Abstract
Purpose:
To examine the eye care practice in the Mumbai Metropolitan Region (MMR).
Methods:
This study consisted of primary and secondary research conducted in five zones of MMR. The primary research included interviews with the patients, eye care providers, and key opinion leaders. The secondary research included analyzing data from the professional ophthalmology societies, public health domain, and health insurance providers. We divided people into three economic classes by annual income – low (<INR 0.3 m), middle (INR 0.31–1.8 m), and high (>1.8 m). We analyzed the collected data to estimate the eye care demand–supply, quality of eye care, health-seeking behavior, gap in eye care delivery, and eye care expenditure.
Results:
We examined 473 key eye care facilities and interviewed 513 people. The ophthalmologist density in MMR was 80/million, and it was the highest in North MMR. Most ophthalmologists visited several facilities. Cataract surgery and glaucoma care coverage were better than other specialties; it was poor for oncology and oculoplastic services. Annual eye examination practice was poor in the low- and middle-income groups than in the high-income group (48%–50% vs. 85%). Most people preferred visiting eye care facilities within 5 km of their residence. Out-of-pocket spending was between 60% and 83%. Lower-income group people preferred public facilities.
Conclusion:
MMR eye care needs further improvement in affordable and accessible eye care, health literacy, public health surveillance, research into the application of newer technologies to provide less-expensive home care for the elderly and minimize their hospital visits, and collection and analysis of big data to address city-specific eye health issues.
Keywords: Eye care, India, Mumbai Metropolitan Region, survey
The United Nations recognizes eye care as an important component of the human health system.[1] Improving eye health and reducing vision impairment are directly or indirectly linked to at least seven of seventeen 2030 sustainable development goals (SDGs), such as good health and well-being (SDG 3), quality education (SDG 4), gender equity (SDG 5), reduced inequalities (SDG 10), no poverty (SDG 1), zero hunger (SDG 2), and decent work and economic growth (SDG 8).[2] Analysis of eye care delivery in any location is important to understand the availability of existing infrastructure, human resources for eye health (HReH), the health finances, and the health-seeking behavior of people. Mumbai is the second largest city in India by population (20.6 million people, 2021).[3] While many eye specialists and facilities are available in the city, there has never been a systematic analysis of Mumbai’s eye care facilities and delivery. We designed a systematic eye care facility and practice survey to document the current eye care delivery in Mumbai Metropolitan Region (MMR). The objectives were to estimate the eye care demand–supply, quality of eye care, health-seeking behavior of people, gap in eye care delivery, eye care expenditure, and the spread of payer network in the MMR.
Methods
The study was approved by Sigma Institutional Review Board (New Delhi; 10084/IRB/21-22), and followed the tenets of the Declaration of Helsinki for human-related study. We adopted a mixed-methods research of quantitative and qualitative analyses. It included primary (data generation) and secondary (data collation and synthesis) research. The primary research was conducted across MMR to determine the demand and supply estimation and the health-care finances. We divided the MMR into five zones – North (Andheri, Borivali, Malad, and Virar), Central (Bandra, Dadar, Dharavi, and Wadala), South (Colaba, Fort, Malabar Hills, and Marine Lines), East (CBD Belapur, Navi Mumbai, Panvel, and Vashi), and Mumbai suburbs (Bhandup, Dombivali, Kalyan, Mulund, and Thane) [Fig. 1, Table 1]. We chose Wadala area as it is situated in the center of MMR and on the central railway line of Mumbai local railways; also, Wadala is easily accessible. Using ESRI-ArcGIS software (Redlands, CA, USA), we mapped 473 critical facilities to assess eye care delivery in these five zones. The selected facilities included a mix of public and private eye hospitals, medical schools, multispecialty hospitals with eye departments, and large and small eye clinics. To analyze the eye care demand, we used the area within a 20-min drive distance from Wadala railway station (central zone in our definition).
Figure 1.
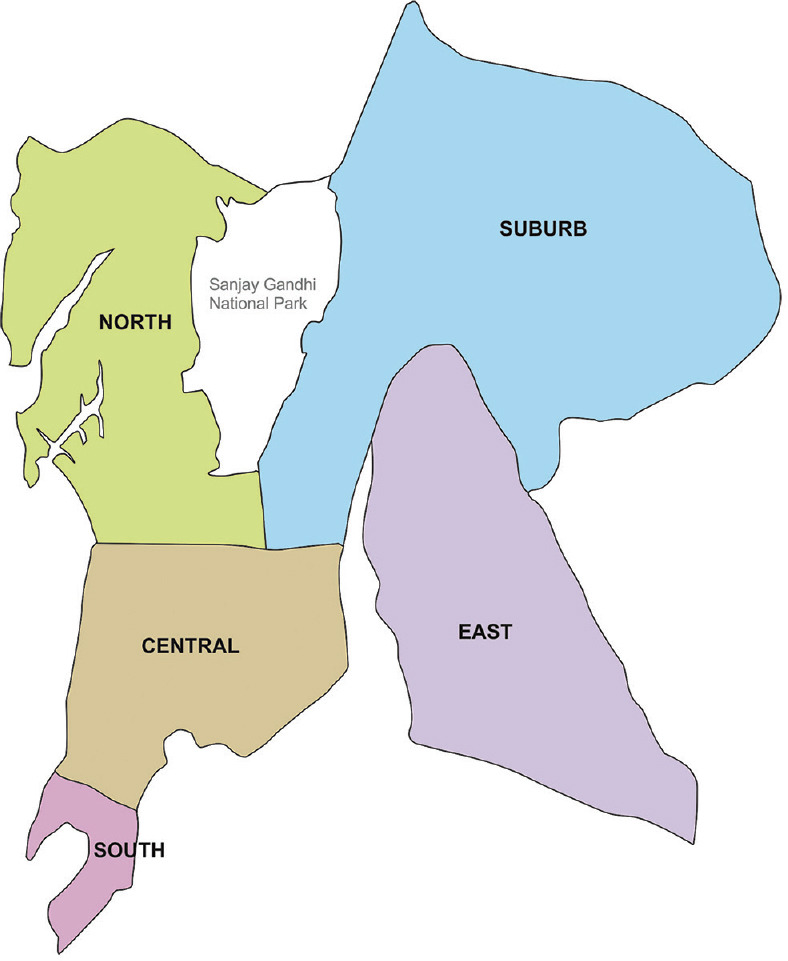
Five zones of the Mumbai Metropolitan Region
Table 1.
Mumbai Metropolitan Region basic information and distribution of eye care
| Region | North | East | South | Central | Suburbs |
|---|---|---|---|---|---|
| Areas | Andheri, Borivali, Malad, Virar | CBD Belapur, Navi Mumbai, Panvel, Vashi | Colaba, Fort, Malabar Hills, Marine Lines | Bandra, Dadar, Dharavi, Wadala | Bhandup, Dombivali, Kalyan, Mulund, Thane |
| Population density/km2 | 9380 | 53,577 | 38,115 | 42,805 | 12,205 |
| Population | 4,034,234 | 18,414,288 | 796,610 | 2,024,626 | 4,109,291 |
| Ophthalmologists, na | 673 | 232 | 41 | 97 | 509 |
| Ophthalmologist/million populationa | 167 | 13 | 51 | 48 | 124 |
aThis is as per the data from 473 facilities. It does not include small single-doctor ophthalmology clinics and part-time/visiting ophthalmologists
The primary research included an interview with the patients, eye care providers, and key opinion leaders in diverse fields of health care, including ophthalmology. Only permanent residents of MMR were included in the patient group. At the facility level, interviews were conducted only with the hospital administrators and senior physicians. Given that these interviews were conducted during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic (April–October 2020), all necessary health-related protocols were followed, such as wearing proper personal protective equipment and frequent use of hand sanitizers. All direct physical contacts were avoided. The questionnaire of primary interview of various groups of people was framed after the data from the health-care facilities and insurance companies were collected and analyzed. The responses were analyzed separately.
We selected four different groups for primary interview. These were (1) students (currently pursuing medicine [undergraduates], ophthalmology residency, and optometry); (2) practicing ophthalmologists providing eye care services in the region; (3) key opinion leaders or top professionals and experts in eye care; and (4) adults who could need eye care in the near future. The people were selected from each of the five regions. Only permanent residents of MMR with the government-issued photo ID (voter or Aadhaar card; Aadhaar card is the proof of residence in India) were included in the survey.[4] We defined permanent residents as those who have lived in Mumbai for at least 1 year and were not planning to move out of the city for another year. At the facility level, interviews were conducted with the hospital administrators and senior physicians. Other hospital staff was excluded. The data were collected after obtaining a written consent. It was kept confidential, and the participants were explained that the anonymized data could be used for research and possible publications.
The secondary research included analyzing data from the city- and state-based professional ophthalmology societies, data available in the public domain, and the health insurance providers. Data were collected from the hospital (n = 75) websites to identify the service mix, qualification of key doctors, type of accreditation, empanelment with insurance providers, so also provision and practice of medical tourism. Data on the clinicians (n = 63) was gathered to identify the clinician engagement models used by these hospitals, average charges for consultation services, and qualification/years of experience. Using the collected data, inter-/intra-hospital comparison was drawn, and 20 key eye care hospitals/clinics were identified for benchmarking. These hospitals/clinics were also examined using the Ayushman Bharat PM-JAY[5] and MJP-JAY[6] (Pradhan Mantri Jan Arogya Yojana, national and Mahatma Jyotirao Phule Jan Arogya Yojana, state public insurance, respectively) data to assess the insurance penetration and identify key packages in ophthalmology in-patient volume, patient profiles (age and sex), and insured beneficiary base. Data was also collected from key third-party assurance (TPA) providers (n = 23) empaneled with major eye hospitals, eye clinics, and multispecialty hospitals in the region.
To measure the demand, we divided the target population (n = 513) into three income groups by annual income – low, middle, and high, which are less than INR 300,000, between INR 300,000 and INR 1.8 million, and above INR 1.8 million, respectively. Two important questions we asked were (1) Do you know the importance of eye examination? and (2) Do you regularly practice annual eye examination? Additional information on the patient feedback was also collected from various health-care apps such as Practo, Google review, and Just dial.
Interviews
All interviews were conducted by field investigators. It consisted of 11 people (eight men, three women) selected locally with a minimum educational qualification of graduation in any discipline. They received training for 2 days to identify key respondents, conduct interviews, and record the correct answers. Virtual interviews were conducted with key opinion leaders or top professionals and experts in eye care because of coronavirus disease 2019 (COVID-19) pandemic (second wave).
The data collection was done utilizing a mixed method of quantitative and qualitative techniques. We used KoBo survey tool (http://www.kobotoolbox.org). KoBo Collect survey application, an open source tool, was installed on android mobile phones given to the field investigators for conducting primary data collection. KoBo is a controlled application protected by password and provides collective user-wise data.
The categorized and open-ended questions used in the survey are show in Supplementary Table 1.
Sample size
We assumed that 5.1 million people, one-quarter of the MMR population, could possibly need eye care any time in their life. This number was used to calculate the sample size for interviewing the Mumbai residents. Using a random sampling methodology, and population proportion needs, we used the following formula:
S = [Z2* p* (1 − p)/E2]/1+([Z2 *p* (1 − p)/E2 − 1]/N),
where
S: sample size
Z: Z-score (which corresponds to the 95% confidence level)
p: population proportion (assumed to be 50%)
E: margin of error (assumed as 5%)
N: population size (5,100,000- possible number of people needing eye care in MMR)
S = [(1.96) 2 *0.5*(1 − 0.5)/(0.05) 2]/1+([(1.96) 2 *0.5*(1 − 0.5)/(0.05) 2 − 1]/5,100,000)
S = 384.13 (~approx. 384)
Incorporating a nonresponse rate of 20%:
final sample size = 384.13/0.8 = 480.16 (~approx. 480) across defined eye service categories in proportion to their population needs.
Minimum sample size required to draw statistically significant conclusion was 480 residents, though in an attempt to increase the precision, we have included a larger sample of 513 residents.
Results
We chose the Wadala area as our point of reference because of its relatively central location, large suburbs with economically middle-class habitats, proximity to a large urban slum (Dharavi), and dense habitation (40,400 population per km2).[7] By annual income (2015 standards), using our division of economic class, we categorized 43%, 31%, and 26% people into low-, middle- and high-income groups, respectively.[8] The investigators ensured that all date were available from all health-care facilities (n = 473) and residents (n = 513).
We mapped 473 key facilities as follows: 56 eye hospitals, 246 multispecialty eye hospitals with an ophthalmology department, and 171 eye clinics. The majority of these facilities were on the western railway line.
National Accreditation Board for Hospitals (NABH) accreditation: One-fifth (92/473 = 19.5%) of these eye care facilities had NABH accreditation- 68.5% (n = 63/92) had full accreditation and 31.5% (n = 29/92) had entry-level accreditation.
Ophthalmic education: Some of these facilities offered ophthalmic and para-ophthalmic courses. These included a bachelor’s degree (n = 56) and diploma (n = 38) in optometry, a postgraduate degree in ophthalmology (DNB, n = 19 of 473), and a fellowship (32 of 473) in ophthalmology subspecialty and optometry.
Demand and availability of eye care services: The demand for cataract, glaucoma, and vitreoretinal services was high in the MMR region, and so was the availability of these services, usually within a 5 km radius of the reference location. But the provision for uvea, pediatric ophthalmology, and ocular oncology was low [Table 2].
Table 2.
Eye care services in the Mumbai Metropolitan region
| Service category | Accreditation | Specialty service (%) | Ancillary service (%) | Health finance (%) | Insurance (%) |
|---|---|---|---|---|---|
| Eye hospital/clinic, n=226 | NABH=27 | Cataract - 100 | Optica l- 35 | Free/charity - 17 | Public -8 |
| Joint Commission International (JCI)=1 | Cornea - 52 | Pharmacy - NA | Out of pocket - 83 | Private - 28 | |
| Glaucoma - 75 | Public + private - 8 | ||||
| Oculoplasty - 22 | None - 56 | ||||
| Oncology - 18 | |||||
| Pediatrics - 41 | |||||
| Retina-vitreous - 30 | |||||
| Eye department, n=246 | NABH=65 | Cataract - 100 | Optical - 9 | Free/charity - 40 | Public - 40 |
| JCI=2 | Cornea - 47 | Pharmacy - NA | Out of pocket - 60 | Private - 20 | |
| Glaucoma - 92 | Public + private - 25 | ||||
| Oculoplasty - 18 | None - 15 | ||||
| Oncology - 15 | |||||
| Pediatrics - 35 | |||||
| Retina-vitreous - 34 |
We benchmarked 20 eye care services; 14 (70%) of these were stand-alone large eye care facilities (eye hospitals) and six (30%) were the ophthalmology services in a large multispecialty hospital (eye department). Either location provided a range of eye care services and included both out- and in-patient facilities. On an average, the outpatient department (OPD) had approximately 80–90 patients per day in eye specialty hospitals and 65–75 patients per day in multispecialty facilities. Annual eye surgery was in the range of 12,228–29,460.
Practice pattern. Most of the time, the engagement of hospitals with clinicians is primarily part-time and visiting consultant mode. Clinicians with more than 15 years of experience tend to establish their private practice while continuing to serve as visiting consultants or specialists with other hospitals. Half of the interviewed clinicians worked part-time at eye care facilities, and the other half had a full-time engagement with one facility. Typically, small and medium-sized providers hired less-experienced clinicians and large and multispecialty providers engaged more experienced physicians. OPD services in most facilities were in two shifts – morning, beginning at 10 AM (ending at 2 PM), and evening, beginning at 4 PM (ending at 9 PM). In most places, there is no regular service between 2 PM and 4 PM on weekdays and none on Sundays. Emergency and inpatient department (IPD) services are available 24 × 7. The ophthalmology residents and fellows-in-training conduct outreach programs for their respective hospitals.
Cost of care: Most people pay all medical bills out of pocket or by private insurance [Table 2]. In the MMR region, the senior clinicians do not provide free consultations for outpatients or surgery. Nominal services are available for people seeking free service. However, free-of-cost surgeries are available in government facilities under the national- or state-level blindness control programs, but patients pay for all additional medicines and all high-cost consumables.
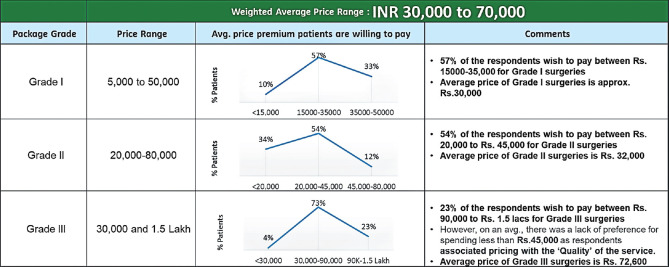
Willingness to pay: All respondents were price sensitive. The average outpatient consultation was INR 857 (INR 500, INR 800, and INR 1200 for the low-, middle- and high-income groups, respectively). The willingness to pay for surgery was procedure dependent. It varied from INR 5000 to INR 150,000 per surgical procedure. We categorized them into three grades for convenience and easy understanding; the weighted average was INR 30,000–INR 70,000. The willingness to pay for the surgical procedure by grades is shown in Fig. 2.
Figure 2.
Willingness to pay for surgical procedures
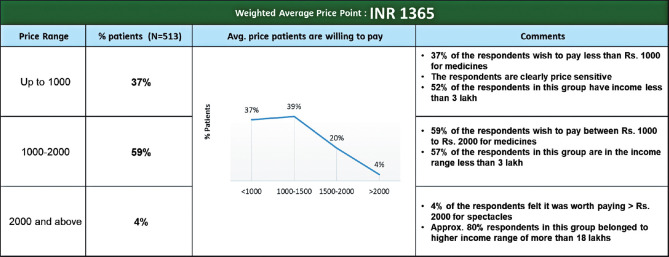
Ophthalmic medicine: The willingness to pay for medicine was based on the economic group: 58% of people were comfortable with spending up to INR 1000/- (predominantly lower-economic group), 39% of the respondents were comfortable up to INR 2000/- (predominantly middle-income group), and 3% of the respondents were willing to pay above INR 2000/- (only higher-income group). The weighted average for ophthalmic medicine was INR 1225.
Spectacles: More than 60% of respondents were inclined to buy better-quality spectacles, ranging from INR 1000/- to INR 2000/-. The lower-income group preferred a modest variety, costing less than INR 1000/-, and were price sensitive. Again, with an increase in the annual income, the tendency was to purchase more expensive and superior-quality spectacles. In this segment, too, the average cost echoed with the competitor analysis, that is, INR 1365 [Fig. 3].
Figure 3.
Willingness to pay for spectacles
In our analysis, all 473 eye hospitals, eye clinics, and multispecialty hospitals were empaneled with various TPAs – 60% (n = 284) of them with less than five TPAs, 34% (n = 161) hospitals with 6–10 TPAs, and 6% (n = 28) hospitals with more than 10 TPAs. Government insurance scheme such as AB PM-JAY offers additional incentives based on the accreditation levels of the health-care facility. Cataract surgery is not a part of the state health insurance scheme MJP-JAY in Maharashtra; hence, the beneficiaries were unable to take the facilities of the public health insurance scheme.
Secondary research was undertaken using the data available on the National Programme for Control of Blindness &Visual Impairment (NPCB VI) website (2018–2019). In the financial year 2021–2022, a reimbursement claim was made for less than 1% (3199 of approximately 400,000) eye surgeries performed in the MMR.
Demand estimation
The health-seeking behavior improved with the increase in the income level. The people got their eyes examined when required –65% in the low-income group and 87% and 89% in the middle- and higher-income groups, respectively. But the routine annual eye examination was low in the lower- and middle-income groups (50% and 48%, respectively); it was much better at 85% in the high-income group. The preference for public and private eye care facilities was 65% versus 35%, respectively, in the low-income group, 56% versus 44%, respectively, in the middle-income group, and 13% versus 75%, respectively, in the high-income group; additionally, 12% of the high-income group preferred to seek eye care treatment outside of the state of Maharashtra [Fig. 4].
Figure 4.
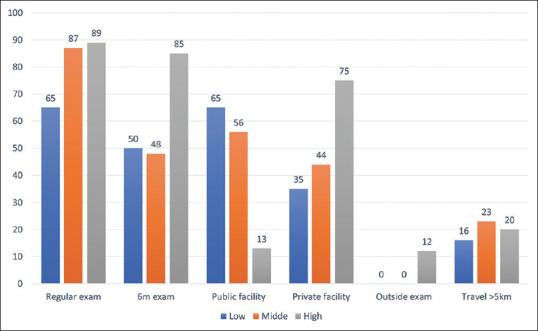
Eye examination pattern and practice
The cost of care was higher in private facilities. In addition to the medical cost, travel distance to the eye care facility was also an important determinant. Nearly all participants across income groups preferred not to travel beyond 5 km for eye care; it was 16%, 23%, and 20% in low-, middle-, and high-income groups, respectively. Other influencing factors were the familiarity with the treating physician (such as the physician had earlier treated one of the family members) and referral by the family physician.
Discussion
Mumbai city in India has many unique characters. It is the economic corridor of India with 33% of India’s income tax collections, 20% of all central excise tax collections, and 40% of India’s foreign trade. It is crowded with high population density [Table 1], and over 35% of people live in urban slums. The per capita income is three times higher than the rest of the country, though 43% of people are either poor or live below the poverty line.[8] The city also is home to 17% of migrant workers. It is cosmopolitan, with half of the people living in the city coming from other states of India.[9]
The current survey is the first systematically designed analysis of the eye care facilities in any metro in India (Medline search). The survey of the MMR collected data from a large number of eye care facilities and gathered information from a large adult population and diverse group of professionals. It showed several eye care practice patterns, possibly unique to the city. MMR has a large spread of eye care practices and facilities. The city HReH is good and boasts 80 ophthalmologists per million, which is better than the Indian average of 13.0/million.[10] Despite this advantage, the study identified two significant disparities in eye care: (1) deficient spread of all specialties other than cataract and glaucoma care [Table 2] and (2) insecure health financing where there is a high proportion of out-of-pocket spending. The city also has a large population of “floating” specialist consultant ophthalmologists who visit several eye care facilities for a few fixed hours every day or on predetermined days. The advantage is that it brings the specialists closer to the people’s residence; but the disadvantage is that it neither provides the specialists enough time to spend with the patients nor provides enough space to resolve technically difficult medical problems. The genesis of this pattern of care partly owes to Mumbai’s traffic conditions. In a survey conducted of 403 cities in 53 countries, Mumbai was found to be the world’s most congested city by traffic;[11] the TomTom N.V (Amsterdam, the Netherlands) reported a 53% congestion level in 2021.[12] This means that the travel time by road is 53% longer than the baseline uncongested conditions; for example, a 30-min trip driven in a free-flow condition will take 16 min longer when the congestion level is at 53%. We also believe that the combination of the traffic situation and the consultant practice in Mumbai city could be behind the origin of three other phenomena in the city: one, low volume of voluntary eye care in the middle of the day (from 2 to 4 PM); two, people like to avail services within 5 km of their residence [Fig. 4]; and three, nonexistence of large eye care institutes with equal emphasis on eye health research and public health similar to those available in a few states in South India.
Provision and proximity of health facilities are the first steps to good eye care. But, by itself, it does not necessarily improve regular health-seeking behaviors. In a study conducted in Hyderabad (South India) city, nearly half of people did not voluntarily seek eye care despite decreased vision, and in a third of the people, routine eye care was not one of the health-care practices.[13] A Singapore study has shown that annual eye examination ranged from 22.4% to 40.4% in three ethnic groups (Chinese, Malaya, Indian) and refractive service was better than other specific eye care services.[14] Our study did not analyze specific services; instead, it looked for the proportion of people visiting the eye care facilities in the event of decreased vision and the practice of annual eye examination [Fig. 4]. It was over 65% in the former and 48% in the latter. The utilization of eye care was less in the lower-income group, and the practice of annual eye examination was less in the lower- and middle-income groups than in the higher economic group. The poor utilization of eye care services even in cities is related to “felt need” and “health literacy.”[15]
Mobile health service is one of the modalities to improving eye care uptake. A quality-assured mobile eye service is known to enhance eye care uptake across many economically less-privileged regions of the world.[16,17] Also, one could improve eye care services using advanced technology.[18] But these measures do not necessarily improve the health-seeking behavior of people. Often, the cost of care is reduced with insurance cover. Our study showed that 60%–83% of people paid for their eye care expenses [Table 2], 57% of people opted for low-premium eye surgery [Fig. 2], and 37% of people opted for less-expensive spectacles [Fig. 3]. While expensive eye surgery may not always parallel better outcomes, superior-quality devices, such as a toric or multifocal intraocular lens and spectacles lens with protective coatings, are also more expensive. Shifting from out-of-pocket spending to prepayment through insurance or pooled funds is likely to ease the financial burden on people.[19] The public insurance, state (MJP-JAY) and national (AB PM-JAY), offers financial support, but not enough for the most common eye surgery, the cataract surgery. It was surprising that reimbursement claim was made for less than 1% (3199 of approximately 400,000) eye surgeries performed in the financial year 2021–2022 (April 2021–March 2022), even accounting that the number of surgeries was comparatively less due to SARS-CoV-2 infection (Maharashtra achieved 67.4% of target cataract surgery in 2020–2021, and the state cataract surgical rate at 4178/million population is 94.7% of the national average at 4410/million population).[20]
Limitations and strengths
Limitations: The current study was conducted during the SARS-CoV-2 infection time, and hence, we could not reach more number of people. Also, many people would have been too depressed during this pandemic to respond more intelligently. We also suspect many needing eye care may have neglected to seek timely eye care and have gotten into this habit. Also, we did not collect ocular disorder-specific data.
Strengths: This is the first survey in the MMR, looking at several aspects of eye care from the perspective of people, eye care providers, and health finance. The study included data from public and private eye care providers and interviewed people in various sections of society – prospective patients, eye care professionals, and key opinion leaders in health care outside of ophthalmology.
Conclusion
The data suggest that the eye health system in the MMR needs different strategic planning. With a literacy rate of 89.2% in Mumbai,[21] higher than the national average of 74.04%,[22] and with a higher per capita income,[9] Mumbai region could consider the following: (1) improve affordable and accessible eye care for ophthalmic disorders not only confined to cataract and glaucoma; (2) incorporate strong public health surveillance system in ophthalmology; (3) research into the application of newer technologies to provide less-expensive home care for the elderly and minimize their hospital visits; and (4) collect and analyze big data to address city-specific eye health issues.
Financial support and sponsorship
Shantilal Shanghvi Foundation, Mumbai (2020).
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We acknowledge Maneck Nicholson, MD, and Jay U. Sheth, MD, for critically reviewing the manuscript.
References
- 1.General Assembly Adopts Resolutions Aimed at Ensuring Global Access to Eye Care. [Last accessed on 221 Nov 23]. Available from:http://www.un.org>press>ga12349.coc.htm .
- 2.Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health:Vision beyond 2020. Lancet Global Health. 2021;9:e489–551. doi: 10.1016/S2214-109X(20)30488-5. doi:10.1016. S2214-109X(20)30488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Population of cities in India. 2021. Available from:https://statisticstimes.com>demographics>country>India .
- 4. Available from:https://dot.gov.in/sites/default/files/2016_11_18%20POIA-AS-II.pdf?download=1 .
- 5.Pradhan Mantri Jan Arogya Yojana (PM-JAY) [Last accessed on 2022 July 24]. Available from:https://nha.gov.in›PM-JAY .
- 6.Mahatma Jyotirao Phule Jan Arogya Yojana. [Last accessed on 2022 Jul 24]. Available from:https://www.jeevandayee.gov.in›MJPJAY .
- 7.Mumbai Wards &Districts:Population &Density by Sector 2001. [Last accessed on 2022 May 22]. Available from:http://www.demographia.com›db-mumbaidistr91 .
- 8.Share of annual household income in Mumbai India 2015. [Last accessed on 2022 Jul 24]. Available from:https://www.statista.com...›Economy .
- 9.Mumbai. UN-Habitat. [Last accessed on 2022 Jul 24]. Available from:https://mirror.unhabitat.org›8528_908_Mumbai .
- 10.Resnikoff S, Lansingh VC, Washburn L, Felch W, Gauthier TM, Taylor HR, et al. Estimated number of ophthalmologists worldwide (International Council of Ophthalmology update):Will we meet the needs? Br J Ophthalmol. 2020;104:588–92. doi: 10.1136/bjophthalmol-2019-314336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Explained:Why Mumbai traffic is the worst in the world. [Last accessed on 2022 Jul 24]. Available from:https://qrius.com .
- 12.Mumbai traffic report. TomTom traffic index. [Last accessed on 2022 Jul 24]. Available from:https://www.tomtom.com>mumbai traffic .
- 13.Dandona R, Dandona L, Naduvilath T, McCarty C, Rao GN. Utilisation of eyecare services in an urban population in Southern India:The Andhra Pradesh eye disease study. Br J Ophthalmol. 2000;84:22–7. doi: 10.1136/bjo.84.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng Y, Cheng C, Lamoureux EL, Chiang PPC, Anuar AR, Wang JJ, et al. How much eye care services do asian populations need?Projection from the Singapore epidemiology of eye disease (SEED) study. Invest Ophthalmol Vis Sci. 2013;54:2171–7. doi: 10.1167/iovs.12-11393. [DOI] [PubMed] [Google Scholar]
- 15.Marmamula S, Kumbham TR, Modepalli SB, Chakrabarti S, Keeffe JE. Barriers to uptake of referral eye care services among the elderly in residential care:The Hyderabad Ocular Morbidity in Elderly Study (HOMES) Br J Ophthalmol. 2022:1–6. doi: 10.1136/bjophthalmol-2021-320534. doi:10.1136/bjophthalmol-2021-320534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wahl S, Leube A, Dhasmana R, Moodbidri P, Kumar VK, Sisodia N, et al. Efficiency of mobile eye camps for providing combined eye and vision care in underserved areas in Uttarakhand. medRxiv. 2020 10.27.20217000. doi:10.1101/2020.10.27.20217000. [Google Scholar]
- 17.Rushood AA. Mobile eye services:Literature review with special reference to the experience of Al-Basar International Foundation. J Family Community Med. 2010;17:46–9. doi: 10.4103/1319-1683.68789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Das T, Sapkota YD. Promoting technology-enabled primary eye care in South-East Asia. [Last accessed on 2022 Jul 24];Comm Eye Health South Asia. 2021 34:7–8. Available from:https://www.cehjsouthasia.org . [PMC free article] [PubMed] [Google Scholar]
- 19.Yu M. Modernizing and expanding universal eye care coverage after VISION. Vis Bioeth. 2020;2020;6 doi:10.7916/d8-852j-2742. [Google Scholar]
- 20.National Programme for Control of Blindness. State wise targets &achievement for various eye diseases during 2020-21. [Last accessed on 2022 Jul 24]. Available from:https://www.npcbvi.gov.in .
- 21.Demography, Mumbai city. India. [Last accessed on 2022 Jul 24]. Available from:https://mumbaicity.gov.in›about-district›demography .
- 22.State wise literacy rate- India guide. [Last accessed on 2022 Jul 24]. Available from:https://www.indiaonlinepages.com›population›literacy .