Abstract
Elevated eosinophil counts in blood and tissue are a feature of many pathological processes. Eosinophils can migrate and accumulate in a wide variety of tissues and, by infiltrating a target organ, can mediate the development of several inflammatory diseases. The normalization of eosinophilia is a common biomarker of a treatable trait and can also be used as a prognostic and predictive biomarker since it implies a reduction in type 2 inflammation that contributes to disease pathogenesis. Biological therapies targeting this cell type and its proinflammatory mediators have been shown to be effective in the management of a number of eosinophilic diseases, and for this reason they constitute a potential common strategy in the treatment of patients with various multimorbidities that present with type 2 inflammation. Various biological options are available that could be used to simultaneously treat multiple target organs with a single drug, bearing in mind the need to offer personalized treatments under the umbrella of precision medicine in all patients with eosinophil-associated diseases (EADs). In addition to reviewing these issues, we also discuss a series of perspectives addressing the management of EAD patients from a multidisciplinary approach, with the collaboration of health professionals from different specialties who manage the different multimorbidities that frequently occur in these patients. We examine the basic principles of care that this multidisciplinary approach must cover and present a multidisciplinary expert opinion regarding the ideal management of patients with EADs, from diagnosis to therapeutic approach and follow-up.
Keywords: eosinophil, eosinophilic inflammation, eosinophil-associated disease, multidisciplinary management, expert opinion
1. Introduction: eosinophilic inflammation as a common ground in different diseases
Eosinophils make up about 3% of all circulating leukocytes in peripheral blood under homeostatic conditions (1). Their development in the bone marrow, activation, release into the bloodstream and survival in peripheral tissues depend on the orderly interaction of multiple transcription factors and cytokines (2–5), among which interleukin-5 (IL-5) is the most specific for this cell type (6, 7). IL-5 promotes the development and recruitment of eosinophils by acting synergistically with other molecules such as eotaxins (8), alarmins (thymic stromal lymphopoietin [TSLP]) and IL-4, IL-13, IL-25, IL-31 and IL-33, among others (9).
Eosinophil counts increase significantly in some pathological processes, both in blood and tissue compartments (10), mainly as consequence of a multi-immune response involving type 2 (T2) cytokines and other proinflammatory mediators. The active metabolism of eosinophils and the cytoplasmic secretory granules they contain allow them to act as inflammatory cells wherever they are recruited (11). Thus, they can trigger powerful cytotoxicity and inflammation processes that persist cyclically and chronically by interacting with other immune system cells that sustain their degranulation activity and lead to inflammation (12–18) ( Figure 1A ). The eosinophilic mediators-containing toxic granules are believed to damage the different tissues where these cells are specifically recruited. This suggests a direct causal relationship between eosinophils and the tissue damage that manifests in diseases such as asthma, chronic rhinosinusitis with nasal polyps (CRSwNP), eosinophilic gastrointestinal diseases (EGIDs) and systemic disorders as eosinophilic granulomatosis with polyangiitis (EGPA) and hypereosinophilic syndrome (HES), among others. All these supports the fact that eosinophil depletion is notably considered in the therapeutic interventions performed in all these pathologies (19–21). Besides, recent publications reported the involvement of T2 inflammation and eosinophils in the context of diverse autoimmune pathologies related to central nervous system, such as multiple sclerosis and neuromyelitis optica (NMO) (22, 23) ( Figure 1B ). As an example, the active role of eosinophils in the generation of tissue damage in the latter disease has been described in NMO mouse models in which the depletion of eosinophils by using an anti-IL-5 antibody was related to the reduction of tissue damage (24). Besides, the extent to which eosinophils participates in other pathologies such as Duchenne muscular dystrophy remains controversial (25).
Figure 1.
The eosinophil as the main cell responsible for diseases that present with eosinophilic inflammation. (A) The eosinophilic inflammation cycle. (B) Migration of eosinophils to the different tissues in which they cause eosinophilic diseases. COPD, chronic obstructive pulmonary disease; DRESS, drug reaction with eosinophilia and systemic symptoms; ECRS, eosinophilic chronic rhinosinusitis; EGPA, eosinophilic granulomatosis with polyangiitis; GM-CSF, granulocyte macrophage colony-stimulating factor; HES, hypereosinophilic syndrome; IL, interleukin; NARES, non-allergic rhinitis with eosinophilia syndrome; N-ERD, nonsteroidal anti-inflammatory drug-exacerbated respiratory disease; T2, type 2 immune response.
While it is important to remark the existence of eosinophilia in the absence of Th2-related processes as in the case of neoplastic or idiopathic HES, in which neither a clonal nor a reactive underlying pathology is detected (26–28).
The identification of eosinophilia as a biomarker of a treatable trait, namely T2 inflammation, has been classically associated with the pathogenesis of a number of respiratory diseases, up to a point that eosinophilia has been used to guide the treatment of some of these diseases (29, 30). A threshold of 300 cells/μL has been postulated to be used when identifying patients candidate to receive a treatment based on inhaled corticosteroids, according to the Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Lung Disease (GOLD) (30). Other definitions of blood eosinophilia are those defined by and absolute eosinophil count of >0.5 × 109/L, whereas hypereosinophilia relates to an absolute eosinophil count ≥ 1.5 × 109/L (28, 31–37). Nonetheless, the normal range of blood eosinophil counts in general population has not been well established yet and this threshold has been criticised and interpreted as a normal eosinophil range (38, 39). Besides, not only eosinophil counts are important, but also the period of time during which eosinophilia is maintained. A difference between transient or episodic and persisting eosinophilia has also been defined (28). Clonal or neoplastic eosinophilia is always related to a persistent increase in the counts of these cells unless specific anti-neoplastic therapies are used to target it (28, 31–37). Also, eosinophil variability, as measured by the recently proposed Eosinophil Variability Index, is associated with the hospitalization of patients with asthma (40).
Eosinophils migrate to the respiratory mucosa and release a large quantity of mediators that trigger a characteristic T2 inflammatory process resulting in airway remodelling (41–43). The eosinophilic cationic protein (ECP) is one of the eosinophil-derived mediators most widely studied among the biomarkers of eosinophil activation (44–46). Although it seems to be unspecific for the diagnosis of eosinophil-associated respiratory diseases such as asthma, ECP is considered as a useful biomarker of airway inflammation and its abundance in peripheral blood has been associated to the control of asthma, and considered as a good biomarker to monitor the efficacy of classical and new biological therapies used in the treatment of this disease (44–47). This eosinophilic inflammation increases during respiratory exacerbations and impairs disease control (48). It also induces the onset of other respiratory diseases such as allergic rhinitis, non-allergic rhinitis with eosinophilia syndrome (NARES) and chronic rhinosinusitis (CRS) (49, 50). In one third of patients with asthma, CRS induces the development of nasal polyps (CRSwNP), which is associated with T2 inflammation in up to 87% of patients (50–55), especially in the presence of eosinophil-associated multimorbidities (56–58). In fact, several studies and Clinical Practice Guidelines define eosinophilia as one of the main criteria to define T2 inflammation, both when measured in peripheral blood and most importantly at the nasal polyp tissue level (50, 52, 59–61). Chronic obstructive pulmonary disease (COPD) and asthma-COPD overlap (ACO) syndrome are two highly prevalent respiratory entities that can also present this T2 signature; the involvement of eosinophils is also important for the pathogenesis (62–66) and treatment of these diseases (67). COPD is a heterogeneous condition characterized by a chronic airflow limitation, defined by a post-bronchodilator FEV1/FVC <0.7, with different components and mechanisms involved (68), while ACO defines a situation in which a persistent airflow limitation is associated with clinical features compatible both with asthma and COPD (69–71), and underlying eosinophilic airway inflammation may be present (62).
The eosinophil is also one of the cell types involved in several pathogenic immune responses that occur in the skin, and systemic involvement may also be a factor, given the interaction of this compartment with the peripheral lymph nodes (72–74). Atopic dermatitis (AD) is the dermatosis most commonly related to this cell type. It is caused by the development of dysregulated T2 immune responses that lead to eosinophil recruitment and activation (75, 76). Similarly, the eosinophil appears as the primary effector cell in the pathogenesis of bullous pemphigoid (BP), a disease typically classified as humoral (77). In fact, the presence of activated eosinophils along the basement membrane of the epidermis has been described in patients with BP (78–81). Furthermore, the interaction of eosinophils and immunoglobulin E (IgE), the production of which is mediated by T2 cytokines (IL-4, IL-5), amplifies the inflammatory response in this disease and the associated tissue damage (82). Likewise, eosinophils play a more important role than previously thought in skin conditions such as chronic spontaneous urticaria (CSU) (83), typically associated with mast cell activity (84). In CSU, the eosinophils accumulate together with these cells in the characteristic perivascular infiltrates of the disease (83, 85), which results in an inflammatory response that subsequently manifests as the typical hives associated with this condition (83).
As mentioned above, eosinophil-mediated inflammation can result in pathological processes at the systemic level. EGPA and HES are two of the systemic diseases in which eosinophils are recruited and activated in peripheral blood and various tissues, mediating proinflammatory effects that lead to widespread tissue destruction (86–89). The pathogenesis of EGPA is partly the result of the complex interaction between innate and adaptive immunity, involving not only eosinophils but also other cells (15, 90, 91). In fact, in the opinion of the American College of Rheumatology, peripheral blood eosinophilia is one of the clinical-pathological factors of interest in the diagnosis of EGPA, since eosinophils appear to be involved in some of its main complications, including pulmonary infiltrates, cardiomyopathy, gastrointestinal and respiratory manifestations, and axonal neuropathy (15, 92). Likewise, it has been postulated that the aetiology of HES is related to a primary dysregulation of eosinophil proliferation or a secondary dysfunction of the T2 immune response, as observed in virus infections or lymphoproliferative disorders (93, 94). Eosinophilic infiltration and local release of proinflammatory mediators have been linked to various HES-associated effects on the heart, skin, nervous system, lungs, liver, and gastrointestinal tract (93, 94).
Eosinophils usually occur in very low proportions throughout the gastrointestinal tissue, although their infiltration into these tissues gives rise to different types of clinical conditions, including EGIDs, depending on the specific location where the infiltration occurs (95, 96). EGIDs include, among others, eosinophilic esophagitis (EoE), and eosinophilic gastritis and gastroenteritis (95, 97). Eosinophils are the characteristic cells in EoE, as their density in the oesophageal epithelium is one of the main histological findings of the disease, and their disappearance determines the effectiveness of its treatment (98).
2. Treatment of eosinophil-associated diseases
Normalization of eosinophilia constitutes an important goal in various eosinophil-associated diseases (EADs), since it is a surrogate biomarker of reduction of the T2 inflammation that contributes to the pathogenesis of these conditions, leading to significant clinical improvements (99–104). Eosinophil counts can also be considered a potential inflammatory biomarker in these diseases (75, 76, 105–112) and a predictor of the response to some of the drugs used in their treatment, such as corticosteroids (65, 66, 99, 113–119).
2.1. Current advances
Treatment with biological drugs is recommended in patients with difficult-to-treat and severe adult-onset eosinophilic asthma (69, 103, 120, 121). Achieving a good control of the symptoms, minimizing future risk of asthma-related morbidity and mortality, exacerbations, persistent airflow limitations and treatment side effects are the main long-term goals of asthma (69). The use of biological therapies such as monoclonal antibodies has been described as useful in the treatment of this disease (122). In these patients, the use of anti-IL-5 drugs (mepolizumab, reslizumab), that bind circulating IL-5 (122), inhibits the maturation and differentiation of eosinophils, thereby decreasing their counts in peripheral blood and tissue (123–125). Furthermore, drugs targeting the IL-5 receptor, IL-5Rα, such as benralizumab, enhance the elimination of eosinophils and their precursors by antibody-dependent cellular cytotoxicity (124, 126), with a correlation between the initial eosinophil counts and the response to some of these treatments (127). Drugs targeting other mediators of eosinophil recruitment to the respiratory mucosa such as the epithelial alarmin TSLP (tezepelumab) have also been related with a specific reduction in the number of eosinophils in the airway submucosa, leading to a reduction in eosinophilic airway inflammation (122, 128) that seems to accompany the improvements in asthma clinical outcomes after the use of this drug (129). These drugs have been shown to be effective in controlling severe eosinophilic asthma, reducing the number of exacerbations, diminishing or eliminating the use of systemic corticosteroids (130–132), increasing lung function, promoting general symptom control, and generally improving patient quality of life (QoL) (133–135). Along with intranasal corticosteroids, these biological drugs have also been approved for use in patients with severe, uncontrolled CRSwNP who have undergone endoscopic sinus surgery (136–139). Other biological drugs such as dupilumab (140–143) and omalizumab (144–147) have also been approved in this indication. Dupilumab blocks the signalling pathways of IL-4 and IL-13 by binding to IL-4Rα, which they share in hematopoietic cells such as B cells, CD4+ helper T cells, and eosinophils (122), while omalizumab targets the Fc fragment of IgE and therefore reduces its levels in serum and inhibits its binding to its high-affinity receptor on mast cells and basophils (122). The use of the dupilumab results in the reduction of eosinophil migration and consequently in lung and blood eosinophil accumulation. This promotion of hypereosinophilia has been observed in 4-25% of patients treated with this drug, in whom the use of anti-IL-5 drugs is therefore preferable (148, 149).
Nevertheless, while these drugs reduce the eosinophil count in patients with CRSwNP, this does not appear to be the only mechanism responsible for their efficacy, as indicated by the results of the latest phase III trials (141, 145, 150). A phase IIa study suggested a response to drugs such as benralizumab and mepolizumab in some subgroups of patients with COPD and eosinophilia (151), but the results of phase III trials with these drugs did not support a significant reduction in exacerbations associated with this disease (152, 153).
Biological therapies targeting eosinophils and their mediators are also included in the therapeutic algorithm of some EGIDs, such as EoE (154). Dupilumab has been associated in this disease with a significant symptomatic, endoscopic and histological improvement in treated patients (155), while in eosinophilic gastroenteritis, a reduction in tissue eosinophilia has been observed in patients with this condition and concomitant HES treated with drugs such as benralizumab (156) and omalizumab (157). Blocking IL-13, a cytokine that activates and promotes eosinophil chemotaxis, also significantly reduces oesophageal eosinophilia and endoscopic and symptomatic disease activity (155). This has also been observed with biological drugs that target other molecules that are central to eosinophil activity in the oesophagus, such as Siglec-8 or eotaxins (155, 158).
The use of drugs directed against various eosinophilic therapeutic targets has also been postulated for some skin diseases associated with the action of this cell type. Suppression of the levels of some eosinophilic mediators and cytokines that regulate the development and activation of these cells has been shown to be effective in moderate forms of AD in paediatric patients (159). IL-31, another eosinophil-related cytokine (160), has been proposed as one of the most promising therapeutic targets in the treatment of AD, since some preliminary data on drugs targeting IL-31 suggest that they are effective in the management of pruritus, one of the symptoms that impacts heavily on the QoL of patients with AD (161). Other drugs that target T2 pathways, such as omalizumab or dupilumab, have shown an effective response in BP (162–165).
2.2. Future directions
With regard to future developments in the treatment of EADs, the efficacy of anti-IL-5/5Rα drugs is being studied in various lung diseases, such as allergic bronchopulmonary aspergillosis, eosinophilic pneumonia and bronchiectasis, and in other inflammatory and immune-mediated processes in which eosinophils may play an effector role (166).
Since eosinophils express low-affinity IgE receptors and their maturation and proliferation depend on IL-5, clinical trials in CSU are being conducted with drugs such as mepolizumab, reslizumab and benralizumab, given that many patients with this disease respond to treatments that inhibit IgE- or IL-5-mediated processes (167).
Resolution of the damage caused by eosinophil infiltration and the consequent release of toxic granules is another potential therapeutic approach in the treatment of systemic eosinophilic complications (115, 119, 168, 169). The normalization of eosinophil counts in peripheral blood and tissues is an important strategy in this regard, which is why the effects of different anti-IL-5/5Rα (reslizumab, benralizumab) and anti-IgE (omalizumab) therapies for the treatment of EGPA (170–172) and HES are being studied (173). Some of these, e.g., mepolizumab, are already approved for the treatment of both diseases (168, 174, 175).
Besides IL-5, some other factors have been related to prolonged eosinophil survival and promoted differentiation of these cells (176–180), and therefore must be considered as a plausible explanation of processes related to eosinophilia that are resistant to anti-IL-5 therapies. Some biological agents targeting IL-5 and other eosinophil-related cytokines (IL-4, IL-13) are also being evaluated for the treatment of a number of EGIDs, although in some cases the data from these studies are still preliminary and insufficient scientific evidence is available to recommend the use of these drugs in routine clinical practice (155, 156, 158, 181). In the context of EoE, the positioning of biological therapies is being evaluated to improve patient QoL and modify the natural course of the disease. These biological agents could be administered as part of the treatment algorithm in the management of patients refractory to corticosteroids, as maintenance therapy in corticosteroid-induced remission, or as treatment of patients with EoE and atopic multimorbidities (182, 183).
In summary, biological drugs that target the eosinophil and its mediators constitute a potential strategy in the treatment of patients with multimorbidities who present with T2 inflammation in which the eosinophil plays a fundamental role. The different therapeutic alternatives discussed, whether already in use or in development, could be useful for treating multiple diseases with a single drug, always with the aim of achieving personalized treatments and precision medicine in all patients with EADs.
3. Discussion: the multidisciplinary management of eosinophilic diseases
Eosinophilia is a common biomarker in several diseases involving T2 inflammation that require a comprehensive management approach involving specialists from different medical disciplines. This would ensure a holistic view that would address the basic principles of care needed in all EAD patients: prompt and accurate diagnosis; referral by a multidisciplinary team if necessary; access to safe and effective treatments; and greater awareness and education about EADs (184). All healthcare professionals responsible for treating these patients must understand these principles and implement them in their routine clinical practice. In fact, the Clinical Practice Guidelines focused on the management of some of the mentioned EADs have been already developed in the context of a multidisciplinary point of view based on the collaboration of several professionals from different Scientific Societies (59), and some approaches to develop multidisciplinary units for the management of some other EADs have been already published (185).
3.1. Prompt and accurate diagnosis of EADs and referral of patients by a multidisciplinary team
Patients with EADs should be diagnosed promptly and accurately (184). One of the main needs in this respect is to establish a multidisciplinary referral pathway for patients with EADs (184) that encompasses aspects ranging from the diagnosis of an EAD and its possible eosinophil-based multimorbidities to patient treatment and follow-up. This pathway does not necessarily require the implementation of multidisciplinary functional units, but it does require open two-way communication channels between the specialists who manage often concomitant eosinophilic multimorbidities. In any case, specialists who treat patients with any EAD should be aware of the coexistence of different eosinophilic conditions and as such, be prepared to consult with other specialists regarding the initial eosinophilic diagnosis and other signs or symptoms that the patient may present. It is important to emphasize that this awareness must be sustained over time, as recurrent eosinophilic multimorbidities can develop gradually, and therefore may be detected during follow-up and not necessarily at the time of initial EAD diagnosis.
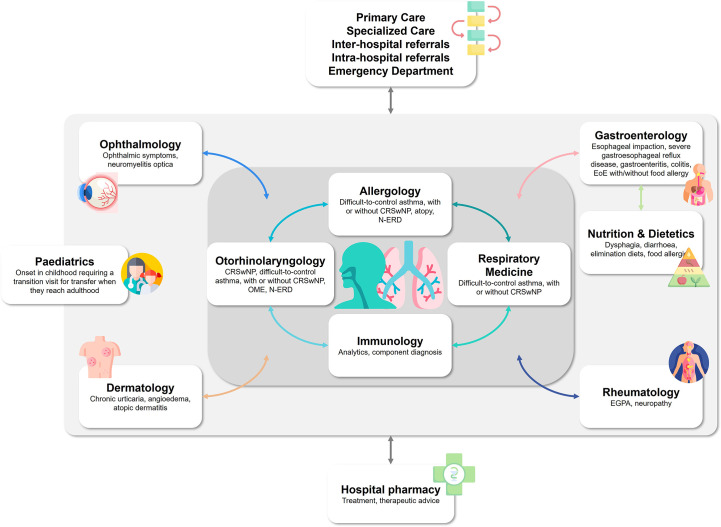
The advisability of multidisciplinary management depends on each patient’s profile: it may be unnecessary in some, while in others, due to the severity of their EADs, it may be crucial to detect and manage the onset of eosinophilic multimorbidities. Accordingly, referral criteria should be established to provide guidance when this is appropriate. Clinical practice experience tells us that a patient does not usually spontaneously notify the specialist of any signs or symptoms of a disease that they believe are not directly related to the reason for their visit, perhaps because they affect organs or systems that this particular specialist does not treat. Therefore, it may be very useful to establish a battery of basic structured interview questions that allow the clinician to probe the signs and symptoms of various eosinophilic multimorbidities. Each specialist should thoroughly examine the patient in order to detect the multimorbidities most frequently associated with their discipline, and maintain close contact with the specialists in the relevant specialties in each case ( Figure 2 ). Criteria for interconsultation between specialists should be defined depending on the final objective of these interconsultations and on the availability of appropriate techniques for EAD diagnosis, treatment and follow-up, as already defined in the context of some of the most characterized EADs in which the intervention of medical professional from different specialties is needed (186–188).
Figure 2.
Perspectives on the ideal pathway for the multidisciplinary management of eosinophilic diseases. CRSwNP, chronic rhinosinusitis with nasal polyps; EGPA, eosinophilic granulomatosis with polyangiitis; EoE, eosinophilic esophagitis; N-ERD, nonsteroidal anti-inflammatory drug-exacerbated respiratory disease; OME, otitis media with effusion.
3.2. Access to safe and effective therapies in the treatment of EADs
Patients with EADs should have access to safe and effective therapies (184), including specifically use of any of the different therapeutic alternatives available for the treatment of the multisystemic eosinophil-related manifestations that could occur concomitantly in a single individual. Beyond diagnosis, multidisciplinary management will ensure that a patient with eosinophilic multimorbidities can be treated with the best available therapeutic options. Particular consideration should be given to the biological therapies described above, the use of which is related with successful management of EADs, especially in patients with severe, difficult-to-treat EADs, in whom multiple different eosinophilic multimorbidities may occur. This is a scenario in which a personalized approach should prevail. Coordinated, comprehensive treatment of all manifestations of eosinophilic disorders using the appropriate therapy could provide great clinical benefits. Furthermore, it could potentially reduce the costs of care and treatment of these patients, who might otherwise receive different, possibly suboptimal interventions for each condition, if the aetiology common to each of the eosinophilic multimorbidities has not been properly analysed. Further considerations include indirect costs of care related to social and professional losses and a reduction in the QoL of inadequately treated patients.
3.3. Awareness and education about EADs
Awareness and education surrounding EADs should be strenuously promoted, especially among patients and the healthcare professionals who treat them (184). Both parties, and especially the latter, must also understand the benefits of multidisciplinary management. The patient must be the focal point in the management of the different multimorbid EADs and healthcare professionals involved in this management must accept the need, supported by scientific evidence, to collaborate with other specialists in certain cases, in order to achieve a holistic view of the patient with eosinophilic multimorbidities.
Healthcare professionals should also collaborate with patient associations to inform patients that they are entitled to multidisciplinary management and to ensure that they identify and report to the clinician any sign or symptom that could be associated with multimorbidities that present in association with the initially diagnosed EAD. Some of these diseases produce non-specific, long-term progressive symptoms to which the patient tends to adapt, resulting in many cases in delays before the patient seeks medical attention. In this respect, medical language will need to be adapted to facilitate patient awareness and understanding of the multidisciplinary pathway. Every patient with eosinophilic diseases should know that they may be treated by professionals from different medical areas who will be involved in the diagnosis and decision-making for optimal treatment of possible multimorbidities.
4. Conclusions
The evidence to date supports the idea that eosinophilia is a biomarker common to many diseases that present with T2 inflammation in different body systems. Biological therapies targeting eosinophils and their development, migration and activation in the tissues associated with the onset of EADs have led to a paradigm shift in the treatment of some of these diseases at the individual level. These drugs, therefore, could become, in the short-medium term, the preferred therapeutic approach in the simultaneous treatment of multimorbid diseases in which the eosinophil plays a pathogenic role. The interventions we describe here are simple and manageable in nature, but robust in effect. They will set us on a challenging path to a place where it will be possible to manage patients with EADs from a multidisciplinary perspective based on awareness and shared training in EADs and on collaboration between professionals from different medical specialties. There is little doubt that this approach will result in a significant benefit for patients with EADs.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Acknowledgments
Medical writing support was provided under the guidance of the authors by Javier Arranz-Nicolás, PhD, and Blanca Piedrafita, PhD, from Medical Statistics Consulting (MSC), Valencia, Spain, and was funded by AstraZeneca Spain, Madrid, Spain, in accordance with Good Publication Practice (GPP3) guidelines (Battisti, WP et al. Ann Intern Med. 2015).
Funding Statement
This study received funding from AstraZeneca. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of interest
Author SQ has received advisor’s and speaker’s honoraria from ALK, Allergy Therapeutics, AstraZeneca, GlaxoSmithKline, LETI Pharma, Novartis, Chiesi, Mundipharma, Teva, and Sanofi. Author BC has received advisor’s and speaker’s honoraria from AstraZeneca, GlaxoSmithKline, Chiesi, Menarini, Novartis, Teva, and Sanofi. Author RB has received advisor’s and speaker’s honoraria from AbbVie, Lilly, Pfizer, Roche, BMS, Janssen and MSD, and research funding from AbbVie, MSD, Lilly and Roche. Author JM has received advisor’s, consultant’s and speaker’s honoraria, and research funding, from AstraZeneca, Genentech-Roche, GSK, LETI, Menarini, MSD, Mitsubishi-Tanabe, NOUCOR/Uriach Group, Novartis, OPTINOSE, Proctor & Gamble, Regeneron Pharmaceuticals Inc., Sanofi-Genzyme, UCB Pharma, and Viatris/MEDA Pharma. Author CS has received consultant’s and trainer’s honoraria from Laborie/MMS, Medtronic Covidien AG, Menarini Consumer Healthcare, Doctaforum Medical Marketing S. L., ISOMED PHARMA S. L. and AstraZeneca and has received research funding from AstraZeneca, EsoCap Biotech, Regeneron Pharmaceuticals Inc., Celldex Therapeutics, Adare Pharmaceuticals Inc., and Dr. Falk Pharma GmbH. Author VP has received advisor’s and speaker´s honoraria, and research funding, from AstraZeneca and GlaxoSmithKline.
The remaining author declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Klion AD, Ackerman SJ, Bochner BS. Contributions of eosinophils to human health and disease. Annu Rev Pathol (2020) 15:179–209. doi: 10.1146/annurev-pathmechdis-012419-032756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bouffi C, Kartashov AV, Schollaert KL, Chen X, Bacon WC, Weirauch MT, et al. Transcription factor repertoire of homeostatic eosinophilopoiesis. J Immunol (2015) 195(6):2683–95. doi: 10.4049/jimmunol.1500510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dougan M, Dranoff G, Dougan SK. GM-CSF, IL-3, and IL-5 family of cytokines: regulators of inflammation. Immunity (2019) 50(4):796–811. doi: 10.1016/j.immuni.2019.03.022 [DOI] [PubMed] [Google Scholar]
- 4. Fulkerson PC. Transcription factors in eosinophil development and as therapeutic targets. Front Med (Lausanne) (2017) 4:115. doi: 10.3389/fmed.2017.00115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weller PF. Cytokine regulation of eosinophil function. Clin Immunol Immunopathol (1992) 62(1 Pt 2):S55–9. doi: 10.1016/0090-1229(92)90041-L [DOI] [PubMed] [Google Scholar]
- 6. Pelaia C, Paoletti G, Puggioni F, Racca F, Pelaia G, Canonica GW, et al. Interleukin-5 in the pathophysiology of severe asthma. Front Physiol (2019) 10:1514. doi: 10.3389/fphys.2019.01514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rothenberg ME, Hogan SP. The eosinophil. Annu Rev Immunol (2006) 24:147–74. doi: 10.1146/annurev.immunol.24.021605.090720 [DOI] [PubMed] [Google Scholar]
- 8. Kim HJ, Jung Y. The emerging role of eosinophils as multifunctional leukocytes in health and disease. Immune Netw (2020) 20(3):e24. doi: 10.4110/in.2020.20.e24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mitchell PD, O'Byrne PM. Epithelial-derived cytokines in asthma. Chest (2017) 151(6):1338–44. doi: 10.1016/j.chest.2016.10.042 [DOI] [PubMed] [Google Scholar]
- 10. Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med (2012) 18(5):716–25. doi: 10.1038/nm.2678 [DOI] [PubMed] [Google Scholar]
- 11. Weller PF, Spencer LA. Functions of tissue-resident eosinophils. Nat Rev Immunol (2017) 17(12):746–60. doi: 10.1038/nri.2017.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Carr TF, Berdnikovs S, Simon HU, Bochner BS, Rosenwasser LJ. Eosinophilic bioactivities in severe asthma. World Allergy Organ J (2016) 9:21. doi: 10.1186/s40413-016-0112-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Diny NL, Rose NR, Cihakova D. Eosinophils in autoimmune diseases. Front Immunol (2017) 8:484. doi: 10.3389/fimmu.2017.00484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fulkerson PC, Rothenberg ME. Targeting eosinophils in allergy, inflammation and beyond. Nat Rev Drug Discovery (2013) 12(2):117–29. doi: 10.1038/nrd3838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Furuta S, Iwamoto T, Nakajima H. Update on eosinophilic granulomatosis with polyangiitis. Allergol Int (2019) 68(4):430–6. doi: 10.1016/j.alit.2019.06.004 [DOI] [PubMed] [Google Scholar]
- 16. Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol (2015) 16(1):45–56. doi: 10.1038/ni.3049 [DOI] [PubMed] [Google Scholar]
- 17. Ramirez GA, Yacoub MR, Ripa M, Mannina D, Cariddi A, Saporiti N, et al. Eosinophils from physiology to disease: a comprehensive review. BioMed Res Int (2018) 2018:9095275. doi: 10.1155/2018/9095275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Trivedi SG, Lloyd CM. Eosinophils in the pathogenesis of allergic airways disease. Cell Mol Life Sci (2007) 64(10):1269–89. doi: 10.1007/s00018-007-6527-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Abdala-Valencia H, Coden ME, Chiarella SE, Jacobsen EA, Bochner BS, Lee JJ, et al. Shaping eosinophil identity in the tissue contexts of development, homeostasis, and disease. J Leukoc Biol (2018) 104(1):95–108. doi: 10.1002/JLB.1MR1117-442RR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jackson DJ, Akuthota P, Roufosse F. Eosinophils and eosinophilic immune dysfunction in health and disease. Eur Respir Rev (2022) 31(163):210150. doi: 10.1183/16000617.0150-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wechsler ME, Munitz A, Ackerman SJ, Drake MG, Jackson DJ, Wardlaw AJ, et al. Eosinophils in health and disease: a state-of-the-Art review. Mayo Clin Proc (2021) 96(10):2694–707. doi: 10.1016/j.mayocp.2021.04.025 [DOI] [PubMed] [Google Scholar]
- 22. Carnero Contentti E, Correale J. Neuromyelitis optica spectrum disorders: from pathophysiology to therapeutic strategies. J Neuroinflammation (2021) 18(1):208. doi: 10.1186/s12974-021-02249-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Costanza M. Type 2 inflammatory responses in autoimmune demyelination of the central nervous system: recent advances. J Immunol Res (2019) 2019:4204512. doi: 10.1155/2019/4204512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhang H, Verkman AS. Eosinophil pathogenicity mechanisms and therapeutics in neuromyelitis optica. J Clin Invest (2013) 123(5):2306–16. doi: 10.1172/JCI67554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tripodi L, Villa C, Molinaro D, Torrente Y, Farini A. The immune system in duchenne muscular dystrophy pathogenesis. Biomedicines (2021) 9(10):1447. doi: 10.3390/biomedicines9101447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kahn JE, Groh M, Lefèvre G. (A critical appraisal of) classification of hypereosinophilic disorders. Front Med (Lausanne) (2017) 4:216. doi: 10.3389/fmed.2017.00216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shomali W, Gotlib J. World health organization-defined eosinophilic disorders: 2019 update on diagnosis, risk stratification, and management. Am J Hematol (2019) 94(10):1149–67. doi: 10.1002/ajh.25617 [DOI] [PubMed] [Google Scholar]
- 28. Valent P, Klion AD, Roufosse F, Simon D, Metzgeroth G, Leiferman KM, et al. Proposed refined diagnostic criteria and classification of eosinophil disorders and related syndromes. Allergy (2023) 78(1):47–59. doi: 10.1111/all.15544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Agusti A, Fabbri LM, Singh D, Vestbo J, Celli B, Franssen FME, et al. Inhaled corticosteroids in COPD: friend or foe? Eur Respir J (2018) 52(6):1801219. doi: 10.1183/13993003.01219-2018 [DOI] [PubMed] [Google Scholar]
- 30. GOLD . Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. (2019). [Google Scholar]
- 31. Bain BJ. Review: eosinophils and eosinophilic leukemia. Clin Adv Hematol Oncol (2010) 8(12):901–3. [PubMed] [Google Scholar]
- 32. Curtis C, Ogbogu P. Hypereosinophilic syndrome. Clin Rev Allergy Immunol (2016) 50(2):240–51. doi: 10.1007/s12016-015-8506-7 [DOI] [PubMed] [Google Scholar]
- 33. Helbig G, Klion AD. Hypereosinophilic syndromes - an enigmatic group of disorders with an intriguing clinical spectrum and challenging treatment. Blood Rev (2021) 49:100809. doi: 10.1016/j.blre.2021.100809 [DOI] [PubMed] [Google Scholar]
- 34. Leiferman KM, Peters MS. Eosinophil-related disease and the skin. J Allergy Clin Immunol Pract (2018) 6(5):1462–82.e6. doi: 10.1016/j.jaip.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 35. Mattis DM, Wang SA, Lu CM. Contemporary classification and diagnostic evaluation of hypereosinophilia. Am J Clin Pathol (2020) 154(3):305–18. doi: 10.1093/ajcp/aqaa056 [DOI] [PubMed] [Google Scholar]
- 36. Valent P, Gleich GJ, Reiter A, Roufosse F, Weller PF, Hellmann A, et al. Pathogenesis and classification of eosinophil disorders: a review of recent developments in the field. Expert Rev Hematol (2012) 5(2):157–76. doi: 10.1586/ehm.11.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Valent P, Klion AD, Horny HP, Roufosse F, Gotlib J, Weller PF, et al. Contemporary consensus proposal on criteria and classification of eosinophilic disorders and related syndromes. J Allergy Clin Immunol (2012) 130(3):607–12.e9. doi: 10.1016/j.jaci.2012.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Felarca AB, Lowell FC. The total eosinophil count in a nonatopic population. J Allergy (1967) 40(1):16–20. doi: 10.1016/0021-8707(67)90055-X [DOI] [PubMed] [Google Scholar]
- 39. Mathur SK, Schwantes EA, Jarjour NN, Busse WW. Age-related changes in eosinophil function in human subjects. Chest (2008) 133(2):412–9. doi: 10.1378/chest.07-2114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Toledo-Pons N, van Boven JFM, Muncunill J, Millán A, Román-Rodríguez M, López-Andrade B, et al. Impact of blood eosinophil variability in asthma: a real-life population study. Ann Am Thorac Soc (2022) 19(3):407–14. doi: 10.1513/AnnalsATS.202103-409OC [DOI] [PubMed] [Google Scholar]
- 41. Nelson RK, Bush A, Stokes J, Nair P, Akuthota P. Eosinophilic asthma. J Allergy Clin Immunol Pract (2020) 8(2):465–73. doi: 10.1016/j.jaip.2019.11.024 [DOI] [PubMed] [Google Scholar]
- 42. Reddel HK, Bacharier LB, Bateman ED, Brightling CE, Brusselle GG, Buhl R, et al. Global initiative for asthma strategy 2021: executive summary and rationale for key changes. J Allergy Clin Immunol Pract (2022) 10(1S):S1–S18. doi: 10.1111/resp.14174 [DOI] [PubMed] [Google Scholar]
- 43. Sonnenberg GF, Hepworth MR. Functional interactions between innate lymphoid cells and adaptive immunity. Nat Rev Immunol (2019) 19(10):599–613. doi: 10.1038/s41577-019-0194-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Amat F, Labbé A. Biomarkers for severe allergic asthma in children: could they be useful to guide disease control and use of omalizumab? Expert Rev Respir Med (2018) 12(6):475–82. doi: 10.1080/17476348.2018.1475233 [DOI] [PubMed] [Google Scholar]
- 45. Lee YJ, Fujisawa T, Kim CK. Biomarkers for recurrent wheezing and asthma in preschool children. Allergy Asthma Immunol Res (2019) 11(1):16–28. doi: 10.4168/aair.2019.11.1.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rufo J, Taborda-Barata L, Lourenço O. Serum biomarkers in elderly asthma. J Asthma (2013) 50(10):1011–9. doi: 10.3109/02770903.2013.834932 [DOI] [PubMed] [Google Scholar]
- 47. Franceschi E, Drick N, Fuge J, Welte T, Suhling H. Eosinophilic cationic protein as marker for response to antibody therapy in severe asthma. ERJ Open Res (2022) 8(3):00138–2022. doi: 10.1183/23120541.00138-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Russell RJ, Brightling C. Pathogenesis of asthma: implications for precision medicine. Clin Sci (Lond) (2017) 131(14):1723–35. doi: 10.1042/CS20160253 [DOI] [PubMed] [Google Scholar]
- 49. Staudacher AG, Peters AT, Kato A, Stevens WW. Use of endotypes, phenotypes, and inflammatory markers to guide treatment decisions in chronic rhinosinusitis. Ann Allergy Asthma Immunol (2020) 124(4):318–25. doi: 10.1016/j.anai.2020.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Stevens WW, Peters AT, Tan BK, Klingler AI, Poposki JA, Hulse KE, et al. Associations between inflammatory endotypes and clinical presentations in chronic rhinosinusitis. J Allergy Clin Immunol Pract (2019) 7(8):2812–20.e3. doi: 10.1016/j.jaip.2019.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ardehali MM, Amali A, Bakhshaee M, Madani Z, Amiri M. The comparison of histopathological characteristics of polyps in asthmatic and nonasthmatic patients. Otolaryngol Head Neck Surg (2009) 140(5):748–51. doi: 10.1016/j.otohns.2009.01.027 [DOI] [PubMed] [Google Scholar]
- 52. Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. Executive summary of EPOS 2020 including integrated care pathways. Rhinology (2020) 58(2):82–111. doi: 10.4193/Rhin20.601 [DOI] [PubMed] [Google Scholar]
- 53. Gelardi M, Fiorella R, Fiorella ML, Russo C, Soleti P, Ciprandi G. Nasal-sinus polyposis: clinical-cytological grading and prognostic index of relapse. J Biol Regul Homeost Agents (2009) 23(3):181–8. [PubMed] [Google Scholar]
- 54. Laidlaw TM, Mullol J, Woessner KM, Amin N, Mannent LP. Chronic rhinosinusitis with nasal polyps and asthma. J Allergy Clin Immunol Pract (2021) 9(3):1133–41. doi: 10.1016/j.jaip.2020.09.063 [DOI] [PubMed] [Google Scholar]
- 55. Sanchez-Collado I, Mora T, Munoz-Cano R, Ribo P, Mullol J, Valero A. Prevalence of chronic rhinosinusitis with nasal polyps in Catalonia (Spain): a retrospective, large-scale population-based study. Rhinology (2022) 60(5):384–96. doi: 10.4193/Rhin21.364 [DOI] [PubMed] [Google Scholar]
- 56. Kowalski ML, Agache I, Bavbek S, Bakirtas A, Blanca M, Bochenek G, et al. Diagnosis and management of NSAID-exacerbated respiratory disease (N-ERD)-a EAACI position paper. Allergy (2019) 74(1):28–39. doi: 10.1111/all.13599 [DOI] [PubMed] [Google Scholar]
- 57. Mullol J, Boyce J, Dahlen SE, Dahlen B, Picado C, Bobolea I. Eicosanoid dysregulation and type 2 inflammation in AERD. J Allergy Clin Immunol (2021) 148(5):1157–60. doi: 10.1016/j.jaci.2021.08.015 [DOI] [PubMed] [Google Scholar]
- 58. Naclerio R, Mullol J, Stevens WW. A decade of clinical advances in chronic rhinosinusitis: 2012-2022. J Allergy Clin Immunol Pract (2023) 11(1):43–50. doi: 10.1016/j.jaip.2022.10.030 [DOI] [PubMed] [Google Scholar]
- 59. Alobid I, Colás C, Castillo JA, Arismendi E, Del Cuvillo A, Gómez-Outes A, et al. Spanish Consensus on the management of chronic rhinosinusitis with nasal polyps (POLIposis NAsal / POLINA 2.0). J Investig Allergol Clin Immunol (2023) 18:0. doi: 10.18176/jiaci.0910 [DOI] [PubMed] [Google Scholar]
- 60. Takabayashi T, Schleimer RP. Formation of nasal polyps: the roles of innate type 2 inflammation and deposition of fibrin. J Allergy Clin Immunol (2020) 145(3):740–50. doi: 10.1016/j.jaci.2020.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Tokunaga T, Sakashita M, Haruna T, Asaka D, Takeno S, Ikeda H, et al. Novel scoring system and algorithm for classifying chronic rhinosinusitis: the JESREC study. Allergy (2015) 70(8):995–1003. doi: 10.1111/all.12644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Cosio BG, Perez de Llano L, Lopez Vina A, Torrego A, Lopez-Campos JL, Soriano JB, et al. Th-2 signature in chronic airway diseases: towards the extinction of asthma-COPD overlap syndrome? Eur Respir J (2017) 49(5):1602397. doi: 10.1183/13993003.02397-2016 [DOI] [PubMed] [Google Scholar]
- 63. de Llano LP, Cosio BG, Iglesias A, de Las Cuevas N, Soler-Cataluna JJ, Izquierdo JL, et al. Mixed Th2 and non-Th2 inflammatory pattern in the asthma-COPD overlap: a network approach. Int J Chron Obstruct Pulmon Dis (2018) 13:591–601. doi: 10.2147/COPD.S153694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Postma DS, Rabe KF. The asthma-COPD overlap syndrome. N Engl J Med (2015) 373(13):1241–9. doi: 10.1056/NEJMra1411863 [DOI] [PubMed] [Google Scholar]
- 65. Price DB, Rigazio A, Campbell JD, Bleecker ER, Corrigan CJ, Thomas M, et al. Blood eosinophil count and prospective annual asthma disease burden: a UK cohort study. Lancet Respir Med (2015) 3(11):849–58. doi: 10.1016/S2213-2600(15)00367-7 [DOI] [PubMed] [Google Scholar]
- 66. Singh D, Kolsum U, Brightling CE, Locantore N, Agusti A, Tal-Singer R, et al. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J (2014) 44(6):1697–700. doi: 10.1183/09031936.00162414 [DOI] [PubMed] [Google Scholar]
- 67. Miravitlles M, Calle M, Molina J, Almagro P, Gomez JT, Trigueros JA, et al. Spanish COPD guidelines (GesEPOC) 2021: updated pharmacological treatment of stable COPD. Arch Bronconeumol (2022) 58(1):69–81. doi: 10.1016/j.arbres.2021.03.005 [DOI] [PubMed] [Google Scholar]
- 68. Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J (2019) 53(5):1900164. doi: 10.1183/13993003.00164-2019 [DOI] [PubMed] [Google Scholar]
- 69.2023 GINA report, Global strategy for asthma management and prevention. (2023). [Google Scholar]
- 70. Soler-Cataluña JJ, Cosío B, Izquierdo JL, López-Campos JL, Marín JM, Agüero R, et al. Consensus document on the overlap phenotype COPD–asthma in COPD. Archivos Bronconeumología (2012) 48(9):331–7. doi: 10.1016/j.arbr.2012.06.017 [DOI] [PubMed] [Google Scholar]
- 71. Toledo-Pons N, van Boven JFM, Roman-Rodriguez M, Perez N, Valera Felices JL, Soriano JB, et al. ACO: time to move from the description of different phenotypes to the treatable traits. PloS One (2019) 14(1):e0210915. doi: 10.1371/journal.pone.0210915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Nestle FO, Di Meglio P, Qin JZ, Nickoloff BJ. Skin immune sentinels in health and disease. Nat Rev Immunol (2009) 9(10):679–91. doi: 10.1038/nri2622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Robert C, Kupper TS. Inflammatory skin diseases, T cells, and immune surveillance. N Engl J Med (1999) 341(24):1817–28. doi: 10.1056/NEJM199912093412407 [DOI] [PubMed] [Google Scholar]
- 74. Streilein JW. Skin-associated lymphoid tissues (SALT): origins and functions. J Invest Dermatol (1983) 80(Suppl):12s–6s. doi: 10.1111/1523-1747.ep12536743 [DOI] [PubMed] [Google Scholar]
- 75. Akdis CA, Akdis M, Bieber T, Bindslev-Jensen C, Boguniewicz M, Eigenmann P, et al. Diagnosis and treatment of atopic dermatitis in children and adults: European academy of allergology and clinical Immunology/American academy of allergy, asthma and Immunology/PRACTALL consensus report. Allergy (2006) 61(8):969–87. doi: 10.1111/j.1398-9995.2006.01153.x [DOI] [PubMed] [Google Scholar]
- 76. Akdis CA, Arkwright PD, Bruggen MC, Busse W, Gadina M, Guttman-Yassky E, et al. Type 2 immunity in the skin and lungs. Allergy (2020) 75(7):1582–605. doi: 10.1111/all.14318 [DOI] [PubMed] [Google Scholar]
- 77. Genovese G, Di Zenzo G, Cozzani E, Berti E, Cugno M, Marzano AV. New insights into the pathogenesis of bullous pemphigoid: 2019 update. Front Immunol (2019) 10:1506. doi: 10.3389/fimmu.2019.01506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Engmann J, Rudrich U, Behrens G, Papakonstantinou E, Gehring M, Kapp A, et al. Increased activity and apoptosis of eosinophils in blister fluids, skin and peripheral blood of patients with bullous pemphigoid. Acta Derm Venereol (2017) 97(4):464–71. doi: 10.2340/00015555-2581 [DOI] [PubMed] [Google Scholar]
- 79. Ishiura N, Fujimoto M, Watanabe R, Nakashima H, Kuwano Y, Yazawa N, et al. Serum levels of IgE anti-BP180 and anti-BP230 autoantibodies in patients with bullous pemphigoid. J Dermatol Sci (2008) 49(2):153–61. doi: 10.1016/j.jdermsci.2007.08.008 [DOI] [PubMed] [Google Scholar]
- 80. Simon D, Borradori L, Simon HU. Eosinophils as putative therapeutic targets in bullous pemphigoid. Exp Dermatol (2017) 26(12):1187–92. doi: 10.1111/exd.13416 [DOI] [PubMed] [Google Scholar]
- 81. Tsuda S, Miyasato M, Iryo K, Nakama T, Kato K, Sasai Y. Eosinophil phenotypes in bullous pemphigoid. J Dermatol (1992) 19(5):270–9. doi: 10.1111/j.1346-8138.1992.tb03224.x [DOI] [PubMed] [Google Scholar]
- 82. Messingham KN, Crowe TP, Fairley JA. The intersection of IgE autoantibodies and eosinophilia in the pathogenesis of bullous pemphigoid. Front Immunol (2019) 10:2331. doi: 10.3389/fimmu.2019.02331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Kay AB, Ying S, Ardelean E, Mlynek A, Kita H, Clark P, et al. Elevations in vascular markers and eosinophils in chronic spontaneous urticarial weals with low-level persistence in uninvolved skin. Br J Dermatol (2014) 171(3):505–11. doi: 10.1111/bjd.12991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Zuberbier T, Abdul Latiff AH, Abuzakouk M, Aquilina S, Asero R, Baker D, et al. The international EAACI/GA(2)LEN/EuroGuiDerm/APAAACI guideline for the definition, classification, diagnosis, and management of urticaria. Allergy (2022) 77(3):734–66. doi: 10.1111/all.15090 [DOI] [PubMed] [Google Scholar]
- 85. Kolkhir P, Altrichter S, Munoz M, Hawro T, Maurer M. New treatments for chronic urticaria. Ann Allergy Asthma Immunol (2020) 124(1):2–12. doi: 10.1016/j.anai.2019.08.014 [DOI] [PubMed] [Google Scholar]
- 86. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheum (2013) 65(1):1–11. doi: 10.1002/art.37715 [DOI] [PubMed] [Google Scholar]
- 87. Nair P, Ochkur SI, Protheroe C, Simms E, Lee NA, Lee JJ. The identification of eosinophilic gastroenteritis in prednisone-dependent eosinophilic bronchitis and asthma. Allergy Asthma Clin Immunol (2011) 7(1):4. doi: 10.1186/1710-1492-7-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Pagnoux C. Updates in ANCA-associated vasculitis. Eur J Rheumatol (2016) 3(3):122–33. doi: 10.5152/eurjrheum.2015.0043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Protheroe C, Woodruff SA, de Petris G, Mukkada V, Ochkur SI, Janarthanan S, et al. A novel histologic scoring system to evaluate mucosal biopsies from patients with eosinophilic esophagitis. Clin Gastroenterol Hepatol (2009) 7(7):749–55.e11. doi: 10.1016/j.cgh.2009.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Al-Hussain T, Hussein MH, Conca W, Al Mana H, Akhtar M. Pathophysiology of ANCA-associated vasculitis. Adv Anat Pathol (2017) 24(4):226–34. doi: 10.1097/PAP.0000000000000154 [DOI] [PubMed] [Google Scholar]
- 91. Fagni F, Bello F, Emmi G. Eosinophilic granulomatosis with polyangiitis: dissecting the pathophysiology. Front Med (Lausanne) (2021) 8:627776. doi: 10.3389/fmed.2021.627776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Masi AT, Hunder GG, Lie JT, Michel BA, Bloch DA, Arend WP, et al. The American college of rheumatology 1990 criteria for the classification of churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheumatol (1990) 33(8):1094–100. doi: 10.1002/art.1780330806 [DOI] [PubMed] [Google Scholar]
- 93. Khoury P, Makiya M, Klion AD. Clinical and biological markers in hypereosinophilic syndromes. Front Med (Lausanne) (2017) 4:240. doi: 10.3389/fmed.2017.00240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Stella S, Massimino M, Manzella L, Pennisi MS, Tirro E, Romano C, et al. Molecular pathogenesis and treatment perspectives for hypereosinophilia and hypereosinophilic syndromes. Int J Mol Sci (2021) 22(2):486. doi: 10.3390/ijms22020486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Dellon ES, Gonsalves N, Abonia JP, Alexander JA, Arva NC, Atkins D, et al. International consensus recommendations for eosinophilic gastrointestinal disease nomenclature. Clin Gastroenterol Hepatol (2022) 20(11):2474–84.e3. doi: 10.1016/j.cgh.2022.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Shaheen NJ, Mukkada V, Eichinger CS, Schofield H, Todorova L, Falk GW. Natural history of eosinophilic esophagitis: a systematic review of epidemiology and disease course. Dis Esophagus (2018) 31(8):doy015. doi: 10.1093/dote/doy015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Collins MH. Histopathologic features of eosinophilic esophagitis and eosinophilic gastrointestinal diseases. Gastroenterol Clin North Am (2014) 43(2):257–68. doi: 10.1016/j.gtc.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 98. Collins MH. Histopathology of eosinophilic esophagitis. Dig Dis (2014) 32(1-2):68–73. doi: 10.1159/000357012 [DOI] [PubMed] [Google Scholar]
- 99. Buhl R, Humbert M, Bjermer L, Chanez P, Heaney LG, Pavord I, et al. Severe eosinophilic asthma: a roadmap to consensus. Eur Respir J (2017) 49(5):1700634. doi: 10.1183/13993003.00634-2017 [DOI] [PubMed] [Google Scholar]
- 100. Green RH, Brightling CE, McKenna S, Hargadon B, Parker D, Bradding P, et al. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet (2002) 360(9347):1715–21. doi: 10.1016/S0140-6736(02)11679-5 [DOI] [PubMed] [Google Scholar]
- 101. Perez de Llano L, Miravitlles M, Golpe R, Alvarez-Gutierrez FJ, Cisneros C, Almonacid C, et al. A proposed approach to chronic airway disease (CAD) using therapeutic goals and treatable traits: a look to the future. Int J Chron Obstruct Pulmon Dis (2020) 15:2091–100. doi: 10.2147/COPD.S263430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Petsky HL, Cates CJ, Kew KM, Chang AB. Tailoring asthma treatment on eosinophilic markers (exhaled nitric oxide or sputum eosinophils): a systematic review and meta-analysis. Thorax (2018) 73(12):1110–9. doi: 10.1136/thoraxjnl-2018-211540 [DOI] [PubMed] [Google Scholar]
- 103. Plaza V, Alobid I, Alvarez C, Blanco M, Ferreira J, Garcia G, et al. Spanish Asthma management guidelines (GEMA) VERSION 5.1. highlights and controversies. Arch Bronconeumol (2022) 58(2):150–8. doi: 10.1016/j.arbres.2021.05.010 [DOI] [PubMed] [Google Scholar]
- 104. Wenzel SE. Asthma: defining of the persistent adult phenotypes. Lancet (2006) 368(9537):804–13. doi: 10.1016/S0140-6736(06)69290-8 [DOI] [PubMed] [Google Scholar]
- 105. Chen YL, Gutowska-Owsiak D, Hardman CS, Westmoreland M, MacKenzie T, Cifuentes L, et al. Proof-of-concept clinical trial of etokimab shows a key role for IL-33 in atopic dermatitis pathogenesis. Sci Transl Med (2019) 11(515):eaax2945. doi: 10.1126/scitranslmed.aax2945 [DOI] [PubMed] [Google Scholar]
- 106. Farnaghi F, Ehsani AH, Kamyab-Hesary K, Abbasian S, Seirafi H, Nasimi M. Correlation of dermal and blood eosinophilia with bullous pemphigoid disease severity. Int J Womens Dermatol (2020) 6(3):171–5. doi: 10.1016/j.ijwd.2020.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Gore Karaali M, Koku Aksu AE, Cin M, Leblebici C, Kara Polat A, Gurel MS. Tissue eosinophil levels as a marker of disease severity in bullous pemphigoid. Australas J Dermatol (2021) 62(2):e236–e41. doi: 10.1111/ajd.13547 [DOI] [PubMed] [Google Scholar]
- 108. Maintz L, Welchowski T, Herrmann N, Brauer J, Klaschen AS, Fimmers R, et al. Machine learning-based deep phenotyping of atopic dermatitis: severity-associated factors in adolescent and adult patients. JAMA Dermatol (2021) 157(12):1414–24. doi: 10.1001/jamadermatol.2021.3668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Morishima Y, Kawashima H, Takekuma K, Hoshika A. Changes in serum lactate dehydrogenase activity in children with atopic dermatitis. Pediatr Int (2010) 52(2):171–4. doi: 10.1111/j.1442-200X.2009.02908.x [DOI] [PubMed] [Google Scholar]
- 110. Raap U, Weissmantel S, Gehring M, Eisenberg AM, Kapp A, Folster-Holst R. IL-31 significantly correlates with disease activity and Th2 cytokine levels in children with atopic dermatitis. Pediatr Allergy Immunol (2012) 23(3):285–8. doi: 10.1111/j.1399-3038.2011.01241.x [DOI] [PubMed] [Google Scholar]
- 111. Ungar B, Garcet S, Gonzalez J, Dhingra N, Correa da Rosa J, Shemer A, et al. An integrated model of atopic dermatitis biomarkers highlights the systemic nature of the disease. J Invest Dermatol (2017) 137(3):603–13. doi: 10.1016/j.jid.2016.09.037 [DOI] [PubMed] [Google Scholar]
- 112. Wu KG, Li TH, Chen CJ, Cheng HI, Wang TY. Correlations of serum interleukin-16, total IgE, eosinophil cationic protein and total eosinophil counts with disease activity in children with atopic dermatitis. Int J Immunopathol Pharmacol (2011) 24(1):15–23. doi: 10.1177/039463201102400103 [DOI] [PubMed] [Google Scholar]
- 113. Bafadhel M, Peterson S, De Blas MA, Calverley PM, Rennard SI, Richter K, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med (2018) 6(2):117–26. doi: 10.1016/S2213-2600(18)30006-7 [DOI] [PubMed] [Google Scholar]
- 114. Brightling CE, McKenna S, Hargadon B, Birring S, Green R, Siva R, et al. Sputum eosinophilia and the short term response to inhaled mometasone in chronic obstructive pulmonary disease. Thorax (2005) 60(3):193–8. doi: 10.1136/thx.2004.032516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Cottin V, Bel E, Bottero P, Dalhoff K, Humbert M, Lazor R, et al. Respiratory manifestations of eosinophilic granulomatosis with polyangiitis (Churg-Strauss). Eur Respir J (2016) 48(5):1429–41. doi: 10.1183/13993003.00097-2016 [DOI] [PubMed] [Google Scholar]
- 116. de Groot JC, Storm H, Amelink M, de Nijs SB, Eichhorn E, Reitsma BH, et al. Clinical profile of patients with adult-onset eosinophilic asthma. ERJ Open Res (2016) 2(2):00100–2015. doi: 10.1183/23120541.00100-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. European Position paper on rhinosinusitis and nasal polyps 2020. Rhinology (2020) 58(Suppl S29):1–464. doi: 10.4193/Rhin20.600 [DOI] [PubMed] [Google Scholar]
- 118. Pascoe S, Barnes N, Brusselle G, Compton C, Criner GJ, Dransfield MT, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med (2019) 7(9):745–56. doi: 10.1016/S2213-2600(19)30190-0 [DOI] [PubMed] [Google Scholar]
- 119. Sinico RA, Bottero P. Churg-Strauss angiitis. Best Pract Res Clin Rheumatol (2009) 23(3):355–66. doi: 10.1016/j.berh.2009.02.004 [DOI] [PubMed] [Google Scholar]
- 120. Dragonieri S, Carpagnano GE. Biological therapy for severe asthma. Asthma Res Practice (2021) 7(1):12. doi: 10.1186/s40733-021-00078-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Tan LD, Nguyen N, Alismail A, Castro M. Management of uncontrolled asthma: a framework for novel and legacy biologic treatments. J Asthma Allergy (2022) 15:875–83. doi: 10.2147/JAA.S369836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Brusselle GG, Koppelman GH. Biologic therapies for severe asthma. N Engl J Med (2022) 386(2):157–71. doi: 10.1056/NEJMra2032506 [DOI] [PubMed] [Google Scholar]
- 123. Brusselle G, Bracke K. Targeting immune pathways for therapy in asthma and chronic obstructive pulmonary disease. Ann Am Thorac Soc (2014) 11 Suppl 5:S322–8. doi: 10.1513/AnnalsATS.201403-118AW [DOI] [PubMed] [Google Scholar]
- 124. FitzGerald JM, Bleecker ER, Nair P, Korn S, Ohta K, Lommatzsch M, et al. Benralizumab, an anti-interleukin-5 receptor alpha monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet (2016) 388(10056):2128–41. doi: 10.1016/S0140-6736(16)31322-8 [DOI] [PubMed] [Google Scholar]
- 125. Laorden D, Romero D, Dominguez-Ortega J. Benralizumab in eosinophilic granulomatosis with polyangiitis. Med Clin (Barc) (2022) 158(9):441–2. doi: 10.1016/j.medcli.2021.07.017 [DOI] [PubMed] [Google Scholar]
- 126. Chaia G, Martín U, Cortés-Telles A, Morett F, Gutiérrez-Mujica J, Zepeda-Gómez A, et al. Benralizumab: efficacy and safety in patients with severe eosinophilic asthma. Rev Alergia Mexico (2020) 67:59–82. doi: 10.29262/ram.v67i7.807 [DOI] [Google Scholar]
- 127. Goldman M, Hirsch I, Zangrilli JG, Newbold P, Xu X. The association between blood eosinophil count and benralizumab efficacy for patients with severe, uncontrolled asthma: subanalyses of the phase III SIROCCO and CALIMA studies. Curr Med Res Opin (2017) 33(9):1605–13. doi: 10.1080/03007995.2017.1347091 [DOI] [PubMed] [Google Scholar]
- 128. Diver S, Khalfaoui L, Emson C, Wenzel SE, Menzies-Gow A, Wechsler ME, et al. Effect of tezepelumab on airway inflammatory cells, remodelling, and hyperresponsiveness in patients with moderate-to-severe uncontrolled asthma (CASCADE): a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir Med (2021) 9(11):1299–312. doi: 10.1016/S2213-2600(21)00226-5 [DOI] [PubMed] [Google Scholar]
- 129. Menzies-Gow A, Corren J, Bourdin A, Chupp G, Israel E, Wechsler ME, et al. Tezepelumab in adults and adolescents with severe, uncontrolled asthma. N Engl J Med (2021) 384(19):1800–9. doi: 10.1056/NEJMoa2034975 [DOI] [PubMed] [Google Scholar]
- 130. Bel EH, Wenzel SE, Thompson PJ, Prazma CM, Keene ON, Yancey SW, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med (2014) 371(13):1189–97. doi: 10.1056/NEJMoa1403291 [DOI] [PubMed] [Google Scholar]
- 131. Nair P, Bardin P, Humbert M, Murphy KR, Hickey L, Garin M, et al. Efficacy of intravenous reslizumab in oral corticosteroid-dependent asthma. J Allergy Clin Immunol Pract (2020) 8(2):555–64. doi: 10.1016/j.jaip.2019.09.036 [DOI] [PubMed] [Google Scholar]
- 132. Nair P, Wenzel S, Rabe KF, Bourdin A, Lugogo NL, Kuna P, et al. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med (2017) 376(25):2448–58. doi: 10.1056/NEJMoa1703501 [DOI] [PubMed] [Google Scholar]
- 133. Bjermer L, Lemiere C, Maspero J, Weiss S, Zangrilli J, Germinaro M. Reslizumab for inadequately controlled asthma with elevated blood eosinophil levels: a randomized phase 3 study. Chest (2016) 150(4):789–98. doi: 10.1016/j.chest.2016.03.032 [DOI] [PubMed] [Google Scholar]
- 134. Buhl R, Bel E, Bourdin A, Davila I, Douglass JA, FitzGerald JM, et al. Effective management of severe asthma with biologic medications in adult patients: a literature review and international expert opinion. J Allergy Clin Immunol Pract (2022) 10(2):422–32. doi: 10.1016/j.jaip.2021.10.059 [DOI] [PubMed] [Google Scholar]
- 135. Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet (2012) 380(9842):651–9. doi: 10.1016/S0140-6736(12)60988-X [DOI] [PubMed] [Google Scholar]
- 136. Bachert C, Han JK, Desrosiers MY, Gevaert P, Heffler E, Hopkins C, et al. Efficacy and safety of benralizumab in chronic rhinosinusitis with nasal polyps: a randomized, placebo-controlled trial. J Allergy Clin Immunol (2022) 149(4):1309–17.e12. doi: 10.1016/j.jaci.2021.08.030 [DOI] [PubMed] [Google Scholar]
- 137. Fokkens WJ, Mullol J, Kennedy D, Philpott C, Seccia V, Kern RC, et al. Mepolizumab for chronic rhinosinusitis with nasal polyps (SYNAPSE): in-depth sinus surgery analysis. Allergy (2023) 78(3):812–21. doi: 10.1111/all.15434 [DOI] [PubMed] [Google Scholar]
- 138. Han JK, Bachert C, Fokkens W, Desrosiers M, Wagenmann M, Lee SE, et al. Mepolizumab for chronic rhinosinusitis with nasal polyps (SYNAPSE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir Med (2021) 9(10):1141–53. doi: 10.1016/S2213-2600(21)00097-7 [DOI] [PubMed] [Google Scholar]
- 139. Hopkins C, Han JK, Lund VJ, Bachert C, Fokkens WJ, Diamant Z, et al. Evaluating treatment response to mepolizumab in patients with severe CRSwNP. Rhinology (2023) 61(2):108–17. doi: 10.4193/Rhin22.200 [DOI] [PubMed] [Google Scholar]
- 140. Bachert C, Han JK, Desrosiers M, Hellings PW, Amin N, Lee SE, et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet (2019) 394(10209):1638–50. doi: 10.1016/S0140-6736(19)31881-1 [DOI] [PubMed] [Google Scholar]
- 141. Bachert C, Mannent L, Naclerio RM, Mullol J, Ferguson BJ, Gevaert P, et al. Effect of subcutaneous dupilumab on nasal polyp burden in patients with chronic sinusitis and nasal polyposis: a randomized clinical trial. JAMA (2016) 315(5):469–79. doi: 10.1001/jama.2015.19330 [DOI] [PubMed] [Google Scholar]
- 142. Fujieda S, Matsune S, Takeno S, Ohta N, Asako M, Bachert C, et al. Dupilumab efficacy in chronic rhinosinusitis with nasal polyps from SINUS-52 is unaffected by eosinophilic status. Allergy (2022) 77(1):186–96. doi: 10.1111/all.14906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Hopkins C, Wagenmann M, Bachert C, Desrosiers M, Han JK, Hellings PW, et al. Efficacy of dupilumab in patients with a history of prior sinus surgery for chronic rhinosinusitis with nasal polyps. Int Forum Allergy Rhinol (2021) 11(7):1087–101. doi: 10.1002/alr.22780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Damask C, Chen M, Holweg CTJ, Yoo B, Millette LA, Franzese C. Defining the efficacy of omalizumab in nasal polyposis: a POLYP 1 and POLYP 2 subgroup analysis. Am J Rhinol Allergy (2022) 36(1):135–41. doi: 10.1177/19458924211030486 [DOI] [PubMed] [Google Scholar]
- 145. Gevaert P, Omachi TA, Corren J, Mullol J, Han J, Lee SE, et al. Efficacy and safety of omalizumab in nasal polyposis: 2 randomized phase 3 trials. J Allergy Clin Immunol (2020) 146(3):595–605. doi: 10.1016/j.jaci.2020.05.032 [DOI] [PubMed] [Google Scholar]
- 146. Hayashi H, Fukutomi Y, Mitsui C, Kajiwara K, Watai K, Kamide Y, et al. Omalizumab for aspirin hypersensitivity and leukotriene overproduction in aspirin-exacerbated respiratory disease. A Randomized Controlled Trial Am J Respir Crit Care Med (2020) 201(12):1488–98. doi: 10.1164/rccm.201906-1215OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Tiotiu A, Oster JP, Roux PR, Nguyen Thi PL, Peiffer G, Bonniaud P, et al. Effectiveness of omalizumab in severe allergic asthma and nasal polyposis: a real-life study. J Investig Allergol Clin Immunol (2020) 30(1):49–57. doi: 10.18176/jiaci.0391 [DOI] [PubMed] [Google Scholar]
- 148. Busse WW. Dupilumab and eosinophils: a red flag? J Allergy Clin Immunol Pract (2022) 10(10):2710–2. doi: 10.1016/j.jaip.2022.08.006 [DOI] [PubMed] [Google Scholar]
- 149. Olaguibel JM, Sastre J, Rodríguez JM, Del Pozo V. Eosinophilia induced by blocking the IL-4/IL-13 pathway: potential mechanisms and clinical outcomes. J Investig Allergol Clin Immunol (2022) 32(3):165–80. doi: 10.18176/jiaci.0823 [DOI] [PubMed] [Google Scholar]
- 150. Bachert C, Sousa AR, Han JK, Schlosser RJ, Sowerby LJ, Hopkins C, et al. Mepolizumab for chronic rhinosinusitis with nasal polyps: treatment efficacy by comorbidity and blood eosinophil count. J Allergy Clin Immunol (2022) 149(5):1711–21.e6. doi: 10.1016/j.jaci.2021.10.040 [DOI] [PubMed] [Google Scholar]
- 151. Brightling CE, Bleecker ER, Panettieri RA, Jr., Bafadhel M, She D, Ward CK, et al. Benralizumab for chronic obstructive pulmonary disease and sputum eosinophilia: a randomised, double-blind, placebo-controlled, phase 2a study. Lancet Respir Med (2014) 2(11):891–901. doi: 10.1016/S2213-2600(14)70187-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Criner GJ, Celli BR, Brightling CE, Agusti A, Papi A, Singh D, et al. Benralizumab for the prevention of COPD exacerbations. N Engl J Med (2019) 381(11):1023–34. doi: 10.1056/NEJMoa1905248 [DOI] [PubMed] [Google Scholar]
- 153. Pavord ID, Chanez P, Criner GJ, Kerstjens HAM, Korn S, Lugogo N, et al. Mepolizumab for eosinophilic chronic obstructive pulmonary disease. N Engl J Med (2017) 377(17):1613–29. doi: 10.1056/NEJMoa1708208 [DOI] [PubMed] [Google Scholar]
- 154. Lucendo AJ, Molina-Infante J, Arias A, von Arnim U, Bredenoord AJ, Bussmann C, et al. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United Eur Gastroenterol J (2017) 5(3):335–58. doi: 10.1177/2050640616689525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Greuter T, Hirano I, Dellon ES. Emerging therapies for eosinophilic esophagitis. J Allergy Clin Immunol (2020) 145(1):38–45. doi: 10.1016/j.jaci.2019.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Kuang FL, Legrand F, Makiya M, Ware J, Wetzler L, Brown T, et al. Benralizumab for PDGFRA-negative hypereosinophilic syndrome. N Engl J Med (2019) 380(14):1336–46. doi: 10.1056/NEJMoa1812185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Foroughi S, Foster B, Kim N, Bernardino LB, Scott LM, Hamilton RG, et al. Anti-IgE treatment of eosinophil-associated gastrointestinal disorders. J Allergy Clin Immunol (2007) 120(3):594–601. doi: 10.1016/j.jaci.2007.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Dellon ES, Peterson KA, Murray JA, Falk GW, Gonsalves N, Chehade M, et al. Anti-Siglec-8 antibody for eosinophilic gastritis and duodenitis. N Engl J Med (2020) 383(17):1624–34. doi: 10.1056/NEJMoa2012047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Jeong K, Kim M, Jeon SA, Kim YH, Lee S. A randomized trial of lactobacillus rhamnosus IDCC 3201 tyndallizate (RHT3201) for treating atopic dermatitis. Pediatr Allergy Immunol (2020) 31(7):783–92. doi: 10.1111/pai.13269 [DOI] [PubMed] [Google Scholar]
- 160. Cheung PF, Wong CK, Ho AW, Hu S, Chen DP, Lam CW. Activation of human eosinophils and epidermal keratinocytes by Th2 cytokine IL-31: implication for the immunopathogenesis of atopic dermatitis. Int Immunol (2010) 22(6):453–67. doi: 10.1093/intimm/dxq027 [DOI] [PubMed] [Google Scholar]
- 161. Kabashima K, Matsumura T, Komazaki H, Kawashima M, Nemolizumab JPSG. Trial of nemolizumab and topical agents for atopic dermatitis with pruritus. N Engl J Med (2020) 383(2):141–50. doi: 10.1056/NEJMoa1917006 [DOI] [PubMed] [Google Scholar]
- 162. Cao P, Xu W, Zhang L. Rituximab, omalizumab, and dupilumab treatment outcomes in bullous pemphigoid: a systematic review. Front Immunol (2022) 13:928621. doi: 10.3389/fimmu.2022.928621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. D'Aguanno K, Gabrielli S, Ouchene L, Muntyanu A, Ben-Shoshan M, Zhang X, et al. Omalizumab for the treatment of bullous pemphigoid: a systematic review of efficacy and safety. J Cutan Med Surg (2022) 26(4):404–13. doi: 10.1177/12034754221089267 [DOI] [PubMed] [Google Scholar]
- 164. Velin M, Dugourd PM, Sanchez A, Bahadoran P, Montaudie H, Passeron T. Efficacy and safety of methotrexate, omalizumab and dupilumab for bullous pemphigoid in patients resistant or contraindicated to oral steroids. a monocentric real-life study. J Eur Acad Dermatol Venereol (2022) 36(7):e539–e42. doi: 10.1111/jdv.17999 [DOI] [PubMed] [Google Scholar]
- 165. Zhang Y, Xu Q, Chen L, Chen J, Zhang J, Zou Y, et al. Efficacy and safety of dupilumab in moderate-to-Severe bullous pemphigoid. Front Immunol (2021) 12:738907. doi: 10.3389/fimmu.2021.738907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Pavord ID, Menzies-Gow A, Buhl R, Chanez P, Dransfield M, Lugogo N, et al. Clinical development of mepolizumab for the treatment of severe eosinophilic asthma: on the path to personalized medicine. J Allergy Clin Immunol Pract (2021) 9(3):1121–32.e7. doi: 10.1016/j.jaip.2020.08.039 [DOI] [PubMed] [Google Scholar]
- 167. Gimenez-Arnau AM, DeMontojoye L, Asero R, Cugno M, Kulthanan K, Yanase Y, et al. The pathogenesis of chronic spontaneous urticaria: the role of infiltrating cells. J Allergy Clin Immunol Pract (2021) 9(6):2195–208. doi: 10.1016/j.jaip.2021.03.033 [DOI] [PubMed] [Google Scholar]
- 168. Gleich GJ, Roufosse F, Chupp G, Faguer S, Walz B, Reiter A, et al. Safety and efficacy of mepolizumab in hypereosinophilic syndrome: an open-label extension study. J Allergy Clin Immunol Pract (2021) 9(12):4431–40.e1. doi: 10.1016/j.jaip.2021.07.050 [DOI] [PubMed] [Google Scholar]
- 169. Ogbogu PU, Bochner BS, Butterfield JH, Gleich GJ, Huss-Marp J, Kahn JE, et al. Hypereosinophilic syndrome: a multicenter, retrospective analysis of clinical characteristics and response to therapy. J Allergy Clin Immunol (2009) 124(6):1319–25.e3. doi: 10.1016/j.jaci.2009.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Celebi Sozener Z, Gorgulu B, Mungan D, Sin BA, Misirligil Z, Aydin O, et al. Omalizumab in the treatment of eosinophilic granulomatosis with polyangiitis (EGPA): single-center experience in 18 cases. World Allergy Organ J (2018) 11(1):39. doi: 10.1186/s40413-018-0217-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Jachiet M, Samson M, Cottin V, Kahn JE, Le Guenno G, Bonniaud P, et al. Anti-IgE monoclonal antibody (Omalizumab) in refractory and relapsing eosinophilic granulomatosis with polyangiitis (Churg-strauss): data on seventeen patients. Arthritis Rheumatol (2016) 68(9):2274–82. doi: 10.1002/art.39663 [DOI] [PubMed] [Google Scholar]
- 172. Raffray L, Guillevin L. Treatment of eosinophilic granulomatosis with polyangiitis: a review. Drugs (2018) 78(8):809–21. doi: 10.1007/s40265-018-0920-8 [DOI] [PubMed] [Google Scholar]
- 173. Trivioli G, Terrier B, Vaglio A. Eosinophilic granulomatosis with polyangiitis: understanding the disease and its management. Rheumatol (Oxford) (2020) 59(Suppl 3):iii84–94. doi: 10.1093/rheumatology/kez570 [DOI] [PubMed] [Google Scholar]
- 174. Roufosse FE, Kahn JE, Gleich GJ, Schwartz LB, Singh AD, Rosenwasser LJ, et al. Long-term safety of mepolizumab for the treatment of hypereosinophilic syndromes. J Allergy Clin Immunol (2013) 131(2):461–7.e1-5. doi: 10.1016/j.jaci.2012.07.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Wechsler ME, Akuthota P, Jayne D, Khoury P, Klion A, Langford CA, et al. Mepolizumab or placebo for eosinophilic granulomatosis with polyangiitis. N Engl J Med (2017) 376(20):1921–32. doi: 10.1056/NEJMoa1702079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Hara T, Miyajima A. Function and signal transduction mediated by the interleukin 3 receptor system in hematopoiesis. Stem Cells (1996) 14(6):605–18. doi: 10.1002/stem.140605 [DOI] [PubMed] [Google Scholar]
- 177. Ilmarinen P, Moilanen E, Kankaanranta H. Regulation of spontaneous eosinophil apoptosis-a neglected area of importance. J Cell Death. (2014) 7:1–9. doi: 10.4137/JCD.S13588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Lombardi C, Berti A, Cottini M. The emerging roles of eosinophils: implications for the targeted treatment of eosinophilic-associated inflammatory conditions. Curr Res Immunol (2022) 3:42–53. doi: 10.1016/j.crimmu.2022.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Valent P, Degenfeld-Schonburg L, Sadovnik I, Horny HP, Arock M, Simon HU, et al. Eosinophils and eosinophil-associated disorders: immunological, clinical, and molecular complexity. Semin Immunopathol (2021) 43(3):423–38. doi: 10.1007/s00281-021-00863-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Walsh GM. Mechanisms of human eosinophil survival and apoptosis. Clin Exp Allergy (1997) 27(5):482–7. doi: 10.1111/j.1365-2222.1997.tb00735.x [DOI] [PubMed] [Google Scholar]
- 181. Lucendo AJ, Lopez-Sanchez P. Targeted therapies for eosinophilic gastrointestinal disorders. BioDrugs (2020) 34(4):477–93. doi: 10.1007/s40259-020-00427-w [DOI] [PubMed] [Google Scholar]
- 182. Choudhury S, Baker S. Eosinophilic esophagitis: the potential role of biologics in its treatment. Clin Rev Allergy Immunol (2020) 59(2):150–9. doi: 10.1007/s12016-019-08749-6 [DOI] [PubMed] [Google Scholar]
- 183. Ko E, Chehade M. Biological therapies for eosinophilic esophagitis: where do we stand? Clin Rev Allergy Immunol (2018) 55(2):205–16. doi: 10.1007/s12016-018-8674-3 [DOI] [PubMed] [Google Scholar]
- 184. Jackson DJ, Akuthota P, Andradas R, Bredenoord AJ, Cordell A, Gray S, et al. Improving care in eosinophil-associated diseases: a charter. Adv Ther (2022) 39(6):2323–41. doi: 10.1007/s12325-022-02110-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. McDonald VM, Vertigan AE, Gibson PG. How to set up a severe asthma service. Respirology (2011) 16(6):900–11. doi: 10.1111/j.1440-1843.2011.02012.x [DOI] [PubMed] [Google Scholar]
- 186. Backer V, Cardell LO, Lehtimäki L, Toppila-Salmi S, Bjermer L, Reitsma S, et al. Multidisciplinary approaches to identifying and managing global airways disease: expert recommendations based on qualitative discussions. Front Allergy (2023) 4:1052386. doi: 10.3389/falgy.2023.1052386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Castillo Vizuete JA, Sastre J, Del Cuvillo Bernal A, Picado C, Martinez Moragon E, Ignacio Garcia JM, et al. Asthma, rhinitis, and nasal polyp multimorbidities. Arch Bronconeumol (Engl Ed) (2019) 55(3):146–55. doi: 10.1016/j.arbr.2018.12.020 [DOI] [PubMed] [Google Scholar]
- 188. Mullol J, Del Cuvillo A, Lockey RF. Rhinitis phenotypes. J Allergy Clin Immunol Pract (2020) 8(5):1492–503. doi: 10.1016/j.jaip.2020.02.004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.