Abstract
Introduction
Acute kidney injury requiring renal replacement therapy (AKI-RRT) is common in the intensive care unit (ICU) and is associated with significant morbidity and mortality. Continuous RRT (CRRT) non-selectively removes large amounts of amino acids from plasma, lowering serum amino acid concentrations and potentially depleting total-body amino acid stores. Therefore, the morbidity and mortality associated with AKI-RRT may be partly mediated through accelerated skeletal muscle atrophy and resulting muscle weakness. However, the impact of AKI-RRT on skeletal muscle mass and function during and following critical illness remains unknown. We hypothesise that patients with AKI-RRT have higher degrees of acute muscle loss than patients without AKI-RRT and that AKI-RRT survivors are less likely to recover muscle mass and function when compared with other ICU survivors.
Methods and analysis
This protocol describes a prospective, multicentre, observational trial assessing skeletal muscle size, quality and function in ICU patients with AKI-RRT. We will perform musculoskeletal ultrasound to longitudinally evaluate rectus femoris size and quality at baseline (within 48 hours of CRRT initiation), day 3, day 7 or at ICU discharge, at hospital discharge, and 1–3 months postdischarge. Additional skeletal muscle and physical function tests will be performed at hospital discharge and postdischarge follow-up. We will analyse the effect of AKI-RRT by comparing the findings in enrolled subjects to historical controls of critically ill patients without AKI-RRT using multivariable modelling.
Ethics and dissemination
We anticipate our study will reveal that AKI-RRT is associated with greater degrees of muscle loss and dysfunction along with impaired postdischarge recovery of physical function. These findings could impact the in-hospital and postdischarge treatment plan for these patients to include focused attention on muscle strength and function. We intend to disseminate findings to participants, healthcare professionals, the public and other relevant groups via conference presentation and publication without any publication restrictions.
Trial registration number
Keywords: acute renal failure, adult intensive & critical care, dialysis, neuromuscular disease, rehabilitation medicine, rehabilitation medicine
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study has several notable strengths including the study design based on multidisciplinary collaboration, the multicentre patient representation, the collection of longitudinal in-hospital and outpatient measures and outcomes, and the wide range of skeletal muscle and physical function tests being performed.
Due to the pilot nature of this study, we will recruit critically ill patients with acute kidney injury (AKI) requiring continuous renal replacement therapy (CRRT) to collect a broad array of study measures and compare them with available datasets of recent historical controls of critically ill patients without AKI requiring RRT. While the use of these control groups enhances the feasibility of the project, it also represents a limitation.
The high morbidity and mortality inherent to the study population may introduce competing risk of death and selection bias when assessing the outpatient outcomes.
Differentiating the exact contributions of AKI, CRRT and underlying acute illness may not be possible in this observational study due to several confounding variables that could be better addressed with an interventional trial design in the future. Nonetheless, our pilot study will generate critical data for the design and sample size estimations of such future trials.
Introduction
Background and rationale
Acute kidney injury (AKI) complicates approximately 20% of all hospital admissions and up to 50% of all intensive care unit (ICU) admissions.1 2 Moreover, 13.5% of critically ill patients develop AKI requiring renal replacement therapy (AKI-RRT).1 AKI is associated with poor short-term and long-term prognoses. Even stage 1 AKI—defined by as little as a 0.3 mg/dL increase or 50% rise in serum creatinine above baseline3—is associated with up to a 10-fold increase in the odds of in-hospital mortality.4 Similarly, AKI-RRT has an in-hospital mortality rate >50%, making it one of the deadliest conditions encountered in the hospital.5 After discharge, AKI survivors are at increased risk of developing chronic kidney disease (CKD), end-stage kidney disease, cardiovascular disease and death.6 Other studies suggest that AKI predisposes to disparate sources of morbidity including infection,7–10 bone fracture,11 stroke,12 gastrointestinal haemorrhage13 and dementia.14 While muscle wasting is well described in patients with CKD,15 16 the contribution of AKI-RRT to muscle wasting in critically ill patients has not been previously studied.
Acute skeletal muscle wasting occurs in up to 65% of patients admitted to the ICU.17 Critical illness myopathy (CIM), defined as a deficit in muscle size and strength that develops as a result of an ICU admission, is associated with high rates of short-term and long-term mortality and morbidity, including decreased quality of life (QoL) due to persistent functional mobility impairments and inability to perform simple activities of daily living.18–21 AKI of any stage is known to alter tissue utilisation of amino acids, making it plausible that AKI exacerbates CIM.15 22 Studies have demonstrated that plasma amino acid levels are reduced and multiple non-essential amino acids become conditionally essential in the setting of AKI.23–25 In addition, AKI leads to a state of increased amino acid oxidation but reduced amino acid transport into muscle.15 RRT exacerbates this issue through non-selective removal of amino acids from plasma.15 Amino acids are small and easily filtered during RRT, and, as a result, daily losses of amino acids in effluent can be immense at up to 18 g daily with continuous RRT (CRRT).26 27
The gold standards for assessing CIM are muscle biopsy or electrodiagnostic testing.28 Furthermore, the measurement of psoas muscle area on a single cross-sectional CT image at the level of the L3 vertebra has been suggested as a standard clinical measure for skeletal muscle quantification.29 However, biopsy, electrodiagnostic testing and CT imaging present challenges which limit their clinical application. Musculoskeletal ultrasound (MSKUS), a relatively inexpensive, non-invasive alternative, has gained significant traction over the last decade for assessing muscle in ICU patients.30 Studies have demonstrated that MSKUS has excellent inter-rater reliability and high clinical utility and have suggested that MSKUS has strong construct validity.31–35 Recent data suggest that MSKUS can be reliably performed at the bedside in the ICU.36
The primary objective of this study is to characterise longitudinal measures of muscle size (rectus femoris (RF) muscle cross-sectional area (CSA) and muscle thickness (mT)) and quality (echo intensity (EI)) in critically ill adults with AKI requiring CRRT during their ICU stay and in postdischarge follow-up among survivors. This trial protocol was designed using the elements of the Strengthening the Reporting of Observational studies in Epidemiology checklist for cohort studies9 whenever applicable.
Objectives
Aim 1: To characterise changes in RF muscle mass and quality at baseline and days 3 and 7 following study enrolment in critically ill adults with AKI requiring CRRT and to compare these measurements with those of historical ICU controls without AKI-RRT.
Hypothesis 1: RF muscle mass and muscle quality will be lower at 7 days in patients with AKI-RRT compared with the corresponding inpatient measurements of historical ICU controls without AKI-RRT.
Aim 2: To characterise changes in RF muscle mass and quality at hospital discharge and within 3 months postdischarge in survivors of AKI requiring CRRT in the ICU and to compare these measurements with those of historical ICU controls without AKI-RRT.
Hypothesis 2: The muscle mass and functional parameters of survivors of AKI-RRT obtained within 3 months of hospital discharge will be worse than the corresponding measurements from historical controls of ICU survivors without AKI-RRT obtained within a similar postdischarge timeframe.
Aim 3: To examine if changes in plasma or effluent amino acid levels correlate with skeletal muscle loss during CRRT or with skeletal muscle function at 1–3 months postdischarge.
Hypothesis 3: The concentrations of amino acids in blood and effluent during CRRT will correlate with MSKUS parameters of muscle mass and will be associated with muscle function following discharge.
Methods: participants, interventions and outcomes
Trial design
This is a prospective multicentre observational study to evaluate longitudinal inpatient and outpatient measures of muscle mass and function in critically ill adults with AKI requiring CRRT and to compare these measurements with those of historical ICU controls without AKI-RRT. The study will have two phases, an ICU phase and a recovery phase for subjects who survive to discharge.
Study setting
This study will be conducted at the adult ICUs at the academic medical centres of the University of Kentucky, University of Iowa and University of New Mexico. Following discharge, survivors will return for outpatient evaluation of skeletal muscle and physical function.
Eligibility criteria
To be included in the study, patients are required to be ≥18 years old and have AKI-RRT with enrolment within 48 hours of CRRT initiation. Exclusion criteria include: (1) ICU admission for >7 days; (2) RRT of any kind at any time before ICU admission; (3) CKD with estimated glomerular filtration rate <20 mL/min/1.73 m2 as calculated by the 2021 CKD-EPI equation;37 (4) underlying muscle disorders or muscle atrophy such as quadriplegia or hemiplegia, stroke with residual motor deficits, end-stage liver disease, active alcohol use disorder, active malignancy (other than non-melanoma skin cancer) within 1 year, burns or other baseline neuromuscular disease; (5) pregnancy; (6) concomitant use of other extracorporeal support devices such as ventricular assist devices or extracorporeal membrane oxygenation or (7) anticipated inability to engage in weight-bearing testing after discharge (eg, trauma or orthopaedic surgery). For outpatient testing, patients will be ineligible if they remain on RRT in the week prior to the research appointment.
Control population
Given the pilot nature of this study, we will use recent historical controls defined as critically ill adults without AKI-RRT in whom similar measurements of muscle size, quality and function were collected. Specifically, we have previously collected data on 41 ICU patients, of which 36 did not have AKI-RRT and will serve as the control group for the ICU phase of this study, and have published the results of MSKUS performed in the ICU and functional assessments performed at both ICU discharge and hospital discharge.38 The controls for the recovery phase will come from an ongoing prospective observational study being performed at the University of Kentucky, which will include outpatient functional assessments performed on 200 ICU survivors (NCT05537298). See table 1 for a summary of the demographic and clinical characteristics of the control cohorts which have been published thus far.21 38 39
Table 1.
Demographic and clinical characteristics of the cohorts being used as our historical controls for this study
| Cohort characteristic | Control cohort for ICU phase*38 | Control cohort #1 for recovery phase† 21 | Control cohort #2 for recovery phase39 |
| ICU or admission type | Medical 73%; cardiothoracic 27% | Medical 100% | Mixed |
| Years of enrolment | 2018–2019 | 2018–2019 | 2018–2021 |
| N | 41* | 12† | 59 |
| Primary inclusion | Acute respiratory failure or sepsis and anticipated ICU stay >3 days | Survivors of acute respiratory failure requiring >48 hours of mechanical ventilation | Survivors of sepsis and/or acute respiratory failure |
| Timing of initial assessment | Within 48 hours of admission; median 1.1 days (IQR 0.7–1.4) | N/A | N/A |
| Timing of outpatient assessment | N/A | 4–8 weeks after hospital discharge | 3 months after hospital discharge |
| Age, median years (IQR) | 61 (55–68) | 58 (45.5–65) | 56 (48–64) |
| Female, no (%) | 18 (44) | 4 (33) | 31 (53) |
| No (%) mechanically ventilated | 30 (73) | 12 (100) | 43 (73) |
| Duration of mechanical ventilation, median days (IQR) | 3.4 (1–7.7) | 6.45 (2.8–11.95) | 8 (5–14) |
| No (%) requiring RRT | 5 (12)* | NR† | 0 |
| Disease severity (SOFA) scores | Mean 8.1 (SD±4.8) | Median 8 (IQR 4.5–10.25) | Median 10 (IQR 8–12) |
| ICU LOS, median days (IQR) | 8 (4) | 7.4 (4.3–18.6) | 10 (6–15) |
| Hospital LOS, median days (IQR) | 11.2 (8–19) | 16.7 (9.4–28.7) | 15 (11–22) |
| Hospital mortality | 12% | N/A | N/A |
Presented here are only previously published data. The two control cohorts for the recovery phase represented in the table are only a subset of the 200 patients in our ongoing registry that will serve as the control for the recovery phase.
*Data for this entire cohort are presented as published, including data from the five patients treated with RRT who will be excluded from the control group in our analysis.
†Though not reported in the published manuscript, RRT status is available for this cohort and any patients with AKI-RRT will be excluded from the control group in our analysis.
AKI, acute kidney injury; ICU, intensive care unit; LOS, length of stay; N/A, not applicable; NR, not reported; RRT, renal replacement therapy; SOFA, Sequential Organ Failure Assessment.
Primary outcome (ICU phase)
The primary outcome is the change in RF CSA, mT and EI measured by MSKUS at baseline, assessed within 48 hours of CRRT initiation, to ICU days 3 and 7 of study enrolment (or at ICU discharge, if sooner). Operational and standardisation procedures have been previously published.35 38 In brief, patients are positioned supine with the lower extremity in neutral alignment. RF ultrasound images are acquired two-thirds of the distance from the anterior superior iliac spine to the superior border of the patella of the right lower extremity at all time points. Sonographers will use a linear probe (5–15 Hz) with the same machine for all time points and a minimal-to-no-compression technique. Sonographers will obtain three images per assessment to reduce variations in EI. Ultrasound images will be assessed for CSA, mT and EI at baseline within 48 hours of CRRT initiation, at days 3 and 7 from enrolment (or at ICU discharge, if sooner). A representative ultrasound image and the techniques for landmarking and probe pressure are provided in figure 1.
Figure 1.
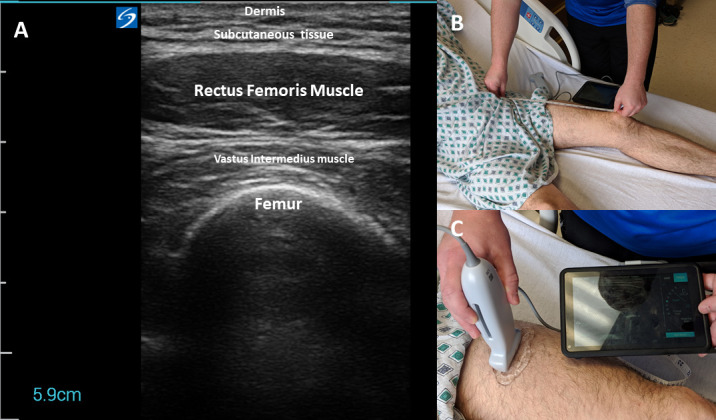
Representative images of ultrasound acquisition techniques and the obtained image of the rectus femoris muscle. (A) is a representative ultrasound image with anatomical structures labelled for the quadriceps muscle. (B) demonstrates the technique to locate the anatomical landmarks for rectus femoris ultrasound (two-thirds of the distance from anterior superior iliac spine to the superior border of the patella). (C) depicts the-minimal-to-no-compression technique using the ultrasound probe with adequate ultrasound transmission gel to obtain images. These images were staged by the authors to demonstrate appropriate technique and were not taken from a patient encounter.
Secondary outcomes (ICU phase)
Patients will have blood collected at baseline (within 48 hours of CRRT initiation), at study days 3 and 7 (or ICU discharge, if sooner). Creatinine and cystatin C will be measured at each time point. In addition, 5 mL blood samples and CRRT effluent samples at each time point will be sent for gas chromatography-mass spectrometry evaluating a panel of analytes including amino acids, carbohydrates and fatty acids. Remaining samples will be stored for future analysis, though no genetic analysis will be conducted now or in the future.
Patients will be scored at the same time points as above using the ICU Mobility Scale, an 11-point scale ranging from 0 to 10 which involves the clinician scoring the patient’s maximum level of mobility in the prior 24-hour period.40 41
Outcomes (recovery phase)
Survivors will participate in skeletal muscle and physical function testing at hospital discharge and during the outpatient visit at 1–3 months postdischarge. Measurements will include MSKUS to determine RF CSA, mT and EI. We will also conduct an array of standardised and validated tests including:
Medical Research Council Sum-score (MRC-ss): MRC-ss is a measure of global peripheral muscle strength that is the current clinical standard for diagnosing ICU-acquired weakness (ICU-AW).42 Muscle strength is assessed by physical exam and rated on an ordinal scale (0–5) at six bilateral muscle groups: shoulder abductors, elbow flexors, wrist extensors, hip flexors, knee extensors and ankle dorsiflexors. A score<48 is considered indicative of ICU-AW, with a score<36 indicative of severe weakness with the inability to act against resistance.43
Muscle strength using hand-held dynamometry for knee extension: Maximal isometric knee extensor strength will be measured as peak force production and rate of force development following previously published standardised positions (figure 2).44
Muscle strength using hand-grip dynamometry: Hand-grip dynamometers will be used to measure maximum isometric strength of the hand and forearm muscles at previously published standardised positions.42 43 The patient will undergo three repetitions with both the right and left hand, alternating between hands.
Short Physical Performance Battery (SPPB): Physical function and physical frailty will be measured using the SPPB, a performance-based composite test with a total of 12 points including components of balance (side-by-side stand, semitandem stand and full-tandem stand), chair-to-stand test and 4 m habitual gait speed.45 46
Timed Up and Go (TUG) Test: The TUG assesses the time (in seconds) for a subject to stand on command from a seated position, walk 3 m, turn around, walk back to the chair and sit down. The purpose of TUG is to assess mobility, physical function and fall risk. TUG has been validated in and recommended for patients with critical illness.47–49
Six min walk test (6-MWT): The 6-MWT assesses the distance a subject can walk in 6 min, providing a global representation of physical function and cardiopulmonary endurance.50 51 Meta-analysis provides benchmark data for survivors of critical illness.52
QoL testing using EuroQol Group 5-dimension 5-level (EQ-5D-5L) questionnaire: The EQ-5D is a standardised measure of health status developed by the Euro-Qol Group to provide an assessment of health for clinical and economic appraisal.53 It consists of two sections: the descriptive system and the Visual Analogue Scale (EQ VAS). The descriptive system assesses five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. The EQ VAS records the respondent’s self-rated health on a 20 cm vertical VAS with endpoints labelled the ‘best health you can imagine’ and the ‘worse health you can imagine’. This information can be used as a quantitative measure of health as judged by individual respondents.51 54 55
Clinical Frailty Scale (CFS): The CFS is designed for clinical use and has been widely adopted as a judgement-based tool to screen for frailty and to broadly stratify degrees of fitness and frailty.56 57 It is not a questionnaire, but a way to summarise information from a clinical encounter to roughly quantify an individual’s overall health status. While CFS has traditionally been used specifically in older patients, recent data have demonstrated its utility in an ICU population demographically similar to our target population.58
Functional Assessment of Chronic Illness Therapy Fatigue (FACIT-F) Questionnaire: The FACIT-F scale is a 13-item measure that assesses self-reported fatigue and its impact on daily activities and function.59 60
Thirty-six-Item Short Form Health Survey Physical Function Scale (SF-36 Physical Function): The SF-36 is a 36-item patient-reported survey of health commonly used to evaluate adult patients which contains 8 domains, including a physical function scale based on 10 of the 36 items which has been shown to have high reliability.61
Additional events: Finally, we will document the occurrence of the following events: return to driving, return to work or hobby, hospital readmission and need for emergency department care.
Figure 2.

Representative image of the performance of hand-held dynamometry to measure isometric knee extensor strength with a subject in the supine position with a towel roll keeping the knee in 20°–30° of flexion. This image was staged by the authors to demonstrate appropriate technique and was not taken from a patient encounter.
Assessor training
This multisite study is an interdisciplinary collaboration with expertise in critical care, nephrology, muscle biology and physical function. Physical therapist–scientists and exercise physiologists with established expertise in MSKUS and functional testing serve as coinvestigators at each site. Three 2-hour sessions of teleconference training will be performed to promote standardisation of ultrasound and outcome assessments. In addition, novice sonographers were instructed to perform and practice a minimum of 10 acquisitions of RF muscle images from healthy individuals before study initiation. To better establish inter-rater reliability of image acquisition, the first five patients at each site will have ultrasound studies conducted by two team members. The first sonographer will obtain images and leave the room, and the second will enter and repeat the test. After a 10 min wash-out period, the team members will sequentially repeat the ultrasound measurements, which will allow us to establish both interobserver and intraobserver variability. Finally, images will be blinded, coded (rater 1 or rater 2; site location) and sent securely to the University of Kentucky to be reviewed by an expert sonographer (KPM, who has >6 years of MSKUS experience) to ensure cross-site standardisation of measurements.35 All images will be analysed for muscle CSA, mT and EI by the same blinded expert sonographer. The images from the first five patients obtained by the two sonographers at each site will be examined with intraclass correlation coefficient (ICC). Sites with ICC<0.7 will receive additional training to improve reliability at each site. ICC values will be disseminated with our final results.
Participant timeline
Patients enrolled in the study will participate in up to two phases, an ICU phase and—for those who survive their critical illness—a recovery phase. The schedule of assessments for both phases is delineated in table 2.
Table 2.
Planned evaluations at each study time point
| Parameter | Time point | ||||
| ICU phase | Recovery phase | ||||
| Within 48 hours of CRRT start | 3±1 days from enrolment | Study day 7 (or ICU discharge) | Hospital discharge | Outpatient 1–3 months |
|
| Rectus femoris US | X | X | X | X | X |
| Amino acids (blood) | X | X | X | ||
| Amino acids (Effluent) | X | X | X | ||
| Cystatin C | X | X | X | ||
| ICU Mobility Scale | X | X | X | ||
| Muscle Strength—MRC-ss | X | X | |||
| Muscle strength—HGD | X | X | |||
| Muscle Strength—HHD | X | X | |||
| SPPB | X | X | |||
| TUG test | X | ||||
| 6-MWT | X | ||||
| EQ-5D-5L | X | ||||
| Clinical Frailty Scale | X | ||||
| FACIT-fatigue | X | ||||
| SF-36 Physical Function | X | ||||
| Return to driving | X | ||||
| Return to work or hobby | X | ||||
| Readmission | X | ||||
| ED visit | X | ||||
ED, emergency department; EQ-5D-5L, EuroQol Group 5-dimension 5-level version; FACIT-F, Functional Assessment of Chronic Illness Therapy-Fatigue; HGD, hand-grip dynamometry; HHD, hand-held dynamometry; ICU, intensive care unit; MRC-ss, Medical Research Council sum-score; 6-MWT, six min walk test; SF-36, 36-Item Short Form Health Survey; SPPB, Short Physical Performance Battery; TUG, Timed Up and Go; US, ultrasound.
Sample size
Our previous study reported a decrease in muscle RF CSA at ICU day 7 of 18.5%.38 To detect an absolute difference in per cent decrease in muscle size of 6% at 7 days (24.5% change at 7 days in AKI-RRT group vs 18.5% change in controls), 61 patients per group are needed assuming an alpha of 0.05 and a power of 80%. This will require inclusion of 20 AKI-RRT patients per site that provide all ICU datapoints. Our previous study also reported that RF CSA was 2.47±0.88 cm2 at ICU day 7, down from a baseline on ICU day 1 of 2.99 cm2.38 To detect a full return to baseline in the outpatient setting with an alpha of 0.05 and a power of 80%, 22 patients are required in each group. To detect a 75% recovery to baseline from day 7 values, 40 patients are required. We anticipate a 40%–50% in-hospital mortality rate which would leave 31–37 patients alive at discharge. Assuming 22 patients are needed, this provides room for attrition or lost to follow-up of 30%–40%.
Recruitment
Patients will be recruited in the multidisciplinary adult ICUs of the three sites involved in the study. Patients will be identified through communication with the nephrology consult services at each site, who will independently make decisions regarding indications for and timing of initiation of RRT. The enrolment will occur for a full year following institutional review board (IRB) approval at each site, with the funding dates ranging from 1 August 2022 to 31 July 2023, at the University of Kentucky and University of Iowa and from 1 October 2022 to 30 September 2023, at the University of New Mexico. To promote subject retention after discharge, we will allow for a 2-month window in which to schedule the postdischarge follow-up visit and subjects will be contacted by telephone a minimum of three times before being considered lost to follow-up. As stipulated in the informed consent form, though subjects may withdraw from the study at any point, all data collected prior to withdrawal will be retained for analysis.
Patient and public involvement
No formal patient advisory committee was established and there was no patient or public involvement in the design or planning of the study. However, to inform future study design, we will conduct a brief open-ended poststudy survey following the outpatient visit at 1–3 months to help discern which of the patient-reported outcome measures and functional assessments performed appear most valuable to the study subjects (online supplemental material 1).
bmjopen-2023-072448supp001.pdf (39.4KB, pdf)
Methods: data collection, management and analysis
Data collection methods
Ultrasound images will be transferred through secure link to the data coordinating site (University of Kentucky). One expert sonographer with clinical and research experience (KPM) will analyse the images for CSA, mT and EI. All muscle analyses will be performed blinded with all images coded by a different research coordinator. The blinded assessor will be unaware of the patient identification, the investigator obtaining the images or the time point of the MSKUS. Blood and effluent fluid will be collected at the defined time points. Plasma samples will be collected in EDTA tubes, centrifuged at 1000 g for 10 min at 4°C. Following extraction of supernatant and transfer into storage tubes, samples will be stored at −80°C. The specimens will be shipped to the biospecimen site (University of Iowa) where we will perform the metabolomic analysis on all samples in one batch. Patient data including demographics, data related to acute illness and comorbidity, and test results will be recorded using standardised case report forms and then uploaded to REDCap.
Data management
Data will be stored using REDCap software at each site. REDCap is a secure web application for building and managing online databases.62 REDCap is HIPAA compliant and is specifically geared to support online and offline data capture for research studies and operations.
Statistical methods
We will summarise descriptive statistics at each time point using frequencies and proportions for categorical variables and means and SD or medians and IQRs, as appropriate, for continuous variables. Binary outcome variables include the diagnosis of ICU-AW (defined as MRC-ss<48/60) and the additional recovery phase events (ie, return to driving, return to work or hobby, hospital readmission and need for emergency department care). Continuous variables include MSKUS parameters, strength testing and physical function testing. Ordinal variables include scores on the EQ-5D-5L, FACIT-F subquestion and CFS.
ICU Phase: The primary outcome in the ICU phase of the study, corresponding to aim 1, will be the change in RF CSA, mT and EI from baseline to day 7 (or ICU discharge) within AKI-RRT patients and in comparison to historical ICU controls without AKI-RRT. Repeated measures analysis will be used with muscle parameters as fixed effects. Of note, in the cohort to be used as the historical control for the ICU phase, MSKUS was performed on ICU days 1, 3, 5 and 7 and muscle strength assessment (by MRC-ss, hand-held dynamometry and hand-grip dynamometry) was performed at ICU and hospital discharge.38 For AKI-RRT patients, time 0 is study enrolment (which must be within 48 hours of CRRT initiation). To account for the resulting differences in timing of assessments, time from ICU admission to MSKUS and muscle strength assessments will be included as covariables in our analyses. We will develop multivariable models for within-group comparisons (in AKI-RRT cases) and between-group comparisons (AKI-RRT cases vs controls). Additional variables entered in the analyses will include demographic variables including age and sex, Charlson Comorbidity Score, illness severity as measured by Sequential Organ Failure Assessment (SOFA) score63 and ICU variables (including mechanical ventilation, trauma, sepsis, corticosteroid use, use of paralytic agents and ICU type). We will conduct univariable analysis to determine if any of these variables are significantly associated with the primary outcomes. To avoid overfitting, only significant variables will be added in the subsequent adjusted model. We will use paired t-test to examine within-group differences and analysis of variance (ANOVA) for between-group differences of MSKUS parameters and other continuous measures. Binary outcomes will be compared by χ2 test. Bonferroni adjustment will be used for multiple comparisons.
Recovery Phase: The primary outcomes in the recovery phase of the study, corresponding to aim 2, will include both (1) the detailed characterisation of longitudinal changes in muscle mass and quality and functional status in AKI-RRT survivors, including comparison of postdischarge recovery of RF size and quality assessed by MSKUS and of muscle strength in AKI-RRT survivors as measured within 1–3 months of discharge compared with in-hospital baselines and (2) comparison of MSKUS parameters and of muscle strength assessed at 1–3 months after discharge in AKI-RRT survivors with the same parameters in historical controls of ICU survivors without AKI-RRT. The assessments of muscle strength at this phase will include MRC-ss, hand-held dynamometry for knee extension and hand-grip dynamometry. Using the same methods and covariables as outlined for the ICU phase analysis, we will generate multivariable models for within-group and between-group comparisons of MSKUS parameters and muscle strength, with the exception that lengths of ICU and hospital stay and time from hospital discharge to outpatient assessment will be included as covariables in this phase. For the SPPB, TUG, 6-MWT, EQ-5D-5L, CFS, FACIT-F, SF-36 and additional recovery phase events, differences between the AKI-RRT survivors and the historical ICU survivor controls without AKI-RRT will be compared using t-test, Wilcoxon rank sum test, Mann-Whitney U test and χ2 test, as appropriate.
Metabolomic analysis: The metabolomic analysis will have no control group. The primary outcome of the metabolomic analysis, corresponding to aim 3, will be the correlation between changes in plasma and effluent amino acid levels measured during CRRT treatment in the ICU phase and both the MSKUS parameters obtained throughout the study and muscle strength measured in AKI-RRT survivors at hospital discharge and 1–3 months postdischarge. The primary analysis will be performed using a mixed effects model with ANOVA using Sidak’s multiple comparison test for paired samples to compare baseline to subsequent samples. Correlations with muscle changes based on MSKUS measurements at days 3 and 7 and correlations with muscle mass, strength and function at hospital discharge and at 1–3 months will be assessed with Pearson correlation test for continuous variables and Spearman’s r test for non-parametric data.
Ethics and dissemination
Research ethics approval
This protocol was approved by the University of Kentucky Office of Research Integrity Medical IRB, which serves as the single IRB for this multisite study according to National Institutes of Health single IRB Policy64 (IRB #71153; initial approval 7 June 2022; protocol version 2 dated 27 November 2022, approved 7 January 2023). Any further significant protocol revisions will be communicated to the IRB and BMJ Open and updated on the ClinicalTrials.gov registry.
Consent
Given the expectation that most AKI-RRT patients will be mechanically ventilated, consent will be obtained prior to enrolment from a legally authorised representative if necessary. Consent will be obtained by the local research team, which may include the site principal investigator, coinvestigators or research assistants. Patients will be identified based on discussion with nephrology consult teams regarding patients about to be initiated on CRRT. The patient or the patient’s legally authorised representative will undergo detailed consent and will be given a copy of the signed consent form (online supplemental material 2).
bmjopen-2023-072448supp002.pdf (1.1MB, pdf)
Confidentiality
Confidentiality of the data obtained from enrolled participants will be achieved by storing the data using REDCap data management to reduce the risk of accidental loss of confidentiality. Each patient will be assigned a unique research ID, which will be used to identify the REDCap record and the biospecimens in storage for each patient. Once all data are collected, the records will be deidentified by removing any identifying information including medical record numbers, names, and dates of birth and hospital admission.
Data access
The final deidentified dataset will be made fully accessible on reasonable request once the results are published.
Dissemination policy
We intend to disseminate results to participants, healthcare professionals, the public and other relevant groups via conference presentation and publication and without any publication restrictions. The final manuscript will be drafted by the primary investigators. We plan to grant public access to the full protocol, data collection forms, participant-level dataset and statistical code on reasonable request.
Supplementary Material
Footnotes
Twitter: @NephCrit_NM, @ch8anya, @FGonzalezSeguel, @KirbyMayerDPT
JPT and BRG contributed equally.
Contributors: The study was conceptualised by JPT, BRG, JAN and KPM. The methodology was developed and revised by JPT, BRG, CAP, FG-S, NJ, BMJ, YY, NG, HPI, LG, JAN and KPM. Resources for developing and carrying out the protocol were provided by JPT, BRG, CAP, FG-S, NJ, BMJ, YY, NG, HPI, JAN and KPM. JPT, BRG, JAN and KPM wrote the original draft manuscript. Funding for the study was obtained by JPT, BRG, NJ, BMJ, YY, JAN and KPM. All authors reviewed and edited this final draft. This manuscript and all subsequent publications stemming from this trial protocol will adhere to the authorship eligibility guidelines of the International Committee of Medical Journal Editors (ICMJE) and will not involve professional writers.
Funding: This work is supported by a Clinical and Translational Award (CTSA) Inter‐Institutional Pilot Project Award (U24TR002260 from the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS). JAN is supported by grants from the NIH National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), including R01DK128208, U01DK12998, and P30DK079337. KPM is supported by the NIH National Institute of Arthritis and Musculoskeletal and Skin Disease under award number K23-AR079583.
Disclaimer: The funder of the study had no role in study design and will have no role in the collection, management, analysis, and interpretation of data; writing of the final study report; and the decision to submit the report for publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Hoste EAJ, Bagshaw SM, Bellomo R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med 2015;41:1411–23. 10.1007/s00134-015-3934-7 [DOI] [PubMed] [Google Scholar]
- 2.Cerdá J, Liu KD, Cruz DN, et al. Promoting kidney function recovery in patients with AKI requiring RRT. Clin J Am Soc Nephrol 2015;10:1859–67. 10.2215/CJN.01170215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Group KDIGOKAKIW . KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2012;2:2–138. [Google Scholar]
- 4.Sparrow HG, Swan JT, Moore LW, et al. Disparate outcomes observed within kidney disease: improving global outcomes (KDIGO) acute kidney injury stage 1. Kidney Int 2019;95:905–13. 10.1016/j.kint.2018.11.030 [DOI] [PubMed] [Google Scholar]
- 5.Cho KC, Himmelfarb J, Paganini E, et al. Survival by dialysis modality in critically ill patients with acute kidney injury. Journal of the American Society of Nephrology 2006;17:3132–8. 10.1681/ASN.2006030268 [DOI] [PubMed] [Google Scholar]
- 6.Gameiro J, Marques F, Lopes JA. Long-term consequences of acute kidney injury: A narrative review. Clin Kidney J 2021;14:789–804. 10.1093/ckj/sfaa177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehta RL, Bouchard J, Soroko SB, et al. Sepsis as a cause and consequence of acute kidney injury: program to improve care in acute renal disease. Intensive Care Med 2011;37:241–8. 10.1007/s00134-010-2089-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Griffin BR, Teixeira JP, Ambruso S, et al. Stage 1 acute kidney injury is independently associated with infection following cardiac surgery. J Thorac Cardiovasc Surg 2021;161:1346–55. 10.1016/j.jtcvs.2019.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Formeck CL, Joyce EL, Fuhrman DY, et al. Association of acute kidney injury with subsequent sepsis in critically ill children. Pediatr Crit Care Med 2021;22:e58–66. 10.1097/PCC.0000000000002541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Formeck CL, Feldman R, Althouse AD, et al. n.d. Risk and timing of de novo sepsis in critically ill children following acute kidney injury. Kidney360:10.34067/KID.0005082022. 10.34067/KID.0005082022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang WJ, Chao C-T, Huang Y-C, et al. The impact of acute kidney injury with temporary dialysis on the risk of fracture. J Bone Miner Res 2014;29:676–84. 10.1002/jbmr.2061 [DOI] [PubMed] [Google Scholar]
- 12.Wu V-C, Wu P-C, Wu C-H, et al. The impact of acute kidney injury on the long-term risk of stroke. J Am Heart Assoc 2014;3:e000933. 10.1161/JAHA.114.000933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu P-C, Wu C-J, Lin C-J, et al. Long-term risk of upper gastrointestinal hemorrhage after advanced AKI. Clin J Am Soc Nephrol 2015;10:353–62. 10.2215/CJN.01240214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guerra C, Linde-Zwirble WT, Wunsch H. Risk factors for dementia after critical illness in elderly Medicare beneficiaries. Crit Care 2012;16:R233. 10.1186/cc11901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teixeira JP, Mayer KP, Griffin BR, et al. Intensive care unit-acquired weakness in patients with acute kidney injury: A contemporary review. Am J Kidney Dis 2023;81:336–51. 10.1053/j.ajkd.2022.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang XH, Mitch WE, Price SR. Pathophysiological mechanisms leading to muscle loss in chronic kidney disease. Nat Rev Nephrol 2022;18:138–52. 10.1038/s41581-021-00498-0 [DOI] [PubMed] [Google Scholar]
- 17.Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med 2014;371:287–8. 10.1056/NEJMc1406274 [DOI] [PubMed] [Google Scholar]
- 18.Latronico N, Herridge M, Hopkins RO, et al. The ICM research agenda on intensive care unit-acquired weakness. Intensive Care Med 2017;43:1270–81. 10.1007/s00134-017-4757-5 [DOI] [PubMed] [Google Scholar]
- 19.Hermans G, Van den Berghe G. Clinical review: intensive care unit acquired weakness. Crit Care 2015;19:274. 10.1186/s13054-015-0993-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koukourikos K, Tsaloglidou A, Kourkouta L. Muscle atrophy in intensive care unit patients. Acta Inform Med 2014;22:406–10. 10.5455/aim.2014.22.406-410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayer KP, Welle MM, Evans CG, et al. Muscle power is related to physical function in patients surviving acute respiratory failure: A prospective observational study. Am J Med Sci 2021;361:310–8. 10.1016/j.amjms.2020.09.018 [DOI] [PubMed] [Google Scholar]
- 22.Fiaccadori E, Regolisti G, Cabassi A. Specific nutritional problems in acute kidney injury, treated with non-dialysis and Dialytic modalities. NDT Plus 2010;3:1–7. 10.1093/ndtplus/sfp017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berg A, Norberg A, Martling C-R, et al. Glutamine Kinetics during intravenous Glutamine supplementation in ICU patients on continuous renal replacement therapy. Intensive Care Med 2007;33:660–6. 10.1007/s00134-007-0547-9 [DOI] [PubMed] [Google Scholar]
- 24.Druml W, Fischer M, Liebisch B, et al. Elimination of amino acids in renal failure. Am J Clin Nutr 1994;60:418–23. 10.1093/ajcn/60.3.418 [DOI] [PubMed] [Google Scholar]
- 25.Druml W. Nutritional management of acute renal failure. Am J Kidney Dis 2001;37:S89–94. 10.1053/ajkd.2001.20757 [DOI] [PubMed] [Google Scholar]
- 26.Oh WC, Mafrici B, Rigby M, et al. Micronutrient and amino acid losses during renal replacement therapy for acute kidney injury. Kidney Int Rep 2019;4:1094–108. 10.1016/j.ekir.2019.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ostermann M, Summers J, Lei K, et al. Micronutrients in critically ill patients with severe acute kidney injury – a prospective study. Sci Rep 2020;10. 10.1038/s41598-020-58115-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hermans G, De Jonghe B, Bruyninckx F, et al. Clinical review: critical illness polyneuropathy and myopathy. Crit Care 2008;12:238. 10.1186/cc7100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lambell KJ, Tierney AC, Wang JC, et al. Comparison of ultrasound-derived muscle thickness with computed tomography muscle cross-sectional area on admission to the intensive care unit: A pilot cross-sectional study. JPEN J Parenter Enteral Nutr 2021;45:136–45. 10.1002/jpen.1822 [DOI] [PubMed] [Google Scholar]
- 30.Looijaard WGPM, Molinger J, Weijs PJM. Measuring and monitoring lean body mass in critical illness. Curr Opin Crit Care 2018;24:241–7. 10.1097/MCC.0000000000000511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parry SM, El-Ansary D, Cartwright MS, et al. Ultrasonography in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J Crit Care 2015;30:S0883-9441(15)00332-9. 10.1016/j.jcrc.2015.05.024 [DOI] [PubMed] [Google Scholar]
- 32.Sarwal A, Parry SM, Berry MJ, et al. Interobserver reliability of quantitative muscle sonographic analysis in the critically ill population. J Ultrasound Med 2015;34:1191–200. 10.7863/ultra.34.7.1191 [DOI] [PubMed] [Google Scholar]
- 33.Strasser EM, Draskovits T, Praschak M, et al. Association between ultrasound measurements of muscle thickness, Pennation angle, Echogenicity and Skeletal muscle strength in the elderly. AGE (Dordr) 2013;35:2377–88. 10.1007/s11357-013-9517-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zaidman Cm, Wu JS, Wilder S. Minimal training is required to reliably perform quantitative ultrasound of muscle. Muscle Nerve 2014;50:124–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mayer KP, Dhar S, Cassity E, et al. Interrater reliability of muscle Ultrasonography image acquisition by physical therapists in patients who have or who survived critical illness. Phys Ther 2020;100:1701–11. 10.1093/ptj/pzaa068 [DOI] [PubMed] [Google Scholar]
- 36.Sabatino A, Regolisti G, Bozzoli L, et al. Reliability of bedside ultrasound for measurement of quadriceps muscle thickness in critically ill patients with acute kidney injury. Clinical Nutrition 2017;36:1710–5. 10.1016/j.clnu.2016.09.029 [DOI] [PubMed] [Google Scholar]
- 37.Inker LA, Eneanya ND, Coresh J, et al. New Creatinine- and cystatin C–Based equations to estimate GFR without race. N Engl J Med Overseas Ed 2021;385:1737–49. 10.1056/NEJMoa2102953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mayer KP, Thompson Bastin ML, Montgomery-Yates AA, et al. Acute skeletal muscle wasting and dysfunction predict physical disability at hospital discharge in patients with critical illness. Crit Care 2020;24. 10.1186/s13054-020-03355-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mayer KP, Ortiz-Soriano VM, Kalantar A, et al. Acute kidney injury contributes to worse physical and quality of life outcomes in survivors of critical illness. BMC Nephrol 2022;23:137. 10.1186/s12882-022-02749-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hodgson C, Needham D, Haines K, et al. Feasibility and inter-rater reliability of the ICU mobility scale. Heart Lung 2014;43:19–24. 10.1016/j.hrtlng.2013.11.003 [DOI] [PubMed] [Google Scholar]
- 41.Tipping CJ, Bailey MJ, Bellomo R, et al. The ICU mobility scale has construct and predictive validity and is responsive. A multicenter observational study. Ann Am Thorac Soc 2016;13:887–93. 10.1513/AnnalsATS.201510-717OC [DOI] [PubMed] [Google Scholar]
- 42.Hermans G, Clerckx B, Vanhullebusch T, et al. Interobserver agreement of medical research Council sum-score and Handgrip strength in the intensive care unit. Muscle Nerve 2012;45:18–25. 10.1002/mus.22219 [DOI] [PubMed] [Google Scholar]
- 43.Parry SM, Berney S, Granger CL, et al. A new two-tier strength assessment approach to the diagnosis of weakness in intensive care: an observational study. Crit Care 2015;19. 10.1186/s13054-015-0780-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vanpee G, Segers J, Van Mechelen H, et al. The interobserver agreement of handheld dynamometry for muscle strength assessment in critically ill patients. Crit Care Med 2011;39:1929–34. 10.1097/CCM.0b013e31821f050b [DOI] [PubMed] [Google Scholar]
- 45.Bakhru RN, Davidson JF, Bookstaver RE, et al. Physical function impairment in survivors of critical illness in an ICU recovery clinic. J Crit Care 2018;45:163–9. 10.1016/j.jcrc.2018.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Parry SM, Denehy L, Beach LJ, et al. Functional outcomes in ICU – what should we be using? - an observational study. Crit Care 2015;19. 10.1186/s13054-015-0829-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Elliott D, Denehy L, Berney S, et al. Assessing physical function and activity for survivors of a critical illness: A review of instruments. Aust Crit Care 2011;24:155–66. 10.1016/j.aucc.2011.05.002 [DOI] [PubMed] [Google Scholar]
- 48.Denehy L, Nordon-Craft A, Edbrooke L, et al. Outcome measures report different aspects of patient function three months following critical care. Intensive Care Med 2014;40:1862–9. 10.1007/s00134-014-3513-3 [DOI] [PubMed] [Google Scholar]
- 49.Connolly B. Describing and measuring recovery and rehabilitation after critical illness. Curr Opin Crit Care 2015;21:445–52. 10.1097/MCC.0000000000000233 [DOI] [PubMed] [Google Scholar]
- 50.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories . ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111–7. 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 51.Needham DM, Sepulveda KA, Dinglas VD, et al. Core outcome measures for clinical research in acute respiratory failure survivors. an international modified Delphi consensus study. Am J Respir Crit Care Med 2017;196:1122–30. 10.1164/rccm.201702-0372OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Parry SM, Nalamalapu SR, Nunna K, et al. Six-minute walk distance after critical illness: a systematic review and meta-analysis. J Intensive Care Med 2021;36:343–51. 10.1177/0885066619885838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cuthbertson BH, Roughton S, Jenkinson D, et al. Quality of life in the five years after intensive care: A cohort study. Crit Care 2010;14:R6. 10.1186/cc8848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ferrão C, Quintaneiro C, Camila C, et al. Evaluation of long-term outcomes of very old patients admitted to intensive care: Survival, functional status, quality of life, and quality-adjusted life-years. J Crit Care 2015;30:1150. 10.1016/j.jcrc.2015.05.005 [DOI] [PubMed] [Google Scholar]
- 56.Brummel NE, Bell SP, Girard TD, et al. Frailty and subsequent disability and mortality among patients with critical illness. Am J Respir Crit Care Med 2017;196:64–72. 10.1164/rccm.201605-0939OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Darvall JN, Greentree K, Braat MS, et al. Contributors to frailty in critical illness: multi-dimensional analysis of the clinical frailty scale. J Crit Care 2019;52:193–9. 10.1016/j.jcrc.2019.04.032 [DOI] [PubMed] [Google Scholar]
- 58.Shears M, Takaoka A, Rochwerg B, et al. Assessing frailty in the intensive care unit: a reliability and validity study. J Crit Care 2018;45:197–203. 10.1016/j.jcrc.2018.02.004 [DOI] [PubMed] [Google Scholar]
- 59.Neufeld KJ, Leoutsakos J-MS, Yan H, et al. Fatigue symptoms during the first year following ARDS. Chest 2020;158:999–1007. 10.1016/j.chest.2020.03.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Spadaro S, Capuzzo M, Valpiani G, et al. Fatigue in intensive care survivors one year after discharge. Health Qual Life Outcomes 2016;14:148. 10.1186/s12955-016-0554-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ware JE, Sherbourne CD. The mos 36-ltem short-form health survey (SF-36). Medical Care 1992;30:473–83. 10.1097/00005650-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 62.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (Redcap)--A Metadata-driven methodology and Workflow process for providing Translational research Informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vincent JL, Moreno R, Takala J. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. on behalf of the Working group on sepsis-related problems of the European Society of intensive care medicine. Intensive Care Med 1996;22:707–10. [DOI] [PubMed] [Google Scholar]
- 64.Single IRB for multi-site or cooperative research. n.d. Available: https://grants.nih.gov/policy/humansubjects/single-irb-policy-multi-site-research.htm
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-072448supp001.pdf (39.4KB, pdf)
bmjopen-2023-072448supp002.pdf (1.1MB, pdf)


