalization data, including details on and exact dates of admission, main and secondary diagnoses, and procedures; drug prescription data with exact dates; medical aid and remedy prescriptions with exact dates; accrued sector-wise costs; and outpatient services and diagnoses data on a quarterly basis, offers good external validity on morbidity, mortality, and prescription drug use in the German population [18]. We used an age- and sex-representative sample population (i.e., approximately 4 million insured persons) created by InGef for research purposes for this study; this sampling strategy is described in detail elsewhere [18]. The InGef database was preferred over other health claims databases to address our research questions as it covers all relevant settings and aspects of the healthcare sector; is representative to the German population; and provides a large sample size. Common limitations inherent to German health claims databases, such as the quarterly transmission of outpatient diagnosis data, were appropriately addressed (see “Study Population”). All patient-level and provider-level data in the InGef research database are anonymized to comply with German data protection regulations and German federal law. Hence, approval from an ethics committee was not required. Informed consent from study subjects to participate in the study and consent for publication were not applicable.
Study Design
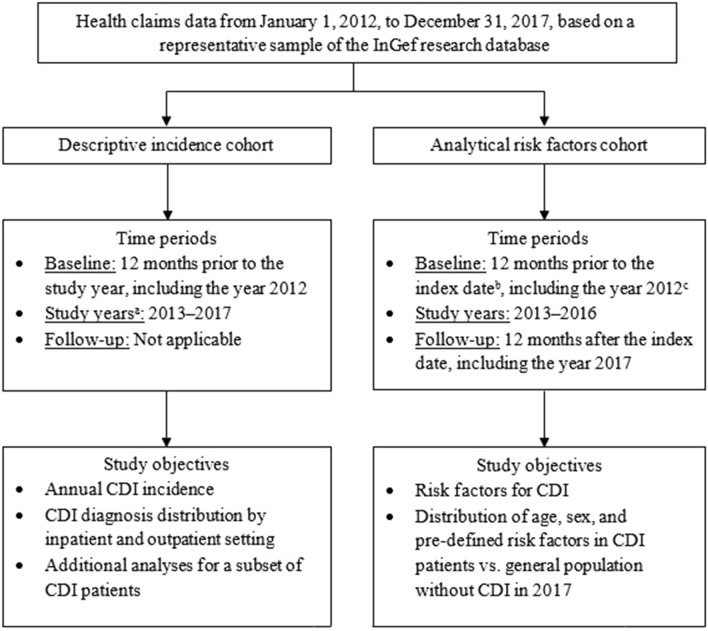
We constructed two retrospective cohorts to investigate incidence- and risk-factor-related study objectives; details are summarized in Fig. 1.
Fig. 1.
Study design schematic. CDI Clostridioides difficile infection, InGef Institute for Applied Health Research Berlin GmbH. a Each eligible person contributed person-time under risk or disease during a given study year. b The index date was the date of the first or incident CDI diagnosis. c For both the descriptive incidence cohort and analytical risk factors cohort, the year 2012 solely served as the baseline period to consider the 60-day gap before an incident CDI diagnosis occurring in the year 2013
Study Population
Table 1 presents the three case definitions (i.e., main, broad, and strict) used to identify CDI cases in this study. The main case definition was used in all analyses, whereas the broad and strict case definitions were applied only for sensitivity analyses related to potential misclassification of CDI cases and in incidence rate calculations. An incident case during a study year had no previous CDI diagnosis matching the case definition in the prior 60 days, including any time in the baseline period. Similar to the approach used by Lübbert et al. [8], the index date was the admission date for a main inpatient diagnosis and the discharge date minus 10 days for a secondary diagnosis. As outpatient diagnosis claims are only available on a quarterly basis, outpatient prescription dates were used as the index date for outpatient CDI cases in the main case definition. To distinguish a new primary CDI diagnosis from an existing CDI episode or recurrence, a gap of 60 days was required between A04.7 ICD-10-GM diagnosis codes, similar to Lübbert et al. [8]. Therefore, every new CDI diagnosis marked the beginning of a 60-day CDI episode, while every subsequent diagnosis or prescription during that episode prolonged the CDI episode for a further 60 days.
Table 1.
CDI case definitions
| Main case definition | Broad case definition | Strict case definition |
|---|---|---|
|
Main inpatient diagnosis with ICD-10-GM code A04.7- and/or secondary inpatient diagnosis with ICD-10-GM code A04.7- and/or verified outpatient diagnosis with ICD-10-GM code A04.7- and a prescription of either metronidazole (ATC code J01XD01), vancomycin (ATC code J01XA01), or fidaxomicin (ATC code A07AA12) in the same quarter |
Main inpatient diagnosis with ICD-10-GM code A04.7- and/or secondary inpatient diagnosis with ICD-10-GM code A04.7- and/or verified outpatient diagnosis with ICD-10-GM code A04.7- |
Main inpatient diagnosis with ICD-10-GM code A04.7- and/or secondary inpatient diagnosis with ICD-10-GM code A04.7- and/or Verified outpatient diagnosis with ICD-10-GM code A04.7- and a prescription of either metronidazole (ATC code J01XD01), vancomycin (ATC code J01XA01), or fidaxomicin (ATC code A07AA12) in the same quarter and a laboratory test for confirmation of CDI (with EBM code 32151, 32700, 32707, 32722, or 32723) in the same quarter |
ATC Anatomical Therapeutic Chemical Classification, CDI Clostridioides difficile infection, EBM German physician fee schedule or Einheitlicher Bewertungsmaßstab, ICD-10-GM International Classification of Diseases, 10th Revision, German Modification
The 2013–2017 analytical incidence cohorts included insured persons from the InGef representative sample aged ≥18 years on 1 January of the study year with continuous insurance during the preceding 12 months baseline period. Continuous insurance in the study year was not required to calculate the CDI incidence rate, including person-time under risk.
The 2013–2016 analytical risk factors cohort included insured persons from the InGef representative sample aged ≥18 years at cohort entry with continuous insurance in the 12 months prior to the index date (i.e., first CDI diagnosis) and until 31 December 2017, death, or study disenrollment. Any persons who met the CDI case definition or had a prescription for fidaxomicin (ATC code A07AA12) in the 12 months prior to the index date were excluded.
Study Outcomes and Statistical Analysis
Study outcomes included CDI incidence rates and cumulative incidence using the annual incidence cohorts, inpatient or outpatient CDI diagnosis using the annual incidence cohorts, and CDI risk factor assessment using the risk factors cohort. All analyses were conducted by InGef staff with R Software version 3.5.
CDI Incidence
We estimated the overall CDI incidence rates as incident CDI cases/100,000 person-years and cumulative incidence as incident CDI patients/100,000 persons for each study year and stratified by sex and age groups (i.e., 18–< 50, 50–59, 60–64, 65–69, 70–74, 75–79, 80–84, and ≥ 85 years, with ≥ 65, ≥ 70, and ≥ 75 years as alternative cut-offs). The estimation of CDI incidence rates and cumulative incidence with corresponding 95% confidence intervals (CI) assumed a Poisson distribution and a binomial distribution, respectively.
Additional Analyses for CDI Patients Identified Using the Broad Case Definition
We investigated whether these patients had a laboratory test performed and antibiotic prescriptions other than metronidazole, vancomycin, or fidaxomicin; these were reported using descriptive statistics.
Risk Factors for CDI
Risk factors were either predefined [i.e., use of immunosuppressants, chemotherapy, radiation therapy, chronic inflammatory bowel disease, use of proton pump inhibitor (PPI) or histamine2-receptor (H2) antagonists, irritable bowel syndrome, gastroesophageal reflux disease, and diverticulosis of the intestine] or identified from the database as common comorbidities with ICD-10-GM codes present in at least one-third of patients with CDI in the year prior to diagnosis or antibiotic prescriptions with ATC codes prescribed to at least 5% of patients with CDI in the 60 days prior to diagnosis. Antibiotic classes, based on five-digit ATC codes, were also summarized; however, the individual drugs were included in the risk factor analysis to evaluate potential differential risk within each class. Furthermore, the distributions of age, sex, and the predefined risk factors in the general adult population without CDI were compared with those of patients with CDI for the year 2017. Additionally, logistic regression was conducted comparing all CDI cases from 2013 to 2016 with a randomly selected group of non-CDI controls (i.e., four controls/case), adjusting for age categories (reference < 50 years) and sex. Age and sex were included as covariates to enable estimation of their association with CDI risk and to maintain statistical power in contrast to a matching approach. The binary, multivariable regression model included the predefined risk factors and the most common comorbidities and prescribed antibiotics described above. All covariates with a statistically significant odds ratio of > 1 (p < 0.05) were considered as CDI risk factors.
Results
CDI Incidence
Annual Incidence Rates of CDI
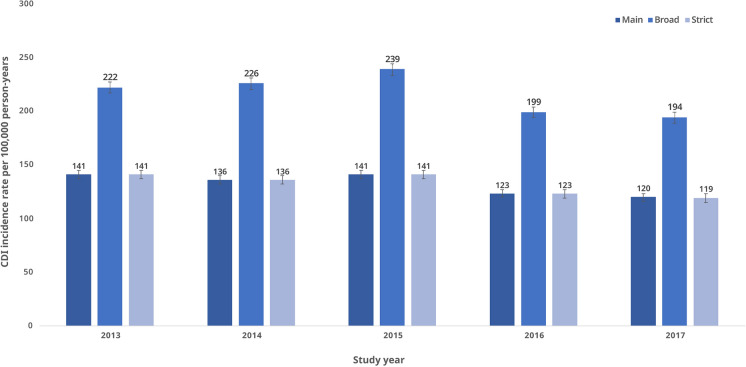
Figure 2 illustrates the overall annual CDI incidence rates stratified by case definition; details, including corresponding 95% CIs, are provided in Table 2. Annual CDI incidence rates between 2013 and 2017 were similar for the main and strict case definitions [e.g., 141 (95% CI 137–145) cases/100,000 person–years and 141 (95% CI 137–145), respectively, in 2013 and 2015]. A decline was observed in CDI incidence rates after 2015. In contrast, annual CDI incidence rates for the broad case definition were higher between 2013 and 2017, with an increase observed from 2014 [226 (95% CI 220–231) cases/100,000 person-years] to 2015 [239 (95% CI 233–244)] followed by a decline in 2016 [199 (95% CI 194–204)].
Fig. 2.
Overall CDI incidence rates stratified by case definition, 2013–2017. CDI Clostridioides difficile infection. The CDI incidence rates and corresponding 95% confidence intervals were estimated on the basis of a Poisson distribution
Table 2.
Overall CDI incidence rates stratified by case definition, 2013–2017
| Study year | Total person-time under risk (person-years) | Main case definition | Broad case definition | Strict case definition | |||
|---|---|---|---|---|---|---|---|
| Incident CDI casesa | Incidence rate per 100,000 person-years (95% CI) | Incident CDI casesa | Incidence rate per 100,000 person-years (95% CI) | Incident CDI casesa | Incidence rate per 100,000 person-years (95% CI) | ||
| 2013 | 3,191,463 | 4509 | 141 (137–145) | 7084 | 222 (217–227) | 4489 | 141 (137–145) |
| 2014 | 3,204,934 | 4367 | 136 (132–140) | 7229 | 226 (220–231) | 4359 | 136 (132–140) |
| 2015 | 3,223,450 | 4554 | 141 (137–145) | 7695 | 239 (233–244) | 4534 | 141 (137–145) |
| 2016 | 3,236,277 | 3994 | 123 (120–127) | 6449 | 199 (194–204) | 3974 | 123 (119–127) |
| 2017 | 3,225,186 | 3859 | 120 (116–123) | 6247 | 194 (189–199) | 3844 | 119 (115–123) |
CDI Clostridioides difficile infection, CI confidence interval
aIncident CDI cases are defined by no previous occurrence matching the case definition within 60 days prior to the CDI occurrence
Female patients had higher CDI incidence rates compared with male patients in 2013 [148 (95% CI 142–154) cases/100,000 person–years versus 134 (95% CI 129–140)], 2014 [144 (95% CI 139–150) versus 128 (95% CI 122–133)], and 2016 [131 (95% CI 126–137) versus 115 (95% CI 110–121)] (Tables S1 and S2 in the Supplementary Material file). Annual CDI incidence rates stratified by age group are presented in Table 3. The rates increased with advancing age, with exponential increases observed for older age groups. For example, the CDI incidence rates in the year 2017 were 373 [95% CI 360–386] cases/100,000 person-years in persons aged ≥ 65 years, 469 [95% CI 452–487] in persons aged ≥ 70 years, and 575 [95% CI 552–598] in persons aged ≥ 75 years.
Table 3.
CDI incidence rates per the main case definition and stratified by age group, 2013–2017
| Age group (in years) | 2013 | 2014 | 2015 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Incident CDI casesa | Total person-time under risk (person-years) | Incidence rate per 100,000 person-years (95% CI) |
Incident CDI casesa | Total person-time under risk (person-years) | Incidence rate per 100,000 person-years (95% CI) |
Incident CDI casesa | Total person-time under risk (person-years) | Incidence rate per 100,000 person-years (95% CI) |
|
| Overall (18–≥ 85) | 4509 | 3,191,483 | 141 (137–145) | 4367 | 3,204,953 | 136 (132–140) | 4554 | 3,223,472 | 141 (137–145) |
| 18–< 50 | 218 | 1,551,073 | 14 (12–16) | 247 | 1,532,992 | 16 (14–18) | 240 | 1,523,331 | 16 (14–18) |
| 50–59 | 263 | 594,016 | 44 (39–50) | 283 | 607,848 | 47 (41–52) | 276 | 620,578 | 44 (39–50) |
| 60–64 | 194 | 257,312 | 75 (65–87) | 237 | 258,370 | 92 (80–104) | 265 | 257,455 | 103 (91–116) |
| 65–69 | 300 | 195,584 | 153 (137–172) | 270 | 200,369 | 135 (119–152) | 315 | 211,072 | 149 (133–167) |
| 70–74 | 565 | 228,137 | 248 (228–269) | 595 | 221,885 | 268 (247–291) | 537 | 208,336 | 258 (236–281) |
| 75–79 | 827 | 175,260 | 472 (440–505) | 838 | 188,043 | 446 (416–477) | 907 | 197,510 | 459 (430–490) |
| 80–84 | 996 | 107,716 | 925 (868–984) | 860 | 108,290 | 794 (742–849) | 897 | 114,312 |
785 (734–838) |
| ≥ 85 | 1146 | 82,386 | 1391 (1312–1474) | 1037 | 87,156 | 1190 (1118–1264) | 1117 | 90,877 | 1229 (1158–1303) |
| ≥ 65 | 3834 | 789,083 |
486 (471–502) |
3600 | 805,743 | 447 (432–462) | 3773 | 822,107 | 459 (444–474) |
| ≥ 70 | 3534 | 593,499 | 595 (576–615) | 3330 | 605,374 | 550 (532–569) | 3458 | 611,035 | 566 (547–585) |
| ≥ 75 | 2969 | 365,362 | 813 (784–842) | 2735 | 383,489 | 713 (687–740) | 2921 | 402,699 | 725 (699–725) |
| Age group (in years) | 2016 | 2017 | ||||
|---|---|---|---|---|---|---|
| Incident CDI casesa | Total person-time under risk (person-years) | Incidence rate per 100,000 person-years (95% CI) |
Incident CDI casesa | Total person-time under risk (person-years) | Incidence rate per 100,000 person-years (95% CI) |
|
| Overall (18–≥ 85) | 3994 | 3,236,293 | 123 (120–127) | 3859 | 3,225,207 | 120 (116–123) |
| 18–< 50 | 220 | 1,512,427 | 15 (13–17) | 197 | 1,482,479 | 13 (11–15) |
| 50–59 | 270 | 627,505 | 43 (38–48) | 286 | 634,073 | 45 (40–51) |
| 60–64 | 217 | 257,413 | 84 (73–96) | 206 | 257,653 | 80 (69–92) |
| 65–69 | 319 | 230,648 | 138 (124–154) | 297 | 238,878 | 124 (111–139) |
| 70–74 | 456 | 189,059 | 241 (220–264) | 392 | 180,287 | 217 (196–240) |
| 75–79 | 740 | 202,284 | 366 (340–393) | 704 | 204,794 | 344 (319–370) |
| 80–84 | 806 | 121,297 | 664 (619–712) | 805 | 129,322 | 622 (580–667) |
| ≥ 85 | 966 | 95,660 | 1010 (947–1076) | 972 | 97,722 | 995 (933–1059) |
| ≥ 65 | 3287 | 838,947 | 392 (379–405) | 3170 | 851,002 | 373 (360–386) |
| ≥ 70 | 2968 | 608,299 | 488 (471–506) | 2873 | 612,125 | 469 (452–487) |
| ≥ 75 | 2512 | 419,240 | 599 (576–623) | 2481 | 431,838 | 575 (552–598) |
CDI Clostridioides difficile infection, CI confidence interval
aIncident CDI cases are defined by no previous occurrence matching the case definition within 60 days prior to the CDI occurrence
Cumulative Incidence of CDI
Table S3 in the Supplementary Material file presents the overall cumulative incidence of CDI between 2013 and 2017 by case definition. Cumulative incidence based on the main and strict case definitions were mostly identical between 2013 and 2017 and were lower than the cumulative incidence per the broad case definition [e.g., for study year 2017, 110 (95% CI 107–114)/100,000 persons with main case definition and 110 (95% CI 106–114) with strict case definition versus 149 (95% CI 145–154) with broad case definition]. Tables S4 and S5 in the Supplementary Material file present age-group-specific annual cumulative incidences of CDI per the main case definition for female and male patients, respectively.
Additional Analyses for CDI Patients Identified Using the Broad Case Definition
Approximately one-third of all CDI cases identified by the broad case definition were outpatient diagnoses without an inpatient diagnosis or CDI-specific antibiotic treatment in the same quarter as the outpatient diagnosis (ranging from 31.9% in 2013 to 35.3% in 2015; data not shown). Approximately half of these CDI cases had a laboratory test for CDI in the same quarter as their outpatient diagnosis, ranging from 47.4% in 2014 to 60.4% in 2016, and almost 34.0% of them had an antibiotic prescription in the same quarter (data not shown).
Risk Factors for CDI
Table 4 presents the clinical characteristics (i.e., most common main inpatient diagnoses, prescribed antibiotics, and predefined risk factors) of incident CDI patients in the risk factors cohort. The most common outpatient and secondary inpatient diagnoses and antibiotic classes are provided in Tables 5 and 6. Across all diagnoses (i.e., main or secondary inpatient and verified outpatient), hypertension (83.7%) was the most common comorbidity followed by other chronic conditions, such as heart failure (43.0%) and chronic ischemic heart disease (39.8%) (Table 6). Heart failure (9.5%) was the most common main inpatient diagnosis (Table 4). Many patients with CDI had a prescription for PPI/H2 antagonists (61.4%) and immunosuppressants (23.4%) in the 12-month baseline period. Furthermore, ciprofloxacin (6.4%) and cefuroxime (6.3%) were among the most prescribed antimicrobial agents for patients with CDI in the 60 days prior to diagnosis. Fluoroquinolones (9.2%), second-generation cephalosporins (6.6%), and combined penicillin (5.0%) were the most frequently prescribed antibiotic classes among patients with CDI (Table 5).
Table 4.
Most common main inpatient diagnoses and predefined risk factors during the 12-month baseline period and prescribed antibiotics up to 60 days prior to diagnosis in patients with CDI (N = 15,499)
| Main inpatient diagnoses | Prescribed antibiotics in the outpatient sector | Predefined risk factors | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ICD-10-GM | Label | n | (%) | ATC code | Label | n | (%) | Label | n | (%) |
| I50 | Heart failure | 1468 | 9.5 | J01MA02 | Ciprofloxacin | 1000 | 6.5 | PPI/H2 antagonists | 9521 | 61.4 |
| J18 | Pneumonia, unspecified organism | 949 | 6.1 | J01DC02 | Cefuroxime | 972 | 6.3 | Immunosuppressants | 3630 | 23.4 |
| I63 | Cerebral infarction | 726 | 4.7 | J01CR04 | Sultamicillin | 402 | 2.6 | Gastroesophageal reflux disease | 2798 | 18.1 |
| S72 | Fracture of femur | 694 | 4.5 | J01CR02 | Amoxicillin and enzyme-inhibitors | 380 | 2.5 | Diverticulosis of the intestine | 2432 | 15.7 |
| B96 | Other bacterial agents as the cause of diseases classified elsewhere | 684 | 4.4 | J01FF01 | Clindamycin | 356 | 2.3 | Chemotherapy | 1404 | 9.1 |
| B95 | Strep as the cause of diseases classified elsewhere | 612 | 3.9 | J01EE01 | Sulfamethoxazole and trimethoprim | 323 | 2.1 | Chronic inflammatory bowel disease | 507 | 3.3 |
| J91 | Pleural effusion in conditions classified elsewhere | 586 | 3.8 | J01CA04 | Amoxicillin | 268 | 1.7 | Radiation therapy | 466 | 3.0 |
| J44 | Other chronic obstructive pulmonary disease | 558 | 3.6 | J01MA12 | Levofloxacin | 265 | 1.7 | Irritable bowel syndrome | 290 | 1.9 |
| A41 | Other sepsis | 548 | 3.5 | J01DD13 | Cefpodoxime | 185 | 1.2 | |||
| I70 | Atherosclerosis | 545 | 3.5 | J01MA14 | Moxifloxacin | 152 | 1.0 | |||
ATC Anatomical Therapeutic Chemical Classification, CDI Clostridioides difficile infection, H2 histamine2-receptor, ICD-10-GM International Classification of Diseases, 10th Revision, German Modification, PPI proton pump inhibitor. All data are ordered in descending frequency
Table 5.
Most prescribed antibiotic classes in patients with CDI (N = 15,499) during the study
| ATC code | Description | n | (%) |
|---|---|---|---|
| J01MA | Fluoroquinolones | 1428 | 9.2 |
| J01DC | Second-generation cephalosporins | 1022 | 6.6 |
| J01CR | Combinations of penicillins, including beta-lactamase inhibitors | 776 | 5.0 |
| J01FF | Lincosamides | 356 | 2.3 |
| J01DD | Third-generation cephalosporins | 342 | 2.2 |
| J01EE | Combinations of sulfonamides and trimethoprim, including derivatives | 323 | 2.1 |
| J01FA | Macrolides | 319 | 2.1 |
| J01CA | Penicillins with extended spectrum | 272 | 1.8 |
| J01XE | Nitrofuran derivatives | 123 | 0.8 |
| J01XX | Other antibacterials | 108 | 0.7 |
| J01AA | Tetracyclines | 71 | 0.5 |
| J01CE | Beta-lactamase sensitive penicillins | 43 | 0.3 |
| J01XA | Glycopeptide antibacterials | 40 | 0.3 |
| J01EA | Trimethoprim and derivatives | 26 | 0.2 |
| J01DB | First-generation cephalosporins | 20 | 0.1 |
| J01GB | Other aminoglycosides | 8 | 0.1 |
| J01CF | Beta-lactamase resistant penicillins | 7 | 0.1 |
| J01DH | Carbapenems | < 5 | – |
| J01XD | Imidazole derivatives | < 5 | – |
| J01XB | Polymyxins | < 5 | – |
ATC Anatomical Therapeutic Chemical Classification, CDI Clostridioides difficile infection
Table 6.
Most common verified outpatient or secondary inpatient diagnoses during the 12-month baseline period in patients with CDI (N = 15,499)
| ICD-10-GM | Label | n | (%) |
|---|---|---|---|
| I10 | Essential (primary) hypertension | 12,971 | 83.7 |
| E78 | Disorders of lipoprotein metabolism and other lipidemias | 8086 | 52.2 |
| E87 | Other disorders of fluid, electrolyte and acid–base balance | 6722 | 43.4 |
| I50 | Heart failure | 6659 | 43.0 |
| N39 | Other disorders of urinary system | 6224 | 40.2 |
| Z92 | Personal history of medical treatment | 6221 | 40.1 |
| I25 | Chronic ischemic heart disease | 6162 | 39.8 |
| N18 | Chronic kidney disease | 5955 | 38.4 |
| E11 | Type 2 diabetes mellitus | 5927 | 38.2 |
| M54 | Dorsalgia | 5603 | 36.2 |
CDI Clostridioides difficile infection, ICD-10-GM International Classification of Diseases, 10th Revision, German Modification
Results from the binary logistic regression analysis, which included identified risk factors from the exploratory assessment (i.e., most common comorbidities and prescribed outpatient antibiotics) and predefined possible risk factors are presented in Table 7. Several covariates in the model with odds ratios > 1 (p < 0.05) were assessed as risk factors for CDI. The most important risk factors for CDI in the model were age ≥ 85 years [OR 40.9 (95% CI 37.1–45.2)] compared with the reference group of patients aged < 50 years; chronic inflammatory bowel disease [OR 4.7 (95% CI: 4.0–5.5)], chemotherapy [OR 4.7 (95% CI 4.1–5.2)], and chronic kidney disease [OR 2.9 (95% CI 2.6–3.3)].
Table 7.
Results of the binary logistic regression analysis for CDI risk factor identification in CDI cases and randomly assigned non-CDI comparison group
| Independent variable | Odds ratio (95% CI) |
p-value |
|---|---|---|
| Patient characteristics | ||
| 50–59 years (ref: < 50 years) | 2.1 (1.9–2.3) | < 0.001 |
| 60–64 years (ref: < 50 years) | 3.3 (3.0–3.7) | < 0.001 |
| 65–69 years (ref: < 50 years) | 4.9 (4.4–5.5) | < 0.001 |
| 70–74 years (ref: < 50 years) | 7.7 (6.9–8.5) | < 0.001 |
| 75–79 years (ref: < 50 years) | 12.6 (11.5–13.9) | < 0.001 |
| 80–84 years (ref: < 50 years) | 23.7 (21.5–26.2) | < 0.001 |
| ≥ 85 years (ref: < 50 years) | 40.9 (37.1–45.2) | < 0.001 |
| Female (ref: male) | 0.9 (0.8–0.9) | < 0.001 |
| Predefined risk factors | ||
| Chronic inflammatory bowel disease | 4.7 (4.0–5.5) | < 0.001 |
| Chronic kidney disease | 2.9 (2.6–3.3) | < 0.001 |
| Heart failure | 2.3 (2.0–2.5) | < 0.001 |
| Other disorders of urinary system | 2.3 (2.0–2.6) | < 0.001 |
| Immunosuppressants | 1.8 (1.7–1.9) | < 0.001 |
| Atrial fibrillation and flutter | 1.8 (1.6–2.0) | < 0.001 |
| Personal history of medical treatment | 1.7 (1.5–1.9) | < 0.001 |
| Type 2 diabetes mellitus | 1.6 (1.5–1.7) | < 0.001 |
| Chronic ischemic heart disease | 1.5 (1.4–1.6) | < 0.001 |
| Essential (primary) hypertension | 1.3 (1.3–1.4) | < 0.001 |
| Diverticulosis of the intestine | 1.3 (1.2–1.4) | < 0.001 |
| Irritable bowel syndrome | 1.3 (1.1–1.5) | 0.007 |
| Disorders of lipoprotein metabolism and other lipidemias | 1.0 (0.9–1.1) | 0.706 |
| Gastroesophageal reflux disease | 0.9 (0.9–1.0) | 0.053 |
| Dorsalgia | 0.8 (0.8–0.9) | < 0.001 |
| Exploratory risk factors | ||
| Chemotherapy | 4.7 (4.1–5.2) | < 0.001 |
| Ciprofloxacin | 2.6 (2.4–2.8) | < 0.001 |
| PPI/H2 antagonists | 2.4 (2.3–2.6) | < 0.001 |
| Cefuroxime | 2.4 (2.2–2.7) | < 0.001 |
| Radiation therapy | 1.7 (1.4–2.0) | < 0.001 |
CDI Clostridioides difficile infection; CI confidence interval; H2 histamine2-receptor; PPI proton pump inhibitor. Data for predefined and exploratory risk factors are presented in descending order
The distributions of demographic characteristics and predefined risk factors of CDI patients based on the main case definition from the 2017 incidence cohort (N = 3630) compared with the general non-CDI adult population in the InGef database (N = 3,293,234) were also evaluated. The mean age of CDI cases was 75.2 ± 13.9 years compared with 51.3 ± 18.7 years for the non-CDI population (data not shown). Females comprised 52.3% (n = 1898) of the CDI population in the 2017 incidence cohort compared with 51.0% (n = 1,679,648) in the non-CDI population (data not shown). Table 8 summarizes the distribution of predefined risk factors. Most of the predefined risk factors were significantly more common in CDI cases compared with the non-CDI population (p < 0.001); the frequency of irritable bowel syndrome was not significantly different between CDI cases (2.0%) and the non-CDI population (1.4%).
Table 8.
Comparison of predefined risk factors between CDI cases and the general adult non-CDI population for 2017
| Risk factor | CDI cases in 2017 (N = 3630) |
Persons without CDI in the InGef database (N = 3,293,234) |
p-value | ||
|---|---|---|---|---|---|
| n | (%) | n | (%) | ||
| PPI/H2 antagonists | 2280 | 62.8 | 653,616 | 19.9 | < 0.001 |
| Immunosuppressants | 945 | 26.0 | 243,685 | 7.4 | < 0.001 |
| Gastroesophageal reflux disease | 740 | 20.4 | 288,663 | 8.8 | < 0.001 |
| Diverticulosis of the intestine | 596 | 16.4 | 165,560 | 5.0 | < 0.001 |
| Chemotherapy | 364 | 10.0 | 45,417 | 1.4 | < 0.001 |
| Chronic inflammatory bowel disease | 127 | 3.5 | 31,318 | 1.0 | < 0.001 |
| Radiation therapy | 124 | 3.4 | 17,909 | 0.5 | < 0.001 |
| Irritable bowel syndrome | 72 | 2.0 | 46,630 | 1.4 | 0.005 |
CDI Clostridioides difficile infection, H2 histamine2-receptor, InGef Institute for Applied Health Research Berlin GmbH, PPI proton pump inhibitor. Data are ordered in descending frequency of CDI cases
Discussion
We estimated CDI incidence and assessed CDI risk factors in this retrospective cohort study using a large health claims database. High CDI incidence rates were observed during the study, particularly in female and older adult patients. The most common comorbidities and prescribed antibiotics during the baseline period were identified. Most predefined risk factors were significantly more common in patients with CDI compared with the non-CDI population in 2017.
Annual CDI incidence rates among eligible adults were high between 2013 and 2017; among all adults and adults ≥ 65 years old, CDI incidence rates ranged from 141 [(95% CI 137–145) cases/100,000 person-years in 2013 to 120 (95% CI 116–123)] in 2017, and 486 [95% CI 471–502] in 2013 to 373 [95% CI 360–386] in 2017, respectively. The main case definition provides a good estimate of CDI hospitalizations but may not reflect the full burden of disease, including outpatient diagnoses. GBE–BUND reports all ICD-10-GM diagnoses at hospital discharge, which can be used to quantify hospitalized CDI burden in Germany. CDI cases reported to GBE–BUND in 2013 and 2017 resulted in an overall hospitalized CDI incidence of 137 and 108/100,000 persons and 540 and 405/100,000 in persons ≥ 65 years, respectively (authors’ calculation based on primary and secondary CDI case counts assessed from [16]) These incidence rates are comparable to our findings, indicating that our analysis is representative for all of Germany. Most studies investigating CDI incidence globally used less recent data from Germany (i.e., between 2009 and 2015) [11]. In these studies, the CDI incidence in Germany was observed to be relatively high and above the average of other countries. When compared with the USA, which had data available on CDI incidence for the same time period as our study, slightly higher incidence was observed, with 155/100,000 persons in 2013 and 144/100,000 persons in 2017, respectively [2]. The findings for our study confirm these recent findings, indicating that CDI remains a severe problem in Europe as well. This knowledge is important to inform healthcare professionals globally about the urgent threat of CDI and to help to further leverage the implementation of existing and innovative treatments and preventive measures to lower the CDI burden. Similar to our findings, hospitalized CDI incidence based on GBE–BUND and in the USA declined between 2013 and 2017; this decline continued into 2018 [2, 14, 16]. This decline can be explained by the increasing application of prevention approaches, such as infection control, hygiene measures, and antibiotic stewardship [19]. However, the decline in the USA was observed mainly in healthcare-associated CDI incidence, with community-associated CDI incidence increasing during this period [2]. Our study provided limited insight on CDI burden in the outpatient setting as only 2–3% of cases were outpatient diagnoses. Further, there is no public surveillance system in Germany that reports community-treated CDI. Lübbert et al. reported an overall CDI incidence of 83 cases/100,000 persons in 2012 and identified 15% of the incident CDI cases in the outpatient setting [8]. Using our broad case definition, which did not require an antibiotic prescription, yielded a much higher incidence rate of approximately 200 cases/100,000 person-years: approximately one-third of these cases were observed in the outpatient setting with no inpatient diagnosis and no antibiotic prescription, and thus likely represent mild cases that self-resolved without treatment. This seems plausible as the German treatment guidelines for CDI suggest waiting for spontaneous resolution of mild CDI cases, combined with close clinical monitoring, before initiating specific therapy [20]. To our knowledge, this is the first study to identify such cases and estimate their frequency relative to those with a more severe clinical course. The high incidence observed suggests that the burden of community-treated CDI in Germany may be comparable to the USA, though additional, prospectively collected data are needed to confirm this observation.
CDI incidence rates were observed to be higher in female patients and in the elderly, as reported elsewhere [8, 21]. When compared with the general population without CDI in 2017, patients with CDI were, on average, more than 20 years older, and adults aged ≥ 65 years had higher CDI incidence. The comorbidity profile of patients with CDI with higher prevalence could also be affected by age, as these patients were older on average. The higher CDI rates in female patients can be explained by the higher female representation in older age groups; after adjusting for age, female sex was protective against CDI in our regression model [OR = 0.9 (95% CI 0.8–0.9)].
The study findings also support the existing evidence on leading risk factors for CDI, including comorbidities, such as chronic inflammatory bowel disease, chronic heart disease, chronic kidney disease, and diabetes. Similar risk factors were identified globally [11]. With an aging population burdened by comorbidities, these risk factors indicate that CDI may pose a more severe threat in the future. The only two antibiotics considered in the regression analysis were cefuroxime and ciprofloxacin, which were prescribed to > 5% of the patients with CDI in the 60 days prior to CDI diagnosis. The odds ratios for both antibiotics were > 2, confirming the significantly higher risk for CDI after antibiotic treatment.
A few limitations of this study need to be considered. First, although the InGef analysis dataset covers approximately 4 million insured persons, representativeness to the national population can only be guaranteed for age and sex [18]. However, the InGef database demonstrated good overall accordance with the German population regarding morbidity, mortality, and drug usage [18]. Second, a possibility of misclassification of CDI cases exists as review of individual patient files to confirm the presence of medical conditions was not done owing to German data protection laws, and laboratory test results were unavailable. Although misclassification is unlikely due to the large sample size, we conducted sensitivity analyses using additional case definitions, i.e., broad and strict, and estimated almost identical CDI incidence rates using the main and strict case definitions, indicating that a laboratory test was almost always performed in case of outpatient diagnoses. The higher number of cases under the broad definition resulted from additional outpatient diagnoses without a prescription of vancomycin, metronidazole, or fidaxomicin, and no further inpatient diagnosis in the same quarter. These cases with outpatient diagnoses have low public health relevance; however, the risk of ICD-10 coding errors remains, resulting in underestimation (i.e., inaccurate coding of patients with CDI who were treated with antibiotics) or overestimation (i.e., patients with diarrhea due to other infectious causes coded as CDI). Third, we may have potentially underestimated the number of CDI cases due to the 60-day “wash-out” period implemented to avoid double-counting of recorded cases. In particular, this limited the identification of recurrent CDI, which contributes to a substantial portion of the disease burden. Although we used binary multivariable logistic regression analysis, we could not control for unmeasured confounders in the risk factor analysis. A fourth limitation is the immeasurable time bias. Since drug dispensation during a hospital stay cannot be reconstructed in German claims data, the only antibiotics which could be identified in this study were those prescribed in the outpatient setting and dispensed in a pharmacy. Therefore, we may not have identified all antibiotics given to a patient before the first CDI diagnosis in the exploratory risk factor assessment.
Conclusions
Our study provides valuable population-level information and insights on CDI incidence and risk factors in Germany, which have previously only been studied in specific subgroups. High CDI incidence was observed in older adults, and the burden of CDI may increase in the future due to the aging population and increasing prevalence of chronic health conditions. Besides providing information on CDI hospitalizations, this study offered early insights on CDI in the outpatient setting, which is not yet clearly understood. Current prevention and hygiene measures may reach their limits in the near future. Additional prevention tools, including vaccines, are highly desired to further lower CDI incidence [22, 23]. Information on CDI burden and trends from a nationally representative health claims database can prove beneficial for clinicians, public health specialists, and other stakeholders to promote the development of such approaches.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Funding
WIG2 received funding from Pfizer Pharma GmbH (Berlin, Germany) for the execution of the study and for preparation of original drafts of the manuscript. InGef GmbH, as a subcontractor, received funding from WIG2 for data extraction, data analysis, and preparation of original drafts of the manuscript. Subsequent revisions to the manuscript, including payment of the rapid service fee, were funded by Pfizer Inc. No honoraria or payments were made for authorship.
Medical Writing and/or editorial assistance
We thank Tina Ploner for assistance with the data extraction and analysis. Tina Ploner is an employee of InGef GmbH and InGef GmbH served as a subcontractor of WIG2. InGef GmbH received funding from WIG2 for data extraction, data analysis, and preparation of original drafts of the manuscript. In turn, WIG2 received funding from Pfizer Pharma GmbH (Berlin, Germany). Medical writing support was provided by Melissa Furtado at Pfizer and was funded by Pfizer Inc. Editorial support was provided by Melissa Furtado and Sonia Philipose at Pfizer and was funded by Pfizer Inc.
Authorship
All authors of this article met the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, including accountability for all aspects of the work and approval of the version to be published.
Author Contributions
Thomas Weinke, Gordon Brestrich, Christof von Eiff, Kirstin Heinrich, Jennifer Moïsi, and Katharina Schley contributed to study conceptualization. Thomas Weinke, Dominik Beier, Dennis Häckl, Kirstin Heinrich, Jennifer Moïsi, and Katharina Schley contributed to the study methodology. Dominik Beier performed the investigation, data curation, and formal analysis. Thomas Weinke and Christof von Eiff supervised the work. Thomas Weinke, Dominik Beier, and Katharina Schley wrote the first draft of the manuscript. Gordon Brestrich, Dennis Häckl, Christof von Eiff, Kirstin Heinrich, and Jennifer Moïsi reviewed and edited prior versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Thomas Weinke received an honorarium from Pfizer in connection with the development of the study. Dennis Häckl is employed by WIG2, which received funding from Pfizer Pharma GmbH for the execution of the study and manuscript preparation. Dominik Beier is employed by InGef, which acted as subcontractor and received funding from WIG2 for the execution of the study and manuscript preparation. Gordon Brestrich, Christof von Eiff, and Katharina Schley are employees of Pfizer Pharma GmbH; Kirstin Heinrich is an employee of Pfizer Inc.; and Jennifer Moïsi is an employee of Pfizer Vaccines—all of whom may hold stocks or stock options in Pfizer Inc.
Compliance with Ethics Guidelines
All patient-level and provider-level data in the InGef research database are anonymized to comply with German data protection regulations and German federal law. Hence, approval from an Ethics Committee was not required. Informed consent from study subjects to participate in the study and consent for publication were not applicable.
Data Availability
The data used in this study cannot be made available in the manuscript, the Supplementary Material file, or in a public repository due to German data protection laws (Bundesdatenschutzgesetz). To facilitate the replication of results, anonymized data used for this study are stored on a secure drive at the Institute for Applied Health Research Berlin (InGef). Access to the data used in this study can only be provided to external parties under the conditions of the cooperation contract of this research project and can be assessed upon request, after written approval (info@ingef.de), if required.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Balsells E, Shi T, Leese C, et al. Global burden of Clostridium difficile infections: a systematic review and meta-analysis. J Glob Health. 2019;9(1):010407. doi: 10.7189/jogh.09.010407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guh AY, Mu Y, Winston LG, et al. Trends in U.S. burden of Clostridioides difficile infection and outcomes. N Engl J Med. 2020;382(14):1320–30. doi: 10.1056/NEJMoa1910215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eze P, Balsells E, Kyaw MH, Nair H. Risk factors for Clostridium difficile infections—an overview of the evidence base and challenges in data synthesis. J Glob Health. 2017;7(1):010417. doi: 10.7189/jogh.07.010417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braae UC, Møller FT, Ibsen R, Ethelberg S, Kjellberg J, Mølbak K. The economic burden of Clostridioides difficile in Denmark: a retrospective cohort study. Front Public Health. 2020;8:562957–8. doi: 10.3389/fpubh.2020.562957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grube RF, Heinlein W, Scheffer H, et al. Economic burden of Clostridium difficile enterocolitis in German hospitals based on routine DRG data. Z Gastroenterol. 2015;53(5):391–397. doi: 10.1055/s-0034-1398803. [DOI] [PubMed] [Google Scholar]
- 6.Heister T, Wolkewitz M, Hehn P, et al. Costs of hospital-acquired Clostridium difficile infections: an analysis on the effect of time-dependent exposures using routine and surveillance data. Cost Eff Resour Alloc. 2019;17:16. doi: 10.1186/s12962-019-0184-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kimura T, Stanhope S, Sugitani T. Excess length of hospital stay, mortality and cost attributable to Clostridioides ( Clostridium) difficile infection and recurrence: a nationwide analysis in Japan. Epidemiol Infect. 2020;148:e65. doi: 10.1017/s0950268820000606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lübbert C, Zimmermann L, Borchert J, Hörner B, Mutters R, Rodloff AC. Epidemiology and recurrence rates of Clostridium difficile infections in Germany: a secondary data analysis. Infect Dis Ther. 2016;5(4):545–554. doi: 10.1007/s40121-016-0135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nanwa N, Sander B, Krahn M, et al. A population-based matched cohort study examining the mortality and costs of patients with community-onset Clostridium difficile infection identified using emergency department visits and hospital admissions. PLoS One. 2017;12(3):e0172410. doi: 10.1371/journal.pone.0172410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olsen MA, Stwalley D, Demont C, Dubberke ER. Clostridium difficile infection increases acute and chronic morbidity and mortality. Infect Control Hosp Epidemiol. 2019;40(1):65–71. doi: 10.1017/ice.2018.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finn E, Andersson FL, Madin-Warburton M. Burden of Clostridioides difficile infection (CDI)—a systematic review of the epidemiology of primary and recurrent CDI. BMC Infect Dis. 2021;21(1):456. doi: 10.1186/s12879-021-06147-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davies KA, Longshaw CM, Davis GL, et al. Underdiagnosis of Clostridium difficile across Europe: the European, multicentre, prospective, biannual, point-prevalence study of Clostridium difficile infection in hospitalized patients with diarrhoea (EUCLID) Lancet Infect Dis. 2014;14(12):1208–1219. doi: 10.1016/S1473-3099(14)70991-0. [DOI] [PubMed] [Google Scholar]
- 13.Robert-Koch-Institut. RKI-Ratgeber: Clostridioides (früher Clostridium) difficile [Internet]. Infection epidemiological yearbook of reportable diseases for 2020. Available from: https://www.rki.de/DE/Content/Infekt/Jahrbuch/Jahrbuch_2020.html. Accessed 1 Dec 2022.
- 14.Nationales Referenzzentrum für Surveillance von nosokomialen Infektionen [Internet]. CDAD–KISS Krankenhaus-Infektions-Surveillance-System module reference data for January–December 2020. Available from: https://www.nrz-hygiene.de/files/Referenzdaten/CDAD/202001_202012CDAD_Ref.pdf. Accessed 1 Dec 2022.
- 15.Statista [Internet]. Number of hospitals in Germany from 2000 to 2020. Available from: https://de.statista.com/statistik/daten/studie/2617/umfrage/anzahl-der-krankenhaeuser-in-deutschland-seit-2000/. Accessed 1 Dec 2022.
- 16.Das Informationssystem der Gesundheitsberichterstattung des Bundes [Internet]. Diagnostic data of the hospitals starting from 2000 (key figures of full-time inpatients) [Internet]. Available from: https://www.gbe-bund.de/gbe/pkg_isgbe5.prc_isgbe?p_uid=gast&p_aid=5195884&p_sprache=E. Accessed 1 Dec 2022.
- 17.Blümel M, Spranger A, Achstetter K, Maresso A, Busse R. Germany: Health system review. Health Systems in Transition, 2020; 22(6): pp.i–273. Available from: https://eurohealthobservatory.who.int/publications/i/germany-health-system-review-2020. Accessed 24 Feb 2023. [PubMed]
- 18.Ludwig M, Enders D, Basedow F, Walker J, Jacob J. Sampling strategy, characteristics and representativeness of the InGef research database. Public Health. 2022;206:57–62. doi: 10.1016/j.puhe.2022.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Sweileh WM. Bibliometric analysis of peer-reviewed literature on antimicrobial stewardship from 1990 to 2019. Global Health. 2021;17(1):1. doi: 10.1186/s12992-020-00651-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hagel S, Epple HJ, Feurle GE, et al. S2k-guideline gastrointestinal infectious diseases and Whipple's disease. Z Gastroenterol. 2015;53(5):418–459. doi: 10.1055/s-0034-1399337. [DOI] [PubMed] [Google Scholar]
- 21.Olsen MA, Young-Xu Y, Stwalley D, et al. The burden of clostridium difficile infection: estimates of the incidence of CDI from U.S. administrative databases. BMC Infect Dis. 2016;16:177. doi: 10.1186/s12879-016-1501-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pletz MW, Uebele J, Götz K, Hagel S, Bekeredjian-Ding I. Vaccines against major ICU pathogens: where do we stand? Curr Opin Crit Care. 2016;22(5):470–476. doi: 10.1097/mcc.0000000000000338. [DOI] [PubMed] [Google Scholar]
- 23.Lawrence J, Kitchin N, Anderson AS, et al. Safety and immunogenicity of different Clostridioides (Clostridium) difficile vaccine formulations in two early phase randomized studies of healthy adults aged 50–85 years. Vaccine. 2021;39(40):5991–6003. doi: 10.1016/j.vaccine.2021.05.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study cannot be made available in the manuscript, the Supplementary Material file, or in a public repository due to German data protection laws (Bundesdatenschutzgesetz). To facilitate the replication of results, anonymized data used for this study are stored on a secure drive at the Institute for Applied Health Research Berlin (InGef). Access to the data used in this study can only be provided to external parties under the conditions of the cooperation contract of this research project and can be assessed upon request, after written approval (info@ingef.de), if required.